THE PRACTICE MANAGER







AAPM’s Professional Development Program supports and promotes members’ personal and professional growth through a system of:
CORE PRINCIPLES
ADVOCACY
AAPM representation on government and industry advisory groups.
HR ADVISORY SERVICE
Comprehensive HR support and advice through telephone, email and website resources and templates.
MEMBER ASSISTANCE PROGRAM
Confidential assistance to support health and wellbeing of members.
PULSE+IT SUBSCRIPTION
Asia Pacific’s eHealth and Health IT digital platform.
MEMBERSHIP BADGE
Recognition of AAPM membership.
THE PRACTICE SPACE
Dedicated fortnightly eNewsletter providing industry updates and helpful advice.
PRACTICE MANAGER JOURNAL
AAPM’s national journal, delivered electronically to members each quarter.
AAPM EDUCARE
Access to AAPM’s Educare program at member rates. Includes face-toface events and a series of webinars.
NATIONAL CONFERENCE
Premier annual conference for Practice Management at member rates.
NETWORKING MEETINGS
Share knowledge and information. Connect with, and support your peers.
ONLINE LEARNING MODULES
Self-guided learning through Practice Management topics.
SCHOLARSHIPS
Expand your skills through AAPM funded scholarships for selected Practice Management courses delivered though UNE Partnerships.
PRACTICE MANAGEMENT OF THE YEAR AWARDS
Prestigious state and national awards recognise and reward a Practice Manager for their contribution to the profession of Practice Management.
CERTIFIED PRACTICE MANAGER (CPM)
Recognition of years of experience and skill development in the profession of Practice Management.
FELLOWSHIP
A prestigious honour in recognition of significant commitment and contribution to the profession of Practice Management.
INDUSTRY PARTNERSHIPS
Exclusive access to resources, discounts and benefits from industry partners.
DEDICATED ONLINE MEMBERS FORUM
Dedicated and exclusive member only forum to share ideas, insights, information and support.
AMBASSADORS
Support and assistance from experienced and highly qualified Practice Managers.
WEBSITE ACCESS
Access latest news, industry information, and member-only resources.

It has been a busy and productive quarter, beginning with the Board's Strategic Planning Day. During this session, our facilitator provided valuable insight into the responsibilities of Board Directors, with a strong focus on our duty to act in the best interests of AAPM - an essential aspect of our role as Directors.
We were fortunate to have the results of the recent member survey available to inform our discussions. Your feedback has been instrumental in shaping the direction of our new strategic plan. I would like to personally thank all members who took the time to complete the survey - your input is greatly
appreciated.
The strategic plan is now in its final stages, and we look forward to sharing it with you in the new financial year.
Having recently attended several conferences; I wanted to share a few reflections with you. One message that resonated deeply throughout these events is that the strategic integration of technology is no longer just an option - it is an essential pillar for the future of healthcare, especially within our diverse and dynamic region.
Effective healthcare systems, supported by strong practice management, form the foundation for meaningful digital transformation. As echoed by many of our peers, the success of technological advancement relies not just on innovation, but
on our collective commitment to cultivating understanding, fostering collaboration, and building trust. Transparency, openness, and good governance must guide us as we navigate this transformation together.
As we approach the end of the financial year, I wish you all the best in your planning and preparation. I also look forward to seeing many of you at the AAPMAANZ Conference in Melbourne, where we will be joined by our colleagues from PMAANZ New Zealand - a wonderful opportunity to connect, learn, and grow together.

Being a Practice Manager is no small task. You wear many hats - team leader, problem-solver, financial planner, policy enforcer, patient advocate, and somehow still make it all run smoothly. But as the healthcare landscape continues to shift, it's clear that the role of Practice Management is more important than ever. That is why promoting our profession and staying actively engaged with others in the field isn't just a nice idea, it is essential.
Engagement can take many forms. It might be joining a local AAPM networking meeting, attending the national conference, participating in webinars, or simply reaching out to a fellow Practice Manager to share ideas or challenges. These connections give support to help us stay ahead of changes and daily challenges.
Being involved also helps raise the profile of the profession. When we share our experiences, whether through networking, participating at events, or contributing to forums, we show the depth, skill, and leadership it takes to do what we do. We are the professionals at the core of quality patient care and efficient, effectivel practice operations.
AAPM offers networking, education, and advocacy, it brings Practice Managers together and gives us the tools to thrive.
Promoting our profession also starts from within our own practices. Let's recognise our contributions and speak up about the impact we have. Let us encourage others, especially younger professionals, to see Practice Management as a rewarding, long-term career. And support each other, especially during tough times, because no one understands our world quite like another Practice Managers.
In short, the more we engage, the stronger our profession becomes. So whether you're new to Practice Management or have decades of experience, there is always a way to connect, contribute, and help raise the bar.

MIRANDA GRACE CHIEF EXECUTIVE OFFICER



It's hard to believe we're nearly at the end of another financial year. And yes, you know what that means - it's time to tidy up the books, review your records, and make sure everything is in order before 30 June arrives.
To help you get organised, we've put together some practical tips that'll make the process a whole lot smoother.
For Doctors: Don't leave these to the last minute.
Service fees are often one of your biggest expenses. Check that they've been paid in full and in line with your agreement before 30 June.
Prepay what you can. Things like professional memberships, subscriptions and donations may be deductible, and bringing these forward could work in your favour.
Make the most of your super. You can contribute up to $30,000 in concessional contributions this financial year, inclusive of Employer contributions, just make sure your payment is received by your super fund well before the deadline. You must also lodge your Notice of Intent to claim a deduction.
You may be able to benefit from unused tax deductible contributions from the last five years where contributions have not been maximised; this needs careful
consideration so plan early.
Update your logbook. If you use your car for work, a current logbook helps you claim fuel, rego, insurance and other running costs up to your business-use percentage.
Bought any assets? Now's the time to pull that info together while it's fresh and easy to find.
ATO Payment Arrangements. If you have one in place, from 1 July the interest is no longer tax deductible. Consider alternative ways to pay off your debt sooner rather than later to maximise your deductible debt.
For Practice Managers: These tasks are key.
End of Financial Year [EOFY] preparation is a team effort, and we know practice managers are often the ones keeping everything running behind the scenes. Here's what to keep an eye on:
Reconcile staff wages and super. Remember, super must be paid before 30 June if you want to claim the deduction this financial year.
Review expenses. Make sure any tricky items, like entertainment, staff training, or repairs are clearly explained.
Clear out the Practice Clearing Account. If this still applies, ensure all service and doctor payments are processed before 30 June.
Sub-leased rooms? Now is a great
time to check that any rent reviews were completed during the year.
STP finalisation is due by 14 July. Best to plan ahead so you're not chasing last-minute fixes.
Make the most of your tax position.
Tax is likely one of your largest outgoings, so it's well worth taking the time to get things right and maximise your available deductions.
We've prepared some detailed EOFY checklists to help you stay on track. Scan the QR codes below to access the tools that'll help make this process easier for you and your team.
For personalised advice contact us




While tax time can be overwhelming, with the right team, it can become an opportunity to set your practice up for success. Staying on top of your reporting, compliance, and deduction opportunities is key to running a healthy practice.
We’ve created a complimentary EOFY tax checklist, specifically for Practice Managers, to help you:
Stay on top of reporting obligations
Maximise practice-related deductions
Prepare for a smoother year-end review
Avoid common pitfalls that impact compliance
Whether you manage a small practice or a busy specialist group, having the right checklist can save time and money.
Download your EOFY checklist today.

MIGA
The prevalence of mental health issues emphasises the need for employers to manage appropriately in the workplace.
Miga receives an increasing number of requests from our clients for assistance in managing workplace conflicts and disputes and it is often necessary to consider the potential for mental health issues to either develop or become aggravated in the event of a workplace investigation or disciplinary process which may be exacerbated if poorly managed.
Mental health issues in the workplace are often associated with common behavioural issues including repeated absences, poor performance, excessive risk taking or risk avoidance and complaints of bullying and harassment. Employers must manage such behavioural issues in a way that does not discriminate their employees and potentially aggravate any mental health issues.
Often clients contact us after a workplace investigation or performance management process has already commenced and before any potential mental health issues have been considered. Workplace investigations in particular have the potential to cause additional stress which may result in a significant exacerbation of pre-existing mental health issues. It is therefore critical for investigations to be treated
sensitively, for confidentiality to be strictly maintained and for adequate support and counselling to be offered to employees throughout the process.
Is performance management acceptable when mental health issues are involved?
The Fair Work Commission, Federal Court and Federal Circuit Court have jurisdiction over workplace disputes and closely scrutinise an employer’s investigative and disciplinary processes, particularly in instances of dismissal or resignation from employment when mental health issues are involved.
The presence of mental health issues may even provide an employee with a complete defence in instances of serious misconduct.
Accordingly, it is critical for an employer to engage in a proper performance management process when mental health issues are involved and if disciplinary action becomes necessary.
If a mental health issue is affecting an employee’s ability to perform the duties required of them in their role, it may be reasonable for an employer to commence a performance management process as follows:
o Consider the terms and conditions of the relevant employment contract as they may provide guidance regarding the performance management process that has been
agreed to by both parties
o Ensure that all relevant incidents are documented in a format that can be provided to the employee as evidence of the concerns raised
o Arrange an initial meeting with the employee and reassure them that confidentiality will be strictly maintained. The employee should also be invited to bring a ‘support person’ to the meeting (this can be a family member or friend, but preferably not a work colleague)
o Maintain a record of all discussions held at the initial meeting in a format that can be provided to the employee following the meeting
o The employee should be given the opportunity to respond to the concerns raised at the initial meeting, whether that be during or following the meeting. The employee should also be offered support and appropriate counselling following the meeting
o Depending on the terms and conditions of their employment contract and the nature of the employer’s concerns, it may be necessary to arrange a follow-up meeting after a reasonable review period to assess whether there has been any improvement in the employee’s behaviour and/or performance
Is it necessary to address mental health issues when performance management is not required?

It is important to note that there is no obligation on an employee to disclose a mental health condition to their employer or prospective employer(s). This presents a difficulty for employers as they have an obligation to support their employees and if necessary, allow for reasonable adjustments in the workplace to avoid aggravating any mental health issues. Reasonable adjustments can include flexible working hours, alternate duties and offering additional supervision, support and counselling.
If an employee has disclosed a mental health issue in the absence of any performance management issues, it is still reasonable for an employer to engage in open dialogue with them and to offer them support and the opportunity to obtain a report from their treating psychologist or psychiatrist in an effort to avoid aggravating their condition in the workplace.
Miga’s Legal Services team can provide advice to our clients requiring assistance and guidance when dealing with workplace investigations, performance management processes and the appropriate management of mental health issues in the workplace.
ANTHONY MENNILLO HEAD OF CLAIMS AND LEGAL SERVICES MIGA



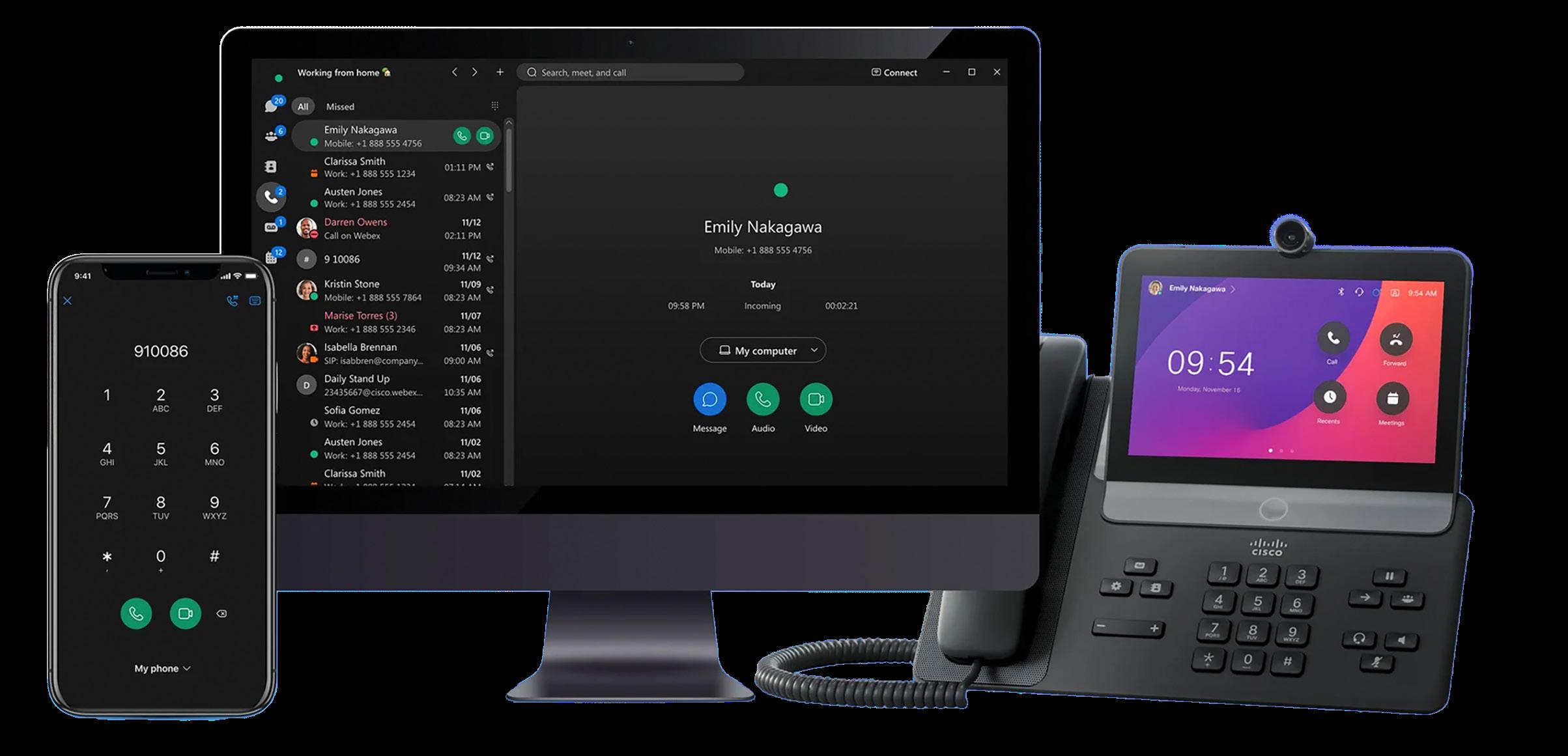
DIGITAL MEDICAL SYSTEMS
The recent Digital Health Festival 2025 (DHF25) held at the Melbourne Convention and Exhibition Centre on 13-14 May was big in every sense, with more than 8,000 attendees, over 200 exhibitors, including over 150 startups, 10 conference theatres with more than 400 speakers, all crammed into two frenetic days1. It was simply impossible to visit every exhibitor and to attend the presentations of interest.
AI and Agentic AI were the overwhelming themes at DHF25 promoted in the latest products and services featured at almost every exhibitor stand, and discussed by so many presenters and in panel discussions; from AI Scribes, digital assistants, Agentic AI telephone receptionist, Agentic AI clinical decision support, Agentic AI for administrative workflows, Agentic AI for cyber security, AI in radiology, AI for clinical coding, AI Virtual care, AI for governance, to … Wow. Too much to absorb all at once…

Summary of AI and Agentic AI Offerings at DHF 2025
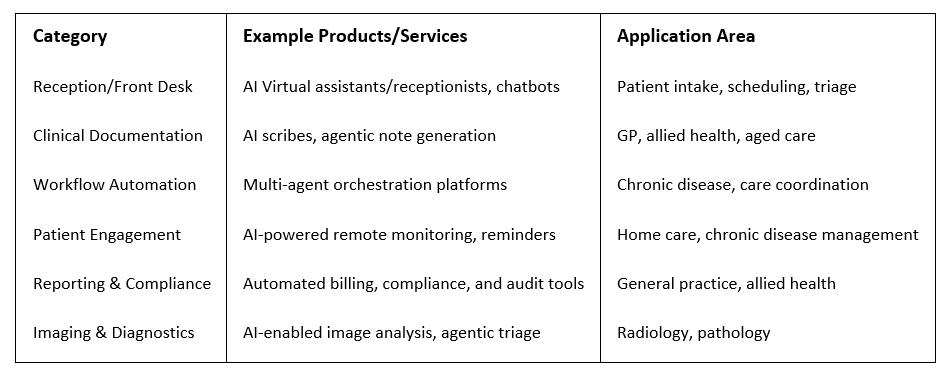
Agentic AI is well and truly here! Perhaps DHF25 should have been called the Festival of AI 2025…
In Bill Gates November 2023 blog post, AI Is About to Completely Change How You Use Computers, Gates foreshadowed the
development of AI “agents” or “personal assistants”:
”You’ll simply tell your device, in everyday language, what you want to do. And depending on how much information you choose to

share with it, the software will be able to respond personally because it will have a rich understanding of your life. In the near future, anyone who’s online will be able to have a personal assistant powered by artificial intelligence that’s far beyond today’s technology. This type of software –something that responds to natural language and can accomplish many different tasks based on its knowledge of the user – is called an agent.
…Agents are not only going to change how everyone interacts with computers. They’re also going to upend the software industry, bringing about the biggest revolution in computing since we went from typing commands to tapping on icons2.”
Gates prediction of a “personal assistant powered by artificial intelligence…” has come to pass in 2025 and is now called Agentic AI. Another tech term to define and understand.
What is Generative AI (Gen AI) again?, What is Agentic AI?, and, What are the differences between Gen AI and Agentic AI?
First let’s refresh our understanding of Gen AI, with a good summary by the Australian eSafety Commissioner:
“ ‘Generative AI’ is a term
used to describe the process of using machine learning to create digital content such as new text, images, audio, video and multimodal simulations of experiences.
This machine learning is often called ‘artificial intelligence’ or ‘AI’. The difference between generative AI and other forms of AI is that its models can create new outputs, instead of just making predictions and classifications like other machine learning systems.
The machine learning that underpins AI is computer modelling that processes information using artificial neural networks, which are mathematical systems structured like the human brain that ‘learn’ skills by finding statistical patterns in the sets of data used to ‘train’ them. The neural networks used for generative AI are built on enormous datasets that are processed using human-like ‘parameters’, which are the factors or limits that define the way something can be done or made.
Some examples of generative AI applications include:
◦ text-based chatbots, or programs designed to simulate conversations with humans, such as Anthropic’s Claude, Bing Chat, ChatGPT, Google Bard, and Snapchat’s My AI
◦ image or video generators, such as the Bing Image Creator,
DALL-E 2, Midjourney, and Stable Diffusion
◦ voice generators, such as Microsoft VALL-E3“
IBM’s Editorial Lead for AI Models, Cole Stryker, explains ‘what is Agentic AI?’:
“Agentic AI is an artificial intelligence system that can accomplish a specific goal with limited supervision. It consists of AI agents— machine learning models that mimic human decisionmaking to solve problems in real time. In a multiagent system, each agent performs a specific subtask required to reach the goal and their efforts are coordinated through AI orchestration.
Unlike traditional AI models, which operate within predefined constraints and require human intervention, agentic AI exhibits autonomy, goal-driven behavior and adaptability. The term “agentic” refers to these models’ agency, or, their capacity to act independently and purposefully.
Agentic AI builds on generative AI (gen AI) techniques by using large language models (LLMs) to function in dynamic environments. While generative models focus on creating content based on learned patterns, agentic AI extends this capability by

applying generative outputs toward specific goals. A generative AI model like OpenAI’s ChatGPT might produce text, images or code, but an agentic AI system can use that generated content to complete complex tasks autonomously by calling external tools. Agents can, for example, not only tell you the best time to climb Mt. Everest given your work schedule, it can also book you a flight and a hotel.4”
To summarise Stryker, Agentic AI moves beyond Generation to Action by the following characteristics:
Agentic AI is Autonomous, Proactive, Specialized, Adaptable, Intuitive, employing;
Perception, Reasoning abilities, Goal setting, Decision-making, Execution, Learning and adaptation, and Orchestration to “automate AI workflows”, and tasks between multiple AI Agents (Multi-Agentic AI Systems, (MAS)5
The answer to “what are the differences between Gen AI and Agentic AI?”, may be explained by comparing the following clinical scenarios:
Scenario 1: Limited AutomationAI scribes
A doctor uses an AI scribe to document the consultation with the patient, where doctor recommends a follow-up appointment with a specialist. The AI scribe records, and transcribes the consultation into patient notes. The doctor checks the
notes and saves the transcript into the patient record. Doctor has saved typing time, and has been able to focus more on the interaction with the patient.
Scenario 2: Agentic AIAutonomous decision making and actions
In contrast, an Agentic AI system could autonomously evaluate the doctor’s recommendation for a follow up appointment with a specialist, taking into account the appropriate timing based on the patient's condition for the follow up specialist appointment, then the Agentic AI would proactively check availability across multiple specialist providers, schedule the appointment, send notifications, insert the appointment into the patient’s calendar and into the specialist’s appointment system, and arrange necessary preparations—all with minimal human intervention, and perhaps all while the patient is with the doctor.
Science fiction? No –Agentic AI is here in 2025.
The use of Agentic AI in healthcare as described above also raises profound questions about the role of human healthcare providers, the nature of the patient-doctor relationship, and appropriate governance structures for highly autonomous systems.
Governments around the world, including Australian governments, have been struggling to understand and to provide timely guidelines and regulations for the use of AI, however, governments and medical regulatory agencies such as TGA6 , AHPRA7, etc., are catching up
with the enormous technological changes, for example, the Australian Government’s National Framework for the assurance of artificial intelligence in government8, or the Australian Government’s Voluntary AI Safety Standard9 , The 10 Guardrails:
“The 10 Guardrails
1. Establish, implement and publish an accountability process including governance, internal capability and a strategy for regulatory compliance.
2. Establish and implement a risk management process to identify and mitigate risks.
3. Protect AI systems, and implement data governance measures to manage data quality and provenance.
4. Test AI models and systems to evaluate model performance and monitor the system once deployed.
5. Enable human control or intervention in an AI system to achieve meaningful human oversight across the life cycle.
6. Inform end-users regarding AI-enabled decisions, interactions with AI and AIgenerated content.
7. Establish processes for people impacted by AI systems to challenge use or outcomes.
8. Be transparent with other organisations across the AI supply chain about data, models and systems to help them effectively address risks.

9. Keep and maintain records to allow third parties to assess compliance with guardrails.
10. Engage your stakeholders and evaluate their needs and circumstances, with a focus on safety, diversity, inclusion and fairness.”10 , We would do well to heed the advice regarding the use of AI by Dr Ian Oppermann, former NSW Government Chief Data Scientist, and Industry Professor at University of Technology Sydney (UTS):
“For any decision which matters, there must always be an empowered, capable and responsible human in the loop ultimately making that decision. That “humanin-the-loop” cannot just be a rubber stamp extension of the AI driven process.”11
Agentic AI will change your healthcare practice workflows and will be used to assist in either partially or fully completing those important and recurring tasks that happen to be important but tedious, repetitive, time consuming, etc., liberating you and your staff from those manual, tedious tasks so they can focus on the “human in the loop” decision making. Cutting and pasting or exporting data from the clinical/practice management software data “silo”, into another “silo” (e.g., into an Excel spreadsheet), creating a report, emailing the result, etc., all this and more can be done by the AI agent, ready to be approved by the human.
Get ready for the coming wave of practical digital assistants that follow instructions, get information (data),
References
1 https://www.digitalhealthfest.com.au/
2 Gates, B., (2023), AI is about to completely change how you use computers, retrieved from https://www.gatesnotes. com/AI-agents
3 esafety.gov.au, (2025)., Generative AI – position statement, retrieved from https://www.esafety.gov.au/industry/ tech-trends-and-challenges/generativeai
4 Stryker, Cole., (2025)., What is agentic AI?, retrieved from https://www.ibm. com/think/topics/agentic-ai
5 ibid
6T GA.gov.au, (2024)., Artificial Intelligence (AI) and medical device software, retrieved from https://www.tga.gov. au/how-we-regulate/manufacturing/ manufacture-medical-device/manufacture-specific-types-medical-devices/ artificial-intelligence-ai-and-medicaldevice-software
7 AHPRA.gov.au, (2024)., Meeting your professional obligations when using Artificial Intelligence in healthcare, retrieved from https://www.ahpra.gov. au/Resources/Artificial-Intelligence-inhealthcare.aspx
8 Finance.gov.au, (2024)., National Framework for the assurance of artificial intelligence in government, retrieved from https://www.finance.gov.au/ government/public-data/data-anddigital-ministers-meeting/nationalframework-assurance-artificial-intelligence-government
9 Finance.gov.au, (2024), Voluntary AI Safety Standard, retrieved from https:// www.industry.gov.au/publications/ voluntary-ai-safety-standard
10 Finance.gov.au, (2024), Voluntary AI Safety Standard, The 10 Guardrails, retrieved from https://www.industry.
gov.au/publications/voluntary-ai-safetystandard/10-guardrails
11 Oppermann, I., (2023)., The AI genie is out of the bottle – here’s how to regulate it, retrieved from https://thepolicymaker.jmi.org.au/the-ai-genie-is-out-ofthe-bottle-heres-how-to-regulate-it/



Calls to the DMS helpdesk are answered literally within seconds, most issues are resolved within minutes.
Guaranteed Level 2 or Level 3 technicians with extensive experience in Australian medical software problem resolution.
Extensive experience and expertise in Australian medical software ecosystems.
87% of helpdesk calls resolved on the same day.
81% of helpdesk calls resolved on the first call.
Managed Cyber Security expertise. Security first approach with Cyber Security qualified staff.
Proactive Managed IT that is fully customised for Australian medical clinics, with high attention to detail.
DMS Private Cloud located in Melbourne and Sydney at leading Tier 4 data centres with latest high performance, and high capacity host servers.

Hayley Hughes, Practice Manager
Show the next generation of nurses why primary health care is the place to be.


APNA is looking for primar y heal th care workplaces to join us and host students as par t of our National Nursing Clinical Placement Program.
In addition to being paid, you’ll have the full suppor t of our exper t placement team f rom star t to f inish - so no paper work! Best of all, you’ll help build a pipeline of new nursing talent for your workplace
Scan the QR code to learn more about the benef its of hosting students, or email placements@apna asn au today




CUBIKO
In today’s general practice environment, quality improvement has become more than just a requirement. It is an opportunity to shape the future of care we provide, grounded in purpose and driven by intention. For Practice Managers, the key to unlocking this potential lies in the data already sitting within our practices.
When we take the time to understand our data, it becomes much more than a collection of numbers. It becomes a source of truth of our patients, our systems and our team. Data can help us see where care opportunities may be falling through the cracks or where patients may not be getting the follow-up they need. It can help us measure how well we are supporting patients with chronic conditions, how effective our recall and reminder systems are or how well we stay on top of collecting key patient health information. With these insights, we are no longer making decisions in the dark. We are working with clarity.
When we lead quality improvement through data, we are not just leading projects. We are building a culture. One where the whole team understands what we are working towards and why it matters. And
importantly, one where they can see the impact of their efforts.
There is something powerful about sharing a moment of success in a team meeting. Perhaps it is showing how the nursing team’s focus on care planning led to a significant increase in completed GPMPs. Or how the front desk team helped reduce the number of missed appointments by identifying patients most at risk. When team members see the difference they are making, they become more invested in the process. It shifts quality improvement from being a background task to something that is lived and breathed in the day-today rhythm of the practice.
One of the strengths of data is its ability to connect the dots between different parts of the practice. When used well, it creates alignment. Each team member can understand not only what needs to be done, but how their individual role contributes to the bigger picture.
For example, the admin team might use appointment data to identify patients due for their annual health assessments, care plans or vaccines. At the same time, the clinical team is reviewing chronic disease registers and proactively following up on outstanding care plans. When everyone is working from the same information, the practice runs with greater intention and fewer missed opportunities.
And because the insights are drawn from your own patient population, the work feels relevant and real. It is not about generic benchmarks. It is about your patients, your outcomes and your team.
For many practices, programs like the Practice Incentives Program Quality Improvement initiative provide a clear framework for datadriven improvement. While there are reporting requirements involved, there is also a real opportunity here. These measures are a starting point for practices to reflect on their own care delivery, and to explore where they can improve in ways that genuinely benefit their patients.
When data becomes part of everyday decision-making, responding to these programs feels less like a burden and more like a natural extension of the work already being done.
Of course, to make this all work, practices need the right tools in place. That might mean investing in platforms that bring data from different systems together, or tools that make it easy to track progress and identify where to focus next. A simple spreadsheet such as a Quality Improvement Register can help you keep track of current and historical initiatives as well as the key data points from Cubiko or your practice management system related to your work.

In addition to having the right tools, creating time and space for conversations around quality healthcare are essential. Whether it is a regular review in the team meeting or a short catch-up between clinicians and admin staff, building those habits helps bring the data to life.
At its heart, quality improvement is about people. It is about the patients we care for, and the team that delivers that care. Data simply helps us do this with greater clarity and purpose.


Empower your patients to live well and thrive. Join
Our six-month program is designed for experienced nurses who want to expand their skills and knowledge in this growing area of primary health care It includes monthly workshops, access to online training, and peer support through our community of practice
And as it’s entirely online, you can join in wherever you are in Australia!
CDMHA is supported by the Australian Government and costs just $220 for both members and non-members
To learn more about the program and join our waiting list scan the QR code You’ll be the first to know when our next intake opens for registrations.




Cybersecurity is a crucial aspect of running a medical practice. An Avant webinar on cybersecurity and privacy highlighted an alltoo-common scenario, the ramifications, and practical tips to help protect your practice.
The Phishing email
Mary, a receptionist at a busy medical practice, received an email that looked like it was from their telecommunications provider. The email included a link to view an outstanding bill. After clicking the link and entering her Microsoft 365 email and password, Mary realised there was no bill.
The next day, patients started calling about emails they received from the practice, asking them to click a link to view their test results. It turned out the email was a phishing attempt. By entering her credentials, Mary had unknowingly given hackers access to the practice’s email account. The hackers then used this access to send phishing emails to patients.
To prevent these kinds of incidents, it’s crucial to implement multifactor authentication (MFA) to add an extra layer of security and prevent unauthorised access even if passwords are compromised. Regularly training staff to recognise
phishing emails and other cyber threats is also essential. Additionally, avoid using email as a storage system for sensitive information; instead, transfer important data to secure storage locations and delete unnecessary emails.
The network compromise
Following the phishing attack, the practice’s IT provider conducted a thorough threat hunt to check for any further network compromise. They discovered the entire email inbox, containing five years of emails, had been downloaded by the hackers. This meant the hackers had access to a significant amount of sensitive patient information.
To mitigate these risks, it’s important to ensure all critical data is backed up regularly and stored securely, separate from the main network. Engaging an external IT provider with healthcare experience can help
implement robust cybersecurity measures and conduct regular security audits. Additionally, developing a contingency plan to prepare for cyber incidents and ensure operations can continue if systems are compromised is vital.
The data breach notification
The practice, with the help of a law firm, assessed the data breach and determined it was likely to cause serious harm to individuals. They notified the Office of the Information Commissioner (OAIC)
and took steps to contact affected patients. The practice reviewed all emails to identify affected individuals and notify them about the breach, providing guidance on how to protect their data.
To handle such situations effectively, it’s important to be aware of the

requirements under the Notifiable Data Breach scheme and take appropriate steps to notify affected individuals and authorities. Working with legal and public relations experts to create clear and concise communications for patients is crucial. Plus, providing support to staff involved in the incident to manage stress and ensure they understand the steps being taken to resolve the issue is key.
The importance of cyber insurance
Despite best efforts to prevent cyber incidents, they can still occur. Cyber insurance, such as the one offered through Avant Practice Medical Indemnity Insurance, can provide protection and support in the event of a cyber-attack. It can cover cyber incidents involving digital asset damage, extortion, and reputational damage.
Key lessons:
◦ Implement multi-factor authentication (MFA): MFA adds an extra layer of security, making it harder for hackers to access your systems.
◦ Train staff regularly: Regular staff training ensures everyone can recognise and respond to cyber threats.
◦ Ensure regular backups and engage an external IT provider: Regularly back up critical data and store it securely, separate from your main network. An external IT provider with healthcare experience can help implement strong cybersecurity measures and conduct regular audits.
◦ Develop a contingency plan: Have a plan in place to maintain
operations during a cyber incident.
◦ Understand legal obligations: Understand your legal obligations under the Notifiable Data Breach scheme to ensure timely notification of affected individuals and authorities.
◦ Consider cyber insurance for financial protection and expert support: Cyber insurance provides financial protection and expert support in the event of a cyber-attack, covering costs like data recovery, legal fees, and reputational damage.
If you are a victim of a cyber-attack on your practice and you are an Avant practice policy holder, you can contact the medico-legal advice team here, or call 1800 128 268, 24/7 in emergencies.
Not an Avant practice policy holder? Protect your practice with Avant’s comprehensive practice indemnity and complimentary cyber cover for eligible practices. Learn more about our policies here.
Avant webinar: Protecting your practice: A webinar on cybersecurity and privacy
Avant case study: Unauthorised access to patient records
Avant factsheet: Storing, retaining, and disposing of medical records
Avant factsheet: Responding to a cyber security incident
*Fictional character
Disclaimers:
Avant Practice Medical Indemnity Insurance is issued by Avant Insurance Limited ABN 82 003 707 471, AFSL 238 765. The policy wording is available at www.avant.org.au or by contacting us on 1800 128 268. Practices need to consider other forms of insurance including directors’ and officers’ liability, public and products liability, property and business interruption insurance, and workers compensation. Avant Cyber Insurance cover is available to eligible Avant Practice Medical Indemnity Policy holders up to the cessation of their policy and is provided under a Group Policy between Liberty Mutual Insurance Company ABN 61 086 083 605 (Liberty) and Avant Insurance.
IMPORTANT: This publication is not comprehensive and does not constitute legal or medical advice. You should seek legal or other professional advice before relying on any content, and practise proper clinical decision making with regard to the individual circumstances. Persons implementing any recommendations contained in this publication must exercise their own independent skill or judgement or seek appropriate professional advice relevant to their own particular practice. Compliance with any recommendations will not in any way guarantee discharge of the duty of care owed to patients and others coming into contact with the health professional or practice. Avant is not responsible to you or anyone else for any loss suffered in connection with the use of this information. Information is only current at the date initially published.











As readers will be aware, payroll tax has become a pressing and evolving issue for health and medical practices across Australia. This includes medical, dental and allied health practices (collectively referred to in this article as health and medical practices). Legislative, judicial and administrative developments have prompted many of these practices to re-evaluate their business structures and compliance strategies in the face of an increasingly complex regulatory landscape.
The application of payroll tax varies from state to state – not only in enforcement, but also in tax rates and annual wage thresholds. This creates challenges for health and medical practices trying to determine their obligations under the relevant legislation, especially those operating across multiple jurisdictions.
Recent changes to legislation and public rulings have provided greater clarity on potential payroll tax liabilities. Some states have also introduced exemptions and amnesties for practices that meet certain criteria. While these measures are welcomed, they signal a strong focus by state revenue
authorities on compliance and may indicate closer scrutiny of those seeking relief under these schemes. This article outlines the current landscape of payroll tax for health and medical practices and highlights key issues for practice owners and managers to consider going forward.
Previously, contracting arrangements between health and medical practices and practitioners did not attract payroll tax. State revenue authorities generally did not view these arrangements as constituting an employee relationship. This was particularly true where practices provided facilities and administrative services to independent practitioners operating their own businesses.
These arrangements were commonly documented through service agreements. Under these agreements, the practice would collect patient fees (including Medicare entitlements) on behalf of practitioners and remit the balance after deducting service fees for the provision of facilities and support services.
However, landmark cases –particularly the initial decision and subsequent appeal in Thomas and Naaz v Chief Commissioner of State Revenue – found that payroll tax can apply under the extended “relevant contractor” provisions of most state payroll tax laws.
The following is a jurisdiction-byjurisdiction summary of payroll tax rates, thresholds, and the current status of exemptions and amnesties available to health and medical practices.
Queensland
◦ Payroll Tax Rate: 4.75%
◦ Threshold: $1.3 million
On 22 December 2022 (updated 21 February 2024), the Queensland Revenue Office (QRO) issued a public ruling clarifying the application of payroll tax to health and medical practices.
In general, if a practice has a service agreement or any form of contractual relationship with a practitioner, that relationship may constitute a relevant contract, potentially attracting payroll tax.
Some limited exemptions apply –for example, where a practitioner provides services for fewer than 90 days in a financial year. Also, where a practitioner is a natural person who receives fees directly from patients, those payments are not considered wages for payroll tax purposes.
Following legislative amendments, payments from GP practices to GP practitioners are exempt from payroll tax.
For dental practices, a specific amnesty is available for payments made to contracted and registered dentists – excluding those who are common law employees or

otherwise exempt.
To qualify, a dental practice must:
1. be a ‘designated dental clinic’;
2. make a voluntary disclosure;
3. be registered for payroll tax by 30 June 2025; and
4. comply with ongoing disclosure obligations from 1 July 2025.
A ‘designated dental clinic’ includes employers who conduct a health and medical practice and one of the following:
◦ meets registration criteria under section 52 of the Act but are not yet registered for payroll tax in Queensland and makes payments to contracted dentists;
◦ are registered for payroll tax in Queensland but not declaring those payments to contracted dentists;
◦ are undergoing unresolved audit activity in relation to its payments to contracted dentists; or
◦ have been assessed for payments to contracted dentists following an audit.
New South Wales (NSW)
◦ Payroll Tax Rate: 5.45%
◦ Threshold: $1.2 million
From 4 September 2023 to 3 September 2024, a 12 month pause was placed on payroll tax audits for GP practices. Following this, the NSW Government introduced a Bulk-Billing Support Initiative, which:
◦ Waives retrospective payroll tax liabilities up to 4 September 2024; and
◦ Offers rebates for practices that
bulk bill at least 80% of patients in metropolitan areas and 70% in other regions.
Victoria
◦ Payroll Tax Rate: 4.85%
◦ Threshold: $900,000
All Victorian GP practices received a payroll tax exemption for payments made to contractor GPs up to 30 June 2024. An additional 12-month exemption is available to practices that have not yet begun paying payroll tax or received advice on it.
From 1 July 2025, an exemption will apply to wages paid to GPs only for bulk-billed primary healthcare consultations.
South Australia
◦ Payroll Tax Rate: Variable up to 4.95%
◦ Threshold: $1.5 million, with a deduction of up to $600,000
A payroll tax amnesty for GP contractors was available from 1 July 2018 to 30 June 2024. Successful applicants are exempt from payroll tax during that period.
From 1 July 2024, an exemption will apply to payments made to GPs for bulk-billed services, calculated based on the ratio of bulk-billed to total billed items.
This exemption does not apply to medical specialists or dental practitioners for the period after 30 June 2024..
Australian Capital Territory (ACT)
◦ Payroll Tax Rate: 6.85%
◦ Threshold: $2 million
Unpaid payroll tax liabilities have been waived for payments made to
general practitioners (GPs) prior to 30 June 2023.
An amnesty is in place until 30 June 2025 for GP clinics that:
◦ bulk bill at least 65% of patients;
◦ are registered for MyMedicare; and
◦ registered for payroll tax by 29 February 2024.
Practices must self-assess their bulkbilling rates and provide evidence if requested by the ACT Revenue Office.
Western Australia
◦ Payroll Tax Rate: 5.5%
◦ Threshold: $11 million
Western Australia does not currently apply payroll tax to payments made to GPs.
Northern Territory
◦ Payroll Tax Rate: 5.5%
◦ Threshold: $1.5 million
The Northern Territory has not issued any specific public guidance on the application of payroll tax to health and medical practices, nor has it introduced any amnesties or exemptions. Its position remains unclear.
Tasmania
◦ Payroll Tax Rate: 6.1%
◦ Threshold: $1,250,001
Like the Northern Territory, Tasmania has not released public guidance regarding the application of payroll tax to health and medical practices. No amnesties or exemptions have been announced to date.

Several amnesties and concessions come with ongoing disclosure obligations to state revenue authorities. These obligations may be extensive and long-term. Practices should carefully assess the suitability of entering such arrangements, considering both payroll tax and broader operational and legal implications.
Health and medical practices and practitioners should:
◦ review the relevant legislation and rulings for their operating states or seek advice from trusted legal and accounting experts;
◦ assess whether their practice is near or exceeds the relevant payroll tax threshold;
◦ audit current contracts with practitioners to assess payroll tax exposure;
◦ evaluate eligibility for any applicable amnesties, and understand the deadlines and requirements;
◦ Weigh the benefits of amnesty applications against the obligation to disclose sensitive practice information to relevant state tax authorities; and
◦ engage trusted legal and accounting advisers to tailor a compliance strategy suited to their circumstances.
While some states have clarified their positions, the payroll tax landscape remains in flux across Australia. Health and medical practices should not assume the matter is settled.
Further changes may arise at both state and federal levels. For instance, other states may follow Queensland’s lead in legislating exemptions for GPs or expanding relief to other healthcare sectors.
The courts may also continue to shape the interpretation of payroll tax laws. A notable development was the September 2024 decision in Uber Australia Pty Ltd v Chief Commissioner of State Revenue, where the NSW Supreme Court ruled that Uber’s payments to drivers were not taxable because they were not “for or in relation to the performance of work.” This ruling is a significantly narrower interpretation of the legislation with previous cases involving health and medical practices, including Thomas and Naaz. The appeal decision in this matter is expected to provide important judicial clarification.
How Hillhouse Can Help Hillhouse Legal Partners has an experienced team of legal professionals who support health and medical owners and managers every day with:
◦ drafting or updating service agreements;
◦ providing strategic advice on practical and operational compliance mechanisms to implement best practice systems; and
◦ supporting practice in the event of an audit.
For tailored advice, contact Craig Hong, Director, Hillhouse Legal Partners, on (07) 3220 1144 or via email at craig@hillhouse.com.au.
Exclusive to AAPM Membersreceive a free 30-minute virtual consultation with Hillhouse Legal Partners to review your practice’s business structure and compliance strategies in preparation for the growing complexity of payroll tax obligations.
This is a valuable opportunity to ensure your practice is aligned with best-practice approaches and ready to navigate evolving regulatory requirements with confidence.








MedicMall is the new online marketplace that helps healthcare providers find quality products and services, saving time and money.
For medical practices and private hospitals, MedicMall brings all the products and services you need to run your business, together, in one convenient, intuitive, and easy to use marketplace Which makes it a smarter way to source, compare and buy premium quality, great value products and services from a range of trusted suppliers





Running a general practice today means working at full capacity, all day. From the front desk to the consult room, everyone is managing more complexity, tighter margins, and rising expectations. It’s a constant juggle between clinical care, compliance, admin, and patient needs.
Technology is often held up as the answer, but too often, it becomes part of the problem. We’ve learned to work around disconnected systems. We tolerate multiple programs, clunky interfaces, re-enter the same data in multiple places, and click through extra steps that don’t belong in a day that’s already full.
The past few years have seen rapid digital shifts across healthcare, but not all of them have helped. Some systems look slick in a demo but create more admin in real life. Some automate the wrong things, or bury the right information under too many clicks. And others simply weren’t designed with the pace and pressure of general practice in mind.
The right technology, especially at a time when clinics are stretched, isn’t the one with the most features. It’s the one that knows when to step
forward and when to get out of the way.
The most meaningful innovations in healthcare tech don’t necessarily come from “what’s new”, they come from what’s useful.
When we speak with practices, the feedback is remarkably consistent:
◦ “Help me do the basics faster.”
◦ “Show me what matters before I have to look for it.”
◦ “Reduce the admin, not just move it around.”
For GPs especially, the stakes are high. They work in short, focused bursts, relying on muscle memory to navigate their systems efficiently while still delivering safe, highquality care. When software doesn’t support that rhythm, it slows everything down. And over time, that has a real cost; clinician burnout, missed opportunities, and in some cases, early exits from the profession.
That’s why better design, responsive systems, and smarter workflows aren’t “nice to haves.” They’re essential.
There’s a lot of noise around “going cloud.” And while cloud-based systems offer advantages; faster updates, better remote access, and more scalability, the path there needs to be realistic.
Many clinics have been burned by
rushed transitions that replaced reliability with latency, or stripped out useful shortcuts in favour of generic interfaces.
That’s why it’s important to take a slower, more deliberate route. It’s not about switching everything overnight. It’s about giving practices the option to adopt cloud features gradually, without disrupting their core workflows.
Think of it as modernising from the inside out, not rebuilding from scratch.
As technology evolves, so should our expectations. The best software should:
◦ Fit into your existing workflow, not force you to change it
◦ Reduce duplicate entry and data friction
◦ Make important information visible at the right time
◦ Respect your time and help your team get more done, with less stress
These are the principles shaping the next generation of tools across the industry. Whether cloud-based or hybrid, what matters is how well the software serves the people using it.
The Human Connection Still Comes First
No matter how advanced the technology gets, general practice

is still fundamentally about people. That means systems should support the human side of care, not distract from it.
The right tech should fade into the background when it’s not needed, and step forward only when it can truly help. If a GP can spend more time with their patient and less time on their screen, that’s not a minor improvement, that’s a win for everyone.
Let’s Set a Higher Bar
The future of general practice technology isn’t just about more features, it’s about better ones. Tools that anticipate needs. Interfaces that feel intuitive. Systems that finally work as hard as the teams that use them.
If the last few years have shown us anything, it’s that resilience isn’t just about surviving change, it’s about designing for it.
And that starts with building better software.
DANIELLE BANCROFT CHIEF PRODUCT OFFICER BEST PRACTICE SOFTWARE



When I first joined AAPM in 2015, I was searching for a professional community that could support my growth as a Practice Manager.
Over the years, my experience with AAPM has evolved into something far more enriching than I initially imagined, providing me with invaluable resources, networking opportunities, and a platform to continuously refine my skills.
The Value of Long-Term Membership
Remaining a member of AAPM has been an easy decision. The ongoing professional development programs, industry insights, and peer connections have been instrumental in shaping my career. The ability to stay ahead of industry trends, access expert guidance, and exchange knowledge with fellow professionals has significantly contributed to my success.
Key Benefits of AAPM Membership
One of the most valuable aspects of my membership has been access to educational programs and resources. Whether through webinars, conferences, or networking events, AAPM has consistently provided opportunities to learn, grow, and adapt to the evolving landscape of Practice Management.
Networking and Inspiration
AAPM has fostered meaningful connections that have benefited
my practice in numerous ways. The networking events and conferences have allowed me to engage with like-minded professionals, exchange ideas, and gain fresh perspectives.
One particularly inspiring experience was attending an AAPM event where industry leaders shared innovative strategies for practice management success. Additionally, the vendor area at conferences has been an incredible space to discover the latest products and solutions— some of which I had never encountered before. Several of these insights have directly influenced improvements within my practice.
Overcoming Challenges with AAPM’s Support
Practice Management comes with its fair share of challenges, but AAPM has helped me navigate through them. Whether it’s adapting to regulatory changes, implementing efficient workflows, or enhancing patient care, AAPM’s resources and discussions have provided practical solutions that I’ve successfully integrated into my practice.
Looking Ahead: The Future with AAPM
As the healthcare landscape continues to evolve, AAPM is helping its members prepare for emerging trends. From digital transformation to patient-centered care, AAPM make certain that Practice Managers are equipped with the knowledge and tools needed to thrive.
I look forward to seeing AAPM expand its educational offerings and advocacy efforts, further strengthening its role as a pillar of support for Practice Managers.




You don’t need to be a tech whiz, or spend hours sifting through fiddly data to spot hidden growth opportunities, just a little know-how and a clear strategy.
If you're like most Australian healthcare practices, you’re probably providing the services patients want. But many in your community may not know it.
Why? Because somewhere between the search bar and your bookings page, the journey gets confusing and lost.
And that means missed appointments, underused services, and growth opportunities left on the table.
But there’s good news. Most practices, and businesses of other industries, already have the answers in their digital data.
What Digital Data Are We Talking About?
We're talking about the digital signals your patients already leave behind when they engage with your practice online.
Things like:
◦ Clicks on your website
◦ Which pages they spend time on
◦ Which pages they book on
◦ How they found you (through
Google, social media, or elsewhere)
◦ What search terms they used
◦ Whether they called or booked online
This data, often sitting quietly in your website analytics, Google Business Profile, or other reports, can help you uncover what services are catching attention, and which ones might need a visibility boost.
For example, our ‘Why Businesses Should Use Social Media’ and ‘5 Awesome Ways to Market Your Healthcare Practice’ article on heartbeatdigital.com.au consistently received big traffic numbers.
This shows us that people are looking for practical, easy-tounderstand marketing tips they can apply to their own business, especially in healthcare..
Common Disconnects We See
We work with healthcare practices across Australia, and we regularly see examples like these:
◦ No page: A clinic runs a popular weight management program but has no dedicated page about it online, so patients never find it, or utilise it.
◦ No paths, no links: A practice offers iron infusions, but the web traffic shows most visitors are only looking at GP bios and never realise it’s an option. This one can be frustrating in regional areas where people unknowingly
assume they have to travel to larger centres for simple services.
◦ Confusing bookings: A page about travel vaccinations gets high traffic, but it isn’t linked to the online bookings, so patients drop off.
These are missed chances to help patients and grow your practice. But the fix doesn’t have to be complicated.

How You Can Use Simple Digital Data to Uncover What Your Patients are Already Looking For:
Start with Search: Look at what search terms people are using to find your practice. Are they Googling "skin checks Port Melbourne" but you’re not mentioning it clearly on your homepage?
How: Use tools like Google Search Console. You’ll often spot common terms you’re ranking for. If you don’t have this set up, it’s worth doing.
Map Attention to Services: Review

your website analytics (or ask us to do it for you). Which service pages get views? Which don’t? What are patients clicking on?
How: You’ll need Google Tag Manager and GA4 (Google Analytics 4) installed correctly. With that in place, you can track pageviews, clicks, and more.
Close the Gaps: If patients are engaging with a service page but not booking, something’s off. Maybe the next step isn’t obvious to visitors, or the booking link is buried, or it just isn’t attractive or offering a nice enough user experience.
How: Look at bookings per traffic, and possibly where people are scrolling to, then consider adding a booking button, or even revamping the page.
Track Conversions: Are calls, form completions, and bookings being tracked? Many practices miss this step. It’s one of the simplest ways to know what’s working.
How: Use Google Tag Manager to view events like clicks on your booking button, calls from your site, or form submissions. This data shows you exactly which actions are being taken.
Use Google Business Profile Insights: Google shows you what search terms people used to find your profile and whether they called, visited your website, or asked for directions. It’s often underused and surprisingly insightful.
How: A quick look now and then can show you what people are actually searching for, and whether your practice is showing up for the right things.
Today, expectations are higher than ever. People want to find what they’re looking for very quickly.
Research:
◦ 10 seconds: Nielsen Norman Group research suggests that online, people make up their mind in 10 seconds, so you’d better wow them pretty quickly.
◦ Milliseconds: Also, Google research and web UX studies (Behaviour & Information Technology Journal), have shown that users often form a first impression in as little as 50 milliseconds (0.05 seconds), but that’s mostly visual/aesthetic.
The other 3-second rule: For actual decision-making (like staying on a page or engaging), 3–5 seconds is a widely accepted estimate in digital marketing circles.
When services are hard to find online, patients don’t think to call your practice. They assume you don’t offer it. And they move on.
A regional NSW clinic we worked with had been offering a sleep apnoea service for over a year. It was listed in just one bullet point on their "Other Services" page.
When we ran a quick digital check, we saw 30+ people per month were landing on their site from searches like "snoring problems", “sleep doctor” and "sleep clinic [town name]". But almost no one booked. We created a dedicated service page, added a clear call to action, and optimised the content using the exact phrases patients were already
searching for.
Bookings tripled in six months. No additional advertising required. Just aligning what the clinic already offered with what patients were already looking for.
Digital Marketing for Healthcare Doesn’t Need to Be Complex
Not everyone wants to talk about bounce rates or ad campaigns. But every healthcare practice deserves to know how to:
◦ Tell if their services are being seen online
◦ Understand what their target patients are looking for
◦ Make booking those services easier
We’ll never throw tech jargon at you or try to sell something you don’t need. Our job is to give you practical insights, backed by real data, and help you grow the services that matter most.
Want to Know What Your Patients Are Really Searching For?
Let's Talk Strategy
(It's Easier Than You Think)
Scan to book a quick, obligationfree chat about how to unlock the


Running a general practice involves more than providing safe and effective care to patients. It also means having clear goals, defined actions, and systems in place to guide both daily operations and long-term development. Strategic and operational planning can help practices make better decisions, allocate resources effectively, improve team performance, and respond to change with greater confidence. This includes planning for workforce development, patient growth, service expansion, technology upgrades, and financial sustainability.
While most practice staff are familiar with emergency plans like fire evacuations, scenarios such as IT system outages, workforce shortages, or the sudden absence of a key team member are increasingly relevant—and may not always be clearly defined or top of mind.
Currently, the Royal Australian College of General Practitioners (RACGP) is developing the 6th edition Standards to reflect evolving changes in general practice.
Although only a first draft has been released and the final version isn’t

expected until 2026, it has offered valuable insight into the likely direction of the new Standards to help your practice prepare and stay ahead when thinking about your strategic and operational planning.
The RACGP 5th edition Standards reference planning through requirements related to business continuity, risk management, information security, and quality improvement. The draft 6th edition is likely to build on this foundation, introducing broader expectations around both strategic and operational planning. Insights from the first draft suggest it will encourage practices to define their purpose, set clear goals, and establish structured actions that support continuous improvement and high-quality care. While emergency and business continuity plans remain important, they’re
likely be explicitly recognised as components within a broader, integrated planning framework.
Even though the final 6th edition Standards may change, it’s advisable for general practices to begin considering these updates now. Early preparation will assist practices in managing future risks, meeting accreditation requirements, and supporting patients and teams more effectively.
What’s
The 5th edition already includes requirements for planning across key areas such as emergency preparedness, business continuity, risk management, and quality improvement—helping practices maintain operational stability and respond to challenges. Emergency planning to date has focused mainly

on events like fires or medical emergencies, with supporting requirements to manage service disruptions.
The draft 6th edition signals a more integrated approach to planning. It places renewed emphasis on both strategic and operational planning as foundations for sustainable practice management. Practices are encouraged to define their mission and values, set long-term goals, and establish practical actions for improvement. This reflects a shift from reactive planning to proactive, forward-thinking leadership and decision-making, emphasising planning as a more dynamic and ongoing process. By integrating planning into regular operations and considering both risks and opportunities, practices can lead with clarity and respond to change with greater confidence.
Planning is being positioned as a core organisational foundation— essential to how practices define their direction, make decisions, and manage everyday operations. This broader recognition supports the development of strategic and operational plans as key tools for building resilient, well-governed practices.
Plans defined
◦ Strategic plan
A strategic plan outlines longterm goals—what your practice stands for and where it’s heading over the next few years. This includes a clear vision, major priorities (e.g., service expansion, patient access, technology investment), and how progress will be measured. Strategic
planning supports big-picture decisions about resource allocation, partnerships, and growth.
◦ Operational plan
An operational plan has a more practical focus—what your team needs to do in the short term to achieve those strategic goals. It outlines actions, responsibilities, timelines, and the tools or resources needed to deliver your objectives.
Both plans should be regularly reviewed, monitored, and updated. They are working tools that support professionalism, quality, ethics, and leadership. The 6th edition draft encourages practices to adopt a more strategic, forward-focused approach that begins with a clear mission and values and is supported by measurable objectives.
What should you plan for?
It’s easy to focus only on obvious risks like fires or extreme weather. But strategic and operational planning goes further—it includes thinking about your practice’s direction, goals, systems, and your ability to deliver care during both expected and unexpected situations. Strategic planning might include goals like expanding services, strengthening patient engagement, or improving access. Operational planning supports those goals through actionable steps— such as hiring staff, improving communication systems, or upgrading clinical software.
Common operational disruptions may include:
◦ Loss of internet or clinical
◦ Staff absences due to illness
◦ Delays in supplies like vaccines or IT equipment
Taking time to consider how these issues would be managed is key. For example:
◦ How would you contact patients if your internet failed?
◦ Who would manage the schedule if a key staff member was suddenly unavailable?
◦ Could you consult remotely if the building was temporarily unusable?
These are operational considerations that link directly to strategic priorities. Asking these questions in advance helps protect patient care, minimise disruptions, and reduce stress when the unexpected occurs. The 6th edition draft also introduces planning considerations for environmental sustainability and digital care, recognising their role in long-term operations. These can be reflected in strategic goals and supported day-to-day—for example, reducing paper use, monitoring energy consumption, or securing telehealth services.
Involve the whole team
One of the most important steps practices can take is to involve the whole team in planning. The RACGP Standards already encourage a team-based approach, and planning is more effective when everyone understands the goals and their role in achieving them.
This doesn’t need to involve formal workshops. Instead, try:

◦ Discussing risks in regular team meetings
◦ Asking team members how they’d respond to various scenarios
◦ Running quick, informal drills (e.g.- for power loss or communication failures)
◦ Making sure staff know where to access emergency contacts and procedures
◦ Providing progress updates in team huddles or monthly meetings
◦ Inviting feedback during plan reviews to uncover gaps or practical solutions
These small steps help embed planning into everyday culture. When the whole team is engaged and informed, your practice is more likely to achieve its goals and adapt successfully to change.
Starting point inclusions for strong planning
Effective planning is most useful when it's structured and actionable. Whether you're developing a strategic, operational, or emergency plan, including key components ensures your team has clear direction, defined responsibilities, and the tools needed to stay on track.
Strategic Plan
◦ Practice values and goals
◦ Three (3) to five (5) year objectives
◦ Measures of success (KPIs, growth targets)
◦ Regular review (e.g., annual strategy sessions)
◦ Patient engagement strategies
Operational Plan
◦ Key actions for the next 12 months
◦ Responsible team members
◦ Timelines and milestones
◦ Progress tracking (weekly or monthly)
◦ Required resources (software, training, policies)
◦ Review mechanisms (checklists, team check-ins)
Emergency and Continuity Plan
◦ Procedures for fire, medical, and evacuation scenarios
◦ Backup systems for IT, communications, and records
◦ Alternative service delivery arrangements (e.g., remote consulting)
◦ Testing and updates of emergency procedures
Final thoughts
Planning doesn’t have to be complex or time-consuming—but it does need to be consistent and embedded in how your practice operates. As the RACGP refines the 6th edition Standards, we’re gaining clearer insight into the future of general practice.
Practices that prepare now—by creating practical, inclusive plans and involving their teams—will be well positioned to meet emerging requirements and continue delivering safe, high-quality care.
AGPAL and QIP are leading accreditation providers across Australia’s health, community and human services sectors. AGPAL is proud to be the exclusive agency chosen to pilot the 6th edition Standards. This opportunity will provide us with unique insight into the proposed Standards’ applicability to best support practice teams during the transition process. As we await further release details, we encourage you to follow AGPAL & QIP via our social media channels for future updates:
AGPAL | LinkedIn @AGPALaccredited | Facebook @AGPALaccredited
QIP | LinkedIn @QIPaccredited | Facebook @QIPaccredited
