THE PRACTICE MANAGER





AAPM’s Professional Development Program supports and promotes members’ personal and professional growth through a system of:

CORE PRINCIPLES
QUALIFICATIONS CERTIFICATION CONTINUING PROFESSIONAL DEVELOPMENT
AAPM representation on government and industry advisory groups.
HR ADVISORY SERVICE
Comprehensive HR support and advice through telephone, email and website resources and templates.
MEMBER ASSISTANCE PROGRAM
Confidential assistance to support health and wellbeing of members.
PULSE+IT SUBSCRIPTION
Asia Pacific’s eHealth and Health IT digital platform.
MEMBERSHIP BADGE
Recognition of AAPM membership.
THE PRACTICE SPACE
Dedicated fortnightly eNewsletter providing industry updates and helpful advice.
PRACTICE MANAGER JOURNAL
AAPM’s national journal, delivered electronically to members each quarter.
Access to AAPM’s Educare program at member rates. Includes face-to-face events and a series of webinars.
Premier annual conference for Practice Management at member rates.
NETWORKING MEETINGS
Share knowledge and information. Connect with, and support your peers.
Self-guided learning through Practice Management topics.
Expand your skills through AAPM funded scholarships for selected Practice Management courses delivered though UNE Partnerships.
PRACTICE MANAGER OF THE YEAR AWARDS
Prestigious state and national awards recognise and reward a Practice Manager for their contribution to the profession of Practice Management.
Recognition of years of experience and skill development in the profession of Practice Management.
FELLOWSHIP
A prestigious honour in recognition of significant commitment and contribution to the profession of Practice Management.
Exclusive access to resources, discounts and benefits from industry partners.
Dedicated and exclusive memberonly forum to share ideas, insights, information and support.
AMBASSADORS
Support and assistance from experienced and highly qualified Practice Managers.
WEBSITE ACCESS
Access latest news, industry information, and member-only resources.


As we reflect on the past year, I am filled with immense pride and gratitude for all that we have accomplished together.
A highlight was certainly our National Conference in Darwin, which proved to be an outstanding success. With inspiring keynote speakers, thought-provoking sessions, and invaluable networking opportunities, the conference demonstrated the strength and unity of our national health practice management community. It was a remarkable gathering that showcased our collective commitment to advancing healthcare, supporting one another, and shaping the future of the industry.
It was a privilege to engage with so many passionate individuals dedicated to leading, promoting and supporting excellence in the profession of practice management.
I want to extend my heartfelt thanks to each of you who attended, contributed, and engaged in meaningful discussions. Your passion, expertise, and dedication were what made the conference such a powerful experience. Together, we have set the stage for continued progress in the year ahead, and I look forward to all that we will achieve together as we build on the momentum created this year.
As we approach the holiday season, I want to take this opportunity to wish you all a safe and joyful Christmas and a prosperous New Year. May this festive season bring you peace, rest, and time to reflect on the positive impact you have made in the lives of those you serve. I hope that you return in the New Year rejuvenated and ready to embrace the challenges and opportunities that lie ahead.
Thank you for your continued dedication to our mission and for being such an essential part of our vibrant community. I look forward to seeing you at future events and working
together to create a healthier and more connected world.
Warmest wishes to you and your loved ones for a Merry Christmas and a Happy New Year!


When writing for this edition of the Practice Manager Journal, I was reflecting on the achievements of the Association, which is a result of you, our members, industry partners, and the dedicated team at the AAPM National Office.
The Australian Association of Practice Management (AAPM) has had a remarkable year in 2024, continuing to support and advance the profession of practice management across Australia. Here are some of the key ways AAPM has served its members this year:
AAPM has placed a strong emphasis on education and professional development. The highlight of the year was the AAPM National Conference held in Darwin from 15 to 18 October. This event featured a variety of educational sessions, including plenary and concurrent options, tailored to different stages of a Practice Manager's career and relevant to various practice specialties. The conference provided a platform for members to gain insights from industry leaders, network with peers, and stay updated on the latest trends and best practices in healthcare management.
Throughout 2024, AAPM has continued to offer a schedule of webinars covering a wide range of topics pertinent to practice management. These webinars have been instrumental in providing members with flexible learning opportunities, allowing them
to stay informed about changes in healthcare, and effective management strategies.
AAPM has been active in advocating for the interests of Practice Managers. The association has engaged with policymakers to ensure that the voices of our members are heard in discussions about healthcare policy and reform. This advocacy work has been crucial in shaping a healthcare environment that supports effective practice management and optimal patient outcomes.
AAPM has continued to support its members, through dedicated offerings including access to a comprehensive HR Advisory Service, Member Assistance Program and Recruitment Services. These resources have been invaluable in helping members navigate the complexities of practice management, especially in the face of ongoing challenges.
AAPM has facilitated networking opportunities throughout the year, both in-person and virtually. These events have allowed members to connect with each other, share experiences, and build professional relationships that enhance their careers and the practice management community as a whole.
In 2024, the Australian Association of Practice Management has demonstrated its unwavering commitment to supporting its members through education, advocacy, and support services. By fostering a strong
community of Practice Managers and providing them with the tools and resources they need to succeed, AAPM continues to play a pivotal role in the advancement of healthcare practice management in Australia.
As we head into the festive season I hope that you, your families and communities are able to take time to rest and relax, before we head into an exciting 2025.
MIRANDA GRACE CHIEF EXECUTIVE OFFICER


Australian Association of Practice Management Ltd (AAPM) Suite 209, Level 2, 517 Flinders Lane Melbourne Victoria 3000 T 1800 196 000 E nationaloffice@aapm.org.au W www.aapm.org.au facebook.com/AAPMAustralia @AAPM_National linkedin.com/company/aapm @aapm1979


Whether you’re looking to develop or grow a successful practice, optimise your business structure, or secure your financial future, we’re here to guide you with practical and individualised support.
As the national partner of AAPM, members benefit from complimentary consultations with our advisors. We’re here to help.








Setting up or revisiting the structure of a healthcare practice is a big decision for any practice manager. Getting the structure right not only boosts day-to-day efficiency but also tackles key areas such as risk management, asset protection, tax savings, and succession planning.
In this guide, we’ll walk you through the essentials of structuring for healthcare practices and provide practical tips to keep your practice aligned with your long-term goals.
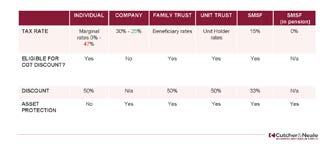
When setting up a new practice, choosing the right structure is key. Each option - sole trader, partnership, company, trusts, or selfmanaged super funds (SMSF) - comes with its own set of pros and cons, especially when it comes to asset protection, tax benefits, growth potential, and succession planning.
Here’s a quick rundown of the main structures:
◦ Sole Trader: Easy and quick to set up, but it offers limited asset protection and can have higher tax rates.
◦ Partnership: Great for sharing decisionmaking and profits, though it brings joint liability risks.
◦ Company: As a separate legal entity, it provides asset protection and tax benefits, although setup and maintenance costs are typically higher.
◦ Trust: Effective for income distribution and asset protection, but the added complexity can drive up administrative costs.
◦ Self-Managed Super Fund (SMSF): While primarily a retirement savings tool, and
SMSF can own business premises or other assets, providing unique tax advantages and flexibility for long-term planning.
It’s a good idea to work with an experienced advisor to weigh up these options and find the structure that best supports your
up assets or accumulated wealth, think about ways to shield them from potential creditors. Recent changes to Capital Gains Tax (CGT) rollovers, for example, might open up new restructuring options that weren’t available before.
goals. You’ll want to look beyond just asset protection and tax benefits - also consider whether your structure assists or hinders the introduction and retirement of practice owners.
Even if your practice is running smoothly under its current structure, it’s important to regularly check if it’s still the right fit. Market shifts, legislative updates, and changes in financial circumstances can all impact whether your setup is still working in your favour. A periodic review can help you adjust to these changes, stay compliant, and take advantage of any new tax or business developments.
Here are some key areas to think about:
◦ Risk Management: Is the current directorship setup still the best way to manage risk? Have any directors acquired new assets that need protection? And do you have a plan if any directors can’t fulfill their roles?
◦ Asset Protection: If your practice has built
◦ Planning for a Future Sale: If selling the practice is something you might consider down the road, having the right structure can make a big difference. Simple adjustments like tidying up shareholdings now could help you qualify for Small Business CGT Concessions when the time is right.
Regular check-ins on your structure keeps your practice flexible, protected, and ready for whatever comes next!
Setting up a flexible structure is important, but it can sometimes add extra layers of complexity. For instance, if your practice is set up with multiple entities, you might end up juggling several accounting files and doing frequent reconciliations to get a clear picture of your performance.
Here’s how to make things easier:
◦ Automate Wherever You Can: Use software that combines accounting, operations, and payroll in one place to

cut down on manual entry and streamline reporting.
◦ Centralise Information for Real-Time Insights: Look into tools that pull data from different sources, so you get a single, clear view of your practice’s financial and operational health.
◦ Review and Update Regularly: Check in on your structure periodically. Sometimes, arrangements set up for specific needs in the past may no longer be necessary.
By focusing on these efficiency tips, practice managers can ease the admin load and free up more time for patient care and strategic planning.
Getting your business’ structure right is also key when it comes to succession and estate planning. If you’re thinking about selling or passing on your practice down the line, make sure your personal and business assets are kept separate. The right setup can make the transition smooth, whether you’re passing it to family, associates, employees, or an outside buyer.
It’s also worth considering what would happen to the practice if something unexpected happens. Having a clear plan for who will take over control and decisionmaking can give you peace of mind and help secure the future of the practice.
If your practice runs through a Trust, it’s a good idea to review the Trust Deed regularly. This helps keep everything aligned with current laws and your practice’s goals. Tax laws can change, which might impact how income and capital are distributed in a taxfriendly way. By reviewing the deed, you can spot any updates required to keep things running smoothly and achieve the outcomes you want or intend.
The value of working with an advisor goes way beyond the initial setup - ongoing advice can be essential to keep your structure aligned with your practice’s changing needs.
Advisors can help you navigate:
◦ Business sustainability (or viability) challenges
◦ New tax laws and concessions that might create new structuring opportunities
◦ Registration requirements and licenses for any new services or expansions
◦ Insurance needs to keep your business and stakeholders protected
By actively managing your practice’s structure, you’re better equipped to handle risks, protect your assets, and adapt quickly as things change.
A well-structured practice isn’t just about smooth operations; it also safeguards both your personal and professional interests. Regularly reviewing your structure ensures you stay on top of legislative changes and can take advantage of any tax savings and asset protection options available. Don’t let your business structure become outdatedembrace regular check-ins to keep it aligned with your goals.
If you’d like help with setting up or reviewing your practice’s structure, reach out to a qualified advisor who can guide you through the complexities and help set your practice up for long-term success.
For more detailed support on business structuring and related services, contact the experts at Cutcher & Neale.
Speak to one of our advisors today at 1800 988 522 or medical@cutcher.com.au
The information in this publication contains general advice only. It has been prepared without taking your personal objectives, financial situation or needs into account. You should consider whether the information contained within this publication is appropriate for you. Where we refer to a financial product you should obtain the relevant Product Disclosure Statement or offer document and consider it before making any decision about whether to acquire the product.

PARTNER, CUTCHER & NEALE SPECIALIST MEDICAL SERVICES


Seeking GP Practice Managers to participate in a national research program.
Are you involved with decision-making about the adoption of digital technologies at your GP Clinic? We are interested in understanding the types of digital technologies you use in your GP practice, how decisions were made to use them at your clinic and how you evaluate them.
This study involves completing an online survey, and if interested, an interview with one of our researchers from The University of Queensland. Those who complete the survey can opt to receive a benchmarking report about their clinic. Our overall goal is to determine how to enhance primary healthcare services to be more efficient and person-centred using digital technologies. This research is being conducted with funding from the Australian Research Council, Australian Association of Practice Management (AAPM), the Australian Primary Health Care Nurses Association (APNA) and Inala Primary Care. Don’t miss this chance to make a difference to the future of primary care.
Find out more here: https://survey.app.uq.edu.au/P2S2-Clinic-performance-and-digital-technologies


Casual employment is commonly used within healthcare to manage fluctuating patient demand and staffing requirements. It provides flexibility for both employers and employees, with no obligation for ongoing work or guaranteed hours. Casual employees have the right to accept or decline shifts. As a result, their working hours can vary considerably, depending on the immediate needs of the practice or healthcare facility.
As a Practice Manager responsible for overseeing casual staff, it is essential you fully understand the legal and operational aspects of casual employment. This includes managing employees' rights to flexibility, recognising the entitlements that come with casual loading (compensation for the lack of leave and job security), and ensuring adherence to conversion rights for long-term casuals. Having a clear grasp of these factors ensures you can manage your workforce efficiently while maintaining compliance with legal obligations.
The following article provides an overview of casual employment and its key considerations.
An employee is categorised as casual when they start employment if there is no firm advance commitment to ongoing work, and they are entitled to receive a casual loading or specific casual pay rate.
A casual employee is offered shifts by an employer on an “as-needed” basis. Under the Health Professionals and Support Services Award 2020 (HPSSA) and Nurses Award 2020 (Nurses Award), casual employees must receive a 25% loading on top of the minimum hourly rate applicable to their classification.
The loading compensates for the lack of paid entitlements and notice of termination.
A casual employee’s shift must be at least 3 hours, the exception being cleaners employed in private medical practices who can be engaged for 2 hours. Under the Nurses Award, casual employees must be paid for a minimum of 2 hours’ for each engagement.
How casual is different to full-time or part-time employment?
Full-time employees generally work an average of 38 hours per week, have access to paid leave, and receive and must provide notice when terminating the employment relationship.
Part-time employees work fewer than 38 hours on a regular schedule. They receive the same entitlements as full-time employees but on a pro rata basis.
Casual employees, as mentioned, have no guaranteed hours or paid leave, but are compensated with higher pay, via casual loading.
Under the National Employment Standards, casual employees receive:
◦ Pathways to becoming a permanent employee either via casual conversion or the new employee choice pathway – more on this later.
◦ 2 days unpaid carer’s leave per occasion
◦ 2 days unpaid compassionate leave per occasion
◦ 10 days paid family and domestic violence leave annually
◦ Unpaid community service leave
◦ Receive a 25% casual loading
◦ Access to long service leave depending on
Casual employees can also request flexible working arrangements and take unpaid parental leave if they:
a. Have been employed as a casual employee on a regular and systematic basis for a period of at least 12 months; and
b. There is a reasonable expectation that the casual will continue to be employed on a regular and systematic basis.
A casual employee can change to permanent employment at any time if both the employer and employee agree. Casuals can also move into full-time or part-time employment through ‘Offers and Requests for Casual Conversion’ or via the new ‘Employee Choice Pathway’.
Offers and Requests for Casual Conversion applies to casuals employed before 26 August 2024. Large employers, being employers with more than 15 employees, must make a written offer to convert a casual employee who commenced prior to 26 August 2024 to permanent employment within 21 days after a casual’s 12-month anniversary if they:
a. have worked a regular pattern of hours on an ongoing basis for the past 6 months ;and
b. could continue to work these hours as a permanent employee without any significant changes.
c. For a small business, the employee can make a request at 12 months if they meet the above criteria, and the employer must respond within 21 days. This casual conversion pathway to permanent employment will continue to be available for casuals until 26 February 2025 (26 August 2025 for small businesses).
Meanwhile, the employee choice pathway allows eligible casuals to notify their employer


in writing of their intention to change to permanent employment. To be eligible, casual employees:
a. need to be employed by the employer for at least 6 months (12 months if employed by a small business);
b. have a regular pattern of hours; and
c. can continue to work these hours as a permanent employee without any significant changes.
The employee choice pathway applies to casuals employed on or after 26 August 2024.
A casual employee who has been employed on a regular or systematic basis may be eligible for unfair dismissal, and can raise the claim if their employment was terminated for harsh, unjust or unreasonable reasons.
Meanwhile, all casual employees have access to general protections. General Protection provisions within the Fair Work Act 2009 protect employees from adverse action for a prohibited reason. For instance, an employer cannot terminate a casual employee for exercising a workplace right, such as the right to raise a grievance.
In summary, casual employment is designed to provide flexibility for both employees and employers, but it comes with tradeoffs. Whilst casual employees do not have the same level of job security as permanent employees, they are covered by general protections and may have access to unfair dismissal claims if they are regular and systematic employees.
If you need assistance in relation to employee wellbeing, or have any questions about this factsheet, please contact the
AAPM HR Advisory Service
Phone: 1800 196 000
Email: HRadvisoryservice@aapm.org.au

Medical Practice Jobs ensures your job ad reaches thousands of medical practice staff across multiple job boards, helping you find and hire your ideal candidate.
Medical Practice Jobs, your ultimate specialist recruitment and HR services partner. With flexible, discounted options we can help write and post your job ad, manage parts of your recruitment process where you require support, or partner with you to deliver the entire recruitment process.

We are experts in

A case of mistaken identity – or something more sinister?
A woman in her early 30s presented to an appointment claiming to be Sarah Long. Sarah was a patient of the practice but attended infrequently. The patient said she had fallen on her wrist and it was very painful. The GP referred her for an Xray, prescribed some analgesia and scheduled a follow-up appointment. When the practice contacted Sarah to confirm the follow-up appointment, she knew nothing about the consultation and said she had not been to the practice for over six months. While this is a fictional scenario, similar cases have occurred.
Mistakes can happen. Patients can have the same name. Records can be confused. However medical identity fraud, where someone deliberately impersonates another patient, has been recognised as an issue for some time in the United States. Australia is also starting to see cases.
There could be many reasons for this deception. Understanding some of the motivations can help you and your practice team be more alert to this issue and take steps to prevent it.
An individual may be using someone else’s Medicare card or insurance information for health treatments they cannot access, cannot afford, or prefer not to pay for.
Data from the United States suggests that lack of access to affordable healthcare may underlie cases of patient impersonation there. We have also seen patients without documentation or access to Medicare presenting to clinics in Australia.
The Australian Institute of Criminology’s regular survey on identity crime in Australia
has begun reporting instances of medical identity fraud. In the 2023 bulletin on identity crime a small number of respondents said they had received a medical bill for a service they did not receive. Others discovered fraudulent claims on their health insurance when they were told they had reached their benefit limits and had their own claims rejected.
Patients with drug-seeking behaviours may be using someone else’s identity to try to gain access to drugs of addiction. Their own identity may be flagged on a real time prescription monitoring database, or they may be using multiple different identities to avoid prescribing limits. Patients may also use someone else’s identity as a way of gaining access to medications at a lower price or with a subsidy.
An individual may use a false identity to avoid having a condition on their own health record, if the condition is reportable or could affect insurance or limit professional opportunities.
An impersonator may also be seeking to get information about someone to harm them personally.
In the scenario above, the motivations of Sarah’s impostor were never clear. It was possible she was an ex-partner seeking access to confidential health information. Or she may have been posing as a known patient to try to access pain medication, as the practice had a clear policy of not prescribing drugs of dependence to patients at the first consultation.
Whatever the reasons for the theft, the fall-out for patients whose identity has been stolen can be catastrophic.
Individuals may face huge medical bills with consequences for their credit ratings and access to finance. The US media, for example, recently reported on a case where a woman was arrested after incurring over $500,000 worth of medical bills in someone else’s name. Her victim had been battling for years to dispute the bills and restore her credit rating.
Your practice may be breaching a patient’s privacy if you give out healthcare information to someone impersonating them. For both practices and individuals, the potential safety risks are even more concerning. Victims of medical identity theft have reported experiencing misdiagnosis and treatment delays. Some report living in fear of being given the wrong blood type or counterindicated medication due to inaccurate information in their patient record.
Some frauds may be very elaborate and hard to detect. Other reported cases involve individuals taking advantage of busy clinics or practices and insufficient identity checks. Revisiting your privacy and security processes may help avert a fraud.
Check that your processes for identifying patients are clear and ideally use three identifiers. Remind staff why it is important to confirm a patient’s identity each time they visit. For more information see the RACGP Standards for General Practices 5th edition. Check your processes for communicating with patients electronically to make sure you are not accidentally disclosing information that could be used by an impostor. For more information see Avant’s factsheet on email communication with patients

Make sure staff are also aware of patient privacy at the reception desk and do not inadvertently disclose identifying information where it could be read or overheard.
Patients whose identity has been stolen say it can involve years of work and anxiety to have their medical records cleared of their impostor’s information. If you become aware that a patient’s medical records have been compromised, you will usually need to take several steps:
◦ Copy any information relating to the impostor into a new ‘unknown patient’ record.
◦ This is one situation where it would be appropriate to delete, rather than striking through, the inaccurate information in the ‘real’ patient’s record. Once the imposter information has been transferred to the ‘unknown patient’ record or other location, add a note explaining what happened. For more information see Avant’s resources on correcting records
◦ If the real patient is unaware of the issue, notify them and keep them informed.
◦ Contact any other providers such as radiology, pathology or specialists and withdraw the referral.
◦ Cancel any prescriptions and follow the procedures for reporting prescription fraud in your state.
◦ If test results were ordered and require follow-up care, the ordering GP remains responsible. See Avant’s Patient followup and recalls factsheet. However, if the patient provided incorrect contact details, follow-up may not be possible. If this is the case, contact your MDO for further guidance.
◦ Contact Medicare. This may mean you might have to reverse the billing for the consultation.
◦ Seek advice on whether you also need to notify the Office of the Australian Information Commissioner (OAIC) and / or
contact police. For further information see Avant’s resource on Responding to a data breach.
If you realise that your practice has treated someone under a false name, it’s important to assess whether a data breach has occurred. Not every instance will qualify as a breach, but if patient information has been disclosed without proper authorisation, it may be considered one. You should follow the guidelines provided by the OAIC to determine if the incident requires notification. For more detailed advice, refer to Avant’s Responding to a data breach factsheet
Additionally, if you are considering approaching the individual who provided a false name, personal safety should be a priority. Evaluate the situation carefully and avoid direct confrontation, particularly if there are concerns about the person’s behaviour or motives. Always follow your practice’s protocols for managing difficult situations which may involve calling security or police.
After the incident, take time to review your practice’s policies and procedures to identify any gaps or areas for improvement. Reflecting on the situation can provide valuable learnings to help prevent similar issues in the future and ensure your team is better prepared to handle these scenarios.



In September this year, the initial draft of the Royal Australian College of General Practitioners (RACGP) Standards for general practices 6th edition were released. This next edition of the RACGP Standards aims to further promote a high standard of general practice care by improving the quality and safety of general practices.
The RACGP’s industry consultation period closed in late October, allowing for the gathering of valuable insights and feedback from practices, peak bodies and other industry organisations nationally.
AGPAL is proud to be the exclusive accrediting agency engaged for accreditation assessments being undertaken as part of the pilot program. The first of two pilots launched in September 2024 and involved ten practices. This first pilot has provided AGPAL with early insights to support practices during the transition period to the new Standards. The second RACGP 6th edition pilot will occur in early 2025.
As the RACGP continues to review the applicability and feedback of the proposed 6th edition Standards, gathered during the pilot and industry consultation period, AGPAL is also liaising closely with the RACGP to advocate for our clients and surveyors.
We recognise that the release of a new set of Standards results in operational impacts for practice teams so we’re doing our best to proactively prepare for this transition period. We’re proud to be advocating for the needs of all our clients, considering potential impacts based on their size and location.
While we wait for the final release of the RACGP Standards, we’ve gathered key information from the RACGP to provide you with insights into the proposed key changes
currently included in the 6th edition draft.
Key proposed changes from the 5th to the 6th edition
In its current draft format, the 6th edition of the RACGP Standards introduces a refined structure that includes four standards:
1. Foundations of general practice –Covering essential elements of practice setup and operations.
2. Clinical governance – Focusing on systems for maintaining the quality and safety of care.
3. Patient participation – Encouraging meaningful patient engagement to improve care quality.
4. Continuous quality improvement (CQI) – Supporting ongoing assessment and performance improvement.
These four standards are supported by 34 criteria, grouped into thematic categories for a more streamlined accreditation process.
Emphasising consumer needs
In collaboration with consumers, the RACGP has included consumer statements linked to each criterion within the 6th edition. These statements highlight the importance of each requirement from the patient’s perspective, ensuring the Standards reflect patient expectations and contribute to better health outcomes.
What’s new in the 6th edition Standards?
The RACGP has provided a fact sheet highlighting key updates within the proposed 6th edition Standards. These updates include: Environmental sustainability
The 6th edition Standards introduce a strong focus on environmental sustainability, encouraging practices to adopt measures that reduce their environmental impact while promoting patient well-being and
satisfaction. This addition supports practice teams in minimising energy consumption, reducing waste, and integrating ecofriendly practices into daily operations. This approach contributes to improved care and helps mitigate the practice's environmental footprint.
The theme of environmental sustainability appears throughout the 6th edition Standards, with specific requirements across various criteria:
◦ At indicators F.3►A and F.3►B in Criterion F.3 – Environmental sustainability and responsibility:
◦ Practices should actively minimise their environmental impact.
◦ At least one team member should promote and engage in environmental sustainability efforts within the practice.
◦ At indicator CG.4►C in Criterion CG.4 –Clinical and Medicines Guidelines:
◦ Practices should provide resources and strategies for sustainable clinical practices, including promoting environmentally friendly options in clinical decisionmaking.
◦ At indicator PP.6►B in Criterion PP.6 –Health Promotion and Preventative Care:
◦ Practices should provide patients with environmental information to help them make informed choices that benefit both their health and the environment, fostering a sense of community and shared responsibility.
◦ At indicators CQI.1►B and CQI.1►C in Criterion CQI.1 – Continuous Quality Improvement Activities:
◦ Practices should monitor, report, and track progress on their environmental performance, using impact metrics to assess and manage their overall environmental footprint.


By integrating these sustainable practices, the 6th edition aims to enhance the role of general practices in contributing to broader environmental goals while ensuring highquality patient care.
Defining and planning for your practice
Criterion F.1 – Defining and Planning for Your Practice asks practices to place greater emphasis on establishing and monitoring their mission and values, and maintaining both strategic and operational plans. These plans set measurable goals and objectives to guide the practice’s operations.
The 6th edition expands the scope of response planning. In addition to emergency response planning, practices must now plan for unexpected events that may disrupt business operations. This broader approach to response planning helps practices consistently identify, document, and manage risks, ensuring they can continue providing clinical care during emergencies or other interruptions.
training of healthcare practitioners
Under the draft 6th edition requirements, practices no longer need to retain registration and CPD documentation for each practitioner but must still ensure all practitioners have current national registration and the necessary accreditation or certification.
Recognising the growing role of technology, Criterion F.10 requires practices to ensure the safe, secure, and effective use of digital healthcare, including telehealth. Practices must integrate digital tools into patient care while ensuring security and quality outcomes.
Criterion CG.1 requires practices to manage all patient information using digital systems, phasing out paper-based systems. This ensures accurate and secure patient health records and supports effective data analysis for quality improvement.
Criterion CG.2 provides more flexibility in how practices match patients to their health records. The draft 6th edition no longer mandates the use of three identifiers, giving practices room to choose the method that best suits their needs.
The 6th edition focuses on codable patient data to support continuous quality improvement. Practices must ensure:
◦ Demographic information includes sex assigned at birth, gender, and pronouns
◦ Nationally recognised medical vocabulary is used for coding.
◦ 100% of active patient records include known allergies or indicate no known allergies.
This ensures improved data management and quality care.
health
The updated Standards refine indicators for patient health records, ensuring data is codable and actionable to support quality improvement activities. This facilitates more accurate record-keeping and better care.
Criterion CG.4 requires practices to give clinicians current, evidence-based information on medicines and clinical guidelines. This supports best-practice prescribing and access
to emergency care resources. Immunisations
Practices must ensure that all team members receive the recommended immunisations based on their role and risks, according to both the Australian Immunisation Handbook and relevant state or territory mandates, ensuring the health and safety of the entire practice.
Informed consent includes consent for third-party presence, clinical procedures, and medicines. This update aligns practices with legislative requirements and best practice standards, ensuring comprehensive consent procedures.
The 6th edition aims to encourage practices to actively involve patients in reviewing and enhancing care through outcome-based CQI processes. When effectively implemented, this approach fosters genuine engagement, leading to improved patient experiences and outcomes.
Criterion CQI.1 requires practices to undertake at least one clinical improvement activity every 12 months. This flexible approach allows practices to tailor CQI activities to their specific needs while promoting ongoing improvements in care.
The 6th edition broadens the definition of general practices to include non-traditional services, such as mobile and outreach services. However, services with limited scope, such as telehealth-only clinics, remain ineligible for accreditation under these Standards.

Practices can choose to be accredited under either the 5th or 6th edition Standards for the first 12 months following the publication of the 6th edition – which is planned for early 2026. After this transition period, all practices seeking accreditation must meet the 6th edition Standards.
AGPAL is honoured to play a key role as the exclusive accrediting agency in piloting these Standards, collaborating with participating practices to shape a more sustainable and patient-focused future for healthcare in Australia. AGPAL thanks all practice managers, pilot participants and industry experts who have provided valuable feedback.
AGPAL has advocated on behalf of the general practice sector and is continuing to liaise with the RACGP as they review industry and pilot feedback to create a finalised version of the RACGP Standards 6th edition. As information becomes available, particularly around key changes, accreditation requirements and timelines, AGPAL will proactively share these updates with clients, surveyors and stakeholders.
Visit the RACGP website to view the current draft of the RACGP Standards 6th edition in its entirety or contact AGPAL for any current accreditation support:
P: 1300 362 111 l E: info@agpal.com.au






At MIGA we often receive enquiries from our members about requests for information and statements by police. The requests may be in relation to Coroner’s or criminal investigations. It is important to remember that patient information is confidential and should not be released to police without careful consideration. Be helpful and co-operative but do not breach patient confidentiality or hospital/ practice policies.
It can be a little intimidating when the Police arrive at your reception desk without prior notice. Admin staff members often ask what is the best procedure to follow in this circumstance.
Questions or requests from the Police should be passed on to the patient’s doctor as the doctor will have an understanding of the issues that are relevant to the patient and their situation. If the doctor is unavailable then you may from time to time, as Practice Manager, find yourself needing to manage the situation.
Receiving a request for information from police
When receiving a request from police the first question that should be asked is whether the patient has consented to the release of information. If the patient has not provided consent, the police should be asked if there is a warrant, subpoena or court order
authorising the release of information.
It is good practice to request a copy of the patient consent, warrant, subpoena or court order and place it on the patient’s medical record. The document should be carefully read and only the information specified should be produced.
Exercise caution when medical records are only requested for a particular period of time. Providing records outside of the dates specified could amount to a breach of confidentiality.
There are limited situations that may justify providing information to police in the absence of consent, a warrant, a subpoena or a court order. These include:
◦ Where there is a serious threat to the life, health or safety of an individual or to public health or safety and
◦ Where you have a good reason to suspect unlawful activity or serious misconduct
It is important to ask questions of the police to understand the nature of the enquiries and the reason why the confidential information is being requested.
If refusal to disclose patient information would significantly impede the investigation of a serious criminal offence disclosure can be justified. Likewise, if a patient behaves in a way that puts your safety, or the safety of your family or others at risk, con dential information can be provided to police. If a decision is made to disclose information, only information that is directly relevant to the issue of concern should be released.
In these situations, we recommend that you contact MIGA before releasing information to ensure that you are complying with privacy legislation. Any and all communications with police should be documented in the patient’s
medical records.
If you have your Practice Indemnity Insurance policy with MIGA you are able to access 24/7 medico legal support.
Providing confidential patient information to police without patient consent or being served with the relevant document, such as a warrant or subpoena can result in serious consequences. This can include complaints to the Medical Board and Privacy Commissioner, monetary fines and in the case of doctors or nurses, conditions on registration.
Providing a written statement to police
Police investigating a coronial or criminal matter will often request a signed statement from doctors or potentially in some cases, from members of your practice staff. In most cases there is no legal obligation to provide them with a statement, but we recommend that you co-operate with police as it will reduce the chances of being subpoenaed to give evidence in court.
Police will provide a template for your statement, and this should be used. You should always sign and date your statement.
In terms of drafting your statement, we suggest that you keep it factual, to the point and consistent with the clinical records. You should always review the clinical records prior to drafting your statement to refresh your memory of events. If you do not have access to the records, you should ask the police to provide you with a copy.
It is best to use plain English in written statements and explain any medical terms so that a lay person would be able to easily understand your evidence. You should avoid offering an opinion unless asked to provide

one, especially when you are a factual witness. It is important to be clear about your role in the treatment of the patient and to limit your statement to your involvement with the patient. You should avoid commenting on the care provided by other practitioners, unless necessary.
Always ensure that your statement is reviewed by MIGA before you sign it.
Key take-away
Be mindful of providing confidential information to police without patient consent, a warrant, subpoena or court order and always ensure that you seek guidance and advice from your hospital or from MIGA.
CARMELINA PARISI
SENIOR SOLICITOR- CLAIMS AND LEGAL SERVICES
MEGAN SHELDON
PRACTICE RISK EDUCATION MANAGER
Information in this article does not constitute legal or professional advice. Call us if you need advice on any of the issues covered in this article.


M y G P M P t o o l ( M G T )
Integrated digital CDM tool
MGT Is Integrated with Best Practice and Medical Director
CDMs (care plans, health assessments, mental health plans, DMMR and reviews
Real-time self-audits and more features to streamline CDMs with less paperwork
MGT eliminates most of your paperwork handling, scanning, faxing and printing.
With MGT practices can generate comprehensive CDMs following RACGP and MBS guidelines.
Allied health, specialist, and other health care providers are connected.
Increase practice revenue
On average adding over 15K per GP in additional MBS billing and improved reviews, HAs, DMMRs and more.

5000+ GPs and nurses
200k+allied health, specialists and other health care providers
1.2M unpaid activities avoided



As the new World (post COVID) starts to feel like the old norm, we are seeing a return to one of the most tried and true knowledge transfer formats: the conference. Certainly, after the strains, stresses and isolation of COVID, stepping beyond the confines of one's usual environment to attend a conference is back to being a novelty, but is it necessary?
Building beyond the essential role educational conferences play in professional development, a well-run conference will enhance both practical and collaborative aspects of general practice. In-person attendance offers medical practitioners and practice staff a really unique opportunity to stay abreast of things like the latest research, best practices in health care, the latest technological and software changes, as well as exposure to vendors who offer products and services that enhance and improve many different aspects of general practice. There’s no other format that brings together a diverse tapestry of professionals whose collaborative interactions can spark innovative approaches to patient care.
Before COVID, we took these face-toface opportunities for granted. In-person networking at a conference can form partnerships that lead to groundbreaking projects and despite the immediate demands of everyday practice, the long-term benefits of conference engagements underscore their essential role in professional growth. Especially in a post COVID world, conferences have become more than mere assemblies; they transform people, practices, and organisations into vibrant ecosystems that
nurture knowledge and innovation. The impact continues long after you exit the doors with your goodie bag in tow. As you reflect on the learnings you take with you, opportunities suddenly begin to present themselves within your practice. An efficiency gain here… a process improvement there… Large, medium or small… an impact is still an impact.
Attending an educational conference is emerging as more than a beneficial endeavour for general practitioners—it becomes a vital element in achieving excellence. Conferences are a strategic investment in one's professional journey, aligning individual growth with the overarching goal of advancing quality care delivery in general practice. Through continued engagement with these dynamic learning ecosystems, practitioners ensure that they remain not only informed participants but also influential contributors to the evolution of modern healthcare. So now, the bigger question is: which conferences are you planning to attend in 2025?

HILLHOUSE LEGAL PARTNERS
When it comes to running a successful practice, a proactive approach to legal, financial, and operational issues can be a game changer. At Hillhouse Legal Partners, we’ve found practices that stay ahead of their legal matters not only avoid unexpected headaches but also find themselves in stronger positions when opportunities arise. To make this easier, here’s our top 10 list of legal matters you should review each year to keep your practice in great shape.
If your practice has grown or shifted focus, it’s worth checking if your corporate structure still fits. The right setup can impact your taxes, liability, and even future growth plans. Take a look at any foundational documents like your shareholder agreements or business terms and ensure they reflect how your practice operates now. Updating your structure with your lawyer or accountant can also help you protect assets and plan for the future.
Reviewing your supplier contracts may sound tedious, but it can save you money and ensure you’re not locked into unfavorable terms. Also, with new Unfair Contract Terms (UTC) rules under Australian Consumer Law, small businesses now have stronger protection against contracts that are unfair. Double-checking that these terms don’t apply to your practice’s supplier contracts can help you avoid issues down the line.
Leases can be surprisingly tricky, especially with renewal windows and negotiation opportunities. If you’re nearing the end of
a lease, early renegotiations can improve your chances of securing better terms or identify if relocation is needed. Start thinking about the size and setup of your space—do you need more room for new patients, or a change in location to attract a different clientele? Do you need to rent an additional premises or purchase a new space? Planning ahead on your premises and lease can pay off significantly.
Recent changes in payroll tax have impacted many practices, particularly in Queensland, where new rulings affect the way practices handle patient revenue. If your practice’s payment setup doesn’t meet these requirements, it could lead to unexpected payroll tax. For example, if patient revenue is first collected by the practice or paid to a clearing account before being distributed it could be considered ‘wages’ and may be subject to payroll tax.
Each State has its own exemption, amnesty or rebate regimes too. These measures all have different requirements, so it is important you continually monitor the position in your State to ensure you are meeting requirements and taking advantage of options available to you. Reviewing service agreements and eligibility for exemptions, amnesties and rebates with legal and accounting support can ensure you’re on the right side of these rules.
Employment law changes quickly, and 2024 introduced a few key updates, including the ‘right to disconnect’ outside of work hours. There’s also been a push for higher minimum wages and more options for casual employees to go permanent. Ensuring your employment contracts reflect these changes is essential. It’s also worth revisiting your performance review process and considering retention incentives like share schemes to
keep your best employees.
Data protection and privacy can be a hot issue, especially in healthcare where patient information is sensitive. Make sure your privacy policy is up-to-date and compliant with the Privacy Act. Reviewing how you collect, store, and use personal information can help avoid both regulatory fines and potential reputation damage.
Alongside privacy compliance, robust cybersecurity policies are essential in preventing cyberattacks and data breaches. Practices should implement protocols to manage cybersecurity risks and conduct employee training to detect and respond to potential threats like phishing or malware attacks. A good cybersecurity plan doesn’t just protect your patients’ data but can also save you from costly disruptions and potential legal consequences.
Document your current arrangements with a signed shareholder agreement. Avoid protracted drafting—clear, concise agreements are better than none at all. This helps prevent future disputes and ensures alignment among stakeholders.
You may not be thinking about leaving the practice anytime soon, but having a solid succession plan is key for a smooth transition whenever the time comes. Succession planning can make a big difference in ensuring your practice retains its value, aligns with your goads, and that your patients are well cared for if and when a change in ownership happens.


Life can bring unexpected changes, so it’s a good idea to keep your personal estate plan current. If you have a new family member, a big purchase, or other life events, updating your Will and estate documents can ensure your wishes are respected. An outdated Will can create a lot of unnecessary stress for loved ones, so consider a quick review with a legal professional every five years or whenever major life changes occur to keep your plans current and enforceable.
Your brand is unique, so make sure it’s protected! Registered trade marks can prevent others from using or diluting your brand. It’s also smart to periodically check for any similar trade marks or brand names that might be infringing on your IP. If you spot any issues, consulting with a legal professional can help you protect your brand effectively.
Getting ahead of legal issues with an annual review may seem like a lot, but the peace of mind and practical benefits it brings can be invaluable. Incorporating these legal checks into your annual review process will strengthen your practice’s foundation and give you a competitive advantage in navigating the complexities of today’s healthcare industry.
At Hillhouse Legal Partners, we recommend that practices complete an annual review with the support of professional advisers to guide you through this essential process and ensure every aspect of your business remains compliant, optimised, and protected.





DIGITAL MEDICAL SYSTEMS

The pace of development and the release to market of new Gen AI software continues at an ever increasing rate. The giant tech companies are furiously competing against each other -and competing against AI startups, all racing to get new Gen AI products to market, and to enhance already released Gen AI products with new features almost on a weekly basis.
For example, Apple Inc., a relative latecomer to Gen AI capability, released Apple Intelligence on 29 October 2024 after announcing the product in June of 2024. Apple Intelligence is available on iPhone, iPad, and Mac computers, and is available as a free software update of iOS 18.1, iPadOS 18.1, and macOS Sequoia 15.1. There is a catch however - Apple Intelligence will only work on relatively newer versions of iPhone, iPad, and Mac according to Apple’s press release, only “available on iPhone 16, iPhone 16 Plus, iPhone 16 Pro, iPhone 16 Pro Max, iPhone 15 Pro, iPhone 15 Pro Max, iPad with A17 Pro or M1 and later, and Mac with M1 and later”1
Apple is playing catchup against the huge market share of the Android/Samsung products. As we would expect, Apple focus is in “giving our users a personal intelligence system that is easy to use — all while protecting their privacy.”:
“Apple Intelligence unlocks exciting new capabilities that make your iPhone, iPad, and Mac even more helpful and useful, from Writing Tools to help refine your writing, to summarised notifications 1Apple Inc., (2024)., Press Release - Apple Intelligence is available today on iPhone, iPad, and Mac, retrieved from https://www. apple.com/au/newsroom/2024/10/appleintelligence-is-available-today-on-iphoneipad-and-mac
that surface what’s most important, to the ability to search for almost anything in your photos and videos by simply describing it,” said Craig Federighi, Apple’s senior vice president of Software Engineering. “And it’s all built on a foundation of privacy with on-device processing and Private Cloud Compute, a groundbreaking new approach that extends the privacy and security of iPhone into the cloud to protect users’ information. We are thrilled to bring the first set of Apple Intelligence features to users today, and this is just the beginning.”2
This new personal intelligence system leverages Apple silicon to enhance language and image processing, streamline tasks across apps, and maintain user privacy with on-device processing and Private Cloud Compute.
Key features include:
◦ Writing Tools: Integrated across iOS, iPadOS, and macOS, these tools help users refine their writing by rewriting, proofreading, and summarizing text in various apps, including Mail, Messages, Notes, Pages, and in third-party apps.
◦ Summarized Notifications: This feature highlights the most important notifications, mail, and messages.
◦ Enhanced Siri: A more natural and capable Siri experience.
◦ Clean Up: A tool to remove distracting objects from images.
Apple is known for pioneering easy to use graphical human User Interface (UI)and this means that other vendors will be forced to follow suit.
Microsoft has not been sitting still either, continuing to transform and enhance
2 ibid
Microsoft Copilot M365 ( the ubiquitous M365 Apps - Outlook, Word, Excel, PowerPoint, Teams, OneNote, Viva Goals, and Forms, etc) with the latest announcements and improvements in Copilot for M365 at Microsoft Ignite event held on 19 November3, including:
◦ Copilot Actions in Microsoft 365 Copilot to help you automate everyday repetitive tasks.
◦ New agents in Microsoft 365 to unlock SharePoint knowledge, provide real-time language interpretation in Microsoft Teams meetings, and automate employee self-service.
◦ The Copilot Control System to help IT professionals confidently manage Copilot and agents securely.
1. Enhanced Integration: Copilot for Microsoft 365 now offers real-time intelligent assistance by coordinating large language models (LLMs), content in Microsoft Graph, and the Microsoft 365 productivity apps that you use every day. This integration provides users with enhanced creativity, productivity, and skills.
2. New Features: The latest features in Microsoft 365 apps include improved data generation and transformation capabilities, allowing users to create and manage emails, documents, spreadsheets, presentations, and meetings more efficiently.
3. Security and Compliance: Essential safety and security guidelines have been implemented to ensure the safe use of Copilot M365. These guidelines help
3 Microsoft, (2024)., Introducing Copilot Actions, new agents, and tools to empower IT teams, retrieved from https://www.microsoft. com/en-us/microsoft-365/blog/2024/11/19/ introducing-copilot-actions-new-agents-andtools-to-empower-it-teams/

practice managers use Copilot M365 with appropriate data safety and security guardrails.
4. Practical Productivity: Copilot M365 promises to enhance productivity in various sectors, including healthcare, by providing tools that streamline administrative tasks and improve overall efficiency.
5. User Experience: The user experience has been significantly improved with modern design, better navigation, and enhanced functionality across all M365 apps. Microsoft is competing against Apple’s claim to better User Interface with the slogan, “Copilot is the UI for AI.”
All this intense competition is going to be great for consumers and with Apple entering the Gen AI race, UI and privacy of data will be a major focus. A good thing for consumers.
The amount of money being invested in Gen AI is staggering – over US$1 trillion according to Goldman Sachs, who pose the question, “Will the $1 trillion of generative AI investment pay off?”4
The answer, of course is that we don’t know.
Investors are betting big on the infrastructure (including investing in nuclear power for the huge amounts of electricity required to power Gen AI 5), the hardware required for Gen AI (has anyone invested in Nvidia?), the Gen AI software developers.
Take up of Gen AI in Healthcare
4 Goldman Sachs, (2024)., Will the $1 trillion of generative AI investment pay off?, retrieved from https://www.goldmansachs.com/insights/articles/will-the-1-trillion-of-generative-ai-investment-pay-off
5 CNBC.com, (2024)., Why Big Tech is turning to nuclear to power its energy-intensive AI ambitions, retrieved from https://www.cnbc. com/2024/10/15/big-tech-turns-to-nuclearenergy-to-fuel-power-intensive-ai-ambitions. html
The so called AI Scribes or transcription tools are increasingly being tried by doctors, especially for complex and detailed case notes where AI Scribes can provide major productivity gains. PulseIT News Weekend Edition 23 November 2024 reports on the take up trends with two interesting surveys:
◦ Primary healthcare provider Ochre health testing the “time saving and stress reduction benefits” on a small number of GPs using Lyrebird AI scribe tools. The results are interesting:
“a small reduction in overall stress, although the non-AI group also reported a reduction
The AI user group predicted that AI transcription would give them a modest but significant improvement in the quality of their medical records, which was backed up in the second survey
14 of the 18 doctors using the tool reported in the second survey that they were getting a saving of two minutes or more per patient, but four said they didn’t save any time. This may be due to time spent proofreading and reordering the AI notes or similar
Of the doctors that did report getting a time saving, they overwhelmingly elected to use it for patient care
Hopes that the tool would enable them to see more patients or leave work earlier were not borne out.”6
◦ Research by Avant Mutual of 600 members, “which found that one in two doctors are either currently using or want to use an AI scribe. At the moment, 11 per cent surveyed said they were using one but 39 per cent said they were likely to
6 PulseIT News, (2024)., Meeting expectations: Do AI scribes for GPs stack up?, retrieved from https://www.pulseit.news/australian-digital-health/meeting-expectationsdo-ai-scribes-for-gps-stack-up/
use one in future, particularly doctors who haven't been practicing that long”7,8
The development of Generative AI is happening at an astonishing pace, that will be a part of every aspect of our use of technology, in our personal lives, and in our professional workflows, including for everyone in healthcare.
Remember the game of Hide and Seek? “Coming, ready or not!”
The Gen AI train has arrived, we will all be on board, one way or another.
More to come…
7 PulseIT News, (2024)., Blog: Would you like a second opinion with your AI scribe?, retrieved from https://www.pulseit.news/ pulseit-blog/blog-would-you-like-a-secondopinion-with-your-ai-scribe/
8 PulseIT News, (2024)., AI.Care 2024: “Significant” interest in AI scribes means proactive regulation needed, retrieved from https:// www.pulseit.news/australian-digital-health/ ai-care-2024-significant-interest-in-ai-scribesmeans-proactive-regulation-needed/






“Beyond impressive, 5 stars! DMS IT are everything they claim to be and more...”
- Hayley Hughes Practice Manager Tandem Health Labrador Medical Centre
Calls to the DMS helpdesk are answered literally within seconds, most issues are resolved within minutes
Guaranteed Level 2 or Level 3 technicians with extensive experience in Australian medical software problem resolution
Extensive experience and expertise in Australian medical software eco systems
87% of helpdesk calls resolved on the same day
81% of helpdesk calls resolved on the first call
Managed Cyber Security expertise - Security first approach with Cyber Security qualified staff
Pro-active Managed IT that is fully customised for Australian medical clinics, with High Attention to detail
DMS Private Cloud located in Melbourne and Sydney Australia at leading Tier 4 data centres with latest high performance, and high capacity Host servers

Make sure you diarise the 2025 AAPM education calendar dates today and plan ahead for next year. The below metro locations will host dedicated education sessions for reception/administrators and practice management teams. The regional locations will be advised next year.

Thursday 05 June Reception/Admin
Brisbane
Friday 06 June Practice Management Brisbane
Thursday 12 June Reception/Admin Melbourne
Friday 13 June Practice Management Melbourne
Thursday 03 July Reception/Admin Adelaide
Friday 04 July Practice Management
Thursday 24 July Reception/Admin Sydney
Friday 25 July Practice Management Sydney
Thursday 31 July Reception/Admin Perth
Friday 01 August Practice Management Perth
Note: All Educare events are held in-person for a face-to-face delivery.




In addition to the face-to-face education events, AAPM will continue to host a series of webinars. Webinar dates will be available on the AAPM website once confirmed.
AAPMAANZ 2025 Conference
Join AAPM and PMAANZ as we reunite to host the 2025 Conference.
Tuesday 21 October to Friday 24 October 2025.
Melbourne Exhibition and Convention Centre, Melbourne, Victoria, Australia

Appointment Book Audit Tool
Appointment Reminders
Appointment Instruction / Follow up Messages
Caller ID
Chatbot
Clinical Reminder Messages
Consent / Questionnaire Forms
Debtors Book
Deposits, Post-Consult Payments & Held Funds
Email Campaign Platform
Kiosk Software
AMS Connect Mobile App
Medicare Benefit Assignment
MyMedicare Appointment & Messaging Filters

New Patient Post-Consult Message
Online Appointments
Online Repeat Scripts & Referrals
Online Booking Confirmation
Queue Display (BYOD)
Results Messaging
SMS Campaigns


As healthcare professionals ourselves, we know that today's healthcare businesses are under more pressure than ever. We understand how tough it is to deal with multiple suppliers, to negotiate the best deal and then to place and manage orders across a variety of different channels. And we know that the more time you spend on routine tasks, like sourcing supplies, the less time you have to focus on what matters to you most – quality patient care and successful patient outcomes.
We've therefore made it our mission to give practice owners and managers a smarter way to purchase premium products and services by creating MedicMall. Instead of making numerous phone calls, running all over town – or the web – to find what you need, MedicMall is your dedicated one-stop online marketplace for quality products and services at very competitive prices in one convenient place.
MedicMall does all the hard work for you by bringing all the products and services you need to run your busy healthcare business, together, in one convenient, intuitive and easy to use marketplace. We’ve assembled a trusted network of national suppliers, which is constantly growing, across a range of categories: Office Stationery & Supplies; Office Technology; Medical Supplies & Equipment; Insurance Services; Bookkeeping and Tax Services; Financial Lending Services; and IT Support Services, to name a few.
You can shop by product, supplier or product category. Simply browse through our selection of products and services or use the search function and then you can either checkout by making one single payment (via secure credit card, Apple Pay or Google Pay)
or request a quote for a service.
As an AAPM/MedicMall member, not only will you receive exclusive wholesale pricing and special offers, but you will also have access to a range of handy reporting tools to improve and track your expenditure, as well as smart buying features to help make your online experience simple, efficient and easy – every time.
“Our team has worked within the healthcare industry for many years and MedicMall was created in response to the need for more time-saving and cost-efficient purchasing channels,” said Charlotte Raman, MedicMall Co-Founder and Chief Marketing Officer. “Our purpose is to simplify the purchasing process of healthcare businesses by offering a convenient, easy-to-use Ecommerce solution which connects healthcare providers with a trusted network of suppliers.”
The MedicMall team is excited about being able to offer this service to all AAPM Members.
Become an AAPM/MedicMall member today to start saving time and money. It’s free to join!
Learn more about MedicMall by visiting www. medicmall.com.au or contact us at info@ medicmall.com.au or on 1300 950 555.





