The Official Journal of the Veterinary Nurses Council of Australia Inc. Reg. No. A0031255G ABN 45 288948433 VOL. 29 • NO. 3 • SEPTEMBER 2023 THE AUSTRALIAN VETERINARY NURSES JOURNAL Just breathe: Mechanical ventilation for small animals Principles of community-centred veterinary care Common presentations of avian emergencies Get ready to celebrate Veterinary Nurse & Technician Awareness Week Thefuture is in yourhand s AWARENESS WEEK VET NURSE & VET NURSE & TECHNICIAN TECHNICIAN 9-13 Oct o ber 2023
BOARD OF DIRECTORS
President Gary Fizgerald
Vice President Trish Farry
Michelle Foxcroft, Anita Parkin, Rebecca Coventry, Asha Yeoman, Samara Blake, Tayla Atkinson
VNCA MEDIA CHAIR
Janet Murray
Email media@vnca.asn.au
EDITORIAL COMMITTEE
Janet Murray
Lauri Steel
Elise MacPherson
Shauna James
REVIEW PANEL
Lauri Steel
Cert IV VN, DipVN (ECC & GP), DipVET, DipTDD, AVN, TAE, DipBus, Dip.Couns, DipBA, DipMgt, Cert IV CAS
Janet Murray
BSc Veterinary Nursing, AssocDegAdult&VocEd, Cert IV TAE, RVN, AVN
Elise MacPherson
Dip VN (GP) & SURG, Dip Lab Technology (Pathology Testing), Cert IV VN, RVN, AVN
Jo Hatcher
Dip VN, Cert IV VN, Cert IV TAE, RVN, AVN
Shauna James Cert IV VN, GradCertCaptVertMgt (CSturt), RVN
VNCA NATIONAL OFFICE
PO Box 7345, Beaumaris VIC 3193
Phone 03 9586 6022
Fax 03 9586 6099
Web www.vnca.asn.au
ADVERTISING
Phone 03 9586 6022
Email vnca@vnca.asn.au
VISION STATEMENT
The VNCA aspires to strengthen the position of Veterinary Nurses as part of the veterinary healthcare profession.
MISSION
The VNCA: Serves and represents all Veterinary Nurses Protects the professionalism of Veterinary Nurses
Promotes the value of Veterinary Nurses as vital in delivery of quality veterinary care Advocates for the increased recognition of Veterinary Nurses across Australia

Supports Veterinary Nurses through the provision of continuing education and networking opportunities
Strengthens the position of Veterinary Nurses across the veterinary industry Engages all Veterinary Nurses across the veterinary industry.

Cover image ©getty images/skynesher CONTENTS Contents VOLUME 29 • NO. 3 • SEPTEMBER 2023 NEWS & UPDATES 01 President’s report 02 VNCA joins forces with Vets for Climate Action 03 AVNAT Registration Scheme sees surge in registrations; moves closer to national recognition 04 Get ready to celebrate Veterinary Nurse & Technician Awareness Week 06 Just breathe – Mechanical ventilation for small animals 12 Principles of community-centred veterinary care 16 Common presentations of avian emergencies
Case Report – Warmblood with cervical vertebral myelopathy (Wobbler syndrome) 30 Anaesthetic monitoring 34 Client fact sheet – How to tell if your pet is in pain 36 VNCA HR Advisory Service – Flexible working arrangements 38 A brief history of VfCA 39 Member Vitals – Iffy Glendinning
Congratulations to our AVNS
Congratulations to our AVNAT registered professionals
VISION & OUR MISSION 30 12
24
40
41
OUR
THE AUSTRALIAN VETERINARY NURSES JOURNAL
President’s report
Ihope this message finds you well, energised, and passionate about the year ahead. As spring approaches, so does an increase in caseload, particularly with anticipated snake envenomation and tick paralysis cases as the weather gets warmer. Let’s remember the importance of open communication with colleagues, friends, and family. We’re all in this together. The upcoming RUOK day on 14 September reminds us to ask, ‘Are you okay?’ and have meaningful conversations.
In October, we have an important week to look forward to – the Veterinary Nurse and Technician Awareness Week (9–13 October). It’s a time to acknowledge and thank each of you for your incredible contributions as part of the one healthcare team. The theme for this week is ‘The Future is in Your Hands’, which resonates with the VNCA’s initiatives this year. Our continuous efforts towards protection of title, national registration, and regulation of veterinary nurses and
technicians will undoubtedly shape the future of the veterinary industry.

Since the last AVNJ issue, the Australasian Veterinary Boards Council (AVBC) and the VNCA collaborated in Melbourne to advance regulation and title protection for veterinary nurses and technologists across Australia. Our board of directors remain committed to progressing this agenda and address it regularly in our meetings.
July witnessed the New South Wales parliament launching an inquiry into the veterinary workforce shortage. Our submission, primarily addressing the role and challenges faced by veterinary nurses, aimed to spotlight the indispensable role we play within the veterinary healthcare team. Recommendations encompassed solutions to the challenges voiced by our members – skills utilisation, remuneration, workloads, attrition rates, and wellbeing for veterinary nurses and technicians.
Our continuous efforts towards protection of title, national registration, and regulation of veterinary nurses and technicians will undoubtedly shape the future of the veterinary industry.
Gary Fitzgerald VNCA President
In the days prior to writing this, I have been invited to represent the VNCA’s submission and present evidence at the NSW parliament hearing in Sydney. This opportunity to address challenges and suggest solutions is both exhilarating and nerve-wracking. Reflecting on past reports, it’s clear that veterinary practices across the nation have struggled with staffing shortages and increased workloads for many years. Change is imperative, and the NSW parliament’s involvement signifies their engagement to find appropriate solutions. The phrase ‘The Future is in Your Hands’ rings truer now more than ever.
Lastly, we have a chance to acknowledge those who consistently go above and beyond. Nominations for the Veterinary Nurse or Technician of the Year Award, as well as Student Veterinary Nurse and Technician of the Year, are now open and will close on Friday 15 September.
I wish you all the best in the upcoming months and eagerly await posts showcasing your team’s recognition and celebration of your contributions as vet nurses and techs.
Thank you
Gary Fitzgerald VNCA President

FROM THE PRESIDENT September 2023 1
VNCA SUPPORTERS 2023 VET NURSE/TECHNICIAN OF THE YEAR SUPPORTER PROFESSIONAL DEVELOPMENT SUPPORTER
VNCA joins forces with Vets for Climate Action
New partnership aims to drive environmental sustainability and animal welfare advocacy
In an exciting development for the veterinary community and the broader cause of environmental stewardship, Vets for Climate Action (VfCA) and the Veterinary Nurses Council of Australia (VNCA) recently entered into a partnership agreement. This collaboration marks a significant step forward in advancing the shared mission of both organisations – to promote responsible environmental practices within the veterinary field while ensuring the wellbeing of animals.
The VNCA and VfCA’s alliance is embedded in their collective commitment to addressing the pressing issue of climate change and its impact on animals, ecosystems, and the veterinary sector as a whole. With a strong focus on sustainability and holistic animal care, this partnership is poised to bring about meaningful change.

Both parties are enthusiastic about the prospects of this collaboration and are
dedicated to progress in the field of climate action and animal care. As a partner, VfCA will offer VNCA members a host of valuable services aimed at fostering knowledge, engagement, and action towards a more sustainable future. These offerings include microlearning sessions, dedicated webinars, lectures at the 30th VNCA Conference, and informative articles in the Australian Veterinary Nurse Journal (AVNJ) centred around climate care, as well as exclusive discounts to VNCA members attending VfCA’s educational webinars, seminars, and climate care programs.
VfCA’s flagship initiative, the Climate Care Program, is set to play a pivotal role in this partnership. The program, developed collaboratively by veterinarians, vet nurses, educators, and researchers, comprises a comprehensive, online 6-module course designed to guide veterinary practices through step-by-step

processes to enhance their environmental sustainability. By focusing on areas such as energy and water conservation, waste reduction, chemical use reduction, and fostering a culture of sustainability, the program not only benefits the environment but also supports increased profitability for practices. This program’s self-paced nature ensures that even busy veterinary practices can effectively implement the recommended changes.
As the VNCA and VfCA join hands to address the pivotal issue of climate change, they are demonstrating that collective efforts within the veterinary field can create a powerful impact on both animal welfare and global sustainability. With the implementation of the Climate Care Program and the wide array of resources offered to VNCA members, this partnership will engage our community through key initiatives that support a more resilient and responsible future.
NEWS 2 September 2023
DIVISION CONTACTS If you would like to attend a divisional committee meeting, it is important that you RSVP. NSW Melissa Shoard E nsw@vnca.asn.au QLD Jade Davies E qld@vnca.asn.au SA Sonia Van De Kamp E sadiv@vnca.asn.au VIC Danielle Gaynor E vic@vnca.asn.au WA Tracey Woods E wadiv@vnca.asn.au DIVISION CONTACTS it
Quality practice through standards and learning
AVNAT Registration Scheme sees surge in registrations; moves closer to national recognition
We have now entered our fifth registration and CPD cycle since the launch of the AVNAT Registration Scheme in 2019. In the last few months, there has been an increase in the number of veterinary nurses and technicians becoming registered, which shows the level of commitment and dedication to your profession and brings us another step closer to becoming a recognised true profession.


The AVNAT Regulatory Council, along with the VNCA Board and Professional Advancement Committee, have been working closely in the last few months with the Australasian Veterinary Board Council (AVBC) on the progression towards national mandatory regulation across Australia.
In May, representatives from the AVNAT Regulatory Committee, the Professional Advancement Committee and the VNCA Board, attended a meeting with the AVBC along with the chairs and registrars from all Australian state veterinary surgeons’ boards and from New Zealand. The day was dedicated to discussion on how national registration of veterinary nurses and technicians could be developed. While there are still some challenges in changes to legislation for this to occur, those who attended agreed this is a step that is vital for the future of the veterinary profession.
Also in May, Jo (the chair of the AVNAT Regulatory Council) was invited to speak at the AVA conference by the
Veterinary Business Group of the AVA. Jo spoke in the ‘State of the Market’ panel and in a lecture on registration of veterinary nurses and technicians and the AVNAT Registration Scheme. Both sessions were well attended and again there was positive support for registration.
The AVNAT Committee has now commenced the process of conducting the audit for the 2022/2023 cycle of registration and CPD. Audits
spent or planned to spend more than 12 months away from work, then you would be subject to the Return to Practice Policy conditions. For more information on this policy, please visit the VNCA website under AVNAT policies and framework. To apply for a career break, please complete the online form on the VNCA website under the renewal hub.
Are you interested in becoming registered
NEWS
September 2023 3
©getty images/Antonio_Diaz
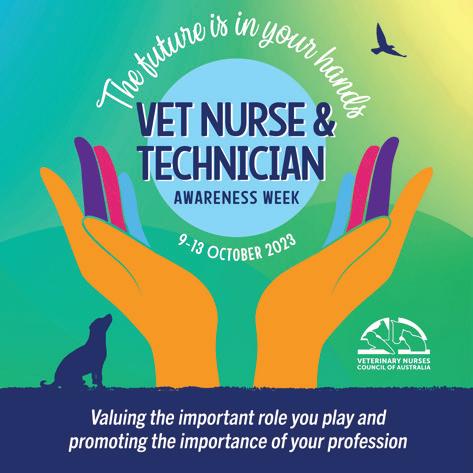
Get ready to celebrate Veterinary Nurse & Technician Awareness Week
As October draws near, veterinary nurses and technicians across Australia are gearing up for an exciting week dedicated to raising awareness about their vital contribution to the animal healthcare industry.
From Monday 9 October to Friday
13 October, Vet Nurse & Technician Awareness Week will shine a spotlight on you – who are often the unsung heroes within the veterinary healthcare team.
The theme for this year’s awareness week is ‘The future is in your hands’. This powerful theme aims to empower veterinary nurses and technicians with essential messages about accountability, self-management, education, skill utilisation, profession advocacy, and goal setting. Throughout the week, daily themes will be unveiled, and these will be reinforced through various communication channels. A daily online micro-learning unit will be made available for our community.
As the week draws to a close, veterinary nurses and technicians are invited to celebrate their achievements and dedication on Veterinary Nurses & Technicians Appreciation Day. The day will be filled with festivities and gratitude, honouring the contribution of our
exceptional community. On this day, the efforts and dedication of these professionals will be acknowledged and celebrated. Undoubtedly, a highlight of the week will be the announcement of the winners of the prestigious 2023 Veterinary Nurse/ Technician and Student Veterinary Nurse/Technician of the Year awards, proudly sponsored by Hill’s and Boehringer Ingelheim.

To further amplify the awareness campaign, various downloadable resources will be released in the lead-up to the Vet Nurse & Technician Awareness Week. These resources are aimed at helping participants bring awareness to their roles, celebrate the week in their workplaces, and participate in exciting initiatives, including a competition centred around the theme ‘The future is in your hands’.
HELP US TO RAISE THE PROFILE OF THE WORK THAT WE DO …
The veterinary community is encouraged to follow the Veterinary Nurses Council of Australia (VNCA)
on social media platforms such as Facebook and Instagram to stay updated with the latest developments. Additionally, they can download social media tiles, add their photos, and share empowering statements using hashtags like #VNTAW23, #myVNCA, and #TheFutureIsInYourHands.
The Vet Nurse & Technician Awareness Week 2023 promises to be a dynamic and inspiring event, fostering a sense of unity, celebration, and professional growth among veterinary nurses and technicians nationwide.
AWARENESS WEEK VET NURSE & TECHNICIAN VET NURSE & TECHNICIAN
The future is in your hands
NEWS 4 September 2023
VNTOY Awards are proudly sponsored by
9-13 October 2023
Dive into the exciting week ahead!
With Veterinary Nurse & Technician Awareness Week 2023 just around the corner, it’s time to gear up for a week filled with empowerment, education, celebration, and camaraderie.










Mark your calendars and get ready to make the most out of this fantastic opportunity to connect with peers, learn, and contribute to the growth of your profession. Here’s a sneak peek into the planned schedule for each day of the week, so you can start planning your participation now:
DAY 1: Accountability
Kickoff Speaker: Amy Newfield
On the first day, embrace the theme of accountability. Tune in to Amy Newfield’s anticipated talk, where she will inspire you to take ownership of your personal and professional development. The day’s focus will be on how each individual can contribute to their growth by being accountable for their journey.
DAY 2: Self-management

























Speaker: Erica Honey
Erica Honey will lead the discussions on self-management. Learn how to set meaningful goals and devise effective plans to ensure your success. This day is all about fostering a proactive approach to your career, allowing you to shape your path with purpose and clarity.
As you prepare for this transformative week, make sure to pencil in the schedule, participate in the planned activities, and engage with the speakers and events. Keep an eye out for updates, resources, and engaging content leading up to the Veterinary Nurse & Technician Awareness Week. Get ready to embrace the theme 'The future is in your hands' and be a part of this enriching experience that celebrates, educates, and empowers veterinary nurses and technicians across Australia.
DAY 3: Education & Utilisation
Speaker: Suzie Mclean
Suzie Mclean’s insights will guide you through the realm of education and skill utilisation. Discover how to build confidence in your abilities and commit to continuous learning for career growth. This day will empower you to harness the power of knowledge and put your skills to effective use.
DAY 4: Advocacy
Keynote Speaker: Patricia Clarke
Advocacy takes centre stage on Day 4. Patricia Clarke’s potential talk will highlight the significance of your role and how you can promote the importance of the veterinary nursing and technician profession. Learn to advocate for both yourself and your profession, acknowledging the valuable contributions you make.
DAY 5: Celebrating Your Success
Celebrate with VNCA: Announcing Vet Nurse/ Technician of the Year Awards





















The week concludes on an exhilarating note. Join the Veterinary Nurses Council of Australia (VNCA) in celebrating your achievements and dedication. The highly anticipated moment arrives as the Vet Nurse/Technician of the Year and Student Vet Nurse/Technician of the Year awards, sponsored by Hills and Boehringer Ingelheim, are announced. The celebration continues as the VNCA takes time to reflect on the organisation’s accomplishments over the past year.

NEWS September 2023 5
Just breathe
Mechanical ventilation for small animals
by Asha Yeoman Cert IV VN DipVN (ECC) RVN AVN
Mechanical ventilation is positive pressure ventilation (PPV) provided by a specialised unit designed to maintain the respiratory functions of a patient who is unable to adequately breathe to sustain life without assistance. There are many circumstances in which a patient may require mechanical ventilatory support and the prognosis will vary according to the individual patient’s conditions and underlying pathology. One retrospective study (Hopper et al., 2007) found that patients receiving mechanical ventilation for pulmonary disease had a survival to discharge rate of 22%, whereas patients with hypoventilation were documented with a 39% survival to discharge.
INDICATIONS FOR MECHANICAL VENTILATION
There are three primary indicators to support the implementation of mechanical ventilation.
Spontaneous ventilation involves a delicate balance of muscular contraction and relaxation, energy expenditure and pressure gradients.
Inhalation is an active process, whereby the thoracic cavity expands in size by contractions of the diaphragm and intercostal muscles.
Severe hypoxaemia
Oxygenation status is assessed by measurement of the partial pressure of oxygen in an arterial blood sample (PaO2). Hypoxaemia is defined as a PaO2 of < 80 mmHg, while a PaO2 of < 60 mmHg is considered severe hypoxaemia. Ideally, PaO2 is measured using an arterial blood sample in a blood gases analyser. If this is not available, pulse oximetry may be used but is less accurate and less reliable. An SpO2 reading via pulse oximetry of 90% is equivalent to approximately 60 mmHg PaO2. Potential causes of severe hypoxaemia may include pulmonary parenchymal disease, ventilation-perfusion mismatch, diffusion defects, and conditions such as ARDS and smoke inhalation.
Severe hypercapnia
Hypercapnia is defined as a partial pressure of carbon dioxide (PCO2) of > 50 mmHg. Severe hypercapnia is a PCO2 of > 60 mmHg. Hypercapnia may be caused by dead space ventilation, increased carbon dioxide production, and various conditions or events such as neurological disorders, airway obstruction, toxicosis, and pleural space conditions, amongst many other potential causes.
Severely increased respiratory effort or risk of respiratory fatigue
Patients who are utilising excessive stores of energy to maintain spontaneous ventilation and are subjectively deemed at risk to be unable to maintain such increased effort, may require mechanical ventilation to support their respiratory function.
RESPIRATORY PHYSIOLOGY
Spontaneous ventilation involves a delicate balance of muscular contraction and relaxation, energy expenditure and pressure gradients. Inhalation is an active process, whereby the thoracic cavity expands in size by contractions of the diaphragm and intercostal muscles. This expansion creates a negative pressure system, and therefore a pressure gradient resulting in air flow between the low pressure space (the airway opening) and the high pressure space (the lungs). Conversely, exhalation is a passive process in which the contracted muscles relax and allow the thoracic cavity to reduce to its original size, expelling the air flow.
The efficacy of spontaneous ventilation not only relies on the effectiveness of the above systems utilised in inhalation and exhalation, but the adequate inflation of the lungs, which is dependent on two aspects –compliance and resistance – which are two factors to consider when selecting appropriate mechanical ventilation settings. Pulmonary compliance is a measure of the lung’s elasticity or expandability and refers to the lung’s ability to stretch and expand. Variables that may impact pulmonary compliance include the elasticity of connective tissues, surface tension, and the position of the patient, as well as pathological conditions such as pneumonia, emphysema, and acute respiratory distress syndrome (ARDS). Airway resistance refers to the resistance of the respiratory tract to air flow along the pressure gradient
6 September 2023 CLINICAL
during both inhalation and exhalation, noting that resistance can differ in inhalation compared to exhalation. This resistance is dependent on the length and diameter of the airway as well as the viscosity and density of the gases (Hagen-Poiseuille equation) and can be affected by changes in such.
During mechanical ventilation there are 4 types of breaths a patient may take. Spontaneous breaths are those that are initiated and undertaken solely by the patient without intervention or support by the ventilator. If a spontaneous breath is initiated by the patient but subsequently supported with air flow from the ventilator, it is deemed a supported breath. Breaths that are initiated and controlled entirely by the ventilator without patient effort are termed mandatory breaths, and breaths that are produced in part or in full by the ventilator are assisted breaths. A breath can be further categorised into four phases: initiation of inspiration, inspiration, end of inspiration, and expiration.
The aim of mechanical ventilation is to provide respiratory support

targeted to the patient’s specific needs, considering how and why the patient’s physiological respiratory function is impaired and what method of support is required to supplement that function. This is addressed by implementing targeted modes and settings designed to support volume, pressure, flow or timing – or a combination of any/all of those factors – according to the impairments identified and support required to sustain adequate respiratory function.
PRIMARY CONTROL VARIABLES
Volume control ventilation
In volume control ventilation, the operator can determine the tidal volume to be delivered by the ventilator over a set period. As such, the volume and flow are controlled and remain consistent, whilst the pressure is determined by the outcomes of the set tidal volume in conjunction with the patient’s pulmonary compliance.
Pressure control ventilation
In pressure control ventilation, the operator can determine a set airway pressure to be delivered over a set period. As the delivered pressure is
fixed and consistent, the resulting tidal volume and air flow will be determined by the patient’s pulmonary compliance and airway resistance.
VENTILATORY MODES
Continuous mandatory ventilation
Continuous mandatory ventilation (CMV) is a mode in which the ventilator delivers exclusively mandatory breaths, at a determined pressure or tidal volume, set at a time-triggered frequency. This mode is utilised in patients who are unable to initiate or deliver any spontaneous breaths, or patients who require specifically titrated respiratory support and spontaneous breaths are not appropriate.
Assist control ventilation
Similar to CMV, assist control ventilation (AC) delivers mandatory breaths at a determined pressure or tidal volume; however, these are set with a minimum respiratory rate and can be time-triggered or patienttriggered by allowing the patient to initiate a breath that is then delivered by the ventilator.
©shutterstock/unoL September 2023 7 CLINICAL Continued next page
Just breathe: Mechanical ventilation for small animals

Synchronised intermittent mandatory ventilation
In synchronised intermittent mandatory ventilation (SIMV), the number of mandatory breaths is set and delivered by the ventilator, but the patient can perform spontaneous breaths in between. The ventilator will synchronise the mechanically delivered breaths with the patient’s breaths to avoid breath stacking, but only the mandatory breaths can be controlled by rate. The patient’s breaths are not controlled and therefore there is no maximum respiratory rate in this setting.
Continuous positive airway pressure
Continuous positive airway pressure (CPAP) is a mode of continuous spontaneous ventilation; in this mode, the patient determines the timing and volume of spontaneous breaths independently initiated, whilst the ventilator provides a consistent positive airway pressure throughout the breath cycle. This supports the patient’s spontaneous breaths and is often used as a ‘weaning’ mode as the characteristics of the respiratory function are evaluated by the ventilator and will alert if inadequate.
Pressure support
Similar to CPAP, pressure support (PS) provides a continuous positive baseline airway pressure during the inspiration phase of the breath cycle, to aid in reducing airway resistance that may impact the patient initiating adequate spontaneous breaths. This mode is often used in conjunction with another simultaneously, such as CPAP or SIMV.
VENTILATOR SETTINGS
Within the selected modes of ventilation there are settings that contribute variable factors to address the patient’s specific support needs. Typically, these settings can be estimated utilising generalised factors and then adjusted according to the monitoring data produced during ventilation by both the ventilator and the patient. Pulmonary compliance and airway resistance are the primary factors to consider when selecting setting parameters.
Trigger variable
This parameter determines the trigger to initiate a mandatory breath; typically, it may be time whereby it determines the period of time that it delivers a mandatory controlled breath if the patient does not initiate a spontaneous breath. The trigger variable may also be pressure or flow sensitive.
Respiratory rate (RR) & I:E ratio
The respiratory rate can be set to a specific factor or by adjusting other variables such as minute ventilation, inspiratory time or expiratory time. While respiratory rates should factor the patient’s specific needs, they are typically set at 10–20 bpm.
The ratio of inspiration to expiration can be set specifically by the operator or calculated by the ventilator. Typically, this is set to 1:2 to ensure full expiration prior to the next inspiration.
Note: If respiratory rates are increased, the expiratory time should be decreased. The I:E ratio should not increase more than 1:1 to avoid intrinsic peep.
Inspiratory time and flow rate
Inspiratory time is typically set for one second but may be reduced if the patient is set to an increased respiratory rate. In VC modes, the flow rate can be set instead of inspiratory time; the faster the flow rate is set the quicker the breath is delivered. Flow rates are typically 40 L/min–80 L/min according to the patient’s needs.
©getty images/Alexandr Lebedko 8 September 2023 CLINICAL Continued from previous page
Consistent monitoring and intensive nursing care should facilitate rapid identification of complications that may occur during the provision of mechanical ventilation.
Tidal volume (TV)
A normal TV in healthy small animals is typically 10–15 ml/kg. In VC ventilation, often the TV is set to 6–8 ml/kg to avoid overdistension causing barotrauma in compromised lungs. The TV can be further increased if deemed insufficient for the patient’s needs, but typically is not set above 10 ml/kg.
Positive end-expiratory pressure (PEEP)
PEEP maintains pressure in the airways during exhalation and prevents full exhalation occurring. This results in the lungs remaining consistently semiinflated, which helps keep open alveoli that may have collapsed. Note: PEEP increases peak airway pressure and can potentially contribute to barotrauma. It also maintains an increased intrathoracic pressure, which could compromise venous return abilities.
MONITORING
Intensive monitoring is a core component of providing critical level care to patients undergoing mechanical ventilation. Ideally, a ventilated patient will receive 1:1 nursing care with a dedicated nurse to facilitate continuity of care and increase the potential for minor changes in condition to be identified early and addressed efficiently. Vital parameters should be assessed and recorded frequently to monitor trends, along with recording ventilator settings and patient data output to correlate findings and identify the potential requirement for adjustments. Parameters that should be regularly assessed may include:
• electrocardiography
• blood pressure
• capnography
• pulse oximetry
• body temperature
• heart rate
• mucous membrane colour and capillary refill time
• fluid intake vs output
• arterial blood gas values.
Recorded data should include nursing considerations provided, types of fluid and volumes, nutritional input, medications administered, sedative or anaesthetic agents utilised and volumes, and maintenance/ placement of all indwelling catheters or tubes.
COMMON COMPLICATIONS ENCOUNTERED DURING VENTILATION
Consistent monitoring and intensive nursing care should facilitate rapid identification of complications that may occur during the provision of mechanical ventilation. These complications may be the result of fluctuating ventilator setting requirements, patient condition changes, environmental changes or equipment dysfunction. Complications that may be encountered include:
Hypoxaemia and oxygen desaturations
Hypoxaemia and oxygen desaturations may occur either acutely or gradually. An acute desaturation can indicate a sudden dramatic decrease in pulmonary function, such as a pneumothorax, or externally to the patient by equipment malfunction, lack of oxygen supply or disconnected circuitry. A gradual desaturation can indicate a progressive decrease in pulmonary function, such as the development of pneumonia, ARDS, or barotrauma. It may also suggest the potential for a circuitry leak or failing oxygen supply.
Troubleshooting would include confirming placement of monitoring equipment to ensure validity of results, assessing the circuitry for leaks or displacement and ensuring the adequate delivery of oxygen supply. The degree of hypoxaemia should be confirmed utilising arterial blood gas analysis and the patient assessed for potentially developing pulmonary conditions.
Hypotension
Positive pressure ventilation can lead to increased intrathoracic
pressure, which in turn can result in reduced venous return. High PEEP levels cause positive intrathoracic pressures during exhalation, which may further compromise venous return, also leading to or exacerbating hypotension. Hypotension may also be caused by hypovolaemia, cardiopulmonary disease, and resultant effects of medications administered.
Troubleshooting may include confirming placement of monitoring equipment and assessing the blood pressure cuffs for air leaks. Hypotension should be measured, and values confirmed utilising either an invasive blood pressure analysis method or an ultrasonic Doppler. If hypovolaemia is suspected, the fluid therapy plan prescribed may require adjustments. A medication review may be required to ensure the hypotension is not secondary to medical therapy or sedative/anaesthetic agents being utilised.
Hypercapnia
Hypercapnia may be noted as acute or gradual onset; however, typically the underlying causes are the same simply in varying severity. The source of hypercapnia is usually derived from either the patient end or the machine end of the ventilator system; causes within the patient may include pneumothorax, increased pulmonary dead space such as barotrauma, or an endotracheal tube obstruction or dislodgement. Ventilator equipmentrelated causes may include increased equipment dead space such as excess circuitry and/or connections, incorrect assembly of the ventilator circuit, or inadequate ventilatory mode and/or settings.
To troubleshoot a hypercapnic event, it is recommended to thoroughly evaluate the equipment and circuitry to confirm adequate and reasonable volumes and flow, consider suctioning or replacing the endotracheal tube and perform air leak and oxygen supply assessments. Blood gas
September 2023 9 CLINICAL Continued next page
Just breathe: Mechanical ventilation for small animals
analysis is beneficial to determine the validity of true hypercapnia, and the patient should be assessed for the development of pulmonary conditions.
Air leaks and air flow obstructions
Most ventilator machines will alert the operator to a detected air leak, or air flow obstruction noted whilst delivering breaths. An air leak is often attributed to disconnected or damaged circuitry or endotracheal tubes, whereas an air flow obstruction could indicate a physical obstruction within the circuitry or endotracheal tube, or progressive pulmonary disease causing increased airway resistance.
Troubleshooting an air leak or air flow obstruction is by similar methods to above: thoroughly evaluating the integrity of the equipment and circuitry, assessing for obstructions, and examining the patient for development or progression of pulmonary conditions.
NURSING CARE
Intensive level nursing care is a critical aspect in maintaining patient wellbeing and preventing complications during the provision of mechanical ventilation. Ventilated patients will be under sedation and therefore recumbent and unable to address their bodily functions or protective needs.
Ocular care
As a ventilated patient is under sedation, they are unable to protect the surfaces of their eye via blinking, which results in an increased risk of ulceration. Protective measures should be implemented by way of instilling topical lubrication into the eye to prevent dryness. It is important to note that in feline patients, recent studies (Eördögh et al., 2016) have documented that irritation can occur through use of ointment style ocular preparations, and so it is recommended to utilise liquid drops or gel-based lubricants in these patients. Topical lubrication should be administered every 2–4 hours. In addition, fluorescein staining should occur every 24 hours to assess for the
development of corneal ulceration so appropriate treatment can commence if necessary.
Oral care
Due to lack of movement, potentially abnormal saliva production, and absence of swallowing reflex, the patient is at increased risk of both oral/lingual drying and pooling of secretions. Oral care techniques should be performed every 4 hours and include gently cleansing the oral cavity with 0.05% chlorhexidine solution to reduce bacterial presence before thoroughly suctioning to remove excess secretions and debris. To prevent lingual drying, the tongue should be positioned within the mouth as best as possible, and a glycerine solution can be applied. Bruising, pressure sores and pressure necrosis are an increased risk due to lack of movement and tissues pressing; this can be minimised by frequent repositioning of equipment such as pulse oximetry probes and endotracheal tube ties, adjusting the tongue position away from the teeth, and utilising cushioning devices to reduce the pressure of the endotracheal tube against the surfaces of the mouth.
Airway maintenance
When intubating the patient for mechanical ventilation, a sterile endotracheal (ET) tube should be used to minimise the risk of bacterial contamination. It is broadly recommended to perform suctioning procedures in the ET tube, typically every 4 hours; however, some literature has suggested suctioning is only necessary when excess secretions or obstructions are suspected. The ET tube should be removed and replaced with a new sterile ET tube to minimise risk of secretions building and potential bacterial contamination. Humidification of the airway can be achieved by utilising heat and moisture exchange (HME) filters, and heated water humidifiers.
Toileting
The ventilated patient is at risk of skin irritation caused by pooling secretions
of urine or faeces, or overdistension from retention of these within their urinary bladder or bowel. The urinary bladder should be assessed for size and tension, and manually expressed at 4 to 6-hour intervals, as required. Alternatively, an indwelling urinary catheter with a closed collection system can be aseptically placed to ensure hygienic collection of urine and avoid potential scalding and associated skin inflammation or infection. If an indwelling urinary catheter is placed, this should be maintained with consistent catheter care protocols every 4–6 hours, such as cleaning with an 0.05% chlorhexidine solution to reduce the risk of bacterial contamination. Patients with or without an indwelling urinary catheter should have appropriate bedding and toileting pads placed underneath them to avoid contamination of the bedding and patient by leaked secretions.
Urine, whether collected by expression or within a closed collection system, should be measured and recorded as output in order to effectively calculate the fluid balances of the patient. This is typically recorded in a ml/kg/hr format.
Faeces should be collected and appropriate hygienic care provided to the patient’s anal region. Emollient creams may be applied if required to protect and soothe skin from inflammation and scalding.
Recumbent care
Pressure ulcers, tissue necrosis, peripheral oedema, and muscular atrophy can occur in patients with prolonged recumbency.
10 September 2023 CLINICAL Continued from previous page
Mechanical ventilation is a complex procedure provided to critical patients, with extensive aspects of care to be considered.
The recumbent patient should be rotated every 4 hours, alternating between sternal, left lateral, and right lateral recumbency. In some patients undergoing mechanical ventilation, lateral recumbency may not be appropriate due to individual needs and ability for thoracic expansion; in these patients it is recommended to maintain their cranial end in sternal recumbency and alternate their hind limbs between left and right lateral placement. Gentle passive range of motion exercises should be performed in conjunction with the regular rotation of the patient to assist in preventing muscular atrophy.
The patient’s bedding should also be considered to ensure adequate padding under all body surfaces. In large breed dogs, and patients predisposed to or with pre-existing joint disease, the bedding provided should include adequate support and positioning of the joints.
Reduction of stimuli
External stimuli, including light and
sound, may result in the need for increased sedative or anaesthetic agents. Implementation of barrier measures to reduce these stimuli sources may be warranted and may include placement of cotton balls or swabs within the patient’s ears and the use of a covering material such as a mask over the eyes. Barrier measures implemented should be recorded on the patient chart and changed at regular intervals to prevent contamination.
CONCLUSION
Mechanical ventilation is a complex procedure provided to critical patients, with extensive aspects of care to be considered. The veterinary nurse or technician providing this care should have adequate understanding of the variables and supportive requirements involved in order to contribute to improved patient outcomes.
References
American Association for Respiratory Care (AARC). AARC clinical practice guidelines.
Unlock boundless opportunities with AVNJ advertising!
Are you seeking to connect, collaborate, and conquer the veterinary industry? Look no further!
Elevate your brand's presence and seize the chance to mingle with top-tier professionals in the field. The Australian Veterinary Nurses Journal (AVNJ) is your gateway to unrivaled networking and relationshipbuilding opportunities.
Why choose AVNJ?
• 25+ years of industry trust and respect
• Exclusive readership of veterinary nurses and technicians
• National exposure through electronic and hard copy distribution
• Quarterly powerhouse of expertise in full-colour vibrance
Your brand deserves a spotlight that shines from coast to coast. Don't miss your chance to access
Endotracheal suctioning of mechanically ventilated patients with artificial airways. Respiratory Care 2010;55:758–764.
Boller M & Fletcher DJ. Post-cardiac arrest care. In: Silverstein DC and Hopper K (eds.) Small animal critical care medicine. 2014:17–25. St Louis: Elsevier. Edwards Z, Annamaraju P. Physiology, lung compliance. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan.
Eördögh R, Schwendenwein I, Tichy A, Loncaric I, Nell B. Clinical effect of four different ointment bases on healthy cat eyes. Vet Ophthalmol. 2016 Jul;19 Suppl 1:4–12.
Epstein S. Care of the ventilator patient. In: Silverstein DC and Hopper K (eds.). Small animal critical care medicine. pp. 185–190. St Louis: Elsevier.
Hopper K, Haskins SC, Kass PH et al. Indication, management, and outcome of long-term positive-pressure ventilation in dogs and cats: 148 cases (1990–2001). Journal of the American Veterinary Medical Association. 2007;230:64–75.
Mellema MS. Ventilator waveforms. In: Silverstein DC and Hopper K (eds.). Small animal critical care medicine. 2014:166–172. St Louis: Elsevier.
Peche N, Köstlin R, Reese S, Pieper K. Postanaesthetic tear production and ocular irritation in cats. Tierarztl Prax Ausg K Kleintiere Heimtiere. 2015;43(2):75–82.
Silverstein DC and Hopper K. Small animal critical care medicine. 2014. 2nd ed. St Louis: Elsevier.
Yagi K. Mechanical ventilation. In Veterinary technician’s manual for small animal emergency and critical care. CL Norkus (ed.). 2018.
a multitude of marketing avenues and amplify your visibility on a national scale.
Dive into the world of limitless potential today!
Scan the QR code or visit www.vnca.asn.
au to unveil a realm of possibilities.
September 2023 11 CLINICAL
Principles of communitycentred veterinary care
What can veterinary nurse/technology students and graduates learn from these principles to create inclusive veterinary practices?
by Courtnay L Baskerville Cert II EqStudies BBiomedSc (Hons) PhD GCertHE
ABSTRACT
Traditionally, education in veterinary nursing has largely focused on the required technical skills with a strong foundation of clinical knowledge. However, with the development and implementation of well-defined day one competencies (DOC) by the VNCA now encompassing communication skills, significant emphasis has been placed on the development of nontechnical capabilities for all veterinary nursing/technology (VN/VT) students. These DOCs essentially require VN/ VTs to reflect deeply – for example, when communicating effectively and expressing appropriate empathy, VN/ VTs must have some awareness of the complex social inequalities that many clients face when accessing veterinary care so that they can holistically support a client through challenging situations.
There has been much consideration of community-based veterinary medicine in the last few years, which largely focuses on the role of veterinarians delivering services to vulnerable community members. It could be argued, however, that there has been little consideration of the role VN/VTs can play here more broadly, and while these opportunities begin to emerge, the aim of this evidencebased, short communication is to consider social determinants of health and complex barriers that many clients face when accessing veterinary care and consider the role of practising VN/VTs in creating inclusive veterinary practices.
INTRODUCTION
In 2018, the Access to Veterinary Care Coalition commissioned a national study in the US to better understand the barriers to veterinary care. Here, it was found that in the previous 2 years, 28% of respondents had experienced a barrier to veterinary care and the primary barrier was financial (Wiltzius et al., 2018). To the author’s knowledge, similar studies have yet to be performed in Australia, but it is reasonable to consider that the current economic landscape of Australia will also likely be impacting access to veterinary care for Australian pet owners. As global events continue to impact households, concepts of accessible veterinary care, founded on the principles of primary healthcare (PHC) and social models of health are now being explored with urgency, as stakeholder groups and the larger veterinary industry work together to curb this emerging critical animal welfare issue. It could be argued, however, that there has been little consideration of the role VN/VTs can play here more broadly.
Like human nursing in medicine, the veterinary nurse/veterinary technician/technologist (VN/VT) remit in clinical practice is wide and varied and absolutely vital to upholding high standards of patient care. VN/VTs are regularly charged with highly specialised tasks such as documenting and administering controlled and cytotoxic drugs; operating radiography equipment, overseeing complicated patient care and monitoring anaesthesia; developing clinic protocols and
standard operating procedures and ensuring the safe storage, handling and disposal of hazardous chemicals (Harvey, Ladyman, & Farnworth, 2014). As we unpack the remit of VN/VTs, it is clear that the contributions of VN/ VTs in clinical practice have played heavily in shaping modern veterinary medicine and veterinary patient care. While the industry works to clarify and bolster the practice of veterinary nursing in Australia and worldwide, the technical aspects of nursing are often the defining characteristic of a VN/VT (Orpet & Jeffery, 2022). It has been noted that clarifying these technical aspects of veterinary nursing is vital for the larger veterinary industry so that VN/VTs may practise to their full capabilities in clinical practice (VN Futures Report, 2016). While these initiatives aim to enhance professional satisfaction and curb the ‘dissatisfaction crisis’ that has been outlined previously (Rumple, 2021), it will likely also enhance society’s understanding of the role of VN/VTs (Davidson, 2017).
VN/VTs should anticipate that like human nursing, the profession of veterinary nursing will likely be required to meet complex societal expectations, and with the implementation of well-defined day one competencies (DOC) by the VNCA now encompassing communication skills, significant emphasis has been placed on the development of non-technical capabilities for VN/ VT students. These DOCs essentially require VN/VTs to reflect deeply –for example, when communicating, effectively expressing appropriate
12 September 2023 CLINICAL
empathy, VN/VTs must have some awareness of the complex social inequalities that many clients face when accessing veterinary care so that they can holistically support a client through challenging situations. It is, therefore, vitally important for VN/VTs to continue to explore the community landscape VN/ VTs operate in, notably regarding accessible and inclusive veterinary care. The aim of this evidence-based, short communication is to consider social determinants of health and complex barriers that many clients face when accessing veterinary care and consider the role of practising VN/ VTs in creating inclusive veterinary practices.
COMMUNITY-BASED VETERINARY MEDICINE
In the human healthcare sector, the area of medicine which is concerned with the health of a community is often referred to as PHC. Here, PHC is an approach which aims to strengthen health systems, bringing healthcare closer to communities in a whole of society approach (WHO, 2023). According to the World
Health Organisation (WHO), PHC is fundamentally grounded in the premise that all people have the right to achieve high levels of health (WHO, 2023) and it is recognised that when PHC is accessed early and consistently, there are associated benefits including improved patient outcomes and reduced health inequalities (Smolowitz et al., 2015). In 1998, WHO identified social determinants of health (SDH) which can influence health in positive and negative ways. These include: income and social protection, systemic and long-term structural conflict, social inclusion and non-discrimination, accessible education and access to affordable health services of good quality (WHO, 2023). Recent research exploring the parallel impact of SDH on animal health found that, not surprisingly, the SDH can and do impact the social determinants of animal health (SDAH) and an animal’s general health status (Card, Epp & Lem, 2018). Overall access to veterinary healthcare, continuity of veterinary care and voluntary preventive health screening for companion animals have been recognised as SDAH and
The aim of this evidencebased, short communication is to consider social determinants of health and complex barriers that many clients face when accessing veterinary care and consider the role of practising VN/VTs in creating inclusive veterinary practices.

these may be further impacted if a person is experiencing one or more SDH (Card, Epp & Lem, 2018).
Different terms in veterinary medicine have been used to describe veterinary care founded on the principles of PHC and social models of health, including community-focused veterinary care and veterinary community medicine. Authors of a large systematic review of veterinary care for underserved communities have recommended the term ‘Community-Based Veterinary
Continued next page ©shutterstock/SeventyFour September 2023 13 CLINICAL
Principles of community-centred veterinary care
Continued from previous page
Care’ (CBVC) to describe interventions and clinics addressing underserved animal populations at the community level (this term will be adopted here) (LaVallee, Mueller, & McCobb, 2017). In practice, principles of CBVC may be offered through exploring incremental or spectrum of care options with clients. The scholarship of spectrum of care suggests that with limited information, clients and veterinary professionals can equate expensive treatment/diagnostics with superior veterinary care (Stull et al., 2018). Yet, the provision of veterinary services will often be influenced by many factors, including principles of best practice or ‘gold standards’, practice goals and values, clinic resources, the knowledge and skills of the veterinarian, as well as the owners’ goals, values, resources and knowledge (Stull et al., 2018). Stull et al. (2018) conclude that providing a continuum of acceptable care that is both evidence-based and client responsive is the cornerstone of the principles of spectrum of care; however, the greatest challenge is perhaps influencing veterinarians and motivating behavioural change. The concepts of CBVC were largely considered ‘hidden curriculum’ in veterinary education where lessons, values or insights are passed on to students, formally or informally and sometimes, purposefully, or not
(Whitcomb, 2014). Today, servicelearning experiences, where studentrun veterinary clinics offering low cost veterinary care are beginning to emerge in the US as part of the embedded veterinary curriculum and the clinical rotation experience. According to current research, after veterinary students attended the service-learning experiences during CBVC clinic rotations, students reported that they were significantly more confident in managing cases where there were barriers to care (King et al., 2021). Further, a study of fourth-year veterinary medicine students found that purposeful information raising awareness about accessible veterinary care enhanced students’ understanding of barriers to veterinary care and students’ opinions of incremental care and/or spectrum of care options were more favourable (Hoffman, Spencer & Makolinski, 2021). Students recognised that regardless of whether they were intending to practise in CBVC, an awareness of care barriers and confidently managing cases where barriers were apparent, was important to gain a broader understanding of diverse communities to meet the needs of all clients (King et al., 2021).
It is clear that these outcomes are relevant to VN/VTs in practice too. In the human healthcare sector, nurses
have historically played strong roles in community care as district or visiting nurses. While the evolution of veterinary nursing/technology has been largely hospital-based care, there are many areas where principles of PHC nursing could be modelled and adapted to a clinical setting. For example, adding CBVC practices to the ever-expanding veterinary nursing consult portfolio. However, to do this VN/VTs will need to be ready to critically evaluate assumptions, values and/or beliefs of accessible veterinary care and who has a right to access this care. In doing this, VN/VTs can lead initiatives by exploring SDAH and CBVC needs through community engagement, applying spectrum of care principles and revising terminology and communications with colleagues and owners around ‘gold standard’ care, and importantly, identifying and removing barriers to care that may have been unknowingly constructed.

In conclusion, accessible veterinary care is a critical animal welfare issue and while veterinary education is working to curb this through the implementation of purposefully curated CBVC curriculum, VN/VTs can also equip themselves and lead CBVC initiatives in the clinic and the community.
References available on request.
14 September 2023 CLINICAL
Learn new animal care skills in days or weeks. Nurture your career with a range of specialised short courses. + Caring for Native Wildlife in a Clinical Environment + Advanced Anaesthesia for Veterinary Nurses + Natural Therapies for Animals - Massage RTO 90003 | CRICOS 00591E | HEP PRV12049 tafensw.edu.au/short-courses
CELEBRATING GROWTH INSPIRING EXCELLENCE
17-19 April 2024
Adelaide Convention Centre
THE VNCA CONFERENCE COMMITTEE WARMLY INVITES YOU TO SUBMIT AN ABSTRACT FOR CONSIDERATION TO PRESENT AT THE 30TH VNCA CONFERENCE.
Your commitment to sharing your knowledge and expertise is paramount to the success of VNCA conferences. We understand the dedication it takes to craft and submit an abstract, and your willingness to contribute to the advancement of the veterinary nursing field is deeply appreciated.
CALL FOR ABSTRACT SUBMISSIONS CLOSING SOON
Don’t miss this unique chance to come together to commemorate 30 years of VNCA conferences with colleagues from around the country and beyond.
Scan the QR code below to visit the website and submit your abstract NOW!

SPONSORSHIP AND EXHIBITION PROSPECTUS NOW AVAILABLE
Over the past three decades, the VNCA Conference has been a beacon of knowledge sharing, professional development, and camaraderie for veterinary nurses and technicians from around Australia, and beyond. The 2024 conference promises to be even more remarkable as we commemorate our 30th anniversary and continue to advance
PRINCIPAL PARTNERS
the field of veterinary nursing. We invite you to be part of these celebrations – which we anticipate could be bigger and bolder than the previous 29 years!
You will need to get in fast – there are a few exclusive options to choose from and these will sell fast!
2024 CONFERENCE KEY DATES
Tuesday 19 September 2023
Abstracts submissions close

Thursday 19 October 2023
Presenter notifications
Wednesday 29 November 2023
Program launch and registration opens
Wednesday 6 March 2024
Early Bird registration closes
Tuesday 16 April 2024
Pre-conference masterclasses and President’s Welcome Drinks
17–19 April 2024
30th VNCA Conference
VNCA Conference
WWW.VNCA.ASN.AU SCAN THE QR CODE TO LEARN MORE ABOUT THE 30TH VNCA CONFERENCE
Common presentations of avian emergencies
by Rebecca de Gier VTS (Exotic Companion Animal), BAppSc (Wildlife Biology and Animal Production), Dip General Practice, Cert IV Vet Nurse, RVN, ALS Certified (RECOVER)
INTRODUCTION
According to our understanding of avian patients, the majority of the health issues that bring them to the veterinary clinic should be considered a medical emergency. Our treatment of these animals is crucial and can mean the difference between life and death, as the mortality rate in exotic animal emergency medicine is high. Avian patients require prompt veterinary attention, and proper first aid and emergency care can help stabilise their condition and increase the chances of a successful outcome. Emergency care involves expertly applying treatment techniques in response to injury or sudden illness, with the goal of preserving life, preventing further deterioration, and facilitating recovery.

©getty images/skynesher
16 September 2023
CLINICAL
RECEPTION
Assessing the severity of a patient’s condition over the phone can be challenging, but if the owner is calling with concerns about their pet, the recommendations from the consultation are crucial. To gather information, staff handling the calls can ask questions, such as the species and gender of the animal, its age, the symptoms, and any medication used. Keep in mind that exotic animals are skilled at hiding signs of illness, so by the time the owner realises their animal is sick, it is often in a serious and urgent state.
It is important for all staff to feel confident in their ability to evaluate a patient and plan for when and who should see them. This is the purpose of triage, which is a process of classifying patients based on the urgency of their situation, and reassessing as needed. This requires training, and the nurses must be competent, qualified, and experienced in handling emergency situations, as well as knowledgeable about emergency procedures. Most importantly, the veterinarian needs to trust the veterinary nurse or technician to determine the order in which patients are seen.
TYPES OF EMERGENCIES
HISTORY TAKING
Many avian patients are known to conceal signs of illness, and some species have limited daily interaction with their owners. Gathering information during a consultation or physical examination, or even handling the pet, can quickly worsen its condition.
It is essential to obtain a comprehensive medical history as many of the medical issues experienced by avian patients are often related to their living conditions and diet. The medical history may be taken after the pet has been rushed into the treatment room or in the consultation room with both the patient and the owner present.
A thorough physical examination can provide a significant amount of information, but valuable diagnostic insights can also be gained from a detailed history and an assessment of the pet’s environment or cage. Observing the patient visually can also be informative, and it is important to be mindful of the pet’s strength and avoid causing stress during manual restraint.
To effectively diagnose abnormal conditions, it is important to first
understand what is normal for the species. With over 200 different species of avian pets, each animal can present differently. Doing research to understand what is normal for the species before the consultation can help you identify subtle signs of illness before it’s too late.
HANDLING OF SICK PATIENTS
The examination of avian patients is similar to that of other species, but it’s crucial to gather as much information as possible from the patient’s history and visual examination before the physical exam. Allowing the pet to acclimatise for 5–10 minutes before the exam can reveal clinical signs that may have been missed and reduce stress on the patient. Before conducting the physical exam, ensure you have all necessary equipment and the room is secure. Avoid trying new techniques on sick or weakened patients as it can worsen their condition quickly. Before the exam, additional heat, a quiet environment, oxygen, and fluid therapy may be required to stabilise the patient. The handling of sick birds should be done with their medical condition in mind and may involve multiple procedures over several sessions or all at once, depending on the veterinarian’s direction. To be cautious when handling a sick bird, watch for signs such as open-mouthed breathing, weakness, dazed behaviour, and a weak grip, which indicate the patient is not coping and should be placed back in its cage for recovery. In some cases, the bird may require oxygen therapy.
A couple of important safe patient handling points to note:
• Birds do not have a diaphragm, so rely on the movement of their skeletal muscles to pass air around their body into their lungs and air sacs, so when handling ensure that the keel can move freely.
• If a patient presents with a fracture, that limb will continue to be painful
Anything not listed above
Triage classification Description Example First priority Life-threatening Treatment must be initiated within seconds to minutes Bring immediately to the treatment room
mentation,
of
Urgent Currently
priority Patient stable Pressing problem that is non-critical Treatment initiated within hours
lacerations, history of but not currently vomiting and/or diarrhoea, etc.
priority Patient completely stable Needs evaluation, but not urgently
Major bleeding, breathing problems, altered
shock, history
toxin ingestion, etc. Second priority
stable, but may become 1st priority patient, need to be reassessed, or have treatment initiated within minutes to hours History of major trauma, history of unsuccessful urination, repeated vomiting, or diarrhoea, etc. Third
Fever,
Fourth
September 2023 17 CLINICAL Continued next page
Common presentations of avian emergencies
until the fracture is stabilised and when you are handling these animals ensure that the injured limb is not placed in an unnatural position that will be causing neurons to be firing and increasing catecholamine release.
AVIAN SUPPORTIVE CARE
Nutritional support
Food is crucial in emergency situations involving birds, as they quickly deplete their glycogen stores. A sick or injured bird may stop eating, causing its condition to rapidly worsen. You can try enticing the bird to eat by offering a variety of foods that match their normal diet as much as possible. If your clinic often sees birds, it is advisable to have a range of food options, including:
• pelleted diets in different brands and sizes, appropriate for the species
• seeds for budgies and finches, and for larger parrots, pigeons, poultry, and waterfowl • lorikeet mix, in dry powder form or watered down to a syrup consistency • nut mixes for parrots as treats following treatment • frozen vegetables, in sizes suitable for smaller parrots or poultry and larger parrots
• chick starter and hen layer pellets, offered dry for poultry and submerged in water for waterfowl • Formulated mixes for omnivores or granivores, which can be mixed with commercial pet food or sprinkled on vegetables • Whole prey items such as mice and rats, for raptors and other species that form casts.
Additionally, you must consider the type of food and water bowls the animals will need to consume their food. Different bird species have different preferences, such as shallow plates for pigeons and doves, the ability to submerge their full beaks into wet lorikeet mix for lorikeets and being able to fit their head into the bowl for parrots. Some birds, particularly wild ones, may not know how to eat from bowls, so scatter feeding may be necessary.
In cases where a bird is not eating on its own, has lost weight, or has an
injury that prevents it from eating, crop feeding may be necessary. The crop volume of a parrot is around 3–5% of its body weight. The diameter of the crop needle should be appropriate for the patient’s oesophagus, and its length should reach the crop, located at the thoracic inlet. A red rubber tube and a 60 ml catheter tip syringe can be used for poultry or large macaws. The crop feeding formula should be mixed with hot or warm water to a pancake-like consistency. Before feeding, it is important to check that the temperature of the formula is between 38°C and 40°C to avoid crop stasis or burns. The bird should be adequately hydrated before starting the feeding process, as dehydration can slow down crop emptying.
When birds regurgitate, they shake their heads from side to side, and it is important to never hold them, as this can cause aspiration. After regurgitation, it is important to monitor the bird’s respiratory rate and effort and clear any food materials from the glottis using a cotton-tipped swab if necessary.
Warming
Birds consume a large amount of energy to maintain their body temperature and sick or injured birds can quickly become hypothermic. This rapid metabolic rate makes small birds particularly susceptible to hypothermia. To keep these birds warm, a heat lamp or brooder should be used. If a bird is cold, it will ruffle its feathers, tuck its head behind its wing and close its eyes. Thus, it is crucial to have a source of heat available for sick birds. The ideal setup is a hospital incubator or brooder that provides controlled heat and humidity.
When using a heat lamp for recumbent birds, a minimum gap of 30 cm should be maintained between the bird and the heat lamp to prevent overheating. Observe the bird for signs of heat stress, such as open beak breathing, and adjust the heat lamp as necessary. Be cautious of overheating, which can be indicated
Food is crucial in emergency situations involving birds, as they quickly deplete their glycogen stores. A sick or injured bird may stop eating, causing its condition to rapidly worsen. You can try enticing the bird to eat by offering a variety of foods that match their normal diet as much as possible.
by flat feathers, outstretched wings, and open mouth breathing. It is especially important to use caution in overweight birds.
For patients that require a brooder, it is advised to use the following temperatures:
• Neonate with no feathers – 32–34˚C
• Ducklings – 30˚C if BAR, 32˚C if QAR or dull, heat lamp and hotties if in a cage
• Adult/fully feathered birds that are critically unwell – 30˚C
• Adult/fully feathered birds that are mildly unwell – 28˚C.
Fluid therapy
Fluid intake is very important as sick or injured birds can rapidly become dehydrated and will always present as a percentage dehydrated. When avian patients are dehydrated, there is concern about poor tissue profusion and selecting the correct fluid type is equally important.
Crystalloid fluids
Crystalloid solutions, including normal saline and Hartmann’s, are balanced salt solutions that are widely used and freely pass through capillary walls. They remain in the bloodstream for a shorter period, typically 30 to 60 minutes, compared to colloids. Crystalloid fluid resuscitation can replenish fluid volume lost from the bloodstream and attract extracellular
Continued from previous page
18 September 2023 CLINICAL
water due to osmotic pressure. However, crystalloids with lower sodium concentrations distribute more evenly throughout the body, while higher sodium concentrations are more effective as plasma expanders.
Crystalloid therapy, however, can negatively impact microcirculatory blood flow and oxygenation in shock cases, leading to hypoxia even after resuscitation. Additionally, excessive use of crystalloid solutions can cause peripheral and pulmonary oedema and should therefore not be used in patients with heart disease.
Colloid fluids
Commonly used colloid solutions include Hetastarch and Plasmalyte. Unlike crystalloids, colloids are better at maintaining circulatory volume because their larger molecules stay in the blood vessels for a longer time, resulting in an increase in osmotic pressure. The proteins also draw water from the cells into the bloodstream. However, excessive use of colloids can cause cells to become dehydrated over time due to the loss of too much water. Colloids are effective in keeping blood volume stable. For birds needing hydration support, treatment can involve either intravenous or subcutaneous administration of warmed Hartmann’s solution.
Sites of fluid therapy administration include subcutaneous fluids in the inner inguinal membrane and intravenous fluid therapy via the jugular vein, medial metatarsal and basilic veins.
• Maintenance support: 5% body weight subcutaneously (SC) q12
• Correcting mild deficit or dealing with a bird that will not self-drink: 10% body weight SC q12
• Significantly dehydrated, primary renal dysfunction, or heavy metal toxicosis: 10% body weight SC q8
• Do not exceed the 30% body weight total daily amount to prevent fluid overload.
Hospital cage setup
To minimise stress for a sick or injured bird in hospital care, it’s important to provide a peaceful environment. A separate ward away from dogs, cats, reptiles, and birds of prey is recommended. The bird should be kept in a quiet, dark area to help it stay calm, and handling should be limited to essential times only. Additionally, the cage should block the view of other animals, and the bird may benefit from a covered area for added security.
For bedding, use newspaper or absorbent pads. Ensure the bird has access to water, food, and a perch if necessary. In special cases, such as a recumbent bird in need of support or
a geriatric bird needing joint support, a towel or cloth bedding can be used, but only after being rolled into a donut or folded into thick layers.
It’s important to weigh the patient at the same time every day, before administering any food or medication, using the same scale. In certain situations, the patient may need to be quarantined, requiring the use of personal protective equipment (PPE) and following proper cleaning and disinfecting protocols to protect other animals, staff, and yourself in the event of zoonotic diseases.
COMMON MEDICATIONS
Depending on the patient’s condition, medications can help with the recovery of a patient. We can look at providing adequate pain relief so that the patient is comfortable to move around, eat and display normal behaviours. Be sure to consider the selection of medications, as some choices will rule out the use of other drugs.
Selecting the route of administration can also be determined by the patient’s condition and access to possible indwelling catheters and IV lines.
Some medications can be given orally, so if the patient is being tube fed, the medications can be added to the slurry and given directly into the crop. Other routes of administration are IM and SQ injections. Be aware of the pharmacology and toxicology of the chosen medications to ensure that they will work as intended.
Common opioids used in birds are:

• Methadone/Morphine – 1 mg/kg IM q 6–12 hr
• Fentanyl – 6–20 mcg/kg/hr
• Butorphanol – 1 to 4 mg/kg IM q 1 to 3 hours
• 50 to 80 mcg/kg/min IV CRI (with 2 mg/kg loading dosage)
• Most used opioid in birds
• For severe injuries such as
Continued next page
September 2023 19 CLINICAL
©getty images/skynesher
Common presentations of avian emergencies
fractures, burns and beak traumas, give 4 mg/kg
• For moderate pain, such as being egg bound or traumatic events (e.g. hit by car) that has not produced fractures, give 2 mg/kg
• Monitor for sedative effects
• Buprenorphine – Suggested dosage – 0.1 to 0.6 mg/kg IM/PO q 12 hours
• Tramadol – 10–30 mg/kg IM, PO q 12 hours
• Questionable bioavailability among species
• To be used in conjunction with meloxicam.
NONSTEROIDAL ANTIINFLAMMATORY DRUGS
Used to relieve musculoskeletal and visceral pain. Effective for both acute and chronic pain.
• Carprofen – 1 to 4 mg/kg PO, SQ, or IM q 12 to 24 hours for less than 7 days
• Meloxicam – 1.0 mg/kg IM/IV q 12 OR 1.5 mg/kg PO q 12
• Only give in euhydrated patients or patients on fluid therapy
• Appropriate for soft tissue trauma
• Can be used in conjunction with butorphanol and tramadol
• Available in liquid form at 1.5 mg/ ml and 0.50 mg/ml. Injectable 5 mg/ml.
The recognition of pain, the assessment of the condition or injury and the treatment choice are important to the advancement of avian medicine. It is important that veterinary professionals understand and recognise signs of pain in their patient and address it appropriately. Through better understanding and early recognition, pain can be appropriately treated in the avian patient.

COMMON AVIAN PRESENTATIONS
Crop stasis
Crop stasis is a common issue where the crop doesn’t empty efficiently, leading to regurgitation or passive expulsion of food from the mouth, oesophagus, and crop, which can result in aspiration. Poor husbandry is a common cause of crop stasis in hand-raised chicks. Other causes include:
• poor hygiene
• incorrect formula temperature or consistency
• overfilling the crop
• antibiotic administration
• crop burn
• ingestion of foreign material
• diseases of the lower gastrointestinal tract
• heavy metal toxicity.
Before handling the bird, you may observe signs of repeated regurgitation, such as dried food on the feathers, especially on top of the head. Crop stasis is also linked to anorexia, dehydration, depression, and a distended crop that has a sour odour from bacterial or fungal overgrowth.
Diagnosis is made through physical examination, palpation of the crop, cytology and/or culture of the crop contents, radiology, and a full blood profile. Treatment may involve emptying the crop, then providing supportive care in the form of nutrition, heating, and fluid therapy. After the bird is warmed and hydrated, small amounts of diluted liquid diet can be given via tube feeding. If the crop empties well, and the bird does not regurgitate, the volume and concentration of the liquid diet can be gradually increased. If gastrointestinal obstruction has been ruled out, motility stimulants may also be administered.
Broken blood feather
When a bird’s blood feather is broken, the feather shaft functions like a straw, causing the vessels to bleed for a prolonged period due to capillary action.
A bird suffering from anaemia may exhibit signs of weakness, leading to collapse and tachypnoea or tachycardia. Blood feathers can become broken as a result of traumatic events such as falling, having too small a cage, flapping wings, or an animal attack.
If the bleeding has stopped or is minimal, place the bird in a darkened and quiet incubator to minimise stress and lower blood pressure. Observe the bird periodically. If the bleeding continues, apply digital pressure until it stops, and provide analgesia as the area is sensitive. Once the bleeding
Continued from previous page
©getty images/dardespot 20 September 2023 CLINICAL
has stopped, the feather can be allowed to grow out, but it should be trimmed to reduce the risk of further trauma or pain.
If the bird’s condition permits, the feather can be removed under general anaesthesia by grasping it at its base with a haemostat and pulling it in the direction of growth, supporting the surrounding skin and applying pressure if the follicle continues to bleed. Ensure that the pulp has been completely removed from the base of the feather, which should have a rounded and bulging appearance. In case of severe bleeding, administer warmed fluids or a blood transfusion. Monitor the haematocrit as needed and provide ongoing supportive care until the bird’s condition improves.
Leg band constrictions
Leg identification bands on birds, which are put on chicks when they are young or before they are sold, are becoming less necessary with the increasing use of microchipping. All leg rings on pet birds must be frequently examined to ensure they do not cause discomfort or problems with fit.
Leg bands may become tight as a result of the bird’s growth, self-inflicted damage from trying to remove the band, or if the leg gets caught on cage furnishings. The bird may experience sudden lameness, swelling of the affected limb and digits, or trauma to the leg from using its beak to remove the constriction.
Since birds have delicate, brittle bones, it’s crucial to remove tight leg bands under general anaesthesia. Stainless steel bands can be particularly difficult to cut, so a super fine diamond bur or a Dremel tool (or a high speed dental handpiece) is recommended. There’s a risk of toxic shock syndrome where trapped, contaminated blood in the affected limb may flood back to the heart, causing cardiac arrest. Close monitoring, analgesia, and fluid support should be provided both during and after the procedure.
Reproductive disorders – dystocia
Reproductive disorders in birds can
refer to any abnormal laying that is either obstructive or non-obstructive. The cause of the disorder can stem from various sources, including environmental stress, nutritional issues such as dehydration, hypocalcaemia, or malnutrition, egg size and shape (for example, too large or lash egg), or health problems specific to the hen (such as systemic disease or oviduct perforation).
The symptoms of reproductive disorders in birds can vary depending on the severity of the condition. Some common signs include abdominal straining, tail bobbing or wagging, drooping wings, a wide stance, depression, loss of appetite, lameness or leg paralysis (due to pressure from the egg on the nerves leading to the legs), a distended abdomen, droppings sticking to the vent area, fluffed feathers, weakness, difficulty breathing (due to pressure on the air sacs), sitting on the floor of the cage, possible prolapse of part of the reproductive tract, and in some cases, sudden death.
The treatment of reproductive disorders will depend on the overall health of the bird, the severity of symptoms, the location of the egg, and the length of time the bird has been egg bound. Before conducting any tests, it is important to stabilise the bird by providing warmth and humidity, subcutaneous fluid therapy, calcium gluconate, nutritional support, and analgesia. Further testing may include physical palpation of the egg, bird-in-a-box radiographs, and ultrasonography. Intensive medical management may include the administration of prostaglandin E2, while surgical management options may include cloacal ovocentesis or abdominal surgery, depending on the specific case.
Toxin exposure
Poisoning caused by ingestion of heavy metals such as lead, zinc, and occasionally copper, is a common type of avian toxicity that veterinarians often see in practice. Other toxic substances that can affect birds include aerosols like Teflon and
ingestible toxins such as avocado, rat bait, onion, garlic, and certain household plants.
Diagnosis of toxin exposure in birds can be challenging and often requires a combination of tests, including X-rays, repeated laboratory results, and observation of clinical signs. To get a clearer picture, it is important to:
• discuss the bird’s environment with the owner, paying special attention to the materials used in the cage, toys, and age of the cage
• conduct a physical examination, looking for symptoms such as regurgitation or vomiting, watery or bloody droppings, weakness, or seizures
• take radiographs, CBC and biochemistry, and specific tests such as measuring blood lead levels.
Signs of heavy metal poisoning in birds can include:
• weakness
• lethargy and fluffiness
• vomiting or regurgitation
• seizures
• watery green droppings
• sudden death
• a general appearance of sickness.
Treatment options for heavy metal poisoning in birds include:
• fluid therapy to protect the organs and flush out the toxins from the body
• administering a chelating agent, calcium EDTA, which traps the lead or zinc and removes it through the kidneys or intestines
• antibiotics to prevent infections during the bird’s recovery
• activated charcoal to bind the toxins
• providing crop feeds to add fluids and calories needed for recovery
• administering vitamin B complex and thiamine to prevent metal deposits in tissues and help the nerves recover
• treating seizures with anticonvulsants
• removing large foreign pieces through general anaesthesia or allowing them to pass naturally
Continued next page September 2023 21 CLINICAL
Common presentations of avian emergencies
• flushing smaller pieces that are not passing through with warm fluids during general anaesthesia
• adding bulking agents to the diet or crop feeding to hasten the removal of particles through the gastrointestinal system.
Trauma
Birds can easily sustain injuries in a typical household environment, such as by colliding with ceiling fans, suffering animal attacks, breaking bones, experiencing feather trauma, improper handling, or flying into windows.
Some general signs that a bird has experienced trauma are:
• unequal pupil size
• partially or fully closed eyes
• tilted head
• limping on one or more limbs
• visible blood or bruises
• missing feathers.
When a bird presents with trauma, it is important to stabilise it first. Further diagnosis, such as X-rays and surgery, should be performed once the bird is in a more stable condition. Simple stabilisation techniques include:
• placing the bird in a warm brooder at 28–30°C
• providing supplemental crop feeding
• administering subcutaneous or intravenous fluids, depending on the degree of blood/fluid loss
• initiating oxygen therapy if needed
• starting pain relief and antiinflammatory medications for fractures, soft tissue trauma, or open wounds
• prescribing antibiotics if there is a risk of infection (e.g. open fracture or wound)
• applying a bandage, such as a figure 8 or modified Y body bandage, to stabilise fractures while avoiding over-tightening that could cause ligament damage or breathing difficulties
• applying pressure and addressing bleeding, administering fluids or blood products after evaluating the PCV/TP.
Dyspnoea
Respiratory problems in birds can occur due to various reasons such as trauma that affects the airways, fractures in the pneumatic bones, blockages, accumulation of fluid in the abdominal air sacs (e.g. egg laying), or respiratory diseases. Until a proper diagnosis is made, it is important to practise caution and wear protective equipment to reduce the risk of infection.
Signs of respiratory distress include open-mouthed breathing, excessive chest movement, and tail swaying. Treatment options vary depending on the cause of the respiratory issue. Ideally, the treatment is based on the results of diagnostic tests, but in some cases, it may need to be based on the bird’s appearance and history.
General therapy may include:
• subcutaneous or IV fluid therapy
• providing nutritional support
• supplementing with vitamin A as needed.
Treatment for upper respiratory tract issues may involve:
• clearing nasal congestion through flushing and collecting samples for laboratory tests and analysis
• in severe cases of sinusitis, surgical curettage.
Treatment for tracheitis may include:
• placement of an air sac cannula in the thoracic or abdominal air sac to relieve tracheal or syringeal blockages and to maintain anaesthesia during treatment
• nebulisation therapy, which involves delivering a mist of medication to the respiratory tract. Nebulisers should produce particles ranging from 3 to 10 µm in diameter, and patients should be nebulised for 15 to 30 minutes, 2 to 4 times daily, within a small enclosure. Saline can be used to soothe irritated respiratory tissue, or antibiotics can be delivered to the lower respiratory tract. However, it is important to monitor the patient carefully as excessive nebulisation may overhydrate the airways.
Emergency care is a combination of many factors, both medical and environmental, so it is wise to have a systematic approach to addressing these cases to ensure that the patient will have the most success with your treatments.
Neonate concerns
Paediatric diseases are common and often related to issues with husbandry and nutrition. The health of a chick depends on many factors, such as the health of the parents, genetics, the incubation process, nutrition (type of food, temperature, and consistency), environment (humidity, warmth, and cleanliness), and exposure to infectious diseases. When an ill neonate presents, the history of not only the chick but also of its parents, the aviary, and the nursery are important.
Common paediatric presentations
Paediatric illnesses in birds are commonly related to problems with care and nutrition. A chick’s wellbeing is impacted by various factors, including the health of the parents, genetics, incubation process, nutrition (such as food type, temperature, and consistency), environment (such as humidity, warmth, and cleanliness), and exposure to infections. When examining a sick neonate, it’s crucial to consider the history of not only the chick but also its parents, the birdhouse, and the nursery.
Common paediatric conditions:
• Aspiration pneumonia is a prevalent cause of respiratory diseases in hand-fed psittacine birds. Chicks can inhale formula if they are fed too much liquid or if the feeder uses improper
Continued from previous page
22 September 2023 CLINICAL
techniques, especially if the feeder is inexperienced. Aspiration often occurs as birds begin to transition from formula to solid food. Clinical signs include increased breathing, breathing difficulties, poor feeding response, and depression. A CBC and radiographs may assist in the diagnosis, but the diagnosis is usually based on the history and physical examination results. Treatment involves oxygen therapy, nebulisation, antibiotics, antifungals, warmth, additional fluids, and antiinflammatory drugs. The outlook is guarded.
• Bacterial diseases and yeast infections are common in neonate patients. In healthy chicks, the gut contains mostly gram-positive bacteria. High levels of gramnegative bacteria or yeast indicate an infection. Candida albicans is present in low amounts in a healthy chick but can grow in the presence of antibiotics, malnutrition, stress, or immunosuppression. Bacterial infections can stem from unsanitary conditions, improper storage of formula, and the use of unclean feeding utensils. Clinical signs can include a stopped-up crop, poor feeding response, regurgitation, depression, and dehydration. The diagnosis is based on clinical signs and results from a faecal or crop gram stain or cytology, CBC, and culture and sensitivity testing. Intestinal or gastric candidiasis can result in poor nutrient absorption, leading to reduced weight gain. Treatment involves antibiotics based on culture and sensitivity results, if available, and supportive care. Neonates on antibiotics are at risk of developing secondary yeast infections, so prophylactic treatment with antifungal drugs such as nystatin or fluconazole may be necessary.
• Foreign body ingestion is common in young birds and can involve items such as substrate, toys, or feeding tubes. The diagnosis is based on clinical signs, history, and results from radiographs or CT scans. Treatment may require
an ingluviotomy to access the mucosal surface and lumen of the crop, proventriculus, or ventriculus. For larger or older birds, a rigid endoscope may be necessary to visualise and remove the foreign body from the upper GI tract. The endoscope may be used orally or through an incision in the ingluviotomy, depending on the location of the foreign body. If endoscopic retrieval is not possible, surgery may be necessary.
• Crop burns occur from feeding the chick formula that is too hot. This can happen if a microwave is used to heat the formula (not recommended because it can create hot spots in the formula). Mild cases may cause red and inflamed skin in the crop. Secondand third-degree burns will be severely inflamed and blistered and may lead to tissue death and fistula formation. In subacute cases, birds may present with food draining from a fistula through the crop wall and skin. The diagnosis is based on the history, clinical signs, and physical examination results. The treatment for burns in birds involves administering antibiotics, providing fluid supplements, using anti-inflammatory medications, and offering nutritional support. Surgery is usually necessary for repairing the burn but should be delayed until the affected area is clearly defined. This procedure includes removing dead tissue, separating the wall of the crop from the skin above it, and closing each layer separately. The outlook is favourable if the crop wall is still strong enough to be closed and the oesophagus has not been damaged.
• Injury to the oesophagus and pharynx can occur when improper hand-feeding techniques are used, such as with a syringe or a rigid feeding tube. This can result in tissue damage, inflammation, and food becoming trapped in the subcutaneous tissues. Birds may exhibit signs of depression, loss of appetite, coldness, dehydration, and poor feeding. Swelling may
be noticeable in the neck area. The diagnosis is made through a review of the hand-feeding history and a physical or endoscopic examination to locate the puncture site. Treatment involves opening the pockets surgically, flushing the wounds, administering antibiotics, pain relief medications, antiinflammatory drugs, and providing supportive care. The outcome depends on the severity of the injury, amount of food deposited, and how quickly the injury is detected and treated. In cases of severe trauma, the prognosis is uncertain and can be poor.
CONCLUSION
The basic principles of emergency medicine and critical care are also the same for all species; however, critically ill avian pets pose special challenges due to their unique anatomy, physiology, and behaviour. Emergency care is a combination of many factors, both medical and environmental, so it is wise to have a systematic approach to addressing these cases to ensure that the patient will have the most success with your treatments. So, what we now know is that it is extremely important with emergencies to be prepped and ready for anything that could present. This could mean the difference between life and death and controls the urgencies of the workday. It is important that we acknowledge and recognise the signs of shock, can treat them along with other conditions that may present with the same patient at the same time (dehydration, haemorrhage, neurological dysfunction, etc.). We can provide our patients with intensive care in the form of fluids aiming to increase blood pressure, oxygen, antimicrobials, and analgesics/anti-inflammatory drugs aiming to prevent or treat pain and reduce inflammation. Additional treatments should always be kept in mind (supplemental feeding, behavioural, etc.) to allow our patients to make a full recovery.
September 2023 23 CLINICAL
Warmblood with cervical vertebral myelopathy (Wobbler syndrome)
by Clare Wheatley
Dip
HBM,
Dip VN (Surgical), Cert IV VN, Cert III EN, RVN, AVN
PATIENT DETAILS:
Species: Equine
Breed: Warmblood
Age: 2 yo
Sex: Gelding
Weight: 563 kg
PRESENTATION
The horse was presented to our hospital on 24 January 2020. The owner reported that the horse was normal before going to the breakers for 5 weeks to begin its education. When arriving home, the horse was immediately noted to have a hind limb problem (when circling), with a swollen left hind leg. Since this time, intermittent abnormalities were suspected by the owner. The owner noted that the horse had lost weight since being at the breakers.
INITIAL DIAGNOSTICS
Neurological examination
A neurological examination can be divided into four sections2:
1. Evaluation of mental status (observing the horse from a distance e.g. in a stable or yard)
2. Cranial nerve examination
3. Spinal reflexes and muscle evaluation (performed standing)
4. Gait and postural examination (performed moving).
This examination assists with neurolocalisation. As an example, intracranial disease will often result in abnormalities in the first two parts of the examination, whereas spinal cord defects will usually have abnormalities noted in the last two stages of the exam.
Evaluation of gait is important for distinguishing musculoskeletal diseases from neurological diseases.1 A horse with a musculoskeletal
disease should be fairly consistent in its mistakes, whereas a horse with a neurological condition will be fairly irregular in its mistakes.1
This neurological examination involved:
1. observing the horse’s natural gait (at walk and trot) in a straight line and on the lunge (in a circle)
2. observing the horse’s gait (at walk) when its head was elevated
3. observing the horse turning in very small circles (at walk) in both directions
4. observing the horse backing up
5. observing the horse’s ability to correct itself while walking and its tail was pulled
6. observing the horse’s response to its legs being placed in unnatural positions (too wide, too narrow, crossed in front of the other, too far forward, too far backwards from normal resting positions).
Note: The use of a blindfold and negotiating obstacles was omitted from this exam due to safety concerns. The level of ataxia present in the basic tests made it unsafe for the handler and horse to perform tests with a higher degree of difficulty

Proprioception
Proprioception is the awareness the horse has of its body and movements, including where they place their limbs and feet.3 Proprioception provides stability to maintain balance and stay upright, perform fine movements and make precise and sudden changes if the situation changes.4

24 September 2023 CASE REPORT
An example of a horse walking with its head elevated Above: An example of the ‘tail pull’
due to the increased risk of the horse falling. This horse was displaying both incoordination (ataxia) and weakness.
Clinical findings from neurological examination
This horse was a tall, long-necked horse. Pertinent clinical findings at rest:
• There was no obvious neck swelling or pain as might be expected with recent trauma.
• The left hindlimb was diffusely swollen, presumably self-trauma as a result of abnormal proprioception.
• The hindlimb toes were scuffed where the horse has been toe dragging (right hind worse than left hind).
• The horse showed obvious proprioceptive deficits at rest with an inability to correct limb positioning when limbs were manipulated into an ‘abnormal’ stance, and a tendency to stand with limbs unusually positioned.
Pertinent clinical findings when gait was assessed:
• The horse had obvious hypermetria evidenced by a long, ‘loose’ gait.
• The horse would stumble intermittently (a sign of weakness).
• During circling, the outer hindlimb showed excessive circumduction (i.e. moved the leg excessively in a circular motion) – a classic sign of ataxia.
Ataxia
Ataxia refers to incoordination. It may affect some or all the horse’s limbs. Spinal ataxia occurs when there is a lack of information coming up the horse’s spinal cord to tell its brain where its body parts are in space and the state of muscle contraction at any given time.5 It is not painful for the horse and they have no sense of the position or movement of the affected areas.5
The Mayhew Ataxia Grading Scale
0 Normal
1 Very subtle gait abnormalities that may be slightly more distinguishable when head is elevated
2 Deficits are moderate abnormalities that can be noted at the walk by most observers
3 Deficits are easily recognisable and are much worse when the animal is negotiating obstacles or when its head is elevated
4 Horse will fall or nearly fall when negotiating normal gaits and activities
5 Horse is recumbent
• Any manipulation performed (e.g. circling and backing) suggested that the horse could easily fall. When all components of the examination were collectively assessed, the horse was displaying grade 4 ataxia (according to the Mayhew Ataxia Grading Scale) of hindlimbs and grade 2 ataxia in the forelimbs.
RADIOGRAPHY
Following the neurological exam, in consultation with the owner, it was decided to take standing radiographs of the horse’s neck to see if a definitive diagnosis could be made. Initial standing radiographs were taken to look for a traumatic injury or fracture
(another differential cause of ataxia), as well as looking for any changes that may be consistent with cervical vertebral myelopathy (CVM).
In order to keep the horse still during the radiography process, it was lightly sedated with 200 mg xylazine and 5 mg butorphanol intravenously. Special care must be taken when sedating an ataxic horse; the sedatives are likely to increase the horse’s ataxia and proprioception deficits. Should the horse move or stumble, it will have a reduced ability to correct itself. For this reason, radiographs were taken in an open area of the room at a safe distance from walls and equipment.

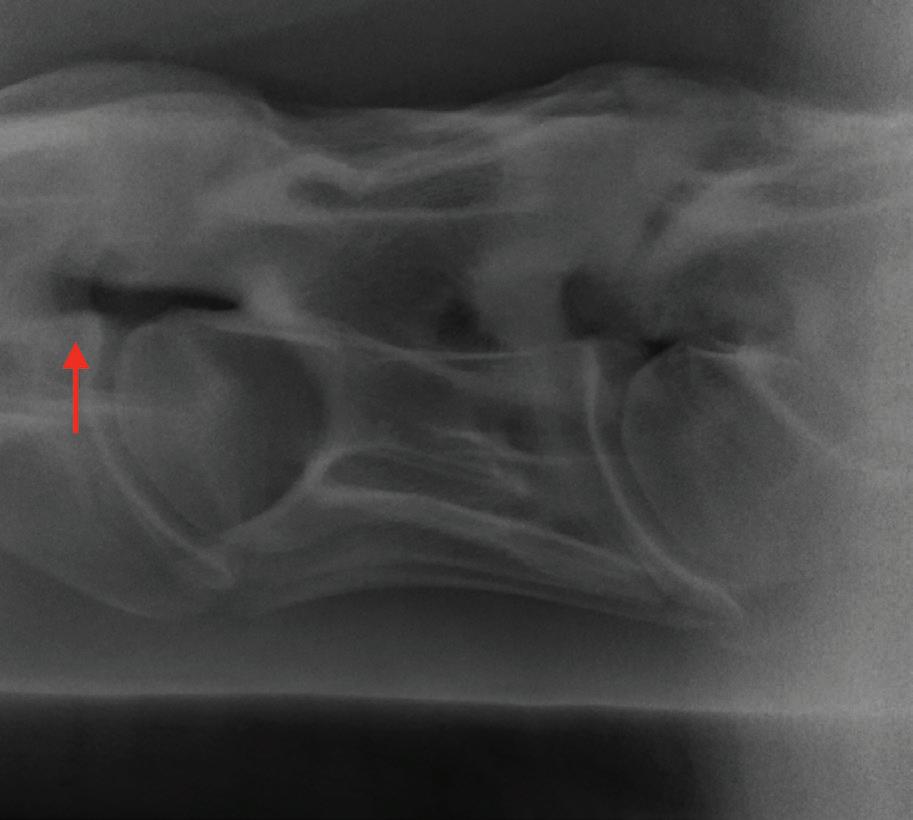
September 2023 25 CASE REPORT
Continued next page
Radiograph showing epiphyseal flaring
Tape markers indicating vertebrae to assist with radiographic plate and generator positioning
AVN and AVNAT Continuing Professional Development
Warmblood with cervical vertebral myelopathy (Wobbler syndrome)
Continued from previous page
Tape was used to identify the position of each vertebra. This assisted the radiographer and plate holder to line up with each other, as due to the height of the horse, one was unable to see the other. The person holding the horse assisted with directions to line them up. It was important that the horse holder did not stand directly in front of the horse, that all the cables from the generator and plate were kept well away from the horse’s legs, that the plate holder was not directly in the beam of the X-ray, and that the horse holder notified the team if the horse was about to move.
Plain radiographs of the cervical vertebrae showed no evidence of fractures. Lateral-lateral radiographs showed there was some slight (subjective but potentially significant) malalignment of C2–C3 and caudal
What is a myelogram?
A myelogram is a radiographical study of the cervical spinal cord using contrast medium to detect pathology. In the case of Wobbler syndrome, it is used to detect the site of spinal cord compression.
epiphyseal flaring (or ‘ski jump formation’) of C2 (and to a lesser degree C3), and epiphyseal flaring on C5–C6. Although these signs were suggestive on plain radiographs, it was not conclusive, therefore a myelogram was indicated.
PROVISIONAL DIAGNOSIS
The most likely provisional diagnosis was cervical vertebral myelopathy (Wobbler syndrome), followed by trauma, then viral encephalitis (the most common in horses in our geographical area are Japanese encephalitis, Kunjin virus and Murray Valley encephalitis). In the years since this case study, flavivirus, predominantly Japanese encephalitis, has become endemic to our area due to the wet conditions we have experienced. However, at the time this horse was presented to the hospital, it was very rare. With the prevalence of the flavivirus we now see, in cases of ataxia, we take blood samples (serum samples in plain tubes and plasma samples in EDTA tubes) at the initial consultation to look for prior and recent exposure to flavivirus. A followup second sample would be taken 2–4 weeks later.
CVM carries a poor prognosis. Surgical fusion of the affected vertebrae can be performed; however, it is seldom performed in Australia due to the potential low level of improvement following surgery. Surgical fusion will typically result in an improvement of one or two grades on the ataxia scale. Many of the horses diagnosed with CVM are intended to be performance animals and a horse that is a grade three or four will not improve enough to safely fulfil this ambition.
THE PLAN
The owner elected to have a myelogram performed under general anaesthesia. Should the diagnosis of CVM be confirmed, the horse would be euthanised while under general anaesthesia. The owner signed consent forms for both anaesthesia and euthanasia once the risks had been explained to her.


PREPARATIONS FOR PROCEDURE UNDER GENERAL ANAESTHESIA Preparing the theatre
Before the horse is anaesthetised, it was important to ensure that the surgical theatre was adequately prepared. The table was positioned for lateral recumbency. Clippers, vacuum cleaner, surgical scrub and gloves were checked and ready for use. The portable X-ray unit was brought into theatre, and the X-ray plate covered with a plastic bag (durable garbage bags are ideal for this) to prevent contrast material from contacting the plate. Enough lead gowns, thyroid collars and lead gloves were brought to theatre for each person required for the procedure.
Contrast radiography is performed using sterile injectable iohexol (Omnipaque®). This was administered through an 18 Ga x 3” spinal needle. Omnipaque® is light sensitive and was only to be drawn up in an aseptic
26 September 2023 CASE REPORT
Above: An example of the clip patch over the atlanto-occipital (AO) articulation
manner by the surgeon once it was time to administer. Until then; it was kept within its packaging.
Sterile gloves for the surgeon, along with 50 ml syringes and 18 Ga needles for drawing up, were also prepared.
Preparing the patient
A 14 Ga x 3.25-inch Angiocath® with injection port was placed in the horse’s left jugular vein. The patient was weighed (563 kg) and his induction drugs were calculated. Analgesia was administered via the catheter prior to surgery.

Induction
The horse’s mouth was washed out to ensure no food was passed into his trachea with the endotracheal tube and he was walked to the induction room. Given the horse’s ataxia and age (he was young and fractious), it was important that the induction process was completed quietly, carefully and as stress free as possible. All movements were made quietly and slowly.
The horse was sedated with xylaxine via the intravenous catheter. Once he reached an adequate depth
of sedation, he was induced with diazepam and ketamine via the intravenous catheter. In a normal induction, the horse’s head is elevated to assist their weight to move backwards as they are induced. Minimal head elevation was performed during this induction as elevation of the head and neck increases this horse’s instability due to his ataxia. His induction was performed smoothly and he was intubated with a size 26 mm endotracheal tube. A slightly smaller tube than normal was selected as there are reported instances of tracheal mucosal damage when the head is repeatedly flexed and extended during the procedure.
Patient preparations under general anaesthesia
The horse was placed in right lateral recumbency on the table, connected to the breathing hoses and maintained on isoflurane with mechanical ventilation. Cushions and pads were placed to support the weight of the horse’s legs and reduce the risk of myopathy. All personnel put on appropriate radiography PPE. Initial radiographs were taken to check marker positioning.
The horse was clipped over the atlanto-occipital (AO) articulation; clipped from the poll (between the ears) extending approximately 15 cm caudally. The area was given an aseptic preparation using chlorhexidine gluconate for a timed five minutes, followed by a final preparation of isopropyl alcohol.
As the aseptic preparation was occurring, the lead surgeon had aseptically prepared the equipment they will need with the help of an assistant.
FURTHER DIAGNOSTICS –CONTRAST RADIOGRAPHY UNDER GENERAL ANAESTHESIA
When the patient preparation was complete, an 18 Ga x 3-inch spinal needle was inserted into the atlanto-occipital articulation. Fifty ml of cerebrospinal fluid was slowly
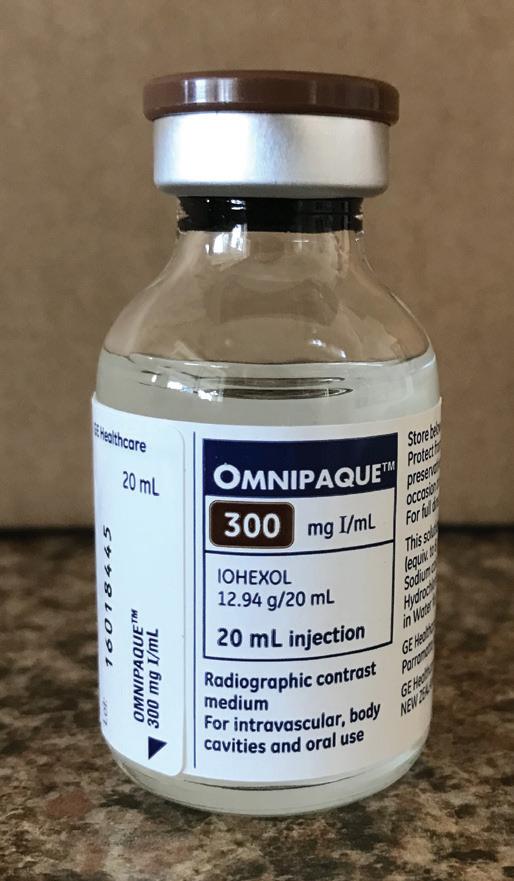
September 2023 27 CASE REPORT Premedication drugs (Patient weight 563 kg) Drug Dose Mg required Mls given Route Phenylbutazone 4.4 mg/kg 2477.2 mg 13 ml IV Induction drugs Xylazine 1.1 mg/kg 619.3 mg 6 ml IV Acepromazine 0.03 mg/kg 16.89 mg 1.7 ml IV Ketamine 2.5 mg/kg 1407.5 mg 14 ml IV Diazepam 0.1 mg/kg 56.3 mg 11 ml IV
A spinal needle is inserted into the atlanto-occipital articulation Continued next page
Warmblood with cervical vertebral myelopathy (Wobbler syndrome)
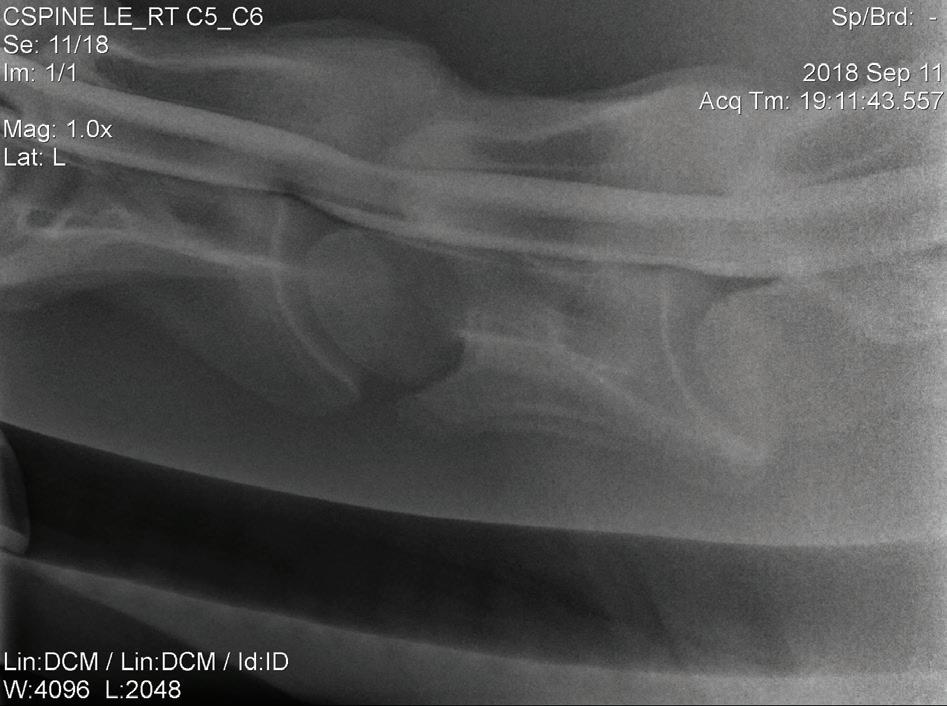
Continued from previous page
removed and 60 ml of Omnipaque® was injected. A halter was left on the horse to make it easier to elevate the horse’s head to allow the contrast material to migrate caudally. A series of neutral and flexed radiographs the length of the neck was taken. Flexed radiographs were achieved by pushing the horse’s nose towards its chest, taking care to ensure the endotracheal tube remains connected to the breathing hoses. Due to the length of a horse’s neck, multiple images were taken, moving approximately 20 cm at a time.

Intraoperative contrast radiography confirmed the provisional diagnosis of cervical vertebral myopathy (Wobbler syndrome).
OUTCOME
The horse was humanely euthanised on the table while under general anaesthesia using 150 ml pentobarbitone. Recovering horses from general anaesthesia is a high risk procedure, even for the ‘normal’ horse. This risk is amplified significantly in horses with any degree of ataxia. Their risk of limb fracture or being unable to stand is so much higher that the owner of this horse elected preoperatively to euthanise if a concrete diagnosis of CVM was made intraoperatively, so that it did not have to undergo the recovery procedure.


SUMMARY
This case was a good opportunity for me to further my skills and understanding of a neurological condition that affects a small percentage of horses but appears to be more prevalent with thoroughbreds and warmbloods. Although I often do it instinctively, writing it down made me think through the safety considerations of handling a large, ataxic horse.
References
1. Hudson NPH & Mayhew IG. Radiographic and myelographic assessment of the equine cervical vertebral column and spinal cord. Equine Veterinary Education. 2005;17(1):34–38.
2. Johnson AL. ‘How to perform a compete neurologic examination in the field and identify abnormalities’. AAEP Proceedings. 2010;56(1):331–337.
3. EquiMed®. Pro-prio-what …? https://equimed.com/news/business/pro-prio-what-why-it-isimportant-for-horse-owners-to-know-about-proprioception/. 2019.
4. Busuttil E. Proprioception – How do our horses know how to put one foot in front of the other, The Equine Documentalist, https:// www.theequinedocumentalist.com/post/proprioception-howdo-our-hoses-know-how-to-put-one-foot-in-front-of-theother#:~:text=Proprioception%20gives%20our%20horses%20 the,changes%20if%20the%20situation%20changes/. 2022.
5. Oaks A. Ataxia explained: why a horse might become weak, wobbly or unable to stand, Horse and Hound https://www.horseandhound.co.uk/plus/vet-clinic/ataxia-explainedwhy-a-horse-might-become-weak-wobbly-or-unable-to-stand-hhplus-742892/. 2021.
28 September 2023 CASE REPORT
One of the findings we see in a myelogram is obliteration or near obliteration of the ventral dye column
Myelogram showing a 50% reduction in dye column
Postmortem pictures highlighting the spinal cord compression that occurs in cervical vertebral myelopathy (Wobbler syndrome)
Want to focus on your Nursing Career



ACM40418

Certificate IV in Veterinary Nursing


This nationally recognised qualification is for students who wish to develop proficiency in providing expert veterinary nursing care for animals and professional support for their owners. You will develop personal and professional skills that are recognised and in demand by employers. ACM40418




Certificate IV in Veterinary Nursing is not only a nationally recognised qualification but also globally recognised.








RTO National Provider No.: 31424 Email aircenquiries@provet.com.au
(07) 3621
to find out more? Contact us today! Website www.provetlearning.com.au Facebook www.facebook.com/ProvetAIRC Course Duration 2 years Study Method Online, self-paced Investment $7,250 Payment plans available Support Phone, email, live-chat Course Intake Start at any time! QUICK FACTS:
Phone
6005 Want
Anaesthetic monitoring
Collaborative article from the trainers at AIRC
The main purpose of monitoring anaesthesia is to warn of any changes in the anaesthetic depth or patient condition in enough time to intervene before it becomes too dangerous for the patient. We aim for a balance between sufficient central nervous system (CNS) depression, analgesia, muscle relaxation and immobilisation for the procedure to be performed without dangerously compromising cardiopulmonary function. So monitoring is aimed at keeping the patient safe while regulating anaesthetic depth.
To keep the patient safe, we need to monitor that the patient’s vital signs remain within acceptable limits while ensuring they are at an adequate depth of anaesthesia to not perceive pain or arouse or reach an excessive depth that could lead to an anaesthetic overdose.
The parameters that we monitor are divided into three classifications: vital signs, reflexes and other indicators. These parameters help to determine patient safety as well as anaesthetic depth. Vital signs give a good indication as to how well the patient is maintaining basic circulatory and respiratory function during anaesthesia, while reflexes and other indicators give a good indication of the patient’s depth of anaesthesia (anaesthetic stage and plane).
Never over interpret one piece of information. The aim of anaesthetic monitoring is to obtain data from a number of different body systems that will allow an overall picture of the patient. The most important monitor is you and your senses – sight, hearing, touch, etc.
MONITORING OF CNS REFLEXES
Basic reflexes and muscle tone are the method of monitoring whether the brain still functions. Under anaesthesia most of the CNS undergoes a selective, dose dependent reversible depression caused by the anaesthetic drugs at their site of action. Basic reflexes are:
• spontaneous motor activity
• jaw tone
• palpebral reflex
• corneal reflex
• lacrimation
• pupil position
• respiratory effort (intercostal/ diaphragmatic).
MONITORING THE CARDIOVASCULAR SYSTEM
The aim of the cardiovascular system is the maintenance of adequate tissue perfusion with oxygenated blood. The aim of intraoperative monitoring of the cardiovascular system is to ensure that it is achieving this and intervene if it is not.
• Mucous membrane colour
• Capillary refill time
• Heart rate and rhythm
General indicators:
– increased heart rate –tachycardiac – decreasing depth of anaesthesia – becoming lighter
– decreased heart rate –bradycardia – increasing depth of anaesthesia – becoming too deep
• Blood pressure.
MONITORING OF THE RESPIRATORY SYSTEM
It is not just good enough to have blood being delivered at an adequate rate and pressure to the body. There must be oxygen in that blood for any good to be done.
• Pulse oximetry
• Respiratory rate, rhythm and nature of breathing effort
Changes in the respiratory rate and effort may indicate a change in areas such as anaesthetic depth.
– Increased respiratory rate –becoming lighter
Decreased respiratory rate –becoming deeper
– Increased or ‘jerky’ respiration may indicate that the patient is feeling pain stimuli
It is also important to monitor both the rebreathing bag and the patient’s thorax to detect:
anaesthetic circuit disconnection
inconsistency between breathing excursions of the chest and the amount of air moving in and out of the bag
airway obstruction problems (kinked endotracheal tube).
Early detection of adverse events and evaluation of corrective intervention is the aim of the game. Various pieces of equipment are of use, but reliance should not be placed on just one item.
30 September 2023 CLINICAL
–
–
–
–
Vitals Heart Rate & Rythm Respiratory Rate & Depth CRT & MM colour Pulse strength, BP & Temp Other Spontaneous Movement, Muscle Tone Eye Position, Pupil Size, Nystagmus Salivary & Lacrimal Secretions Response to Surgical Stimuli Reflexes Palpebral, Comeal, Pedal, Swallowing & Laryngeal Pupillary Light Reflex
AVN and AVNAT Continuing Professional Development
The parameters that we monitor are divided into three classifications: Vital Signs, Reflexes and Other Indicators.
STAGES OF ANAESTHESIA
Four stages and planes of anaesthesia have been classified. The use of intravenous anaesthetic agents plunges the animal through the initial stages so rapidly that they may not be recognised.

To achieve surgical anaesthesia, we must maintain the animal at Stage 3 between Planes 2 and 3. The deeper Plane 3 will be needed for painful procedures that require good muscle relaxation – e.g. orthopaedic and ophthalmic operations. If the patient is being maintained at Stage 3, Plane 3, careful monitoring and I/V fluid support if the procedure is prolonged will be required.
Summary of central nervous monitoring
Jaw tone
Palpebral reflex
Absent following induction – by Stage 3
Absent by Stage 3 Plane 2 – 3 in dog and cat
Slowed in horse at Stage 3 Plane 3
Corneal reflex Very dulled, almost absent by Stage 3 Plane 3
Pedal reflex
Lacrimation
Absent by Stage 3 Plane 2
Absent by Stage 3 Plane 3
Eye position Stage 3 Plane 1 – located in medial canthus with 3rd eyelid partially protruding
Stage 3 Plane 3 – ventral medial direction
Stage 3 Plane 4 – central and fixed, eye dry and dull
Pupil position Stage 3 Plane 1 – pupils constricted
Stage 3 Plane 3 – pupil midpoint
Stage 3 Plane 4 – pupils dilated
*Remember certain drugs affect pupil size.
Laryngeal reflex
Absent in the dog by Stage 3 Plane 2 (can intubate dog at Stage 3 Plane 1)
Reduced (but not absent) in cat at Stage 3 Plane 2
Absent in cat at Stage 3 Plane 3
Respiration Stage 3 Plane 1 – regular with full use of muscles & diaphragm
Stage 3 Plane 2 – slight decrease in tidal volume & slight increase in respiratory rate
Stage 3 Plane 3 – intercostal muscles weaken and lag behind diaphragm contraction; creates unevenness & a ‘rocking’ boat type respiratory movement
Stage 3 Plane 4 – only diaphragmatic breathing
Stage 4 – apnoea
September 2023 31 CLINICAL
©getty images/Alexandr Lebedko
Anaesthetic monitoring
Continued from previous page
Awareness is a problem in approximately 2% of human anaesthetics primarily because human patients are paralysed. Seven of the nine reflexes used to assess anaesthetic depth require skeletal muscle activity, which is impossible in a paralysed patient. In veterinary surgery, awareness is highly unlikely as the depth of gaseous anaesthesia required to produce adequate muscle relaxation is usually more than is required to cause loss of consciousness in the spontaneously breathing patient.
REMEMBER THESE KEY POINTS:
• Monitor the patient, not the equipment.
• Check the patient before checking the equipment.
• A machine should not replace a skilled anaesthetist.
A machine is primarily directed at the body systems that are essential for the maintenance of life – the CNS and the cardiovascular system. Thus, we need to monitor the following:
• CNS – reflexes, depth of anaesthesia
• cardiovascular system – heart rate, perfusion
• pulmonary system & airway
• oxygenation
• temperature – this is difficult to maintain, and subnormal temperatures will slow metabolic rate and lengthen recovery and post anaesthetic complications.
RECORD KEEPING
Once anaesthetised a patient’s critical parameters must be continually assessed by the anaesthetist, which in most cases is the responsibility of the veterinary nurse. Recording in a graph form allows early identification of trends and variations in the patient’s anaesthetic depth. While recording typically occurs every 5 minutes, assessment is occurring continually as a lot can change in 5 minutes!
STAGES OF ANAESTHESIA
Stage 1 Still conscious but disorientated, amnesia, unaltered threshold to pain, but some pain is tolerated
Stage 2
Unconsciousness, excitement, delirium & uninhibited action
Suppression of higher control centres; struggling, crying, exaggerated response to pain/stimuli
Irregular respiration
Stage 3
Progressive depression of respiration, circulation, protective reflexes, muscle tone
Divided into 4 planes
Plane 1
Respiration: regular, full use of intercostal muscles & diaphragm
Pupils: constricted, slow nystagmus may be present
Eye: located in medial canthus; 3rd eyelid partially protruding Salivation and lacrimation and pharyngeal and laryngeal reflexes persist. Can intubate a horse or dog but not a cat
Muscle tone still present
Painful stimuli cause limb retraction and elevation in HR, RR and blood pressure.
Plane 2
Respiration: slight decrease in tidal volume (intercostals not working as well) and increase in respiratory rate
Eye: eccentrically fixed with halothane, centrally fixed with ether and methoxyflurane, centrally fixed with halothane in the horse
Lateral nystagmus still present in the horse
Surgical stimulation produces HR, BP and RR
Oropharynx reflexes abolished in dog but not completely in the cat
Deep tracheal reflexes persist
Muscle tone lessens.
Plane 3
Deep surgical anaesthesia
Respiration: the intercostal muscles weaken and lag behind the diaphragm contraction. This unevenness creates a rocking boat type respiratory movement
Abdominal muscles are relaxed
Eye: eyeball is slightly downwardly rotated in a ventromedial direction
Palpebral reflex: absent in dog and cat but only slowed in the horse
Corneal reflex: absent in dog and cat but present in the horse
Lacrimation, salivation, oropharynx and laryngeal relaxes; all abolished but deep visceral pain and vagal responses remain Muscle relaxation is good.
Plane 4
Too deep
Respiration: only diaphragmatic breathing; tidal volume is reduced
The inspiratory diaphragmatic contraction may produce a tracheal tug which is an exaggerated movement of the trachea and larynx and even the mandible, all of which can be incorrectly (and dangerously) interpreted as lightening of depth of anaesthesia
Eye: cornea is dry and dull; pupils are dilated
Corneal reflex vanishes in the horse
Heart rate and blood pressure fall.
Plane 4 is a dangerous and unnecessary depth of anaesthesia.
Stage 4
The period between respiratory arrest and cardiovascular collapse and arrest. The length of this period depends on the anaesthetic used, degree of oxygenation at the beginning of respiratory arrest and the species i.e. this time is zero for birds!
32 September 2023 CLINICAL
SUMMARY TABLE OF ANAESTHETIC COMPLICATIONS
Symptom Possible causes
Bradycardia Excessive anaesthetic depth
Drugs: opioid, xylazine, gas anaesthetics
Hyperkalaemia
Vagal reflex (intubation, oculocardiac reflex)
Visceral manipulation
Hypothermia
Terminal stages or hypoxia
Exogenous and endogenous toxaemias
Tachycardia Drugs: ketamine, thiobarbiturates
Anticholinergics, sympathomimetics
Hypokalaemia
Hyperthermia
Inadequate anaesthetic depth
Hypercapnia, hypoxemia
Anaemia, hypovolaemia
Hyperthyroidism, pheochromocytoma
Anaphylaxis
Atrial and ventricular premature contractions
Light anaesthesia
Deep anaesthesia
Hypoxia, hypercapnia
Hypovolaemia
Exogenous catecholamine therapy
Digitalis toxicity
Hypokalaemia
Hyperkalaemia
Hypercalcaemia
Certain anaesthetics (xylazine, halothane, thiobarbiturates)
Endocarditis or myocarditis
Severe hypothermia
End-stage visceral organ failure
Intracranial disorders
Hypotension Hypovolaemia (i.e. blood loss)
Sepsis
Shock Drugs (thiobarbiturates, inhalants)
Tachypnoea Pain
Hypoxia
Hypercapnia
Hyperthermia
Acidosis
Drugs (i.e. doxapram)
Airway obstruction
Apnoea Hypothermia
Hyperventilation with 100% O2
Drug effects (thiobarbiturates, ketamine)
Deep anaesthesia
Aminoglycoside administration
Actions to correct
Correct underlying cause if possible
Administer anticholinergic agent
Administer sympathomimetic agent
Correct underlying cause if possible
Correct underlying cause if possible
Evaluate anaesthetic depth
Check anaesthetic machine and oxygen flow Assist ventilation
If arrhythmia persists and meets one or more of the following criteria:
• > 20 per minute
• increasing in frequency
• multifocal
• occurring in runs
• causing significant effect on pulse
Treat arrhythmia as follows:
• turn off anaesthetic gas
• increase fluid administration rate
• administer lignocaine IV (maximum: 4 doses)
Increase fluid administration rate
Decrease anaesthetic concentration
Administer sympathomimetic agents
Correct underlying cause if possible
Treat pain
Correct underlying cause if possible
Assist ventilation until spontaneous ventilation returns
September 2023 33 CLINICAL
How to tell if your pet is in pain
The VNCA and VetCheck have supplied this information to assist vet nurses to educate, brief and assist their clients to care for and manage their pets.
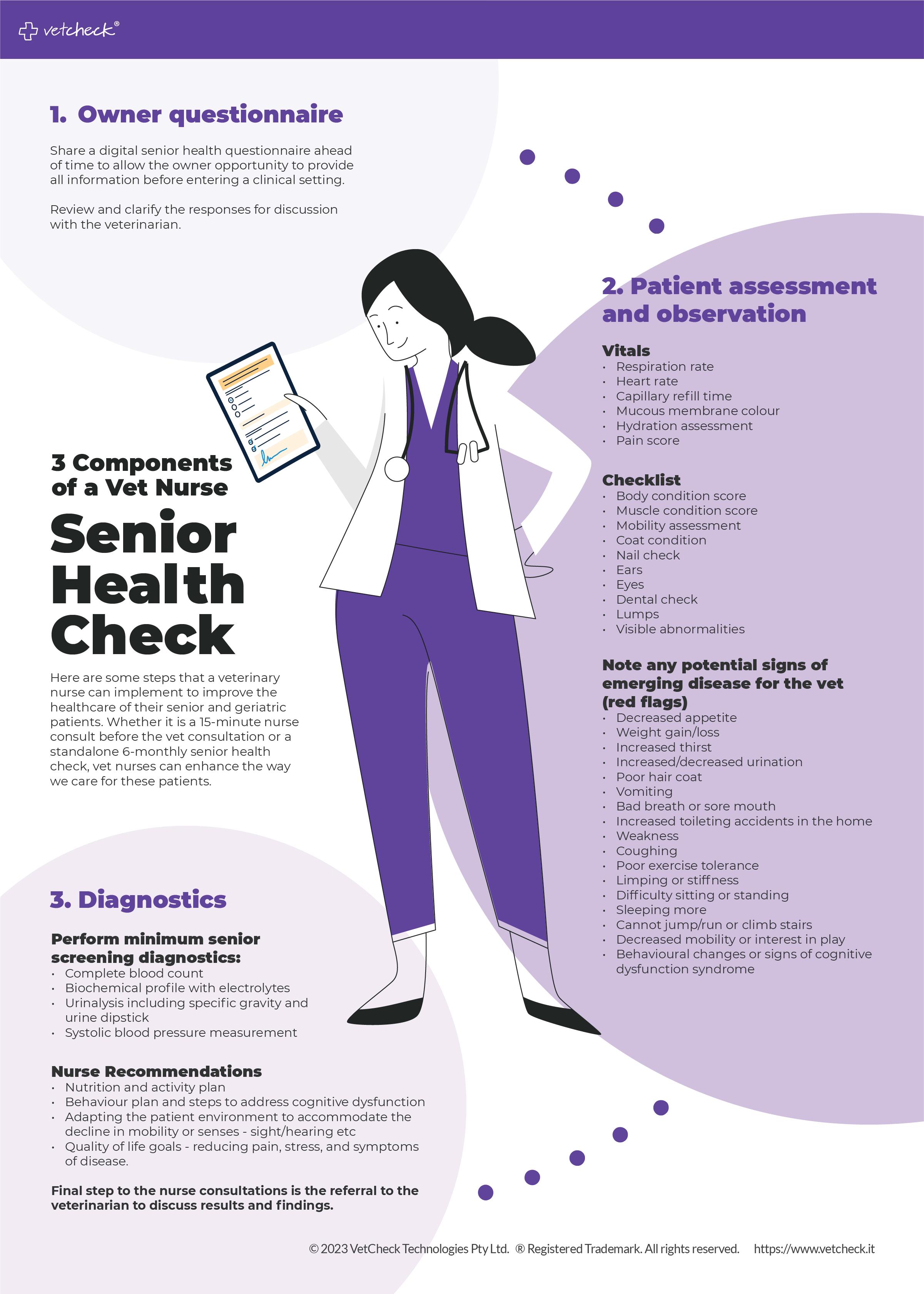
You are in the best position to identify early behavioural changes that may be associated with pain.
OVERVIEW
Pets show pain in many different ways. Change in behaviour or activity is certainly an early sign of a problem and should not be ignored.
COMMON SIGNS OF PAIN:
Howling
Growling
Vocalisation
Grunting
Whimpering
Yelping
Decreased interest in social interaction
Decreased appetite
MANAGEMENT
Depending on the cause of pain, your veterinarian may prescribe pain medications such as NSAIDs (non-steroidal anti-inflammatories). NSAIDs are medications that help reduce pain and inflammation. Pets are often prescribed anti-inflammatories (NSAIDs) to help relieve the pain following surgery, dental, or long-term for pets with chronic conditions such as osteoarthritis. These products can provide very effective pain relief but are not advised for pets with kidney, liver, or stomach issues.
Other types of natural pain relief for dogs may include:
• laser therapy
• cold therapy
• acupuncture
Daily habits
Changes in sleeping habits
Changes in drinking habits
Changes in toilet habits
Excessive licking
• rehabilitation therapy
• hydrotherapy.
Self-mutilation
Biting itself
Scratching excessively
Restless
Pacing
Decreased interest in exercise or playing
Your veterinarian will determine the right anti-inflammatory and pain management therapy for your pet.
TIPS
If your pet is prescribed NSAIDs, always monitor for side effects:
• Vomiting
• Diarrhea (with or without blood)
Activity level
Shows difficulty in rising or sitting down
Less energy
Less eager at greetings
Difficulty walking upstairs or on tiles
Grimace
Vacant stare
Facial expressions
Sleepy look
Enlarged pupils
Flattened ears
Excessive panting
Protects a body part
Does not weight bear on a leg
Self-protection
Limps
Doesn’t want to be petted or held
Growls
Bites
Aggression
Posture
Snaps
Pins ears back
Hunched over Lies on its side
If your pet is showing signs of pain, seek veterinary attention immediately.
• Inappetence
• Tense abdomen
• Black stools
• Drinking a lot
• Urinating a lot
• Pale gums.
Notify your veterinary hospital immediately if you notice any of these signs.
NEVER use human NSAIDs on your pets!
Source: VetCheck is a powerful client education platform that helps veterinary teams save time, increase client engagement, retention and grow the practice through digital pet health summaries, handouts, best practice tools (digital dental charts, GA monitoring charts, hospital workflow) and forms with e-sign. To add your practice logo and start sharing directly to the pet owner’s mobile phone, visit www.vetcheck.it
© VetCheck Technologies Pty Ltd. ® VetCheck is a registered trademark. All rights reserved.
For digital case reports, handouts and request forms for veterinary teams visit www.vetcheck.it
34 September 2023 CLIENT FACT SHEET
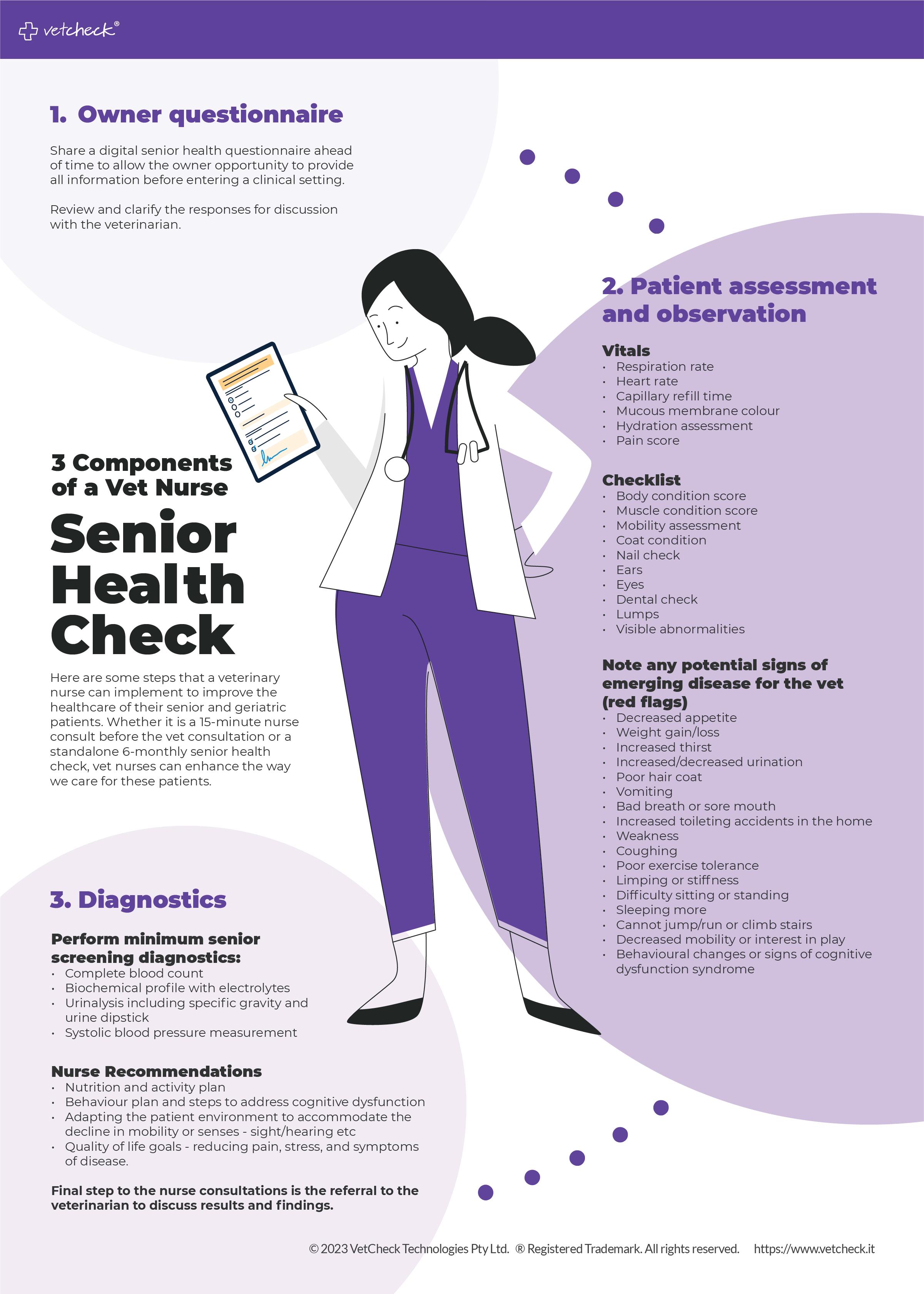
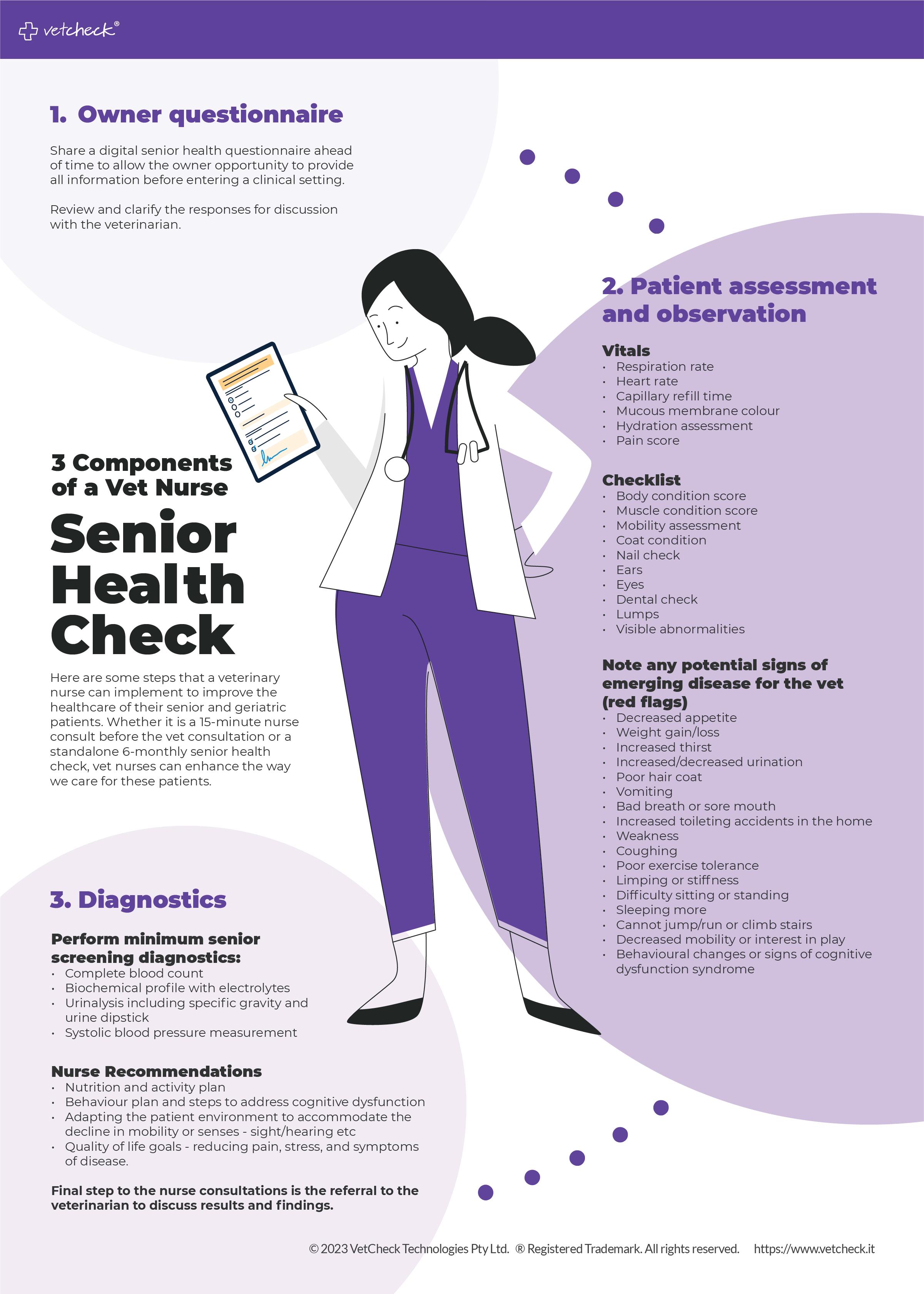
VNCA HR Advisory Service
Flexible working arrangements
Workplace flexibility is increasingly becoming a crucial factor determining overall job satisfaction – even more so in a post-covid landscape. Employees should be aware of the legislative provisions available to them to request more flexibility in how they perform their role to allow them greater work/life balance.
This article will discuss the provisions for flexible working arrangements outlined within the National Employment Standards (NES). It will also reflect changes that took effect on 6 June 2022 after the passing of the Secure Jobs, Better Pay Bill in late 2022.
WHO IS ELIGIBLE TO MAKE A REQUEST FOR A FLEXIBLE WORKING ARRANGEMENT?
The NES prescribes certain groups of employees can request flexible working arrangements. These include:
1. employees with caring responsibilities in accordance with the Carer Recognition Act 2010
2. parents or guardians with the responsibility of caring for a child who is school age or younger
3. employees with a disability
4. employees who are 55 years or older
5. employees that are pregnant
6. employees who are experiencing family violence or who are providing care or support to a family or household member who is experiencing family violence.
To be eligible to make a request, employees in these groups must have completed at least 12 months of continuous service. Long-term casual employees with at least 12 months of continuous employment and a reasonable expectation of continuing employment are also eligible to make such requests, provided they meet at least one of the above criteria.
EXAMPLES OF FLEXIBLE WORKING ARRANGEMENTS
• Changes in hours of work (e.g. reduction/increases in hours worked, changes to start/finish times)
• Changes in patterns of work (working extra hours for taking time off)
• Changes in location of work (e.g. working from home or another location)
• Requests for part-time employment or job share arrangements
• Arrangements for time off in lieu of being paid overtime payments. This isn’t an exhaustive list. Negotiating other flexible arrangements is possible as long as they are mutually suitable for both the employee and the employer, and may depend on the type of workplace, the scale of the business, and the employee’s role.
REQUESTING (AND RESPONDING TO A REQUEST FOR) FLEXIBLE WORKING ARRANGEMENTS
Employees must submit their request for flexible working arrangements in writing, providing details of the desired changes and the reasons behind them. Employers are required to provide a written response within 21 days, indicating whether the request is granted or refused.
However, before issuing a written response, the Secure Jobs, Better Pay Bill has introduced new obligations within the NES. These require employers to first discuss the employee’s proposed request and engage in genuine discussions with the employee to explore alternative agreements if the initial request is not feasible – as well as to consider the consequences of refusal from the perspective of the employee.
If the employer declines the request, they must provide a written response outlining the reasonable business grounds for refusal, any alternative changes they are willing to consider, and information on how to refer the dispute to the Fair Work Commission (FWC).
All requests for flexible working arrangements must be seriously considered by the employer but may be refused only where reasonable business grounds exist.
WHAT ARE REASONABLE BUSINESS GROUNDS?
While the Fair Work Act 2009 does not define ‘reasonable business grounds’, employers should consider a nonexhaustive list of relevant factors, including:
• The impairment on the workplace and the employer’s business on approving the request, including the financial impact of doing so and the impact on efficiency, productivity and customer service.
• The difficulty or inability to reorganise work among existing staff.
• The inability to recruit a replacement employee or the practicality or otherwise of the arrangements that may need to be put in place to accommodate the employee’s request.
CAN A REFUSAL OF A REQUEST BE CHALLENGED?
It is important to be aware that there is no obligation for an employer to agree to a request for flexible working arrangements. However, recent changes to the Fair Work Act 2009 identified a gap in the existing legislation. They empower the FWC, upon application by either party, to deal with a dispute about flexible working arrangements if the dispute concerning an employer’s decision
VNCA HR ADVISORY SERVICE 36 September 2023
(or failure to respond within 21 days) cannot be resolved at the workplace level. This would be most relevant when an employer has refused an employee’s request.
If this were to occur, the FWC will first look to resolve the dispute by means other than arbitration, such as:
• conciliation
• mediation
• making a recommendation or expressing an opinion.
Where it still cannot be resolved, the FWC may arbitrate the dispute and make a mandatory order concerning the matter. This might stipulate
whether or not the refusal of a request is to be taken to have been refused on reasonable business grounds or not.
The Fair Work Commission can also commence court proceedings for alleged breaches of the flexible working arrangements.
IN SUMMARY
While flexible working arrangements have been in existence for a considerable period, employees should be mindful of recent amendments designed to expand the scope of these provisions to encompass vulnerable demographics. Additionally, these amendments
empower employees to seek resolution in the event of a dispute. For more information about this article, please contact the VNCA HR Service on 02 8448 3266 or email helpline@ myadvantage.com.au. Alternatively, templates and other resources can be found online at the HR Portal available to members.

©shutterstock/Olezzo VNCA HR ADVISORY SERVICE September 2023 37
It is important to be aware that there is no obligation for an employer to agree to a request for flexible working arrangements.
A brief history of VfCA
Vets for Climate Action (VfCA) started with a Facebook post in 2019 where Dr Jeannet Kessels sent a rallying cry, asking for other members of the veterinary community to join her and take meaningful action – to be a voice for animals following the Black Summer bushfires where over 3 billion animals were killed or displaced. From this, a core group of individuals established VfCA.

VfCA is a charity that exists because our changing climate is significantly impacting animal health and welfare, and even though animals hold no responsibility for the causes of this, they feel the consequences most strongly. VfCA represents concerned vets, vet nurses, and industry partners who want to see climate action.
Veterinary professionals are on the frontline experiencing the impacts of devastating events like fires, floods, droughts and heatwaves first hand. We carry a deep responsibility to use our knowledge, skills and influence to protect animals.
We are solutions focused and would love you to join us in our quest to ensure all animals have a voice.
Our vision: A world where animals and people thrive in a healthy climate
Our mission: To mobilise the veterinary profession and broader animal care community to tackle the climate crisis within and beyond our sector

Our purpose: To lead those who love, care for and work with animals to act urgently on climate change
Some benefits from participating clinics:
• Greater Springfield Veterinary reduced water usage by 278 L (30%) per day! This is an easy way to be more sustainable and improve profitability – win win!
• Brimbank Vet Clinic minimised waste through implementing simple, day-to-day changes, saving a total of $3000 p.a. – a positive change for a small investment of time.

Climate change can be scary, but at VfCA we like to say ‘Don’t get depressed – get active!’ We hope you can join us on our journey to protect the animals we love and need.
How can you get involved?
Here are 4 ways you can be a voice for our animals:
Sign up to our newsletter to stay up to date on the work we’re doing to reduce emissions, advocate to governments, and create action-based programs to help turn this ‘climate ship’ around.
1 2 3 4
Volunteer with us! If you love writing, editing, social media, attending events, fundraising or speaking to the media, we would love you to join our volunteer team.
Make a small, tax deductible donation to support our work.
Talk to your clinic about joining VfCA’s Climate Care Program (CCP) to empower your team to take the lead on environmental sustainability in your practice. You can get AVNAT points for participating!
The CCP is an online toolkit with 6 modules that will help you and your team to be more sustainable in your dayto-day veterinary work. AND it can help the clinic to:
• reduce energy, waste and water
• reduce chemical use
• create a culture of sustainability
• increase profitability
• attract values-aligned staff
• reduce overall emissions, creating a better world for the animals we love and need.
38 September 2023 NEWS
Member Vitals
outside of work (I also run a non-profit guinea pig sanctuary, which takes a lot of time and care). When I heard of the veterinary technology degree through the University of Queensland, specifically how much emphasis there was on learning about avian, exotic and wildlife species in the degree, I realised that the veterinary industry better aligned with my goal.
Having a supportive work environment that hypes up your achievements and sympathises with your losses is so important for not spiralling with ‘what ifs’ outside of work.
Name: Iffy Glendinning
Qualification:
Registered Veterinary Technician with a Bachelor of Veterinary Technology (First Class Honours) and a Bachelor of Science
(Zoology and Marine Biology)
Currently studying anything?
Formally, no. But for the purpose of professional development, I’m always completing online CE courses, reading journal articles and attending or presenting at conferences. Particularly given that the field of avian and exotics is still so novel, there’s always something new to learn and always something new that I can teach other people within the industry.
Why did you choose veterinary nursing as your career?

As a child, I had grand plans of becoming a zoologist and a marine biologist. The geckos that I kidnapped and held hostage in my shoe-box zoo probably weren’t as excited by that notion as I was, but luckily they always managed to escape my wellintended love. I had always wanted to work in wildlife conservation and educate the general public regarding wildlife welfare. In reality, jobs in such a niche field are so few and far between and involve a lot of travelling, which unfortunately didn’t fit with my life
Inspired by the likes of Rebecca de Gier and Gary Fitzgerald, both VTS’s in avian and exotics, and such kind, knowledgeable and humble people, I completed my degree, furthered my skills with a clinical honours year in avian and exotics, and am excited to work towards achieving a VTS myself. I now have the immense pleasure of lecturing for the veterinary technology degree, to hopefully inspire other hopeful avian, exotic or wildlife techs into the industry.
What has been your most memorable moment as a veterinary nurse and why?
It’s impossible to choose just one. Working in avian and exotics, I frequently get to work with unique species that very few people have worked with in their careers. From doing an anaesthetic on a penguin, to being the surgical nurse for a bilby, to doing a CT on an emu, to admitting a koala with chlamydia, to a bandage change on a Wedge-tailed eagle, every day brings memorable moments that reignite my passion for my career.
If you could give other nurses one piece of advice or a tip you have learnt, what would it be?
Never stop learning. It wasn’t that long ago that dogs and cats were considered new and scary, yet nurses and technicians today work with these animals with such confidence in their abilities due to having put in the time and effort to learn about them. The same goes for other fields of veterinary nursing, such as avian and exotics, equine or production
animals. There’s always something new to learn, there are always more experienced people that you can learn from, and there’s always something you can teach others.
Also, when placing an IV catheter in a tiny patient, priming your catheter with saline before placement can help you appreciate the teeny tiny flash of blood you’ll get to confirm your placement.
How do you keep a work/life balance?
It’s an ongoing battle that I still struggle with. When I check my weekly schedule, if I have a patient coming in that’s a species I haven’t worked with before, I’ll put a lot of time into researching and planning for that case outside of work. The biggest thing I’ve learned over time is to be kind to myself. If I spend the night before a case researching, I should spend the night after that case hopefully celebrating a job well done. Having a supportive work environment that hypes up your achievements and sympathises with your losses is so important for not spiralling with ‘what ifs’ outside of work. And on your days off, turn your mind off work. Make time for your hobbies, or even just to catch up on sleep if you need it. Your work will still be waiting for you come Monday regardless of whether you think about it over the weekend. So you may as well not think about it and take the time to rest or recharge.
September 2023 39 MEMBER VITALS Continued next page
Member Vitals
For me personally, I love taking the time to sit down with a good book and a warm cup of tea. I make sure to go for a run with my dogs every day. I spend time with my husband binge-watching the latest Netflix series or working with my cockatoo who’s currently learning how to use an iPad (she loves to play games designed for toddlers on it). And I take time off throughout the year to travel and go diving to satisfy the marine biologist in me.
What animals do you own?
As a director of a registered non-profit guinea pig sanctuary, I currently have sixty-two palliative care guinea pigs in my care. They live in what I affectionately refer to as the Pig Pod – a modified granny flat on my property designed purely for them and their needs. Outside of the sanctuary, I have two Siberian huskies, a coastal python, two alexandrine parrots, a red-tailed black cockatoo, three budgies, a cockatiel, a kakariki, and fourteen pigeons – all rescues with medical needs. My husband is an aquaculturist who also likes to bring his work home, so we have many fish tanks in the mix as well. My front doormat aptly says ‘welcome, it’s a zoo in here’.
How long have you been a VNCA Member?
I first joined as a vet tech student and have retained my membership over the past 6 years. I find the networking opportunities, the conferences and the CPD invaluable towards my professional development and can’t wait for next year’s VNCA Conference.
Congratulations Accredited Veterinary Nurse Scheme

Launched in 2002, the Accredited Veterinary Nurse (AVN) Scheme is a joint initiative between the VNCA and the AVA (working together through the National Industry Advisory Group for Veterinary Nursing – NIAG).

It recognises veterinary nurses who demonstrate currency of skills and dedication to the veterinary nursing profession and is the gold standard for clinical veterinary nurses, providing an avenue for those who wish to extend themselves beyond AVNAT registration.
We recognise recently approved and renewing Accredited Veterinary Nurses:
New Accredited Veterinary Nurses:

Kristen Booth
Shannon Crozier-Rankin
Leonie Cukela
Telea Hotker
Shereece Kaden
Elizabeth McConnell
Daphne McNeill
Gemma Murphy
Sarah Price
Helen Waller
©gettyimages/Julia_Sudnitskaya
40 September 2023 MEMBER VITALS
The AVNAT Registration Scheme
The AVNAT Registration Scheme has been established by the VNCA to set the standards of professionalism across the veterinary industry. Congratulations to our newest AVNAT registered veterinary nurses and technicians for their commitment to quality practice
NEW MEMBERS
Emily Aiello
Sarah Ali
Alexandra Allanson
Jesse Andrewartha
Amanda Arbon
Hannah Ashford
Chanel Assetta
Dianna Atherton
Ellie Attleir
Anna Bailey
Linda Banks
Stacey Barlow
Kristina Barr
Meg Barua
Ava Baxter
Samantha Bell
Alexia Benic
Jessica Benjamin-
Young
Rachael Bison
Tiffany Black
Samantha Bleakley
Madison Blunden
Madeline Bowe
Jasmine Braybrooks
Sophie Brown
Melanie Burns
Samantha Burton
Jessica Burton
Tyneal Callus
Louise CameronMurphy
Cherene Campbell
Hayley Cecil
Nicole Chamberlain
Amy Chapman
Oi Ting Lora Chow
Jacinta Clarke
Shannon Cobb
Emily Coleman
Melissa Collins
Lara Connell
Vivien Cook
Brie Coxsedge
Neil Coy
Tessa Cross
Shannon CrozierRankin
Leonie Cukela
Olivia Day
Lucy Dimmick
Chantelle Diolosa
Fiona Docherty
Melania Doueihi
Taryn Dowsley
Hannah Doyle
Natalia Duczkowski
Tania Egan
Elisabeth Ellicott
Elizabeth Ellis
Stephanie Eric
Naomi Evans
Colleen Finn
Christina Fitzpatrick
April Ford
Emma Foster
Elizabeth Foster
Michelle Fuller
Isobel Fuller
Kristina Gaddi
Olivia Gallagher
Anna Godschalk
Catherine Gotch
Lisa Grainger
Hannah Greyson
Belinda Guarnaccia
Maria Guinan
Brooke Guscott
Tracey Hall
Tahlia Hann
Sarah Harrison
Annie Hazel
Elke Henderson
Rose Hermanek
Leanne Hill
Renee Hodges
Amorie Hodgson
Christine Holden
Kim Hollis-Simpson
Laura Hopkins
Shaelee Howell
Kimberley Hughes
Sarah Hunting
Taryn Ineson
Lynette Jackson
Chloe Johnson
Mckenzee Jones
Amanda Kennedy
Amanda King
Rebecca Kirk
Zoe Kirwan
Pippa Klein
Danielle Koetsveld
Josef Kohlmetz
Odette Kolenich
Anna Kolodziejczyk
Annabelle Korner
Kate Last
Pui Yin Law
Chloe Leggett
Hoi Kun Leung
Alison Liddicoat
Shana Lin
Tate Liversidge
Isabella Lomax
Angelica Luansing
Teal Lunin
Gabrielle
Maczkowiack
Renee Martin
Lea Mathy
Janelle Matthewman
Simone Mayer
Georgia McCasker
Sonya McDowall
Lauren McFarland
Isabelle McGlade
Alexander McGuire
Tamarra McInerney
Courtney McIntosh
Sarah McIntosh
Erika McKay
Alexandra McKendry
Lana McLaren
Heather McLean
Michayla McRae
Alexandra Meddings
Tayla Menna
Caitlin Menzies
Shannon Molloy
Riccardo Monti
Holly Moore
Jodie Moretti
Lauren Morgan
Anna Munro-Faure
Dana Murison
Gemma Murphy
Shayna Murphy
Thi thanh mai (Anna
Nguyen)
Tahnee Olsson
Penny (Penelope)
O’Neil
Krystle Orndahl
Jenna Owen
Rhiannon Paddick
Sunae Park
Katie Parker
Emily Paterson
Meredith Pendleton
Hollie-May Penny
Brooklyn Perrin
Kate Perry
Allison Prentice
Sarah Price
Erin Pridgeon
Claire Ramage
Giuliana Randall
Danielle Reeves
Annie Renouf
Suzannah Robinson
Rosemarie Robinson
Rhiannon Sanderson
Abbey Santas
Sharon Schultz
Annette Scott
Jordi Shearer
Maddison Shepheard
Hanna Shepherd
Amy Sloan
Hailley Smith
Natasha Smith
Morgane Soquet
Tamara St Eain
Jessica Starr
Shae StewartHughes
Elizabeth Street
Kathy Teall
Chloe Thomas
Amber Thomas
Olivia Thursky
Blake Tickner
Sweet Yee Tong
Man Yi Tsang
Nathan Turner
Kara Turner
Evie Verdini Fensom
Taryn Walker
Kristie Wallis
Ashleigh Walsh
Monique Walters
Samm Walton
Jessica Walton
Eliza Watters
Dana Whitaker
Emilie Whitehead
Dora Williams
Samantha Williams
Abbey Williams
Megan Wilson
Natalie Woods
Paige Worden
Chelsea Wright
Belinda Wright
Roxanne Yates
Jasmin Zouroudis
OUR PROFESSION September 2023 41 OUR PROFESSION
Join the VNCA today and start enjoying all the benefits of belonging ...
There’s never been a better time to become a member of the VNCA and support our work to promote the interests of veterinary nurses and technicians across Australia.

You will receive huge discounts on AVNAT registration, education opportunities and everyday purchases like petrol! And … you will be rewarded with all the #benefitsofbelonging.
Follow the QR code to our website - www.vnca.asn.auto find out more and join online today!
E: admin@vnca.asn.au | P: 03 9586 6022
#myVNCA #benefitsofbelonging
Special offers!
• Up to 8 weeks free when joining in May/June and Nov/Dec
• Cheaper for students
• Clinic discounts
The AVNAT Registration Scheme: Demonstrate your commitment to your profession

Did you know that the number of veterinary nurses and technicians voluntarily registered through the AVNAT Registration Scheme is increasing annually by more than 10%?
With mandatory registration a priority for the veterinary industry, now is the ideal time to commit to your profession by becoming registered As well as guiding you through your career, being AVNAT registered will demonstrate your commitment to quality practice through standards and learning.
Maintaining quality practice through standards and learning

Workplace Helpline Industrial Relations & Human Resources for vet nurses Member Discounts $
www.vnca.asn.au/avnat