







Medicalsocietieshavebeenaroundforcenturies,and theycontinuetoplayanimportantroleinthehealthcare industrytoday.Thesesocietiesprovideaplatformfor physicianstonetwork,shareknowledge,andlearnfrom eachother.Whiletherearemanydifferentmedical societiesatthenationalandinternationallevels,it's equallyimportantforphysicianstoconsiderjoiningtheir localmedicalsociety.Inthisarticle,we'llexplorewhya physicianshouldjointheirlocalmedicalsociety.
Oneoftheprimarybenefitsofjoiningalocalmedicalsocietyistheopportunitytonetworkwithotherphysicians andhealthcareprofessionalsinthearea.Thesesocietiesoftenhostevents,suchasconferences,seminars,and workshops,wherememberscanmeetandsharetheirexperiences.Networkingcanhelpphysiciansbuild relationshipswithcolleagues,whichcanleadtoreferrals,collaborations,andevenjobopportunities.Byjoininga localmedicalsociety,physicianscanestablishthemselvesasactivemembersofthehealthcarecommunityintheir area,whichcanenhancetheirreputationandcredibility.
Medicalknowledgeandpracticesareconstantlyevolving,andit'sessentialforphysicianstostayup-to-datewith thelatestdevelopmentsintheirfield.Localmedicalsocietiesoftenoffercontinuingeducationprograms,which provideopportunitiesforphysicianstolearnnewtechniques,technologies,andtreatments.Theseprogramscan helpphysiciansimprovetheirclinicalskillsandstayinformedaboutemergingtrendsintheirspecialty.Inaddition, continuingeducationcreditsareoftenrequiredforlicensureandboardcertification,sojoiningalocalmedical societycanhelpphysiciansfulfilltheserequirements.
Localmedicalsocietiesalsoplayanimportantroleinadvocatingforphysiciansandtheirpatients.Thesesocieties worktoinfluencehealthcarepolicyatthelocal,state,andnationallevels,advocatingforissuesthataffect physiciansandtheirpatients.Byjoiningalocalmedicalsociety,physicianscanhaveavoiceintheseadvocacy effortsandhelpshapehealthcarepolicyintheircommunity.Inaddition,localmedicalsocietiescanprovidea platformforphysicianstoadvocateforissuesthatareimportanttothem,suchasaccesstocare,patientsafety,and medicalliabilityreform.
Localmedicalsocietiesalsoofferopportunitiesforphysicianstodeveloptheirleadershipskills.Manysocieties haveleadershippositions,suchascommitteechairs,boardmembers,andofficers,whichprovideopportunitiesfor physicianstotakeonleadershiprolesandmakeadifferenceintheircommunity.Servingina leadershiprolecanhelpphysiciansbuildtheirprofessionalnetwork,enhancetheircommunicationskills,and developtheirstrategicthinkingabilities.
Finally,joiningalocalmedicalsocietycanprovidephysicianswithasenseofcamaraderieandsupport. Physicianscanoftenfeelisolatedintheirpractice,andjoiningamedicalsocietycanhelpthemconnect withlike-mindedindividualswhosharetheirpassionformedicine.Thesesocietiescanprovideaforum forphysicianstodiscusschallengestheyarefacing,shareexperiences,andprovidesupporttoone another.
Inconclusion,joiningalocalmedicalsocietycanprovidephysicianswithnumerousbenefits,including networkingopportunities,continuingeducation,advocacyandpolicyinfluence,leadershipopportunities, andcamaraderieandsupport.Byjoiningalocalmedicalsociety,physicianscanenhancetheir professionaldevelopmentandmakeapositiveimpactontheircommunity.

Warmly,
J. Richard Rhodes, MDAt night, emergency departments across the country are filled with persons suffering the adverse effects of drug abuse or actively experiencing an overdose. Unfortunately, these patients have become little more than routine, especially in America’s urban healthcare facilities.According to the Centers for Disease Control, in 2020 alone, more than 93,000 individuals died from drug overdoses—an increase of over 30% from the prior year. Three-quarters of these deaths were due to opioid overdose, rather than from prescription medicationsoralcohol.Itisspeculatedthatthis increase is an effect of the isolation and stress that many endured throughout the COVID-19 pandemic. However, this figure serves to highlightanequallygrimtruth:theresourcesto treat substance abuse disorder patients are simply not there. Because of this paucity, preventable deaths from a treatable disease take the lives of tens of thousands of Americanseachyear.
During the year and a half that Joseph worked in an emergency department, he saw many complex patients, but there was one who particularly affected him. Upon arrival at the ER one day, Joseph came face-to-face with a patient on the brink of death. This young woman was progressing through an overdose on opioids before his eyes, with her chest remaining frozen still and the color drained fromherface.
lifesaving power of Narcan.As the following hours ticked by, the young woman whose death he had nearly witnessed slowly recovered and was back on herfeetbeforethedaywasover.
Months later, and without another visit from this patient, it was discovered that she was homeless. Despite her trying circumstances, she had sought rehabilitation and, with time, was able to overcome her addiction. Joseph’s account provides just one tale among many as to why education about addiction and increasing the use and availability of Narcan is necessary if we are to provide substance use disorder patients the chance at life they deserve. Truly, this medication has the power to keep familieswhole,livesintact,andgravesempty.
Within minutes of his first visitation, this patient was given the lifesaving medication Narcan, and immediately regained consciousness and the ability to breathe. In this singledramaticepisode,Josephlearnedofthe
Through various social and medical measures, patients like this one could also overcome their addictiontoopioids.Onewaytohelpthosefighting addiction is to increase the availability of Narcan and to take a community-based approach to fight opioid addiction. A study in Pittsburgh performed by Dotson et. al (2018) implemented several social interventions in the interest of discovering which were most effective at reducing the mortality of opioid overdoses. The study found that increasing the distribution of Narcan in pharmacies and allowing it to be dispensed without a prescription, in conjunction with bystander training on recognizing the signs of opioid overdose and the use of Narcan, significantly reduced opioid overdose deaths. This model is both applicable and readily implemented in many other communities in this country and could serve as a model across the state of Florida. Emily and Joseph are active in several student organizations that are working toward expanding the availability of Naloxone with the hope to save numerous lives across the state of Florida.
Paul M. Graham, M.D.According to the American Cancer Society, skin cancer is by far the most common type of cancer worldwide. Non-melanoma skin cancer accounts for approximately 3million cases in the United States eachyear withtheincidence continuing toclimb. Approximately1out ofevery 3cancers diagnosed worldwideisaskincancer.Additionally,1outofevery5Americanswill develop a skin cancer during their lifetime. The two most commontypes of non-melanoma skin caner arebasal cell carcinoma (BCC)andsquamous cell carcinoma (SCC).Basal cell carcinomaaccounts for approximately 80%of all non-melanoma skin cancer diagnoses. Chronic sun exposure is the single most important cause of all forms of skin cancer with damage oftenoccurring during childhood and adolescence years in those who practice poor sun protection habits.
Basal cell carcinoma is the most common type of skin cancer worldwide, occurring primarilyin fair-skinned individuals with a history of sun exposure. Risk factors include numerous blistering sunburns, immunosuppression, family history of BCC, and a history of radiation exposure. Basal cell carcinoma develops from cells contained withinthe bottom layer of the epidermis called the basal layer. Fortunately, theyare often slow-growing with a very lowrate of cancer cell spread (metastasis) outside the primary site of occurrence. It is very importantto have all BCCs treated to preventlocal surroundingskindestructionifleftuntreated.
Squamous cell carcinoma (SCC) isthesecond most common form of skin cancer worldwide.The majority of SCCs develop in individualswith a history of chronicsun exposure. The closer to the equator one lives, the more likely that individual willdevelop SCC. The immune system also plays an important role in the development of SCC. Those that are immunosuppressed or on immunosuppressive medication have a significantly higher risk of developing SCCs. Certain high-risk types of thehuman papillomavirus (HPV) may also play a role in SCC development. This type of skin cancer develops from cells that make up the bulkof the epidermis. Squamous cell carcinomahasaslightlyhigherriskduetoitsabilitytospreadintobloodvesselsandnerves.Itisforthisreasonwhy theyshouldbeproperlytreatedearlyon.

Numerous treatment options exist for these non-melanoma skin cancers, including the use of topical immune system modifyingmedications (5-flurouracil, imiquimod, ingenol mebutate), cryotherapy (freezing), electrodessication and curettage(“scraping and burning”), surgical excision, and Mohs micrographic surgery. After beingdiagnosed with a non-melanoma skin cancer, your physician will determine the besttreatment option based on the lesion size, type, location, and aggressiveness of the skin cancer. Some skin cancers have small “roots” that may extend deeper in the skin, beyond what we can see on the biopsy. Intheseinstances,surgicalinterventionisneededtocompletelyremovethe skincancer.



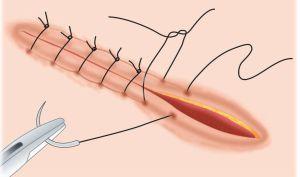
Mohs micrographic surgery provides a highly specialized and effective treatment option in patients with qualifying skincancers.Thisprocedurehasa97-99%curerate,which is superior to manycancer treatments in medicine. Mohs micrographic surgery was developed in 1938 by Dr. Frederick Mohs, a surgery professor at the University of Wisconsin. With this specialized procedure, the skin cancer is conservatively removed while simultaneouslyattempting to preservenormal skin. The removed portion of theskinis then carefully mapped, color-coded, and prepared for examination under the microscope, which all takes place withinthesameday.
The Mohs surgeon will meticulously examinethe tissue specimen and determine if any residual skin cancer is present. If residual tumor is found, the Mohs surgeon will only go back to that specific location to remove another small portion of tissue. One of the most important aspects of Mohs microscopic surgery is the ability to examine approximately100%of the skin margins under the microscope, ensuring that all of theskin cancer is completely removed prior to closingthesurgicalwound.



In contrast, a conventionalsurgical excision requiresseveral days for both tissue processing and microscopic examinationby a trained dermatopathologist. During this process, only approximately 1%of the skin margins are examined. This small percentage of examined skinmay contribute to a higher rate of recurrence if adequate surgical margins are not taken at the time of the surgery. In the event that more skin cancer cells are found in the examined skin,thesurgeonwillthereforehavetoperformasecondsurgicalexcisiontocompletelyremovetheresidualtumor.
∙ Largeskincancersonthehead andneck
∙ Skincancersinareaswhere preservationofnormalskinis vital
∙ Face,scalp,neck,nose, ear,eyelids,lips,hands, andgenitalia
∙ Sitesofhightumorrecurrence andriskoftumorspread
∙ Recurrentskincancers
∙ Aggressiveskincancers
Mohs micrographic surgery involves a series of stages consisting of the surgical excision followed by immediate microscopic examination of the tissue. TheMohs surgeon is focusedon removingthe least amount of tissue, while still providing adequate surgical margins to completely removethe skin cancer. Initially, it is not possible to know the final sizeof the surgical wound. This is often dependent on the number of stages that are required to completely remove the skin cancer cells. For reference,approximately50%ofallMohsmicrographicsurgery
cases require at least 2 stages for complete skin cancer clearance.After all theskin cancer cells are removed, the Mohs surgeon will surgically close the wound and the procedure will becomplete. Some wounds may be too large for simple closure and willrequire a skin graftor flap. In this case, the Mohs surgeon will design a closure that willpreserve the skin’s function and movement, while reducing the appearance of the scar. Stay tunedforafuturearticleonskingraftsandflapsusedinwoundclosure.
FollowingMohs micrographic surgery, it is recommended to minimize strenuous activity to reduce tension on the wound and decrease the risk of bleeding from blood pressure elevation. Pain is usually minimal butTylenol may be taken for discomfort. Suture removal time canvary depending on the location of the surgical wound,ranging from 5-14 days. Keep in mind that it often takes 12months for the surgical wound to regain similar strength of the surrounding skin. Surgical site redness may take up to 6 weeks to fade.The appearance of the scarwillfade over time, but incasesof elevated (hypertrophic or keloidal)scars, steroid injections may be used to assist inflattening. Various options exist for the treatment of noticeable scars including resurfacing lasersandmicroneedlingifthecosmeticresultisunacceptable.
AdvantagesofMohsMicrographicSurgery
∙ Highestcurerateofalltreatmentproceduresforskin cancer
∙ Preservationofnormalskin,allowingfora goodcosmeticoutcome,whilereducingthe appearanceofthesurgicalscar
∙ Lowassociatedriskwithlocalanesthesia(numbing)in anoutpatientsetting

References:
1. James,WilliamD,DirkM.Elston,TimothyG.Berger,andGeorgeC.Andrews. Andrews’Diseases of the Skin: Clinical Dermatology.London:Saunders/Elsevier,2011.Print.
2. http://www.cancer.net/cancer-types/skin-cancer-non-melanoma/statistics
3. http://www.dermatology.ucsf.edu/skincancer/mohs.aspx
4. http://www.who.int/uv/health/uv_health2/en/index1.html
5. http://www.skincancer.org/skin-cancer-information/mohs-surgery/mohs-overview
PhotoCredit:Onlinedermclinic.com,UCHospitals, Drugs.com,WebMD.com,Healthwise,OnSurg.com, MDpulp.com,FDA.govFlorida State University Department of Behavioral Sciences and Social Medicine
ACTS2 Project:African-AmericanAlzheimer’s CaregiverTraining and Support

TheACTS2 Project meets the needs of distressed caregivers of older adults with dementia.The program offers faith-integrated, skills-training and support over toll-free telephone to African-American dementia caregivers residing in Florida.ACTS2 also conducts a robust outreach effort to raise awareness about dementia through social media and community-based presentations (reaching over 7,000 annually), while also providing no-fee, telephone-based consultations and community referrals to caregivers and other stakeholders across Florida and the U.S.
Research has found manyAfrican-American adults do not participate in social service programs outside their culture and community. In addition, financial challenges and limited transportation options to get to appointments prevent caregivers from accessing help.To overcome these barriers, ACTS 2 has successfully trained 23African-American faith community workers (lay pastoral care facilitators) to deliver faith-integrated, skills-building and support sessions (a 12-part series ranging from relaxation training integrated with prayer and meditation to problem-solving through goal setting). Over 150 family caregivers have enrolled in the 12-sessionACTS2 program over the past 4 years. Caregivers reported:
significant improvement in health and emotional well-being
significant improvement in self-identified caregiving and self-care problems
· strong bonds between caregivers and lay facilitators who offer ongoing support
· very positive perceptions of the usefulness of the program
The U.S. Health Resources and ServicesAdministration Geriatric Workforce Enhancement Program, Florida State Primitive Baptist Convention, WinterFall Night of Giving, Joseph G. Markoly Foundation, Synovus Corporation, Florida State University College of Medicine, and private donors provide financial support to theACTS2 Project.


Ifyouweretoaskmeto lay in a recliner for four hourscoveredin a mountain of blankets and read my favorite book, I would probably say yes. Ofcourse!Whodoesnotwant4hoursto relax in a recliner? But there’s a catch isn’t there? This recliner comes with kidneyfailure,itrequiresvascularsurgery to create an arteriovenous access, it comes with a machine that filters your blood500ml/minforthreetofourhours. A recliner that makes you feel tired instead of rested and cold instead of warm. It is an extra trip you will have to make3timesaweek;youmayevenneed to cancel your lunch date and take time offwork.
I replayed our visit when I met you at thehospital.Walkinginyourroomatthe crack of dawn with my papers and some notes I scribbled down from your chart. I was in a rush to report to my attending nearlytrippingovermyselfineveryroom. However, I saved your place for last. A fewminutesgoby,asIstandoutsideyour door; I re read my bulleted notes. 58-year-old female with a history of chronic kidney disease, type 2 diabetes, and hypertension; hospital day three. Consult to nephrology should have been made earlier, if not for a possible congestive heart failure exacerbation. Yourcreatinehadjumpedfrom2to5and your electrolytes were less than ideal. Yourkidneyfunctionbarelyhangingonat 17.Iforcedmybestsmileandopenedthe door. “Hello Mrs. K! I am a medical student working with the nephrologist today. Can I talk with you about your kidneys?” I started. Excitement in your eyes I later learned you were a teacher. You came to the hospital with difficulty breathinganddizziness,andthiswasn’t
the first time. You recollected the struggles you had this past year in and out of the hospital for complications of both your heart and the diabetes. Unfortunately, this time it took a larger tollonyourkidneys.
Going back in the room my preceptor and I had only one plan: dialysis or no dialysis. She looked tired and weighed down, held up only by the hope of her husband and daughter next to her. This retired teacher almost took the words from us, she knew the options. She had been seeing nephrology for years and hoped her kidney function would eventually turn around, but always knew the inevitable. Her husband braced her fortheimpactofthenews.Mrs.KIthink weshouldtalkaboutdialysis andnowI can’tforgetyou.
ThedoctorandItoldyouweneededto prepare for dialysis. We explained the twotypes,andyouchosetherecliner.Are you scared for your arteriovenous fistula surgery? Are you worried this is the end stage of life and not just end stage renal disease? Unfortunately, I don’t need to ask,theanswersarewrittenonyourface, as your eyes gaze down and up to your family.Thelightinyourfacegoesdimand with it the hope in your heart. Did you wonder how this happened? Did you have any regrets? Can you handle the stigma of other’s opinions on your lifestyle choices? You have slowly declined for months now in and out of the hospital. It is difficult for me to imagine what you have experienced in your life with diabetes, heart failure and now kidney failure. I’ve never watched my blood sugar, had my legs swell twice the size, struggled to walk to the bathroom,orlaidinahospitalbedasyou have. I have nothing more to say but stand in the silence. The guilt inside me still lingers after we left you there. An interactionIhopetoneverforgetbecause I know you won’t. I changed your life by puttingyouinthat
chair; and I hope if it was me, I would havethecouragetositinthatrecliner. IwishIcouldmeetyouagain.Iwonderif you are doing better now. Was your central venous port put in with care? How was the first time in the recliner? Were you able to schedule for a fistula? But no that is where it ended. I have watched many times the delivery of devastatingnewsinmypatients,butuntil thisoneIhadneverdoneitmyself.Ithink we often forget our own mortality, even when we know the inevitable will happen. Many patients struggle with chronic disease; some carrying more mortalitythanothers.Inthemedicalfield we often see the disease process and stages, but never encompass the full picture of the chronic disease. The physical and emotional injuries our patientsmustendure.
Throughout my time in nephrology, I spent six weeks driving to multiple dialysis clinics. Sometimes 3 in one day. I spent countless hours with my preceptor flipping through papers analyzing and developing treatment plans and checking potassium and calcium over and over. I examined patients sitting in those recliners. I wonder is there anything we can do different to ease this burden for you?
Astaticvoiceon the intercom shouted, “We have a nursing home resident found unresponsive. Asystole on arrival. CPR started immediately. ETA 10 minutes.” Everyone around me quickly jumped into action to prepare. The afternoon had been slow in the emergency department, and the whole team was excited to jump into actiontoprepareforthearrivalofa
critical patient. It was my first day as a medical student in the emergency department. I had not yet figured out how I could best help the team in moments of chaos. Everyone seemed to havetheirnicheinthesescenarios,andit felt like I might disrupt the intricate flow ofthedepartmentwithanywrongturn.I tried my best to be present but also stay out of the way. However, it seemed like everywhere I turned to get out of the wayputmeinthewayofsomeoneelse.
With the blink of an eye, EMS was rollinginthebay.Ourpatientwasalready attached to the Lifeline Arm. Her eyes were wide open and fixed towards the ceiling. Her skin was leathery and gray. She had a single drop of blood falling fromthecornerofhermouth.Thethrust ofthecompressionswastheonlycatalyst causingthebloodtoslidedownherchin. Therestofherbodywascompletelystill. Shelookedalmostdoll-like.Itwashardto believe that she had been alive earlier thatday.
After an initial assessment, she was pronounced dead. Our team crowded around her lifeless body and took a moment of silence. With nearly no informationaboutthepatient,wehadto relyonherbodytotellherstory.Looking at her, I assumed she must have been olderthanmygrandparents.Herhairwas sparse and unkempt. She looked emaciated.
After further examination, the picture becamemoresinister.Itwasevidentthat shehadnotbeenabletocareforherself. HermusclesweresoatrophicthatIcould not imagine her body giving her the strength to move even the smallest of muscles. She looked like she had been sitting in the same soiled bottoms for days. Sores filled her backside. She had evidently been severely neglected at the place she entrusted to keep her safe. I was shocked by her condition. My preceptorexplainedtomethatitwasnot uncommon to have a patient brought in fromanursinghomeinsuchadeplorable condition. Much of the staff in nursing homes work tirelessly every week to treat patients as best they can. But budgetcutsandstaffingshortagescause
the patients to suffer the most. My perspective shifted. I could not be angry at the nursing home staff for failing this patient. The problem lies in the medical system at large. How can we as a society let our elders suffer in their time of greatest need? There is not a single person or group to blame. Our national medical system fails this vulnerable populationeveryday.
Ithinkofthispatientquiteoften.Inthe emergency department, we must report the ill-treatment of elderly adults in nursing homes. We hope the complaint findsitselfintherighthandsandpositive changes soon follow. But change is a long,slowprocess.Wehavethegreatest impact on our patients when we treat themwiththeutmostrespectwhenthey come through our doors. Even if our patienthaspassedbeforetheyarrive,we can help bring them peace. We can observe a moment of silence for the deceased. We can change their bedding, clean them up, and designate a quiet, dark room for their bodies to lie while waiting for family or the coroner to arrive. These small notions of respect quicklybecomeapartofourroutineona busy day in the emergency department. However, it is important to do our due diligence for our patients and resist the temptation to go through the motions without thinking of the deeper meaning of our actions. Even with a patient who wasmistreatedbywayofafaultysystem in the final years of their lives, we have an obligation to create a sense of peace and dignity for our patients as their lives cometoaclose.
While physicians in other specialties may not interact with patients in this samecapacity,itisstillvitaltoremember ourroleasaphysician.Wemaynotknow all of the hardships our patients face in their daily lives. However, we have an opportunity to create a safe haven for our patients by advocating for them and treatingthemwithrespect.


6 Weeks
by Alyssa FerlinKnock,knock.Afresh third-year medical student enters the room. It’s the last week of her first rotation. She dawns bright green OR scrubs and a white coat with pockets that are visibly packed with papers, a small book, multiple pens, a mini spiralized notebook, and granola bars,whicharenecessarysinceshenever knows when her next meal will be given the chaos that is general surgery. The room is tiny but pretty standard for a doctor’s office. There’s an exam table, 2 chairs, a rolling stool, a sink, and a desk connected to the wall. There are no computers in the room. She notices the rather pregnant woman sitting in the chairnexttothepatient.Theirhandsare interlocked.Beforeaskingaboutonsetof symptoms and where it hurts and what makesitbetterandwhatmakesitworse, she learns a lot about the couple. They are expecting not only their third child but their third girl. She is due 10 weeks from now. He works in security just down the road. He likes to fish. His youngest daughter likes to fish with him, but his oldest daughter wants nothing of the sort. They’ve been married for 10 years. They love their life. They smile big and they smile often. He’s here because ofasmalllumpinhisgroinarea.Ahernia perhaps? He casually mentions a history of melanoma. A 32-year-old with a historyofmelanoma?
He’s rather unconcerned about the history of melanoma. He was cleared a few years ago. He’s young, in-shape, and healthy. Life got busy so follow up with his oncologist wasn’t necessarily a priority.Butthislumppoppedup.It’snot painful; a little bothersome perhaps, and he just wanted to get it checked out. On their way out of the room, there are handshakes, head nods, smiles, laughs anda“takecare,youtwo.”
The third-year medical student goes about her life. The patients she thought aboutdailyandcaredfordeeplyoverthe
past several weeks, she’ll probably never seeagain.6weekshavepassedsinceshe met the kind couple in the tiny clinic room for a lump in the groin. Her white coat pockets aren’t quite as full these days, and the green surgery scrubs have beenexchangedforaslickblackscrubset more commonly worn by the internists. At the computers in the doctor’s lounge, she notices a familiar name on the patient list. She reads the notes in his chart like a story book. She’s stunned. Metastatic melanoma. Everywhere. A 32-year-oldguywhowashealthy6weeks agoandexpectinghisthirdchildisinthe intensive care unit. And he’s dying, quickly.
Thethird-yearmedicalstudentwalksup thestairs.Shethinks,whatdoyousayto someone who was seemingly fine 6 weeks ago but is now a frail, dying version of who they once were? The gameplan:getin,giveyourcondolences, chat if they want but keep it short if not, do your physical exam, and be on your way.ButwhentheICUdoorsopen,sheis met with his two young daughters being ushered down the hallway by a nurse. Sheismetwiththeshrillcryandscreams of a 36-week pregnant woman, who just 6weeksagowassmilingeartoearbutis now watching her husband take his last breaths, entirely helpless. 6 weeks ago, sheandherhusbandcrackedjokesabout the cost of the three weddings they’d be paying for 20 years down the road. 6 weeksago,therewereonlysmilesandno tears.6weeksago,lifewasnormal.But6 weekshavepassed.
The third-year medical student feels tears coming on. She is unsure what is allowedinamomentlikethis.Isitbadto cry?Isitokayforhertofeelpainlikethis for people she barely knows? How does she push these feelings aside so she can go see the next patient on her list with a smileonherface?
That night she drives home in silence. She weeps. She weeps for the young wife,whojust6weeksagodidn’thaveto plantogothroughchildbirthwithouther husband by her side. She weeps for the little girls, who just 6 weeks ago were playingoutsidewiththeirdadwithouta
careintheworld.Sheweepsforthebaby girl, who will never get to meet her dad. She weeps for the man, who is now at rest,whofoughtsohardtomakeittohis third daughter’s birth so he could hold herjustonce.
The third-year medical student learns that it is okay to feel pain for those she hascaredfor.Shelearnsthatmedicineis not always about curing and fixing people. And she learns, most importantly, that the heart of medicine lies not in the science, but in the human-to-human bond that is formed betweentwopeople.
Itwasthethirdweek of my neurology rotation around 10 in the morning when my attending and I werefinishingourmorningroundsinthe community hospital. As we filed through the long fluorescent-lit, vinyl-lined hallways, we were urgently paged for a consultation on a patient post-cardiac arrest. With haste, we logged into the nearest computer to learn more about ournewpatient.
On one hand, a thorough review of his chart revealed an average 54-year-old with an uneventful health history until beset by a heart attack early that morning. On another hand, the scans of his brain showed the extensive devastation that his brain endured while only being without oxygen for a few minutes.Hewasseverelybraindamaged, but I retained a small glimmer of hope that our physical exam would elicit something positive, some sign of consciousawareness.
Following my physicians lead, we marchedintothathospitalroomtofindit filled with this patient’s family. We learned about the events preceding this hospitalization and conducted our usual neurologic exam. As we proceeded throughit,wetestedhisvision,reflexes,
ability to follow commands, and tone of his muscle. Every stimulation was met with no response. My physician stood facing the family, offering a gentle and comfortinghand,andgavethenewsthat no one ever wishes to hear, that their lovedonewouldnotrecover.
We shared the images of his brain, and explained the disease process that their love one succumbed to in their current state. The physician assured the family that he did not suffer. He wasn’t brain dead, but brain damaged. In a sense, he neitherexistedwiththelivingnoramong thedead.Hisdamagewassevereenough that he would never awaken, but he could remain alive with the appropriate medicalcare.Hisfamilywasperplexedat this thought, to which my physician followedwithhispreferredanalogy,“The lightsareon,butnoone’shome.”Thisis a phrase that everyone easily understands,aphrasethatwillstickwith methroughtherestofmycareer.Asthe words left my attending’s mouth, I witnessed a unified epiphany spread amongst the family about their loved one’s condition and the realization that big decisions would have to be made in thedaystocome.
As I left that room with tears streaming down my face, I now saw life through a new lens. In all my prior brain injured patients, “The lights were on, and someone was home.” This phrase gave the family hope for recovery and that their loved one was still in their physical body. But this was the first time that it wasn’tthecase.Ireflectedonhowweall experience loss and share this as a core human experience. I have experienced loss myself and know of its pain and devastation.Thisexperienceofdelivering bad news showed me what it means to be human, and the heartbreak experienced by families receiving the worstnews.Wealwaystalkaboutputting the needs of our patients first, but what happens when our patients can’t make decisions for themselves? What about theneedsoftheirfamilies?
As a future physician, I will have many roles.Iwillwalkthelinebetweenlifeand death.Iwillbetheretosupport both my

best and worst times of their life. In medicine, we are always strapped for time, but I hope we all remember to support and listen to the families of our patients. They are the advocates of our patients, and deserve our time and respect to make informed decisions. There is something special about being heard, and we as physicians are sometimes a family’s only source of knowledge about what is happening. I hopewealllearnhowtoexplaincomplex diseases and tests in a way that anyone can understand. As physicians, we spend more than a decade developing our knowledgeandexpertise,anditwouldbe a waste to not have the capability to share this information in manageable pieces.
Ultimately, our patient was disconnected from life support, had his organs procured to give life to another, and was allowed to peacefully pass on. Despite their heartbreak, our patient’s family expressed their gratitude to my physician for the time he spent with them and the knowledge shared. They were able to process what had happened, understand their options, and make those hard decisions that no one ever wishes to make. They were able to givetheirlovedoneadeathwithdignity, andtheyfoundcomfortinthis.
If anything, my short four weeks in neurology, eight months into my clinical rotations,gavememoreappreciationfor life than any other experience in medical school. It gave me a more profound perspective on the fragile line between life and death, and furthermore, to take nothing for granted. My physician demonstrated extraordinary empathy and compassion to every one of his patients and their families, he took the time to have difficult conversations, and he endowed in me the understanding thatwordscanheal.

ItwasSpringof
I was in my junior year at UF taking a course called Introduction to Medical Professions II, a course that allows undergraduate studentstolearnaboutthevariousfields of medicine and shadow physicians at Shands Hospital. I followed my resident physician into the patient’s room where we were met by a seemingly healthy, jovial man in his early 60s, Mr. Seto. He had severe squamous cell carcinoma of thetongueandmouth.Hewasscheduled tohaveamandibularreconstructionwith afibularfreeflaplaterthatmorning.Ifelt sad for the patient for being inflicted by this disease but was excited at the same time about being able to watch the surgeonshealhisaffliction. Thesurgery was long and arduous and took several hours, but ultimately went smoothly. I distinctly remember how grateful the patient’s family was as my preceptor explainedthegoodnewstothem.

LittlehadIknownwouldIseethesame patient four years later during my third yearofmedicalschoolaspartofthecare team. I was on the second week of my internalmedicinerotationwhenIwalked into the room to find Mr. Seto, the same patient I had seen four years earlier for his mandibular reconstruction. I remembered him instantly. However, rather than speaking to the same healthy-appearing, jovial man that I had metfouryearsearlier,Iwasspeakingtoa cachectic, severely ill individual who was barely able to speak a single sentence. As I asked him what brought him in, he merely stated “it’s . leaking again .” as he pointed toward his abdomen. I was barely able to understand what he said but lifted his gown up to find a gastrostomy tube placed with gastric secretions covering his abdomen, slowly eating away at his epidermis. I asked him how long this has beengoingonfor,
whichhereplied,“aweek.”Irealizedthis patientwasgoingtobefarmorecomplex than I initially anticipated and decided to tackle his unchanged G-tube dressings first. The nurses were busy, so I decided tochangethedressingsmyselfasIwould be able to collect additional history from Mr.Seto.Itwasstillincrediblydifficultfor me to understand him, but it got easier the longer I talked to him. During this, I learned that despite the attempts by the surgeons, his oral cancer had metastasized to several parts of his body includinghisesophagusandlarynxwhich endedupaffectinghisspeech.
Iwasdevastated.IperceivedMr.Setoto be my ‘first patient.’ I had scrubbed in, assisted with the procedure, and stood bytheattending’ssideasheexplainedto thefamilythatthesurgerywasasuccess.
I wondered how this could have happened, and whether the surgery failed. I later learned that he had a 40 pack-year smoking history. While he had quit smoking after his mandibular reconstruction, it was too little too late andthecancermetastasized.
I rounded on Mr. Seto every morning. This was my first time being able to followthesamepatientformultipledays at a time. As the weeks went by, I got to know him quite well. I learned that he lovedworkinginhisgardenandwasabig Nascarfan.Ilearnedabouthisfamily;he has a wife, kids, and grandchildren. Medical school ethics taught me: They are people first then patients. It wasn’t until taking care of Mr. Seto that I had actually felt this notion. I had been working in the healthcare environment for9monthsandwasbeginningtoforget that patients were not just patients, but ratherpeoplewhobecomeill.Iknewthis conceptintheorybutwasnotapplyingit to my practice. Having met him four yearspriorandgettingtoknowhisfamily and hobbies, I realized that this was an incrediblyhumanizingexperience.
As time went on Mr. Seto’s condition continued to deteriorate. The surgeons and gastroenterologists were unable to seal the tube. His metastatic disease was progressing rapidly in severity. TPN was initiatedashewasnolongerableto
tolerate nutrition via the G tube. By the end of the week, he was on dialysis. My preceptorandIinformedthepatientthat his prognosis appeared to be extremely poor.MypreceptoraskedMr.Setotocall his family so he can inform them of the situation.Iquicklyrealizedthattherewas a significant chance of my ‘first patient’ dying before I had even finished medical school. I was overcome with emotion as the empathy and compassion I felt toward Mr. Seto overwhelmed me. I constantly thought about Mr. Seto, and how his condition affected those around him. I began to apply a similar sense of empathy and compassion toward my other patients. I began thinking about their emotions, fears and how their affliction affected their friends and family.
When I returned Monday morning, I was greeted by some of his family members who had flown in from various partsoftheUS.Tomysurprise,oneofhis daughters had recognized me from before.Onphysicalexam,Ifoundthathe was disconnected from his IVs, dehydrated, had fallen out of bed, developed a sacral decubitus ulcer, and his abdomen was soaked by gastric secretions from the leaky G tube. I was overcome with frustration that he was not being cared for appropriately. I had never felt anger that a patient was being uncared for until this time. I quickly found the nurse and helped apply dressings and reconnect his IVs. I stood there and made sure everything on my list was done as I texted my preceptor asking to increase his pain medications andorderanairbed.Onmywayout,the patient’sfamilythankedmeforbeing too attentive. I thought: I guess I have been extra attentive to Mr. Seto However, I realized that because I had begun to feel compassionate and empathetic toward this patient, I was being more thorough and ultimately providingbettercare.
I began applying the same values towardmyotherpatients.Iremembered: They are people first then patients. I realized that I must never lose touch of thesevaluesandthatImustfeel

compassion and empathy for all my patients. Compassion can be defined as: a deep response to the suffering of another. Caring for Mr. Seto emphasized that medicine is both a science and an art. He taught me that compassion is a critical part of the art of healing. True healing must involve empathy and compassion, and I realized that I must keep these values for the rest of my career. Before he was discharged, his family divulged to my preceptor that “I was one of the providers to care for Mr. Seto at Halifax.” Upon further introspection, I realized that this patient hadfinallytaughtmethe art ofmedicine.
Scanning my eyes downthelaundry list of patients’ names androom numbers, I was filled with anticipation and anxiety as I was told that we were expected to makeroundsonthefortypatientsonour daily census. This was my first day as a third-year medical student starting on inpatient internal medicine, and I was terrified. My preceptor ran down the list with his fingers and then used his black pentoindicatewhichpatientshewanted me to “claim,” as if they were commodities. After reading the short blurb explaining each patient’s chief complaint,hestoppedatonepatientand said, “Oh this will be a good one for you to see; you’ll see this diagnosis all the time on inpatient.” After reviewing my patient’s chart, I learned that she was a 51-year-oldfemalewhopresentedtothe emergency room complaining of sharp abdominal pain in the midepigastric region as well as nausea, vomiting, and signs of dehydration. Due to the state of her dehydration, continuous vomiting, andabdominalpain,shewasadmittedto theinpatientfloor,whereshereceivedIV fluids,andmoretestswereordered. Walkingintothepatient’sroomhavinga generalsenseofwhat’sgoingon,I
they are in the hospital. Upon initial observation, I notice an obese female who appears her stated age sitting up in bed in acute distress with a green vomiting bag in hand connected to multiple IV’s and monitoring systems. “I’m in a lot of pain and I can’t keep anything down,” my patient said. Using theCLCscriptinmyhead,Istartedasking the “focused problem” questions and learned that she rated the “sharp” pain an 8/10 and that she had a similar episode approximately 1.5 years ago, where she stayed in the hospital for 2.5 weeks with three days in the ICU. “I’m scared,”mypatientsaidasshelookedme intheeye,“Idon’twanttohavetogoto the ICU again.” I looked at her and said, “We are going to do everything in our power to try to prevent that from happening,” having no idea if we can preventthatfromhappening.
AfterIlefttheroom,Iwenttogocheck on my patient’s labs. She had a WBC of 14.5, calcium of 6.6, glucose of 330, lipase of 333, total cholesterol of 397, and triglyceride level of 7,534. I reported myfindingstomypreceptorincludingthe updated labs, and he said, “Just as I suspected, acute pancreatitis.” We kept her on IV fluids, nothing by mouth, morphine for pain, and anti-emetics. I came back the next morning to check on my patient to see if anything improved. She said her pain had decreased to a 6/10 but she was still vomiting most of the night. On the third day of her inpatientstay,Iwenttocheckonher,and instead of only talking about her symptoms, she started to confide in me. “I’masinglemom,andI’mreallyworried about my kids. I just want to go home to themandmakesurethey’reok.”Isaidin reply, “First, we have to make sure that you are ok before you can go and help them, but it’s normal to feel this way.” This was the first statement I made where I felt confident in what I said was true. She reluctantly nodded and started blaming herself for why she was in the hospitalinthefirstplace.“Iknowmydiet isn’t the best,” she said, “and I could exercisemore.”Althoughthese
statements were true, now was not the time for her to start getting more depressedandanxiousabouthercurrent hospital stay. I tried to navigate the conversation away from her blaming herself and towards using this as motivationtoputherhealthfirstinorder to be there for her kids. She seemed receptive to my feedback and appreciativeofthetimeIspenttalkingto herlikeanotherhumanbeinginsteadofa labvalue.
On the sixth day of checking in on her and learning that she was still nauseous with a few vomiting episodes, my preceptorstartedtolosehispatienceand accuse other diagnoses that she had for why she was still in the hospital. “It’s all heranxiety;it’sallinherhead,”hesaid.I then rounded on my patient with my preceptor and could tell how overwhelmed he was with his growing patient list and how he was ready to discharge my patient no matter how she felt. On paper, my patient was getting better, but in person, she was still vomiting, unable to keep most food down, and not physically ready to be discharged.
When I went back to check on my patient before I headed home for the night,Icouldtellthatshewasaffectedby my preceptor’s reaction earlier that morning. “I don’t mean to be a burden, but I don’t think I’m ready to go home just yet.” I knew from what I had seen throughout the week and after my conversationswithher,mypatientwould notbeinthehospitalifshedidn’thaveto be. “I know you don’t,” I told her, again confident in my statement. I felt incredibly sad that my patient felt like a nuisance for trying to heal in a place designated to help those suffering. My experience led me to realize though that if the people assigned to help you are overcomebytheirownstrugglesandthe medicalsystemcontinuesinthedirection of putting profits over patients, it makes it much harder to fully invest one’s energy into helping those who need them. I hope in my future practice that I continuetolistentomypatients,evenon thesixthday,becauseIknowhow
terrifyingitcanfeeltobeinthehospital, evenwhenyou’renotthepatient.
Growingup in Ithaca, a small town in upstate New York knownbest for being home of the prestigious Cornell University, I found myself always longing to leave. As a kid, I’ve always had a natural talent for buildingthings,usingmyhands,andonly looked forward to shop class in junior high. I certainly never dreamed of workinginconstructionwhenIwasakid, but it was a job that suited me and paid well enough to support an 18-year-old withachildontheway.Iknewthatonce I found out I was going to be a father, moreschoolingwasnotanoptionforme. I quickly joined the field of construction the day after I graduated high school because I made my mother a promise that she was still going to have a child with a high school diploma. For the next 3 decades of my life, I witnessed a field that changed tremendously with enforcements of regulations and safety requirements that made me question whether my own health was ever impacted as a construction worker. Nevertheless, I was proud to say I had a hand in building a large majority of the homes and office retail space in upstate New York during a hard-working career lasting just over 30 years. While I’m proud of the career I left behind, retiring at 52 was certainly not what I expected tooccur,either.
Over the last decade of my career, I transitioned to a pure supervisory role. My managers helped me save face and told my coworkers it was because they neededmeasasitesupervisor;however, everyone knew later in my career that I wasn’tquitetheworkerIwasonce.Iwas never an athletic guy and I certainly neverexercised,butIdidn’tthinkIwould tire so easily in my late-40s. Often, my guyswouldseemehavetotakeabreak

and fall short of breath. Having never smokedadayinmylife,Ijustassumedit was the physicality of the job taking its toll on me. It wasn’t until I retired that I truly felt like my body was giving out on me. Persistent cough spells lasting minutes at a time followed by gasping breathsforairwerealltoofrequentofan occurrence. Although I knew something waswrong,IpusheditoffforyearsuntilI achieved the second greatest accomplishment of my life, becoming a grandfather.
Shortly after having my son, his mother andIwerenotabletoseeeyetoeyeand grewapart.Mygreatestregretinlifewas not spending enough time with my son. I’ve missed baseball games, birthday parties, and taking him to school on many mornings all so I could provide as best as possible. I was never a rich man, but I made sure my son always had enough to be comfortable. Fortunately, mysonwasabletodomanythingsthatI couldn’t. First and foremost, he received acollegedegree.Healsoworkedhardto make his relationship work with his wife, whom he met at college. His success as an engineer afforded him a lifestyle that allowed him to comfortably have a child inhislate20s.HemoveddowntoFlorida to be closer to his wife’s family and they extendedtheinvitetome.Ifiguredsince heistheonlyfamilymemberIspeakto;a change of scenery may not be a bad thing. Shortly after, my grandson came into this world. I knew that there was now another life to live for and that my healthshouldbeprioritized.
I still remember the deafening, ringing tone I heard from my ears and the sensation of my stomach dropping when the word “mesothelioma” came out of my doctor’s mouth. This was only a condition I had heard of on TV commercials and never expected to see anyone with it in person, let alone be diagnosed with it. When I received the diagnosis, I was devastated––I couldn't bear the thought of my life ending like this. I first thought of the new life I wished to have in Florida, finally being able to be a part of my grandson’s life. Afterhearingmanynumbersand
I figured it was best to just be present with my family. I’ve accepted that my time will come, just like everyone else. Althoughmyconditionworemedownto thepointwhereIlost40poundsandwas coughing up blood almost monthly, I knewtherewasstillmoreoflifetoenjoy. However, when lumps of tumor starting to poke out of my rib cage and raise my skin, I quickly felt that it would be difficulttoenjoylifeincomfort.Thepain of taking a simple breath would send a shockwave throughout all of my body thatwasunbearable.
On my 58th birthday, almost one year ago, I watched my grandson play soccer for the first time. It took all of my strength to ignore the constant chest pain I was having or the lack of sleep catchinguptomeasIwasunabletorest while I was chronically aching. Previous doctorshavetriedtomanagemypainby theguidelinestheyweretaught.Theydid notlistentomeasapersonandwentby what protocol told them to. When I told them that the pain of a t-shirt rubbing against the lumps of tumor protruding through my skin felt like an 18-wheeler crashingintomyribcage,theystatedthat anymorepainmedicationsissomethingI would have to see a pain specialist for. Painspecialistsrecommendedallsortsof surgicalinterventionsandlong-termpain pumps. I felt that undergoing surgery would probably be something I’d never wake up from and turned to a new doctortoseeiftherewashope.
Mynewfamilydoctoristhefirsthuman I’ve seen cry when I described the pain I went through on a daily basis. He was able to provide me with medication that allowed me to live a comfortable life. He trusts me enough to use these pain medications responsibly and aimed to relievemeofmyburden.Iamfinallyable to sleep and spend the remaining time I have with my grandson in comfort. He later introduced me to the idea of hospice, and it frightened me, however his explanation of what services may be provided to me to keep me in comfort were encouraging. For the first time in mylife,Ilookforwardtomymonthly
visits with my doctor. He is not a doctor who looks back at my previous life choices and tries to pinpoint what may havecausedmycondition.Hefocuseson howIcanbeabletomaximizemyquality of life. It brings me joy to see how he is sharing his empathic qualities to his students and is helping create a generationofnewdoctorsthatwillfocus onthepatient.

I was the eagereyed, hopeful future surgeon walking into my first third-year rotation with the notoriously toughest surgeons at my campus.Ihadnoideawhattoexpectand held my reservations as to any prior judgement that was bestowed in my mind. As the day progressed, I continued to become more comfortable in working with and around my preceptors. Nearing the end of the day, our final case was with SJ. He is middle aged man with a long-standing history of Crohn’s disease in which he had previously been treated with an extensive bowel resection some 20+ years prior leaving him with an ileostomy. His complaint was that the past few weeks he has noticed some “painandslowingoftheflowthroughthe ileostomysite.”
I follow my preceptor into the pre-op holding area and see a pensive man surrounded by his wife and daughter. Theyalllookanxious,includingSJ,whois unsure what this process will hold. My preceptor explains to them what he believes is happening based on the imaging and the conservative steps surgically to be made today. SJ agrees to thisplan.AsthesurgeonandIgobackto prep, I rattle off my questions about his thoughts of potential outcomes and subsequent adverse events that may ensue.However,allIcanthinkofarethe anxiousfacesthatwerestoodwaiting
with baited breath at what the surgeon wasgoingtosay,allwhiletheirfacesheld complete confidence in his plan. The surgery proceeded without issues and the minor dilation we enacted at the ileostomyorificewasthebestfirststepto resolving his issue. The next morning as I am rounding, I stop by to check in on SJ. His wife was patiently waiting at the bedside watching him as he slept. In an effortnottodisturbhimatthemoment,I spoke to SJ’s wife about how he was overnight and delve into deeper subjects onhispasthistoryandhowhehasended up in this predicament. Through the few minutesIspokewithher,Icouldfeelher anxiety lifting as she had a voice in that momenttoexpressherconcerns.Igently awaken SJ to do a brief physical exam including checking his ileostomy site while asking some questions. No issues werepresentonmyexamandIexplained I would return later with the surgeon. A few hours pass and we return to the roomasateam.Thesurgeonexplainshis procedureandrationaleandinformsSJif he can eat and have reasonable flow at the ileostomy, discharge is an option. Later in the day, we return and find SJ withgreatflowanddischargehimhome.
A brisk few days pass on the surgery service. As I log into the computer and check my preceptor’s list of patients, I notice a familiar name, SJ. How was SJ back in the hospital? We sent him home and he was doing fine, I thought to myself.AsIproceedthroughmyrounds,I stopbyhisroom,andtomysurpriseheis up at the early hour. I begin to inquire about what’s brought him back in. The soft-spokenSJexplainstheprogresswhile in the hospital but the weakness and the continued issues of blockage at the ileostomy he had at home again. I knew as the surgical team we were going to have to try again. We returned to the operating room again trying with our most conservative treatment of a more extensive dilation with the intent of keeping him a few extra inpatient hospital days to ensure a proper recovery.AsIroundedthenextfewdays, SJandIbegantobondwhilehewas
awake in those early morning hours. I provided a reassuring smile and ensured he was comfortable while maintaining a jovial relationship with him for the times whenhiswifeordaughterweren’tthere. His symptoms resolved during the hospital stay and he was recovering well from the surgery so he was discharged. This was the first patient relationship I had built as a third-year medical student withoneofmypatients.Iwasabletosee the care and compassion I could build just over a few days and how this impactedbydesiretocontinuetosoothe the patients with whom I was on the treatmentteamwith.
Adaypassed,noSJ.Anotherday,noSJ. A week passed, no SJ. I was beginning to miss our comforting conversations of my experiencesstartingmyclinicalrotations. But I also understood, not seeing him back was for the best. Another week passes and my preceptor received a page from the ED: “Patient with an ileostomy complaining of bowel obstruction.” My heart was gutted as I knew the sweet and kind SJ was back at thehospital.
The outlook now entailed a more extensive open surgery since the prior twoyieldednopositivelong-termresults. My expectations were that the kind, caring family members of SJ would begin to turn on the surgery team as it now seemed he was in a perpetual cycle in and out of the hospital. However, his wasn’ttheresponsewereceived.Coming to speak with them in the pre-op, while mildly agitated, they were still extremely grateful for the efforts so far in trying to postpone the major open abdominal surgery. With a reassuring nod to his family, I ensured he would be in good hands. A small tear fell from his wife’s eye as she nodded in reciprocation as he wasbeingwheeledback.
Over the next two weeks, SJ remained on our patient list as his hospital course was complicated with prolonged antibiotic regimens, postoperative bowel rest, and electrolyte abnormalities. Through that time, I ensured I left home a few minutes early to have some extra timetotalkwithSJ.Wecontinuedto
build the bond as I wanted to make his hospitalstayjusta littlebitbetter.
My time on the surgery rotation was coming to an end and yet SJ was still sitting, waiting, and hoping his hospital course would come to a close soon. On myfinalday,Iwalkedintohaveourfinal chat. I thanked him for being so reassuringtomyinitialclinicalexperience and so positive about the entirety of the situation he was in. I thanked him for comforting me and expressed how unfortunate it was that we had to meet thisparticularway.SJgesturedformeto take a seat on the foot of his bed. He grasped my hand and said, “Thank you. Thankyouforspendingthetimewithme and my family. As a father myself, I can only imagine the pleasure your parents have to call you their son. You are going to make a wonderful physician.” Tears were rolling down his face as I knew this hospital course was one of the toughest battles he faced. I thanked him, received ahugfromhiswifeandexitedtheroom.I held those words as I walked down the hallway, holding back my own tears, as not only was I grateful for spending the extra time with SJ but also to be in a position to make an impact in the way I had. I knew from this experience that no matter what is happening in your life or how busy it is on your day, those few extra minutes to connect will mean the most.
Itwasapproximately 7:05amwhen I and the rest of the day team huddled in the nurse’s station receiving sign-out. Overnight, the pediatric emergency department received an 11-year-old female in status asthmaticus. With proper execution of thestatusasthmaticusprotocol,thenight team was able to drastically improve her conditionandshewas
reportedly “looking pretty good” by morning rounds. When we walked into the room to meet and assess her, we notedminimalworkbreathing,saturating around 97% on high flow oxygen, diffuse but mild wheezing on auscultation. To a layman, she looked like a normal kid resting in bed; to a medical professional, shehadcheateddeath.
Around 10 AM, the patient’s mother, who spent the night at the hospital, notified the nurse that she wanted to take her child home now that she was feeling better. The nurse rushed back to the station to convey to the rest of the medical team how this “ghetto mom” couldn’t understand that her child was only appearing well due to the steroids, albuterol, and oxygen being provided to her. The mother, however, was adamant that the child was fine and she simply needed a refill of her albuterol inhaler beforeshetookthepatienthome.Outof concern for the wellbeing of the child, the attending physician decided to call DCF in an effort to overrule the desire of the mother to take the child home against medical advice. I remember feelingsotornasthephysicianmadethe call; I understood that the doctors and nurses believed a discharge was not in the child’s best interest, and even considered it to be child neglect. However, involving DCF was an overstep of parental authority in medical decision makinglikeIhadneverwitnessedbefore. Ultimately, DCF denied the physician’s request for required the patient to remain in the hospital as her condition was now stable and seemingly no longer life-threatening. The medical team was furious. They proceeded to tell the mother they would call the police if she tried to take her daughter home. As one would imagine, the mom did not take these statements and threats very well, and this conversation quickly turned combative.
When the doctors and nurses walked out,Istayedinthepatient’sroomtotalk to the mom alone. With a calmer voice and kinder words than had previously been hurled at her, I tried to explain the severityofthesituationtothemomand

why the patient needed to stay in the hospital. It was during this conversation that the mom disclosed to me that she hassixotherkidswithnosupportsystem and needed to leave so she could take care of her other children. She felt like shehadnochoice.Thiswasaperspective ofthecasethatthedoctorsandstaffdid not know and maybe did not care to know. They just felt like she was an “ignorantmom”notdoingwhatwasbest for their child. Despite our conversation, the mother eventually collected the patient’s belongings and took her home. None of the medical team, including myself, was surprised when the patient’s sats dropped to 83% as soon as the little girl took the nasal cannula out of her nose.Mybiggestfearforthepatientwas that she would decompensate later that dayandenduprightbackinourcare.
This situation was difficult for me as someone who tries to always see both sides of an argument. I certainly understood the medical reason for why the patient needed to remain in the hospital; it was clear that the patient’s status improvement was due to the medications and care that were being provided for her in the hospital. However,partofmewantedtosidewith the mother as well. I believe this cognitive dissonance originated because the medical team did not try to understand the mom’s motivations or understanding. They just saw her as a senseless woman and later joked about herhavingmorekidsthanshecouldtake care of when they found out the real reason behind wanting to take the patient home. But in my time with her, I wasabletoseeherasahuman,makinga difficultdecision,wantingtodowhatwas best for her kids. This situation reminds me that while I will advocate for my patients, I will do it with humanity, empathy, and understanding. We are seeing our patients and their families in some of their most stressful moments, and we owe it to them to meet them with genuine care and respect. While advocating for our pediatric patients can sometimes require DCF involvement, I willalwaysremembertoinvestigatethe
situation to the best of my ability and refrain from making character judgements without gathering all the information.

Dr.ViktorE. Frankl was an Austrian psychiatrist, and he wrote that there are three aspects of human existencethatareinevitable–pain,guilt, and death. Yet his books ask that we declare optimism in the face of this tragedy hecallsit“tragicoptimism.”
For a number of the patients I met in the hospital and clinic this past year, it was clear to see that they were encountering some or all of the parts of this triad. In the face of their tragedies, I witnessed a wide range of responses. Somecourageous,someoptimistic,some melancholy, terrified, depressed, angry, resigned, etc. Often it was a mix. But I saw that people have the ability to find meaning despite their tragedy and I strongly believe that the role of the medical person in this case is to help facilitate this in each patient. From my own personal experience of death and dying,itisultimatelytheresponsibilityof theindividualtofindtheoptimisminthe face of tragedy. And the optimism only can come from finding meaning, and no one else can do that task for you. But! I think this task is something facilitated by the heart and soul of a person and therefore the physician, by being loving and tender to the patient, may help create that freedom in the soul that enables a person to seek the meaning. AndI’veheardtheseconclusionsinsome patients: great deeds they did, people they loved, and trials which they had gone through with dignity and courage. Thesewonderfulthingsstoredupintheir lives like treasures, which cannot be lost anddonotfadeaway.
Oneday,Imetapatientintheclinic.I
walked in the room, and he was sitting hunched forward with his hands on the bench and had the thousand-yard stare I had become very familiar with. I smiled and introduced myself; he scrunched a quick smile and then back to the weary gaze.Hewasonly67yearsoldbutlooked much older and had a strong New York accent.Hewasthinandhadwire-framed glasses over a weathered tan face with grey hair that flowed out from the sides of his head; he kind of looked like Doc Brown. I decided to do more of an open, no-agenda type interview since the visit didn’t include a specific, acute problem. He had worked for a record company for decades in New York City before moving toFloridawithhiswife.Hehadlivedabit on the wild side throughout his life; was very politically active and outspoken during the ‘70s and had led many demonstrations during college. The nature of his career included lots of drug use, and of course, rock and roll. He was basically healthy since birth: never significantly sick throughout his life and always active. Yoga was a big part of his lifeforseveraldecadeswhichwasoneof his favorite hobbies and accomplishments.
When he hit age 50, he was diagnosed with squamous cell carcinoma of the head and neck and received successful treatment for it. But a decade later, was diagnosed with scleroderma and then amyloidosis. His trips to Mayo Clinic ended with the conclusion that although symptoms could be targeted, there was nothing real that could be done for the diseases themselves. He explains to me now – “I am not interested in going back to Mayo I want to focus on living the bestlifeIcanforthetimeIhaveleftand that’sit.”Itisclearhehurts.Hewalkslike apersoninpainandhebreatheswithhis eyes open and closed randomly, like a person in pain. He has oxygen at home andmovesfromroomtoroomonaline. “Enough length,” he explains, “to make my big trip each day.” He means the trip from the living room to his office where hiscomputerissetupforZoomcallseach day.Hestillworksandisabletodosoas afree-floatingheadonZoom.He
explains, “when you work like that, no one knows you look like a tired old bird and that you’re sick…there’s no context soit’snicetojustworkandnothavethat surrounding you. Plus, I work with a bunchofyoungkidsnowandIthinkthey think of me as some grandfather to them but it works out; it’s a nice relationship.Ilovemywork.”
Myeyesshiftdownatsomepoint,andI see Elvis Costello on the faded old gray t-shirthe’swearing.“ElvisCostello!”Isay. He looks down and smiles, “Oh yea, I’ve seen him too many times to count he’s justspectacular,Iwaskindaaroadie.”I’m excited.“YouknowoneyearIlistenedto his album with Burt Bacharach almost everyday?”Isaid.PaintedfromMemory, he says with a wide grin. “Yes!” And we dive into the world of music. We go through the songs in the album and talk about its genius and then we’re talking about other artists and we’re on the same exact musical wavelength as time soars past us; he throws out a favorite line and I counter with another line. We laugh and we just smile ear to ear we’re talking about Joni Mitchell and how he, if stranded on an island, would choose to take Court and Spark with him, and I said I might take Bruce Hornsby’s Hot House, and he almost jumpsupwithexcitementforthatalbum too and pretty soon in my smiling I notice my eyes feel a little wet and I feel that heaviness on my chest that is a dull type of devastation because I can hate the nature of that inevitable triad, “pain, guilt,anddeath.”Whenthepatientison the table, I am auscultating and I can’t help but look at him as he sits there and imagine his younger self, pain-free and doingyogaoratanElvisCostelloconcert. AsIpercusshisabdomenandpalpatehis posterior tibial pulses, I feel a sort of communion with my new friend; it’s bittersweet. He laughs as I am looking in his ear and I ask what is funny. He says, “You know I haven’t talked about music like that in a while, what a pleasant morning.” I wholeheartedly agree. The visit comes to end as I jot a note or two down. I notice he wipes a couple tears awayas
he is sitting back on the bench, looking out the window. A bit later when he leaves the office, we both turn to meet again before he rounds the corner, and we shake hands to say goodbye. He is beaming and I feel a sort of love in my heart for this patient, that love that comes from fellowship with another humanbeing.
Of all the things we do in a day; all the things we pine over, worry about, or strive for…I believe these loving encounters with patients is what seems to really matter. Thinking back to Dr. Frankl’s philosophy, I know that if even little acts or expressions of compassion can be exchanged, it brings the human spirit to a place a little less vulnerable to despair. It is my privilege to be able to take care of patients and love them throughthisuniquefellowship.

The second day of my general surgery rotationwaspacked fullof patients and procedures. After a long day, I was just about to leave late in the evening when there was a page from the emergency room describing a young man in cardiac arrestthatneededanemergencysurgical consult. I was offered to leave since it was getting late, but a hurricane was quicklyapproachingourarea,soIwanted tolearnallthatIcouldwiththetimethat I had. Little did I know the impact this man would have on me and my medical career. When I walked down for the consult, I thought to myself how crazy it was that this man was only a few years older than me. How could he possibly be a victim of cardiac arrest? When the surgeon and I arrived at his room, chaos hadalreadyensued.
Once the patient was stabilized and intubated, the surgeon told me I would be placing his femoral catheter. I was ecstatic to take the lead on the procedure,butverynervousforapoor
outcome. I had never seen a catheter placementbefore.Heguidedmethrough the procedure. I worked carefully, and successfully placed the catheter. I felt so proud of myself for completing my first procedure, while also thankful to this man for affording me the opportunity to learnanewskill.
The next morning when I rounded on him, he was rapidly decompensating. He had no kidney function, and the femoral catheter had blown. Another catheter wasplacedontheothersideofhisgroin, but it was only a matter of time before that one would blow too. A few days after his admission, the decision was made to start a central venous catheter. The surgeon instructed me that I would be performing this procedure, and I was even more nervous than the first time. I had never seen a catheter placed in the neck before, and there is little margin of error when directing a needle into the jugular vein. I kept my hands steady and focused on the instructions being delivered to me. After the successful completion of this procedure, I tore my gown off, and thought again to myself howthankfulIwastobeabletolearnoff ofthispatient.
I rounded on this patient in the ICU every morning and every evening. After his first week in the ICU, his parents began to come sit with him during the day.Wechattedabouthislifebeforethis horrific event. Learning his story made me realize this patient has a whole life outside of these walls, and although I have never seen him awake or communicating, he had two small children at home that had no idea what he was going through. His parents told me of how the patient’s brother died on a skiing trip 10 years ago, and how the patient never recovered. He struggled with depression and alcohol for majority of his adult years after that incident, and now here he was laying in the hospital bed,unconsciouslyfightingforhislife.
After the second week he was in the ICU, he was not turning the corner. His kidney function had not resumed, so he still required frequent hemodialysis. He wasonaventilator,withnumerous
medications all looming over his hospital bed.Afterseveralfailedextubationtrials, the decision was made to give him a tracheostomy tube. This time, the procedure felt different. He was no longera“cardiacarrestinbed3.”Hewas a son, a father, a brother. He was Michael.
After three weeks in the ICU, there was little to no improvement. When I would round on him in the quiet mornings, I would note the beads of sweat dripping down his face. I noticed how much weight he had lost since his admission. A face that was once full of life, now pale and without adipose tissue. I began to wonder if he was going to make it throughthis.Hisfamilyhungphotosona bulletinboardinhisroom,illustratingthe life he had before he was confined to thesefourwalls.Ilookedatthephotoof him with his four-year-old daughter, which was attached to a drawing labeled “feel better daddy, I miss you.” I hoped witheverypartofmybodythathewould pullthroughforthislittlegirl.
A month after admission, his kidney function started to rise. He had finally startedturningthecorner.Hewasawake and able to move his extremities, although he was not alert or oriented. Many thought he had suffered brain damagefromtheincident,andmaybehe wouldneverbethesameMichaelhewas before. How terrible it would be for the familytomournthelossofamanwhois still alive. I continued to root for Michael’s success and I kept my hopes high.

Gradually day by day he improved. I bonded with the family over how far he had come. Eventually, he began to communicate and walk with assistance. Bythelastweekofmyrotation,wewere discharging him from our service. The family had gotten him a spot at a rehabilitation facility in town that would work with him further. I could not help but think what a miracle this has been. Although I only played a small role in his overall care, I was so proud to be part of the team that helped save his life. Every patienthasastoryoutsideofourhospital walls,andthisexperience
illuminated the importance of understanding our patients as people, ratherthanjust“thepatientwithcardiac arrest.”
Caringforthispatientgavemea“why.”I found a love for critical care medicine through this experience, because although there are many poor outcomes in situations like his, recoveries like this make it worth it. This experience ignited apassioninmetowanttointerveneand do all that I can do for critically ill patients,justtohavetheopportunityfor another patient to improve like he did. Watching him recover every day for over amonthwasmorerewardingthanIcould have imagined. I enjoyed learning more abouthim,andamthankfulIwasableto careforhimontheworstdaysofhislife. He may not remember me in his story, butIwilltrulyneverforgethiminmine.
I walk into our patient’sroominthe emergency department and see a young26-year-oldfemalesittingupinthe bed. She is drinking a soda and eating gummy bears. She smiles and waves at me and asks how my day is going. It struck me as surprising that someone with her diagnosis was still this upbeat and bright. She had come to the emergency room thinking she only had a cold with a cough and increasing fatigue, only to find out she had acute myeloid leukemia. I come in to gather her history aswegetreadytoadmither.Weprepare her for her bone marrow biopsy and for induction of chemotherapy. As medical students we learn so much from our patients,abouthowtotalkwithpatients, theirdiseaseprocess,andsomuchmore. However, I had no idea just how much I wouldlearnfromthisyounggirlwhohad just been diagnosed with this serious disease.
This26-year-oldfullofresiliencehadthe resultsofherbonemarrowbiopsyreturn that confirmed the diagnosis of acute myeloid leukemia. She was started on induction chemotherapy with daunorubicin and cytarabine. As she was receivingherchemotherapyIwouldgoin and check on her every day. Every morning when I walked in the room I heard, “there’s my buddy.” I would see how she was feeling and one day she disclosedtomethathermotherhadjust passed away last week. She further discussedwithmethatshewashopingto makeitoutofthehospitalintimeforher funeral next week. I was shocked. This girl who had just been handed this diagnosis and lost her closest family member still greeted everyday with a smile and always made sure she asked how I was doing. This patient’s resilience and selflessness left a lasting impression on me. She taught me that you never truly know what is fully going on in a patient’s life. As a physician, we can always make an effort to show our patients the utmost compassion and to be patient with them. As I moved forward in my medical school journey after this encounter I always kept her in mind.WheneverIhadadifficultpatientI always reminded myself that I do not know fully what this patient is going through. I always made sure to stop and maintain my patience, keep a calm demeanor no matter the situation, and aboveallexhibitempathy.
Everythinghappenedsofasttogivethis 26-year-old the best chance possible at life. As the days continue to pass by, we continue monitor her labs. We notice that her red blood cells and platelet levels are dropping due to the chemotherapy. We begin to discuss transfusion with the patient, and we find out she is unwilling to accept blood due toherreligion.Thiswasnotdocumented and was not discussed ahead of the induction chemotherapy. This posed a dilemma. The chemotherapy she is receiving will cause her to have pancytopenia. She would most likely not make it through the chemotherapy regimenwithoutthetransfusions.We
discussed with her the risks and benefits of the transfusions, however, she opted to continue without them. We gave her alternative means to increase her red blood cell and platelet counts. However, this was not enough, and her numbers were continuing to drop. We sat down and talked with the patient, and we found out the reason that she did not wantthetransfusion.Shestatedthatshe, in fact, wanted the transfusion, but was fearful of what her community would thinkofher.Wediscussedwithherthatit is completely her decision and no one else’s. She eventually opts to undergo transfusionandthehospitalworkedwith her so her community would not find out.Thisexhibitedtometheimportance ofpatientautonomy.
It is of utmost importance for a patient to retain their autonomy in the hospital. This is yet another quality that this patient left a permanent imprint in my life that I carry with me with every patientinteraction.Ittaughtmetonever make assumptions. It was assumed since she did not have another member of her religious community with her, which is usuallythecase,thatshewasnotpartof this specific community that did not allow blood transfusions. However, this assumption should not have been made and should have been explicitly asked. It also taught me to always clearly explain everything to the patient and make it clear that any decision about their healthcare is nobody else’s choice but theirs, such as what was done with this patient. The original decision to not receive the blood transfusion was out of fear and not her own decision. However, after explaining autonomy to the patient shemadethedecisionthatshewanted.
NoweverypatientroomIwalkintoIsee this 26-year-old girl smiling. I take the lessons that she taught me into every patient interaction. I take with me the lessons of humanism in medicine that I learned from her, to always exhibit empathy,andthatitisimportanttolisten tothewholestorybehindeverypatient.I alwaysmakesuretonotonlyaskabouta patient’s symptoms or disease, but their personallifeaswell.ImakesureItake
thetimetotrulygettoknowmypatients and to have the cognizance that they mightbegoingthroughmorethanmeets the eye. Additionally, for every patient’s autonomy I always remember this 26-year-old. For every patient I always make sure to ask if they would accept blood products and to never make assumptions about patients. I always keep in mind it is better to ask too many questions than not enough. I always make sure to take extra time to emphasize that what treatment plan we decideonistheirchoiceandIamhereto be their advocate. As I walked into that patient room in the emergency department to greet this 26-year-old, little did I know the profound effect she would have on me. She taught me so much more than just about acute myeloidleukemia.Shetaughtmehowto exemplify humanism in medicine and to emphasize patient autonomy above all. As I move on in my medical career I will always remember this patient and the lessons she taught me to give patients theexcellentcarethattheydeserve.
Internal medicine wasonlymy second rotationasamedical student. It was also my first real experience working in a hospital and I had no idea what to expect. I began working in a small hospital during a time whereCOVIDwasverymuchstillpresent in Florida. To make matters worse, my small hospital was centered in a community consisting of mostly older aged residents. Residents who checked off many of the morbidity and mortality risk factors for COVID. This combination createdaperfectstormformyhospital,a situation seen throughout hospitals acrosstheUS.
I could see the exhaustion on the doctors’ and nurses’ faces as I entered thehospitaltoroundonpatients.
Everyone seemed to be juggling multiple tasks and always appeared to be in a rush. I began to truly understand the amount of work needed to care for such an overwhelming number of sick patients. Tasks needed to be completed asfastaspossibletokeepthingsflowing. This is where one of the common problems in medicine became apparent to me. I realized how easy it was to get caughtupinthemanytasksofmedicine, dehumanizingpatientcare.Furthermore, patients and healthcare workers were required to wear layers of protective gowns,masks,ventilators,andotherPPE. This constant physical separation betweenhealthcareproviderandpatient made losing sight of humanity much easier.
One patient in particular, truly helped mestayontherightpathofpatientcare. Thispatientwasan85-year-oldladyIwill call Mrs. Jane. She was a small frail lady withahistoryofCOPD.Shewasadmitted to the hospital due to a severe bout of COPDexacerbationfromCOVID.Thefirst time I saw her, she was in poor shape. She had IVs, ventilators, and various otherwiresconnectedtoher.Nursesand Doctors moved rapidly around her, coming in and out of her room to give meds and record stats. In all the commotion I noticed no one was really talkingtoher.AsIapproachedhertosay hello, I saw she was shivering. Her face was full of fear and in a weak voice she told me she was cold. I ran to retrieve a warm blanket, happy to be able to help evenifonlyinaminorway.
I introduced myself to Mrs. Jane and askedherhowshewasdoing.Onceagain in a weak voice she told me she was scared and didn't want to die. In this moment I realized that a big part of medicine does not revolve around traditionalmedicine.Inthatmoment,the most important thing I could do was comfort my patient and make her feel at ease. I held her hand and told her she was in good hands and that the team would do everything they could to keep her safe. In busy times such as COVID, I understood how easy it is to get caught upinmanytasksofmedicalcare.This
cycle can cloud providers' minds and makethemlosetouchwiththehumanity ofthepatient.
The next day Mrs. Jane’s condition finally stabilized. Her breathing was controlled,andshewasabletotalk.Once againtherewasn’tmuchmoreIcoulddo from a medicine standpoint so I decided tojusttalkwithher.Igaveheranupdate on her situation and answered any questionsshehadmakingsuretoremind herthatshewasingoodhandsandthatI would be coming every day to check in on her. As I promised, each day I visited her to talk, regardless of whether I had anything to add to her medical care. As the days went on I noticed how excited she was when I visited her. Her face would light up when I entered the room and she would always say how grateful she was to see me again. Our conversations often shifted away from medicineandwediscussedlifeandother everydaytopics.DuringthosemomentsI didn’t feel like a medical student talking to a patient, I felt like a regular person talking to a friend. These conversations helpedmeseethruthelayersofPPEand reminded me of the humanity within eachpatient.
TowardstheendofMrs.Jane’sstayshe thankedmeonceagainforalwayscoming to talk with her. She told me that she didn’thavemanypeopletotalktoinlife. Most of her family and friends had passed away and she didn’t have many visitors. Mrs. Jane expressed to me that talking with me was a highlight of her days and that it made her stay much moremanageable.
Several weeks later I was in my outpatient clinic when one of the nurses pulled me aside and told me a patient was looking for me. There was Mrs. Jane ready to say hello again, looking just as happy as she did during our past talks. I was surprised that she had remembered me and was glad to see her again. Months after my rotation was over, my internalmedicinepreceptortoldmeMrs. Jane would still ask about me during her outpatient visits. I saw the impact my seemingly simple conversations had on her.Simpleactsofkindnessand
genuinely caring made a lasting impact onapatient.

During busy days, chatting about random topics may seem like a waste of valuable time. But to many patients, this may be the closest thing they get to normal life. The hospital setting can be very overwhelming and chaotic. Dealing with illness in this foreign environment alonecanseemlikeamonumentaltask.I saw first hand how taking time to sit downandtalkwithapatientcouldhavea tremendous impact on their overall healthcare experience. Mrs. Jane helped meavoidgettingcaughtupintherobotic cycle of task completion. She helped remind me of the importance of treating patientsashumans.
When the next patient walked in for his routine healthmaintenance exam, he asked me if menopause could be causing his racing heartbeat. I was perplexed. He had opened an entirely newalgorithmfordifferentialinmyhead. This was a 50-year-old white trans-male presenting with the complaint of new onset heart palpitations. He said his mother went through menopause at 50 and that the possibility seemed very likely to him. After presenting to my preceptor, she told me that although he was most likely experiencing premature atrial contractions, that was certainly something to explore deeper. We educated him on the benign causes of heart palpitations like premature atrial contractions along with the possibility of menopausebeingthereasonforsomeof his other complaints such as hot flashes, insomnia, weight gain, and decreased concentration.
I found this experience to be a huge learning moment. Although he had transitioned into a trans-male, we, as healthproviders,mustnotforgetabout
managementtohisbiologicalorgansand their functions/disorders like going throughmenopause.
We asked if he needed a referral to his gynecologist or if he wanted to alter his testosterone therapy, and he declined. He decided to not make any changes to his testosterone replacement therapy and would address these symptoms in thefutureiftheystarttodrasticallyaffect hisdailyactivities.However,heagreedto get an ECG, chest x-ray and to see a cardiologist for management of his heart palpitations.
I was able to follow him to his referred cardiologist appointment, and initially I wasabitworried.Hementionedthatmy preceptorwasoneoftheonlyphysicians helikedtoseeregularlybecauseshewas both accepting to his transition, and she kept herself up to date with the medical management of transgender people. So, whenweenteredthecardiologistoffice,I was hyper aware to the interactions he had with the staff and medical professionals. I then thought to myself how exhausting it must be to be in his shoes meeting others for the first time, especially in the medical field. Does he wonder if his care is adequate? Does he havetoworrythatthestaffwilltreathim differentlybecauseheisatrans-male?As if reading my mind, when he finished checking in with the receptionist, he sat down next to me and sighed in relief. “Well,shewaskind.Youshouldseesome of the looks I get from people once they seemychartandbiologicalsex.”
We had some time before he got called backintotheoffice,andsoIgottoheara bit about his story. He started his transition eleven years ago and was rejected by most of his family members because they refused to accept his transition. A few years after coming out, he lost both his dad and sisters to drug overdose. He and his aunt moved to SouthCarolinaforafreshstart;however, a year after their move, he became a full-time caregiver to his aunt because shewasinaboatingaccidentthatlefther disabled. They then moved to Florida, and he was in charge of finding both he andhisaunthomesalongwith
forher.Thisexperiencemadehimrealize that he wanted to give back and become a social worker to help others in situations like his own. So now, he takes care of his aunt, is getting his masters degree, and is a full-time teacher at a local elementary school. When hurricane Ian hit, his aunt’s home completely floodedsoitwasuptohimtohelpmove her out and fix up her place. It was around then when the heart palpitations started.Tosayapersonhasbeenthrough alotisanunderstatement.
Whenthecardiologistcalledusback,he told us that his ECG showed a normal sinusrhythmandthathischestx-raywas clear. The cardiologist asked if he was under a lot of stress. We both laughed, and he answered yes with his full HPI. The cardiologist said out loud what I was thinking,“Itisclearthatyouhavealotof responsibilities in your life right now and it seems likely that it’s causing stress to your heart.” He then proceeded to explain PACs, what a supraventricular premature beat would present as, and how it can be caused by lifestyle risk factors such as smoking, alcohol, caffeine,andstress.
Due to the sporadic nature of PACs and theinconclusiveECG,thedecisionforthe patient to undergo ambulatory monitoring via a 24-hour Holter ECG was made. The cardiologist then proceeded with reassurance on the benign disorder and told him to avoid the common triggers if possible. The physician then offerediftherewasanythinghecoulddo to help reduce his stress regarding his mother and her hurricane destroyed home. The patient declined but shared hisappreciationfortheoffer.
Thislearningexperiencewasimmensely influential and helped me gain insight into the challenges that transgender individuals may face when seeking medical care. By acknowledging the uniqueness of each individual and showingrespectandactivelistening,one is helping to create a more inclusive and supportive environment for all patients. From the moment a patient enters the office,allinteractionsmatter,as
highlighted from this person’s anxiety at the front desk of his cardiology appointment. The newfound understandingofthechallengesfacedby transgender individuals can help provide morecompassionateandeffectivecarein the future. The patient felt fortunate to have my preceptor as a primary care doctor who is accepting and proactive in staying up to date with inclusive medical treatment for transgender individuals. Thisshouldbethenorm.Experienceslike this can be invaluable in shaping one’s practice. This encounter has shown me how important it is to continue learning andgrowingasahealthcareprovider.
Home by Samantha SnowMy parents immigrated from Russia two years before I was born anddidnot speak a word of English until I started kindergarten. Growingupinanareawith great cultural diversity, my parents and ourextendedfamilywereabletofitright inwithotherRussianfamilieswhichkept usspeakingRussian,watchingRussianTV and preserved the culture at home. I did notrealizewhatablessingthiswaswhile constantly being pulled out of class to attend additional English classes, but I haveneverfeltsomuchgratitudeformy upbringing and cultural roots as I have thisyearinmedicalschool.
My earliest memories of healthcare consistofvisitstotheoncologistwithmy grandma. As soon as I was old enough, I served as the amateur translator when her or my mom did not understand something in English which gave me my first glimpse into language barriers in healthcare and inspired my love for language. The ability to effectively communicate thoughts, fears, beliefs, and uncertainties lifts so much of what burdens us and can itself be medicinal. Thediversityoflivinginameltingpot
unfortunately also creates inequality and barriers to access in healthcare. Having seen the impact this can have on health outcomes and medical decisions inspired me to major in Spanish to broaden my ability to connect with, communicate, and care for more people. The most rewarding parts of my clinical experiences has been developing trust andconnectingwithmypatients,hearing their stories and seeing how therapeutic communication can be. There is no greater privilege than that trust between physicians and their patients. It is the art ofmedicinetoknowourpatientsdeeply, toknowtheirfearsandtohealthemwith intangibletherapies.
When I started my OB/GYN rotation, I quickly learned that there was a significantRussianpopulationinthearea. Iwasfinallyabletousemyknowledgeof the language to connect with my patients. The day I met Lena was the most memorable of my medical school experience to date. As soon as I walked intotheroom,hervoiceremindedmeof my mom’s and I immediately spent the first few minutes learning that she grew up in Belarus just like my mom’s side of thefamily.Ilearnedthatherparentshad passedawayafewyearsagoandthatshe had recently moved to Palm Coast with herhusband.Theybothworkedtwojobs and had two young children at home so she always came to her OB visits alone. I imagined everything my mom must have experienced having us in a foreign country, barely knowing the language and could not imagine how alone she must have felt. I had the privilege of seeing her for her weekly third trimester visits. She always came alone, and we always spoke Russian the entirely of the visit and truly got to know each other. We both lit up when we saw each other, and she always thanked me and my preceptor for allowing us the chance to voice her questions and concerns in her nativelanguage.Thisbroughtmebackto being a child at the doctor’s appointments with my grandma, using my incredibly limited knowledge and understandingofanythingpertainingto

medicine to help my family make life or deathdecisions.
When I walked into her room in labor and delivery, I felt sad that she did not have anyone with her, but she insisted that she’s done it before and she can do it again and that she did not need her husband seeing this. This feisty strength and independence reminded me of the tough Russian women in my family and made me admire and reflect on everything they experienced immigrating to this country so I could have the life I have. As her labor progressed, the fetal monitors started showing some concerning signs and she was growing exhausted and scared. It was close to 1am, her husband was asleep at home with their kids and I felt that I was the closest thing she had to family in that moment. I wanted to comfort her as I wish someone had for my grandma navigating her cancer treatments in a foreignlanguage.Iwantedtobringsome familiarity, a sense of safety, peace and home to Lena navigating something as frightening, emotional, and uncertain as childbirth. I stayed by her side, spoke to thenursesaboutanythingshewantedto makehermorecomfortableandcoached her through her delivery in her native language. As I was helping deliver her beautiful and healthy baby girl, I realized Ineveraskedwhatshewasnamingher.I was overwhelmed with emotion when she coincidentally said the same name my dad used to call me as a nickname when I was a kid. The next morning, I camebacktocheckonherandthewhole family was there with Russian snacks waiting for me. I finally got to meet her husband and kids that I have heard so much about, and he was equally as excited to meet the Russian medical student she had been telling him about the last few weeks and thanked me so muchfortakingcareofhiswife.
Getting to know this family and being therefortheminsuchanemotionaltime is something that will stay with me forever.Ittrulymademeunderstandhow important it is to take the time to listen to and connect with people. We all want tofeelheard,understood,cared
about and to belong. I felt so grateful to be able to combine my culture and upbringing with my passion for helping people. There is so much diversity in this country yet so much division and hate. I believethatseeingourpatientsasasum of all their life experiences instead of as isolated medical conditions is what makes a great physician. Taking the time to understand their culture, values and beliefsisessentialtounderstandingtheir needs and developing the connection andthetrustnecessarytoheal.

How has it already beenalmost a year ofclinicalrotations?
I feel like just yesterday I was starting with Dr. Parsons in his family medicine clinic. I learned so much about medicine in such a short time. Having donesomuchthispastyearrangingfrom suturing in surgery, to caring for patients in the ICU, to seeing a patient put on ECMO in an attempt to save his life, to seeing acutely manic and schizophrenic patients, there was still one more thing on my list I felt like I needed to experience as a medical student. I wanted to deliver a baby on my last rotationforobstetricsandgynecology.
This is the one rotation I felt like I had learned nothing from my first- or second-year studies to prepare for it clinically. I mean yes, we learned about endometriosisandgynecologicalcancers, but a mom in active labor? I had no idea what to expect. I wish the rest of this story was going to be about how great myfirstdeliverywent,butitwasfarfrom that.
Dr. Bagwell told me we have one in triage. I saw her first at the same time the nurses were doing her vitals and checking for fetal heart rate. Momma is anexperiencedG7P5015.G7P5015isnot the name of a robot, but a shorthand thattellsphysiciansthemothersbirthing
history.Shehasbeenpregnant7times,5 babies were born at term, 0 were preterm, 1 was an abortion, and 5 are living.Hercurrentbabyis27weeksand5 days. She comes in because she has not feltbabymoveforafewdays.Herblood pressure comes back 152/88. I asked if she has had any headaches, “Yes my head has been hurting for the past 3 days.”Ithennoticedthenurseseemedto get a little nervous as she was having trouble finding the fetal heart rate on doppler.Oneoftheothernursessaidshe wasgoingtogetDr.Bagwell.Istayedwith mom asking her a couple more questions, but more importantly I wanted to be there for support because she had no family with her. This was my first day, so I did not know a lot, but I knew not finding a fetal heart rate was not a good sign. As I asked her questions about her other children trying to keep herascomfortableaspossible,allIcould think about was the possibility that Dr. Bagwell may not be able to find a heart rate. The next couple of minutes that I was waiting for Dr. Bagwell to run over, felt like a lifetime. I was in a position where I wanted to reassure mom, but I knewIcouldn’tinthecasethatherbaby boy is not okay. I think I was seeking reassurancemyself.Ididmybesttohide my uncertainty and be there for mom whilewewaited.
Dr. Bagwell comes in with the ultrasoundandlistenstomeasItellhera briefpatienthistory.InoticeDr.Bagwell’s attitude change very quickly and a tear cometohereye.InthismomentIalready knewwhatwascomingnext.Iwassickto my stomach, and despite all the noise in the typical hospital room, I felt like I could all the sudden hear a needle drop. She asked mom if baby had a name yet, and mom said “JJ.” Dr. Bagwell empathetically said “I am really sorry to tell you mom, but JJ did not make it, the most important thing for you to know is thatthiswasnotyourfault.”Iwantedto cry, but I held back my tears. Mom had no emotion, understandably, I think she wasinshock.Wewaitedwiththepatient for a second ultrasound technician to comeand
confirm the fetal demise. Mom did not have anyone to come and give her support, so I wanted to be there in any waypossible.Thesecondultrasoundwas no different, and the fetal demise was confirmed.Dr.Bagwelltoldmomitwould be best to deliver the baby today for her own health so we would induce her labor. At this point I had no idea what to expect. The uneasiness I had when I first sawthispatientintriageneverleft.
After we left the room Dr. Bagwell told me this is the worst part of obstetrics. Her emotions were a reflection as if she just lost one of her own children. The patient was started on misoprostol and oxytocin. I checked on mom over the nextfewhoursandthenDr.BagwellandI deliveredJJ.
Being my first delivery, I really had no idea what to expect. Dr. Bagwell told me shewashopingthebabywouldcomeout all in one piece, otherwise if baby breaks apart it can be very challenging to get everything out. This then is not only more traumatic for mom, but it puts her at risk of hemorrhage or DIC. Luckily when we started delivery, JJ was in occiput posterior positioning and he cameoutonlyafteracoupleofpushesby mom. JJ came out complete and the placenta was delivered shortly after. JJ’s head was full of hair, but all his bones, specifically his skull looked very soft and seemed mushy. One of the nurses asked meifIwasokay,Itoldheryes,whilethe inside of me was screaming no. For the purpose of looking more presentable we swaddled JJ and then gave him to mom. Mom was in tears and we stayed there for support. I was at a loss of words and wanted to help, but I have never felt so helpless.
We were able to get some family on facetime to be there for her too. I could not stop thinking about the mental trauma she will experience from this. Thankfully she does have 5 healthy childrenathome,whichIdothinkmakes this easier than it being her first born. I went home for the night and told her I wouldseeherinthemorning.Ireflected a lot that night and was still processing myownemotions.
ThefollowingmorningwhenIwalkedin mom was looking over JJ’s crib. I asked her how she was doing, and she said “okay.” I told her that it was okay to grieve and to feel all the emotions she was feeling. I knew her getting back to herfamilywouldalsobegoodforher.Dr. Bagwell and I talked with her about postpartum depression, eclampsia, and contraceptive. She was really interested in contraceptive and opted for Depot. Shewasdischargedhomethatday.
This was my reminder that medicine does not always have good outcomes. More importantly though, were the interactionswehadwiththispatientand the ways we delivered the bad news. Dr. Bagwell did it in such a compassionate waythatIcanonlyaspiretobelikewhen I am a practicing physician. This experience flooded me with mixed emotions. At the same time, it made me gain tremendous respect for pregnant mothers and everything they go though. Despite the bad outcome, I think it is important for us to realize we made the best situation possible out of it. I cannot imagine the difference in care mom would have experienced if a physician came in and had no compassion or empathy. JJ would have been delivered and mom would be okay, but the toll on mom’s mental health would be so much worse. I am glad Dr. Bagwell walked me through this experience and showed me howtohandlebadnewssuchasthis.
As a medical student, I had witnessed many patientswhoweregravelyillandinneed ofurgentmedicalcare.However,nothing couldhavepreparedmefortheprofound momentwhenIhelpedcarefor,Mr.O,a 76-year-old patient with stage 4 lymphoma in the intensive care unit (ICU). It was an experience that will stay withmefortherestofmylife.

Mr.OwasadmittedtotheICUfromthe emergency department with initial complaints of shortness of breath. It was discovered that he had both a malignant pleural and peritoneal effusion, leading to a significantly protuberant abdomen that made breathing laborious. He was visibly in unbearable pain and required supplemental oxygen. The first thing his wifesaidtouswhenweenteredhisroom fortheconsultwasthatshewantedusto do everything in our power to save her husband. She wanted all measures taken to prevent his death, but the patient himselfseemeduneasyasshespoke.
HewasadmittedtotheICUandstarted on fluids and medications to keep his vital signs as stable as possible, with a plantoperformaparacentesistooffload some of the fluid and help his breathing. Once we “tapped his belly” fluid began rapidly pouring out in the collection canister and I noted the immediate look of relief on Mr. O’s face. There was complete silence in the room, even the fluid had a blissfully silent laminar flow. Mrs.Owasaskedtoexittheroomduring the procedure. Mr. O transitioned in and out of sleep and this was likely the first time he felt comfortable in a long while. After we collected nearly 3 liters of fluid from his abdomen, I stood next to the monitor and watched Mr. O’s heart rate begin to rapidly increase. The doctor asked, “how do you feel?” and while he could barely get the words out, Mr. O said tearfully, “I am tired of living like this, I don’t want any more procedures, but I am afraid to leave my wife.” He became increasingly anxious as the doctor began asking more questions on his wishes for his care. He was weak and haddifficultymoving,buthereachedout and asked me, “can you please hold my hand?” It was a poignant moment, and my stomach sank as I realized that this manknewhewasenteringhisfinaldays.
Since he had full decision-making capacity,werespectedhiswishes,andhe asked us to relay the information to his wife. I stood by the doctor as he relayed Mr. O’s wishes to his wife. Once she heardthewords"lethimlivehisfinal
days in peace," I watched as she fainted her eyes quickly rolled to the backofherhead,andshefelltothefloor nearly hitting her head in what seemed to be slow motion to me. I stood still in fear, as the rapid response team was called to assess Mrs. O. She quickly revived and but was visibly distraught. Sheaskedfortimetotalktoherhusband and daughter to make sure this is truly what he wanted. Through the glass window of Mr. O’s room, I watched her scurry in and embrace her husband as if it were the last time she would see him. A little while after the family spoke, Mrs. O came over to the nurses’ station and told us they were ready to sign the DNR and proceed with palliative care. A few momentslater,hospicearrivedattheICU todiscussnextstepswiththepatientand hisfamily.
Theydecidedhewouldbedischargedto home hospice. The doctor I was with cautioned me that his lungs were not strong enough to be off oxygen and that he would likely expire soon after it was removed. As this was one of my first experiences in the ICU, it was a sobering reminderoftherealitiesofmedicineand end-of-lifecare.
Thiswasatoughtimeforme,andIhad been following this patient for over a week I could only imagine how it felt for his daughter or his wife of 44 years. AswedidallwecouldforMr.Oatthe
beginningofhistimeintheICU,wewere so hopeful that our interventions would work. He had moments where he began to improve but quickly deteriorated and continuedtoworsenthroughouthisstay. Throughout his time there, I often witnessedMr.Ospaceoutasheseemed to be thinking deeply about something. NowthatIreflectonmytimewithMr.O, Irealizethiswasafirst-handdepictionof one’s life flashing before their eyes. His communication was limited, but his expressionsspokevolumes.
Mr. O was more than just a patient in room X with stage 4 lymphoma. That message holds true for all patients. We mustrememberthatpatientsarenotjust medical cases, but individuals with unique experiences, values, and emotions. Taking the time to listen to their concerns and understanding their perspectives can make a significant difference in the quality of care they receive. This experience with Mr. O was eye-opening. It was a reminder that we must also respect the wishes of our patients and provide them with the care they need, even if it means letting go. It was also a lesson in the importance of communication, both with our patients and their families, and with our colleagues.
I am grateful for this humbling moment inmymedicaleducation.Nomatterhow
Volusia County Medical Society
Welcomes 2023 New Members:

RossWheeler,MD–SkinDermatologyandCosmeticSvcs.
JayaBadhwarKumar,MD–FloridaRetinaInstitute
DennisWen,MD–SportsMedicineHalifaxHealth
RebeccaPeck,MD–FamilyMedicine
LindsayLucas,MD–TheOrthopedicClinic
BenjaminPeck,MD–FamilyMedicine
William“Champ”Douglas,MD–FamilyMedicine
HughColeman,DO–GeneralMedicine
MariaNovoaVillavicencio,MD–HalifaxOB/GYN
PaulGraham,MD–OrmondDermatology
much we may wish to cure our patients, therecomesatimewhenwemustaccept the inevitable and provide comfort and care in their final days. It also reminded me of the importance of empathy and compassion, and the vital role that medical professionals play in helping patients and their families navigate the difficultjourneytowardstheendoflife. Offeringahandtoholdmayseemlikea small gesture, but its value cannot be overstated. It allowed me to meet Mr. O where he needed me most. This is the true essence of patient-centered care, showing him that, whether this was our firstor30thencounteroftheday right then, in that exact moment, he was the onlypersonthatmattered.
ZophiaMartinez,DO–RadiologyImagingAssociates
TravisFuchs,MD–RadiologyImagingAssociates
JonathanFriedman,MD–RadiologyImagingAssociates
BoydHatton,MD–RadiologyImagingAssociates
JesseGreenblum,MD–HalifaxHealthOB/GYN
JulieDegele,MD–FamilyMedicineHalifaxHealth
LarissaRaymond,MD–FamilyMedicineHalifaxHealth
Dr.ClaudiaLagoToro,MD–BreastCancerSurgicalOncology
MiriamStaub,MD–Psychiatry/BehavioralHealthFHCP
Medicine – Daytona Beach Regional Campus Class of 2024As many of you know, my last 20 years of work have been about helping patients not only lowering weight, but reversing disease. Our intestinal biome and its health has everything to do with our personal health and the health of our patients. Every year, I try to focus not only on educating on the pathophysiology of disease as it’s currently discussed in the literature, but also on an overarching theme, and this year it's the biome.

I have decided to make 2023 “The Year of the Biome - Our Newly Discovered 'extra organ’.” The nature of the biome, how to maximize its impact on our health, the details of its functions and interactions with our body, are profound and the knowledge around it is growing rapidly.
There are many important details on how this biome is impacted not only by nutrients, but also by sleep, exercise, spirituality, and the community you keep. This month I will focus on the vitamins our biome makes and how these vitamins impact us and our patients. In our Shield of Life “Heal Program" we have 9 core videos every participant receives explaining the pathophysiology of disease which is constantly changing. Now our Shield of Life company is developing a learning management system (LMS) to break these key lectures down into more specific learning bites.
Our video number 9, for example, is on the biome: “Understanding the Intestinal Biome, the Bacteria in Your Gut, and How They Can Help You Make the B and K vitamins.”
After reviewing many complex scientific articles on how B an K vitamins are created by a healthy biome and their impact on our health, I decided to summarize them in an article our monthly coaching group of clients reviewed and would now like to share it with you to help you understand the level of education and guidance our participants receive. If any of you have seen my husband's, Dr. Scott Klioze, more sophisticated educational videos on YouTube, please forgive my much simpler graphics, as I'm not an engineer!
In order to begin this discussion, we must first understand the makeup of our intestinal tract. The picture or cartoon below depicts one wall of our intestine and the bacteria in our intestine, the biome.
Here you see the tight junctions and the two mucosal layers (inner and outer layers) which are vital to the health of our intestinal wall and body. If there is a breakdown of the mucosal layers and tight junction between intestinal cells (epithelium), you can get “leaky gut” or intestinal permeability leading to many diseases.

Some of these include autoimmune, inflammatory bowel, diabetes, obesity, cancer and cardiovascular diseases, etc. As you know from our previous review, Lecture 3: Grain and Free Radicals, free radicals can disrupt cell walls and cell wall function.
Keeping the intestinal barrier in check depends on a healthy diet, adequate sleep and exercise, and avoiding free radicals including diets high in glucose, fructose, saturated fats and chemicals; but, a big part is maintaining adequate vitamin D levels!
Vitamin D activates vitamin D receptors (VDR) that activate reactions inducing the formation of many of these tight junctions and help maintain a strong mucosal barrier.
Now that we understand a healthy intestinal wall depends on a healthy lifestyle, avoiding free radicals and maintaining healthy vitamin D levels, we can next address our intestinal or gut biome, the bacteria in our intestines.
Ahealthy gut biome is a diverse biome made up of a variety of bacteria and other organisms. Often it is referred to as a “rainforest” as it has many players including bacteria, eukaryotic and archaea, but also protozoa, fungi and viruses. We will focus on the bacteria.Ahealthy diverse biome is primarily made up of bacteroidetes, and firmicutes and, on a smaller scale, by actinobacteria, proteobacteria and verrucomicrobia. They all work symbiotically with the human body and have been noted to affect our circadian rhythm, help make neurotransmitters, endocrine hormones, stabilize the immune system to control inflammation, infection, prevent cancer, and also make vitamins.
The primary ones are the B and K vitamins. For our biome to be productive, it must be healthy and it requires nutrients, vitamins, elements and a healthy gastrointestinal tract.
The microbiome produces micronutrients like the B and K vitamins, but also requires them for survival. Currently, research shows that the majority of our B and K vitamins comes from our diet, but our gut biome makes a large number of them as well. The foods that have most B and K vitamins include: broccoli, Brussel sprouts, cabbage, kale, spinach, liver, seafood, poultry, eggs, seeds etc.
Our gut biome not only makes vitamins, but helps regulate the absorption of vitamins and minerals from our diet. Interestingly, our biome helps regulate the absorption of certain vitamins such asA, B, C, D, E and K; and minerals such as calcium, iron, zinc, magnesium and phosphorus. Yes, the biome makes the B and K vitamins, but it also helps regulate the absorption of the exact levels we need. Now you can see why it is so important to eat your vegetables, as they are full of these vital nutrients that help us, but also help the gut bacteria do their job. In addition to the vitamins and minerals we mentioned above, the gut bacteria need fiber, and vegetables have a lot of fiber! Diets higher in protein lead to microbial by-products that can slow down gastric emptying, therefore inducing constipation. Have you ever been constipated after eating a high protein diet?
Often, when processed foods are lacking in important vitamins and minerals, the industry modifies the food item by “fortifying" it with x minerals, vitamins etc. So, yes, you’re getting the vitamins and minerals, mostly chemical, but why settle when you can get them naturally from vegetables?
Another very important point, for a healthy diet with appropriate vitamins and minerals, is that certain vitamins (A, B2, D, E & beta-carotene) help increase the abundance of the biome while others help maintain its biodiversity (A, B2, B3, C, K) and quality (vitamin D). VitaminsAand D help with the immune response via supporting the mucosal lining which provides intestinal and biome health. Vitamin B2 and E help produce more bacteria that generate short chain fatty acids. Remember we mentioned them in lecture 9? Short chain fatty acids are post-biotic or the “poop” of the bacteria. Post-biotics act as an anti-inflammatory agent to the body and organs. I know, “gross”, but we do depend on a “healthy” biome, therefore we must choose wisely to stay healthy.
So, does this mean you need to run to the store and buy all these supplements? No!This is why over the 20 years of working with patients, I have seen crazy and really amazing changes in people's bodies and their body's ability to overcome disease by just eating more vegetables and taking certain extra vitamins and minerals.
If you have been following our Shield of Life program for a while, you can see that part of the reason your body is transforming, is because the foundation of our “Healthy Food Choices” nutritional platform is providing you with these vitamins and minerals your body has perhaps not only been missing, but maybe even craving! We want to empower you with the understanding of how your body works, so you will resist putting bad fuel in your engines, but strive to always make correct choices.
Below I will summarize just what the B and K vitamins do for you: There are eight B vitamins (B, thiamine, B2, riboflavin, B3, nicotinic acid, B5, pantothenic acid, B6, pyridoxine, B7, biotin, B9, folate, and B12, cobalamin).They are water soluble and are produced by the microbiome. Currently it is felt we need more than what the biome produces, especially in patients with inflammatory bowel disease, diabetes and other metabolic diseases, but this could be the current state of our unhealthy bodies and biome.
Vitamin B1 -Thiamine is a key vitamin in the generation of cellular energy from glucose. Many bacteria make thiamine and its exact role is not know, but it is felt to be involved in intestinal immunity.
Vitamin B2 - Riboflavin helps in the redox reaction to reduce free radicals: it's an anti-oxidant. It also promotes healthier bacteria, where in its absence there are more pro-inflammatory bacteria in the biome. It also promotes healthy intestinal mucosal and when there is a deficiency, the intestinal lining is inflamed.
Vitamin B3 - Nicotinic acid like Vitamin B2 is a very important cofactor in decreasing free radicals. Many of the bacteria that make up the biome have the ability to make vitamin B3.This is also very important in maintaining a healthy intestine and decreasing inflammation in the bowel mucosa. Patients with inflammatory bowel disease have lower vitamin B3 levels and treatment with vitamin B3 have shown improvement in acute intestinal cell inflammation.
Vitamin B5 - Pantothenic acid is important in metabolic pathways that help generate cellular energy, neurotransmitter formation, and breakdown of fatty acids. Several bacteria make pantothenic acid, but several require it to make vitamin B6.
Vitamin B6 - Pyridoxine is important cofactor in making amino acids which are the building blocks of proteins. It is also needed to breakdown proteins. There are many intestinal bacteria that make vitamin B6. As we have seen with many of the B vitamins, a deficiency in vitamin B6 is associated with irritable bowel disease. It is felt that an abundance of pyridoxine induces the activation of anti-inflammatory cytokines, whereas a deficiency causes pro-inflammatory cytokine activation.
Vitamin B7 - Biotin is a coenzyme for glucose breakdown, cellular interaction, epigenetic regulation, and genetic expression. It may be involved in anti-inflammatory activities. Many bacteria make biotin, but there are bacteria that decrease it.
Vitamin B9 - Folate primarily comes from diet, but some comes from gut microbiome. It is involved in cell growth and DNAactivation. When vitamin B9 is deficient, it affects cell survival and proliferation. It is also associated with maintaining the intestinal lining, providing nutrients needed for brain activity, decreasing cytotoxicity of natural killer cells and decreasing lymphocyte growth. Many bacteria in the biome make folate, but when it is deficient, it jeopardizes the integrity of the intestinal lining and has been related to a higher risk of intestinal cancers.
Vitamin 12 - Cobalamin is important in DNA and RNA synthesis, and is involved in the breakdown of protein and fat. It is very important to the central nervous system and the formation of red blood cells. A large majority of the biome requires vitamin B12, but not as many make it. For this reason, a deficiency in vitamin B12 effects the growth of the biome.
Other key vitamins that are made by our biome:
Vitamin K1- can activate clotting the cascade and has effects on bone health. It can stop cancer cells from proliferating, but vitamin K2 is more potent for this.
Vitamin K2 - has anti-cancer properties. It induces cancer cell death (apoptosis) and can stop cancer cells form proliferating. Cancers noted to be affected are liver, colon, bile duct (cholangiocarcinoma), ovarian, pancreatic, lung and bone (leukemia). It is also noted to decrease osteoporosis, and liver cirrhosis.
Vitamin K3 - has anti-inflammatory and anti-cancer effects, but due to its toxicity to liver and disruption of red blood cells in carrying oxygen, it is not used.
In general the B vitamins should not be taken in isolation other than vitamin B12. I hope this sheds some light on the power of the biome and of a healthy diet.
In conclusion, we have reviewed the importance of our intestinal biome, the bacteria in our intestine, and the vitamins B and K that our microbiota produces. We have discussed how the vitamins and minerals from our diet are necessary for our gut bacteria to thrive and produce these vitamins, but also for our body to absorb the exact levels of vitamins and minerals we need. We have also discussed how these vitamins have several roles in maintaining a healthy intestinal lining, decreasing inflammation, decreasing free radicals, and aiding in DNAand RNAsynthesis. Finally, we have also discussed how vitamin K1, K2 and K3 have anti-inflammatory and anti-cancer properties.
It is important to remember that in order to maintain a healthy intestinal wall and microbiome, we must maintain a healthy lifestyle, a diet high in vegetables, avoid free radicals and maintain healthy vitamin D levels. In addition, we must also be mindful of the vitamins and minerals our microbiome needs to thrive and make the vitamins we need to maintain a healthy body.

1. Akimbekov NS, Digel I, Sherelkhan DK, Lutfor AB, Razzaque MS. Vitamin D and the Host-Gut Microbiome: A Brief Overview. Acta Histochem Cytochem. 2020 Jun 26;53(3):33-42. doi: 10.1267/ahc.20011. Epub 2020 Jun 16. PMID: 32624628; PMCID: PMC7322162.
2. Sun J, Zhang YG. Vitamin D Receptor Influences Intestinal Barriers in Health and Disease. Cells. 2022 Mar 27;11(7):1129. doi: 10.3390/cells11071129. PMID: 35406694; PMCID: PMC8997406.
3. Gut microbiome–micronutrient interaction:The key to controlling the bioavailability of minerals and vitamins? Journal article·2022·Barone, D'Amico, Brigidi,Turroni
4. LA Frame, E Costa, SA. Jackson. Current explorations of nutrition and the gut microbiome: a comprehensive evaluation of the review literature. Nutr Rev, 78 (2020), pp. 798-812, 10.1093/nutrit/nuz106
5. Hossain KS, Amarasena S, Mayengbam S. B Vitamins and Their Roles in Gut Health. Microorganisms. 2022 Jun 7;10(6):1168. doi: 10.3390/microorganisms10061168. PMID: 35744686; PMCID: PMC9227236.
6. Xv F, Chen J, Duan L, Li S. Research progress on the anticancer effects of vitamin K2. Oncol Lett. 2018 Jun;15(6):8926-8934. doi: 10.3892/ol.2018.8502. Epub 2018Apr 16. PMID: 29805627; PMCID: PMC5958717.
Each year, the Educational Foundation proudly partners with Daytona State College to provide a medical track student with a Scholarship. This year we announce the Scholarship was awarded to O’Liyah Wilson. Best wishes to you on your way to becoming a CRNA!

Volusia County Medical Society Educational Foundation is a tax exempt 501(c)3 and your contribution matters! Send a check to PO Box 9595, Daytona Beach, FL 32120. Together we can make a difference!
Are you a Volusia County physician that is not a Member yet? Join us!
www.vcms.org

Over 50% of women in Volusia County use Medicaid insurance to obtain prenatal care. Over half of these women can’t find any. First trimester access to prenatal care has declined. Maternal death rates have increased. In 1929, Dr. Howard Haggart wrote:
“The position of woman in any civilization is an index of the advancement of the civilization; the position of woman is gauged best by the care given her at the birth of her child. Accordingly, the advances and regressions of civilization are nowhere seen more clearly than in the story of childbirth.” A century later, we are observing the regression of our county’s health and future prosperity in the egregious lack of care we tolerate for our mothers and babies.
In 2011, Florida privatized the state’s Medicaid system. Florida, like other states, hoped to transfer to a third party, the responsibility of assuring that Medicaid dollars reached Medicaid covered citizens for their healthcare. As stated in 2015 by D. Douglas Stephenson in the Gainesville Sun, “The companies are paid by state government and their profit depends on spending as little as possible on Medicaid patients It’s hard to imagine any greater disconnect between public good and private profit.” Presented to Floridians as a cost savings measure, privatization rolled out and by 2015, the insurance companies stated they were over $500 million in the red, and requested increases in rates that eliminated the anticipated cost savings. It is now 2023 and Medicaid ingests 48% of the state budget. Again, half of our mothers cannot get prenatal care. In what world can this be considered a success? This privatization is a failed venture and those in the position to rectify this situation need to admit that the emperor is not wearing any clothes.
In a state that already is spending 32% of its budget on Medicaid, the legislators consider Medicaid expansion off the table. And one should ask why isn’t 32% of the State budget enough? Shouldn’t one half of Florida’s budget be able to create accessible health care? And shouldn’t we at least be prioritizing pregnant women?
Nowhere is the emperor’s nakedness more apparent than in care for childbirth. And we cannot ignore the birth of babies because babies must be born. They need to be if we are to survive as a species. A civilization that acknowledges this should protect childbirth as if its existence depended on it, because it does.
Prior to 2011, the Volusia County Health Department ran a perinatal care clinic, with Halifax Health Family Practice Residents and community physicians. Women came to one of three sites and their pregnancy was confirmed, their applications for “Pregnancy Medicaid” were completed on site, coverage assured in 72 hours and a visit scheduled. Women were also networked to needed services. The private Medicaids lowered reimbursements to these clinics and large health departments closed them. Smaller counties that could prove they have no other prenatal care providers maintained “carve outs.”
Halifax Health and Advent Daytona Beach opened prenatal clinics intended to make up for the loss of the VCHD clinic, but they fall far short. “Secret shoppers” have called both these clinics and told eight weeks until the first visit. Not one private office would schedule any pregnant patient with Medicaid and referred them to the two hospital-based clinics. It is estimated that Volusia needs 18 additional obgyn physicians to cover our pregnant population.
When the state privatized the Medicaids, The Department of Children and Families, tasked with overseeing enrollment, discontinued access to onsite Medicaid enrollment navigators. All applications are to be completed online. This assumes that women have access to the internet and can navigate the tortuous application. Any blanks, inaccuracies, or current enrollment in non-pregnancy Medicaid delays the process
and it now can take over two months.
So, too many women do not have Medicaid coverage before their fifth month, and then cannot find a provider who will take them. We are seeing more women arrive at our hospitals in preterm labor with complications that could have been avoided or minimized. This means longer hospital stays for moms and babies, with long term consequences and costs.
Other parts of Florida have developed relationships between the maternity hospitals, taxing authorities, Healthy Starts, Federally Qualified Health Care Centers, doctors, and health departments. They have created collaborative clinics that provide early and consistent perinatal care. It is reflected in the outcomes of their mothers. The counties in Florida that do not have these collaborations are experiencing similar access issues and higher morbidity for mothers and babies. Volusia County has all the players—two taxing authorities, three hospitals, a health department, a Healthy Start Coalition, three FQHC ‘s and obstetricians. Yet, Volusia County fails to provide access to prenatal care for most of its pregnant population.

This is not an insignificant concern. This is a dumpster fire on which we are spraying gasoline, as the few remaining local physicians stop seeing Medicaid covered moms. Issues of diabetes, hypertension, obesity, domestic violence, and substance abuse are now belatedly treated in our hospital triage units, as women arrive with emergencies that could have been avoided, addressed earlier, less expensively and more effectively. The cost for “the system” pales in comparison to the poor outcomes for mothers in our community.
AHCA, DOH and our legislators must hold the private Medicaids accountable for providing the health care they promise. The Medicaids need to assure early access to care and realistic rates for providers. DCF needs to create access to Medicaid enrollment and assure that women don’t have to wait months to start their search for a prenatal care provider. And Volusia County needs to hold all the stakeholders accountable and demand a collaborative system that uses all funds effectively, filling in gaps and avoiding duplications in administrative services and oversight.
Perhaps, if enough of us acknowledge this crisis and work to restore care for our women, we can reach 2029, one hundred years after Dr. Haggard’s wrote his book and show that our civilization is again advancing.
Way out yonder in the rural part of Volusia County lies the small town of DeLeon Springs population 2,481 (2023 census). Passing many horses and cattle ranches for thirty minutes after leaving Ormond Beach farms, we pulled into Karling’s Inn. This quaint restaurant that has been a local fixture for over 30 years is still worth the trip. Not too long agotheowners,ChefJimmyBuzzaandhiswifeLilyopenedtheTwinBrothersKafenextdoor.Namedaftertheirtwin boys,BurleyandElliot,theymakehomemadebakedgoodsandservebreakfastandlunchfrom9-2Wednesday through Sunday.DinnerisinKarling’sfrom5-9WednesdaythroughSaturday.
Entering the German farmhouse style eatery, the hostess led us to our table. The menu was then presented to us along with a sample of their Kafe bread served warm and wonderful. Karling’s is noted for their German fare and seafood. Appetizers ranged from Escargots (French snails, Muenster cheese, tomatoes, concasse and garlic butter) toAngels on Horseback (lightly breaded oysters wrapped in bacon, fried, and served with Bérnaise sauce).The classic French onion soupbakedtoorderwithhousemadebuttercheese,andofcourseBavariansausagewithsauerkraut.

We went straight to the entrées. Lisa and I decided to share two entrées. The first was the Roast Crispy Duck Montmorency which was half a deboned duck and served with apple dressing and cherry bing sauce. It came with a side of a scrumptious potato pancake and an incredibly delightful German cucumber salad. We enjoyed it but we felt the duck was somewhat overcooked. We also chose the absolutely mouthwatering, satisfying Karling’s black grouper which was a 10 oz. thick cut, sautéed with a creamy Scotch sauce with 2 jumbo shrimp, roasted peppers, olives, and pine nuts.This came with the potato pancake and a great cheese covered spätzle with which my glass of Ruffino Pinot Grigio from Italy paired well. One of our friends that joined us for this great meal ordered an end cut of prime rib that hethoroughlyenjoyedandwascookedperfectly.

Yes of course we saved room for dessert. Lisa and I thoroughly enjoyed the Key Lime BakedAlaska, and our friends shared their apple strudel with vanilla ice cream which was amazing as well. Our total bill for Lisa and myself without tip was just over $100. Karling’s is located at 4640 US Highway 17. Be prepared that they only take Visa and Mastercard. They serve beer and wine as well as after dinner cordials. They have a Kids menu as well. Reservations may be made by calling (386) 985-5535. I give Karling’s Inn: Ambience 5 stethoscopes Quality of food 4 1/2 stethoscopesValue4stethoscopesService4stethoscopesIknowwe’llbebacktodineagainrealsoon!





Are you a Volusia County physician and want to know more about becoming a member of the Medical Society. For over 100 years, the Volusia County Medical Society (VCMS) has been here. We keep you informed when legislation threatens your profession. We provide dinners, holiday parties, continuing education courses, social events, and gatherings throughout the year.
Membership Benefits:
Physician Referral Service
Online Directory
Legislative Updates and Voice
24/7 Access to Healthcare Attorney on Call
Exclusive Webinars and CME Courses
Access to Free Confidential Mental Health sessions
Annual Daytona State College Scholarship Partnership
Medical Student and Medical Residency Memberships
The Stethoscope Journal, a member driven magazine with Member articles
Access to community banking, investing and insurance companies
Monthly Digital Newsletter posting current articles, legislative news, and VCMS events

Job postings and referral service
Social Networking Events, Outings and more…
New or Returning Members – talk, type or text for a membership application or visit us online www.vcms.org docs420@aol.com (386) 255-3321