Allegheny County Medical Society


Allegheny County Medical Society
Allegheny County Medical Society
November 2025 / Vol.
Editorial
• Winter Nourishment
Deval (Reshma) Paranjpe, MD, MBA, FACS
Editorial
• War Stories 2.0
Richard H. Daffner, MD, FACR
Membership
• Q&A with Marissa TremogliBarkowski, MS4
ACMS News
• ACMS Distinguished Awards Recap
ACMS News
• ACMS Member Acknowledgements
ACMS News
• ACMS in Action - 2025 PAMED House of Delegates
ACMS News
• Foundation Grantees

ACMS News
• Specialty Group Updates
ACMS Staff: Nadine Popovich, Melanie Mayer and Haley Thon
Article
• ACIC Recap
Sara Hussey, MBA, CAE
Materia medica
• Donanemab-azbt (KisunlaTM) Lauren Fasth, PharmD; Madeline Dillen, BCPS PharmD; Julia Zheng, MD

2025
Executive Committee and Board of Directors
President
Keith T. Kanel, MD
President-elect
Kirsten D. Lin, MD
Secretary
Richard B. Hoffmaster, MD
Treasurer
William F. Coppula, MD
Board Chair
Raymond E. Pontzer, MD
Board of Directors
Term Expires 2025
Anuradha Anand, MD
Amber Elway, DO
Mark A. Goodman, MD
Elizabeth Ungerman, MD, MS
Alexander Yu, MD
Term Expires 2026
Michael M. Aziz, MD, MPH, FACOG
Michael W. Best, MD
Micah A. Jacobs, MD, FIDSA
Kevin G. Kotar, DO
Jody Leonardo, MD
Term Expires 2027:
David J. Deitrick, DO
Sharon L. Goldstein, MD
Prerna Mewawalla, MD
Raymond J. Pan, MD
Nicole F. Velez, MD
James Latronica, DO, DFASAM
Richard B. Hoffmaster, MD
Finance
William F. Coppula, MD
Nominating
Kirsten D. Lin, MD
Women’s Committee
Prerna Mewawalla, MD & Meilin Young, MD
Managing Editor
Sara C. Hussey, MBA, CAE
ACMS Executive Director shussey@acms.org
Medical Editor
Deval (Reshma) Paranjpe, MD reshma_paranjpe@hotmail.com
Bulletin Designer
Victoria Gricks victoria@thecorcorancollective.com
2025 Bulletin Editorial Board
Richard Daffner, MD, FACR
Robert Howland, MD
Anthony Kovatch, MD
Charles E. Mount, MD, FAAD
Alexandra Johnston, DO
John P. Williams, MD
Executive Director
Sara Hussey shussey@acms.org
Vice President - Member and Association Services
Nadine M. Popovich npopovich@acms.org
Manager - Member and Association Services
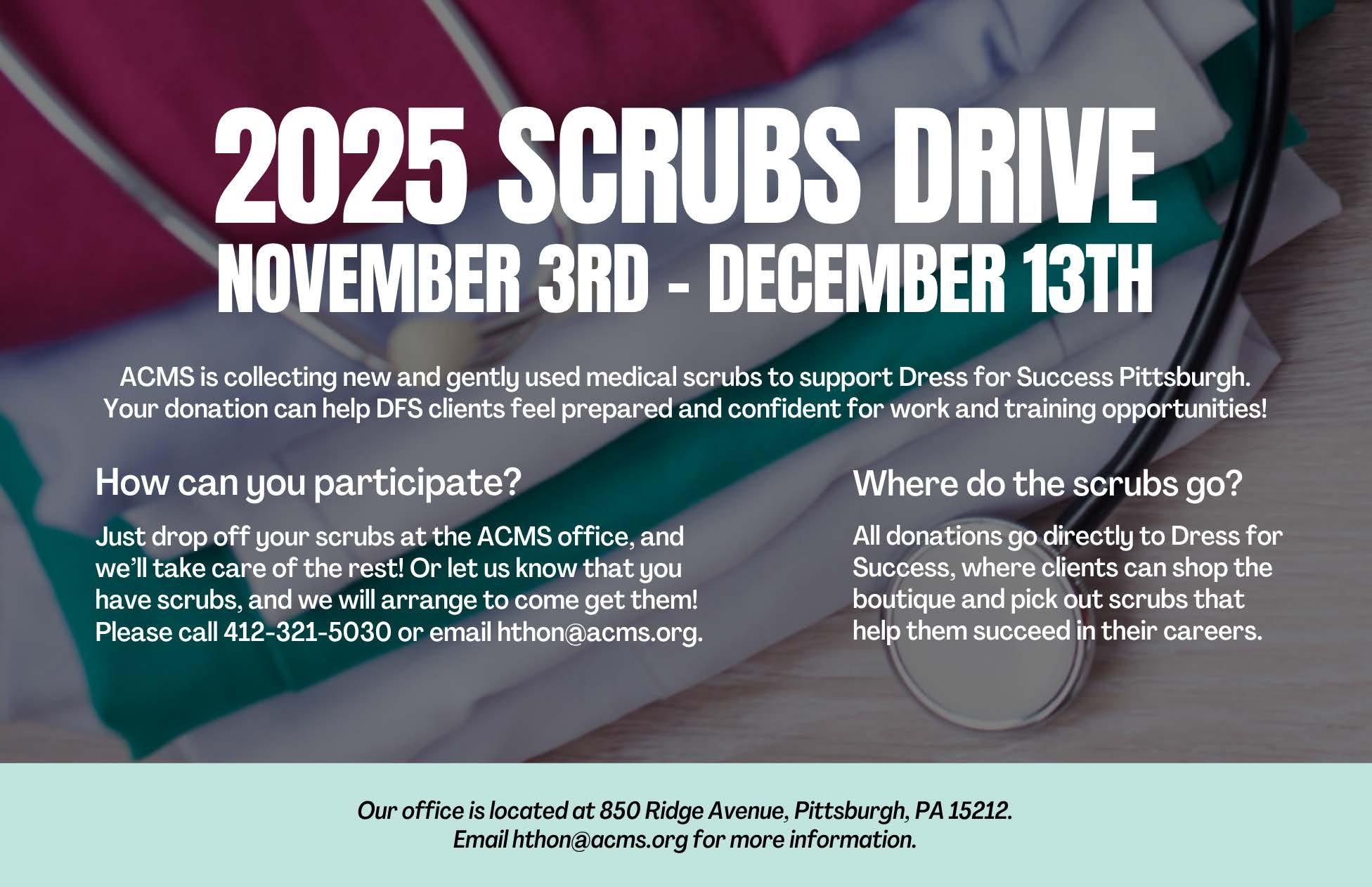
Haley Thon hthon@acms.org
Operations CoordinatorACMS & ACMS Foundation
Melanie Mayer mmayer@acms.org
Manager - Operations and Finance
Elizabeth Yurkovich eyurkovich@acms.org
Bulletin Designer Victoria Gricks victoria@thecorcorancollective.com
EDITORIAL/ADVERTISING
OFFICES: Bulletin of the Allegheny County Medical Society, 850 Ridge Avenue, Pittsburgh, PA 15212; (412) 321-5030; fax (412) 321-5323.
USPS #072920. PUBLISHER: Allegheny County Medical Society at above address.
The Bulletin of the Allegheny County Medical Society is presented as a report in accordance with ACMS Bylaws.
The Bulletin of the Allegheny County Medical Society welcomes contributions from readers, physicians, medical students, members of allied professions, spouses, etc. Items may be letters, informal clinical reports, editorials, or articles. Contributions are received with the understanding that they are not under simultaneous consideration by another publication.
Issued the third Saturday of each month. Deadline for submission of copy is the SECOND Monday preceding publication date. Periodical postage paid at Pittsburgh, PA.
Bulletin of the Allegheny County Medical Society reserves the right to edit all reader contributions for brevity, clarity and length as well as to reject any subject material submitted.
The opinions expressed in the Editorials and other opinion pieces are those of the writer and do not necessarily reflect the official policy of the Allegheny County Medical Society, the institution with which the author is affiliated, or the opinion of the Editorial Board. Advertisements do not imply sponsorship by or endorsement of the ACMS, except where noted.
Publisher reserves the right to exclude any advertisement which in its opinion does not conform to the standards of the publication. The acceptance of advertising in this publication in no way constitutes approval or endorsement of products or services by the Allegheny County Medical Society of any company or its products.
Annual subscriptions: $60
Advertising rates and information available by calling (412) 321-5030 or online at www.acms.org.
COPYRIGHT 2025: ALLEGHENY COUNTY MEDICAL SOCIETY POSTMASTER—Send address changes to: Bulletin of the Allegheny County Medical Society, 850 Ridge Avenue, Pittsburgh, PA 15212. ISSN: 0098-3772

By: Deval (Reshma) Paranjpe, MD, MBA, FACS
As the first flakes of snow begin to fall and we all think of hibernating for the next six months, take heart: there are new restaurants worthy enough for you to brave the elements and the dark and treat yourself and those you love to a lovely meal.
Poulet Bleu
517 Butler Street, Lawrenceville Dinner: Tue-Sat 5-10pm, closed Sun Mon.
First things first—Poulet Bleu has reopened, and this alone is cause for celebration. This lovely French bistro in the heart of Lawrenceville is a reliable, charming and warm place for date night, special occasions, or even a simple midweek treat when the week has been too much. Tuck into a divine bowl of cognac-laced French onion soup, enjoy a glorious dish of mussels with baguette, try the delicious Salade Lyonnaise, or have the star of the show, the luscious pate de campagne. For mains, you can try the variety of fine steaks with various sauces (Bordelaise, Bearnaise, Cognac Peppercorn or House) and fitting accompaniments (roasted carrots with crème fraiche and hazelnuts, or heavenly Aligot potatoes made with Comte and Gruyere cheeses, or truffle frites with aioli, or a Sicilian preparation of charred cauliflower with pine nuts, raisins and capers). If steak is not your pleasure, other mains include roast duck, lobster spaghetti, gnocchi Parisienne, halibut with champagne cream sauce, truffle-laden roast chicken, and a good old-fashioned bistro burger. Look for seasonal specials. Save room for
dessert—currently chocolate souffle, mousse, crème brulee and profiterole. Bon Appetit!
F and F Pizzeria
Beverly Road, Mt. Lebanon
Dinner: Monday (5-9pm) Wed/Thu (5 10pm). Fri (5-10pm), Sat (12-10pm), Sun (12-9pm)
Closed Tuesdays.
Two guys named Frank (Falcinelli and Castronovo) from Queens open a successful Italian restaurant in Brooklyn and then decide they want to start making pizza. Jimmy Kimmel hooks them up with mentor and pizza master Chris Bianco from Netflix’s Chef’s Table. Chad Robertson from Tartine Bakery in San Francisco teaches them how to ferment dough. Spoiler: their pizza is a big hit in Brooklyn. Plot twist: they open a location in Mt. Lebanon!
Through a partnership with Pittsburgh Winery owner Rob Mullin and Anthony Simasek, the Franks have opened a pizzeria restaurant in the former home of Bado’s in the Beverly Road plaza across from Iovino’s Restaurant. The lines have been halfway down the block but are sure to quiet down once everyone in Pittsburgh has sated their curiosity. The verdict is already in: the pizza is undeniably great. Fermented dough and organic ingredients including fresh cheese and the owners’ own olive oil make these New York style pies special. In addition to classic cheese, tomato and white pizza pies, look for guanciale and leek pie, wild mushroom pie, clam pie (red or white) and salumeria biellese pie. Also look out for the calzone and the
calzoagie (you read that right). Not in the mood for pizza? Try the beans and greens, arancini, fried calamari, vodka rigatoni al forno or shrimp with polenta.
Jillian’s Restaurant
400 Freeport Street, New Kensington Dinner: Wed-Sat 5-9 pm
Named to Pittsburgh Magazine’s 27 Best Restaurants list this year, this gem of a destination foodie magnet is helmed by chef Philip Call, formerly of Eleven, Meat and Potatoes, Andora and Willow. If you have a weakness for phenomenal duck-fat fried potatoes, this place was made for you. The offerings are farm fresh and hyper-local—all suppliers are from Pennsylvania and are listed with pride on the back of the menu. The menu changes weekly and dishes are inventive and joyful. The restaurant is named after co-owner and New Kensington native Jillian Call, who is an RN as well as a dining industry veteran who worked at DiAnoia’s in the past. Philip and Jillian are married and opened this eatery after initially opening a catering business together, so this restaurant is a true labor of love. Inquire about the monthly wine dinners, which are spectacular. Wednesdays and Thursdays are also take-out nights, when you can get a hearty upscale family-style to-go meal of either roast chicken or meatloaf paired with potato, vegetable, salad and focaccia for $55.
Enjoy and celebrate the season!















By: Richard H. Daffner, MD, FACR
I shared some of my War Stories from my service time in the US Air Force in a previous editorial1. Space limited the number of memories I could share at that time. And so, here are a few more. Those readers who have served in the military will be able to identify with them.
The General Wright-Patterson Air Force Base (Wright-Pat) was the home of several different commands, all of which were, not surprisingly, led by General Officers (Generals) as they were called. During the time of my service, we had 37 Generals, who lived in a very upscale part of the base known as the “Brick Yard” after their fancy brick houses. Generals were allowed house calls for medical issues so that they and their families wouldn’t have to wait in our Emergency Room following triage. I made several house calls, accompanied by a corpsman, who also served as my driver. Major General Joseph DeLuca was the exception and always accompanied one or more of his many children to our ER rather than take advantage of his privilege. (In the military there is a saying that “Rank has its privileges.”) He would always wait patiently for his turn. When I asked him why he hadn’t requested a house call he told me he had joined the Army Air Corps during World War II and had risen through the ranks and appreciated what the lower ranks were experiencing.
One cold, rainy night Gen. DeLuca brought in his youngest son, who was coughing and had a high fever. The general had hastily thrown on a raincoat that was devoid of any evidence of rank over his uniform. Our corpsman sitting
at the triage desk was smoking a cigar and was tipped back in his chair, with his feet on the desk reading a copy of Sports Illustrated. (The bad weather had significantly decreased the number of patients coming to the ER). After being ignored for several minutes, the general said, “Excuse me, corpsman. My child is very sick and needs to be seen by one of the doctors.”
Without removing his eyes from his magazine, the corpsman replied, “Just a minute, Mac. Let me finish this article.”
At that point, I saw the interaction and started toward the triage desk to bring in the general and his son. Before I got there, the general removed his coat. revealing the two stars on his epaulets. The corpsman almost fell out of his chair and swallowed his cigar. He gave the general a snappy salute just as I arrived and escorted the general and his sick child into one of our examining bays. X-rays revealed the boy had pneumonia and we admitted him for treatment. I apologized to the general for the boorish, unprofessional, and unmilitary behavior of the corpsman. Two days later the child responded to antibiotic treatment and was discharged. And the corpsman received orders transferring him to our air base in Thule, Greenland.
Throughout my medical career I have always admired the knowledge that many older nurses and technologists have gained. On rare occasions, their opinions conflicted with my own experiences. Colonel Carlson was the senior nurse responsible for managing the Emergency Room. She was well respected by all, particularly
the physicians. One night when she and I were on duty in the ER together, a father brought in his sixteen-yearold son who was vomiting and had abdominal pain. My physical exam showed tenderness over McBurney’s point in his right lower abdominal quadrant accompanied by a fever and an elevated white blood cell count.
The findings were “classic” for acute appendicitis. The problem, however, was that he had a McBurney scar, which his father told me was the result of an appendectomy three years earlier. I asked nurse Carlson to call a surgeon.
“That’s not necessary,” she said.
“It’s very necessary,” I insisted. “The boy has appendicitis.”
“He had his appendix removed three years ago,” she replied. “They don’t grow back.”
“Yes. He has it again. Now please call.”
She decided to pull rank. “Listen, Captain, I don’t think it’s necessary. I’ve never heard of anyone having appendicitis twice.”
And then, I pulled rank. “This is a medical decision. I’m the doctor and you’re the nurse. Now please call the surgeon.”
“Yes, sir,” she replied.
The surgeon arrived shortly thereafter and took the boy to the operating room. Once he opened the abdomen, he called the ER and asked me and nurse Carlson to come up to the OR. When we arrived, the surgeon showed us a classic example of appendicitis in an appendiceal stump.
Col. Carson was duly impressed. “I never thought that was possible,” she said.”
The surgeon told her that the
condition is not uncommon. I remarked that I had seen several cases as a medical student and as an intern.
On our way back to the ER I felt an apology was necessary after I had gone “full curmudgeon” on her. “Colonel, you outrank me. Outside this hospital you can order me to do anything you want,” I said. “But inside these walls I ask you to respect my medical judgement.”
“Yes, sir,” she replied. We never had any management issues after that.
“Choo-choo”
Senior Master Sergeant Brown was the chef for the officer’s dining room at the hospital. His nickname was “Choo-choo” stemming from his having learned his cooking skills while working on the New York Central railroad prior to joining the Air Force. I must admit, Choo-choo and his team produced some of the best hospital food I have ever had. Using his connections through his Master Sergeant’s network, it was not unusual for us to have Kansas City steaks or fresh Maine lobsters on our menu. But Choo-choo had another problem that was common in the military. He was an alcoholic, and frequently would come to work with a hangover, at best, or even highly intoxicated. One Monday morning Sgt. Hogue greeted me as I came in. “Doc,” he said, “I’ve got Choo-choo waiting to see you. You need to put him on ‘quarters’ (military jargon for assigning a sick day). He’s got a bad case of the flu.”
“You mean he’s drunk again?” I said.
“Well, sir, I’m not a doctor (wink wink).”
Sarge brought Choo-choo in, reeking of alcohol. My original assessment was correct. After a brief exam I said to him, “Well, Choo-choo, you’ve got a bad case of the “flu”. I’m putting you on quarters for two days. Go home, and drink lots of clear liquids – but not the kind that gave you the flu, and go to bed. I’ll see you on the third day.”
As Choo-choo staggered out the door, Sgt. Hogue gave me a piece of paper on which he had used a highlighter on one section. “You’re going to need this in about 20 minutes, doc.” Sure enough, 20 minutes later
my phone rang. It was Choo-choo’s supervisor, the Head Dietician, a nasty Lt. Colonel. “Captain Daffner, is Sgt. Brown drunk again?”
“No, ma’am. He’s got the flu,” I replied.
“Don’t give me that “flu’ BS.”
I picked up the sheet of paper that Sgt. Hogue had given me. “Colonel, are you familiar with Air Force Regulation xxxx?” I asked.
“What’s that?”
“Well,” I answered, “It’s part of the Public Health Code.” I read her the part that Hogue had highlighted. “The important part says, ‘Nobody with a communicable disease should handle food.’ In my book, flu is a communicable disease.”
“Goddam doctors,” she shouted into the phone before slamming it down. Where had I heard that before?
Several days later I found a box of frozen steaks on my desk. The accompanying note said, “Thanks doc. You save my stripes and my pension. Choo-choo.”
“Hey doc, how’d you like a flight jacket?” Sgt Hogue asked me one morning.
“Who do I have to kill to get one?” I replied. I had been told that flight jackets were reserved for pilots, air crews, and flight surgeons.
“Nothing like that,” Sarge said. He held out his clipboard, on which was a blank requisition form. “Just put your ‘John Hancock’ on this.”
“Don’t you think we can get in trouble for this?” I asked.
“Well, by the time you get your jacket, sir, merchandise will have changed hands at least seven times. That’s the way the system works here.” (Fans of the TV program MASH saw that in most episodes.)
I signed the form and promptly forgot about it. Three weeks later, when I came into my office there was a brandnew nylon flight jacket, complete with an official leather name tag sewn on that said, “Capt R H Daffner, USAF, MC”.
Just give me some ipecac Alcohol abuse is common in military
personnel. One evening, when I was on duty in our ED, a visiting Army sergeant came in complaining of abdominal pain. He told me he had “rum belly”, thought, at the time to be a mild case of pancreatitis. His examination and abdominal x-rays were negative. Then he asked me if we had any ipecac syrup. At the time (1969), as older physicians will remember, syrup of ipecac was recommended for inducing vomiting in children who had ingested suspected poison. (Now, medical studies have shown that ipecac is not effective in ridding the body of the poison.) “Doc,” he said, “Whenever I get this if I can just throw up, I’ll feel better. Just give me some ipecac” And so, having seen good results from using ipecac in children who had ingested various toxic substances, I gave him an adult dose. Usually, with children, vomiting occurs in 30 to 45 minutes following a dose of syrup of ipecac. After an hour, the sergeant had not vomited, and still had his abdominal pain. “Hey doc,” he said, “Sometimes I need another dose.” I consulted the “Merck Manual” which said I could safely give him another dose.
Another hour elapsed, again without any results from the ipecac. I was reluctant to try a third dose. While I was debating what to do, the sergeant walked up to me and said, “You know, doc, I feel a lot better. My belly pain is gone. Can you call me a cab to take me back to the barracks?” I called for the base taxi and watched the taillights diminish in size as the cab left our ER. Suddenly, the brake lights came on, and the cab quickly backed up to our door. The taxi driver raced into the ER and said, excitedly. “Hey, that guy who just got in is sick. He just puked all over the back of my cab!”
A taste for Jim Beam®
Chief Master Sergeant Kelly was the top enlisted man in charge of the General Medical Clinic. He often referred to the physicians working in the clinic as “His Doctors”. During my tour of duty at Wright-Patterson, he was promoted to oversee all the
enlisted personnel in the hospital with the title of Noncommissioned Officer in Charge (NCOIC). His best friend, Don, was the NCOIC in the personnel office of the base, who handled all the incoming reassignment orders. Don was also my next-door neighbor. Sgt. Kelly asked Don to notify him any time orders came through that would send any of “His Doctors” to Viet Nam. Whenever that happened, Sgt. Kelly would ask his friend to find a reason to change the orders so that the physician could stay at Wright-Patterson.
One day, Don came to my office and told me he had bad news and good news. Knowing where he worked, I correctly figured out what the bad news was. He handed me orders for me to go to Viet Nam. With my heart racing, I said, “So how can there be good news?”
“Well, doc,” he said, “You don’t have to go. You’re essential personnel. You’re the VD Control Officer for the base. Orders can be changed.”
“And what does it take to get them changed?” I asked.
“Well, I have a taste for Jim Beam.” Don, unfortunately, like many military personnel, was an alcoholic.
“I think I can handle that for you,” I said.
That noon, I went to the liquor store in the Officer’s Club and purchased a case of Jim Beam bourbon. I put a big red ribbon on the box and that evening I brought it next door. “Well, Don,” I said, “It looks like Christmas has come early. Now, you let me know when you need a refill.”
The next day, I received orders permanently assigning me to WrightPatterson. I never had to get Don any more Jim Beam.
Health inspection
Military protocol required all officers and enlisted persons to stand for semiannual uniform inspections as we changed from winter to summer uniforms in the Fall and again in the Spring when we changed back. The conscript physicians felt this was a step too far. One day, Chief Master Sergeant Kelly overheard a group of us
complaining about this and decided to do something about it for “His Doctors”. He told several of us to get our caps and meet him at the hospital motor pool. “Where are we going, sarge?” I asked.
“We’re going to the Officer’s Club to do a Health Inspection. They’re supposed to have one every six months and it’s been over a year since the last one,” Kelly said.
“What do we do?” one of the others asked.
“Don’t worry. I’ll tell you what to mark down. Just make sure if anyone questions you that you give them the “stink eye” and growl at them,” he said.
When we arrived at the club, Kelly handed each of us a clipboard on which was an inspection form. We headed to the kitchen, where, within ten minutes, Sgt. Kelly found a dozen violations, such as food being stored at improper temperatures and mouse droppings in the storage areas. We issued an order closing the club for 48 hours while the staff corrected the violations. Two days later we went back and “passed” the kitchen. Then we inspected the bathrooms, found another list of health violations, and closed them for another two days.
The 37 generals at Wright-Pat were upset that they couldn’t do their drinking at the Officer’s Club and complained to the Base Commander, who, understanding the system, knew that somebody at the hospital wanted something. He called the Hospital Commander and ordered him to find out why his staff had closed the club. Sgt. Kelly was summoned, and on being asked what was going on, told the Hospital Commander that the doctors didn’t want to stand for uniform inspection.
“Goddamn doctors,” he said. (Where had I heard that before?) “OK, no inspection. Just reopen the goddam club.”
And that was how the system worked.
References
1. Daffner RH. War Stories. ACMS Bulletin, Sep 2023, pp 8-10.
Dr. Daffner is a retired radiologist, who practiced at Allegheny General Hospital for over 30 years. He served in the US Air Force from 1968 to 1970.

Marissa Tremoglie-Barkowski is a fourth-year medical student at the University of Pittsburgh School of Medicine (UPSOM). A graduate of Saint Joseph’s University and a McNulty Scholar for Women in Science, Marissa worked as a Clinical Research Assistant at the Children’s Hospital of Philadelphia and then at Allegheny Health Network as a Clinical Research Coordinator before deciding to go to medical school. At UPSOM, Marissa served as President of the AMA/PAMED Chapter of Medical Students and has been an active member of ACMS for the past three and a half years, as Board Liaison for Medical Students and as a delegate to the Pennsylvania Medical Society HOD. She is currently applying for residency training in Internal Medicine–Pediatrics with the

goal of improving acute care outcomes across the lifespan through research, strengthening trust between academic medicine and the communities it serves, and continuing to elevate physician voices through active participation in organized medicine at the local and national levels.
Q: HOW DID YOU FIRST GET INVOLVED WITH THE ALLEGHENY COUNTY MEDICAL SOCIETY OR WHAT HAS YOUR OVERALL ENGAGEMENT BEEN WITH THE ACMS?
A: I first heard about ACMS during my husband's residency training in Pittsburgh (he now practices as a palliative care physician with Allegheny Health Network), but my decision to get involved came from my own experiences before medical school. Working in hospital-based clinical research, I saw how often the physician’s perspective was missing in conversations that shaped policy, hospital operations, and patient care delivery. That absence stayed with me. I joined ACMS because I thought it might offer a forum where physicians across specialties could engage in those discussions collectively, advocating not only for their patients, but for the conditions that make good medicine possible. Over the last several years, serving as the Board Liaison for Medical Students and a delegate to the PAMED House of Delegates have underscored
for me the importance of organized medicine in strengthening the physician voice and promoting thoughtful, evidence-informed advocacy.
Q: WHAT HAS BEEN THE MOST REWARDING ASPECT OF BEING AN ACMS MEMBER?
A: The most rewarding part of my time with ACMS has been watching medical students find their voice and recognize the influence they can have through organized medicine. I am proud of the work our Pitt team has done to double student participation during my time with the organization. Many of our students come to medicine with rich prior experiences, including doctoral training, Fulbright awards, and years of national service through programs such as AmeriCorps. As a non-traditional student myself, it has been inspiring to see them bring that expertise and perspective to ACMS and to use it to drive meaningful change for their patients and colleagues. I am equally proud of how ACMS physicians have listened to, mentored, and stood beside these students. I hope that by engaging students early, we are building the foundation for lifelong participation in organized medicine and ensuring that advocacy, for patients and the profession, remains a central part of how they practice. That spirit of mutual respect and shared purpose reflects what I value most about organized
medicine and the impact it can have for each other and communities we serve.
Q: ARE THERE ANY ACMS INITIATIVES (OR PAMED INITIATIVES) OR EVENTS THAT YOU ARE PARTICULARLY PASSIONATE ABOUT?
A: During my time with the organization, I have been thrilled to see the development of the Women in Healthcare initiative. My career has been advanced by women mentors at every turn, beginning with a scholarship for Women leaders in Science. Having the opportunity to collaborate and seek mentorship with other women physicians across health systems, specialties, and practice models has been both grounding and energizing. As a woman and, especially as mom in medicine, I have also seen the many subtle and overt ways sexism continues to appear even in 2025, and I find strength and encouragement in the solidarity and mentorship this community provides.
The other would be the advocacy task force. While nascent, I am excited to see the ways it continues to extend advocacy beyond the House of Delegates, where I have seen how powerful organized physician voices can be. The group is exploring how to bring that same energy into broader civic and public spaces where our voices are desperately needed. At a time when misinformation and political polarization threaten trust in medicine, ACMS has the opportunity to be that trusted voice in our communities on behalf of doctors across the county.


I am encouraged by its vision and by the recognition that physician voices belong in every conversation that shapes the health and well-being of our communities.
Q: WHAT DO YOU THINK IS THE BIGGEST CHALLENGE FACING HEALTHCARE TODAY?
A: I feel one of the greatest challenges facing healthcare today is the gradual dehumanization of both physicians and patients. As more physicians are employed by large health systems, many find themselves facing growing administrative demands, productivity pressures, and staffing shortages that leave little time for meaningful connection. It can be easy to feel replaceable, and the result is often burnout and moral injury that erode the joy and purpose of medicine. The rise of artificial intelligence adds a new layer of complexity. While these tools have enormous potential to support decision-making and reduce burden, they also risk pushing medicine toward greater efficiency at the expense of empathy. What remains irreplaceable is the human connection at the heart of our work: the ability to listen, to understand, and to translate deep expertise into compassionate care. Preserving that human dimension requires physician leadership at every level of healthcare
and within government, where consequential decisions about care are increasingly made. Safeguarding a meaningful, trusted physician voice in those arenas is essential to protecting both our profession and the humanity that underpins medical care. I believe this will be one of the defining responsibilities of my generation of physicians.
Q: WHY DO YOU THINK MEDICAL STUDENTS AND RESIDENTS SHOULD JOIN ACMS?
A: From an advocacy perspective, ACMS gives medical students and residents the space to make their voices heard on a broader stage- from instruction on how to write an oped, create an effective public health TikTok, opportunities to lobby state representatives, and the chance to vote in the House of Delegates where “what Doctors in Pennsylvania think” about current events and practice issues is decided. If advocacy is not your passion, ACMS is also a great space to network and increase your circle of mentors. There are so many more practice models then we are exposed to in medical school and residency and having a variety of mentors is helpful. Meeting people of various career stages and different specialties really broadens your perspective about the field and the path your own career might take. ACMS works hard to supports medical student and resident networking, education, and advocacyfrom re-designing events based on student and resident feedback to even paying our state dues. The final point I would make is this: if we do not participate in organized medicine- if we do not make our voice a collectivewe will continue to find ourselves even further siloed and with less power to act on behalf of our patients and our profession in the face of large selfinterested healthcare conglomerates and a world full of misinformation. Our generation of physicians is uniquely positioned to make a difference if we work together and speak as one.
This year's event, attended by over 300 guests, was a night filled with connection, gratitude, and the inspirational stories behind the work. The evening also recognized the leadership of the Allegheny County Medical Society itself, acknowledging those steering the organization's mission and initiatives. Enjoy these snapshots from a night filled with connection, gratitude, and the stories that inspire our work.


















What began as a $10,000 fundraising goal quickly grew to $30,000…and then $40,000. We’re proud to share that, with the help of our members, partners, and friends, Dr. Larry John’s campaign has officially reached—and exceeded— the $40,000 mark in support of the ACMS Physician Wellness Program. Additional contributions are still welcome. Simply scan the QR code to join in.


By: Sara Hussey, MBA, CAE – Executive Director of
On November 5, 2025, nearly 200 clinicians, public health officials, educators, and community partners gathered at the Regional Learning Alliance for the 20th Annual Allegheny County Immunization Coalition (ACIC) Conference. This milestone year—celebrating two decades of the coalition’s leadership—focused on a timely theme: “Uniting for Immunity: The Role of Vaccination in Public Health.”
The event underscored a truth that has become increasingly clear in recent years: vaccines alone don’t save lives— vaccination does. And vaccination depends on trust, communication, coordination, and system-level support. Throughout the day, speakers from Pitt, CMU, AHN, UPMC, and the Allegheny County Health Department examined not only where we’ve been, but where we must go as a community to strengthen vaccine confidence and preparedness.
Key Themes
The State of Vaccine Confidence
A major thread woven through the conference was the need to rebuild and sustain public trust in immunization. Presenters highlighted behavioral science strategies, narrative framing, and the importance of equipping health-care professionals to speak confidently and compassionately with patients. The takeaway was clear: trusted messengers—especially physicians—remain our most powerful tool against misinformation.
Emerging Diseases & Preparedness
Experts reviewed current infectious disease trends and shared approaches for turning epidemiologic data into
local action. Sessions also explored the value of root-cause analysis when preventable disease events occur— focusing less on blame and more on improving systems, communication pathways, and community readiness.
School-Based Vaccination Efforts
Speakers emphasized the critical role of schools in reaching families and boosting immunization rates. Discussions covered logistics, barriers to buy-in, and collaborative strategies that can be implemented across districts.
Policy, Systems, and Collaboration
Across panels and sessions, one message came through repeatedly: improving vaccination rates is a systems issue, not an individual burden. The coalition highlighted the importance of cross-sector collaboration—uniting health systems, primary care practices, pharmacists, school nurses, and community organizations.
× ACIC: Strengthening a Shared
This year’s conference was also an opportunity to highlight the growing collaboration between ACIC and the Allegheny County Medical Society. As ACMS expands its public health engagement, particularly through the ACMS Foundation and the Physician Wellness Program, the alignment with ACIC’s mission continues to strengthen.
ACMS President Dr. Keith Kanel and incoming President Dr. Kirsten Lin have both emphasized the importance of ACMS serving not only as an advocate for physicians, but also as a partner in community health. The ACIC Conference provided a platform for
those goals to come together—bridging clinical leadership with communitybased immunization work.
With 20 years of ACIC’s leadership behind us—and an ever-evolving public health landscape ahead—the work continues. The insights shared at this year’s conference point us toward a future where:
• Vaccine communication is rooted in compassion and clarity.
• School and community partnerships grow stronger and more coordinated.
• Local data guides meaningful, onthe-ground action.
• Physicians remain trusted leaders in promoting immunization across Allegheny County.
As ACMS deepens its connection with ACIC, we look forward to continued collaboration that strengthens vaccine education, expands community partnerships, and supports healthier outcomes for all.
1. ACIC Executive Committee Jennifer Kneuppers, Patrick Hussey, Jenny Bender, Raymond Pontzer, MD, Miriam Messick, Kristal Ross, Sarah Frost, Lauren Posterero
2. Jennifer Bender, MPH, BSN – ACIC Chair
3. Peter Salk, MD
4. Khlood Salman, MD
5. Michael Deem, PhD
6. Emily Scott, DO
7. John Alcorn, PhD
8. Amesh Adalja, MD








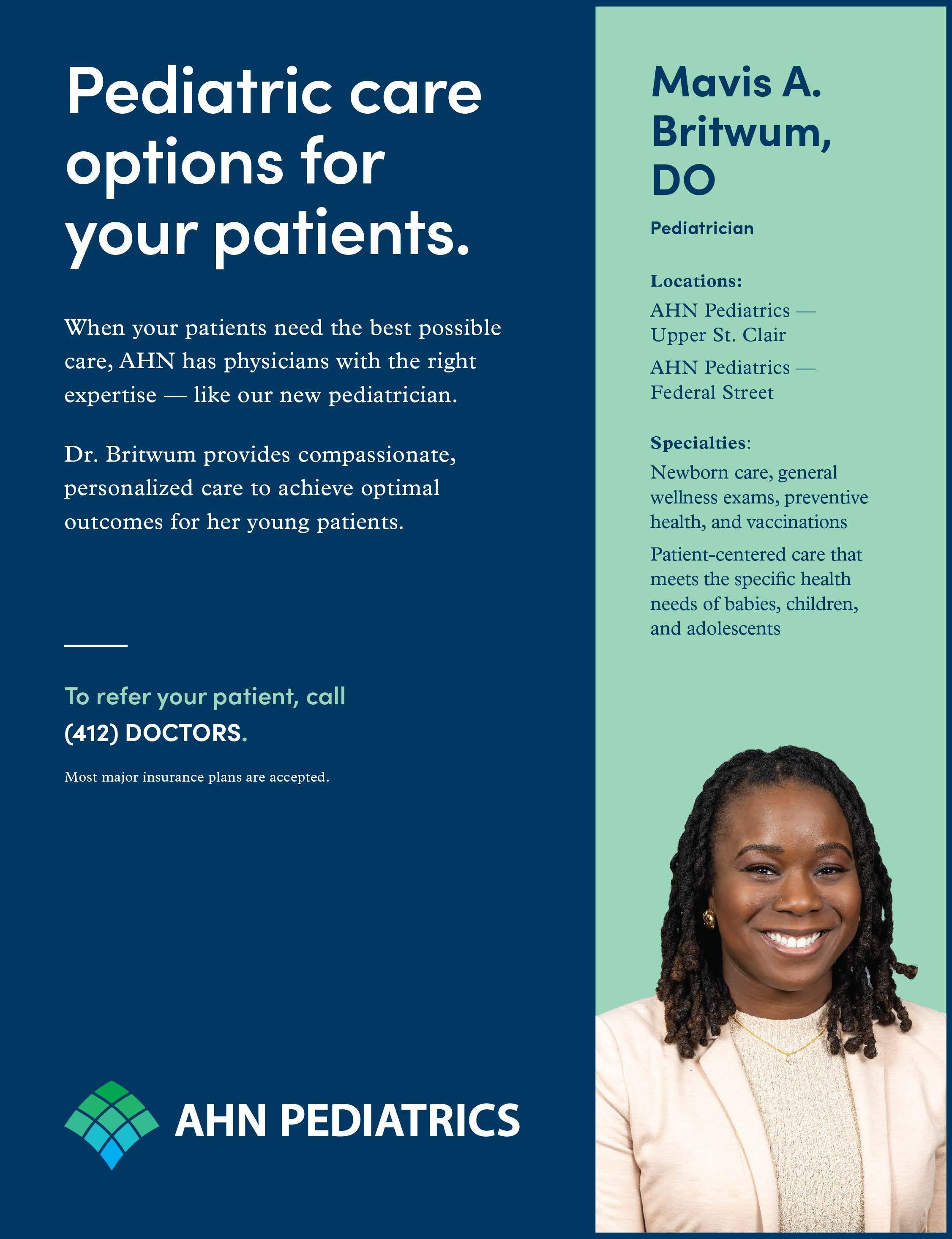
AHN Recognized for their Wellness Initiatives
Allegheny Health Network (AHN) was recently recognized nationally for its commitment to physician well-being, earning Gold-level distinction through the American Medical Association’s Joy in Medicine® program and being named a Wellbeing First Champion. AHN’s initiatives—including removing stigmatizing behavioral health questions from credentialing forms and appointing wellness officers across its clinical institutes—demonstrate strong leadership in supporting physician health and a sustainable medical workforce.
ACMS Board Members represent at TAPI Annual Meeting
At the Annual Scientific Meeting of the Tri-State Association of Physicians of Indian Origin (TAPI) in Warrendale, PA on October 11, 2025, ACMS President Keith T. Kanel, MD, delivered the keynote address, “How We Organize.” Dr. Kanel highlighted ACMS’s 2025 accomplishments in advocacy, physician wellness, and community
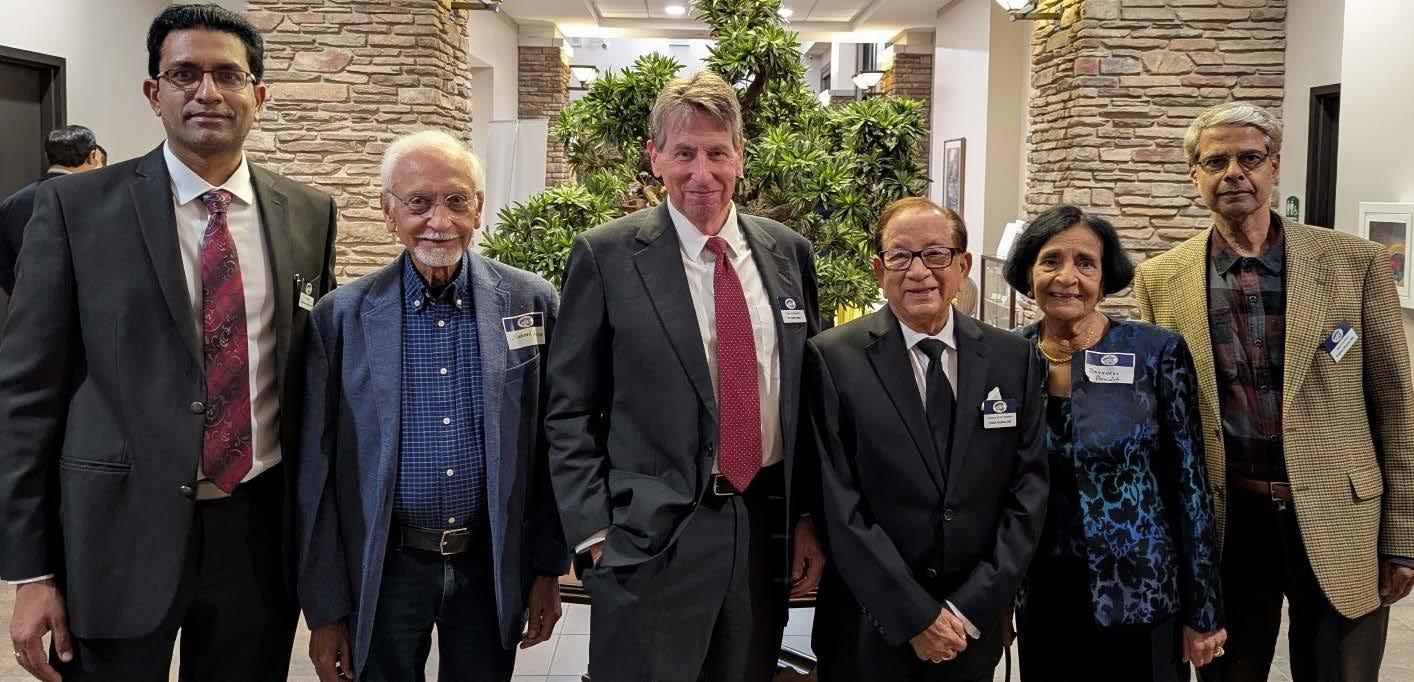
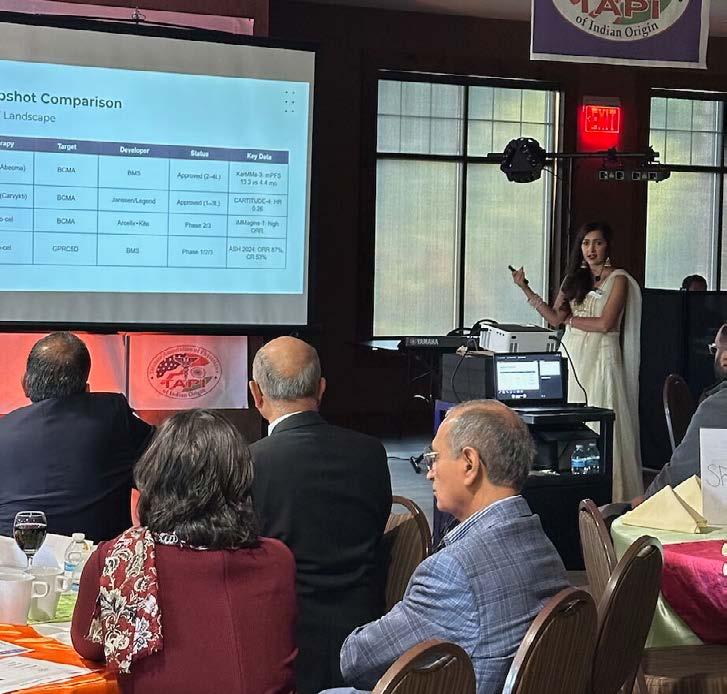
health, and encouraged TAPI physicians to strengthen their engagement with ACMS and PAMED. Also presenting at the conference was Prerna Mewawalla, MD, who shared updates on Bispecific Antibodies and CAR-T Therapy in Multiple Myeloma. The event brought together physicians from Pennsylvania, Ohio, and West Virginia for education, collaboration, and celebration— including a Diwali gathering that reflected TAPI’s commitment to
connection and community.
ACMS Members elected to PAMED Leadership positions
On behalf of the Allegheny County Medical Society (ACMS) we are delighted to extend our warmest congratulations to our members from Allegheny County who have been elected to leadership positions within the Pennsylvania Medical Society for 2025:
• Todd M. Hertzberg, MD, FACR –Speaker, House of Delegates
• Noah B. Rindos, MD – Obstetrics Gynecology Trustee
• Nicole Don – Medical Students Section Trustee
• Holly Appleberry, DO – AMA Alternate Delegate
• David J. Deitrick, DO – Judicial Council
Their election highlights the strength of our physician community, their dedication to advocacy and service, and the respect they’ve earned statewide. We’re proud to support their work and thank them for representing ACMS at the state level.
Learn more about the final resolutions at www.pamedsoc.org/HOD. November 2025



The 2025 PAMED House of Delegates (HOD) united Pennsylvania Medical Society members to shape healthcare policy and governance. Delegates focused on bylaws, public health, diversity, and advocacy for physicians and patients.Thank you to all ACMS members who participated, especially Dr. Michael Aziz, 2025 Delegation Chair, and Dr. Vint Blackburn, 2025 Delegation Vice-Chair.




Tucker Arensberg Lawyers Have Experience in All Major Healthcare Law Issues Including:
• Compliance
• Reimbursement
• Mergers & Acquisitions
• Peer Review and Credentialing for Physicians
• Employment Contracts and Restrictive Covenants
• Tax & Employment Benefits
For additional information contact any of the following attorneys at (412) 566-1212
• Mike Cassidy - Compliance; Contracts, Peer Review, Stark/AKS
• Jeremy Farrell - Labor & Employment and Commercial Litigation
• Adam Appleberry - Compliance, Credentialing, Reimbursement, and Physician Contracts
• Jerry Russo - Criminal Defense and Investigations
• Paul Welk - Mergers & Acquisitions







Visit our med law blog for the latest news and information for you and your medical practice: medlawblog.com

Congratulations to the 2025 - 2026 ACMS Foundation Grant Award recipients! This year, we are honored to support 15 remarkable organizations with a total of $245,000 in grants, furthering our commitment to advancing health, wellness, and access to medical care across Allegheny County. Through the ACMS Foundation—the charitable arm of the Allegheny County Medical Society—we strive to improve the lives of residents by supporting innovative programs, health services, and community-driven initiatives. Thank you to all recipients for your impactful work in our community.
Keep an eye out for the 2025 ACMS Foundation Annual Report and an opportunity to complete your year-end giving with a contribution to the ACMS Foundation.
To learn more about the ACMS Foundation visit: www.acms.org/foundation
Anchorpoint Counseling Ministry
Angels' Place, Inc.
Beverly's PGH
Familylinks
Global Links
Jeremiah's Place - Pittsburgh Relief Nursery
Light of Life Ministries, Inc.
Mary & Alexander Laughlin Children's Center
The Children's Institute Foundation
The Dragon's Den
The Neighborhood Resilience Project
North Hills Affordable Housing (HEARTH)
Our Giving Kitchen Pittsburgh
Roots of Faith
Sojourner House
Looking to boost your year-end giving? The ACMS Foundation could use your support! Scan this QR Code to donate via Qgiv or visit acms.org/acms-foundation/donate/
By: Lauren Fasth, PharmD; Madeline Dillen, BCPS PharmD; Julia Zheng, MD
Introduction
Donanemab-azbt (Kinsula™) is an amyloid beta-directed antibody indicated for the treatment of early Alzheimer’s Disease (AD), including minor neurocognitive impairment and mild major neurocognitive impairment due to AD.1,2 Kinsula™ is manufactured by Eli Lily and was FDA-approved on July 2, 2024 following the results of TRAILBLAZER-ALZ 2, a phase-3, randomized clinical trial.3 As a diseasemodifying therapy, donanemab decreases the presence of amyloid beta plaques, which are a hallmark neuronal abnormality seen in patients with AD.4
Safety
Like other amyloid beta-directed antibodies, including lecanemab (Leqembi™) and aducanumab (Aduhelm™; removed from the market in November 2024), donanemab has a boxed warning for amyloid related imaging abnormalities (ARIA).1 ARIA can involve edema and effusion of the brain (ARIA-E), caused by increased cerebrovascular permeability and extracellular volume, or hemorrhage (ARIA-H) from blood leakage into the tissue or subarachnoid space. Among patients in a 2023 phase-3 randomized control trial comparing the effects of donanemab to placebo, 24% of the treatment group experienced ARIA-E and 31.4% of the treatment group experienced ARIA-H (compared to 2.1% and 13.6% in the placebo group, respectively).3 While ARIA reactions typically are mild and self-resolving, severe adverse effects and death have been reported.1,3 While no deaths were associated with donanemab-induced ARIA reactions in the phase-2 trial,10
3 deaths associated with ARIA were identified in the phase-3 study and were deemed to be treatment-related.3 For lecanemab, ARIA-E occurred in 12.6% of treatment group participants, and ARIA-H occurred in 17.3% of the treatment group in CLARITY-AD, a phase-3 study (compared to 1.7% and 9% in the placebo group, respectively).5 None of the deaths among patients receiving lecanemab (n=7) in the phase-3 study were attributed to ARIA.5 Although lecanemab numerically has a lower incidence of ARIA compared to donanemab, a superiority trial comparing the two agents has not been performed.
Both ARIA-E and ARIA-H are associated with apolipoprotein E (ApoE) ɛ4 homozygous carriers, a genetic variation closely linked with the development of AD.4 Greater than 40% of patients in the donanemab group with an ARIA-E reaction were classified as homozygous carriers for ApoE; because of this, genetic testing for ApoE ɛ4 status is recommended prior to starting treatment with donanemab.3
In addition to ApoE ɛ4 homozygous carriers, concomitant antithrombotic medications (i.e., aspirin, antiplatelets, anticoagulants) have emerged as a potential risk factor for ARIA-H. Incidences of ARIA-H (30%) and intracerebral hemorrhage (0.6%) were slightly higher at 30 days among patients who received an antithrombotic (most commonly aspirin) compared to those who did not receive an antithrombotic (ARIA-H 29%, intracerebral hemorrhage 0.4%).1,3 Currently, there is insufficient evidence to provide recommendations
for appropriateness of continued use of antithrombotic medications with donanemab and additional research is needed to explore this correlation.
As listed in the boxed warning for donanemab, clinicians should consider ARIA-E in their differential for patients presenting with signs and symptoms of an ischemic stroke (i.e., headaches, dizziness, neurological deficits) due to the overlap in clinical presentation.1 This is pertinent in patients who may be candidates for thrombolytic therapy if the diagnosis is confirmed as an ischemic stroke. For these reasons, it is recommended that patients on donanemab carry information that they are taking this medication.1
Tolerability
The most common adverse effects associated with donanemab that emerged in the phase-3 trial include headache (14%), infusion-related reactions (8.7%), dizziness (6.2%), and arthralgias (5.7%).3 Infusion-related reactions were mild-moderate and occurred within the first 30 minutes of subsequent infusions. Similar adverse effects were experienced by participants in the phase-3 trial for lecanemab.5
Efficacy
The primary endpoint in the TRAILBLAZER-2 was change in the Integrated Alzheimer’s Disease Rating Scale (iADRS) from baseline to 76 weeks (iADREs scores range from 0-144, with lower scores indicating greater impairment).3 Previous research has defined a clinically meaningful difference as a point change ≥ 9 points.6 To elucidate the relationship between donanemab and disease
severity, participants were stratified into “low/medium tau” and “high tau” pathology groups determined by baseline PET imaging. Among those with lower disease burden (low/medium tau), iADRS decreased by 6.02 in the donanemab group (95% CI, -7.01 to -5.02) and 9.27 in the placebo group (95% CI, -10.23 to -8.31), representing a 35.1% slowing of AD progression.3 In the combined population (which included those with more advanced disease), iADRS decreased by 10.19 in the donanemab group (95% CI, -11.22 to -9.16) and 13.11 in the placebo group (95% CI, -14.10 to -12.13), representing a 22.3% slowing of AD progression.3
Improvement in iADRS score corresponded to an increase in amyloid clearance achieved at 76 weeks among groups. By study end, 80.1% (95% CI, 76.12 to 83.62) of participants in the low/medium tau group reached amyloid clearance, defined as <24.1 centiloids on PET scan.3 This achievement of amyloid clearance is below the pre-specified threshold for amyloid positivity of 30 centiloids seen in the literature; by this definition, the majority of participants in the low/ medium tau group reached a clinically normal amyloid level at 76 weeks.11 Participants in the combined group achieved 76.4% clearance, a lower degree of clearance compared to those with milder disease (95% CI, 72.87 to 79.57).3
The cost of treatment will vary based on insurance type and treatment duration (i.e., 6 months, 12 months, or 18 months), which will be determined by assessment of amyloid burden.1 Per the drug manufacturer Eli Lilly, the estimated cost of 18 months of treatment is $48,696 with current price-per-vial of $695.65.7 Donanemab coverage via Medicare is available through the National Coverage with Evidence Development, which grants drug coverage if patients participate in a registry. Eli Lilly offers the drug through the Lilly Cares Foundation and through a Savings Care Program, to
increase access to patients who meet pre-specified financial qualifications.7 Providers, patients, and caregivers will also need to consider the costs of MRIs, transportation to and from an infusion center, and care coordination required for treatment as these are not included in the drug price.
Prior to starting treatment, the presence of amyloid beta pathology should be confirmed. A baseline MRI and subsequent MRIs prior to 2nd, 3rd, 4th, and 7th infusions are required to monitor for ARIA.1 The recommended dosage of donanemab is 700 mg (requires two of the 350 mg/20 mL vials) as a 30-minute IV infusion administered by a health care professional every four weeks.1 Following the first three doses, the dose is increased to 1,400 mg every four weeks until a reduction in amyloid plaque burden on PET imaging is observed. No renal or hepatic dose adjustments are required.1 Currently, donanemab is formularyrestricted at many major health care institutions within Allegheny County, similar to lecanemab. Prescribers must participate in a CMS-facilitated registry and drug coverage must be confirmed prior to administration. Prescribers at other institutions should check their institutional protocols and restrictions prior to recommending initiation of donanemab.
Donanemab is a promising diseasemodifying agent for the treatment of mild cognitive impairment associated with AD. However, its high cost, imaging requirements, and risk of ARIA may be a barrier for implementation into general practice. As current practice guidelines do not include discussion of anti-amyloid antibodies, the decision to start donanemab would involve shared decision making with the patient, provider, and caregiver. Further research is needed to compare longterm outcomes of disease progression with donanemab compared to Eisai’s competitor product Leqembi™ (lecanemab-irmb).
The authors and reviewers have no conflicts of interest:
Dr. Lauren Fasth, PharmD is a PGY2 Pharmacy Resident in Geriatrics at UPMC St. Margaret and can be reached at fasthl@upmc.edu.
Dr. Madeline Dillen, PharmD, BCPS, is a Clinical Pharmacist at MetroHealth and can be reached at madeline.dillen@gmail.com.
Dr. Julia Zheng, MD is a geriatrician at Denver Health and can be reached at Julia.zheng@dhha.org.
Dr. Heather Sakely, PharmD, BCPS, BCGP, the Director of Ambulatory Pharmacy Services at UPMC and served as editor and mentor for this work and can be reached at kudiha@upmc.edu.
References:
1. Donanemab. Package Insert. Lilly Inc; 2024.
2. About Kisunla. Kisunla. Accessed September 24, 2024. https://kisunla.lilly.com/what-is-kisunla.
3. Sims JR, Zimmer JA, Evans CD, et al. Donanemab in Early Symptomatic Alzheimer Disease: The TRAILBLAZER-ALZ 2 Randomized Clinical Trial. JAMA 2023;330(6):512-527. DOI: 10.1001/jama.2023.13239.
4. Cummings J. Anti-Amyloid Monoclonal Antibodies are Transformative Treatments that Redefine Alzheimer's Disease Therapeutics. Drugs 2023;83(7):569-576. DOI: 10.1007/s40265-023-01858-9.
5. van Dyck CH, Swanson CJ, Aisen P, et al. Lecanemab in Early Alzheimer's Disease. N Engl J Med 2023;388(1):9-21. DOI: 10.1056/NEJMoa2212948.
6. Wessels AM, Rentz DM, Case M, Lauzon S, Sims JR. Integrated Alzheimer's Disease Rating Scale: Clinically meaningful change estimates. Alzheimers Dement (N Y) 2022;8(1):e12312. DOI: 10.1002/trc2.12312.
7. Lilly’s Kisunla (donanemab-azbt) Approved by the FDA for the Treatment of Early Symptomatic Alzheimer’s Disease. Lilly Investors. Accessed October 1, 2024. https://investor.lilly.com/news-releases/news-releasedetails/lillys-kisunlatm-donanemab-azbt-approved-fdatreatment-early.
8. Petersen RC, Lopez O, Armstrong MJ, et al. Practice guideline update summary: Mild cognitive impairment: Report of the Guideline Development, Dissemination, and Implementation Subcommittee of the ™ Neurology 2018;90(3):126-135. DOI: 10.1212/WNL.0000000000004826.
9. McKhann GM, Knopman DS, Chertkow H, et al. The diagnosis of dementia due to Alzheimer's disease: recommendations from the National Institute on AgingAlzheimer's Association workgroups on diagnostic guidelines for Alzheimer's disease. Alzheimers Dement 2011;7(3):263-9. DOI: 10.1016/j.jalz.2011.03.005.
10. Mintun MA, Lo AC, Duggan Evans C, et al. Donanemab in Early Alzheimer's Disease. N Engl J Med 2021;384(18):1691-1704. DOI: 10.1056/NEJMoa2100708.
11. Fleisher AS, Chen K, Liu X, et al. Using positron emission tomography and florbetapir F18 to image cortical amyloid in patients with mild cognitive impairment or dementia due to Alzheimer disease. Arch Neurol. 2011;68(11):1404-1411. doi:10.1001/archneurol.2011.150
By: Nadine Popovich, Melanie Mayer, and Haley Thon
Allegheny County Immunization Coalition (ACIC) — 2025-2026 ChairJenny Bender, MPH, BSN, RN, CIC: The Allegheny County Immunization Coalition invites physicians, public health professionals, and community partners to take part in two meaningful opportunities this season.
Volunteer: Support our mission at the Annual Thanksgiving Distribution Event – November 22, 2025
Join ACIC volunteers as we share vaccine education and connect with families across Allegheny County.
Engage: Learn more about our upcoming Quarterly Membership Meeting with Arvind Venkat, MD on December 11 by visiting www. immunizeallegheny.org
Together, we’re building a healthier, better-informed community—one event at a time.
American College of Surgeons Southwestern Pennsylvania Chapter (ACS-SWPA) — 2025 President – Richard Fortunato, DO, FACS:
The ACS Leadership & Advocacy Summit will be held February 28–March 3, 2026, at the Grand Hyatt Washington, DC. This in-person event helps ACS members strengthen leadership and advocacy skills through workshops, expert sessions, and congressional visits. The Leadership Summit focuses on communication and leadership development, while the Advocacy Summit centers on healthcare policy and surgeon advocacy. For details, visit Leadership and Advocacy Summit | ACS
For any questions or membership inquiries, please contact Haley Thon, Chapter Administrator, at 412-321-5030 x105 or hthon@acms.org
Pennsylvania Geriatric Society Western Division (PAGS-WD) — 2025 President - Heather Sakely, PharmD, BCPS, BCGP: Fall Program 2025
The Pennsylvania Geriatrics Society – Western Division hosted the 2025 Fall Program and Business Meeting on Wednesday, October 29, 2025, from 5:30 to 8:30 p.m. at the PNC Champions Club at Acrisure Stadium. The evening began with the Society’s final business meeting of the year, followed by an engaging panel discussion titled “From Impact to Action: Understanding Shifts in Medicare and Medicaid for Pennsylvanians.”
The program featured expert panelists Alex Bardakh, MPP, CAE, PLC, Senior Director of Advocacy and Strategic Partnerships for the Post-Acute and Long-Term Care Medical Association (PALTmed); Howard Degenholtz, PhD, Professor in the Department of Health Policy & Management at the University of Pittsburgh School of Public Health and the Center for Bioethics and Health Law; Chad Worz, PharmD, BCGP, Chief Executive of the American Society of Consultant Pharmacists and boardcertified geriatric pharmacist; and Rob Maher, BS, PharmD, President and Chief Operating Officer of the Pennsylvania Pharmacists Care Network, Administrative Pharmacist, and Assistant Professor of Pharmacy Practice at Duquesne University School of Pharmacy.
Together, the panel explored the implications of the July 2025 budget bill, which reshaped Medicare, Medicaid, and healthcare funding
across Pennsylvania. Topics included changes in post-acute, long-term, and home health services; access to care in rural and aging communities; and provider pay and reimbursement. Attendees gained valuable insight into the evolving healthcare landscape and connected with colleagues across the region.
2025 Geriatrics Teacher of the Year Award – Nominations Submission Deadline is December 15th
The Society is proud to announce that nominations are now being accepted for the 2025 Geriatrics Teacher of the Year Award. This prestigious annual honor recognizes two outstanding educators, one physician and one healthcare professional, who have shown exceptional commitment to advancing geriatrics education. Award recipients are individuals who have made a lasting impact on the training and development of future geriatric professionals and have significantly contributed to the growth of geriatrics education across the healthcare continuum. Full details, including eligibility requirements, selection criteria, and the nomination form, are available on the Society’s website at Pennsylvania Geriatrics Society - WD - Teacher of the Year.
Clinical Update 2026
Mark your calendars! The 2026 Annual Conference: Clinical Update in Geriatric Medicine will be held April 16–17 at the Sheraton Pittsburgh Hotel at Station Square. Further event details will be shared with members of the Society soon.
For any questions or to join the society, please contact Haley Thon, Chapter Administrator, at 412-321-5030
x105 or hthon@acms.org.
The Pittsburgh Ophthalmology Society (POS) — 2025 President - Laurie A. Roba, MD: Pittsburgh Ophthalmology Society: 2025-2026 Monthly Meeting Series Begins | November Monthly Meeting Highlights
The Pittsburgh Ophthalmology Society gathered on November 6 to welcome guest speaker Christopher Teng, MD, PhD, board-certified cataract and glaucoma specialist, and Professor and Chair of the Department of Ophthalmology and Visual Sciences. The meeting drew an exceptional turnout, with over 55 members in attendance — a strong showing that reflected great interest in the evening’s program.
Dr. Teng’s dynamic lectures captivated attendees with his engaging style and numerous references to the Pittsburgh area, creating a lively and locally inspired discussion. In addition to his presentation on microinvasive glaucoma surgery (MIGS), he delivered a thought-provoking non-clinical lecture titled “Business School Entrepreneurship Class 101.” In this session, Dr. Teng shared practical insights on how physicians can approach entrepreneurship, offering a framework for understanding the processes entrepreneurs follow to build consumer product companies. Attendees gained perspective on the risks associated with product-focused ventures compared to technologyand service-based models, strategies for achieving profitability through direct-to-consumer channels, and the importance of balancing customer acquisition costs with lifetime customer value.
As an entrepreneur himself, Dr. Teng brought an embroidered black-and-gold “Eye Surgeon” hat, which was raffled off during the meeting — a fitting tribute to the city of Pittsburgh. Daniel Buerger, MD, FACS, was the lucky winner of the prize.
In addition, John Gote, MD, a secondyear ophthalmology resident at the

University of Pittsburgh, presented a clinical case for review and commentary by Dr. Teng, fostering an excellent exchange of clinical insight.
The Society extends special thanks to Ken Cheng, MD, for coordinating Dr. Teng’s visit, and to our meeting sponsors — Alcon, Glaukos, and Sight Sciences — for their generous support. Member Acknowledgement
The Pennsylvania Academy of Ophthalmology (PAO) has been honored with the 2025 Star Award by the American Academy of Ophthalmology. This prestigious award recognizes ophthalmology societies for their exceptional programs and initiatives. Presented by the Academy's Secretariat for State Affairs, the Star Award celebrates outstanding efforts in areas such as membership development, public information, and advocacy.
Sharon Taylor, MD, FACS, a key leader of the initiative, dedicated significant time and effort to advancing Pediatric Medicaid Advocacy in Pennsylvania. In recognition of her commitment, Donald Morris, DO, President of the Pennsylvania Academy of Ophthalmology, proudly presented Dr. Taylor with the award plaque during the
POS business meeting.
The Society will reconvene on December 11 to welcome Nitish Mehta, MD, Clinical Assistant Professor of Vitreoretinal Surgery, Department of Ophthalmology, NYU Langone Health, New York. Members may register for the meeting beginning November 20 at www.pghoph.org.