Battle Erupts on Hotel Evictions
by ANNE DONAHUE
MONTPELIER – Some 2,800 individuals, including children, who have been housed at hotels during the COVID pandemic face losing shelter by July 1, leading to a contentious political battle over the state’s budget and its responsibility to keep a safety net in place.
In late May, the administration announced new steps to make the transition less abrupt, and
on May 30, the Vermont Legal Aid announced a lawsuit to attempt to block the evictions. Those actions leave many individuals with uncertainty about what may happen, and when.
A single mother with two children living in a hotel in Berlin, who identifies as a person who has experienced mental health challenges, has taken a leading role in gathering testimonials and sending them to legislators from others around the state feeling desperation about imminent homelessness.
“Many people are going to die, including myself and children,” Rebecca Duprey wrote. “Do people’s lives really mean that little to you? Continuing to fund housing while creating permanent housing will save
lives.” Duprey is one of five hotel residents named as class action representatives in the Legal Aid lawsuit.
The prospect of a massive surge of unsheltered Vermonters drove a group of legislators in the House to vote against the state’s budget for the coming year based on its failure to extend the emergency hotel program until alternative housing is found for current residents.

That could set up a further showdown if those legislators block a veto override vote on June 20. They wanted more money allocated to keep the motel program open until alternatives are in place, but the governor vetoed the budget saying it already spent too much, resulting in new taxes.
People with psychiatric disabilities are among those now facing a return to homelessness and some advocates have said that among the repercussions will be an increase in emergency room use. “They’re getting dumped, and [being told] ‘where you fall is where you fall,’” said Vermont Psychiatric Survivor Executive Director Walt Wade. VPS has been sending outreach staff
‘I’ve Got To Walk the Walk’
by ANNE DONAHUE
news, she is the consummate professional: composed, articulate, relaxed.
That reflects a large part of how she sees herself. As her high school’s class valedictorian and someone who “strives for perfection,” she said she was “taught as a woman and as a professional that [one] can be branded as weak or sensitive or outof-control” if feelings are exposed.
Guessferd knew the experience of being branded, because she was hospitalized several times in her high school and college years, diagnosed with PTSD and anxiety and living through wearing “the scarlet letter” as she walked through the hallways with her head down.
“I knew that everyone knew,” she said.
By 2018, with help from a course of dialectical behavioral therapy in college, Guessferd had pulled away from her symptoms and had entered the world of broadcast journalism, living her dream to be a writer and “tell people’s stories.”
Then COVID hit. Guessferd found herself reporting on how others were experiencing the pandemic but keeping her own challenges siloed away and wondering, “was I the only person to struggle?”
She found herself deeply depressed and unmotivated and felt she had lost the love of her job.

“Rock bottom is such a lonely place,” she reflected in her interview with Counterpoint. “At the end of the day, it’s you and yourself.”
Finally, one day, she walked into her boss’ office to say, “I can’t do this. I need help.”
She felt like a failure and was terrified she was going to ruin her reputation.
Instead, her supervisor offered her the potential of taking time off under the federal medical leave act, telling her it was “an option that you have a right to.”

That had never occurred to her.
“You think of a physical, debilitating condition” as the basis for a medical leave, Guessferd said, but that’s a misconception. The support from her work environment “was truly the cornerstone” for recovery.
She kept doubting the validity of taking the
(Continued on page 4)
BURLINGTON – When Christina Guessferd takes to the air as co-anchor on the WCAX nightly
NEWS, COMMENTARY, AND ARTS BY PSYCHIATRIC SURVIVORS, MENTAL HEALTH PEERS, AND OUR FAMILIES VOL. XXXVIII NO. 1 • FROM THE HILLS OF VERMONT • SINCE 1985 • SUMMER 2023 22 Editor Says Farewell 14 The Arts 5
VPS
New
Executive Director
Christina Guessferd, WCAX Reporter and Producer
(Photo by Anne Donahue)
Vermont Psychiatric Survivors Board Vice-President Zachary Hughes testifies before the House Judiciary Committee in April.
(Photo by Anne Donahue) (Continued on page 27)
Peer Leadership and Advocacy
Meeting Dates and Membership Information for Boards, Committees and Conferences
Peer Organizations State Committees
VERMONT PSYCHIATRIC SURVIVORS BOARD
A membership organization providing peer support, outreach, advocacy and education. Board meets monthly. For information call 802-775-6834 or email info@vermontpsychiatricsurvivors.org.
COUNTERPOINT EDITORIAL ADVISORY BOARD
The editorial advisory board for the Vermont Psychiatric Survivors newspaper can always use help! Assists with policy, editing and brainstorming on topics for articles. Contact counterpoint@vermontpsychiatricsurvivors.org
ALYSSUM Peer crisis respite. To serve on board, call 802-767-6000 or write to information@alyssum.org
DISABILITY RIGHTS VERMONT PAIMI COUNCIL
Protection and advocacy for individuals with mental illness. Call 1-800-834-7890.
ADULT PROGRAM STANDING COMMITTEE
Advises the Commissioner of Mental Health on the adult mental health system. The committee is the official body for review of and recommendations for redesignation of community mental health programs (designated agencies) and monitors other aspects of the system. Members are persons with lived mental health experience, family members, and professionals. Meets monthly on 2nd Monday, noon-3 p.m. Check DMH website www.mentalhealth.vermont.gov or call-in number. For further information, contact member Daniel Towle (dantowle@comcast.net) or the DMH quality team at Eva.Dayon@vermont.gov
LOCAL PROGRAM STANDING COMMITTEES
Advisory groups, required for every community mental health center. For membership or participation, contact your local agency for information (listings on back page.)
Advocacy Organizations
DISABILITY RIGHTS VERMONT
Advocacy in dealing with abuse, neglect or other rights violations by a hospital, care home, or community mental health agency. 141 Main St, Suite 7, Montpelier VT 05602; 800-834-7890. disabilityrightsvt.org
VERMONT CENTER FOR INDEPENDENT LIVING
Peer services and advocacy for persons with disabilities. 800-639-1522. vcil.org
HEALTH CARE ADVOCATE To report problems with any health insurance or Medicaid/Medicare issues in Vermont 800-917-7787 or 802-241-1102. vtlawhelp.org/health
VERMONT CLIENT ASSISTANCE PROGRAM
Rights when dealing with service organizations such as Vocational Rehabilitation. Box 1367, Burlington VT 05402; 800-747-5022.
NAMI-VT
Family and peer support services, 802-876-7949 x101 or 800-639-6480; 600 Blair Park Road, Suite 301, Williston VT 05495; www.namitvt.org; info@namivt.org
PEER WORKFORCE DEVELOPMENT INITIATIVE
Webpage provides an up-to-date account of statewide peer training and registration information as well as updates about its progress and efforts. www.pathwaysvermont. org/what-we-do/statewide-peer-workforce-resources/ MADFREEDOM
MadFreedom is a human and civil rights membership organization whose mission is to secure political power to end discrimination and oppression of people based on perceived mental state. See more at madfreedom.org
MENTAL HEALTH LAW PROJECT
Representation for rights when facing commitment to a psychiatric hospital. 802-241-3222.
ADULT PROTECTIVE SERVICES
Reporting of abuse, neglect or exploitation of vulnerable adults, 800-564-1612; also to report violations at hospitals/nursing homes through Licensing and Protection at (802) 871-3317
Hospital Advisory
VERMONT PSYCHIATRIC CARE HOSPITAL
Advisory Steering Committee, Berlin, check DMH website for dates at www.mentalhealth.vermont.gov
RUTLAND REGIONAL MEDICAL CENTER
Community Advisory Committee, fourth Mondays, noon, call 802-747-6295 or email lcathcart@rrmc.org
UNIVERSITY OF VERMONT MEDICAL CENTER
Program Quality Committee, third Tuesdays, 9-10 a.m., for information call 802-847-4560.
ACTIVE MINDS CONFERENCE
BRATTLEBORO RETREAT
Consumer Advisory Council, fourth Tuesdays, 12-1:30 p.m., contact Director of Patient Advocacy and Consumer Affairs at 802-258-6118 for meeting information.
CENTRAL VERMONT MEDICAL CENTER NEWLY forming. Contact counterpoint@vermontpsychiatricsurvivors.org for more information. Every other month, 4th Tues, 11-12.
Conferences
Calling it “the nation’s leading mental health conference for young adults,” Active Minds will host its 2023 conference in Washington, D.C., July 7-8. For more information go to: www.activeminds.org/programs/national-conference-2023/speakers/
ABCT 2023 CONFERENCE
The Association for Behavioral and Cognitive Therapies (ABCT) 2023 conference will be held November 16-19 in Seattle. Its theme is “Cultivating Joy with CBT [Cognitive Behavioral Therapy].” For more information, go to: www.abct.org/convention-ce/
NARPA 2023 CONFERENCE
The 2023 conference of the National Association for Rights Protection and Advocacy (NARPA) will be held in New Orleans September 6-9. For more information, go to: narpa. org/conferences/narpa-2023/ Conference Keynoters include Ira Burnim, J.D., Director, Bazelon Center for Mental Health Law; David Cohen, Ph.D., Professor and Associate Dean, Luskin School of Social Work, UCLA; Working for Racial Justice and Equity: panel presentation led by Kwamena Blankson, J.D., NARPA President; Innovative Non-Police Responses in Crisis Situations, group presentation; Robert Dinerstein, J.D., American University Washington College of Law, Annual updates on recent cases affecting disability rights/mental health law.
VT Psychiatric Survivors, 128 Merchants Row Suite 606, Rutland, VT 05701
Phone: (802) 775-6834
email: counterpoint@ vermontpsychiatricsurvivors.org
MISSION STATEMENT:
Counterpoint is a voice for news and the arts by psychiatric survivors, ex-patients, and consumers of mental health services, and our families and friends.
Copyright 2021, All Rights Reserved
FOUNDING EDITOR
Robert Crosby Loomis (1943-1994)
EDITORIAL BOARD
Kara Greenblott, Zachary Hughes, Joanne Desany, Sara Neller, Laura Shanks
The Editorial Board reviews editorial policy and all materials in each issue of Counterpoint. Review does not necessarily imply support or agreement with any positions or opinions.
PUBLISHER
Vermont Psychiatric Survivors, Inc.
The publisher has supervisory authority over all aspects of Counterpoint editing and publishing.
EDITOR
Anne B. Donahue
Brett Yates, Co-Editor
Opinions expressed by columnists and writers reflect the opinion of their authors and should not be taken as the position of Counterpoint
Counterpoint is funded by the freedom-loving people of Vermont through their Department of Mental Health. Financial support does not imply support, agreement or endorsement of any of the positions or opinions in this newspaper; DMH does not interfere with editorial content.
Counterpoint is published by Vermont Psychiatric Survivors three times a year, distributed free of charge throughout Vermont, and also available by mail subscription. Vermont Psychiatric Survivors is an independent, statewide mutual support and civil rights advocacy organization run by and for psychiatric survivors. The mission of Vermont Psychiatric Survivors is to provide advocacy and mutual support that seeks to end psychiatric coercion, oppression and discrimination. Counterpoint does not use pseudonyms in its reporting without stating that a pseudonym is being used and without an explanation for why the person’s identity is not being disclosed. Counterpoint does not use anonymous sources under any circumstances.
Department of Mental Health
802-241-0090
www.mentalhealth.vermont.gov
For DMH meetings, go to web site and choose “more” at the bottom of the “Upcoming Events” column.
ADDRESS: 280 State Drive NOB 2 North Waterbury, VT 05671-2010
c Enclosed is $10 for 3 issues (1 year).
c I can’t afford it right now, but please sign me up (VT only).
c Please use this extra donation to help in your work. (Our thanks!)
Checks or money orders should be made payable to “Vermont Psychiatric Survivors.” Send to: Counterpoint, Vermont Psychiatric Survivors, 128 Merchants Row, Suite 606, Rutland, VT 05701
Access Counterpoint online at www.vermontpsychiatricsurvivors.org
Fall 2018
2
Don’t Miss Out on a Counterpoint!
NAME ADDRESS CITY • STATE • ZIP Mail delivery straight to your home — be the first to get it, never miss an issue.
-
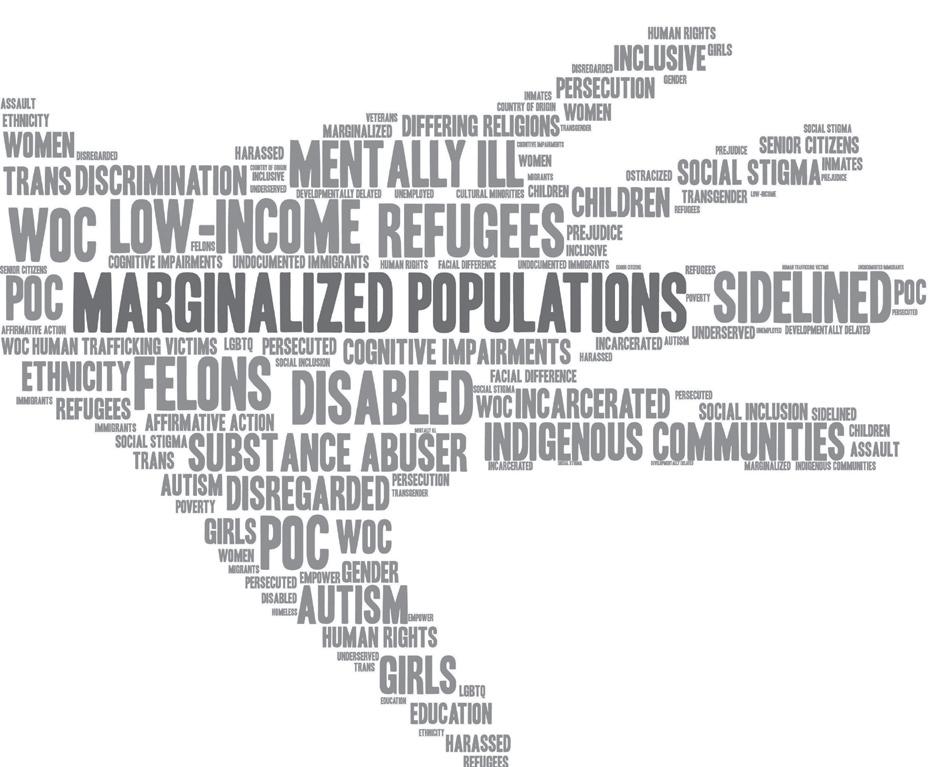
VERMONT MAD PRIDE is a march and celebration organized by psychiatric survivors, consumers, mad people, and folks the world has labeled “mentally ill.”


MAD PRIDE is about shedding shame, challenging discrimination, advocating for rights, affirming mad identities, remembering and participating in mad history, and having fun. Our lives and contributions are valuable and need celebration!
DATE: July 15, 2023
TIME: 1 PM - March 2-4 PM - Program



LOCATION: Battery Park
Burlington, VT
SPEAKERS (TO DATE):
ROUTE: Assemble at Hood Plant parking lot on King Street, between S. Winooski Avenue and Church Street and march to Battery Park.
PROGRAM: Spoken word, music, speeches, and more; Food and commemorative T-shirts provided
For more information: info@madpridevermont.org
Fall 2018 NEWS . 3 Summer 2023
Sera Davidow Director, Wildflower Alliance Bob Whitaker Author, Mad in America
Wilda L White Founder, MadFreedom
I’VE GOT TO WALK THE WALK • Continued from page 1 time for something that no one could see. “You can feel a lot of shame. It’s misplaced shame.”
It was her colleagues who told her, “You deserve it, don’t let anyone tell you otherwise.”
And it was the company’s Human Resources department that focused on what their employee needed, and why.
“What do you need from us?” they asked; “Take what you need.”
Going to her boss was really hard, she said. “It was scary.”
She feared the response would be, “you’re fired.” But Guessferd now reflects that “if that was how they handled it, I wouldn’t want to work here.”
She took 12 weeks off in all, six to center herself while on a waiting list for treatment, and then an intensive six-week course of DBT.
She was encouraged by her therapist, who told her, “What you need is more than what I can give,” and she recognized that she had lost what she had gained in the DBT skills she had learned in college.
“I was not exercising that muscle,” she said. She needed to “give myself the grace to take a breather and not feel I failed.”
Did she feel labeled by taking that time, as she had in her school years?
“At first, I did,” Guessferd said. But then she decided to write a public tweet to share her experience. She opened it by saying, “You may not have seen me on air” recently.
As a long-time mental health advocate, Guessferd said she recognized that “if I’m going to talk the talk, I’ve got to walk the walk.”
She believes in living with transparency, and if she expects others to ask for help, “I can do my part to let them know they are not the only one” by making her story public. Just because “you view the world a little differently” shouldn’t be a basis for discrimination, she said.
One of her transformational moments was when she started the DBT and, as she poured her heart out, received the advice that she should reconsider her diagnosis.
She looked at the list of symptoms for borderline personality disorder and found it resonated. “I have never felt so seen,” she said. It was “a day and a moment that I’ll never forget” because recognizing a diagnosis takes its power away. Rather than controlling her, she sees it as just one part of who she is.
The “white noise” may still be in her brain, causing “shame – guilt – fear – doubt,” and while “you can’t silence those thoughts,” you can analyze their validity. When her brain is leading her toward catastrophic symptoms, like “I’m blowing up my life,” she has learned to say, “I see you. Now go away.”
Guessferd said she has “learned to embrace and celebrate my mental illness and consider it my superpower,” because the so-called negative traits are also “part of what makes me, me.”
That is someone who is empathetic, compassionate, and fiercely loyal, with strong convictions, and who takes accountability for herself, she said.
Her ongoing challenge is making the
distinction between “who’s Christina the human being” and “who’s Christina the journalist,” telling the stories of other people without “losing my identity in the process.”
She “doesn’t want to sacrifice professionalism” by bringing her personal feelings or her own strong personal convictions into stories and needs to “navigate a career with the traits of myself that can be to my detriment,” she said. She fears that recognizing her “me” could influence her perspectives as a journalist, yet, “you can’t ignore what you are feeling.”
care of yourself” and be able to communicate one’s needs to others. Guessferd said that she works on how to “balance the formula” between therapy, medication and taking that time needed for self-care. She said she’s “baking with [that] recipe every day.”
Mental health also requires having empathy for others and understanding that every person is carrying their own story. It means needing to see that “everyone’s doing the best they can.”
Classmates who were mean to her in high school and college days, calling her “crazy” and “psycho” were too young to “have that wisdom to understand.”
It was her boss who told her she didn’t need to make that sacrifice, she just needed to “respect every other opinion out there” as well. He told her, “I never want to stifle that creativity” that makes her so good at what she does, Guessferd said.
Guessferd believes that her journey also taught her employer “the urgency of every employee taking care of themself.”
Putting oneself out publicly as a journalist makes one subject to criticism, so taking care of employees is crucial, she said.
It is a trend she sees starting in the larger society, as companies experiment with ideas on how to support their employees and begin to recognize that doing the best for one’s employees is also “doing what is best for the business.”
Guessferd said she has come to recognize that living with an illness is okay; it “makes you who you are. You can walk tall.” Developing the tools to do so can be painful, because one must “dig deep into the place you didn’t want to go.”
Instead of putting bandaids on a wound, it requires “cleaning out the wound – that’s painful,” she said. She remembers “being so scared of how much it’s going to hurt.” But in pulling away the bandaid, she said she found herself. It enables one “to be able to thrive as opposed to just surviving.”
“My job for my health is to make sure I have those tools” and to recognize that mental health requires that “you must carve out time to take
After one college episode in which she took off from the school and was picked up by ambulance to be taken to the hospital, the school conditioned her pending study abroad application on her taking DBT – which was highly positive for her.
But it also meant she was rejected by many friends who said, “I can’t deal with you anymore.” In the future, “I would hope they would ask questions instead of judging.”
Only two classmates were willing to ignore her “rumored reputation” and “would not let that taint their view of me.” They helped change her life and they remain best friends.
Guessferd said her experience with discrimination shows it can frequently be subtle: a doctor dismissing concerns about medication side effects, or family members saying someone is spoiled.

“It’s ingrained in us, that the pain of breaking a bone is more real.”
But she sees hope in the way society is talking more about mental health and with the help of science, the impact of mental health on physical health is being recognized.
Guessferd’s plea to others now is that if someone in their life is struggling, “Don’t just say you support them. Prove it.”
“Practice compassion, because if you practice judgment, it will escalate,” while compassion “will stay with you forever.”
Treat them “not with pity but as a human being,” she said. “You don’t have to talk with them about it,” Guessferd said. “Just be there.”
She likened it to holding one’s arms open and saying, “You don’t have to come in here, but you can if you like.”
Fall 2018 NEWS 4 Summer 2023
When her brain is leading her toward catastrophic symptoms, like “I’m blowing up my life,” she has learned to say, “I see you. Now go away.”
Christina Guessferd on a nightly news edition on WCAX in Burlington.
Counterpoint has a public comment section online! You can respond to any of our articles on our Wordpress at www.vermontpsychiatricsurvivors.org/counterpoint-articles/ !!!!!! WOW! Did you know?
(Photo by Anne Donahue)
ED Looks To Increase Advocacy
by ANNE DONAHUIE
RUTLAND – Walt Wade, a longtime advocate for youth and those with addictions who joined Vermont Psychiatric Survivors in 2020, has been named its new Executive Director.

He said his vision is “making VPS the agency that it should be” that “advocates [for] and protects people who can’t help themselves right now.”
“I remember being there,” he told Counterpoint. Counterpoint is published by VPS.
Wade identifies as a survivor who has been “through a whole life and all phases of addiction.”
There was a time in his life that he said he didn’t care about anyone else.
It was on March 12, 1982 that a moment in time changed his life. He went to drink at his usual bar and saw three men sitting at the same three seats where they sat every single day.
“Wow, that’s going to be me.”
He called the AA hotline. He is now 41 years sober. At the same time, he went from “taking advantage of everybody” to becoming “driven to help other people.”
“It was so strange to me,” he said.
Since then, he and his wife have been foster parents for some 40 years and adopted four of the teens who were in their care.
One of them died three years ago of an overdose, bringing the addiction crisis home once again.
Foster care started when he was asked to “do a favor” and take in a youth in crisis who needed a place for the weekend. Seven months later, he was still there.
“Our house was wild,” with as many as seven teenage boys living there at one time in a crisis placement. The youngest was nine, and he was one of the boys that Wade and his wife, Mary, adopted at age 13.
For 19 years, Wade worked for Rutland High School as the in-house suspension supervisor –a job he said he loved. “It was all the kids who acted like me” when he was younger, he said.
Meanwhile, he got his bachelor’s degree in human services.
In 2020, two weeks before the COVID pandemic closed down the state, Wade started a new job as the peer support outreach coordinator at VPS. Because everything changed with COVID, and hospitals were no longer accessible for offering peer support, the position lost its clear focus.
“COVID kind of changed what we did,” he said. Wade ended up taking on assorted roles helping with the VPS community links project in Rutland and with supporting individuals staying in the emergency hotel program.
“It has been eye-opening,” he said. “The thing I found… we had many, many people that were going to get left out” once the emergency ended. The resources now available don’t match with the needs of those who will be losing their hotel placements when the budget ends on July 1.
That crisis will require agencies around the state to work together to build a stronger system, and Wade wants VPS to become an active part of collaboration.
He wants to “show them that I care what we do as an agency and as a state… advocating for people in the state who are having a hard time.”
He told her how proud he was of her, and she started crying. “No one’s ever told me they were proud of me,” she said.
The challenges are harder when also dealing with the stigmatization of people with mental health diagnoses, Wade said, and he wants to make people more aware of those obstacles. VPS has an opportunity to make a difference for them, he added.
The staff at VPS all “know what it’s like to feel hopeless [and] looked at like ‘less than.’”
“It just kills me to see someone doing so well” and then see symptoms “kick up” but being unable to get help because of waiting lists.
Wade said it used to take several calls to connect someone with help, but now, even after eight or nine calls or more, he might still be unable to find the right services.
VPS is now getting back into hospital units to offer peer representative support, and there’s a lot of need to rebuild relationships, Wade noted. Staff have changed on both sides, and many of the nursing staff are “travelers,” meaning they are hired under temporary contracts.
“They have no clue” what VPS patient representatives are, he added.
VPS needs to rebuild its advocacy role as well, Wade said.
“We need to be in the middle of it,” he said. “You may help one person,” but that means there are likely 100 more facing the same challenges.
Wade said that includes being a voice in the legislature. The VPS board vice president, Zachary Hughes, began testifying this spring on critical rights issues.
An example Wade pointed to was a bill that would allow people who are waiting for care in an emergency department to be arrested if they get out-of-control.
“Nobody deserves to [go to] work and get hit and spit at,” he acknowledged, but people in a mental health crisis “are not their real selves” and “we’re punishing them.”
Wade pointed to one of the personal experiences he had doing outreach in being able to see what is possible.
Through another contact, he learned about a young woman who was sleeping in her car with her 5- and 7-year-old daughters in November. She was too afraid to ask for help out of fear that the Department of Children and Families would take the girls away from her.
Wade told her, “If you let me help you, they’re not going to take your kids.” He got her into a hotel, and she was able to find part-time work.
“She’s an excellent, excellent mother,” he said. “I believe she’s going to make it.”
He wants VPS to advocate “where people with mental health [labels] are getting shortchanged.” If the legislature “is making a law that hurts people, how is that ever right?”
He wants VPS to be an agency that “helps make laws that help” instead.
“People shouldn’t be punished for having a mental illness,” he noted.
Another example is the number of additional locked beds being added to the system, including plans for a new forensic unit.
That kind of planning is “probably because it’s easier” than building a stronger system of community supports, he reflected.
But, “how does it help?”
VPS Blocks Change to Law on Consent
MONTPELIER – A move to allow an advance directive to be explained remotely instead of in person was dropped by a legislative committee after testimony by Vermont Psychiatric Survivors.
The legislation addressed a type of advance directive that allows a person to lock themselves into a decision and forgo the right to object to a treatment if they are later found incompetent. Otherwise, laws require a court hearing to impose involuntary treatments.
The bill in the House Human Services Committee would have made permanent the current COVID exception, allowing remote witnessing for regular advance directive.
It proposed for the first time that the special “Ulysses clause” to allow treatment over objections – which requires added protection for witnesses and assurances that the person understands the decision – could be completed remotely as well.
Zachary Hughes, vice president of the board of VPS, said that the decision that is being made in those cases is so important, the in-person requirement should remain.
“It’s handing over power,” he said. “It’s about power. It’s about trust.”
The committee’s chair, Rep. Theresa Wood, responded by saying that his testimony was an example of how sometimes “a few short minutes
and a few short words can change one’s mind.”
She and some other members of the committee had expressed potential openness to make the change.
Immediately after Hughes’ testimony, Wood polled the committee, and the proposal was unanimously removed from the bill.
The Ulysses clause can be used by anyone writing an advance directive, but has generally been focused on being available to persons with a diagnosis of mental illness who might want to ensure they can receive a treatment in the future despite objecting after being found not competent to make a decision.
The bill is now in the Senate.
NEWS . 5 Fall 2018 NEWS Summer 2023 5
Walt Wade
His vision is “making VPS the agency that it should be” that “advocates [for] and protects people who can’t help themselves right now; where people with mental health [labels] are getting shortchanged.”
State Expands Urgent Care Sites
by BRETT YATES
WATERBURY — Projects intended to keep Vermonters out of emergency departments during mental health crises are coming to nearly every part of the state.
Of the 12 submissions generated last year by the Department of Mental Health’s request for proposals for mental health urgent care services, eight will receive funding, including seven brand-new programs.
Iterations of three different models of crisis care will move forward: psychiatric urgent care clinics (“PUC” or “PUCK”), community crisis centers (“Living Room”), and crisis response teams (“CAHOOTS”).
Using time-limited federal dollars, DMH has awarded grants to six of Vermont’s community mental health centers – Counseling Service of Addison County, Washington County Mental Health Services, Health Care & Rehabilitation Services of Southeastern Vermont, Lamoille County Mental Health Services, United Counseling Service, and Howard Center – and to the Burlington Police Department.
There is no clear plan yet as to how the programs will be sustained after the two-year federal grants expire in 2025.
CAHOOTS Model
Per city documents, BPD’s CAHOOTS-style crisis team will allow mental health clinicians and EMTs to “intervene in crisis situations where armed law enforcement is not necessary.”
Burlington allocated $400,000 for the program in its municipal budget for fiscal year 2023 and subsequently applied to DMH for funds to cover the difference between that sum and the estimated annual cost, between $800,000 and $950,000 in total.
The concept comes from Eugene, Oregon, which called it Crisis Assistance Helping Out On the Streets. Now labeled “Burlington CARES,” the model does not involve peers.
“After this two years, the city intends to fund this on their own, so we kept the model as it was as a whole,” DMH Deputy Commissioner Allison Krompf said.
Last year, the city’s plan included references to “qualified mental health professionals empowered to require emergency evaluations,” which serve to begin the process of involuntary hospitalization. At the time, Burlington expected to contract Howard Center, which employs QMHPs, to run the program. More recently, however, the city decided to manage the program in-house instead. That led DMH to “go back” and look at the proposal again, Krompf related.
“We want the person who’s responding to know what the threshold is for involuntary hospitalization, but we are not going so far now as to say that... they on their own could go out to the community and involuntarily hospitalize somebody,” she clarified. “So we did [tell] the Burlington PD that we wouldn’t authorize them in this program to be doing that.”
Urgent Care Model
PUC stands for Psychiatric Urgent Care, and PUCK stands for Psychiatric Urgent Care for Kids. These programs provide assessments by Masters-level clinicians, crisis de-escalation, and access to psychiatric consultation, according to Krompf. They can also
treat co-occurring medical needs of mild to moderate severity. Despite the model’s “clinical” focus, it “still comes with a space that’s much more well suited for people in a mental health crisis” than an emergency room, Krompf said.
DMH “has asked and required that there be peer supports” at each clinic, she noted, and those accepting pediatric patients will have “sensory spaces.”
“If you have a child or even an adolescent who’s really having a difficult time, putting them in a space where they can’t touch anything, and if they do, they can get in trouble… it’s just really tough,” Krompf said.

Pathways Vermont submitted a response to DMH to create a peer-run respite center but Krompf said that it didn’t meet the federal criteria for funding.
“We are really interested in finding a way to move that forward. We couldn’t use this bucket of money,” she said.
Living Room Model
The Living Room model, coming to Addison County and Washington County, intends to create a warm, homelike environment for patients. In DMH’s vision, this works to promote “autonomy, respect, hope, empowerment, and social inclusion.”
DMH said launch dates may vary by program.
UCS has run a PUCK clinic in Bennington since 2019. Its DMH grant will support the hiring of full-time staff and expanded operating hours, including evenings and possibly Saturdays, likely by July or sooner, per UCS.
According to UCS Executive Director Lorna Mattern, PUCK has “decreased emergency room utilization for children between 33% and 40%” in its catchment area.
“When kids would get picked up, often from school, by the police, they didn’t have anywhere else to go, and so they would often, if not always, end up in the emergency department. And I think what PUCK showed the state and funders and others is that we can create alternatives,” Mattern said.
“We can provide trauma-informed, familyfriendly, kid-friendly environments and still respond to a mental health crisis and help stabilize and keep them in the community.”
Howard Center’s PUC clinic in Burlington will serve adults only.
Krompf characterized the proposal as a collaboration that also included the University of Vermont Medical Center and the Community Health Centers of Burlington.
The University of Vermont Health Network is expected to be contributing about $8 million toward three years of operating costs and the initial space renovations to fill a funding gap beyond the DMH grant.
That money is part of a proposal for reuse of reserved funds that still needs approval by the Green Mountain Care Board. According to a submission by the health network, the DMH grant covers only $1.6 million over two years, while three years of operating costs will total about $7.65 million.
Psychiatrists and peers will work together in what Krompf called a “multidisciplinary team approach” for “person-centered care.”
“When someone enters that space, there isn’t some prescription of, ‘Oh, you get exactly this,’” she described. “There’s a peer involvement that says, ‘What are you looking for? What are your goals, and how can we support you?’”
Launch dates for the new urgent care services may vary by program.
“Each proposal has a different timeline,” Krompf told the House Committee on Health Care in May.
“But the money that we have to spend on this needs to be expended by 2025. So, if that gives you an indication – we aren’t looking for a twoyears-out implementation. These are things that had dates within six months, nine months.”
Anticipating a future need for state dollars, legislators asked whether DMH had a plan in mind for how to pay for the programs in the long term.
Krompf told them that “the leaders on this, in terms of funding, are well aware that they’re putting things in motion to serve the population for mental health urgent care that don’t have sustainable funding, and I do think some of this is going to be a need for CMS and Medicaid to acknowledge that.” But “Medicaid can’t pay for all services for everyone,” she added.
Northeast Kingdom Human Services’ project did not qualify for the special federal funding because it proposed to offer patient stays longer than 24 hours, so DMH asked the legislature for an allocation from the state’s general fund.
Its proposed Front Porch Crisis Care treatment center will offer four to six crisis beds in the region of the state that has fewer than any other. Stays will range from two to ten days.
For same-day services, NKHS Executive Director Kelsey Stavseth described a plan that would incorporate aspects of both PUC(K) and the Living Room, with “access to nursing, psychiatric, and medication management services” on a “walk-in” basis within a “therapeutic environment” featuring peer support.
NKHS will need to buy a new building to house the program, which it will develop in a phased approach that will, however, allow some components to start up within its existing facilities.
Stavseth noted in February that a realtor had already identified some potential candidates for a new property, which, “for staffing access,” would preferably lie within the I-91 corridor, no more than an hour’s drive for patients from Orleans, Essex, or Caledonia County.
NEWS 6 Fall 2018 NEWS 6 Summer 2023
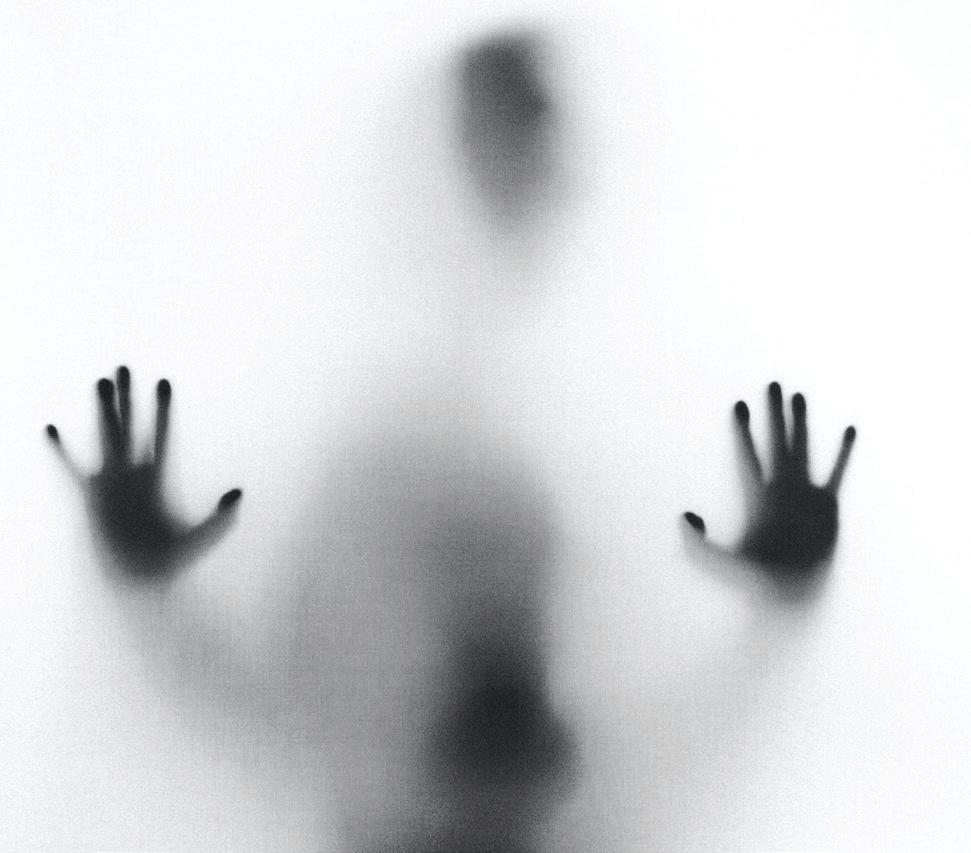
(Photo by Nik Shuliahin, Unsplash)
Mobile Crisis To Go Statewide
by BRETT YATES
WATERBURY – The Vermont Department of Mental Health expects to launch a unified statewide mobile crisis response service this year. It follows a 13-month pilot program in Rutland which had to limit operations due to challenges recruiting workforce.
DMH selected Healthcare & Rehabilitation Services, the community mental health center for Windham and Windsor counties, as its vendor. HCRS will subcontract Vermont’s nine other community mental health centers, creating a unified system for the entire state.
Deputy Commissioner Allison Krompf told legislators that “the go-live date is set for Sept. 1,” but HCRS leadership was not clear whether that would be possible. Contract negotiations between DMH and HCRS have not yet concluded.
Last year, the legislature mandated that the mobile crisis response program incorporate peer support workers.
“Having people with lived experience being able to be deployed is a really important theme as we roll this out,” Chief Operating Officer Anne Bilodeau said.
According to DMH, each two-person mobile response team will have at least one clinician. A peer can fill the other role but, by HCRS’s account, may not always do so. “It will be flexible,” Karabakakis said. “In many cases, the response will be based on what the family or what the individual needs. Oftentimes they might be working with a case manager who really knows the individual, who really knows the family, and they might be that second person.”
In testimony before the House Committee on Health Care, Rutland Mental Health Services Director of Emergency Services Loree Zeif
wondered where the needed employees would come from. “While I support this two-person initiative,” she said, “I cannot imagine how we will staff it.”
Zeif suggested that it would “cost many more
request for proposals last year that offered a maximum of five DMH contracts to serve 10 catchment areas throughout Vermont. Its executives characterized the proposal as a statewide collaboration.
“There were other options, like maybe taking regional approaches, but I think in the end we all agreed that, if we worked together, HCRS would be the lead,” Karabakakis said. “I met with all the executive directors for many hours to really sort of flesh this out.”
times what the state has anticipated to provide the level of service we’re looking at.”
In May, the legislature allocated $422,812 to fund four new positions within DMH to oversee the program, which is intended to reduce strain on emergency departments by sending mental health workers into homes and communities at callers’ request.
“We’re hopeful” about the timeline, HCRS Executive Director George Karabakakis told Counterpoint. “If we really want to operationalize this and make this happen in a successful way, we need to have that date reflect the reality of what’s on the ground, so we’re in the process of discussing that.”
“I would just say that there is a lot of complexity to creating a statewide initiative that involves saving lives in crisis situations,” Bilodeau added. “And we want to be particularly thoughtful and caring to make sure that everyone has the staffing that they need and those staff are trained and that we have the right protocols in place.”
HCRS submitted the only response to a
Each of Vermont’s community mental health centers already offers emergency services, for which DMH data indicates rising demand. But capacity varies, and in DMH’s telling, none can currently provide mobile outreach at all times. The new program will standardize practices in accordance with requirements set by the Centers for Medicare & Medicaid Services, which include an obligation for 24/7/365 readiness. Special CMS funding will help bolster the program for a three-year start-up period.
“You shouldn’t have to worry about which [community mental health center] it’s attached to. It’s just mobile crisis response,” Krompf said. “And at some point, it may be able to be dispatched through 988, which would even provide a centralized number.”
Per a DMH report, the youth-oriented pilot by RMHS “experienced significant workforce challenges,” reducing operations to 40 hours a week. “It’s clear to us that there’s a vacancy issue in existing programming,” Krompf told Counterpoint. “It’s clear to us that any expansion will also have to manage the fact that there’s a staffing crisis. So the hopeful news is that not all of this has to be brand new. There’s ways to take existing resources and leverage them.”
‘Soft Restraints’ Required of Police
 by BRETT YATES
by BRETT YATES
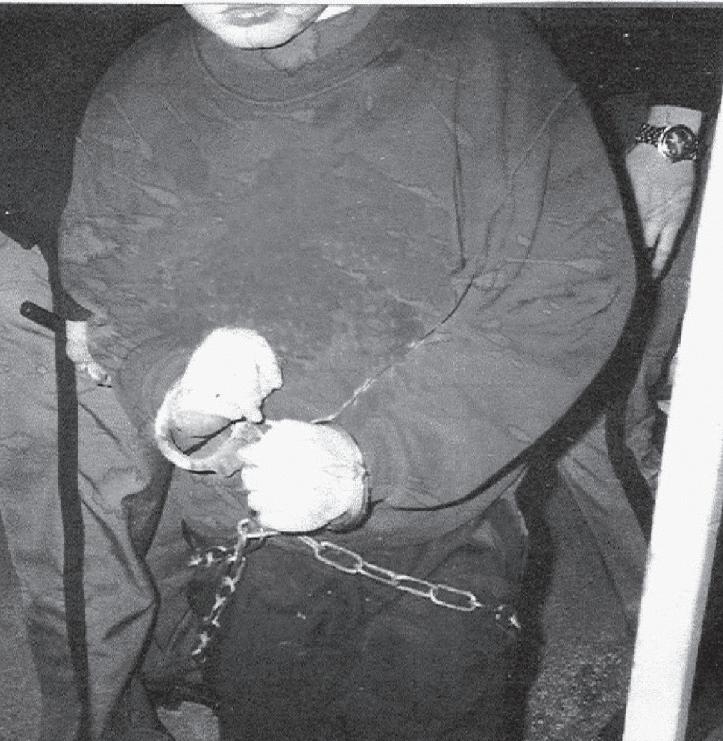
MONTPELIER – Starting in July, police cruisers throughout Vermont will have to carry “soft restraints” for transporting individuals after responding to a mental health crisis.
These devices, with fabric resembling that of a seat belt, will offer an alternative to “mechanical restraints” such as metal handcuffs. A new law specifies that officers will use soft restraints “as a first option” for these passengers when restraint is deemed necessary for safety.
The requirements also extend the same criteria that have been in effect for sheriff transports since 2005 to all law enforcement. Those include avoiding physical and psychological trauma, respecting privacy, and using means that are the least restrictive necessary for the safety of the patient. That 2005 law was passed as a result of advocacy by Vermont Psychiatric Survivors after hearing from the parent of a young boy who was taken to the Brattleboro Retreat by sheriffs in wrist, ankle and waist shackles.
The overall new bill focused on the transportation of individuals who have been taken into the temporary custody of law enforcement based upon a finding that the person presents an “immediate risk of serious injury to self or others.”
The legislation made several other changes to the procedures by which a person can be brought unwillingly to healthcare facilities for an emergency examination to be hospitalized against a person’s will. Sen. Ginny Lyons introduced the bill following several months of
meetings organized last year by Vermont Care Partners, the umbrella organization for the state’s community mental health centers.
The workgroup, which included representation by Vermont Psychiatric Survivors, examined the statutes that govern involuntary interventions during apparent mental health crises that take place outside of medical settings.
In the absence of a physician who would certify the need to hold the individual in advance of potential inpatient admission, a Superior Court judge’s warrant is the alternative authority.
State law previously allowed a police officer or a mental health professional to take a community member into custody and transport them to a hospital only if such a warrant was granted. The revisions to the law will now allow the forced transport to take place as soon as the warrant is applied for.
Lawmakers added language drafted by Jack McCullough of Vermont Legal Aid’s Mental Health Law Project. He described a growing problem of judges permitting involuntary interventions based on inaccurate secondhand information. Warrant applications must now rely on the applicant’s own observations unless accompanied by a signed statement of facts from another source.
Through the bill, Vermont Care Partners said it hoped to shift more of the responsibility for the warrant and court-ordered transport onto police officers specifically, citing fears of physical harm among its agencies’ clinicians and resulting workforce recruitment challenges. According to
Brandi Littlefield, the Howard Center’s assistant director of First Call for Chittenden County, the desired change would resolve delays in “access to hospital care as a result of confusion of who will provide the emergency transport.”
In the final legislation, only law enforcement can take individuals into custody for mental health reasons without a physician’s certificate. A mental health professional can still provide transportation to them “if clinically appropriate,” but not by court order.
NEWS . 7 Fall 2018
NEWS Summer 2023 NEWS Summer 2023 7
This photo of a 10-year-old boy (taken by his father) being led into the Brattleboro Retreat by sheriff’s officers in 2004 led to the first change in law to begin eliminating such practices. (Photoshop used to remove identifiers on sweatshirt.)
One director said she supported the approach, but “I cannot imagine how we will staff it.”
Peer Certification Plan Funded
by BRETT YATES
MONTPELIER – The Vermont Department of Mental Health’s new budget includes funds for a “Peer Supports Credentialing Program.”

DMH requested an allocation of $187,500 from the state’s general fund to cover half of the projected cost of its startup and its first year of operations, based on the expectation that federal Medicaid dollars would pay for the remainder.
“The bulk of that money would actually go towards training,” Director of Adult Services Patricia Singer told the House Committee on Health Care. “We hope to train up to 60 folks in the first year.”
According to Singer, the program will target adult mental health peers exclusively, despite “some overlap” between their work and that of peer recovery coaches, who offer support for substance use conditions.
MadFreedom founder Wilda White, who testified alongside Singer, noted that the budget would support “the very basics of a certification program,” which she envisioned would someday offer additional credentials for mental health subspecialties such as geriatric support, forensic support, and peer supervision.
“That’s a ways off,” White predicted.
Most U.S. states have already established official certification processes for peers, which can make their services eligible for Medicaid reimbursement. Last year, after Vermont’s legislature failed to pass a bill to implement such a system, DMH – with the urging of the peerled organizations who’d drafted the legislation – determined to proceed through internal rule-
making. First, the department issued a $30,000 grant to Pathways Vermont’s Peer Workforce Development Initiative, which subcontracted Wilda White Consulting to host stakeholder meetings for a potential certification program. This spring, White completed a report with recommendations for DMH.
DMH does not have a specific timeline for a decision to accept or reject those recommendations, according to Deputy Commissioner Allison Krompf.
White’s report distinguishes between “assessment-based” and “professional” certification programs. The former would certify peers on the basis of their performance during a training period, while the latter would
require an additional body to administer a test following the training. According to the report, the input received by White over the course of six public sessions, which 77 individuals attended, demonstrated a consensus in favor of a professional program.
The report calls for DMH to contract a peerrun organization for each of three central tasks: to screen candidates for eligibility to enroll in peer support training (on the basis, for instance, of testimony of “lived experience”); to develop and administer a training curriculum; and, in tandem with the Office of Professional Regulation, to issue credentials. A single vendor would handle the training statewide and could potentially take on the contract for screening as well. The endorsed screening standards would not disqualify applicants on the basis of their education or their state of residence. A criminal history would not bar them automatically.
The report also includes a draft of a Medicaid state plan amendment. Peer supporters employed by Medicaid-enrolled providers would practice under its guidelines, serving clients “who have a mental health or substance use condition and who have peer support included as a component of their person-centered, wellness plan, which serves as the plan of care.”
Once DMH has affirmed or rejected the report’s policy recommendations, the Peer Workforce Development Initiative will move on to what it calls “phase two” of its “work plan,” which will include helping to draft requests for proposals from peer-run entities for DMH’s possible use.
Gun Restrictions Focus on Suicide
 by BRETT YATES
by BRETT YATES
MONTPELIER – A bill described as intending to protect Vermonters at risk of suicide by boosting safety through restrictions on gun owners and purchasers passed the legislature this spring. It awaits action from the governor.
Rep. Alyssa Black introduced “An act relating to implementing mechanisms to reduce suicide” in February. All three of its “mechanisms” related to firearms: their acquisition, possession, and storage.
The legislation cited Vermont’s 142 suicides in 2021, of which 83 (or 58%) used guns. These suicides accounted for 89% of Vermont’s deaths by firearm that year. Black’s son died by suicide in 2018 shortly after buying a gun.
Black suggested that Vermont’s troubling suicide rate – about 45% higher than the national average in 2021 – is owed to its high rate of gun ownership. Suicide attempts by other means are far less likely to achieve a lethal outcome.
“The rates of suicide in states with high gun ownership [are] double what it is in states with low gun ownership,” Black told fellow legislators. “And the interesting part is, when you look at the number of firearm suicides between the two groupings of states, they are dramatically different – when you look at suicides by all other methods, they are equal.”
First, the bill would require gun owners whose households include children or persons prohibited from possessing firearms to keep their guns locked and stored separately from their ammunition.
Second, it would extend the right to file a petition for an “extreme risk protection order” to the person’s household and family members. Such orders, if granted by a judge, can force a
potentially dangerous person to relinquish their legally purchased firearms. Currently, only a state’s attorney or the Attorney General can file the petition.
Finally, the bill would impose a waiting period for gun buyers, except at gun shows. A licensed dealer would transfer the firearm 72 hours after its purchase.
amount of time, they are less likely to have a mental health diagnosis, they’re less likely to be involved in the mental health system, and they’re less likely to have made a prior suicide attempt.”
Much of the debate about the bill centered on its constitutionality. But Rep. Anne Donahue, who proposed a strike-all amendment in March, questioned the likely efficacy of its provisions in a state with “a large amount of gun ownership.”
Donahue pointed to what she saw as a lack of available data on relevant details of Vermont’s suicides, such as how long before the incident each victim had acquired their weapon and whether it was stored in a safe or unsafe manner at the time. She entreated the legislature to mandate a study before moving forward.
In testimony before the House Committee on Judiciary, Dr. Rebecca Bell, a pediatrician at the University of Vermont Children’s Hospital, represented the Vermont Medical Society and the Vermont chapter of American Academy of Pediatrics, both of which supported the bill. She emphasized what she regarded as the particularly spontaneous nature of suicides by firearm.
“When researchers look at people who have attempted suicide with a firearm versus other methods, what they find – and this is true when I look at my cases in Vermont of young people – is… that those who choose a firearm are doing so more impulsively than those who choose another method,” she said.
“So they’ve thought about it for a shorter amount of time, they planned for it for a shorter
“My hunch is that there might be a case to be made for safe storage, but I don’t think we know that,” Donahue said. “I think the 72-hour hold, given the circumstances of our state, is extremely unlikely to do anything significant. But I could be wrong.” The amendment failed.
“If H. 230 is postponed for one more year and one extra person dies that wouldn’t have had to die – we’re not willing to put it off,” Black said.
A subsequent attempt to modify the bill to add police officers but to delete the addition of family and household members from among the groups able to initiate extreme risk protection order petitions also failed.
NEWS . 8 Fall 2018 NEWS Summer 2023 8
“The rates of suicide in states with high gun ownership [are] double what it is in states with low gun ownership.”
(Photo by Kateryna, Unsplash)
New Law Allows Arrests in EDs
by BRETT YATES
MONTPELIER – Arrests by law enforcement may become a more common sight in Vermont’s emergency departments. Owing to a change in law, police can arrest and remove hospital patients or visitors for certain misdemeanors without a warrant even if an officer was not present to witness it – something they cannot do now.
Advocates who opposed the change cited fears that it would serve to criminalize mental health crises. That led legislators to shrink the scope of the bill, which originally applied to all healthcare settings.
The bill was also narrowed to ensure that no patient could be arrested and removed from the hospital if they had not been evaluated yet, were not in stable condition, or were waiting for an inpatient admission.
Zachary Hughes, the vice president of the board at Vermont Psychiatric Survivors, voiced opposition to increasing the number of arrests in hospitals. “I think a citation is maybe less traumatic than an arrest,” he observed. “You may be deterring people from the hospital.”
Hughes encouraged legislators to consider ways of calming emergency room patients before violence occurs.
“I think there are times when you can involve the peer population, who can provide support while the person is in waiting mode, depending on how acute the situation is,” he said.
In order to make an arrest without first obtaining a warrant from a judge, police must have “probable cause” to believe that a crime has taken place.
On this basis, an officer can arrest a felony suspect even without witnessing the incident directly, but in the case of a misdemeanor, an officer arriving after the incident occurred, can only take the accused party into custody if the alleged offense appears on a list of 17 crimes in current law. The bill added three more to protect healthcare workers in hospitals and for emergency service responders, targeting assaults, threats, and disorderly conduct in those settings.
Before voting in favor of the bill, the House Committee on Judiciary added a requirement that the Vermont Program for Quality in Health
Care compile a report examining how adequate training and sufficient staffing levels, among other possible improvements that would not involve police, may support safer hospitals. The legislature will receive it next January.
The Vermont Association of Hospitals and Health Systems pushed for the bill. Nurses, doctors, and paramedics appeared before the legislature to describe what they said was an increasingly dangerous working environment, particularly in understaffed emergency departments, and a sense of having little recourse for burnout-inducing harms endured on the job.
at hospitals. “If we’re talking about a person who’s brought to a hospital, there’s typically a reason why,” said DPS Deputy Commissioner Daniel Batsie.
“They’re having a psychiatric breakdown, they’re having a medical condition, they’re having something that has brought them there for evaluation or treatment.”
Colonel Matt Birmingham of the Vermont State Police conjectured that such an arrestee would likely return to the same hospital after their arraignment.
“I would find it to be challenging, if not impossible, for a judge to impose conditions of release that they’re not allowed to go to an emergency room,” Birmingham said, “because that’s probably illegal.”

Jack McCullough from Vermont Legal Aid’s Mental Health Law Project doubted whether the bill would make healthcare workers safer.
“I have never once in my 20 years thought about leaving emergency medicine,” said Jill Maynard, a nursing director at Southwestern Vermont Medical Center. “However, over the past 12 months, I ponder leaving the ED and, on the most difficult days, leaving the profession altogether.”
Recalling incidents of spitting, hair-pulling, sexual harassment, and death threats, Maynard reported that she’d been “made to feel guilty for calling the police” or had been told that “the patient had a mental health diagnosis –therefore, they would not be held responsible for their actions.”
Alison Davis, a medical director at Rutland Regional Medical Center, shared a secondhand account: “One night, a female staff member had a urinal thrown at her and was then punched in the side of the head by a patient. That patient remained in the ED that night, awaiting bed placement, but the following day was reported by staff to be bragging about ‘hitting that broad’ and asking staff, ‘This is Vermont: what are they going to do?’”
Representatives from the Vermont Department of Public Safety expressed concerns, especially from the standpoint of legal liability, about the possibility of interrupting crucial care
“While superficially appealing, nothing in this bill provides an opportunity to interrupt, cease or prevent a crime when it is happening – everything in this bill is about responding to a criminal act after it has occurred,” he said.
Washington County Mental Health Services Executive Director Mary Moulton testified about the need for “upstream services” that would reduce burdens on emergency departments.
Speaking as an advocate, Rep. Anne Donahue criticized committee discussions for the “degree of the focus on mental health” despite reports of increases in violent behavior among Americans irrespective of any psychiatric diagnosis.
She said that the bill “could end up being a highly disproportionately used tool, driven in part by implicit bias” against psychiatric patients.
Sen. Dick Sears, who introduced the bill, stressed during the Senate hearings what he saw as an imperative to give officers a stronger signal to intervene in attacks upon healthcare workers.
The Vermont Rules of Criminal Procedure similarly single out “assault against a family member, or against a household member” among the misdemeanors for which officers can make immediate arrests without seeing them firsthand. “The goal was to put together legislation that would mirror what we do with domestic violence right now,” Sears said.
Fall 2018 NEWS . 9 Summer 2023
Counterpoint Opinion Poll If you threaten ED staff while in a mental health crisis, should you be arrested for a crime? Results of the poll will be published in the next issue of Counterpoint. OR by going to www.vermontpsychiatricsurvivors.org/counterpoint/ QUESTION: VOTE by scanning this onto your mobile phone: Current law permits a citation, but not an arrest, for misdemeanors.
Feasibility Study Failed To Include Required Input from Advocates
Youth Inpatient Unit Is Funded
by BRETT YATES
BENNINGTON – The state legislature budgeted $9.225 million in fiscal year 2024 for the construction of an adolescent psychiatric inpatient unit at Southwestern Vermont Medical Center, indicating its approval of the project.

The Department of Mental Health told legislators that the plan was moving forward to develop a 12-bed unit. The recently completed feasibility study “suggests the need for more than
not reach out to any other groups during the preparation of the feasibility study, Director of Planning James Trimarchi acknowledged.
“There has been no public input to the process at this point,” said Trimarchi, who characterized the feasibility study as a technical procedure carried out via spreadsheets and diagrams.
Trimarchi noted that SVMC’s Board of Directors hasn’t yet reviewed the results.
Part of the feasibility study was a “demand analysis,” which sought to quantify Vermont’s need for additional adolescent inpatient beds. One model used figures from Massachusetts, which has 38.4 beds per 100,000 kids. The same rate, transposed to Vermont, would yield a total of 18.5 youth beds.
12” such beds in addition to the existing 10 to 14 beds at the Brattleboro Retreat, DMH reported.
However, according to SVMC Director of Planning James Trimarchi, the final status of the proposal remains uncertain until the hospital Board of Directors decides whether to move forward, which is not expected to occur before August or September.
That would be a delay of three or more months from the original timeline, which he attributed to uncertainty surrounding the legislature’s appropriations bill.
The feasibility study – which Trimarchi said was still a draft – reported that “clinical experience, anecdotal information, and state reports indicate that a crisis exists in access” to adolescent inpatient care but that no “structured data is available to accurately calculate the number of additional beds needed in Vermont,” which “could be zero to12.”
“The real answer is that we don't know,” Trimarchi said.
DMH initially requested an allocation for the project in January during the annual budget adjustment, stressing a need to “reduce the number of youth waiting in an emergency department” and to serve “individuals who are currently denied admission at the Brattleboro Retreat due to medical needs that cannot be managed in a non-medical hospital setting.”
But legislators waited until spring, when SVMC had completed the initial feasibility study, to approve the funds.
The study identifies a former area for medical records within the hospital as a suitable site for the unit. The document’s schematic shows 12 bedrooms, as well as a dining room, two social rooms, a consult room, and a seclusion suite, as well as access to an outdoor area.
DMH had contracted SVMC to perform the feasibility study in October. The contract included a requirement to “obtain feedback on the design and operations from the local Designated Agency, mental health advocacy organization[s] such as Disability Rights Vermont and persons with lived experience.”
While SVMC maintains regular contact with United Counseling Service, Bennington County’s “designated agency” for mental health, it did
The Chair of the House Health Care Committee, Rep. Lori Houghton, appeared to believe the commitment to the site was more definite when she said on the House floor on May 12 that SVMC will be beginning the Certificate of Need process this summer to get approval for the project from the Green Mountain Care Board. Based on testimony by DMH to the committee earlier that week, “The intent by the Department of Mental Health... is for the beds to be placed at Southwestern Medical Center,” Houghton said.
In a timeline presentation to the committee, Commissioner Emily Hawes showed a graph from the SVMC feasibility report based upon Board approval by May and the Green Mountain Care Board application to be filed by June, which could not actually occur until after the SVMC approval.
Meanwhile, a “queuing theory model” – based on Vermont Association of Hospitals and Health Systems data suggesting that 48 adolescents per quarter need inpatient care, with an average length of stay of 15 days – seemed to indicate that Vermont should have 12 or more youth beds.
Trimarchi views a model developed by the American Psychiatric Association in 2022 as the most accurate for calculating demand . He pointed to its consideration of “more than 40” factors, including the availability of communitybased resources. But by his account, Vermont hasn’t yet aggregated all the information needed to use it.
And even if it did, that information could shift at any time. Demand could change if, all of a sudden, there is an investment in equal resources dedicated to building out outpatient services,” Trimarchi posited. “I have very little sense that the calculation of demand can even be done sensibly.”
Still, for him, the need to “do something” remains apparent. The current thinking is, let's build this 12-bed unit. If it eliminates the languishing in the emergency departments,” Trimarchi theorized, “then we know we've met demand. Until we do, we just gotta keep building these things.”
DMH Deputy Commissioner Allison Krompf told Counterpoint that she believes there is a consensus on the need for it. “I think the question mark still is, can an organization in this climate right now stand up a new wing of a facility, build staff? I would imagine any organization is not going to feel extremely definitive.”
Some legislators and advocates, however, have both questioned whether Bennington is the right place to do it. “I’m just wondering if there are any other potential places that are further north,” Sen. Ginny Lyons said.
The SVMC feasibility study referenced the same question, asking, “Should new beds be created in southern Vermont since the current beds are also in southern Vermont at the Brattleboro Retreat (Vermonter’s expectation that care resources, particularly those funded by the state, are nearby and equitably located.)”
Trimarchi indicated that the hospital would begin to survey advocates and community members after the Board approval in late summer.
“We're a long ways to ‘yes’ on this thing,” he observed. “So if we decide to proceed, the input from the public will be critical because that's where we will share with them the block diagram and say, ‘Does this layout for individuals with lived experience make sense?’”
The feasibility contract ended on March 31. But Trimarchi emphasized in May that the study was “not technically done. It’s still in draft phase.”
“I haven't received input from the Department of Mental Health yet,” he said. “If they come back and say, ‘Hey, we gotta share this with the disability rights group to have their input before we can close the book on it,’ then let's do that.”
“Additional [requests for proposals] must be requested and ways found to help other institutions, such as the UVM Medical Center, meet the requirements of those RFPs,” NAMIVermont Board President Charles R. Siler urged in written testimony.
SVMC was the sole respondent to the second issuance of DMH’s RFP last year. The University of Vermont Medical Center initially threw its hat in the ring before withdrawing its plan on account of financial difficulties.
If the project moves forward at SVMC, it will aim for a launch date in December 2024. The projected annual cost of operations will exceed $7 million. It would likely require Medicaid to subsidize the costs as a result of private insurers’ tendency to under-reimburse inpatient psychiatric services. “The initial goal, although unlikely, would be to achieve reimbursement parity across payers,” the feasibility study said.
NEWS 10 Fall 2018 NEWS 10 Summer 2023 NEWS Summer 2023
“Demand [for beds] could change if, all of a sudden, there is an investment in equal resources dedicated to building out outpatient services... I have very little sense that the calculation of demand can even be done sensibly.”
Southwestern Vermont Medical Center in Bennington. The inpatient unit would be created through rehabilitation of the wing at the far right. (Photo courtesy SVMC)
Forensic Unit Gets Green Light
by BRETT YATES
MONTPELIER – A years-long legislative effort to create a separate forensic mental health system culminated in the passage of a law that will, by next summer, turn the four and five-bed units of the Vermont Psychiatric Care Hospital into a locked “therapeutic community residence” that will allow the use of restraint and seclusion for psychiatric patients being held based upon criminal charges.
Most U.S. states already have separate psychiatric facilities for defendants deemed incompetent to stand trial or found not guilty by reason of insanity. But until now, Vermont’s system of care has not distinguished between such patients and those involuntarily committed by civil courts.
The new law stipulates that two units at VPCH, a locked, 25-bed, state-owned hospital in Berlin, will serve as the “initial” site for segregated forensic treatment, seeming to imply the eventual construction of an all-new facility.
But Deputy Commissioner of Mental Health Allison Krompf said the Department has no such plan. She said the intent was to grant flexibility in case the VPCH conversion falls through.
“There was no sort of, ‘We’re gonna start here and then in three years plan to move it somewhere else,’” she said.
In order to change uses, VPCH will receive a new license from the state to treat justiceinvolved patients on court orders of nonhospitalization (restrictions outside a hospital.) This changeover – which was exempted from requiring a Certificate of Need from the Green Mountain Care Board – will result in a loss of nine high-security, “level-one” inpatient beds when they become forensic beds instead.
But as part of addressing a patient population committed based on allegations of violent offenses, the new law requires the Department of Disabilities, Aging and Independent Living to modify its licensing and operating regulations to create a new category of “residential” treatment
that will have permission to use emergency restraint and seclusion and administer courtordered drugs.
In 2021, psychiatric survivors campaigned successfully against a plan by the Department of Mental Health to use restraint and seclusion at its new locked residence in Essex, which belongs to a category of 24 facilities statewide that have never legally deployed such practices.
The forensic facility at VPCH will be the first.
Vermont Psychiatric
defendant’s mental state at the moment of the alleged offense, that of competency addresses their ongoing ability or inability to stand trial.
Under the new law, DMH-appointed psychologists – not just psychiatrists, as before – will be eligible to evaluate defendants for competency during a one-year trial period.
The original bill instructed DMH and DAIL to develop a plan for a treatment program specifically aimed at restoring someone’s competency to stand trial, but the final legislation instead mandated a report from the departments “on whether a plan for a competency restoration program should be adopted in Vermont.”
Zachary Hughes, the vice president of Vermont Psychiatric Survivors’ board of directors, offered testimony on both bills. He urged legislators to remember that, once a doctor has judged a defendant incompetent to stand trial or a court has found them not guilty by reason of insanity, “this isn’t a criminal situation anymore.”
Over recent years, Vermont police have attributed a handful of high-profile crimes, including the murder of a young woman in Bennington in early 2021, to perpetrators with psychiatric diagnoses. In their aftermath, victims’ families have pushed legislators to address public safety concerns.
Two years ago, at the legislature’s demand, DMH convened a workgroup for the purpose of developing a plan to remedy “any gaps in the current mental health and criminal justice system structure.” But its diverse membership, which included both psychiatric survivors and crime victims, failed to reach a consensus.
This year, lawmakers moved forward to modify laws that govern competency exams and insanity defenses in Vermont’s criminal courts, as well as authorizing the new facility.
While the question of sanity addresses a
He also encouraged them to “keep politics out” of their decision-making, and to consider making more investments in voluntary mental health programs before building a forensic facility. “You may not need it if we can get more community services rolling,” he said.
The Senate version of the bill set criteria for admissions (and for expedited admissions) at forensic facilities that included not just individuals in DMH custody but also those in DAIL custody based upon being “persons with an intellectual disability” who, according to a civil court, had committed violent acts. They have received care only in community placements since the Brandon Training School closed in 1993.
Testimony by Green Mountain Self-Advocates and Disability Rights Vermont, among others, protested the plan. The legislature ultimately created a workgroup to assess specifically “whether a forensic level of care is needed for individuals with intellectual disabilities.” A report is due by Dec. 1.
DMH Head Ruled in Contempt of Court
BURLINGTON – A Superior Court found the Commissioner of the Department of Mental Health, Emily Hawes, in contempt of court in May for what it described as “knowingly and willingly disobeying the Court’s order” for an updated psychological evaluation of a defendant’s competency to stand trial.
Judge Alison Sheppard Arms of the Chittenden Criminal Division will fine Hawes, in her role as commissioner, $3,000 if DMH does not act to comply with the order.
DMH’s communications director, Alexandra Frantz, said that DMH had not initially received a “clear directive to complete the evaluation” last
November, and once it understood the order, it placed the individual on the current wait list.
According to the court decision, DMH had asserted that it was only under a statutory obligation to perform one evaluation per defendant.
Arms said DMH used “nonsensical assertions and nonexistent legal grounds” to defend against its “continued obstruction of the criminal justice process.”
Frantz noted that DMH has had a significant backlog of evaluation cases, made worse by the COVID pandemic, that has caused waits of up to a year. She said DMH hopes that some of
the issues raised by the case will be addressed through S. 91, a bill passed by the legislature this year revising laws on forensic evaluations and now awaiting signature by the governor.
The legislature rejected language from DMH to no longer require it to provide further evaluations once there was an initial finding of competency, but did add a required showing of a change in circumstances before a new evaluation can be ordered in such cases. It allows, for a oneyear trial period, forensic psychologists as well as psychiatrists to conduct evaluations. It also allows a warrant to be issued if a defendant fails to appear for a scheduled evaluation.
Mental Health Budget Upped by 4.63%
MONTPELIER – The Department of Mental Health’s budget for next year was increased by 4.63%, or slightly more than $14 million, including funding added by the legislature.
There were no funds added to expand peer-led programs.
The DMH budget proposal was for slightly more than a $7 million increase to contribute to an expansion of the Blueprint for Health program, to add four staff positions to oversee a new statewide mobile crisis response system, for new urgent care programs, and for funding a
peer certification program (see articles on pages 6 through 8 about those programs.)
However, it included no increase in that base budget for community mental health centers, which advocates testified would result in a cut to community services because of inflationary pressures and the number of vacant staff positions at current salary scales. The legislature added a five percent increase for community mental health centers and a new staff position for quality oversight staff. The final budget brought the total DMH budget from last year’s $303,469,211 to a
new $317,528,698. The Blueprint expansion is a two-year pilot project intended to help primary care doctors in addressing patients who have both mental health and substance use diagnoses. It will expand a program called “Hub and Spoke” that currently focuses only on opioid addictions. The pilot will increase staff for existing Community Health Teams embedded in primary care, “who will help with screenings for social determinants of health, referrals and care coordination,” testified Jessa Barnard of the Vermont Medical Society.
NEWS . 11 Summer 2023
Survivors urged the legislature to consider making more investments in voluntary mental health programs before building a forensic facility.
Integration Council Stresses Peer Work
by ANNE DONAHUE
WATERBURY – The Mental Health Integration Council, which was charged by the legislature with “helping to ensure that all sectors of the health care system actively participate in the state’s principles” for a holistic health care system, is nearing the end of its two years of work.
Peer support services emerged as a key component in discussions in the second year’s work, with a subgroup on primary care strongly endorsing development of peer and community health workers in support of whole health and as a point of entry to primary care.
The Department of Mental Health said at the Council’s May meeting that a final report and recommendations would be completed in July.
Mark Levine, MD, Commissioner of the Department of Health, said that national experts have said that the magnitude of change to achieve a “whole health” approach to health care would take decades of work and a “seismic cultural change.”
But in Vermont, “we have a fighting chance” to make it work, Levine told the group, because of the “positivity and energy” he witnessed in the collaboration among the many participants.
At the May meeting, members heard from the Veteran’s Administration peer program, which will have two peer support specialists in every primary care clinic by next year. The VA has some 13,000 peer specialists employed across the country, according to Christina Strook, PsyD, from the VA Center for Integrated Healthcare.
The discussion evoked questions from Allison Krompf, Deputy Commission at DMH, about how peers are recruited and certified, and what their roles are, noting that it was a topic Vermont is “trying to work through right now.”
David Kanar, who started as a peer support specialist in Georgia 18 years ago and now works for the VA in Tampa, explained that the role meant being someone “willing to self-identify as in recovery from mental health and substance abuse” and with training to use that experience “in a strategic way to provide hope.”
He sees it as a “pay it forward” role from his own recovery journey, saying that he was “someone you’d never, never expect” to be where he is today after having been a long-term patient with schizophrenia who was predicted 22 years ago to never leave the hospital.
Strook said the VA requires certification and continuing education through recognizing certain state programs which meet its criteria for vigor, as well as accepting two national programs.
Peer work in primary care is often a relationship of shorter duration, she said, but peer specialists have a unique role in supporting patients to be “engaging or not giving up on care.” They help as system navigators who “know access to community resources best” and are “acutely aware when [individuals] need more intensive services.”
“They have that gut instinct” and patients are often more likely to disclose challenges than with a clinician, she added.
Kanar and Strook both stressed that peer specialists are not clinicians and that it would be destructive to the peer relationship if they were.
The Council, which was jointly chaired by the Department of Mental Health and Department of Health, focused on sub-committees in different specific areas: primary care, pediatric care, workforce, and funding and alignment of performance measures. Membership covered almost every sector of health care, including insurers, the state, private health delivery, hospitals and regulators. Recommendations in a preliminary report in February reflected the reports of the subcommittees, including the peer focus from the primary care group.
But Towle said that work, in which he participated, still just felt like “talk, talk, talk” with “very little evidence of action” to create structures that would actually build a system of peer support staff.
The tasks assigned to the Council by the legislature included “identifying obstacles to the full integration of mental health into a holistic health care system and identifying means of overcoming those barriers; helping to ensure the implementation of existing law to establish full integration within each member of the Council’s area of expertise; establishing commitments from non-state entities to adopt practices and implementation tools that further integration; and proposing legislation where current statute is either inadequate to achieve full integration or where it creates barriers to achieving the principles of integration.”
A peer specialist is “walking alongside [the peer] in building a self-directed life… not pushing someone from behind or pulling from ahead,” Kanar explained.
The systems-level approaches that were directed by the legislature in its creation of the Council never fully developed in its discussions, according to some. The proposals for primary care were one of four areas of focus, rather than part of a comprehensive proposal.
There was “some good awareness” and the creation of “collaboration among silos” among different health sectors that were positive, according to Dan Towle, who filled one of two positions on the Council appointed by Vermont Psychiatric Survivors.


However, the final outcomes that are emerging are a disappointment, he said, given “the number of people and amount of time, and how little we’ve accomplished.”
In a draft report, a pediatric subgroup made recommendations to incentivize serving child, youth, and family through pediatric-specific applications of the local integrated care model(s) and to increase integration of healthcare in Coordinated Services Planning.
A subgroup on integration of funding and alignment of performance measures recommended a formal needs assessment to assess parity by health insurance payers; the use of performance measures across health care providers and organizations, state government entities, and health insurance payers; and to pilot selected integration care models. The workforce subgroup recommended aligning with the work of the Health Equity Advisory Commission; identifying opportunities for shared or leveraged staffing; exploring best services at community mental health agencies or federally qualified health centers; and developing guiding principles.
COMMENTARY 12 Fall 2018 NEWS Summer 2023
NAMI WALKS NAMI-Vermont held its annual fundraiser and stigma-awareness walk in Burlington despite some late April showers. It was an occasion for Ramsay Grassley, almost 4, of New Haven (left photo) to get a kiss from support dog Hoke (owned by Leslie Dunn of Jericho).
(Photos by Anne Donahue)
A peer specialist is “walking alongside [the peer] in building a selfdirected life… not pushing someone from behind or pulling from ahead.”
Regulators Defend Safety Rules
by ANNE DONAHUE
State and federal regulators on hospital safety have defended the level of requirements for suicide prevention and say hospitals are the ones that still have responsibility – and enough leeway – to assure that patient emotional and therapeutic needs are met.
Regulators were contacted as follow-up to an article in the winter Counterpoint that quoted patients as saying that inpatient psychiatric units have become less welcoming and less healing in recent years as hospitals put an ever-increasing priority on making them physically safe from suicide attempts.
Activity areas have been closed off, patients are less able to take care of needs on their own, and the furnishings have become more sterile, they told Counterpoint.
Hospital leadership said new changes continue to be required by the Joint Commission, a private organization that accredits hospitals at a high cost and sometimes to the detriment of a therapeutic environment.
In written responses that they agreed to provide to Counterpoint, the Commission said that “hospitalization is intended to provide patients a safe, protected environment designed to heal and stabilize during periods of crisis when they are most vulnerable,” and given data that shows that hanging is the most frequent cause of inpatient suicide, standards “are appropriately focused on mitigating risks associated with hanging.”
The responses noted that the Joint Commission “requires organizations to treat individuals receiving care in a dignified and respectful manner” but that it does not define what creates a therapeutic environment, “as this is up to each organization based on their setting.”
“Accredited organizations have options when it comes to developing environments that are both safe and conducive to healing [and] are responsible for developing policies and procedures to promote individual autonomy and maintain a safe environment,” it said.
When a hospital is accredited by the Joint Commission, it is automatically deemed to be in compliance with the Centers for Medicare and Medicaid, according to Suzanne Leavitt, RN, who directs Vermont’s Licensing and Protection Division, which is the local arm for federal enforcement. CMS compliance is a requirement for federal funding.
She agreed that there is a difficult balance
Standards for ‘Environmental Hazards’
between protecting patient safety while also meeting the CMS definition, which includes emotional safety. Her agency does try to weigh “the personal dignity versus the hospital’s ability to keep people safe,” she said.
Leavitt said the difference in recent years is not new standards, but availability of new products that better meet safety goals.
“What strikes me” from the discussion, she said, is how it “is easier to change the environment” than make changes in other ways, such as staffing or policies – but it’s “not the CMS role” to direct hospitals on how they should meet the requirements.
Former patients have shared the distressing impact of physical safety measures. Of the 16 responding to a Counterpoint poll, 11 (68%) said that safety features to prevent self-harm made psych units feel less healing. One person commented on the online Counterpoint article, saying that, “So many things that allowed for a therapeutic and healing environment have been stripped away due to the changes,” so that the hospital experience “feels more like incarceration or punishment rather than a place to heal.”
“The pendulum needs to swing away from the extreme and find a balance... in the name of patient rights, dignity and healing,” the comment said. “What we have done to people who need this level of care is a shame. It needs to be rectified.”
Leavitt said she agreed with the suggestion that there was a potential that creating highly sterile inpatient environments might increase the risk to patients after they leave the hospital. “[We] don’t want to infantilize folks so they don’t feel prepared” after discharge, she noted.
“I would love to see that explored by the researchers in psychiatry,” Leavitt said, because regulators have to follow what research shows to “help us with the best practices.”
A report of the Joint Commission’s expert panel that developed its newest standards observed in 2017 that, “Most experts think that far more suicides occur shortly after hospital discharge, although conclusive national data are not available.” When asked by Counterpoint about any pending new research, the Joint Commission said it was “not aware of any data or studies that explore specific characteristics of the inpatient hospital environment and an association with post-discharge suicide rates or psychiatric readmission rates.”
The Joint Commission standards say it attempts to provide “clear guidelines on what constitutes serious environmental hazards that must be corrected and what mitigation strategies are acceptable in those situations when all potential hazards cannot be removed” in relation to a risk of suicide. A detailed list first published in 2017 includes requirements for areas that must be ligature-resistant, defined as meaning, “Without points where a cord, rope, bedsheet, or other fabric/ material can be looped or tied to create a sustainable point of attachment that may result in self-harm or loss of life.” The list includes:
- Psychiatric units must be ligature-resistant in patient rooms and patient bathrooms and in corridors and common patient care areas that do not have an unobstructed view from a nursing station.
- The doors between patient rooms and hallways must contain ligature-resistant hardware; the doorway between patient rooms and patient bathrooms must be ligature-free or ligature-resistant.
Excerpts from some of the responses:
“Rather than responding to suicidality with fear, responses need to be based in connection and support. What people need is hope and care, self-harm prevention provides neither.”
“There’s so much emphasis on Do No Self Harm, with little time, money, and training given to understanding what leads to that state.”
“It is dependent upon the facility. Rutland Regional Medical Center used patient input for artwork and other amenities to make the units feel less sterile or institutionalized as compared to their contemporaries operating within the state.”
“Having been in a locked ward before I can tell you this was more triggering for me. If you have ever been confined, tied down, restrained from an abuser and you suffer from claustrophobia, this heightens your panic and thus is counter-productive. Having been raped far too many times, having your clothing taken away is a massive trigger. So, for myself, the safety measures are not healing for me.”
“I believe that honoring one’s full humanity and trusting one’s ability to choose is the most healing. If that choice is taken away people can be left feeling disempowered, angry, and trapped. If I need to seek a safe place where I can get medical care when I’m feeling unbalanced, but I don’t want that place to force me to stay indoors and give up all my freedoms in exchange for the care, I might not go.”
- Patient rooms and bathrooms must have a solid ceiling.
- Medical needs and the patients’ risk for suicide must be carefully assessed and balanced to determine the optimal type of patient bed.
- Standard toilet seats with a hinged seat and lid are not a significant risk for suicide attempts or self-harm; therefore, the panel concluded that traditional toilet seats are as safe as toilets without movable seats and covers (that is, the type used in prisons), offer patients more comfort, and are less stigmatizing.
For emergency departments: Patients must be in a “safe room” that is ligature-resistant, or in the main area of the emergency department with continuous 1:1 monitoring, and removal of all objects that pose a risk for self-harm that can be easily removed. The use of “safe rooms” is not mandated. Patients with serious suicidal ideation must be placed under 1:1 continuous monitoring with observations allowing for 360-degree viewing, linked to the provision of immediate intervention by a qualified staff member.
COMMENTARY 13 Fall 2018NEWS . 13 Summer 2023
The winter Counterpoint poll asked, “Do safety features to prevent self-harm in hospital psych units make them feel like a less healing environment?”
Less Healing 68% Not Less Healing 31%
Hospitals “have options when it comes to developing environments that are both safe and conducive to healing.”
What Is a ‘Found Poem’?
by ANNE DONAHUE
If you begin reading Parallel Pathways by thumbing through, looking for a poem or story that looks appealing to read, you are likely to pause as some point and ask, “What is a ‘found poem’?”
Something written a long time ago, and recently rediscovered? Some unsigned piece of work discovered in the trash? Or maybe fluttering on a bus seat?
What you will discover, once you turn back to the opening comments, is far more intriguing.
They are works that emerge from a creative weekly process at the Pathways Writing Circle group. Members of the group begin with free writing and then sharing. During the sharing, those listening jot down, verbatim, words or phrases that “jump out at or stick with us.”
For the following week, one group member creates a new poem that is a written collage that uses as many of the group’s shared words and phrases as possible. There may be modifications to tense or a few added words, but the point of the collage is to keep the content of the group process intact.
And that is a “found poem.”
The result is a collection of works by seven writers that includes 65 stories and poetry, the majority of them labeled as found poetry – pieces that flow from a common labor but without a skip in step.
Being is not enough.
Of that, I am bitterly aware.
Maybe I’m just bitter.
Maybe this choking, suffocating feeling is from life’s half-hearted platitude; My trivial place in this desolate world; The fact that I am the person trapping me, begins the found poem, “But, I Want To Feel Important,” by Abby Levinsohn.
It’s hard to imagine it was assembled using scattered phrases, and while it’s worth admiring the process, it probably just makes more sense to enjoy the products, no matter whether labeled as found or original. They are truly captivating.
I am shouting
With no sound
Screaming at the walls
My voice
Was locked away A knot inside Me I was
Cramped in
My own body, begins another piece, by Eryn Sheehan. The works are organized in intriguing categories such as “Periods of Soul Starvation” and “Bare Feet on Pavement.” Each one reverberates with the authenticity of lived experiences of pain, fear, solidarity and mindfulness.
The Pathways Writing Circle began in 2014, with themes that “vary from homelessness, isolation, addiction, abuse, nature, relationships, recollection of childhood and early youth, death,” and more.
“All of our poems are ‘parallel pathways’ –we are all travelers through the dark night of the soul changes, each arriving stronger and wiser at the beginning of a new dawn,” the book acknowledgment says.
At the end, the contributors share brief autobiographies. They include Levinsohn, who says the weekly group “forces me to get thoughts onto paper, even if the process feels jumbled and foggy;” Eryn Sheehan, who is Studio Manager at the Howard Center Arts Collective and describes herself as “a quiet and loud, outgoing soft-spoken person;” and Edward Burke, a peer support specialist who writes that, “I would rather be a little chilly rather than hot and sweaty, and prefer maple cream on my toast to avocado.”
Katharine O’Donnell writes that she contributed three found poems; Galen Knight shares that in his imaginative world, “I prefer to dwell in solitude in mythical caves, commune with monsters and robots or live in outer space” – but likes meaningful conversations on challenging topics in his real world.
Sarah Smith says that writing “has helped me express myself” and she’s found that it is important to share her feelings with other artists; Vesna Dye closes her comments by saying, “I will continue to write till the day I die.”
Anyone is welcome to join the group, which meets every Wednesday from 4 to 5 p.m. at the Pathways Community Center at 279 North Winooski Avenue, Burlington.
“Drop in sometime and experience this breeding ground for creative expression yourself,” the authors urge.
Of the book of collected works, they write in the introduction, “We are so excited to share a snapshot with you and hope you will find our eclectic offerings to be compelling and potentially inspiring.”
And they are, indeed.
14 Summer 2023
The Arts
Morgan Brown, on Art

An Empty, Colorless, Canvas
To my way of thinking, the best art comes from the deep depths found within the soul of an individual, free flowing, without the need to necessarily adhere to either highly rigid institutional constraints or certain given social norms or other restrictions placed upon it (i.e., both the art and the individual artist; within reason, of course) fully exploring what it means to be alive as well as being someone who is living among other beings of every form and shape on this planet and, at the same time, also exploring the vast universe in every form, as these are and it uniquely is, not merely or necessarily how these might be perceived or how one might want these to be in order to fit their own limited purposes and needs.
 by Morgan Brown, Montpelier
by Morgan Brown, Montpelier
Absent requisite artistic studio space, not to mention various and necessary art supplies, currently unavailable with which to explore and pursue one’s lifelong dream, hope and vision to potentially endeavor among the ever beautiful, flowering, glorious, promising and often satisfying fields found in the creative and expressive arts; due to these being rather unaffordable, while subsisting on a low fixed income; which is also something that one well knows about how they, having been overly priced out, are not, by any means, alone in experiencing, for that matter, either; since it has been often said that “a picture is worth a thousand words”; save for doing so within one’s imagination; not to mention within a somewhat conversely or unconventional fashion; one is left to draw, paint and sketch with words alone, in black and white, on an otherwise bland and empty, colorless, canvas; however, done in far short than the sufficient amount of 1000 words; yet still being hopeful that the point as well as lingering disappointment, frustration and inner torment manages to be conveyed all the same.
(circa:
by MORGAN BROWN
Writing Contest
Fall 2018 The Arts . 15 15 Summer 2023 $250 in Prizes! Send submissions by email to: counterpoint@vermontpsychiatricsurvivors.org or by mail to: Counterpoint , The Service Building, 128 Merchants Row, Suite 606, Rutland, VT 05701 include Named for a former Vermont activist to encourage creative writing by psychiatric survivors, mental health consumers and peers. One entry per category
or poetry); 3,000 word preferred maximum. Repeat entrants
to two First Place awards. Entries are judged by an independent panel. Winners will be published in the fall, 2023 Counterpoint
(prose
limited
‘Old computer generated art of mine from years ago. Left, circa: 2009; while still living without permanent housing: i.e., living unhoused aka homeless; Right, unknown date however more than likely from 2009 as well.’ Morgan Brown
An old pencil sketch of mine of my cat Cleopatra, using various techniques including the use of small pieces of paper as well as a pencil eraser to smudge for the purposes of creating an illusion or sense of texture. Cleo was actually laying on her side snoozing away on the nearby living room chair at the time. In my youth, I had learned the artistic technique –from an elementary school art teacher – of drawing from one’s mind’s eye rather than from directly looking at a subject and it can be much more effective in my opinion.
2016)
Clara Martin Center Artists Are
Being Together Warm Heartfelt Hugs
I think of being healthy
Together forever
With friends that last
Looking to the future with hope
Remember the good times
Being together is better
Than being alone.
by MIKE FITZGERALD
I would rather have a warm heartfelt hug than any opiate drug. There is no match from the high you get from a heartfelt hug. It will take you higher than an opiate drug. I know this for a fact. I have been in both places and seen the faces and that opiate drug will take you to many dark places.
by JAMES MURRAY
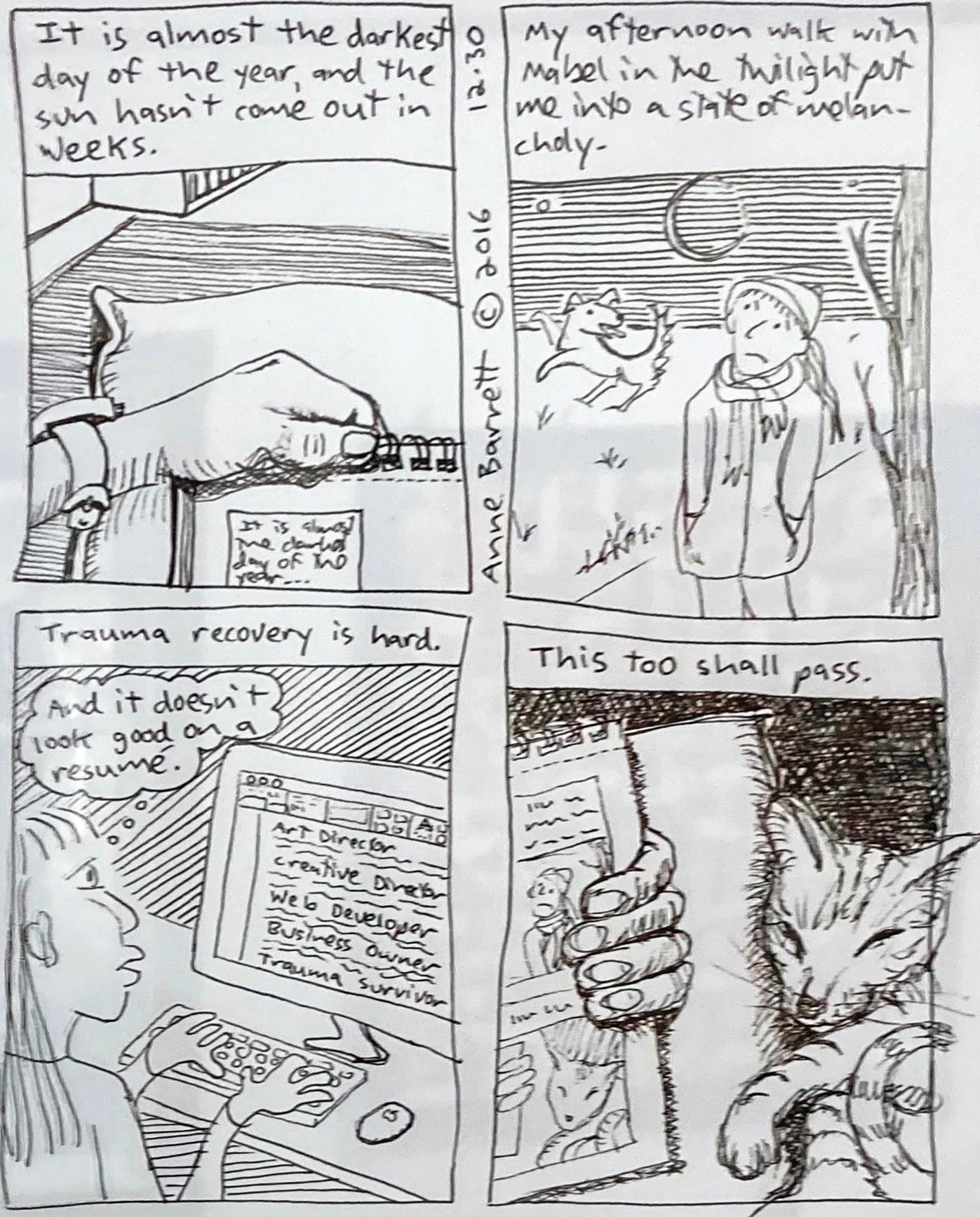 by SHERRY DUVAL
by SHERRY DUVAL
Poetry by our readers
The Deer
I am a deer, a very big buck
You see I’m on an adventure
To be the best buck I can be
Running through the forest
Seeing all I can see
Maybe finding other deer to frolic with
Would be nice finding my own herd
Finding my own family to call my own
But for now, I will keep on running through the woods
On to the sunset to be free and happy
To be the best deer I can be
Finding a sense of peace and tranquility
See the day turn to night and the night turn to day
psych place
there is progress in this slow race nobody here keeps the same pace you can tell by the look on their face but no one wants to be in this place And they always take away your shoelace the security is too tight for me to escape so I’ll just do what I need to until they let me out of the gate
by COLIN STOCKWELL Brattleboro
Ah, Paradise
This poem shall be a poem about flowers. The flowers of doom. And they tell me I like it, And yet, studies show, And I don’t know why, nor do I know how, But I like to do what I like to do.
Is there more to it than that?
And why is this poem so self-centered anyway?
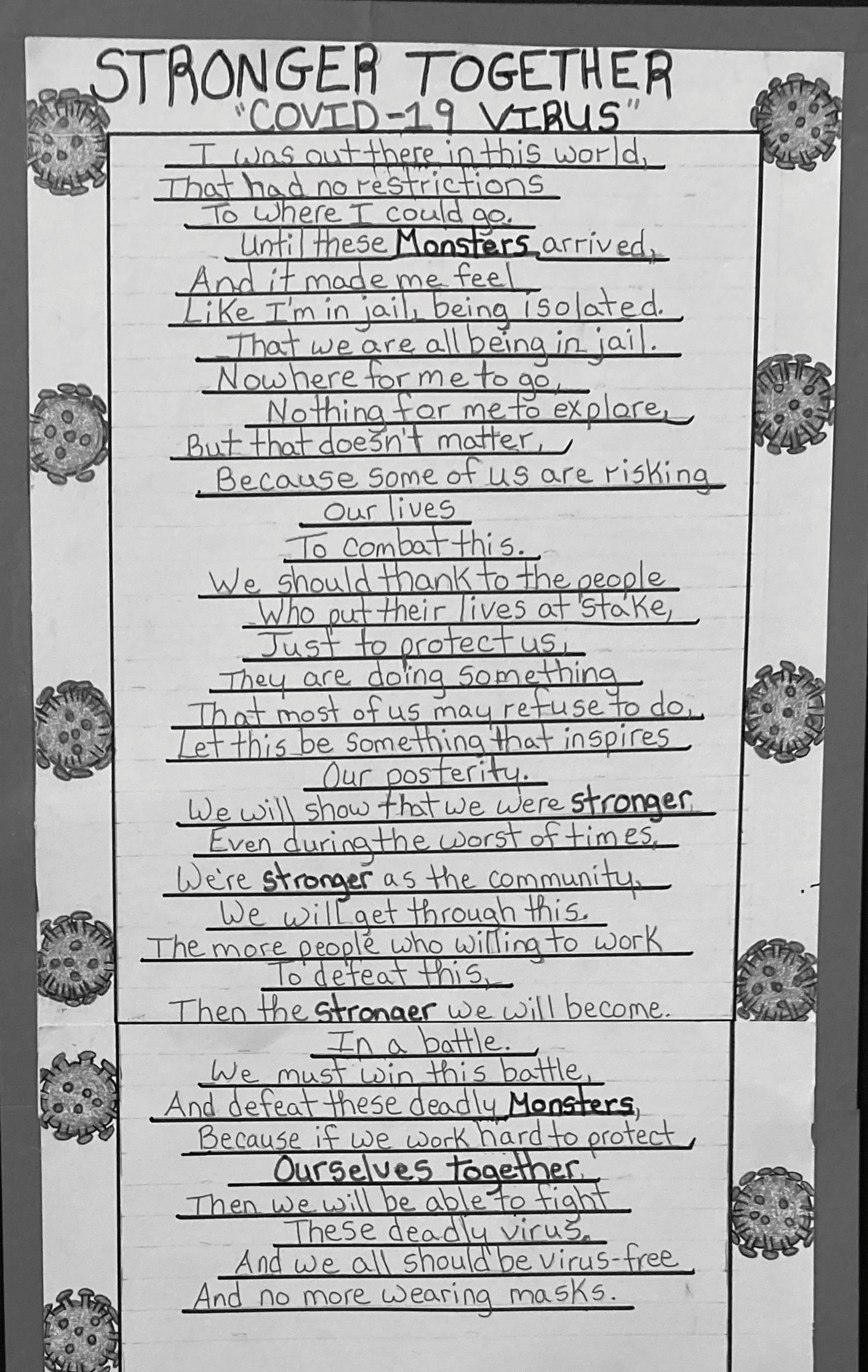
Now I must go drink from a stream and eat leaves from a tree
Hoping one day for that herd of mine
When that day comes we will all be the best deer we can be
The greatest herd roaming through the forest
by NATHANIEL GREENE Bellows Falls
I’ll write in Czechoslovakian if I know how, I’ll write however I write.
Is there any end to the trials that one endures
Before one reaches paradise?
Ah, paradise, what a nice idea.
by ANTHONY PARSHALL Essex Junction
The Arts 16 Fall 2018
Trauma Recovery by ANNE BARNETT
Summer 2023
Stronger Together
Show Celebrates Creativity In Mental Health, Wellness and Recovery
The 6th annual Clara Martin community art show celebrated mental health and creative expression as an essential part of overall well-being. The White River Craft Center in Randolph hosted the exhibition.




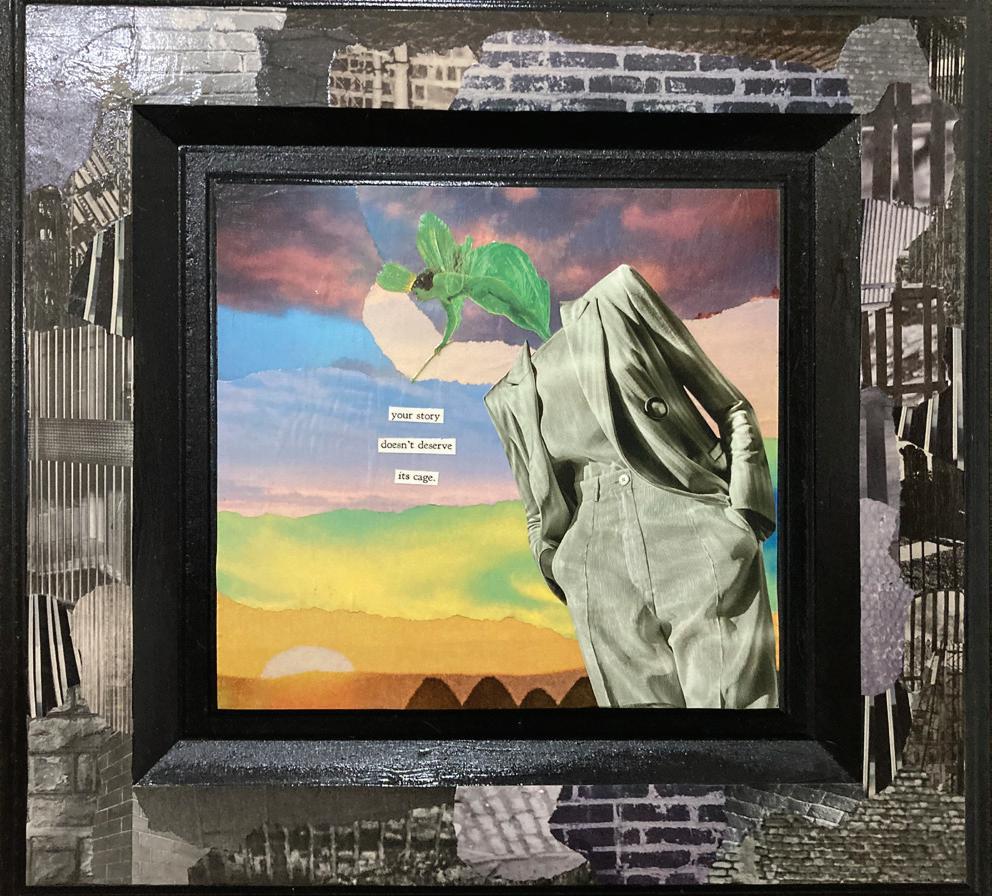

Titles, descriptions and artists’ names are recorded as posted at the exhibition. Some were anonymous.

The Arts . 17 17 Summer 2023
Untitled, collage and construction paper, by ALLYSA DYKEMAN
Your Story, collage on cabinet door, by HEATHER STERNS
Into Fall 3, acrylic and collage, by DAWN LITTLEPAGE
Come Together, watercolor and marker by KOHL COMTESS
Signs photo series, n1 of 3
We Drew a Circle, fabric, by KAREN LOWRY REED
Yester Years Lessons for Us Today, watercolor on sap bucket cover, by MICHAEL BARNABY
Quilted Flag wall hanging
Stronger Together, acrylic and mixed media, by MARLANNE MULLEN
Garden at Night, by MEG DUNN
When Help Hurts
The good intention to help others sometimes flies smackdab into causing harm instead.
How does one balance the good intent of creating a safe physical space for people in crisis against the damage of a space so sanitized and dehumanizing that those same people are at greater risk of self-harm once they are discharged from the hospital?
How does one balance the desire to send help to interrupt an intended suicide against the betrayal from a breach of confidentiality and the potential lives lost if people in crisis do not feel safe to call a hot line?
How does one balance the desire to help someone escape the pain of a psychotic episode against the loss of all trust in a system that uses forced medication?
These are all real questions, both old and new. The sad thing is that the policy decisions that prioritize immediate help are based neither on research nor on patient-driven principles. There is rarely input from the people who are subjected to these “safety measures” but may be damaged by the effects.
The debate over forced treatment is a longstanding one. There is no research, however, on the long-term impacts on people who might be temporarily stabilized and able to leave the hospital, but then never reach long term recovery because they reject future voluntary help from a system that violated them. Advocates have begged for this kind of research, to no avail.
Over the past several decades, oversight agencies have demanded “ligature-proof” hospital units to prevent inpatient suicides, even though they have always been rare events.
Patients have lost access to simple opportunities to rebuild skills for a return to the community. Once there were group cooking sessions, the simple availability of self-care by making tea or using the laundry, opportunities to exercise or get fresh outside air. Now, some hospitals even lock bathrooms, forcing patients into the inherently demeaning position of having to ask staff to allow them to use it.
These types of disempowerment clearly interfere with a recovery-oriented environment, and research has long established that the time of greatest risk of suicide is not in the hospital, but in the time frame immediately after leaving. A person goes from a totally protected environment to a totally unsupported one.

To what degree are deaths from self-harm after discharge on the increase, as those protected environments become more and more sanitized of any normal environmental risks?
We don’t know, because it is not being researched.
Now, just in the past year, we have seen the elimination of any remaining confidential suicide prevention hot lines. They say they are confidential, because the conversations are private.
But if you admit during that “confidential” phone call that you have a serious intention and plan for suicide our modern world of GPS and phone tracking means that even if you refuse consent, “help” will be sent to your location. And that help may be in the form of a police response.
No one wants someone to die for lack of help – to be on the phone and have the call be cut off by a lethal act of selfharm. “Allowing” that to happen may be inconceivable.
But how many people use a hot line precisely because they believe it is a confidential way to reach out, only to discover that it is not? How many people may die instead because they are now afraid to even make that call? Because they want someone to support them, but don’t want their confidentiality breached or the police to be called in?
We don’t know. There is no research.
And there may be conversation among the “helpers” about how to balance among priorities, but the voices of those affected by the decisions are, once again, being left out.
Opinions
Cartoon by Thompson

Tips To Fight Panic Attacks
by STAN POPOVICH
As a published author of a managing fear book, I struggled with fear and anxiety for over 20 years.
I am sharing my thoughts here on how to deal with a panic attack.
A person can experience a panic attack when they least expect it. This can cause a great deal of fear and anxiety for the person.
Many people do not know what they should do when dealing with a panic attack. As a result, here are my eight easy steps a person can follow when a panic attack strikes unexpectedly.
1. Take a break:
A panic attack can be very uncomfortable and can affect a person’s thinking. The best thing to do when this happens is to take a break in order to calm down. You don’t want to do anything when you’re not thinking clearly.
2. Take deep breaths:
A person should take some deep breaths to help feel better and to get rid of some of the excessive fear and anxiety. There are many kinds of breathing exercises a person can learn to follow with the help of a mental health counselor. Taking some deep breaths can help a person relax right away.
3. Distract yourself: A person should try to distract themselves from the panic they are experiencing.
A person could get some fresh air, listen to some music, take a brisk walk, read the newspaper, or do something relaxing that will give them a fresh perspective on things.
4. Visualize a red stop sign: A person should visualize a red stop sign in their mind when they encounter a fearful thought.
When the negative thought comes, a person should think of a red stop sign that serves as a reminder to stop focusing on that thought and to think of something else. A person can then try to think of something positive to replace the negative thought.
5. Get the facts of your situation: Many people feel helpless when they experience a panic attack for the first time. The fact is that you will be OK and that it takes a few minutes for the anxiety to go away.
Talk to a counselor and get the facts of what a panic attack is and what you can do when a panic attack occurs.
6. Don’t dwell on your thoughts:
A person must not dwell or focus on their thoughts during a panic attack. The more a person tries to reason out their thoughts the longer a panic attack will last. Read some positive statements from your favorite self-help book to help overcome your negative thoughts during a panic attack.
7. Read positive affirmations:
Another technique that is very helpful is to have a small notebook of positive statements that makes you feel good. Whenever you come across an affirmation that makes you feel good, write it down in a small notebook that you can carry around with you in your pocket.
Whenever you feel depressed, open up your small notebook and read those statement.
8. Get help:
It is important to talk to a qualified professional in order to learn how to survive a panic attack.
By talking to a professional, a person will be helping themselves in the long run because they will become better able to deal with any panic attacks that may occur in the future.
Fall 2018 E18 Summer 2023 COMMENTARY Editorial
Stan Popovich is the author of the managing fear book, “A Layman’s Guide to Managing Fear.” He is from Pittsburg.
Needs of Brain Injury Patients Are Not Being Met
To the Editor:
(This comment was in response to the article in the winter Counterpoint on federal rules regarding conflict of interest practices, and the need to correct violations in Vermont.)
Where will the funding come from?
It MUST come from federal dollars.
Please watch [a] world-renowned economist describing how such a national healthcare program should look: www.youtube.com/ watch?v=lypnn9fLTVs
We brain injury patients are not told what services and treatments are available to us and do not receive the care we need to meet our needs. I didn’t even get a case manager after suffering a complex head injury including a moderate TBI, skull fractures, excruciating pain from facial fractures (trigeminal neuralgia), vision impairment from eye socket reconstruction, cognitive impairment (couldn’t comprehend
written material), medically restricted from driving (being the only adult in my home)…
I clearly qualified as a complex patient case. Because I went without, I now suffer chronic issues that are difficult to treat. I found out through Brain Injury Peer Support groups that my peers were receiving care that I didn’t but should have.
The medical literature describes BI care and services that I should have received. Why aren’t we?
Actually, the most common question my peers ask is, “Who is coordinating my care?”
There is so much more going on here: “conflict of interest” of case management than what this article describes, what our medical professionals and administrators will admit to.
I was told “If I give you that referral, I’d have to give one to everyone.” Which says to me something is wrong here and we should
investigate. I’ve a feeling it has to do with BI patients being “high cost patients.”
What is the mission of our healthcare system if not to meet the needs of our patients?
CHERYL L. VAN EPPS
Dissatisfaction
To the Editor:
I am extremely dissatisfied with my local community mental health agency. I do not receive the support that I need... except to prescribe my meds.
Phone calls are never returned. Shortage of staff. High absenteeism of staff. Never very dependable, either. Always some excuse for not being there.
If you do have any suggestions as to how I can deal with this situation, please write!
RICHARD A. WILLIAMS Bennington
Discovering and Embracing Neurodiversity
by LAURA SHANKS
When I started working at Vermont Psychiatric Survivors, I was introduced to the term neurodiversity and discovered I am neurodivergent.
As someone who doesn’t support most modern Western psychiatric practices, diagnoses, or forms of treatment (I follow holistic and alternative health care practices), I was delighted to learn about the movement.
Diagnosed with ADHD, I think and function differently than the average person. Neurodiversity embraces alternative ways of cognitive functioning as just another way of being rather than a disease that needs to be cured. As someone who didn’t finally get “better” until I started to love and embrace myself for who I really am, this really resonates with me.
The word “neurodiversity” was coined by sociologist Judy Singer in 1998 and is a shortened version of neurological diversity. It is the concept that there are natural variations in human brains that lead to differences in how we think, behave, and interact with our environment.
Neurological differences like autism, ADHD, dyslexia, etc. are just that differences. The
neurodiversity movement purports that different brains work differently and have inherent strengths and weaknesses and that this is not a pathological disorder, but rather a form of diversity, like race or ethnicity.
Neurodiversity is viewed as an asset to society as different approaches and skillsets are valuable and provide more growth.
The movement proposes that challenges met by the neurodiverse community aren’t necessarily inherent to their brain’s differences, but rather, the social and physical environment we live in (Social Model of Disability).
people (those who do not fall under the neurodiverse umbrella) aren’t aware of it. Many still misunderstand autism, ADHD, Tourette’s, etc., and assume they are only the exaggerated and distorted views portrayed in the media.
The same way non typical sexual and gender preferences were once viewed as disease, I have no doubt acceptance of neurodiversity on a larger scale is around the corner, we just need to spread the word.
At the end of the day, while I personally feel a strong connection to the neurodiversity movement and agree that neurodiversity very much exists and is a beautiful thing, I also recognize that overly identifying with any label can be harmful.
Neurodiversity has been a popular topic in our weekly peer support, and I have found that neurodiverse peers resonate with the movement, embracing their differences rather than viewing them as symptoms.
We all have brains that are designed to work and learn differently, giving us unique and special personality traits.
Being told that these differences are wrong, or being forced to mask them, often comes at the cost of our self-esteem, as well as mental, emotional, and physical well-being.
The neurodiversity movement is still young, however, and one of the biggest issues I ran into in writing this article is that most neurotypical
It is the nature of the mind to categorize and label. This is how it sorts and stores information as memory, which is helpful, but when we cling to these labels it can create an “us versus them” mentality which is dangerous.
“People really need to take a step back and remember who they really are without any of these labels.” – from a Vermont peer
We are all unique, special, and different. Accepting and supporting ourselves and others, no matter the label, is ultimately the most effective form of care.
Laura Shanks is a Patient Representative at Vermont Psychiatric Survivors.

Fall 2018 19 Summer 2023 COMMENTARY
Letters to the Editor
Do You Have Thoughts or Reactions to Our Commentaries? Please Share Them! COUNTERPOINT IS THE PLACE FOR YOUR VOICE. Have an Issue to Discuss with Other Survivors? Send your comments or reactions to editorials or commentaries to: Counterpoint, The Service Building, 128 Merchants Row, Suite 606, Rutland, VT 05701, or to counterpoint@vermontpsychiatricsurvivors.org Please include name, address and email. Counterpoint welcomes letters to the editor and commentaries on all topics. Names and contact information must be disclosed to verify authorship, but requests may be made to withhold them from publishing. Submissions may not include names of private individuals without consent. The editor reserves the right to edit submissions for length or clarity or if they are libelous or profane. Letters or commentaries do not represent the opinion of the publisher.
“It is no measure of health to be adjusted to a profoundly sick society.”
– J. Krishnamurti
Officer, Now a Peer Specialist, Chronicles His Recovery ‘You Could Be a Light’
by ADAM A. MEYERS
My name is Adam A. Meyers and I was a police officer in Wisconsin for 21 years.

On Friday, April 8, 2016, at 5:15 p.m., I was involved in a critical incident when I used deadly force against someone who armed themselves with a hatchet inside a busy department store. This person died.
I faced many personal and professional mental health challenges after my critical incident. I have been diagnosed with a mental illness, and it has taken me many years to get back on track. I continue to struggle, but I am better than I was.
There are many different coping strategies people may use after experiencing trauma. They may be good and healthy, or they may be bad and unhealthy.
My coping strategies were bad, unhealthy, self-destructive, and dangerous. I used alcohol, marijuana, casual sex, and self-harm as some of my poor coping strategies for years after my critical incident.
My poor coping strategies easily put my relationships, my job, and my health at risk, but I did not care. I wanted to escape from what I was feeling. I wanted to numb my emotions, my thoughts, my body, and any memory of taking someone’s life. I wanted to feel better even if only momentarily.
I was selfish, reckless, and I did not care how my self-destructive and dangerous behavior might affect other people. I did not even care how my behavior affected my family, friends, co-workers, or the public.
Prior to my critical incident I collected wine and enjoyed a glass of wine every now and then. However, after my critical incident I began abusing liquor, mainly whiskey and the cheapest vodka I could get my hands on.
I would consume whiskey and vodka straight from their bottles or on the rocks, or I would create my own cocktails by combining over-thecounter liquid sleep aids or allergy medicines.
There were times that I would mix in whatever leftover prescription medicines I had in the medicine cabinet, and it did not matter if they were prescribed to me or someone else. Abusing alcohol may have been a quick fix, but it caused me even more stress, anxiety, and depression.
There were many times I did not want to go to work. This was not because I had other plans or that I was hungover from consuming too much alcohol, but I just wanted to stay at home and isolate myself from the world. I wanted to lock all the doors of my home, close all the curtains, and shut everyone out of my life.
Sure, I called in sick from time to time, but on one occasion, I intentionally injured myself so that I did not have to work.
I used an old 12-inch adjustable steel wrench to cause superficial injuries to my left knee. I struck my knee a dozen or more times, enough to cause redness, abrasions, and bruising, and limped into the local emergency room.
I explained to the doctor and nurses that I had tripped and fell down walking out of the back door of my house and struck my knee on the steel covering of an underground septic tank.
My story was believable enough. I received x-rays of my knee, a prescription for pain medication, and crutches. I was discharged from the emergency room with a doctor’s letter releasing me from work for about one week.
Another way I was able to get out of working was to intentionally make myself sick. I remember while taking a shower before my shift I was thinking about the many ways I could get out of working.
While I was putting on my ballistic vest, uniform, boots, and duty belt, I thought to myself, “I’m going to get out of working by binge eating and making myself vomit.” I constructed a plan to visit the local Burger King drive-thru while traveling to work.
I ordered a bunch of breakfast food and made sure I washed it down with a large soda and a large orange juice. I was about to pass the local McDonalds and thought to myself, “Two is better than one.” I quickly binged what I purchased and proceeded to work.
I arrived at work and upon exiting my vehicle I played the role of the sick employee. I walked into the police department and made myself vomit in
was a Glock 22 Gen 4 – 40 Caliber. I put my duty weapon to my head at least a dozen times. Sometimes I even placed the barrel in my mouth. I would always remove the magazine, but the round from the chamber could still be discharged. I very easily could have accidentally killed myself. I did this while I was under the influence of alcohol.
I still do not truly understand why I did this and sometimes wonder how many times it happened while I was blacked out from excessively consuming alcohol. I am very fortunate to be alive.
I suffered in silence for many years after my critical incident and I am ashamed for the ways I poorly coped. I find it hard to believe that nobody realized or even had a gut feeling that I was not doing well.
I could not have been that good at hiding my poor coping strategies, or was I? I have always wondered if people were slowly watching me self-destruct because they did not know what to say to me, how to help me, or they simply did not want to get involved.
I was diagnosed with a mental illness in January 2022 and deemed unfit for duty by the police department’s psychologist. I was granted a 90 day leave of absence and began intensive therapy two and three times a week.
This therapy included in-person psychotherapy, Eye Movement Desensitization Reprocessing (EMDR), Biofeedback, and Dialectical Behavioral Therapy (DBT).
I was finally undergoing treatment that helped me heal and understand why I’d adopted poor coping strategies such as self-medication. I only wished I would have begun this therapy five years earlier, but it was better later than never.
the bathroom. I made sure the bathroom door remained open so that anyone walking by could see or hear me. I was immediately sent home.
Another way I dangerously coped was drinking and driving.
Prior to attending any type of social event, even as simple as going to the grocery store, I would consume alcohol. I would travel to a nearby gas station and purchase many small bottles of liquor containing about 1.5 ounces of whiskey, vodka or whatever I could afford at the time.
I would immediately consume the alcohol in my vehicle prior to traveling to my destination. I tossed the empty bottles in the back of my vehicle or out the window while I was driving.
I would rationalize that it would take about 30 minutes for me to feel the effects of the alcohol and by the time I was impaired I would have arrived at my destination. I was very fortunate that I was not arrested for drinking and driving or even worse, killing someone.
I used casual sex as a coping strategy and to distract myself from my emotional discomfort and pain. I would meet women and sometimes within 30 minutes we would have sex.
Although this type of sexual behavior was risky, self-destructive, and caused me stress and anxiety, it was not enough to convince me to stop. I wanted an instant feel-good escape from my life and casual sex provided that for me.
Another dangerous and unexplainable way I coped was putting my duty weapon to my head. My duty weapon during my critical incident
In May 2022 my leave of absence was not extended and I was given the option to resign or be terminated from the police department. I refused to resign and was terminated.
I continue weekly therapy that includes inperson psychotherapy and EMDR. I am also prescribed Lexapro and Propranolol that help me with my depression and generalized anxiety.
I have been able to move past my poor coping strategies because of the support I receive from family, friends, therapist, girlfriend, and my current employer and co-workers.
I would not be where I am today without their support. I am very grateful and will never be able to put into words how much their support means to me.
Please reach out to someone if you believe they are struggling with their mental health.
I know it may feel awkward or uncomfortable, but most people will not admit they are struggling, and most people will not reach out for help. You could be a light during a very dark time in their life.
Adam A. Meyers is a Certified Peer Specialist who lives in Oconomowoc, Wisconsin. His experience of killing a suspect as a police officer plagued him with feelings of guilt and trauma, and led him to found Stop the Threat — Stop the Stigma in 2020, an organization devoted to eliminating the stigma around speaking about mental health in a profession often linked to facing fears daily and carrying on. More information about Stop the Threat — Stop the Stigma is available at its website: stopthethreatstopthestigma.org
COMMENTARY 20 Fall 2018 Summer 2023 COMMENTARY
‘My coping strategies were bad, unhealthy, self-destructive and dangerous... I did not care.’
Reaction to a Bill To Arrest Patients in the Emergency Room:
Address Causes of Violence First
by HEIDI HENKEL
Isupport the goal for health care workers in emergency rooms to have good workplace safety and not get injured or work under the threat of possible injury.
I doubt that arresting people who threaten or commit violence in the ER, and sending them back out onto the street with their physical and mental health conditions untreated, is a good way to accomplish that.
I am concerned that it would leave the causes of the person’s poor social functioning, which could include mental illness and/or delirium caused by the medical condition they’re seeking help for by going to the ER, untreated, and push the behavior out into the community.
Perhaps the person will be terrified by having been arrested, and will be afraid to seek medical care or mental health care in the future.
I also don’t think arresting people in the ER will do much to make the ER a safer place to work, because it wouldn’t address the reasons why people become violent in the ER.
There are three reasons for violence in the ER:
1. Delirium from serious medical problems.
A wide range of medical problems can cause delirium. Infections, organ failures, extreme blood loss, etc. Delirium can include anger, confusion, and even violence.
Treat the medical condition. Try to deescalate the patient. If needed, restrain and sedate the patient in order to do that. Be quick to treat the medical condition that is causing the delirium.
How to prevent violence in cases of delirium: Check patients for delirium and for medical conditions that could lead to delirium, thoroughly and frequently. Some physiological causes of delirium can be detected more quickly by regularly taking blood pressures, oxygen saturation, temperature, and other simple things.
Preventing, detecting, and rapidly treating delirium and the physiological causes of delirium is the primary strategy.
2. A mental health crisis, when the patient has come to the ER to get help with their crisis.
If the patient doesn’t get help soon, the patient’s condition can deteriorate, so it’s important to help the patient soon. Having a cozy, friendly, low-stress architecture and décor, well-staffed living-room type situation for people in mental health crisis, would help.
Peer support specialists could be a big part of this. Focus on psychosocial strategies and start addressing the mental health crisis immediately, no warehousing.
Open Dialogue is the most effective modality for psychosis in the world, and can be carried out by peer support specialists who are trained in Open Dialogue. One reason Open Dialogue is so effective is because it is started within a few hours of when the patient or their family makes a request for help.
Peer support strategies are also very effective more effective than hospitalization and medication for people considering suicide.
Peer support specialists should be in ERs to help people in mental health crisis. It would be great for there to be other mental health professionals there, too. The long-term outcome of a mental health crisis is much better if psychosocial interventions begin very quickly.
It should be prioritized like any other medical condition in which the long-term outcome is better if intervention begins very quickly.
A lumbar spine fracture with pressure on the spinal cord is an example of an injury where the long-term outcome is likely to be much better if intervention happens quickly (permanent paralysis vs not having permanent paralysis).
That’s triaged right after severe bleeding, cardiac arrest, and respiratory arrest. Mental health crises should be prioritized similarly because the long-term outcome is similarly impacted by how quickly they’re responded to.
The most effective interventions are psychosocial, so let’s make sure that gets started within an hour after the patient walks in the door. That would prevent most assaults due to mental health crisis.
Psychosocial strategies can also help in deescalating patients who are already escalated when they first walk in the door.
to interact interpersonally with patients, to make them feel heard, make sure they understand what’s happening, detect delirium early, start meaningful psychosocial interventions quickly for people who are there for psych reasons, etc.
More other places for people to go with emergencies, to alleviate the overload on ERs. More urgent care centers, primary care, and peer-run crisis respites.
Fewer mental health emergencies, by having more and better outpatient mental health care.
Video monitoring in the emergency department, so that people can be held accountable later, for violent or threatening behavior. If there’s an assault or threat that’s a clear behavior choice and not driven by the patient’s medical condition, the hospital can prosecute using the video footage.
Video footage can also protect patients in the event that they’re being accused of something they didn’t do or that’s more complex (for example, a staff person assaulted them first, or their behavior was misunderstood, or their behavior was caused by the condition they came to the ER to get treated.)
A variety of pain mitigation strategies, including other methods besides opioids.
I had a severe, rapidly bleeding puncture wound in the Brattleboro ER, and they had someone to just hold my hand during the entire surgery because I didn’t want to be anesthetized.
Hand-holding is an excellent pain mitigation strategy. Be creative. There’s something in between giving opioids, and ignoring the patient’s pain.
Things to bear in mind:
The biggest investments should be in psychosocial training for all ER staff in deescalation and interacting with people who have emotional trauma and/or are in an extreme state, and into making sure that mental health crisis patients begin getting meaningful psychosocial care within an hour of walking in the door.
3. Patients who have some trauma background and then get triggered in the ER by a misunderstanding, miscommunication, or something a staff person does.
People can get triggered if they don’t understand what’s happening, if a staff person doesn’t explain what they’re going to do before doing it, if there isn’t consent, if the patient doesn’t feel heard, if the patient’s concern isn’t being addressed and the patient doesn’t know why, etc. Staff need training about how to do trauma-informed care.
Peer support workers could help as communication helpers to make sure the patient understands what is happening, and to listen to the patient about their feelings and concerns. This could defuse some tension and help make sure the patient is getting their questions answered and getting their concerns heard.
Some patients don’t know how to assert their needs without coming across as too aggressive. The communication support person can help them communicate in a way that they get taken seriously but that doesn’t come across as aggressive.
Some other things that may be helpful:
More staff in the ER, so patients can be treated more quickly and there are more staff available
Many patients have combinations of mental health and physical health issues. One patient can have significant mental health needs and physical health needs at the same time.
People who go to ERs are in a lot of distress. Openly expressing their distress shouldn’t be criminalized. ER staff need to learn to deal with patients’ distress with compassion and without being distracted by it.
Have communication support helpers listen to some of the patients’ raw feelings. Don’t criminalize behavior that’s part of the condition they went to the ER to get help with. You don’t want to deter people from seeking help in the ER in the future.
Use prosecution, not arrest, as the deterrent. Use video footage (with other patients blurred) to prosecute people who intentionally choose to threaten or assault ER staff.
It’s important to make sure ER staff have adequate debriefing so that they have enough emotional support about the tough and sometimes scary things they go through, working in the ER.
Heidi Henkel is a psychiatric survivor from Putney. She provided written public comments to the House Judiciary Committee on the proposed bill to permit arrest and removal of patients in health care facilities, and this commentary provides excerpts from that testimony.
Henkel has a B.S. in “Human Movement and Health,” has worked as a one-on-one community mental health worker with traumatized children and adults and currently does home health personal care for people with serious illnesses and disabilities, including with delirium and dementia.

COMMENTARY . 21 Fall 2018 COMMENTARY. Summer 2023
Don’t criminalize behavior that’s part of the condition a person went to the ER to get help with.
It’s Time To Say Farewell
by ANNE DONAHUE
Almost 25 years. That’s how long it’s been since I took on the job as editor of Counterpoint. This is my final issue; I’m retiring this month.
The changes over that time in the psychiatric survivor world have been a kaleidoscope of the good and bad, of progress and setbacks.
Some moments are etched into memory:
The day that Running Deer Hunter sat in front of the Public Oversight Committee in 2000 and told them what it meant, as a psychiatric patient confined to a ward for weeks, to be able to place one’s hands into the soil and connect with the earth.
Simple, profound words that resonated. The committee was considering criteria for approval of the new inpatient units at what is now the University of Vermont Medical Center. Her words led them to include a requirement that the hospital create an outdoor area for patients. That small patch of garden exists today thanks to her words.
Her words reverberated beyond that, because today, it is considered the standard of care when designing new psychiatric inpatient units to include outdoor space.
Fast forward to 2022, when another expatient described the “Walk of Shame” experienced when escorted from the emergency room to an inpatient unit by a security guard, for all the public to see. Those words led a hospital administrator to “walk in those shoes” and recognize for the first time what that must feel like. The routine use of security ended.
And sometimes, it is a picture that is worth 1,000 words. A little boy, chained at the waist and feet with handcuffs nearly slipping off his wrists because they were so much too big for him.
A photo snatched by his father, who watched in horror when sheriff’s officers shackled the 10-year-old for the trip from Rutland to the Brattleboro Retreat. He raced to a drugstore to buy a box camera and beat the sheriffs to the hospital to snap his son being escorted down the sidewalk.
He brought those pictures to Counterpoint. We contacted the Secretary of the Agency of Human Services and asked whether he wanted to be the subject of a press conference, or a cosponsor. He chose co-sponsor and announced an immediate suspension of the automatic practice of shackling for all transports, and within a year, the legislature banned the practice for both children and adults being transported to the hospital by sheriffs, unless it was essential for safety – in which case, soft restraints should be used.
Now finally, well over a decade later, that same standard has a been adopted in law for transports by local police as well.
Shocked by a commentary that a reader sent into Counterpoint several years ago, legislators saw to it that children waiting in emergency departments now get activity kits to distract and comfort them.
Each of these were the voices of a single person, but Counterpoint was there to record
the moment and carry the momentum forward.
Counterpoint has recorded the frustrations of our movement for dignity and fair treatment as well, and I have lived through both the celebrations and frustrations.
The Brattleboro Retreat continues to lock off its bathrooms and to require patients to have to find a staff person to get access, despite our front-page coverage after they first initiated the degrading practice and despite our advocacy with oversight bodies.
Forced medication continues in our hospitals, as does restraint and seclusion. It was advocacy, however, that forced greater transparency in tracking when and where it happens, most recently with the addition of when it happens to patients not in the custody of the state: those who are admitted voluntarily for care.
The Department of Mental Health continues to act as though creating a consumer-led system means telling psychiatric survivors after major decisions are made, and asking for input on finishing touches such as what the color of the paint should be in a new lock-up.
Institutions continue to get funding priority over peer supports, and the Department insists on calling locked facilities “community-based” programs.
This year, for the first time ever, the Department gained legislative authority to use restraint and seclusion in a locked “residence” that will be used for forensic patients.
In these 25 years, a lot has changed in the newspaper publishing world as well. When I started, I had a darkroom in my basement where I developed film, and “cut and paste” meant scissors and glue to attach articles to the sheets of paper matting that would be hand carried and driven over to the printing presses.
Now, it is all computerized, from downloading digital photos to page makeup to online transfer to the printer. Counterpoint, too, has become available online as well as in hard copy –including archived editions since 2005. It went through a major new graphic redesign in 2015 and added color pages.
I still drive the roads to every part of Vermont to place it on the newsstands at grocery stores and health clinics and laundromats and mental health centers in order to be easily accessible. I love driving that route three times a year, most especially to hear the welcoming voices saying, “Oh, great, the new Counterpoint. People have been asking when it is coming.” I’ll miss that.
I won’t stop being a voice for all of us who struggle with stigma and discrimination. I’ll continue as a citizen advocate, as well as in the legislature.
Being elected to the legislature 20 years ago as a known psychiatric survivor was a proud moment. I had battled through multiple hospitalizations and spent years recovering from memory loss from two rounds of ECT.
But I had also achieved name recognition leading Vermont Psychiatric Survivors’ role in blocking UVMMC from building its new psych inpatient units in Colchester, under the slogan, “We learned a long time ago there is no such thing as separate but equal.” The CEO went to federal prison for lying to regulators about the project.
In the early legislative sessions, I was still experiencing a lot of ups and downs, but the time already spent with Counterpoint – my first job coming off disability – had strengthened me.
Despite our voices saying that the term “behavioral health” is offensive and hurtful, DMH has failed to re-title a new federal project that is being adopted in Vermont.
This spring, a legislative committee refused to remove that same term from the language of a bill, reversing years of policy that respected that request from psychiatric survivors. Coming from legislative peers who were thought to be allies, it was a deep hurt and the most traumatic experience of my years in the legislature.
Although the pressure to grow more peer programs continues to make little headway, there are symbols of major success over the past decade, like Alyssum, the peer respite in Rochester that opened in 2011 and Soteria, the peer hospital-alternative in Burlington that opened in 2015.
The Collaborative Care model – a Vermontmade version of Finland’s groundbreaking “Open Dialogue” collaboration that includes peer support – continues to grow.
A certification program for peer support staff finally seems imminent and will open the path for more positions.
Maybe one day those peer staff will finally be welcomed into emergency departments to help reassure and calm patients in crisis, in place of the “sitters” who stand guard without interacting at all.
One survivor who had come to Vermont to give a talk about peer support work and who had a job in a psychiatric hospital in Massachusetts joked that it was a literal case of “the inmate having the keys to the asylum.” I teased back, “well, I have the keys to the statehouse.”
I think I have made a difference in being there and have no immediate plans to retire from the legislature.
What makes me happiest as I retire from Counterpoint is in knowing that it is in good hands. It isn’t easy to find the combination of a peer who also has journalism experience, but that has appeared in the person of Brett Yates, who was a news writer who started two years ago doing freelance articles for Counterpoint and has grown in responsibilities since then.
He takes over an honorable tradition of providing news and space for commentary and arts through our pages that began 1985. We’re only a few years away from a 40 birthday!
So, as I say goodbye, it is also welcome, to a new editor, who will usher in future years of recording the aspirations, successes and disappointments as the psychiatric survivor movement continues the efforts to provide mutual support and to educate and advocate for self-determination and dignity.
Anne Donahue has been editor of Counterpoint since the winter of 1997 and will retire at the end of June. She has been a state legislator since 2003 and lives in Northfield.

.COMMENTARY COMMENTARY 20 Summer 2023 22
‘Twenty-five years... The changes over that time in the psychiatric survivor world have been a kaleidoscope of the good and bad, of progress and setbacks.’
Commission Finds No Fault by Police In Killing; Advocates Assert Report Erred
By ANNE DONAHUE MONTPELIER
– The commission charged with analyzing police shootings when a mental health issue is involved has reported that officers acted appropriately – or even were deserving of praise – when they confronted Mark Johnson in June of 2019 and attempted to get him to drop the gun he was carrying.
One of the two officers shot and killed him on the Elm Street Bridge when he raised the gun toward them despite their efforts at deescalation, according to the report. The handgun was later found to be a BB gun.
Several local advocates have challenged the 10-page report. The commission came to its conclusions in ways that were “inexcusable, not to mention appalling” by neglecting to collect key facts about what had taken place that morning, said one advocate.
The Mental Health Crisis Response Commission, in its annual report released in February, said it “did not find that any of the police actions or adherence to policy were concerning,” and that the “attempts at deescalation not only followed policy but were laudable for their extensive attempts at verbal engagement in which officers treated Mr. Johnson in a respectful fashion.”
The commission noted that its mandate is to identify underlying causes and make recommendations. It suggested that the fact of Johnson’s “mental health symptoms… worsening” in the weeks before his death could have been because his case manager was away and coverage was being provided by “a person unknown” to him.

Its recommendation was that community
health agencies should provide both a primary and a secondary case manager to clients to ensure coverage by a known person. It said that resources should be allocated to make that possible.
However, a local advocate, Steve Whitaker, charged that, “The investigation failed to address the root cause of the shooting death,” which he said was a dispatch error regarding crucial background information known to the police.
Whitaker cited a police response only a few weeks earlier when they brought Johnson to a treatment program after being told he had threatened to jump off the Elm Street bridge, had stopped taking some of his medication and was becoming more paranoid.
The police report said Johnson “admitted he was suicidal and said he had not been sleeping” and agreed to go to the program. When police responded to the report in June that Johnson had a knife and had tried to enter a neighbor’s apartment, the dispatcher failed to connect the report to the earlier incident, Whitaker said.
Officers were more than 138 feet away when
they ordered Johnson to get down from the bridge railing that morning and “were in no imminent danger,” Whitaker argued. “Why not let him jump into the river?” he asked. “He would have dropped the pellet pistol and maybe broke a leg or got a little water in his lungs at worst.”
“Why order him down off the rail,” Whitaker said, only to then shoot him?
Morgan Brown, a nearly decadeslong neighbor of Johnson, wrote a list of errors and “serious omissions” that he found in the report, largely caused by a lack of thorough factfinding, he said. Brown said that a basic investigation would have shown that “Johnson was clearly not attempting to arm himself with a potential weapon” when he took a kitchen knife to jimmy a door. It was something he had used before when he locked himself out of his apartment going out for an early morning smoke, Brown reported.
Contradictions included saying that Johnson’s “mental health was managed with a medication regimen with appropriate oversight by his clinical team” but then stating that it was discovered after his death that Mr. Johnson was not regularly taking his oral medication as prescribed. This actually suggested a lack of appropriate oversight, Brown pointed out.

The Commission’s report recognized that Johnson “was not known to be violent, and he generally got along well with others in his community.
“He helped to shovel snowy walkways for his neighbors and participated in craft projects with others. He had an excellent relationship with the manager of the building. He had a daily routine which involved walking around Montpelier each morning.”
Clients Face Loss of Payee Services
by BRETT YATES
BURLINGTON – Howard Center, the agency serving people with mental health diagnoses and developmental disabilities in Chittenden County, will cease to offer representative payee services as of July 1, leaving clients in a financial pinch.
A representative payee is a person or organization that receives payments from the Social Security Administration, such as Supplemental Security Income, on behalf of a beneficiary who may have a disability that prevents them from managing their own finances. By its own count, Howard Center plays this role for nearly 400 clients, free of charge, and has done so “for a very long time.”
In February, Howard Center sent a letter to these clients, informing them that they would need to find a new representative payee or else begin to pay $48 per month to another SSAapproved nonprofit which would enroll them automatically in its own representative payee program at Howard Center’s instruction.
Howard Center called BalancedCare’s price a “discounted rate,” relative to the maximum fee ($52) allowed by the SSA. The agency plans to cover the cost for the first three months following the transfer, which will give clients a chance “to review and reset their budgets
to accommodate this additional expense,” according to Cathie Buscaglia, Howard Center’s Director of Innovation & Special Projects.
In Vermont, individual SSI beneficiaries receive monthly payments ranging from $72 to $1,378. “The Social Security Administration did give recipients an increase this year. And none of us like to spend our increases on new fees, but at least there is that,” Buscaglia said. “Howard Center recognizes that it’s a significant change for people to receive a service at no cost and then have a cost tied to it.”
Howard Center’s letter contained a reference to a “shift toward conflict-free case management,” an idea promoted by the Centers for Medicare & Medicaid Services.
But Buscaglia characterized conflict-free case management as a broader “philosophy” that Howard Center had begun to embrace, irrespective of any approaching regulations.
Buscaglia described how the issue of financial control can become a “distraction” in the relationship between a client and a case manager, “who’s supposed to be helping a person on their path to whatever their goals are.”
“Sometimes, people want access to their money for different things, and they see their case manager as an obstacle to them getting their money,” she explained. “It can create conflict,”
she observed. Buscaglia also brought up the lack of reimbursement for the service from the state, as well as the labor shortage at Howard Center. “It takes significant time for case managers to do this rep payee service in addition to all of the other things they’re doing for a person,” she said.
Disability Rights Vermont Executive Director Lindsey Owen lamented Howard Center’s plan.
“It seems like this decision to stop the representative payee service is missing the mark and not resolving any conflict of interest,” she said. “Eliminating a service doesn’t necessarily eliminate any of the conflict of doing both case management and direct services. It’s just taking away one of the direct services.”
“Not having a rep payee, or having to pay for it, is a really difficult position to put someone in who has very, very limited means,” she added.
According to Vermont Care Partners, the umbrella organization representing Vermont’s community mental health centers, two others already don’t offer representative payee services and more agencies within its network could soon join Howard Center in dropping the service.
VCP Mental Health Services Director Dillon Burns Burns cited “ethical concerns around being in that role” but also stressed a lack of resources.
23 NEWS . Summer 2023
l
Mark Johnson
A memorial stone for Johnson sits within the courtyard square of the Pioneer Apartments, where he lived.
(Photos courtesy of Morgan Brown)
New Data Show Use of Restraint Is Rare For Voluntary Patients, Except at Retreat
WATERBURY Emergency restraints and seclusion are rarely, if ever, used on voluntary patients on psychiatric units in hospitals, with the exception of the Brattleboro Retreat, according to new data being gathered by the Department of Mental Health.
The data is not completely clear because only the Retreat information is broken out between patients who are voluntary or involuntary.
However, in nine months of data reviewed by Counterpoint, there were no uses of restraint or seclusion at all reported at Central Vermont Medical Center in Berlin or on the general unit at Rutland Regional Medical Center, which both serve voluntary patients together with those under involuntary custody of the Commissioner of Mental Health.
There were also no uses of restraint or seclusion on the Shepardson 3 Unit at the University of Vermont Medical Center, which primarily serves voluntary patients.
The three quarters that were reviewed included January-March, April-June, and
October-December of 2022, because the JulySeptember quarter was not available from DMH. The Retreat’s rates for the use of restraint and seclusion among all patients, and particularly among highest-risk patients, also exceeded all other hospitals among similar patient profiles, a trend that has continued over a number of years.
The Retreat is Vermont’s largest psychiatric hospital, with eight units.
During those periods, the DMH report specific to voluntary patients at the Retreat showed use of restraint or seclusion 334 times with youth and 220 times with adult patients.
The most frequently used type of restraint with those patients was hands-on, which accounted for 334 uses.
There were 197 uses of mechanical restraints, a term used for physical restraint tied to a bed or chair. A seclusion room was used 148 times during those nine months, and forced drugs were used 58 times.
The DMH data does not provide the rate of use of restraint and seclusion per patient hour for voluntary patients.
A new law passed in 2021 required restraint and seclusion data to be reported by DMH for all patients, regardless of whether they are in the involuntary custody of the Commissioner, but the current data is aggregated for voluntary and involuntary patients except at the Retreat.
Court-Ordered Drug Numbers Decline
WATERBURY The annual consultant report on court-order psychiatric drugs shows that the number of petitions being filed by hospitals and granted by judges has been on the decline over the past several years. The number of petitions granted was the lowest since 2013.
The report, which covered July, 2021 through June, 2022, did not include a comparison to the number of hospitalized patients, which decreased overall during the COVID-19 pandemic.
There were 52 petitions filed for involuntary medication under Act 114 during that one-year period. Of those, 36 were granted, 10 were dismissed, three were denied, and two resulted in an order of hospitalization.
The external review, conducted by Flint Springs Associates, includes comments from patients who were subjected to orders, hospital staff, and Vermont Legal Aid. There were five patients who replied to the request for input.
Among the complaints shared were of “losing all control over my own body,” as well as loss of
personal freedoms: “Having my clothes taken …” and, “Being stuck in a facility where you are required to share the bathroom with 8 to 13 other people, staff didn’t clean bathroom between our shower or bath times.”
Comments about staff among the patients who responded included, “They were usually not very caring and they didn’t respect my perspective.” One said that, “The experience of receiving medication was ‘physical torture.’”
The consulting firm said it recommended “that staff at hospitals administering Act 114 medication continue efforts to help patients understand the reasoning behind the decision to seek an order for involuntary medication and to invest time in talking with patients about the process and available options.”
Staff at one hospital, in response to a question about alternatives available to patients, said staffing shortages were a significant problem.
“There seems to be nothing to help patients that are experiencing crisis even though there
are signs stating we have a gym (that no one can use because there is never staff unless it’s first shift).” Another staff member raised a concern about the patient environment on the small, intensive unit where that employee works. “Patients are often extremely upset due to the behaviors of other patients and cannot escape the over stimulus that is happening. The space is small and confined.”
The report also asked for staff perception of the court process, and some said it helped with fairness while others complained about involving judges in the decision-making. “Judges that are not with these patients, do not see what we see, do not see the way the patient struggles or how it saves patients, should not have any say on these medications.”
Patients under court-order drugs included 15 from the Brattleboro Retreat, nine from Rutland Regional Medical Center, two from the University of Vermont Medical Center, and 13 from Vermont Psychiatric Care Hospital.
$18 Million from Hospital To Be Shifted
MONTPELIER – The University of Vermont Health Network is proposing a wide range of mental health services investments totaling $18 million in place of reserving it for construction of a new inpatient wing at Central Vermont Medical Center. The inpatient wing had been determined to be too costly a project.
UVMHN submitted a proposal for 10 projects at the end of May to the Green Mountain Care Board, which will have the final say on reuse of the funds. The two largest projects proposed were funds for the urgent care clinic being planned in Burlington (see article, page 6) and renovations to the current CVMC inpatient psychiatric unit.
The GMCB had required that the proposal be developed in consultation with the Department of Mental Health and with contributions from community stakeholders. Members of the UVM Medical Center inpatient psychiatric advisory group and the Department of Mental Health State Program Standing Committee were included among those asked to provide
comments, according to the cover letter to the Board.
The largest single proposed investment would be $8 million over three years for startup of the urgent care center to supplement the $1.6 million grant the Howard Center is receiving over two years from DMH. Another $4.5 million would be used to enable CVMC to accommodate more patients and “improve the environment of care.” The major change would be conversion of three double bedrooms to six single ones, which would allow more flexibility in using all of them, the proposal said.
Additional smaller projects would include new psychiatric capacity in the UVMMC primary care integration project, establishing esketamine and Transcranial Magnetic Stimulation (TMS) treatment capacity, adding providers to its eating disorders and transgender care clinics for youth, developing best practice protocols for suicide risk assessment and treatment, creating a pilot program for ambulance transport to the Brattleboro Retreat between 5 and 11 p.m.,
and conducting a bed need and feasibility study of future expansion of UVMMC inpatient psychiatric capacity for adults and children.
The Board’s order said that the proposal must show “how the use of funds will reduce the frequency and length of stay for adults, adolescents, and children experiencing a mental health episode who are boarded in EDs,” and “how the use of funds will increase capacity for mental health services.”
In 2017, UVMHN raised more money than it was permitted under the budget approved by the Board for that year. The Board ordered that $21 million in surplus funds be held for addressing the reported shortage of psychiatric hospital beds. Extensive planning was done on the creation of a new wing at Central Vermont Medical Center in Berlin. The project estimate was much higher than expected, and UVMHN announced last year that the project had to be shelved after having spent $3 million in planning costs. It then asked the Board to provide more leeway on how the remaining money could be spent.
COMMENTARY 24 Fall 2018 NEWS Summer 2023
(Photo by Stefano Polliouns, Unsplash)
Advocate Against Force Retires
By ANNE DONAHUE MONTPELIER
The longest-term advocate in the fight against forced treatment in the state announced this year that he was retiring.
Well, somewhat.
Morgan Brown, who became involved in the Vermont Consumer Network in Rutland in 1988 (the precursor to Vermont Psychiatric

take better care of myself.” In particular, Brown hopes to put more time into his longstanding interest in art. (Some of his work is profiled in this issue’s Arts section.)
Brown said he never put the label, “advocate,” on himself; it was others who applied it. Becoming a voice for others “didn’t happen all at once” after he moved to Vermont in 1988.
Brown said it can take him time to engage on an issue, but he’s “never cared for bullies,” so when he sees someone in need. “I have a tendency to want to do something about it.”
As a result, “forced treatment has always been the catalyst” for his involvement, because “people are losing their liberty and rights.”
Despite what many people believe, he isn’t anti-medication, Brown stressed.
“I believe people should have true informed consent and access,” he explained, yet people who want support are left on waiting lists while “so much money is going into forced treatment.”
Brown said his style has always been to try to be proactive and positive, rather than reactive and negative, as he addresses legislators or others in leadership.
He did a lot of listening in committees to understand points of view and then focused on education.
“One of the best places to go is the [statehouse] cafeteria,” he said, just to chat with legislators. “Don’t go right into advocacy mode.”
“I have a certain agenda… [but] I want people to make up their own mind.”
“We keep rewarding failure” by repeating failed efforts to rely on hospital beds and prisons and security.
People think, “we’re locking the scary ones up” and that addresses the problem.
“We can do better and different.” He ticked off examples: the ‘Open Dialogue’ model, Emotional CPR, and joint housing where people can be in charge of their own decision-making and have both personal and shared spaces, with options like case management for support.
“You can’t just dump someone in a place and forget about them.”
“There are peers out there who can do this… [and] build hope and trust,” he added, suggesting that the system needs to be using peers much more than it does. “Empathy is so huge. Seeing the other person as a human being.”
Brown can bring to mind many of the allies in the legislature he found along the way – but noted that mentioning some will always leave out others.
From the early years, he cited Rep. Andrew Christiansen of East Montpelier, who served from 1986 to 1996, and Sen. Sally Conrad, who represented Chittenden County and served three terms after being elected in 1986.
“Conrad was great, as a state Senator, [as] chair of Senate Health and Welfare and as a human being. She truly cared as well as listened,” Brown reflected.
Survivors) and has been a frequent face in the legislature for decades, has acknowledged that he will keep working on his current agenda to have a bathroom facility built in the state’s capital so that people who are unhoused have a facility to use.
He described it as continuing the fight for “the public toilet and related issues,” using the term “and related issues” because “that still leaves me wriggle room to weigh in” on other subjects.
He said he wants to give others more opportunity to step up as advocates.
“I believe if we hope for other people [to get involved] we need to get out of the way,” he told Counterpoint. “I never meant it to be a career.”
He also feels that he can’t continue to be as effective, because people stop hearing his message when they see the same person and think, “nothing new from him.”
“It has been a labor of love,” he reflected, but “I don’t have the energy anymore. I have to
OBITUARY Rene Rose
He said his life experiences don’t define him, but “if I can do something to put a human face on things…”
Has there been there been progress over the 35 years?
Some people have done a lot, he reflected, pointing to the help he received after a long period of being unhoused. In his case, it was intervention by caring individuals that made the difference.
“They bent over backwards,” he said. Relationships are always what make the difference, he observed. Without those, “I’d still be out there, or institutionalized, or dead.”
But there’s still “huge room for improvement” with still too much focus on psych beds and emergency rooms.
“I’m not sure how much has really changed” in forced treatment, he added. “It doesn’t matter [to] how many or how few, it’s still happening” and that is not something that’s insignificant.
ST. JOHNSBURY Rene Rose, a leader in the psychiatric survivor movement and peer advocacy in the Northeast Kingdom for nearly three decades, died Dec. 12, 2022, in a car accident in Walden. She was 76.

Rose had been a past board member at Vermont Psychiatric Survivors. She worked in peer support at Northeast Kingdom Human Services and was a member of the Peer Workforce Development Initiative based at Pathways Vermont.
Rose was known as an extraordinarily patient listener who encouraged peers to take the lead in improving their own wellness. She employed mindfulness-based cognitive therapy strategies to assist people in recovering from serious illnesses.
In collaboration with Gladys Mooney, she headed up several Vermont Psychiatric Survivor Peer Operated Projects grants.
In private practice, she co-facilitated Chronic Pain,
When it comes to state leadership, though, he easily jumped to pointing out Patrick Flood, who was both a Deputy Secretary of the Agency of Human Services and later, Commissioner of the Department of Mental Health for a brief time after Tropical Storm Irene wiped out the state hospital in Waterbury in 2011.
“He availed himself to people like me and listened,” Brown reflected.
Brown stood proudly at the table when the postIrene bill was signed into law creating reforms to the system that included commitments to increased community supports.
But he stood there with “a lot of skepticism” inside, questioning if those investments would really be made when he knew some of those in charge had “different agendas.”
Some of those investments did happen but in recent years there have been new locked facilities built as well.
Does that mean his hopes are a lost cause?
“The only lost causes are the ones we give up on,” he answered. “Especially people.”
Depression Relapse, and WRAP (Wellness Recovery Action Plan) support groups. Her gift was in seeing people as human beings — not as broken; not as lessthan; just as people — struggling at times, like her, and looking for a way forward.
Rene was born in Brooklyn, New York on Aug. 8, 1946 and studied at Brooklyn College and Syracuse University for her doctorate in women’s studies and taught undergraduate and graduate classes in Counseling, Encountering Illness, and Death and Dying at the St. Johnsbury branch of Springfield College of Human Services.
She lived and worked at a Gurdjieffian community in Walden on the community’s farm for 23 years. She sustained a number of debilitating injuries during this time, including broken ankles, knee replacements, and permanent injury to her back. She lived with chronic pain and used crutches after a fall 20 years ago. She is survived by her daughter Cathy and grandson Tristan.
COMMENTARY 25 Fall 2018NEWS . 25 Summer 2023
Morgan Brown
(Photo by Anne Donahue)
Rene Rose
The annual membership meeting for Vermont Psychiatric Survivors is where we elect the new Board of Directors, catch up with one another, and generally have some fun!
For information:
Contact Board President Sara Merrow at 802-417-5468 or merrowsara@gmail.com
SAVE THE DATE
October 23, 2023 Annual Meeting
Support Line Celebrates 10 Years
BURLINGTON – Pathways
Vermont is celebrating the tenth anniversary of the Pathways Vermont Support Line. The Support Line was developed to provide confidential, non-judgmental support and connection for all Vermonters over the age of 18 by phone or text.
Since the inception of VSL, more than 87,200 calls have been completed, and 2,268 calls have been diverted from emergency services, the organization reported.
Different from a crisis hotline or emergency line, the support line is a “warm line,” a resource that can help prevent a situation from escalating to an emergency, Maria Moore, a spokesperson for the agency said, filling a previously unmet need in the system of care through immediate access to support.
The creation of a statewide warm line was mandated in 2012 in Act 79, the legislature’s plan to redevelop the system of care following the closure of the Vermont State Hospital. It was intended as an alternative resource for individuals who regularly contact crisis and other emergency-level services in search of
support. A year later, the Pathways Vermont service began taking its first calls. In response to increased need during the pandemic, the Support Line expanded to becoming a 24/7 line, as originally envisioned in Act 79.
Pathways Vermont has a relationshipfirst practice, Moore said. This means the organization values lived experience, recognizes each person as their own expert, and fosters connection through empathy, she explained.
A relationship-first practice places principles of humanity, authenticity, collaboration,
curiosity, and hope at the forefront of every connection, Moore said.
Support Line staff utilize lived experience to provide peer counseling on a wide range of issues including loneliness, substance use, medical concerns, relationship challenges, or thoughts of suicide.

“Our support line is unique in that all relationships and connections are rooted in autonomy, mutuality, and trust. Someone can call the line when they are having a bad day and just need someone to talk to,” Moore added. “Pathways Vermont champions the peer support model and the success of connections without agendas or a helper/helpee relationship.”
Moore shared a comment from one caller, who said, “The support line is one place where I don’t feel alone in the world. It’s so good to be able to pick up the phone and hear an empathetic voice on the other end. I call each day because I find this line very effective.”
The Support Line can be accessed via call or text at (833) VT-TALKS / (833) 888-2557.
Mixed Results from Other Commitments in Act 79
Save the Date
Along with the 24-hour warm line, Act 79 – passed in 2012 after Tropical Storm Irene forced the closure of the 54-bed Vermont State Hospital in Waterbury – directed development of new hospital and residential beds along with additional community-based support services. Not all of the peer or community programs were completed, but more secure hospital and state-run facility beds were added to the original plan.
Act 79 said:
Oct ober 19, 2023
The Status Today:
The Killington Grand Hotel Killington, VT
• High security (“Level 1”) inpatient beds: 25 state-run; 6 at Rutland Regional Medical Center; 14 at the Brattleboro Retreat
• State-run secure (locked) residential recovery beds: 7
• Level 1 inpatient beds: 25 Vermont Psychiatric Care Hospital; 6 at Rutland Regional Medical Center; 26 at the Brattleboro Retreat
• State-run locked residence: 16; state-run locked forensic: 9 planned
VermontDepartmentofMentalHealthPresents:
• Added community agency-run intensive residential: 31
• Peer-supported intensive residential: Soteria House beds, 5
• Other peer: workforce development; peer-run transportation services
DMH Conf ere nce 2023:
Save the Date
Oct ober 19, 2023
The Killington Grand Hotel Killington, VT
hear about successful and researched approaches to integrated care .
VermontDepartmentofMentalHealthPresents:
DMH tracks:
• Wellness & Self Care
Save the Date
• Integrated Care & Policy
Conference 2023:
• Added community agency-run intensive residential: 23

• Peer-supported intensive residential: Soteria House beds, 5
• Other peer: Peer Workforce Development Initiative
Eating Disorders Study: State Lacks Services
disorders clinic, if that use is approved for reserved funds.
DMH Conf ere nce 2023:
Reshaping Mental Health Systems Through Integration

• Mental Health & the Criminal Justice System
WATERBURY – The state lacks any moderate- to high-level treatment settings for individuals with eating disorders, according to a special review on services available for eating disorders in Vermont that was directed by the legislature in 2021. “The stark reality is that none of these programs exist in Vermont at this time, for any age group,” the report by the Department of Mental Health said.
eshaping Menta l Health Systems Through Integ ration
Featuring workshops for child, teen, adult, and families :
Oct ober 19, 2023
A Statewide Symposium on Advancing the Mental Health System
• Promising and Evidence-Based Practices
• Panel Presentations
The Killington Grand Hotel Killington, VT
October 19, 2023
• Locally Developed Innovative Approaches and service models
A Statewide Symposium on Advancing The Mental Health System
The Killington Grand Hotel, Killington, VT
• Learning Sessions Watch for upcoming details from:
VermontDepartmentofMentalHealthPresents:
The Vermont Department of Mental Health https://mentalhealth.vermont.gov/

It has been a long few years , therefore the goal of this conference will bring together key stakeholders in mental health, health care and forensic system to positively impact the well-being of Vermonters. Join in an opportunity to gain knowledge about innovative practices, influence change and service delivery, and hear about successful and researched approaches to integrated care
DMH Conf ere nce 2023:
Menta l Health Systems
DMH tracks:
Wellness & Self Care Care
Integ ration
“Vermont has a small pool of exceptional multidisciplinary outpatient providers specializing in eating disorder treatment,” the report said, but “available resources do not come close to meeting the need for individuals in Vermont.” A new program expansion planned by the University of Vermont Medical Center may help address that through the addition of staff to its existing eating
The report made eight recommendations to expand supports but only one was acted upon by the legislature this year. A bill on a model policy for schools that is to be developed to address suicide prevention includes education of school staff about prevention and identification of eating disorders. Other recommendations included establishing partial hospital and intensive outpatient programs and a number of training and educational initiatives.
Development of the model policy for schools was part of a larger bill to improve statewide coordination of suicide prevention efforts. A model protocol must also be submitted to the legislature for health care facilities regarding suicide prevention and “postvention” services.
NEWS 26E COMMENTARY 26 NEWS .
Vermont Support Line staffers Jennifer Furey (left) and Cynthia Christensen give a smile with headphones at the ready for calls. (Photo courtesy of Pathways Vermont)
g
Through
Statewide
on
Symposium
Advancing
& Policy
Vermont Psychiatric Survivors’
VPS Names New Patient Representatives
RUTLAND
Vermont Psychiatric Survivors has announced two new patient representative staff members.
Introductions on the VPS web site give these brief self-descriptions:
Kat Parker worked in the medical field for 12 years, working mostly in cardiology and neurology, prior to coming to VPS. She always made sure to take extra time for her patients to make sure that
they felt comfortable and cared for. She takes a Carrie Fisher approach to her mental health. She is not afraid to be transparent about her own mental health and neurodivergence. She is active in researching new ways to help people with different ways of neurodivergent thinking.
Kat lives at home with her husband and cat. She enjoys kayaking, being outdoors, and gaming. She has hobbies in arts, crafts and embroidery. She also enjoys reading and writing.
She is a nerd and can have conversations about many nerdy things like gaming, movies, Broadway and books.
Zachary Stroup, a psychiatric survivor, comes to VPS as a former EMT. His experience as a frontline worker in the community led him to
seek options that would allow him to assist in the community’s mental health as well.
When he isn’t engaging with the community, Zach’s other passion is the stewardship of animals. If not taking care of the family menagerie of cats, dogs, chickens and fish, he can occasionally be found assisting rescue organizations or trying to commune with a random critter.
Health Equity Office Gains Momentum

MONTPELIER – The Health Equity Advisory Commission made 37 recommendations and requested a base budget of $1.57 million from the legislature in its annual report in February. Part of the funding was appropriated late in the session.
The report said that health equity “must be pursued with an understanding of the persistent nature of the disparate outcomes across all social determinants of health – housing, education, employment, economic development, criminal justice, etc.,” and that those disparities “compound adverse outcomes, including poor health, to a life altering, life threatening degree.”
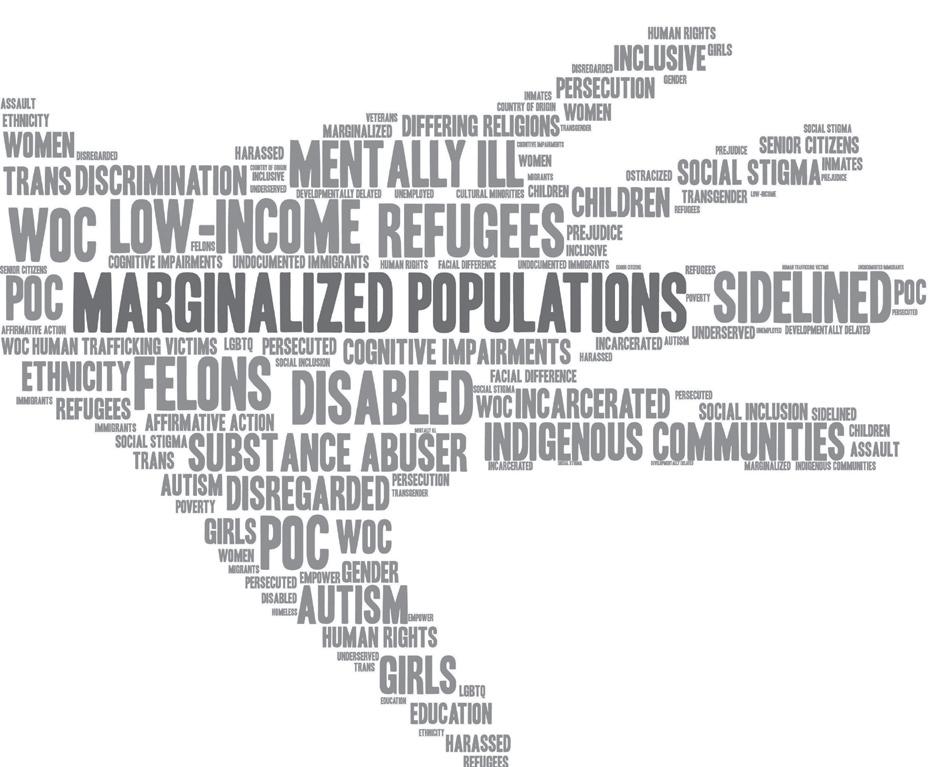
It stated that as a result, “advancing equity is the responsibility of the whole of our government” and that “all agencies and departments within state government must address inequities in their existing and new policies and programs.”
The legislature responded to the request for
funds to establish and staff an Office of Health Equity and to create a community grant program for equity projects
and $500,000 of the $750,000 it requested for the funding of grants.
Commission member Sarah Launderville, executive director of the Vermont Center for Independent Living, said that she was “very excited about the ‘whole government’ approach and how that can really begin to change how we engage on health equity overall.”

with a total of $750,000, but with the condition of receipt of a specific recommendation from the Council by January on where the new office would be situated within the state government structure. The funds, which would be released after the report is received, includes $250,000 for executive director and assistant positions,
The Commission was created in 2021 to address health disparities from systemic discrimination against people with disabilities, the LGBTQ+ community, people of color and indigenous peoples. Launderville said she thought the community-based and neighborhood-based grant component “is very important as we look at how health equity is already happening.
"It’s in the communities, it’s led by people with lived experience and in order for that to thrive, having grant funding to shore up that community programming is important.”
BATTLE ERUPTS ON HOTEL EVICTIONS
• Continued from page 1 to support residents in the emergency program since it began with the COVID shutdown in the spring of 2020.
In the days leading up to the budget vote in the legislature, housing advocates fiercely lobbied for an extension while leaders at the statehouse insisted that the program had to end, since the federal COVID money that paid for it had come to an end. Between March 2020 and December 2022, the state paid more than $160 million to hotels and motels.
The legislature had already extended the program for four months beyond the administration’s March closing date by adding $19 million in supplemental state funding
The governor announced in late May that persons who were eligible for emergency housing under pre-COVID criteria would be allowed to re-start the clock on its standard 28-day limit. Those individuals would gain an extra month after July 1 before losing their hotel room.
A special website has been established for ongoing information about the transition at dcf. vermont.gov/pandemic-era-ga-program-2023.
Duprey wrote a searing letter to legislators a few days before the vote on the budget. “How are you going to live with yourselves, sleep at night, when people are outside dying, and you could have done something to help?
“Until you personally, yourselves, every single one of you, Governor included, step into our shoes, don’t cut the budget,” she urged.
Duprey said that those “enduring this crisis on a personal level are for many reasons unable to speak up for themselves. They need a voice. I will be that voice at any cost,” she wrote.
As an abuse survivor, she said, “What I’ve learned from my experience and fight to get back on my feet, is that a state in its entirety, managed to make me feel like I am still living in an abusive situation, this time the abuser is someone different. It’s you…”
She continued to send messages from other residents in the weeks following the budget vote.
The messages from hotel program residents that Duprey forwarded included descriptions of urgent medical and psychiatric conditions and fears of ending up living in a car or in the woods.
“I have bipolar disorder and am currently in recovery from drug use. My life will be at risk if I’m thrown out on the streets,” said one message.
“I have absolutely nowhere to go, besides the streets,” said another. “If that happens, my medical conditions such as PTSD, seizures from two brain surgeries, among other things… It will cause a serious decline to all progress I have made.”
A message forwarded from another individual described being homeless as a result of domestic
Editor’s Note: Governor’s Veto of Budget
violence and added, “I have bi-polar, PTSD and I’m in recovery.”
Legislators who spoke on the House floor to object to a budget that did not include an extension of the hotel program appeared to agree with Duprey’s outrage.
“Rather than creating a transitional ramp, we have created a cliff,” said Rep. Jubilee McGill, and “the effects of that decision will be more damaging than the people in this body can even begin to imagine.”
Rep. Mari Cordes insisted, “It is not a money problem but a problem of political will and a disaster in the making.”
Another legislator, Rep. Taylor Small, said in her vote explanation that “I refuse to sign the death certificates of our most vulnerable Vermonters. That is what we are doing with this budget’s unhousing plan.”
Legislative leadership who backed the budget pointed to the addition of $17 million in the budget for services to help relocate hotel residents and to the hundreds of millions that have been invested over the past several years to respond to the state’s housing crisis.
Another $16 million was included in the budget to maintain or expand emergency shelters. In the meantime, however, there is little available affordable housing in the state.
Many of the legislative actions reported on in this edition of Counterpoint are conditioned on funding through the state budget. The governor has vetoed the budget, which will face an override vote in late June. None of the budget items related to mental health were in controversy, so a new budget will not likely change them, but they will not be certain until a final budget has passed. Non-budget bills have all been signed by the governor, unless specifically stated otherwise in the article.
NEWS 27 Fall 2018 Summer 2023 NEWS 27
Zachary Stroup Kat Parker
Resources Directory
SURVIVOR PEER SERVICES
Vermont Psychiatric Survivors
VPS is a membership organization providing peer support, outreach, advocacy and education 128 Merchants Row, Suite 606, Rutland, VT 05701 802-775-6834 www.vermontpsychiatricsurvivors.org
VPS OUTREACH AND PATIENT REPRESENTATIVES (800) 475-4907 info@vermontpsychiatricsurvivors.org
WARM LINE
VERMONT SUPPORT LINE (STATEWIDE): 833-888-2557; 24 hours, 365 days [833-VT-TALKS]

By call or text
CRISIS RESPITE
Alyssum, 802-767-6000; www.alyssum.org; info@alyssum.org
HOSPITALIZATION ALTERNATIVE
Soteria House, information and online application at www.pathwaysvermont.org/what-we-do/ our-programs/soteria-house/ or call Pathways Vermont Intake Line, 888-492-8212, ext. 140
Peer Centers & Employment Support
ANOTHER WAY
125 Barre St, Montpelier, 802-229-0920; info@anotherwayvt.org; www.anotherwayvt.org; see website for events calendar.
PATHWAYS VERMONT COMMUNITY CENTER
279 North Winooski Avenue, Burlington, 802-777-4633; pvcc@pathwaysvermont.org www.facebook.com/PathwaysVTCommunityCenter; www.pathwaysvermont.org/what-we-do/ our-programs/pvcc
Some Peer Centers and Recovery Centers may have changed hours as a result of COVID-19 crisis. Call to check on up-to-date schedules.
Vermont Recovery Centers
WWW.VTRECOVERYNETWORK.ORG
BARRE, Turning Point Center of Central Vermont, 489 N. Main St.; 479-7373; www.tpccv.org; tpccvbarre@ gmail.com
BENNINGTON, Turning Point Center, 160 Belmont Dr; 802-442-9700; info@tpcbennington.org
BRATTLEBORO, Turning Point Center of Windham County, 39 Elm St.; 802-257-5600; tpwc.1@hotmail.com
BURLINGTON, Turning Point Center of Chittenden County, 179 South Winooski Ave, Suite 301; 802-8613150; www.turningpointcentervt.org or support@ turningpointcentervt.org
MIDDLEBURY, Turning Point Center of Addison County, 5 A Creek Rd; 802-388-4249; info@turningpointaddisonvt.org
MORRISVILLE, North Central Vermont Recovery Center, 275 Brooklyn St., 802-851-8120; JOHNSON, 117 St. John’s St. 802-730-8122; recovery@ncvrc.com
NEWPORT, Journey to Recovery Center, 212 Prouty Dr. 802-624-4156
JOHNSON, Jenna’s Promise, 114 St. John’s Rd, 802343-8741; info@jennaspromise.org
RUTLAND, Turning Point Center, 141 State St; 802-7736010; turningpointcenterrutlandvt.org
SPRINGFIELD, Turning Point Recovery Center of Springfield, 7 Morgan St., 802-885-4668; webadmin@ spfldtp.org; www.spfldtp.org
ST. ALBANS, Turning Point of Franklin County, 182 Lake St; 802-782-8454; contacta@turningpointfranklincounty.org
ST. JOHNSBURY, Kingdom Recovery Center, 297 Summer St; 802-751-8520; recoveryinfo@stjkrc.org; www. kingdomrecoverycenter.com
WHITE RIVER JUNCTION, Upper Valley Turning Point, 200 Olcott Dr; 802-295-5206; www.uppervalleyturningpoint.org; info@secondwindfound.org
SUICIDE & CRISIS LIFELINE 988 24/7 support
Crisis Text Line
Around the clock help via text: send “VT” to 741-741 for ground rules; message routed to a trained counselor.
Vermont Federation of Families for Children’s Mental Health
Statewide support for families of children, youth or young adults in transition who are experiencing or at risk to experience emotional, behavioral or mental health challenges. 800-639-6071, 802-876-7021; www.vffcmh.org
Pride Center of Vermont
LGBTQ Individuals with Disabilities Social and Support: Connections and support around coming out, socializing, employment challenges, safe sex, self-advocacy. For center hours call (802) 860-7812 or go to www. pridecentervt.org
Brain Injury Association
Support Group locations on web: www.biavt.org; support@biavt.org; 802-244-6850
Trans Crisis Hotline
The Trans Lifeline (dedicated to the trans population) can be reached at 877-565-8860.
LGBTQ Youth Crisis Hotline: The Trevor Lifeline, 866-488-7386. TrevorText : 678-678
Hearing Voices Network Online Groups
Opportunities to connect, share experiences, and find mutual support via web-based platforms and by phone specifically for those with personal lived experience with hearing voices, seeing visions, and/or negotiating alternative realities. For questions and for details on how to access the group[s]: info@hearingvoicesusa.org.
NATIONAL ALLIANCE ON MENTAL ILLNESS-VT (NAMI-VT): 802-876-7949 x101, or 800-639-6480; 600 Blair Park Road, Suite 301, Williston, 05495; www.namivt.org; info@namivt.org
Connections Peer Support Groups
Meetings are led by trained Peer Support Leaders. The groups provide a safe place that offers respect, understanding, encouragement, and inspires hope to all who attend. Zoom Meetings: Every Monday 7-8:30 p.m. and 1st & 3rd Tuesday 4-5:30 p.m. In-Person: Every Thursday from 3-4:30 p.m., Cathedral Church of St. Paul, 1st floor, Commons Room, 2 Cherry Street, Burlington. To learn more, visit: www.namivt.org/support-groups/peer-support/
Summer
Counterpoint publishes this resource directory to allow readers to seek out choices for support. Counterpoint has not reviewed or evaluated the quality or biases of these resources, and makes no representation about their value for any individual.
Public Community Mental Health
COUNSELING SERVICE OF ADDISON COUNTY, 89 Main St., Middlebury, 05753; www.csac-vt.org; 802-388-6751
UNITED COUNSELING SERVICE OF BENNINGTON COUNTY, PO Box 588, Ledge Hill Dr., Bennington, 05201; 802442-5491; 5312 Main St., Manchester, 802-3623950; www.ucsvt.org
CHITTENDEN COUNTY: HOWARD CENTER, 300 Flynn Ave., Burlington, 05401; 802-488-6000; www.howardcenter.org
FRANKLIN & GRAND ISLE: NORTHWESTERN COUNSELING AND SUPPORT SERVICES, 107 Fisher Pond Road, St. Albans, 05478; 802-524-6554; www.ncssinc.org
LAMOILLE COUNTY MENTAL HEALTH SERVICES, 72 Harrel Street, Morrisville, 05661; 802-888-5026; www.lamoille.org
NORTHEAST KINGDOM HUMAN SERVICES, 181 Crawford Road, Derby; 802-334-6744; 2225 Portland St., St. Johnsbury; 802-748-3181; www.nkhs.org
ORANGE COUNTY: CLARA MARTIN CENTER, 11 Main St., Randolph, 05060-0167; 802-728-4466; www.claramartin.org
RUTLAND MENTAL HEALTH SERVICES, 78 So. Main St., Rutland, 05701; 802-775-2381; rmhsccn.org
WASHINGTON COUNTY MENTAL HEALTH SERVICES, 9 Heaton St., Montpelier, 05601; 802-223-6328; www.wcmhs.org
WINDHAM AND WINDSOR COUNTIES: HEALTH CARE AND REHABILITATION SERVICES OF SOUTHEASTERN VERMONT, 390 River Street, Springfield, 05156; 886-4500; 51 Fairview St., Brattleboro, 05301, 802-254-6028; 49 School St., Hartford, 05047, 802-295-3031; www.hcrs.org
24-Hour Crisis Lines and Involuntary Custody Screening
ADDISON COUNTY: Counseling Services of Addison County
802-388-7641
BENNINGTON COUNTY: United Counseling Service, 802442-5491; (Manchester) 802-362-3950
CHITTENDEN COUNTY: Howard Center, 802-488-7777
FRANKLIN AND GRAND ISLE COUNTIES: Northwestern Counseling and Support Services, 802-524-6554; 800-834-7793
LAMOILLE COUNTY: Lamoille County Mental Health, Weekdays 8 a.m.-4 p.m. 802-888-5026; Nights and weekends 802-888-8888
ESSEX, CALEDONIA AND ORLEANS: Northeast Kingdom Human Services 802-334-6744
ORANGE COUNTY: Clara Martin, 800-639-6360
RUTLAND: Mental Health Services, 802-775-1000
WASHINGTON COUNTY: Mental Health Services, 802-229-0591
WINDHAM,WINDSOR COUNTIES: Health Care and Rehabilitation Services, 800-622-4235
Please contact us if your organization’s information changes: counterpoint@vermontpsychiatricsurvivors.org
Veterans’ Services
TOLL-FREE HOTLINE (24/7) 800-273-8255
CRISIS LINE: Toll-Free: 866-687-8387, press 7
FREE TRANSPORTATION: Disabled American Veterans:
Toll Free: 866-687-8387 X5394
HOMELESS PROGRAM COORDINATOR: 802-295-9363, ext 6184
TRANSITIONAL RESIDENCES: Canal Street Veteran’s Housing, Winooski 802-864-7402; Dodge House, Rutland, 802-775-6772; Veteran’s Inc, Bradford, 802-627-7838; The Veteran’s Place, Northfield, 802-485-8874.
VERMONT VETERANS SERVICES: program for homeless veterans with very low incomes: 802-656-3232.

VA Mental Health Services
VA HOSPITAL: Toll Free 866-687-8387
Vermont Veterans Outreach Team
Peer-to-Peer Support: Veteran’s Outreach program staff with very diverse backgrounds including service in different branches of the military.
OUTREACH TEAM LEADER: 802-338-3022
ADDISON COUNTY: 802-338-4313
CALEDONIA/ORANGE/WINDSOR COUNTY: 802-338-4324
CHITTENDEN NORTH: 802-338-3078
CHITTENDEN SOUTH: 802-338-4316
LAMOILLE COUNTY: 802-338-3411
ORLEANS/ESSEX COUNTY: 802-338-4325
RUTLAND COUNTY: 802-338-4315
WASHINGTON COUNTY: 802-338-4318
WINDHAM COUNTY: 802-338-4171
MENTAL HEALTH SERVICES: 802-338-3445
www.MakeTheConnection.net
MENTAL HEALTH CLINIC, White River Jt, Toll Free 866-687-8387 Ext 6132
OUTPATIENT CLINICS: Bennington: 802-440-3300; Brattleboro: 802-2512200; Burlington Lakeside Clinic: 802-657-7000; Newport: 802-6242400; Rutland: 802-772-2300
VET CENTERS: (So. Burlington) 802-862-1806; (White River Jctn) 802-295-2908
Web site sponsored by The Department of Veterans Affairs with testimonials by veterans to help connect with the experiences of other veterans, and with information and resources to help transition from service, face health issues, or navigate daily life as a civilian.

28
2023












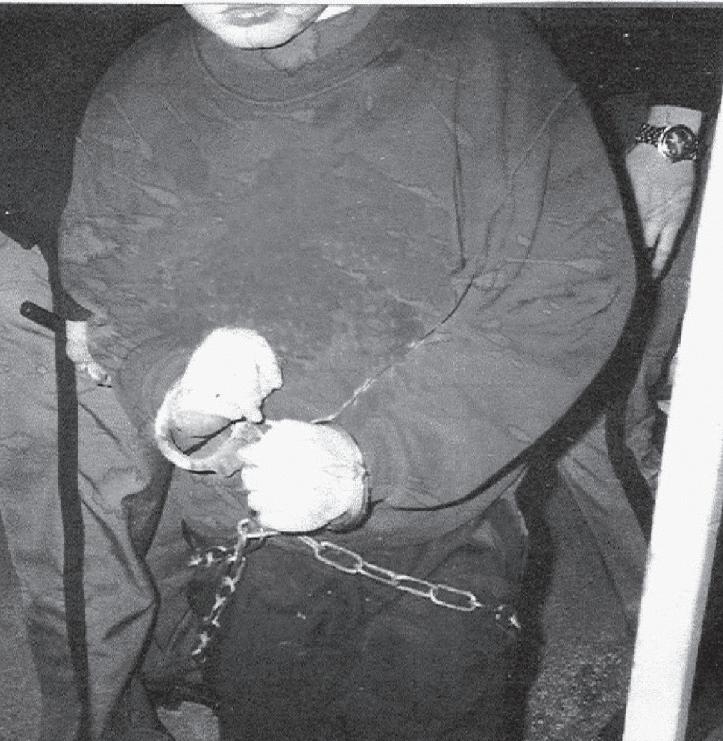 by BRETT YATES
by BRETT YATES

 by BRETT YATES
by BRETT YATES





 by Morgan Brown, Montpelier
by Morgan Brown, Montpelier
 by SHERRY DUVAL
by SHERRY DUVAL