THE PRACTICE MANAGER






AAPM’s Professional Development Program supports and promotes members’ personal and professional growth through a system of:

CORE PRINCIPLES
QUALIFICATIONS CERTIFICATION CONTINUING PROFESSIONAL DEVELOPMENT
AAPM representation on government and industry advisory groups.
HR ADVISORY SERVICE
Comprehensive HR support and advice through telephone, email and website resources and templates.
MEMBER ASSISTANCE PROGRAM
Confidential assistance to support health and wellbeing of members.
PULSE+IT SUBSCRIPTION
Asia Pacific’s eHealth and Health IT digital platform.
MEMBERSHIP BADGE
Recognition of AAPM membership.
THE PRACTICE SPACE
Dedicated fortnightly eNewsletter providing industry updates and helpful advice.
PRACTICE MANAGER JOURNAL
AAPM’s national journal, delivered electronically to members each quarter.
Access to AAPM’s Educare program at member rates. Includes face-to-face events and a series of webinars.
Premier annual conference for Practice Management at member rates.
NETWORKING MEETINGS
Share knowledge and information. Connect with, and support your peers.
Self-guided learning through Practice Management topics.
Expand your skills through AAPM funded scholarships for selected Practice Management courses delivered though UNE Partnerships.
PRACTICE MANAGER OF THE YEAR AWARDS
Prestigious state and national awards recognise and reward a Practice Manager for their contribution to the profession of Practice Management.
Recognition of years of experience and skill development in the profession of Practice Management.
FELLOWSHIP
A prestigious honour in recognition of significant commitment and contribution to the profession of Practice Management.
Exclusive access to resources, discounts and benefits from industry partners.
DEDICATED ONLINE MEMBERS FORUM
Dedicated and exclusive memberonly forum to share ideas, insights, information and support.
AMBASSADORS
Support and assistance from experienced and highly qualified Practice Managers.
WEBSITE ACCESS
Access latest news, industry information, and member-only resources.


As we reflect on the start of this year, I am pleased to share that we have already made great strides in advancing our educational opportunities for the year ahead. Thanks to the unwavering support of our members, we can offer a wide range of initiatives that will continue to help us grow professionally and foster deeper connections within our practice management community.
I would also like to take a moment to express our thanks to our partners, including the Australian Government, Department of Health and Aged Care, for their continued support in making these opportunities possible. Their commitment to helping us enhance the skills and knowledge of our members plays a crucial role in the ongoing success of our association. Together, we are building a stronger, more informed community that is
equipped to navigate the evolving challenges and opportunities in healthcare.
As your President, I want to emphasise the importance of completing the member survey that was emailed to you recently. Your feedback is crucial and will directly shape the direction of the Board's upcoming strategic planning day. Each and every member’s voice matters, and your responses will help the Board understand your priorities, concerns, and aspirations for the future of our association. Strategic planning is crucial for the growth and effectiveness of AAPM. It enables us to set clear goals, allocate resources effectively, and address challenges proactively. By engaging in this process, we ensure that our association remains relevant, resilient, and responsive to the ever-changing healthcare
landscape. Your participation in this survey is an essential step toward building a stronger, more united future for all of us.
Thank you once again for your support, and I look forward to what we can achieve together this year.

We have started 2025 with a refreshed energy and looking forward to delivering a series of activities for members and the greater Practice Management community this year.
The Educare 2025 series dates have been released and we hope to see as many of you there as possible. We will also be hosting the Reception/Administration Educare Series in each location again. We are delighted to deliver this series of education for the full practice team. Make sure the dates are in your diary.
By now you would have seen our updated website. We now have a more contemporary site, with the same features as before, with capability for more features! The most important thing is to ensure our members are able to familiarise themselves with the website now, then we can add further features in the future.
A new feature in the membership portal is a Digital Membership Card. This replaces the former plastic cards. Another great feature is the automatic calendar invite when you register for an event. We hope you find the new look easy to navigate and enjoy some of these features.
While we are always looking for ways to increase benefits and activities for our members, I would
like to thank the continued support of our national partners. These organisations may be able to assist you in your day-to-day work, and provide support or direction. Please visit the Partners page on the website, or reach out if you would like a personal introduction. We value and appreciate their contribution to AAPM and the profession.
October this year, will be the tenth anniversary of the first AAPM and PMAANZ joint conference. We are so excited to be collaborating again and bringing our two organisations together in Melbourne. The Conference Committee will be working hard to deliver a program filled with latest industry updates, dynamic plenary presentations and concurrent sessions on the core principles of Practice Management.
Along with the education will be the social activities to network and enjoy the experience. There is something for everyone!
AAPM continues to work closely with the Australian Government, Department of Health and Aged Care. AAPM is represented on several committess, working groups and meetings, that enables the voice of Practice Management to be heard. This year AAPM and Services Australia are collaborating to deliver a dedicated series "MyMedicare: Ask Me Anything" series. These
interactive webinars will enable updates along with practical tips.
There is a lot happening in 2025 and we hope that you will be able to enjoy the updates and deliverables as they unfold.

MIRANDA GRACE CHIEF EXECUTIVE OFFICER



CUTCHER & NEALE
Understanding tax deductions, especially around travel, is essential for managing your finances and reducing your tax bill, but knowing what you can claim – and what you can’t – can be tricky. Failing to claim eligible expenses could mean missing out on significant tax savings each year.
Let’s take a closer look at the basics along with some practical examples.
For most employees, including many doctors and Practice Managers, travel between home and work is not deductible. However, there are specific scenarios where travel expenses may qualify for deductions, such as:
◦ Travel Between Work Locations: If you travel between two or more work locations on the same day, this travel is deductible.
For example, Mrs. Smith, who works across two clinics, can claim the kilometres between her morning shift at Clinic A and her afternoon shift at clinic B.
◦ Work-Related Duties During Travel: When travel involves performing employment-related tasks, such as visiting patients or attending multiple clinics, these expenses may qualify.
Imagine Dr. Jones, who performs house calls between shifts at the hospital. The trips between the hospital and patient homes can be claimed.
◦ Seminars and Training: Travel expenses for attending workrelated seminars, conferences, and continuing education are generally deductible if the primary purpose is professional development.
Mr. Patel flew to Sydney to attend a Practice Manager conference and stayed for two nights. These flights and accommodation expenses are deductible because they directly relate to his work.
◦ Special Circumstances: For roles that require transporting bulky work equipment, this travel may be deductible.
Dr. Taylor frequently carries a portable ultrasound machine between hospitals. They can claim these journeys provided they meet the bulky equipment criteria.
While logbooks are more applicable to sole traders and contractors, employed medical professionals can still benefit from understanding motor vehicle deductions. If your employer provides a travel allowance, you can claim deductions for expenses above this amount.
For instance, Mr. Lee receives a small allowance for his travel between rural clinics, but he incurs higher fuel costs due to the distances. He can claim the excess expenses.
Medical professionals and Practice Managers should always consider other deductible items, such as professional memberships, medical journals, home office expenses, insurance premiums and uniforms.
For example, Dr. Adams, who maintains a subscription to the Journal of Clinical Medicine and purchases his own scrubs, ensures these are included in his tax return. If Dr. Adams also undertakes telehealth consultations from home, a portion of his internet and electricity expenses may be deductible.

To streamline your processes and maximise your tax savings, it’s important to use smart strategies and stay informed. Here are some practical tips to help you tackle your tax like a pro:
◦ Keep detailed records of workrelated expenses.
◦ Consult with a tax professional to ensure you’re claiming all eligible deductions.
◦ Keep an eye on tax law changes.
◦ Use a digital tool or spreadsheet to track expenses throughout the year rather than scrambling at tax time.
Ms. Murphy, who uses a digital app to log her mileage and keeps all receipts for work-related purchases, finds tax time much easier and ensures she doesn’t miss any deductions.
Navigating tax deductions may seem complex, but with the right approach, it becomes an opportunity to reduce your tax burden. Every dollar you claim legally is money that stays in your business – money that can be reinvested in your practice, used for further education, or even set aside for the future.
Tax laws can be tricky, but you don’t have to go it alone. If you have questions or need guidance, feel free to reach out to a member of the Specialist Medical Services team at Cutcher & Neale.

STUART CHAN PARTNER, CUTCHER & NEALE SPECIALIST MEDICAL SERVICES

End of financial year comes around sooner than you think. Is your practice prepared?
Tax time isn’t just about getting through 30 June unscathed – it’s about setting your practice up for long-term success.
We can help you keep more of your hard-earned by:
Starting early and getting a solid plan in place
Avoiding common mistakes that can cost you
Maximising your deductions and minimising your tax bill
Don’t miss out on what’s rightfully yours this year.
As the national partner of AAPM, members benefit from complimentary, obligation-free consultations with our advisors. Contact us today.
Learn more about our services for AAPM members


I-MED e-Referrals are a proactive solution to help you
• save time
• reduce patient/clinical risks
• improve communication
Take back your time from the burden of administrative tasks – faxing, attending to phone calls about lost referrals, and completing excess paperwork.
You can easily integrate I-MED e-Referrals to both Best Practice and Medical Director software today.
I-MED e-Referrals also seamlessly integrate with our online booking portal, I-MED’s unique feature that allows your patients to book their own appointments online 24/7.
Contact our team about streamlining your practice today:
• call us on 1300 147 852
• email Key Account Specialist at kas@i-med.com.au

Many health practitioners understand that patients have the right to access their records. However, the full scope of their obligations including under the Australian Privacy Principles (APPs), as outlined in the Privacy Act 1988 (Cth), is often less familiar.
In the recent case of AGX and AGY (Privacy) [2024] AlCmr 16, the Information Commissioner (the Commissioner) considered the obligations imposed by APP 12, which concerns an individual’s right to access their personal information, with certain exceptions specified in APP 12.3.
This case highlights several key points:
◦ A patient’s prior access to their personal information through other means does not absolve the practitioner from the obligation to provide access.
◦ Health practitioners must grant access to health information, unless there are valid grounds for refusal, as detailed in APP 12.3, which should be considered carefully, before denying a request.
◦ Fees for accessing personal information, must be reasonable and proportionate.
The patient, AGX, had consulted a specialist health care practitioner AGY (‘the practitioner’) on one occasion. Six-months later the patient requested a copy of their full medical file. The practitioner’s administrative assistant responded by saying that the file had been reviewed, and only an imaging report and a letter to the GP had been identified, both of which the patient had been given by the GP, and therefore they had nothing further to provide.
A second request was made by the patient who alleged that further information was held by the practitioner. Dissatisfied with the practitioner’s failure to respond to the second request, the patient complained to the Office of the Australian Information Commissioner (OAIC).
In defending the complaint to the OAIC, the practitioner sought to assert that the patient already had copies of information held, and therefore the request was frivolous or vexatious. In support of this, it was also stated that the patient had harassed staff and had in fact wasted time in attending on the practitioner in the first place, as they were seeking treatment which the practitioner could not provide.
The OAIC’s investigation identified two additional records held by the practitioner that had not previously
been provided to the patient. The practitioner had sought to charge the patient $440 for time taken to research the APPs and respond to the OAIC. In correspondence to the patient, the practitioner stated that if the patient paid the invoice, they would provide access to the personal information.
In determining whether the practitioner had breached APP 12, the Commissioner considered whether the patient’s request was vexatious or frivolous, and therefore the practitioner had grounds to refuse the access request.
The Commissioner ultimately dismissed the practitioner’s argument, referring to the APP Guidelines which state that there must be a clear and convincing basis to decide that an access request is frivolous or vexatious, and causing inconvenience or irritation is not sufficient.
It was found that although the patient may have already obtained copies of some of their personal information from other sources, this did not discharge the practitioner from the obligation to provide access to the personal information it held.
Given that two further records were found to exist during the investigation, the Commissioner

found it was not unreasonable for the patient to dispute the practitioner’s decision to refuse to provide access or make a second access request.
The Commissioner declared that the practitioner had interfered with the privacy of the patient by refusing to give the patient access to their personal information, and by attempting to charge the patient an excessive fee.
The fact a patient has accessed personal information held by a health care practitioner in some other way, does not in itself discharge the practitioner from the obligation to provide access to the personal information. Such a request will not necessarily be considered vexatious or frivolous.
When an access request is received, it is important to undertake a thorough review to identify all records held containing personal information, which may be captured by the request.
Fees charged to a patient for access to their personal information, must be reasonable and proportionate. Generally, your fee should be set based on the real cost of copying and providing records. Such costs may include the actual cost of staff retrieving, reproducing and sending the personal information, and the costs of postage.
Normally fees should not involve any significant component for reviewing the records to determine if appropriate for release. It is not reasonable to charge a patient for
the time taken responding to the OAIC.
We recommend speaking to MIGA's Claims and Legal Services team before refusing a patient’s request to access their personal information. It is essential that any grounds to refuse access are considered carefully before being relied upon, and even if access is refused, that you comply with minimum access requirements.
KATE HODGKINSON SENIOR SOLICITOR, CLAIMS & LEGAL SERVICES



Calls to the DMS helpdesk are answered literally within seconds, most issues are resolved within minutes.
Guaranteed Level 2 or Level 3 technicians with extensive experience in Australian medical software problem resolution.
Extensive experience and expertise in Australian medical software ecosystems.
87% of helpdesk calls resolved on the same day.
81% of helpdesk calls resolved on the first call.
Managed Cyber Security expertise. Security first approach with Cyber Security qualified staff.
Proactive Managed IT that is fully customised for Australian medical clinics, with high attention to detail.
DMS Private Cloud located in Melbourne and Sydney at leading Tier 4 data centres with latest high performance, and high capacity host servers.

Hayley Hughes, Practice Manager

DIGITAL MEDICAL SYSTEMS
News reports about Generative AI (Gen AI) topics continue to feature across all media channels on an almost daily basis, including mainstream news, financial news, environmental news, healthcare news, technology news, including on security concerns about Gen AI, disinformation and misinformation.
For example, on January 20, 2025, DeepSeek R1 version was released by newcomer Chinese AI startup, Hangzhou DeepSeek Artificial Intelligence Basic Technology Research Co., Ltd, (founded in December 2023 by Liang Wenfeng).
DeepSeek AI R1 is free to download and use, and is a ‘reasoning’ open source AI chatbot, which looks and works like OpenAI’s ChatGPT, has caused enormous press across the world, as it has been called a disrupter technology, since DeepSeek claimed that the R1AI chatbot was developed for only US$6m by using a small number of low cost Nvidia H800 chips, instead of the using high performance Nvidia chips, (because of the high performance Nvidia chips have been banned from export to China by the US in 2022) 1. DeepSeek also claims that R1 rivals the power of OpenAI’s o1 model, which was released in late 2024, and reportedly cost over
US$100m to train, and also rivalling Meta’s advanced models, all for US6m. 2
This combination of DeepSeek’s AI computational performance for extremely low cost has stunned AI experts and rattled investors across the AI space – Nvidia’s shares dropped 17% on January 27, falling from it’s spot as the most valuable company in the world at US$3.5 trillion market capitalisation, to third place at US$2.9 trillion, a fall of almost US$600 billion, the biggest one day market capitalisation loss of any company in history, placing Nvidia now behind Apple and Microsoft.3

around the world have banned DeepSeek.
DeepSeek became the worlds most downloaded app on Apple and other App Stores. AI experts have praised DeepSeek R1, “as an excellent AI advancement”, but have also questioned the veracity of DeepSeek’s claim for development and training at such low costs with low end Nvidia chips.
DeepSeek’s high performance and quality at such a claimed very low cost has not only upset investors in AI companies, but governments
On February 5, the Australian government banned the installation and use of DeepSeek on all federal government computers and devices, followed by bans by all state governments, except for Victoria and Tasmania.4 Federal Home Affairs Minister Tony Burke said that the Australian government ban was to “protect Australia’s national security and national interest”.5 Citing warnings by Australian security agencies that the data collected by DeepSeek could be available to the Chinese government [possibly under compliance with China’s Article 7 of National Intelligence Law6]. (DeepSeek is not banned for private entities and individuals in Australia.)
South Korea, Taiwan and Italy have also restricted or banned DeepSeek at the time of writing this article,

with other governments considering bans.7
We shall see how all this unfolds, however, what is clear is that the competition for AI dominance, commercially and internationally is ramping right up. US President Trump called the release of DeepSeek AI a wake-up call…:
“The release of DeepSeek AI from a Chinese company should be a wake-up call for our industries that we need to be laser-focused on competing to win because we have the greatest scientists in the world,” Mr Trump said.”8
Geo-politics and intensifying competition in the AI space are not the only concerns Australians should be aware of before downloading and installing DeepSeek.
Security and privacy concerns about DeepSeek are mounting.
On January 29 CSOonline.com reported on US cyber security company Wiz Research finding a significant data leak in DeepSeek, involving over 1 million records, including, “chat histories, backend details, API secrets, and sensitive operational information”.9 Even worse, Wiz Research reported that;
…“ the database was entirely unprotected, allowing unrestricted access to internal logs and potentially compromising user interactions.
The unprotected database also granted full administrative control over its contents. Attackers with access could have retrieved proprietary
data, extracted plaintext passwords, and even accessed local files stored on DeepSeek’s servers. Wiz researchers noted that there were no authentication mechanisms in place, making the breach particularly alarming.”10
Further, Wired magazine reported that more alarming findings by security researchers from Cisco and University of Pennsylvania, who “tested 50 well-known jailbreaks against DeepSeek’s popular new AI chatbot. It didn’t stop a single one”: …”when tested with 50 malicious prompts designed to elicit toxic content, DeepSeek’s model did not detect or block a single one. In other words, the researchers say they were shocked to achieve a “100 percent attack success rate.”11
Following the Australian government’s banning all government users from downloading and installing DeepSeek may very well be the wise and safe policy to follow for Australian primary healthcare users also. We cannot say we have not been warned about DeepSeek AI…
Of course, we must not forget other cybersecurity concerns about the malicious use of Gen AI by cyber criminals.
White Hat ethical hacker, FreakyClown (FC), writing for leading behavioural AI based email security company, Abnormal, warns that …” like any tool, even ones that are built for the good of the world, AI can be used by bad people to do bad things.”12 Cybercriminals are, “attempting to employ AI to develop
sophisticated malware, phishing schemes, and even automated attack vectors that can bypass conventional security measures.”13
FC warns that:
“Unfortunately, traditional security measures often fall short in detecting and responding to these AI-driven threats—highlighting the need for AI-enhanced defenses.”14 , and advises;
“Organizations should invest in robust AI-based security solutions, continuously monitor and leverage threat intelligence, and conduct regular training and awareness programs for employees.” 15
FreakyClown’s warnings are echoed by leading cybersecurity insurer, CFC, warning of “Threats of unprecedented complexity”;16
“As cybercriminals adapt to evolving technology, their attacks are becoming increasingly hard to prepare for. Organizations face not only traditional risks like ransomware and phishing attacks, but also advanced threats like deepfake fraud and AI-produced malware. Bad actors can now combine automation, data analytics, and social engineering to target vulnerabilities with precision.”17
Meanwhile, reports of positive Gen AI use cases in healthcare are increasing, with a simple search of PulseIT.news reports on AI finding many promising and interesting developments. Here are just a few examples:

◦ AI Scribe/transcription:
The uptake of AI Scribe / transcription tools by clinicians as seen as having the “potential to pave the way for wider public acceptance of AI in healthcare…”18
◦ AI analysis and diagnosis of respiratory diseases: Collaborative research from Charles Darwin University, United International University and Australian Catholic University, has “developed and trained an AI model to analyse lung ultrasound videos and diagnose respiratory diseases”. Lead researcher and “co-author CDU adjunct Associate Professor Niusha Shafiabady said the model had an accuracy of 96.57 per cent, with the AI analyses verified by medical professionals,” and explained that, “This model helps doctors diagnose lung diseases quickly and accurately, supports their decision-making, saves time, and serves as a valuable training tool.”19
◦ AI in breast cancer risk prediction: Quoting Associate Professor Wendy Ingman, from University of Adelaide, the lead author of a paper published in Trends in Cancer; “Artificial intelligence is enabling us to delve deeply into the information inherent in a mammogram and identify novel features associated with higher risk of a future breast cancer diagnosis.” Professor Ingman further said that, “AI methods are now uncovering mammographic features that are stronger predictors of breast
cancer risk than any other known risk factor.”20
◦ AI in retinal imaging: Research funded by the Lowy Medical research Institute at the Walter and Eliza Hall Institute of Medical Research (WEHI) has used AI-to create “the most detailed maps of the retina ever produced, paving the way for routine eyecare as a disease screening tool.”, with researchers using “the maps to link retinal thinning to a range of diseases as well as identifying new genetic factors that influence retinal thickness.”
Lead researcher Dr Vicki Jackson said that, “We’ve shown that retinal imaging can act as a window to the brain, by detecting associations with neurological disorders like multiple sclerosis and many other conditions.”21
◦ AI in wound care:
PulseIT reports that Amplar Home Health will incorporate the Net Health Tissue Analytics platform, an application it says can transform iPads and smartphones into “sophisticated imaging platforms” that allow clinicians to use artificial intelligence and computer vision for advanced wound assessment.” Quoting Kylie Mayo, Amplar Home Health general manager, saying, “the technology would improve the consistency of measurements and help streamline wound management for patients in their homes, and emphasised the importance of continuous wound monitoring”, Mayo further explains that, “Wounds
require daily attention. Clinicians need to ensure that a wound is improving and not deteriorating or becoming infected. Traditional methods often involve physical measurements, which can be challenging due to the organic shapes of wounds. AI and machine learning are the future of wound measurement.”22
Here is an interesting PulseIT report confirming Australians as early adopters of new technology at scale by peer reviewed research from the University of Sydney
◦ One in 10 Australians seek medical advice from ChatGPT: A survey of more than 2000 people found that, “Almost 10 per cent of Australians have used ChatGPT to ask medical questions, while just under 40 per cent were considering using it”, and that, 84.7 per cent of participants knew about ChatGPT and 9.9 per cent had already used it to obtain health-related information, while a further 38.8 per cent were considering doing so in the next six months.”23
Finally, as with any great innovation in technology, we must identify the pros and cons, maximising the pros, such as those reported above from PulseIT.news, while minimising or avoiding the cons, for example, the Deloitte APAC-AI at a crossroads report (December 2024), urges that “Building trust as a path to scale”, is critical “to unlock AI’s full potential responsibly”24, highlighting the top concerns of nearly 900 senior leaders surveyed on the use of Gen AI:

“This pace and scale of AI adoption means leaders are encountering AI related risks in real time as they experiment and roll out the technology.
Our survey of nearly 900 senior leaders reveals that risks related to security vulnerability (86%), surveillance (83%) and privacy (83%) are the most common concerns for senior leaders when using AI (Figure 1). These risks have become even more pronounced since the advent of GenAI, which has seen a step change in the capabilities of the technology alongside more user-friendly interfaces that have broadened the number of people who can use these powerful tools.”25
Minimise the cons of Gen AI, such as not using unsafe AI bots like DeepSeek, employ the latest cybersecurity protections with AI capabilities, in order to maximise the positive use of Gen AI in medical research and applications which enhance healthcare and human wellbeing. More to come…
References
*Image source: https://economictimes. indiatimes.com/tech/technology/explainerwhat-is-deepseek-and-why-is-it-disruptingthe-ai-sector/articleshow/117609853.cms
1 Reuters, (2025)., What is DeepSeek and why is it disrupting the AI sector?, retrieved from https://www.reuters.com/technology/ artificial-intelligence/what-is-deepseek-whyis-it-disrupting-ai-sector-2025-01-27/
2 ibid
3 Forbes, (2025)., Biggest Market Loss in History: Nvidia Stock Sheds Nearly $600 Billion as DeepSeek Shakes AI Darling, retrieved from https://www.forbes.com/sites/ dereksaul/2025/01/27/biggest-market-lossin-history-nvidia-stock-sheds-nearly-600billion-as-deepseek-shakes-ai-darling/
4 The Mandarin, (2025)., DeepSeek ban imposed by state and territory governments, retrieved from https://www.themandarin.com. au/286128-deepseek-ban-imposed-by-stateand-territory-governments/
5 SMH, (2025)., Australia bans Chinese AI platform DeepSeek on government devices, retrieved from https://www.smh.com.au/ politics/federal/australia-bans-chinese-aiplatform-deepseek-on-government-devices20250204-p5l9js.html
6 Wikipedia, (2024)., National Intelligence Law of the People's Republic of China, retrieved from https://en.wikipedia.org/wiki/National_ Intelligence_Law_of_the_People%27s_ Republic_of_China
7 ZDNET.com, (2025)., These nations are banning DeepSeek AI - here's why, retrieved from https://www.zdnet.com/article/thesenations-are-banning-deepseek-ai-heres-why/ 8 AFR.com, (2025)., ‘A wake-up call for US’: Trump on DeepSeek, retrieved from https:// www.afr.com/world/north-america/trumpcalls-deepseek-a-wake-up-call-for-america20250128-p5l7n0
9 CSOonline.com, (2025)., DeepSeek leaks one million sensitive records in a major data breach, retrieved from https://www.csoonline. com/article/3813224/deepseek-leaks-onemillion-sensitive-records-in-a-major-databreach.html
10 ibid
MIROSLAV DONCEVIC MANAGING DIRECTOR DIGITAL MEDICAL SYSTEMS
11 Wired.com, (2025)., DeepSeek’s Safety Guardrails Failed Every Test Researchers Threw at Its AI Chatbot, retrieved from https://www. wired.com/story/deepseeks-ai-jailbreak-
prompt-injection-attacks/
12 Abnormal Security, (2025)., The Rise, Use, and Future of Malicious Al: A Hacker's Insight, retrieved from https://abnormalsecurity.com/ resources/malicious-al-hackers-insight, p4
13 ibid, p5
14 Op cit, p15
15 Ibid, p15
16 CFC.com, (2025)., Top cyber security threats in 2025 and how to respond, retrieved from https://www.cfc.com/en-au/knowledge/ resources/articles/2025/01/top-cyberthreats-2025/
17 ibid
18 Pulseit.news, (2025)., Scribes pave the way for AI acceptance in healthcare, retrieved from https://www.pulseit.news/australiandigital-health/scribes-pave-the-way-for-aiacceptance-in-healthcare/
19 Pulseit.news, (2025)., Artificial intelligence diagnosing lung diseases, retrieved from https://www.pulseit.news/australian-digitalhealth/artificial-intelligence-diagnosing-lungdiseases/
20 Pulseit.news, (2025)., AI shaping the future of breast cancer risk prediction, retrieved from https://www.pulseit.news/australiandigital-health/ai-shaping-the-future-ofbreast-cancer-risk-prediction/
21 Pulseit.news, (2025)., Retinal imaging doorway for disease detection, retrieved from https://www.pulseit.news/australian-digitalhealth/retinal-imaging-doorway-for-diseasedetection/
22 Pulseitnews, (2025)., Wound care boosted by artificial intelligence, retrieved from https://www.pulseit.news/australian-digitalhealth/wound-care-boosted-by-artificialintelligence/
23 Pulseit.news, (2025)., At least one in 10 Australians seek medical advice from ChatGPT, retrieved from https://www.pulseit. news/australian-digital-health/at-least-onein-10-australians-seek-medical-advice-fromchatgpt/
24 Deloitte.com, (2024)., AI at a crossroads, retrieved from https://www.deloitte.com/ global/en/offices/apac/perspectives/apactrustworthy-ai-report.html
25 Deloitte Access Economics, (2024), AI at a crossroads_Building trust as the path to scale, retrieved from https://www.deloitte.com/ global/en/offices/apac/perspectives/apactrustworthy-ai-report.html, p6


�� Step-by-step marketing for small & medium businesses
�� How ads, SEO, social media & content work together
�� More revenue, better profit margins & less stress
�� Success stories + live Q&A

CUBIKO
The integration of Continuing Professional Development (CPD) and quality improvement initiatives represents a significant opportunity for general practices and Practice Managers. Within the current frameworks and accreditation standards, practices can now implement strategies that meet practice accreditation goals, enhance professional development for GPs, and improve patient care outcomes simultaneously.
The RACGP's CPD requirements are straightfoward: GPs must complete 50 hours of annual professional development across Educational Activities (EA), Reviewing Performance (RP), and Measuring Outcomes (MO). This structured approach ensures practitioners maintain comprehensive skill development while focusing on measurable improvements in patient care.
As it stands, many of the activities GPs embark upon to achieve measuring outcomes hours overlap with the activities many practices are completing as part of quality
improvement. We’re seeing both GPs and practice teams working towards similar goals independently in many practices, however a smaller number of practices have started to created team based approaches to QI and CPD, enabling better teamwork, resourcing and results for patients.
How can Practice Managers work closely with GPs to create these integrated approaches? It largely comes down to forward planning, giving you and your team time to identify the joint-activities you want to embark upon, and then creating a system which keeps everyone organised and on the same page.
Team meetings serve as a cornerstone for integration, every team QI needs to set aside dedicated time to review their programs, and including GPs in these meetings is one of the simplest ways to include them in decision making and demonstrate the value of their involvement. These meetings can address immediate practice challenges while contributing to practitioners' CPD requirements, particularly in the MO category.
Second to team meetings is regular clinical audits, which demonstrate the practical benefits of the activities. A well-designed audit
simultaneously:
◦ Provides data for practice improvement initiatives
◦ Contributes to practitioners' Measuring Outcomes CPD requirements
◦ Generates evidence for practice accreditation
◦ Identifies specific areas for service enhancement
In addition, patient feedback systems offer another integration opportunity. While accreditation currently requires triennial surveys, implementing continuous feedback mechanisms provides ongoing data for both quality improvement and CPD activities. This approach ensures patient experiences directly inform practice enhancements and professional development.
Success requires a systematic approach:
◦ Audit current quality improvement and CPD activities2.
◦ Identify integration opportunities3.
◦ Implement tracking systems such as Cubiko and other tools4.
◦ Regular review and adjustment of strategies5.
◦ Continuous monitoring of outcomes
The combination of both QI and CPD activities present valuable

opportunities for improving patient outcomes. As practices implement new systems and workflows, technology can play a huge role in reducing the administrative burden of activities as well as increasing the accuracy of the documentation surrounding them.
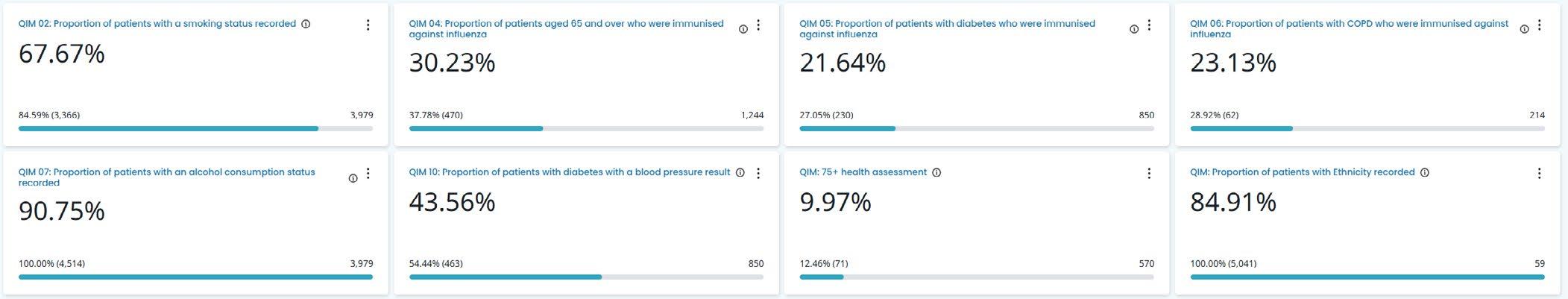
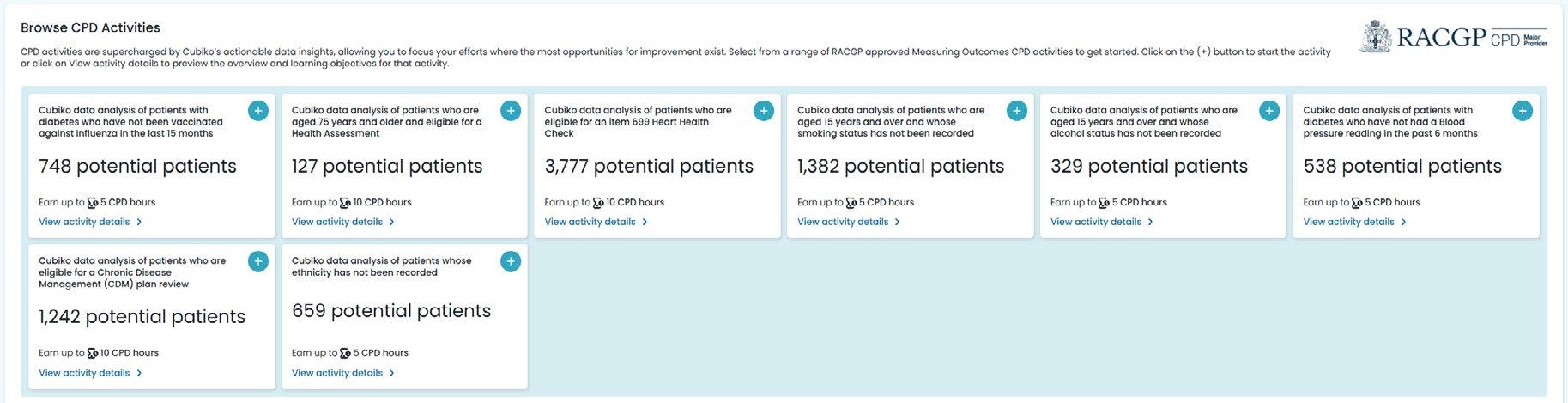
Currently, almost 1 in 3 General Practices in Australia use Cubiko’s Quality improvement dashboards to identify and complete QI activities. These range from administrative activities such as recording of ethnicity, smoking and alcohol status and more, to more clinically focussed activities such as blood pressure results for diabetic patients and completing health assessments. When practice teams use reporting softwares to manage activities, it becomes far easier to communicate what needs to be undertaken by specific team members as well as generate the reporting required to satisfy accreditation standards.
Released in late 2024, Cubiko's My CPD Outcomes feature represents a significant advancement in this integrated approach. This purposebuilt solution addresses the challenge of managing Measuring Outcomes CPD requirements while at the same time, ensuring the outcomes are having a real impact on patient health. Cubiko's CPD metrics are pre-approved by the RACGP and provide realtime insights into key areas for improvement, including:
◦ Patient ethnicity recording
◦ Chronic Disease Management outcomes
◦ Health Assessment completion rates
◦ Proactive care opportunities
Many of which directly overlap with the aforementioned QI activities. These dashboards allow practitioners to focus on patient care while ensuring CPD requirements are tracked and aligned with practice goals. By providing clear visibility
of both individual CPD progress and practice-wide quality metrics, Cubiko enables healthcare teams to work cohesively toward common objectives.
Through careful implementation and technology support from platforms like Cubiko, practices can transform their approach to professional development and quality improvement. This integration creates a more efficient healthcare system that benefits practitioners, practices, and patients alike.
The shift toward integrated CPD and quality improvement, supported by innovative solutions like Cubiko's CPD features, represents a practical path forward for Australian general practices. By embracing this approach, practices can ensure professional development activities directly contribute to improved patient outcomes while meeting regulatory requirements efficiently and effectively.



A practice’s predicament – do patients have the right to access their medical records?
Jane, the receptionist, has just got off the phone with Douglas, a longtime patient of the practice, who made an unexpected request: a full copy of his medical records. “I heard that, legally, the records belong to me, not the practice, and so I want a copy,” he said. Jane is in your office, recounting the conversation with a mix of uncertainty and concern. “Are we allowed to release his records? What should I do?” she asks.
While Douglas is not correct that his records belong to him, patients generally do have the right to access their medical records, whatever their reasons (for example, for their own reference or because they are moving to a new practice), except in limited circumstances.
A patient’s right to access includes having a copy of their records, inspecting their records, and providing a copy of their records to an authorised third party (for example, a solicitor or insurer).
A patient’s request for their records should be in writing. This is required for all requests in NSW and in some situations in Victoria and the ACT, such as when the request is from lawyers representing a deceased individual.
The Privacy Act 1988 (Privacy Act) contains 10 exceptions to giving patients access to their records. Two grounds that are most likely to arise for healthcare providers are:
◦ Serious threat – You have grounds to believe that if a patient accessed their health information, it would pose a serious threat to the life, health or safety of the patient, another person, or the public.
◦ Unreasonable impact on the privacy of other individuals –The patient’s health information contains another individual’s information, which would impact that individual’s privacy.
You can charge the patient for access to their medical records, but not for making a request. The amount you charge depends on several factors, such as your relationship with the patient and knowledge of their circumstances (for example, known financial hardship) as well as the nature, size and resources of your practice. Therefore, a flat fee is generally inappropriate.
The amount must not exceed the cost you would incur or include any costs relating to legal advice around handling the request. You should advise the patient of the cost before
arranging access. You may negotiate the patient’s request (for example, the volume of records) to minimise the charge.
In Victoria and the ACT, the cost of providing medical records is capped by regulations which are updated periodically.
You should aim to provide access to records in the form that the patient requests it, where possible. Health information can be provided in several ways, such as:
◦ sharing a copy of the information (electronic or hard copy)
◦ providing a summary of the information
◦ providing information over the phone (for example, test results)
◦ allowing the patient to view or listen to an audio or video recording of the information and take notes.
While this request came from Douglas, in other situations patient records may be requested by third parties (for example, from a solicitor for the purpose of legal proceedings or an insurer in relation to a patient’s workers’ compensation or life insurance claim). In that situation, your response depends on whether you have ‘authority’ (the

patient’s consent) to release the information.
Often these requests are accompanied by a document signed and dated by the patient. To ensure the authority is valid, you should check the patient’s full name, date of birth, and address and ensure it is signed and dated by the patient. While the authority doesn’t necessarily expire, we recommend you contact the patient to confirm if it is more than 12 months old.
This may also be useful if you need to confirm the scope of the request. Sometimes the request might be for a whole record but the authority itself might be limited, for example to records relevant to an injury or a claim. This can be complicated as what is legally relevant to an insurance claim might not necessarily be what you would consider clinically relevant. In this case, you should seek clarity from the patient in the first instance, or from the lawyer or insurer requesting the records.
A copy of the request and a copy of the practice's response should be retained. If the scope of the documents provided is very specific, it is wise to also keep a copy of what was provided with that correspondence. You should also document any conversations you have with the patient about the authority.
To avoid breaching the patient’s confidentiality or releasing records inappropriately, only provide a copy of the documents that are captured
by the scope of the authority. Where the included records contain sensitive information, you should confirm with the patient that they are aware their authority extends to such information and confirm it can be released. Document this conversation.
Sometimes, correspondence from non-GP specialists has a standard sentence stating the letter should not be supplied to third parties without their consent. However, once received by another doctor or health provider, these letters form part of that medical record for the patient and, like any other part of the record, should be released to the patient or third party if captured by the scope of the request.
For more information, refer to Avant’s Providing medical records to a third party factsheet.
So, for Douglas’ request, Jane should document the phone call in the records, or if in NSW, she should ask Douglas to send a written request. Unless any of the exceptions apply, she can then arrange for Douglas to have a copy of his records after determining any fee based on his circumstances and reasonableness, or any regulations dictating the amount.
Avant factsheet: Medical records: the essentials
Avant factsheet: Providing medical records to a third party
RUANNE BRELL SENIOR LEGAL ADVISOR AVANT
We can automatically block patients that owe money from booking online until they make payment.
Our Patients no longer have to worry about spam SMS when all our messages are from a dedicated mobile number.
No more time spent on frantic early morning calls to patients as I can trigger a bulk message when my doctors are sick.
My doc tors can offer online booking to their Own patients
I can trigger a secure SMS to request payment on outstanding debt and when paid, the funds are reconciled back to my PMS


M y G P M P t o o l ( M G T )
Integrated digital CDM tool
MGT is the next-generation care collaboration platform that streamlines care planning, connects healthcare providers, reduces admin burden, and improves patient outcomes. �� Join the Future of Healthcare Collaboration

Level 3, 480 Collins Street, Melbourne, 3000, VIC TP: 03 8610 6353
www.mygpmptool.com.au
Key Benefits
�� Care plans made easy
Easily create, manage, and update care plans across multidisciplinary teams.
�� Automated care collaboration
Real time referrals, care plan and reviews updates across all team members.
�� Tracking, monitoring and self-audits
Review progress tracking, CDM activity monitoring and MBS self audits are just a few of the practice benefits.


HILLHOUSE LEGAL PARTNERS
As a Practice Manager in the healthcare profession, you are responsible for ensuring the smooth operation of your clinic, from staff coordination to financial oversight. While much of your focus is on the present, have you and your team considered the longterm planning necessary to protect your personal assets and provide security for your loved ones?
Estate planning is not just for the wealthy or elderly; it is essential for anyone who wants to safeguard their family’s future, manage tax obligations effectively, and ensure their wishes are carried out. While your role may be primarily operational, planning for your personal financial future is crucial. With your respected financial acumen, you're well positioned to encourage your colleagues to consider their own estate planning needs.
WHY ESTATE PLANNING MATTERS FOR PRACTICE MANAGERS
◦ Protecting Your Personal and Professional Assets
Your financial situation is unique. For some of you, you may have ownership stakes in a practice, have a family trust, be a cosignatory on business loans,
or hold professional insurance policies. You may also have employment benefits, retirement accounts, or financial obligations tied to your role. A wellstructured estate plan ensures that both your personal and business interests are managed correctly in the event of your passing or incapacity.
The same applies to others who have ownership in the practice and it would be helpful to encourage your colleagues to consider their estate plan for the same reasons.
◦ Providing for Your Family and Dependents
Beyond business concerns, estate planning ensures that your personal assets are distributed according to your wishes. If you have dependents, setting up trusts or appointing guardians
provides stability and financial security for them.
◦ Minimising Tax Burdens
Estate planning allows you to structure the assets left in your estate in a way that minimises tax liabilities and often gives tax advantages. This can be particularly important if you have investments, retirement accounts, or business interests that could otherwise be subject to unnecessary taxation. Planning ahead ensures that more of your wealth goes to your beneficiaries rather than being lost to tax obligations.
◦ Ensuring Business Continuity
If you are a co-owner or key decision-maker in your medical practice or play a key role in the daily operations of the practice, what happens to the business if you are no longer there? A will, power of attorney, and a


business succession plan can help ensure that operations continue smoothly and that your partners or successors are not left in a difficult position.
◦ Managing Healthcare Directives
As someone working in the healthcare industry, you understand the importance of medical decisions. An advanced healthcare directive and a power of attorney for medical decisions ensure that your wishes are followed should you become unable to make such decisions yourself.
◦ Roles Appointed for Clarity and Reducing Risk, Conflict and Costs
When drafting your Will, you designate a trusted person as your Executor to manage your estate after your passing. Without a Will and an appointed Executor, your family will need to apply to the Supreme Court, so that someone is legally recognised to be able to deal with your assets and affairs. This will incur legal expenses reducing the overall value of your estate and the amount left for your beneficiaries. All of this takes time and places financial and emotional stress on loved ones at a sensitive time.
A clear, professionally drafted Will helps reduce the risk of conflict by minimising misunderstanding and disagreements, speeds up the estate administration process, and provides peace of mind for you and your loved ones.
Succession planning is often complex and involves thorough consideration of both the legal aspects and your personal

circumstances. Professional legal advice is highly recommended to avoid undesired outcomes.
These are the essential estate planning documents and components for you to consider:
◦ Will - outlines how your assets should be distributed and who will be responsible for carrying out your wishes.
◦ Enduring Power of Attorney (EPA) - appoints someone to manage financial and legal matters if you become incapacitated.
◦ Advanced Health Directive (AHD) - specifies your preferences for medical treatment in case you are unable to communicate them.
◦ Testamentary Trusts - can be used to manage and distribute assets in a tax-efficient manner, particularly if you have dependents.
◦ Superannuation – as this does not automatically form part of your assets, consider a Binding Death Benefit Nomination (BDBN) to ensure your superannuation is distributed as you wish.
To safeguard your estate and reduce the risk of disputes, it is essential to follow a structured approach when preparing your Will. It doesn’t have to be overwhelming – just following these essential steps to ensure your estate is handled according to your intentions.
1. Select your Beneficiaries –clearly define who will receive your assets and in what proportions.
2. Decide how you want your estate distributed – your assets can be divided with specific gifts, residual gifts, percentage gifts, or as a whole estate.
3. Choose an Executor – select someone you trust to manage and distribute your estate.
◦ Business Succession Planensures a smooth transition for your medical practice, protecting its future stability if you hold part ownership.
4. Appoint Guardians for minor

children – if you have minor children, name a guardian to ensure someone you trust will be taking care of them.
5. Write your Will with a legal professional – legal experts ensure your Will is properly structured and comprehensive to safeguard your estate, prevent conflict and guide Executors through the process with confidence.
6. Signing your Will correctly –a Will is only valid if signed and witnessed correctly.
7. Keep it safe – store your original Will securely—many choose to keep it with their lawyer. Make sure your executors know its location, and consider providing them with a copy.
Life circumstances evolve, and your Will should evolve with them. Whether you're getting married, welcoming a child, experiencing a separation, or purchasing a key
asset, each milestone can change your priorities and responsibilities. An outdated will might not capture your current wishes, leading to legal disputes, misallocated assets, or the exclusion of new family members. In the worst cases, your assets could be distributed contrary to your intentions, leaving loved ones vulnerable or financially disadvantaged. Regularly review your estate plan with a legal professional to ensure it remains aligned with your current needs and protects your family's future.
Estate planning may seem complex, but taking proactive steps now can save your family, business partners, and colleagues from unnecessary challenges in the future. Consulting a legal professional who specialises in Wills and Estates ensures your plan is comprehensive, up to date, and aligned with your current circumstances.

If you haven’t reviewed your estate plan recently - or if your business or personal situation has changed -now is the time to act. Planning today provides peace of mind for you, your loved ones, and the medical practice you’ve worked hard to support.
Every day without an estate plan is a risk you don’t need to take. Contact your legal professional to review your plan or start the process. Taking action now secures your legacy, protects those who matter most, and ensures your wishes are carried out with certainty.
Offer exclusive to AAPM members
Free 30 minute virtual consultation with the Hillhouse Legal Partners Wills and Estates team to review your current plan or get started on preparing one.






Streamline your practice's finances and give your team more time to focus on patient care. HotDoc Payments is the solution that automates your payment collection, ensuring your clinic runs smoothly and profitably.

Collect telehealth fees upfront with ease: Seamlessly collect telehealth fees with HotDoc Payments, ensuring secure, hassle free transactions with every consultation.
Automate your payments: No more chasing missed payments! HotDoc Payments automatically stores patient card details and enables your team to collect payments easily.
Upfront payment protection: Protect your practice’s revenue with guaranteed upfront payments for every booking. No more waiting, payments are secure before consultations even begin.
Minimise debt and reduce failed payments: Preauthorise appointment fees upfront to secure funds quickly! With a 99.98% success rate, you can trust HotDoc Payments to collect funds quickly and securely.
More time for your receptionists: Say goodbye to front desk payment processing and awkward debt collection calls. Let HotDoc handle the heavy lifting with automations to also help reconcile payments back to your PMS.
Direct to practitioner payouts: Simplify your finances with direct to practitioner payouts. Reduce admin time and improve cash flow for a smoother practice operation.
HotDoc helps over 11 million patients connect with practices just like yours. Be part of Australia’s biggest patient platform, trusted by 1 in 3 Australians, with over 22,000 practitioners using HotDoc every day to provide top-tier care.
Book a Demo Today




MedicMall is the new online marketplace that helps healthcare providers find quality products and services, saving time and money.
For medical practices and private hospitals, MedicMall brings all the products and services you need to run your business, together, in one convenient, intuitive, and easy to use marketplace Which makes it a smarter way to source, compare and buy premium quality, great value products and services from a range of trusted suppliers





BEST PRACTICE SOFTWARE
It almost goes without saying, but Practice Managers are increasingly burdened with high staff turnover, frustrated patients, pressures of legislative changes and higher than ever running costs. Never has the role of a Practice Manager become just so pivotal. As the keystone in this intricate ecosystem, Practice Managers bear the responsibility to navigate and mitigate these challenges to ensure the seamless operation of the practice – but how can you increase efficiencies, profit and staff morale, when you just don’t have the time?
Through the implementation of targeted communication strategies, staff training programs, and wellness initiatives, Practice Managers can craft an environment that not only supports their teams but also fosters a harmonious workplace culture. Such initiatives are not mere reactionary measures, but rather strategic endeavours aimed at building resilience and adaptability among staff members. Out of a competing priority list, start by prioritising effective communication strategies to bridge any gaps between staff
and patients. This in turn will help to mitigate misunderstandings and fostering a more respectful atmosphere. Simultaneously, wellcurated staff training programs equip team members with the necessary skills to adeptly handle the evolving demands of their roles, thus reducing turnover rates. Is technology or your practice software causing your issues? Your software vendor might be able to help equip your team with some additional skills.
Building upon these strategies, Practice Managers must delve deeper into their implementation to genuinely transform the workplace culture and that starts with the right people. Leveraging researchbased tactics in staff selection and training can fundamentally alter the dynamics within a workplace. By meticulously selecting and interviewing potential hires, Practice Managers ensure that new staff members align with the ethos and demands of the practice, effectively reducing future turnover. Once they’re on board, developing robust training programs equips staff with pertinent skills, but also fosters a sense of preparedness and confidence. This proactive approach aligns with best practices in crisis management by emphasizing ongoing development and followup as crucial components in staff support systems. You don’t have to do it alone though. There are external organisations full of highly
skilled and accredited trainers to outsource to, should you wish.
The role of Practice Managers in addressing the multifaceted challenges faced by General Practitioners' offices is both pivotal and transformative. Through the implementation of targeted communication strategies, tailored staff training programs, and holistic wellness initiatives, you as leaders construct a resilient framework that not only mitigates immediate stressors but also fosters longterm adaptability within your team. By bridging gaps through clear communication, equipping staff to meet evolving demands, and prioritising mental well-being alongside physical health, Practice Managers really can influence an environment where team members feel supported and empowered. This proactive approach transcends mere crisis management by embedding resilience and cohesion into the very fabric of workplace culture.
SUZIE
ELEY STREAM MANAGER TRAINING AND DEPLOYMENT
BEST PRACTICE SOFTWARE


What does it take to become the AAPM National Practice Manager of the Year? AAPM spoke to Namarata Sawheney about her journey.
Vision and leadership
What was your vision when you first stepped into this role, and how has it evolved over time?
When I first started as Practice Manager, my vision was more shortterm, focusing on the immediate goal of ensuring happy doctors and happy patients. I aimed to create a positive and harmonious environment where staff could thrive, and patients received excellent care.
Over time, my vision has evolved into a more expansive, forwardthinking approach. Through demographic studies of our community, I’ve gained a deeper understanding of the growing needs of our population. For example, our area has seen a rise in chronic conditions, mental health challenges, and a need for more accessible preventive care services. This insight has shaped my commitment to addressing these emerging health needs through advocacy, community-based interventions, innovative health solutions, and fostering creativity in healthcare delivery.
Additionally, I’m focused on breaking patterns of reactive healthcare by promoting preventive care and wellness. By identifying
gaps in access and addressing systemic issues. I aim to create a model of care that not only treats illness but also empowers individuals to lead healthier lives.
This evolution reflects my growing understanding of the practice's role, not just in delivering exceptional care, but in actively contributing to the broader community. By emphasising adaptability, innovation, and sustainability, I aim to address current challenges while building a resilient and impactful practice for the future.
What unique strategies or initiatives do you believe set you apart and contributed to this achievement?
I have introduced tailored quality improvement initiatives like chronic disease management and mental health workshops based on demographic studies. I shifted my focus from reactive care to preventive care through wellness education and outreach programs such as collaborated with Diabetes Victoria for the Life! program.
I also implemented professional development and support initiatives to create a motivated and engaged team and have fostered a culture of open communication and innovation, enabling dynamic responses to challenges.
By engaging with referring partners in the local community to extend care, and work with hospital department heads to provide
education sessions and explore joint initiatives has also been advantageous.
I actively listen to the needs of our patients, incorporating their feedback to improve services and ensure their voices shape the care they receive. By building on the strengths of our providers by tailoring roles to their expertise and encouraging innovation in their approaches to care, along with the other strategies have enhanced patient care, strengthened team cohesion, and fostered meaningful community connections.
How do you inspire and maintain motivation among your team during challenging times?
I am fortunate to work with a team that is highly dedicated, reliable, and deeply passionate about patient care. To maintain motivation during challenging times, I focus on:
◦ Understanding and address individual challenges within the team to foster trust and a sense of support.
◦ Acknowledge both small wins and major achievements which helps to boost morale and remind the team of their impact.
I think we have created a space where team members feel heard and valued which strengthens collaboration and resilience.
In uncertain times, I offer clear guidance and setting achievable

goals which ensures everyone stays focused and aligned.
I support staff through initiatives like mental health resources, flexible schedules, or debrief within safe team hurdles which keeps them engaged and energised.
I regularly express gratitude for their hard work and commitment which reinforces their sense of purpose and pride in what they do.
This approach has been instrumental in keeping the team motivated and united, even in the face of adversity.
What has been the most transformative challenge you’ve faced as a Practice Manager and how did you overcome it?
The most transformative challenge I faced as a Practice Manager was navigating the complexities of COVID-19. Each time the Victoria State Premier addressed the public and urged people to contact their GPs, our phone lines were bombarded, creating overwhelming pressure on our team.
In the midst of this, I had to ensure that the practice could operate smoothly while keeping both staff and patients safe.
Leading through this crisis meant providing clear communication to staff, ensuring they understood how to handle the increased demand and what the next steps were, which helped reduce confusion and stress. I also had to create a safe environment for both patients and staff, enforcing necessary health protocols while maintaining an
efficient workflow despite the unpredictable circumstances. Additionally, I made sure to create space for staff to decompress and feel supported during such a challenging time.
Although it was extremely difficult, we came out of it stronger, more informed, and better equipped to handle future challenges. This experience reinforced the importance of adaptability, leadership, and teamwork in times of crisis.

Can you share a moment when a setback turned into a breakthrough for you or your team?
A significant setback that turned into a breakthrough occurred at the start of the COVID-19 pandemic when our practice was overwhelmed by a sudden surge in demand for telehealth services. Our existing infrastructure and systems weren’t equipped to handle the volume, causing delays and frustration on both IT and reception desk. However, we quickly adapted by implementing a streamlined telehealth platform, offering training for staff, and clearly communicating with patients about the new process. This shift not only allowed us to maintain patient care but also
improved accessibility, particularly for vulnerable patients. The experience strengthened our team's adaptability and transformed our practice, making us more resilient and better prepared for future challenges.
What innovative practices or technologies have you implemented to improve efficiency and patient care in you Practice?
To improve efficiency and patient care, I have prioritised the adoption of innovative technologies and systems tailored to our community's needs. Implementing streamlined telehealth platforms, introducing

chronic disease management programs, and collaborating with organisations like Diabetes Victoria for wellness initiatives have been transformative. Additionally, I’ve utilised data analytics, quality improvement activities with NWMPHN to identify gaps in care, empowering the practice to take proactive steps in addressing patient needs. These innovations have improved accessibility, optimised workflows, and strengthened the overall quality of care.
How do you balance operational excellence with fostering a patientcentric culture?
Balancing operational excellence with a patient-centred culture requires a strategic and empathetic approach.
By focusing on clear communication, team empowerment, and operational clarity, I ensure that the systems in place enhance—not hinder—patient care. I actively listen to patient feedback and adapt processes to meet their needs while investing in staff training to provide compassionate and informed care. This dual focus enables us to deliver exceptional service while maintaining high operational standards.
Who or what inspires you as a leader, and how does that inspiration shape your management style?
My leadership is grounded in the
belief that true impact stems from serving others with purpose and compassion. Guided by the values of humility, integrity, and the profound responsibility we hold as healthcare professionals, I view leadership as an opportunity to uplift those around me.
The women who have been a constant source of strength in my life, alongside the mentors who guided me, and the resilience of the communities I’ve served, inspire me daily. Their influence drives me to lead with empathy, build meaningful connections, and create a legacy of positive change. This approach shapes every decision I make, ensuring a balance between patient care, team growth, and the broader vision of transforming healthcare for the better.
What advice would you give an aspiring Practice Manager(s) who aim to make a lasting impact in this field?
For aspiring Practice Managers, adaptability, empathy, and continuous learning are key.
Be open to change and embrace challenges as opportunities to grow. Lead with empathy to foster trust and collaboration within your team and with patients.
Invest in your professional development and learn from mentors and peers.
Always keep the bigger picture in mind: creating a meaningful impact for your practice and the community it serves.
If you could summarise your leadership philosophy in one sentence, what would that be?
Leadership, in my view, is about serving others with empathy, strategy, and purpose, guided by the timeless principles of ancient Indian philosophy. Drawing from the teachings of the Bhagavad Gita, a revered scripture in Hinduism that offers profound insights on duty, righteousness, and leadership. I believe true leadership is rooted in selfless service and a deep responsibility to others. In the Bhagavad Gita, Lord Krishna teaches that leadership is not about personal gain but about fulfilling one’s duty (or dharma) for the greater good, with compassion and wisdom. The word dharma comes from ancient Sanskrit and means righteousness, moral law, or duty, guiding leaders to act with integrity and responsibility.
Embracing these principles, I strive to lead with empathy and align every decision with the well-being of those I serve, fostering growth, harmony, and lasting, positive change.
What do you see as the biggest opportunity for growth or innovation in healthcare Practice Management over the next few years?
The biggest opportunity lies in leveraging digital health technologies and data-driven insights to enhance care accessibility

and efficiency. From AI-powered decision support systems to telehealth advancements, innovation will transform how practices deliver care. Integrating preventive health strategies and fostering collaboration across the healthcare sector will also be critical in addressing emerging challenges.
How do you plan to use the recognition from this award to drive further improvement or inspire others in the field?
This award is a powerful reminder of my unwavering commitment to raising the bar in healthcare practice management.
It strengthens my resolve to not only elevate standards but also to drive significant, transformative change in the industry. I aspire to use this platform to mentor and empower emerging leaders, share actionable insights, and advocate for innovations that tackle the evolving needs of patients and communities.
My goal is to inspire others to join me in building a healthcare system that is not only more efficient and accessible but also more equitable, with a lasting impact that extends far beyond today’s challenges. Through collaboration and bold leadership, I am determined to contribute to shaping a stronger, more resilient healthcare future for all.


AAPM is proud to celebrate International Women’s Day (IWD) on the 8th of March 2025.
The 2025 campaign theme #AccelerateAction emphasises the urgency in the advancement toward gender equality. Celebrating IWD is a perfect opportunity to recognise the progress we have made thus far and explore ideas and opportunities on how we can collectively work together in achieving gender parity.
Initiate. In the words of Robin Williams, “No matter what people tell you; words and ideas can change the world.” Change starts from an idea with the willingness to initiate action. This was the case for Share the Dignity Founder and Managing Director Rochelle Courtenay aka the “Pad Lady.” When Rochelle learned
about homeless women who were unable to access or afford sanitary items, which many included those fleeing domestic violence, she decided to act and started collecting sanitary items to distribute to local shelters. The idea of giving dignity to women led to the creation of “Share the Dignity” which grew to a national charity with over 6,000 volunteers Australia-wide. Since its inception, they have installed 1,000 Dignity Vending Machines across Australia and distributed over 4 million products to those who menstruate. Rochelle also spearheaded the #axethetaxperiod campaign lobbying for real parliamentary change to abolish tax on sanitary items. Her tireless efforts and engagement with local and federal politicians, the bill was passed on October 3, 2018, and the tax was abolished by state
and federal governments. The tax was officially removed as of 01 January 2019. What an achievement for women and everyone who menstruate!
Recognise. It is important to acknowledge the importance of men as allies to accelerate and deliver action for women’s equality. Men play a critical role in creating a gender-balanced workplace by supporting and advocating for women’s rights. Men use their platform to promote women’s equality like American professional basketball player Steph Curry who plays for the Golden State Warriors. Steph has spoken publicly and written an essay for The Player’s Tribune about women’s equality. It is amazing to see the growing number of men in leadership roles around us who support and advocate for change.
We sat down with Shane Patten, Senior Leader, Network Content Management, Optus Telecommunications, and Stuart Bunt, Practice Manager, Forest Family Practice to talk about their thoughts on women’s equality and their motivations in advocating for change.
Shane Patten is a strong advocate for women’s equality and inclusivity for all in the workplace. He states that he is very proud in the direction Optus leads in creating a diverse and inclusive environment. Gender Diversity, part of Optus’ diversity, inclusion and belonging strategy, is its initiative “to build a culture of equality committed to greater female representation in leadership and key


technical roles”. When asked about his motivations for advocating for women’s equality, Shane shares that he was raised by two very loving parents who raised him in a way that he believes is just the right thing to do. In a professional context, his motivation to act is prompted by seeing inaction. His values and beliefs guide him in knowing what actions to take and ensure processes are put in place to avoid previous negative experiences from reoccurring again. Shane added that he does not, however, believe he is doing anything different from what a good human being should be doing. With advocacy comes barriers and challenges, one of which is stigma. Shane explains that one stigma that comes with equality is that it means bringing men down. This mindset will take time to shift due to societal expectations of how men should be, and we need to acknowledge that equality is not about putting men down, rather it is about raising women up.
Stuart Bunt is not only sharing his perspective as a Practice Manager, he also comes with experience in corporate, small business and his general view of the community.
Stuart recognises that we have seen a lot of changes in our generation regarding the advancement of women’s equality. However, there is a long way to go, and it is a work in progress, particularly relating to fairness and opportunities for women in leadership. Stuart shares that his driving force in advocating for women is fairness and equality for all where everyone is treated identically to have fair and equal opportunity to participate and contribute. Stuart acknowledges that there are challenges we face today to achieve this such as preconceived and biased views on gender, age, or race. And the key to changing this mindset is education. He further explains as an example is that there are educational programs delivered in schools around respect for women which are important especially in their formative years and help shape the right mindset of the younger generation towards gender equality. And while equality can be a polarising topic, an educational approach is likely to be received better and get the message across. When asked if Stuart had any message for men and women on how we can #AccelerateAction for gender equality, he states his main
message is, “Call out, speak up, and if it doesn’t look right, question it. You may be one voice but there may be another person who shares the same views and there is definitely a shift in the momentum in favour of women’s equality.”
Inspire. Women in leadership inspiring change is one key in the advancement of women’s equality. It is imperative to recognise how influential women in power can be for the younger generation. Not only should we commend these women, but we must also celebrate them by sharing their journey.
We spoke with Kelsey Tukiri, Venue Operations Manager, Poodle Bar & Bistro and Rocco’s Bologna Discoteca, and Georgina van de Water, Chief Executive Officer, Royal Australian College of General Practitioners (RACGP) to share their experiences and views on women’s equality.
Kelsey Tukiri has been in the hospitality industry for 20 years, she started as a dishwasher and now manages two successful restaurants, Poodle and Rocco’s in Melbourne. Over the years, Kelsey has seen the progress in having more and more women in leadership roles in hospitality such as venue Operations Managers, Beverage Directors and Head Wine Buyers. Kelsey also acknowledges, there is still a long way to go. When asked what inspires her to advocate for women’s equality, Kelsey shares that working with amazing women who are collaborative, smart, and driven, makes her proud of their work as a team. In turn, she wants to make them proud by advocating for them. Kelsey further added that having

a 25-year-old niece makes her want to advocate for the younger generation, showing successful women in their role doing well will hopefully push them to strive for their own excellence. While Kelsey acknowledges there is still a lot of room for advancement, she believes that we have gone this far because of women’s drive to achieve change, that women can now be assertive in the workplace, that they can choose the jobs they want and affirm that they deserve the next promotion. Women today have a stronger voice which fuels drive for change. To keep pushing forward, women must continue supporting and inspiring one another.
Georgina van de Water has extensive experience in working in the primary healthcare sector and senior leadership roles. As we discussed her thoughts on women’s equality, Georgina said that women's choices of careers these days are much more varied than they were historically but there is still a lot of tradition around the types of roles that women choose. Georgina adds that whilst we have come a long way, there is still opportunity for greater
inclusion and structures to support women accessing opportunities. She further shares that in Nov 24, RACGP launched their first Diversity, Equity, and Inclusion (DEI) Plan, that aims to foster a fair, respectful, and psychologically safe workplace for everyone and create a sense of belonging. Georgina spoke of her personal motivation for advocating for women’s equality, as she fondly shared when she was first a CEO several years ago, she had not appreciated the impact that that would have for women. And while she was incredibly humbled, she was also surprised at the number of women who approached her to express how pleased they were to see a woman in leadership. Georgina explains that she has always felt fortunate to have the opportunities that had come her way in her career however, she had not really reflected on the responsibility that came with it. She tries to be overt in taking up opportunities when they present like this but also in sharing the challenges that she faces. And so, we asked Georgina if she had any words of encouragement for men and women. Georgina, with a beaming smile on her face, said, “Be
courageous. Focus on the end goal. Respect each individual for who they are and who they want to be, and not only use opportunities, but create them. Acknowledge that things get tough, but that’s for now, and you can always move past that and draw on others around you.”
As we reflect on the progress of women’s equality, let us not forget that change can start from us. We can initiate, recognise and inspire action. Collectively, we can achieve greater things, break down barriers, challenge the status quo and advance closer to the end goal – equality and fairness for all.




AGPAL
Climate change is a growing global challenge with farreaching impacts on health, environmental sustainability, and human wellbeing. The United Nations, local governments, businesses and individuals are increasingly prioritising sustainability to address the impacts of climate change and its associated risks.
Human activities such as burning fossil fuels, deforestation, and carbon emissions are driving unprecedented climate shifts, threatening the foundations of good health: clean air, safe water, nutritious food, and stable shelter. Australia is particularly vulnerable to climate-related events such as floods, bushfires, and heatwaves, further highlighting the need for proactive measures.
The healthcare sector is a significant contributor to environmental change, accounting for approximately 7% of Australia’s greenhouse gas emissions. This impact stems from diverse sources, including energy consumption, waste, and the use of medical resources. Health service organisations, from large hospitals to specialist facilities, general practices and allied health teams, can play a key role in addressing these challenges through
sustainable strategies. Implementing these initiatives not only reduces environmental harm, it also enhances the resilience of services susceptible to climate-related disruptions.
While sustainability may seem complex, health service organisations can begin with implementing manageable steps. Your team is likely to be undertaking a number of proactive measures already (consciously or unconsciously) to reduce their environmental impact. To further support these efforts, the AGPAL and QIP Teams have compiled some practical strategies for minimising your environmental footprint:
1. Managing e-waste effectively
◦ Conduct regular audits of outdated or unused devices
◦ Partner with certified recyclers for responsible disposal of e-waste.
◦ Invest in durable, energy-efficient equipment to reduce long-term waste.
2. Reducing single-use plastics
◦ Replace disposable items with washable, reusable alternatives where feasible
◦ Set up recycling and composting bins for waste separation
3. Conserving energy
◦ Switch to energy-efficient LED lighting.
◦ Use smart thermostats and schedule regular maintenance of systems.
◦ Consider renewable energy sources where possible, to reduce reliance on non-renewable energy.
4. Promoting sustainable transport
◦ Provide facilities like bike racks to encourage staff, patients and visitors to cycle.
◦ Offer telehealth services to reduce patient and visitor travel.
5. Engaging patients in sustainability
◦ Share information about health benefits associated with environmentally friendly practices, such as reducing waste.
◦ Encourage sustainable habits such as bringing reusable water bottles and bags for appointments.
To further support and guide your team’s sustainability efforts, the Australian Commission on Safety and Quality in Health Care (the Commission) has developed the Environmental Sustainability and Climate Resilience Healthcare Module
This framework helps health services integrate environmental sustainability into leadership, governance, and everyday practices


while maintaining high standards of care.
The Commission governs a number of industry Standards as part of accreditation requirements for many healthcare organisations throughout Australia. Recognising the significance of sustainability, as the Commission reviews its governed frameworks, future updates will likely include a sustainability focus as they evolve and reflect industry needs.
Dedicating efforts to creating a sustainable health service can support operational efficiencies and long-term benefits across various aspects of your business operations. For instance, reducing energy consumption and waste can lower operational costs and patients are increasingly valuing environmental responsibility in healthcare providers. This can enhance the reputation and trust of your practice’s services committed to sustainability.
The Environmental Sustainability and Climate Resilience Healthcare Module also outlines actions that health service organisations can take using their existing governance systems. These include identifying high-impact processes, redesigning clinical practices to minimise waste, and integrating sustainability indicators into routine monitoring and reporting. By incorporating these environmental targets into governance structures, organisations can ensure continuous improvements while staying accountable.
Today, it’s essential to track and evaluate environmental initiatives to make meaningful progress. The module published by the Commission recommends that health services set measurable goals, such as reducing energy consumption or waste, and track these metrics over time.
Some key steps towards measuring progress include:
◦ Setting clear goals
Establish achievable targets for
waste reduction or energy savings
◦ Monitoring performance
Use diverse tools and metrics to assess your environmental performance.
◦ Reporting on progress
Share updates with your staff and community to keep accountability.
◦ Encouraging feedback
Invite suggestions from staff, stakeholders and patients to identify new opportunities for improvement.
Your sustainability efforts will be most effective if embraced as part of your practice’s culture.
Here are some pointers to help your team foster commitment:
◦ Lead by example
Encourage leadership to visibly support environmental initiatives.
◦ Train staff
Provide regular education on sustainable practices and their benefits.

◦ Celebrate achievements
Recognise and reward contributions to sustainability goals.
◦ Communicate transparently
Share your goals, strategy, and progress with your patients, local community and key stakeholders. The Commission emphasises that sustainability should be embedded within health service delivery and governance rather than a standalone project. By integrating sustainability into safety and quality standards, practice teams can align with broader national objectives to help Australia meet its emissions reduction targets.
Healthcare organisations play a unique role in supporting the health of both humans and the planet. By adopting practical measures and leveraging frameworks such as the Environmental Sustainability and Climate Resilience Healthcare Module, health service providers can make significant contributions to sustainability while also improving their service delivery.
Starting small and focusing on continuous improvement can lead to long-term benefits for the environment, patients, and your organisation. Together, we can contribute to a healthier, more sustainable future for everyone.
AGPAL and QIP are leading accreditation providers across Australia’s health, community and human services sectors. The current draft of the RACGP Standards 6th edition proposes environmental sustainability accreditation requirements for general practices and AGPAL is proud to be the exclusive agency chosen to pilot the 6th edition Standards. This opportunity will provide us with unique insight into the proposed Standards’ applicability to best support practice teams during the transition process. As we await further release details, we encourage you to follow AGPAL & QIP via our social media channels for future updates:
AGPAL
LinkedIn @AGPALaccredited
Facebook @AGPALaccredited
QIP
LinkedIn @QIPaccredited
Facebook @QIPaccredited

