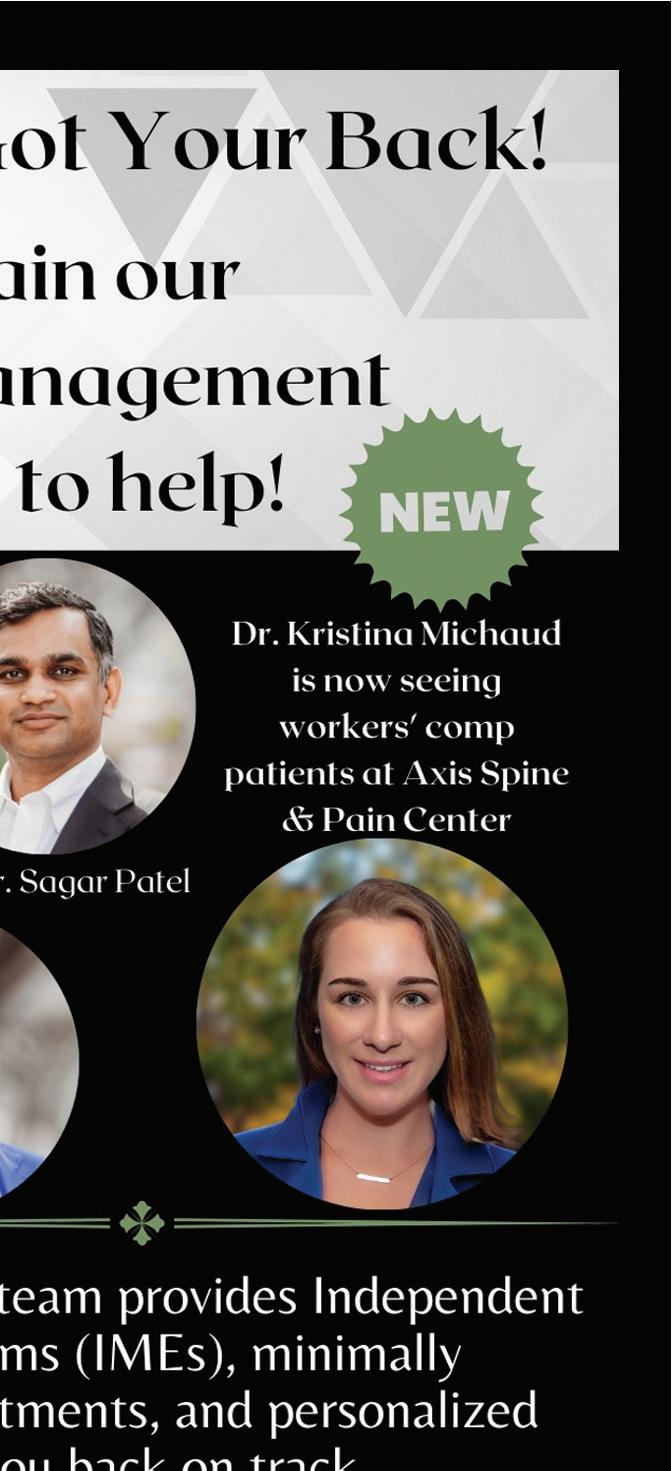
















Tiffany Langeman, PA-C
Physician Assistants (PAs) and Nurse Practitioners (NPs) are collectively known as Advanced Practice Providers (APPs). APPs have been working in medicine for the past sixty years and have proven themselves valuable members of a patient’s healthcare team. They have advanced degrees and maintain a state medical license. APPs work collaboratively with physicians to improve patient care, playing a critical role in the care and management of patients within the workers’ compensation system.
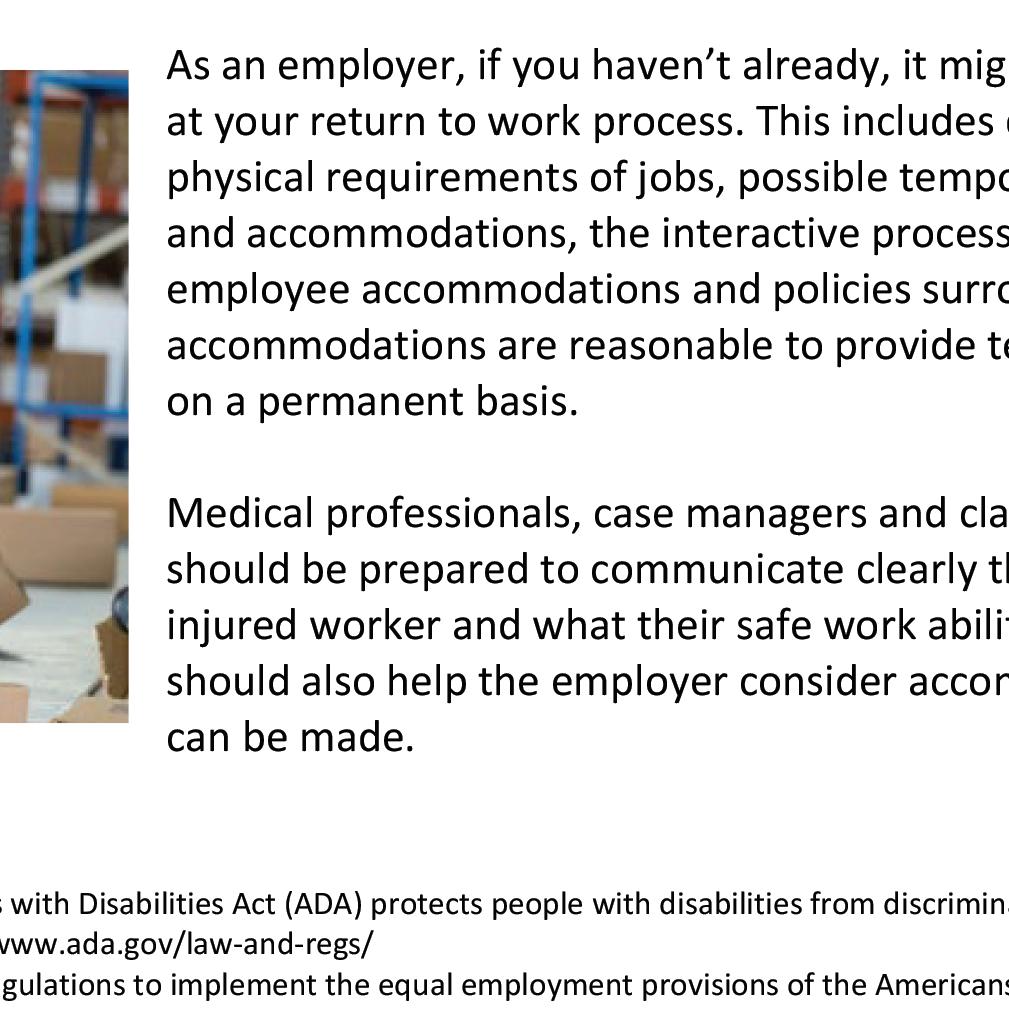
1. Initial Evaluation and Diagnosis: When a person is injured at work, it is best if they are seen quickly for an initial evaluation. APPs often serve as the first point of contact for patients, performing a detailed history and physical exam. They can also order any diagnostic testing that may be needed to assess the extent of the injury. Having the injured worker see a medical practice that has both an APP and a physician can allow for the patient to be seen sooner as there is often more flexibility in scheduling.
2. Treatment and Planning the Return to Work: Once a diagnosis is made, APPs can work with their physician to develop individualized treatment plans aimed at pain relief, recovery, and returning the patient to work. They can prescribe medications, start physical therapy, and explore other interventional treatment options if indicated. PAs and NPs can work closely with their supervising physician to help tailor the patient’s treatment to the specific demands of the patient’s occupation, considering factors such as job responsibilities and physical responsibilities of the job.
Often, there are many forms and paperwork that must be filled out so the treatment plan and timeline for recovery can be shared with the employers, case managers, and others involved in the rehabilitation of the injured worker. APPs can make the entire process move faster so the injured party can get pain relief and back to work safely.
3. Monitoring Progress and Returning to Work: PAs and NPs also play a key role in monitoring the patient’s progress throughout their recovery. APPs can be the first line of contact if the patients have questions or concerns in-between visits. Regular follow-up appointments allow them to assess the effectiveness of treatment, adjust when necessary, and document improvements or setbacks. Their close involvement and collaboration with their supervising physician ensures that patients are on track to regain functionality and return to their jobs safely.
As we all know, every patient deserves a caring and responsive treatment team so they can progress toward being pain-free. In the workers’ compensation space, this also includes returning to work safely and quickly. The addition of Advanced Practice Providers to the treatment team can only benefit all parties involved in making sure the injured worker is appropriately diagnosed and treated for their work-related injury.






Tiffany Langeman, a certified physician assistant at Axion Spine & Neurosurgery in Alpharetta, Georgia, received her undergraduate degree from Wake Forest University and her physician assistant degree from Emory University. Her passion for collaborating with patients to craft an individualized approach to addressing their spine issues is remarkable.



Disclosure: Event dates could be postponed, cancelled, or virtual. Please use the following as a guide. If you would like your event added to the Workplace Health magazine calendar of events, please contact Michelle Wilds at michellewilds@selectonenetwork. com. Workplace Health magazine would love to come and cover your event.

April
2-4- Georgia Public Risk Management Association Conference-Rome, Georgia
3- Atlanta Logistics – Cornhole Tournament
9-11-Florida Bar Workers’ Compensation Forum- Orlando, Florida
9-11-Mississippi WC Educational Conference-Biloxi, Mississippi
22- Alabama DOL WC Seminar- Huntsville, Alabama
23-Georgia State Board of WC Regional Seminar-Alpharetta, Georgia
24-CWCP Recertification Class-Alpharetta, Georgia
30-May 2- National Association of Rehabilitation Providers and AgenciesLegislative and Regulatory AgendaWashington, DC
May
4-7-RISKWORLD 2025- Chicago, Illinois
6-Georgia State Board of WC Regional Seminar-Savannah, Georgia
6-Alabama DOL WC Seminar- Orange Beach, Alabama
8- Atlanta Logistics Annual Golf Tournament- Locust Grove, Georgia
12-14- Alabama SHRM Conference and Expo- Orange Beach, Alabama
14-15- Georgia Mining Association Safety Seminar- Macon, Georgia
15-South Florida PRIMA Meeting- TBD
16-South Carolina WC Employers Association-One Day Seminar on WCColumbia, South Carolina
1-3- Georgia Workers Compensation Association Conference- Jekyll Island, Georgia
1-4-National Council of Self Insureds- St. Petersburg, Florida
1-4-National PRIMA- Seattle, Washington
5- Moore Ingram Johnson & Steele Annual Claims Adjuster Seminar- Atlanta, Georgia
17- South Florida PRIMA Meeting- TBD
21-25- Southern Association of WC Administrators – Port Charlotte, Florida
29-August 2- Florida RIMS-Naples, Florida
30-31- Manufacture Alabama HR, Safety, and Environmental Conference –Birmingham, Alabama


3-5-Alamaba Self Insured ConferenceSandestin, Florida
17-20- WCI-Orlando, Florida
24-27-HR Florida Conference and ExpoKissimmee, Florida
25-27- Georgia State Board of WC Conference- Alpharetta, Georgia
September
3-5-Georgia Safety Conference-Savannah, Georgia
11-Atlanta Logistics Cornhole TournamentHapeville, Georgia
12-Alabama DOL WC Seminar- Orange Beach, Alabama
30-October 2- North Carolina WC Educational Conference-Raleigh, North Carolina
October
8-10- Georgia SHRM Conference- Stone Mountain, Georgia
9- Atlanta Logistics Fall Golf TournamentLocust Grove, Georgia
15-17- National Association of Rehabilitation Providers and Agencies- Fall Conference-Phoenix, Arizona
19-21-South Carolina WC Employers Association Annual Conference- Myrtle Beach, South Carolina
22-Alabama DOL WC SeminarBirmingham, Alabama
25-30-American Congress of Rehabilitation Medicine- Chicago, Illinois
28-Defense Collaborative Atlanta eventTBD
November

6-7- Alabama Workers Compensation Organization-Birmingham, Alabama0
10-14- Southern Association of WC Administrators All Committee ConferenceColorado Springs, Colorado
11-13- National WC and Disability Conference- Nashville, Tennessee
19-21- Tennessee PRIMA Annual Conference- Franklin, Tennessee




















With the opioid crisis still a known issue and concern for physicians, nurse case managers, and the work comp carriers are always looking for alternative options. Not only trying to get away from opioids but also finding noninvasive options to help with musculoskeletal healing and pain management.
While looking for these options, we are also looking for those that are effective, efficient, and are getting our workers back to work faster all while being cost conscious. Hearing the many concerns around DME products and companies regarding cost of the devices, lack of communication, and getting the devices to the patients in a timely manner to help with recovery, we have listened and developed a product line to address these issues and have a team that has the same goals in mind around patient care.
Teaming up with some of the well-known TPAs and Payers around Workers’ Compensation, we are helping by providing solutions to the many concerns around Workers’ Compensation injuries and treatments to get the injured workers back to work faster. Here at Smart Recovery Technologies, we had all this in mind when designing our products.
Working closely with the Carriers and TPAs, we have been able to create a product line that helps speed the recovery process for musculoskeletal healing, helps manage the pain, and speeds the recovery process postoperatively. Offering devices to help with injuries whether acute, sub-acute, non-operative, surgical, or chronic pain issues. We can help all while making sure staying cost efficient and not price gouging.
Offering cutting edge technology with our Pain Away Red Laser, Triad 3LT (Red Light and Infrared Therapy), SmartDVT, Smart-Wave (3 in 1 eStim), Smart-Stim (wireless TENS) and our Smart-Ice Compression (wireless, iceless cold compression), we are truly able to our providers, nurse case managers, and adjusters provide the best and most efficient care options with the same goal in mind, getting our injured workers back to work faster and improving their ADLs. We want to always work together with everyone to provide the best and most cost-efficient options to accomplish the same goals.






David Langham, Judge
Medical care delivery challenges confront us, whether a system is capitalistic, socialistic, or somewhere in between. This is driven by financial economics and broader economics of time, convenience, and consequences. Exacerbating those, we are in an era of persistent change, supercharged by evolving technology and societal pressures.
In 2025, we begin the second quarter of the 21st century. The last twenty-five years brought the Affordable Care Act (Obamacare), extended Medicaid, Medicare secondary payer, and mounting federal debt. Federal omnibus budgets were abandoned in favor of continuing resolutions or supplemental appropriations. Federal spending has largely stumbled from one corner to the next with no global view of a plan, constraint, or destination.
Federal debt exceeds $36 trillion; the interest alone will be $1 trillion annually in 2025 (sixteen percent (16%) of total expenditures). There are many nuances, arguments, and explanations. However, the bottom line is expenses exceed income, and the debt grows. Potential solutions include less expense, greater income, and market growth.
Medicaid alone is about nine percent (9%) of the federal budget, co-funded by state and federal money. Changes in federal law may potentially directly impact state budgets. Secondary payers are impacting insurance, employers, and carriers. Many employees depend on Medicaid. And, recent Medicaid reform discussions suggest imposing mandatory work requirements, enhancing chances of workplace Medicaid interaction.
In the realm of medical care, economic scarcity deserves consideration. Whether one embraces communism, socialism, capitalism, or any “ism,” there is scarcity. The isms merely define or delineate who apportions the scarcity and how. This implicates all goods and services; medicine is not immune.
Provider scarcity is systemic, suppressing supply and raising prices. Physicians today are capable of recently unimaginable miracles. Science is advancing and enhancing care. The first artificial joint surgery in America was a hip replacement in 1969. Today, we see daily joint replacement surgeries, personalized cancer treatment, robotic care, and Mohs surgery—amazing. Each requires specialists. Care consumption (demand) has thus increased and provider populations (supply) have not kept pace.
Broader care complexity is similarly illustrated in the recent popularity of diabetes drugs (GLP-1s) for off-label weight loss for non-diabetics. Many physicians are committed to these novel and expensive treatments ($950$1,350 monthly). Admittedly, controlling weight supports good health, but is medication the “go-to” answer? Some states provide such therapy through Medicaid, but not all. Not all group health carriers provide GLP-1s for nondiabetics. Though America is capitalistic, through Medicaid, the government could exert market influence. Some would argue it already does and would advocate different control. This conversation will continue.
Obesity is pernicious. The U.S. National Institute of Health says “two in five adults” are obese (forty-two percent (42%) of adults). The “children and adolescents” rate is better, but still almost twenty percent (20%). Despite these rates, SNAP (food benefits) is useable for candy, sugary sodas, chips, cookies, and more (though not alcohol or tobacco). There is little limitation on unhealthy food choices. Some see it as the government funding obesity and then funding drug-fueled weight loss.
Another recent supply/demand example is the socialistic United Kingdom National Health Service (NHS). This government system provides medical care for all. Prime Minister Starmer says the NHS should be “reformed from top to bottom.” One reform is “prehabilitation,” which will at least delay surgical intervention for “tens of thousands of patients.” This is direct government control. Prehabilitation will dictate that obese patients and smokers are denied surgery until deemed “fit to proceed,” meaning that they have attempted weight loss and been “urged to quit” smoking. A day could come when “attempted” is not the qualifier. Will care also be rationed?
government programs. Medical care systems will struggle with supply, demand, and regulation. The challenges

The broad point is there are multiple supply and demand issues in care delivery. There are competing goals, increased specialization, insufficient provider volumes, misaligned incentives, and ever-increasing costs. This will impact the workplace through employee-provider access, interaction with Medicaid, and the solvency of government programs. Medical care systems will struggle with supply, demand, and regulation. The challenges seem to persist in various systems, and costs continue to rise.




David Langham has been Florida’s Deputy Chief Judge of Compensation Claims since 2006. He has delivered more than 1,900 professional lectures, published over 40 articles, and 1,800-plus blog posts regarding the law, technology, and professionalism. He authored Florida Workers’ Compensation: Its History, Evolution, and Function (2023) and The Mock Trial Performance (2023). He lives in Pensacola, Florida with his wife Pamela Langham, Esq.






William Zimmerman
In an era where systemic waste and abuse in institutions require vigilant attention, workers’ compensation presents a significant challenge that costs insurance stakeholders an estimated $34 billion annually.
Who is hurt by this besides you?
• Legitimate injured team members - When systems are overburdened with fraudulent claims and premium avoidance, truly injured workers sometimes face increased scrutiny, delayed benefits, and potentially inadequate care as insurers implement stricter verification processes.
• Honest employers - Businesses that properly classify employees and pay accurate premiums effectively subsidize those committing premium deception. This creates an uneven playing field where law-abiding companies face higher costs and competitive disadvantages.
• Consumers - The costs of workers’ compensation waste and abuse are eventually passed on to consumers through higher prices for goods and services as businesses offset their insurance expenses.
• Taxpayers - In some cases, when injured workers cannot get proper benefits through workers’ compensation due to system inefficiencies, they may turn to public assistance programs, shifting costs to taxpayers.
• State economies - States with high levels of workers’ compensation waste experience reduced economic productivity, increased litigation costs, and diverted resources that could otherwise support economic growth and development.
• Insurance systems - The entire insurance market becomes less efficient and more expensive to maintain when significant resources must be devoted to fraud detection and prevention rather than legitimate claim processing.
This staggering figure reflects a system where employer premium waste and abuse and questionable worker behavior—ranging from outright misrepresentation to deliberate protraction of care for conscious or unconscious secondary gain—strains resources and drives up costs across industries.
According to the Coalition Against Insurance Fraud, recent analyses estimate that workers’ compensation waste and abuse results in approximately $34 billion in losses annually across the United States. This figure encompasses various problematic activities, involving the carriers, employers, and injured workers.
Employers engaging in premium avoidance, such as underreporting payroll or misclassifying employees, contribute to about $25 billion of these losses each year.
On the other hand, claim misrepresentation, while less prevalent (is it?), still poses a $9 billion concern. Studies suggest one to two percent (1-2 %) of all workers’ compensation claims involve some form of deception, leading to billions in unwarranted payouts. Meanwhile, providers may engage in less-than-ideal billing practices, such as charging for services not rendered or unnecessary treatments, further inflating costs.
Effective claim management can be hindered by any number of factors, one example being the ability to attract adjusters. The industry is facing a significant challenge with a shortage of claims examiners which is not just a staffing challenge but one that has a spider web effect, leading to decreased efficiency and prolonged claim resolution times. Adjusters who diligently manage excessive caseloads may inadvertently place claims on “autopilot,” as they address the most pressing issues resulting in insufficient oversight and increased opportunities for questionable activities to go undetected.
Improper claims and inefficiencies vary significantly across the U.S. States with higher litigation rates tend to have inflated claims, whereas those with stricter oversight see lower problematic activity. Among the states with the highest workers’ compensation costs per month are Alabama, Mississippi, and Missouri. In contrast, states with the lowest costs include Massachusetts, Texas, and Idaho.
Undisclosed employment during claims has become an increasing concern. Some claimants work “side hustles” while receiving disability benefits. Advanced detection techniques, such as employment searches and social media monitoring, have uncovered numerous cases of workers engaging in alternative employment while collecting benefits.
• Early Reporting and Intervention: Implementing systems for immediate injury reporting can significantly reduce claim costs. Studies show that delays in reporting injuries can increase claim costs by up to fifty-one percent (51%). Early intervention through the prompt direction of care, appropriate medical assessment with key risk indicators, and appropriate treatment plans help prevent claim escalation and reduce long-term disability.
• Team Approach to Claim Management: A collaborative team approach involving claims adjusters, medical providers, injured workers, and employers creates a transparent environment where all stakeholders understand the recovery goals and timeline. Regular communication among all parties helps identify potential issues before they develop into costly problems.
• Ongoing Team Discussions: Regular meetings between healthcare providers, injured workers, and employers help establish clear expectations and monitor progress via both hard and soft data, including specific medical and disability guidelines as well as injured worker input on progress or lack thereof. These discussions should focus on all providers’ clear objective input, injured worker input on progress and roadblocks, realistic recovery timelines, appropriate accommodations, and return-to-work planning. Setting clear benchmarks before issues escalate helps maintain focus on recovery rather than prolonged disability.

There is a critical balance to be achieved amongst the parties to ensure a commitment to the most appropriate, cost-conscious, and expeditious plan to achieve maximal medical improvement and a timely return to work. Without that balance and commitment, the potential for unnecessary waste can spiral, impacting recovery and cost.






William Zimmerman is an insurance professional with over ten years in Workers’ Compensation, emphasizing on employers who retain risk (self-insurance and large deductibles). He speaks on AI, automation, and sales.






















Ben Vinson, Chairman and Chief Appellate Judge
Happy Spring everyone! Hope all of you are having a great start to the year and looking forward to what lies ahead in 2025. On behalf of the State Board of Workers’ Compensation, I am proud to report that 2024 was a successful year across our many divisions and services.
We conducted rehab conferences, mediations, hearings, and appeals, approved numerous settlements, improved our enforcement compliance process, focused on necessary IT projects, and hosted important events as well. We aim to operate efficiently and be responsive to all of our public and private sector stakeholders, so I am particularly grateful to our staff for their hard work to accomplish these goals and keep the Board functioning so well.
On the legislative front, the 2025 Session of the Georgia General Assembly began on January 13, 2025, and kicked off the annual three-month journey. Governor Brian Kemp delivered a significant speech on Tuesday during that first week at the Georgia Chamber Eggs & Issues breakfast and then gave his 2025 State of the State address two days later. He focused on state income tax cuts, tort reform, school safety, and mental health. The Governor also released his budget proposals for the amended FY2025 budget and the FY2026 budget, where he emphasized infrastructure, education, prison reform, and law enforcement. We are following these budget items and other legislation through the process, including proposals affecting professional employer organizations (PEOs), longshoremen, peace officers, and other first responders. We very much appreciate Governor Kemp’s leadership on the important issues for our state.

Our new Settlements Committee of the Advisory Council has been busy and making progress on its mission to analyze issues and suggest improvements to our process. Our settlement division director Michelle Thomas and defense counsel Wade McGuffey are leading this effort and taking input from stakeholders on the nuances and challenges of our occasionally complicated stipulations. I am grateful for their hard work and look forward to implementing some of the changes soon.
Speaking of changes, our IT division has been working diligently to revamp the computer system for investigations by our enforcement division and to upgrade the look and feel of our vital Integrated Claims Management System (ICMS). You can visit our website at https://sbwc.georgia.gov for new features and updates on these and other important developments.
Hope everyone has a fantastic year in 2025. Please join us this spring at our regional seminars in Valdosta, Alpharetta, or Savannah, then mark your calendar for this summer’s annual educational conference to be held August 25-27 at the Hotel Avalon in Alpharetta.


Feel free to contact me anytime with questions or comments about the Board or any other matter.


Ben Vinson is the Chairman and Chief Appellate Judge of the State Board of Workers’ Compensation, appointed by Governor Brian Kemp in May 2021. He handles policy and regulatory issues for the state agency in addition to hearing workers’ compensation cases on appeal. He graduated from Furman University and the University of Georgia School of Law. He resides in Greensboro, Georgia with his wife and two children.










Nelson Gonzalez, OTR/L, CHHC, CCT, CPMT, CORE, CLT
It’s time to face a harsh truth in workers’ compensation: we’re not doing enough. We have the knowledge, the evidence, and the science to do better, yet we continue to overlook this powerful connection. We must step up. For too long, we’ve neglected one of the most critical, yet underappreciated, aspects of recovery—the gut-brain axis.
The gut-brain axis is the communication highway between the gut and the brain. Emerging research shows that this relationship affects everything from sleep and mood to chronic pain and immune function. In the realm of workers’ compensation, where recovery is often long, painful, and complex, addressing the gut-brain axis can be a game-changer. This is not a “nice-to-have” approach—this is essential.
Sleep: When a worker is injured, their sleep quality deteriorates, worsening pain, slowing healing, and impairing cognitive function. A healthy gut microbiome produces serotonin and melatonin, which are essential for restful sleep. If we’re not addressing gut health, we’re prolonging recovery. By ignoring the gutbrain axis, workers will remain trapped in a cycle of poor sleep, stress, and pain.
Nutrition: Injured workers often struggle with poor gut health, which leads to nutrient malabsorption, increased inflammation, and prolonged pain. We cannot afford to ignore this. When we address gut health, we’re not just improving digestion, we’re reducing inflammation and accelerating healing. We’re giving the body the fuel it needs to recover, and we’re empowering workers to rebuild their strength and return to work.
Stress: Chronic stress—whether from the injury itself, financial uncertainty, or recovery—throws the gut microbiome into chaos, leading to inflammation, anxiety, and depression. This vicious cycle must be broken. We have the power to disrupt it by addressing gut health through probiotics, nutrition, and stress-reduction techniques. When we help workers manage stress and heal the gut, we open the door to improved physical and emotional well-being, leading to faster recovery and a return to a purposeful life.
Chronic pain: Chronic pain, particularly persistent pain after an injury, is a silent epidemic. The gut-brain axis plays a pivotal role here. An imbalanced microbiome can amplify pain signals, turning what should be a temporary recovery into a never-ending struggle. Chronic pain is more than just a physical issue—it erodes mental and emotional health, making recovery even harder. But we know that by restoring gut health, we can modulate pain, reduce reliance on medication, and break the vicious cycle. It’s time we start treating chronic pain for what it is—an issue that starts in the gut.
Workers suffering from orthopedic injuries, neurological trauma, amputations, or catastrophic events deserve a comprehensive approach. The gut-brain axis is the missing piece in their recovery puzzle. By addressing it, we can improve pain management, enhance mood, and reduce recovery time. More importantly, we can give these workers hope, dignity, and a reason to keep fighting. It’s not just about getting them back to work; it’s about restoring them to a life of purpose and strength.
As physicians, case managers, adjusters, therapists, and nurses, we cannot afford to wait. The research is clear, the evidence is there, and the time to act is now. We must take this to heart: The gutbrain axis is the key to unlocking the full potential of our injured workers’ recovery. Let’s stop overlooking it. Let’s start addressing it head-on. The future of workers’ compensation depends on it.
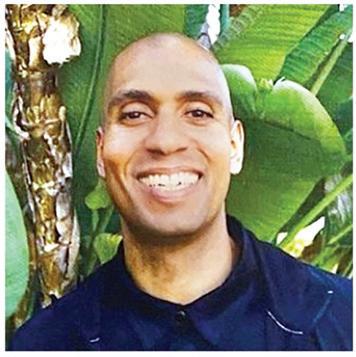
Nelson Gonzalez, Executive Director of Rehab Without Walls Neuro Rehabilitation in Florida, is a published author and occupational therapist with over twenty years of experience. A passionate advocate for chronic stress and the gut-brain axis, he empowers individuals and organizations to overcome stress and build resilient, thriving communities.
Graham Newsome, Esq.
Last year was a whirlwind for employers across the country. From rules issued by the Federal Trade Commission, the U.S. Department of Labor, and rules promulgated by the EEOC to provide guidance on the Pregnant Workers Fairness Act, there was a great deal of information that employers had to keep up with, digest, and implement in the workplace. This new year is sure to be just as tricky with the Trump administration signaling certain changes, like ending taxes on overtime or tips.
There are a few topics for employers to keep an eye on in the coming months:
1.Non-Compete Agreements: As you may recall, on April 23, 2024, the FTC announced its Final Rule to ban non-compete clauses. The Final Rule was set to become effective September 4, 2024. The Final Rule would prohibit an employer from entering into, or attempting to enter into, a non-compete clause with a “worker” (including, e.g., employees and independent contractors) or representing that a worker is subject to a noncompete clause. On August 20, 2024, in the case of Ryan, LLC v. Federal Trade Commission, Civil Action No. 3:24-CV-00986-E (N.D. Tex. 2024) the Honorable Ada E. Brown, U.S. District Court Judge for the Northern District of Texas, struck down the FTC’s ban on non-compete agreements.
The state of the rule remains uncertain; with the Trump administration, there could be guidance coming in the future from the FTC. However, employers should be wary. There are still some state laws that regulate and ban non-competes. In the meantime, employers should be aware of all existing non-competes and review them with legal counsel in the event of substantive changes by the Trump administration.
2.Overtime Thresholds Under the FLSA: On April 23, 2024, the U.S. Department of Labor (DOL) issued a final rule raising salary thresholds for certain overtime exemptions under the Fair Labor Standards Act (FLSA). In essence, the rule raises the minimum salary threshold an employee must be paid to be exempt from overtime. This meant that possibly millions of employees would no longer be exempt under the FLSA and would be entitled to receive overtime for all hours worked over 40 hours in one workweek.
Beginning July 1, 2024, the final rule called for an increase in the threshold for bona fide executive, administrative, and professional employees to $844 per week, which is $43,888 per year. The final rule would have raised the annual compensation threshold for highly compensated employees to $132,964 per year.
Beginning January 1, 2025, the final rule called for a raise of the threshold for bona fide executive, administrative, and professional employees to $1,128 per week, which annualizes to $58,656 per year. The final rule would have raised the annual compensation threshold for highly compensated employees to $151,164 per year.
However, the final rule was vacated, again in the state of Texas, in the case of State of Texas, et al., v. U.S. Dept. of Lab., et al., No. 4:24-CV-00468-SDJ (E.D. Tex. 2024). A Trump-guided U.S. DOL could institute more modest threshold raises, which would still need to be reviewed carefully by employers.
3.Tipped Wages under the FLSA: In 2021, the U.S. Department of Labor promulgated the 80/20/30 Rule. Under the 80/20/30 Rule, an employee is not engaged in a dual occupation while performing “work that produces tips” and “work that directly supports the tip-producing work, if the directly supporting work is not performed for a substantial amount of time.” 29 C.F.R. § 531.56(f) (2021). Under the 80/20/30 Rule, an employer could take a tip credit so long as the employee’s time spent on non-tipped did not exceed 20% of their work time or did not extend beyond a period of 30 minutes. 29 C.F.R. § 531.56(f) (2021).
The Fifth Circuit vacated the 80/20/30 Rule nationally, holding it was contrary to the text of the FLSA and arbitrary and capricious. Rest. L. Ctr. v. United States Dep’t of Lab., 120 F.4th 163, 177 (5th Cir. 2024). Furthermore, the US Department of Labor withdrew the 80/20/30 Rule based on the Fifth Circuit’s decision. 89 Fed. Reg. 101884 (Dec. 17, 2024). However, a new administration could enact an earlier version of the rule that is easier to implement in the workplace, contrary to the rigid and impractical aspects of the 80/20/30 Rule.
4.Independent Contractor Status: On January 10, 2024, the U.S. Department of Labor (DOL) published a final rule, returning to the multifactor, totality-of-the-circumstances analysis to determine whether a worker is an employee or independent contractor under the Fair Labor Standards Act (FLSA). Effective March 11, 2024, the new rule rescinded the January 2021 rule that has governed independent contractor designations since 2021.
The new rule focused on “economic reality” to determine whether an individual is an employee under the FLSA. It establishes a new six-factor totality-of-the-circumstances test: opportunity for profit or loss depending on managerial skill investments by the worker and the potential employer degree of permanence of the work relationship nature and degree of control extent to which the work performed is an integral part of the potential employer’s business skill and initiative
It is possible that the US DOL could return to the 2021 rule, which was issued by the Trump administration. The 2021 rule was more employer-friendly, meaning that individuals were more likely to be classified as independent contractors rather than employees. This is a big difference because numerous laws only apply to employees and not independent contractors, like FMLA, Title VII, and the ADA, just to name a few.





5.State Laws: Employers should also be aware of certain state laws that took effect on January 1 of this year. Some states have enacted laws prohibiting mandatory workplace meetings on certain topics, expanding paid sick leave, providing for family leave outside of traditional sick leave, state increases in minimum wage, and numerous state laws relating to marijuana use. It would be prudent for employers to consult legal counsel and make sure internal HR teams are on the lookout for new laws that take place and begin early strategizing on how to implement new requirements for employers.




Graham Newsome, J.D., is a partner with Chartwell Law out of Atlanta, defending corporations in employment litigation cases. He received both his undergraduate and law degrees from the University of Georgia.

Rafael Gonzalez, Esq.
On January 17, 2025, the Centers for Medicare and Medicaid Services (CMS) announced that Medicare had finally put together the parameters under which it considers Medicare’s interests to have been appropriately taken into consideration when it comes to $0 Workers’ Compensation Medicare Set-Asides (WCMSAs).
This was a long time coming. For more than twenty years, the Medicare Secondary Payer (MSP) leadership team at CMS continued to indicate that $0 WCMSAs would be looked at by Medicare on a case-by-case basis, thereby necessitating submission of a WCMSA to the Workers Compensation Review Contractor (WCRC), the CMS contractor responsible for reviewing and approving WCMSAs, including those that proposed a $0 allocation, if the parties wanted some form of protection or approval from CMS. On January 17, 2025, that old-fashioned, antiquated, obtuse, and burdensome policy came to a screeching halt.
WCMSA Reference Guide Section 4.2
In its latest version of the Workers’ Compensation Medicare Set-Aside Arrangement (WCMSA) Reference Guide, published on January 17, 2025, section numbered 4.2 titled “Indications That Medicare’s Interests Are Protected” indicates that beginning July 17, 2025, CMS will no longer review or approve $0 WCMSAs, but instead now indicates that Medicare’s interests may be appropriately considered and demonstrated through one of the following:
•The individual’s treating physician documents in medical records that to a reasonable degree of medical certainty, the individual will no longer require any treatments or medications related to the settling WC injury or illness; or
•The workers’ compensation insurer or self-insured employer denied responsibility for benefits under the state workers’ compensation law and the insurer or self-insured employer has made no payments for medical treatment or indemnity (except for investigational purposes) prior to settlement; or
•A Court/Commission/Board of competent jurisdiction has determined, by a ruling on the merits, that the workers’ compensation insurer or self-insured employer does not owe any additional medical or indemnity benefits; or
•The workers’ compensation claim was denied by the insurer/self-insured employer within the state statutory timeframe allowed to pay without prejudice (if allowed in that state) during the investigation period.
What do these changes mean for injured workers and their employers and carriers wishing to settle a claim in which no monies will be allocated for future medical care related to the work comp claim? What does this new policy require from the settling parties in order to ensure that Medicare’s future interests have been appropriately considered and the claimant’s future Medicare coverage has been protected?
What follows is a breakdown of Medicare’s 4 stated policies and their requirements for $0 WCMSAs to effectively apply. In other words, according to CMS’ latest policy, if the settling parties can document any one of the following 4 requirements, it is determined that the settling parties have appropriately considered Medicare’s future interests and may settle the file without having to allocate any portion of the settlement amount for future medical needs related to the work injury or illness.



The first stated policy is not new. As a matter of fact, it is the longest-standing CMS policy on how to ensure a $0 WCMSA is appropriate:
1.The injured worker’s treating physician’s written medical opinion documenting that to a reasonable degree of medical certainty the individual will no longer require any treatments or medications related to the WC injury or illness.
B. Claim Denied by Employer/Carrier and No Payments Made
The second stated policy is new. It provides 4 requirements for $0 WCMSAs to effectively apply:
1.The workers’ compensation insurer or self-insured employer must have denied responsibility for benefits under the state workers’ compensation law, and
2.The insurer or self-insured employer must have made no payments for medical treatment or indemnity (except for investigational purposes) prior to settlement, and
3.Medical and indemnity benefits are not actively being paid by the workers’ compensation insurer or selfinsured employer, and
4.The settlement agreement does not allocate a certain amount for specific future or past medical or pharmacy services as a condition of settlement.
The third stated policy is also new. It provides 3 requirements for $0 WCMSAs to effectively apply:
1.A Court/Commission/Board of competent jurisdiction has determined, by a ruling on the merits, that the workers’ compensation insurer or self-insured employer does not owe any further or additional medical or indemnity benefits, and
2.Medical and indemnity benefits are not actively being paid by the workers’ compensation insurer or selfinsured employer, and
3.The settlement agreement does not allocate a certain amount for specific future or past medical or pharmacy services as a condition of settlement.
The fourth stated policy is also new. It provides 3 requirements for $0 WCMSAs to effectively apply:
1.The workers’ compensation claim was denied by the insurer/self-insured employer within the state statutory timeframe allowed to pay without prejudice (if allowed in that state) during the investigation period.
2.Medical and indemnity benefits are not actively being paid by the workers’ compensation insurer or selfinsured employer.
3.The settlement agreement does not allocate a certain amount for specific future or past medical or pharmacy services as a condition of settlement.
Not all situations and factual patterns will fall neatly into these 4 policy scenarios CMS has recently announced. Consequently, we will continue to provide our $0 WCMSA Legal Opinions in situations in which the settling parties seek the verification, analysis, review, conclusions, and assurance from an outside expert source as to whether the facts, issues, documentation, settlement, state and federal statutory law, regulation, administrative policy, and case law warrant a $0 WCMSA. Our legal opinion will ensure the settling parties have appropriately considered Medicare’s future interests, protect the claimant’s future Medicare coverage, and therefore provide legal assurance that the parties may settle the file without having to allocate any portion of the settlement amount for future medical needs related to the work injury or illness.

Rafael Gonzalez is a partner in Cattie & Gonzalez, PLLC, assisting clients in all 50 states and US territories with mandatory reporting, conditional payments, and future medical allocations in auto bodily injury, medical malpractice, nursing home, products liability, no-fault, workers compensation, and wrongful death claims and litigated cases. He earned his Bachelor of Science degree from the University of Florida, and his Jurisprudence Doctorate degree from the Florida State University.






Andrew T. Smith
Temporary Total Disability benefits (TTD) are weekly payments made by the workers’ compensation carrier to the Claimant in certain circumstances. These payments are typically made when an employee is placed out of work by an authorized medical provider. TTD can also be owed when the Employer cannot accommodate the Claimant’s light duty restrictions.
As a workers’ compensation defense attorney, one of the most common questions I receive from adjusters is, “Andrew, can I stop TTD?”
This question arises in many different scenarios. For example, TTD can be terminated within 150 days of the date of the accident if the Claimant returns to a suitable light-duty job with the Employer. The problem with the question, however, is that South Carolina law has established different requirements for terminating TTD depending on the circumstances of the claim.
To begin with, an SCWCC Form 15-I must be filed when TTD benefits are initiated. If still within 150 days of notice of the accident, then the carrier can unilaterally terminate TTD—i.e., without the Claimant’s consent. To do this, the carrier must complete and file a Form 15-II. The Form 15-II must check the box of one for the six grounds to stop TTD, including:
(1) the Claimant returned to work for at least fifteen days and no TPD is due,
(2) the Claimant agrees that he or she can return to work and signs a Form 17, (3) based on a good faith investigation, the claim is denied, (4) the Claimant was released to full duty and full-duty work was offered by the Employer, (5) the Claimant was released at light duty and light duty work was offered by the Employer, or (6) the Claimant has refused authorized medical treatment or evaluation.
While most of these grounds are self-explanatory, it is critical to investigate the merits of the claim quickly if ground #3 is appropriate. Regardless of the basis of the termination of TTD, Form 15-II must be filed immediately, and the Claimant must be served with a copy of the same.
When beyond 150 days from the date of the accident, there are different procedures required in different circumstances for terminating TTD. For example, if the Claimant returns to work at full duty or light duty for the Employer, then the carrier can suspend TTD. Once TTD is suspended, the carrier must obtain and submit a signed Form 17 from the Claimant to terminate TTD. If the Claimant refuses to sign Form 17, then the employer/carrier’s representative must file Form 21 to seek Commission approval of the termination.
In another example, if a Claimant reaches MMI while on TTD, then the carrier must continue TTD until the Claimant either signs a Form 17 or until the Commission can rule at a hearing on the termination of TTD. Although these examples are not exhaustive, they represent two of the most common scenarios regarding TTD termination.
As a practical matter, the easiest way to ensure TTD is properly suspended or terminated is to make a quick call to a defense counsel before taking action.

Andrew T. Smith is a workers’ compensation defense attorney in the Charleston, South Carolina office of Willson Jones Carter & Baxley, P.A. Andrew handles a wide variety of workers’ compensation claims. Andrew is also a member of the South Carolina Workers’ Compensation Educational Association. He can be reached at atsmith@wjcblaw.com.



















































Nathan Kukowski, M.D.
Intervertebral discs are essential components of the spine. These discs are cushion-like structures located between the bony vertebrae, acting as shock absorbers for the spine. Composed of a tough outer layer called the annulus fibrosus and a gel-like center known as the nucleus pulposus, their unique composition allows for flexibility of the spine while also contributing to the stability of the spinal column. Due to the repetitive, heavy stresses placed on these discs, they are vulnerable to injury, particularly in the lower back, otherwise known as the lumbar spine.
A lumbar disc herniation occurs when the nucleus pulposus pushes through the weakened or damaged annulus fibrosus, possibly resulting in nerve compression. This condition is prevalent in the workplace due to the physical demands placed on the lumbar spine which bears the brunt of lifting, twisting, and other strenuous activities. Workers in physically demanding roles are at heightened risk, although those with sedentary jobs can also be affected by poor ergonomics and posture.
Lumbar disc herniations often arise from a combination of degenerative changes and mechanical stress. Over time, discs lose hydration and elasticity, making them more prone to tearing. Acute injuries from lifting heavy objects, twisting motions, or falls are common precipitators.
Lumbar disc herniations are most often symptomatic when they impinge upon a nerve root. Specific symptoms can vary depending on the severity and location of the herniation. Common symptoms include lower back pain, sciatica (radiating pain down the leg), numbness, tingling, and muscle weakness. These symptoms can cause significant functional impairment.
In the office, doctors will obtain a medical history, including a detailed description of the injury and symptoms from the patient. A thorough physical examination will test motor strength, sensation, and reflexes to assess for any neurologic deficits. Diagnostic maneuvers specific to lumbar disc herniations, such as a straight leg test or femoral stretch test, may also be performed. If a disc herniation is suspected, imaging studies are needed to confirm the diagnosis.
Magnetic Resonance Imaging (MRI) is the gold standard for diagnosing lumbar disc herniations. It provides detailed images of the soft tissues, allowing visualization of the disc and any nerve impingement. A CT (computed tomography) myelogram can be used in patients unable to undergo an MRI. X-rays may also be employed to assess for abnormal spinal alignment or instability.

The good news is that most lumbar disc herniations can be managed conservatively. Non-operative treatments include physical therapy aimed at strengthening the core muscles, improving flexibility, and correcting posture. Nonsteroidal anti-inflammatory drugs (NSAIDs) and muscle relaxants may be prescribed to alleviate pain and inflammation. Epidural steroid injections can also provide relief by reducing nerve irritation.
Surgery is considered when several weeks of conservative measures fail to provide relief or when there is significant neurological impairment. The most common surgical procedure is a microdiscectomy, where the herniated portion of disc material is removed to relieve pressure on the nerves. This surgery is typically performed under a microscope through a one to two (1-2) inch incision. More complex disc herniations may require a traditional open discectomy to safely remove the disc.


Most surgeons will send patients home on the day of surgery with instructions to limit their bending, twisting, and heavy lifting for approximately six (6) weeks to prevent re-herniation. A full return to activities is expected in three to four months.

Nathan Kukowski, M.D., is a fellowship-trained orthopedic spine surgeon at Georgia Carolina Orthopedics (previously Augusta-Aiken Orthopedic Specialists). He completed his orthopedic surgery residency at Emory University followed by a spine surgery fellowship at Harvard University.















The spine is one of the most vital structures in the human body, supporting the entire weight of the upper body and enabling movement. However, in the workplace, various activities can put excessive strain on the spine, leading to a range of injuries and ailments. These conditions can affect anyone, from office workers to manual laborers, with differing causes and symptoms.
Understanding the most common spine ailments and injuries in the workplace can help prevent long-term damage and improve overall worker health.
1. Lower Back Pain: Lower back pain is one of the most prevalent spine-related ailments seen in the workplace. It affects people in all types of jobs, from desk workers to those in physically demanding roles. For office workers, poor posture, prolonged sitting, and improper ergonomics often contribute to strain on the lower back. In manual labor jobs, heavy lifting, bending, twisting, and repetitive movements can cause stress on the lumbar spine, leading to muscle strain or more serious issues like herniated discs. The discomfort can range from mild aches to severe pain that impedes daily functions.
2. Herniated Discs: A herniated disc occurs when one of the discs between the vertebrae in the spine ruptures or slips out of place. This condition often leads to pain, numbness, and weakness, particularly in the lower back or neck. In the workplace, repetitive lifting, poor posture, and sudden movements, such as twisting while lifting, can cause the discs to bulge or rupture. For office workers, sitting for prolonged periods without proper back support can also contribute to this condition. It’s especially common in physically demanding jobs where employees are lifting or handling heavy objects regularly.

3. Spondylolisthesis: Spondylolisthesis occurs when one vertebra slips out of position onto the vertebra below it. This misalignment can result in nerve compression, causing pain, weakness, and numbness in the legs. It can be caused by repetitive stress, improper lifting techniques, or even a congenital defect. In the workplace, workers who engage in tasks involving bending, twisting, or heavy lifting are at a higher risk of developing this condition. It is particularly prevalent in laborintensive jobs, but it can also occur in individuals with poor posture at desks.
4. Muscle Strains and Sprains: Muscle strains and sprains in the workplace can lead to spinal discomfort. A muscle strain occurs when a muscle or tendon is overstretched or torn, while a sprain involves injury to ligaments. These injuries often happen due to improper lifting techniques, sudden movements, or prolonged awkward postures. Workers who engage in repetitive motions, whether they are lifting, bending, or sitting, are susceptible to these types of injuries. Symptoms include localized pain, stiffness, and limited range of motion.
5. Cervical Spine Disorders: The cervical spine, which refers to the neck region of the spine, can also suffer from a range of injuries and ailments. In the workplace, repetitive movements like looking down at screens or holding the head in a fixed position for long periods can lead to cervical strain. Office workers, in particular, are vulnerable to developing conditions such as cervical disc herniation, whiplash, or chronic neck pain due to poor posture or prolonged sitting. Physical tasks involving lifting or turning the head awkwardly can also increase the risk of cervical injuries.
6. Sciatica: Sciatica refers to pain that radiates along the sciatic nerve, which extends from the lower back through the hips and buttocks and down each leg. It typically occurs when the sciatic nerve becomes compressed, often due to a herniated disc or a misaligned vertebra. Sciatica is commonly caused by improper lifting techniques, sitting for long hours, or poor posture. It can lead to severe pain, numbness, and tingling sensations in the legs, and in some cases, it may affect a person’s ability to walk or move comfortably.
Preventing spine injuries in the workplace often requires ergonomic adjustments, proper training, and lifestyle changes. For office workers, investing in ergonomic furniture, taking regular breaks, and practicing good posture can significantly reduce strain. For those in physical labor, learning proper lifting techniques and using assistive devices like lifting belts can help avoid injury. Encouraging regular stretching and strengthening exercises also plays a crucial role in maintaining a healthy spine.
With a combination of awareness, education, and proper care, spine-related ailments in the workplace can be minimized, leading to healthier and more productive employees.

Dr. Parker is a specialist in spine surgery treating disorders including cervical, thoracic, and lumbar. He graduated cum laude from the University of Alabama at Birmingham in 1989 and did his residency in orthopaedic surgery at Emory University School of Medicine in Atlanta, serving as administrative chief resident. He has received numerous honors, has made several spinal health presentations, and has published various papers.






Robyn Lewis, PT, CEAS is Regional Director of WorkStrategies with Select Medical (Physio/ Emory Rehab). She has thirty years of experience in industrial medicine specializing in return to work and injury prevention programs and is certified in Ergonomics, Functional Capacity Evaluations, and Employment Testing.









Steve Heinen
An interesting 60 Minutes piece explained the difference between cost and price. The patriarch of French designer Hermes explained that cost is the actual price of doing something properly with the required level of attention, so you have a quality product (I would add for workers’ comp purposes program or processes). Expensive is not delivering what the product (program or process) is supposed to deliver. One in which you have paid quite a lot of money for the goods or services then betray you. That is expensive.
Therefore, you should choose your workers’ comp vendors carefully. The lowest price and lowest cost are not the same. When selecting your vendors, always choose cost over price.
Here are three (3) tips to help guide you:
Tip 1: Choose your insurance carrier and/or TPA carefully. In most cases there isn’t a claims action plan in place so when a claim happens everyone is upset about the outcome. The employer feels helpless, and predictably workers’ comp costs go up. Not to pick on brokers, remember I am one, but when rates go up so does a broker’s revenue.
Many of my clients have twenty-plus years of relationships with the same carrier or TPA. I know this is old school, but the relationship is built on a strong foundation of partnership.
Takeaway: While some carriers and TPAs are better than others, most are capable of doing a good job. If you partner with them, they will step up their performance. So, forge a relationship. Also, build a claims action plan. A claims action plan ensures that the claims start on the right track. Claims that start on the right track, generally stay on the right track.
Tip 2: You also need to review your other vendors. One of the advantages of being a large, self-insured employer is you can unbundle services. This means instead of the carrier choosing the vendors, the employer does. This is a major cost-reduction strategy. Most employers that aren’t self-insured feel they don’t have a choice which is not true. A consultative insurance broker can weigh in on vendor selection. Input on a wide range of services including legal, private investigators, nurse case management, nurse triage, and technology.
Takeaway: With most insureds, the vendor relationship is transactional and frequently changes. When the employer builds a personal relationship with a vendor it gives the risk management process traction.
Tip 3: Partner with an insurance broker that has a track record for helping organizations improve their risk profile. Most employers do not have a risk manager. This is not a closely guarded secret; brokers make a lot of money. In addition to placing insurance coverage, brokers should step up to serve as their outsourced risk manager. Brokers with a risk management pedigree will make a difference.
Takeaway: The employer has to own their risk profile, but the brokers’ experience makes them an invaluable guide. In addition to recommending the right carrier, they can also recommend the right third-party vendors and a process to tie it all together.



The conclusion to this is: Don’t beat down your vendors. Pay them fairly and then place high expectations on their performance. Georgia has become a very challenging state for workers’ comp. So, paying your vendors to step up and help you manage your risk and insurance program will help you take care of your employees and also reduce costs.

Steve Heinen, CWCP, AAI, and partner with Sterling Seacrest Pritchard, has been an active influencer in the insurance industry since 1983 focusing on Workers’ Compensation. He is also the President of Risk Management Inc. where he developed the comP4® process which has helped organizations reduce workers’ compensation associated costs. He is a graduate of the University of Georgia and is active in the Independent Insurance Agents of Georgia. His Work Comp Playbook for Employers has sold over 6,000 copies.




Graham Newsome, Esq.
The U.S. Department of Labor recently announced that the Occupational Safety and Health Administration has finalized a revision to the personal protective equipment standard for construction (the “New Rule”). The New Rule explicitly requires the equipment to properly fit any construction worker who needs it, improving protections from hazardous conditions. The New Rule becomes effective on January 13, 2025, and amends 29 C.F.R. 1926.95(c).
In response to the proposed rule, OSHA received 85 public comments. The vast majority of commenters supported the change. These commenters generally agreed that the change would provide greater clarity about employers’ responsibility to make sure employees wear properly fitting personal protection equipment (PPE) and would improve the workplace safety and health of construction workers. Some commenters raised concerns about the revisions, stating, for example, that the specifics of the requirement were unclear or that the change would result in prohibitive costs for employers.
The New Rule will have a great impact on both employees and employers in construction industries. The purpose of the New Rule is to ensure that proper size PPE is available to employees on job sites. The revision to the standard adds specific language requiring that employers provide PPE that properly fits construction industry workers. The change aligns the construction industry standard with the standard already in place for the general industry.
Many types of PPE must be sized to fit a worker properly. Improperly sized PPE can be ineffective in protecting workers; create new hazards for the worker, such as oversized gloves or protective clothing being caught in machinery; and discourage use because of discomfort or poor fit. The matter has been a longstanding industry safety concern, particularly among some women as well as among physically smaller or larger workers. The New Rule will require that PPE – such as hard hats, safety harnesses, gloves, and protective footwear – is not only appropriate for protecting against specific job hazards, but also fits each worker properly based on their body size and shape.

In light of this forthcoming update to the rule, construction industry employers should consider taking the following actions:
1.Assess PPE Fit for Each Worker: Employers should assess the fit of PPE for each worker individually. PPE that doesn’t fit properly can reduce its effectiveness, leading to an increased risk of injury and exposure to the employer. This includes evaluating the fit of all types of PPE. For workers with varying body types, employers must ensure that the PPE offered suits different anatomical needs.


2.Inspect PPE for Proper Fit and Functionality: Employers should regularly inspect PPE to ensure that it remains in good condition and fits workers properly throughout their use. You should replace damaged or worn-out equipment immediately to ensure continued protection. Employers are also responsible for ensuring that PPE is properly maintained and adjusted as needed, particularly for workers who may experience changes in body size or shape over time.
3.Provide Training on PPE Usage and Fit: Employers should provide training to workers on how to properly wear, adjust, and maintain their PPE. This includes educating workers on the importance of proper fit for optimal safety and performance, as well as how to adjust equipment to suit their individual needs. Workers should also be taught to identify when PPE no longer fits properly and how to request replacement or adjustment if necessary.


4.Document Compliance Efforts and Maintain Records: Employers should maintain detailed records of their PPE compliance efforts. This includes documentation of PPE assessments, inspections, training sessions, and any instances where PPE was replaced or adjusted for fit. Keeping clear records will ensure that employers are prepared for potential OSHA inspections and audits and demonstrate your commitment to maintaining a safe workplace.
The New Rule snuck into the Federal Register on December 12, 2024, before the Trump Administration’s issuance of the executive order entitled “Regulatory Freeze Pending Review”, issued on January 20, 2025. The executive order, although it did not name OSHA by name, will likely affect other OSHA rules as stated in the relevant part:
•Do not propose or issue any rule in any manner, including by sending a rule to the Office of the Federal Register (the “OFR”), until a department or agency head appointed or designated by the President after noon on January 20, 2025, reviews and approves the rule.
•Immediately withdraw any rules that have been sent to the OFR but not published in the Federal Register, so that they can be reviewed and approved as described in paragraph 1.
•Consistent with applicable law and subject to the exceptions described in paragraph 1, consider postponing for 60 days from the date of this memorandum the effective date for any rules that have been published in the Federal Register, or any rules that have been issued in any manner but have not taken effect, to review any questions of fact, law, and policy that the rules may raise.
While this executive order would not affect the New Rule, it would affect the “Heat Injury and Illness Prevention in Outdoor and Indoor Work Settings” rulemaking and the “Emergency Response Standard” rulemaking.
The challenge for employers will not only be the increased cost of providing PPE in various sizes and styles for a diverse workforce, but also the lack of a clear definition for “proper fit.” This could lead to confusion or disagreement over whether the PPE is suitable and properly fits each employee’s body type.
In conclusion, the implementation of the New Rule by OSHA marks an important step toward enhancing safety and protection for construction workers by ensuring proper fit for all workers, regardless of their body type. While employers may face challenges, such as the cost of providing appropriately sized equipment and addressing ambiguities in the definition of “proper fit,” the New Rule aims to improve both the comfort and effectiveness of PPE. By following the outlined steps, including assessing PPE fit, inspecting equipment regularly, providing training, and documenting compliance, employers can help ensure a safer and more compliant workplace.
Ultimately, the New Rule reflects a necessary evolution in safety standards for construction industries, emphasizing that proper fit is critical to protecting workers in hazardous environments.

Graham Newsome, J.D., is a partner with Chartwell Law out of Atlanta, defending corporations in employment litigation cases. He received both his undergraduate and law degrees from the University of Georgia.
Jaime Sigurdsson
When an injured worker presents to a medical professional with symptoms that don’t match their diagnosis, or ones that seem “exaggerated,” what is the expected plan of care? How do you determine which symptoms are sincere? Which limitations are valid? What is an appropriate treatment plan? How many diagnostic tests do we allow? As medical professionals, how do we identify injured workers who present with symptom magnification and what is the best course of action?
To answer these questions, we must first define symptom magnification and explain the difference between magnification and malingering.
By medical definition, symptom magnification is the conscious or subconscious behavioral pattern where the individual’s subjective reports of symptoms are inconsistent with the known impairment. The individual tends to underrate their abilities and/or overstate their limitations, however, it does not imply intent.
Malingering is the term used when the magnification is both conscious and intended for a variety of secondary gains such as financial compensation; avoiding school, work, or military; obtaining drugs; or getting lighter criminal sentences. Malingering is often tied to fraud, whereas symptom magnification without the goal of a secondary gain may just require a deeper interaction between the medical professional and the patient to determine the cause of the behavior.
To determine symptom magnification all injury evaluations should initially determine if subjective complaints correlate to impairment. If there is questionable correlation then the medical professional should perform distraction-based testing for under-rated functional limitations and compare pain questionnaires to reported and tested function to determine inconsistencies. When symptom magnification is identified, not associated with malingering, then the goal should be to overcome that behavior.
Symptom magnification is most often identified with the following risk factors: low job satisfaction, monotonous/ repetitive work, lower education level, adverse employee-employer relations, recent/new employment, frequent lifting, and ongoing litigation or multiple claims. These risk factors in conjunction with the injured worker struggling to be heard, having a hard time coping with the pain, or struggling with the loss of function may lead to exaggeration of symptoms.
The medical professional needs to disarm the fear that leads to the magnification of symptoms and arm the injured worker with knowledge of the recovery process so that they can improve their potential for successful recovery. When an injured worker is committed to his/her rehabilitation the success rate increases exponentially.
The worst reaction a medical professional can exhibit when confronted with positive symptom magnification is a lack of empathy or frustration with subjective complaints; rushed appointments with minimal time to listen to the patient; and not explaining the recovery time, the process of healing, and the expectations for pain, edema, and gradual improvement in function. When a worker gets injured, just like any other injury, the initial reaction is fear. However, the difference between an injured worker and someone who injures themselves when not working is the ability to guide and determine their medical treatment.
An injury that does not occur at work allows the injured to make all treatment decisions, whereas the injured worker is told which doctor to see, when treatment is authorized, and which medications they are approved to take. When a person has to give up control many times, they feel unheard. Although the medical professionals chosen for the injured workers are often the best in their fi eld, the choice of provider was not made by the injured worker, and therefore preconceived notions of “not being in their best interest” are often formulated. If this is the belief of the injured worker, then the goal is to disarm and engage from day one. Often, this is not the case and therefore their need to be heard is compounded by every medical choice that is made for them.
Physical therapy is often the easiest place to disarm and engage due to the frequency and duration of the rehabilitation process. As opposed to having a monthly appointment with the physician, the injured worker may attend therapy two to three (2-3) times a week for up to eight (8) weeks depending on the extent of the injury. If the therapist can disarm any fear or need to exaggerate symptoms during the initial evaluation while including the patient in their treatment plan and goals, then the road to recovery can be fast and the ability to return to work is improved. This commitment to the injured worker’s recovery by the therapist allows the patient to commit to their care each visit and trust the rehab process. Without the commitment from the patient and the understanding of realistic expectations, there is a risk of delayed or prolonged recovery.
In addition to physical therapy, all medical providers can help overcome symptom magnification by acknowledging the subjective complaints, hence putting more weight on the objective findings and test results. The medical providers need to listen to the injured worker’s concerns and then have a discussion about the expected symptoms that correlate with the diagnosis and the normal course of treatment. It is also important for the medical provider to be the authority and expert, and direct the plan of care. When patients are given the expected rate of recovery and have reasonable expectations of residual pain while feeling heard, they are more likely to accept the process and return to work when able to perform the essential job demands safely; even if they are not yet at prior level of function or without pain.
When symptom magnification is unable to be overcome, the medical providers must maintain the appropriate plan of care, limit discussions of exploratory surgery, avoid multiple diagnostic tests, and limit continued treatment. Continued evidence of symptom magnification with no evidence of objective findings should result in rapid assignment of MMI and release to work.


To return to work, all barriers to rehabilitation should be identified including symptom magnification. When the barrier has the potential to be overcome then it’s the responsibility of the medical provider to acknowledge the limitation to recovery and make every attempt to eliminate or reduce its role in the patient’s treatment. By listening to the injured worker, disarming and engaging them, and allowing them to commit to their recovery, one can facilitate faster discharge to work and back to function.



Jaime Sigurdsson is the CEAS, Vice President and Executive Director of Work Comp Services, CORA Physical Therapy. Jaime graduated from the University of Florida with a Bachelor of Science in Exercise Science. Jaime has worked with CORA for almost twenty-five years and oversees CORA’s WorkTracks program.

Mark Pew
Steve was a highly paid union oil pipeliner in October 2015 when he was involved in a fiery truck crash as another driver drove through a stop sign. It took more than two hours for the “jaws of life” to extract him. A passerby held his hand while he was trapped, even calling his wife, who was over a thousand miles away, to let Steve tell her things he wanted her to know. During that time, he thought he may have killed the other driver, so in those two hours, he was dealing with both physical and psychological pain. To say the circumstances of his occupational injury were traumatic would be an understatement.
The financial impact: The two-thirds compensation rate with a state maximum did not come close to the $5,000 per week income he had before the injury. While the benefits check was helpful, it did not come close to covering his expenses. Four months later, those checks ceased because of the cap on benefits. While “compensation” is ingrained in the name of the industry, he took a gigantic step back financially. It took him nine years to settle the claim, so for almost eight years he and his family had to make major adjustments to their lifestyle. Fortunately, his wife and four children were extremely supportive and accommodating.
The physical and emotional impact: He manages ongoing pain every day. He had to learn how to walk again. He balanced clarity and control when it came to his medications and other pain management regimes after a variety of surgeries and rehabilitation. The industry calls it MMI (maximum medical improvement), but he has had to find a way to work around limitations that did not exist before the accident. At a variety of points during his treatment, he felt like he did not have much to offer his family and community anymore because of his impairment.
The industry’s lesson: Regulations are mandatory. However, they may not be enough to truly restore that injured worker’s life to how it was before the injury or illness, regardless of the level of personal resilience they may have. Adopting a “whole person recovery” mindset will help work comp stakeholders identify issues beyond the letter of the law that will impact outcomes. Regulations or statutes are the minimum, not maximum, expectation.
Steve understands that fraud is real—he knows people who have filed multiple work comp claims—and has an impact on how injured workers can be perceived. He evolved from being offended (“they don’t believe me”) to anger (“how dare they”) to hopeless (“it takes too long; wheels of system turn so slow”) to acceptance (“not going to work again”). Steve also heard stories where the injured worker was treated unfairly, which helped shape his early expectations for how the system would treat him. That is quite a psychological and emotional journey on top of the physical recovery.
The industry’s lesson: Fraud is less than ten percent of all claims and more work comp fraud is perpetrated by employers than employees. Give each injured worker the benefit of the doubt until proven otherwise. An unmistakably skeptical and cynical attitude will come through in conversations and e-mails that increase anxiety, slow the recovery process, and increase the total cost of the claim.
In addition to what the industry can learn from Steve’s experience, he also has advice to share with injured workers:
• The recovery journey may be a long rollercoaster ride, but ultimately it will conclude. The system works, it may just take time. Be assertive but patient.








•Know your rights provided by the jurisdiction’s rules and hold the stakeholders accountable for compliance.
•Maintain high expectations but always be realistic.
•Do your part by embracing what the doctor, therapist, nurse case manager, and other involved clinicians recommend. And assume the claims adjuster is doing their best on your behalf.
•Life post-accident, especially in such a catastrophic case, will be different and it’s not the system’s fault.
•Workers’ compensation is not necessarily “great” but is better than the alternative of having no medical and financial help in the recovery process.
These lessons come directly from someone who has admirably overcome extreme challenges to adapt to his new normal. Steve is an amazingly positive person who, through his perseverance, wants to make a difference with his story and insights. The industry needs to listen and adapt as well.
If you’d like to speak with Steve directly and assist in his quest to help others by using his story, please let me know.

Mark Pew, WorkCompCollege.com founding partner, and Provost, is an award-winning international speaker, author, and jurisdictional advisor in Workers’ Compensation. He is a cofounder of The Transitions and Advancing Advocacy. He has received numerous industry awards and was inducted into Who’s Who in America in 2024.

As technology has progressed, fraud, waste, and abuse (FWA) and billing schemes have also evolved in both speed and sophistication. This is because technology makes it easier for bad actors to accelerate abusive billing and referral schemes. In simple terms, bad actors have been winning the billing war by adopting technology faster than healthcare and workers’ compensation plans. However, with advanced AI technologies, this tech gap does not have to continue, and winning the FWA war has never been more attainable.
How do you need to think about AI in terms of winning the FWA war in your workers’ compensation plan? Here are some key ways AI empowers you:
•See “everything” around the entire episode of care in near real-time,
•Analyze every provider bill, patient encounter, and provider relationship in the context of all historical and current activities,
•Continuously credential providers to ensure they are eligible on every bill,
•Detect provider behaviors, schemes, patterns, outliers, and relationships in near real-time to prevent overpayment and ensure patient safety.
Shows depicting the NSA or CIA racing against time to save the nation and the world are fascinating. That scenario is similar to what workers’ compensation administrators are facing every day. While under assault from bad actors, your plan is trying to care for workers and save the company.
Integr8 AI Risk Detection™ technology is an advanced, patented AI platform that powers the 4L FWA Prevention™ solution. The Integr8 AI patent was issued for the detection of operational threats using artificial intelligence. A second patent was recently issued for collusion detection.
Overbilling and fraudulent referral schemes involving physicians, attorneys, pharmacies, or non-emergency medical transport companies are your daily ‘operational threat’. A technology platform like Integr8 AI enables you to see your FWA and overbilling threats as they are forming, in near real-time and in time to prevent overpayments and ensure the well-being of your employees and members.
AI Turns Simple Bill Review into A Sophisticated Overpayment Detection Machine
Bill review today is usually an old-school, rules-based process. The result is massive overpayment because bills are reviewed individually rather than being analyzed in relationship to all providers and all bills (current and historical).
With advanced AI, you can now understand a bill in the context of how that bill fits into all other bills. It’s like turning the light on in a room versus shining a flashlight into one corner of the room. You need to see ‘everything’ to understand the one thing completely. With a technology like Integr8 AI powering the 4L FWA Prevention™ solution, this means that simple CMS edits turn into over 5.8 million sophisticated permutations and combinations of analyses including procedures and episodes of care on every claim.
AI Saves More & Costs Less Than Traditional Bill Review
Historically, large health plans had vast technological resources to manage payment integrity, while self-insured employers and workers compensation plans lacked the budget for giant, on-premise systems. Today, AI brings the most powerful of all programs and payment integrity capabilities to even the smallest of plans. The ability to flexibly deliver highly automated and sophisticated analysis and increased savings through a cloud-based environment means that big plans and small plans can have the most powerful FWA and overbilling detection and prevention within a matter of days.

Clay Wilemon is the CEO & Chairman of 4L Data Intelligence as well as a founder and investor in healthcare technology and artificial intelligence-based companies. Clay is also a board member of OCTANE, a non-profit economic development organization focused on accelerating tech and med-tech companies in Orange County, CA. His is a graduate of Vanderbilt University.



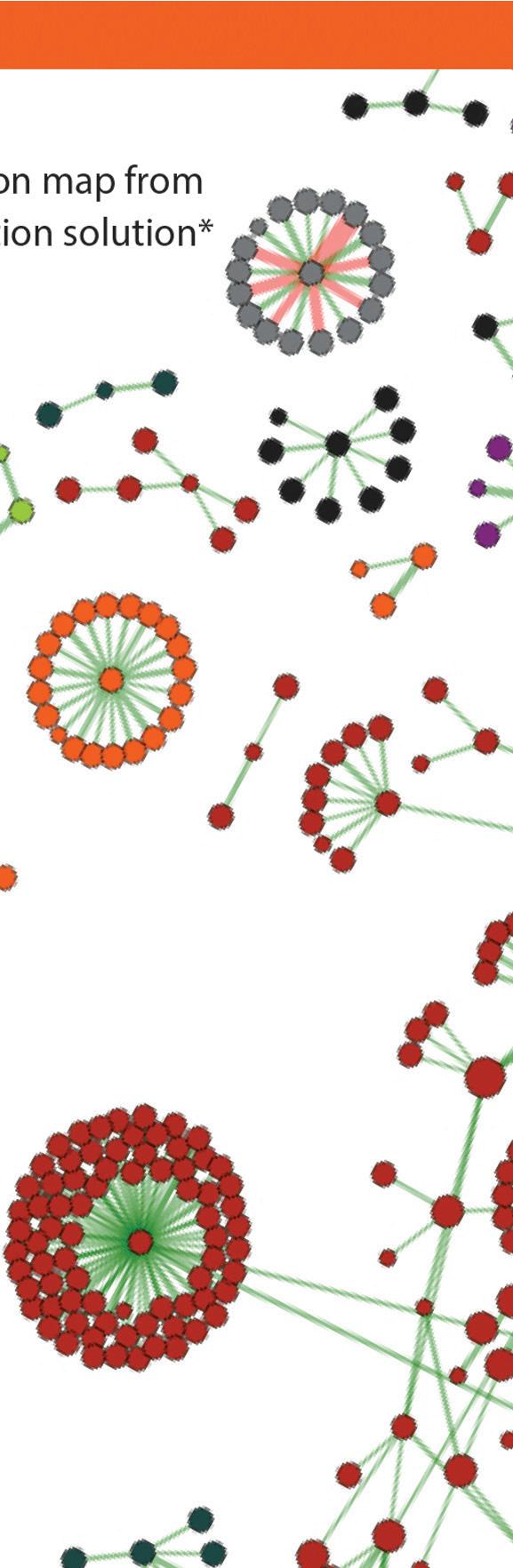

















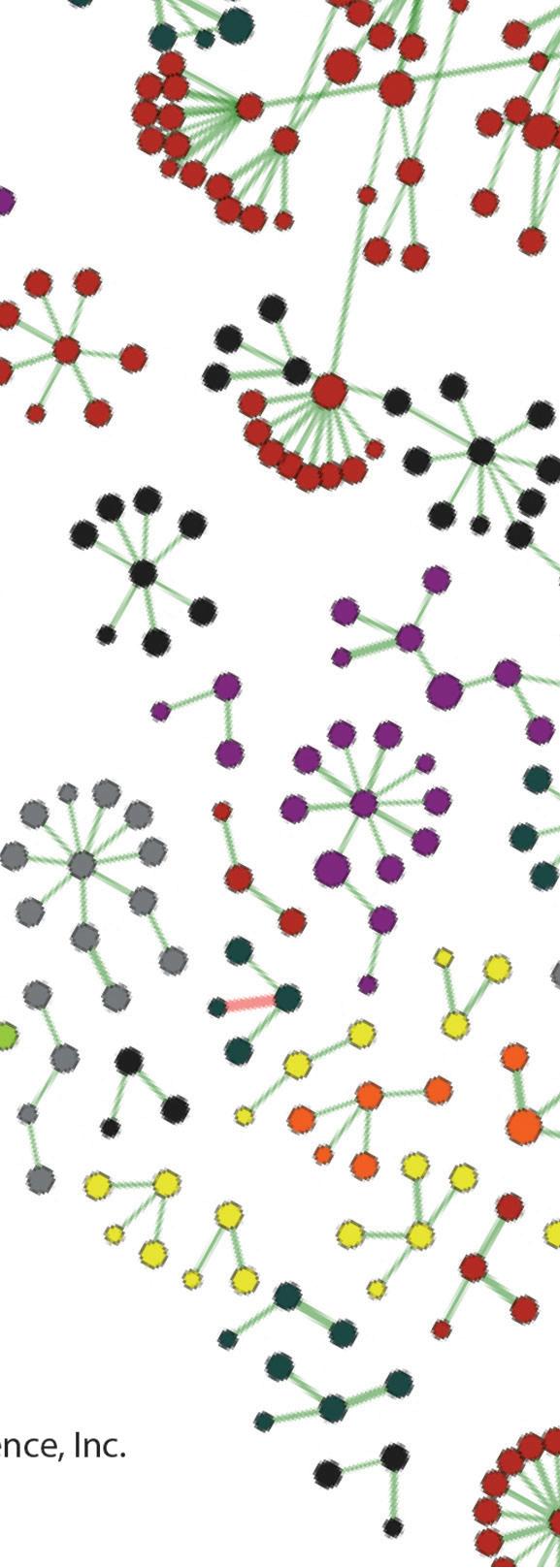
Robert M. Thornsberry, M.D.
Many people will needlessly suffer with even minor orthopaedic issues simply because they’re afraid that the only remedy for their pain is a costly, time-consuming surgery with months of painful healing and follow-up therapy. However… that’s not usually the case. There are very few diagnoses in orthopaedics that don’t have non-surgical treatment alternatives:
Surgery Alternative #1: Time
It is said that “time heals all wounds.” While time may not be the only thing needed to treat all wounds, time is a great ally. Simply relieving symptoms and restoring mobility to allow your body to have the time it needs to heal can be the only steps to remedying many orthopaedic injuries.
The body has great healing potential. When you are injured, the body goes to work releasing agents that signal your body to heal. These agents, however, also start up an inflammation cascade that can cause pain. If you have an injury, RICE therapy works well to reduce the symptoms of inflammation:
•Rest – Don’t exert the injured body part until it is properly healed.
•Ice – Use ice packs for ten minutes at a time to reduce inflammation in the injury.
•Compression – Wrap or bind the injury with compression bandages to reduce and prevent swelling.
•Elevation – Keep the injury elevated above the heart to reduce swelling and inflammation.
When used together, these four treatments help decrease swelling and the presence of pain-causing chemicals in the body.
Surgery Alternative #2: Therapy
Gentle therapy targeting range of motion and strengthening will help you recover. “No pain, no gain” is not the answer. Steady progress is the answer. Most musculoskeletal problems can be solved with physical and RICE therapy.
Provided there is nothing significantly wrong, such as a fracture or torn muscle, you can begin to exercise to restore the general range of motion and experience progressive strengthening soon after your injury.
Sometimes, more advanced therapy is needed. While most people think of physical therapy as the follow-up to surgery, a trained therapist can help educate and guide you in your recovery from almost any musculoskeletal issue. In fact, pursuing therapy before an issue has developed to the point of needing surgery is an excellent way to avoid the surgery in the first place.
Therapists, with their advanced education and experience, can help decrease pain and increase mobility and function. Many therapists utilize various tools and techniques to help control inflammation, such as:
•Ultrasound
•Electrical nerve stimulation
•Massage therapy
•Moist heat
•Other treatment modalities
Alternative
Dozens of over-the-counter and prescription medicines can help control inflammation and pain. Most are short-term aids to control pain while you heal from an injury.
Of these, non-steroidal anti-inflammatory drugs (NSAIDs), of which ibuprofen is the most common, are the mainstay of over-the-counter inflammation management. A short burst of steroids can be of benefit as well.
While these medicines are not entirely without risk, our providers are trained to review your medical history and help you make educated decisions regarding medications.
Alternative
Orthotics, including bracing and foot inserts, can help “realign” the body to aid and control body mechanics to help reduce pain and dysfunction.
When used in combination with other tools and techniques, bracing can aid in overcoming musculoskeletal pain. OrthoGeorgia has trained orthotics specialists who are experts in the field of bracing. These specialists are also skilled in modifying bracing with multiple orthotics – including orthotics controlling the extremities as well as the spine.
Alternative
As stated before, the body can heal itself. It’s the greatest healer. However, choices that we make in our lifestyles can affect our musculoskeletal health.
Foremost among these lifestyle risk factors in the United States is excess weight. Obesity affects our musculoskeletal system in multiple ways, not least of which is simply by requiring our muscles and joints to work exponentially harder. One pound of weight loss is four pounds of pressure off of your knee joints.
Not only does obesity increase the mechanical stress on joints, but it also promotes inflammation. Obese patients have increased inflammatory markers in their bloodstream, resulting in more pain and inflammation.
Likewise, one’s diet can affect musculoskeletal inflammation. There are multiple examples of anti-inflammatory diets available, such as the Mediterranean diet or a vegan diet, that give the body the nutrients it needs without all the inflammatory ingredients that do more harm than good.
To further tackle inflammation, some of the newer drugs for weight loss, known as GLP-1, are showing increasing evidence that they can lead to decreased inflammation in the body. The use of these types of medications is best discussed with one’s primary care physician.
There is abundant advertising for regenerative medicine in the media. Special clinics are popping up everywhere, claiming that they can cure musculoskeletal problems with injections and other medications. Many of these clinics advertise stem cell therapy, blood therapy, and hormone therapy.
OrthoGeorgia offers stem cell therapy and a blood therapy known as platelet-rich plasma therapy. These therapies can help control symptoms of arthritis and assist healing, but they do not “rebuild” damaged joints.
Our providers are up to date on all of these biologics, including their benefits and limitations, but we do not usually recommend them as first-line therapies. While we try to keep our prices reasonable, these treatments are not typically covered by insurance and are fairly expensive. When a patient’s circumstances suggest that one of these treatments might be effective, we can discuss it at that time.
They are not magic bullets but are just another alternative treatment option in the vast array of treatments we offer. Our providers can discuss these and all of our other treatment options in the context of our total treatment program.
Robert M. Thornsberry is a Board-Certified Orthopaedic Surgeon Fellowship Trained in Sports Medicine. He earned his undergraduate degree from Davidson College and received his Doctor of Medicine from the Medical College of Georgia and completed his orthopaedic residency at the University of Kentucky where he spent a year at the Shriner’s Hospital for Crippled Children in Lexington, KY. He also provides care for workers’ compensation injuries.





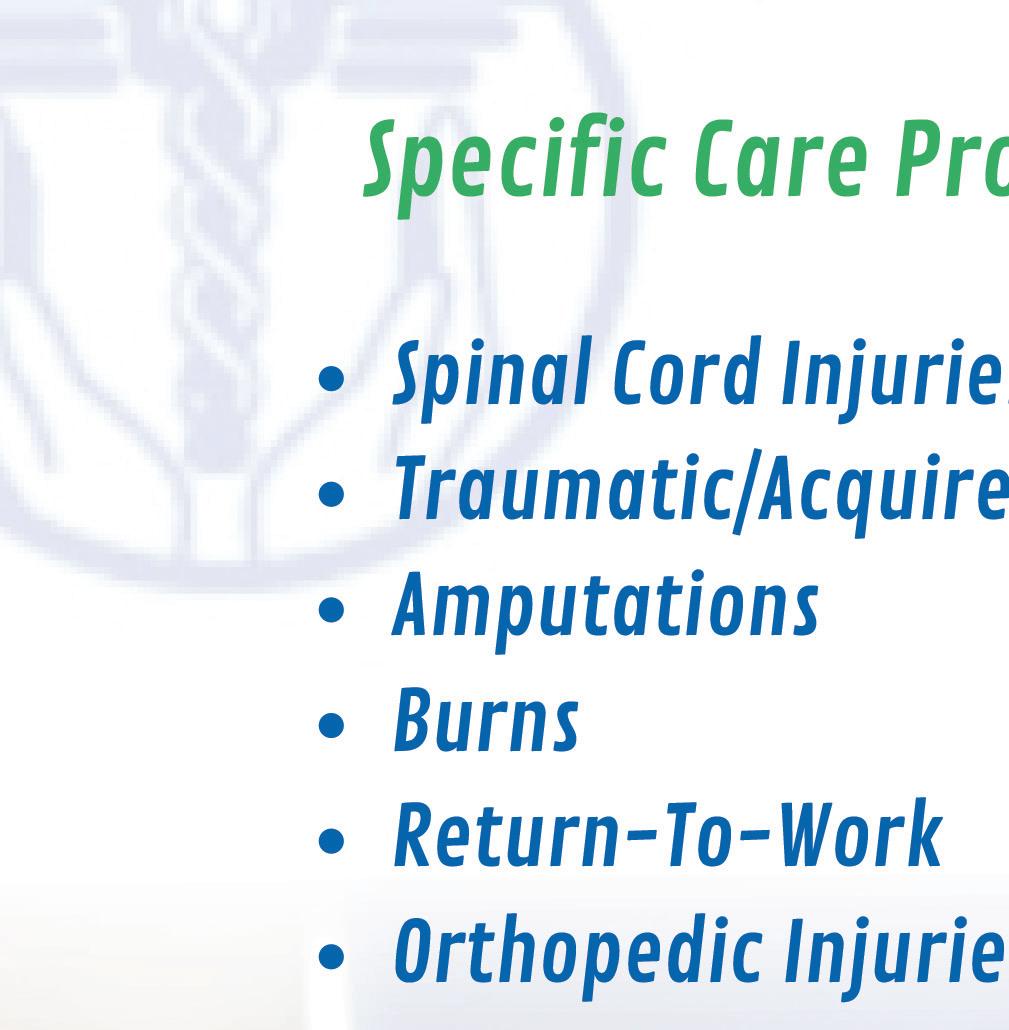




WPH is super excited about our influencers! They are all over the country sharing our magazine at industry events! When you are out and see one of them- snap a picture and post on social media with our hashtag #wphrocks!



Janna Godfrey RN, BSN, CCM
Senior
Area Sales Manager at GENEX
Janna has worked multiple states throughout her career and is an industry leader in her field. Currently working for Genex, we are excited to have Janna as a WPH Influencer in Alabama and Mississippi.
Michael Anderson, VP of National Sales- MTI
A National Industry Leader with ties to every state, we are looking forward to having WPH in all the places Michael goes!
Jackie Woods
Jackie travels extensively across multiple states for CORA Physical Therapy, building strong connections with clients and fostering meaningful relationships. As the Director of Workers’ Compensation Business Development with nine years of experience at CORA, she is passionate about creating new opportunities and collaborations.



The Public Risk Management Association (PRIMA) is North America's largest risk management association dedicated solely to the practice of public entity risk management. For three decades, PRIMA has been dedicated to providing hard-hitting, practical education and training for public entity risk management practitioners like you.
There are more than 2,200 PRIMA member entities, of which 1,800 are local governments. These entities realize that membership provides the necessary tools and solutions needed in today's complex and changing risk management environment.
The Georgia Chapter of the Public Risk Management Association (PRIMA) was established in 2004 to provide education, training and professional development opportunities for public sector risk management professionals in the State of Georgia.
Our mission is to enhance the professional skills of our members through:
• quarterly meetings with topics and speakers directly related to the profession
• our annual Educational Series is generally held in spring, an education-intensive multi-day seminar where members learn, network, and meet with private sector representatives from businesses offering services to the membership.
• Networking opportunities throughout the year, allowing members to effectively share and exchange ideas and solutions with their colleagues.
We work to further the best interests of governments, governmental agencies, intergovernmental risk pools, school districts and other special districts in their risk management activities.


We invite you to join us at an upcoming meeting to discover how Georgia PRIMA can contribute to the success of your risk management programs, and benefit your career through our many professional development opportunities.
Workplace Health is excited to be a partner with Georgia PRIMA.





Garlana Mathews – President and CEO
While Workplace Health has focused on education since its inception, WPH Training Services is a more explicit extension for workers’ compensation stakeholders. In partnership with WorkCompCollege.com, WPH Training Services includes a variety of professional development opportunities for physician offices, employers, and insurance carrier/TPA staff. Workers’ Comp is complicated and nuanced, but once understood, it is a consistent process and suite of expectations.
Many seasoned Workers’ Compensation professionals are retiring and taking their knowledge with them. Partnering with these seasoned industry professionals is important for gathering and transferring knowledge. Collaborating with these experts, sharing ideas, and gaining industry insights will enable our team to deliver top-notch workers’ compensation training.
WPH Training Services contains standard training from WorkCompCollege and (coming soon) training customized specifically for various constituencies of WPH. For those interested in an in-depth understanding of the workers’ compensation ecosystem, you can access the following standardized programs on the WorkCompCollege.com virtual campus at https://workcompcollege.com/
• Workers’ Recovery Professional (WRP): This is a certification comprised of 64 courses/50 hours of content spanning eight schools of discipline (Claims, Humanities, Legal, Medical Management, Regulatory / Legislative, Return to Work, Risk Management, and Stakeholders). This is typically selected by claims professionals who want a broad but detailed understanding of the system’s workings.
• WRP Associate (WRPA): This is a certification comprised of 19 courses/15 hours of content spanning the same eight schools of discipline. This is typically selected by stakeholders involved in the work comp process but not directly managing claims (e.g. customer service representatives, ombudsman, risk managers, service providers). This is often used in onboarding for claims professionals who can continue their education onto the full WRP if desired.
• Advanced Training and Education Center (ATEC): This is a continuing education platform with an ever-increasing library of courses alongside detailed tracks (e.g. Mastering Medical Settlements, Technology Essentials). ATEC also includes the full State Education Program, where human faculty explain not just the letter of the law but also the nuances that come from experience (this currently consists of 33 states). ATEC is a monthly subscription that provides unlimited access to the growing content library.
• MSPCollege: Medicare Secondary Payer (MSP) compliance is a large and complex component of the work comp settlement process. The MSP Accreditation (MSPA) and Medicare Set-Aside Certified Planner (MSACP) curriculum provides expert training modules with a detailed explanation of the process. This is valuable to anyone responsible for compliance or part of an MSA program.
We’re excited about this new partnership and we’re confident that it will bring about positive changes for our industry.













With locations in: Alpharetta, Atlanta, and College Park
Workers’ Compensation Director
Linda Lee: Direct Line: 470.357.0196
Ph: 470-579-3962
Email: workerscomp@axionspine.com
Web address: www.axionspine.com
Physicians: Raymond Walkup, MD • Shane Mangrum, MD

and Pain
With locations in: Macon, Warner Robins, and Dublin
Workers’ Compensation Coordinator
Danielle Bohannon-CWCP Direct Line: 478.333.1275
Fax: 478.449.1466
Email: danielle.bohannon@partnercare.com
Credentialing Coordinator
Samantha Merrell: Direct 478.474.2947 ext 6421
Email: smerrell@axispaincenter.com
Web address: www.axispaincenter.com
Physicians: Chandresh Viradia M.D • Vijay Thillainathan M.D.
• Sagar Patel M.D. • Jacob Prine M.D. • Bryan Covert M.D.
• Kristina Michaud M.D.

Caduceus TeleMed 535 North Central Avenue Hapeville, GA 30354
Workers’ Compensation Coordinator
Jackie Martinez
Ph: 254-TELEMED
Email: telemed@caduceusoccmed.com
Multiple Providers (22 MD/PA/NP)

With locations in: Augusta, Thomson, Sandersville, Waynesboro, Louisville, Evans, and Aiken SC
Workers’ Compensation Coordinator
Alisha Bond: Ph: 706.863.9797 ext 291 | FAX: 706.941.5000
Email: Workerscomp@ortho-augusta.com
Web address: www.augustaaikenortho.com
Augusta- Aiken Physicians: John Bojescul, MD • Justin V. Bundy, MD
• Nicholas M. Capito, MD • Ty William Carter, MD • John H. Franklin, MD
• David Gallagher, MD • Justin M. Head, DO • Douglas E. Holford, MD
• Jeremy M. Jacobs, MD • R. Vaughan Massie, MD • Karim Mahmoud, MD
• Richard W. Pope, MD • Timothy J. Shannon, MD • Mark Snoddy, MD
• Nathan Kukowski, MD • David Doman, MD
Physiatrist: Tara Swim, MD
Legend Orthopedics Physicians: Brian Abell, DO
• Terry Arrington, MD • Randall Meredith, MD
• Zachary Herzwurm, MD • Matthew Link, MD
• Joseph Rectenwald, MD • Douglas Phillips, MD
• Samuel Pitts, MD
Contact for above Legend providers: Keeley LaMarsh: workerscomp@legendortho.com
With locations in: Carrollton, Bremen, and Villa Rica
Workers’ Compensation Coordinator
Sherrie Ford: Direct Line: 770-834-0873 ext 225
Ph: 770-834-0873 | FAX: 770-834-6118
Web address: www.orthowest.com
Physicians: Taylor B. Cates, MD • Kevin M. Charron, MD
• Anthony W. Colpini, MD • Ralph E. Fleck, Jr., MD • Richard A. Herman, MD
• Bryan P. Kirby, MD • Ki Lin, MD • Daniel L. Maxwell, MD
• E. Franklin Pence, Jr., MD • Gregory S. Slappey, MD
• Adam M. Sunderland, MD • Krishna Guidyala, MD • Robert O’Connell, MD

*Optim Health System works in collaboration with Optim Orthopedics and the physician-owned Optim Medical Center-Tattnall. With locations in: Baxley, Brunswick, Claxton, Dublin, Glennville, Hawkinsville, Hinesville, Macon, Metter, Milledgeville, Millen, Reidsville, Rincon, Sandersville, Savannah, Statesboro, Sylvania, Vidalia, and Waycross
Primary Care Physicians in: Glennville, Metter, Millen, Reidsville, and Sylvania, ENT Physician in Vidalia
Physicians:
• Patrick Hanson, MD (Ortho) • Joseph Hegarty, MD (IPM)
• Markus Neiderwanger, MD(IPM) • Kevin L Stevenson, MD(Neurosurgeon)
• Michael D. Dykes MD(IPM) • Rabindar Bhatti, (DO)
• Michael Appeadu, MD(IPM) • Ruben Diaz, MD(IPM)
• R. Wayne Williams, MD FACS (ENT)
Workers’ Compensation Manager
Joshua Sutphen Ph: 912-644-5384 | FAX: 912-644-6190
Direct Line: 912-320-0053
Email: jsutphen@optimorthopedics.com
Web address: www.optimorthopedics.com
Physicians: Don G. Aaron, MD • Thomas Alexander, MD
• Johnathan Christy, MD • Travis Farmer, MD • Delan Gaines, MD
• Jeffrey Goldberg, MD • Juha Jaakkola, MD • Mark Kamaleson, MD
• Gregory Kolovich, MD • Thomas Lawhorne, MD • John McCormick, II, MD
• Thomas Niemeier, MD • Christopher Nicholson, MD
• David Palmer, MD • Justin Lancaster, MD • David M. Sedory, MD
• George Sutherland, MD • James Wilson, Jr, MD • Chad T. Zehms, MD
• Amir Shahien, MD • Robert Shelley, MD • Jordan Paynter, MD
• Wesley Stroud, MD • Jay Cook, MD • Kevin Brooks, MD • John Burke, MD
• Michael Dunn, MD

With locations in: Atlanta and Duluth
Workers’ Compensation Manager
Kathy Fuentes: Direct Line: 404.220.7843
Ph: 404-973-2444
Email: manager@performanceatl.com
Web address: www.performanceatl.com
Physicians: Stephanie Martin, MD


Georgia Bone and Joint
With locations in: Newnan, Fayetteville, Covington, Stockbridge, LaGrange
Workers’ Compensation Coordinator
Donna Stone: Direct Line: 770-502-2128
Ph: 770-502-2175 | FAX: 770-502-2131
Email: Donna.Stone@surgerypartners.com
Web address: www.GeorgiaBoneandJoint.org
Physicians: George Ballantyne, MD
• Michael Gruber, MD • Chad Kessler, MD • Michael Cushing, MD
• Jayson McMath, MD • David Heinsch, MD • Clark Walker, MD
• David Love, MD • Shivam Desai, MD • Michael Webber, MD
• J. Carl Sutton, III, MD • Michael Burke, MD

Safeway Psychological Services
For Mental Health: 170 Specialists across the US
For Cognitive rehabilitation, Post TBI/Speech and language: 6 Specialists across the US
For information and referrals: Phone: 888.306.1119
Referrals@safewaycenters.com
Web Address: www.safewaycenters.com
OrthoGeorgia –Orthopaedic Specialists
With locations in: Macon, Milledgeville, Dublin, Warner Robins, Hawkinsville, and Kathleen
Workers’ Compensation Manager
Peggy Boyles, CWCP Manager (Macon): Direct Line: 478-254-5302 | FAX: 478-832-6509
Email: pboyles@orthoga.org
Drs. Blackwell, Dasher, Lee, Thomas
Workers’ Compensation Coordinators
Rita Boling, CWCP 478-254-5387 rboling@orthoga.org
Drs. Jorgensen, Levina, Thornsberry
Barbara Rodriguez, CWCP 478-242-6379 x 701 brodriguez@orthoga.org
Drs. Harris, Kinnebrew, Ludwig, Yaseen
Dawn Coursey, CWCP 478-254-5363 dcoursey@orthoga.org
Drs. Schnetzer, Robinson, Pope, Chrabuszcz
Amber Hart, CWCP 478-749-1613 ahart@orthoga.org
Drs. Brooks, Floyd, Kelley, Stapleton
Rachel Wiggins, CWCP 478-254-5363 rwiggins@orthoga.org
Drs. Ojo, Patel, Toth
Web address: www.orthoga.org
Physicians: William W. Brooks, MD
• William B. Dasher III MD • Wayne Kelley Jr., MD • Ryan E. Schnetzer, MD
• Jonathan S. Harris, MD • Dennis K. Jorgensen, MD • Todd E. Kinnebrew MD
• Greg P. Lee, MD • Brian J. Ludwig, MD • Wood D. Pope, MD
• Joseph E. Slappey, MD • Timothy R. Stapleton, MD • Richard R. Thomas, MD
• Robert M. Thornsberry, MD • Matthew J. Toth, MD • Zaneb Yaseen, MD
• Robert E. Blackwell, MD • Waldo E. Floyd, MD • Yelena Levina, MD
• Maharsh K. Patel, MD • Elliot P. Robinson, MD • John Z. Chrabuszcz, MD
• Oluwatosin J. Ojo, MD

Advanced Hearing Providers
Ph: 800-598-5300
Email: orders@hearingprovider.com
Web Address: hearingprovider.com

Compass RMS, Risk Management Inc.
Steve Heinen
Ph: 770-540-3810
Email: sheinen@pjins.com
Web Address: Managedcomp.net

Work Bridge Group
National RTW Program Resource
Mail drop locations are situated on both the East and West Coasts
Main - Reno, NV • Corporate – Atlanta, GA (Marietta)
Kerri Butler, Managing Director
Direct Line: 770-294-5936
Ph: 800-890-1620
FAX: 888.530.3222
Emails: Kerri@Workbridgelink.com
Referal@workbridgelink.com
Scheduling@workbridgelink.com
Web Address: www.workbridgelink.com

BeyondCare
470 Johnson Road, Suite 140, Washington, PA 15301
John Tramontina, Executive Vice President Direct Line: 304.216.3258
Ph: 866-839-8819
Email: jtramontina@medicaloutcomeindicators.com
Web Address: beyondcare.us
PBCP Services, LLC
10205 Access Rd Ste B Covington, GA. 30014
Cathy Bowden, MHA, CPC, CPMA, CHISP, CH-CBS
Direct Line: 678-218-9522
Ph: 470-242-7584 ext 101
FAX: 470-443-9230
Email: cathy.bowden@pbcpservices.com

Team Post-Op
14133 NW 8th Street Sunrise, Florida 33325
Oscar Salazar
Direct Line: 954-289-8024 ext 104
Ph: 877-252-0968
FAX: 954.541.5561
Email: info@teampostop.net
Web Address: www.teampostop.net

Jesse Dantice Direct Line: 954-289-8024 ext 104
Ph: 888.405.8893
Emails: jd@zenjuries.com workcomp@zenjuries.com
Web Address: www.zenjuries.com