Hospital Eyes New Beds for Youth
By BRETT YATES
BENNINGTON – Vermont could have ten to 12 new inpatient psychiatric beds for adolescents by 2024 if a proposal by Southwestern Vermont Medical Center comes to fruition.
Direct input from psychiatric survivors or family members has yet to be brought into discussion on the idea, and some have questions about whether it is an appropriate plan.

Hospital officials have stressed the uncertain nature of the plan thus far. The first step will be a feasibility study, which was scheduled to begin by late fall and is due for completion by March 31.
SVMC has targeted a 4,500-square-foot area within its main hospital building in Bennington for a potential renovation that would create a private room for each patient, as well as an “education space” for schoolwork and a common area for “visits with family, peers and support persons.”
Its preliminary cost calculation for the project estimates a price tag as high $10.425 million from pre-construction to launch.
Prolonged delays in emergency departments across the state for kids awaiting inpatient psychiatric placements — sometimes for a week or more — led the Department of Mental Health to issue a request for proposals for a new highacuity pediatric psychiatric unit last January.
It called for “up to 10 beds” to supplement Vermont’s only children’s psych ward at the Brattleboro Retreat.
But DMH initially received just one response, which the University of Vermont Medical Center subsequently withdrew, citing a budgetary shortfall.
DMH reissued the request for proposals in June, and this time, SVMC decided to throw its hat in the ring. “The first time they offered the RFP, we started to pull together a proposal and really started looking at this and realized that it was just really a significant lift for SVMC,” Director of Planning James Trimarchi recalled.
By BRETT YATES
An increased regulatory focus on removing psychiatric inpatients’ opportunities for selfharm has led Vermont’s hospitals to make major changes to improve safety. But according to psychiatric survivors, some of these changes have yielded unintended consequences in how supportive the units feel.
The Centers for Medicare and Medicaid Services defines a “ligature risk” as “anything which could be used to attach a cord, rope, or other material for the purpose of hanging or strangulation.”
Possible ligature points, per CMS, include “shower rails, coat hooks, pipes, and radiators,” among other common objects.
Hospitals offering psychiatric care can achieve regulatory compliance by removing such objects or, when removal may not be possible, by restricting patient access to spaces that contain them.
By some accounts, this effort has had the side effect of creating a less hospitable and less free environment in psychiatric units.
After several earlier stays, a psychiatric inpatient returned this fall to Central Vermont
Medical Center. She noticed a number of differences. In the past, by her recollection, patients had enjoyed unsupervised use of the laundry facilities.
Now, they had to ask staff to unlock the
“When the proposal that they did receive got withdrawn,” Trimarchi continued, “they
(AdobeStock) (Continued on
Does Safety Hurt More Than Help?
staff looked on. The unit’s microwave had also disappeared, and patients had lost access to hot water for tea.
Under CMS rules, hospital patients have “the right to receive care in a safe environment.” The agency’s interpretive guidelines specify that this requirement intends to protect “the patient’s emotional health and safety as well as his/her physical safety.” Sometimes, however, these paired promises appear to come into conflict with one another.
laundry room each time they wanted to wash, dry, or retrieve their clothes.
The same locked area of the psychiatric unit also contained books, puzzles, and an exercise bike, as well as a small, semi-enclosed terrace that patients used to be able to visit as they pleased.
Now, however, staff had to bring books out to them, and the terrace was off-limits all day except for an hour, during which patients would crowd together for a few breaths of fresh air as
“How can you feel comfortable enough to start healing if you feel that you can’t do things for yourself, and you have to feel you’re bothering someone to do something simple?” the CVMC patient asked. Understaffing had compounded the problem. Overburdened workers could still be “pretty accommodating if people were patient,” but the patient also reported an instance in which one staffer became “very annoyed” by a request for assistance. An encounter of this kind “really impacts the way you feel about yourself,” the patient said.
officials attributed most of the changes experienced by the Central Vermont (Continued on

NEWS, COMMENTARY, AND ARTS BY PSYCHIATRIC SURVIVORS, MENTAL HEALTH PEERS, AND OUR FAMILIES VOL. XXXVII NO. 3 • FROM THE HILLS OF VERMONT • SINCE 1985 • WINTER, 2022 22 Out of the Darkness Walk 12 The Arts 8 Telepsych May Expand in EDs
“We didn’t submit a proposal in that first round, but we had good conversation with the
Department of Mental Health about a kind of shared vision of what the need is in the community and what we might be able to do.
page 3)
page
Hospital
4)
The federal CMS guidelines say hospitals are supposed to protect “the patient’s emotional health and safety as well as his/her physical safety.”
VERMONT PSYCHIATRIC SURVIVORS BOARD
A membership organization providing peer support, out reach, advocacy and education. Board meets monthly. For information call 802-775-6834 or email info@vermont psychiatricsurvivors.org.
COUNTERPOINT EDITORIAL ADVISORY BOARD
The editorial advisory board for the Vermont Psychiatric Survivors newspaper can always use help! Assists with poli cy, editing and brainstorming on topics for articles. Contact counterpoint@vermontpsychiatricsurvivors.org
ALYSSUM Peer crisis respite. To serve on board, call 802-767-6000 or write to information@alyssum.org
DISABILITY RIGHTS
VERMONT PAIMI COUNCIL
Protection and advocacy for individuals with mental ill ness. Call 1-800-834-7890.
DISABILITY RIGHTS VERMONT
Advocacy in dealing with abuse, neglect or other rights violations by a hospital, care home, or community mental health agency. 141 Main St, Suite 7, Montpelier VT 05602; 800-834-7890. disabilityrightsvt.org
VERMONT CENTER FOR INDEPENDENT LIVING
Peer services and advocacy for persons with disabilities. 800-639-1522. vcil.org
HEALTH CARE ADVOCATE To report problems with any health insurance or Medicaid/Medicare issues in Vermont 800-917-7787 or 802-241-1102. vtlawhelp.org/health
VERMONT CLIENT ASSISTANCE PROGRAM
Rights when dealing with service organizations such as Vocational Rehabilitation. Box 1367, Burlington VT 05402; 800-747-5022.
NAMI-VT
Family and peer support services, 802-876-7949 x101 or 800-639-6480; 600 Blair Park Road, Suite 301, Williston VT 05495; www.namitvt.org; info@namivt.org
ADULT PROGRAM STANDING COMMITTEE
Advises the Commissioner of Mental Health on the adult mental health system. The committee is the official body for review of and recommendations for redesignation of community mental health programs (designated agencies) and monitors other aspects of the system. Members are persons with lived mental health experience, family mem bers, and professionals. Meets monthly on 2nd Monday, noon-3 p.m. Check DMH website www.mentalhealth.ver mont.gov or call-in number. For further information, con tact member Daniel Towle (dantowle@comcast.net) or the DMH quality team at Eva.Dayon@vermont.gov
LOCAL PROGRAM STANDING COMMITTEES
Advisory groups, required for every community mental health center. For membership or participation, contact your local agency for information (listings on back page.)
PEER WORKFORCE DEVELOPMENT INITIATIVE
Webpage provides an up-to-date account of statewide peer training and registration information as well as updates about its progress and efforts. www.pathwaysvermont. org/what-we-do/statewide-peer-workforce-resources/
MADFREEDOM
MadFreedom is a human and civil rights membership organization whose mission is to secure political power to end discrimination and oppression of people based on perceived mental state. See more at madfreedom.org
MENTAL HEALTH LAW PROJECT
Representation for rights when facing commitment to a psychiatric hospital. 802-241-3222.
ADULT PROTECTIVE SERVICES
Reporting of abuse, neglect or exploitation of vulnerable adults, 800-564-1612; also to report violations at hospi tals/nursing homes through Licensing and Protection at (802) 871-3317
Hospital Advisory
CENTRAL VERMONT MEDICAL CENTER NEWLY forming. Contact counterpoint@ vermontpychiatricsurvivors.org for more information and meeting schedule.
VERMONT PSYCHIATRIC CARE HOSPITAL Advisory Steering Committee, Berlin, check DMH website for dates at www.mentalhealth.vermont.gov
RUTLAND REGIONAL MEDICAL CENTER Community Advisory Committee, fourth Mondays, noon, call 802-747-6295 or email lcathcart@rrmc.org
UNIVERSITY OF VERMONT MEDICAL CENTER Program Quality Committee, third Tuesdays, 9-10 a.m., for information call 802-847-4560.
BRATTLEBORO RETREAT
Consumer Advisory Council, fourth Tuesdays, 12-1:30 p.m., contact Director of Patient Advocacy and Consumer Affairs at 802-258-6118 for meeting information.
Trainings and Conferences
PEER WEBINARS
Doors to WellBeing hosts monthly one-hour webinars for peer programs on every last Tuesday of the month. For more information and to register, https://www.doorstowellbeing.org/webinars
MENTAL HEALTH ADVOCACY DAY
A “save the date alert” has been posted for January 30, 2023 for the annual Mental Health Advocacy Day traditionally held at the state capital building. It will continue this year in its interim virtual format.
PEERPOCALYPSE
The Mental Health & Addiction Association of Oregon has announced a “save the date” for the tenth annual Peerpocalypse conference May 8-11, 2023. More information will follow on the conference web page at www.mhaoforegon.org/peerpocalypse when the date is nearer.
PEER WORKFORCE DEVELOPMENT INITIATIVE
See page 8 for details on three new training offerings through Pathways Vermont.
VT Psychiatric Survivors, 128 Merchants Row Suite 606, Rutland, VT 05701
Phone: (802) 775-6834
email: counterpoint@ vermontpsychiatricsurvivors.org
MISSION STATEMENT:
Counterpoint is a voice for news and the arts by psychiatric survivors, ex-patients, and consumers of mental health services, and our families and friends.
Copyright 2021, All Rights Reserved FOUNDING EDITOR
Robert Crosby Loomis (1943-1994)
EDITORIAL BOARD
Kara Greenblott, Zachary Hughes, Sara Neller, Laura Shanks, Dan Towle
The Editorial Board reviews editorial policy and all ma terials in each issue of Counterpoint. Review does not necessarily imply support or agreement with any posi tions or opinions.
PUBLISHER
Vermont Psychiatric Survivors, Inc.
The publisher has supervisory authority over all aspects of Counterpoint editing and publishing.
EDITOR
Anne B. Donahue
Brett Yates, Co-Editor
Opinions expressed by columnists and writers reflect the opinion of their authors and should not be taken as the position of Counterpoint
Counterpoint is funded by the freedom-loving people of Vermont through their Department of Mental Health. Financial support does not imply support, agree ment or endorsement of any of the positions or opinions in this newspaper; DMH does not interfere with editorial con tent.
Counterpoint is published by Vermont Psychiatric Survivors three times a year, distributed free of charge through out Vermont, and also available by mail subscription. Vermont Psychiatric Survivors is an independent, statewide mutual support and civil rights advocacy organization run by and for psychiatric survivors. The mission of Vermont Psychiatric Sur vivors is to provide advocacy and mutual support that seeks to end psychiatric coercion, oppression and discrimination.
Counterpoint does not use pseudonyms in its reporting without stating that a pseudonym is being used and without an explanation for why the person’s identity is not being disclosed. Counterpoint does not use anonymous sources under any circumstances.
Checks
Send to: Counterpoint, Vermont Psychiatric Survivors, 128 Merchants Row, Suite 606, Rutland, VT 05701
Access Counterpoint online at www.vermontpsychiatricsurvivors.org
Fall 2018
2 c Enclosed is $10 for 3 issues (1 year). c I can’t afford it right now, but please sign me up (VT only). c Please use this extra donation to help in your work. (Our thanks!)
or money orders
made
should be
payable to “Vermont Psychiatric Survivors.”
Don’t Miss Out on a Counterpoint! Peer Leadership and Advocacy
NAME: ADDRESS: CITY • STATE • ZIP Mail delivery straight to your home — be the first to get it, never miss an issue.
Advocacy Organizations Department of Mental Health 802-241-0090 www.mentalhealth.vermont.gov For DMH meetings, go to web site and choose “more” at the bottom of the “Upcoming Events” column. ADDRESS: 280 State Drive NOB 2 North Waterbury, VT 05671-2010
Meeting Dates and Membership Information for Boards, Committees and Conferences
Peer Organizations State Committees
-
Counterpoint Opinion Poll
Do safety features to prevent self-harm in hospital psych units make them feel like a less healing environment?
Fall Poll Results:
The Small Number Responding Support a Separate Forensic Facility

RUTLAND – Of a total of only 25 responses to Counterpoint’s fall poll question, about two-thirds supported creation of a separate hospital for patients who are involved with the criminal justice system.
In Vermont – unlike most states – such forensic patients are held in facilities which also have individuals who are being held based on being perceived as a danger to self or others, but not accused of a crime.
“Too many people with psych Dx are grouped with real, criminally insane sociopaths who prey on us,” one person wrote in the comments section. “They carry on their deadly routines in hospital. Which makes recovery from a suicidal, depressive, or hallucinatory episode
all that much harder. Being housed together also reinforces stigma and unfounded stereotypes.”
The poll was open to anyone who accesses it through Counterpoint or other Vermont Psychiatric Survivor links which do not distinguish whether responses are coming from psych survivors, families or other members of the public. The number of replies make the results particularly random, rather than an indicator of general opinion.
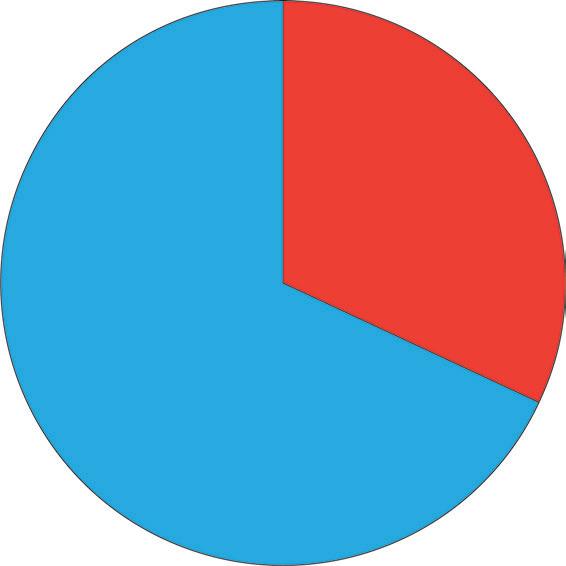
One of the comments suggested that some individuals may not have understood the question. “I believe we do [need a forensic hospital] because without one where are people of Vermont supposed to go to get the mental health they need to get so that they can start to
feel better?” they wrote. “Without the help for mental health and [from] VPS I feel and know that I would probably not be around or in the state of Vermont.” The writer urged services “for the homeless, mental health and [such as] VPS.”
One person’s thoughts included a message to potential forensic patients based upon her own experiences. It is printed in full on page 17 as a commentary.
HOSPITAL EYES NEW
BEDS
FOR YOUTH • Continued from page 1 reached back out to us and they said, ‘Is there a possibility that we could do a joint feasibility study and see whether or not this makes sense?’”
SVMC signed a contract for $25,000 with DMH in late October to examine the statewide demand for inpatient psychiatric beds for children between the ages of 12 and 17, and the potential cost of construction and operations at SVMC. The contract commits DMH to “share perspective and concerns from other Vermont agencies and departments in order to ensure that collateral impacts are considered in the design of the unit and its operations.”
SWMC is also required to “obtain feedback on the design and operations from [United Counselling Services, Bennington’s community mental health center], mental health advocacy organization such as Disability Rights Vermont and persons with lived experience.”
However, the resulting report, which must include “reflective anticipated impact on state agencies and departments,” does not require any similar assessment of impact on children and families.
Trimarchi, the SWMC planning director, said they’ll solicit input from “organizations that can speak to lived experience, to make sure that we have the design right and the model right and the programming right.”
“We haven’t had the kickoff for the feasibility study, so there has been no firm commitment to engage any specific group. What I can tell you is we will engage groups,” he clarified.
The contract doesn’t compel SVMC to build the unit.
“We’re a medical facility, not historically
an inpatient psychiatric facility,” Trimarchi acknowledged. “We’re exploring the idea.”
In doing so, SVMC expects to get a better understanding of several potential roadblocks.

“There’s a lot of challenges from the space constraints, from the regulatory constraints,” Trimarchi noted. “There’s staffing challenges, in terms of recruitment of the right providers to staff it... If we’re going to do this, we want to do this right, and the right way to do it is traumainformed, in the least restrictive way,” he said.
proposal, but to the extent it’s constructing another locked facility to serve youth, I think that that might be not what Vermont really needs right now,” she commented. “There needs to be a lot more work done in Vermont to provide better, proactive, and progressive treatment options in the communities.”
Counterpoint asked DMH whether any input was solicited from psychiatric survivors in the lead-up to or writing of the request for proposals for this or other new projects it is pursuing.
A spokesperson said that the state “made a reasonable assumption that some peer communities and providers may likely be bidders” on the projects, and allowing direct participation in drafting an RPF would exclude them from bidding.
But soliciting input and questions has been a consistent part of all the planning, DMH said, including through the adult and children’s mental health standing committees.
Vermont Psychiatric Survivors Executive Director Karim Chapman expressed hope that VPS could offer peer support at the facility if SVMC’s proposal pans out.
“For various reasons, such as liability issues, VPS traditionally hasn’t had a history of doing that kind of work with adolescents,” he said. “I would love to see VPS in a position where we are supporting young people.”
Disability Rights Vermont Executive Director Lindsey Owen’s first reaction to SVMC’s plan was unenthusiastic.
“I haven’t had a chance to look at that exact
“Many stakeholders, including peers, have identified the need for expanding the options for care offered in a diversity of settings, rather than relying on the Brattleboro Retreat,” it said in a written response. The RFP was developed “to gauge the interest and feasibility” for an increase in child and adolescent inpatient beds and if it goes forward, “it will begin the process of diversifying available choices for care.”
The DMH statement said that with the feasibility report from SWMC, it “anticipates being able to work collaboratively to develop a project plan that best meets the needs of Vermonters, which will include stakeholder engagement at that time.”
Fall 2018 NEWS . 3 Winter 2022
Results of the poll will be published in the next issue of Counterpoint. OR by going to www.vermontpsychiatricsurvivors.org/counterpoint/
QUESTION:
VOTE by scanning this onto your mobile phone: 8 responses “NO” 16 responses “YES”
(by Graham Ruttan, Unsplash)
PHYSICAL SAFETY MANDATES
Medical Center patient directly to new ligature risk requirements. They pointed to stricter inspections by surveyors from the Joint Commission, the organization that accredits US hospitals. In 2019, the Joint Commission revised its “national patient safety goals” for suicide prevention, following a 2017 decision by CMS to prioritize ligature risk within its own regulatory framework.
“There were reports of increased amounts of inpatient deaths on psychiatric units,” Dr. Robert Althoff, the chair of psychiatry at the University of Vermont Health Network, recalled.
“That then translated into surveys that specifically looked at what are opportunities on inpatient psychiatric units for people to hurt themselves.”
Althoff mentioned that the University of Vermont Medical Center had needed to buy new, safer beds for inpatient psychiatry, in addition to addressing smaller items like door handles and shower bars.
Those beds, which replaced previously approved “psych-safe” beds, are single piece plastic molded units with a mattress on top. UVMMC solicited input from its patient advisory committee in its attempt to select ones that felt least institutional.
“Any flat surface had to have something that was diagonal, so that a ligature would slide off of it rather than wrap around it,” he recounted. “Things that may have met the standard 10 years ago now don’t meet the standards.”
“I can imagine, having talked to people, that it would feel like it’s a more sterile environment – that it’s just a plainer environment than you would want, that it could not feel as friendly,” Althoff acknowledged.
Dr. Conor Carpenter, the medical director for inpatient psychiatry at CVMC, told a similar story about the Joint Commission surveys.
“Their reviewers are not unaware that things that they may ask in terms of creating safe environments have a trade-off for a therapeutic environment. Yet they make it clear that their priority is in safety, and we do the best we can to work with that and maintain as therapeutic an environment as we can here,” he said.
New ligature safety standards aren’t the only changes that have taken place in psychiatric units over the years. Since 2020, COVID-19 precautions have periodically limited visitors and, at times, confined patients to plastic “anterooms.” Before that, health and sanitation standards had already evolved, such as favoring surfaces that don’t allow liquids to soak in.
“You don’t want rugs because they collect pathogens or whatever you want to call it,” said a former UVMMC inpatient, whose most recent stay, in 2020, brought back memories of a “dramatically more homey” environment at the same hospital during earlier hospitalizations between 1999 and 2004, with comfortable couches and available snacks.
“If you restrict food, you’re less likely to have
• Continued from page 1
food scattered around, so you’re not going to have germs from this food that gets spilled,” he elaborated. “It’s a progression, I think, that’s been happening for a while.”
A patient who had been hospitalized at CVMC in the 1980s found herself at the same facility again this August. In the old days, she had passed the time by making mosaic tile hot plates and had sometimes received permission to leave the hospital temporarily.
But this year, she found no arts-and-crafts program inside the psychiatric unit, which she couldn’t exit until her discharge.
Two patient representatives at Vermont Psychiatric Survivors, Grace Walter and Laura Shanks, relayed comparable anecdotes from clients in inpatient settings.
Walter described a Vermont Psychiatric Care Hospital patient who “has been in the psychiatric system for a long time” and “enjoyed collecting leaves or flowers and hanging them on his walls or door” after time in the yard. More recently, however, the patient was “told he wasn’t allowed.”
Shanks brought up an inpatient at UVMMC who, at the start of her third stay this year at the facility, discovered suddenly that she would not be able to bring her wedding band or other small personal items that “provide therapeutic support” into the psychiatric unit with her.
“It didn’t make sense. To me, those don’t pose a risk of harm,” Shanks said.
A third VPS patient representative, Nate Lulek, offered a happier picture of Rutland Regional Medical Center, which, starting in 2019, spent more than $4 million to redesign its psychiatric unit to “correct risks of self-harm.”
Lulek’s account suggested that, by reconstructing the unit from top to bottom, RRMC had managed to provide ligature safeguards without adding restrictions upon patient movement, resulting in few complaints.
He also praised efforts to offset the sterility of the ligature-resistant environment.
“They had artists go up and do murals in common areas. Each one of the rooms are single, and they have artwork from local artists, so that it gives it less of an institutional feel, to a certain extent.”
A patient comment supported what Lulek said. “When I was in RRMC in August 2021, it was not oppressive, but freeing, and health restoring,” she said.
But Lulek noted in November that RRMC was due for a survey by the Joint Commission, which must reaccredit hospitals every three years. “RRMC got notified, I think, last month,” he said. “And who knows if there’s going to be any more stuff thrown on that now has to be done?”
A 2019 report by the National Association
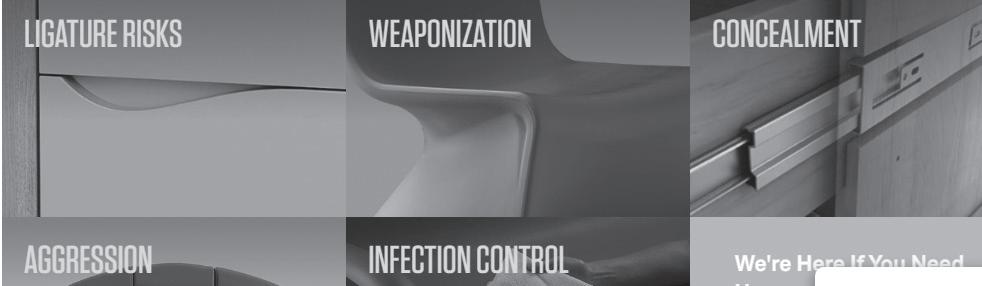
for Behavioral Healthcare estimated that, nationwide, hospitals had to spend $880 million annually in order to comply with ligature risk regulations that could be “unpredictable” and “inconsistent.”
The report recommended reforms such as “a more evidence-based approach to ligature-risk review,” whereby regulators would not demand modifications without “a compelling empirical basis.”
According to NABH President Shawn Coughlin, the report made an impact.
“We were able, in working with CMS, to get some clarifications and some standardization that we had hoped for,” he said.
But that doesn’t mean that Joint Commission surveyors have necessarily altered their judgments yet.
“It absolutely does take time to filter down through the various survey processes, and there probably will always continue to be various interpretations by surveyors,” Coughlin surmised. “Obviously, we’d like to see them be in lockstep.”
In 2018, an article in the Joint Commission Journal on Quality and Patient Safety debunked the commonly cited statistic that the United States sees 1,500 inpatient suicides annually. In fact, the researchers found that the number was closer to 50 or 60.

“There’s so few incidences of people committing suicide in hospitals,” a patient told Counterpoint.
“We’re spending a lot of money to avoid a very, very rare event. And that’s money that could otherwise have been spent someplace else and could have affected lives and reduced suicides in a different way.”
In 2018, Counterpoint reported on a change at the Brattleboro Retreat that required bathrooms to be locked, meaning that patients had to find a staff person to unlock one any time they needed to use the facilities.
The Retreat attributed the change to its own assessment of safety needs, and said there were no alternative measures that would keep patients safe.
”Being denied autonomy over one’s basic bodily functions – being made to ask permission to relieve oneself – is... demeaning and humiliating...” said Calvin Moen, a patient representative from Vermont Psychiatric Survivors at that time.
VPS called it an “affront to patient dignity” and said that patients found it “dehumanizing and degrading.”
The Retreat did not respond to requests by Counterpoint for comments for the current article.
Editor’s note: psychiatric survivors interviewed for this story asked not to be identified by name to protect their privacy.
Fall 2018 NEWS 4 Winter 2022
(by Kateryna4, Unsplash)
An advertisement for psychiatric furniture displays the selling features being highlighted.
New Legislative Agenda Unclear
by BRETT YATES
MONTPELIER – With at least 47 new faces entering the Vermont House of Representatives and nine freshman senators, the 2023-2024 legislative biennium looks more than usual like a blank canvas. Mental health advocates will be watching closely to see how it fills up.
The governor typically submits his executive budget recommendations about two weeks after the start of the session. At that point, legislators –and the public – will hear about the Department of Mental Health’s funding priorities for fiscal year 2024, which begins in July of 2023.
Among potential areas for attention, DMH policy director Nicole DiStasio pointed to workforce shortages “at all levels of service delivery, particularly for psychiatry;” the 988 Suicide & Crisis Lifeline, where efforts to increase in-state call center capacity continue; and mobile crisis response services.
Mobile Crisis Units

Following the start of a pilot program for a youth-oriented mobile crisis team in Rutland, the legislature instructed DMH last spring to develop a model for statewide mobile services. DMH issued a request on Nov. 1 for proposals from “qualified providers that could include, but are not limited to, Vermont Department of Mental Health Designated and Specialized Service Agencies.”
The vendor or vendors will provide “rapid
community crisis response, screening and assessment, stabilization and de-escalation services, coordination with and referrals to health, social, other services and supports, and follow-up services as needed” to Vermonters of all ages.
DMH will consider “a range of staffing models,” though the RFP notes that “best practices include incorporating trained peers.”
A report on the Rutland pilot is due to arrive on legislators’ desks by Jan. 15. DMH sees mobile crisis services as one way to keep Vermonters with mental health needs out of emergency departments.
Blueprint for Health Expansion?
According to Senator Ginny Lyons, the presumptive chair of the Senate Committee on Health and Welfare, mobile crisis teams won’t be enough on their own to solve the problem.
Lyons praised the Vermont Blueprint for Health, a healthcare reform initiative that has supported several programs for “whole-person care” since 2006, calling it “a model for the country,” but said that it could do more for mental health.
“I’ve been in conversation with folks about expanding Blueprint to cover mental health,” she revealed, “so that we have in place comprehensive primary care for folks with mental health needs and make it as important as any other area of primary care.”
An upcoming report by the state’s Mental
Health Integration Council, also due by Jan. 15, could offer related recommendations.
Forensic Hospital Discussion
The intersection of criminal justice and mental health is likely to be a major topic among legislators. A Forensic Working Group studied the issue for a year and will soon issue a report of its own, but philosophical divisions appeared to prevent its members from arriving at a unified recommendation for how Vermont’s psychiatric facilities should deal with patients who’ve faced criminal charges.

“They didn’t provide any resolution to that issue. It just threw it back on our table,” Lyons said. Lyons anticipates working on a bill that would propose a forensic hospital – a locked facility that would treat arrestees deemed incompetent to stand trial or adjudicated not guilty by reason of insanity.
By Lyons’s account, it could also house some convicted criminals who have mental health needs. “The thinking is, well, we need to have something for people who have committed these crimes,” she said. “I don’t want to put them in Corrections, but how do we handle this? That continues to be a huge question. And so having a secure facility is the direction, I think, that some folks are going.”
“Right now, there are funds for a facility,” she added.
Urgent Care Options Are Underway
by BRETT YATES
BURLINGTON – The Department of Mental Health is actively looking to relieve Vermont’s overburdened emergency departments by expanding other options for care during mental health crises. There has not yet been any direct involvement by psychiatric survivors about specific criteria that should be included.
The Howard Center, Chittenden County’s community mental health center, has one idea. It has already been under development and a spokesperson said it would be seeking broader input, but not until its proposal is further along.
DMH issued a request for proposals for new urgent care services from qualified Medicaid providers in October. The document listed four potential models: a hospital-based “EmPATH” program (Emergency Psychiatric Assessment, Treatment & Healing); a “Living Room”-style crisis center with peer support; a “PUC” (Psychiatric Urgent Care) clinic; and a “CAHOOTS” (Crisis Assistance Health Out On The Streets) mobile response team.
There was no requirement for those who submit proposals in response to DMH to solicit input from the survivor community about their intended urgent care model.
Furthermore, the request for proposals appears to bypass the efforts of peer groups to develop peer respite programs that might provide crisis support options in similar ways.
Last year, the effort by four peer-affiliated organizations to propose that model failed to gain funding by the legislature. DMH said that the new programs described by the RFP were all based on a special federal funding opportunity, so they can only be developed by organizations that can receive Medicaid funds.
“Peer respites are not eligible for enhanced
funding because services are not billable to Medicaid,” DMH said. Peer support staff are not certified in Vermont, which is a barrier to that funding.
Howard Center Has Possible Plan
Before the RFP’s release, the Howard Center had already begun working to develop a plan for an urgent care clinic for mental health needs in Burlington. Initial conversations included potential partnerships with the University of Vermont Medical Center and the Community Health Center of Burlington.
According to Howard Center Chief Client Services Officer Catherine Simonson, it would operate much like an urgent care clinic for physical injuries and illnesses. “For instance, if you sprain your ankle,” Simonson said, “that doesn’t necessarily mean you have to go to the emergency department, but you need attention. You can’t wait till your doctor’s office opens up.”
The clinic would be open to the public, with no appointments needed, for about 12 hours a day. Clients would not be able to stay overnight, but Simonson envisions that those in need of additional stabilization would return the next day for a follow-up.
The Howard Center aims to find a communitybased site for the program in the vicinity of UVMMC, which would allow staff to easily refer patients to the emergency department if they meet criteria for hospitalization.
“Right now, for Howard Center, we don’t have a building set up such that there’s a lot of space for walk-ins,” Simonson observed.
The Howard Center already has a mobile response team for mental health emergencies, but Simonson believes that a brick-and-mortar clinic would provide a valuable supplement.
“It’s recognizing that many people in our community are choosing either not to wait for mobile outreach, or they want a place to go,” she said. “They don’t want somebody coming to their home or to wherever they are.”
DMH initially took part in discussions about the idea with the Howard Center and its partners but later assumed the role of a neutral party as it prepared to evaluate responses to the request for proposals. “Once an RFP is issued, they can’t be a part of any planning,” Simonson noted.
Pathways Vermont, Burlington’s peerled specialized service agency, joined later conversations. In Simonson’s vision, peers from Pathways and from the Howard Center’s own peer support team would join mental health clinicians, crisis workers, case managers, administrative staff, and a medical provider in a “multidisciplinary approach.”
“Our hope with the urgent care center is that it will be staffed such that people are not having to wait a long time to get their needs met and to be able to see somebody,” Simonson added.
Patients, she said, would enjoy a “calmer, trauma-informed” environment with “a little bit more personal space” than they’d find in an ED.
Simonson pledged that the Howard Center would solicit broader input on the plan upon securing a location and a contract with DMH. This would include consulting the Howard’s Center Community Advocacy Network Standing Committee and holding forums “for folks who identify as psychiatric survivors and other groups.”
“The fact that we haven’t done it yet is not so much not seeing the value in that, but feeling like we need to be further along, because there’s still a lot of work to be done,” Simonson explained.
DMH’s deadline for proposals was Nov. 14.
NEWS . 5 Fall 2018 NEWS Winter 2022 5
Conflict of Interest?
State Lags on Requirement To Divide Case Management from Services
By BRETT YATES
MONTPELIER – In 2014, the Centers for Medicare and Medicaid Services issued new regulations intended to protect Medicaid beneficiaries who receive care outside of institutional settings.
Vermont is still playing catch-up, which is frustrating advocates who have worried for years about a conflict of interest between agency case managers and the services their clients are eligible to receive.
A category of programs called “homeand community-based services” accounts for about $115 billion in annual Medicaid spending nationally.
In Vermont, under the administration of the Department of Mental Health and the Department of Disabilities, Aging, and Independent Living, they have five names: Choices for Care, Community Rehabilitation and Treatment, Developmental Disabilities Services Program, Intensive Home- and Community-Based Services, and Traumatic Brain Injury Program.
Through home- and community-based services, the state’s community mental health centers and specialized service agencies deliver care to Vermonters with psychiatric diagnoses and developmental and intellectual disabilities. But before they do, for each client, they perform an assessment of needs and design a plan to address them.
According to CMS, its new regulations require that part of the process to start taking place under a different roof. Under the updated rules, in order to avoid conflicts of interest, case managers cannot work for the same agency tasked with delivering the package of services that they’ve coordinated.

The federal regulators say that this revision relieves case managers of “possible pressure to steer the individual to their own organization.” They should instead offer clients “full freedom of choice of types of supports and services and individual providers” and be prepared to tackle “problems related to outcomes and quality,” which, as CMS points out, can be hard to do if the problems owe to “the performance of coworkers and colleagues within the same agency.”
This summer, CMS approved Vermont’s application for a five-year extension on its Global Commitment to Health waiver, the agreement that governs the state’s Medicaid program. In doing so, it conditioned that agreement upon Vermont’s willingness to enter compliance with its conflict-of-interest rules. Once CMS has okayed the state’s plan, it will appear within the waiver, on page 250, as Attachment Q.
So far, the page sits blank. Last December, the Vermont Agency of Human Services proposed a five-year transition to conflict-free case management, as it’s called, but CMS rejected it and demanded a three-year timeline.
It hasn’t yet approved Vermont’s hastened corrective action plan, originally scheduled to begin its stakeholder engagement phase this past September with the assembly of an advisory committee of “consumers, providers, families, guardians, advocates, and other groups.”
But the state has continued to get ready. In November, AHS executed a contract for technical assistance. A long process of analysis will precede the actual implementation of the
new system of case management, set to begin in 2025. A new stakeholder engagement plan is also being developed, and the process will begin after the plan is finalized, AHS indicated.
to tell them that,” she observed. Most states have already fully adopted conflict-free case management, but Vermont officials were initially reluctant to disentangle their “vertically integrated system,” as Murphy called it.
“We are by far the farthest behind,” she said. In her view, the creation of an “ombuds office” will be a key reform. The ombuds would investigate complaints by individuals who receive home- and community-based services.
An option the state could pursue to meet the federal requirements would be to contract with an organization to provide mandatory conflict-free case management throughout Vermont, or it could require each agency to find a third-party case management service of its own choosing.
The agencies themselves could provide reciprocal case management in one another’s geographic catchment areas, or some could transition exclusively to case management with others functioning exclusively as service providers.
Other states offer examples, but so far, no one knows what will happen here.
That has made some people nervous, including Rutland Mental Health Services CEO Dick Courcelle. “We’re still trying to understand what this really means because, in some cases, it makes no sense,” he opined.
Until recently, Vermont hoped to achieve conflict-of-interest compliance simply by offering Medicaid beneficiaries the option of receiving case management separately from the provision of their home- and community-based services, but CMS let the state know last year that simply providing clients with an option wasn’t good enough.
The Vermont Center for Independent Living has been a longtime advocate for a move to conflict-free case management.
“It’s about people truly understanding all their different choices, and I think that we have had a history in Vermont where people aren’t always given all the information,” said Sarah Launderville, VCIL’s executive director.
“It’s not like the federal government said, ‘Here’s a new rule we want to see.’ It was people with disabilities nationally coming together and saying, ‘We want to see this happen,’” she added.
Kirsten Murphy, the executive director of the Vermont Developmental Disabilities Council, also expressed support for the change to address the conflicts of interest that she said do exist in Vermont’s system of care.
“People don’t have to receive their services from their regionally designated agency, but sometimes they don’t learn about that because it’s not in the interest of their regional agency
“Consider you’re going to your doctor, and your doctor diagnoses you with type-two diabetes, but your doctor says, ‘I am diagnosing you with diabetes, and we need to manage that diabetes. However, I cannot be the one to do that, so I’m going to refer you to someone else for your care.’ That’s sort of what this is.”
By Courcelle’s judgment, the service provider is in a better position than a third party to design a plan of care because the service provider knows “what can be delivered, what’s available, and how to arrange those services.”
He also wondered where funding for case management contractors would come from and whether cash-strapped community mental health centers would suffer financially under the new arrangement.
“You’re dealing with a system that is fragile and has been fragile for many years due to chronic underfunding,” he commented. “My assumption is that this is a zero-sum game. If the money has to go somewhere, it’s going to have to come from somewhere.”
Courcelle pointed out that Vermont’s community mental health centers don’t operate on a fee-for-service basis, so they don’t have an incentive to load up clients with unnecessary services.
“But the federal government tends to like a one-size-fits-all approach,” he said.
Eating Disorders Treatment Input Sought
WATERBURY — The Department of Mental Health has announced that it is seeking public input on eating disorder treatment in Vermont.
An eating disorders work group, chaired by the department, is seeking comment from those who are struggling with eating disorders or those who have had problems in finding care for themselves or others. Suggestions are being solicited for improving treatment options, and input will be shared with state health care
providers, lawmakers, and school systems to help to build a better system of care, DMH said. Further information, is at mentalhealth.vermont. gov/about-us/boards-and-committees/eatingdisorders-workgroup
Those interested in sharing their experiences or recommendations can address them to: AHS.DMHCommunications@vermont.gov. All communications will remain confidential unless unless permission to use a name is provided.
NEWS 6 Fall 2018 NEWS 6 Winter 2022
“It’s about people truly understanding all their different choices, and I think that we have had a history in Vermont where people aren’t always given all the information.”
(by Jason Wong, Unsplash)
Town Says Plan To Replace Woodside Mislabels Youth Violence as a Disability
By BRETT YATES
WATERBURY – A growing preference for community-based care for justice-involved youth led the state to close the scandal-plagued Woodside Juvenile Rehabilitation Center in Essex more than two years ago.
Since then, the Agency of Human Services has struggled to find a new setting for juvenile offenders who are deemed to need a locked facility and mental health support.
“I’m as frustrated as you,” Secretary of Human Services Jenney Samuelson told lawmakers at a meeting of the Joint Legislative Justice Oversight Committee this fall.
A plan to open such a facility in the small town of Newbury has ended up in a legal debate as to whether the small but growing number of youths who have been alleged to have committed violent acts should be categorized as having a disability.
That category would bypass restrictions in a town’s zoning laws, but the town has declared its opposition to what it has called “the notion that any juvenile who commits a crime is, by default, mentally disabled.”
The case has ended up in Environmental Court, which found that the program did qualify as a group home for persons with disabilities. The town declared that it would file an appeal.
Since 2020, Vermont has sent children charged with delinquent or criminal acts across state lines to the Sununu Youth Center, but amid indictments against staff for physical and sexual abuse, the New Hampshire legislature ordered its closure in 2023.
A recent VTDigger report revealed that nine minors have spent time in Vermont’s adult jails.
Last year, Newbury’s land use authority rejected an application by a state-contracted nonprofit for the construction of a “residential treatment facility” with six beds for justiceinvolved adolescents on the outskirts of the village of Wells River.
The local zoning dispute has drawn into question the nature of the proposed program in Newbury and appears to have revealed the need for an additional facility elsewhere to fulfill the former’s original purpose: to replace Woodside.
Since 1984, the state’s Department for Children and Families, which is under the Agency of Human Services, had operated Woodside as a juvenile detention center. In 2011, the state added psychiatrists to the staff and, partly in order to draw federal funding through Medicaid, relabeled it a treatment facility.
In 2016, the Centers for Medicare and Medicaid Services rejected the reclassification, deeming Woodside’s so-called patients to be “inmates” instead, meaning the program was not eligible for federal funds.
In 2020, the legislature instructed AHS to submit “a long-term plan for Vermont youths
who are in the custody of [the state], are adjudicated or charged with a delinquent or criminal act, and who require secure placement.”
It called for a “physically secure” program with a “no eject/no reject” policy, meaning any
maintaining a clear distinction between mental health treatment and criminal detention.

Conflating them “doesn’t help the situation at all,” he commented. “That’s a bad mix.”
Jessica Kell, the director of the Child, Youth and Family Services Division at Washington County Mental Health Services, criticized a “fragmented” system that, for reasons of zoning or funding, requires children to demonstrate that they fulfill specific criteria before they can receive care.
“These kids need help, and there is no way of getting it when we can’t agree on who is responsible for it,” Kell said.
The starting point should not be to “define by law what they need,” but instead, for a clinical process of diagnosing what is needed to get underway even as the help is occurring.
child in need of the program had to be admitted.
A property was identified in Newbury, to be operated by Becket, a New Hampshire-based nonprofit.
State law requires a “residential care home or group home” which serves eight or fewer “persons with a disability” to be considered in the same way as a single-family home for zoning purposes.
The Newbury Development Review Board ruled that, as a proposed replacement for Woodside, it was not a residential care home or group home, but rather a “high-security detention facility,” just as CMS had determined regarding Woodside.
The board cited plans for a 12-foot fence and 24-hour infrared video cameras throughout the site. The board then rejected the application under its zoning bylaws.
The Environmental Court sided with the state, saying that “DCF anticipates the individuals who will be served at the facility to have disabilities or disorders (mental, social-emotional, developmental, etc.) or need assessments for such based on their behaviors and needs at time of presentation.”
The court noted testimony of the operator’s intention to transfer youths who do not meet the criteria for a “mental health disability” to a “more appropriate treatment setting” following such assessments.
Declaring their intention to file an appeal, municipal officials emphasized what they still regarded as the project’s primary aim as a lock-up: “It’s clear that the proposed facility is a detention center first and any mental health services they offer are secondary.”
In an interview with Counterpoint, Vermont Psychiatric Survivors Executive Director Karim Chapman stressed the importance of
Kell said that isn’t a quick process or just a matter of an assessment at an intake – it needs to happen by allowing the professionals who are licensed by the state to be given the space to do their jobs.
Disability Rights Vermont Executive Director Lindsey Owen has also followed the saga in Newbury.
“I would like to be able to take the state for its word that, if somebody goes to that program and does not have a diagnosis that would be appropriate for that setting, they would find an alternative and appropriate placement for that child,” she said.
“I think Disability Rights Vermont’s position is really not so much the legal status of the kids that are there,” Owen continued, “but really just making sure that those children are being served in the best way possible and in a therapeutic setting.”
To Owen, the biggest impediment is the location. “The grocery stores are at least 20 minutes away,” she described. “If the goal in the long run is to successfully rehabilitate and reintegrate these children into communities, it’s questionable how that’s going to happen in such an isolated rural environment.”
At the Oct. 25 meeting of the Joint Legislative Justice Committee, Samuelson said that placement in Newbury would depend upon a clinical determination of eligibility for care. “The provider makes the decisions about who is admitted,” she said.
That would leave unmet the need for the program that was originally described as required to replace Woodside: one that must admit and hold any juvenile deemed in need of a locked facility. According to AHS, the solution will take place in two steps: the establishment of a short-term detention center, followed by the development of a long-term one.
Samuelson pledged to return to the committee at its December 12 meeting with more information.
Peer Workforce Training Sessions Offered
Vermont’s Peer Workforce Development Initiative has announced several upcoming free training opportunities. For more information on any of these three, including how to register, contact training@ pathwaysvermont.org
Intentional Peer Support Core Training will be starting Monday, January 23 via Zoom on Mondays and Wednesdays for 10 half days. There is a $100 fee for IPS Core materials.
Mad Movement Histories will be April 4 and 6, 12:30 - 4:30 p.m. each day. It will explore mad movement histories through themes of
resistance to oppression and building alternative supports, and through lenses of racial, disability, economic, and gender justice.
Harm Reduction Approach to Psychiatric Drugs will be May 2 and 4, 12:30 - 4:30 p.m. each day. “As peer support workers, we are sometimes discouraged from having conversations about psychiatric drugs and are encouraged to leave it to the medical professionals. This two-day participatory workshop introduces a model for thinking about psych drugs as neither good nor bad, but as chemicals that can have benefits and also come with risks,” PWDI said.
NEWS . 7 Fall 2018 NEWS Winter 2022
(AdobeStock)
Telepsych May Expand in EDs
By BRETT YATES
A one-year federally funded project aims to help expand telehealth-based psychiatric assessments to emergency departments across the state.
Thanks to an earmark secured by Senator Patrick Leahy, the Substance Abuse and Mental Health Services Administration sent $901,123 in congressionally directed spending to the Vermont Program for Quality in Healthcare in September. VPQHC, a nonprofit established by the state legislature, will build what’s it calling a Vermont Emergency Telepsychiatry Network to support coordination among hospitals, prepare medical and administrative staff, look for ways to access long-term funding, and evaluate outcomes.
“The problem we’re trying to solve is that Vermonters, adults and youth and children, are waiting a long time in emergency departments. They’re having mental health and psychiatric needs that are unmet,” said Quality Improvement Specialist Ali Johnson, the project lead.
Earlier this year, with the help of the Northeast Telehealth Resource Center, VPQHC used a philanthropic donation to research existing emergency telepsychiatry practices in Vermont’s hospitals.
“We found that some of them had it, and some of them didn’t,” Johnson recounted. “The ones who didn’t, some of them don’t want it; some of them do want it.”
During VPQHC’s needs assessment, the organization reached out to “all kinds of stakeholders,” as Johnson put it, including Vermont Psychiatric Survivors, with the intention, ultimately, of assembling an advisory board. The board, once it comes together, will meet monthly to make recommendations over the course of the project.
“There will be some psychiatrists on that board. We also will include people from governmental agencies like the Department of Mental Health and Medicaid. We will include, hopefully, people with lived experience,” Johnson said. “People who are receiving services are one of the key sectors of this coalition we’re trying to build.”
She also cited an expected board seat for Disability Rights Vermont. VPQHC may “look into stipends” to promote participation.
Johnson described emergency telepsychiatry as a “consentbased” service. The choice to wait for an assessment by an in-person provider will remain available for both voluntary and involuntary patients, she said. Telepsychiatry has expanded globally since the start of the COVID-19 pandemic. Increased need and workforce shortages, especially acute in rural areas, both appear to have played a role.

“There is some good evidence that telepsychiatry can be effective in working with people,” observed Kevin Martone, board president of the National Association for Rural Mental Health. “But you don’t just want to default to it as a cost-saving measure.”
Martone noted that emergency departments that replace in-person physicians with
best environment that they can,” Martone said.
Johnson said that, “We’re hoping to learn best practice from the hospitals that already do this, turn that into training for the newcomers to telepsychiatry, and also buy equipment and services for hospitals that might already have telepsychiatry in place or are trying to build it.”
Trainings will cover big-picture topics such as, in Johnson’s words, “Is this evidence-based? Is this a good idea?” in addition to nuts-and-bolts details related to electronic health records and insurance. Other sessions will focus on “traumainformed care and thinking about Englishlanguage learners and people with disabilities.”
Among the hospitals that don’t already have telepsychiatry, VPQHC will pick two – a “midsize hospital” and a smaller “critical access hospital,” both yet to be named – for “demonstration projects.” A portion of the SAMSHA funding will pay for these institutions to hire emergency telepsychiatry vendors vetted by the Northeast Telehealth Resource Center.
telepsychiatrists will have to rely on the rest of their staff – including social workers, peer supporters, and nurses – to provide a stabilizing human presence for patients in crisis. “If the clinical assessment to make a determination about inpatient care needs to be done by a psychiatrist and they don’t have that and they need to consult with someone [virtually], the other folks on that team need to really be trained on engagement and be warm and welcoming and all of those things to try to create at least the
According to Johnson, the “midsize hospital” intends to contract a Vermont-based treatment center that specializes in children and adolescent psychiatry. The other contract could go to an instate or out-of-state vendor.
“We’ve modeled our project on some work that’s been really great in North Carolina, and one of the ways they show their impact is in overturned involuntary commitments. And telepsychiatry is used in that process,” Johnson added.
Peer Certification Efforts Continue
By BRETT YATES
After a bill that would have created a statewide certification program for peer support workers in Vermont failed in the legislature last spring, advocates continued to pursue the idea.
“When they kind of shut it down, the peer movement, in their own way, went back to the drawing board: OK, we’ve got to come at it a different way. Let’s try to redefine what we’re trying to say,” Vermont Psychiatric Survivors Executive Director Karim Chapman said.
Vermont is one of only four states that does not have a mental health peer certification process.
The Department of Mental Health issued a $30,000 grant to Pathways Vermont, which operates the state’s Peer Workforce Development Initiative, to pay for a series of meetings that would seek to resolve “key issues and risks” associated with peer certification by soliciting stakeholder input. Pathways subcontracted Wilda L. White Consulting, a firm owned and operated by the founder of the nonprofit MadFreedom.
Over the course of six Zoom sessions hosted
by White this fall, peers and others discussed various potential forms of certification and certifying bodies, eligibility requirements and training focuses, as well as how the mental health continuum of care would incorporate certified peers. After each session, White distributed a survey to gather more detail from participants. DMH will review responses.
“Part of my job here is to submit a report,” White explained at the final meeting. “And in that report, it should contain a recommended design of a statewide peer support worker certification program, include a summary of items that need resolution, and then create a work plan of what are the next steps and how will we get that done.”
She explained that phase two of the process will be “convening a smaller group, still with broad stakeholder representation, to finalize where we go from here, so we can move into certification and move into implementation of a certification program.”
DMH intends to make use of this work, according to Director of Policy Nicole DiStasio.
“The Department expects to have a
recommendation from the stakeholder workgroup that will inform the next steps for this critical work,” she said.
Last spring, after the legislature had stripped the funding from the peer certification bill drafted by Vermont’s peer-led organizations, those same organizations sent a letter to ask lawmakers to allow them to “work cooperatively with DMH to develop and implement a statewide peer certification program outside of the legislative process.”
But Vermont’s precise path to peer certification, if it happens, is not yet certain. Senator Ginny Lyons, the presumptive chair of the Senate Committee on Health and Welfare, mentioned her awareness of ongoing discussions involving the Office of Professional Regulation and the Secretary of State’s office as well as DMH and peers.
“Do we need to do anything legislatively, except maybe rubber-stamp what’s happened or make some tweaks to what they’re proposing?” Lyons wondered. ““I will be catching up with that. I would like to bring them into committee and have that conversation.”
NEWS . 8 Fall 2018 NEWS Winter 2022 8
(AbobeStock)
The pilot program for telehealth services for those in a psychiatric crisis will be “consent-based,” the organization said.
Group Joins Battle for Parity
‘Inseparable’ Seeks Recognition of Mind-Body Interconnection
By ANNE DONAHUE
PORTLAND, OR – A new, national organization has been formed with a stated purpose to press state and federal policymakers to recognize that “health of the body is inseparable from health of the mind.”
The organization – named Inseparable – was founded in 2020 with the purpose of “creating a movement” to demand and win policy changes that improve care for all Americans, according to Angela Kimball, Senior Vice President of Advocacy and Public Policy.
‘Lived Experience’
Kimball said in an interview that its leadership includes psychiatric survivors along with family members of people labeled with mental illness and mental health professionals.
Kimball cited the organization’s Vice President of Partnership, Keris Myrick, as evidence of its commitment to keep its mission “grounded in people with lived experience.”
Myrick’s background as a psychiatric survivor includes serving on the board of the National Association of Peer Supporters and as a CoEditor of the Journal of Psychiatric Services “Lived Experience and Leadership” column. She was also a past director of the Office of Consumer Affairs for the Substance Abuse and Mental Health Services Administration.
Initiative with Legislators
Kimball said while hosting a booth at this year’s annual convention of the National Council of State Legislators, staff from Inseparable discovered an “upswell of interest” among legislators about addressing mental health challenges in their states.
“They were hungry for resources,” she said.
As a result, Inseparable began a new initiative this fall to develop a coalition of legislators across state lines and across political parties to help advance the states’ mental health priorities.
The founder and president, Bill Smith, has a career in campaign management, messaging research and communications, and movement
building and lead national efforts on marriage equality. It was the loss of a family member to suicide that led Smith to create Inseparable, Kimball said. The organization is taking “an issue-oriented campaign approach” to its efforts, and is not trying to replicate others who do broad based advocacy, she said.
Organizational Priorities
The Inseparable web site identifies its three immediate priorities for policy action as:
1. Eliminate the gap between the number of people who need help and the people who get help.
2. Ensure every school has services to provide for the health and well-being of all students.
3. Stop criminalizing mental illness and expand crisis response.
The web site stresses the universality of mental health issues, and says it “fights for a future where mental health policy, no longer an
911 can too often turn a crisis into tragedy like in the Daniel Prude case.” Prude died after being physically restrained by Rochester, New York police officers while experiencing a mental health crisis in 2020.
“We’ve been focusing the conversation on how to really build a fully equipped crisis response system, but we’re still worried about it because the system’s not fully ready for it,” Smith said in a blog post.
“The conversation has really been around the three-digit number [988], not around the full crisis response system,” he said.
Focus on Parity
In terms of parity, the organization says on its web site that federal legislation for equal health coverage “was never properly enforced, as states are responsible for their own implementation.”
As a result, it “has left too many without the care they’re entitled to... Closing the treatment gap and increasing access to care includes addressing affordability, expanding insurance coverage, integrating mental health into primary care, and building a much bigger, culturally and linguistically competent
bodies. Each affects the other — just like us. Together, we are inseparable.”
The organization’s web site says that it can “feel overwhelming to experience the broken pieces of our system and frustrating to not see this crisis prioritized by our elected officials.
“The shared trauma brought on by the pandemic, a national reckoning around systemic racism, the threats of the climate crisis, and our broken approach to mental health have all laid bare the need for change.”
View on Crisis System
Inseparable’s priority on ending the criminalization of mental illness includes “working with mental health and criminal justice reform advocates to build and expand a robust crisis response system that prioritizes health and well-being,” it says, “because calling
RESEARCH REVIEWS IMPACTS OF BIAS
Two new reports have discussed the impact of bias on health equity and on research.
The first study, reported on in the Key Update from the Mental Health Consumer’s Self-Help Clearinghouse, is titled The Economic Burden of Mental Health Inequities in the United States.
“For the first time,” Daniel E. Dawes JD, was quoted as saying, “there is tangible evidence demonstrating how decades of systemic health inequities have yielded significantly worse outcomes for racial and ethnic minoritized, marginalized, and under-resourced populations.” In the study, the Satcher Health Leadership Institute reported on a four-year period (2016-2020) when, at minimum, nearly
117,000 lives and approximately $278 billion could have been saved. The free, 62-page study is available for download at satcherinstitute. org/research/ebmhi/
In a second recent report, The University of Vermont’s fall magazine summarized research that says the new scientific field measuring nature’s effect on human well being has “a diversity problem that threatens its ability to make universal scientific claims.”
The report is titled, “Nature Helps Mental Health, Research Says – but Only for Rich, White People?” The field in psychology and environmental science “has produced numerous important studies detailing the benefits of
The web site lists the organization’s values as: Caring – We can better care for each other by demanding a mental health policy that better cares for us.
Unity – The health of our minds cannot be separated from the health of our bodies, and we cannot be separated from each other on this issue.
Progress – We are moved by our hearts, but act with our minds, deploying skill, strategy, and innovative tactics to ensure we don’t just fight, but win.
Power – Together, we have the power to lift each other up. Together, we are a force. A force for help. A force for hope. A force for healing.
Relentless Hope – We harness our hurting for healing, to fight for a world we believe is possible: one with the mental health support we all need to thrive.
nature, forests and parks on human wellbeing and mental health, including happiness, depression and anxiety,” the article said.
But analysis of the research by UVM found that study participants were overwhelmingly white and that BIPOC communities were strongly underrepresented.
“This narrow sample of humanity makes it difficult for the field to credibly make universal scientific claims,” the magazine said that the UVM researchers reported.
The impact of research that discriminates has been one of the issues that gained public awareness after COVID, which impacted the BIPOC community more severely.
Fall 2018 NEWS . 9 Winter 2022
(AbobeStock)
by SARAH ROBINSON
by ADAM FORGUITES
by RAGHAD AMJED
by VESNA DYE
by LUKE CARLSON
Artists Wow Burlington in 2 Exhibitions
 By BRETT YATES
By BRETT YATES
Does anyone write old-fashioned letters anymore? In front of the Howard Center at 300 Flynn Avenue in Burlington, a collection of 13 decorated mailboxes pays tribute to the history of the United States Postal Service and to the human bonds forged over centuries by handwritten communication.
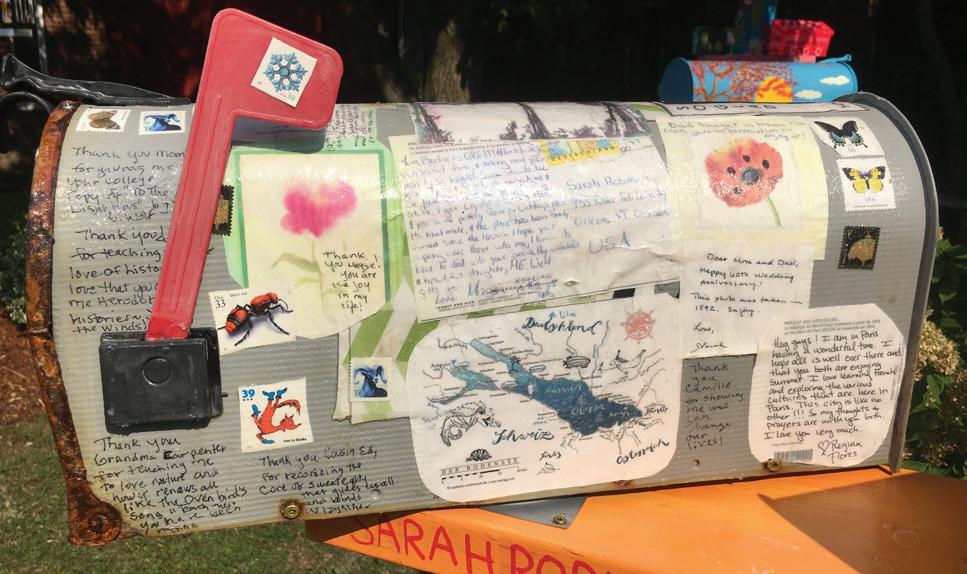
The outdoor installation, titled Connections, opened to the public on Sept. 10 during Burlington’s South End Art Hop, an annual three-day festival, with members of the Howard Center Arts Collective uncovering their veiled works one by one before a crowd.

It was one of two major fall events for the arts program. Call and Response is an exhibition hosted by the Fleming Museum. (See article below.)
The Arts Collective describes itself as “an alternative arts program for people who have lived experience with mental health and/ or substance use challenges” and includes Howard Center clients, staffers, and unaffiliated community members.
“Our mission is really to create opportunities
to make art together, to share our art with one another and learn from one another – and then also to exhibit our work to the community,” Arts Collective Coordinator Kara Greenblott said. Connections casts a skeptical eye upon the dominance of email, Facebook, and Twitter today. An introductory statement by artist Sarah Robinson, read aloud at the opening, criticized the “fractured” thought processes of the internet era and the “reduced services” and slowed delivery times at USPS.
According to Eryn Sheehan, the group’s studio manager, the project that would become Connections began in 2020, when the Arts Collective started to solicit donations of old mailboxes. “We posted on Front Porch Forum and different places around town. And then we’ve been painting them and working on this exact project since spring,” she recounted.

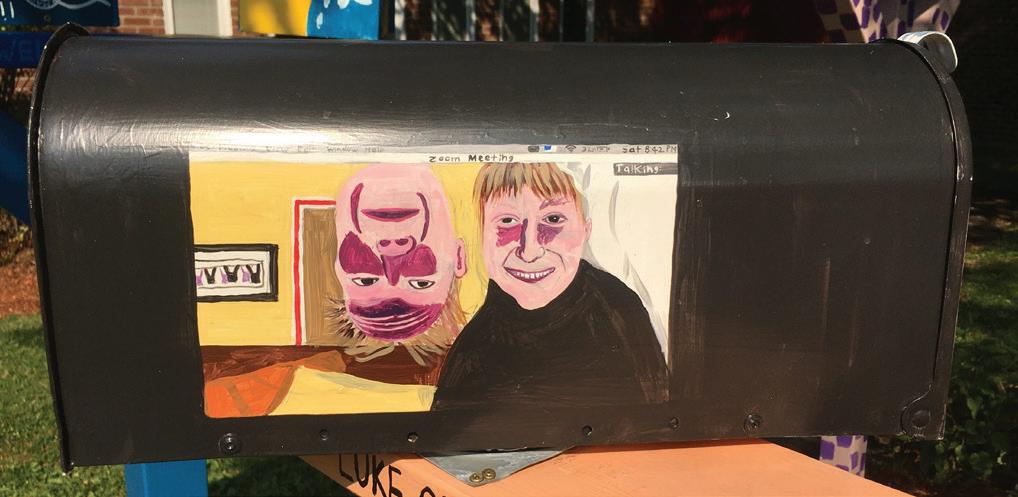
Each mailbox sits on a six-foot post, sunk into concrete. Sheehan expects the installation to withstand Vermont’s winter weather and to last for one and a half to two years in the Howard’s meditation garden. The painted mailboxes display both abstract and figurative designs.


Sheehan, who joined the Arts Collective four and a half years ago as a Howard Center client, pointed to the “little musical symbols” on her mailbox, noting that she had drawn inspiration from what she called “the music of the spheres” – the sounds that she can hear “coming from trees and different celestial bodies.”
A newer member, Vesna Dye, joined the collective after hearing about Connections at Pathways Vermont. “I’m not much of an artist, but I said I’ll do it because I love the post office, and I’m writing hundreds of letters everywhere in the world,” she explained. Dye borrowed her mailbox design from a “thinking of you” card that she received shortly after signing up for the project. Raised in Croatia, Dye lived in Canada and California before moving to Vermont and, by her account, relies on letters, cards, and packages to stay close to family members and friends.
“I only write short emails,” Dye related. “The letters are, I think, much more personal. They’re much more creative – you can say more. I have this nice paper that I like to get, and then a nice card, and I’m hoping people are saving this.”
Second Project Debuts at Fleming Museum
By BRETT YATES
BURLINGTON – A temporary exhibition at the University of Vermont’s Fleming Museum of Art dives deep into its archives and comes up with something new. Call and Response: Personal Reflections on the Fleming Collection
opened on Sept. 13 and features 16 members of the Howard Center Arts Collective. Call and Response found inspiration in paintings and objects as old as the 17th century. Each new work reshapes an artistic vision from the past.

Manager of Collections and Exhibitions Margaret Tamulonis pointed out that the Fleming’s first director, Henry Perkins, was a leaders in eugenics in the early 1900’s. Eugenics supported sterilization of people who were deemed unfit to have children, including those with psychiatric disabilities. She described the show as part of an ongoing process of “examining and reckoning” with the museum’s historically exclusionary practices.
Curator of Education and Public Programs Alice Boone noted the impact that the show had already had upon visitors. “I brought the psychiatry medical students into this space, and [it] was so affecting for them that the professor who I work with actually brought his entire department back, and we spent about an hour and a half talking in that space,” she told the artists at an opening reception. “What they all came to was this sense that they were really transformed by
NEWS 10 Fall 2018 The Arts 10 Winter 2022
Saint Man of Peace (2022) by AMJED JUMAA
seeing your art and really transformed into thinking about the ways that they need to do their work differently.”
(2022)
Progression
of Modern Medicine
by THOMAS G. STETSON
Founding Director To Step Down
By BRETT YATES
ROCHESTER – The peer-run respite Alyssum announced this summer that after 11 years, the organization’s founding director, Gloria van den Berg, had made plans to step down.

Alyssum held an open house at its homelike, rural property in the White River Valley on Sept. 16. Former guests, employees, peer leaders, and state officials gathered to celebrate van den Berg’s accomplishments with live music, lunch, and a bonfire.
Alyssum’s two crisis beds, funded by the Vermont Department of Mental Health, have offered a voluntary, non-clinical alternative to psychiatric hospitalization since 2011, when it became the state’s first (and, to date, only) peer-run respite. According to a directory maintained by the National Empowerment Center, such facilities exist in only 13 states.
“She’s just been a tremendous asset to Vermont,” DMH Adult Services Director Patricia Singer said of van den Berg. “Alyssum models a tremendous peer support model. I think it shows how good respite care can really be beneficial to people who are in distress.”

Van den Berg noted that as far back as 2019, she’d formulated a “five-year plan” for “stepping away from mental health.” Since then, “a lot of things happened” in her personal life.
“My daughter had cancer. We had Covid. My sons all moved back home,” she recounted. “And I found myself having a really hard time with cold weather, probably as a result of my age. And so, in the big Covid transition, you have to make sense out of this somehow. I wound up purchasing a house in Florida.”
Van den Berg’s sons will inherit the working farm that she operated for three decades on a hillside down the road from Alyssum. She has given up full-time Vermont residency, following a switch to telework during the pandemic. An earlier transition to “collaborative management” at Alyssum had already reduced her on-premises role.
“It happened when our house manager left about three years ago. We decided not to hire another house manager and to sort of distribute the house manager’s responsibilities amongst staff,” she remembered. “It’s a very well thoughtout structure that we operate under. The great benefit of where Alyssum is at now is that the staff can collaboratively manage the day-to-day program.”
From Florida, van den Berg continues to oversee Alyssum’s budget and financial reporting, to apply for grants (most recently, for a new kitchen), and to participate in Vermont’s “statewide stuff,” like the ongoing effort to design a peer certification program.

She expects her exit to take place “within the time frame, probably, that I was thinking of.”
“The board really felt that they wanted a director who was in residence in the state,” she observed. “I would be remote eight, nine months out of the year. They want something more
than that. So, it was kind of a push-me-pull-me situation with the board.”
As of September, Alyssum’s board of directors hadn’t yet initiated a formal search for van den Berg’s replacement. No one knows exactly how long it will take once it begins.
According to longtime board member Marty Roberts, who had scheduled her own retirement for Oct. 1 this year, the position could possibly become a part-time role, leaving “more funding for the staff.”
Before Alyssum’s founding, Roberts joined a working group assembled by Vermont Psychiatric Survivors and tasked by DMH to help replace services at the Vermont State Hospital, then still operational, by creating a peer-run program.
This effort led to the creation of a 501(c)(3), and Roberts became part of the board that hired van den Berg.
“It was one of those things that was just no question,” Roberts recollected. “To me, she stood out particularly for her personal qualities, for her passion. She had a lot of background of lived experience, which we really wanted. We wanted somebody who understood what it was like to be in a crisis sort of situation.”
“She had some administrative experience, but we were actually really looking for someone to develop a program, which is what she did. There wasn’t any program to start with. She worked all that out, did all kinds of training, and hired people.
“And she even found the building,” Roberts added. “She was clerking for a
lawyer who lived in this house back here and was wanting to sell her house and move away. So, she kind of facilitated that.”
For Alyssum’s staff, van den Berg won’t be an easy act to follow.
“She’s a team leader, but she’s also a team member,” said Niclas Thein, a peer supporter. “Technically, she’s the boss. But she has a way to not be bossy but get her vision established by just suggesting, having this gentle way of, ‘Hey, let’s do it this way.’
“We all have input, but somehow Gloria was able to really put her vision into and create this reality here.”
“We feel a little bit in limbo of not knowing what’s gonna happen, who may take over,” said Serenity Lohr, who’s worked at Alyssum for five years.
“A lot of it’s going to come down to finding the right person that can fit in and let us basically take the lead in showing them what we do and how to do it. So, it’s going to take a very special person.”
Another staffer, Jenniflower, first experienced Alyssum as a guest. Meeting van dan Berg, she recalled, was “life-changing.”
“She’s got radical perspectives, which is what we do here,” Jenniflower said. “It’s really about thinking and experiencing and feeling and making decisions for yourself.”
Other former guests shared similar sentiments. Colchester resident Heather Smith first visited four years ago and has returned on multiple occasions.
“This was the first time that I didn’t feel alone in the world,” she described. “It’s where I learned that I could live outside of my symptoms and my diagnosis.”
She praised Alyssum’s selfdirected program, which gave her time during her stays to paint, garden, do puzzles, and take field trips. And she especially credited the healing effect of a particular meditation technique shared by van den Berg.

“I took that with me. I use that all the time,” she said. “My hope always, when I come here, is that I can take more of Alyssum home with me and create that at home.”
Earlier this year, an unsuccessful proposal to create additional peer-run respites, in the model of Alyssum, came before the legislature.
Van den berg believes that Vermont could use more peer-run respites, but she pointed out that new facilities, if they’re established, will likely differ in some ways from the program she developed.
“The executive director makes the flavor of the respite,” she said. “And depending on where you put it, it takes on different parts of a community.”
She attributed the particular culture of Alyssum in large part to her “background in Buddhism and spiritual stuff.”
“It’s unique to this place,” she continued. “And it’s unique to the staff that are here. It doesn’t make it better. It’s worked for us.”
NEWS . 11 Winter 2022
Photos by Brett Yates
Serenity Lohr
Jenniflower
Heather Smith
Gloria van den Berg, Alyssum’s founding director, stands in the yard with its mountains behind.
Deconstructing Stigma
In 2021, Burlington International Airport hosted a pop-up installation of “Deconstructing Stigma: Changing Attitudes About Mental Health,” a series of larger-than-life photographs of people who have been affected by mental illness and who volunteered for the project. The project was developed by McLean Hospital in Massachusetts and has traveled the world. The project’s website explains, “Each story is told through the eyes of the campaign’s participants as they boldly tear down the misconceptions of mental health. Not statistics or nameless faces, the volunteers in this project are everyday people.” Counterpoint is reprinting some of the vignettes from the project to memorialize Vermont’s display. Excerpts from participant stories are also included.
Lexi
It felt like I had a big hole in my chest.
Persephone
I often fall through the cracks.
Someone I worked with posted on social media that all of these mass shooters are mentally ill, that you have to be mentally ill to do that. For me, that feels like a huge stigma and putting somebody in a box. And yes,
I have mental illness, but I am more of a harm to myself than I would be to anyone else.
Persephone experiences epilepsy, autism, attention-deficit/hyperactivity disorder, obsessive compulsive disorder, post-traumatic stress disorder, anxiety, and depression. In her attempts to find help, she has been frustrated by society, law enforcement, and the medical community.
I am afraid of asking for help from the police. Any time I call for help or say I’m suicidal, three to four police officers will show up. I have to be escorted by the police instead of having maybe the EMTs come down to me. Where I was living, rumors were getting spread about me.
Persephone says that sometimes health care providers can’t differentiate her disability from her mental illness—or they have a lack of experience with autism.

I am more than my mental illness. I am an artist. I feel there needs to be a change. I try to voice it by talking with my friends, going on social media, creating artwork. I like to consider myself a freelance advocate— advocating wherever and whenever I feel there’s a need for it.
Jodi
Jodi recalls the time when she first experienced auditory hallucinations — and how she hid from the fact she might have a mental illness.
It began when I started working as a teacher...As I was working, I saw abuse and neglect of the children, and it was the first trigger to my auditory hallucinations. I tried to make the voices, the noise in my head, go away. They didn’t go away, and by hiding, I was more vulnerable and quickly had a breakdown and ended up in the hospital.
Jodi was diagnosed with anxiety, post-traumatic stress disorder (PTSD), and bipolar disorder in her late teens, and she attempted suicide at age 17.
The mental health system has never given up on me. Countless case managers, psychiatrists, therapists, and day program staff have believed in my ability to heal. People have been listening and helping me over these last 30 years.
Perseverance and the power of sharing her story has helped her find a path to recovery.

I think the greatest help has been finding my voice to share my trauma, to empower myself to share my struggles. I’ve found that the more that I share with others, the more that I tell my story, the more I am empowering myself. I am able to stand taller, be more confident, and perhaps help others no longer hide.
By speaking out, Jodi wants “to encourage those who are fearful to take one day at a time.” She recommends that people share their “hard reality” with caregivers and family.
Begin with one moment, one emotion that makes you feel a certain way. Let the others in your life relate to you.
When Lexi was 14, she began to experience severe paranoia in which she hesitated to stray far from home or from a medical facility.
I had this one specific fear of not being able to breathe or that my throat would suddenly seal up.
When she looks back on those years, Lexi, now 21, recalls she didn’t feel complete. She fantasized about suicide.
It was almost a comforting thought, in a sense, like I could get out of all this if I needed to when things became too much.
[A hospitalization] was the first step on a path of recovery. Six hospitalizations and 20 medications later, Lexi feels she has the correct diagnosis and is receiving the right treatment.
People should keep in mind that I’m just a really regular person. I have the same exact emotions as anybody else, even if they express differently.
Lexi can be hard on herself too.
There’s a lot of judgment we put on ourselves, regardless of whether we have a mental illness or not. I want to be able to juggle a lot of different things in my life because that’s what I’ve always seen other people do. Since I ended up in the hospital, I realized I can’t take on as much as I once did: It was frustrating. Now, I’m a little better about telling myself, ‘You’re doing what’s good for your health right now. That’s just how it needs to be, and there’s nothing wrong with that.’
Lexi now works as a recovery support specialist in a residential mental health facility. She loves her job and is now studying to become a psychiatric nurse.

Tian
People should be seen as people and not as a set of symptoms.
Tian has been diagnosed with major depressive disorder, generalized anxiety disorder, an eating disorder, and obsessive compulsive disorder. She does not, however, want to be defined by her diagnoses. When I was in the hospital, someone would check in with me every day and ask me how I was feeling, ask about my urges.... I began to feel like the only parts of me that mattered were the ones that I didn’t want — the parts that were depressed and anxious.
Based on this experience, Tian has become a proponent of person-first language.
My narrative didn’t really change, but the simple change in wording made me feel more confident in myself and more compassionate.
Tian’s experience in the mental health system has also inspired her to make another change — to embrace the concept of community. Although she says that inpatient treatment was critical for her, it didn’t address “what was actually missing in my world — community.”
I strongly believe in community, and even though treatment is what got me out of the hospital and back into the ‘real’ world, my community is what allows me to stay, experience, and grow in it.

The Arts 12 Winter 2022
Jen
Seeking help saved my life.
Jen’s experience is a testament to the importance of getting help for mental health issues — and to the power of trusting oneself and telling the truth.
I was first diagnosed with depression in my 20s.
I found a therapist, spilled the whole story, and then proceeded to sit on her couch in almost absolute silence for many sessions. I’m grateful to her. She helped me navigate my conflicted feelings over a journey that took years.
Jen kept up with therapy for many years, but when she “bottomed out” in her late 40s, she knew she needed a higher level of care. She took part in an outpatient CBT program that required her to miss six weeks of work.


I was ashamed, and I was convinced that I would have nothing in common with the other patients, but it was wonderful. There was much about the world of emotion that I had never learned, and the program demystified some of my thoughts and reactions in an amazing and supportive environment. You just don’t know what you don’t know.
Now remarried, Jen is the mother of two college-aged children. She loves running, writing and reading, hiking, skiing, and kayaking. She works as a teacher, and she is open about her mental health struggles, hoping to serve as a role model for her students and others who may be reluctant to confront mental health issues.
People will understand eventually. As they grow, your desire to be healthy will make more sense to them. You may become their role model. And if they don’t understand, well, that’s their issue and certainly not worth staying sick or dying for.
Linda
Mental illness was a part of her. It was not all of her.
When Linda was growing up, she’d walk home from school and know when she wouldn’t see her mom for a few days. She’d look at her mom’s bedroom window.
If the shade was down, it meant she was in bed.
Linda’s mom, Fannette, who had bipolar disorder (back then, known as manic-depressive illness) would take to her room to be alone. Only the doctor was allowed to come in to give her “an injection to take away the pain.”
Ashley
He didn’t know how good he was.
Ashley believes the only time her older brother Ian was truly free was when he was in his race car.
That’s why he had five track records and dozens of trophies and checkered flags. He got in that car, where nothing was causing him pain. He didn’t know how good he was — not just good on the track, but good as a human — and what hurts me more than anything was that he never let anyone know how deeply he was suffering on the inside.
When Ian took his life in 2016, his death changed Ashley’s perceptions about suicide. She had thought suicide was for people with blatant problems that everyone should have noticed. She also had thought suicide was selfish.
Ian was the least selfish person on the planet. I learned immediately when he died that suicide has nothing to do with being selfish; it’s about being desperate, and Ian was desperate.
To honor Ian, Ashley has devoted her energy to suicide prevention and mental health awareness. She gives talks in her community in northern Vermont, campaigns for the American Foundation for Suicide Prevention, and recently became certified as a trainer for the Vermont Suicide Prevention Center’s (VTSPC) Umatter® program.
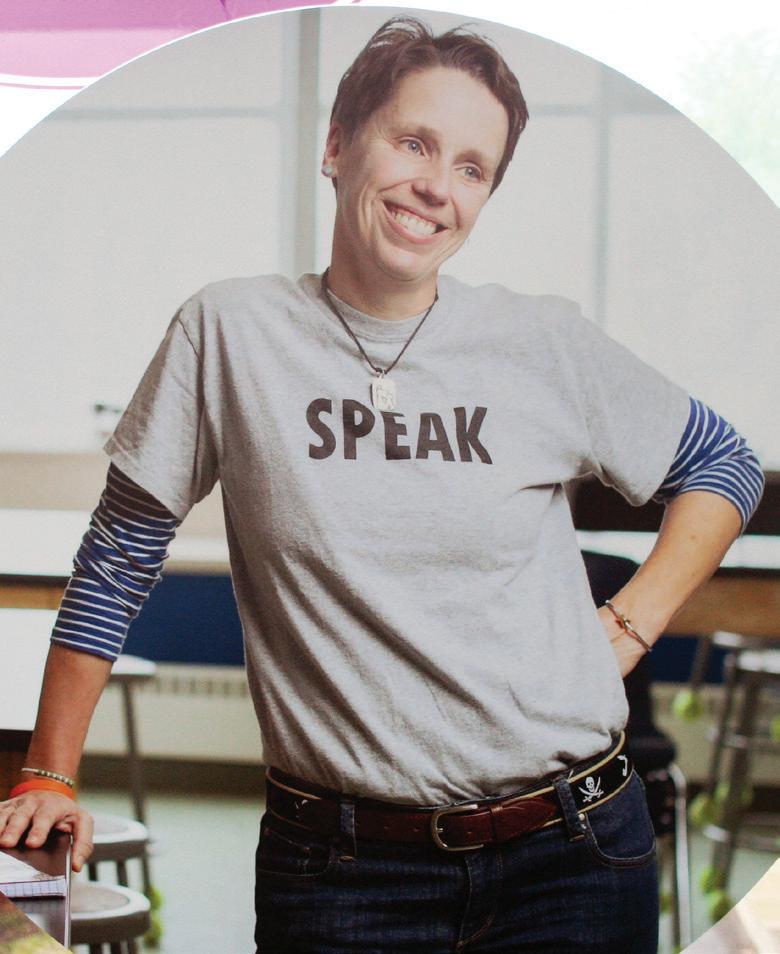
Right now, people are in the process of taking their lives. It’s so devastating to me because I think these are so often good, loving people who are simply overwhelmed by. I want to say to anyone who is suffering that you are not alone, you are not frail, you are not crazy, you are not broken. You are a human who has needs that have not been met yet. And above everything else, there can be no shame at all in whatever is going on in your mind, body, and soul. It is our obligation as a society to be there with open arms, without judgment, and with a promise that it will get better.
Lise
There is no shame in needing help.
From her personal history and her family history, Lise knows a lot about the struggles people can have with mental illness and how stigma makes those struggles worse.
Mental illness runs in my family. So does resilience. You can see that plainly through the generations with our many achievements and lives well-lived, despite struggle. My father swore us to secrecy about my sister’s schizophrenia. Later, he died by suicide. The resulting toxic shame from in and outside my family impacted my development and played a part in sabotaging my chance for a happy and well-adjusted childhood and teen years. It took me into adulthood to really learn about my sister’s illness and the fallout from suicide. Without stigma, much of what happened would have been easier to bear.
Lise’s own problems with mental illness began in high school following her father’s death. Her depression became more problematic through her college years. Years later, a doctor switched Lise’s antidepressant medication, and she was hospitalized for the first time with mania. At age 43, she was diagnosed with bipolar disorder.
I have been in the hospital some dozen times, and I have been on many, many medications. My illness is treatment-resistant, and though I have had relatively long periods of stability, they have not been longer than 18 months to two years.
When Linda’s mom was doing well, she was very caring. Linda says that because her father traveled often for his work in sales, and because she was the youngest child, she and her mother were especially close.
We understood each other. We shared the same sense of humor.
When Linda reached her teens, her mom’s illness became more severe, and she spent time in hospitals, including McLean. Fannette’s mental illness was not something that was hidden, though.
I don’t remember anyone ever trying to hide it. My mom had close friends, and there was family that would take her to the psychiatrist.
Once Linda was an adult, Fannette would feel guilty and say she had been a terrible mother. But Linda didn’t think her mom was a terrible parent at all.
When I was at summer camp, I received a letter from her every day. She never got to go to college, she never got to do certain things, and she encouraged me to have those experiences. And we just had fun together. I always felt that she was there for me.
Once, when her mom was at McLean, Linda wrote a letter — a list of all the values her mom had taught her.

Accept people for who they are, accept myself for who I am, you can always depend on your mother…
Despite the challenges she faces, Lise lives a full and vibrant life.
I maintain a home, work as a librarian, keep up a terrific relationship with my three sons, read, write, garden, walk my dogs, and provide a lap for my sweet cat.
Lise also has a large circle of friends and belongs to a wonderful church community. She attends a support group for people with mood disorders, and she works with the National Alliance on Mental Illness as a connection facilitator. In addition to encouraging people to get help, Lise wants people to understand that mental illness is no different than any other kind of illness.
Life is immeasurably better when you get help, and there is no shame in needing help — there is just misery in feeling depressed or anxious. Last time I checked, the brain is part of the body.
Fall 2018 The Arts . 13 13 Winter 2022
A Tribute
To Intentional Peer Support
The Three Principles From Helping to Learning Together: For together we Become who we may become Therefore we can hum
This silent riddle Which is that which yields true thought. What is or is naught?
So you are magic That welds us together, zeal, Binding us as truth!
Individual to Relationship: Perhaps both of us Will say together now how? What do you do, phew?
Past into present, So what is it you now knew? As if it were true?
Fear to Hope and Possibility: Emotion is true, To cry but not to know why. Ok, as is, do be shy. You are who you are, There is no need to make due. Feel as you feel true.
The Four Tasks Connection:
And if there is both we and you also, true, This connection, here, is bold for me and you, How so, then, and therefore, Did you speak to me of yore? Because yesterday is true just as the score!
Worldview:
Think of how we began from whence or therefore, And thought shall spew forth as though a healing ore! As boundless near to time, Or some silent bell to chime, Upon such height of emotion out of lore.
Mutuality:
And if truth betold, therein of youth this mould, Which tells not of magic, nor of what you hold, But rather truth in thought, As if you had indeed bought, Not what’s yours but to love selfsame what is sought!
Moving Towards:
As such, perhaps, for you this same solution? To believe that there is this one emotion! This selfsame one true hue, Is fine for both me and you. Then perhaps we build upon such devotion?
By BERT DYER
Psychotherapy to the Rescue! Fiction
by RON MERKIN
The more therapy I got the more my interest in women disintegrated. Don’t get me wrong, it didn’t transfer to men. Call it asexuality, distrust. My libido began fading after the psychologist Dr. Bloomstuck began our eleventh session by saying she’d forgotten how we’d ended things the week before.
“You asked me what my mother was like and I told you she was very destructive,” I reminded her.
“Oh. Well I don’t know how that’s relevant to your analysis.” Then she changed the subject.
By our fortieth session (yes, I counted them) I’d gained 60 pounds. That had never occurred before. Then happening to read a book of testimonials by members of Over Eaters Anonymous, I noticed every writer attributed excessive eating to repressed, unexpressed anger.
“Unconsciously I imagined I was consuming my boyfriend,” one wrote.
So I asked Dr. Bloomstuck about that during our next session.
“Oh, have you gained weight?” she asked me. “You haven’t noticed?” I answered.
“Eating more during therapy” (her voice tolerant, a “look here, young man” sort of tone) “connotes gratification of the oral instinct. It’s healing, like a nursing baby sucking up its dependency needs.”
Thinking that a therapist would know better than me, I didn’t argue the point. On the other hand, after gaining another 35 pounds over the next several months, I didn’t feel the warm nurturing effect Dr. Bloomstuck had pointed out to me.
As the sessions continued, I learned that Dr. Bloomstuck was a devoted Yankee’s fan. Little by little she shared so many historic anecdotes about baseball that once when her eyes were distracted I glanced at my watch. Nearly 40 of my 50 minutes had been spent learning things like, “Joe DiMaggio’s fifty six hitting record is to this day unbroken!” and “The number of consecutive games played by Lou Gehrig has never been equaled.”
As her commentary increased, I decided it must be some sort of “diversion” therapy. Instead of reinforcing clients’ obsessions with their problems and thereby perpetuating their neuroses, immerse – in other words distract and involve them – in someone else’s life and interests! I was convinced this must be brilliant when Bloomstuck interrupted herself near the end of our fifty sixth session by observing, “You haven’t been talking much. I think you’re avoiding. Exactly what, we’ll have to look into.” Then standing, “Think about that before our session next week,” she instructed me.
Confused, I decided not to spend the entire week brooding about this. Instead, I went skiing that Saturday. Half way down the advanced slope, I noticed her.
A beginning skier, Bloomstuck was snow plowing so cautiously from left to right that I couldn’t imagine how long it might take her to get to the bottom. Why she wasn’t on an easier slope was beyond my understanding.
Then an epiphany struck.
Why...wasn’t she… on an... easier slope!?!!
Symbolic. I had no idea what it referred to.
On the other hand, a sudden unexpected enlightenment that appears incomprehensible
at first can release a buried insight long struggling to be free. Distracted by this, I lost my footing and plowed directly into Bloomstuck’s back.
Bloomstuck fell.
I did not.
Dazed, lying on her side with her back to me, she seemed to be struggling for breath. Finally catching it, “What kind of idiot? Asshole, you stupid,” she managed, then glancing up at me, “Oh! My God! What are you doing here?”
“I…”
“You what? Don’t just stand there. Help me get UP!”
“I... what are you...why are you...on an advanced slope?” I stammered.
“HELP... ME UP FOR HEAVEN’S SAKE!”
Of course! Why was I standing there doing nothing?
Extending my arm, I noticed she couldn’t extend hers. By now two skiers had stopped to ask if she was all right.
“Try your other arm,” one suggested. But seeing the pain that caused her, “Just relax,” and he searched for his cell phone to call the ski patrol.
They arrived around ten minutes later. A broken collar bone, it needed a full arm cast for a month and a half.
Thinking that the awkwardness imposed by her injury might somehow compromise her effectiveness, Dr. Bloomstuck decided to cancel appointments until her injury healed. All this happened before the pandemic. Few people knew anything about ZOOM. Not having heard that Bloomstuck was willing to do sessions by phone, I thought it best not to call her. Then after a few weeks I noticed I’d begun losing weight. I hadn’t launched a diet, without thinking I was simply eating less. And if that wasn’t enough, three dates I’d had with a woman my age suggested we were moving toward a relationship…
Wow! Let nature take its course!
I never returned to psychotherapy.
But two years after this I received a notice sent by post office mail indicating that Dr. Bloomstuck had left me something in her will.
What, wasn’t specified. I hadn’t even heard that she’d died. So, phoning her attorney, I learned that her gift was a full season’s pass to Yankee Stadium baseball games.
Her motivation – “...my conviction that George needs this…” – seemed so missing the point about what I needed that it helped ease the guilt I still harbored about crashing into her. The facts that I didn’t do that on purpose and its outcome freed me to have a life of my own clarified the meaning of that “epiphany” I had, also. In fact, by disorienting me, the epiphany –not I – had caused the accident.
By the time I phoned Bloomstock’s attorney I’d been married for a year. We were expecting a son; not only that, I’d maintained a weight between 140 and 145 pounds. And if all that’s not enough, I sold the Yankee pass Bloomstock left me for a price exceeding her psychotherapy fees!
Fate! A happy ending!
(What more could a psychotherapy survivor hope for?)
Ron Merkin is a retired psychiatric social worker, journalist, fiction writer and entertainer. He lives in Montpelier.

Fall 2018 The Arts 14 Winter 2022
Seahorse Celebrations
by CYNTHIA CHRISTENSEN, Montpelier
Art has been a major healing force in my life, and I draw while supporting Vermonters as a full-time peer operator on our Vermont Support Line!
These originals are created with Sharpie Markers/Tom Bow Dual Brush Markers to lay down colors, Unibell Gold, White, and Silver Pens to highlight, on 18” x 24” Swarthmore Heavyweight Drawing Paper.
I’ll Love You to Infinity: The rainbow colors represent all colors of humanity, and hopes for unity in diversity, hope of light emerging from darkness, fear to hope, grief and joy, for those in challenging times, healing times.

Courage
There needs to be some differences made
The old ways are ineffectual, not serving the needs anymore
Well at least not in the healthy ways. Change.
Oh No! Not the C word No, it’s too scary, Uh, Uh, no it’s too lonely, its hurts
Why can’t I stay here in the womb of complacency? It is warm and comfortable here Yet, there is restlessness there But I don’t want to experience this new birth. Uh, uh, nope no not me to scary Maybe I can help Who are you?
Courage
Oh, great another C word Here, hold my hand We’ll do the journey together How’s that?
Better? Still scared? Well a little, just keep holding my hand ok? Yes, we will
We?
Yes, God and I
ANONYMOUS by Request
I’ll Love You to Infinity
Seahorse: Thinking about beloved creatures in our oceans is healing for me, and I have always been drawn to and fascinated by seahorses.
Celebrations... was drawn after healing from my unexpected surgery last March, when my appendix massively burst. I spent three days in ICU and another on Medical Surgery Unit, and a month to heal a very deep wound with daily dressing changes. It was a traumatic, but profound event of healing, feeling well supported by over 30 surgeons, doctors, RNs, LPNs, folks who cleaned my room, made food, etc. I went through a hard time but was able to celebrate coming home with all I have to be grateful for.
See more of my art at www.cynthiachristensenart.com/

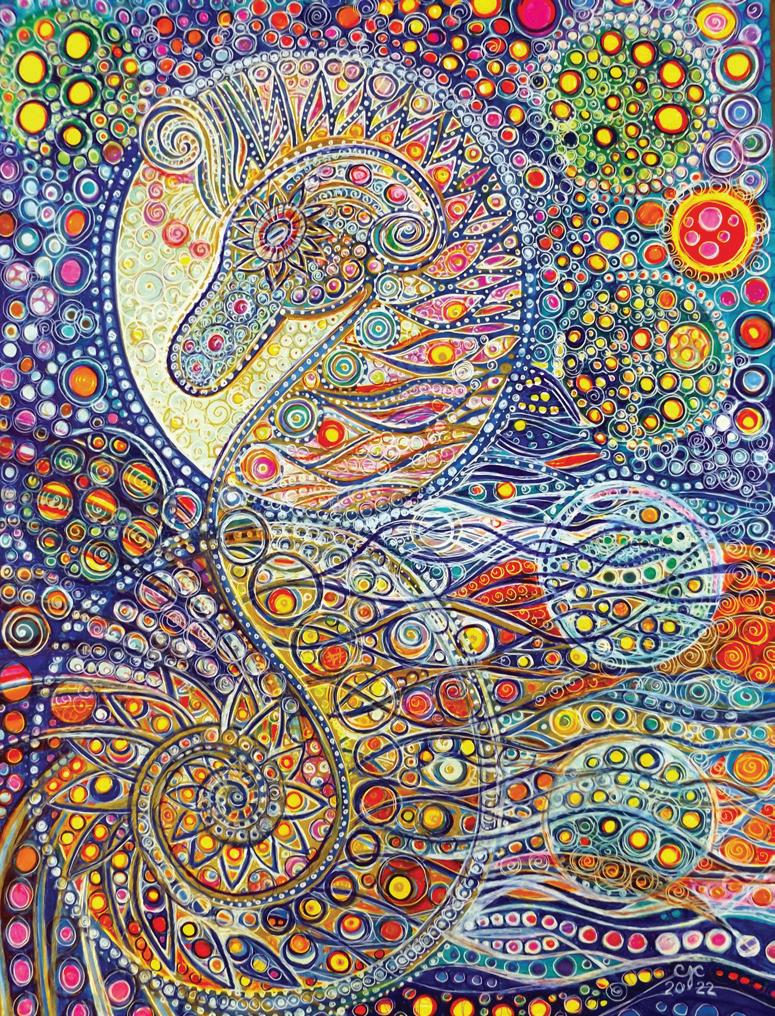
Strength in Knowledge
I held in my hands, the truth for you to see. I showed you a future that you and I can have. I helped you fight your battles and I cried your tears. I gave you the power to be who you were meant to be. You have become human: after all the years you have fought to stay numb to humanity. I gave you a picture to hold onto: an image in your mind of hope. I gave you a purpose to know: strength in knowledge is what makes the world grow. A world without sorrow, hate, anger and pain where all humanity flourishes and all sufferings end, is only possible with truth at its head.
by GABE SIMPSON Rutland
January of ‘21
“The card of the day.”
Jody shuffled her Tarot deck on the small, cafe-style table where we were served all three meals by the staff of the Unit. She was known as “Splash” by the patients (as in bringing “a splash of color/positivity” to the floor) but, of course, she was never called this by the staff; these psychiatric professionals did not engage with nicknames. They had a lot of beliefs about, as they said, “boundaries.”
“The Tower.” She looked out from under her dark bangs at me, ominously. A problematic card... but, also, a fitting one, perhaps. Towers have long been symbols of psych facilities, asylums, “Bedlam.” Splash’s Tarot-ing had become a kind of action of resistance.
The director of this hospital diversion program was promoting a daily mindfulness group meeting (as is standard, now) but after we all had an extremely bad emotional experience at one session (wherein we were asked to cultivate compassion toward a past abuser in our lives), Splash was advocating the Tarot as a spiritual practice. Our “Mad Bible,” as she called it.
Now we were studying the card’s image under the glare of the staff, entrenched behind glass at the nurse’’ station. “It’s about questioning, destruction, and chaos.” She smiled at Pamela Smith’s illustration. “It’s about us...”
By PATRICK STANTON
The Arts . 15 Winter 2022
Poetry and Prose t $250 in Prizes! Winners and Runners-Up Published in Counterpoint Deadline July 10, 2023 For more information, write to counterpoint@vermontpsychiatricsurvivors.org Start Getting Ready for the 2023 Louise Wahl Writing Contest!
Opinions
Editorial Defining Input
A brand-new initiative to develop a child and adolescent psych unit at Southwestern Medical Center in Bennington is already off on the wrong foot when it comes to input from psychiatric survivors and their families. Likewise for an initiative to develop an urgent care program in a collaboration between the Howard Center and the University of Vermont Medical Center.
Repeatedly, the federal directive for “mental health care that is consumer and family-driven” is misunderstood in two ways:
1) that it is only talking about a person’s own care, not the system as a whole; or
2) that consumer-driven means getting some input on a plan that is already underway (or sometimes, already nearly complete).
If you go way back to 2003 and President George Bush’s final report on “Achieving the Promise” for transforming mental health care in America, you find a very clear description. It says:
“Consumers of mental health care must stand at the center of the system of care... In a consumer and family-driven system... (t)heir needs and preferences drive the policy and financing decisions that affect them... Local, state, and federal authorities must encourage consumers and families to participate in planning and evaluating treatment and support services. The direct participation of consumers and families... is a priority.”
This is about the system, not about individual care. This is about driving policy and about planning the programs, not about giving generic advance input or involvement in discussions after key decisions have been made.
The Department of Mental Health is now in the second stage of the planning for the new hospital unit in Bennington. It sent out a request for proposals from hospitals without involving families in what the criteria should be. DMH has now signed a statefunded contract for Southwestern Medical Center to conduct a feasibility study without family input into what such a study should include. Although it was good to hear that the hospital may bring stakeholders into the feasibility review, that was its initiative, not a requirement from DMH.
DMH also participated in a meeting of various interested providers and community members about possible development of an urgent care center. The discussion failed to include any survivor voices. When the Howard Center began refining the early plans, they also did not bring any survivors or peer support workers into the discussion, saying it was still premature.
The whole system is still stuck in the tired old concept of asking for input after the policy decisions are made, instead of having survivors, peers and families be a part of that decision-making. These proposals may all be terrific. It may be that we all support them. But DMH is in the driver’s seat for choosing the priorities and implementation. We were most definitely not in “the center of the system of care.” Has everyone forgotten that it is supposed to be, “Nothing About Us Without Us”?
Fortunately, it is still early enough in the work to correct course and bring us on board. Survivors can help review proposals, even if not involved in drafting the original requests for them, thereby helping to prioritize which plans are best, and what next steps should happen. Contracts must require our inclusion in the actual development of programs.
It’s time for us to be brought into the decisionmaking process if we are ever to “achieve the promise” of almost 20 years ago.
Publisher’s Commentary
Cartoon by Thompson
Peer Divisions Are Hurting Us
By KARIM CHAPMAN
Despite our broad common interests, divisions in the peer movement are getting in the way of our ability to be successful in the state. In the past two years, there have been efforts in the peer community to push to be on the same page, but individual opinions seem to get in the way of presenting a unified front to the public and to legislators. That has hurt us.
What are some examples of division?
1. Survivors have different perspectives when it comes to police and procedures on mental health. What are the best ways to make progress in these relationships?
2. There has been ongoing debate on definitions for “peer specialist” and “peer worker.” It is hard to make progress on agreement about peer support certification if we can’t even come together on definitions.
3. The peer movement is not on the same page when it comes to community mental health agencies working with peers versus peer-run organizations taking the lead with funding opportunities. Are peer programs only fully “peer-run” if they are within a peer agency? Or do traditional mental health agencies actually present the best opportunity
to get peer support available to more survivors? These views are sometimes in conflict.
What’s important to understand is that when legislators see that we’re not on the same page it makes it harder for them to understand our path to success.
Last year, we had two great bills that survivors submitted, and they held no weight as they moved through the process. One was on peer certification, and the failure of that bill to pass has added delay to moving ahead on this important effort.
The other would have established peer respite centers around the state. When the bill died, it left us with no clear path forward on expansion of peer-run programs. Instead, the Department of Mental Health issued a request for proposals this fall for urgent care and hospital diversion programs that made no reference to peer-run models.
I believe that the loss of these two initiatives in the legislature was in part because of the inconsistency that the peer movement has shown through testimony.
I think the focus should be on a model that represents us as psych survivors in Vermont and how we save the state money through the work that we do.
If we cannot work together on our shared goals, we will continue to lose chances to move forward on them.
Karim Chapman is the Executive Director of Vermont Psychiatric Survivors, the publisher of Counterpoint.

Fall 2018 E16 Winter 2022 COMMENTARY
Send comments to: Counterpoint, Vermont Psychiatric Survivors, 128 Merchants Row, Suite 606, Rutland, VT 05701, or to counterpoint@ vermontpsychiatricsurvivors.org. Reactions to Our Commentaries? Write Us a Letter!
Letters to the Editor
Mental Anguish Versus Mental Illness
To the Editor:
Thanks for the article on Any Given Day (film review, Counterpoint, Fall 2022)
I agreed with you on almost every point. The premise of the film is that Mental Illness is Real… an a priori with which I take issue. The fact is that smoking weed or PCP or drinking or taking unknown drugs seemed to be the main trigger for the various diagnoses claimed in the film.
I myself think that getting a diagnosis is what causes mental illness, that this has no other reality except as an iatrogenic condition. Mental yes, but mental in the sense of imaginary.
And of course, there is the problem of the criminalization of substance using… and a mental health court that creates chronic “mental patients” who were formerly created (by their act of using substances) “criminals.”
I would never deny the existence of suffering, but suffering is part of life and is always mental.
Anyhow, the film gave me food for thought but was not in itself earth shattering or even mildly iconoclastic. Mostly it was the assenting nod of those who have been co-opted by psychiatry and well-psychiatrized!
I wish PBS were less cowed by the psychiatric
establishment and their lies about psychotropic drugs efficacy, and mental illness in general, but they are, I’m afraid, probably sponsored by the American Psychiatric Association or some group upon whose toes they dare not step.
I found this was true also of NPR when I lived in Connecticut.
Someone interviewed me for nearly 2.5 hours about the use of restraints in Connecticut hospitals, but when the radio show was aired, that long interview had been cut down and dishonestly condensed to two sentences taken out of context.
The rest of the hour was given to voices of people I knew and had been “treated by” in these hospitals, who lied knowingly, in saying that restraints were rarely used and only when necessary and never excessively or as punishment… when I knew for a fact the opposite was true of each statement, and had said so in my interview.
The same hospitals that claimed they almost never used restraints, had restrained me routinely for up to 20 hours and nearly every day…and why? As one nurse told me, “you don’t follow directions”...
The fact is, my voice was silenced by the NPR editors while they accepted without even questioning it, whatever the hospital staff or spokesman avowed. It was both disappointing and utterly disgusting. I was almost as traumatized by this as by the brutality I experienced in these hospitals.
PHOEBE SPARROW WAGNER Brattleboro
Ending Homelessness
To the Editor:
To end homelessness, they really need more housing for people who have mental health issues who have low income and need more support with supervised apartments.
There needs to be temporary housing for those coming out of rehab centers and prison that’s staffed with case managers and staff onsite; secured apartments with video surveillance on the premises and in hallways to protect the safety of others; community services until finding a job.
TIFFANY KANGAS South Royalton
Helping Those Who Need a Safe Space
I’ve been thinking about the question from the reader poll in the fall Counterpoint: Does Vermont need a forensic psychiatric hospital? A separate place from a regular psychiatric hospital?
I’ve been giving this a lot of thought.
If you think you’re the Second Coming, act like it; if you have been violent, scary, or inappropriate in a way that disturbs the peace or the peace of a parent, child, spouse, significant other, couple, family, an individual, yourself, or anyone, you need healing.
One good way to heal is: to have a safe place (where both you and others will be safe) where you can be quiet, be comfortable,
have zero contraband but have some or all of your belongings. We heal by observing our relationships. When humans are too confusing for me, I find my relationships with my things is helpful to me in figuring things out.
It should be a place where you can see a tree (proven to increase healing), where you can see the sky, the sun, the clouds, the stars, and where you can see the moon or new moon, as I can tonight, as I write this. New moons are beginnings, my older sister told me.
It should be a place where you can eat foods you like and drink plenty of water.
If you want a chance to heal, a forensic hospital could be a good place to heal, if you
make it healing, by being open to a path that takes you somewhere good.
I don’t know you or your situation, but I want to know you, if you’re working and working on yourself. This commentary is my work today.
As a psychiatric survivor, my recent experience of disturbing those around me, and then a crisis, and then finding a new path towards good, leads me to offer some tips that I am hoping are helpful. They are: having access to a safe, quiet place, food you want to eat, plenty of water, and access to your belongings and the sky.
It will be a wonderful start.
The writer of this commentary requested anonymity.
By GRACE WALTER
Performing
a job that is based on “lived experience” at the young age of 23 has been difficult but rewarding to develop.
For a period of time when I first began this job I was dealing with impostor syndrome, the feeling that you are not good enough for a role. In this case, I had the thought that because I was so young, I would not be taken as seriously as someone with lived experience.
For someone my age I have lived darker days than most, but I am adamant about healing those pains from the past and helping others.
Before I had accepted this, I was less confident in my interactions with peers. I had in my head that I was being looked down upon,
and I felt inferior, because a lot of the people I was working with were older and lived through much more than I.
Note – I have never had a peer tell me this, but that’s how anxiety works, your brain twists the way others perceive you and allows you to act from that place of inferiority.
After a couple of months in this position that anxiety began to loosen when I realized how inmy-head I really was. A peer I had been working with who was about 60 years older than me said, “You are really easy to talk to and I look forward to our conversations.”
Such a small compliment went such a long way in my head. I could really see where my position has benefited another just through my words and experience. I no longer felt like I hadn’t lived through enough.
It became clear that it does not matter how much life experience you may have, but instead your kindness, vulnerability, and attentiveness do. These are all attributes that I have kept close throughout my lifetime and have been
highlighted through this position. Over time I have realized that no matter your age you always have something to offer. I have become a better person based on the interactions I have had in this job.
Although I have had my downs, I am very fortunate for what I do have. To see the resilience of so many peers throughout their life has made me appreciate the people in my life that love me and the resilience I have inside of me.
This role has highlighted human connection for me and sharing words with people from all walks of life. Humans innately are social creatures, and connection is one of the things that I believe keeps us going.
Living in the generation of social media our society has lost the emphasis on face-to-face connection. This job allowed me to find that again, and gain a confidence in myself that I had never had before.
Grace Walter is a patient representative at Vermont Psychiatric Survivors, serving northern Vermont.

Fall 2018 17 Winter 2022 COMMENTARY
Beating Back
Tell Us What You Think! Send comments to:
or to Counterpoint,
the Imposter Syndrome
counterpoint@vermontpsychiatricsurvivors.org
Vermont Psychiatric Survivors, 128 Merchants Row, Suite 606, Rutland, VT 05701
A Vermont Advocacy Resource Toolkit

A New Legislative Session Begins in January: Writing Letters to the Editor Is One Way to Have Your Voice Heard
By MORGAN BROWN
“Never doubt that a small group of thoughtful, committed citizens can change the world; indeed, it’s the only thing that ever has.”
– Margaret Mead
“I’m convinced of this: Good done anywhere is good done everywhere. For a change, start by speaking to people rather than walking by them like they’re stones that don’t matter. As long as you’re breathing, it’s never too late to do some good.”
– Maya Angelou
If you want to be heard on certain matters of concern (e.g., affordable housing or addressing homelessness, including what is really needed and what truly works versus what does not work and is not needed), it is crucial to do so in various ways. This includes by contacting your local state legislators who serve in the Vermont General Assembly in Montpelier, as well as to write and submit letters to the editor (LTE) or op-ed commentary both to local newspapers as well as to newspapers with a more regional or statewide circulation (e.g., Rutland Herald, Times Argus as well as VTDigger).

“To be an activist is to speak. To be an advocate is to listen. Society can’t move forward without both.”
– Eva Marie Lewis
Tips on Writing Letters to the Editor
Letters to the editor are great advocacy tools. After you write letters to your members of the Vermont Legislature, sending letters to the editor can achieve other advocacy goals because they:
● reach a large audience.
● are often monitored by elected officials.
● can bring up information not addressed in a news article.
● create an impression of widespread support or opposition to an issue.
Keep it short and on one subject. Many newspapers have strict limits on the length of letters and have limited space to publish them. Keeping your letter brief will help assure that your important points are not cut out by the newspaper.
Make it legible. Your letter doesn’t have to be fancy, but you should use a typewriter or computer word processor if your handwriting is difficult to read.
Send letters to weekly community newspapers too. The smaller the newspaper’s circulation, the easier it is to get your letter printed.
Be sure to include your contact information. Many newspapers will only print a letter to the editor after calling the author to verify his or her identity and address. Newspapers will not give out that information, and will usually only print your name and city should your letter be published. (These tips on writing LTE’s were drawn from a previous version of a national ACLU Web page on the subject.)
Some newspapers limit a person to one letter to the editor per subject per month, so when you write, besides keeping it simple, brief and to the
point, make it count. Most importantly, use your own words: i.e., keep it original.
“Power
Frederick Douglass
This advocacy resource is a listing for e-mailing or online submissions of Letters to the Editor and Op-Ed commentaries to Vermont newspapers (however, please note, this is not an exhaustive or complete listing of all Vermont newspapers).
Vermont daily newspapers:
Times Argus (Barre - Montpelier), online submission form and guidelines: www.timesargus.com/site/ forms/online services/letter editor/ or, submit to: letters@timesargus.com; Bennington Banner: news@ benningtonbanner.com; Brattleboro Reformer: news@ reformer.com; guidelines for submission: www. reformer.com/site/forms/online services/letter editor/ ; Burlington Free Press: unfortunately, Letters to the Editor or ‘My Turn’ commentary are no longer accepted nor published by this newspaper; Newport Daily Express: guidelines and online submission form, www.newportvermontdailyexpress.com/site/forms/ online services/letter editor/; Rutland Herald: online submission form and guidelines, www.rutlandherald.com/ site/forms/letters/ or, submit to: letters@rutlandherald. com; Valley News: guidelines and online submission form, www.vnews.com/Opinion/Submit-a-letter/ or, submit to: forum@vnews.com; VTDigger (online publication only): policy and submission guidelines, vtdigger.org/submit-aletter-to-the-editor/
miltonindependent.com: Middlesex Newspaper: Letters: middlesexnewspaper@madriver.com; The Mountain Times: editor@mountaintimes. info; (Lamoille County) News & Citizen: edit@ newsandcitizen.com; The Northfield News: thenorthfieldnews@gmail.com; Randolph Herald: editor@OurHerald.com; St. Albans Messenger: elynn@orourkemediagroup.com or online form, www.samessenger.com/site/forms/online_services/ letter_editor/; Seven Days: online submission form and guidelines, posting.sevendaysvt.com/vermont/ LetterstotheEdditor/Page/; Stowe Reporter: news@ stowereporter.com; The (Washington) World: online form: www.vt-world.com/letters-to-the-editor/ or, submit to: editor@vt-world.com; Valley Reporter: news@valleyreporter.com; Vermont Standard: letters@thevermontstandard.com; Waterbury Roundabout: waterburyroundabout@gmail.com; Williston Observer: editor@willistonobserver.com
“Find out just what any people will quietly submit to and you have the exact measure of the injustice and wrong which will be imposed on them.”
– Frederick Douglass
“You may never know what results come of your action, but if you do nothing there will be no result”
– Mahatma Gandhi
Additional advocacy resources: Video: The People’s Guide to the Vermont Legislature (via CCTV): The People’s Guide to the Vermont Legislature is a half-hour program designed to encourage Vermonters to participate in their government by making the legislative process easier to understand. Viewers learn why the Legislature is so important, how it is structured, why committees are important, how bills can become law and how to get involved.
“When the world is silent, even one voice becomes powerful.” – Malala Yousafzai
Vermont non-daily newspapers: Addison County Independent: online submission form, www.addisonindependent.com/send-a-letter-to-theeditor/ or, submit to: news@addisonindependent.com; The (Montpelier) Bridge: editorial@montpelierbridge.com; The Commons: voices@commonsnews.org; The (Barton) Chronicle: news@bartonchronicle.com; Counterpoint: Vermont publication of news, commentary & art by psychiatric survivors, mental health consumers and their families: counterpoint@vermontpsychiatricsurvivors. org; Deerfield Valley News: letters@vermontmedia.com; Hardwick Gazette: news@hardwickgazette.com; The Independent: Vermont publication for elders and people with disabilities. info@vcil.org; (Bradford) Journal Opinion: editor@jonews.com; Manchester Journal: news@ manchesterjournal.com; The Milton Independent: news@
COMMENTARY 18 Fall 2018 Winter 2022 COMMENTARY
concedes nothing without a demand. It never did and it never will.” –
“Nothing strengthens authority so much as silence.” – Leonardo da Vinci
Compiled by Morgan W. Brown (last updated: October 14, 2022; Photos: Vermont State House, taken by Morgan W. Brown.
Reflections of a Recovering Community System Psychiatrist
 By DAVID MCKAY
By DAVID MCKAY
Hello. My name is Dave. I have been in recovery since 2009. I was addicted. I thought I could control it. Then an old friend who had been in the program for many years invited me to a meeting.
I was skeptical at first. I had heard lots of negative things about the program, all sorts of things about how it didn’t work, horrible things about how it abandoned people who needed it in order to recover. I was skeptical, but at the invitation of an old friend, I went to my first meeting.
And that was my first step on the road to recovery from Vermont’s community mental health system.
I spent many years in Vermont’s community mental health system. Hey, it’s the system, so what else have we got? I fully supported its ideals, its purpose, its goals. I did my best to make it work.
But there were problems. I didn’t understand them at first. Underfunding. Unresponsiveness. Resistance to change. Incompetent management. Failure of vision and initiative. And the list goes on. Well-intentioned, but ineffective. I was in way over my head but I didn’t realize it.
At that first meeting, I listened to people in the program talk about their own struggles. They spoke frankly about disillusionment with the program, about its weaknesses and failings. But they also spoke with great respect about the good work the program had done for millions of people whose lives literally had been saved because of its existence.
I was not an easy convert. It took time to loosen the knots I had gotten myself tied up in, trying to straighten out all the twists in Vermont’s community mental health care system. I was always looking for that next fix, thinking that if I could score just once more I could turn the corner onto Easy Street.
My old friend just shook his head and tried to show me I was not on a healthy path. Vermont’s community mental health system has always limped along, shunned and even despised by many of Vermont’s other health care providers.
Stigma. Disrespect. Denial. Refusal to accept and support mental health as a vital component of an integrated health system. Always the stepchild, never the prodigal son.
There is a better path. It is not an easy one. In fact, it can be very muddy. Hard to keep slogging forward. Hard to see your way through the fog. You really have to work for it in order to make it work for you. One day at a time. One step at a time.
I came to admit that I was powerless over Vermont’s mental health system, and that I needed to turn my career over to a greater power so I could restore my life to sanity. And that is
think they know how to make the system work.)
They are on the spot in case of mental health emergencies or urgent situations. They offer immediate access to wraparound supports such as food, housing and legal services. And of course, they provide specialized mental health care for veterans struggling with mental health conditions.
They work together, all under the same roof. It is a kind of “one-stop shopping” that seems disappointingly lacking elsewhere in America’s patchwork health care system.
that seems disappointingly lacking elsewhere in America’s patchwork health care system.
how I found the Veteran’s Administration.
The VA health care system is admittedly flawed and imperfect. And so are we all, all of us are flawed and imperfect. But for all its faults and failings, the VA has come to terms with the essential reality that the mental and emotional well-being of military veterans is integral to caring for their overall health.

The VA places mental health caregivers inside its hospitals and outpatient clinics. They are present and available for immediate consultation with primary care staff.
They participate in team meetings to suggest approaches and supportive interventions to engage veterans whose health would benefit from psychological treatment. They offer behavioral treatment for conditions such as chronic pain, substance abuse, diabetes and obesity.
They provide training and support for front line staff, from receptionists to lab techs and nurses to seasoned internists. (And those front line staff provide training and support for all those administrators and bean counters who
The program is not perfect, not by any means. It has its quirks and its shortcomings. But it is always open to change and improvement. And it is dedicated to caring for the military veterans who have served our country through the worst of times.
Perhaps it could serve as a model for change in a broken system ravaged by greedy drug manufacturers, profiteering insurance companies, Wall Street traders, and a plenitude of other duffers who just want to milk a buck out of the system before it goes down.
I am old and retired now. The problem of health care reform is no longer mine to solve. A new generation needs to step up and figure out what they want to do about it. I don’t need to give a damn what you people decide to do.
But, strangely, I still care. And I wish you the best.
Hello. My name is Dave. I have been working on my recovery since I entered the VA program in 2009. Thank you for listening to my story.
David McKay describes himself as “a retired physician from Middlebury, a lifelong Vermonter, a survivor of America’s prodigious health care system, past president of the Vermont Medical Society and the Vermont Psychiatric Association, and a proud veteran of service at the Burlington Lakeside Clinic of the Department of Veterans Affairs.” His commentary was first published in VT Digger.
Making Community Connections, Virtually
By LAURA SHANKS
In April, I launched a virtual peerrun wellness collaborative group on Zoom through Vermont Psychiatric Survivors with my colleague, Carter Kinoy, with a mission to provide a safe community space for open discussion, synergetic support,
creative problem solving, and mindful movement. This mutual support group, called Creative Collaborative Connections, meets every Tuesday from 5 to 6 p.m., the group also holds space to voice concerns and enlist support for advocacy to create positive change with likeminded individuals.
Now, six months in, I can say that this group has become one of my favorite times of the week. As a facilitator, I always come with discussion topics and creative potential, but hold space for the group to choose the direction.
They say you get what you get when you need it and no matter what, the evenings’ exchanges
always seem to be exactly what I need in the moment. Even if I’m feeling good, I aways leave group with a deeper sense of happiness, connection, and understanding. I am grateful to all those who attend and hope they leave each meeting with a similar sense of serenity.
We anticipate the group will continue to grow and welcome all those who wish to join. Email me at Laura@vermontpsychiatricsurvivors.org for the link.
Laura Shanks is Peer Support Coordinator and a patient representative for Vermont Psychiatric Survivors.

COMMENTARY . 19 Fall 2018 COMMENTARY. Winter 2022
It [the Department of Veteran’s Affairs health care system] is a kind of “one-stop shopping”
Then... A Comparison from the Pages of Counterpoint:
35 Years of ‘Regionalization’
The summer issue of Counterpoint in 1988, 34 years ago, focused on a new plan called “regionalization” that had begun the year before to shift people who were being held at the Vermont State Hospital in Waterbury to living in their local communities with support services from mental health agencies. (Vermont Psychiatric Survivors has stored copies of Counterpoint beginning with 1988. It started publication in 1985, but there are no saved issues from the first three years.) The lead article featured a review of some of the early goals to reduce the number of patients being housed at VSH, which at the time was the only place where individuals were held against their will. What was happening then, and where do we stand now?
.COMMENTARY COMMENTARY 20 Winter 2022 20
Average Number in Hospitals
1988:
A goal of regionalization was to reduce the average daily number of patients being held against their will in the hospital. The average daily patient count at Vermont State Hospital was 152. This was down from 189 when the regionalization efforts began one year before. The all-time high had been 1,301 in 1954.
152
Hospital Beds and Admissions
1988:
The goal was to be able to close down the number of involuntary hospital beds that were, at the time, all at Vermont State Hospital.
In the first year after the regionalization plan started, the Department of Mental Health reported that, “Contrary to what many had feared (that is, the creation of mini-state hospitals) no new involuntary units have been created.” (Counterpoint, Spring 1988.)
The number of annual admissions in 1991 (the closest date with published data) was 329.
1988:
61 ...and Now
2022:
The average daily patient count of individuals being held in hospitals against their will was 61. This included 36 at the Vermont Psychiatric Care Hospital and the other “Level 1” (highest security) hospital units in Rutland and Brattleboro that replaced VSH after it closed in 2011, and an additional 25 patients on other locked units at regional hospitals or the Brattleboro Retreat. (An average daily patient count is not the same as knowing how many different people are hospitalized each year, because if someone is there for a long time, it increases the average number of total days that there are people being held.)
2022:
Within 10 years, all regional hospitals with psychiatric units had begun admitting involuntary patients onto locked units. In 2002, the Retreat was the last to add patients being held against their will. In 2011, the last unlocked unit in the state became a locked unit. After Tropical Storm Irene closed the remaining 54 beds at the Vermont State Hospital in 2011, they were replaced by the new 25-bed Vermont Psychiatric Care Hospital, two “Level 1” units at regional hospitals (14 beds at the Brattleboro Retreat and 6 at Rutland Regional Medical Center) and seven locked residential beds, for a total of 52.


329 573
In 2021, 12 new “Level 1” beds at the Brattleboro Retreat opened. An expansion in locked residential beds from 7 to 16 scheduled to open in 2023. Discussion is underway on whether a new facility for forensic patients (those with criminal system involvement) is needed. The number of admissions of involuntary patients increased between 1991 and 2021 from 329 to 573.
Crisis Services and Use of Peers
A Task Force recommended these new programs: 1) a 24/7 statewide crisis hotline, 2) an alternative crisis system with a crisis center and “safe house” for 6-8 persons for stays up to 6 months, 3) new crisis outreach services in the mental health centers with peer available to stay with a person in crisis and individual crisis beds, (All three of these to be using consumer/ex-patient/peer staff), and 4) expanded public education on “what is a mental health crisis.”
Community Funding
1988:
Funding for new crisis services was cut from an anticipated $2 million to $700,000 for the second year of the regionalization plan. Predictions were made about savings from closing hospital beds being earmarked for community services, but there were complaints about lack of money for community services.
2022:
Funding for expansion of peer-led crisis centers was rejected by the legislature. Regular complaints are made about inadequate community funding to meet the original promise of closing Vermont State Hospital beds. There are no data reports for the ratio of money spent on hospital versus community services over the past 34 years.
2022:
1) The Pathways Support Line started statewide in 2013 and became 24/7 in 2020,
2) Community support centers exist in Burlington and Montpelier and Soteria House opened as an alternative residence with six beds in 2015;
3) Some community mental health centers (called “designated agencies”) have peer outreach staff. Several peers do outreach through Vermont Psychiatric Survivors. Alyssum hosts two peer-run crisis beds. The legislature has funded the start of an expansion of mobile outreach, with inclusion of peer staff, and
4) public education in recent years has included youth and adult suicide
And so, after 35 years of efforts, it might bring to mind the old French saying, “plus ça change, plus c’est la même chose”: the more things change, the more they stay the same.
21 COMMENTARY. Winter 2022
The Dale yard at the Vermont State Hospital in Waterbury, 1988, Building at left is 5 South; on right, patient library.
Walk Calls Attention to Suicide
 By BRETT YATES
By BRETT YATES
BURLINGTON – A sunny Saturday morning in October drew a crowd to Burlington’s Battery Park, the starting point for an annual Out of the Darkness walk organized by the American Foundation for Suicide Prevention.

The group of survivors of suicide loss and mental health advocates gathered to support AFSP’s work, share stories, and remember loved ones.
“This Out of the Darkness event helps raise funds not only for innovative and exciting medical research that will enable us to find better ways to stop suicide and advocacy events that support important mental health legislation, making real change at the public policy level, but [also] educational intervention programs and resources for survivors of suicide loss in your own neighborhoods,”
RUTLAND – Vermont Psychiatric Survivors has announced the start of two new peer outreach staff.

Mariah Sullivan
Mariah Sullivan has joined VPS as a patient representative for southern Vermont. She holds a bachelor’s degree in psychology and a master’s degree in counseling psychology.
Sullivan has spent time working in a variety of areas in mental health/substance abuse including as a mental health therapist, at a needle exchange, at a crisis center, and at inpatient facilities and residential homes.
She describes herself as passionate about the reform of both our mental health and criminal justice systems. Having lived mental health experience, Sullivan says she entered the field in the hopes of being a positive force within a system that she felt she’d often been let down by.
Sullivan says that she found that she was not satisfied working in many of these positions and felt that they were not in alignment with her personality and sometimes her values. She felt that she wasn’t
able to create the change and have the impact she wanted within the structure of the mental health system. As a result, she says she shifted her focus and interest to advocacy, peer work, and alternative models of mental health.
Grace Walter
Grace Walter has also joined Vermont Psychiatric Survivors as a patient representative., covering northern Vermont areas. Born and raised in Connecticut, she graduated from Newtown High School and then found her way to Vermont for college.

Walter discovered her interest in working with nonprofits when she volunteered with Gun Sense Vermont to advocate for common sense gun laws. She holds a B.A. in Political Science from the University of Vermont.
Walter says she is passionate about advocacy for a number of social, racial and environmental issues, but is especially passionate about reforming the mental health system. Mental health strikes as a personal issue, she says, and she feels fulfilled helping others struggling. In order to prioritize healing she says she takes refuge in the things that make her happy, like being outdoors in beautiful Vermont, practicing painting and drawing, and listening to music.
Walter enjoys traveling, and spent a month in Florence, Italy exploring and learning about the culture.
said AFSP Area Director Heather White.
Walkers wore custommade T-shirts and beads in honor of those who died by suicide and held signs to promote mental health.
An AFSP volunteer, Bob Purvee, said that he and his family have attended the Out of the Darkness walks since the death of his son five years ago. “Some of it is just plain camaraderie, knowing that there are others like you have been affected by suicide,” he explained.
“I don’t know if it’s possible to save very many lives or not, but if you only save one, you’ve accomplished something.”
AFSP organizes walks in more than 400 cities and towns across the country. Rutland, Newport, Brattleboro, and Montpelier have all also hosted Out of the Darkness events this year.
See Walter’s photo and reflections about her work in the commentary on page 19.
Stephanie Kacanich
Stephanie Kacanich has come on board as a part time peer advocate. She describes herself as a psychiatric survivor as well as a person who is in recovery from alcohol, whose passion for peer advocacy came “in my early days of figuring out who I was in my recovery journey.”
Kacanich’s professional experience began at Turning Point of Chittenden County where she made her way from a volunteer to a Recovery Coach for the Moms in Recovery Group and as an emergency department Recovery Coach at the University of Vermont Medical Center.
“I also had the chance to go back to UVMMC psych units as a Mental Health Tech and not a patient, which was a great experience because it gave me a way to show my peers that there was a path forward to a healthier life,” she says.
“My mission in life is to help peers gain their confidence, happiness, and ability to live a happy life through forming a connection and by letting them choose their path to wellness.”
NEWS 22 Fall 2018 E COMMENTARY 22 NEWS . Winter 2022
Vermonters held “Out of the Darkness” walks in Burlington, Rutland, Newport, Brattleboro and Montpelier this fall to call attention to the need for suicide prevention. Above, marchers file along the sidewalk in Burlington. (Counterpoint Photos: Brett Yates)
NEW STAFF ANNOUNCED
VPS Reviews Challenges, Efforts Supporting Peers
RUTLAND – In its first in-person annual membership meeting since the COVID pandemic, Vermont Psychiatric Survivor’s Executive Director, Karim Chapman, told the staff and board members present not to be discouraged by the small turnout.

“There is some great work happening in the state because of what we do,” he said.
A lengthy afternoon discussion focused on the lack of participation, since VPS is a membership organization, but not enough members came to allow a quorum for voting on bylaws changes or board terms.
A subcommittee was established to address how to get the word out and to engage with the community.
In his comments, Chapman reflected that there were “a lot of people out there suffering every day,” and staff were helping peers to navigate the system and get the supports they needed.
“We had a rough time” as an organization in the past year, he said, with “some tornadoes that came our way. But we are here surviving; we are still here.”
He said that VPS has “lost its name” in terms of community awareness, but is doing active outreach in the community to rebuild and to be “advocating and fighting for people who don’t have a voice.” VPS needs to be “fighting for more funding” in order to hire more staff for the work it
needs to be doing, he said.
“We all need to play a role getting the word out.”
Several staff also spoke about their work.
“I love what we do,” said peer outreach worker Walt Wade. “We’re there for the people who need us.” When you talk to peers, he said, “it makes you really aware how tough it is out there.”
Stephanie Kacanich described herself as “a fierce advocate for my peers in mental health and my peers in recovery” –but also for the people working with them.
“I have had too many friends die of this [drug] epidemic,” she said, because of “not seeing a way out; not having a hand to hold; seeing the only way out as suicide.”
She stressed that people don’t need support that is “one time and then we leave you,” but instead, knowing they can rely on someone being there for them. “I have my phone on all the time,” she noted.
The newest staff member, Mariah Sullivan, said she brought her lived experience as well as years of working on the clinician side of the mental health system.
From both perspectives, she could “see so many of the flaws that are in the mental health system,” and she wants to help address them, she said.
Membership Has Real Power!
By ZACHARY HUGHES, VPS Board Member
Have you ever seen this?
“We are having a membership meeting.”
“Come renew your membership.”
Why does it matter? VPS is a membership-driven organization. A member has obligations and has power! What obligations and power?
Our membership is empowered to: act on matters brought before them; elect members to our board of directors; and approve or reject changes in our bylaws. The membership holds VPS accountable to our community! You are the stakeholders! If this were corporate you would be shareholders!
Here is example of why the membership matters. Someone had suggested getting rid of the position of Executive Director at VPS. At the time the bylaws had no section on an Executive Director. The person had made a compelling argument. Thankfully the board rejected the idea, although they could have gone the other way. To prevent this from occurring in the future I inserted proposed language in the bylaws that requires VPS to have an Executive Director. The bigger point here is now the membership would have to approve undoing this; that’s YOU!
I urge you to learn more about membership at VPS: visit our website https://www. vermontpsychiatricsurvivors.org/members/aboutmembership/ or call the VPS Office 802-775-6834. Interested
Be a leader in the psychiatric survivor and peer movement!
Contact the board chair, Sara Merrow at merrowsara@gmail.com for more information and how
Former Peer Support Worker Is Honored
RUTLAND – Vermont Psychiatric Survivors board members offered a tribute to longtime staff advocate Amy Wales at the opening of the organizations Annual Meeting this past fall.

Wales was a peer support worker at Second Spring, an intensive recovery residence, for 10 years before her death on July 8, 2022.
Marty Roberts called Wales “one of the best friends I ever had” and “a tireless advocate for people at Second Spring.” When she became ill, an eagle became her totem, Roberts said, and “she trusted her wings” – referencing the opening of her obituary. The obituary was on display for the meeting and was read aloud by Roberts.

It included a comment from a co-worker at Second Spring, who said, “Amy believed in their strengths, and advocated tirelessly in support of their rights, especially when the system failed them.”
“Her unbridled empathy, the product of a neverhardened, pure and delicate spirit, enabled her to relate to others who suffered emotional and physical trauma,” the obituary said.
She was gifted with a sense of wit, it said. It went on to also note
her son, Patrick, as the pride and joy of her life.
After the tribute to Wales, several others rose to offer remembrances of others who were close to them and passed away. “How we deal with death is as important as how we deal with life,” said board member Zack Hughes.
NEWS 23 Fall 2018 Winter 2022 NEWS 23
VPS Board president Sara Merrow holds an enlarged copy of Amy Wales’ obituary as board member Marty Roberts reads it aloud.
Board members, staff and several other members of Vermont Psychiatric Survivors joined in a discussion about how to increase membership during the annual meeting
Wales
Amy
Articles and photos of the VPS Annual meeting by Anne Donahue.
in being a board member for Vermont Psychiatric Survivors? Your help is welcomed and needed!
to apply.
SURVIVOR PEER SERVICES
Vermont Psychiatric Survivors
VPS is a membership organization providing peer support, outreach, advocacy and education 128 Merchants Row, Suite 606, Rutland, VT 05701 802-775-6834 www.vermontpsychiatricsurvivors.org
VPS OUTREACH AND PATIENT REPRESENTATIVES (800) 475-4907 info@vermontpsychiatricsurvivors.org
WARM LINE
VERMONT SUPPORT LINE (STATEWIDE): 833-888-2557; 24 hours, 365 days [833-VT-TALKS]
By call or text
CRISIS RESPITE
Alyssum, 802-767-6000; www.alyssum.org; info@alyssum.org
HOSPITALIZATION ALTERNATIVE Soteria House, information and online application at www.pathwaysvermont.org/what-we-do/ our-programs/soteria-house/ or call Pathways Vermont Intake Line, 888-492-8212, ext. 140
Peer Centers & Employment Support
ANOTHER WAY
125 Barre St, Montpelier, 802-229-0920; info@anoth erwayvt.org; www.anotherwayvt.org; see website for events calendar.
PATHWAYS VERMONT COMMUNITY CENTER 279 North Winooski Avenue, Burlington, 802-777-4633; pvcc@pathwaysvermont.org www.facebook.com/PathwaysVTCommunityCenter; www.pathwaysvermont.org/what-we-do/ our-programs/pvcc
Some Peer Centers and Recovery Centers may have changed hours as a result of COVID-19 crisis. Call to check on up-to-date schedules.
Vermont Recovery Centers
WWW.VTRECOVERYNETWORK.ORG
BARRE, Turning Point Center of Central Vermont, 489 N. Main St.; 479-7373; www.tpccv.org; tpccvbarre@ gmail.com
BENNINGTON, Turning Point Center, 160 Belmont Dr; 802-442-9700; info@tpcbennington.orgBRATTLE BORO, Turning Point Center of Windham County, 39 Elm St.; 802-257-5600; tpwc.1@hotmail.com
BURLINGTON, Turning Point Center of Chittenden County, 179 South Winooski Ave, Suite 301; 802-8613150; www.turningpointcentervt.org or support@ turningpointcentervt.org
MIDDLEBURY, Turning Point Center of Addison County, 5 A Creek Rd; 802-388-4249; info@turningpointaddi sonvt.org
MORRISVILLE, North Central Vermont Recovery Cen ter, 275 Brooklyn St., 802-851-8120; JOHNSON, 117 St. John’s St. 802-730-8122; recovery@ncvrc.com
NEWPORT, Journey to Recovery Center, 212 Prouty Dr. 802-624-4156
JOHNSON, Jenna’s Promise, 114 St. John’s Rd, 802343-8741; info@jennaspromise.org
RUTLAND, Turning Point Center, 141 State St; 802-7736010; turningpointcenterrutlandvt.org
SPRINGFIELD, Turning Point Recovery Center of Springfield, 7 Morgan St., 802-885-4668; webadmin@ spfldtp.org; www.spfldtp.org
ST. ALBANS, Turning Point of Franklin County, 182 Lake St; 802-782-8454; contacta@turningpoint franklincounty.org
ST. JOHNSBURY, Kingdom Recovery Center, 297 Sum mer St; 802-751-8520; recoveryinfo@stjkrc.org; www. kingdomrecoverycenter.com
WHITE RIVER JUNCTION, Upper Valley Turning Point, 200 Olcott Dr; 802-295-5206; www.uppervalleyturn ingpoint.org; info@secondwindfound.org
SUICIDE & CRISIS LIFELINE 988
24/7 support
Samaritans Hotline 877-870-HOPE (4673)
Crisis Text Line
Around the clock help via text: 741-741 for a reply explaining ground rules; message routed to a trained counselor.
Vermont Federation of Families for Children’s Mental Health
Statewide support for families of children, youth or young adults in transition who are experiencing or at risk to expe rience emotional, behavioral or mental health challenges. 800-639-6071, 802-876-7021; www.vffcmh.org
Pride Center of Vermont
LGBTQ Individuals with Disabilities Social and Sup port: Connections and support around coming out, socializing, employment challenges, safe sex, self-advo cacy. For center hours call (802) 860-7812 or go to www. pridecentervt.org
Brain Injury Association
Support Group locations on web: www.biavt.org; support@biavt.org; 802-244-6850
Trans Crisis Hotline
The Trans Lifeline (dedicated to the trans population) can be reached at 877-565-8860.
LGBTQ Youth Crisis Hotline: The Trevor Lifeline, 866-488-7386. TrevorText : 678-678
NATIONAL ALLIANCE ON MENTAL ILLNESS-VT (NAMI-VT): 802-876-7949 x101, or 800-639-6480; 600 Blair Park Road, Suite 301, Williston, 05495; www.namivt.org; info@namivt.org
Connections Peer Support Groups
Meetings are led by trained Peer Support Leaders. The groups provide a safe place that offers respect, understanding, encouragement, and inspires hope to all who attend. Zoom Meetings: Every Monday 7-8:30 p.m. and 1st & 3rd Tuesday 4-5:30 p.m. In-Person: Every Thursday from 3-4:30 p.m., Cathedral Church of St. Paul, 1st floor, Commons Room, 2 Cherry Street, Burlington. To learn more, visit: www.namivt.org/support-groups/peer-support/
Counterpoint publishes this resource directory to allow readers to seek out choices for support. Counterpoint has not reviewed or evaluated the quality or biases of these resources, and makes no representation about their value for any individual.
Public Community Mental Health
COUNSELING SERVICE OF ADDISON COUNTY, 89 Main St., Middlebury, 05753; www.csac-vt.org; 802-388-6751
UNITED COUNSELING SERVICE OF BENNINGTON COUNTY, PO Box 588, Ledge Hill Dr., Bennington, 05201; 802442-5491; 5312 Main St., Manchester, 802-3623950; www.ucsvt.org
CHITTENDEN COUNTY: HOWARD CENTER, 300 Flynn Ave., Burlington, 05401; 802-488-6000; www.howardcenter.org
FRANKLIN & GRAND ISLE: NORTHWESTERN COUNSELING AND SUPPORT SERVICES, 107 Fisher Pond Road, St. Albans, 05478; 802-524-6554; www.ncssinc.org
LAMOILLE COUNTY MENTAL HEALTH SERVICES, 72 Harrel Street, Morrisville, 05661; 802-888-5026; www.lamoille.org
NORTHEAST KINGDOM HUMAN SERVICES, 181 Crawford Road, Derby; 802-334-6744; 2225 Portland St., St. Johns bury; 802-748-3181; www.nkhs.org
ORANGE COUNTY: CLARA MARTIN CENTER, 11 Main St., Randolph, 05060-0167; 802-728-4466; www.claramartin.org
RUTLAND MENTAL HEALTH SERVICES, 78 So. Main St., Rutland, 05701; 802-775-2381; rmhsccn.org
WASHINGTON COUNTY MENTAL HEALTH SERVICES, 9 Heaton St., Montpelier, 05601; 802-223-6328; www.wcmhs.org
WINDHAM AND WINDSOR COUNTIES: HEALTH CARE AND REHABILITATION SERVICES OF SOUTHEASTERN VERMONT, 390 River Street, Springfield, 05156; 886-4500; 51 Fair view St., Brattleboro, 05301, 802-254-6028; 49 School St., Hartford, 05047, 802-295-3031; www.hcrs.org
24-Hour Crisis Lines and Involuntary Custody Screening
ADDISON COUNTY: Counseling Services of Addison County 802-388-7641
BENNINGTON COUNTY: United Counseling Service, 802442-5491; (Manchester) 802-362-3950
CHITTENDEN COUNTY: Howard Center, 802-488-7777
FRANKLIN AND GRAND ISLE COUNTIES: Northwestern Counseling and Support Services, 802-524-6554; 800-834-7793
LAMOILLE COUNTY: Lamoille County Mental Health, Week days 8 a.m.-4 p.m. 802-888-5026; Nights and weekends 802-888-8888
ESSEX, CALEDONIA AND ORLEANS: Northeast Kingdom Human Services 802-334-6744
ORANGE COUNTY: Clara Martin, 800-639-6360
RUTLAND: Mental Health Services, 802-775-1000
WASHINGTON COUNTY: Mental Health Services, 802-229-0591
WINDHAM,WINDSOR COUNTIES: Health Care and Rehabili tation Services, 800-622-4235
Vermont Veterans Outreach
BENNINGTON AREA: 802-442-2980; cell: 802-310-5391
BERLIN AREA: 802-224-7108; cell: 802-399-6135
BRADFORD AREA: 802-222-4824; cell: 802-734-2282
COLCHESTER AREA: 802-338-3078; cell: 802-310-5743
ENOSBURG AREA: 802-933-2166; cell: 802-399-6068
JERICHO AREA: 802-899-5291; cell: 802-310-0631
NEWPORT AREA: 802-338-4162; cell: 802-399-6250
RUTLAND AREA: 802-775-0195; cell: 802-310-5334
VERGENNES AREA: 802-877-2356; cell: 802-881-6680
WHITE RIVER AREA: 802-295-7921; cell: 802-881-6232
WILLISTON AREA: 802-879-1385; cell: 802-734-2123
Homeless?
Vermont Veterans Services (VVS) program for homeless veterans with very low income, call 802-656-3232.
www.MakeTheConnection.net
OUTREACH TEAM LEADER: 802-338-3022; cell: 802-881-5057
TOLL-FREE HOTLINE (24/7) 1-888-607-8773
VA Mental Health Services
VA HOSPITAL: Toll Free 1-866-687-8387
MENTAL HEALTH CLINIC: Toll Free 1-866-687-8387 Ext 6132
OUTPATIENT CLINICS: Bennington: 802-447-6913; Brattle boro: 802-251-2200; Burlington Lakeside Clinic: 802-6577000; Newport: 802-334-9777; Rutland: 802-772-2300
VET CENTERS: (Burlington) 802-862-1806; (White River Jnct) 802-295-2908
Please contact us if your organization’s information changes: counterpoint@vermontpsychiatricsurvivors.org
Web site sponsored by The Department of Veterans Affairs with testimonials by veterans to help connect with the experiences of other veterans, and with infor mation and resources to help transition from service, face health issues, or navigate daily life as a civilian. Veterans’ Services HOMELESS PROGRAM COORDINATOR: 802-742-3291 BRATTLEBORO: Morningside 802-257-0066 RUTLAND: Open Door Mission 802-775-5661; Transi tional Residence: Dodge House, 802-775-6772 BURLINGTON: Waystation/Wilson 802-864-7402
TRANSPORTATION: Disabled American Veterans: Toll Free: 1-866-687-8387 X5394
FREE
Resources Directory 24
Winter 2022




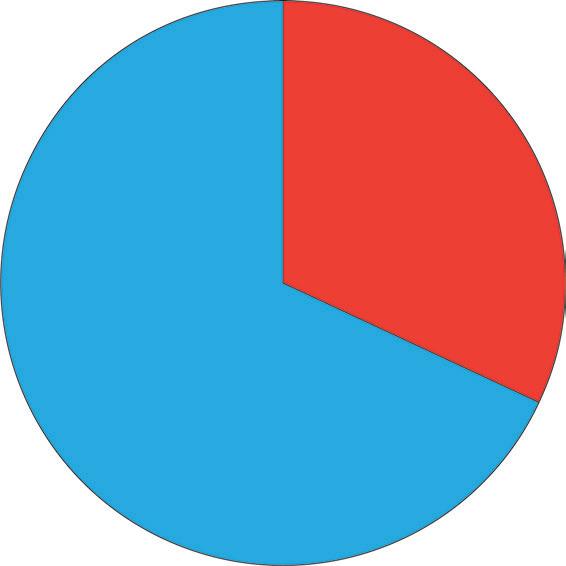







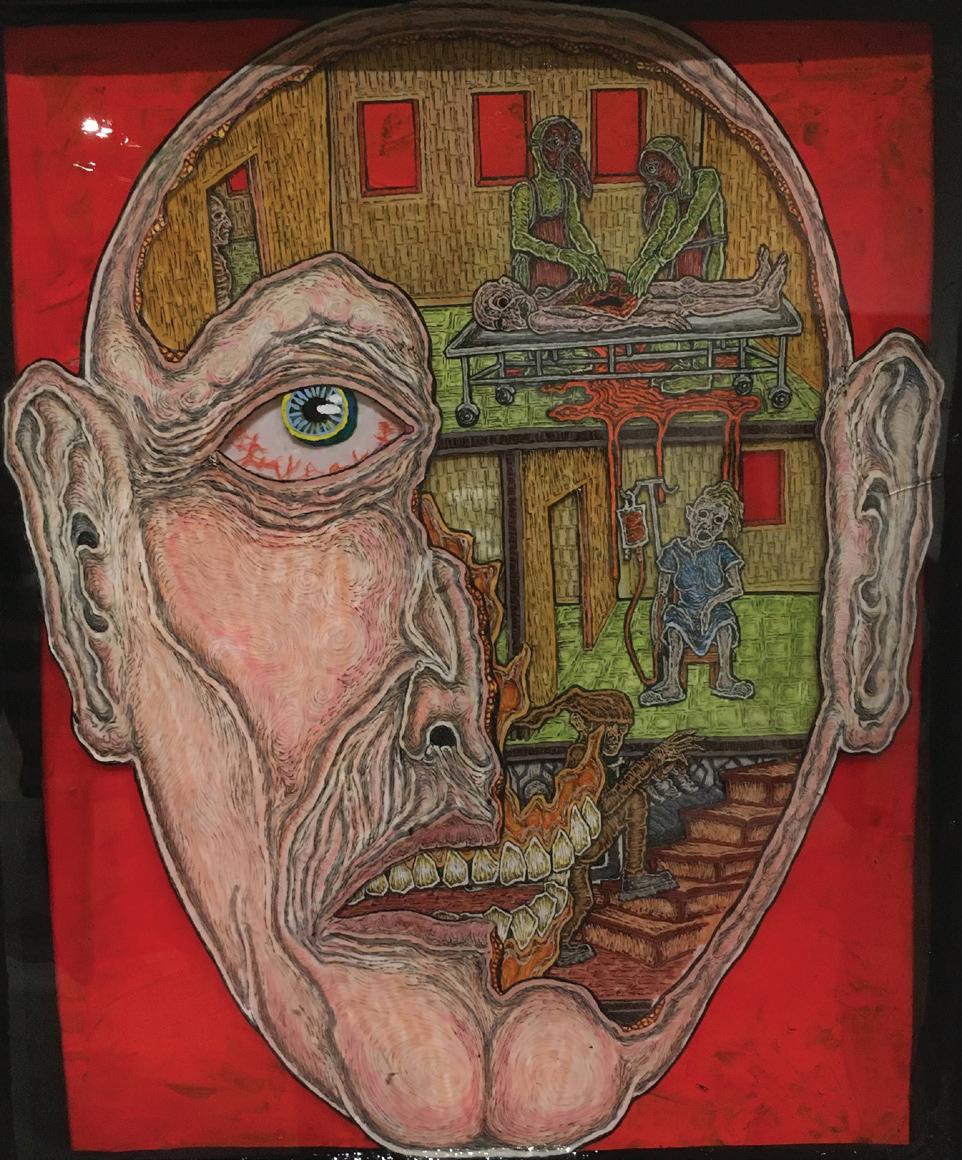 By BRETT YATES
By BRETT YATES
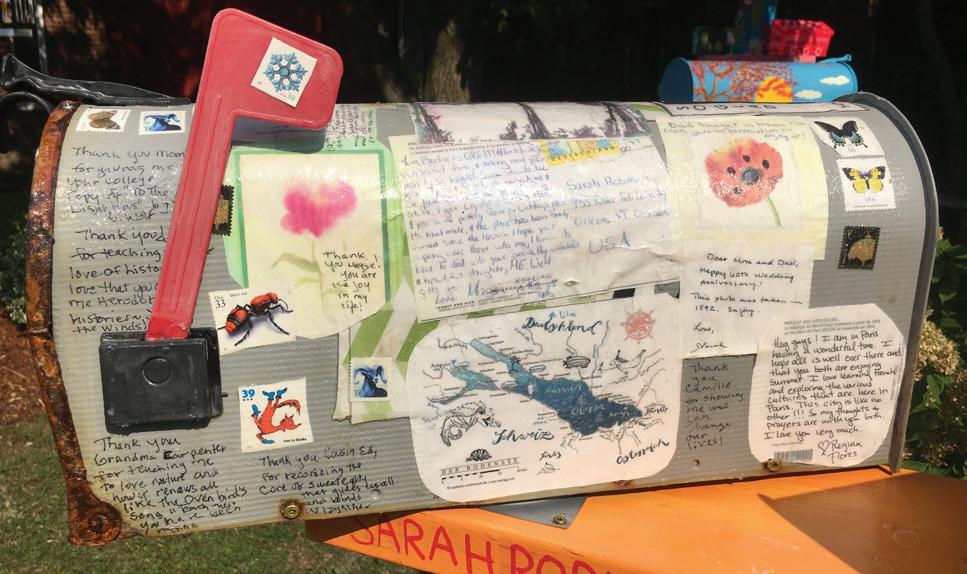


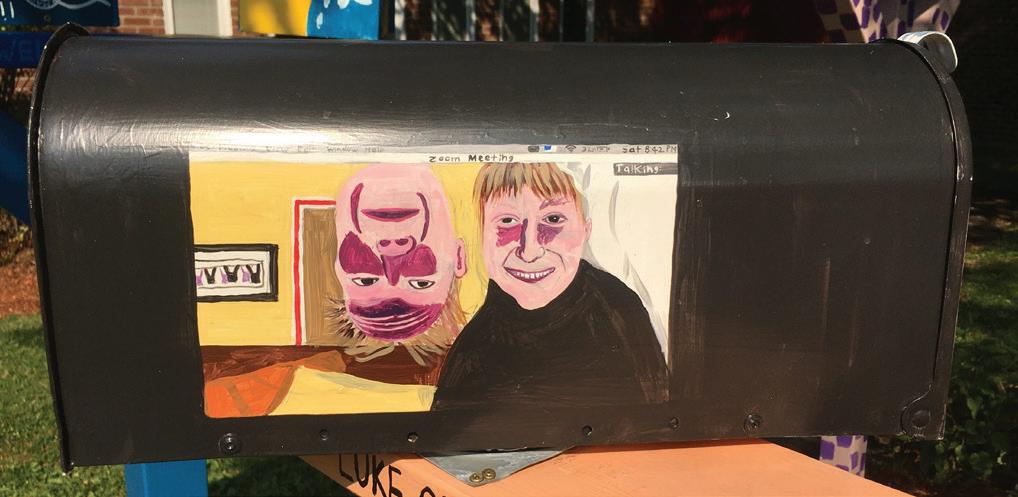













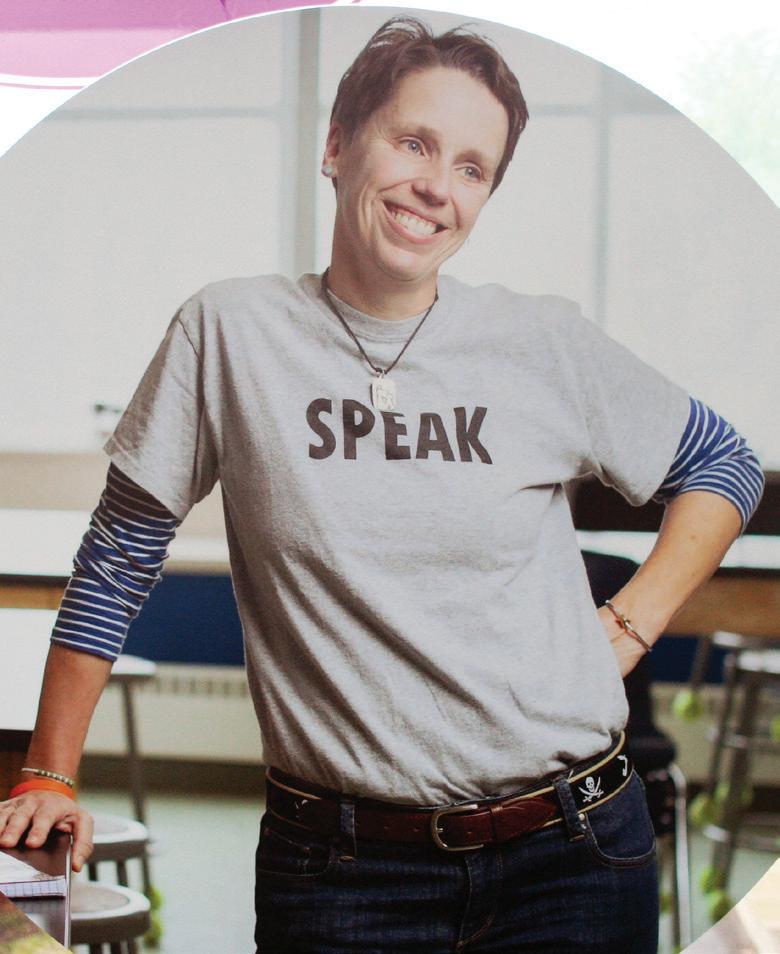




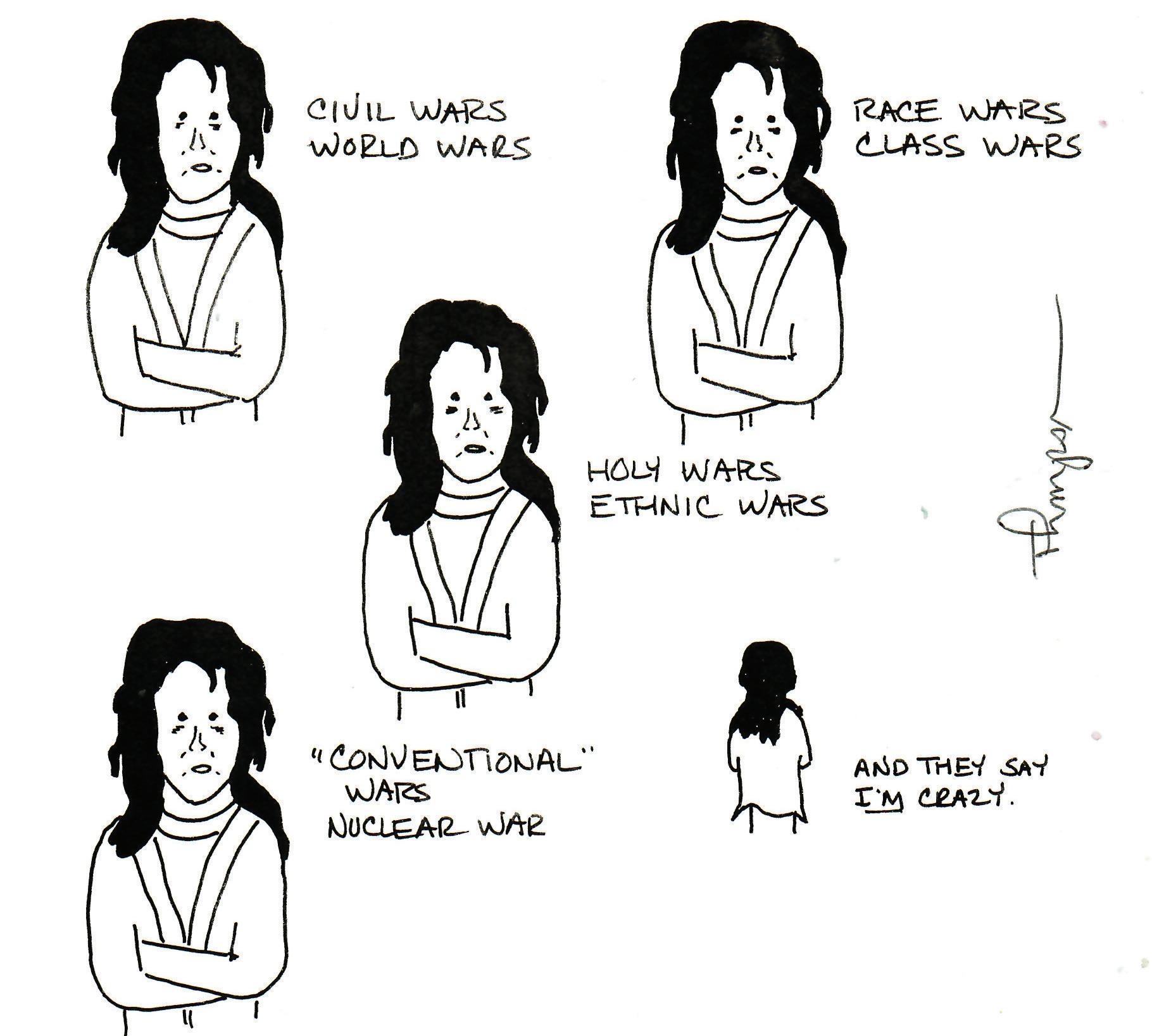




 By DAVID MCKAY
By DAVID MCKAY


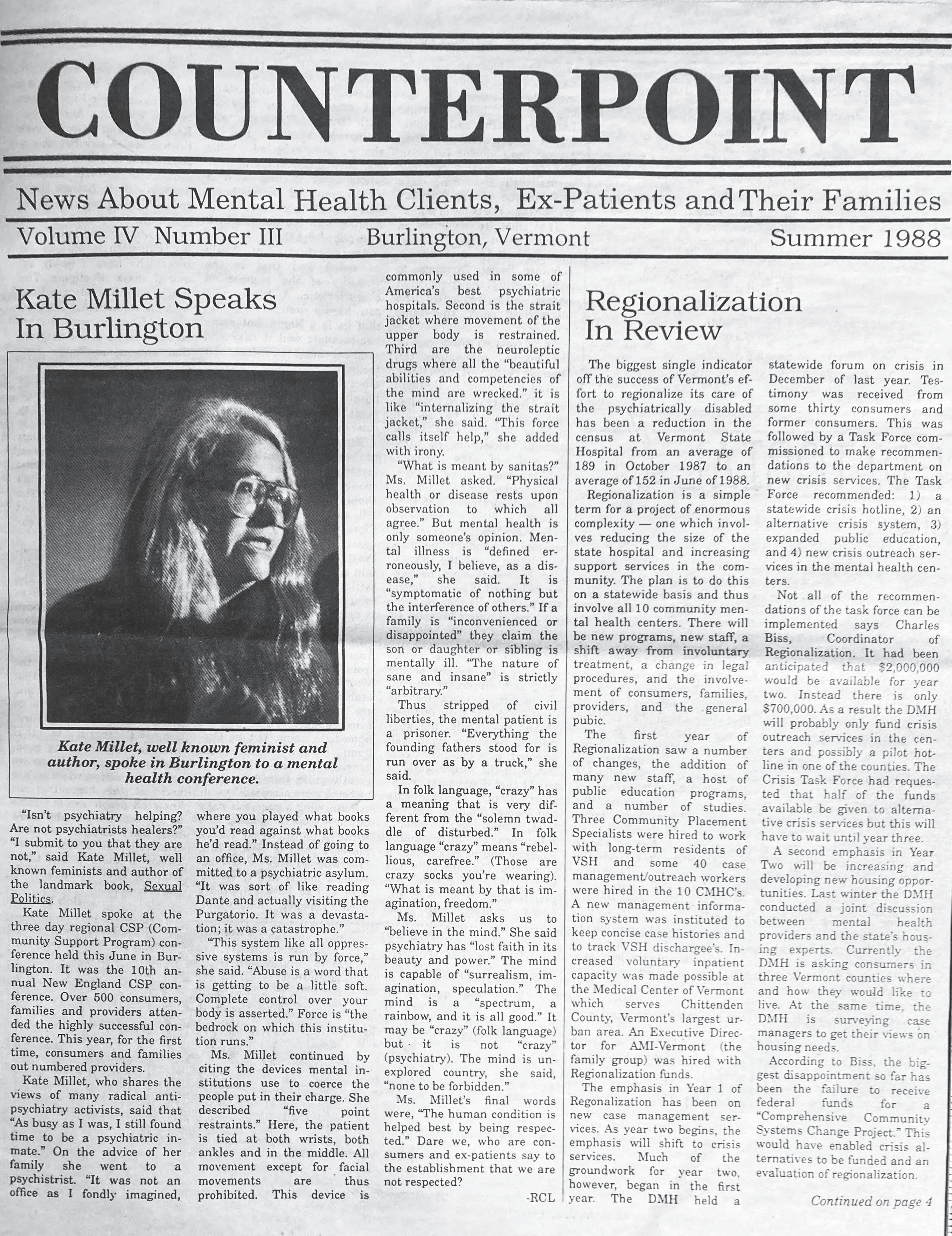


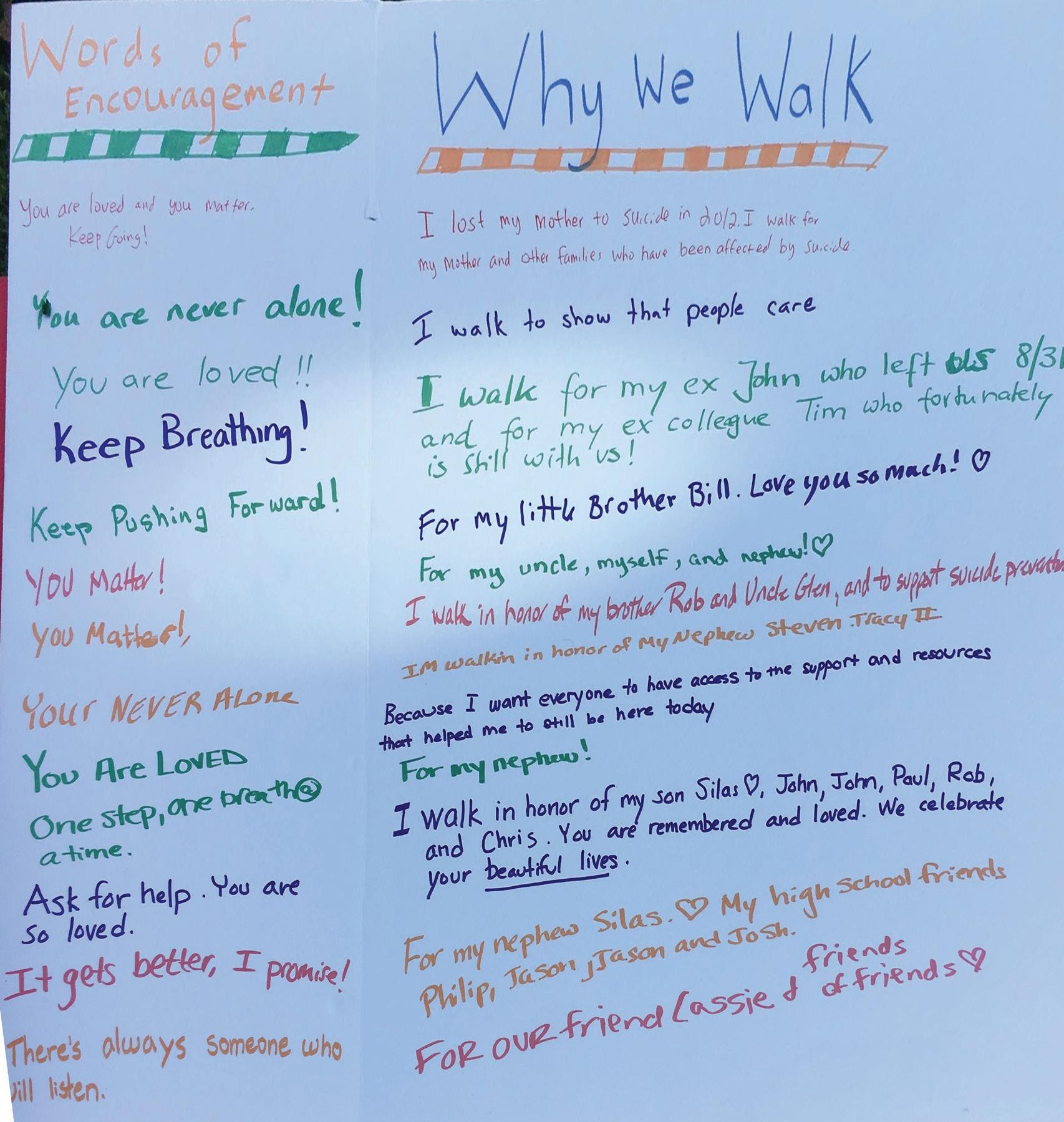 By BRETT YATES
By BRETT YATES





