Sushanth Boda, DO
Degenerative disc disease (DDD) is an “age-old story” - quite literally.
This condition affects approximately thirty to fifty percent (30-50%) of all individuals, with certain studies reporting prevalence rates as high as eighty percent (80%). Discogenic low back pain has a significant ongoing impact, particularly as the aging population continues to grow. While multiple factors contribute to disc degeneration, certain occupational activities—such as posture, heavy lifting, and forceful bending—have been identified as accelerants of lumbar disc degeneration and exacerbating pre-existing disc pathology.
Intervertebral discs are subject to deterioration due to the natural aging process and/or trauma. This degeneration leads to dehydration, flattening, and a reduction in the disc’s inherent cushioning properties. Analogous to the dehydration of grapes into raisins, intervertebral discs undergo a comparable process of water loss over time. Consequently, this dehydration renders the discs more susceptible to mechanical stress, inflammation of the spinal nerves, and the development of low back pain. It is widely believed that alterations in the nucleus pulposus serve as the primary etiology of these degenerative changes. It functions as a “shock absorber” and redistributes the loading forces of the spine. This region exhibits the most pronounced alterations during the early stages of disc degeneration.
Until recently, the current treatment paradigm was lacking an intermediate option to provide patients before considering spinal fusion surgery. Research published by Joshua Anderson et al. yielded a “low return to work rates and other generally poor outcomes…may indicate a more limited role for lumbar fusion among patients with DDD who have workers’ compensation claims.”
Viadisc has emerged as a potentially transformative addition to the treatment paradigm for intervertebral disc degeneration. It represents the first and only nucleus pulposus allograft designed to restore the cushioning function and replace tissue lost due to degenerative changes in the intervertebral disc. Unlike epidural steroid injections, which primarily provide symptomatic relief, Viadisc aims to address the underlying pathology of disc degeneration.
This therapeutic approach offers several advantages. It is administered in an outpatient setting, incision-free, and allows patients to return home the same day with minimal postoperative downtime. Recovery is swift with patients typically resuming normal activities the following day and recommended to avoid physical or strenuous activities for seventy-two (72) hours post-procedure. Over the ensuing weeks, the graft is expected to integrate with the disc, promoting regeneration and repair. Most notably, this therapy is opioid-free; allowing patients to resume work significantly quicker compared to conventional treatment options. This aspect is particularly crucial, given that individuals undergoing chronic opioid therapy have been reported to have a return-to-work rate of only eleven percent (11%).
It is promising to observe that our clinical outcomes at Southern Pain and Spine align with the findings reported in the literature. Investigators have shown at the three-year mark post-Viadisc injection – sixty percent (60%) of patients continued to have at least a fifty percent (50%) pain reduction, while seventy percent (70%) of patients reported an improvement of more than twenty (20) points in their Oswestry Disability Index (ODI) scores. This results overall in a significant reduction in pain, enhancement of functional capacity, and resolution of symptoms in discs exhibiting degeneration as confirmed by imaging.
These results are encouraging and substantiate the potential efficacy of this treatment.


Sushanth Boda, DO, is a board-certified anesthesiologist and interventional pain management physician. He completed his training at New York University and currently practices at Southern Pain and Spine in Newnan, Georgia. He specializes in minimally invasive and opioid-free interventional treatment therapies.



Disclosure: Event dates could be postponed, cancelled, or virtual. Please use the following as a guide. If you would like your event added to the Workplace Health magazine calendar of events, please contact Michelle Wilds at michellewilds@selectonenetwork. com. Workplace Health magazine would love to come and cover your event.
11-13 – Alabama Self Insurers Association Summer Conference, Sandestin, Florida
18-21 – WCI, Orlando, Florida
25-28 – Georgia State Board of Workers’ Compensation Annual Conference, Alpharetta, Georgia
3-6 – Georgia Safety Health and Environmental Annual Conference, Savannah, Georgia
11-12 – Alabama Department of Labor Workers’ Compensation Seminar, Huntsville, Alabama
12 - Defense Collaborative, Fort Worth, Texas
25-27 – SHRM Georgia Annual Conference, Columbus, Georgia
OCTOBER
3 – GWCA Fall Employer Forum, Gainesville, Georgia
11– Inaugural Clay Shoot SCEAA, Camden, South Carolina
15-17 – National Workers’ Compensation
and Disability Conference, Las Vegas, Nevada
22-23 – Alabama Department of Labor Workers’ Compensation Seminar, Birmingham, Alabama
28 – GWCA Kids Chance Golf Tournament, Macon, Georgia
29 – Defense Collaborative, Atlanta, Georgia
4 – FFVA Mutual Golf Invitational, Heathrow Country Club, Lake Mary, Florida
6-8 – Louisiana Self Insured (LASIE)
Annual Conference, Golden Nugget Resort, Lake Charles, Louisiana
7-8 – AWCO Seminar, Birmingham, Alabama
7-9 – IARP National, San Francisco, California
12 – Physio/Emory CEU Symposium, Atlanta, Georgia
18-22 – SAWCA All Committee Meeting, Amelia Island, Florida
5 – SCEAA Regional Event, Columbia, South Carolina
FEBRUARY 2025
11 – Defense Collaborative, Orlando, Florida
3-5 – National Retail and Restaurant Defense Association, Fort Worth, Texas
MAY
4-7 – RIMS RISKWORLD, Chicago, Illinois
JUNE
1-4 – National PRIMA, Seattle, Washington




Nathan C. Levy
If you handle workers’ compensation claims for an employer or an insurer, then you are already aware of the dayto-day challenges that come with the job. It has been my experience that the role of the employer in the reporting of an injury and the post-accident investigation is vital in the assessment of any early claim.
First, be certain you obtain written statements of the facts of the accident from the injured worker. A postaccident reporting form should always be used for this purpose and at a minimum should include all the important and relevant details of how the event occurred, who witnessed it and the injuries resulting from the accident. In addition, you also want the names of all witnesses that could have seen the event first-hand or who played a role in interacting with the injured worker soon after the event.
All too often, employers do not take the time to have this document created and simply relay information later to either the Insurer or the defense attorney assigned. We all know memories fade as time passes, so immediate documentation of these details is paramount.
Also, we cannot stress enough the importance of having this document completed by the injured worker personally. Provide ample space for a detailed description of the events and injuries in their own handwriting. Provide any assistance needed to the employee as they complete the form and then review it if clarification on any point is needed, including any confusion in spelling or other vague details. Once this form is completed, a similar form should be utilized for the purpose of obtaining statements from all key witnesses referenced by the injured worker and even those within the vicinity of the accident.
After statements have been obtained, your job is far from finished. The most prepared employers begin the next phase of the investigation which includes photographs of the area where the injury took place, as well as videos that might preserve key evidence. We all possess cameras on our phones that do an amazing job with this task, so preserve the scene as it exists following the accident If the mechanism of injury is a slip or a trip and fall involving water or an uneven surface, capture photographs of the location where the injury purportedly occurred, especially if there is apparent inconsistency.
From the employer’s perspective, your job is still not finished after your initial investigation. As the claim continues, remain in contact with your claim’s specialist and the assigned defense counsel about any additional information you acquire. Although hearsay has no place in court, any rumors or gossip obtained may lead to important details that can impact a case. Finally, social media has a major impact on most workers’ compensation claims, as well, so it’s a good thing to keep an eye on things going on there.
An employer’s job is never done. With diligence, claims can be ended with direct involvement at the employer level. Of course, the best workers’ compensation claim is the one that never occurs, so efforts made at establishing a safety culture focused on the health and welfare of all employees are always time well spent.

Nathan Levy, partner with Levy, Sibley, Foreman & Speir, LLC, has practiced in workers’ compensation defense since 1998. He earned his Bachelor of Arts degree from Auburn University in 1994 and his Juris Doctorate degree from the Cumberland School of Law of Samford University in 1997.

Elliot P. Robinson, MD
An amputation is a devastating outcome following a severe limb injury both on and off the job site. Improvements in patient function and pain have made Targeted Muscle Re-innervation (TMR) the most promising technology in amputation medicine since the advent of the myoelectric prosthesis (MP). TMR is essentially the concept of nerve transfers to maximize the number of independently controlled muscles available to control MPs.
A myoelectric prosthesis (MP) uses electromyography (EMG) sensors to activate electric motor-powered motion. This offers significant advantages over body-powered devices, including more intuitive and precise control, power, comfort, and less fatigue. Because MPs are controlled by EMG signals, the number of motion patterns they can perform is a function of the number of muscles that can be activated by the patient and sensed by the device.
TMR involves surgically transferring nerves severed in the amputation process to available, superficial, and redundant muscles. By working with a therapist and a prosthetist, patients can learn to activate these reinnervated muscles and control their MP device, often with greater degrees of control than without TMR.
An exciting secondary outcome of TMR has quickly become a primary benefit: pain relief. It is well-recognized that amputees are often troubled by neuropathic pain including phantom sensations and neuroma. Neuroma pain is one of the most significant limitations of prosthesis wear. In TMR, severed nerves are coapted to a muscle unit, so the axons are provided “something to do” and do not create painful neuroma. TMR surgery is now routinely performed as primary or secondary neuroma management in both upper and lower extremity amputations.
Collaboration between surgeons and prosthetists greatly improves outcomes. On one hand, “cross-pollination” of ideas continues to lead to advances. An example of MP device technology and the surgical technique evolving together is the “Starfish” procedure. This allows independent activation of fingers in transmetacarpal hand amputations by repositioning the deep interosseous muscles of the hand more superficially where they can be picked up by the EMG sensors.
Another way collaboration improves outcomes is through coordination of care. Many patients with amputations have complex clinical challenges coupled with difficult social and return-to-work adjustments. There has been a trend in establishing dedicated amputee care clinics bringing surgeons, therapists, and prosthetists together face-to-face to lower logistical hurdles for the patient and allow for good communication between care team.
Hopefully, this technology and continued advancement will give amputee patients the best chance at maximizing their return to an independent life.

Elliot P. Robinson, MD, specializes in the full spectrum of disorders and surgical treatments relating to the hand, wrist, and elbow and provides care for workers’ compensation injuries. Fluent in French and proficient in Spanish, Dr. Robinson also directs a monthly Amputee Care Clinic at OrthoGeorgia.

David Langham, Deputy
There is growing recognition of addiction challenges. Everyone is familiar with substance use. But, our brains produce innumerable chemical reactions. We are slowly grasping that addiction may be about substances or behavior, drugs, alcohol, gambling, video games, and more. We are slowly grasping this.
One villain is at our fingertips. In Dopamine Nation, Dr. Anna Lembke says we have all begun to “turn to (our smartphones) for quick hits, seeking attention, validation, and distraction.”
This is too readily part of today’s workplace. It is rare to see a coworker without an earbud. That is not a typo. The single bud is becoming ubiquitous as workers strive to multitask with a persistent stream of simultaneous distractions. Maybe this is innocuous background music, or increasingly platforms like YouTube and TikTok, a droning undercurrent in our workflow. Some cannot fathom the constant distraction and others revel in it.
Going for coffee, the restroom, or lunch, (or sitting in a meeting) we are drawn to the smartphone and need to re-join the world. We must escape the “distraction” of work. With its detriment and threat, it draws us back. Social media persistently infuses consciousness with the beautiful, rich, successful, and lucky. There is an element in social media of validation, but also a recurrent reinforcement that you are not keeping up with the Joneses. And each “quick hit” may remind us of our success or not.
The Centers for Disease Control and Prevention states, “Mental health disorders are among the most burdensome health concerns in the United States.” It notes how mental health issues impact the workplace in various forms, including simple stress and more. The mental health issues are, themselves, important, but more so as comorbidities with a raft of physical complaints and diagnoses. There are performance and attendance concerns attributed to mental health, as well.
The inputs from social media are double-edged blades. You may love this article and send me accolades to feed my Dopamine desire. Or, you might remain quiet, causing me self-doubt and anxiety. Further, you could insult my thoughts or me personally. The fact is, those outcomes are just as possible for every story, post, or picture. (“Can you believe he wore/said/ate that?!?!”)
The effects are patent. People are withdrawing. Some are “turning to artificial intelligence” for companionship (as in dating an AI). People complain of suffering symptoms and dread because of critics who comment about them on social media, but they do not log off. We see a constant cycle of seeking social media distraction, entertainment, and/or engagement and the all-too-frequent triumph of the malcontents hiding behind their keyboards, pseudonyms with criticisms or vitriol.
The news recently described an Olympian who has learned to block, disregard, and ignore negativity. Her focus and discipline are admirable. However, is it realistic for the rest of us?
Those who believe this is not impacting the workplace are at least naïve. Every business likely has workers with mental health challenges. Recognizing, addressing, and maintaining productivity and success will require insight, support, and imagination.
In the broadest context, what is management doing to recognize the threat? How can management increase engagement, interaction, and civility? How can workers regain stability, mental health, and freedom from the nagging smartphone? Well, I have to get back to my story/feed/etc.

David Langham has been Florida’s Deputy Chief Judge of Compensation Claims since 2006. He has delivered more than 1,900 professional lectures, published over 40 articles, and 1,800-plus blog posts regarding the law, technology, and professionalism. He authored Florida Workers’ Compensation: Its History, Evolution, and Function (2023) and The Mock Trial Performance (2023). He lives in Pensacola, Florida with his wife Pamela Langham, Esq.




Alejandra N Klopstock, LPC, CFMHE, CRC
Injured workers who suffer from chronic pain oftentimes report depression and/or anxiety complaints related to their injury. Cognitive behavioral therapy (CBT) is an effective treatment for depression and anxiety that may also have a positive impact on an individual’s pain perception. CBT strategies can help individuals adapt to living with chronic pain and may motivate them to return to work.
Pain, depression, and anxiety are related. Depression may cause physical pain and physical pain may cause depression. An individual may also experience persistent anxiety along with chronic pain due to the fear associated with the anticipation of pain. Most patients avoid some activities to avoid pain. When depressed, they may also feel emotional fatigue, which also reduces physical activity. Pain perception is exacerbated by anxious or/and depressed mood and is alleviated by feeling happier and/or relaxed.
Pain is a subjective experience that is influenced by psychological, biological, cultural, and environmental/social factors. It is crucial to explore and identify barriers and advantages that may impact psychotherapy treatment outcomes. For example, someone may believe that their work accident was the result of divine punishment and that they deserve to suffer. Or an individual’s emotional complaints or pain might result in significant positive attention from loved ones. Negative cultural core beliefs in the former example, and secondary gain from environmental factors in the latter, can interfere with an individual’s motivation to recover and must be addressed in therapy. Social support, on the other hand, has been shown to play a crucial role in recovering from depression and anxiety and can make a significant difference in how patients manage their chronic pain.
Suffering from physical and emotional pain resulting from a work injury can negatively impact an individual’s sense of self. Patients may report not being themselves and no longer knowing who they are. They may feel “stuck” in a cycle of actual or perceived disability that is oftentimes based on fear of re-injury. Doctors and patients need to have excellent communication to avoid misunderstandings about pain.
CBT assumes that thoughts, feelings, and sensations are related. In therapy injured workers receive psychoeducation about the shared biological mechanisms of pain, anxiety, and depression and they are encouraged to break free from the vicious cycle of emotional and physical pain. The patient-counselor relationship must be based on trust. When a patient trusts his/her provider they may feel supported and motivated to take control of their lives. CBT seeks to empower individuals by providing them with emotional support and by teaching them coping strategies that promote acceptance, adjustment, and adaptation to living with the consequences of an injury, including chronic pain. Cognitive restructuring skills and relaxation strategies provide patients with a locus of control to stabilize their mood. Patients with sleep disorders may learn hygiene strategies to improve their quality of sleep.
It is important to be aware of a patient’s physical limitations as outlined by their physician. In therapy, homework assignments encourage patients to engage in activities within their physical capacity, promoting adaptation and bringing about positive emotions.
In conclusion, cognitive behavioral psychotherapy can be a powerful treatment for injured workers suffering from depression, anxiety, and chronic pain and may assist them in successfully returning to work.


Alejandra Narino Klopstock is a bilingual psychotherapist in private practice in Atlanta, Georgia. She is a Licensed Professional Counselor, a Certified Forensic Mental Health Evaluator, and Certified Rehabilitation Counselor. She earned her undergraduate degree in Psychology and her Master of Science degree in Rehabilitation Counseling from Georgia State University.
Charles Land, MD
Back pain is a leading cause of missed work. A sharp pain in the lower back, which can sometimes travel through the buttocks, thighs, and groin, can indicate many things. One possible cause is sacroiliac (SI) joint dysfunction. Studies suggest that fifteen to thirty percent (15-30%) of lower back pain cases are due to a problem or dysfunction in the sacroiliac joint.
These problems can be due to too much movement such as constant repetitive motion or a continuous vibration. In other cases, it can be the opposite - not moving enough in that one becomes too sedentary for long periods of time. Both of these situations can lead to instability.
Located in the pelvis, the sacroiliac links the iliac bones (pelvis) to the sacrum (lowest part of the spine above the tailbone.) Unresolved chronic lower back pain without a solution could be coming from this area and show as some of the following symptoms:
•Lower back pain
•Pain, numbness, tingling, weakness in legs
•Feeling of leg instability (buckling/giving way)
•Disturbed sleep patterns due to pain
•Inability to sit for long periods, sitting on one side
•Pain going from sitting to standing
•Pelvis/buttock pain
•Hip/groin pain
A possible solution can involve a minimally invasive iFuse procedure to stabilize and fuse the SI joint. This involves inserting three triangular-shaped titanium implants across the sacroiliac joint to maximize SI joint stability, reduce pain, and improve function. The procedure is done through a small, one-inch incision and only takes about an hour. This can make for a quick recovery time and is very effective in reducing or eliminating lower back pain due to SI joint problems.
At Pinnacle Orthopaedics, we provide quality care, convenience, and assurance that patients receive the most advanced and comprehensive orthopedic care professionally and courteously. With five offices throughout the northwest Atlanta area, the practice has sixteen (16) physicians with a wide range of orthopedic specialties, including arthroscopic surgery, total joint replacement, surgery of the hand, surgery of the foot, fracture care, pain management, spine surgery, traumatic injuries, limb lengthening, and deformity repair, and treatment of work-related injuries.

Charles Land, MD, is board certified by the American Board of Orthopaedic Surgeons, specializing in surgical and non-surgical care of the cervical, thoracic, and lumbar spine including degenerative spinal conditions, lumbar and cervical stenosis, disc herniations, minimally invasive spine surgery, spinal trauma, kyphoplasty, and sacroiliac joint disease. He treats patients in Pinnacle’s Canton, Marietta, and Woodstock offices.

Eric F. Patten RN, BSN
Triage plays a vital role in managing workers’ compensation injuries, ensuring timely and appropriately directed medical care for injured workers. It is also fundamental in significantly reducing medical costs and claim processing times.
Here’s a look at the benefits of triage in claims management:
Understanding Triage:
Triage involves the prompt clinical assessment of an injured individual and the appropriate direction of care. This quick and accurate assessment helps the claims team allocate resources efficiently and effectively.
Triage ensures injured individuals receive timely and appropriate levels of treatment through clinical assessments. This guarantees that an injured worker receives the most suitable and effective care for their condition, improving the quality of care, and reducing unnecessary treatments and cost.
Enhanced Communication and Transparency:
Triage establishes clear lines of communication between all parties involved in the injured individual’s care. The transparency fostered by triage builds trust and ensures that all stakeholders are informed. Clear and timely communication prevents misunderstandings and disputes, which can otherwise delay the claim process.
Reduced Claim Processing Time:
Triage helps reduce overall claim processing time by providing prompt medical reports and clear documentation of the injury and its treatment. This streamlines communication between medical providers, insurers, and employers, leading to faster claim approvals, reduced lost time, and quicker returns to work or settlements if needed based on the injury.
Prompt medical attention through triage can prevent minor injuries from becoming major ones, thereby reducing overall medical expenses. Triage ensures appropriate treatments are provided at the right time, avoiding unnecessary procedures that can increase costs.
Early medical intervention facilitates quicker recovery times and earlier returns to work. When injuries are addressed promptly, the chance of complications decreases, enabling individuals to resume their normal activities sooner.
Prevention of Fraudulent Claims:
Early and proactive management of injuries through triage reduces the potential for fraudulent claims. Timely documentation and verification of injuries and treatments make it difficult for false claims to be lodged, protecting insurers’ financial interests and ensuring genuine claimants receive their due benefits without unnecessary delays.
In summary, triage is an essential component of an effective claims management strategy. Ensuring timely and appropriate medical care and providing proper direction of care as the first step in a cohesive claims management strategy helps reduce medical costs, speed up recovery times, and optimize resource use, all while streamlining the claim process. Emphasizing an efficient triage process and direction of care as that first step in the overall strategy is crucial for delivering better outcomes for both the injured worker and the insured.

Eric F. Patten, RN, BSN, is the President of Operations at the Kingstree Group with thirty-one years of nursing experience, specializing in workers’ compensation for twenty-five years. He leverages clinical expertise to drive innovation and efficiency, executing solutions that enhance company values, growth, and team excellence.
Ben Vinson, Chairman and Chief Appellate Judge
Greetings from the State Board of Workers’ Compensation. Hope everyone is having a healthy and successful year so far. We are staying busy at the Board across all of our divisions covering issues with claims, investigations, rehabilitation, insurance, mediations, settlements, hearings, and appeals. This spring our regional seminars drew big crowds at each of four cities and featured a very engaging program to the delight of those in attendance. We are expecting the same for our Annual Educational Conference in August at the Hotel at Avalon in Alpharetta, where we will have an exciting agenda with a Las Vegas theme and our 2nd annual Adjuster Training Program. When most people think of Las Vegas, they think of late nights, gambling, and entertainment…
This kind of reminds me of the Georgia General Assembly. The 2024 Legislative Session finished up after three months on March 28th when the legislature adjourned Sine Die. Governor Brian Kemp addressed the House and the Senate on the final night to thank the legislators for their hard work on the state budget and other important items. The Fiscal Year 2025 budget includes substantial investments in infrastructure, education, law enforcement, mental health, and pay raises for state employees.
Importantly for our industry, the Amended Fiscal Year 2024 budget includes $125 million to fund workers’ compensation settlements for state claims through the Department of Administrative Services. Similar to an investment in the budget from two years ago, this appropriation is a proactive step that should reduce outstanding state claims and connected costs.

This year we also witnessed the final passage of House Bill 451 to assist first responders with post-traumatic stress disorder injuries (“PTSD”). HB 451 began as a workers’ compensation presumption concept but then was amended into an insurance-based approach akin to the cancer benefit for firefighters that was enacted several years ago. HB 451 garnered broad support from first responders, cities, counties, and other groups, including our Advisory Council with full consideration of it as a viable alternative to the workers’ compensation presumption proposal. HB 451 was passed by the House and Senate Insurance Committees, then passed both chambers without a dissenting vote, and was signed into law by Governor Kemp on May 1st. I appreciate the level of communication and collaboration by so many parties on this issue and look forward to the implementation of a program that should assist our vital first responders in a meaningful way.
This session we also tracked Senate Bill 371 by Senator Brian Strickland to help peace officers injured in the line of duty while engaged with a criminal. SB 371 started as an effort to provide increased workers’ compensation benefits for such peace officers and ended up as a way to focus attention on the existing state indemnification fund for those peace officers injured in the line of duty. SB 371 passed the Senate but did not make it out of the House before Sine Die so we will watch for any developments on this issue over the next year and into the 2025 Session.
I wish everyone a great finish to 2024 and I look forward to seeing many of you at our annual conference or other events this fall. Feel free to contact me anytime with questions or comments about the Board and please visit our website at https://sbwc.georgia.gov for information and updates.

Ben Vinson is the Chairman and Chief Appellate Judge of the State Board of Workers’ Compensation, appointed by Governor Brian Kemp in May 2021. He hears workers’ compensation cases on appeal and handles policy issues for the state agency. He graduated from Furman University and the University of Georgia School of Law. He resides in Greensboro, Georgia with his wife and two children.


Lyndsey Palmer, WCI Exhibitor/Sponsor
My name is Lyndsey Palmer, the Exhibitor/Sponsor Administrator for the Workers’ Compensation Institute (WCI®). I joined WCI in November 2022, and my first conference last year left me in awe as I witnessed the event come to life. Despite my relatively short time with this amazing organization, I have gained extensive knowledge about the Workers’ Comp field and have met countless incredible people along the way.
At WCI, our commitment is to make the annual conference the best experience possible. This year, we have introduced numerous new changes, and we are eager for everyone to participate. Our primary goal is to ensure that attendees receive top-notch education, ample networking opportunities, and a memorable experience overall. With a wide array of session topics, a unique Exhibit Hall, diverse sponsorship options, and convenient meeting spaces throughout the hotel, it’s no wonder our conference has gained national recognition.
Join us at one of our major events, such as the Monday Night Reception featuring live performances by renowned entertainers—this year’s headliner is the rock band Daughtry. Additionally, our Give Kids the World Gala supports children in need, with a dedicated day for volunteering and providing fun for families at the Give Kids the World Village at https://www.wci360.com/.
Our Exhibit Hall is a lively and exciting atmosphere where we host themed contests, dress up, and offer numerous prize giveaways. Be sure to stop by and join in the fun if you’re at the conference! As we continue to grow, we appreciate everyone spreading the word and supporting WCI. Our success is due to the unwavering support of our attendees, vendors, and sponsors. Thank you for making WCI what it is today. I look forward to seeing everyone at this year’s conference.

• August 17 – 20, 2025 at The Orlando World Center Marriott
• Sunday, August 17, 2025: 12:00 pm to 5:00 pm – Exhibitor Move-In
• Monday, August 18, 2025: 10:00 am to 5:00 pm
• Tuesday, August 19, 2025: 9:00 am to 3:30 pm
• Tuesday, August 19, 2025: 3:30 pm to 5:30 pm – Exhibitor Move-Out

For more info contact: Lyndsey Palmer
850-425-8186 lyndsey@wci360.com www.wci360.com
The Workers’ Compensation Institute (WCI®) is a nonprofit educational organization that serves as a comprehensive resource to all workers’ compensation stakeholders. WCI sponsors the annual Workers’ Compensation Educational Conference and brings together workers’ compensation professionals from across the country. It is the nation’s largest work comp conference and the programming, networking, exhibit hall, and entertainment cannot be matched.
Phillip B. Russell
On July 2, 2024, the U.S. Occupational Safety and Health Administration (OSHA) unveiled a notice of proposed rulemaking, titled, “Heat Injury and Illness Prevention in Outdoor and Indoor Work Settings.” The proposed rule seeks to set the first nationwide standard addressing the hazards of excessive heat in indoor and outdoor work settings.
In April 2022, OSHA launched a three-year national emphasis program (NEP) on indoor and outdoor heatrelated hazards. Employers have already been subject to possible inspections and citations under the General Duty Clause, Section 5(a)(1) of the Occupational Safety and Health Act, and the NEP has provided some foundation. However, OSHA has wanted to implement a specific standard for years, especially under the BidenHarris Administration and the leadership of Assistant Secretary Doug Parker (formerly the head of Cal/OSHA).
It is entirely possible with legal challenges and political changes that the proposed rule never goes into effect. Perhaps there is much to be learned from the proposal that would help employers keep workers safe and avoid or minimize any OSHA citations.
The proposed standard would apply to practically all employers and be triggered when employees are exposed to heat indexes of 80˚F—defined as the “initial heat trigger”—for over fifteen minutes in any sixty-minute period. Employers with outdoor work sites would have to monitor the temperature with “sufficient frequency to determine with reasonable accuracy employees’ exposure to heat.” For indoor work sites, employers would identify areas where the heat index could be 80˚F or more and include a temperature “monitoring plan” in their written heat injury and illness prevention plan (HIIPP).
The proposal includes additional provisions—more breaks, an observation/buddy system to monitor workers for signs of heat illness, and training—that would apply at the “high heat trigger” of a heat index of 90˚F. Employers would have to monitor temperatures to determine when the high heat trigger is met. Given temperature fluctuations that occur even during a single work shift, employers would have to monitor temperatures carefully to determine when the HIIPP must be implemented. Rather than monitoring, an employer may assume that the temperatures will reach the initial and high heat triggers.
The HIIPP: What must be included?
The proposed rule sets forth a written HIIPP requirement for all employers with over ten employees. The plan would include:
•a “comprehensive list of the types of work activities covered by the [HIIPP]”
•a description of how the employer complies with the OSHA standard
•the means the employer will use to monitor temperatures (e.g., heat index or web bulb globe temperature)
•emergency phone numbers and procedures employees must follow when an employee experiences signs and symptoms of a heat-related illness
•a list of the “heat safety coordinators” with “authority to ensure compliance with all aspects of the HIIPP”
•Employers would be required to “review and evaluate the effectiveness” of the HIIPP whenever a recordable heat illness occurs and update the HIIPP “as necessary.” This means a review would have to be performed any time an employee receives medical treatment, such as an IV, or misses a day of work due to overexposure to heat. For large employers with many outdoor workers, these reviews could be frequent.
What steps would be required to protect employees?
The proposal includes an extensive list of heat injury prevention measures that employers would implement, including:
•readily accessible “cool” drinking water in an amount greater than one quart per hour per employee
•break areas for outdoor work sites that are artificially or naturally shaded (shade from equipment is not sufficient) or enclosed spaces with air conditioning

•break areas for indoor work sites that are air-conditioned or have “increased air movement” from fans or natural ventilation; dehumidification would be required “if appropriate”
•“allow[ing] and encourag[ing] employees to take paid rest breaks” as “needed to prevent overheating”
•two-way communication with employees
If the high heat trigger of a heat index of 90˚F was met, the following additional protective measures would have to be implemented:
•paid fifteen-minute rest breaks every two hours
•a “hazard alert” issued by the employer to notify employees of the importance of staying hydrated and taking the mandatory rest breaks (and additional breaks as needed) and the procedures to follow in an emergency
•one of these methods of monitoring employees for signs and symptoms of heat illness is a buddy system where coworkers observe each other or observation by a supervisor or heat safety coordinator
One issue OSHA will likely need to resolve: the proposal contains no definition of what constitutes a break. Specifically, does time spent driving from one work site to another count as a break? What about sedentary time spent in the heat performing a job briefing or similar activities?
The proposed rule would also require employers to develop and implement acclimatization procedures for new and returning employees that include: lower workloads in the early days of the job. Employers would also have to develop and implement emergency response procedures for what to do if an employee shows signs and symptoms of heat-related illness. Finally, employers would also have training requirements for all employees, including supervisors.
Stakeholders will have 120 days to file comments on the proposal. The 120-day comment period (which OSHA may ultimately extend) will run when OSHA publishes the proposal in the Federal Register (which has not happened as of August 1, 2024). Once comments are filed, OSHA will review them and publish a final standard.
The fate of the final standard may be tied to the results of the upcoming presidential election. If OSHA finalizes the standard during the Biden-Harris Administration and Vice President Harris loses the election, the standard will be vulnerable to a congressional challenge under the Congressional Review Act. If a final standard is not issued and former President Trump wins the election, he could withdraw the proposal.
No federal OSHA standard addressing heat injury and illness prevention has been finalized. OSHA already uses the General Duty Clause to issue citations alleging employers are not trying to protect employees from heat hazards. Many employers already have heat illness prevention plans that include many elements proposed by OSHA, and state OSHA plans in California, Minnesota, Oregon, and Washington have existing standards that include some of the same provisions federal OSHA proposes. To the extent employers have existing heat illness prevention plans, no changes are required by OSHA’s proposal.
Employers may want to consider evaluating existing plans to determine whether the elements OSHA proposes are included. If an employer can show that its existing plan contains the elements OSHA proposes, OSHA likely cannot sustain a violation of the General Duty Clause. Also, comments from the industry regarding the feasibility and practical difficulties of implementing programs containing the elements OSHA proposes are critical to shaping the final standard.

Phillip B. Russell is a board-certified OSHA and employment lawyer, litigator, and advisor. He is a strategic, practical, and trusted partner to clients on labor and employment law matters with Ogletree Deakins.
Robyn Lewis, PT, CEAS
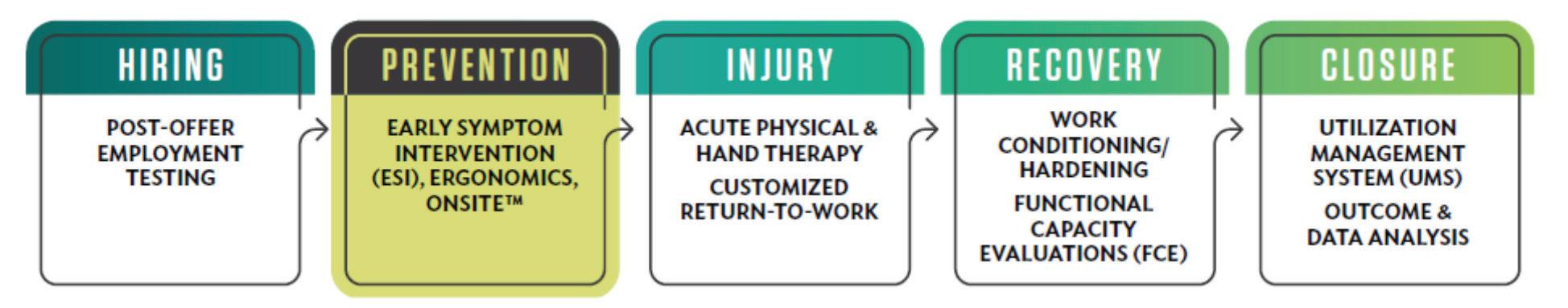
In the ever-evolving world of work, the health and safety of your employees are crucial to your company’s success. Investing in an effective injury prevention program isn’t just about regulatory compliance; it’s about creating a culture of health, safety, and productivity. Industry leaders have implemented injury prevention programs designed to reduce injuries, claims, and costs for employers, ultimately leading to increased performance, productivity, profits, and an enhanced quality of life for employees.
According to the U.S. Bureau of Labor Statistics, there were approximately 2.8 million nonfatal workplace injuries/ illnesses reported in 2019, with 32% represented by musculoskeletal disorders. These incidents lead to significant costs, both in terms of workers’ compensation and lost productivity, with an average cost of $67,248. Due to an aging workforce, costs are expected to escalate over the next decade. In order to combat this, employers need an approach that starts before injuries occur which address these challenges head-on, providing your organization with the tools and strategies needed to maintain a healthy and productive workforce. Industry leaders using these proactive solutions have observed reductions of work-related musculoskeletal injuries on an average of 40%.
Comprehensive, proactive onsite services should be tailored to meet the specific needs and goals of your organization. Analyzing data including injury rates, injury severity, claim costs, mechanism of injury, job classes with highest injury rates, as well as when the injury is most frequently occurring (i.e. within 6 months of hire or after 20 years of work) helps to identify which service would be most effective. Below are some injury prevention best practice service options:
Preventing injuries before they happen is critical. Early symptom intervention services include:
•Pre-injury assessment and triage of worker discomfort complaints: Early detection of potential issues can prevent serious injuries.
•First aid care of minor injuries: Immediate care to prevent escalation.
•Service provided by healthcare professionals with expertise in musculoskeletal injuries: Expert care ensures effective management and prevention strategies.
•Valuable strategy in managing OSHA 300 recordables: Reducing recordables significantly lowers costs and liabilities.
Creating a safer and more efficient workplace is key. Ergonomic services include:
•Work risk analysis: Identify, quantify, and document risks associated with selected jobs.
•Work task analysis (physical demand analysis): Identify and list essential functions and associated physical demands.
•Workstation analysis (office work area assessment): Identify improper workstation setups or designs and implement corrective changes.
Empowering employees with knowledge is crucial. Education services include:
•Risk-specific education: Tailored around the risks associated with the job tasks and recordable history.
•Tools for proactive risk management: Equip employees and management to recognize and minimize risks while maximizing performance.
•Techniques to minimize job stresses: Demonstrate methods to reduce accumulated stresses from job performance.
•Customized stretches: Taught to counteract job tasks and prevent injury.
•New hire training/conditioning: Teach and reinforce best practices and body mechanics, and provide progressive exercises to prepare for the job’s physical demands.
Proactive coaching can prevent many workplace injuries:
•Provided by healthcare professionals: Experts who understand the physical demands of your work environment.
•Hands-on approach: Work alongside employees as they perform their daily tasks, offering real-time advice and corrections.
Supporting employees’ return to work is vital for their recovery and your productivity:
•Job coaching: Help reintegrate returning workers by focusing on risk factor recognition and re-injury prevention strategies.
•Work conditioning: An intensive, goal-oriented program designed to restore physical capacity and function in individuals who have been out of work for long periods.
•Return-to-work programs: Minimize re-injury through ergonomic risk reduction and goal-oriented conditioning programs.
Empower your team to sustain a culture of safety:
•Company-specific program design: Comprehensive assessment of risk factors and tailored educational goals.
•Instructing your implementation team: Certification classes for trainers and annual review sessions to ensure ongoing effectiveness.
Implementing customized, interactive injury prevention programs will yield numerous benefits:
•Reduced injuries and claims: Directly lowers costs and improves workforce health.
•Increased performance and productivity: Healthy employees are more effective and engaged.
•Higher profits: Reduced costs from fewer injuries and claims translate into better financial performance.
•Enhanced employee quality of life: A safer, healthier workplace fosters loyalty and job satisfaction.
Investing in injury prevention programs is an investment in your company’s future. By prioritizing the health and safety of your employees, you are laying the foundation for long-term success and sustainability. Work with musculoskeletal and ergonomic experts to create a thriving work environment where everyone can perform at their best.

Robyn Lewis, PT, CEAS is Regional Director of WorkStrategies with Select Medical (Physio/ Emory Rehab). She has thirty years of experience in industrial medicine specializing in return to work and injury prevention programs and is certified in Ergonomics, Functional Capacity Evaluations, and Employment Testing.


Linda Yates
Some would say success is being rich. Others would term success as fame. Perhaps it is having relationships that inspire and lift your spirit. When considering this topic, search yourself by taking time to ponder how you define success.
Defining what is important to you and what you value will help you create goals in your life and work. For instance, health is one of my strongest values. When I jeopardize my health by not getting the proper nutrition, exercise, and sleep, all other areas of my life are impacted. I am knocked out of balance and begin to fall short of reaching my goals. When planning individual goals, reflect on how reaching a particular goal will impact the other areas of your life.
The ingredients of success that have a lasting impact are discipline, sacrifice, commitment, and heart.
Discipline is defined as an activity, exercise, or regimen that develops or improves a skill. Discipline is sticking to your project plan even when you feel like doing something else. Discipline is fundamental in all aspects of lifeincluding being disciplined in what is fun. When I was younger, I looked at discipline as harsh and unbending. What I now know is that it is a gift. The more discipline I show in all parts of my life, the happier I am and the more I can achieve; thus, discipline is my friend.
One of the great examples of discipline has been my youngest son. He is extremely disciplined in every aspect of his life. Discipline is the foundation for all success. Without discipline, you cannot achieve your goals as it is the keystone to achieving all else.
Sacrifice is something that if you continually strive to incorporate in your life, will help you experience pure joy. Sacrificing ego is often the way to solve challenges that arise. However, knowing what your core values are helps you determine when sacrifice is imperative. Defining those values is the driving force for all aspects of life. Your core values influence the thousands of different decisions you make every day.
Next on the list is commitment. There is a picture of a runner before sunrise running through the forest getting her workout that inspires me. This runner has only one foot. When I feel like giving up on achieving my goals I think about this picture and reflect on what it is I am striving to achieve. Honoring commitments brings peace. When other distractions come up, remembering the commitments that you have made will help you stay focused.
Lastly, when you put your heart and soul into your work and life, you will see success. It may not look like you originally thought it should and it may arrive when you least expect it.
Success becomes a private definition for each one of us. Everyone, and I mean everyone, is successful in ways unique to them. The secret is in discovering what it is for you and what makes you feel successful.

Linda Yates, “The Image Energizer,” is a highly sought international Keynote Speaker, Leadership Consultant, Executive Coach, Corporate Trainer, Author, Stylist, and Voice-Over Talent. She has produced over 300 educational seminars on helping individuals and businesses accomplish their goals.
Mark Snoddy, MD
Work-related hand injuries are prevalent in various industries, ranging from construction and manufacturing to healthcare and office settings. These injuries can vary in severity from small cuts and sprains to fractures and nerve damage. With each of these injuries, early identification and rehabilitation are essential for restoring functionality and preventing long-term complications. Hand therapy is crucial in this recovery process, providing targeted treatment and exercises to help individuals regain strength, flexibility, and dexterity in their hands.
Hand therapy is a specialized field focusing on treating conditions affecting the hands and upper extremities. Certified hand therapists are trained to address various injuries, including fractures, tendon and ligament injuries, nerve damage, and strains. They employ various techniques and modalities to promote healing and enhance function. The primary goal of hand therapy is to enable patients to resume their normal activities, whether at work or in daily life, as quickly and safely as possible.
Therapeutic exercises are a key component of hand therapy, designed to improve strength, range of motion, and coordination in an injured hand. After a fracture, for instance, a patient might start with gentle stretching exercises to prevent stiffness and maintain flexibility, eventually progressing to strengthening exercises to rebuild muscle power. Manual therapy such as massage, joint manipulation, and myofascial release, are utilized and aimed at reducing pain and improving mobility.
Manual therapy is particularly beneficial for conditions like tendonitis, where soft tissue restrictions can impede recovery. Additionally, various modalities such as heat and cold therapy, ultrasound, electrical stimulation, and splinting are used to aid healing. For example, heat therapy can relax muscles and increase blood flow to the injured area, while cold therapy can reduce inflammation and numb pain. Ultrasound and electrical stimulation enhance tissue healing, and splinting provides support and immobilization to protect injured structures and facilitate proper healing.
A hand therapist’s role also involves education and ergonomic training for the injured worker. Individuals learn how to perform tasks safely and efficiently to avoid re-injury, including proper body mechanics, posture, and techniques for lifting and carrying objects. Ergonomic training involves modifying the work environment to reduce strain on the hands and upper extremities, such as adjusting workstation heights, using ergonomic tools, and implementing regular breaks to prevent overuse injuries. By equipping patients with the knowledge and tools to protect their bodies, hand therapists play a crucial role in preventing future injuries.
In conclusion, hand therapy is a critical component of rehabilitation for work-related hand injuries. Through therapeutic exercises, manual therapy, modalities, and education, hand therapists help patients regain function and return to their daily activities.


Mark Snoddy, MD is a board-certified hand, shoulder, and elbow surgeon at Augusta-Aiken Orthopedic Specialists. He earned his medical degree from the Medical College of Georgia and completed orthopedic surgery training at Vanderbilt University. He completed a fellowship in hand and upper extremity surgery at Harvard University, training at Brigham and Women’s, Mass General, and Boston Children’s Hospital.

Plantar fasciitis is a common and often debilitating condition affecting the feet, particularly the heel and arch areas, prevalent among individuals who spend long hours standing or engaging in repetitive activities. Developing, diagnosing, and treating plantar fasciitis in the workplace requires a comprehensive approach to mitigate its impact on productivity and employee well-being.
Creating an understanding of plantar fasciitis begins with recognizing its causes and risk factors. It typically results from repetitive strain on the plantar fascia, a band of tissue connecting the heel bone to the toes, causing inflammation and pain. Factors such as prolonged standing or walking on hard surfaces, improper footwear, obesity, and biomechanical issues contribute to its development. Workplace environments that involve these factors, such as retail, healthcare, and manufacturing, increase the likelihood of employees developing plantar fasciitis.
Diagnosing plantar fasciitis involves a combination of clinical evaluation and imaging studies. Healthcare providers, including occupational health specialists, often assess symptoms like heel pain, especially in the morning or after prolonged sitting or standing. Physical examinations may reveal tenderness at the base of the heel and stiffness in the foot. Diagnostic tools such as X-rays or an MRI help confirm the diagnosis by ruling out other potential causes of heel pain, ensuring an accurate assessment for effective treatment planning.
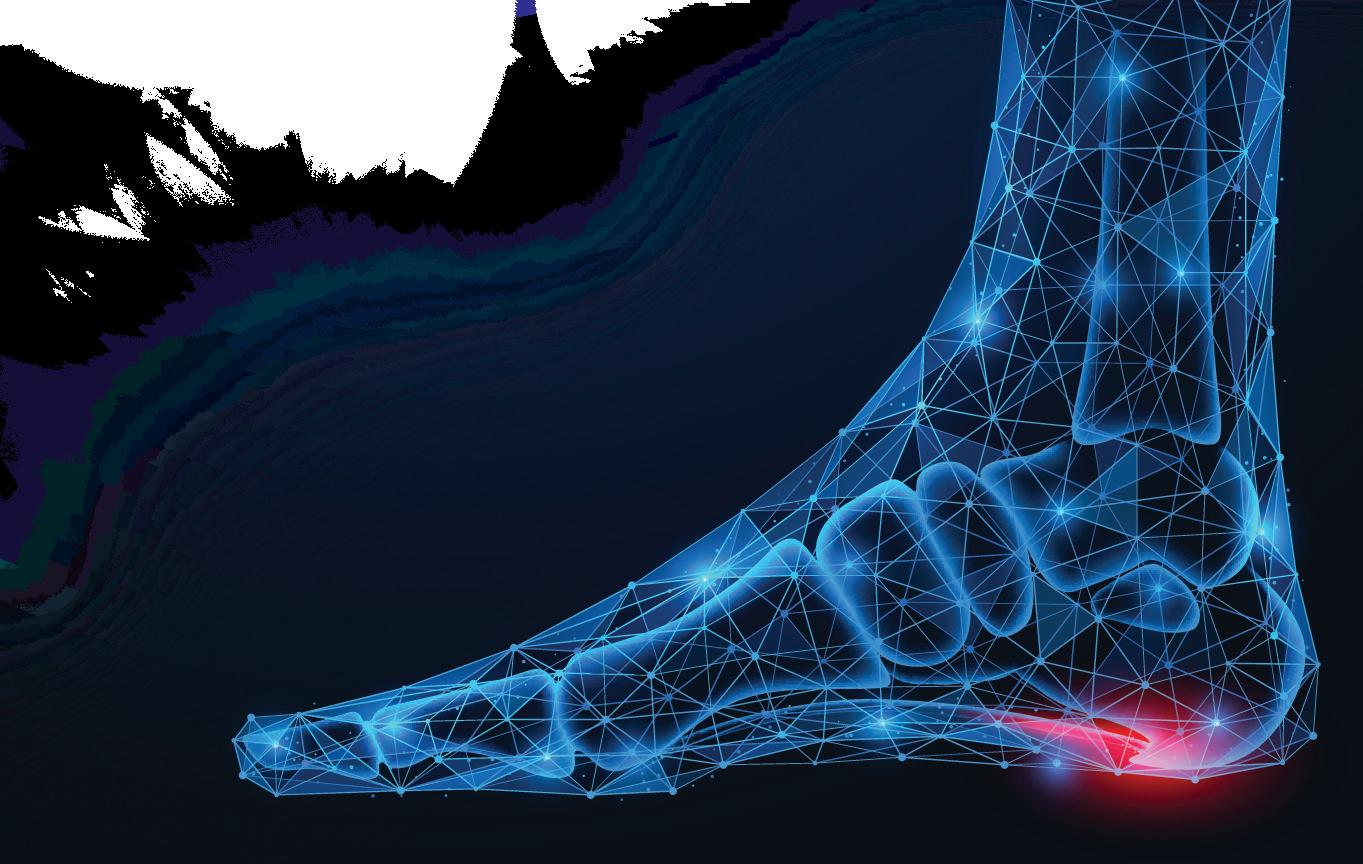
Treating plantar fasciitis in the workplace focuses on reducing pain, promoting healing, and preventing recurrence. Initial treatments typically involve conservative measures such as rest, ice therapy, stretching, and non-steroidal anti-inflammatory drugs (NSAIDs) to alleviate inflammation and discomfort. Occupational health programs may emphasize ergonomic assessments to improve workplace footwear and flooring, reducing strain on the feet during work activities. Custom or non-custom orthotic inserts or supportive footwear can provide additional cushioning and arch support, aiding in long-term management.
Physical therapy plays a crucial role in rehabilitation by incorporating stretching exercises both for the plantar fascia as well as the calf muscles. Workplace wellness initiatives can integrate educational workshops on foot care and injury prevention, empowering employees to adopt healthier habits and recognize early signs of plantar fasciitis.
For severe or persistent cases of plantar fasciitis that do not respond to conservative treatments, advanced interventions such as corticosteroid injections or surgery may be considered for treatment. Surgical options, though rare, may be recommended for cases resistant to other treatments, aiming to release tension on the plantar fascia and alleviate chronic pain.
Preventing the recurrence of plantar fasciitis requires ongoing vigilance and collaboration between employees and employers. Workplace ergonomics should prioritize comfortable and appropriate footwear, anti-fatigue mats, and regular breaks to relieve foot pressure. Regular stretching and strengthening exercises can be incorporated into daily routines to maintain foot flexibility and strength, reducing the risk of injury.
In conclusion, developing, diagnosing, and treating plantar fasciitis in the workplace necessitates a multifaceted approach encompassing education, ergonomic adjustments, conservative therapies, and, when necessary, advanced medical interventions. By prioritizing foot health and preventive measures, workplaces can foster a supportive environment that enhances employee comfort, productivity, and overall quality of life.

Dr. David Kyle, a podiatrist for the Foot and Ankle Team at The Orthopaedic Center in Huntsville, Alabama, is board-certified by the American Board of Foot and Ankle Surgery and by the American Board of Podiatric Medicine. He has extensive experience in podiatric surgical and non-surgical treatment, diabetic limb salvage, and wound care.



Andrew T. Smith
On July 10, 2024, South Carolina’s Supreme Court effectively eliminated an affirmative defense that has been used to defend claims for more than fifty years—fraud in the application of employment.
Imagine this scenario: a prospective employee applies for a job as a material handler. The job description makes clear that the physical requirements of the job include lifting up to fifty pounds. The prospective employee completes a pre-employment questionnaire in which he denies any prior back injuries or permanent physical restrictions. The employer, relying mostly on the answers in the questionnaire, hires the employee to perform the physically demanding job. The employee then injures his lower back during the second day on the job while lifting a fifty-pound pallet. However, unbeknownst to the employer and shortly before he applied for the job, a spine specialist had issued the Claimant permanent physical restrictions of no lifting over ten pounds as the result of a prior workers’ compensation accident involving his back. The employee was aware of his restrictions when he completed the questionnaire. The employee—now a claimant—files a claim seeking benefits for a back injury.
Under the 1973 case Cooper v. McDevitt Street & Company, employers and carriers have been able to assert the defense of fraud in the application of employment in this scenario. In sum, this defense was a bar to compensability where the employee intentionally makes a false representation of his physical condition in a job application, the employer relies in substantial part on his misrepresentation in the hiring of the employee, and there is a causal connection between the false representation and the injury. It is the employer/carrier’s burden to prove these three elements. In recent years, however, South Carolina courts chipped away at the effectiveness of this defense.
The death knell for this defense came in July 2024 with the Supreme Court’s decision in Brailey v. Michelin North America, Inc. There, the Court noted that federal law—namely the ADA—prohibits an employer from asking about prior impairments until after the decision is made to hire the employee. Further, the Court noted that the South Carolina Workers’ Compensation Act does not address fraud in the application. Instead, the defense is a courtmade doctrine—which doctrine the Court said is now out of date. The Court was clear that it does not condone fraud in workers’ compensation claims, but the defense as outlined in Cooper is flawed as a matter of law. The Court ultimately found that the employer/carrier in the Brailey case had not proven the third element of the Cooper test. Still, the Court urged that the best way to address fraud in the application of employment is for the South Carolina legislature to resolve the issue by statute.
So, what does this mean for stakeholders? First, stakeholders must consult with employment counsel when utilizing postoffer medical questionnaires to ensure the questionnaires comply with state and federal law. Second, employers and carriers should consult with workers’ compensation defense counsel as soon as fraud is suspected in a claim. Finally, stakeholders in South Carolina need to contact their representatives in the General Assembly to ensure that the legislature addresses this scenario to provide protection from fraud for businesses and stakeholders of all sizes.


Andrew T. Smith is a workers’ compensation defense attorney in the Charleston, South Carolina office of Willson Jones Carter & Baxley, P.A. Andrew handles a wide variety of workers’ compensation claims. Andrew is also a member of the South Carolina Workers’ Compensation Educational Association. He can be reached at atsmith@wjcblaw.com.

WPH is super excited about our influencers! They are all over the country sharing our magazine at industry events! When you are out and see one of them- snap a picture and post on social media with our hashtag #wphrocks!



Janna Godfrey RN, BSN, CCM
Senior Area Sales Manager at GENEX
Janna has worked multiple states throughout her career and is an industry leader in her field. Currently working for Genex, we are excited to have Janna as a WPH Influencer in Alabama and Mississippi.
Steve Garrett, Retired Director Alabama Workers’ Compensation DOL
Steve is an Industry leader, fresh into his retirement from the Director role for the Alabama Workers Compensation Department with the State. We are happy to have him be one of our distinguished WPH Influencers in Alabama!
Michael Anderson, VP of National Sales- MTI
A National Industry Leader with ties to every state, we are looking forward to having WPH in all the places Michael goes!












The Public Risk Management Association (PRIMA) is North America's largest risk management association dedicated solely to the practice of public entity risk management. For three decades, PRIMA has been dedicated to providing hard-hitting, practical education and training for public entity risk management practitioners like you.
There are more than 2,200 PRIMA member entities, of which 1,800 are local governments. These entities realize that membership provides the necessary tools and solutions needed in today's complex and changing risk management environment.
The Georgia Chapter of the Public Risk Management Association (PRIMA) was established in 2004 to provide education, training and professional development opportunities for public sector risk management professionals in the State of Georgia.
Our mission is to enhance the professional skills of our members through:
•quarterly meetings with topics and speakers directly related to the profession
•our annual Educational Series is generally held in spring, an education-intensive multi-day seminar where members learn, network, and meet with private sector representatives from businesses offering services to the membership.
•Networking opportunities throughout the year, allowing members to effectively share and exchange ideas and solutions with their colleagues.
We work to further the best interests of governments, governmental agencies, intergovernmental risk pools, school districts and other special districts in their risk management activities.


We invite you to join us at an upcoming meeting to discover how Georgia PRIMA can contribute to the success of your risk management programs, and benefit your career through our many professional development opportunities. Workplace Health is excited to be a partner with Georgia PRIMA.

Jim Sorrells
With decades of experience working in P&C insurance, I am acutely aware of the challenges carriers face in optimizing claims workflows. For example, medical data analysis imposes a significant administrative burden on claim professionals, detracting from the time they could invest in evaluating and negotiating claims. This is a common concern I hear from carriers and is a target for improvement. Gathering all relevant information about a case is a critical step. But, while reviewing thousands of pages of documents, it’s all too easy to overlook crucial information. Designing efficient and accurate claims process flows has never been more challenging.
Adding to this, experienced claim professionals are leaving the industry, creating a growing skill and competency gap. Workers’ compensation carriers urgently need to address these gaps. Also, the rise in advertising spend from a highly organized plaintiff’s bar intensifies the pressure on carriers. The impact of this industry losing valuable expertise, and the constant threat of litigation or fines from delayed actions, underscores the need for advanced capabilities to analyze the vast amount of medical data carriers must sift through.

This is where artificial intelligence (AI) comes into play. AI solutions, like those offered by DigitalOwl, can reduce medical analysis time by up to seventy-two percent (72%). This addresses the industry imperative of reducing the administrative burden on claim professionals, creating capacity for more complex or expertise-based actions. An AI-powered medical analysis solution standardizes and structures information, translates complex terminology into layman’s terms, and reduces the variance from personal bias, training, or opinion. Soon, claim professionals may even be able to automate Utilization Review for greater impact.
Quick access to accurate and evidence-based medical insights facilitates more informed evaluations and decisions. Detailed analysis of the injury, treatment, and recovery enables claim professionals to promptly assess and determine if additional resources or case management are required to achieve optimal recovery. This proactive approach helps remove disputes, reducing the risk of litigation expense. Furthermore, a comprehensive analysis of medical records ensures that claim professionals can take necessary actions within the required timelines, significantly reducing the risk of fines. With the integration of expert-level medical data analysis, workers’ compensation insurers can significantly enhance the speed, accuracy, and quality of their evaluations and decisions.
Knowing this, it’s no wonder that the number of P&C insurance professionals using AI has skyrocketed. According to a survey of 250 P&C insurance professionals by the Ethical AI in Insurance Consortium, sixty-six percent (66%) of carriers plan to use AI in 2024. This is a significant increase from the fourteen percent (14%) of carriers using AI today. However, despite the surge of interest in AI solutions, trust remains one of the primary concerns for carriers considering adopting AI in workers’ compensation claims. This is a valid concern, and carriers must select AI service providers committed to the responsible use of AI with fully transparent solutions.
Visit digitalowl.com/trust to discover why leading carriers trust DigitalOwl to keep their data safe. For more insights, check out our white paper, “Navigating Evolving AI Regulation in the Insurance Industry,” at digitalowl. com/ai-regulation.

Jim Sorrells has over thirty years of experience in the P&C insurance industry, with twentysix of those spent leading claims organizations. He serves as Sales Director of P&C Insurance where he is transforming the medical data analysis for Bodily Injury, Uninsured Motorist, and Workers’ Compensation Claims.
In the evolving landscape of dental care, artificial intelligence (AI) is making significant strides in reviewing treatment plans, particularly for occupational injuries. This article delves into AI’s potential to align treatments with injury specifics, safeguarding payers and ascertaining the precision and necessity of dental treatments.
It’s crucial to make sure that dental treatments are accurately matched to the specifics of occupational injuries through review. However, when these reviews are missing, it can result in payers having to cover unnecessary costs. This is where Artificial Intelligence (AI) coupled with a seasoned dentist steps in, offering a transformative solution to this challenge.
The integration of AI into dental treatment plan reviews is a game-changer. By harnessing machine learning and a vast database of dental case histories, AI can evaluate treatment plans for their relevance to specific injuries. For instance, AI can discern when a minor dental injury is met with an overly extensive treatment plan and suggest more suitable and cost-effective alternatives. This ensures optimal patient care and financial prudence for payers. The risks associated with non-clinician review include over-treatment and under-treatment. Overtreatment can lead to unnecessary procedures for patients and increased costs for payers. On the other hand, under-treatment can compromise patient care and potentially worsen their condition.
MTI’s dental program powered by Workforce Dental Solutions, harnesses AI for dental treatment review. Our Dental Director, Dr. Maria Kunstadter, DDS, and her team of dentists use AI to evaluate the accuracy and necessity of dental treatments. This tool allows her team to review treatment plans efficiently, ensuring their relatedness, appropriateness, and cost-effectiveness. Proprietary AI technology assesses dental risks and validates treatment necessity. The process begins with X-ray uploads, followed by an AI evaluation of recent injury-related dental anomalies. Dr. Kunstadter’s review enhances the accuracy of the treatment plan’s relevance to the injury.

In conclusion, AI’s role in dental treatment plan reviews is a promising development for ensuring treatment appropriateness, especially concerning occupational injuries. AI facilitates a thorough and efficient review process, helping to avoid unnecessary payer costs and guaranteeing suitable patient care. As AI continues to evolve, its significance in dental care is set to increase. To illustrate, consider a case where AI was able to identify areas not work-related due to its ability to determine the age of a condition in the mouth. This capability of AI helps in avoiding unnecessary treatments and costs, further emphasizing the importance of AI in dental treatment reviews.

Leane St. Peter has three decades dedicated to the workers’ compensation industry and brings with her a wealth of experience in operations, network development, and strategic planning. As CEO of Workforce Dental Solutions, she has partnered with MTI America to revolutionize workers’ compensation dental claims management, providing a range of virtual and in-person dental care backed by strategic clinical oversight and utilizing AI-driven treatment plan evaluations.
Steve Heinen
Employers are getting increasingly frustrated with the costs of growing litigation in our workers’ compensation system. While benefits are statutory, almost fifty percent (50%) of the lost time claims in Georgia end up in litigation and the period of indemnity is significantly longer in Georgia.
In a recent LinkedIn post viewed by over 6,000 people the question was posed: In most cases the claimant attorney’s goal is to…

Get the employee back to work 17%
Keep the employee out of work 83%
To most employers/insurers, these results are quite predictable. The real question is what are employers/insurers doing to stem the rising cost of litigation? In a webinar I recently hosted, we touched on the following ten (10) topics:
1. Leadership: Everything rises or falls with leadership
2. Poor hiring decisions: Ninety percent (90%) of employers say they hired a workers’ compensation claim
3. Two bad apples: It doesn’t take much to undermine culture
4. Attorneys advertise and employers/insurers don’t: Education > Advertising
5. Work comp claims require trust: If the employee doesn’t trust the employer, they probably will not trust the adjuster
6. Adjusters are overloaded: Case files are typically fifty percent (50%) above best practices
7. Communication: We are becoming more disconnected
8. Accountability: Employers want it but don’t invest in the training to drive it
9. Curiosity: The WC industry lacks the curiosity to get better
10. Action plans: You cannot win a relay race if your fumble the handoff
You can listen to the recording at this link: https://attendee.gotowebinar.com/recording/2163050974400104448
Also, in the webinar, we discussed some tools and resources to use and as a bonus, attendees were given the tools afterwards by completing a survey. If you would like to receive those tools, as well, please fill out the survey: https://survey.sogolytics.com/r/GinS0j

Steve Heinen, CWCP, AAI, and partner with Sterling Seacrest Pritchard, has been an active influencer in the insurance industry since 1983 focusing on Workers’ Compensation. He is also the President of Risk Management Inc. where he developed the comP4® process which has helped organizations reduce workers’ compensation associated costs. He is a graduate of the University of Georgia and is active in the Independent Insurance Agents of Georgia. His Work Comp Playbook for Employers has sold over 6,000 copies.
Effective control of your workers’ compensation (WC) program includes taking charge of the vendors who provide essential services like medical bill review, pharmacy benefit management, nurse case management, defense attorneys, and adjusters. These professionals are hired to safeguard your interests—primarily your financial assets. But how can you be sure they are truly working in your best interest? Do you receive monthly activity reports that focus on net results?
Is your input actively utilized in managing your claims? Effective handling of workers’ compensation claims demands constant communication with injured employees, doctors, and employers. In loss-sensitive programs, employers are the payors, making their input vital in controlling losses within their unique cultures. Your perspective is invaluable; does your third-party administrator (TPA) integrate your insights into their claim action plans to enhance investigations, medical treatments, and return-to-work (RTW) strategies? Furthermore, does your TPA treat your employees with the empathy they deserve? Remember, your employees are a crucial asset, and they need professional support throughout the claim process.
While larger TPAs often follow rigid protocols, boutique TPAs offer the flexibility and personalized service necessary to adapt to your specific needs. They understand that each employer’s environment is unique and tailor their approach to maximize efficiency and satisfaction. By choosing a boutique TPA, you ensure that your employees receive the individualized attention they deserve, leading to quicker recoveries and better outcomes.
Minimizing Timeframe Delays: Speed
Delays are a significant factor in escalating claim costs. Does your TPA have robust controls to minimize these delays? In WC claim handling, speed is of the essence. The most efficient programs ensure minimal delays from initial contact (ideally within four hours of receipt), through medical treatment and diagnostic testing, to physical therapy scheduling, independent medical examinations (IMEs), bill payments, RTW, and settlements. If you are experiencing significant delays, it could be due to high file loads, off-diary files, or unnecessary bureaucratic hurdles aimed at internal profit centers. Engage with your TPA to discuss improvement strategies to eliminate these large and unnecessary costs.
The above is by no means an exhaustive list; there are numerous ways to enhance your risk management program. Your TPA should be a true partner, prioritizing your best interests in every aspect of their handling. While TPAs must adhere to statutory or legislative requirements, they also have to protect your human and financial assets. If you are not seeing this level of commitment, it may be time to explore alternatives. Boutique TPAs offer a unique approach that combines compliance with a personalized touch, ensuring your program is both effective and efficient.


John Brown, the founder of Convergent CMS, is a thirty-nine-year claims veteran. He initially worked for a national TPA as well as large insurance companies. He transitioned to insurance brokerage, specializing in national accounts in loss-sensitive programs, established a TPA within the firm, and eventually rebranded it as Convergent CMS, focusing on clients in Captive, SelfInsured, and High-Deductible programs.

Garlana Mathews – President and CEO
Workers’ compensation marketing professionals face significant challenges when planning signature events after COVID. More industry professionals are working from home and love the benefits of not having to commute or get dressed in business attire. Getting industry professionals to change out of their comfy house clothes to dress in casual business attire, and leave their homes to attend a work event is more challenging than ever. One of the most pressing issues is securing accurate RSVPs and ensuring attendance. Despite initial enthusiasm, many invitees either fail to attend or cancel at the last minute, adding to logistical headaches and financial losses.
Venues typically require payment upfront, which means the cost of no-shows can be substantial. Addressing this issue involves reinstating the good old etiquette of RSVPing and honoring commitments, or at the very least, providing timely cancellations.
Here are some strategies to tackle this challenge effectively:
Understanding the Impact of No-Shows - No-shows at workers’ compensation events not only waste financial resources, but also affect the overall experience and success of the event. When people RSVP and don’t attend, it leads to:
1. Financial Losses: Venues, catering, and other services require advance payments based on expected attendance. When turnout is lower than anticipated, these costs don’t go away.
2. Logistical Issues: Planning becomes difficult without accurate headcounts. Overestimating attendance can result in surplus supplies, while underestimating can lead to shortages.
3. Reputational Damage: Frequent no-shows can harm the credibility of the event organizers, making it harder to attract attendees in the future.
Strategies to Encourage RSVP Etiquette
1. Clear Communication and Early Invitations
• Send Early Invitations: Send invitations well in advance to allow attendees ample time to plan. State the importance of their attendance and the value they will gain from the event.
• Follow-Up Reminders: Send reminder emails as the event date approaches to confirm attendance and highlight any changes or important information.
2. Simplify the RSVP Process
• User-Friendly Platforms: Use simple and accessible platforms for RSVPs, such as Eventbrite or Google Forms. Ensure that the process is quick and straightforward.
• Mobile-Friendly Options: Ensure the RSVP system works seamlessly on mobile devices, making it convenient for busy professionals to respond.
3. Incentivize Attendance
• Exclusive Benefits: Offer exclusive content, networking opportunities, or early access to event materials for those who attend.
• Raffles and Giveaways: Conduct raffles or giveaways for attendees who show up, adding an element of excitement and motivation.
4. Implement a Cancellation Policy
• Flexible Cancellation Options: Allow attendees to cancel their RSVP up to a certain date. This flexibility can encourage people to update their status if their plans change.
5. Personalized Follow-Ups
• Direct Communication: Send personalized follow-up emails or make phone calls to confirm attendance. Express appreciation for their interest and reinforce the importance of their presence.
• Address Concerns: In your follow-ups, offer to address any concerns or logistical issues they might have, making it easier for them to attend.
6.
• Showcase Attendee List: With permission, share a list of confirmed attendees to create a sense of community and commitment.
• Public Acknowledgment: Publicly acknowledge RSVPs on social media or during pre-event communications, enhancing accountability.
7. Post-Event Feedback and Analysis
• Collect Feedback: After the event, collect feedback to understand why some RSVPs didn’t convert into attendance. Use this data to improve future events.
• Analyze Patterns: Look for patterns in no-shows to identify and address specific issues, such as inconvenient timing or location.
By implementing these strategies, workers’ compensation marketing professionals can mitigate the impact of no-shows and foster a culture of commitment and accountability. Encouraging proper RSVP etiquette not only ensures better event planning and resource allocation, but also strengthens the overall relationship with our workers’ compensation professionals and vendor partners. With consistent efforts, the tradition of honoring RSVPs can be revived, leading to more successful and impactful events.

C. Todd Ross
“What on earth are they talking about?”
Maybe you just sat through your first file review and wondered what the heck everyone was talking about.
Maybe you’re a human resources professional who tried to read the claims adjuster’s notes and you were confused by all the acronyms and abbreviations.
Maybe you’re a new claims adjuster who recently finished training that was like sipping water from a fire hose and now, you’re still trying to figure everything out.
No matter how you start, the good news is here is a cheat sheet to help you navigate the sea of acronyms and abbreviations in the world of workers’ compensation.
Before getting started, please know that each state has its own workers’ compensation jurisdiction. While many acronyms may be similar across jurisdictions, some are very specific. This guide is designed for Georgia.
ADL: Activities of Daily Living
ALJ: Administrative Law Judge
AOE/COE: Arising out of employment/In the course of employment.
Appor: Apportionment
Appt.: Appointment
ATP: Authorized Treating Physician
AWW: Average Weekly Wage
BOR: Bill of Rights (accompanies the POP)
C: Complaints
CA: Claimant’s Attorney
CAT: Catastrophic Designation
C/B: Call Back
CMS: Centers for Medicare/Medicaid Services
COP: Change of Physician
CWCP: Certified Workers’ Compensation Professional
DA or DC: Defense Attorney / Defense Counsel
Depo: Deposition
DME: Durable Medical Equipment
DOH: Date of Hire
DOI: Date of Injury, also expressed as DOL for Date of Loss
DOS: Date of Service
Dx: Diagnosis
EE: Employee
EOB: Explanation of Benefits
ER: Employer
FCE: Functional Capacity Evaluation
FCM: Field Case Manager
FD: Full Duty, sometimes expressed as ND for Normal Duty.
FMLA: Family Medical Leave Act
FROI: First Report of Injury
F/U: Follow Up
Fx: Fracture
HEP: Home Exercise Program
Hx: History
IBR: Independent Bill Review
ICMS: Integrated Claims Management System
IME: Independent Medical Examination
IW: Injured Worker
LD: Light Duty or LDW for Light Duty Work
LE: Lower Extremity
LOV: Last Office Visit
LTD: Long-term Disability
LVM: Left Voice Mail, also expressed as LM for Left Message.
MCO: Managed Care Organization
MMI: Maximum Medical Improvement
MO: Medical Only
MSA: Medicare Set Aside
NCM: Nurse Case Manager (if all work is done telephonically, this may be expressed as TCM for Telephonic Case Manager)
NOC: Notice of Claim
NOH: Notice of Hearing
NOR: Notice of Representation
NOV: Next Office Visit
OC: Opposing Counsel
OOW: Off of Work/Out of Work
PI: Private Investigator
POP: Panel of Physicians
PPD: Permanent Partial Disability, also as IR for Impairment Rating
RFA: Request for Authorization
RFC: Residual Functional Capacity
RTW: Return to Work
RX: Prescription Medication or Pharmacy
SBWC: State Board of Workers’ Compensation
SIL: Salary in Lieu
SIR: Self-Insured Retention
SOL: Statute of Limitations
SSA: Social Security Administration
SSDI: Social Security Disability Income Benefits
SSI: Social Security Income Benefits
STD: Short-term Disability
Stip: Stipulation and Agreement (settlement documents)
Subro: Subrogation
S/w: Spoke with
Sx: Mostly used for Surgery, but it can also be for Symptoms
TC: Telephone call
TOC: Taken Off Calendar
TPA: Third Party Administrator
TPD: Temporary Partial Disability
TTD: Temporary Total Disability, or TD for Temporary Disability.
Tx: Treatment
UE: Upper Extremity
UR: Utilization Review
VR: Vocational Rehabilitation
WFL: Within Functional Limits
WS: Work Status


C. Todd Ross serves on the Legal Committee for the Georgia State Board of Workers’ Compensation’s Steering Committee. He has presented on workers’ compensation topics to numerous claims associations, TPAs, employers, insurers, and self-insureds, and at State Bar of Georgia seminars. He is also active with the Georgia Association of Manufacturers.
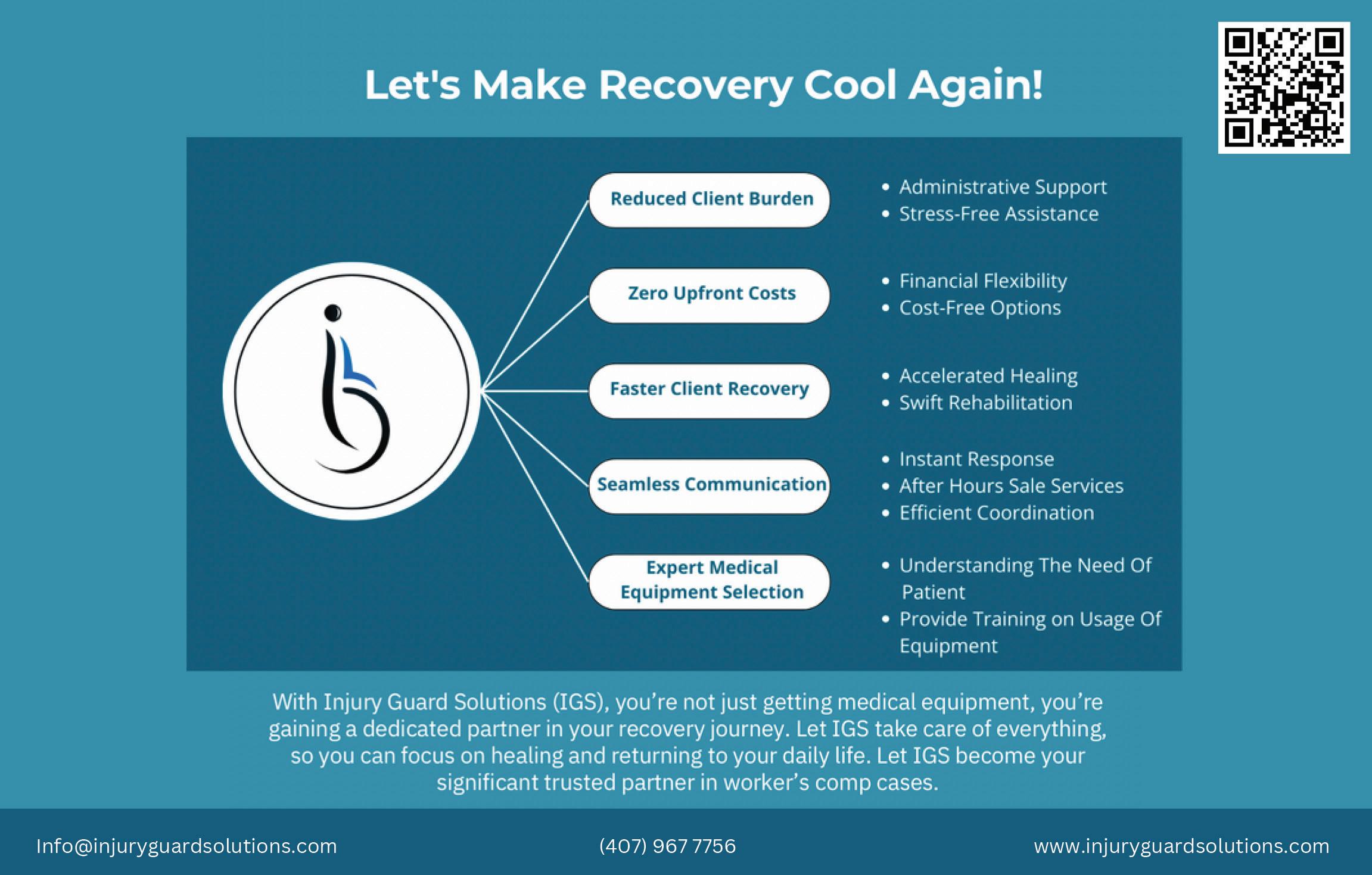




Though the awareness of mental health—specifically Post Traumatic Stress Disorder (PTSD)—has increased over recent years, one of the main challenges of identifying and treating occupational PTSD is the lack of a clear definition and diagnosis criteria. Different professions may have varying levels of exposure to traumatic events, and individuals may react differently to the same event. Moreover, the symptoms of PTSD may not appear immediately after the trauma, but rather develop over time, making it harder to link them to a work-related incident.
Therefore, it is important to establish a common framework for recognizing and assessing occupational PTSD, as well as providing adequate support and intervention for workers who suffer from it.
If an employee has been injured on the job, they are probably experiencing some symptoms of anxiety, stress, and/or depression. These are normal reactions to a traumatic event such as a workplace injury. In some cases, the signs may resolve spontaneously within a few days or weeks without any intervention. However, in many cases, the signs may persist for months or years and even interfere with the recovery process. Untreated psychological injuries can impair physical healing and lead to a mental health disorder such as PTSD, Major Depression, or Anxiety Disorder.
What we know
PTSD is a mental condition triggered by experiencing or witnessing trauma involving death or the threat of death, serious injury, or violence. It results in an array of symptoms that can eventually affect a person’s ability to work, perform day-to-day activities, and engage in relationships.
Those who receive support for a psychological injury early after a trauma are less likely to develop PTSD. Left untreated, a psychological injury can lead to long-term disability putting a strain on the worker, their family, the workplace, and society.
The statistics related to the prevalence of psychological injury, like PTSD following a workplace injury varies greatly in the literature but ranges from ten to fifty percent (10-50%) of workplace injuries. It’s hard to predict who will have issues and who will not. It is not dependent on the seriousness of the trauma or the extent of physical injuries. In addition, it can be tough to detect. Workers are reluctant to discuss it and many health care providers don’t ask.
Psychological injuries can have a marked impact on a survivor’s quality of life. They can become fearful of driving, returning to work, or even leaving their home. In addition, the symptoms are sometimes normalized and trivialized by themselves and others. This can prevent them from seeking treatment.
And, of course, the societal perception of mental health issues which tend to be invisible to others, results in many clients keeping the symptoms to themselves. This can result in prolonged psychological distress and left unmanaged, can contribute to the development of mental health disorders like post-traumatic stress disorder (PTSD) or Major Depressive Disorder (MDD), Anxiety Disorder, or exacerbate negative outcomes such as social disengagement. At this stage, treatment becomes more complex making recovery more difficult and sometimes resulting in lifelong suffering.
As an employer or health care provider, a good preventative approach is to expect all workers involved in a workplace injury to have or be at risk for a psychological injury. Ensure they have access to help from a mental health professional as soon as possible after the incident. Early identification and intervention is the key to mitigating the risk of developing a more serious mental health disorder.

Josefina Bates, a bilingual, Licensed Clinical Social Worker with over twenty years of experience in the social work and mental health field, is the Clinical Director of Safeway SouthEast Psychological Services. Her specialties include trauma, mood disorders, anxiety, depression, and anger management. She believes therapy is a personal journey that should be celebrated by creating an individualized approach based on the client’s needs.
Shane Mangrum, M.D.
What is the worst drug you can take? Turns out, it’s unemployment.
Believe it or not, the relative risk of increased mortality for simply being unemployed is greater than that of diabetes, hypertension, smoking, or obesity. Worklessness is associated with increased rates of death, suicide, obesity, heart attack, depression, alcohol consumption, drug use, accidents, and criminality. Gordon Waddell said, “If worklessness were a drug, it would be malpractice to prescribe it.”
What can we do to help injured workers avoid this hazardous condition?
Strong evidence shows that positive expectations regarding return to work are the best indicator of a successful work outcome. When a person indicates low expectations for recovery, it is likely this is a result of the various factors they are experiencing. These can include medical history, symptoms, and psychological and psychosocial factors. Of those, we can control and improve the following areas:
1. Support at work, and
2. Framing of expectations regarding recovery
We know people will rise or fall to the level of our expectations. Two contrasting psychological phenomena are illuminating here. The first is called “The Pygmalion Effect” in which high expectations lead to improved performance. It is named for the Greek myth of Pygmalion, the sculptor who fell in love so much with the beautiful statue he created that the statue came to life.
This effect was first studied in a famous 1960s experiment by psychologists Robert Rosenthal and Lenore Jacobson. They gave a group of elementary school teachers a special test they claimed would identify students about to experience a “growth spurt” in their IQ. However, the test was a fake, and the growth spurt a myth. Over a school year, the researchers found that the students labeled as “intellectual bloomers” did, indeed, perform better academically than their peers.
The only difference was the teachers had high expectations of these students.
The darker side of this dynamic is the “Golem Effect.” In Hasidic mythology, the Golem is a monster created by a 16th-century rabbi in Prague. In this myth, life is infused into a creature made of clay to enable it to serve its creator. On the Sabbath, the Golem needs to be shut down or it will become destructive. One Sabbath, the rabbi forgot to shut the Golem down, it ran amok, and had to be destroyed; thereby fulfilling the prophecies of its potential bad behavior.
A classic example of the Golem Effect in medicine is the NOcebo effect, which is the opposite of the PLAcebo effect. Expressing the expectation that a treatment (or entire course of care) will NOT improve a patient’s condition has often been found to be self-fulfilling.
We should be aware of the more significant points of contact in the Workers’ Compensation system where expectations can rub off and create either a positive or negative effect:
• FROI
• Adjuster/employer communication
• Office visits
• Return-to-work
During these interactions, it is important to remember there is strong evidence that work disability duration is significantly reduced by:
1. Work accommodation offers, and
2. Contact between healthcare provider and workplace.
Worklessness is a hazard within our system and is a complex phenomenon. Yet, the more we understand the factors impacting it, the better we can structure the workers’ compensation system to minimize it.

Shane Mangrum, MD, is a board-certified physiatrist at Axion Spine & Neurosurgery in Atlanta. He is double-boarded in physical medicine and rehabilitation, as well as sports medicine. He earned his undergraduate degree in organismic and evolutionary biology from Harvard College in Cambridge, Massachusetts, and medical school at the University of Utah in Salt Lake City.

Advanced Hearing
Providers
Ph: 800-598-5300
Email: orders@hearingprovider.com
Web Address: hearingprovider.com

Compass RMS, Risk Management Inc.
Steve Heinen
Ph: 770-540-3810
Email: sheinen@pjins.com
Web Address: Managedcomp.net

Work Bridge Group
National RTW Program Resource
Mail drop locations are situated on both the East and West Coasts
Main - Reno, NV • Corporate – Atlanta, GA (Marietta)
Kerri Butler, Managing Director
Direct Line: 770-294-5936
Ph: 800-890-1620
FAX: 888.530.3222
Emails: Kerri@Workbridgelink.com
Referal@workbridgelink.com
Scheduling@workbridgelink.com
Web Address: www.workbridgelink.com
PBCP Services, LLC
10205 Access Rd Ste B Covington, GA. 30014
Cathy Bowden, MHA, CPC, CPMA, CHISP, CH-CBS
Direct Line: 678-218-9522
Ph: 470-242-7584 ext 101
FAX: 470-443-9230
Email: cathy.bowden@pbcpservices.com

Team Post-Op
14133 NW 8th Street Sunrise, Florida 33325
Oscar Salazar
Direct Line: 954-289-8024 ext 104
Ph: 877-252-0968
FAX: 954.541.5561
Email: info@teampostop.net
Web Address: www.teampostop.net

Jesse Dantice
Direct Line: 954-289-8024 ext 104
Ph: 888.405.8893
Emails: jd@zenjuries.com
workcomp@zenjuries.com
Web Address: www.zenjuries.com


Augusta-Aiken Orthopedic Specialists and Legend Orthopedics are pleased to announce, as of July 1st, we have become one group to better expand the great Orthopedic services we offer across the Augusta, Aiken and surrounding communities.
In addition to our outpatient surgery centers that offer orthopedic and spine surgery at the Downtown campus and on the J. Dewey Gray campus, we have expanded access to imaging, physical therapy, and specialty care in the region to provide convenient access to expert care that is close to you.
912-667-0441
31416
Garlana@selectonenetwork.com
Michelle Wilds
Director Of Client Relations
Cell +1 478-232-0660
Michelle@selectonenetwork.com

With locations in: Augusta, Thomson, Sandersville, Waynesboro, Louisville, Evans, Millen and Aiken SC
Workers’ Compensation Coordinator
Alisha Bond: Ph: 706.863.9797 ext 291 | FAX: 706.941.5000
Email: Workerscomp@ortho-augusta.com Web address: www.augustaaikenortho.com
Augusta- Aiken Physicians: John Bojescul, MD
• Justin V. Bundy, MD • Nicholas M. Capito, MD
• Ty William Carter, MD • John H. Franklin, MD
• David Gallagher, MD • Justin M. Head, DO
• Douglas E. Holford, MD • Jeremy M. Jacobs, MD
• R. Vaughan Massie, MD • Karim Mahmoud, MD
• Richard W. Pope, MD • Timothy J. Shannon, MD
• Mark Snoddy, MD • Nathan Kukowski, MD Physiatrist: Tara Swim, MD
Legend Orthopedics Physicians: Brian Abell, DO
• Terry Arrington, MD • Randall Meredith, MD
• Zachary Herzwurm, MD • Matthew Link, MD
• Joseph Rectenwald, MD • Douglas Phillips, MD
• Samuel Pitts, MD
Contact for above Legend providers: Keeley LaMarsh: workerscomp@legendortho.com
With locations in: Alpharetta, Atlanta, and College Park
Workers’ Compensation Coordinator
Crystal Fowler: Direct Line: 470-751-4180
Ph: 470-579-3962
Email: crystalfowler@axionspine.com Web address: www.axionspine.com
Physicians: Chris Tomaras, MD • Raymond Walkup, MD Physiatrist: Shane Mangrum, MD

With locations in: Louisville, Millen, Waynesboro, Sandersville, and Barnwell SC
Workers’ Compensation Coordinator
Beth Benton: Direct Line: 912.245.7932
Ph: 912.542.0444
Email: bbenton@burkehealth.com Web address: burkehealth.com
Physicians: Jonathan Le, MD • David Doman, MD
With locations in: Carrollton, Bremen, and Villa Rica
Workers’ Compensation Coordinator
Sherrie Ford: Direct Line: 770-834-0873 ext 225 Ph: 770-834-0873 | FAX: 770-834-6118
Employers/Patients can also text to: 770-830-4136
Email: bbenton@burkehealth.com Web address: www.orthowest.com
Physicians: Taylor B. Cates, MD • Kevin M. Charron, MD
• Anthony W. Colpini, MD • Ralph E. Fleck, Jr., MD
• Richard A. Herman, MD • Bryan P. Kirby, MD • Ki Lin, MD
• Daniel L. Maxwell, MD • E. Franklin Pence, Jr., MD
• Gregory S. Slappey, MD • Adam M. Sunderland, MD
• Krishna Guidyala, MD • Robert O’Connell, MD

210 E DeRenne Avenue
Savannah, GA 31405
With locations in: Baxley*, Brunswick*, Claxton, Dublin*, Hawkinsville*, Hinesville*, Macon*, Metter, Milledgeville*, Millen*, Pooler, Reidsville*, Richmond Hill, Rincon, Sandersville*, Statesboro, Sylvania, Vidalia, Waycross*, Bluffton SC
Workers’ Compensation Manager
Joshua Sutphen Ph: 912-644-5384 | FAX: 912-644-6190
Direct Line: 912-320-0053
Email: jsutphen@optimorthopedics.com
Web address: www.optimorthopedics.com
Physicians: Don G. Aaron, MD • Thomas Alexander, MD
• Johnathan Christy, MD • Travis Farmer, MD
• Delan Gaines, MD • Jeffrey Goldberg, MD
• Patrick Hanson, MD* • Joseph Hegarty, MD*
• Juha Jaakkola, MD • Mark Kamaleson, MD
• Gregory Kolovich, MD • Thomas Lawhorne, MD
• John McCormick, II, MD • Thomas Niemeier, MD
• Markus Neiderwanger, MD*
• Christopher Nicholson, MD • David Palmer, MD
• Justin Lancaster, MD • David M. Sedory, MD
• Kevin L. Stevenson, MD* • George Sutherland, MD
• James Wilson, Jr, MD • Chad T. Zehms, MD
• Michael D. Dykes, MD* • Amir Shahien, MD
• Robert Shelley, MD • Jordan Paynter, MD
• Rabindar Bhatti, DO* • Michael Appeadu, MD*
• Wesley Stroud, MD, • Jay Cook, MD
*Optim Health System works in collaboration with Optim Orthopedics and the physician-owned Optim Medical Center-Tattnall.

With locations in: Atlanta, Lawrenceville, and Villa Rica
Workers’ Compensation Manager
Kathy Fuentes: Direct Line: 404.220.7843
Ph: 404-973-2444
Email: manager@performanceatl.com
Web address: www.performanceatl.com
Physicians: Stephanie Martin, MD • Shomari Ruffin, MD

Georgia Bone and Joint With locations in: Newnan, Fayetteville, Covington, Stockbridge, LaGrange
Workers’ Compensation Coordinator
Donna Stone: Direct Line: 770-502-2128
Ph: 770-502-2175 | FAX: 770-502-2131
Email: Donna.Stone@surgerypartners.com
Web address: www.GeorgiaBoneandJoint.org
Physicians: George Ballantyne, MD
• Michael Gruber, MD • Chad Kessler, MD
• Michael Cushing, MD • Jayson McMath, MD
• David Heinsch, MD • Clark Walker, MD
• David Love, MD • Shivam Desai, MD
• Michael Webber, MD • J. Carl Sutton, III, MD
• Michael Burke, MD

For Mental Health: 170 Specialists across the US
For Cognitive rehabilitation, Post TBI/Speech and language:
6 Specialists across the US
For information and referrals:
Phone: 888.306.1119
Referrals@safewaycenters.com
Web Address: www.safewaycenters.com
OrthoGeorgia –Orthopaedic Specialists
With locations in: Macon, Milledgeville, Dublin, Warner Robins, Hawkinsville, and Kathleen
Workers’ Compensation Manager
Peggy Boyles, CWCP Manager (Macon): Direct Line: 478-254-5302 | FAX: 478-832-6509
Email: pboyles@orthoga.org
Workers’ Compensation Coordinators
Rita Boling, CWCP (Macon): Direct Line: 478-254-5387 | FAX: 478-832-6509
Email: rboling@orthoga.org
Amber Hart, CWCP (Macon, Milledgeville): Direct Line: 478-749-1613 | FAX: 478-841-3178
Email: ahart@orthoga.org
Barbara Rodriguez, CWCP (Warner Robins, Hawkinsville, Kathleen):
Direct Line: 478-971-1153 Ext. 701 | FAX: 478-971-1174
Email: brodriguez@orthoga.org
Danielle Bohannon, CWCP: Direct Line: 478-254-5412 | FAX: 478-841-3178 Email: dbohannon@orthoga.org
Jennifer Youngclaus, CWCP: Direct Line: 478-254-5363 | FAX: 478-832-6509 Email: jyoungclaus@orthoga.org
Web address: www.orthoga.org
Physicians: William W. Brooks, MD
• William B. Dasher III MD • Wayne Kelley Jr., MD
• Ryan E. Schnetzer, MD • Jonathan S. Harris, MD
• Dennis K. Jorgensen, MD • Todd E. Kinnebrew MD
• Greg P. Lee, MD • Brian J. Ludwig, MD
• Wood D. Pope, MD • Joseph E. Slappey, MD
• Timothy R. Stapleton, MD • Richard R. Thomas, MD
• Robert M. Thornsberry, MD • Matthew J. Toth, MD
• Zaneb Yaseen, MD • Robert E. Blackwell, MD
• Waldo E. Floyd, MD • Yelena Levina, MD
• Maharsh K. Patel, MD • Elliot P. Robinson, MD
• John Z. Chrabuszcz, MD • Oluwatosin J. Ojo, MD
Southern Pain and Spine Associates With locations in: Gainesville, Jasper, Newnan, Sandy Springs, and Athens
Director of Workers Compensation
Linda Lee:
Email: llee@southernpainandspine.com
Web address: workcomp@southernpainandspine.com
Workers’ Compensation Coordinator
Ashley Jones: Direct Line: 678-617-3443
Ph: 678-971-4167 FAX: (678) 971-5205
Email: ajones@southernpainandspine.com
Web Address: www.southernpainandspine.com
Physicians: Ankur Patel, DO, RPh • Jordan Tate, MD
• Peggy Riso, MD • Lori Kiefer, MD • Sushanth Boda, DO

Caduceus TeleMed 535 North Central Avenue Hapeville, GA 30354
Workers’ Compensation Coordinator
Jackie Martinez
Ph: 254-TELEMED
Email: telemed@caduceusoccmed.com
Multiple Providers (22 MD/PA/NP)