Wellness Hub
Wellness Hub
Relaunched
Nurturing the heart of veterinary care

IPP ... what?
Introduction to intermittent positive pressure ventilation specifically under anaesthesia
Small animal endoscopy in veterinary nursing: A guide
Levelling up your consulting nurse game
The Official Journal of the Veterinary Nurses Council of Australia Inc. Reg. No. A0031255G ABN 45 288948433 VOL. 30 • NO. 01 • MARCH 2024 THE AUSTRALIAN VETERINARY NURSES JOURNAL
for vet nurses and technicians
Lauri
Cert
DipTDD, AVN, TAE, DipBus, Dip.Couns, DipBA, DipMgt, Cert IV CAS
Janet Murray
BSc Veterinary Nursing, AssocDegAdult&VocEd, Cert IV TAE, RVN, AVN
Elise MacPherson
Dip VN (GP) & SURG, Dip Lab Technology (Pathology Testing), Cert IV VN, RVN, AVN Jo Hatcher
Dip VN, Cert IV VN, Cert IV TAE, RVN, AVN
Shauna James
Cert IV VN, GradCertCaptVertMgt (CSturt), RVN
VNCA NATIONAL OFFICE
PO Box 7345, Beaumaris VIC 3193
Phone 03 9586 6022
Fax 03 9586 6099
Web www.vnca.asn.au
ADVERTISING
Phone 03 9586 6022
Email vnca@vnca.asn.au

VISION STATEMENT
The VNCA aspires to strengthen the position of Veterinary Nurses as part of the veterinary healthcare profession.
MISSION
The VNCA: Serves and represents all Veterinary Nurses
Protects the professionalism of Veterinary Nurses
Promotes the value of Veterinary Nurses as vital in delivery of quality veterinary care
Advocates for the increased recognition of Veterinary Nurses across Australia
Supports Veterinary Nurses through the provision of continuing education and networking opportunities
Strengthens the position of Veterinary Nurses across the veterinary industry Engages all Veterinary Nurses across the veterinary industry.
01
President’s report
02 Wellness Hub – Nurturing the heart of veterinary care
04
06
AVNAT – Recency of practice demystified: Essential insights for veterinary nurses and technicians
Wellness Hub – Setting your new year workplace goals
08 IPP … what? Introduction to intermittent positive pressure ventilation specifically under anaesthesia
14 Levelling up your consulting nurse game
16 Small animal endoscopy in veterinary nursing: A guide
24 Meet VfCA’s Rural and Regional Program
Case Report – Proximal interphalangeal (PIP) joint arthrodesis in a warmblood
32
Client fact sheet – Fear and stress-free treats for dogs
34 Member Vitals – Tamaryn Bond and Tarlea Hann
37 Congratulations to our AVNs and

Cover image ©shutterstock/PeopleImages.com - Yuri A CONTENTS Contents VOLUME 30 • NO. 01 • MARCH 2024 NEWS & UPDATES
26
OUR VISION & OUR MISSION 14 08 06 THE AUSTRALIAN VETERINARY NURSES JOURNAL BOARD OF DIRECTORS President Gary Fitzgerald Vice President Trish Farry Michelle Foxcroft, Anita Parkin, Rebecca Coventry, Asha Yeoman, Samara Blake VNCA MEDIA CHAIR
Murray Email media@vnca.asn.au EDITORIAL COMMITTEE
Murray Lauri Steel Elise MacPherson Shauna James REVIEW PANEL
AVNAT registered professionals
Janet
Janet
Steel
IV VN, DipVN (ECC & GP), DipVET,
President’s report
Dear VNCA Members,
I trust this message finds you well. In the busy months since our last AVNJ, our commitment to advancing the veterinary nursing and technician profession has led to significant developments that I am excited to share with you.
OUR COLLABORATION WITH AVBC FOR VN AND VT REGISTRATION
In December, the AVBC convened a workshop, inviting the VNCA and several other stakeholders to establish a pathway towards statutory regulation for veterinary nurses and technicians in Australia. The day saw robust discussions and diverse perspectives from stakeholders.
ANZSCO SUBMISSION – SHAPING THE FUTURE
In December, the VNCA submitted recommendations to the Australian and New Zealand Standard Classification of Occupations (ANZSCO). Our proposal suggests future-focused changes, including updates to occupation titles, minimum qualifications, and listed skills. We advocate for recognising advanced practitioners with the addition of an Advanced Veterinary Nurse/Technician category. Additionally, we support elevating Certificate IV in Veterinary Nursing to a diploma level, fostering academic career pathways.
ADVOCATING FOR POSITIVE CHANGE – NSW RADIATION REGULATION FEEDBACK
Our active involvement in shaping the future of our profession was evident when we provided feedback on proposed changes to the NSW Protection from Harmful Radiation Regulation.
Committees, including AVNAT, Professional Advancement, and NSW, collaborated on a detailed submission under the oversight of the Board of Directors. This engagement reflects our commitment to positive change benefiting veterinary nurses and technicians.
NEW MEMBER ASSISTANCE PROGRAM – PRIORITISING WELLBEING
A huge thank you to the Membership Committee for their efforts to produce our most recent member benefit. The VNCA has partnered with Converge International to provide members with access to a highly regarded Employee Assistance Program (referred to as MAP – Member Assistance Program), commencing January 15, emphasising holistic wellbeing. This initiative aims to provide valuable support to our members, contributing to your overall wellbeing.
VNCA/ROYAL CANIN/LINCOLN INSTITUTE PARTNERSHIP –FOSTERING LEADERSHIP
We are thrilled to announce our partnership with Royal Canin and the Lincoln Institute, offering 150 sponsored positions for VNCA members in the ‘Emerging Leaders Course’. Emphasising non-clinical skills development, this initiative seeks to elevate the leadership potential of veterinary nurses and technicians.
STRATEGIC PLANNING FACILITATED SESSION – SHAPING OUR FUTURE JOURNEY
The VNCA Board of Directors participated in a facilitated strategic planning session to meticulously chart our course for the next 3 years. Strategic planning is a pivotal
 Gary Fitzgerald VNCA President
Gary Fitzgerald VNCA President
Your involvement and dedication are the driving forces behind these achievements. Together, we are shaping a brighter future for veterinary nursing and technology. Stay tuned for more updates, and I look forward to celebrating further successes with each of you.
step in ensuring our continued success and growth as an association. This process allows us to align our objectives, identify key priorities, and set a clear direction for the VNCA’s future. Stay tuned for more detailed information about the outcomes of this session as we look forward to sharing the exciting developments that will shape our journey ahead.
Your involvement and dedication are the driving forces behind these achievements. Together, we are shaping a brighter future for veterinary nursing and technology. Stay tuned for more updates, and I look forward to celebrating further successes with each of you.
Warm regards
Gary Fitzgerald VNCA President
FROM THE PRESIDENT DIVISION CONTACTS If you would like to attend a divisional committee meeting, it is important that you RSVP. NSW Melissa Shoard E nsw@vnca.asn.au QLD Jade Davies E qld@vnca.asn.au SA Sonia Van De Kamp E sadiv@vnca.asn.au VIC Danielle Gaynor E vic@vnca.asn.au WA Tracey Woods E wadiv@vnca.asn.au DIVISION CONTACTS it March 2024 1
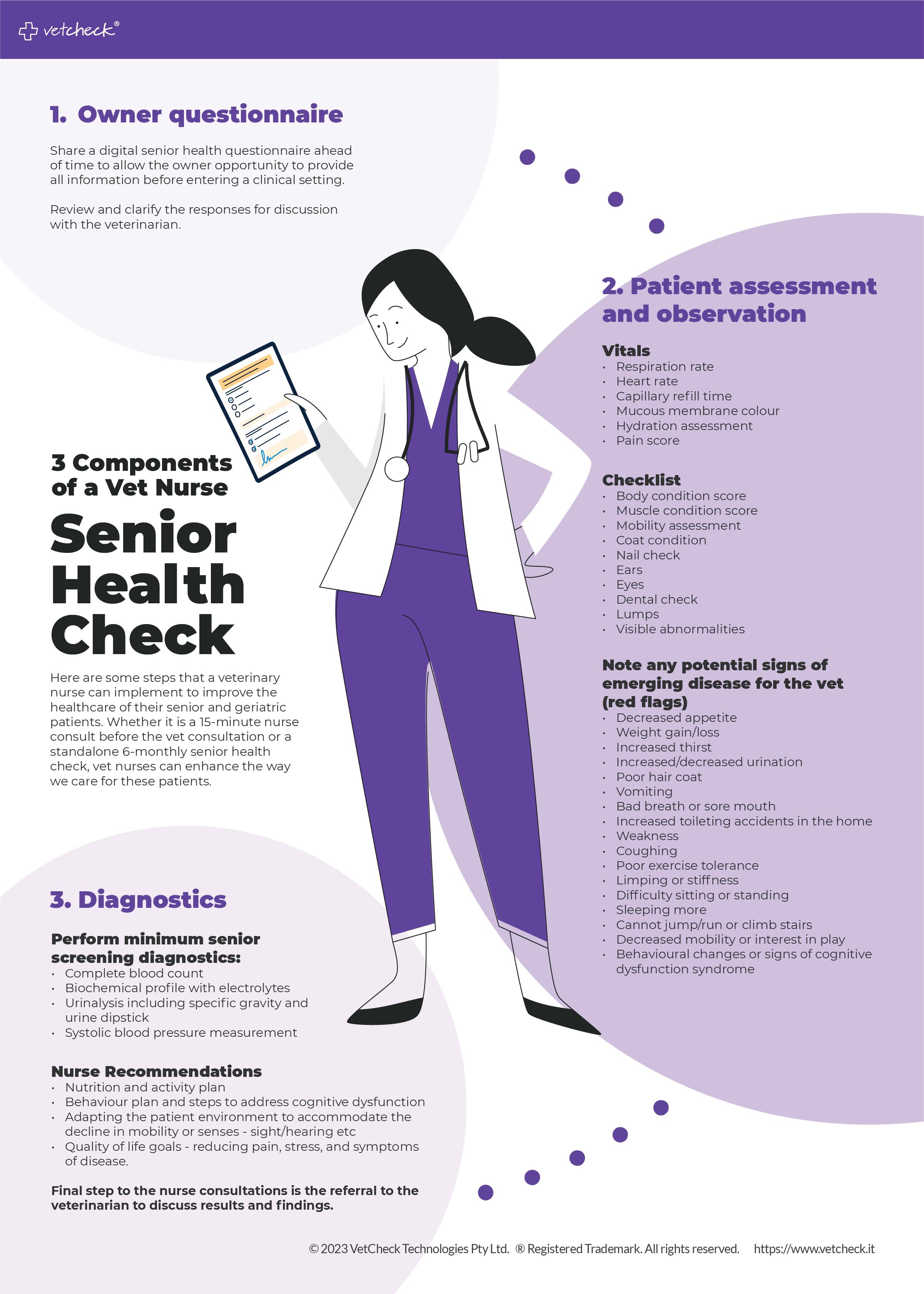
Nurturing the heart of veterinary care
VNCA Wellness Hub relaunch elevates member benefits and workplace wellbeing
In the dynamic world of veterinary care, where compassion meets professionalism, the Veterinary Nurses Council of Australia (VNCA) has taken a giant leap forward with the relaunch of its Wellness Hub. Dedicated to the tireless veterinary nurses and technologists who play a pivotal role in the wellbeing of animals and clients, the revamped Wellness Hub promises a transformative experience that extends beyond individual members to benefit the entire workplace.
A HOLISTIC APPROACH TO PROFESSIONAL WELLBEING
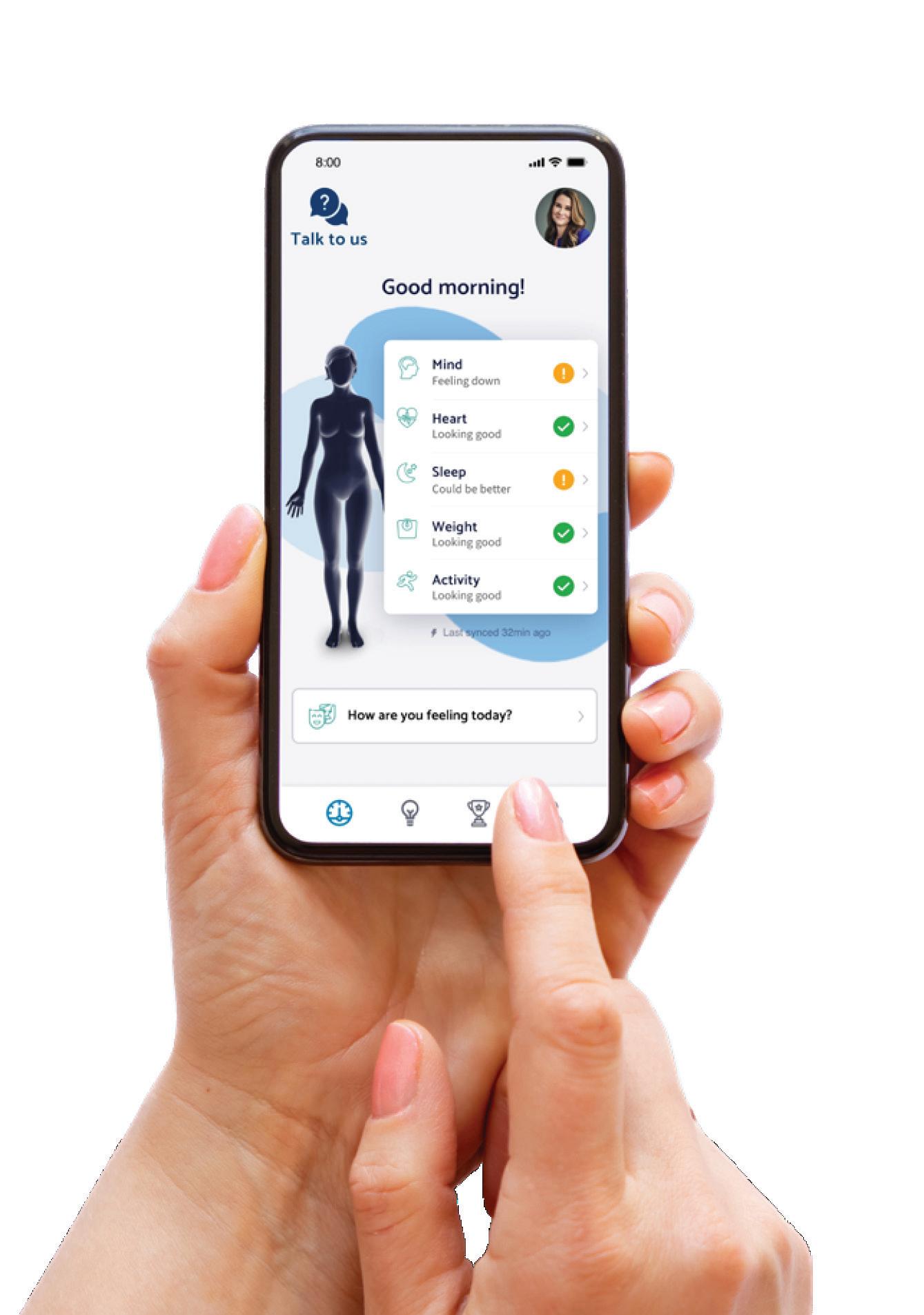
At the core of VNCA’s mission is a commitment to supporting the health and wellbeing of its members. The refreshed Wellness Hub, unveiled as a dynamic space for personal and professional growth, introduces a Member Assistance Program (MAP). This program, developed in partnership with Converge
International, provides comprehensive support to members, acknowledging the unique challenges faced by veterinary professionals.
MEMBER ASSISTANCE PROGRAM (MAP)
The MAP offers a huge range of resources designed to effectively manage both mental and physical health. The program covers a wide range of assistance from career guidance and conflict resolution to nutrition and lifestyle support. VNCA members can gain access to a team of professionals, including organisational psychologists, leadership coaches, and accredited conflict resolution mediators.
The MAP goes beyond the ordinary, offering specialist support for diverse demographics, including First Nations, LGBTQI+, Eldercare, Disability and Carers,
At the core of VNCA’s mission is a commitment to supporting the health and wellbeing of its members.
The refreshed Wellness Hub, unveiled as a dynamic space for personal and professional growth, introduces a Member Assistance Program (MAP).
Student, and Spiritual & Pastoral client needs. This inclusive approach reflects VNCA’s dedication to fostering a workplace culture that respects and supports the diversity within its community.
CONVERGE ONLINE LIBRARY AND WELLNESS APP
In addition to personalised support, members can explore a wealth of resources through the Converge online library. Fact sheets, articles, videos, and animations cover a spectrum of wellbeing topics, empowering members to take control of their health journey.
The award-winning Converge Wellness App further enhances engagement by providing tools, autonomy, self-awareness, and motivation to VNCA members. This initiative aligns with the hub’s commitment to not only address immediate concerns but to empower individuals to proactively manage their wellbeing.
FLOURISH E-MAGAZINE
Stay informed with the latest in health and wellbeing through the Flourish e-magazine. A curated collection of articles and insights from Converge offers valuable perspectives on maintaining a healthy work/life balance.
EDUCATION FOR EVOLUTION
Recognising the ever-evolving landscape of veterinary care, the VNCA continues its commitment to member growth through education and networking opportunities. The education section of the Wellness Hub provides access to ongoing personal and professional development, fostering a culture of continuous learning within the veterinary community.
2 March 2024 WELLNESS HUB

Wellness Hub
for vet nurses and technicians
RESOURCES FOR A BALANCED WORKPLACE
The VNCA understands the pivotal role workplace environments play in the wellbeing of its members. With a focus on promoting mentally healthy workplaces, the resources section of the Wellness Hub offers a curated list of free and accessible resources. Advocating for individual wellbeing not only benefits the members but contributes to animal welfare, staff productivity, and retention.
WITH THANKS TO WELLNESS HUB SPONSORS
None of this would be possible without the generous support of the Wellness Hub sponsors. The VNCA extends its gratitude to gold sponsor Royal Canin and silver sponsors Hill’s Pet Nutrition and VetPay for their unwavering commitment to advancing the wellbeing of veterinary nurses and technologists in Australia.
The relaunched VNCA Wellness Hub marks a significant milestone in the journey towards holistic wellbeing for veterinary nurses and technologists in Australia. By prioritising the health and happiness of its members, the VNCA sets a benchmark for workplace wellbeing in the veterinary care sector, reinforcing its commitment to excellence in every aspect of veterinary nursing and technology.


Sponsorship opportunities
We invite you to consider a partnership with the VNCA by becoming a Wellness Hub sponsor as we endeavour to make a meaningful impact on the community of veterinary nurses and technologists across Australia. Our sponsorship packages are thoughtfully crafted to align with the goals of your organisation, and they offer varying levels of support.
We encourage you to reach out to us to receive a comprehensive copy of
our sponsorship prospectus and to initiate a discussion regarding potential sponsorship opportunities.
Contact Information
Phone: 03 9586 6022
Email: admin@vnca.asn.au
We look forward to the opportunity to discuss how your organisation can contribute to and benefit from our mission to enhance the wellbeing of veterinary professionals in Australia.
March 2024 3 WELLNESS HUB
©gettyimages/AnnaStills
Quality practice through standards and learning

Recency of practice demystified: Essential insights for veterinary nurses and technicians
WORKING TOWARDS FORMAL REGISTRATION OF VETERINARY NURSES AND TECHNICIANS
In December, VNCA and AVNAT representatives attended a meeting hosted by the Australasian Veterinary Boards Council (AVBC) to work on the path forward to formal regulation of veterinary nurses and technicians in Australia. The meeting was attended by various veterinary surgeon board registrars, the AVA and veterinarians in practice. It was pleasing to once again see the positivity in the room for the registration of veterinary nurses and technicians and this is another step along the pathway to national registration. Discussions have also occurred with the South Australian Veterinary Surgeons Board as they work on developing the veterinary practice regulations for the state.
WHAT IS RECENCY OF PRACTICE AND HOW DO I SHOW EVIDENCE OF THIS?
A common question asked of the AVNAT Regulatory Council is what is recency of practice and how do I show evidence of this if I have not been working in a clinical setting in the last 12 months?
To be eligible for registration in the AVNAT Registration Scheme, veterinary nurses with an Australian Certificate IV in Veterinary Nursing qualification (or equivalent), an Associate Degree or Bachelor of Veterinary Nursing, and veterinary technicians with an approved Bachelor of Veterinary Technology qualification (or equivalent) who are currently practising in the profession are eligible to apply for registration.
Importantly, the definition of ‘practice’ in the AVNAT Framework and Policies includes any role in which the individual uses their skills and knowledge as a practitioner in their profession. Practice includes the direct provision of services to patients and the use of professional knowledge and/or skill in a direct clinical or non-clinical way. This includes non-direct relationships with patients such as working in management, administration, education, research, advisory, regulatory or policy development roles and any other role that impacts the safe, effective delivery of veterinary nursing and related services.
As such, individuals employed in veterinary practices, animal welfare organisations, research and teaching institutions, appropriate government bodies or related

It was pleasing to once again see the positivity in the room for the registration of veterinary nurses and technicians and this is another step along the pathway to national registration.
4 March 2024 NEWS
©shutterstock/David Herraez Calzada
employment, and in veterinary nutrition and pharmaceutical companies, are all eligible to be registered under the AVNAT Registration Scheme. There is no requirement to be working purely in a veterinary practice to be registered; however, you are required to provide details of your employment in the last 12 months. The current industry, regulatory and legal framework in Australia precludes self-employed (independent) veterinary nurses and veterinary technicians from being registered under the AVNAT Registration Scheme. This position will not change until mandatory registration is more widely implemented in Australia.
To show recent practice, registered individuals must demonstrate completion of at least 1000 hours of practice in the preceding five years, with not more than two consecutive years out of practice. The recency of practice for periods of less than five years can be demonstrated by the completion of at least 200 hours of practice within each of the last three consecutive years AND no more than two consecutive years out of practice. Those individuals who may have taken a career break due, for example, to maternity/paternity leave of more than two years, are subject to the AVNAT Return to Practice policy.
Completion of annual continuing professional development (CPD) requirements does not constitute recent practice. Recent practice requires showing active use of knowledge and skills relevant to the profession in a professional practice setting.
Other methods of demonstrating recency of practice include:
• completion of case studies or logbooks that clearly demonstrate that you have undertaken tasks such as surgical and medical nursing in a veterinary workplace setting
• research or a workplace study undertaken to demonstrate you have applied time and effort into seeking continuous improvement in a veterinary workplace setting
• resources developed for the workplace such as policies, procedures and training materials.
For more information, please refer to the AVNAT Framework and Policies on the VNCA website.
View AVNAT Framework and Policies here

AVNAT registration for the 2024/2025 cycle
There are only 4 months left before it is time to renew your AVNAT registration as the AVNAT registration year runs from 1 July to 30 June each year. So, it’s best to start to get yourself organised now!
Apart from the financial aspect (i.e. paying the renewal fee), the renewal process involves three key elements:
1. Meeting your continuing professional development (CPD) requirements
2. Preparing a career plan for the coming financial year
3. Confirming your compliance with the mandatory declarations. Meeting your CPD requirements is often the area that strikes terror into the hearts of vet nurses and technicians when they think they won’t have enough CPD points. Fear not, the situation is never as dire as you think –you just need to understand what, when and how you are going to meet your target. For more information, visit the Renewal Hub.


March 2024 5 NEWS
TO BE UPDATED
2024 VET NURSE/TECHNICIAN OF THE YEAR SUPPORTER PROFESSIONAL DEVELOPMENT SUPPORTER
VNCA SUPPORTERS
Setting your new year workplace goals
The New Year is officially here, and as everyone slowly filters back into the workplace after the summer holidays, it’s natural to start rethinking about your professional goals as reality starts to kick in.
While we all love the allure of a fresh start, we also know that good intentions can get lost in the shuffle of our busy everyday lives. Achieving goals and New Year’s resolutions in the workplace can be especially difficult without forming a plan and strategy to tackle them. So, here are five tips to make this the year you achieve some of your workplace goals!
Take some time to reflect
Before you make any goals, take a step back and review what you actually want to achieve in the short and long-term. Are these the same as last year? If not, why do you think that’s the case? Articulate your
aspirations — whatever they may be! The key reason why it’s important to do this is because it’s hard to stick to resolution if your heart’s not in it.
When you commit to making a change, you need to make sure that your actions align with your core values. One exercise that can help you decipher what you want your future to look like is asking:
What am I doing?
• Who am I working for?
• How do I feel?
Be honest in your assessment. If you’re not, it will be harder to inspire yourself to make the necessary changes that are in line with your goals.
Focus on smaller goals
At the start of a New Year, it’s so easy to get caught up in the euphoria of a new start. As a result, it’s common to make sweeping generalised goals without knowing how to achieve them. While it’s okay to set big, long-term targets, your next step should be breaking it up into small, realistic objectives. If your goal is to achieve a promotion, for example, you could set smaller goals like talking to your manager or relevant professional about it, taking the time to produce more accurate work, or researching how others have been successful in your organisation or industry.

... it’s common to make sweeping generalised goals without knowing how to achieve them. While it’s okay to set big, longterm targets, your next step should be breaking it up into small, realistic objectives.
6 March 2024
WELLNESS HUB ©shutterstock/PeopleImages.comYuri A
It can be helpful to map out a timeline of when and how you want to make strides towards your career aim. Prioritising one or two action items to work on every quarter can also help you meet your ultimate goal. Don’t be afraid to ask for honest feedback. Many people wait until an end-of-year evaluation to seek out feedback, but it can be more productive to ask regularly throughout the year.
Increase your knowledge
No one knows everything, but there are always ways to improve yourself, and this is especially true in your professional career. Identify one or two actions you can take, like an industry meeting you can attend or regularly reading publications that will offer insight about the future. You could also take a course to learn or improve a skill that’s useful in your current position, or that will help you get the next one.
Nurture your workplace relationships
If you enjoy your working environment, you’re more likely to be more effective and productive in your job. In fact, regardless of the industry, positive workplace relationships are one of the most important factors in your career success. Make a habit of learning the preferences of others and you will have better relationships at work. Improving your workplace relationships might mean taking the time to understand your boss’s
One of the most important things to keep in mind about professional resolutions is that they don’t have to be intimidating. Your goal is often not something far off or unobtainable. You’re simply resolving to change something, right now. Don’t worry too much about the future. Just focus on the progress you can make right now.
personality and communication style to better interact with them professionally. Master the art of managing up, down and across in all your workplace relationships.
Stay on track and keep at it! So, you’ve set yourself up for success. How do you make sure you actually get there? There are a few easy ways to help you stay motivated along the process. The first is to develop a habit. If your goal is to improve your communication, perhaps implementing a time every week where you get together with your team or manager to discuss what you’ve done or what you have in the pipeline can help make this action more natural to you.
It can also be beneficial to share your professional goal(s) with a trusted friend or co-worker and aim to reach them together.
You can create a shared Google Doc with your chosen person where you write down your goals, deadlines, plans and other thoughts or schedule a monthly check-in to update each other on your progress. Another tactic is using rewards. If you reach one of your goals, or micro-goals, treat yourself to something you really enjoy, whether that’s a meal out with your partner, a special bottle of wine or champagne, or expensive chocolates. The reward will help your desire to reach your next goal.
Article written and produced by Wellness Hub Member Assistance Provider Converge
converginternational.com.au

Learn new animal care skills in days or weeks A TAFE NSW short course is a great way to upskill and gain the skills you need quickly. Nurture your career and enrol in a specialised short course today. RTO 90003 | CRICOS 00591E | HEP PRV12049 tafensw.edu.au/short-courses March 2024 7
WELLNESS HUB
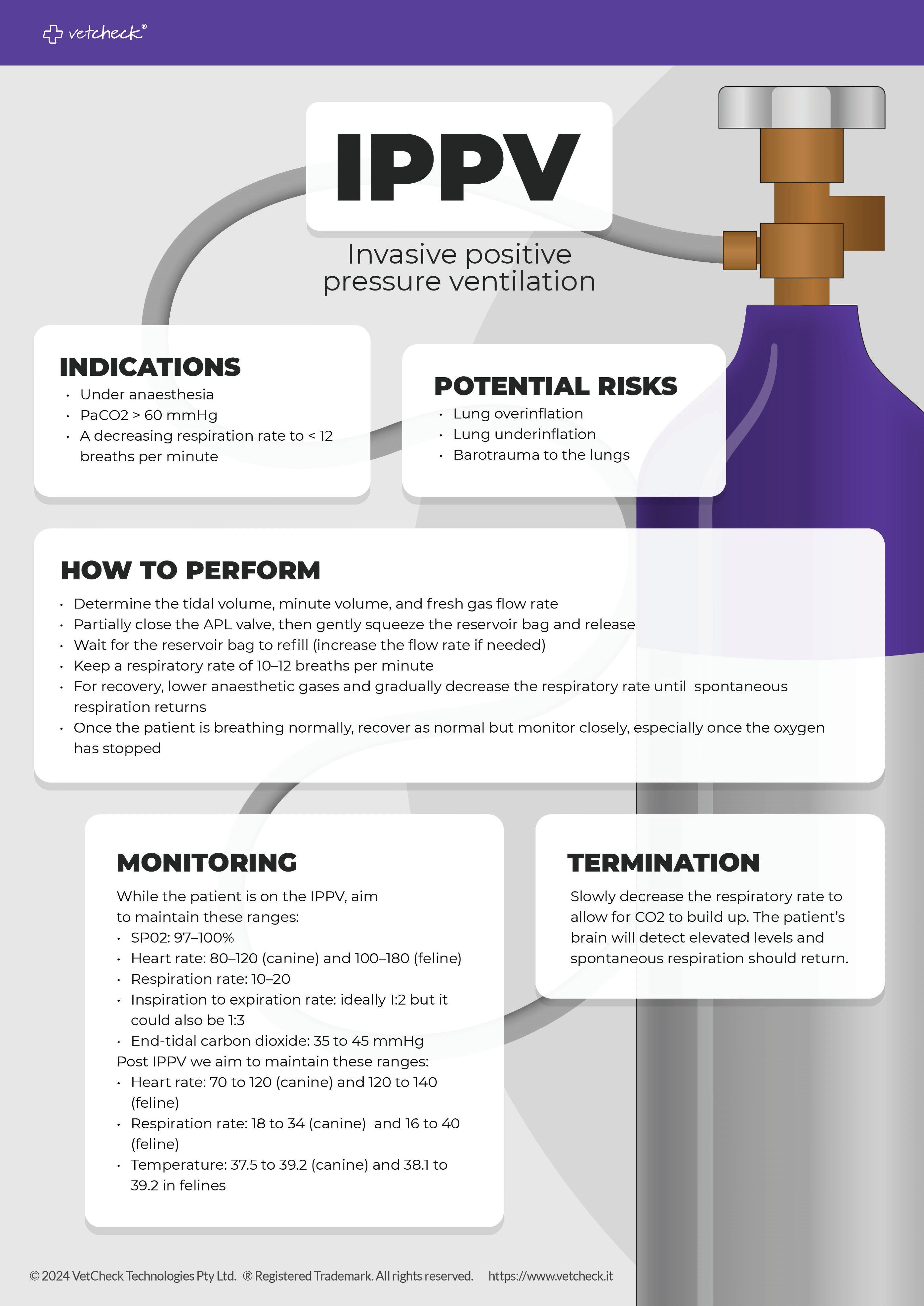
IPP … what? Introduction to intermittent positive pressure ventilation specifically under anaesthesia
by Samantha Dhatt
DipVN ECC, Dip Ldrshp & Mgt, Cert IV VN, VTS ECC, RVN
The administration and monitoring of anaesthesia for surgical procedures can be a complex process that requires knowledge, technical skills, awareness, critical thinking, and a level head.
A thorough understanding of normal and abnormal vital signs/physiology and patients’ conditions, the principles of anaesthesia and anaesthetic depth, and the ability to ask questions regarding a patient’s condition are the most important factors in monitoring anaesthesia safely.
INTERMITTENT POSITIVE PRESSURE VENTILATION (IPPV)
Positive pressure that is maintained only during inspiration (manual or mechanical).
POSITIVE END-EXPIRATORY PRESSURE VENTILATION (PEEP)
Positive pressure that is maintained within the lungs at the end of expiration (not covered).
WHEN WOULD PPV BE INDICATED?
Positive pressure ventilation is indicated when a patient cannot ventilate adequately. This is defined as a PaC02 (partial pressure of carbon dioxide) of > 60 mmHg (normal 35–45 mmHg).
1. Thoracic surgery
2. Hypoventilation
3. Apnoea/respiratory arrest
4. Cardiopulmonary cerebral resuscitation
5. Anaesthesia
6. Neurological alterations affecting CNS
7. Toxins
8. Snake envenomation
9. Pulmonary parenchymal disease –causing impaired gas exchange
WHEN WOULD PPV BE INDICATED DURING ANAESTHESIA?
• To manage post-induction apnoea
• To manage respiratory arrest
• To manage hypoventilation/ hyperventilation
• To manage hypocapnia/hypercapnia
• In circumstances where ventilation is compromised (diaphragmatic hernia, pleural space disease, gastric dilation and volvulus)
• In open chest/thoracotomy surgeries During cardiopulmonary cerebral arrest
• In circumstances where inflated chest radiographs or CTs are required
WAYS TO PROVIDE POSITIVE PRESSURE VENTILATION – USING HANDS OR A MECHANICAL VENTILATOR
1. Anaesthetic circuit
2. Anaesthetic ventilators – are a good way of providing mechanical ventilation to surgical patients. Anaesthetic ventilators are not used for long-term ventilation due to the limited modes; the delivery of 100% oxygen does not allow for a fraction of inspired oxygen to be adjusted, and no humidification systems. Using a mechanical ventilator for anaesthesia has both pros and cons (discussed later)
3. Ambu bag (not covered)
4. ICU ventilators (not covered)
AIMS OF IPPV (ANAESTHESIA)
1. To deliver appropriate amounts of oxygen to patients to maintain normal oxygen gas exchange
2. To remove appropriate levels of carbon dioxide from the patients to maintain normal blood gas levels
3. To maintain the appropriate depth of anaesthesia by delivery of consistently low levels of gaseous anaesthetic
IPPV or ‘squeezing the bag’ may seem like a benign procedure but can have catastrophic consequences if not performed correctly. Nurses monitoring anaesthesia ideally should be trained and deemed competent in both the technical and theoretical aspects of IPPV to minimise the chances of complications.
DEFINITIONS (OXFORD DICTIONARY)
Lungs – each of the pair of organs situated within the ribcage, consisting of elastic sacs with branching passages into which air is drawn, so that oxygen can pass into the blood and carbon dioxide be removed.
Pleural pressure – is the pressure surrounding the lung, within the pleural space.
Intrapulmonary pressure – intra-alveolar pressure is the pressure of the air within the alveoli, which changes during the different phases of breathing.
Intercostal muscles – the intercostal muscles are a group of muscles found between the ribs that are responsible for helping form and maintain the cavity produced by the ribs. The muscles assist with expansion and contraction during breathing.
Ribs – each of a series of slender curved bones articulated in pairs to the spine (12 pairs in humans), protecting the thoracic cavity and its organs. The ribs help in the expansion and contraction of the thoracic cavity and protect the lungs and heart.
Diaphragm – a dome-shaped muscular partition separating the thorax from the
8 March 2024 CLINICAL
AVN and AVNAT
Continuing Professional Development

A thorough understanding of normal and abnormal vital signs/ physiology and patients’ conditions, the principles of anaesthesia and anaesthetic depth, and the ability to ask questions regarding a patient’s condition are the most important factors in monitoring anaesthesia safely.
abdomen in mammals. It plays a major role in breathing.
Tidal volume – the air that moves in or out of the lungs with each breath.
Atmospheric pressure – is the force exerted on a surface by the air above it as gravity pulls it to Earth. Atmospheric pressure is commonly measured with a barometer. Measured in cm of H20.
ATMOSPHERIC PRESSURE IN RELATION TO BREATHING
Atmospheric pressure is 760 mmHg. The pressure in the lungs (intrapulmonary pressure) is equal to atmospheric pressure. Air (gases) moves along a pressure gradient from high pressure to low pressure. Hence, air will only move into the lungs when the intrapulmonary pressure drops or becomes more negative.
PHYSIOLOGY
The breathing cycle involves air going into the lungs during inspiration and air leaving the lungs during expiration. During a cycle, there are both pressure and volume changes.
There are three phases of a breath cycle:
1. Rest – where there is no airflow
2. Inspiration – where air enters
3. Expiration – where air leaves
INSPIRATION – ACTIVE
The intercostal muscles and the diaphragm are the two most important muscles/organs in normal respiration. Then you have the two most important pressures: atmospheric pressure and intrapulmonary pressure – both 760 mmHg. They are balanced; there is a difference of 0.
During inspiration, the diaphragm contracts and moves down, and the intercostal muscles contract, expanding and raising the rib cage. This allows the intrapleural volume to increase, resulting in the intrapulmonary pressure decreasing to approximately 759 mmHg (in relation to atmospheric pressure this is -1 mmHg). Allowing air to move into the lungs.
EXPIRATION – PASSIVE
The diaphragm relaxes and moves back to its original place. The intercostal muscles relax resulting in a decrease in the thoracic cavity. This causes the intrapulmonary volume to decrease, causing an increase in pulmonary pressure to 761 mmHg (+1 mmHg). Gases will move out from the lungs into the air (outside) down its pressure gradient.
POSITIVE PRESSURE VENTILATION
Two different types of positive pressure ventilation:
1. Positive pressure ventilation (PPV)
2. Positive end-expiratory pressure ventilation (PEEP) (not covered)
INSPIRATION – POSITIVE PRESSURE
Air is pumped into the alveoli (via an endotracheal tube); alveoli pressure becomes much more positive, causing gas exchange. This causes the diaphragm to passively descend and the lungs/chest to passively expand as you are forcefully pushing air into the lungs.
March 2024 9 CLINICAL
Continued next page ©shutterstock/Anamaria Mejia
IPP … what? Introduction to intermittent positive pressure ventilation specifically under anaesthesia
Continued from previous page
EXPIRATION – POSITIVE PRESSURE
The forceful push of air is released, driving gas inside the ventilator housing (outside the bellows) or reservoir bag to be exhausted into the atmosphere.
This causes elastic recoil of the diaphragm resulting in it returning to its original place. The chest cavity decreases and results in an intrapulmonary pressure difference of -1 mmHg resulting in air moving out of the lungs.
CHANGES IN PHYSIOLOGY
Positive pressure ventilation is changing the normal physiology of the body, and this can have profound consequences on all the systems of the body (including cardiac, renal, gastric, nutritional, neurological and neuromuscular).
The main cardiovascular, respiratory and neurological physiological consequences relating to an anaesthetic ventilator can include:
hypotension (low blood pressure)
• reduced cardiac output (cardiac output is the amount of blood the heart pumps in one minute, and it is dependent on the heart rate and stroke volume)
• decreased lung volume
• hypercapnia (elevated carbon dioxide level)
• hypocapnia (decreased carbon dioxide level)
Positive pressure ventilation can reduce cardiac output, which can result in hypotension. The increased intrathoracic pressure decreases venous return and right heart filling, which may reduce cardiac output. This occurs when inspiration is too long, and/or expiration is too short, and respectively when inspiratory pressure is too high.
Positive pressure ventilation may also increase pulmonary vascular resistance. The alveolar pressure is increased, which has a constricting effect on the pulmonary vasculature. This results in a decrease in blood flow to the lungs, and inadequate exchange of oxygen and carbon dioxide. When the inspiratory pressure is too high, the pulmonary vascular collapses. When the inspiratory pressure is too low, the alveoli collapse.
A decreased lung volume occurs when the tidal volume is too low, resulting in the collapse of the alveoli and occurs when an inadequate minute volume (minute volume is the tidal volume x the respiratory rate) is set.
The potential cerebral effects of positive pressure ventilation on an anaesthetic ventilator are related to the variations in carbon dioxide levels which directly affect blood flow to the brain. Carbon dioxide levels are measured using a capnograph (ETC02), which can effectively be controlled by altering the respiratory rate and tidal volume. ETC02 is the most accurate noninvasive method of determining if a patient is ventilating appropriately.
Hypoventilation causes an increase in ETCO2, generally with the patient not ventilating enough to remove carbon dioxide due to being in a deep anaesthetic plane. This leads to vasodilation, respiratory acidosis and increased blood flow to the brain.
Hyperventilation causes a decrease in ETCO2, with too much carbon dioxide being removed. This leads to vasoconstriction, respiratory alkalosis and decreased blood flow to the brain. Oxygen delivery to the tissues is reduced and brain damage can result.
DANGERS OF IPPV (ANAESTHESIA)
1. – Overinflation
– Initially, there may be no obvious signs of injury
– Traumatic lung injury from overdistension results in an inflammatory response
– Reduction in lung function
– Reduced cardiac output resulting in hypotension
– Excessive respiration rate resulting in hypocapnia
2. – Underinflation
– Failure to deliver appropriate amounts of oxygen (patient becomes hypoxaemic)
– Failure to deliver anaesthetic agent (light patient or patient wakes up)
– Failure to remove appropriate carbon dioxide (patient becomes hypercapnic)
3. – Consistency (manual vs mechanical)
– Ventilated patients reach the anaesthetic surgical plane more quickly compared to spontaneous breathing
ANAESTHETIC CIRCUITS
Typically, in general practice, IPPV under anaesthesia is performed using a t-piece or circle circuit.
T-PIECE
– Gas flow is controlled by pressure
– A high fresh gas flow is typically used
– The fresh gas flow flushes out the waste gas and carbon dioxide
– Difficult to reintroduce waste gas to the patient
HOW TO PERFORM IPPV USING T-PIECE
1. Occlude the end of the reservoir bag or close the valve.
2. Allow gas to fill the bag.
3. Squeeze the bag to inflate the chest (squeezing the bag will forcefully push fresh gas and inhalation anaesthetic into the patient).
4. Release the bag or open the valve and allow the patient to exhale (when the valve is released the incoming high FGF rates ensure the exhaled gas goes out via the expiratory limb of the circuit).
5. Repeat.
HOW TO PERFORM IPPV USING A CIRCLE CIRCUIT
1. Much safer than using a reservoir bag on the expiratory circuit (t-piece or bain).
2. Circle circuit has its own valves; inspiration and expiration valve and pop-off valve.
3. Close the pop-off valve.
4. Squeeze the reservoir bag (this forces fresh gas and inhalation anaesthetic to the patient, no carbon dioxide).
5. Release the reservoir bag (this allows waste gas to go into the circle).
6. You can give several breaths before opening the valve (and refilling with fresh gas).
10 March 2024 CLINICAL
WHAT RATES/VALUES DO WE NEED TO KNOW?
1. Target ventilation pressures are not related to weight or volume (you will only know the pressures reached during IPPV if you have a manometer attached to the anaesthetic machine).
– Generally, pressures of 10–20 cm H20 will adequately ventilate patients
– Cat: 10–14 cm H20
– Small dog: 10–14 cm H20
– Medium dog: 15–20 cm H20
– Giant dog: 18–25 cm H20
2. If you do not have a manometer to measure the pressure, the lungs should be inflated by approximately ⅓. You must be actively watching the patient’s chest when performing IPPV. Start with small squeezes of the reservoir bag and increase slowly to a point of obtaining a ‘normal’ chest movement for your patient (each patient will be different depending on the species, size and chest conformation), and maintain normocapnia.
ANAESTHETIC VENTILATORS
History
One of the earliest mechanical ventilators in human use was the Drinker respirator (or ‘iron lung’), which was developed during the polio epidemic in the 1920s. The ventilator, however, worked using a negative pressure gradient. The machine created a sub atmospheric pressure around the thorax, expanding it and causing air to be drawn into the lungs by a negative pressure gradient. The first positive pressure ventilator was invented by John Emerson in 1949 and is the preferred method of ventilation.
Anaesthetic ventilators play a vital role in anaesthesia and have different requirements than those of an ICU ventilator. The anaesthetic ventilator (including bellows) is used in combination with a circle system, adjustable airway pressure limiting valve (mechanical or digital), entrance for fresh gas, entrance for an anaesthetic inhalation agent, scavenge system, and carbon dioxide absorber.
BENEFITS OF USING AN ANAESTHETIC VENTILATOR VS HAND VENTILATING
• Maintains constant and consistent ventilation
• Optimises the delivery of inhalation anaesthetic
• Frees up the anaesthetist
• More labour efficient
AIM: The goal when using an anaesthesia ventilator is to maintain physiologic homeostasis.
TYPES OF VENTILATORS
There are 3 types of positive pressure ventilators used in veterinary medicine.
1. Volume: volume cycled; pressure limited = volume is set but once a pressure limit is reached no more volume is delivered
2. Pressure: pressure cycled; volume limited = pressure is set but once the volume limit is reached the ventilator ends the breath even if the pressure was not reached
3. Time cycled: fixed inspiratory time is set (not covered)
The most common type of anaesthetic ventilator is the volume cycled, pressure limited.
WHAT RATES/VALUES DO WE NEED TO KNOW
1. Respiratory rate (RR)
a. Breaths per minute
b. Initial: 8–12 bpm
c. Adjustments 6–15 bpm generally
2. Tidal volume (TV)
a. Amount of air/oxygen delivered in one breath
b. Initial: 10–12 ml/kg
c. Adjustments: 8–14 ml/kg
3. Minute volume (MV)
a. Amount of air/oxygen delivered in one minute
b. MV = TV x RR
c. 150–250 ml/kg/min
4. Inspiratory:expiratory ration (I:E)
a. Ratio of inspiratory to expiratory time
b. Ideal: 1:2, 1:3
c. Inspiration approx. 1 second
5. Peak inspiratory pressure (PIP)/pressure limit
a. The highest airway pressure applied to the lungs during inhalation
b. Generally, pressures of 10–20 cm H20 will adequately ventilate patients
c. Cat: 10–14 cm H20
d. Small dog: 10–14 cm H20
e. Medium dog: 15–20 cm H20
f. Giant dog: 18–25 cm H20
PERFORMED WITH THE CIRCLE CIRCUIT
1. Leak test the anaesthetic machine as per normal
2. Select the correct size bellows
– Paediatric for TV < 250 ml generally
3. Depending on the type of ventilator either:
– Flip the lever ‘ventilator’ and attach the ventilator hose (if not already connected)
– Remove the reservoir bag and replace it with the ventilator hose
– Close the pop-off valve
– Attach the scavenge hose (if not already connected)
– Check all hoses and connections are correct
4. Leak test the ventilator (you should have already leak tested the anaesthetic machine)
– Essential that you know there are no leaks in the systems before placing an animal on the machine)
5. Remove the ETC02 sensor (if you have one available) and hold a finger over the Y-piece of the circuit or use a reservoir bag in place of it.
6. Fill the bellows:
– Use the oxygen flush – The bellows should remain at the top and filled
– Most common source of a leak is the housing if not placed on correctly
7. Set the pressure relief valve (depending on what type of ventilator you have will depend on if this is done manually or automatically calculated via the system interface of the ventilator)
– Generally, pressures of 10–20 cm H20 will adequately ventilate patients
Continued next page
March 2024 11 CLINICAL
Continued from previous page
– Cat: 10–14 cm H20
– Small dog: 10–14 cm H20
– Medium dog: 15–20 cm H20
– Giant dog: 18–25 cm H20
– This valve will open when the pre-set pressure is reached within the circuit
8. The manometer is used to evaluate the pressure within the circuit
CONNECTING THE PATIENT TO THE VENTILATOR
1. Double-check all connections and settings
2. Fill the bellows to the top before turning on the ventilator (this gives some oxygen to the bellows once the patient is initially attached)
3. Turn on the ventilator
4. Connect the patient to the circle system
5. Initially keep the FGF high so the bellows fill to the top (this may take several breaths; once filled the FGF rates can be set to normal)
6. Do NOT use the oxygen flush once the patient is attached
7. If the bellows are not rising to the top, there is a leak (most leaks are due to an insufficiently inflated ET t ube cuff)
8. Read the TV at the top of the white discs (or the system interface)
9. Adjust the TV as required by using either the inspiratory flow knob or the system interface
10. Watch the patient on inspiration: – Should look like a ‘normal’ breath for that individual patient
Monitoring specific to anaesthetic ventilators includes:
Normal values/rates/description
Oxygen saturation (Sp02)
Heart rate (HR)
• Normal SpO2: 97–100%
• The patient’s SpO2 is the percentage of oxygensaturated haemoglobin and indicates how well the lungs are delivering oxygen to the blood
• The pulse oximeter measures both SpO2 and heart rate and is monitored continuously
• Normal – canine: 80–120 bpm
• Normal – feline: 100–180 bpm
• Bradycardia (low heart rate) may indicate excessive anaesthetic depth or a response to vagal stimulation (HR < 80 in dogs and < 100 in cats should be reported to the supervising veterinarian or technician for evaluation
• Tachycardia (high heart rate) may indicate light plane of anaesthesia/inappropriate response to surgical stimulus, from an inadequate anaesthetic level
Respiratory rate and depth (RR)
• Normal RR: 10–20 breaths/minute
• Normal inspiration lasts 1–1.5 seconds and expiration lasts 2–3 seconds (a ratio of 1:2)
• Basic respiratory monitoring is based on clinical observations
• Chest excursions should be assessed with both spontaneous respiration and IPPV and should be a depth of ⅓ of the chest cavity
• Breathing should be smooth and regular, with thoracic and diaphragmatic components
• Advanced respiratory monitoring can be done using a capnograph
• Hypoventilation can be a result of increased anaesthetic depth (patient is too deep)
• Hyperventilation can be a result of inadequate anaesthetic depth (patient is light)
11. Check the pressure gauge to see what the pressure is reaching with each breath
– If pressure is too high the pressure valve will open (some make an audible noise)
– Double-check the TV value – Increase the inspiratory flow?
12. The pressure gauge should go to 0 +/- 2 cm H20 on expiration
MONITORING
The monitoring of the anaesthetised patient is a continual process and parameters should be monitored every 5 minutes. Monitoring patients on an anaesthetic ventilator is aimed at maintaining physiologic homeostasis and monitoring and responding to trends.
Specific to ventilator
• No changes to normal rates/values should be observed provided patient is oxygenating normally
• Heart rate trends should consistently be monitored when using an anaesthetic ventilator to assist in determining depth of anaesthesia (patients on a ventilator generally require less anaesthetic to maintain an appropriate level of anaesthesia)
• Both bradycardia and tachycardia can be a result of physiological changes to the patient
• Trends more important than values
• Inspiratory to expiratory ratio should remain the same at 1:2
• Respiratory rate will be determined by the level of end-tidal carbon dioxide
• Generally, start 8–12 bpm (increase only when required to maintain carbon dioxide levels)
• Monitor anaesthetic ventilator settings vs actual RR; if the RR is higher than the settings the patient may be bucking the ventilator (check anaesthetic depth and adjust accordingly)
12 March 2024 CLINICAL
End-tidal carbon dioxide (ETC02)
Normal values/rates/description
Normal 35–45 mmHg
• Measured by a capnograph
• End-tidal carbon dioxide (ETCO2) is the level of carbon dioxide that is released at the end of an exhaled breath and is one of the best non-invasive ways to monitor a patient’s ventilation status under anaesthesia
• Characteristics of a normal capnograph waveform include:
– waveform starts at zero and returns to zero – the amplitude of the waveform depends on the ETC02 concentration – the width of the waveform relates to the expiratory time – each waveform has 4 phases
Specific to ventilator
Use the ventilator settings (tidal volume and respiration rate) to assist in maintaining the patient’s ETC02 to normal values
• Hypercapnia (elevated ETC02) is directly related to hypoventilation. Treatment is focused on treating the cause:
– check anaesthetic depth (generally the patient is too deep)
– reduce anaesthetic administration
– ensure fresh gas flow is adequate; increase if metabolic rate is increased
– increase RR rate on the ventilator
– check TV and minute volume rates
Hypocapnia (reduced ETC02) is directly related to hyperventilation. Treatment is focused on treating the cause:
– check anaesthetic depth (generally patient is too light)
– increase anaesthetic
– check temperature
– check cuff is still inflated (deflated cuff will result in a low ETC02 when on a ventilator due to the forceful push of gases)
– check perfusion parameters
Arterial blood pressure (non-invasive)
Depth of anaesthesia
Normal BP: 120/80 mm Hg (80–120 mmHg systolic, 60–100 mmHg diastolic)
• Normal mean arterial pressure between 70–90 mmHg
• BP may be measured in a variety of ways including Doppler or automated oscillometer devices
• The most common cause of hypotension is excessive anaesthetic depth
• Other causes include hypovolemia due to intraoperative bleeding or preoperative dehydration, hypothermia or hypoxia
Hypotension – Check anaesthetic depth (generally the patient is too deep)
• Due to changes in normal physiology of positive pressure ventilation, hypotension may be a result – reduce the tidal volume (to increase cardiac output)
• Ventilated patients reach anaesthetic surgical plane more quickly and thus checking of anaesthetic depth is a priority when on an anaesthetic ventilator
• Generally, a reduced concentration of inhalation is required
WEANING BACK TO SPONTANEOUS BREATHING
1. Using mechanical ventilation
– Anaesthetic ventilators do not allow for efficient weaning, so this is performed by changing your settings
– Gradually decrease the RR to 5 bpm – ETC02 will increase = lightened anaesthetic depth
– Patient will attempt to take spontaneous breaths
– Take off ventilator by reverting to a manual system
2. Using manual ventilation
– Revert to a manual IPPV system
– Attach reservoir bag or switch toggle from ventilator to reservoir bag function
– Open pop-off valve
– Attach scavenge
– Manually ventilate using PPV until the patient breathes well on their own – Wait 20–30 seconds before giving a breath to enable the ETC02 to build
References
JM Burkitt Creedon and H Davis. Advanced monitoring and procedures for small animal emergency and critical care. Wiley-Blackwell, 2012.
DC Silverstein, K Hopper. Small animal critical care medicine. 3rd ed. Elsevier, 2023.
Veterinary Anesthesia and Analgesia. 5th ed of Lumb and Jones; KA Grimm et al. editors. 2015.
March 2024 13 CLINICAL
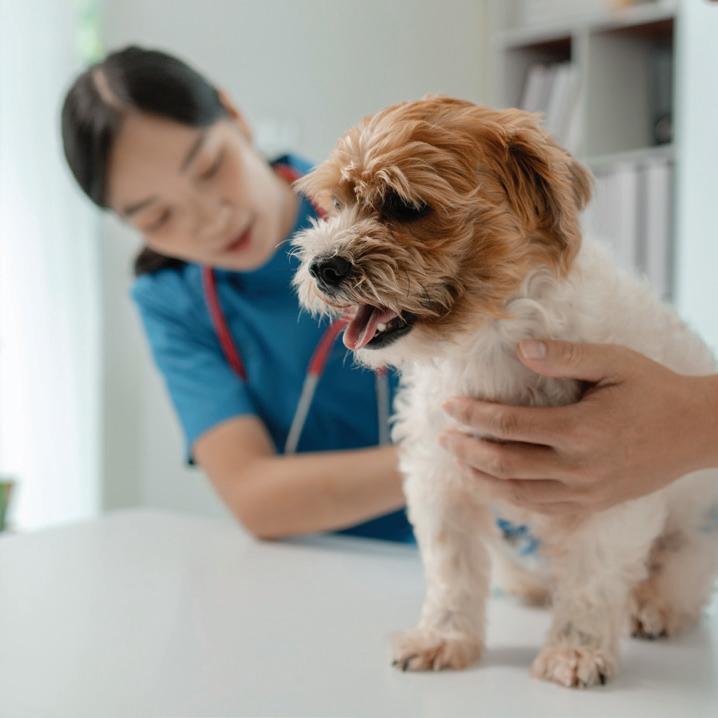
Levelling up your consulting nurse game
by Kim Healy VTS(Nutrition), FFCP(Veterinary), RVN, AVN
It’s no secret that clinics are getting busier, staff are getting more burnt out and job advertisements are staying posted for far longer than we ever thought possible. With no end in sight for the vet shortage and simply training more is not the answer, we are seeing so many qualified and skilled nurses leave the industry for good. We are working harder than we ever have for arguably less job satisfaction, more frustration, and comparatively low wages. For this reason, the average nurse walks away after 5 years and most never look back. So how do we fix this? We adapt, we change our roles, and we change our expectations – and this is where the consulting nurse role slots in quite nicely.
Becoming a consulting nurse can be challenging but highly rewarding. This role should be reserved for highly skilled nurses who are confident in their ability and knowledge. Presently a number of clinics refer to a consulting nurse as one who assists the vet, cleans the rooms postconsult, and performs services such as anal glands, nail trims and minor injections. In my opinion, this is not a consulting vet nurse role and I do feel these types of ‘consults’ seriously devalue our skill and knowledge.
STARTING OUT
If you feel like consulting might be for you but you are unsure where to start, consider team consulting. This consulting style has been implemented by several clinics that
have seen the value and better utilisation of their staff. Team consulting generally involves the nurse starting the consulting process by identifying the reason for the visit and history taking. Depending on clinic protocols, the nurse may then perform a clinical exam, record vitals and flag any deviation from normal. Some clinics do reserve this as a vet job, so role clarification for team consulting is imperative. At this point, the nurse will either move on to another consult or will stay and write the clinical notes for the consulting vet. This is a crucial and incredibly important step in learning consulting skills: watching how others speak with clients, presenting information and understanding body language. The feedback I have had from various nurses is they either lack the confidence to speak with clients or do not see the value in themselves performing such a role. Once they have the opportunity to stand in on routine consults, the mystery of what happens behind closed doors is lifted and instead of thinking ‘I’m not good enough’, their mindset shifts to ‘I could do that’.
SKILLS OF A CONSULTING NURSE
Being a consulting nurse is not a role that everyone is suitable for and that’s okay! One of the biggest mistakes a practice can make is putting people in roles they are not comfortable doing and may not have been employed to do. This ultimately leads to the failure of the role. As this is still an evolving area of practice, don’t be
Team consulting generally involves the nurse starting the consulting process by identifying the reason for the visit and history taking. Depending on clinic protocols, the nurse may then perform a clinical exam, record vitals and flag any deviation from normal.
surprised if you need to prove yourself. This is not a negative point, as this shows you’re confident to work on your own and provide the correct information. This may sound counterintuitive but you also need to prove you can ‘tap out’. You need to know when you have reached your limitations and say no; this will increase trust between yourself and other co-workers. It is very easy to get caught up in being a yes man and wanting to take up as many opportunities as you can, but this is where mistakes happen and this can be detrimental to the patient, client and co-workers. Remember, as there is currently no mandatory registration, our actions fall under the supervising vet, which is why trust between the 2 parties is so incredibly paramount.
Along with recognition of limitations, these attributes make for an excellent consulting nurse:
• Personable and approachable
• Empathetic and supportive
• Keen to learn
• Attention to detail
• Excellent communication skills
• Confidence! Confidence! Confidence!
TYPES OF CONSULTATIONS
The types of consultations you can perform will ultimately depend on your practice and your relationships with the vet team. My advice is to play to your strengths and focus on your area of interest first. It’s likely that you will immediately have more confidence in this type of consult because you already have extra knowledge to deliver the information and answer questions.
Some examples of consults:
• Nutrition, including food trials, supplements, weight loss and general health
Ear revisits, with associated cytology and examination of ears
Juvenile checks
14 March 2024 CLINICAL

• Behaviour plans
• Chronic disease management, such as kidney disease, diabetes, thyroid or cardiac
• Six-monthly senior checks, including geriatric rehab
• Exotic husbandry.
Every consult that you perform can free up a spot for a sick animal. How many times have you seen short revisits booked but needed to turn away a sick patient?
We want to work smarter, not harder! Nurse consultations are NOT free of charge. For years we have had this blanket rule of ‘It’s free to see a nurse’. Why? Is our time not valuable? Do we not have a specific skill set that should be valued? Do we not invest both time and financially into ourselves? When looking at performing anal glands, for example, that is a skill and we bill for that, but we do not bill for the time. When was the last time you had an anal gland expression and were not asked ‘How can I prevent this?’ – and you gave advice. Value your time and value your skill; that is why clients are coming to you.
Every consult that you perform can free up a spot for a sick animal. How many times have you seen short revisits booked but needed to turn away a sick patient?
IMPLEMENTING NURSE CONSULTATIONS
The first step is to identify how nurse consults will benefit the practice. Look at the current staffing situation; is one nurse able to dedicate themselves to consulting for a full day or even half a day? Perhaps the clinic is consistently down a vet, or the consulting vet is consistently running behind and feels overwhelmed. Looking at team consulting may be a good avenue to start down.
Some
benefits to present to employers:
• Increased financial revenue
• More clients through the door = more regular visits
• Decreased workload for vets, especially when short-staffed
• Increased job satisfaction leading to
better staff retention
More vet availability for higher revenue consults
• Utilisation of skills
• Be considered an industry leader. Team meetings to discuss who wishes to be involved and who doesn’t are also important. Hearing from the vets and what would help them out should certainly be considered. Once you become established as a consulting nurse, it is worth keeping track of your figures. There were some days I would have a higher spend per consult than the vets! This type of information can be used at annual reviews and when negotiating a pay rise. The consulting nurse skill set is in high demand in several progressive practices, so if this type of role is something you wish to establish yourself in, the sky is the limit!
March 2024 15 CLINICAL
©shutterstock/Pickadook
Small animal endoscopy in veterinary nursing: A guide
by Animal Industries Resource Centre Team
Endoscopy is a crucial diagnostic and therapeutic tool in veterinary medicine, allowing visual examination of internal organs and body parts without invasive surgery.
Since its inception in the early 19th century, endoscopy has revolutionised veterinary diagnostics and treatment. The skill and knowledge of veterinary nurses are pivotal to the success of endoscopic procedures, ensuring the safety and comfort of the patient throughout the process.
UNDERSTANDING ENDOSCOPY
Endoscopy involves the use of an endoscope (a rigid or flexible optical instrument equipped with a light source) to conduct a detailed visual examination of the body’s internal organs and structures.
The roots of this technology trace back to 1806. The first documented instance of thoracoscopy, an endoscopic procedure examining the chest cavity, occurred in 1912. Since then, the evolution of endoscopy has been remarkable, particularly with the integration of internal light sources, enhancing visibility and diagnostic accuracy.
Endoscopic procedures have numerous benefits, primarily due to their minimally invasive nature. They tend to involve shorter recovery times, reduced risk of infections, and less postoperative discomfort for the patient. The direct visualisation capability of endoscopy enables accurate and immediate diagnosis, swift and precise treatment decisions, and allows for
immediate interventions like biopsy and the retrieval of ingested foreign objects.
However, despite its numerous advantages, endoscopy does come with certain limitations. The procedure needs specialised equipment and a high level of expertise and training. The physical dimensions and design of the endoscope can restrict its application, as certain body areas may be inaccessible or unsuitable for examination with the available endoscopic equipment. The initial cost of acquiring high quality endoscopic systems and the ongoing maintenance they require represent a significant investment.

16 March 2024 CLINICAL
©shutterstock/Lebedko Inna
Additionally, while complications are relatively infrequent, the potential risks associated with sedation or anaesthesia, as well as the procedure itself, must be carefully considered and managed.
TYPES OF ENDOSCOPES
There are various types of endoscopes, each designed for specific diagnostic and therapeutic needs. Primarily, endoscopes are categorised into 2 main types: rigid and flexible.
Rigid endoscopes
Rigid endoscopes, known for their durability and relatively lower cost, are predominantly used in procedures where the area of interest is directly accessible. These endoscopes consist of a solid tube equipped with a light source and an eyepiece or camera at one end, providing a clear view of the internal structures. The design variations in rigid endoscopes cater to different applications, including otoscopy for ear examinations, arthroscopy for joint inspections, and laparoscopy for abdominal or pelvic cavity examinations. Their robust construction allows for the attachment of additional instruments, such as biopsy forceps or suction channels, enhancing their functionality in various surgical procedures.
Parts of the rigid endoscope
Eyepiece
The eyepiece is the part of the endoscope through which the clinician views the internal images captured by the objective lens. It often contains additional lenses to magnify the image for detailed observation. The clarity and precision of the eyepiece are crucial for accurate diagnostics and successful procedures.
Light guide adaptor
The light guide adaptor transmits light from the external source into the endoscope. It ensures that the area under examination is well-illuminated, providing a clear and vivid visual field.
Endoscopic procedures have numerous benefits, primarily due to their minimally invasive nature. They tend to involve shorter recovery times, reduced risk of infections, and less postoperative discomfort for the patient.
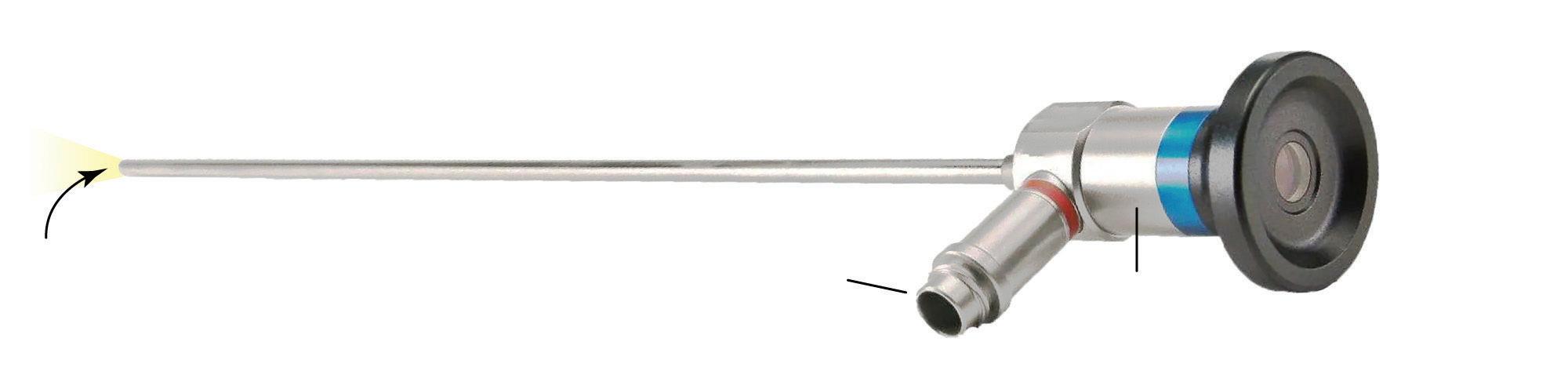
Insertion tube
The insertion tube is the part of the endoscope that is introduced into the patient’s body. It houses the optical fibres or camera system, light fibres, and in some models, channels for instruments or fluid passage. The rigidity of the insertion tube varies slightly according to its purpose and the specific area it is designed to explore.
Objective lens
The objective lens is located at the distal end of the endoscope and is responsible for capturing the images of the internal structures. It is a crucial component, as the quality of the images obtained during the endoscopic procedure directly depends on the clarity and precision of the objective lens. The lens must be meticulously maintained and handled to ensure optimal performance and accurate diagnostics.
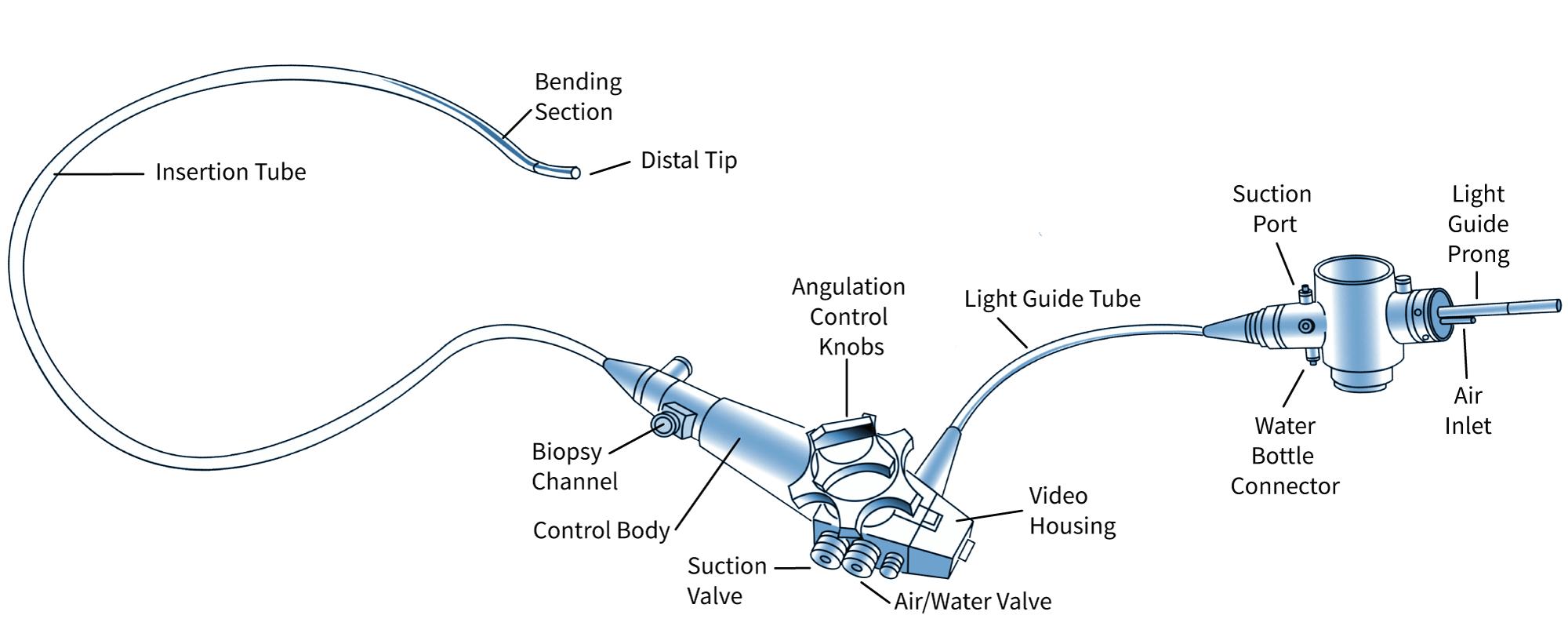
FLEXIBLE ENDOSCOPES
Flexible endoscopes are characterised by their adaptability and intricate design, allowing access to convoluted and delicate internal pathways. These endoscopes utilise a flexible insertion tube containing fibreoptic bundles or a video camera at the distal end, transmitting high quality images to an eyepiece or a digital monitor. The flexibility of these endoscopes makes them indispensable for gastrointestinal procedures like gastroscopy and colonoscopy, as well as respiratory examinations through bronchoscopy. The intricate design includes channels for air,
water, and surgical instruments, facilitating tasks such as biopsy, foreign body retrieval, or stenosis dilation.
Parts of the flexible endoscope Insertion tube
The insertion tube stands as the backbone of the flexible endoscope, its design varying to meet the diverse requirements of veterinary examinations. Attributes such as length, diameter, stiffness, and tip flexibility are meticulously calibrated to navigate different anatomical structures. Within this tube, the light source and camera or fibreoptic bundles are housed, alongside air and water conduits, crucial for maintaining clarity and facilitating precise manoeuvres during examinations. Additionally, channels within the tube are designed to accommodate specialised instruments and facilitate biopsy collection, significantly enhancing the scope of diagnostic and therapeutic interventions. The delicate nature of the insertion tube, however, necessitates cautious handling to avoid damage, underscoring the importance of gentle navigation and protection against external pressures.
Distal tip
The distal tip of the endoscope, housing the objective lenses or CCD chip, is the focal point of the examination, casting light on the internal structures under scrutiny. This tip is adeptly illuminated and designed for intricate manoeuvring, Continued next page
Objective
Insertion tube
Light guide adaptor
Marking ring
March 2024 17 CLINICAL
Eyepiece
Main parts of the rigid endoscope
Small animal endoscopy in veterinary nursing: A guide
Continued from previous page
allowing endoscopists to navigate complex anatomical landscapes and ensure comprehensive exploration. The precision with which the distal tip can be navigated ensures that every examination is thorough and captures clear, detailed visual data from the internal examination site.
Air insufflation pump
The air insufflation pump introduces air under mild pressure into the examination area to enhance visibility. This gentle insufflation expands the area being examined, providing a clearer view, and facilitating a more detailed and accurate examination. Carefully controlled introduction of air is crucial for maintaining the balance between visibility and patient comfort.
Water and suction systems
The water and suction systems are designed to maintain the clarity of the objective lens and manage the examination environment. Water, stored in a dedicated bottle attached to the light source or cart, is directed across the objective lens to remove any obstructions to clarity, ensuring that the visual field remains unimpeded throughout the procedure. The suction system complements this by removing fluids or air present at the distal tip, ensuring that the examination area is kept clear for the most precise observational conditions.
Handpiece
The handpiece of the endoscope is ergonomically designed, offering the endoscopist intuitive control over the device’s various functions. Positioned to be held in the left hand, it provides control over the up/down and right/left angulation knobs and locks, as well as the air/water and suction valves. Additionally, the handpiece houses the eyepiece or control buttons for video scopes, along with the focusing ring, ensuring that every adjustment and control is within easy reach. The biopsy/accessory channel also features here, making the handpiece a central hub for managing the functions of the endoscope during examinations.
TYPES OF ENDOSCOPIC PROCEDURES
Endoscopy encompasses a diverse array of procedures, each tailored to examine and treat specific parts of the body. From gastroscopy providing insights into stomach health, to auroscopy dedicated to ear examinations, endoscopy spans a broad spectrum of applications.
GASTROINTESTINAL ENDOSCOPY
Gastrointestinal endoscopy provides a non-invasive way to visually examine the interior of the gastrointestinal tract. This type of endoscopy encompasses several procedures, each tailored to specific sections of the gastrointestinal system.
Oesophago-gastro-duodenoscopy (OGD) allows for the detailed inspection of the oesophagus, stomach, and the beginning of the small intestine, making it crucial for diagnosing conditions like gastritis, ulcers, or tumours.
Colonoscopy focuses on the lower GI tract, offering insights into the health of the colon and the distal part of the small intestine. It is used to detect mucosal irregularities, polyps, and areas of inflammation or bleeding.
Beyond diagnosis, gastrointestinal endoscopy plays a significant role in therapeutic interventions, such as the removal of ingested foreign objects, polyp excision, and the collection of biopsy samples for histopathological examination.
The indications for gastrointestinal endoscopy are diverse. For animals presenting with symptoms such as chronic vomiting, diarrhoea, unexplained weight loss, or gastrointestinal bleeding, endoscopy offers a direct way to investigate the underlying causes. It’s particularly useful in cases where noninvasive imaging techniques, such as X-rays or ultrasound, fail to provide definitive answers. The ability to perform targeted biopsies during the procedure allows for the precise identification of conditions like inflammatory bowel disease or gastrointestinal cancers. In emergency
18 March 2024 CLINICAL
parts of the flexible endoscope
Main
TERM AREA(S) EXAMINED USES
Gastroscopy Stomach
Gastroduodenoscopy Upper GI tract (stomach, duodenum)
Enteroscopy Small intestine
Colonoscopy Lower GI tract (colon, distal small intestine)
Rhinoscopy Nasal passages
Diagnosing and treating conditions like ulcers, tumours, and inflammation
Examining and treating diseases in the stomach and beginning of the small intestine
Diagnosing issues in the small intestine such as inflammation, bleeding, or blockages
Examining the colon for polyps, cancer, and areas of inflammation or bleeding
Investigating causes of nasal discharge, bleeding, or obstruction
Bronchoscopy Lower airways (trachea, bronchi) Diagnosing and treating conditions in the airways like chronic cough or tumours
Cystoscopy Bladder
Arthroscopy Interior of a joint
Examining the bladder for stones, tumours, or inflammation
Diagnosing and treating joint diseases and injuries
Laparoscopy Abdominal or pelvic cavity Performing minimally invasive surgeries in the abdomen or pelvis
Urethrocystoscopy Urogenital tract and bladder
Thoracoscopy Thorax (chest cavity)
Examining and treating diseases in the urogenital tract and bladder
Inspecting the chest cavity for conditions like pleural effusion or tumours
Auroscopy Ear Diagnosing and treating ear conditions such as infections, blockages, or tumours
situations where an animal has ingested a foreign object, endoscopy can often be a lifesaving procedure, enabling the removal of the object without the need for invasive surgery.
RESPIRATORY ENDOSCOPY
Respiratory endoscopy is a pivotal diagnostic and therapeutic tool, particularly for conditions affecting the lower airways and lungs.
Bronchoscopy involves the insertion of a flexible endoscope into the trachea and bronchial tree, allowing veterinarians to visually inspect the airways for abnormalities. This procedure is invaluable for investigating persistent coughs, wheezing, shortness of breath, or haemoptysis. Bronchoscopy facilitates the direct observation of the mucosal surfaces, the detection of foreign bodies, the collection of biopsy samples, and even the removal of obstructive material or masses. For conditions like chronic bronchitis, pneumonia, or lung tumours, bronchoscopy offers critical insights that guide diagnosis and treatment.
Bronchoalveolar lavage, a procedure often performed during bronchoscopy, allows for the collection of cells and fluids from the lower respiratory tract, providing material
for cytological examination and culture, thereby aiding in the diagnosis of infections, inflammation, or neoplastic diseases.
The indications for respiratory endoscopy are diverse and cater to a range of respiratory conditions. For animals presenting with clinical signs such as chronic cough, unexplained respiratory distress, or suspected inhalation of foreign objects, respiratory endoscopy offers a minimally invasive yet highly effective diagnostic approach. It’s particularly beneficial when conventional imaging methods, such as radiography or computed tomography, cannot fully elucidate the nature or severity of the condition. In addition to its diagnostic capabilities, respiratory endoscopy can be a life-saving therapeutic intervention, especially in cases involving airway obstruction due to foreign bodies or excessive mucus accumulation.
EQUIPMENT PREPARATION
Before any endoscope procedure is performed the following procedures should be performed to ensure it is in working order.
Inspection of the insertion tube
Ensure the insertion tube is free from irregularities by visual inspection and tactile
examination. Look for dents or protrusions, maintaining the tube’s integrity.
Inspection of the bending mechanism
Check the bending mechanism using angulation knobs, ensuring smooth movement in all directions. Confirm that the knobs move freely and that the tube tip stabilises properly.
Inspection of the optical system
Clean lens surfaces with 70% alcohol and a gauze swab. Assess image clarity and check for broken fibres or black dots, indicating potential damage. Perform white balance for video scopes as needed.
General inspection
Ensure proper light output and check eyepiece contact pins. Clean any deposits and inspect all parts for signs of wear or damage.
Leakage testing
Conduct routine leakage tests to prevent fluid ingress, which could lead to significant damage. Follow the manufacturer’s guidelines strictly to avoid inadvertent damage.
Assemble endoscope
Choose the appropriate endoscope size and type. Connect to the light source,
Continued next page
March 2024 19 CLINICAL
Table 1: Summary of the different types of endoscopic procedures, the specific areas of the body they examine, and their primary uses
Small animal endoscopy in veterinary nursing: A guide
Continued from previous page
video processor, suction device, and water reservoir. Ensure functionality of the suction and flushing apparatus, air insufflation, and image quality. Assemble any additional equipment required for the procedure.
PATIENT PREPARATION AND CONSIDERATION
Diligent patient and equipment preparation and consideration ensure the success and safety of endoscopic procedures in veterinary practice.
The typical process includes:
conducting a thorough pre-procedure assessment to:
– review the patient’s medical history
– perform a comprehensive physical examination
– complete pre-anaesthetic blood work – identify underlying conditions affecting the procedure or anaesthesia choice
– anticipate potential complications
– formulate a tailored anaesthetic protocol
• tailoring anaesthesia protocols and monitoring to:
– consider patient’s age, breed, underlying health conditions, procedure nature – ensure comfort and immobility during procedure
– minimise stress and prevent pain – monitor vital parameters (heart rate, respiratory rate, blood pressure, oxygen saturation)
– address adverse reactions or vagal responses promptly
– choose anaesthetic agents and plan for smooth induction, maintenance, recovery
• ensuring proper positioning and handling by:
– adhering to correct positioning (e.g. left lateral recumbency for upper GI procedures, sternal recumbency for respiratory endoscopy)
– ensuring optimal access and patient safety
– providing best visualisation and accessibility
– minimising risk of injury or discomfort.
The veterinary team’s careful handling and support during the procedure contribute to the patient’s stability and the overall success of the endoscopy.
GASTROINTESTINAL ENDOSCOPIC PROCEDURES
Endoscopic evaluation of the gastrointestinal tract always requires the patient to be heavily sedated or anaesthetised. Therefore, any clinic policies regarding pre-anaesthetic patient preparation (e.g. fasting) will apply.
Essential steps and considerations involved in this preparation
• Fasting: It’s crucial to enforce a fasting period before the procedure to ensure that the stomach and upper intestinal tract are empty. Typically, the fasting period might last for 12 to 24 hours, depending on the species and the specific instructions of the veterinarian.
• Bowel preparation: This is also required for lower gastrointestinal procedures. This can be achieved through the administration of enemas and/or oral purgatives. The specific agents and the frequency of administration should be decided by the veterinarian.
• Pre-procedural assessment: A thorough physical examination and review of the patient’s medical history are vital to identify any potential risks or contraindications for endoscopy. Laboratory tests such as complete blood count, serum biochemical profile, and urinalysis may be advisable to evaluate the patient’s health status.
Pre-medication: Pre-medication with sedatives or analgesics can aid in the smooth induction and maintenance of anaesthesia. Additionally, anticholinergic drugs may be used to decrease salivary secretions which could obscure the endoscopic view.
• Anaesthesia: Administering appropriate anaesthesia is vital for the comfort and immobility of the animal during the procedure. The anaesthetic protocol should be tailored to the individual patient, taking into account factors such as age, breed, and health status.
The patient is typically positioned in left lateral recumbency for upper gastrointestinal tract evaluation. The exception to this is if the endoscope is being used to assist in the correct placement of a gastroscopy tube. In this case, the animal is usually placed in the right lateral recumbency.
For all upper gastrointestinal tract procedures (where the endoscope is passed orally) the patient should have a mouth gag applied. This ensures that the animal does not bite down and damage the insertion tube of the endoscope.
The anaesthetic nurse should use standard monitoring procedures that would be carried out on all patients undergoing a general anaesthetic. In addition, it is important to be aware that gastrointestinal endoscopy can induce vagal responses (i.e. hypotension and bradycardia). While monitoring, the nurse must ensure that the stomach does not become overinflated and if so the endoscopist must be alerted.
RESPIRATORY ENDOSCOPIC PROCEDURES
Lungs/airway
Urethra
NB
Bronchoscopy typically necessitates general anaesthesia to ensure the animal remains still and comfortable throughout the examination.
20 March 2024 CLINICAL
PROCEDURE POSITION
gastrointestinal tract (gastroduodenoscopy) Left lateral recumbency
gastrointestinal (colonoscopy) Left lateral recumbency
Upper
Lower
(tracheobronchoscopy) Sternal recumbency
(rhinoscopy) Sternal recumbency
Nose/pharynx
(esp. male dogs) (urethroscopy) Lateral recumbency
Table 2: Typical positioning for flexible endoscopy
– Position may vary according to endoscopist preference or irregularities of the particular case

Essential steps and considerations in preparation
Fasting: As with gastrointestinal procedures, fasting is crucial before bronchoscopy to minimise the risk of aspiration during anaesthesia. Typically, the fasting period lasts between 12 to 24 hours, as directed by the veterinarian, based on the species and specific health condition of the animal.
Pre-procedural assessment: A comprehensive physical examination and a detailed review of the patient’s medical history are imperative to identify potential risks or contraindications for bronchoscopy. Laboratory tests, such as a complete blood count, serum biochemical profile, and urinalysis, are often recommended to assess the patient’s overall health status.
• Pre-medication: The administration of pre-medications like sedatives or analgesics facilitates smooth induction and maintenance of anaesthesia. Anticholinergic drugs may also be used to reduce respiratory secretions and prevent mucus from obscuring the endoscopic view.
• Anaesthesia: Appropriate anaesthesia is crucial for the animal’s comfort and safety during bronchoscopy. The anaesthetic protocol should be carefully tailored to the individual patient, considering factors such as age, breed, and existing health conditions.
For bronchoscopy, the patient is typically positioned in sternal recumbency with the neck extended to facilitate the passage of the bronchoscope into the trachea. Special attention is given to supporting the patient’s head and ensuring the airway remains clear throughout the procedure.
Close monitoring of the patient’s vital signs, including heart rate, respiratory rate, and oxygen saturation, is essential during bronchoscopy, ensuring any signs of distress or complications are promptly addressed.
THE ROLE OF THE VETERINARY NURSE
The veterinary nurse’s role in the endoscopic process extends far beyond mere assistance during the procedure. From the initial stages of patient preparation to the critical moments of post-procedure recovery, veterinary nurses are at the forefront, ensuring that each step is executed with precision and care. Their responsibilities commence with the preprocedure assessment, where they play a pivotal role in obtaining and reviewing the patient’s medical history, performing preliminary examinations, and preparing the patient for anaesthesia. They ensure that all necessary diagnostic information, such as blood work and imaging results, is available and thoroughly reviewed to anticipate potential complications.
During the endoscopic procedure itself, veterinary nurses are actively involved in managing anaesthesia, monitoring the patient’s vital signs, and providing the necessary instruments and support to the veterinarian. They are adept at handling the endoscopic equipment, ensuring that it is functioning correctly and is ready for use. Their quick thinking and dexterity are crucial in situations requiring immediate intervention, such as adjusting anaesthetic levels, responding to sudden changes in the patient’s condition, or assisting with the removal of foreign bodies or tissue samples.
In the post-procedure phase, the veterinary nurse’s role is characterised by vigilant monitoring and compassionate care. They oversee the patient’s recovery from anaesthesia, continually assessing their vital signs and ensuring their comfort and safety. Pain management is a critical aspect of their responsibilities, requiring them to administer medications as prescribed and to monitor the patient’s response to ensure effective pain relief. Furthermore, they provide detailed instructions to pet owners on post-procedure care, including dietary recommendations, medication administration, and signs of potential complications that should prompt immediate consultation.
Continued next page
March 2024 21 CLINICAL
©gettyimages/Alexandr Lebedko
Small animal endoscopy in veterinary nursing: A guide
Continued from previous page
Veterinary nurses are also responsible for maintaining the sterility and functionality of the endoscopic equipment. They follow stringent protocols for cleaning, disinfecting, and storing the instruments, ensuring that they are ready and safe for use in subsequent procedures. Their role in equipment maintenance is vital for preventing cross-contamination and prolonging the lifespan of valuable medical instruments.
In essence, the role of the veterinary nurse in the endoscopic process is comprehensive and critical. Their expertise, vigilance, and compassionate care are instrumental in ensuring the success of the procedure and the wellbeing of the patient. Through their dedication and skill, veterinary nurses uphold the highest standards of patient care and contribute significantly to the field of veterinary medicine.
EQUIPMENT MAINTENANCE
Equipment maintenance is a critical aspect of the endoscopic process. Diligent equipment maintenance is crucial for the successful and safe execution of endoscopic procedures. It involves a comprehensive understanding of the equipment,
Unlock Boundless Opportunities with AVNJ Advertising!
Are you seeking to connect, collaborate, and conquer the veterinary industry?
Look no further!
Elevate your brand's presence and seize the chance to mingle with top-tier professionals in the field. The Australian Veterinary Nurses Journal (AVNJ) is your gateway to unrivaled networking and relationship-building opportunities.
Why choose AVNJ?
25+ years of industry trust and respect
• Exclusive readership of veterinary nurses and technicians
• National exposure through electronic and hard copy distribution
• Quarterly powerhouse of expertise in full-colour vibrance Your brand deserves a spotlight that shines from coast to coast. Don't miss your chance to access a multitude of marketing avenues and amplify your visibility on a national scale.
Dive into the world of limitless potential today! Scan the QR code or visit www.vnca. asn.au to unveil a realm of possibilities.

adherence to rigorous cleaning and disinfection protocols, careful storage and handling, and regular maintenance checks. These practices ensure the reliability, safety, and longevity of the delicate and expensive endoscopic equipment.
Cleaning and disinfection protocols are key to help prevent infections and maintain a sterile environment.
Typical protocol
• Pre-cleaning: Involves the removal of organic material from the endoscope immediately after use. This step is crucial for preventing the drying and adherence of biological material, which can make subsequent cleaning more challenging.
• Leak testing: Performed to ensure the integrity of the endoscope’s seals, preventing the infiltration of cleaning fluids that can damage internal components.
Manual cleaning: Performed using detergents and brushes specifically designed for endoscopic equipment to meticulously clean all accessible parts and channels.
• High level disinfection: Carried out to eliminate any remaining microorganisms. This involves immersing the endoscope in a disinfectant solution, ensuring that all internal and external surfaces are in contact with the solution for the recommended duration.
• Post-disinfection rinsing: Performed with sterile or filtered water removes any residual disinfectant, preventing chemical irritation or toxicity during the next use.
Follow clinic protocols and manufacturer’s recommendations in relation to sterilisation of endoscopes. Ethylene oxide (EtO) is an effective sterilant, especially for rigid veterinary endoscopes. However, its use requires careful consideration of its potential health hazards, environmental impact, and the need for thorough aeration to remove toxic residues. While EtO can be used for sterilising flexible endoscopes, its application is limited due to the lengthy aeration time required, toxicity concerns, and compatibility issues with some endoscope materials.
Storage and handling of endoscopic equipment are equally important. After the cleaning and disinfection process, endoscopes should be dried thoroughly to prevent microbial growth. They should then be stored in a clean, dry, and well-ventilated area Dedicated storage cabinets are ideal, allowing endoscopes to be hung vertically with their valves and caps removed to ensure proper air circulation. Proper handling is crucial to prevent damage to the delicate components of the endoscope. This includes careful transportation, avoiding sharp bends or twists in the tubing, and protecting the distal tip and control knobs from impacts.
Regular maintenance checks and troubleshooting are essential for the longevity and proper functioning of endoscopic equipment. This involves routine inspections for wear and tear, checking the functionality of the light source, camera, and working channels, and ensuring the clarity of the visual output. Keeping a maintenance log can be beneficial, recording any issues encountered, repairs made, and the dates of routine maintenance and disinfection. This not only helps in maintaining the equipment in optimal condition but also assists in identifying recurrent problems that may indicate the need for more thorough servicing or replacement of parts.
22 March 2024 CLINICAL
TREATING SMALL DOGS WITH ADVERSE FOOD REACTIONS?
Introducing ROYAL CANIN® Hypoallergenic
Small Dog, created for adult small breed dogs and precisely formulated for patients suffering from Adverse Food Reactions (AFR).
HYDROLYSED PROTEIN
Hydrolysed protein with low molecular weight to ensure the food is hypoallergenic.
SKIN BARRIER
Formulated to help support the skin’s natural protective barrier for optimal skin health.
SPECIFICALLY FORMULATED FOR SMALL DOGS
Specially adapted benefits to meet digestive, dental and urinary sensitivities of small dogs and suitable for their small jaws.




For more information speak to your Royal Canin Representative Scan to learn more
Meet VfCA’s Rural and Regional Program
by Elise Anderson (Regional Lead, Rural and Regional Program)
Ilive on Taungurung country, in northeast Victoria. It’s a region of river valleys and alpine mountains, farmland and towering mountain ash forests. My little town of not quite 3000 people sits almost in the shadow of the mighty dam wall that holds back the waters of Lake Eildon, a body of water six times the size of Sydney Harbour. It’s a paradise for wine lovers, water skiers, cyclists and fly-fishing enthusiasts. It’s a truly wonderful place to live, work and raise a family.
Like most parts of rural Australia, however, my community is very much at the mercy of the elements, and that means that the impacts of climate change are an everyday reality. This is a region that is no stranger to natural disasters. In 2009, the Black Saturday bushfires devastated this area. Vast tracts of forest were burnt, homes were lost, and people died in unthinkable numbers. I wasn’t living here at the time, but everyone I know in this community who was has a story to tell of their personal connection to tragedy; of property destroyed, of friends and family lost.
Just over a year ago, a seemingly opposite disaster occurred, when huge amounts of spring rain, following several years of
mild and wet La Nina weather, caused Lake Eildon to fill beyond capacity and forced local water authorities to open the spillway. Megalitres of water poured into the Goulburn River, adding to levels already swollen from tributaries across the catchment, and the river burst its banks. We didn’t lose any people in those floods, thankfully, but vast areas of farmland went under, roads were cut, and much stock was lost, including hundreds of thousands of trout from local fish farms.
It was a scenario that locals thought they would never see again after the millennium drought at the start of this century; in 2007, water levels in Lake Eildon were as low as 5.7%, leaving enormous tracts of lake bed exposed to the elements, a cracked and baking desert of dried mud and dead trees. Talk at the time was that the lake might never refill. How wrong we were. While the currently full dam is a reassurance to irrigators all down the Goulburn-Murray system, with another El Nino declared and a hot dry summer ahead, the current question on everyone’s lips is, how long will that water last?
This is a resilient community, and in the face of each drought, each fire and each flood, the people here dust themselves off,

rally together, and get on with their lives. Every disaster leaves its mark, however. When the rain falls and keeps falling, people obsessively check their weather apps, and all the talk in the main street is of the water level in the lake, the outflow rates and the prospect of flooding. When the first hints of smoke scent the air from distant fires each summer, there is a simmering sense of anxiety in the atmosphere of the town, a collective trauma that rises closer to the surface of everyday life.
The economic welfare of this region is highly dependent on the elements too. Our main industries are agriculture, tourism, and native forestry. The first of these is obviously very dependent on the weather. The second, tourism, is no less so; no one comes to Lake Eildon to waterski or laze on a houseboat in drought years when there is little water in the lake, cyclists don’t want to ride our rail trails in heatwave conditions, and wine that is tainted by bushfire smoke is no drawcard. As for forestry, well, that is coming to a rapid end, a step that is necessary for our forests and our climate, but one which is pushing the community into a painful transition period that will be faced by many towns reliant on timber, coal or gas for their livelihoods.
The economic welfare of this region is highly dependent on the elements too. Our main industries are agriculture, tourism, and native forestry.

 Lake Eildon at capacity (above), and in a drought year (right)
Lake Eildon at capacity (above), and in a drought year (right)
24 March 2024 CLIMATE ACTION

No, climate change is no stranger to towns like mine, and neither is it a hypothetical future scenario. Rural and regional communities everywhere across Australia have this very much in common; climate change is here, right now, impacting our everyday lives. Our work, our leisure, and our safety are all at risk.
As much as this is something that they all have in common, it is also true that communities outside of our major cities are as diverse as the landscapes in which they are located, and the people who live in them. The nature of the threat that climate change poses will be different in every town, on every farm and in each area of habitat.
At Vets for Climate Action, we recognise that rural and regional areas are at the coalface of climate change, but that there is also the potential for much opportunity as the nation makes the essential transition away from polluting and destructive practices, towards the development of renewable energy, regenerative agriculture, and sustainable industries. We also
As much as this is something that they all have in common, it is also true that communities outside of our major cities are as diverse as the landscapes in which they are located, and the people who live in them. The nature of the threat that climate change poses will be different in every town, on every farm and in each area of habitat.
understand that there are no cookiecutter solutions to this wicked problem. The strategies and solutions that will most benefit my Victorian, agriculturedependent community in its transition away from native timber harvesting will not be the same as what is required in a coal mining community in central Queensland. That is why VfCA’s Rural and Regional Program seeks to elevate the voices of local people. We want to give vets and other veterinary and animal care professionals in our country towns and small cities skills and confidence in climate advocacy, and connections with others who share their concerns. This will enable them to identify and support action on climate change that is best suited to their local context, acting as climate champions both within their communities and with their elected representatives.
It’s something of a big and hairy plan, we know, but it’s a program that I am personally very passionate about and a program that occupies an important place in VfCA’s strategic plan. The Rural and Regional Program is in its very early days, with a pilot version having begun in the federal electorate of Nicholls, in northern Victoria, earlier this year.
I’ll be keeping our supporters up to date with the progress of the program as I travel about regional Victoria and beyond, visiting vet clinics, attending events, and meeting the people who are caring for all our precious animals in the face of climate change.
In the meantime, if you would like to learn more about this program or get involved, please don’t hesitate to reach out to me via email at elise@vfca.org.au
March 2024 25 CLIMATE ACTION
©shutterstock/PeopleImages.comYuri A
Proximal interphalangeal (PIP) joint arthrodesis in a warmblood
by Clare Wheatley
Dip VN (Surgical), Cert IV VN, Cert III EN, AVN, RVN
PATIENT DETAILS:
Species: Equine
Breed: Warmblood
Sex: Gelding
Age: 17 yo
Weight: 578 kg
PRESENTATION AND HISTORY
The horse originally presented to our hospital in February 2021 with proximal interphalangeal (PIP) joint osteoarthritis (OA) previously diagnosed by another hospital approximately one year earlier. He was a high-level (Grand Prix) dressage horse who had previously been acceptably maintained on Pentosan®, Epiitalis® and intravenous hyaluronic acid (HA). The owner reported he was now struggling with some of the required movements for higher-level dressage.
Over the following 10 months, the horse was managed with intra-articular medications: 20 mg triamcinolone

and 10 mg hyaluronic acid initially, and subsequently IRAP® therapy. Interleukin-1 receptor antagonist protein therapy (or IRAP®) produces autologous (from the animal’s own blood) conditioned serum (ACS), which contains beneficial antiinflammatory and regenerative cytokines used to improve the quality of tissue healing in dogs and horses.1 It involves taking approximately 60 ml of blood from the horse, in an aseptic method, and incubating it. The sample is spun down using a centrifuge and the IRAP-rich fluid portion of the sample is harvested and reinjected back into the horse2 in the affected location – in this case, the PIP joint. Most samples will typically produce 6 treatments; any samples not used initially can be stored in the freezer.
In the 10 months following the patient’s initial presentation to our hospital, repeat radiographs of the right hind pastern showed continual deterioration of the previously identified PIP joint osteoarthritis. In November 2021, increased swelling of the pastern region was noted. Radiographs showed increased articular and nonarticular new bone formation on the lateromedial view. Joint space was

still evident with a cystic lesion present dorsomedial distal P1 (first/proximal phalanx).
On 17 January 2022, the horse was admitted to hospital for a pastern arthrodesis. He was in good general body condition with the owners deliberately reducing his weight before surgery to reduce some of the complications associated with anaesthetising large, heavy horses. Such risks include myopathies of large muscle groups, particularly those on the right hindquarter, as his leg will be extended for the entirety of the surgery, as well as the recovery period where he must lift all his weight to stand up.
The owners elected to perform the arthrodesis to allow the horse to continue his competitive performance career. An arthrodesis of certain (high motion) joints, for example, the fetlock or carpus, is performed only as salvage operations, with the aim to make the horse sound enough for a breeding career or comfortable retirement. In contrast, as the pastern is a low-motion joint, arthrodesis surgery has a promising

26 March 2024 CASE REPORT
Above: LCP combi hole with threaded portion (left) and sloped dynamic compression unit (right)
Above: 4.5 mm 3-hole locking compression PIPJ plate (pastern arthrodesis plate)
Above: DCP screw hole
AVN and AVNAT
Continuing Professional Development
success rate for return to athleticism. In a study conducted from 1994 to 2003, 87% of horses could be used as intended following arthrodesis surgery, including 81% who had a forelimb arthrodesis performed, and 95% of those who had a hindlimb arthrodesis performed.3
EQUIPMENT PREPARATION
As arthrodesis is not performed routinely in our hospital, it was important to inventory the equipment that would be required for the procedure before the surgery. The one item that is specific to this surgery is a 4.5 mm 3-hole locking compression PIPJ plate (pastern arthrodesis plate). This plate is designed so that the distal stacked combi hole provides minimal intrusion to soft tissues over the middle phalanx and distal interphalangeal (coffin) joint.
What is the difference between locking compression plates (LCPs) and older dynamic compression plates (DCPs)?
The mechanical support in traditional DCPs depends on the compression of the plate to the bone by the plate screws. If the screws loosen, stability is jeopardised. The LCP has a threaded hole, which means the screws are locked into the plate to create a more stable construct. For this to work, the screws are at a fixed angle (90° to plate), whereas in DCPs the screws can be placed at an angle.4
As arthrodesis is not performed routinely in our hospital, it was important to inventory the equipment that would be required for the procedure before the surgery.
Locking compression plates (LCP) have a combi hole with a threaded portion for the locking screw and the sloped dynamic compression unit head for the cortical screw.
Other items for this surgery that are used regularly in the hospital include 5.0 mm locking screws and 5.5 mm cortex screws of lengths ranging from 30–50 mm, the 5.5 mm cortex kit and the 5.0 mm locking kit. These kits were used with the orthopaedic drill which runs off a medical air cylinder. It was important to make sure there was a full backup medical air cylinder in case of emergency.
On the morning of surgery, the final preparations can be put into place. Items required in theatre include:
• routine kit – includes 2 x Olsen Hegar needle holders, 2 x Metzenbaum scissors (curved and straight), 3 x scissors (blunt/ blunt, blunt/sharp, sharp/sharp), 3 x Allis tissue forceps, 4 x haemostats (curved and straight), 2 x artery forceps, 10 x Backhaus towel clamps, 2 x #3 scalpel handles, 1 x #4 scalpel handle, 2 x Adson Brown tissue forceps, 1 x dressing forceps, scalpel sizes 10, 11 & 23 with gauze swabs and a hand towel
• 4.5 mm 3-hole locking compression PIPJ plate
• 5.0 locking kit and screws – T25 star drive screwdriver, 3.2 mm quick coupling (QC) drill bit, 4.3 mm QC drill bit, 5.5 mm QC drill bit, 5.0 mm drill sleeve3, T-handle, articulated tension device, spanner for articulated tension device
• 5.5 (cortex) orthopaedic kit and screws – 4.5 mm hexagonal head screwdriver,
5.5 mm quick coupling (QC) drill bit, 4.0 mm QC drill bit, 5.5 mm QC tap, 5.5 mm protective sleeve, 4.0 mm drill guide, 90 mm depth gauge, QC T-handle, counter sink. air drill and air hose
• medical air cylinder on trolley
• sterile drapes x 6
• sterile pillowcase for covering X-ray plate intraoperatively 18 Ga needles x 4 (to use as landmark reference for radiographs)
• portable X-ray unit with a plate covered by a plastic bag to prevent blood or lavage fluid from contacting the plate sterile skin stapler (for holding skin flaps out of the way to maximise visibility)
• chisel (osteotome) and hammer
• curette
• 18 Ga catheter, standard giving set, 1 L lactated Ringer's solution (LRS) for flushing surgical site intraoperatively
• suture (polydioxanone is the surgeon’s preference)
• casting material – Gypsona® in 4 & 5-inch widths, Delta Lite Plus® in 3, 4 and 5-inch widths
• radiography PPE – lead gowns, thyroid collars, gloves for plate holder
• clippers, chlorhexidine scrub, isopropyl alcohol swabs, vacuum cleaner for patient preparation
• leg stand to position right hindlimb for surgery
• cushions to adequately support patient Surgical gowns, lead X-ray gowns, masks, surgical caps and sterile gloves were placed in the scrub area for each of the three surgeons. Two specialist surgeons and one surgical resident were scrubbed into this surgery.
Continued next page
March 2024 27 CASE REPORT
Proximal interphalangeal (PIP) joint arthrodesis in a warmblood
Continued from previous page
PATIENT PREPARATION
A current radiographic series of the affected joint was acquired immediately before surgery. These radiographs were used to ensure the proposed implants were appropriately sized and the plate contoured to minimise anaesthetic time.
On the morning of surgery, the horse was catheterised in the left jugular vein with a 14 Ga x 3.25-inch Angiocath® and injection port in the cranial third of the neck. The catheter was covered by gauze swabs and Tensoplast® bandage to protect it until surgery. The horse was weighed and premedication drugs were calculated and administered.
Immediately before surgery, the patient’s mouth was washed out to prevent feed matter from entering the trachea with the endotracheal tube. The patient underwent a smooth induction, was intubated with a size 30 mm endotracheal tube, and was moved to the surgical theatre and positioned on the table in dorsal recumbency. Anaesthesia was maintained on isoflurane with mechanical ventilation. Care was taken to ensure that the patient was positioned correctly for working on the right hindlimb and optimally padded to prevent myopathies from occurring during this expected lengthy procedure.
The patient’s leg was clipped from the coronet band to the proximal region of his metatarsus. The proximity of the surgical site to the hoof necessitates waterproofing the foot with two latex gloves and duct tape to minimise debris from the hoof contaminating the surgical site. The patient’s heel was suspended in the leg stand, which attaches to the end of the table. This kept the horse’s leg extended and prevented any movement during surgery.
The leg was given pre-scrub using a neutral soap and cleaned off with isopropyl alcohol before the timed five-minute aseptic preparation using chlorhexidine gluconate was performed. A final application of isopropyl alcohol was performed when the surgeons were ready.
THE SURGERY
An inverted T incision was made from the proximal phalanx and ended with the horizontal incision 2 cm above the coronet band. The skin flaps were dissected abaxially, and the extensor tendon was incised in an inverted ‘V’ shape. The tendon was dissected off the underlying bone and the proximal interphalangeal (PIP) joint. The collateral ligaments were cut to allow the PIP joint to be opened. The articular cartilage was removed entirely with a curette. A 2.5 mm drill bit was used
to drill holes in the subchondral bone plates of both joint surfaces. These holes were flushed out using an 18 Ga catheter and giving set attached to a 1-litre bag of LRS. The purpose of these holes is to encourage bone formation and therefore assist fusion.
The plate was positioned so that the distal screw is in the second phalanx (below the pastern joint) and the middle screw is in the proximal phalanx (above the pastern joint). A 4.3 mm drill bit was used to drill the most distal hole through which a locking screw was placed but not tightened. At this stage, we switched from the locking kit to the routine dynamic compression kit to place a 5.5 mm cortical screw in the second hole of the plate. We then placed 2 trans articular lag screws on either side of the plate using 5.5 mm cortex screws. After they were fully tightened, plate application was completed by tightening the distal locking screw, the second cortical screw and then finally placing a locking screw in the most proximal hole.
The tendon was closed with a size 1 polydioxanone suture (PDS). The skin was closed with 2-0 PDS, and a half-limb cast was applied. The cast has two primary functions: it protects the bone implant construct during recovery, as well as immobilises the soft tissue to promote healing.
28 March 2024 CASE REPORT
PREMEDICATION DRUGS (PATIENT WEIGHT 578 KG) Drug Dose Mg given Ml given Route Procaine penicillin 22 mg/kg 12,716 mg 42 ml IM Gentamicin 6.6 mg/kg 3,814.8 mg 38 ml IV Phenylbutazone 4.4 mg/kg 2,543.3 mg 14 ml IV Tetanus antitoxin 1500 IU Not given as patient is confirmed vaccinated against tetanus INDUCTION DRUGS Xylazine 1.1 mg/kg 635.8 mg 6.4 ml IV Acepromazine 0.03 mg/kg 17.34 mg 1.7 ml IV Ketamine 2.5 mg/kg 1,445 mg 14.5 ml IV Diazepam 0.1 mg/kg 57.8 mg 11.5 ml IV
Casting technique
The lower limb is bandaged with cotton wool and cohesive wrap from the hoof to the lowest point of the tarsus. The initial casting layer is Gypsona® (or Plaster of Paris) as it conforms well to the limb. This material is quite heavy, so as little as possible is used – enough to cover the limb without creating extra layering. The Delta Lite Plus® (or fibreglass) layer is then applied. This has an excellent strength-to-weight ratio. To get the two layers to ‘bond’, each roll is submerged in very hot water before handing it to the surgeon. The cast is applied, covering the
RECOVERY FROM ANAESTHESIA
The patient had a smooth anaesthetic maintained on isoflurane. Additional intravenous triple drip (guaiphenesin/ ketamine/xylazine) was used to minimise the amount of gaseous anaesthetic agents needed. Fluid therapy in the form of LRS was administered throughout the entirety of the surgery. A continuous rate infusion (CRI) of dobutamine was used to maintain blood pressure above 60 mm Hg, as hypotension is common in larger horses and longer surgeries. Total surgical time was 2¼ hours. The patient was allowed to recover unassisted and was returned to his stable 15 minutes after standing.

entire hoof and extending to the proximal metatarsus. The cast must extend this high to prevent a fulcrum effect that may cause the horse to fracture its metatarsus. The toe of the horse is held to ensure the hoof is positioned as it would be if the horse was standing; this prevents the horse from placing too much weight on the toe of the cast, risking the toe prematurely wearing through the cast and preventing the horse from standing with an elevated heel for the weeks that it is in the cast.
POSTOPERATIVE CARE
The patient remained in the hospital for one-week post-surgery.
Postoperatively the patient’s antimicrobial therapy consisted of procaine penicillin intramuscularly BID for six days and gentamicin intravenously SID for six days. Anti-inflammatories (given at 2.2 mg/ kg, as opposed to the premedication dose of 4.4 mg/kg) were given orally SID as phenylbutazone for 7 days. Further analgesia on the first day postoperatively was provided by 30 mg of morphine given intramuscularly. He also received 4.4 mg/kg oral omeprazole SID. Gastric ulcer prophylaxis is important in horses
experiencing stress and pain and receiving NSAID medications.
The patient was radiographed one-week post-surgery, through the cast, to ensure there was no implant failure or signs of implant infection (for example, lysis around screw heads).
The patient was discharged on oral phenylbutazone and oral omeprazole. The owners were directed to represent the horse to remove the cast in 14–20 days. He was to be confined to a stable/yard for the next three months, with no hand walking while the cast was on. Grazing and hand walking were permitted for the next six weeks once the cast was removed, and an increasing program of hand walking could be commenced after this period. On week one of the hand walking program, he could be started on 5–10 minutes of controlled walking twice daily, followed by weekly increases of 5–10 minutes.
At three months he was to be represented to the hospital for re-evaluation. The owners were advised to call the clinic immediately if the horse was dull, lame or inappetant. Instruction was also given for them to monitor faecal output and consistency as any horse on prolonged antibiotic treatment has the potential to develop serious diarrhoea as a result. They were instructed to call the hospital if any diarrhoea was seen and to discontinue all medications immediately.

Continued next page
March 2024 29 CASE REPORT
5.0 mm locking screw
5.5 mm cortical screw
5.5 mm cortical lag screws
5.0 mm locking screw
5.0 mm locking screw
Proximal interphalangeal (PIP) joint arthrodesis in a warmblood
Continued from previous page
SUMMARY
This case required a large degree of nursing organisation and preparation.
As it is an elective procedure, there was ample time to become familiar with the surgical plan and equipment required.
As with any procedure that involves a number of surgical kits, orthopaedic and radiographic equipment, theatre setup must be well-planned around the positioning of the patient and surgeons.
Having extra equipment to hand in the correct order will be required by the surgeons intraoperatively, improving the efficiency and flow of the surgery. In these types of cases, a nurse’s ability to multitask and think ahead contributes to a smooth and successful surgery.
OUTCOME
Since this surgery, the horse has returned successfully to elite-level Grand Prix dressage competition with a number of wins at major championships.



References
1. Medical Plus, Orthokine Vet iRap, accessed 29.04.23, https://medicalplus.com.au/product/ orthokine-vet-irap/
2. Randwick Equine Centre, IRAP Therapy, 2023.
3. Knox PM & Watkins JP. Proximal
interphalangeal joint arthrodesis using a combination plate-screw technique in 53 horses (1994–2003). Equine Veterinary Journal 2006;38(6):538–542.
4. Nixon AJ. Equine Fracture Repair. 2nd ed. Hoboken, NJ USA, Wiley & Sons Inc, 2020.

This course presented by Taronga will support veterinary professionals and veterinary nurses to develop knowledge and skills in native wildlife triage, including first aid, initial treatment and emergency care.
• Supported by the NSW Government Department of Planning and Environment
• AVA and VNCA certified
• Online Course (20 CPD points)
• Hands-on Workshop (12 CPD Points) –available in NSW, QLD and Vic (see website for details)
• Subsidised positions available to eligible applicants nationally
Semester 2, 2024
Applications open on 3 June
Email: tarongaprofvet@zoo.nsw.gov.au

Visit: https://taronga.org.au/vet-professional-training
Workshops available at:

30 March 2024 CASE REPORT
Postoperative dorsoplantar view taken through the cast
Postoperative lateromedial view taken through the cast
GOLD CO AST • A USTRALI A
Tar�nga Veterinary Pr�fessional Training � Wil�life Treatment � Care

"Education is essential for personal and professional growth in the field of veterinary nursing. Whether you ' re just beginning your journey or aiming to advance your career, having a strong foundation in education is crucial. Discover why studying with AIRC is your key to success in veterinary nursing "
ACM10121 Certificate I in Animal Care Industry Pathways
Do you have a strong interest in animal care and wish to acquire foundational knowledge before pursuing advanced qualifications? If the answer is yes, the ACM10121 Certificate I in Animal Care Industry Pathways serves as an excellent introduction to this field
ACM20121 Certificate II in Animal Care
Cultivate a strong foundation of knowledge to champion animal welfare and offer invaluable support to veterinarians This qualification not only equips you with essential skills but also acts as your gateway to fulfilling the entry criteria for a Certificate IV in Veterinary Nursing, reinforcing your dedication to the well-being of animals and the vital role you play in being part of the veterinary healthcare team.
ACM40418 Certificate IV in Veterinary Nursing
This nationally accredited qualification caters to students aspiring to excel in delivering expert veterinary nursing care for animals and offering professional support to their owners You will cultivate personal and professional skills highly valued and sought after by employers The ACM40418 Certificate IV in Veterinary Nursing stands out as not only the nationally recognised credential but also holds recognition as the standard in veterinary nursing education.
ACM50219 Diploma of Veterinary Nursing
The ACM50219 Diploma of Veterinary Nursing is the next step to advance your knowledge and skills in veterinary nursing and leadership AIRC offers Diploma specialisations in the fields of General Practice, Dental, Emergency and Critical Care, and Surgical.


UNLEASH YOUR VET NURSING POTENTIAL: EXPLORE OUR CERTIFICATES!"
Find out more today! Phone: (07) 3621 6005 Email: enrolments@provet.com.au Website: https://www.provetlearning.com.au RTO CODE: 31424
Fear and stress-free treats for dogs
Are your dogs or cats feeling fearful? Do they seem super stressed? Or are they always highly distracted? Well, treats may be a way of combatting this stress.
There are many different types of treats, but not all are valued the same way by every pet. The treat’s value is decided by your pet’s preferences. The more they prefer the treat, the higher the value of the treat.
It is not uncommon for pets to become extremely stressed or aroused when they visit the vet. This makes it very difficult for the veterinarian to examine the pet and this further handling can further heighten the pet’s anxiety. Calming your pet or distracting them with treats will not only help them feel more comfortable and happier but also make it easier for the vet to perform their important examination.
Here are some examples of pets being stressed at different levels and the potential treats that you can try out with your pets to calm them down or get them distracted for

For
The VNCA and VetCheck have supplied this information to assist vet nurses to educate, brief and assist their clients to care for and manage their pets.
each stress level. Remember to be careful and get pet-friendly treats for your pets because some of the ingredients in human food are toxic to your furry babies!
HIGH-LEVEL STRESS SCENARIO –HIGH-VALUE TREATS
Going to the vet might be stressful for dogs and they might display behaviours such as hesitation to interact with you or constantly turning away to partially avoid interaction. At the same time, they might seem reluctant to take treats for a while or only take a bit of the treat. In this case, high-value treats may be the only way to regain their attention and break them from their heightened anxiety:
Peanut butter
• Cheese (cubes or squeezy cheese)
• Cooked chicken, beef, or pork
• Cooked sausages (chicken, beef, pork)
• Canned food (chicken, beef, lamb)
MODERATE-LEVEL STRESS SCENARIO – MODERATE-VALUE TREATS
Sometimes, it might be intimidating to get dogs into the vet clinic or animal hospital as they would be surrounded by unfamiliar animals and people. So, they might display behaviours such as moving the ears slightly to the side or the back, being restless or moving slowly, furrowing their brows, and seeking attention from the owner while panting with a slightly opened mouth and slightly dilated pupils. In this case, moderate-value treats may do the trick to calm these pets:
• Bully sticks
• Hard cheese sticks
• Bone chews (rawhide aka pressed bone)
• Mayonnaise (only for dogs with healthy weight and without egg allergies)
• Pate (chicken, beef, or salmon)
• A small scoop of ice cream (use your regular spoon to make the scoop)
LOW-LEVEL STRESS SCENARIO –LOW-VALUE TREATS
When walking your dogs in the park, taking them to the pet salon, or when your family or friends are visiting your place, your dogs might be less anxious than when going to the vet clinic, but they might still be a bit anxious or on alert. In this case, they might display behaviours such as avoiding eye contact, looking directly with their mouth closed, or licking their lips. They might also pant slightly and turn away their heads without moving away. In this case, most dogs would prefer the below treats:
Cooked pumpkin cubes
• Vegetables without seeds if any (carrot, cucumber, or capsicum)
• Fruits without seeds if any (apple, banana, watermelon, or blueberries)
• Kong bites (beef-flavoured or fruitflavoured)
• Cookies
• Ice cubes
Determining your pet’s high to lowvalued treats will come in handy when approaching new or stress-related environments or situations.
Source: VetCheck is a powerful client education platform that helps veterinary teams save time, increase client engagement, retention and grow the practice through digital pet health summaries, handouts, best practice tools (dental charts, anaesthesia monitoring charts, hospital workflow)
CLIENT FACT SHEET
digital case reports, handouts and request forms for veterinary teams visit www.vetcheck.it ©gettyimages/yellowsarah
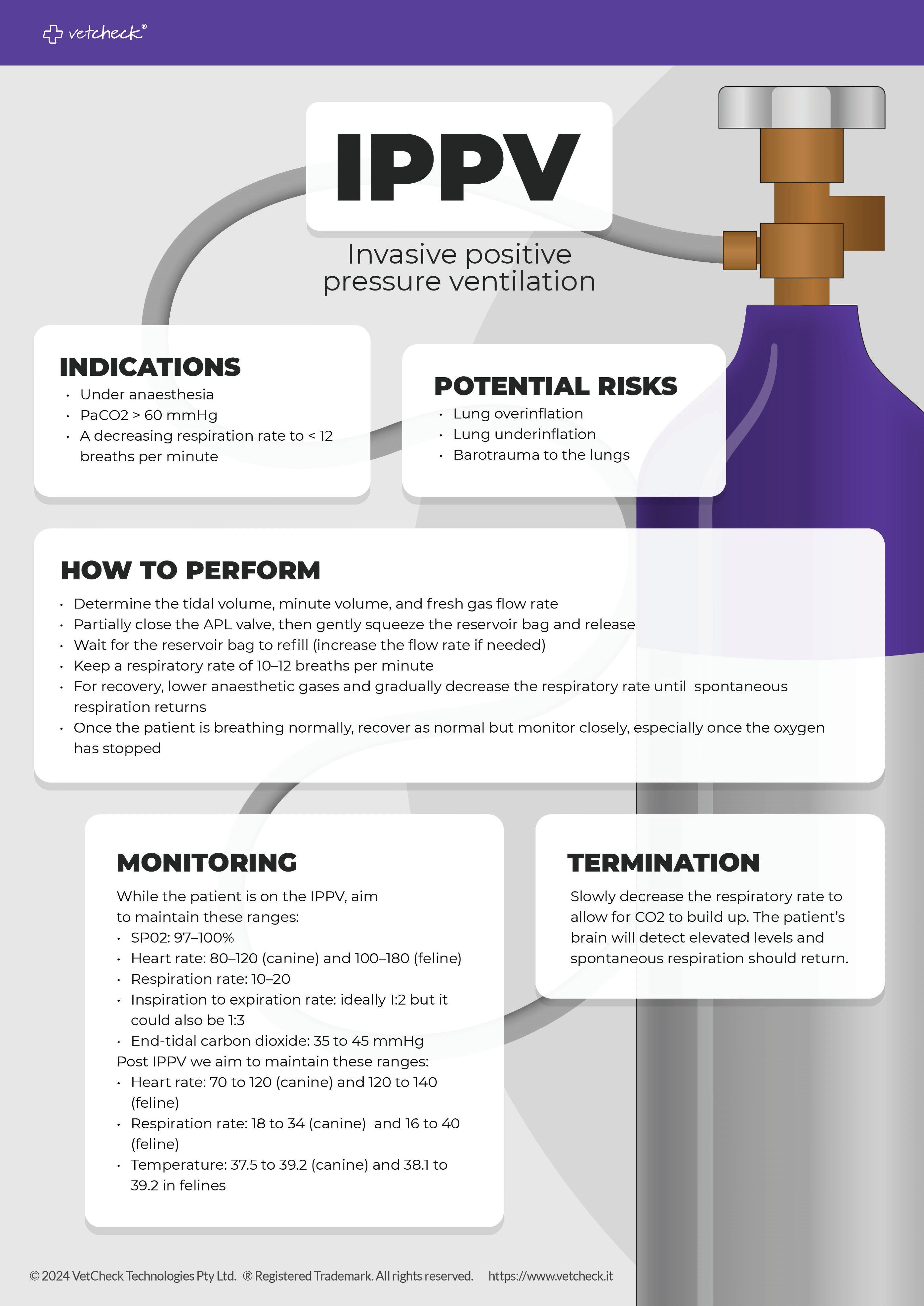
Member Vitals

My qualifications
Extended Diploma in Animal Care & Management (UK Qualification) Certificate III Animal Studies (ACVN)
Certificate IV Vet Nursing

I studied my Cert IV through AIRC, and they were absolutely amazing. My tutor was Jasmine Pengelly, and she was just an awesome support, although all the tutors that I spoke with were so inspiring and helpful.
Currently studying anything?
Not at the moment, however, I do have a few things lined up that I am aiming for!
I have just started in a practice manager role and so my future studying is aimed in that direction. I am enrolled in the VNCA Leadership Symposium, which should be great! I am also looking into the ‘Diploma of Leadership and Management’ through AIRC which I hope to have started before the end of this year. I love that this course is nationally recognised and is aimed at the management of veterinary clinics; also that it is run by AIRC, I feel very confident knowing that I will gain a great education with even better support! I have also been eyeing completing my Cert in Training and Assessment, but one step at a time! I do not, of course, want to lose my nursing roots! So, I participate in regular CE to maintain my AVNAT registration and to keep my skills and knowledge fresh.
Experience in the profession
I do still consider myself a ‘Baby Nurse’ having only been in the veterinary industry for 3 years (2020), although I feel very lucky to have found such an awesome first clinic that believed in me and allowed me to grow. I have recently (April 23) stepped up into a practice manager role in a new clinic, and I am loving learning more about the behind-the-scenes of the veterinary clinic. I have such a great team around me that inspires me to do the best job possible! Before my veterinary nursing career, I had worked with horses from the age of 14, first in the UK, and then when I moved to Australia, I worked in the horse racing industry. You get to learn a lot by working with horses – they seem to injure themselves on purpose!
Why did you choose veterinary nursing as your career?
I always had this voice in my head saying, ‘I should have been a vet nurse’. Except one day that voice said, ‘Why are you not a vet nurse?’ Later that week I left my
job at the racing stables and enrolled in my Certificate 3 in Animal Studies. I completed my Cert 3 first because I was not currently employed as a nurse, which is a prerequisite for Cert IV. However, not long after enrolling in Cert 3, I saw a job advert at a local vet clinic looking for an ‘Experienced & Qualified Nurse’, and I thought, ‘Oh well, I’ll apply anyway!’ And would you know it, they offered me a job as an SVN. By this time, it was too late to withdraw my Cert 3 enrolment, so I just ran with it and used the Cert 3 as credits towards my Cert IV.
I originally wanted to become an equine vet nurse; however, during my studies, I discovered how cool small animal medicine is and found a real love for it.
What has been your most memorable moment as a veterinary nurse and why?
I think it would have to be my first emergency ex-lap, which ended up being a splenectomy, on a Saint Bernard named ‘Thor’ (pictured). It was performed at 6 pm at the end of the day when most staff had clocked off for the day. The other nurse that was there had a call from her husband that her dog had been bitten by a snake and so she needed to attend to her dog! So … I was it! And it was AWESOME! The vet had full faith and trust in me, and I felt like a total pro! I went home that night knowing that the voice in my head all those years was so right, I should have been a vet nurse!
If you could give other nurses one piece of advice or a tip you have learnt, what would it be?
Just do it! Throw yourself into the vet nursing life and watch yourself thrive! Never let anyone tell you that you cannot do something. If you don’t know how to do it, go away and learn, talk to people, and come back and prove them wrong!
How do you keep a work/life balance?
I spend time outdoors! If I am not riding and spending time with my horse, I am walking my dog!
My husband and I also enjoy 4WDing and off-grid camping – and of course, if my dog can’t go, I don’t go either!
There’s something about being up in the mountains with no phone signal, no internet, and being surrounded by your favourite people and nature!
34 March 2024 MEMBER VITALS
Tamaryn Bond

Tarlea Hann
My qualifications
Registered student veterinary nurse with a Bachelor of Science (animal science)
University of Adelaide.
Currently studying anything?
I am currently studying for a Certificate IV in Veterinary Nursing. Working at a specialist centre means there are always ways to improve and grow. I’m continuously expanding my professional development by completing online CE courses and reading articles. There is always something new to learn as technology and techniques are updated.
Experience in the profession
I have been working at a specialist centre for over a year and a half now. Being a student nurse, I have quickly found a passion for the hustle and bustle that occurs across varying specialist departments. I have already developed my
knowledge and skills immensely working alongside amazing colleagues, each one teaching me as they bring a personalised skillset to every situation from their varying experiences.
Why did you choose veterinary nursing as your career?
Growing up, I’ve always been surrounded by animals big and small, with my mum being an example of the passion for animal welfare and conservation as she cared for them. With this early influence as a child I have always wanted to work with animals and that hasn’t changed. Alongside this, I wanted to have a career that made me want to get out of bed, that challenged me intellectually and a job that I would always have a way to continue learning. I did not know what capacity that would be, so I dove into the broad degree of animal science, in which I formed opinions on what parts of the animal industry I loved and what I wanted to focus on. Being eager and wanting to start my career as soon as possible, I landed in veterinary nursing. I now have the immense satisfaction of making a difference not only to animals but also to pet owners. Inspired by those I work with and those I have met, I am excited to continue learning as veterinary nursing evolves.
What has been your most memorable moment as a veterinary nurse and why?
It is so hard to choose just one. Working in a specialist centre brings so many new and exciting things every single day. Rotating between being an imaging, surgical, ward or medicine nurse, brings such a broad range of experiences: from doing a CT on a lion, a gastroscope on a dog, to doing the anaesthetic of an elevenweek-old kitten for a diaphragmatic hernia repair, to assisting in the ultrasound of a chimpanzee. Every day is a new opportunity
for memorable moments that fill me with excitement and wonder.
If you could give other nurses one piece of advice or a tip you have learnt, what would it be?
Be an advocate for your patients’ rights and needs, ensuring they receive the best care and treatment available. Having confidence in my abilities and what I know has made all the difference. Improving your knowledge truly improves the lives of the patients you touch.
How do you keep a work/life balance?
Keeping a work/life balance can be extremely hard in any profession, although being passionate about both work and study can make it a lot easier. It’s not always easy but being in a field I love and love to learn about definitely makes it easier. I think it’s important to know yourself, your limits, your strengths, your weaknesses and what work/life balance looks like for you. It looks different for everyone and not one solution works. Consequently, knowing yourself and being able to communicate that with a supportive workplace makes all the difference as others will know how to support you.
What animals do you own?
In my family home lives a beautiful staghound x kelpie, three cats, four chickens, two little barking geckos, one turtle, two rats and two rabbits. Along with my siblings, it can be quite the excitement. How long have you been a VNCA Member?
I have been a VNCA Member since March 2023. I have found that in this short time, my opportunities for CPD and interacting with like-minded people have been very rewarding. It is great to feel a sense of belonging as a member of this organisation and I am eager to be a part of the future that the VNCA is building.
What animals do you own?
I have a 3-year-old Black Labrador, ‘Sabre’ (no one can ever say his name, so he responds to pretty much anything!). Sabre is a typical ‘vet nurse curse’ dog that likes to vomit for no reason! But I love him so much; he completely changed my life! I also have an 8-year-old thoroughbred, ex-racehorse, ‘Mussoorie Magic’ aka ‘Moose’ (no one can say his race name either, so I figured
‘Moose’ was easier!). Moose is my first horse here in Australia and I can’t believe it took me 5 years to get one!
How long have you been a VNCA Member?
I joined the VNCA and AVNAT Registration Scheme in early 2022 as a Student Member until I completed my Cert IV and I have since upgraded to a VNCA Full Member and AVNAT registered veterinary nurse. It
is something that I am super passionate about, and I am lucky enough to work for a company that supports the progression of veterinary nurses and finances the VNCA membership. I encourage all nurses to become a member and my entire nursing team at the clinic I manage are members – even the students!
March 2024 35 MEMBER VITALS







THE AUSTRALIAN VETERINARY NURSES JOURNAL If you are considering publishing in the AVNJ as your next career goal but are not sure how to get started, we are here to help! There are lots of options available – from clinical and research articles through to case studies, opinion pieces and the ever-popular ‘Member Vitals’. As a starting point, check out the Author Guidelines on our website at www.vnca.asn.au/resources/avnj/authorguidelines/ When you are ready to submit, or if you have further questions, please email us on media@vnca.asn.au – whether it is the first time or you are a frequent contributor, we’ll make sure your journey to publishing in AVNJ is rewarding. The Official Journal of the Veterinary Nurses Council Austral ia Inc. Reg. No. A0031255G ABN 45 288948433 VOL MARCH THE AUSTRALIAN VETERINARY NURSES JOURNAL Obstructive urolithiasis in a guinea pig Cognitive needs of animals in urban society Equine nurse’s role in lameness examinations Distributive shock caused by a bee sting Workplace Helpline Industrial Relations & Human Resources for vet nurses Member Discounts $ The AVNAT Registration Scheme: There’s never been a better time to become a member of the VNCA and support our work to promote the interests of veterinary nurses and technicians across Australia. You will receive huge discounts on AVNAT registration, education opportunities and everyday purchases like petrol! And … you will be rewarded with all the #benefitsofbelonging. Follow the QR code to our website - www.vnca.asn.auto find out more and join online today! E: admin@vnca.asn.au | P: 03 9586 6022 #myVNCA #benefitsofbelonging Join the VNCA today and start enjoying all the benefits of belonging ... 50% Discount on Membershipsall Payment options for all of your clients vet care needs Australian Credit Licence Number 391975 • Available 24/7 to talk to your clients • VetPay works exclusively with Veterinary Practices • 10 years experience within the industry The VetPay Difference Proud to be partnering with VNCA in promoting wellness for vet nurses

Congratulations Accredited Veterinary Nurse Scheme
Launched in 2002, the Accredited Veterinary Nurse (AVN) Scheme is a joint initiative between the VNCA and the AVA (working together through the National Industry Advisory Group for Veterinary Nursing – NIAG).
It recognises veterinary nurses who demonstrate currency of skills and dedication to the veterinary nursing profession and is the gold standard for clinical veterinary nurses, providing an avenue for those who wish to extend themselves beyond AVNAT registration.
We recognise recently approved and renewing Accredited Veterinary Nurses:
New Accredited Veterinary Nurse
Lara Czarnota-Bojarski
Renewing Accredited Veterinary Nurses
Anja Dhalluin
Helena Davies
Rhonda-Anne Ponder
The AVNAT Registration Scheme
The AVNAT Registration Scheme has been established by the VNCA to set the standards of professionalism across the veterinary industry. Congratulations to our newest AVNAT registered veterinary nurses and technicians for their commitment to quality practice
Julie-Anne Austin
Deanna Bailey
Hannah Benfield
Jodie Borschmann
Riley Braund
Jesy Bright
Shannon Broome
Renee Burke
Bernice Chee
Grace Christiansen
Taylah Conlin
Dimiti Davidson
Kaylene Doust
Tara Edwards
Isabella Ellis
Jordyn Fox
Flora Foxx
Jordan Fraser-Seed
Jorgia Gibbs
Natalie Groeneveld
Melissa Hunter
Sarah Jafer
Jasmin Jimenez
Sophie Johnson
Gemma Kadiric
Antonia Laing
Ka Ki Todd Lau
Shannon Maskell
Camille Melone
Cherie Murdoch
Thailah Nienaber
Olivia Okely
Tracey Paterson
Sara Pineo
Elizabeth Raggio
Melody Ralph
Kirstin Reid
Carly Richmond
Darcy Scott
Charmaine Shilling
Mia Smith
Alex Soule
Phoebe Sparkes
Dayanara Suarez Jacobo
Georgina Symons
Sharnee Thomsen
Valeriya Tkachenko
Milly-rae Weight
Yardena Wenger
Lora Wiggins

AVNAT Registered Veterinary Nurses and Registered Veterinary Technicians demonstrate their commitment to their profession by:
• meeting entry level education
• completing ongoing continuing professional development
• abiding by a Code of Professional Conduct and Ethical Practice and related standards.
Find an AVNAT registered professional today via the AVNAT Online Register
March 2024 37 OUR PROFESSION
©gettyimages/Julia_Sudnitskaya
CELEBRATING GROWTH INSPIRING EXCELLENCE
17–19 April 2024
Adelaide Convention Centre
Register now for this unique chance to come together to commemorate 30 years of VNCA conferences with colleagues from around the country and beyond.
CONFERENCE HIGHLIGHTS
• Over 35 specialised lectures – Serving as a cornerstone for knowledge dissemination and intellectual exchange, these informative sessions provide a structured and comprehensive overview of key topics.
• Pre-conference masterclasses – These full-day sessions, conducted by experts in their field, will enhance your conference experience by providing a focused, interactive, and personalised learning opportunity.
• Conference workshops – Our two-hour workshops enrich the learning experience and provide tangible, hands-on skills that extend beyond the traditional lecture-style presentation.
• Three social functions – What better way to celebrate than to come together – amongst all the amazing education – and have some well-earned fun!
WHO SHOULD ATTEND?
We are excited to welcome a varied audience to participate in the conference, including experienced veterinary nurses/technicians seeking to broaden their knowledge, students embarking on their professional journey, those who look to strengthen their clinical skills, and emerging leaders in our profession prepared to advance to the next stage of their careers.
Limited sponsorship and exhibition opportunities are still available. Contact us today to secure the final places.
PRINCIPAL PARTNERS

REGISTER NOW TO AVOID MISSING OUT!
2024 CONFERENCE KEY DATES
Now available
Education Program
Tuesday 16 April 2024
Pre-conference Masterclasses and President’s Welcome Drinks
17–19 April 2024
30th VNCA Conference

VNCA Conference
WWW.VNCA.ASN.AU SCAN THE QR CODE TO REGISTER FOR THE 30TH VNCA CONFERENCE NOW


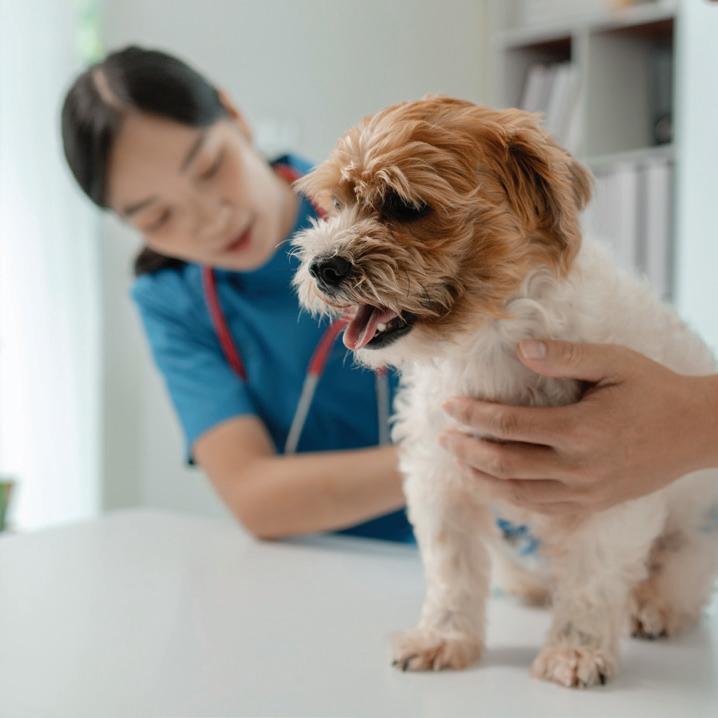


 Gary Fitzgerald VNCA President
Gary Fitzgerald VNCA President
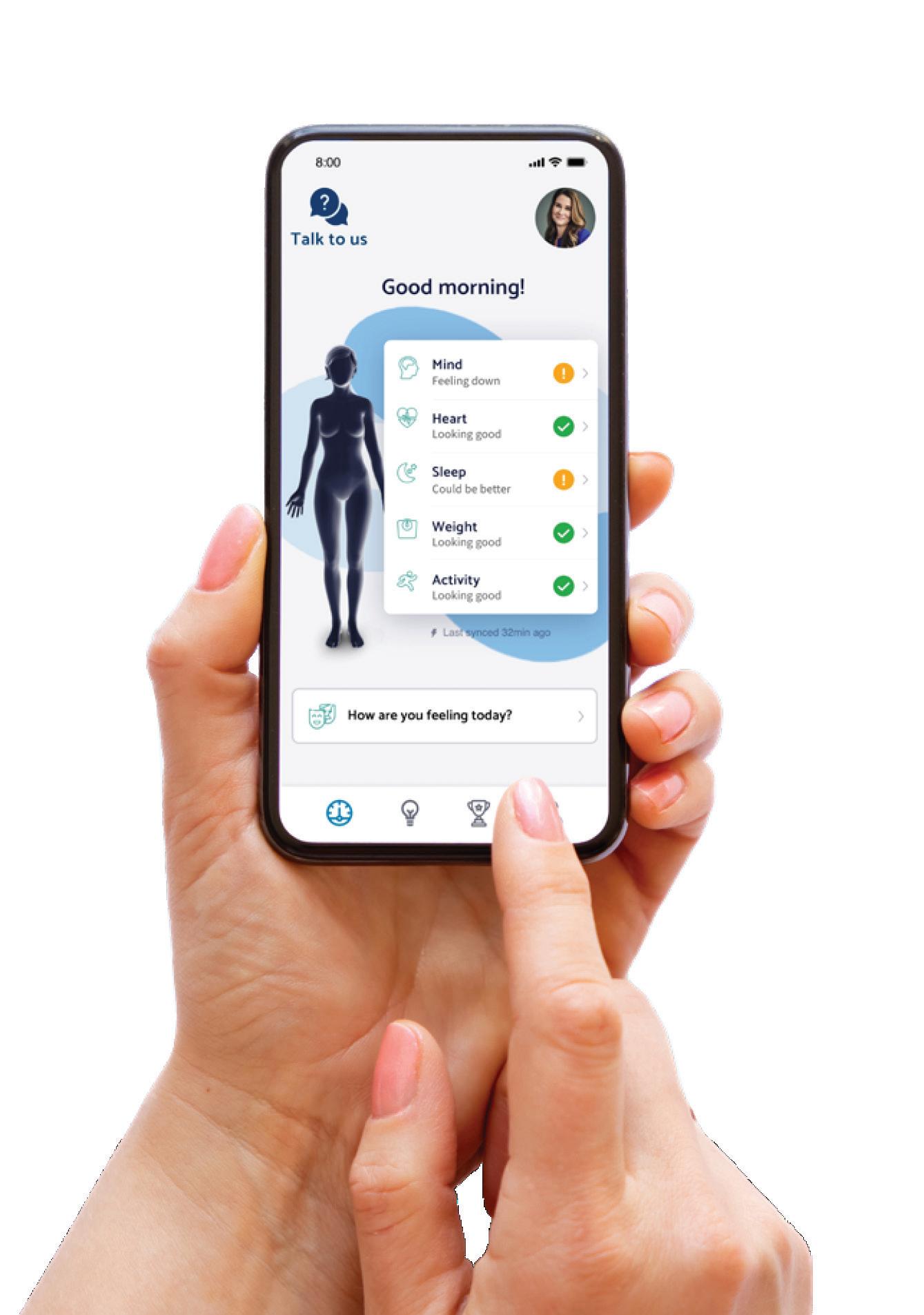













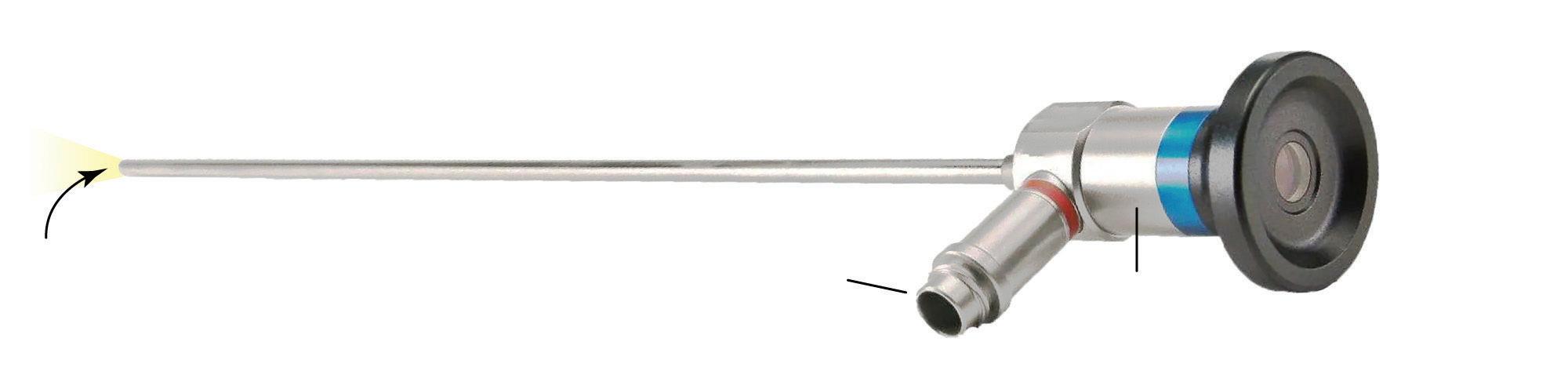
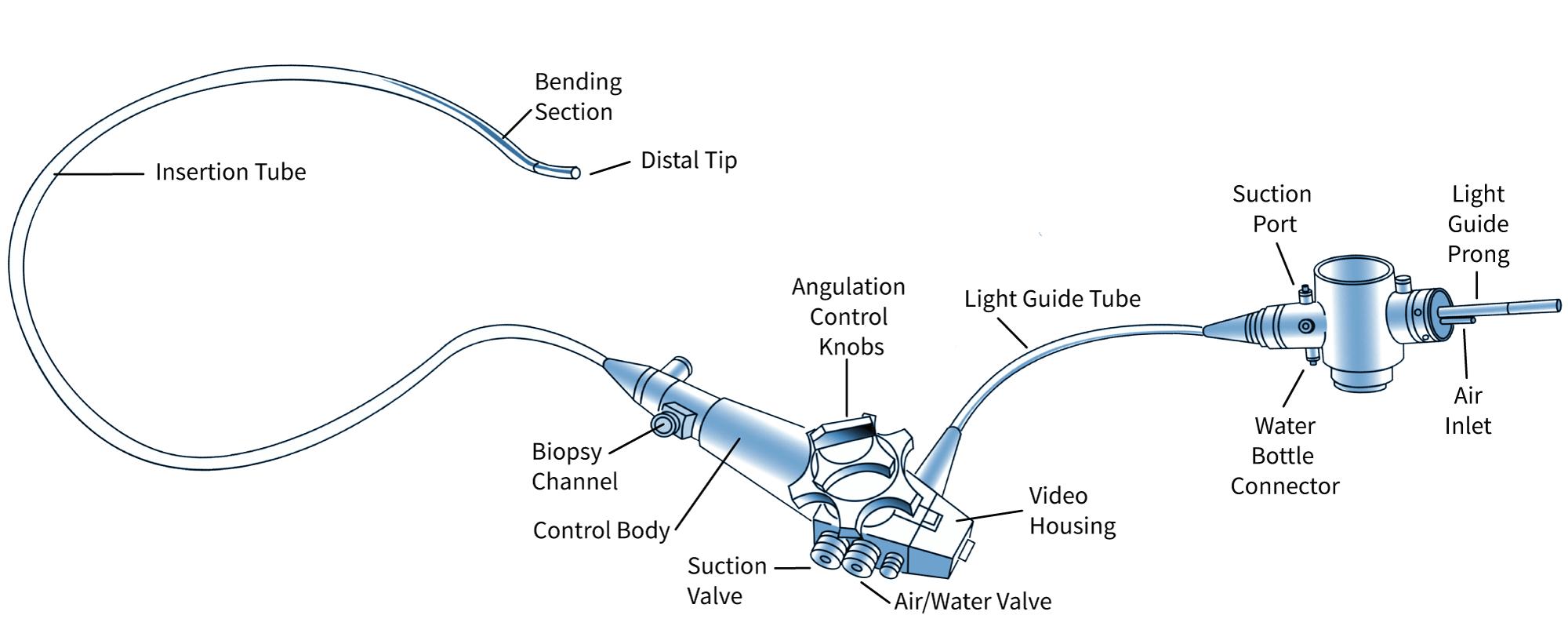








 Lake Eildon at capacity (above), and in a drought year (right)
Lake Eildon at capacity (above), and in a drought year (right)