@aestheticsgroup
@aestheticsjournaluk
Aesthetics
aestheticsjournal.com
Retrobulbar Injections in Filler-related Vision Loss Miss Rachna Murthy and Professor Jonathan Roos explore the emergency management of filler-induced vision loss Modern hyaluronic acid (HA) based dermal fillers have the power to change lives. Their popularity has grown,1 and with it the concern around complications.2 Although exceedingly rare, none is perhaps more feared than the onset of vision loss after an injection.2 Not surprisingly, a brief internet search will find many courses offering training in retrobulbar injection with hyaluronidase – the enzyme that can break down HA. However, is there evidence to suggest that it works? This article explains the latest evidence for the emergency management of filler-induced vision loss, why retrobulbar injections could compound the injury and why this approach is best avoided.
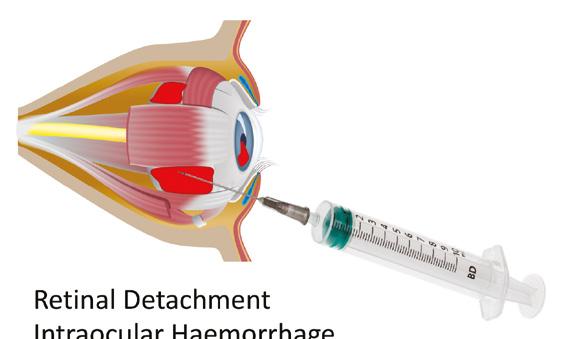
eye). Haemorrhages behind the eye can cause further damage to nerves and muscles and a painful compartment syndrome. Introduction of infection can spread back into the cavernous sinus with devastating consequences. In fact, there is even danger to the opposite unaffected eye; ocular trauma can reveal antigens normally hidden from the immune system and cause an autoimmune disease against the previously healthy eye.4 When blindness in one eye becomes blindness in both eyes, medicolegal questions will arise – particularly if the clinician is inexperienced in the technique.
Basic research evidence for retrobulbar hyaluronidase Understanding retrobulbar injections A retrobulbar hyaluronidase injection is often advocated as an emergency treatment following blindness caused by HA dermal filler injection. It involves passing a sharp 23 gauge bevelled needle behind the globe.3 It is passed either through skin or conjunctiva at the outer third of the orbit and advanced straight back for 15mm and parallel to the floor, before changing to point upwards and inwards, passing through into the muscle cone behind the eye. As shown in the larger central image in Figure 1, the globe itself is 23.5mm and the orbit 4.8mm – so a needle length of 38mm (red) is more likely to hit the optic nerve than 24mm (green). However, optic nerve damage is not the only potential danger. Needles can penetrate the globe, causing glaucoma, retinal detachment and eventual phthisis (an unsightly shrunken
Retinal detachment intraocular haemorrhage
Iris trauma cataract
Given that there are courses available for teaching retrobulbar technique, one would have thought that there would be strong preclinical evidence for its use. Indeed, HA can be digested when a ligated cadaveric blood vessel filled with HA is suspended in a bath of hyaluronidase overnight.5 But when this experiment was repeated with living blood vessels the enzyme could not cross the wall into the lumen.6 The orbit and vasculature also have inhibitors of hyaluronidase activity which will deactivate any injected enzyme.7,8 Furthermore, the central retinal artery, which is blocked with filler in filler-related vision loss, enters inside the optic nerve and is covered with dura, pia and arachnoid mater layers preventing passive enzyme ingress.9,10 Despite the pre-clinical improbability – could retrobulbar hyaluronidase still work clinically?
Damage to optic nerve
Corneal opacity pthisis bulbi
Retrobulbar haemorrhage damage to muscles
Figure 1: Retrobulbar injections should be performed with a needle not of excessive length (centre image) but can nevertheless cause a myriad of complications to both internal and extraocular contents.
Reproduced from Aesthetics | Volume 8/Issue 8 - July 2021