PAINMEDICINE ACASE-BASED LEARNINC SERIES
The Knee
STEVEN D. WALDMAN
Elsevier
1600JohnF.KennedyBlvd. Ste1800 Philadelphia,PA19103-2899
PAINMEDICINE:ACASE-BASEDLEARNINGSERIES THEKNEE
Copyright © 2022byElsevier,Inc.Allrightsreserved
ISBN:978-0-323-76258-8
Allunnumberedfiguresare ©ShutterstockCh1#1385631854,Ch2#570884644,Ch3#1650374824, Ch4#542540116,Ch5#150366125,Ch6#1409196740,Ch7#124731106,Ch8#199824266, Ch9#576774043,Ch10#1431018935,Ch11#1176349708,Ch12#207716434,Ch13#1503719018, Ch14#1223884714,Ch15#422100022.
Nopartofthispublicationmaybereproducedortransmittedinanyformorbyanymeans, electronicormechanical,includingphotocopying,recording,oranyinformationstorageand retrievalsystem,withoutpermissioninwritingfromthepublisher.Detailsonhowtoseek permission,furtherinformationaboutthePublisher’spermissionspoliciesandourarrangements withorganizationssuchastheCopyrightClearanceCenterandtheCopyrightLicensingAgency, canbefoundatourwebsite: www.elsevier.com/permissions
Thisbookandtheindividualcontributionscontainedinitareprotectedundercopyrightbythe Publisher(otherthanasmaybenotedherein).
Notice
Practitionersandresearchersmustalwaysrelyontheirownexperienceandknowledgein evaluatingandusinganyinformation,methods,compoundsorexperimentsdescribedherein. Becauseofrapidadvancesinthemedicalsciences,inparticular,independentverificationof diagnosesanddrugdosagesshouldbemade.Tothefullestextentofthelaw,noresponsibility isassumedbyElsevier,authors,editorsorcontributorsforanyinjuryand/ordamageto personsorpropertyasamatterofproductsliability,negligenceorotherwise,orfromanyuse oroperationofanymethods,products,instructions,orideascontainedinthematerialherein.
LibraryofCongressControlNumber:2021936715
ExecutiveContentStrategist: MichaelHouston
ContentDevelopmentSpecialist: JeannineCarrado/LauraKlien
Director,ContentDevelopment: EllenWurm-Cutter
PublishingServicesManager: ShereenJameel
SeniorProjectManager: KarthikeyanMurthy
DesignDirection: AmyBuxton
PrintedinIndia.
Lastdigitistheprintnumber: 987654321
It’s Harder Than It Looks
MAKING THE CASE FOR CASE-BASED LEARNING
For sake of full disclosure, I was one of those guys. You know, the ones who wax poetic about how hard it is to teach our students how to do procedures. Let me tell you, teaching folks how to do epidurals on women in labor certainly takes its toll on the coronary arteries. It’ s true, I am amazing. . .I am great. . .I have nerves of steel. Yes, I could go on like this for hours. . .but you have heard it all before. But, it’ s again that time of year when our new students sit eagerly before us, full of hope and dreams. . .and that harsh reality comes slamming home. . .it is a lot harder to teach beginning medical students “doctoring” than it looks.
A few years ago, I was asked to teach first-year medical and physician assistant students how to take a history and perform a basic physical exam. In my mind I thought “this should be easy. . .no big deal” . I won ’t have to do much more than show up. After all, I was the guy who wrote that amazing book on physical diagnosis. After all, I had been teaching medical students, residents, and fellows how to do highly technical (and dangerous, I might add) interventional pain management procedures since right after the Civil War. Seriously, it was no big deal...I could do it in my sleep with one arm tied behind my back blah blah blah.
For those of you who have had the privilege of teaching “doctoring,” you already know what I am going to say next. It’s harder than it looks! Let me repeat this to disabuse any of you who, like me, didn’t get it the first time. It is harder than it looks! I only had to meet with my first-year medical and physician assistant students a couple of times to get it through my thick skull: It really is harder than it looks. In case you are wondering, the reason that our students look back at us with those blank, confused, bored, and ultimately dismissive looks is simple: They lack context. That’ s right, they lack the context to understand what we are talking about.
It’ s really that simple. . .or hard. . .depending on your point of view or stubbornness, as the case may be. To understand why context is king, you have to look only as far as something as basic as the Review of Systems. The Review of Systems is about as basic as it gets, yet why is it so perplexing to our students? Context. I guess it should come as no surprise to anyone that the student is completely lost when you talk about let’ s say the “constitutional” portion of the Review of Systems, without the context of what a specific constitutional finding, say a fever or chills, might mean to a patient who is suffering from the acute onset of headaches. If you tell the student that you need to ask about fever, chills, and the other “constitutional” stuff and you take it no further, you might as well be talking about the
InternationalSpaceStation.Justsaveyourbreath;itmakesabsolutelynosenseto yourstudents.Yes,theywanttoplease,sotheywillmemorizetheelementsofthe ReviewofSystems,butthatisaboutasfarasitgoes.Ontheotherhand,ifyoupresentthecaseofJannettePatton,a28-year-oldfirst-yearmedicalresidentwithafever andheadache,youcanseethelightsstarttocomeon.Bytheway,thisiswhat Jannettelookslike,andasyoucansee,Jannetteissickerthanadog.This,atitsmost basiclevel,iswhat Case-BasedLearning isallabout.
Iwouldliketotell youthat,smartguy thatIam,Iimmediatelysawthelight andbecameaconvert to Case-BasedLearning. Buttruthbetold,it wasCOVID-19that reallygotmethinkingabout Case-Based Learning.Beforethe COVID-19pandemic, Icouldjustdragthestudentsdowntothemed/surgwardsandwalkintoa patientroomandriff.Everyonewasawinner.Forthemostpart,thepatients lovedtoplayalongandthoughtitwascool.ThepatientandthebedsidewasallI neededtoprovidethecontextthatwasnecessarytoillustratewhatIwastrying toteach thewhyheadacheandfeverdon’tmixkindofstuff.HadCOVID-19 notrudelydisruptedmyabilitytoteachatthebedside,Isuspectthatyouwould notbereadingthis Preface,asIwouldnothavehadtowriteit.Withinaveryfew daysaftertheCOVID-19pandemichit,mydaysofbedsideteachingdisappeared,butmystudentsstillneededcontext.Thisgotmefocusedonhowto providethecontexttheyneeded.Theanswerwas,ofcourse, Case-BasedLearning. Whatstartedasadesiretoprovidecontext becauseitreallywas harderthanit looked ledmetobeginworkonthiseight-volume Case-BasedLearning textbookseries.Whatyouwillfindwithinthesevolumesareabunchoffun,real-life casesthathelpmakeeachpatientcomealiveforthestudent.Thesecasesprovide thecontextualteachingpointsthatmakeiteasyfortheteachertoexplainwhy, whenJannette’schiefcomplaintis, “MyheadiskillingmeandI’vegotafever,” itis abigdeal.
Havefun!
StevenD.Waldman,MD,JD
Spring2021
14 AnaliRojas A28-Year-OldYogaInstructorWithPain, Numbness,andaFootDrop188
15 MartinNash A21-Year-OldSprinterWithMedialCalfPainand Bruising204
Index 217
RoseWilliams A72-Year-OldFemaleWith RightKneePain
LEARNINGOBJECTIVES
• Learnthecommoncausesofkneepain.
• Developanunderstandingoftheuniqueanatomyofthekneejoint.
• Developanunderstandingofthecausesofarthritisoftheknee.
• Learntheclinicalpresentationofosteoarthritisoftheknee.
• Learnhowtousephysicalexaminationtoidentifypathologyofthekneejoint.
• Developanunderstandingofthetreatmentoptionsforosteoarthritisof thekneejoint.
• Learntheappropriatetestingoptionstohelpdiagnoseosteoarthritisof thekneejoint.
• Learntoidentifyredflagsinpatientswhopresentwithkneepain.
• Developanunderstandingoftheroleininterventionalpainmanagementinthe treatmentofkneepain.
122/74.Herhead,eyes,ears,nose,t hroat(HEENT)examwasnormal,as washercardiopulmonaryexamination.Herthyroidwasnormal.Her abdominalexaminationrevealedno abnormalmassororganomegaly. Therewasnocostovertebralangle(CVA)tenderness.Therewasnoperipheraledema.Herlowbackexaminationwasunremarkable.Ididarectal examandpelvic,whichwerebothnormal.Visualinspectionoftheknee revealednocutaneouslesionsorobviousherniaorotherabnormalmass. Theareaoverlyingtherightkneewaswarmtotouch.Palpationofthe rightkneerevealedmilddiffusetenderness,withnoobvioussynovitisor pointtenderness.Onballottementoftherightknee,therewasasuggestion ofmildeffusion.Therewasmildcre pitus,butIdidnotappreciateany poppingorcatching.Rangeofmotionwasdecreased,withpainexacerbatedwithactiveandpassiverangeofmotion.Theleftkneeexamination wasnormal,aswasexaminationofherothermajorjoints,otherthansome mildosteoarthritisinthefingers.Acarefulneurologicexaminationofthe upperandlowerextremitiesrevealedtherewasnoevidenceofperipheral orentrapmentneuropathy,andthedeeptendonreflexeswerenormal.
KeyClinicalPoints—What’sImportantandWhat’sNot
THEHISTORY
’ Nohistoryofacutekneetrauma
’ Nofeverorchills
’ Gradualonsetofrightkneepainoverthelastseveralweekswith exacerbationofpainwithkneeuse
’ Gratingsensationintherightknee
’ Sleepdisturbance
’ Difficultywalkingupstairsduetopain
’ Painonkneeling
THEPHYSICALEXAMINATION
’ Thepatientisafebrile
’ Normalvisualinspectionofknee
’ Palpationofrightkneerevealsdiffusetenderness
’ Nopointtenderness
’ Mildwarmthofrightknee
’ Crepitusandpainwithrangeofmotion
’ Noevidenceofinfection
’ Suggestionofamildeffusion
’ Noactivesynovitis
OTHERFINDINGSOFNOTE
’ NormalBP
’ NormalHEENTexamination
’ Normalcardiovascularexamination
’ Normalpulmonaryexamination
’ Normalabdominalexamination
’ Noperipheraledema
’ Nogroinmassoringuinalhernia
’ NoCVAtenderness
’ Normalpelvicexam
’ Normalrectalexam
’ Normalupperextremityneurologicexamination,motorandsensory examination
’ Examinationofjointsotherthantherightkneewerenormalotherthan somemildosteoarthritisofthehands
WhatTestsWouldYouLiketoOrder?
Thefollowingtestswereordered:
’ Plainradiographoftherightknee
TESTRESULTS
Theplainradiographsoftherightkneerevealedsignificantjointspacenarrowingandosteophyteformationconsistentwithsevereosteoarthritis(Fig.1.1).
CLINICALCORRELATION—PUTTINGITALLTOGETHER
Whatisthediagnosis?
’ Osteoarthritisoftherightkneejoint
TheScienceBehindtheDiagnosis
ANATOMYOFTHEKNEEJOINTS
Althoughbothcliniciansandlaypeoplethinkofthekneejointasasingle joint,fromtheviewpointofundersta ndingthefunctionalanatomy,itis morehelpfultothinkofthekneeastwose paratebutinterrelatedjoints:the femoral-tibialjointandthefemoral-patellarjoint( Fig.1.2 ).Thetwojoints shareacommonsynovialcavity,anddysfunctionofonejointcaneasily affectthefunctionoftheother.
Fig.1.1 Osteoarthritisoftheknee.AnteroposteriorstandingkneeX-raywithjointspaceloss,especiallyinthemedialcompartmentandosteophytesbilaterally.(FromVincentTL,WattFE.Osteoarthritis. Medicine.2018:46[3]:187 195[Fig.3C].)
Thefemoral-tibialjointismadeupofthearticulationofthefemurandthe tibia.Interposedbetweenthetwobonesaretwofibrocartilaginousstructures knownasthemedialandlateralmenisci(Fig.1.3).Themeniscihelptransmitthe forcesplacedonthefemuracrossthejointontothetibia.Themeniscihavethe propertyofplasticityinthattheyareabletochangetheirshapeinresponseto thevariableforcesplacedonthejointthroughitscomplexrangeofmotion.The medialandlateralmenisciarerelativelyavascularandreceivethebulkoftheir nourishmentfromthesynovialfluid,whichmeansthatthereislittlepotential forhealingwhentheseimportantstructuresaretraumatized.
Theprimaryfunctionofthefemoral-patellarjointistousethepatella,which isalargesesamoidboneembeddedinthequadricepstendon,toimprovethe mechanicaladvantageofthequadricepsmuscle.Themedialandlateralarticular surfacesofthesesamoidinterfacewiththearticulargrooveofthefemur (Fig.1.4).Inextension,onlythesuperiorpoleofthepatellaisincontactwiththe articularsurfaceofthefemur.Asthekneeflexes,thepatellaisdrawnsuperiorly intothetrochleargrooveofthefemur.
CLINICALPRESENTATIONOFARTHRITISOFTHEKNEEJOINT
Arthritisofthekneeisacommonpainful condition.Thekneejointissusceptibletothedevelopmentofarthritisfromavarietyofconditionsthathave theabilitytodamagethejointcartilage.Osteoarthritisisthemostcommon formofarthritisthatresultsinkneepain;rheumatoidarthritisand
Vastus medialis m
Vastus lateralis m
Iliotibial tract
Lat sup genicular a
Iliotibial tract
Popliteus t
Ant cruciate lig
Lat meniscus
Peroneus longus and extensor digitorum longus mm
Ant tibial recurrent a
Med sup genicular a
Adductor magnus t
Femur
Post cruciate lig
Med meniscus
Tibial collateral lig
Sartorius t
Tibia
Med inf genicular a
Gracilis and semitendinosus tt
Fig.1.3 Coronalviewoftheknee. a,artery; t,tendon; n,nerve; lig,ligament; m,muscle; tt,tendons. (FromKangHS,AhnJM,ResnickD. MRIoftheExtremities.Philadelphia:Saunders;2002:301.)
Thepainisconstantandischaracte rizedasachinginnature;itmay interferewithsleep.Somepatientscomplainofagratingorpoppingsensationwithuseofthejoint,andcrepitusmaybepresentonphysical examination.
Inadditiontopain,patientsoftenexperienceagradualreductioninfunctional abilitybecauseofdecreasingkneerangeofmotion,makingsimpleeveryday taskssuchaswalking,climbingstairs,andgettinginandoutofacarquitedifficult(Fig.1.5).Withcontinueddisuse,musclewastingmayoccur,andafrozen kneeduetoadhesivecapsulitismaydevelop.
Tibial n
Rectus femoris m
Prefemoral fat body
Quadriceps t
Suprapatellar bursa
Suprapatellar fat body
Patella
Transverse lig
Lat inf genicular a Infrapatellar fat body
Patellar lig
Tibia
Lat sup genicular a
Tibial n
Femur
Oblique popliteal lig and joint capsule
Ant cruciate lig
Post meniscofemoral lig of Wrisberg
Post cruciate lig
Gastrocnemius, lat head, and plantaris mm
Popliteal v and tibial n
Popliteus m
Soleus m
Fig.1.4 Sagittalviewoftheknee.(FromKangHS,AhnJM,ResnickD. MRIofthe Extremities.Philadelphia:Saunders;2002:341.)
TESTING
Plainradiographyisindicatedinall patientswhopresentwithkneepain (Fig.1.6).Basedonthepatient’sclinicalpresentation,additionaltestingmay bewarranted,includingacompletebloodcount,erythrocytesedimentation rate,andantinuclearantibodytesting.Magneticresonance(MRI)andultrasoundimagingofthekneeisindicated ifinternalderangement,aseptic necrosis,oranoccultmassortumoriss uspected,orifthediagnosisisin question( Figs.1.7 and 1.8).
Arthritis of the knee joint
Fig.1.5 Patientssufferingfromosteoarthritisofthekneeoftenexperienceagradualreductioninfunctionalabilitybecauseofdecreasingkneerangeofmotion,makingsimpleeverydaytaskssuchaswalking,climbingstairs,andgettinginandoutofacarquitedifficult.(FromWaldmanSD. Atlasof CommonPainSyndromes.4thed.Philadelphia:Elsevier;2019:Fig.105.1.)
Fig.1.6 X-raysofosteoarthritisoftheknee:(A)grade0normal,(B)grade1lateralfemoralosteophyte,(C)grade2lateralfemoralosteophyte,and(D)grade3lateralfemoralosteophyte.(From AltmanRD,GoldGE.Atlasofindividualradiographicfeaturesinosteoarthritis,revised. Osteoarthr Cart.2007:15[1]:A1 A56[Fig.22].)
Fig.1.8 Ultrasoundimageofthekneedemonstratingatornmedialmeniscus.(CourtesySteven Waldman,MD.)
TABLE1.1 ’ CausesofKneePainandDysfunction
Arthritis
• Osteoarthritis
• Rheumatoid
• Gout
• Pseudogout
• Reactivearthritis
• Septicarthritis
Trauma
• Fractures
• Meniscalinjuries
• Tendinitis
• Bursitis
• Ligamentousinjuries
MechanicalAbnormalities
• Jointmouse
• Alteredgaitduetohip,foot,orankleproblems
• Iliotibialbandsyndrome
• Patellarabnormalities(e.g.,patellaalta,bipartitepatella)
OtherCauses
• Avascularnecrosis
• Foreign-bodysynovitis
• Charcotjoint
• Neurofibromatosis
• Malignancy
• Pseudorheumatism
cyclooxygenase-2inhibitorsandphysicaltherapy.Thelocalapplicationofheat andcoldmayalsobebeneficial.Forpatientswhodonotrespondtothese treatmentmodalities,intraarticularinjectionoflocalanestheticandsteroidisa reasonablenextstep.
Forintraarticularinjectionoftheknee,thepatientisplacedinthesupinepositionwitharolledblanketunderneaththekneetogentlyflexthejoint.Theskin overlyingthemedialjointispreparedwithantisepticsolution.Asterilesyringe containing5mLof0.25%preservative-freebupivacaineand40mgmethylprednisoloneisattachedtoa1.5-inch,25-gaugeneedleusingstrictaseptictechnique. Thejointspaceisidentified,andtheclinicianplacesathumbonthelateralmarginofthepatellaandpushesitmedially.Atapointinthemiddleofthemedial edgeofthepatella,theneedleisinsertedbetweenthepatellaandthefemoral condyles.Theneedleisthencarefullyadvancedthroughtheskinandsubcutaneoustissuesthroughthejointcapsuleandintothejoint(Fig.1.9).Ifboneis encountered,theneedleiswithdrawnintothesubcutaneoustissuesandredirectedsuperiorly.Afterthejointspaceisentered,thecontentsofthesyringeare gentlyinjected.Thereshouldbelittleresistancetoinjection.Ifresistanceis encountered,theneedleisprobablyinaligamentortendonandshouldbe advancedslightlyintothejointspaceuntiltheinjectioncanproceedwithoutsignificantresistance.Theneedleisthenremoved,andasterilepressuredressing andicepackareappliedtotheinjectionsite.Clinicalstudiessuggestthat
Femur Patella
Inflamed and arthritic joint
Fig1.9 Intraarticularinjectionoftheknee.(FromWaldmanSD. AtlasofPainManagementInjection Techniques.4thed.StLouis:Elsevier;2017:Fig.132-4.)
viscosupplementationandtheinjectionofplatelet-richplasmamayalsoprovide symptomaticreliefofkneepainsecondarytoosteoarthritis.Theuseofultrasoundguidancemayimprovetheaccuracyofneedleplacementintotheintraarticularspace(Fig.1.10).
Physicalmodalities,includinglocalheatandgentlerangeofmotionexercises, shouldbeintroducedseveraldaysafterthepatientundergoesinjection. Vigorousexercisesshouldbeavoidedbecausetheywillexacerbatepatient symptoms.
HIGH-YIELDTAKEAWAYS
• Thepatientisafebrile,makinganacuteinfectiousetiology(e.g.,septicarthritis) unlikely.
• Thepatient’ssymptomatologyisnottheresultofacutetraumabutmorelikely theresultofrepetitivemicrotraumathathasdamagedthejointovertime.
• Thepatient’spainisdiffuseratherthanhighlylocalized,aswouldbethecase withapathologicprocesssuchasprepatellarbursitis.
• Thepatient’ssymptomsareunilateralandinvolveonlyonejoint,whichismore suggestiveofalocalprocessthanasystemicpolyarthropathy.
• Sleepdisturbanceiscommonandmustbeaddressedconcurrentlywiththe patient’spainsymptomatology.
• Plainradiographswillprovidehigh-yieldinformationregardingthebony contentsofthejoint,butultrasoundimagingandMRIwillbemoreuseful inidentifyingsofttissuepathology.
Fig.1.10 Ultrasound-guidedinjectionoftheknee.(CourtesyStevenWaldman,MD.)
BrendanBeckham
A32-Year-OldMaleWithAcute LeftMedialKneePainFollowing aSoccerInjury
LEARNINGOBJECTIVES
• Learnthecommoncausesofkneepain.
• Developanunderstandingoftheuniqueanatomyofthekneejoint.
• Developanunderstandingoftheanatomyofthemedialmeniscus.
• Understandthefunctionofthemusclesofthemedialmeniscus.
• Developanunderstandingofthecausesofmedialmeniscustear.
• Developanunderstandingofthevarioustypesofmedialmeniscusinjury.
• Learntheclinicalpresentationofmedialmeniscustear.
• Learnhowtoexaminetheknee.
• Learnhowtousephysicalexaminationtoidentifypathologyofthemedial meniscus.
• Developanunderstandingofthetreatmentoptionsformedialmeniscustear.
BrendanBeckham
“CallmeBrendan, ” mynew patientsaidasIintroducedmyself. Brendanwasa28-year-oldprofessionalsoccerplayerwithourlocal farmteamwiththechiefcomplaint of, “ Iblewoutmyrightknee.” Brendanstatedthataboutaweek ago,hewastakingtheballdown tothegoalandpivotedtoavoida defendertomoveinforthescore whenhefeltlike “something poppedinmyleftknee.Doc,itreallyhurt,butIwentaheadandmadethe kick,scored,andthenheadedofftothelockerroomtoicemyknee.Itook aquickshower,buttheinsideofmykneewaskillingme.Ididn ’timmediatelysayanythingtoanybodybecause,youknow,atmyage ... ” ashis voicedjusttrailedoff. “ButIfiguredwithice,Tylenol,andacoupleof daysoff,Iwouldberightasrain.ButhereIam, ” hesaidwithaweak smile.Iaskedifhehadeverhadanythinglikethisbeforeandheshookhis headandsaid, “ Justtheusualachesandpains.Inevermissagame.Ilove playingsoccer.Ihopetoplayforalongtimeyet,soIneedyoutogiveme ashotorsomething.Noharddrugs,becausetheleagueisalwaysdoing drugscreens. ”
ItoldBrendanIwoulddoallIcouldforhim,andthefirststepwasto figureoutexactlywhatwasgoingonwithhisknee.IaskedBrendanhowhewas sleepingandhesaid, “Prettywell,buteverytimeIrollontomyleftknee,Iwake up. ” Brendandeniedanyfeverorchills.
Onphysicalexamination,Brendanwas afebrile.Hisrespirationswere16 andhispulsewas64andregular.Hisbloodpressurewas118/82.Hishead, eyes,ears,nose,throat(HEENT)examwasnormal,aswashiscardiopulmonaryexamination.Histhyroidwasnormal.Hisabdominalexamination revealednoabnormalmassororgano megaly.TherewasaleftlowerquadrantscarthatBrendansaidwasfromanappendectomywhenhewasakid. Therewasnocostovertebralangle(CVA)tenderness.Therewasnoperipheraledema.Hislowbackexaminationw asunremarkable.Visualinspection oftheleftkneerevealedasmallareaofecchymosisoverthemedialjoint space.IaskedBrendanaboutitandhesaid, “Oh,that ’ snothing,justalittle bruisingfromtheacupuncture.” Iaskediftheacupuncturehelpedandhe gavemeawrysmileandsaidifitdid,hewouldbeatpracticeratherthan sittingonmyexamtable.
Fig.2.1 Elicitingthebulgesignforsmallkneejointeffusions.(FromWaldmanSD. PhysicalDiagnosis ofPain:AnAtlasofSignsandSymptoms.3rded.StLouis:Elsevier;2016:Fig.202-1.)
IaskedBrendantopointwithonefingertoshowmewhereithurtthe most,andhepointedtotheareaoverthemedialjointspace.Hesaid, “ Doc,itfeelslikeit ’ sdownintheknee;notontheoutside. ” Hevolunteered, “ Sometimesafterasquat,whenIgetup,itfeelslikemykneeis goingtocatchorlockup. ” Igentlyflexedandextendedthekneeandhe saidthatreproducedthepain.Theleftkneewasalittlewarmmediallybut didnotappeartobeinfected.IfeltlikeBrendanhadalargejointeffusion, soIperformedthebulgesigntestforkneejointeffusions,whichwaspositive,aswashisballottementtest( Figs.2.1 2.3).BrendanexhibitedapositiveMcMurraytestaswellasapositivesquattest( Figs.2.4 and 2.5).
Brendan ’ srightkneeexaminationwasnormal,aswasexaminationofhis othermajorjoints.Acarefulneurolo gicexaminationoftheupperandlower extremitiesrevealedtherewasnoevi denceofperipheralorentrapment neuropathy,andthedeeptendonreflexeswerenormal.ItoldBrendanI wasprettysureIknewwhatwasgoingonandweweregoingtogetsome teststoconfirmit.
Fig.2.4 TheMcMurraytestfortornmeniscus.(FromWaldmanSD. PhysicalDiagnosisofPain:An AtlasofSignsandSymptoms.3rded.StLouis:Elsevier;2016:Fig.219-1.)
KeyClinicalPoints
THEHISTORY
’ Ahistoryofsuddenonsetleftmedialjointpainfollowingasoccerinjury
’ Ahistoryofasuddenpopinthekneeatthetimeoftheacuteinjury
’ Ahistoryofcontinuedpaininspiteofconservativetherapy,including acupuncture
’ Nohistoryofprevioussignificantkneepain
’ Nofeverorchills
’ Sleepdisturbance
THEPHYSICALEXAMINATION
’ Thepatientisafebrile
’ Palpationofleftkneerevealstendernessoverthemedialjointspace
’ Aneffusionoftheleftkneejointasindicatedbyapositivebulgeand ballottementtest
Fig.2.5 Thesquattestfortornmeniscus.(A)Thesquattestformeniscaltear.Thepatientisasked firsttoperformafullsquatwiththefeetandlegsfullyexternallyrotated.(B)Thesquattestformeniscal tear.Thepatientisthenaskedtoperformafullsquatwiththefeetandlegsfullyinternallyrotated. (FromWaldmanSD. PhysicalDiagnosisofPain:AnAtlasofSignsandSymptoms.3rded.StLouis: Elsevier;2016[Figs.221-3and221-4].)
’ Thepresenceofmildecchymosisoverthemedialrightkneejointspace
’ Painonflexionandextensionoftheleftknee
’ ApositivedropMcMurraytest
’ Apositivesquattest
OTHERFINDINGSOFNOTE
’ NormalHEENTexamination
’ Normalcardiovascularexamination
’ Normalpulmonaryexamination
’ Normalabdominalexaminationwithawell-healedappendectomyscar noted
’ Noperipheraledema
’ Normalupperextremityneurologicexamination,motorandsensory examination
’ Examinationofotherjointswasnormal
WhatTestsWouldYouLiketoOrder?
Thefollowingtestswereordered:
’ Plainradiographsoftheleftknee
’ Magneticresonanceimaging(MRI)oftheleftknee
’ Ultrasoundoftheleftkneewithspecialattentiontothemedialmeniscus
TESTRESULTS
Theplainradiographsoftheleftkneerevealednoevidenceofbonyabnormality orfracture,butshowedpatellartiltingduetothelargeeffusionbehindand aroundthepatellartendon(Fig.2.6).TheMRIrevealedabuckethandletearof themedialmeniscus(Fig.2.7).Theultrasoundoftheleftmedialmeniscusreveals complextearingofthemeniscus(Fig.2.8).
ClinicalCorrelation—PuttingItAllTogether
Whatisthediagnosis?
’ Buckethandletearofthemedialmeniscus
TheScienceBehindtheDiagnosis ANATOMYOFTHEMEDIALMENISCUS
Themedialmeniscusisacrescent-shapedfibrocartilaginousbandthatspans themedialkneejoint(Fig.2.9).Thefunctionofthemedialmeniscusisto providechondroprotectionbyreducingpeakcontactforcesandfrictionbetween thefemurandproximaltibia(Fig.2.10).Themedialmensicusisattachedtothe tibiabythecoronaryligaments,whicharealsosubjecttotraumaticinjury (Fig.2.11).
Fig.2.7 Magneticresonanceimaging(MRI)revealsabuckethandletearofthemedialmeniscus.(A) TheparasagittalprotondensityMRIindicatesasmallmeniscus (whitearrows).(B)Thesagittalproton densityMRIthroughtheleveloftheintercondylarnotchshowsadisplacedbuckethandlefragmentof themedialmeniscus (brokenwhitearrows) lyinginferiorandanteriortotheposteriorcollateralligament.(C)Full-thicknesstearofthesupraspinatustendonaswellas(D)morechronictendinopathyof theinfraspinatustendonasevidencedbythickeningandhighsignalintensityofthetendon.(From WaldmanSD,CampbellRSD. ImagingofPain.Philadelphia:Saunders;2011:Fig.146.2A,B.)
section,whichisapproximately3.5cminlengthfromanteriortoposterior(see Fig.2.10).Itiswiderposteriorlyandisattachedtothetibiabythecoronaryligaments,whicharealsosusceptibletotrauma,asarethefibrousconnectionsfrom thejointcapsuleandmedialcollateralligament.
A B
C D
Fig.2.8 Longitudinalultrasoundimagerevealingcomplextearingofthemedialmeniscus.(Courtesy StevenWaldman,MD.)
Vastus lateralis m.
Lat. sup. genicular a.
medialis m.
Med. sup. genicular a.
Infrapatellar fat body
Iliotibial tract
Transverse lig.
Lat. meniscus, ant. horn
Iliotibial tract
Extensor digitorum longus m.
Med. meniscus, ant. horn
Sartorius, gracilis and semitendinosus tt.
Med. inf. genicular a.
Fig.2.9 Themedialmeniscusissubjecttodegenerativechangesaswellastearingsecondaryto acutetrauma. m,muscle; a,artery; ant,anterior; tt,tendons.(FromKangHS,AhnJM,ResnickD. MRIoftheExtremities:AnAnatomicAtlas.2nded.Philadelphia:Saunders;2002:305.)
Femur
Tibia
Vastus
Fig.2.10 Longitudinalultrasoundimagedemonstratingthetriangularmedialmeniscusnestled betweenthemedialbordersofthefemurandtibia.(CourtesyStevenWaldman,MD.)
Articular portion of femur
Medial portion of coronary ligament
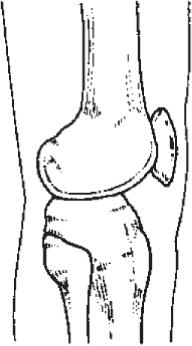
Fig.2.11 Themedialmensicusisattachedtothetibiabythecoronaryligaments,whicharealsosubjecttotraumaticinjury,whichcanresultinmedialkneepain.(FromWaldmanSD. AtlasofUncommon PainSyndromes.3rded.Philadelphia:Saunders;2014:Fig.102-1.)
TABLE2.1 ’ FunctionsoftheMedialMeniscus
• Loadbearing
• Convertingthecompressiveforcestotensileforces
• Loaddistribution
• Stabilizationofthejoint
• Lubricationofthejoint
• Proprioception
Tibia
TABLE2.3 ’ MostCommonCausesofKneePain
LocalizedBonyor
JointSpace
Pathology
Fracture
Primarybonetumor
Primarysynovialtissuetumor
Jointinstability
Localizedarthritis
Osteophyte formation
Jointspaceinfection
Hemarthrosis
Villonodularsynovitis
Intraarticularforeign body
Osgood-Schlatter disease
Chronicdislocation ofthepatella
Patellofemoralpain syndrome
Patellaalta
Periarticular Pathology
Bursitis
Tendinitis
Adhesivecapsulitis
Jointinstability
Musclestrain
Musclesprain
Periarticularinfection notinvolving jointspace
Systemic Disease
Rheumatoid arthritis
Collagenvascular disease
Reitersyndrome
Gout
Othercrystal arthropathies
Charcotneuropathicarthritis
Sympathetically MediatedPain
Causalgia
Reflexsympathetic dystrophy
ReferredFrom OtherBody Areas
Lumbar plexopathy
Lumbar radiculopathy
Lumbar spondylosis
Fibromyalgia
Myofascialpain syndromes
Inguinalhernia
Entrapment neuropathies
Intrapelvictumors
Retroperitoneal tumors
FromWaldmanSD. PhysicalDiagnosisofPain:AnAtlasofSignsandSymptoms.3rded.StLouis: Elsevier;2016:Table201-1.
TESTING
PlainradiographsandMRIareindicat edinallpatientswhopresentwith kneepain,particularlyifinternalderangementoroccultmassortumoris suspected( Fig.2.13 ).Inaddition,MRIshouldbeperformedinallpatients withinjurytothemedialmeniscuswhofailtorespondtoconservative therapyorwhoexhibitjointinstabilityonclinicalexamination.Bonescan maybeusefultoidentifyoccultstressfracturesinvolvingthejoint,especiallyiftraumahasoccurred.Basedonthepatient ’ sclinicalpresentation, additionaltestingmaybewarranted ,includingacompletebloodcount, erythrocytesedimentationrate,an dantinuclearantibodytesting.
DIFFERENTIALDIAGNOSIS
Anyconditionaffectingthemedial compartmentofthekneejointmay mimicthepainofmedialmeniscaltear.Bursitis,arthritis,andentrapment neuropathiesmayalsoconfusethediagnosis,asmayprimarytumorsofthe kneeandspine.
Fig.2.13 (A C)Sagittalprotondensitymagneticresonanceimaging(MRI)demonstratingahorizontal tearofthemedialmeniscalbodywithananteriorhornfragmentdisplacedanteriortothemedialfemoralcondyle(A)andaposteriorhornfragmentdisplacedintotheintercondylarnotchadjacenttothe posteriorcruciateligament(B).BothdisplacedfragmentsweremissedonMRI.(C)Coronalshorttau inversionrecovery(STIR)MRIalsodemonstratingthedisplacedanteriorhornmeniscalfragmentmentionedin(A).Thisfragmentwaspalpabletothepatient,whobroughtittotheattentionofthesurgeon beforearthroscopy.(D,E)Arthroscopicimagesofthesamecasedemonstratingthehorizontaltearof themeniscalbodyandthedisplacedposteriorhorn(D)andanteriorhornfragments(E). (FromSampsonMJ,JacksonMP,MoranCJ,etal.ThreeteslaMRIforthediagnosisofmeniscaland anteriorcruciateligamentpathology:acomparisontoarthroscopicfindings. ClinRadiol.2008;63 [10]:1106 1111.)
TREATMENT
Initialtreatmentofthepainandfunctionaldisabilityassociatedwithinjuryto themedialcollateralligamentincludesacombinationofnonsteroidalantiinflammatorydrugsorcyclooxygenase-2inhibitorsandphysicaltherapy.Thelocal applicationofheatandcoldmayalsobebeneficial.Anyrepetitiveactivitythat exacerbatesthepatient’ssymptomsshouldbeavoided.Forpatientswhodonot respondtothesetreatmentmodalitiesanddonothavelesionsthatrequiresurgicalrepair,injectionwithlocalanestheticandsteroidisareasonablenextstep. Ultrasoundguidancewillincreasetheaccuracyofneedleplacement(Fig.2.14).
Physicalmodalities,includinglocalheatandgentlerangeofmotionexercises, shouldbeintroducedseveraldaysafterthepatientundergoesinjection. Vigorousexercisesshouldbeavoidedbecausetheywillexacerbatepatient symptoms.