THE PRACTICE MANAGER






AAPM’s Professional Development Program supports and promotes members’ personal and professional growth through a system of:

CORE PRINCIPLES
QUALIFICATIONS CERTIFICATION CONTINUING PROFESSIONAL DEVELOPMENT
AAPM representation on government and industry advisory groups.
HR ADVISORY SERVICE
Comprehensive HR support and advice through telephone, email and website resources and templates.
MEMBER ASSISTANCE PROGRAM
Confidential assistance to support health and wellbeing of members.
PULSE+IT SUBSCRIPTION
Asia Pacific’s eHealth and Health IT digital platform.
MEMBERSHIP BADGE
Recognition of AAPM membership.
THE PRACTICE SPACE
Dedicated fortnightly eNewsletter providing industry updates and helpful advice.
PRACTICE MANAGER JOURNAL
AAPM’s national journal, delivered electronically to members each quarter.
Access to AAPM’s Educare program at member rates. Includes face-to-face events and a series of webinars.
Premier annual conference for Practice Management at member rates.
NETWORKING MEETINGS
Share knowledge and information. Connect with, and support your peers.
Self-guided learning through Practice Management topics.
SCHOLARSHIPS
Expand your skills through AAPM funded scholarships for selected Practice Management courses delivered though UNE Partnerships.
PRACTICE MANAGER OF THE YEAR AWARDS
Prestigious state and national awards recognise and reward a Practice Manager for their contribution to the profession of Practice Management.
Recognition of years of experience and skill development in the profession of Practice Management.
FELLOWSHIP
A prestigious honour in recognition of significant commitment and contribution to the profession of Practice Management.
Exclusive access to resources, discounts and benefits from industry partners.
Dedicated and exclusive memberonly forum to share ideas, insights, information and support.
AMBASSADORS
Support and assistance from experienced and highly qualified Practice Managers.
WEBSITE ACCESS
Access latest news, industry information, and member-only resources.


As we navigate through the last quarter of 2024, I wanted to take a moment to reflect on a fundamental aspect of our mission to support excellence in healthcare practice management.
A component of this is educating our members and our members' commitment to continual learning. It is easy to get caught up in the whirlwind of deadlines, projects and meetings, but let’s remember that education is not just a set of tasks on a checklist; it’s the cornerstone of our Association and a catalyst for personal and professional growth. Each of us plays a crucial role in fostering a learning environment, whether we are directly involved in teaching or supporting those who are.
Embracing a mindset of continual learning allows us to stay relevant,
enhance our skills whilst fostering innovation and providing personal growth. The upcoming AAPM National Conference will provide a significant opportunity for us to further our knowledge and network with peers in our industry.
As we move forward this quarter, let us keep the importance of education at the forefront of our minds. It is the foundation upon which we build our successes and the light that guides us through our endeavours.
Thank you all for your hard work and dedication to Practice Management and Health Care in Australia. Let us continue to support each other and make a difference through continual learning.
JACKIE BEER NATIONAL PRESIDENT

This addition of the Journal is a time to reflect of the recent achievements of AAPM and its members. It is always so pleasing to be able to highlight the outstanding work of our members and share these with you. In particular, I want to highlight the applications received for the Practice Manager of the Year Awards program. This year we had a sustantial and varied range of applicants that demonstrated the exceptional work and standard in our practice management community. We have announced our State Winners and will award our 2024 National Practice Manager of the Year at the National Conference, being held in Darwin, from 15 - 18 October. I hope to see many of you there and encourage you to take advantage of exploring the top end destination while there.
The 2024 Educare series has just concluded. There has been over 500 delegates that have attend from around the country, in both metro and regional locations. This year we had a full program that offered latest information and updates, along with practical tools and reminding you to look after you.
AAPM's work with the Department of Health and Aged Care continues to make traction. We participate in many consultations, workshops and meetings to ensure the voice of Practice Management is not only represented but more importantly heard.
AAPM has been represented at a series of engagements over the past few months, including, attendance and presentations at the National Primary Care Congress, the National AMA Conference, presented the inital General Practice Aged Care Incentive Seminiar with the DOHAC, participated in subsequent workshops, webinars and sessions and myself and our National President, Jackie Beer, attended the official "Principals of Healthcare Practice Management" book launch, hosted by the authors, AAPM Life Members, Gary Smith AM and Colleen Sullivan OAM.
The main focus for the National Office over the next six weeks is the build up to our National Conference. As always there is lots to be done, but I wanted to acknowledge the outstanding contribution of our National Conference Committee
who have dedicated their time to assist us in developing the program, consider keynote presenters, and work on the overarching elements associated with delivering the conference. You will see them at work at the conference as they will also be assisting with registrations, sessions and general assistance to members.
We are excited to be welcoming you to Darwin in October and invite you experience this unique conference. We will start with an official saltwater ceremony of the Tuesday evening ahead of a great program of education and social activities. If you haven't already, please make sure you take advantage of the early bird savings!
If you are not able to join us at the National Conference in person, we hope to see you at another activity soon. In the meantime, follow us on social media for updates! The team and I look forward to seeing you soon.
MIRANDA GRACE CHIEF EXECUTIVE OFFICER
Australian Association of Practice Management Ltd (AAPM) Suite 209, Level 2, 517 Flinders Lane Melbourne Victoria 3000 T 1800 196 000 E nationaloffice@aapm.org.au W www.aapm.org.au facebook.com/AAPMAustralia @AAPM_National linkedin.com/company/aapm @aapm1979






“Beyond impressive, 5 stars! DMS IT are everything they claim to be and more...”
- Hayley Hughes Practice Manager Tandem Health Labrador Medical Centre
Calls to the DMS helpdesk are answered literally within seconds, most issues are resolved within minutes
Guaranteed Level 2 or Level 3 technicians with extensive experience in Australian medical software problem resolution
Extensive experience and expertise in Australian medical software eco systems
87% of helpdesk calls resolved on the same day
81% of helpdesk calls resolved on the first call
Managed Cyber Security expertise - Security first approach with Cyber Security qualified staff
Pro-active Managed IT that is fully customised for Australian medical clinics, with High Attention to detail
DMS Private Cloud located in Melbourne and Sydney Australia at leading Tier 4 data centres with latest high performance, and high capacity Host servers

Australia for APP data sovereignty and data residency requirements?
The development of Gen AI personal assistants is a significant milestone in the development of practical productivity enhancing tools designed to automate many internal business processes, for example, the growing number of AI transcription assistants for clinicians to accurately, automatically, and unobtrusively, create consultation notes, referral letters, etc., allowing the clinician to focus on the patient interaction without having to stop and turn away from the patient to type notes. The clinician of course must check the transcription notes and validate before saving the notes to the patient record. Many Australian doctors who have embraced AI transcription technology save many minutes for each consultation and are now enthusiastic users of AI transcription. There is no going back to the back and forth pattern of patient interaction to manually typing clinical notes consulting for them!
Of course, compliance with the Privacy Act Australian Privacy Principles and stringent cyber security requirements is essential, and informed patient consent is mandatory. Discuss with your MDO Risk Advisor.
Evaluate AI transcription products by asking the following questions:
• Is the recording and transcription data processed and stored in
Is the data encrypted in transit and at rest?
• Does the AI transcription product retain the data, recordings for training of the LLM? For what time period? Why? How is the data deidentified?
• Are the recordings and transcription notes deleted from the AI transcription service after the notes have been saved?
What about enhancing the productivity of other practice workflows such as administration staff and practice managers with AI personal assistants?
Integrating Gen AI into an organisation is not a simple install and start using it situation. First however, we must focus on privacy and cyber security considerations.
In fact, data privacy and security settings must be specifically configured and set to prevent the very real risks of data leakage, privacy violations, intellectual property loss, insider threats such as employee misuse, and of course inaccurate results and cyber security risks.
For example, in the case of implementing Copilot for Microsoft 365, a staged approach is recommended by AvePoint Inc, a Microsoft 365 and Software as a Service (SaaS) specialist vendor as summarised by Figure 1:
Microsoft has addressed the critical issues of data privacy, intellectual property and security have been addressed with Microsoft Copilots–“your data belongs to you and is not used to train or to enrich the Copilot AI Large Language Models (LLMs)”, however there is very important catch – data
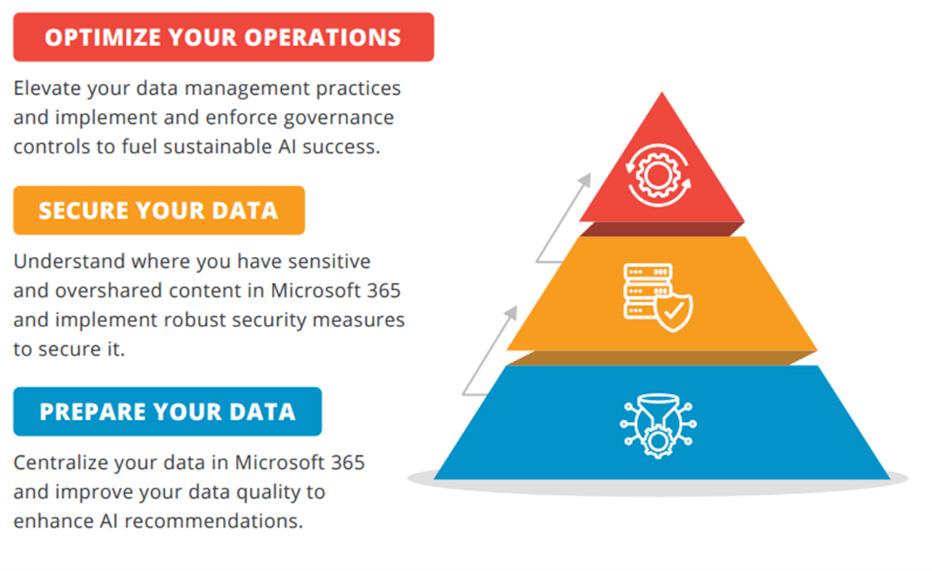
privacy and cyber security are not an out of the box given, and data governance and preparation, which includes data classification, data security, appropriate role based user access controls must be implemented before unleashing Gen AI on the organisation. The safe implementation and effectiveness of Gen AI tools such as Microsoft Copilot is very much dependant on the quality and security of the data the AI interacts with.
After the initial Microsoft Gen AI offering Bing Chat in the Microsoft search engine Bing, Microsoft have released a whole family of Gen AI personal assistants under the generic branding of Microsoft Copilot. These Copilots range from generic and free Copilots in Windows, Bing search engine and the Edge browser, to cleverly designed and customised Copilots for users performing different roles.
There are many other Microsoft Copilots, however, they are beyond the scope of this article.
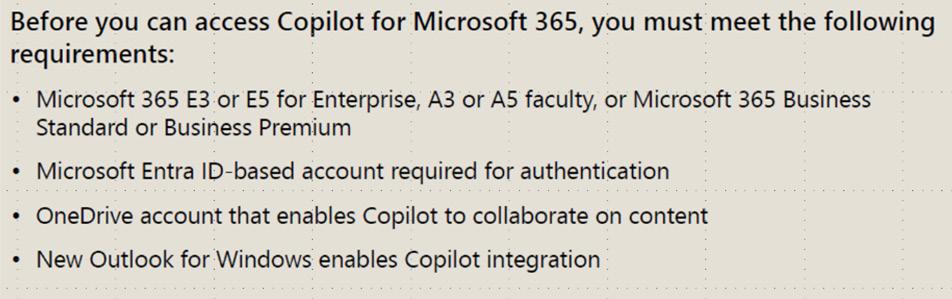
We will here focus on Copilot for Microsoft 365, which brings Gen AI productivity to those who use the ubiquitous Microsoft Office 365 (M365) applications such as Word, Excel, PowerPoint, Teams, Outlook, etc.
Now this is where any discussion about the growing family of Microsoft Copilots can get downright confusing, hence the following table:
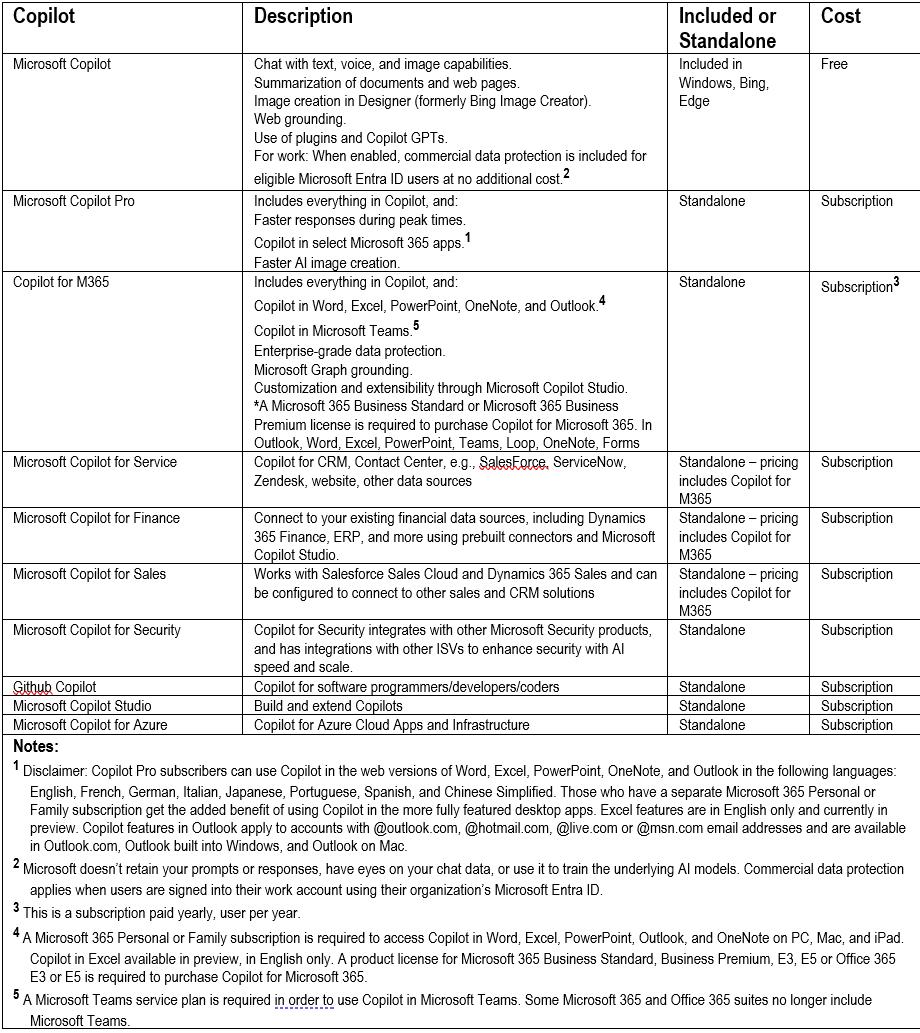
Data compiled from following source: https://www.microsoft.com/en-us/microsoft-copilot
Note the licensing requirements on the right for Copilot for Microsoft 365:
Microsoft Copilots are available as add-ons to Microsoft 365 subscriptions. To use Microsoft Copilots, you need to have a valid Microsoft 365 license, as well as a Microsoft Copilots license for each component you want to use. The Microsoft Copilots licenses are based on the number of users and the usage volume.
According to Microsoft marketing, M365 Copilot can help to “Achieve anything you can imagine with your everyday AI companion”1 Now that’s a big claim! We shall see!
Microsoft describes Copilot for Microsoft 365 “is an AI-powered productivity tool that coordinates large language models (LLMs), content in Microsoft Graph, and the Microsoft 365 productivity apps that you use every day, such
as Word, Excel, PowerPoint, Outlook, Teams, and others. This integration provides realtime intelligent assistance, enabling users to enhance their creativity, productivity, and skills.”2
The following table summarises features in Microsoft 365 apps:
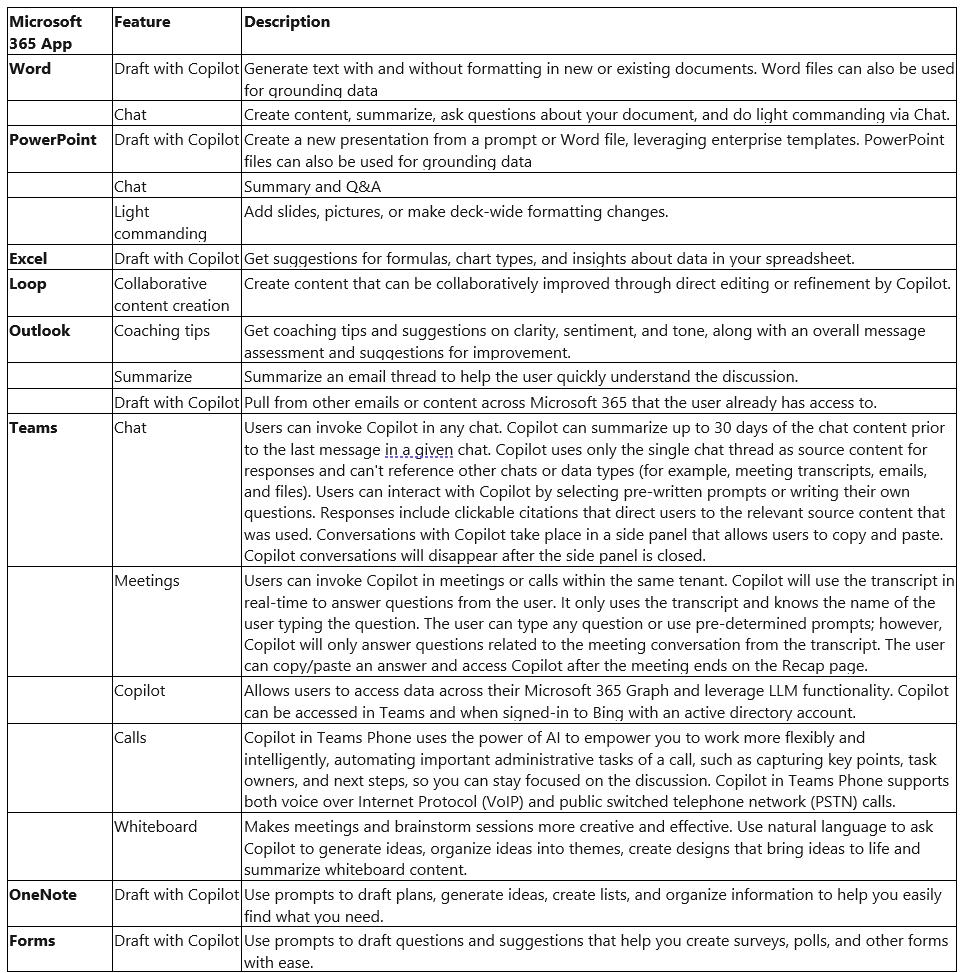
Data compiled from following source: https://www.microsoft.com/en-us/microsoft-copilot
Once the data environment has been setup (in OneDrive) you can start to use Copilot.
In Microsoft Word, for example, there are two ways to interact with Copilot:
1. The Microsoft Copilot logo / button in most of the Microsoft 365 apps is located to the right hand side of the Home Menu Toolbar RibbonClicking on the Copilot button opens a Copilot pane to the right hand side of the document where the interaction with Copilot is done via the prompts input box.
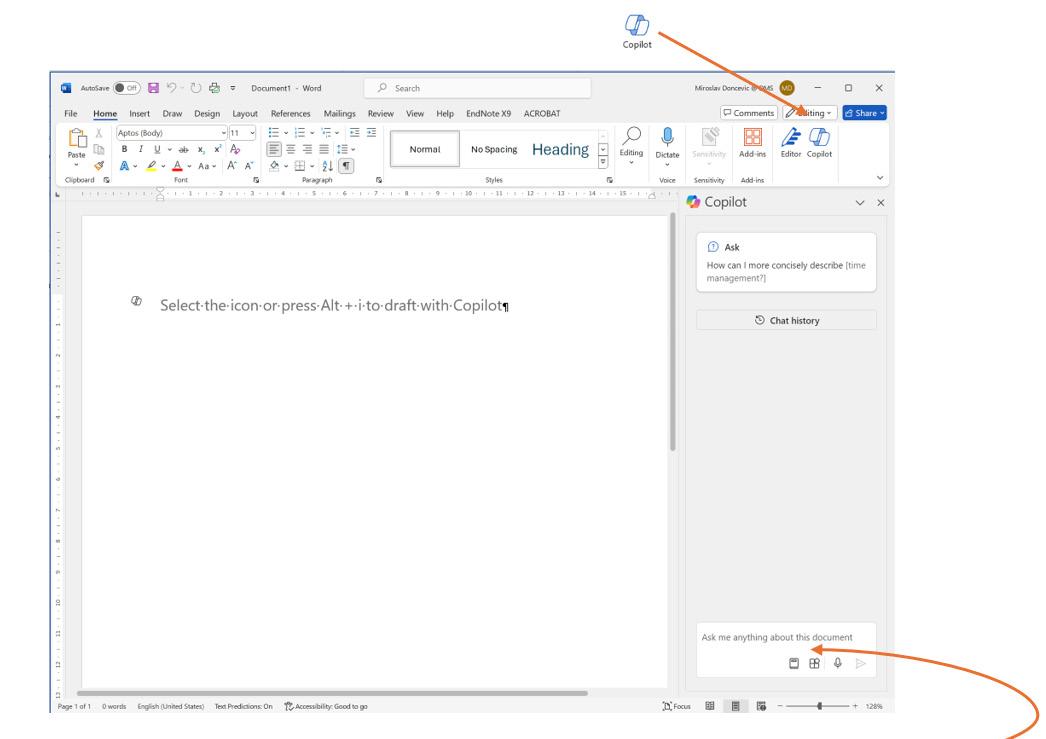
This pane is where you can ask questions, , get information about the document or from the LLM, or generate content from another external document or from other external sources into the current document, such as other data, the internet, etc. The width of this pane can made larger and adjusted left from the left boundary for easier viewing, and copying and pasting
2. The other location is the floating Copilot logo in the body of the document.
This is used to add or generate text in the body of the document: Within the other Microsoft 365 apps; Excel, Outlook, PowerPoint, Loop,
Teams, OneNote, and Forms, Copilot functions and features are specific to those apps and workflows, for example, Copilot in Teams can transcribe and summarise a meeting, brainstorm ideas for the meeting, projects, schedule meetings, etc.
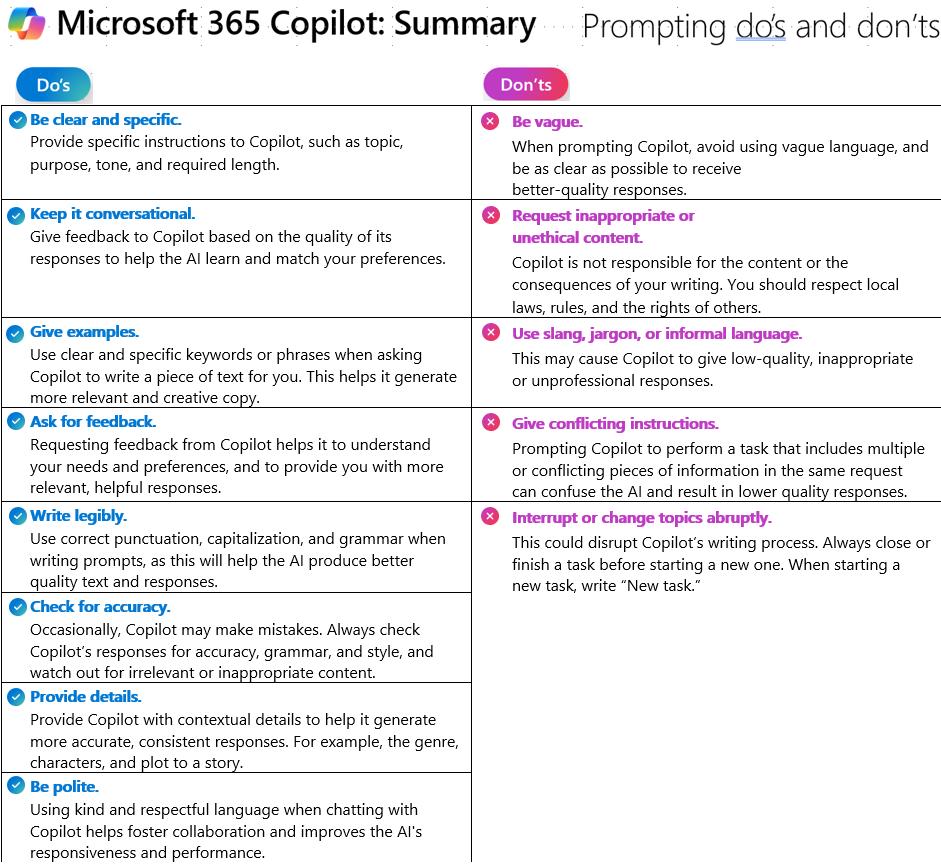
The key to successful results from Microsoft 365 Copilots is mastering prompting. On the next page is a handy chart from Microsoft for Copilot Prompting do’s and don’ts.
Using AI Copilots is a whole new way of working, so be prepared for lots of learning and experimenting. Keep asking the Coplot to refine the results is you are not happy with the output, you will be on the path to achieving the promised productivity gains. And remember to check the output!
Happy Copiloting! (Some content generated by Copilot)
MIROSLAV DONCEVIC MANAGING DIRECTOR DIGITAL MEDICAL SYSTEMS
References
1 Microsoft, (2024)., Microsoft Copilot, retrieved from https://www.microsoft.com/en-us/microsoft-copilot
2 Microsoft (2024)., Microsoft-365-Copilot-Overview, retrieved from https://learn.microsoft.com/en-us/copilot/microsoft-365/microsoft-365-copilot-overview

Practice Managers are no strangers to managing change in their practices. Avant’s risk advisors are talking to practices contemplating yet another potential change – the introduction of artificial intelligence (AI) scribes for documentation. We have found this change can raise great excitement as well as strong concerns.
It can be helpful to use a change framework that addresses both concrete issues (legal requirements, processes and systems) as well as the more intangible elements (such as culture and values). If you are considering using an AI scribe, the following change management approach can be helpful.
Start by clarifying how the AI scribe will support your practice and achieve the practice’s goals. How will it assist the practice, and how will the outputs be monitored and used?
For example, if the motivation for using an AI scribe is to save time for clinical note-taking, make sure you understand the kinds of notes it produces. Some practices have found AI scribes generate excessive notes that make it harder for doctors to find relevant details later or generate notes that leave out important information.
Being clear about your reasoning
will also help to explain the change to staff and patients.
Non-negotiable considerations include whether the AI scribe will allow you to satisfy your legal and professional obligations.
The legal obligation to protect patient privacy attaches to the practice as well as the doctor. Therefore, you need to understand enough about how the AI scribe works to be confident the practice will be able to comply with its privacy and security obligations when using it.
Make sure you check how and where data is processed and stored, and how it will be used. If the AI scribe generates documentation such as reports or referrals, consider whether you need to update or amend any processes to ensure that there will be no breach of patient confidentiality by accidently including clinically irrelevant information.
Outline in your privacy notice and policy that you are using a thirdparty AI scribe in your practice and provide your patients with information from the service provider about how they manage patient information.
Because an AI scribe ‘listens’ to a consultation between you and your patient, it would be considered a listening device under state and territory listening devices legislation. Legislation differs in each state and territory as to whether specific consent is required for a party to a private conversation to make a recording. For more information see our article Watch out for pitfalls when recording your consult –Avant by doctors for doctors. If there is an audio recording, find out whether the recording is immediately deleted or if it is held for a period of time, where it is held and whether you can access it.
Your practice’s patient cohort and approach to patient care should be considered when choosing an AI scribe. It will also help you identify and potential concerns you will need to address in your communications with doctors and patients.
Generative AI such as AI scribes currently fall outside the Therapeutic Goods Administration’s medical device regulatory processes. So, you need to be satisfied that the AI scribe is fit for purpose for use in your practice. For example, check how the AI scribe will ‘understand’ accents or languages other than standard English spoken by your patient cohort. If the AI scribe provides clinical decision support, consider the data on which this
is based. AI may be trained on limited historical datasets, which can result in biases in the outputs. For example, there may be bias based on race, gender or sexuality. It is important to be aware of these risks to ensure that AI use in healthcare does not have a negative impact negatively or entrench or worsen existing inequities.
The success of a change project can depend on how well it aligns with an organisation’s culture and structure. AI, perhaps even more than other technologies, can be polarising. In your practice, do you need to reach a consensus decision, or can individuals choose whether to use it?
Some practices have chosen to offer opt-in AI scribes, for example. If not all doctors choose to use it, be clear about how patients are informed about this. You will want to avoid patients receiving mixed messages if the first doctor they see dismisses AI as too risky and the next is using it enthusiastically.
Doctors need to be aware of, and work within the AI scribe’s limitations. While AI scribes can save considerable time, they are not a complete solution to record-keeping.
The notes produced will not capture non-verbal cues or signs and may miss important information that is discussed. In some cases it may also be inappropriate for doctors to verbalise all their observations, for example recording the BMI of a patient being treated for anorexia
nervosa or recording concerns about the cause of a patient’s injuries. AI scribes may be unable to interpret inconsistent information, for example, a patient who says they have no allergies, then later mentions an adverse reaction to a medication. Some scribes may try to fill gaps or extrapolate findings, which could lead to a misleading record.
Doctors are ultimately responsible for ensuring the record accurately reflects the consultation and must always exercise their own clinical judgment. This means they will still need time to check the record and add in additional notes or continue recording after the patient has left the room to add further observations to ensure clinical accuracy.
Doctors should treat any AI-generated outputs as drafts and ensure that they review and check that:
◦ the record is correct
◦ the AI has captured and correctly interpreted relevant details
◦ the tool has not raised an inaccurate diagnostic issue
◦ the record captures sufficient detail to justify any Medicare item numbers billed for the consultation.
Review systems and processes
Introducing AI will require you to review existing technology and other systems and processes and consider what may need to change.
One important consideration will be how well an AI scribe will integrate with your existing software. If the integration is not seamless, consider whether switching between
programs could increase the risk of errors, for example from cutting and pasting between systems. Documentation you should review includes your:
◦ Privacy policy
◦ Software governance policies
◦ Data breach policies.
Communicating change to staff and patients
Even if AI seems like a simple add-on to existing tools, bear in mind that staff may have strong views about AI and what it may mean for their jobs. Even if a change seems intuitive or incremental, it will be quicker in the long run to spend time implementing and communicating the change effectively from the start.
Assume that staff will need to be trained on how to use any AI you introduce and how to communicate with patients about it.
Consider how you plan to introduce the change to patients, and who will be responsible for documenting and recording their consent. Discussing this as a team and preparing staff with responses to potential concerns will help staff feel more confident and minimise the risks of dealing with angry or upset patients.
If you are considering introducing an AI scribe to your practice, a change management framework can help you assess and plan for the change. This involves addressing both tangible factors such as legal and compliance requirements as well as intangible elements such as cultural shifts within your practice.
Practice responsible for:
◦ ensuring compliance with privacy and security obligations
◦ providing thorough staff training
◦ developing effective policies for the use of AI
◦ amending current policies to cover the use of AI, for example privacy and data protection policies
◦ communicating with patients and informing them at the front desk about AI use in the practice
◦ managing psychosocial risks – including through poor change management or patient aggression
It is important to understand both the benefits and the limitations of AI in healthcare and foster clear communication with both staff and patients to help mitigate any potential challenges.
MS ANGELA MASON-LYNCH
GAICD, CPMAAPM, DIP PRAC MGT, FAAMP (LIFE), CERTAA, RN, JP RISK ADVISER, AVANT
Doctors responsible for:
◦ retaining full responsibility for clinical management – this cannot be delegated to the practice or AI
◦ ensuring clinical notes accurately reflect the consultation, including all clinical findings and relevant negative findings
◦ ensuring clinical notes contain sufficient detail to satisfy any Medicare item numbers billed
◦ obtaining patient consent to use the AI scribe to record or “listen to” consultations if necessary
◦ following practice policies
◦ providing feedback to management about the software and any concerns or risks
RACGP Position statement – Artificial intelligence in primary health care. April 2024. https://www.racgp.org.au/FSDEDEV/media/documents/RACGP/Position%20 statements/Artificial-intelligence-in-primary-care.pdf
Australian Medical Association. AMA position statement on AI in healthcare. 2023. https://www.ama.com.au/articles/artificial-intelligence-healthcare
Avant webinar. Ask the expert. CPD requirements, complaints and AI. 13 March 2024. https://www.youtube.com/watch?v=q5x2sjA-jMY&t=4s
Brell R. Watch out for these pitfalls when recording your consult. 17 November, 2020. Avant. https://avant.org.au/resources/watch-out-for-these-pitfalls-whenrecording-your-consult
Coiera EW, Verspoor K, Hansen DP. We need to chat about artificial intelligence. Med J Aust. 2023;219:98-100. doi.org/10.5694/mja2.51992
Tierney AA, Gayre G, Hoberman B et al. Ambient artificial intelligence scribes to alleviate the burden of clinical documentation. NEJM Catalyst. 2024:5(3). doi: 10.1056/CAT.23.0404
Verspoor K, Hansen D, Coiera E. AI is already being used in healthcare. But not all of it is ‘medical grade’. CSIRO. 21 June, 2023 https://www.csiro.au/en/news/All/ Articles/2023/June/AI-in-healthcare
Patient feedback is a cornerstone of continuous improvement and quality assurance in general practice. It serves as an essential tool for understanding patient experiences, identifying areas for improvement, and enhancing overall service delivery. For practices, integrating patient feedback into everyday operations improves patient satisfaction and plays a key role in supporting practices with their accreditation requirements under the RACGP Standards for General Practices 5th edition. This article explores the benefits of patient feedback and outlines the specific criteria for patient feedback under the RACGP Standards.
Improved patient care
Patient feedback provides valuable insights into the patient experience, highlighting what works well and what needs improvement. By actively seeking and addressing feedback, practices can identify gaps in service delivery, streamline processes, and implement changes that directly enhance patient care.
Increased patient satisfaction
When patients feel heard and see their feedback being acted upon, their satisfaction and loyalty to the practice increase. This positive relationship not only encourages
repeat visits but also promotes word-of-mouth referrals, which are invaluable for any practice.
Enhanced practice reputation
A practice that consistently seeks and responds to patient feedback builds a reputation for being patient-centred and committed to quality care. This reputation can attract new patients and help retain existing ones, contributing to the overall success and sustainability of the practice.
Staff morale and engagement
Incorporating patient feedback into practice operations can also have a positive impact on staff morale. When staff members see that their efforts are appreciated and that patient feedback is used to make constructive changes, it fosters a sense of accomplishment and engagement.
UNDERSTANDING PATIENT FEEDBACK WITHIN THE RACGP STANDARDS
Criterion QI1.2 – Patient Feedback
The RACGP Standards emphasise the importance of having a robust system for managing patient feedback. Criterion QI1.2 outlines the following requirements:
◦ QI1.2 A > Practices must collect feedback from patients, carers, and other relevant parties in accordance with the RACGP’s Patient Feedback Guide.
◦ QI1.2 B > Practices are required to analyse, consider, and respond to feedback. This involves reviewing the feedback, identifying areas for improvement, and implementing necessary changes.
◦ QI1.2 C > Practices must inform patients, carers, and other relevant parties about how they have responded to feedback and used it to improve the quality of care provided.
These criteria ensure that practices are continuously improving based on the feedback received while supporting them to demonstrate the specified accreditation requirements and enhancing patient care.
STEPS TO IMPLEMENT EFFECTIVE PATIENT FEEDBACKSYSTEMS
Establishing a feedback system
Step-by-step guide:
1. Gain access to feedback mechanisms: Access various methods for collecting feedback, such as surveys, suggestion boxes, and digital platforms. Ensure these methods are easily available to all patients. NOTE: To support the RACGP Standards requirements, practice teams must utilise RACGP-approved patient feedback tools or gain approval for a self-designed tool.
2. Promote feedback opportunities: Encourage patients to provide feedback by promoting these opportunities through multiple
channels, including the practice website, social media, and in-clinic posters.
3. Ensure confidentiality: Implement measures to ensure that all feedback is confidential and that patients feel comfortable sharing their experiences.
Training staff
Training staff on how to handle and respond to patient feedback is essential to supporting the appropriate collection and management of patient feedback. This training should cover the importance of feedback, how to encourage it, and the correct procedures for managing and acting on it.
Training tips:
◦ Conduct regular training sessions for all staff members.
◦ Provide clear guidelines and protocols for handling feedback.
◦ Emphasise the importance of a positive and constructive approach when dealing with feedback.
Analysing feedback
Data Analysis:
Collected feedback data should be comprehensively analysed to identify common themes and trends. Use this analysis to pinpoint specific areas that require improvement.
Actionable Insights:
Transform the insights gained from feedback into actionable steps to support quality improvement initiatives Develop a plan to address identified issues and track the
progress of these actions.
Completing the feedback cycle
Responding to feedback:
Always respond to patient feedback, letting them know how their input has been used to make improvements. This shows that the practice values their feedback and also enhances patient trust and satisfaction.
Communicating changes:
Communicate any changes made based on patient feedback to both patients and staff. This transparency reinforces the practice’s commitment to continuous improvement and patient-centred care.
There are many RACGP approved patient feedback tools available to support your accreditation requirements, such as CFEP Surveys’ Practice Accreditation Survey. These tools have been designed to streamline the feedback process and assist practices in collecting essential patient feedback to comply with accreditation standards.
Incorporating patient feedback into practice operations fosters a culture of continuous improvement and patient-centred care while supporting practice teams in meeting their accreditation requirements. By understanding and implementing the requirements outlined in the RACGP Standards, practice managers and GPs can enhance the quality of care, improve patient satisfaction,
and demonstrate compliance with the relevant accreditation requirements. Prioritising patient feedback ultimately leads to a more successful and sustainable practice, benefiting both patients and healthcare providers.
As part of the AGPAL Group of Companies, CFEP Surveys offers a 10% discount on Practice Accreditation Survey to AAPM members who use the code "AAPM" at checkout. Click here to find out more.
Australian General Practice Accreditation Limited (AGPAL) is a leading not-for-profit organisation, established in 1997 by industry members, as a provider for general practice accreditation and quality improvement services within Australia. AGPAL is part of the AGPAL Group of Companies. Here at AGPAL, we are dedicated to servicing and supporting general practices, Aboriginal medical services, medical deputising services, after hours services and Royal Flying Doctor Services throughout their accreditation and quality improvement journeys.


Meet Lyrebird Scribe. A fully integrated generative AI tool that makes taking clinical notes a breeze.
Now integrated with Bp Premier.
While you focus on your patient, Lyrebird is listening for all the relevant information to generate your notes within seconds. Best Practice Software has partnered with Lyrebird Health, the creators of Lyrebird Scribe, an artificial intelligence (AI) transcription tool specifically designed for healthcare.
This collaboration aims to streamline clinical workflows, enhance patient care, and provide healthcare professionals with cutting-edge tools to optimise their practice. Not only does Lyrebird learn your documentation style, but it also generates any document you need within seconds. Customisable and learning over time, Lyrebird structures your letters and assessments the way you need them to be.

With this integration, healthcare providers can significantly reduce administrative burdens and spend more time on patient care. Lyrebird Scribe ensures that documentation is accurate, compliant, and efficiently integrated into the Best Practice Software platform, reducing errors and improving overall workflow efficiency.




Is your website accessible to everyone, including individuals with disabilities?
Imagine a patient trying to book an appointment online, only to find that the website’s design prevents them from doing so due to their visual, auditory, cognitive, or motor impairment. This creates a barrier for them and means your practice loses a potential patient.
Do you want to get on the right side? Check your website against Web Content Accessibility Guidelines, or WCAG. Developed by The World Wide Web Consortium (W3C), WCAG are a globally accepted set of guidelines developed to provide a single shared standard for web content accessibility that meets the needs of individuals, organisations, and governments.
If you operate in Australia, the Federal Disability Discrimination Act 1992 protects people from discrimination based on disability. In particular, Section 24 explicitly prohibits providers of goods, services, and facilities from discriminating against users based on their disability.
So, if your clinic’s website is not accessible, your clinic may be failing to provide its services to a person with a disability. If a person with a disability cannot access the service through the website just like other people without disabilities can, this could conceivably constitute discrimination. There have been a few big cases in Australia, like Coles and ABC, that were raised on the basis of discrimination online.
Besides not meeting the Disability Discrimination Act 1992 requirements, meeting web accessibility standards makes good business sense for private businesses. People with disabilities represent a significant portion of the population. One in seven people under 64 years and half of the population above 64 have a disability (https:// australiandisabilitynetwork.org.au/ resources/disability-statistics/).
By ensuring your website is accessible, you open your services to a wider audience. This inclusivity can lead to increased patient satisfaction, loyalty, and referrals. Additionally, search engines factor in user experience when assessing rankings, meaning that accessible websites often perform better in search engine rankings.
Increasing your site’s accessibility will enhance your online presence and potentially attract more patients. Below is a list of no-cost steps you can take to run your website accessibility validation:
Use Online Accessibility Tools:
◦ WAVE is a website where you enter a URL, and it will analyse the page for accessibility issues.
◦ axe Accessibility Checker is a Chrome and Firefox browser extension that allows you to run accessibility tests directly on your website.
◦ Keyboard Navigation Test: Manually test your website by navigating using only the keyboard. Ensure all interactive elements (links, buttons, forms) are accessible using the Tab key and can be activated with the Enter key.
◦ Screen Reader Testing: Use a screen reader (like NVDA or VoiceOver) to navigate your website. This will help you identify issues with content structure and labelling.
◦ Colour Contrast Checker: Use a colour contrast checker tool (like the WebAIM Contrast Checker) to ensure your text has sufficient contrast against its background.
Privacy law is constantly evolving and crucial for Practice Managers to understand their legal obligations to protect their practice from reputational damage and costly penalties.
In this article, we cover privacy requirements, breach protocols, safe data collection and storage, data usage, and key privacy legal tips to help you navigate this complex area.
In Australia, any data that is “personal information” falls within the scope of Australia’s privacy law framework. Personal information is defined as ‘information or an opinion about an identified individual, or an individual who is reasonably identifiable.’ This can include a person’s:
◦ name;
◦ phone numbers;
◦ drivers licence details;
◦ health information; and
◦ religious beliefs.
The Privacy Act 1988 (Cth) sets out requirements surrounding personal information and sensitive information. All medical businesses must be compliant with this law.
Currently all businesses with an annual turnover greater than $3,000,000, all medical businesses (regardless of turnover), and certain other types of entities classified as Australia Privacy Principles Entities (APP Entities) are required by law to have a privacy policy. This policy must be freely available, most commonly on a website, and must be tailored to reflect the operations and practices of the business.
A privacy policy informs third parties of:
◦ what personal information you collect;
◦ how that information is held;
◦ what you use that information for;
◦ whether you will disclose personal information to any overseas recipients; and
◦ other required matters.
The Privacy Act 1988 (Cth) includes a number of requirements around the collection and storage of personal and sensitive information. Unless an exception applies, APP Entities should only collect personal and sensitive information with consent and only if collection of that information is reasonably necessary for or directly related to its functions or activities.
AAP Entities must take reasonable steps to ensure the personal information they hold is protected from misuse, interference, loss, unauthorised access, modification, and disclosure. Good data hygiene and regularly updated policies and procedures around collecting and storing personal information are necessary to ensure compliance.
An APP Entity is required to destroy or de-identify information when it holds personal information about an individual; and
1. the business no longer needs the information for any purpose for which the information may be used or disclosed by the business under the Privacy Act;
2. the information is not contained in a Commonwealth record; and
3. the business is not required by or under an Australian law, or a court/tribunal order, to retain the information.
APP Entities must notify the Office of the Australian Information Commissioner (OAIC) if they have reasonable grounds to suspect that an Eligible Data Breach has taken place. An Eligible Data Breach is where there is unauthorised access to, disclosure of, or loss of, personal information held by an APP Entity and such access, disclosure, or loss is likely to result in serious harm to
individuals the information relates to.
Between July 2023 and December 2023 more than 20% of data breach notifications were made by Health Service Providers, more than double every other sector (Australian Government, 2024). It is vital for health and medical practices to have a carefully considered procedure in place for dealing with a data breach before it happens.
A report to the OAIC does not need to be made if the entity takes action which reasonably prevents the serious harm. This can include reaching out to any persons affected and informing them of the scope of the breach and what actions they should take to protect themselves. However, a decision not to report a data breach on this basis should be made carefully.
In the event of a data breach, the business must as soon as practicable provide a statement to the Privacy Commissioner sharing:
1. the identity and contact details of the business;
2. a description of the eligible data breach that the business has reasonable grounds to believe has happened;
3. the particular information concerned;
4. recommendations about the steps that individuals should take in response to the eligible data breach that the business has reasonable grounds to believe has happened; and
5. any other required information (Data Breach Statement)
Businesses need to take reasonable
steps to provide the information in the Data Breach Statement as soon as practicable after it is prepared:
1. to either all individuals whose personal information was the subject of the data breach;
2. to either all individuals who are at risk from the eligible data breach; or
3. if neither option above is practicable, by publishing a copy of the Statement on its website and taking reasonable steps to publicise the contents of the Statement.
Direct marketing involves using personal information to promote goods and services when communicating directly to an individual. There are only certain circumstances where AAP Entities can use an individual’s personal information for direct marketing purposes.
APP Entities can only use or disclose the personal information of a person for the purpose of direct marketing if:
1. the business collected the information from that person;
2. that person would reasonably expect the organisation to use or disclose the information for direct marketing purposes;
3. the business provides a simple way for the individual to easily request not to receive direct marketing communication from the business; and
4. the person has not made that request to the business.
Sensitive information, which includes medical information, is subject to more strict requirements than other personal information and greater care should be taken with this information.
Here are 10 tips for your business to follow to assist in your compliance with the Privacy Act 1988 (Cth).
1. Have an up to date and accurate privacy policy that you regularly review.
2. Seek informed consent before collecting personal information.
3. Take a conservative approach and lodge a report to the OAIC if you are unsure if a data breach has occurred.
4. Ensure good housekeeping measures are in place to ensure unnecessary personal data is not being collected or stored.
5. Have a plan in place in the event of a data breach.
6. Ensure staff are appropriately trained on cybersecurity and privacy issues.
7. Be vigilant in only providing personal information to third parties who are trusted and under an obligation not to breach the Privacy Act, or similar legislation in their country.
8. Avoid using personal information in AI prompts or otherwise in material that AI learns from
9. Ensure you have systems in place to guard against bad actors and human error.
10. Make sure you are only engaging in permitted direct marketing
activities and have a simple means for individuals to opt out.
Ensuring you are compliant with privacy laws is a proactive and crucial step in safeguarding your business. We encourage you to seek professional legal advice around your practice’s needs with regards to privacy.
Australian Government. (2024, February 22). Notifiable data breaches report July to December 2023. Retrieved from Australian Governement Office of the Australian Information Commissioner: https://www.oaic.gov.au/privacy/ notifiable-data-breaches/notifiabledata-breaches-publications/ notifiable-data-breaches-reportjuly-to-december-2023
Hillhouse Legal Partners has extensive industry knowledge and expertise in the medical sector working with clients on these issues.
To discuss your practice’s privacy requirements, please contact Craig Hong, Director, Hillhouse Legal Partners on (07) 3220 1144 or email craig@hillhouse.com.au. As a special benefit to AAPM members, we offer a no-obligation 30 minute virtual consultation regarding privacy policies issues in your practice.
Our legal team specialises in providing expert legal advice to businesses and individuals in the medical sector.
We understand that in practice management, you work across a number of legal issues and as a full-service law firm, we can assist you and your practitioners with all their business and personal legal needs.
We have a proven track record of supporting businesses at each stage of a practice’s lifecycle, from establishment through to structuring and growth and finally through to business succession events. Our extensive experience allows us to provide tailored legal advice and assistance during all stages.
It is our mission to be your trusted legal partner to help you navigate the complex legal landscape of the health and medical industry.
Corporate Advisory
Corporate & Commercial
Employment & Industrial Relations
Intellectual Property & Technology Litigation & Dispute Resolution
Property & Projects
Private Conveyancing
Family Law
Wills, Estates & Trusts
We understand the time constraints faced by practice managers and offer meetings after hours in person, online or on location to accommodate your schedule. Contact our team today to schedule a consultation and receive expert advice on all your legal needs.

Zac Herps, Managing Director
Zac provides strategic advice and solutions to some of the firm’s largest and most prominent clients. With a business and commercial focus, Zac partners with clients to support them in achieving their career and personal objectives. He offers a flexible and responsive service, frequently meeting clients at their business premises, after hours.
0407 347 484 zac@hillhouse.com.au



Medical Practice Jobs ensures your job ad reaches thousands of medical practice staff across multiple job boards, helping you find and hire your ideal candidate.
Medical Practice Jobs, your ultimate specialist recruitment and HR services partner. With flexible, discounted options we can help write and post your job ad, manage parts of your recruitment process where you require support, or partner with you to deliver the entire recruitment process.

We are experts in
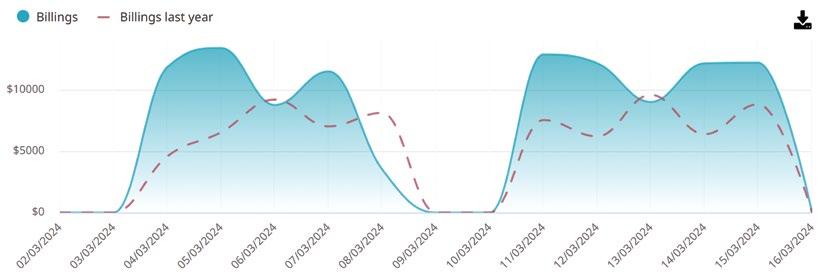
No work. No Spreadsheets. No uploads. Just simple, actionable insights from Cubiko. Book a




MGTcare is an Integrated SaaS to streamline workflows by saving time and money to improve productivity, efficiency and profitability within the primary care organizations. Increase







Register today and take advantage of the Early Bird savings!
Early Bird closes Friday 13 September REGISTER HERE
15 to 18 October 2024
Darwin Convention Centre, Northern Territory