
PROACTIVE OR REACTIVE? YOUR SAFETY CONTINGENCY PLAN








The odds are high you have experienced back pain at some point in your life. According to the Centers for Disease Control (CDC), back pain is the highest reported type of pain in adults. Most acute episodes of back pain go unreported and a minority seek care. However, when related to a workplace injury, those who seek additional treatment can maintain or return to work in a few weeks.
Many of the nonsurgical options to treat acute lumbar strain/sprain focus on stopping the pain by blocking pain signaling. Now, there is a novel approach to decrease pain by restoring function.
The Reactiv8 device is a system that targets improving the function of the main stabilizing multifidus muscles in the back. Instead of “drowning out” the pain, the ReActiv8 device works to retrain your back muscles to increase core strength, improve function, and decrease pain.
The ReActiv8 device is an implantable system consisting of two leads and a generator implanted in the back (see image). The leads are placed next to the medial branch nerves that supply the multifidus muscles. Twice a day, the patient activates the generator to deliver a thirty-minute custom therapy. The therapy signals the nerve to contract the muscle. By doing so, the brain is activated to overcome the neural inhibition pathway to regain control of the multifidus.
This device is best for those with mechanical low back pain without radicular leg pain who have failed physical therapy, medication treatment, and injection therapy. It is not for those with radiating pain into the legs, pain being generated from nerves, or patients who have had or are candidates for back surgery. With mechanical low back pain, the pain is generated from injury or stress on the tissues that support the spine. Pain is worse with prolonged sitting or standing and improved with shifting positions.
Long-term outcomes with ReActiv8 have shown substantial improvement with the majority of patients describing decreased pain and improved functionality. Even more promising is that patients continue to improve over time. At two years, seventy-six (76%) percent of patients had improvement and sixty-five (65%) percent of patients had resolution of the chronic low back pain.
Adverse events with the ReActiv8 device are like other permanently implanted pain devices. The most common complication is the migration of the leads. The U.S. Food and Drug Administration (FDA) is actively determining the compatibility of the device with magnetic resonance imaging (MRI). Currently, the ReActiv8 is not approved for MRI, but hopefully, it will gain approval from the FDA in 2024. It is safe to have x-rays, CT scans, and ultrasounds with ReActiv8.
A second clinical trial, the RESTORE trial, is currently underway and compares patient outcomes using individualized optimal medical management to the restorative neurostimulation of ReActiv8. Publication of the results of the RESTORE trial is planned for 2024. Talk to your pain physician about their specific treatment recommendations.


Lori Kiefer, MD, is dual board-certified in pain management and anesthesiology. She graduated magna cum laude with a Bachelor of Arts degree in Chemistry from Indiana State University and then attended Indiana University School of Medicine for her Doctor of Medicine degree. Dr. Kiefer completed her internship and residency at Vanderbilt University Medical Center in Nashville, Tennessee, practiced as an anesthesiologist for nine years in Bloomington, Indiana, and then decided to pursue further training in pain medicine at Indiana University School of Medicine’s multidisciplinary pain medicine fellowship. She enjoys spending time with her husband and three children, as well as walking, hiking, fishing, and reading.



Disclosure: Event dates could be postponed, cancelled, or virtual. Please use the following as a guide. If you would like your event added to the Workplace Health magazine calendar of events, please contact Michelle Wilds at michellewilds@selectonenetwork. com. Workplace Health magazine would love to come and cover your event.
April
10-12 – GA PRIMA – Rome, GA
10-12 - MWCEA - Biloxi, MS
17 - GA SBWC Regional - Macon, GA
18-19 - FL Bar Workers Compensation Forum (WCCP) - Orlando, FL
24 - GA SBWC Regional - Cartersville, GA
25 – Workplace Health SymposiumAugusta, GA
25 - Atlanta Claims Association Annual Conference - Atlanta, GA
May
2 - BMW Tour SC Employers Advocacy Association - Greer, SC
3 - GA SBWC Regional - Lawrenceville, GA
5-8 – RISKWORLD – San Diego, CA
8 - GA SBWC Regional - Savannah, GA
14-16- National Safety Council Spring Conference and Expo - Rosemont, IL
17 – SCWCEA Seminar – Columbia, SC
20-21 - AL DOL WC Seminar - Orange Beach, AL
June
2-4 – GA Workers’ Compensation Association Spring Conference –Savannah, GA
2-5 - NCSI Annual Meeting and Conference - St. Petersburg, FL
6-9 – National PRIMA - Nashville, TN
10 - SCEAA Annual Golf TournamentColumbia, SC
20 - Moore Ingram Johnson & Steele CEU Symposium - Atlanta, GA
23-26 – SHRM National – Chicago, IL
July
29-August 2 - SAWCA Annual Convention - Miramar Beach, FL
30-August 3 - FL RIMS - Naples, FL
August
11-13 – AL Self Insurers Association Summer Conference – Sandestin, FL
18-21 – WCI-Orlando, FL
25-28 – GA State Board of Workers’ Compensation Annual Conference –Alpharetta, GA
September
3-6 – GA Safety Health and Environmental Annual Conference - Savannah, GA
11-12 - AL DOL WC Seminar - Huntsville, AL
25-27 – SHRM GA Annual Conference –Columbus, GA
October
11 - Inaugural Clay Shoot SCEAA – Camden, SC
15-17 – National WC and Disability Conference – Las Vegas, NV
20-22 – SCWCEA Annual Conference –Myrtle Beach, SC
22-23 - AL DOL WC Seminar - Birmingham, AL
November
7-8 - AWCO Seminar - Birmingham, AL
12 - Physio/Emory CEU SymposiumAtlanta, GA
18-22 - SAWCA All Committee MeetingAmelia Island, FL
December
5 - SCEAA Regional Event - Columbia, SC






One of the most underused tools in workers’ compensation is Return to Work (RTW) programs. Luckily, many companies have their own internal RTW programs. Some companies have relationships with other industry stakeholders who provide volunteer opportunities to implement an RTW program for their employees. Either serves to help companies figure out a way to create an environment that will return injured workers to their jobs.
However, it must be taken into consideration the loss that happens when a person is injured and the employer needs to fill a void—whether permanently or temporarily—while waiting for the employee to return to work. The void is typically a matter of experience, not only by the employer, but by also the employee.
During the COVID-19 pandemic, one of the daunting things was performing our jobs without the camaraderie of our colleagues every day while we were working from home. For many people, that was a difficult adjustment to make leading to lowered morale, depression, and isolation, just as an injured worker might experience.
Here are some ways we, as an industry, can fix this:
• Create a top-down culture of recognizing the benefits of having your injured worker return to work, giving them opportunities to be around colleagues to continue to provide necessary support to the company.
• Discuss RTW with your employees during the hiring process and show how workers’ compensation is not only a benefit to them in the event they are injured, but the company values them and wants to find ways they can accommodate restrictions either on-site or at a local community partner.
• Consider opportunities for an injured employee to return to work at a higher position if their skill set allows it. If not, training and allowing learning and growing into the other position, even if temporary, would be a benefit to everyone.
• Communicate regularly (at least bi-weekly) with your workers before asking them to return to work. Many times, a worker’s first communication from their employer is about return to work opportunities after there has been a period of silence or lack of communication from the employer. Without check-ins for how they are doing post-accident, the employee might feel as though the RTW is a punishment versus an opportunity to contribute.
• Initiate an RTW champion or tsar in-house as a benefit and a liaison to/for injured workers. The value is this person would focus solely on assisting and returning to work employees, finding jobs for injured workers after they’ve been injured, being at their level, above their level, and sometimes below their level to keep them at the job. They can also discuss and advocate for employees to return to work, even if on a part-time basis, recognizing that the benefits are limitless.
While no two workers are ever alike, having the injured employee remain a part of the team is valuable. There will be some injured workers, unfortunately, who believe they’re unable to do anything once they have an injury. However, the lion’s share of injured workers want to be on a team, remain involved, be communicated with, and keep working. Finding ways to bridge that gap will certainly bring better claims results.

Ya’Sheaka C. Williams is a partner at Quintairos, Prieto, Wood & Boyer, P.A., in Tampa, the largest woman/minority-owned law firm in the country. Ms. Williams represents employers, self-insured employers, and insurance carriers in all aspects of workers’ compensation claims throughout Florida. She received her Juris Doctor from Stetson University College of Law and a Bachelor of Arts from Brenau University Women’s College.

Shoulder injuries are an all-too-common occurrence in the workplace. The shoulder joint is one of the most mobile joints in the body so it undergoes a tremendous amount of stress and force throughout the range of motion. Of these shoulder ailments, one of the most common is an injury to the rotator cuff, particularly tears. Without proper diagnosis and treatment, rotator cuff tears can lead to significant disability, cost, and loss of productivity.
The rotator cuff is made up of four (4) distinct muscles: the supraspinatus, infraspinatus, subscapularis, and teres minor. Each of these plays a distinct role in providing stability to the shoulder joint—and the arm—throughout a range of motion. These muscles insert onto different aspects of the humeral head which is typically where injuries occur. There is a spectrum of damage that can occur to the rotator cuff from tendinitis and partial tears to complete full-thickness tears with retraction and atrophy of the muscle.
Initial evaluation of the patient with a suspected rotator cuff injury is crucial in helping to make the correct diagnosis. The mechanism of injury is particularly important as rotator cuff tears can occur when lifting heavy objects, especially overhead, as well as with falls onto the shoulder and dislocations of the joint in patients over the age of forty. Patients will typically complain of pain and weakness while trying to lift the affected arm, often with lateral pain in the shoulder and discomfort throughout the night.
A thorough physical exam of the shoulder helps supplement the history of the injury with muscle strength and range of motion particularly important to evaluate. The patient may have a difference in active range of motion (when the patient is moving their arm at the shoulder) compared to passive range of motion (when the clinician is moving the arm at the shoulder) as well as weakness with internal rotation, external rotation, and abduction of the shoulder. Patients often will be tender to palpation along the lateral rotator cuff insertion along the humeral head.
While the history and physical exam are the most crucial pieces of evidence, imaging studies are also valuable tools in making the correct diagnosis and getting the best treatment for the patient. X-rays are typically obtained at the initial evaluation to rule out any abnormal anatomy or fractures. They may also demonstrate cysts in the greater tuberosity of the humeral head. An MRI can help confirm clinical suspicion of a rotator cuff injury, demonstrating rotator cuff tendinopathy or tearing of the rotator cuff. The interpretation of these studies, in addition to the history and physical exam, is crucial for making the diagnosis and getting the patient the right treatment.
Treatment of rotator cuff injuries varies depending on the pathology. Tendinitis and partial rotator cuff tears can initially be managed non-operatively with physical therapy, anti-inflammatory medications, and subacromial steroid injections. Failure of conservative management is subsequently treated with surgery, typically with debridement of the tendon or repair of the partial tear, either through minimally invasive arthroscopic or open techniques. Full-thickness rotator cuff tears should be managed operatively with the repair of the tendon to its insertion, again through arthroscopic or open techniques. Full-thickness tears that are not repaired can lead to retraction of the tendon and subsequent atrophy of the muscle leading to subsequent shoulder weakness and dysfunction. Tears of multiple rotator cuff tendons with significant retractions, so-called “massive” tears, are often more difficult to repair and often have worse outcomes.
Additionally, massive irreparable rotator cuff tears often lead to shoulder arthritis, termed rotator cuff arthropathy, where there is degradation of the cartilage of the shoulder joint from lack of stabilization of the joint by the rotator cuff leading to stiffness and pain with a range of motion. These patients often require surgical management with a special kind of shoulder replacement called a reverse total shoulder arthroplasty, which puts limitations on the amount of stress that can be placed on the shoulder through activities such as lifting.
Although workplace injuries to the rotator cuff are common and can affect patients to varying degrees, they can lead to significant pain, dysfunction, and cost. Prompt recognition of these injuries is crucial to restoring normal function and getting patients back to work.

Matthew J. Toth, MD, is a board-certified orthopaedic surgeon fellowship trained in sports medicine at OrthoGeorgia. He received his Bachelor of Science in Biology and Doctor of Medicine from Georgetown University in Washington, D.C., graduating Cum Laude. He serves as a team physician for John Milledge Academy, Georgia Military College, and a physician for Georgia College and State University where he is also the Medical Director of the Athletic Training program. Dr. Toth serves on the Board of Directors for the Milledgeville-Baldwin County Chamber of Commerce.


Another Florida legislative session has concluded. Every session starts with a raft of bills, each addressing some challenge, shortfall, or urgency. One issue raised in 2024 that directly impacts health is the physician shortage and perceptions of its cause. Multiple bills were introduced to limit the impact of non-compete agreements on medical practices. A non-compete agreement is just that, a contract that prevents a physician from competing with a former employer when the relationship ends.
There are sound arguments for non-compete agreements. An employer, such as a hospital, will invest significantly in a physician’s practice. Patients must be attracted through referrals and advertisements, and success may require patience as much as patients. Doctors may be paid hiring bonuses or relocation costs. They may draw salaries based on the expected growth of a practice, subsidized by the hospital. These are fixed-cost investments the employer hopes to recoup over time. When the investment begins to pay off with a robust practice, the physician might elect to leave and open a clinic across the street or across town. Patients likely follow them and the hospital that made the investment begins the process again with the next physician hired.
There are sound arguments against non-compete agreements. A physician subject to such an agreement may become dissatisfied or disenchanted. There are potentials for “buyer’s remorse” and regret of having contracted. The physician may have relocated for a job at personal expense, monetary, familial, social, or otherwise. A disenchanted doctor is faced with relocating the family yet again, commuting extensive distances, or re-aligning a practice.
Florida Senate Bill 458 proposed a limited restriction on such agreements, and a broader invalidation of restrictive covenant was in House Bill 11. Neither seems destined to be a reality soon. However, the access to care issues remain.
Notably, this is broader than Florida. NBC reported in March that concerns are voiced elsewhere. NBC also reported these “agreements have become standard practice” for those “employed by hospitals or large health systems.” Some physicians are resisting non-compete agreements in court. One notably claims societal detriment in preclusion from seeing “critically ill children,” who he says will therefore “travel significant distances…to…access care.”
How far is the geographic distance? Should it matter? What if the constraint applies to “this state” for three years? If the physician leaves that employer, she or he might have to practice elsewhere for years; perhaps less of a challenge for a Pensacolan with opportunities next door in Alabama. But what of an employee physician in Miami or Tampa?
Patient frustration is predictable and understandable. The country faces a physician shortage that is likely to worsen. The AMA notes “nearly half of all practicing physicians in the U.S. today are over age 55.” Some predict “a national physician shortfall of at least 37,000—and possibly well over 100,000—over the next decade.”
The hospitals are striving to keep the doctors in whom they have invested. Hospitals are needed in all communities, large and small. Physicians are striving to practice in the recently predominant employee-doctor paradigm. They are likely reluctant to sign non-competes. With the physician shortage limiting patient access generally, non-competes may be impacting decisions by hospitals and doctors. This may impede the market’s ability to react and adjust to supply and demand. While changes do not appear imminent, it is perhaps inevitable that something will have to give.

David W. Langham, has been the Florida Deputy Chief Judge of Compensation Claims since 2006. His legal experience includes workers’ compensation, employment litigation, and medical malpractice. He has delivered hundreds of professional lectures, published over forty articles in professional publications, and has published over 950 blog posts regarding the law, technology, and professionalism. David is a student, a teacher, a critic, a coach, and a leader. He lives in Pensacola, Florida, with his wife, Pamela Langham, Esq.





As a defense attorney, I typically think about repetitive trauma in the traditional sense. For example, Carpal Tunnel Syndrome can develop when an employee performs the same repetitive task over many years. South Carolina’s Workers’ Compensation Act even has a heightened standard of proof for these kinds of injuries. However, in 2022, the Court of Appeals issued a decision making it substantially easier for claimants to succeed in repetitive trauma claims. Although our Supreme Court should issue its own decision in this case soon, stakeholders should be aware that repetitive trauma claims could become increasingly common.
Under the Act, a repetitive trauma injury is compensable only if a single commissioner makes a specific finding of fact of a causal connection established by medical evidence between the repetitive activities and the injury. This statute arguably sets forth a two-part test requiring (1) a specific finding of fact that the activity is repetitive and (2) medical causation. This standard of proof is higher than the standard for “normal” acute injuries by accident.
In Brooks v. Benore Logistics Systems, Inc., the Court of Appeals effectively relaxed the standard of proof for repetitive trauma claims:
In Brooks, the claimant worked as the driver of a “switcher truck.” His job duties required him to climb in and out of the truck cabs, sometimes up to over two hundred times during a twelve-hour shift. In 2017, the claimant began having pain in his back and leg. His initial report of injury was consistent with an acute injury, but the treating physician later recorded it as a gradual onset of symptoms as the result of his job activities above. The carrier denied the claim.
At the hearing, the claimant relied on the treating physician’s opinion, which stated that his repetitive work activities caused the injury. However, the physician was never asked if the job duties were actually repetitive, nor was he shown a job description. The Claimant also did not submit any expert evidence showing that his activities were, in fact, “repetitive.” The defendants submitted an ergonomics report stating that the claimant’s activities did not expose him to a higher risk of injury.
The single commissioner found the claimant had met his burden of proof despite not submitting an opinion that his job duties were repetitive in nature. The full commission disagreed, holding that claimant failed to prove that his job duties were repetitive. The Court of Appeals agreed with the Claimant, finding that the treating physician’s opinion was sufficient to prove compensability because the Act does not require a separate finding of fact that the activity was repetitive.
So, what does this mean? Ultimately, if South Carolina’s Supreme Court affirms Brooks, it may open the floodgates for repetitive trauma claims. Brooks is especially concerning if “normal” work activities—like getting in and out of a truck—now qualify as repetitive trauma as long as the Claimant’s physician assumes that the work activities were repetitive and then issues a causation opinion based on that assumption.
Regardless of how the Supreme Court decides, it is critical that defendants obtain the appropriate expert evidence, including expert medical evidence, to support their position in repetitive trauma claims.


Andrew T. Smith is a workers’ compensation defense attorney in the firm’s Charleston, South Carolina office. He earned his B.A. from the College of Charleston and his J.D., summa cum laude, from the Charleston School of Law. Prior to joining the firm, Andrew practiced in the areas of workers’ compensation, employment law, and general tort liability. Andrew is admitted to practice in state and federal court in South Carolina and before the United States Court of Appeals for the Fourth Circuit. Andrew is also a member of the South Carolina Workers’ Compensation Educational Association.





The ongoing discourse on artificial intelligence (AI) holds profound implications for workers’ compensation, directly impacting risk managers and buyers in this sector. In the evolving workplace landscape, critical considerations demand the attention of those managing risks and making purchasing decisions in workers’ compensation.
A central concern revolves around the potential introduction of biases in decision-making processes driven by AI tools. The Wired article explores AI’s use in résumé screening and promotion recommendations, revealing instances where biases were embedded in algorithms. For risk managers and buyers in workers’ compensation, this raises a critical question: How might AI impact hiring or promotion decisions within their organizations? The inherent biases pose a risk of discriminatory outcomes, prompting a need for vigilance to ensure fair and equitable practices in workforce-related processes.
Transparency and accountability take center stage in navigating the AI landscape. Risk managers must possess a clear understanding of the algorithms powering AI tools in workers’ compensation processes. The opacity of these algorithms presents challenges in assessing whether decisions align with ethical and legal standards. Advocating for transparency becomes essential for risk managers, enabling scrutiny and validation of the fairness of AI-driven decisions.
Data security and privacy concerns become prominent as AI integration often involves handling sensitive worker data. Robust measures are necessary to protect this information. Risk managers and buyers must prioritize data security to comply with regulations and safeguard the privacy rights of the workers involved. This includes assessing the data handling practices of AI providers and ensuring alignment with industry standards and legal requirements.
Vendor selection and due diligence emerge as critical steps in mitigating risks associated with AI in workers’ compensation. Buyers and risk managers need to thoroughly vet AI providers, scrutinizing their operations and understanding the potential biases embedded in their algorithms. A comprehensive evaluation of the provider’s track record and commitment to ethical AI practices is essential for making informed decisions about the adoption of AI tools.
Ethical considerations loom large as AI becomes an integral part of the workplace. Risk managers play a pivotal role in advocating for and implementing fair and ethical practices in AI-driven processes. Ongoing monitoring, assessment, and adjustment of AI systems are imperative to ensure alignment with organizational values and legal standards. This proactive stance is essential for maintaining trust among employees and stakeholders.
Legal and regulatory compliance adds complexity to the adoption of AI in workers’ compensation. Risk managers must navigate the evolving legal landscape surrounding AI use, ensuring that these technologies comply with relevant laws and regulations. Staying informed about legal requirements and adapting AI applications accordingly is crucial to avoiding legal ramifications.
Employee relations and trust emerge as critical considerations in the context of AI implementation. The introduction of AI into the workplace can impact employee trust, prompting risk managers to strategize communication efforts to address concerns and build confidence. Emphasizing transparency, fairness, and the responsible use of AI can contribute to positive employee relations.
In conclusion, the evolving landscape of AI in workers’ compensation demands a proactive and informed approach from risk managers and buyers. Addressing concerns related to biases, transparency, data security, vendor selection, ethics, legal compliance, and employee relations enables stakeholders to navigate the complexities of AI adoption and contribute to a fair and responsible integration of these technologies into the workers’ compensation sector.

Eric F. Patten RN, B.S.N., is the Executive Vice President of Operations & Business Strategies for The Kingstree Group, a leader in the Workers’ Compensation industry for over 24 years, utilizes a consultative approach to lead, create and manage clinical product lines for customers. As a national speaker and educator on trending healthcare topics, Eric is known to execute solutions that create custom and company values and growth.
Happy New Year from the State Board of Workers’ Compensation. I am honored to serve as your chairman and grateful to Governor Brian Kemp for his continued friendship and support. As a recap of last year, I am happy to report that we had a successful year in 2023 across all Board functions and divisions, owing to the hard work and focused attention of our dedicated staff.
We continue to stay busy with mediations, hearings, appeals, and settlements. In fact, our settlement unit staff has been busier than ever processing just under 20,000 stipulations last year—an all-time high. The overall system is healthy and stable as the board continues its primary mission to keep it that way as we launch into 2024.
I was delighted to participate in three of our important events during the second half of last year: the Board’s Annual Educational Conference, the Chairman’s Advisory Council, and the State Bar Workers’ Compensation Law Institute. At the Annual Conference, we enjoyed an action-packed lineup of information and activities, including a very special session focused on our Spirit Award, Tom Howell Award, and Kids’ Chance of Georgia. Each year, these recognitions allow us to hear about inspiring real-life stories and to appreciate the true impact of the workers’ compensation system on the lives of fellow Georgians. We look forward to hosting our conference this year at The Hotel at Avalon in Alpharetta from August 26-28, 2024.

At the Chairman’s Advisory Council, we gathered on the coast for two days to facilitate discussion in general sessions and committee meetings to advance consensus ideas for consideration. The six committees spent time analyzing a host of issues and then gave detailed reports to the entire council. Some of the topics covered included plans for the regional seminars, updating fees and the manual for rehab suppliers, guidelines for nurse case managers, work release programs, the panel of physicians, the medical fee schedule, independent medical evaluation fees, filing board forms, direct deposits, appeals to superior court, conservatorships, subrogation, and post-traumatic stress disorder (PTSD) legislation. At this time, only the PTSD insurance-based solution in House Bill 451 emerged as a consensus issue for the Georgia General Assembly, while a few other issues are pending in the Rules Committee and still others will continue debate in their respective committees.
At the Workers’ Compensation Law Institute, we experienced three days of practical advice on the core aspects of workers’ compensation cases. The panels were staffed with subject matter experts and often included a representative from the Board, the claimants’ bar, and the defense bar. Each year this approach leads to open and fair discussion on a range of issues for the benefit of hundreds of attendees. I am grateful to our judges who participated, the chairs who organized the program, and the entire bar for continuing this annual tradition that promotes congeniality and cooperation.
I hope everyone has a great start to 2024 and I look forward to seeing you at our regional seminars or other events this spring. Feel free to contact me anytime directly with questions or comments about the Board or any other matter. For the latest updates and information, please visit our agency website at https://sbwc.georgia.gov.

Ben Vinson was appointed Chairman and Chief Appellate Judge of the State Board of Workers’ Compensation by Georgia’s Governor Brian Kemp in May 2021. He previously served as Director and Appellate Division Judge for the Board, appointed by former Governor Nathan Deal in July of 2017. In addition to hearing Workers’ Compensation cases on appeal, Chairman Vinson shares responsibility with Judges McKay and Bahl for governing the state agency, which includes regulatory, policy, and operational matters.





Meet a rock star coach. No, not Andy Reid or Kyle Shanahan. “Coach” Keisha Dewey-Sanders, Claims Operations Supervisor at the Louisiana Workers’ Compensation Corporation (LWCC) and the individual responsible for incorporating a Workers’ Recovery Professional (WRP) mindset into the onboarding process of new and recent hires. This is the story of how someone with a vision and empowered to execute it can create a lasting impact in an organization.
LWCC is Louisiana’s largest workers’ comp provider. Like many large organizations, they experienced turnover during COVID-19 and had to innovate their onboarding process to help new hires—many of whom had little or no direct workers’ comp experience—effectively and efficiently learn their roles.
Their interest was piqued about a workers’ recovery mindset when I spoke at their annual OMNET Provider Forum in January 2023. Leadership sampled our curriculum and discovered it bolstered their evolving injured workercentric claims model. Keisha was the logical choice to create a new training program that fuses a “whole person” mindset with the soft skills to make it happen. She has been a Claims Rep since 2001 and it was “very eye-opening” because “we didn’t have that kind of training when I first started.”
Jill Leonard, Vice President of Claims Operations, and Paul Buffone, Senior Vice President and Chief Claims Officer, quickly realized “we did not want to just hand off a program to them and say, ‘good luck … let us know when you’re done’.” Rather, they embraced a highly collaborative and moderated study group approach, and thus the legend of “Coach” Keisha was launched.
The first cohort at LWCC was launched in Fall 2023, consisting of ten (10) individuals who had been with the company between six months and one year. Although Coach had not done anything like this before, Keisha is surrounded by educators within her family and leaned on them for advice.
Coach led by example, going through the same curriculum as her students. “I have learned a lot and I’ve been a rep for over twenty years. The information I learned was insightful and helpful and it would help everyone in their claim-handling experience. Once you’ve handled claims for so long, you tend to put people in categories, so you may need to change your mindset. I think it will have a positive impact on our claim-handling experience. It will decrease litigation, contain costs, and create many other positive outcomes.” One big takeaway by everyone was that “the injured worker ultimately decides if and when they return to work,” and LWCC focuses on tailoring support to help in the best way possible.
Coach utilized Microsoft Teams to create a calendar to cover all nineteen (19) courses over ten (10) weeks. LWCC provided each student with up to one hour per day of undistracted company time – five hours per week – to work through the assigned courses and homework. They still had claims to manage and productivity to prove, but the key was the Coach working with each student and their manager to ensure they had proper balance during the workday. Keisha was initially concerned they would be overwhelmed, but “nobody had a single complaint.”
Coach created a discussion board to help guide and organize their process, including a “lesson reflection” that included open-ended questions like …
What’s the most important thing you learned today?
“I learned about the importance of putting the injured worker first. Sometimes I do not think about the injured worker as my client, I think of the policyholder as the client. But it is kind of the other way around. Treating the injured worker as a client and putting our best foot forward could be the change in the claim.”
What was surprising?
“Insurance rates being based on the law of large numbers.”
What can/should you do with what you know?
“Identifying barriers by asking open-ended questions and allowing the injured worker to explain their unique situation.”
What do you want to learn more about, and why?
“What more could we offer, do, or change from the injured worker’s point of view to make the workers’ comp process better for them instead of what we as the company think we could change/offer.”
Coach provided supplemental information to reinforce the courses. For example, she found additional resources for a deeper dive into emotional intelligence and communicating with empathy after taking the “Emotional Intelligence” course in the School of Humanities. Coach also provided “cheat sheets” about how LWCC processes claims so students were learning broad best practices from the WRPA faculty, while at the same time understanding how they were specifically applied at LWCC.
At the end of each week, they met as a group for an hour. Each student was expected to share their thoughts on the curriculum. As is usual in a group environment, they learned from each other. Coach said, “It was cool to see their eyes light up when they were sharing” their answers to these three questions:
• Things I learned this week
• How will I apply what I learned in my role
• Things I still have questions about
Coach engaged with each student’s supervisor to explain what they learned that week so it could be reinforced in their one-on-one discussions and ensure what was learned was applied in their daily job. She not only preached accountability, but lived it as well, keeping the management team aware of her progress, adjustments, and results from the program.
In 2024, LWCC started a cohort of new hires, which will be the standard going forward. Given the success, they’re also discussing how to make the program optionally available to everyone regardless of tenure or role. What became evident during the discussion was that the ripple effects from this program go well beyond the professional development of those ten initial students:
• The perception, and reality, are that LWCC is invested in the professional and personal growth of each of their employees.
• Team bonding developed among the cohort will reap benefits as they return to their departments.
• Built-in mentorship with cohort graduates paying it forward to future cohort members.
• The presentation to leadership further reduced barriers between management and their team.
• Holistic learning will ultimately have a positive impact on LWCC’s business results.
The leadership presentation finished with a quote from Benjamin Franklin: “Tell me and I forget. Teach me and I remember. Involve me and I learn.” IMHO, Coach nailed it.
*Article originally published on WorkCompCollege.com Outreach Center


Mark Pew, WorkCompCollege.com founding partner and Provost, is an award-winning international speaker, author and jurisdictional advisor in Workers’ Compensation. The RxProfessor has focused on the intersection of chronic pain and appropriate treatment since 2003. Mark created “Qualified Medical Intervention” which won a 2012 Business Insurance Innovation Award. He received WorkCompCentral’s Magna Comp Laude award in 2016, IAIABC’s Samuel Gompers Award in 2017, “Top 100 Healthcare Leader” by IFAH in 2021 and the Health 2.0 Outstanding Leadership award in 2022. He is a co-founder of The Transitions and is on the Advisory Boards of Harvard MedTech, Simple Therapy, and Goldfinch Health.

Tennis elbow, medically known as lateral epicondylitis, is a common condition that affects millions of people worldwide, not just tennis players. Despite its name, it can occur due to various repetitive arm motions beyond the tennis court. This article delves into the causes, symptoms, treatment options, and prevention strategies for tennis elbow.
Causes:
Tennis elbow develops from overuse or repetitive strain on the forearm muscles and tendons, particularly those around the outside of the elbow. Activities such as tennis, gardening, painting, typing, and carpentry, to name a few, that involve repetitive gripping and wrist movements, can contribute to its development. Poor technique, inadequate equipment, and insufficient warm-up routines may exacerbate the risk.
Symptoms:
The hallmark symptom of tennis elbow is pain and tenderness on the outer side of the elbow. This discomfort may radiate down the forearm and worsen with gripping or lifting objects. Over time, individuals may experience weakness in their grip strength, making everyday tasks challenging. In severe cases, even simple activities like turning a doorknob or shaking hands can be painful.
Treatment:
Managing tennis elbow typically involves a combination of rest, ice, physical therapy, and pain relief medications. Resting the affected arm, applying ice packs to reduce inflammation, and avoiding activities that aggravate the condition are crucial initial steps. Physical therapy exercises aim to strengthen the forearm muscles and improve flexibility, while braces or splints may provide support during recovery. In some cases, corticosteroid injections or platelet-rich plasma therapy may be considered to alleviate symptoms.
Prevention:
Preventing tennis elbow involves adopting ergonomic techniques and incorporating proper warm-up and stretching routines into physical activities. When engaging in repetitive tasks, maintain good posture, use ergonomic tools, and take frequent breaks to rest your arms. Strengthening exercises targeting the forearm muscles and maintaining overall fitness can also reduce the risk of developing tennis elbow. Additionally, using appropriate equipment, such as a properly fitted tennis racket or ergonomic keyboard, can help prevent unnecessary strain on the tendons.
Tennis elbow can significantly impact daily life and hinder participation in sports and other activities. Recognizing the early signs, seeking prompt treatment, and implementing preventive measures are essential for managing this condition effectively. By understanding its causes, symptoms, treatment options, and prevention strategies, individuals can take proactive steps to alleviate pain, regain strength, and prevent recurrence, enabling them to pursue their passions with confidence both on and off the court.


Heather Licht, MD, is a board-certified orthopaedic surgeon specializing in hand surgery and treats conditions that involve the bones, tendons, nerves, and muscles of the hand. As a team member at Orthopaedic Center’s Hand, Wrist, & Elbow, Dr. Licht believes in applying the least invasive, most effective techniques in surgical treatment and rehabilitation of hand, wrist, and elbow injuries. She loves the diversity of her specialty of being able to treat all ages and the vast array of disorders and treatment options. She believes it’s important to listen to her patients compassionately and strive to individualize their care to meet their specific needs.
WPH is super excited about our Influencers and looking forward to having them join our team. We can’t wait to see where they take Workplace Health Magazine next! When you see them out and about, make sure to take a picture and post it with our hashtag #WPHROCKS



Janna Godfrey RN, BSN, CCM Senior Area Sales Manager at GENEX
Janna has worked multiple states throughout her career and is an industry leader in her field. Currently working for Genex, we are excited to have Janna as a WPH Influencer in Alabama and Mississippi.
Steve Garrett, Retired Director Alabama Workers’ Compensation DOL
Steve is an Industry leader, fresh into his retirement from the Director role for the Alabama Workers Compensation Department with the State. We are happy to have him be one of our distinguished WPH Influencers in Alabama!
Michael Anderson, ARM-P, All Lines Adjuster. C.H.E.S. / Senior Executive for Triune Health Group
A National Industry Leader with ties to every state, we are looking forward to having WPH in all the places Michael goes! Michael is with Triune Health Group.

In the intricate landscape of workers’ compensation insurance, the experience modification factor, commonly referred to as an “e-mod,” stands as a pivotal modifier that can either mitigate or escalate your premium costs based on your loss history. Understanding how this factor is calculated is paramount to navigating the intricacies of insurance premiums.
Essentially, an experience mod is measured on a scale, with 1 being the industry average. When a business surpasses this benchmark and registers a 1.5, it is classified as having a high e-mod. This distinction carries financial implications, as the e-mod directly influences ones workers’ compensation premium.
Imagine a scenario where your business boasts an e-mod of 1.5. In practical terms, this means you would be paying an additional $50,000 for every $100,000 in premium, compared to a business with an average e-mod. The chart below vividly illustrates the financial repercussions of various mod factors, emphasizing the significant impact on the final workers’ compensation premium.
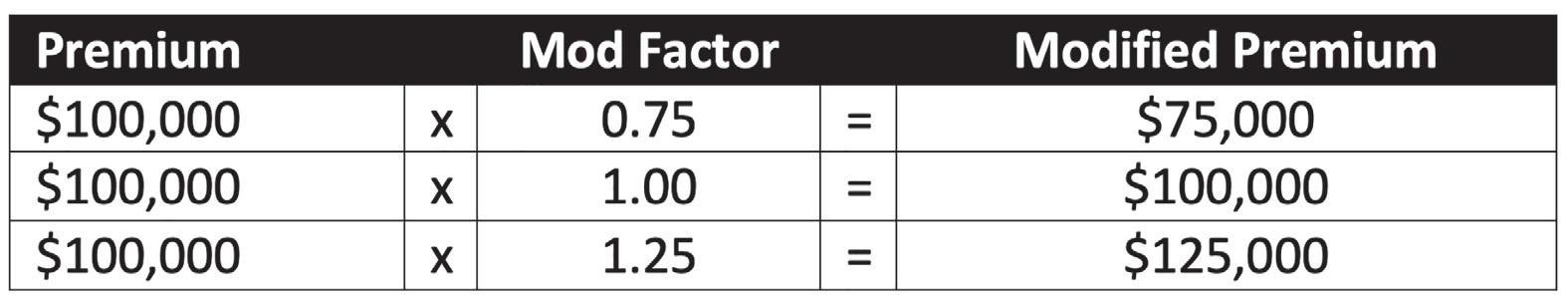
Proactively managing and comprehending the experience mod is not just a prudent move; it’s a financial imperative. The key lies in recognizing the steps to take in order to lower the experience mod, subsequently curbing insurance costs. For an in-depth exploration of these strategies and insights tailored to your unique business circumstances, consider reaching out to Synergy Comp.
In conclusion, the experience mod is a powerful determinant in the realm of workers’ compensation insurance. By mastering its nuances and strategically managing your loss history, you hold the key to substantial cost savings. For a personalized guide on lowering the experience mod and optimizing insurance expenditure, connect with Synergy Comp.
Through empowerment and knowledge, let the mastery of the experience mod be a beacon in navigating the path to costeffective workers’ compensation coverage.
To learn more about Synergy Comp’s team of workers’ compensation specialists, visit www.synergyinsurance.com.

 James First handles the marketing at Synergy Corp, a monoline workers’ compensation insurance company. He studied Marketing and Graphics and recently graduated with a Masters in Business Administration.
James First handles the marketing at Synergy Corp, a monoline workers’ compensation insurance company. He studied Marketing and Graphics and recently graduated with a Masters in Business Administration.



Like so many of us who work in the safety field, I have a story as to how I got here. Mine began twenty-four years ago when I began working at The Home Depot as a loss prevention supervisor. All my jobs prior to arriving at the home improvement retailer had been in traditional loss prevention roles… in other words… catching bad guys. That all changed. As a working warehouse, safety had to be the top priority and fell to all leaders to support and drive a culture of safety for our associates and customers.
Over the years at The Home Depot, safety was always a part of my duties. However, in 2012, it become my primary responsibility. I took on the role of corporate safety manager, responsible for operational safety programs and communications. Like so many people with new career paths, I approached this role with a great deal of optimism and enthusiasm, but also a bit of nervousness as to what would be expected of me. My new manager decided the first order of business would be to send me to a safety conference to help with my development.
Thus, began an annual ritual for me I have not missed since that first conference. What I discovered at the Georgia Safety Conference was an opportunity not only to learn and gain insight into what the safety profession was, but to develop a camaraderie with likeminded individuals with the same goals: Keep workers safe.
As the years went by and my praise of the conference continued to grow, I convinced coworkers—and even vendor partners—to attend. In fact, two of them have not missed since I invited them the first time and they have volunteered to join the board with me.
In terms of why the conference is special to me, I’d say it begins with the keynote speaker and through the breakout sessions and continues to the lunch and closing speakers. Each year, I have taken away at least one nugget containing an “A-ha!” moment I carried with me back home. I also value the reminder that there are many of us out there who take safety personally and it goes a long way to keeping more people safe in the workplace.
Above all, I have always walked away from the conference completely inspired. Encouraged to go back and do the work that means so much to us all, the employees we support, and the families who need them to come home safely each day. That means something to us.


Patrick is currently the corporate safety team leader at The Home Depot, where he has worked for the last twenty-four years in various field and corporate support roles. He’s worked on the safety team for the last twelve years supporting various parts of the safety organization. He is a Certified Safety Professional and a member of the Georgia Safety Conference board.


When you need Case Management, these Independent Case Managers are here to help you! Each one is dedicated to the best care for the injured worker!!
Comprehensive Healthcare Consultants, LLC
Catastrophic Care Management
Cannon Peppers, RN, BSN, CCM
Cannon.peppers@mychccare.com
Phone: 678.205.6645
Fax: 800.814.8122
Www.mychccare.com

ARM Case Management Solutions
Georgia Catastrophic Rehabilitation Supplier
01183C- Multi Lingual
Aruna Rao-McCann, MS, CRC, CCM
Aruna@armcasemgmtsolutions.com
Office: 770.723.0861
Mobile: 678.357.7958
Fax: 404.420.2195

Parker Group Case Management
Catastrophic Case Manager
Yvonne B. Parker, CRC, CCM
Yvonnebparker@gmail.com
Phone: 404.314.0281
Fax: 770.322.7335
Swain Case Management LLC
Catastrophic Case Manager #1333
Sheryl Swain, MEd, CRC, CCM
sswain@swaincasemgt.com
Phone: 770.823.3847
Fax: 770.573.6473
Milford Medical Management
Brandi Milford, MS, CRC, CCM
Ga Catastrophic Rehabilitation Supplier #01585
404-293-1109 (mobile)
770-407-5128 (fax)

Here is a look at the City of Atlanta v. Sebastian which was heard before the Court of Appeals of Georgia - A23A1185, Decided July 27, 2023.
The issue before the Court of Appeals was as follows: Who is the actual Authorized Treating Physician for purposes of determining the validity of a suspension of income benefits based on a regular duty work release. The unilateral suspension of indemnity benefits is contemplated by O.C.G.A. 34-9-221 (c) with the mechanism of proper suspension detailed by Board Rule 221 which states in relevant part:
Board Rule 221 (i) (4) (a) …“When suspending benefits for release to return to work without restrictions, the employer/insurer shall attach to the WC-2 a copy of the supporting medical report from employee’s authorized treating physician who must have examined the employee within sixty days of the effective date of the release.” Of course, the Board rule also provides that suspension on this ground is a change in condition and ten (10) days written notice is required.
In the Sebastian claim, the injured police office was receiving treatment for multiple injuries from Dr. Craig Weil, a panel physician chosen from the employer’s panel. Dr. Weil represented the employee’s one-time free change from the original panel physician. Dr. Weil provided medical treatment to the injured worker for multiple injuries including cervical, hand/wrist, and carpal tunnel. However, at one point, Dr. Weil recommended follow-up treatment with a cervical spine specialist and recommended Dr. Thomas Dopson.
On November 17, 2020, Dr. Weil issued a light duty work release to the claimant with the provision that the patient was not returning to Dr. Weil’s office for treatment. Dr. Weil indicated that any future restrictions should be determined by a spine specialist through Workers’ Compensation with a recommendation for Dr. Christopher Edwards.
Although Sebastian never saw Dr. Edwards, he did see Dr. Thomas Dopson on multiple occasions for his cervical spine. On September 16, 2020, Dr. Dopson was of the opinion that the claimant was at maximum medical improvement and capable of his regular work without restrictions. Dr. Dobson reiterated his opinion that the claimant was capable of full duty during office visits in January and February of 2021. After the last visit with Dr. Dopson, the City of Atlanta unilaterally suspended Sebastian’s benefits on the following grounds:
“Employee was able to return to work on February 3, 2021 without restrictions from the authorized treating physician.”
Sebastian moved for reinstatement of his benefits on the grounds that Dopson was not the authorized treating physician; therefore, benefits could not be suspended based on Dobson’s work release. The Administrative Law Judge assigned to the case (“ALJ”) agreed with Sebastian and reinstated his benefits and awarded $2,600 in assessed fees against the City. The Appellate Division affirmed the decision and Superior Court upheld that finding.
The Court of Appeals in dicta noted there was no clear definition of “authorized treating physician” within the Workers’ Compensation Act nor the Board Rules, however, it noted that the O.C.G.A. 34-9-201(b) draws a clear distinction between a “primary authorized treating physician” and a referral or consulting physician. The Court concluded as follows:
“We agree with the Board that the City’s unilateral suspension of benefits based on a work release from a referred physician violated the workers’ compensation rules and contravened the Act. The trial court, therefore, properly affirmed the Board’s decision to reverse the suspension and reinstate Sebastian’s benefits.”
In a footnote, the Court noted in the Appellant’s argument Dr. Weil had clearly deferred any decision on Sebastian’s work status to Dr. Dopson. However, the Board found otherwise due to Dr. Weil’s later referral to Dr. Edwards. The Court stated thus:
“We need not address therefore, whether an employer may unilaterally suspend benefits based on the findings of a referred specialist to whom the authorized treating physician has deferred the work status decision.”
The Sebastian decision could certainly make it more difficult to accomplish a unilateral suspension of benefits based on a full duty release if the claimant is treating with multiple providers or treating for multiple injuries. There are opinions on both sides of the aisle as to whether the Court of Appeals decision in Sebastian should remain the law of the land. A writ of Certiorari has been denied, but a Motion for Reconsideration is pending with a ruling expected within days.
In the interim, this attorney’s recommendation is to pay close attention to the purpose behind the referral. If, for example, the Occupational Clinic intends to discharge the claimant from care post referral to a specialist, try and obtain clarification in a signed document from the primary doctor’s office. I have also come across references in notions from certain Occupational Clinics where the entry for work restrictions plainly states: “per the referral physician or deferred for specialist.” Clearly, this is the situation the Court of Appeals references in its footnote.
One attorney involved in the Sebastain litigation pointed out that the decision can be used as a sword or shield. For example, if the authorized treating physician refers the claimant to an orthopedic specialist with recommendation for MRI stating: “Full duty no restrictions pending referral/MRI.” What if post-MRI the orthopedic notes full thickness rotator cuff tear and recommends light duty work restrictions. Would a suspension based on a full duty release from the occupational clinic stand? I believe not; however, the Sebastian decision does not provide an answer to the question posed.
Finally, another solution might be an employer’s willingness to give a claimant a “free pass” to the occupational clinic for one or two visits. Thereafter, if it becomes clear that the claimant requires an orthopedic specialist, ask the claimant to choose one from the panel and designate that physician as authorized in writing. If the orthopedic choice is agreed upon as the “authorized treating physician” without requiring a designation as the “second choice”, it might prove easier in the long run than a more circuitous route of having to refer the injured worker back to the non-specialist occupational clinic that might have nothing more to offer in terms of providing treatment or feedback as to the injured employee’s work status.


Paula F. Smith practices Georgia Workers’ Compensation Defense with Willson Jones Carter & Baxley in Atlanta. She has thirty-five years’ experience representing both self-insured and commercially insured employers in a wide array of workers’ compensation matters. She graduated cum laude from The University of Alabama and earned her law degree from Vanderbilt University School of Law in 1988. She enjoys spending time with her family, cooking, running, and dancing.

Most people do very well after total knee replacement with the overall goal of having a pain-free knee, allowing the patient to continue with a productive life. However, as a surgeon, I must add a word of caution in that total knee replacements have a dissatisfaction rate of approximately twenty percent (20%), according to academic research. With our current technology-enabling techniques, we can perform better.
Approximately 850,000 total knee replacements are performed in the United States annually. Over half a million will be robotic assisted by 2026. The reason why robotic-assisted total knee replacements are increasing is that we want to perform better surgeries to decrease the cost of care. Surgeons and patients alike are requesting technologies to improve surgical outcomes and satisfaction.
Robotic-assisted total knee replacement has been shown to improve early pain and function, reduce physical therapy duration, and have a higher precision of implantation compared to manual techniques. These advantages lead to a lower ninety-day episode of care cost compared to conventional total knee replacements. The average cost savings during the ninety-day episode of care averages around $2,400 per case with a cost savings estimated at $14,737 per case for avoiding revision total knee replacements.
Counterintuitively, robotic-assisted total knee replacement utilizes fewer resources than manual techniques while achieving better outcomes. Historically, robotic-assisted total knee replacement required a large, several hundredpound machine with an upfront cost of around one million dollars and required advanced imaging—such as an MRI or CT scan prior to surgery. These large and expensive machines could only be utilized by hospitals due to the physical and financial burden.
Now, newer robotic-assisted systems, such as the CORI robotic system by Smith & Nephew, can be carried in a briefcase and require no MRI or CT scan before surgery. This small, portable robotic system can easily be used in both the hospital and the ambulatory surgery setting. We can achieve better outcomes with fewer resources while not being constrained to a hospital setting.
The ambulatory surgery center is the perfect setting for utilizing robotic-assisted technologies. Same-day robotic-assisted total knee replacement in an ambulatory surgery center is forty to sixty percent (40-60%) less expensive compared to a manual total knee replacement in the hospital setting. This allows us to offer better surgery and quicker recovery at half the cost. Same-day surgery utilizing robotic-assisted technology is the future for better patient outcomes and decreasing the financial burden of medical care.
So, as you can see, embracing the use of technology is important for the future practice of medicine.


Nate Sbravati, MD, is a Summa Cum Laude graduate of Mississippi State University in Biomedical Engineering. He received his Doctor of Medicine from the University of Mississippi School of Medicine and now works in Mobile, Alabama, specializing in orthopedic surgery.
In 1999, the State Board of Workers’ Compensation (SBWC) asked me to create a claims training program for adjusters. The charge from the SBWC was to improve claims handling. A few years into the program, I received an email from a claimant stating: “Workers’ compensation doesn’t work, nor does it compensate.” Communication had broken down. I was taken aback because two decades ago, communication was generally good and litigated claims were outliers.
Fast forward to 2024. Georgia now has one of the most litigated workers’ compensation systems in the country. We lead the country in settlements and length of indemnity. Since January 2019, the cap on indemnity benefits has increased by forty percent (40%). We probably have the worst subrogation law in the country. It is becoming the exception when a claim stays on track.
However…there is good news.
One of the best things about the Georgia workers’ compensation system is its stability. The last big legislative changes were ushered in almost thirty years ago. So, while there are several alarming trends in Georgia, the predictability also gives employers and insurers a roadmap for success.
Here are my top five (5) recommendations:
1. Employers must do a better job of building a culture of trust with their employees. If the employee doesn’t believe the employer will do right by them, they probably will not believe anything the adjuster tells them.
2. Having pre-claim paperwork in place that educates the employees about their rights and responsibilities under Georgia’s workers’ compensation system is critical. Documentation at the time of hire and ongoing is extremely important.
3. Supervisors are a huge cost driver in workers’ compensation claims. Employers that invest in supervisor leadership training generally have fewer litigated claims which results in lower costs.
4. Safety training is crucial. Having an accountable new-hire training program and meaningful ongoing training helps employers build the right culture. As the Burdette case showed us, an accountable safety program could lead to the denial of workers’ compensation benefits if the employee willfully refuses to follow safety rules.
5. Communication (or the lack thereof) is probably the biggest cost driver. Employers must own that seventy percent (70%) of the management of a workers’ compensation claim falls on them. They cannot outsource care and concern to the adjuster. While the cumbersome forms for the 240 processes are typically completed by the adjuster, the employer must own the return-to-work program. And, the employer must communicate rights and responsibilities to an injured employee (including direction to medical).
If these five recommendations are followed, the Georgia workers’ compensation system works and compensates fairly.
One bonus recommendation for employers: take the time to form a relationship with your vendors so they understand your business. Connectivity is the theme of our upcoming Certified Workers’ Compensation Professional (CWCP) Program on May 7, 2024, at the Hotel Avalon in Alpharetta, GA, where there will be two hundred employers, insurers, TPAs, and vendors sharing strategies to help improve outcomes.

Steve Heinen, CWCP, AAI, and partner with Sterling Seacrest Pritchard, has been an active influencer in the insurance industry since 1983 focusing on Workers’ Compensation. He is also the President of Risk Management Inc. where he developed the comP4® process which has helped organizations reduce workers’ compensation associated costs. He is a graduate of the University of Georgia and is active in the Independent Insurance Agents of Georgia. His Work Comp Playbook for Employers has sold over 6,000 copies.






 Georgia Safety Conference Committee Meeting in Atlanta
National WC Conference in Vegas!
Workers’ Compensation Family enjoying the Vendor Candle Pouring Event in Atlanta, GA
Holiday Wine Tasting event at Moore Ingram Johnson & Steele office in Marietta
Industry Professionals enjoying the Candle Pouring and Scent Mixology Workshop
Enjoying the Networking at the RIMS Conference
Georgia Safety Conference Committee Meeting in Atlanta
National WC Conference in Vegas!
Workers’ Compensation Family enjoying the Vendor Candle Pouring Event in Atlanta, GA
Holiday Wine Tasting event at Moore Ingram Johnson & Steele office in Marietta
Industry Professionals enjoying the Candle Pouring and Scent Mixology Workshop
Enjoying the Networking at the RIMS Conference





 Amy Middlebrooks, Case Management Manager and and RJ Tompkins, Area Vice President at CorVel Corporation networking at the RIMS Conference in Atlanta
Congratulations to Southern Pain and Spine on their new location in Athens, GA.
Enjoying the Workers’ Comp Tailgate Party at Southern Pain & Spine in Athens, GA. GO DAWGS!
Savannah Tech Skills USA Team was recognized during the GA Safety Conference for receiving 1st Place in the State and National Competition.
Distinguished forum for the Fall GWCA Conference
Amy Middlebrooks, Case Management Manager and and RJ Tompkins, Area Vice President at CorVel Corporation networking at the RIMS Conference in Atlanta
Congratulations to Southern Pain and Spine on their new location in Athens, GA.
Enjoying the Workers’ Comp Tailgate Party at Southern Pain & Spine in Athens, GA. GO DAWGS!
Savannah Tech Skills USA Team was recognized during the GA Safety Conference for receiving 1st Place in the State and National Competition.
Distinguished forum for the Fall GWCA Conference







Injuries and ailments affecting the neck and shoulder are among the most common and most costly in the workers’ compensation system, averaging $65,000 and $50,000 respectively, per injury. And yet, the overlapping presentations of shoulder disorders with cervical spine problems and the intertwined anatomy, along with the lack of precision in physical examination testing, often result in ineffective or disorganized treatment plans.
The average number of days of lost work for a shoulder injury is 123 days. Shoulder pain impacts sixteen percent (16%) of the general population and rotator cuff pathology increases in physically demanding occupations, with shoulder injuries making up eleven percent (11%) of workers’ compensation claims. Similarly, eleven percent (11%) of all injured workers with lost time claims had neck pain, with the healthcare sector having the highest percentage of claims with neck pain.
Moreover, these diagnoses join forces, occurring together in thirteen to sixteen percent (13-16%) of injured workers with shoulder or neck pain. The older the patient, the more likely these two problems came bundled together.
Complicating things further, this is not just a matter of teasing out the precise diagnosis to get to the root of the symptoms and address the injury. Recent studies have shown that degenerative cervical spine pathology may predispose a patient to rotator cuff tears. Perhaps in an instance of turnabout being fair play, other research demonstrated injury to the shoulder can negatively influence neck alignment. Clearly, the diagnostician must not only understand the differentiation of shoulder and cervical spine pathology, but must appreciate how closely these two systems interact.
Fortunately, the informed and engaged diagnostician has an array of physical assessment tools to employ, inducing various maneuvers to load the shoulder and/or neck respectively. The importance of these tests’ use in clinically correlating imaging findings can hardly be overstated, given the fact that the MRIs “diagnose” superior labral tears in asymptomatic patients aged forty-five to sixty (45-60) years of age in fifty-five to seventy-two percent (55-72%) of cases. These tears may simply be age-related findings, much like “degenerative” spine findings in similarly aged patients. Clearly, we cannot rely on advanced imaging alone to sort out these issues.
It is also notable that injections for pain relief can also be diagnostic in nature and are quite predictive of whether or not surgery for the ailment will have a successful outcome. When it comes to the “neck” portion of the equation, studies have shown that ninety-two percent (92%) of cervical radiculopathy patients who experienced pain improvement of greater than fifty percent (50%) with a cervical transforaminal epidural injection had successful outcomes with cervical decompression surgery. Similarly, individuals who have a positive response to a shoulder injection (even temporarily) tend to have better outcomes following surgery.
At the end of all the diagnostic processes, of course, the goal is to reduce symptoms and get the injured worker back on the job. All in all, there are significant challenges in navigating this complex area, which only highlights the importance of judiciously using the tools at our disposal.


Shane Mangrum, M.D., is a board-certified physiatrist at Axion Spine & Neurosurgery in Alpharetta in the Atlanta, Georgia metropolitan area. He is double-boarded in physical medicine and rehabilitation, as well as sports medicine. Dr. Mangrum earned his undergraduate degree in organismic and evolutionary biology from Harvard College in Cambridge, Massachusetts. He completed medical school at the University of Utah in Salt Lake City and finished medical training at the Mayo Clinic and the University of Utah. Drawn to the climate and culture of Atlanta, Dr. Mangrum now resides in Milton with his wife and four beautiful children.
Survey




















