4 minute read
Mohs Micrographic Surgery: A Marvel in Dermatology
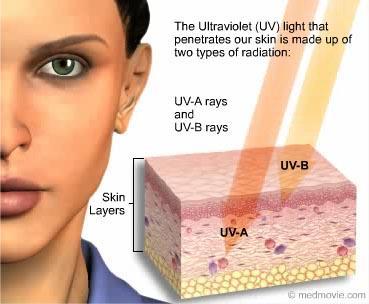
According to the American Cancer Society, skin cancer is by far the most common type of cancer worldwide. Non-melanoma skin cancer accounts for approximately 3million cases in the United States eachyear withtheincidence continuing toclimb. Approximately1out ofevery 3cancers diagnosed worldwideisaskincancer.Additionally,1outofevery5Americanswill develop a skin cancer during their lifetime. The two most commontypes of non-melanoma skin caner arebasal cell carcinoma (BCC)andsquamous cell carcinoma (SCC).Basal cell carcinomaaccounts for approximately 80%of all non-melanoma skin cancer diagnoses. Chronic sun exposure is the single most important cause of all forms of skin cancer with damage oftenoccurring during childhood and adolescence years in those who practice poor sun protection habits.
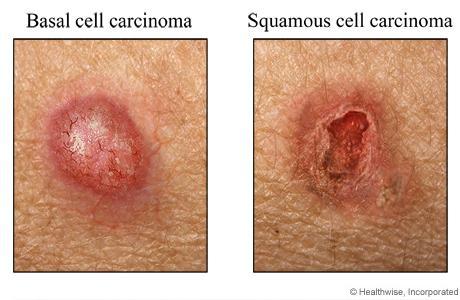
Basalcellcarcinomavs.Squamouscellcarcinoma
Advertisement
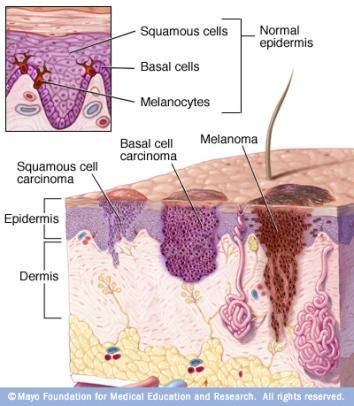
Basal cell carcinoma is the most common type of skin cancer worldwide, occurring primarilyin fair-skinned individuals with a history of sun exposure. Risk factors include numerous blistering sunburns, immunosuppression, family history of BCC, and a history of radiation exposure. Basal cell carcinoma develops from cells contained withinthe bottom layer of the epidermis called the basal layer. Fortunately, theyare often slow-growing with a very lowrate of cancer cell spread (metastasis) outside the primary site of occurrence. It is very importantto have all BCCs treated to preventlocal surroundingskindestructionifleftuntreated.
Squamous cell carcinoma (SCC) isthesecond most common form of skin cancer worldwide.The majority of SCCs develop in individualswith a history of chronicsun exposure. The closer to the equator one lives, the more likely that individual willdevelop SCC. The immune system also plays an important role in the development of SCC. Those that are immunosuppressed or on immunosuppressive medication have a significantly higher risk of developing SCCs. Certain high-risk types of thehuman papillomavirus (HPV) may also play a role in SCC development. This type of skin cancer develops from cells that make up the bulkof the epidermis. Squamous cell carcinomahasaslightlyhigherriskduetoitsabilitytospreadintobloodvesselsandnerves.Itisforthisreasonwhy theyshouldbeproperlytreatedearlyon.
Numerous treatment options exist for these non-melanoma skin cancers, including the use of topical immune system modifyingmedications (5-flurouracil, imiquimod, ingenol mebutate), cryotherapy (freezing), electrodessication and curettage(“scraping and burning”), surgical excision, and Mohs micrographic surgery. After beingdiagnosed with a non-melanoma skin cancer, your physician will determine the besttreatment option based on the lesion size, type, location, and aggressiveness of the skin cancer. Some skin cancers have small “roots” that may extend deeper in the skin, beyond what we can see on the biopsy. Intheseinstances,surgicalinterventionisneededtocompletelyremovethe skincancer.

WhatisMohsmicrographicsurgery?
Mohs micrographic surgery provides a highly specialized and effective treatment option in patients with qualifying skincancers.Thisprocedurehasa97-99%curerate,which is superior to manycancer treatments in medicine. Mohs micrographic surgery was developed in 1938 by Dr. Frederick Mohs, a surgery professor at the University of Wisconsin. With this specialized procedure, the skin cancer is conservatively removed while simultaneouslyattempting to preservenormal skin. The removed portion of theskinis then carefully mapped, color-coded, and prepared for examination under the microscope, which all takes place withinthesameday.
The Mohs surgeon will meticulously examinethe tissue specimen and determine if any residual skin cancer is present. If residual tumor is found, the Mohs surgeon will only go back to that specific location to remove another small portion of tissue. One of the most important aspects of Mohs microscopic surgery is the ability to examine approximately100%of the skin margins under the microscope, ensuring that all of theskin cancer is completely removed prior to closingthesurgicalwound.
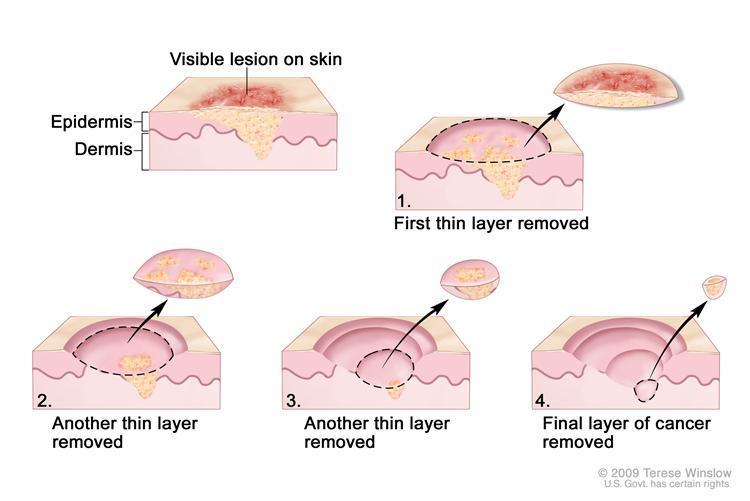

In contrast, a conventionalsurgical excision requiresseveral days for both tissue processing and microscopic examinationby a trained dermatopathologist. During this process, only approximately 1%of the skin margins are examined. This small percentage of examined skinmay contribute to a higher rate of recurrence if adequate surgical margins are not taken at the time of the surgery. In the event that more skin cancer cells are found in the examined skin,thesurgeonwillthereforehavetoperformasecondsurgicalexcisiontocompletelyremovetheresidualtumor.
WhataretheindicationsforMohs micrographicsurgery?
∙ Largeskincancersonthehead andneck
∙ Skincancersinareaswhere preservationofnormalskinis vital
∙ Face,scalp,neck,nose, ear,eyelids,lips,hands, andgenitalia
∙ Sitesofhightumorrecurrence andriskoftumorspread
∙ Recurrentskincancers
∙ Aggressiveskincancers
WhatcanIexpectduringtheprocedure?
Mohs micrographic surgery involves a series of stages consisting of the surgical excision followed by immediate microscopic examination of the tissue. TheMohs surgeon is focusedon removingthe least amount of tissue, while still providing adequate surgical margins to completely removethe skin cancer. Initially, it is not possible to know the final sizeof the surgical wound. This is often dependent on the number of stages that are required to completely remove the skin cancer cells. For reference,approximately50%ofallMohsmicrographicsurgery cases require at least 2 stages for complete skin cancer clearance.After all theskin cancer cells are removed, the Mohs surgeon will surgically close the wound and the procedure will becomplete. Some wounds may be too large for simple closure and willrequire a skin graftor flap. In this case, the Mohs surgeon will design a closure that willpreserve the skin’s function and movement, while reducing the appearance of the scar. Stay tunedforafuturearticleonskingraftsandflapsusedinwoundclosure.
WhatshouldIexpectaftertheprocedure?
FollowingMohs micrographic surgery, it is recommended to minimize strenuous activity to reduce tension on the wound and decrease the risk of bleeding from blood pressure elevation. Pain is usually minimal butTylenol may be taken for discomfort. Suture removal time canvary depending on the location of the surgical wound,ranging from 5-14 days. Keep in mind that it often takes 12months for the surgical wound to regain similar strength of the surrounding skin. Surgical site redness may take up to 6 weeks to fade.The appearance of the scarwillfade over time, but incasesof elevated (hypertrophic or keloidal)scars, steroid injections may be used to assist inflattening. Various options exist for the treatment of noticeable scars including resurfacing lasersandmicroneedlingifthecosmeticresultisunacceptable.
AdvantagesofMohsMicrographicSurgery
∙ Highestcurerateofalltreatmentproceduresforskin cancer
∙ Preservationofnormalskin,allowingfora goodcosmeticoutcome,whilereducingthe appearanceofthesurgicalscar
∙ Lowassociatedriskwithlocalanesthesia(numbing)in anoutpatientsetting
References:
1. James,WilliamD,DirkM.Elston,TimothyG.Berger,andGeorgeC.Andrews. Andrews’Diseases of the Skin: Clinical Dermatology.London:Saunders/Elsevier,2011.Print.
2. http://www.cancer.net/cancer-types/skin-cancer-non-melanoma/statistics
3. http://www.dermatology.ucsf.edu/skincancer/mohs.aspx
4. http://www.who.int/uv/health/uv_health2/en/index1.html
5. http://www.skincancer.org/skin-cancer-information/mohs-surgery/mohs-overview
Florida State University Department of Behavioral Sciences and Social Medicine
ACTS2 Project:African-AmericanAlzheimer’s CaregiverTraining and Support
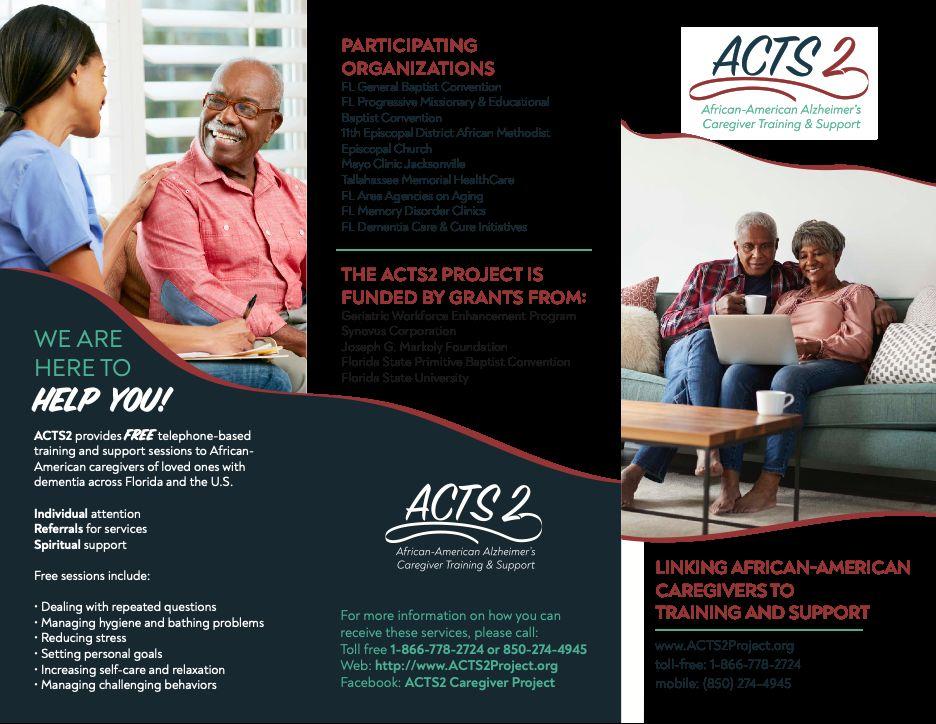
TheACTS2 Project meets the needs of distressed caregivers of older adults with dementia.The program offers faith-integrated, skills-training and support over toll-free telephone to African-American dementia caregivers residing in Florida.ACTS2 also conducts a robust outreach effort to raise awareness about dementia through social media and community-based presentations (reaching over 7,000 annually), while also providing no-fee, telephone-based consultations and community referrals to caregivers and other stakeholders across Florida and the U.S.
Research has found manyAfrican-American adults do not participate in social service programs outside their culture and community. In addition, financial challenges and limited transportation options to get to appointments prevent caregivers from accessing help.To overcome these barriers, ACTS 2 has successfully trained 23African-American faith community workers (lay pastoral care facilitators) to deliver faith-integrated, skills-building and support sessions (a 12-part series ranging from relaxation training integrated with prayer and meditation to problem-solving through goal setting). Over 150 family caregivers have enrolled in the 12-sessionACTS2 program over the past 4 years. Caregivers reported: significant improvement in health and emotional well-being significant improvement in self-identified caregiving and self-care problems
· strong bonds between caregivers and lay facilitators who offer ongoing support
· very positive perceptions of the usefulness of the program
Current Funding
The U.S. Health Resources and ServicesAdministration Geriatric Workforce Enhancement Program, Florida State Primitive Baptist Convention, WinterFall Night of Giving, Joseph G. Markoly Foundation, Synovus Corporation, Florida State University College of Medicine, and private donors provide financial support to theACTS2 Project.




