Flooding Tests Mental Health
by BRETT YATES
By Vermont Emergency Management’s preliminary count, July’s floods damaged 4,087 homes and 839 businesses statewide. Emotionally and psychologically, the event and its aftermath will yield serious, long-lasting challenges for Vermonters, according to mental health providers.

“It's awful, and it's a tragedy, and people need to seek out as much support as they can get in order to maneuver through this,” said Christopher Sloane, a mental health trauma counselor in Montpelier. “Literally, our emotional systems, our nervous systems, they're flooded right now as well.”
Catherine Baird, who operates Inner Care Counseling and Wellness in downtown Barre, described natural disasters as “overwhelming” events that can strip away people’s feeling of agency.
“The weather is just this thing that's happening to you, out of your control, sometimes unexpectedly, in many cases not knowing exactly
how bad the damage could be,” Baird said. “That's very terrifying, and when something's just kind of taken from you – your home, your possessions, your job – that really threatens your sense of livelihood and your sense of being connected and grounded in this world.”
Similarly, Timothy Ricciardello, a clinical social worker who practices in Morrisville, spoke of the storm’s “traumatic effect” upon Vermonters for whom the “threat of physical harm” quickly gave way to “a threat to the sense of self.”
“A lot of people lost everything. Watching old family albums wash away, or grandma's quilts get ruined from the basement, or whatever it is –it's very much tied to their identity. Our identity is tied into our security, into our housing, into our livelihood,” Ricciardello said.
This psychological stress can exacerbate the difficulties posed by the practical burdens of recovery, as Tina Ghantous, who provides psychotherapy in Hardwick, pointed out.
“There's people who are in the stages now of
trying to fill out their FEMA form and decide who to talk to and make appointments,” she said. “And all of those basic, kind of administrative, here-and-now, logical functions are really challenging when someone is in a trauma response. So it kind of just sets up for the person not being able to necessarily do what they need
(Continued on page 4)
Does Patient Advocacy Advocate?
by BRETT YATES
Not everyone leaves the hospital content with the quality of their care. At the University of Vermont Medical Center, dissatisfied patients have a place to go: the Office of Patient & Family Advocacy. But what happens once they’ve filed a complaint?

Last November, “some mental health issues” brought Evan Webster to UVMMC’s emergency department. Upon discharge, they wanted to stop at City Market in Burlington to pick up “some basic necessities” before taking an Uber back to their home in Charlotte.
But by Webster’s account, staff told them that this would present a conflict with hospital policy. “They’re like, ‘No, sorry, sorry, sorry, you have to go directly home,’” they remembered.
Instead, UVMMC would call a taxi to provide Webster with “direct passage” to their house and give them a voucher to pay for the ride. After “hours” of debate, Webster gave in.
“I get in the cab,” they recalled, “and then another person gets in the cab, who had just been released from the ED, was slurring his words, was talking about how his brother died in a car accident. And so we’re going to get in a joint cab, and we’re going to go to Winooski first.”
Webster called the experience “really scary”
and “just totally contrary to everything [hospital staff] said.” They wound up exiting the cab and hailing an Uber after all.
Because the Uber couldn’t accept the hospital’s voucher, Webster paid out of pocket, hoping for later reimbursement. This – among other alleged issues that arose in November and
“Our patient advocates look into and help resolve patient care-related complaints,” the official description continues. “We can also answer your questions about confidentiality and patient rights and can get you information about your care.”
In general, a patient advocate may work for an independent patients’ rights organization or – as in the case of UVMMC – for the healthcare provider itself. While the latter arrangement arguably carries an intrinsic conflict of loyalty, it also, at least in theory, offers easier access to information and internal channels for resolving problems and disputes promptly.

But how much power does Patient Advocacy really have at UVMMC? For some who’ve used the service, it doesn’t seem like much.
then in January, when Webster returned to the ED – led them to contact UVMMC’s Office of Patient and Family Advocacy.
According to the University of Vermont Health Network, UVMMC’s Office of Patient and Family Advocacy can step in when hospital services “fall short” of their goal “to provide the best care experience possible.”
Webster asserted that they’d experienced misgendering at the hospital. Indeed, they’d become aware of Patient Advocacy in the first place as a result of their call for “different help” in the midst of the incident, which prompted a staffer to hand over a business card with the office’s phone number on it. Webster immediately noted its limited hours of operation: Monday to Friday, from 9 a.m. to 5 p.m.
“I was like, are you serious?” they said. “If
(Continued on page 6)
NEWS, COMMENTARY, AND ARTS BY PSYCHIATRIC SURVIVORS, MENTAL HEALTH PEERS, AND OUR FAMILIES
12 The Arts 10 Mad Pride 7
VOL. XXXVIII NO. 2 • FROM THE HILLS OF VERMONT • SINCE 1985 • FALL 2023
Survivor Trains Hospital Staff
Downtown Montpelier (Counterpoint photo)
UVM Medical Center (Counterpoint file photo)
Peer Leadership and Advocacy
Meeting Dates and Membership Information for Boards, Committees and Conferences
Peer Organizations State Committees
VERMONT PSYCHIATRIC SURVIVORS BOARD
A membership organization providing peer support, outreach, advocacy and education. Board meets monthly. For information call 802-775-6834 or email info@vermontpsychiatricsurvivors.org.
COUNTERPOINT EDITORIAL ADVISORY BOARD
The editorial advisory board for the Vermont Psychiatric Survivors newspaper can always use help! Assists with policy, editing and brainstorming on topics for articles. Contact counterpoint@vermontpsychiatricsurvivors.org
ALYSSUM Peer crisis respite. To serve on board, call 802-767-6000 or write to information@alyssum.org
DISABILITY RIGHTS VERMONT PAIMI COUNCIL
Protection and advocacy for individuals with mental illness. Call 1-800-834-7890.
ADULT PROGRAM STANDING COMMITTEE
Advises the Commissioner of Mental Health on the adult mental health system. The committee is the official body for review of and recommendations for redesignation of community mental health programs (designated agencies) and monitors other aspects of the system. Members are persons with lived mental health experience, family members, and professionals. Meets monthly on 2nd Monday, noon-3 p.m. Check DMH website www.mentalhealth.vermont.gov or call-in number. For further information, contact member Daniel Towle (dantowle@comcast.net) or the DMH quality team at Eva.Dayon@vermont.gov
LOCAL PROGRAM STANDING COMMITTEES
Advisory groups, required for every community mental health center. For membership or participation, contact your local agency for information (listings on back page).
Advocacy Organizations
DISABILITY RIGHTS VERMONT
Advocacy in dealing with abuse, neglect or other rights violations by a hospital, care home, or community mental health agency. 141 Main St, Suite 7, Montpelier VT 05602; 800-834-7890. disabilityrightsvt.org
VERMONT CENTER FOR INDEPENDENT LIVING
Peer services and advocacy for persons with disabilities. 800-639-1522. vcil.org
HEALTH CARE ADVOCATE To report problems with any health insurance or Medicaid/Medicare issues in Vermont 800-917-7787 or 802-241-1102. vtlawhelp.org/health
VERMONT CLIENT ASSISTANCE PROGRAM
Rights when dealing with service organizations such as Vocational Rehabilitation. Box 1367, Burlington VT 05402; 800-747-5022.
NAMI-VT
Family and peer support services, 802-876-7949 x101 or 800-639-6480; 600 Blair Park Road, Suite 301, Williston VT 05495; www.namitvt.org; info@namivt.org
PEER WORKFORCE DEVELOPMENT INITIATIVE
Webpage provides an up-to-date account of statewide peer training and registration information as well as updates about its progress and efforts. www.pathwaysvermont. org/what-we-do/statewide-peer-workforce-resources/ MADFREEDOM
MadFreedom is a human and civil rights membership organization whose mission is to secure political power to end discrimination and oppression of people based on perceived mental state. See more at madfreedom.org
MENTAL HEALTH LAW PROJECT
Representation for rights when facing commitment to a psychiatric hospital. 802-241-3222.
ADULT PROTECTIVE SERVICES
Reporting of abuse, neglect or exploitation of vulnerable adults, 800-564-1612; also to report violations at hospitals/nursing homes through Licensing and Protection at (802) 871-3317
Hospital Advisory
VERMONT PSYCHIATRIC CARE HOSPITAL
Advisory Steering Committee, Berlin, check DMH website for dates at www.mentalhealth.vermont.gov
RUTLAND REGIONAL MEDICAL CENTER
Community Advisory Committee, fourth Mondays, noon, call 802-747-6295 or email lcathcart@rrmc.org
UNIVERSITY OF VERMONT MEDICAL CENTER
Program Quality Committee, third Tuesdays, 9-10 a.m., for information call 802-847-4560.
NARMH
VT Psychiatric Survivors, 128 Merchants Row Suite 606, Rutland, VT 05701
Phone: (802) 775-6834
email: counterpoint@ vermontpsychiatricsurvivors.org
MISSION STATEMENT:
Counterpoint is a voice for news and the arts by psychiatric survivors, ex-patients, and consumers of mental health services, and our families and friends.
Copyright 2023, All Rights Reserved
FOUNDING EDITOR
Robert Crosby Loomis (1943-1994)
EDITORIAL BOARD
Kara Greenblott, Zachary Hughes, Sara Neller, Laura Shanks, Joanne Desany
The Editorial Board reviews editorial policy and all materials in each issue of Counterpoint. Review does not necessarily imply support or agreement with any positions or opinions.
PUBLISHER
Vermont Psychiatric Survivors, Inc.
The publisher has supervisory authority over all aspects of Counterpoint editing and publishing.
EDITOR
Brett Yates
News articles without a byline written by the editor Opinions expressed by columnists and writers reflect the opinion of their authors and should not be taken as the position of Counterpoint
Counterpoint is funded by the freedom-loving people of Vermont through their Department of Mental Health. Financial support does not imply support, agreement or endorsement of any of the positions or opinions in this newspaper; DMH does not interfere with editorial content.
BRATTLEBORO RETREAT
Consumer Advisory Council, fourth Tuesdays, 12-1:30 p.m., contact Director of Patient Advocacy and Consumer Affairs at 802-258-6118 for meeting information.
CENTRAL VERMONT MEDICAL CENTER
NEWLY forming. Contact counterpoint@vermontpsychiatricsurvivors.org for more information. Every other month, 4th Tues, 11-12.
Conferences
The National Association for Rural Mental Health will convene in Pittsburgh, PA, on Sept. 19-21. The conference’s theme is “Building Your Bridge: Linking Voices to Promote Rural Mental Health.” Go to narmhconference.org.
ISPS-US
The annual conference of the American chapter of the International Society for Psychological and Social Approaches to Psychosis will take place from Oct. 27 to 29 in Newark, DE, and online. Go to page 23 for more information or visit isps-us.org.
N.A.P.S.
On Oct. 25 -26, the National Association of Peer Supporters will hold its annual conference in Norfolk, VA. Speakers include Dr. Louise Byrne, Tiara Springer-Love, and Jamie Bailey. Visit peersupportworks.org.
NIMH
The National Institute of Mental Health, alongside international partners, will host the 12th Global Mental Health Research Without Borders Conference on Oct. 30-Nov. 1 in the Natcher Conference Center in Bethesda, MD. Registration at gmhconference.com.
c Enclosed is $10 for 3 issues (1 year).
c I can’t afford it right now, but please sign me up (VT only).
c Please use this extra donation to help in your work. (Our thanks!)
Checks or money orders should be made payable to “Vermont Psychiatric Survivors.” Send to: Counterpoint, Vermont Psychiatric Survivors, 128 Merchants Row, Suite 606, Rutland, VT 05701
Access Counterpoint online at www.vermontpsychiatricsurvivors.org
Counterpoint is published by Vermont Psychiatric Survivors three times a year, distributed free of charge throughout Vermont, and also available by mail subscription. Vermont Psychiatric Survivors is an independent, statewide mutual support and civil rights advocacy organization run by and for psychiatric survivors. The mission of Vermont Psychiatric Survivors is to provide advocacy and mutual support that seeks to end psychiatric coercion, oppression and discrimination. Counterpoint does not use pseudonyms in its reporting without stating that a pseudonym is being used and without an explanation for why the person’s identity is not being disclosed. Counterpoint does not use anonymous sources under any circumstances.
Department of Mental Health
802-241-0090
www.mentalhealth.vermont.gov
For DMH meetings, go to web site and choose “more” at the bottom of the “Upcoming Events” column.
ADDRESS: 280 State Drive NOB 2 North Waterbury, VT 05671-2010
Fall 2018
2
Don’t Miss Out on a Counterpoint! NAME ADDRESS CITY • STATE • ZIP Mail delivery straight to your home — be the first to get it, never miss an issue. -
• Sen. Bernie Sanders, Sen. Peter Welch, and Rep. Becca Balint hosted a “town meeting on youth mental health” on June 29 at Spaulding High School in Barre. Sanders cited “a mental health crisis in America,” particularly “for our young people, who are living with enormous stress, anxiety, and loneliness.”
• Howard Center CEO Bob Bick will retire in June 2024. He has served in the position since 2015. The agency’s board of trustees will “launch a national search” for his replacement, soliciting input from clients and families, among others.
• State Treasurer Mike Pieciak organized a “virtual policy forum on homelessness” on July 24, inviting Lindsay Mesa from Pathways Vermont, Will Eberle from Recovery Vermont, Jess Graff from the Vermont Coalition to End Homelessness, Maura Collins from the Vermont Housing Finance Authority, and author Gregg Colburn. According to a press release, “Professor Colburn argued the cost and availability of rental housing best explains the rate of homelessness in a given community rather than individual factors like mental illness or generosity of public assistance.”
• Northeastern Vermont Regional Hospital in St. Johnsbury held a ribbon-cutting on July 25 for a new “mental health support area” in its emergency department. Funded by a $3 million Congressional earmark, the Patrick and Marcelle Leahy Suite adds “four patient rooms and two easily accessible bathrooms; a staff station; and a social room for commingling, consultation and family meetings,” per NVRH.
• The Chittenden County State’s Attorney and the Vermont Attorney General announced on Aug. 3 that they would not prosecute Burlington Police Department Sergeant Simon Bombard for a non-fatal shooting of a suicidal man on Manhattan Drive. An errant bullet struck the occupied car of a passerby in the same incidient.
• The Vermont Attorney General is investigating the Brattleboro Retreat, Vermont’s largest psychiatric hospital, for Medicaid fraud. Ongoing since 2020, the investigation became public in August when the AG petitioned a state court to force the Retreat to turn over relevant documents.
• Centerpoint Adolescent Treatment Services, which offers outpatient counseling for young adults in Chittenden County and operates a therapeutic school, will close on Sept. 1 due to a budgetary deficit, according to its three parent organizations: Howard Center, Northeastern Family Institute VT, and Matrix Health Systems. Howard Center, facing financial difficulties of its own, will phase out three additional programs by the end of the year.
• The U.S. Department of Education awarded an $820,000 grant to Vermont State University to support full-time paid internships for graduate students. They will serve as counselors in K-12 schools currently deemed to lack sufficient mental health services, starting this fall.

Another Way Stays Above Water
On Barre Street in Montpelier, Another Way Community Center sustained little damage from the flooding that devastated much of the rest of the city in July, keeping its doors open during and after the storm.
“We did have some minor flooding in the basement. There was some flooding just two
“It’s as though people struggling with ongoing homelessness are somewhat inured to this,” Cremo said.
Brown agreed. “You’ve got some that’s stressed because they lost all their camping gear, and you’ve got some that’s like, ‘It’s part of life. It happens.’”
Another Way has helped replace washedaway tents, tarps, and sleeping bags. Some community members saw the cars in which they’d been living engulfed by the floodwaters.
“A lot of folks who lost their home, or their lives were turned upside down, were able to come here and regroup,” Russell recalled. “There was a lot of mutual support, some basic needs, emotional support, helping to find resources, and sometimes replaying really traumatic experiences.”
Russell pointed out that the destruction of homes during the flood would exacerbate a severe housing shortage that had already impacted psychiatric survivors in Montpelier.
doors down, on the backside, on Stone Cutters Way,” Executive Director Ken Russell reported. “But we never felt we were in imminent danger.”
Another Way has provided what it calls “voluntary peer-run alternatives for people who avoid conventional mental health services” for nearly four decades. Seven days a week, it offers a safe haven for psychiatric survivors, especially those who struggle with homelessness.
“We’ve ended up working with more folks who are living outside than maybe some of the other peer organizations,” Russell said.
On July 10, while some community members hunkered down inside the building on Barre Street to stay dry, Another Way staffers ventured out to check on those still on the streets.

“We were sending outreach folks out into the field to help people who were camped out get away from the river and get onto higher ground,” Russell recollected. “There was some real intensity there. Luckily, it’s a peer-to-peer relationship, and folks knew how to reach people.”
In the subsequent days, traffic picked up at the community center.
“It’s been a lot busier,” said Cindy Gauthier, who works in Another Way’s kitchen and garden. “Normally, it’s a lot of familiar faces.”
“I can’t keep track of the number of people I’ve encountered who have lost housing, either temporarily or permanently,” he said. “What I hope is that the tremendous amount of
Save the Date
Oct ober 19, 2023
community support and people stepping up to take care of each other results in an even greater commitment to taking care of the most vulnerable people.”
The Killington Grand Hotel Killington, VT
VermontDepartmentofMentalHealthPresents:
“Now we’re getting new ones that lost everything,” shift worker Jason Brown added.
to offer the same free services, including daily breakfasts and weekly dinners, that it provided before the flood. But by Gauthier’s account, the need for these services has become “more urgent.”
That includes peer support.
“Some folks, they need to talk. A lot of them just want to vent,” Brown said.
DMH Conf ere nce 2023:
“But we need it to be sustained,” Russell continued. “There’s already some fatigue, but it’s going to be a marathon. It’s going to be a long recovery. So we’re in it for the long haul.”
Save the Date
Oct ober 19, 2023
The Killington Grand Hotel Killington, VT
hear about successful and researched approaches to integrated care .
VermontDepartmentofMentalHealthPresents:
DMH tracks:
• Wellness & Self Care
Save the Date
• Integrated Care & Policy
Conference 2023:
Reshaping Mental Health Systems Through Integration
DMH Conf ere nce 2023:
• Mental Health & the Criminal Justice System
Others appear less affected by the storm. Office manager Edward Cremo observed that many of Another Way’s regulars had long become accustomed to living without the sense of comfort and safety that other Vermonters, who’d had secure housing, lost only as a result of the flood.

Featuring workshops for child, teen, adult, and families :
Oct ober 19, 2023
A Statewide Symposium on Advancing the Mental Health System
Reshaping Menta l Health Systems Through Integ ration
• Promising and Evidence-Based Practices
• Panel Presentations
The Killington Grand Hotel Killington, VT
October 19, 2023
• Locally Developed Innovative Approaches and service models
A Statewide Symposium on Advancing The Mental Health System
The Killington Grand Hotel, Killington, VT
• Learning Sessions Watch for upcoming details from:
VermontDepartmentofMentalHealthPresents:
The Vermont Department of Mental Health https://mentalhealth.vermont.gov/

Reshaping Menta l Health Systems Through Integ ration
It has been a long few years , therefore the goal of this conference will bring together key stakeholders in mental health, health care and forensic system to positively impact the well-being of Vermonters. Join in an opportunity to gain knowledge about innovative practices, influence change and service delivery, and hear about successful and researched approaches to integrated care
DMH tracks:
DMH Conf ere nce 2023:
• Wellness & Self Care
A Statewide Symposium on Advancing
Care & Policy
Fall 2018
NEWS
3
IN THE NEWS
.
Fall 2023
Cindy Gauthier and Jason Brown (Counterpoint photo)
125 Barre Street (Counterpoint photo)
FLOODING • Continued from page 1 to do to get repairs done or get their business up and running again.”
According to Sloane, in upsetting or dangerous situations, the fight-or-flight reaction of the “primitive brain” can disable a person’s capacity for decision-making and reason.
“When you're in trauma, when you're having a PTSD response, and then when the frontal lobes go offline, then you're completely subject to whatever fear or trauma happens to be gripping you,” he said.
Vermonters whose homes stayed dry in July aren’t necessarily immune.
“People were overwhelmed by the impact of three and a half years of COVID, and this on top of it,” Sloane said. “And it can also be overwhelming just to follow the media.”
“You can get addicted to tracking the news, and which town is flooding and how many inches of rain have we had, and what roads are wiped out right now,” he elaborated. “That just keeps our nervous systems on high alert the whole time, and then it gets more and more difficult to function.”
Ghantous cited her experience as an example of the catastrophe’s inescapability even for those who, in a direct sense, stood relatively unscathed.
“It impacts everyone. I am driving to work, and I'm looking at the devastation of my neighbors. A good part of the way, I'm looking at a farm that lost a whole bunch of their crops,” she described. “My office is on the Lamoille Valley Rail Trail, which is closed down, and this beautiful bridge that I used to walk to on my lunch break is like a matchstick.”
Ghantous, Baird, and Sloane all faced professional roadblocks in the days following the flooding, either because washed-out roads had trapped them or their clients at home or because floodwaters had damaged the buildings housing their offices. But as they had during the pandemic, they managed to keep most of their appointments via Zoom or phone.
Ricciardello’s office in Morrisville was “relatively unaffected,” but Hardwick, the town where he lives, saw more severe flooding. On the night of the rainstorm, he’d signed up as a volunteer at the emergency shelter at the local high school.
“We were kind of just hanging out on the cots, and we didn't expect it to be that bad,” Ricciardello remembered. “And we kind of joked ‘Who brought the grill and the beers and the hamburgers?’ And then, within two hours, it was like, ‘Oh, this is actually a much more serious event.’”
In Ricciardello’s telling, Hardwick “kind of became an island,” leaving delivery drivers and construction workers to seek refuge overnight. Residents, rescued from their homes by boat, arrived via police cruiser.
“Of course, they were in a lot of shock. And so it was just making sure they were warm and fed and had dry clothes and had a place to lay their head,” Ricciardello recalled.
As a nearby inn washed away, its guests made their way toward the shelter. The owner, “of course, was devastated,” and volunteers like Ricciardello did what they could to provide emotional support, mostly just by “listening to his story.”
While the initial jolt of the loss of a business or a house may be considerable, Baird warned that victims may become even more vulnerable in subsequent weeks and months.
During the disaster itself, “your brain is going to do everything it can to get you through that stress,” she said. “But it's when you're able to
actually relax, that's when a lot of symptoms come up for people.”
Baird emphasized that experiences of trauma don’t always have to lead to the set of long-term symptoms that psychologists call post-traumatic stress disorder or PTSD.
“I will work with people soon after they've experienced an acute trauma to help them process what's happened and help them learn skills and strategies to help their system navigate this major stressor that they're now adjusting from to prevent further distress in the system later on,” she said.
Sloane shared a handful of tactics that –although they can’t replace “one-on-one trauma resolution work,” as he put it – can function as “stop-gap measures to help people self-regulate” when they can’t access additional support. They’re designed to keep people in what he called “the here and now.”
“What you do is you walk through your five senses. And you notice what your five senses are telling you about the space that you're in,” he said. “The only way to do it is to really be in that present moment. And I don't mean that as a cliche – I mean that as, like, you’ve got to look around. You gotta feel the material of the chair that you're sitting on. You have to feel your feet on the floor.”
“You're noticing the quality of the light in the room. You're noticing the smells of the soup on
“People want to help. And instead of becoming frozen in that fear response and sort of despondent, it’s a way of accessing your own power to do something about it,” she said.
But Ghantous also highlighted the risk of burnout. By late July, she’d already begun to notice signs of emotional fatigue among the scrappy residents of her town, so she and another local therapist began to organize community events that would give them a chance to put down their shovels and engage in conversation and reflection instead.

The first one would take place at the West Glover Congregational Church on July 25. Ghantous hoped it would help boost her community’s long-term resiliency.
“People are pretty tough up here in the Northeast Kingdom,” she said. “If we're just talking about this place, I don't think it's a new idea that, like, oh, this horrible thing happened, and we're going to get through it.”
Ghantous recognized, however, that some residents might fare better than others in the recovery.
“What I'm seeing is that the people who are the most affected by natural disasters,” she said, “are the people who don't really have a lot to begin with. There’s some trailers in my area that are completely unlivable at this point – that was a person's primary residence because they were on, maybe, cheaper land that was in a kind of a swampy area or something like that.”
Just as the toughest financial hardships would, it seemed, serve to compound preexisting financial disadvantages, the flood's worst psychological impacts would likely fall upon those who already harbored deep emotional wounds.
the stove. You're noticing the air on your face, whether the room is cool. Or you go outside and you feel your toes in the grass,” he went on. “And you say, ‘Yes, I am safe.’”
A loved one can help.
“Eye contact with a safe, understanding, sympathetic person is one of the keys to selfregulating. And at that point, it becomes coregulating,” Sloane said.
Ricciardello described psychological trauma as “really complicated on an individual level.” But he observed that July’s flooding hadn’t happened to an individual – it had happened to entire towns.
“It's affected a community, and so it ends up being kind of this collective trauma, which I think then the approach ends up being slightly different, in the sense of kind of reassuring people that you're not alone in this, that there are other people there who have experienced similar things who can relate,” Ricciardello said. “There's a whole community that is stepping up with resources and access to information, access to various forms of support, whether that's physical or emotional support.”
In Ricciardello’s telling, these free resources ran the gamut in flooded areas of Vermont after the storm, from excavator loans and volunteer driveway repair crews to “community suppers where you can go and just have a free meal and sit with people and share and be supported in that way.”
Ghantous also mentioned volunteer efforts as a source of hope and solace.
“You know about the studies, I'm sure, where adverse childhood traumas predispose people for more trauma later in life, for addiction, for health problems. And it's a lot of the people who live in socioeconomic conditions that are already dire, and you put something like climate disaster on top of it, and it's just this really difficult situation for them that's not going away anytime soon,” Ghantous said.
Ricciardello speculated that, for some Vermonters, unfortunately, there will be no recovery.
“There's people who, the reality is, there isn't coming back from this,” he lamented. “Yes, you can rebuild and fix and these things, but many towns here were completely underwater, and for people who were already kind of towing that line and kind of breaking even, it’s like this has now pushed them over to where it's, ‘Hey, we can't actually afford this house, and we have to cut our losses and go,’ or, ‘Hey, this small business that I started a handful of years ago, it's just not the right time, and it's not feasible.’”
“And then that shifts more into a grieving process, in my opinion: dealing with the loss –and not in the sense of a loss of life, but just a loss. You know, it's a loss nonetheless,” Ricciardello continued. “I think there's going to be plenty of people that are very much going to look at life as before and after the flood of ‘23.”
Meanwhile, luckier Vermonters will still have to worry about the next flood.
“People are not naive to the fact that climate change is happening and has been happening,” Baird said. “We're going to be experiencing natural disasters again in our lifetime, perhaps many times. And I think people are thinking ahead to, “OK, well, how can I get through this, but also how am I going to get through this again?’”
Fall 2018 NEWS 4 Fall 2023
Route 2, Williston (Counterpoint photo)
June Motel Evictions by State Appear To Increase Unsheltered Homelessness
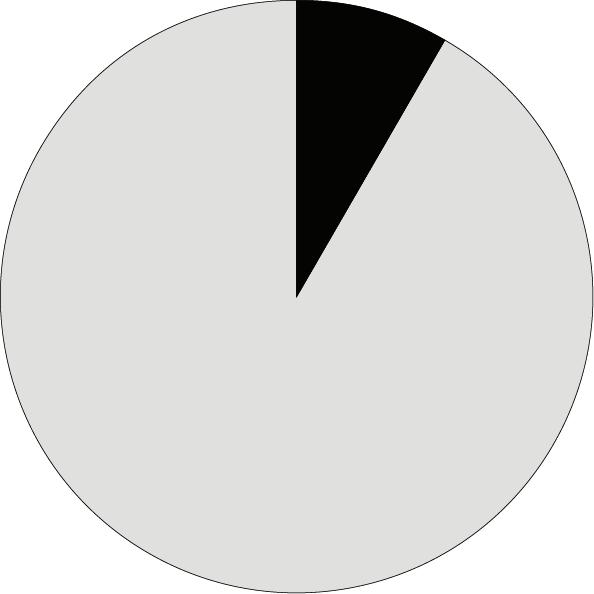
Roughly 800 homeless Vermonters lost their state-funded motel placements on June 1. The government didn’t collect data on where they went, but service providers have made observations of their own in the months since.
The group in question had not met vulnerability criteria – by virtue of disability or old age, for instance – that qualified 2,000 other beneficiaries of the pandemic-era emergency housing program for voucher extensions. Thanks to additional funding that the legislature allocated during the veto session on June 20, those extensions will last until next April.
In the lead-up to June 1, advocates, state officials, politicians, and journalists debated what would happen to the evictees.
Some argued that they would mostly land on their feet. After an influx of federal COVID-19 funds opened doors to motels across Vermont to all comers, the state’s homeless tally (which includes everyone sheltered by the emergency housing program) suddenly jumped from 1,110 to 2,591, generating suspicions that more than a handful within that count had chosen voluntarily to forgo rental housing for the no-questions-asked promise of a free room.
According to this rationale, upon the offer’s withdrawal, the motel residents would return to their prior living arrangements. But at the Champlain Valley Office of Economic Opportunity, Community Action Network Director Travis Poulin cast doubt on that premise.
“I have never in my experience, nor have any of my staff reported to me that they are working with someone who was stably housed and chose to become homeless so they could get a motel,” Poulin said. “I have never heard of that happening. I have never seen that happen.”
CVOEO offers case management and coordinated entry services to homeless and at-risk residents of Chittenden, Franklin, and Addison counties, helping them to find housing. It also operates a Community Resource Center, where clients can get meals, clothing, and internet access.
“We definitely were doing a lot of outreach leading up to June 1, trying to connect with people one-on-one. Many of the folks already had housing navigators,” Poulin recalled, “either through CVOEO or through one of the other agencies providing services. Some folks I know did go back to literal unsheltered houselessness. Some folks were able to move into apartments because the [coordinated entry] process had already been started and was just coming to an end around the same time.”
“It continues to be a challenge,” he continued. “We’ve got more people experiencing houselessness now than we’ve ever worked with
before to this point, and also people requesting financial assistance to prevent the loss of housing. It’s an extremely busy time.”
Poulin also reported “an uptick in the number of new faces at the Community Resource Center” in Burlington.
In White River Junction, Upper Valley Haven Executive Director Michael Redmond shared similar observations.
“We have seen, for us, an increase in the number of people who are camping, in that we purchase tents and other equipment that someone would need – tarps, sleeping bags –and we have given away a ton: over 50, last time I checked, since May,” he recounted.
In addition to running a temporary shelter, Upper Valley Haven provides other services, including a public shower, whose usage it tracks. The numbers have gone up this summer.
“We have seen increases in the number of people coming to our food shelf, which could be a lot of reasons associated with that,” Redmond added. “But we have routine days now where we have over 100 visitors to our food shelf. More
academic literature on homelessness, she said she’d never encountered the term in a case study.
“I will tell you what I think ‘self-resolve’ means,” she said. “I think what it means is when
typically, a year ago, it was more in the 70s. Last year, in May, the high number was 77, I think, once. And we’ve gone over 100 many times, 108 being the highest.”
At Groundworks Collaborative in Brattleboro, Director of Development & Communications Libby Bennett told a nearly identical story.
“We’re busier every day in our drop-in center here on South Main Street. We’re seeing a lot of new faces, and we’ve been at capacity for shelter beds just about every night. We’ve distributed, I would estimate, about 55 tents, including replacing some tents for people whose tents were a total loss after the heavy rains,” she said.
Bennington County Coalition for the Homeless Executive Director Chloe Viner Collins criticized the state for its reassurances that 800 June evictees would “self-resolve.” Despite her familiarity with the
they’re out in the woods, they can’t get captured for [the Homeless Management Information System] or coordinated entry. Basically, you’re only homeless if you’re entered into our system of homelessness and captured as an individual in our database.”
“I don’t think it means that they’ve successfully found housing,” she continued. “I’ve asked a lot for data. That doesn’t exist.”
By Viner Collins’s judgment, conditions in Bennington –which doesn’t have a 24-hour public restroom, a cooling shelter, or a public sharps disposal – have deteriorated visibly since June 1.

“What has happened is exactly what I told everybody would happen. For the first time ever, the main park in town, called People’s Park or Rotary Park, is having to be closed down constantly by the police,” she said. “There’s tons of complaints by everybody that Bennington is disgusting and full of needles and feces.”
The Vermont Coalition to End Homelessness and the Chittenden County Homeless Alliance will conduct Vermont's next annual point-intime homelessness county in January.
NEWS . 5 Fall 2018 NEWS Fall 2023 5
“We’ve got more people experiencing homelessness now than we’ve ever worked with before to this point.”
Counterpoint has a public comment section online! You can respond to any of our articles on our Wordpress at www.vermontpsychiatricsurvivors.org/counterpoint-articles/ !!!!!! WOW! Did you know? Be a leader in the psychiatric survivor and peer movement! Interested in being a board member for Vermont Psychiatric Survivors? Your help is welcomed and needed! Contact the board chair, Sara Merrow, at merrowsara@gmail.com for more information on how to apply.
At 220 North Winooski Avenue in Burlington, Feeding Chittenden houses CVOEO’s Community Resource Center, open 9 a.m to 2:30 p.m., Monday to Friday.
PATIENT ADVOCACY • Continued from page 1 someone’s being abused or harmed… their only recourse is to leave a message with you and maybe wait, like, three actual days while this is going on?”
After the fact, Webster reached out – to no avail, they reported – for a written apology, while encouraging Patient Advocacy to agitate for new personnel trainings to prevent the misgendering of patients in the future.
“They were kind of saying, like, ‘Oh, yeah, I hear you.’ That was kind of all they could do,” Webster lamented.
At the same time, Webster wanted “a better understanding about how medication works within [UVMMC’s] system.” During their November stay at the ED, they’d allegedly had to go without their normal prescription medications, which they’d left at home.
Upon returning to UVMMC in January, “I brought all the bottles with me. They were in my bag, which they had with my stuff somewhere else,” Webster said. When it came time for their nightly dose, medical staff “wouldn’t let me get my bag.” Another refusal followed in the morning.
Webster still doesn’t know for sure whether these denials contradicted UVMMC policy. Details about hospital procedures – such as when a psychiatric patient can or can’t leave the premises of their own will, and whether patients are required to share taxi rides with other patients upon discharge – remained murky to them even after several email exchanges.
“I was asking for internal documents,” Webster said. “And they said that they can’t provide those, but they can act as a conduit, in the sense that they themselves could read it and then answer my questions. And they never did that with any kind of satisfaction of mine.”
Meanwhile, the $28 reimbursement request for the Uber ride appeared to exceed Patient Advocacy’s authority, escalating Webster’s case to UVMMC’s risk management program, “where they have an actual lawyer heading it,” Webster said. “If the hospital is going to disburse any money at all, it has to go through there.”
Still, the reimbursement never arrived.
“It is really frustrating, and I haven’t felt like I’ve been heard or that there’s been any kind of resolution,” Webster complained. A hospital official “would say, ‘Your care has been excellent.’ And she’d tell me what my own experience was when I was contacting her to bring up different concerns that I had.”
Laura Shanks works as a patient representative for Vermont Psychiatric Survivors, the civil rights advocacy organization that publishes Counterpoint. Normally, she covers Southern Vermont – particularly the Brattleboro Retreat – but occasionally she’s subbed in for a colleague in Northern Vermont, which has given her some familiarity with UVMMC as well.
According to Shanks, the Retreat doesn’t have an Office of Patient & Family Advocacy, but it has one employee who plays a comparable role. Even though the Retreat “has notoriously had a worse reputation” (as Shanks put it) than UVMMC overall, she has witnessed quicker and more effective responses to patient complaints at the former institution.
“Their patient advocate is significantly better getting back to me and meeting with individuals as needed at the Retreat and actually working on problem-solving or finding resolutions than what I came across with all the UVM incidents,” Shanks said. “This one person has done so much more than this whole department at UVM.”
Shanks recalled a situation in Brattleboro
where a “person was having complaints around their doctor.” While the patient advocate couldn’t accommodate the request for a new physician, a meeting took place, and within “the next few days, the doctor made adjustments that this person was asking for in the way that they were communicating with them.”
On the other hand, in Shanks’s experience, UVMMC’s Office of Patient & Family Advocacy seems routinely to go “on vacation” for “literally two weeks or something. And then we’ll hear back.”
When a reply does arrive, it may not be pleasant. Shanks mentioned a patient “who may be contacting them too often, but they’re forwarding me pretty rude responses from the Office of Patient Advocacy.”
In Shanks’s telling, communications from UVMMC’s patient advocate have, at best, a perfunctory or lawyerly quality: “It seems every response we’ve had for any grievance or complaint put in has shuffled around it without actually touching on it, if that makes sense.”
Brandon, an Essex Junction resident who requested that Counterpoint withhold his last name for privacy, described speaking on the phone with the Office of Patient & Family Advocacy following an inpatient stay at UVMMC’s psychiatric unit over Memorial Day weekend. The conversation itself didn’t go badly.
“I got a hold of someone and was like, ‘I want to file a complaint.’ And they listened to my story. They were really sweet and kind of apologetic –like, not an actual apology, of course, but like, ‘Oh, I’m so sorry that you’re upset,’ basically. But they took all the information down, and they were like, ‘We will pass this along,’” Brandon recounted.
Brandon, who has a diagnosis of obsessivecompulsive disorder, had found himself “spiraling” last spring amid what he termed an addiction to alcohol and cocaine. He arrived at UVMMC on the advice of his psychiatrist and, in the ED, had “an incredible experience.”
“An ED resident came and talked to me, and basically, they were explaining the options. I expressed a preference for what is called an IOP, an intensive outpatient program, like the one run by UVM, which is called Seneca.”
By this point, though, it was “like 2 a.m. I’ve been there forever, I’m exhausted, I’m coming down off of all these substances, and I just want to crash. And they were like, ‘Let us take you inpatient overnight. You’ll go to a quiet place. You’ll be able to get some sleep.’”
By his account, Brandon complied happily. But in the inpatient psych unit, on Shepardson 3, he wasn’t as lucky.
With most of UVMMC’s doctors seemingly out of town for the holiday, a covering psychiatrist from Plattsburgh initially offered him what he’d wanted: a prescription for an antipsychotic and a referral to services at the Seneca Center, which he would use alongside continuing sessions with his own psychiatrist. Brandon was ready to go. But then the covering psychiatrist went home, and a psychiatric resident took charge.
“The psych resident comes into my room
with the med student and says, ‘So I hear you’re asking about discharge,’” Brandon recollected. “And I was like, ‘Yeah, I would like to do an IOP. I would like to do the three things we talked about, starting now.’
“He told me, ‘Based on what I understand about you, if I let you go, you are going to kill yourself.’ And I was like, ‘Dude, I’m totally not. Were you not listening to anything that I said?’ The whole thing is that I have obsessivecompulsive disorder: I never had the intention to kill myself, but I have these obsessive thoughts that come with a fear of intention. And it’s this whole thing, but I never actually wanted to kill myself, and I made that very clear on every chance possible.”
The resident didn’t seem to hear Brandon.
“He was like, ‘Here’s the deal: if you want to be discharged, we are going to have to pursue an involuntary hold.’” It would likely last seven days.
The threat struck Brandon as “an absurd escalation,” and he went into “full-blown panic mode.” Ultimately, his wife found “someone that looks important” and “raised hell” on his behalf, “until, basically, they agreed to give me a discharge against medical advice.”
The discharge let Brandon go home, but it canceled his prescription and his referral. Sobriety has been hard.
“I’ve got my support network that’s holding me together, but I am not receiving any form of institutional support,” Brandon said.
Four weeks after filing a complaint against the psychiatric resident by phone, Brandon received a follow-up email from the Office of Patient & Family Advocacy, stating that it had forwarded his complaint to the resident’s “leadership committee,” as he recalled it.
“And then they were like, ‘However, everything after this is personnel records, so we’re not privy to those details.’ So, basically: ‘We told them about it, but we’re not allowed to know if anything’s actually happening.’”
Disciplinary measures for the resident seemed unlikely, but Brandon still wanted to receive services at the Seneca Center. Patient Advocacy didn’t offer to help him get the referral reinstated.
“I assumed that acting through the Office of Patient Advocacy would be my route, and all they did was listen to my story,” Brandon said.
“At the very least,” he’d hoped for “maybe a call from someone on the leadership committee being like, ‘Hey, I heard about this,’ and either, ‘I want your side of the story,’ or ‘It wasn’t cool.’ The problem is that I don’t know what my medical documentation says. So maybe the story that they’re seeing is totally different.”
VPS’s new patient representative for Northern Vermont, Kat Parker, previously worked at UVMMC as a licensed nursing assistant and as a medical assistant.

“Even to a lot of staff, they’re not sure what patient advocacy really does there. To me, it was sort of this impression of, like, this pacifier to make patients shut up,” Parker said. “That’s what a lot of the nurses kind of used it as: ‘OK, you put in your complaint. Cool. Bye.’”
Even so, Parker wouldn’t try to dissuade patients from using the service.
“It’s definitely still the first step,” she said. “I would encourage my peers to put it in writing, save a copy, date it, keep track of time and everything, and then just be a squeaky cog about it. Call in every two to three weeks and be like, ‘Hey, I just want to see where we are on the on the progress of “blank” grievance.’”
NEWS 6 Fall 2018 NEWS 6 Fall 2023
Laura Shanks of VPS
Survivor Trains ED Staffers
by BRETT YATES
With the Department of Mental Health still working to resolve prolonged wait times for psychiatric inpatient beds, hospitals have turned to the Vermont Program for Quality in Health Care to learn how to improve services within their emergency departments. One of its instructors, mental health advocate Kristy Hommel, makes use of her lived experience as a patient.
VPQHC, a state-sponsored nonprofit, has organized a four-hour course called “Trauma Responsive Care in Emergency Departments.” When Senior Program Manager Mary McQuiggan spoke to Counterpoint in August, eight hospitals had received the training, with two more scheduled.
According to McQuiggan, the course has a special focus on hospital workers’ interactions with children with psychiatric needs, who, owing to a relative scarcity of pediatric inpatient beds in Vermont’s mental health system, tend to end up stuck in EDs the longest. It begins, however, from the premise that trauma-informed practices can benefit anyone who shows up to the hospital in an emergency, no matter their age or the nature of their crisis.
“Ultimately, the thought is that you don’t know who has trauma,” McQuiggan said. “And it’s in no way advocating to ask everyone about their trauma history, because that would be really traumatizing. But the idea is that if you come from a perspective of understanding that anybody who walks in may have a trauma history, then you can work with them in a really curious, understanding, and supportive way that will make the experience better and more supportive for them and also better for their families and for the staff.”
Alongside Hommel, VPQHC hired a nurse practitioner, Matt Dove, and a social worker, Pete Cudney, to deliver the training. Although Hommel, who has a master’s degree in childhood education, had previously shared her story of suicidality and recovery in schools, on panels, and at the Vermont Police Academy, her colleagues’ clinical credentials made her, in her words, “a little nervous” at first.
It didn’t last long, though. “The three of us clicked, and it’s a joy to work with them,” Hommel said.
Hommel, who has survived two suicide attempts, has had some negative experiences in hospitals. She remembers how, when she was 14, she had to stand naked and fearful in front of a doctor and a nurse for a process called “body mapping,” which they used to track self-harm.
Years later, when she went to the ED for a kidney stone, the doctor – in a case of what she called implicit bias – misdiagnosed her symptoms as pancreatitis on account of her

history of substance abuse. Eventually, a CT scan proved him wrong.
Visiting the ED on another occasion, during a mental health crisis, Hommel ended up in a closed, empty room and began, for the first time, to dissociate, feeling as though she were watching herself in a black-and-white movie.
“People kept coming in and asking me the same question, basically to relive the crisis: ‘What brought you here today? What happened?’” she recounted.
But Hommel has also had positive experiences. She recalls a nurse who brought her a warm blanket when she was cold and didn’t feel bold enough to ask for one. Another nurse spotted
Department of Mental Health, VPQHC received funding from the federal Health Resources and Services Administration to bring the idea statewide.
The first training took place on April 26. The course has four sections.
McQuiggan called the first “Trauma 101, understanding what trauma is, the basics.” The next deals with “secondary traumatic stress” – in other words, the potentially traumatizing effects of working within a trauma-laden environment – and what hospital employees can do to take care of themselves.
The third section centers on de-escalation during mental health crises.
“We provide them some strategies,” Hommel said. “We’ve got a really nice slide where it has all the things you can do if you have five minutes, all the things you can do if you have 10 minutes.”
The trainers also role-play various scenarios.
“Basically,” Hommel explained, “we’re showing me having a panic attack, [Dove] coming in, getting on my level, telling me that we’re in it together. So they get to see an interaction that could possibly happen.”
The final section highlights children’s particular needs. The trainers can administer the course twice in a day, making it available to workers on different shifts.
VPQHC reports positive feedback.
“Just anecdotally, the hospitals we’ve spoken to have asked us to come back. They’ve said, ‘Oh, we really want to bring all of our sitters into this training, or we want to get our security team to attend this training,’” McQuiggan said. “We’re hopeful that we’ll be able to do that next year and bring more folks in to be trained.”
her sweet tooth and “would grab me an extra vanilla pudding” when she could.
“It’s a small thing, right? But she thought, she noticed, and then she was kind,” Hommel said.
As an instructor, she shares these examples with ED staffers.
“I talk about how people just want to be heard and seen and believed. Because, having a mental illness, you can’t really see it,” she observed.
According to McQuiggan, Hommel’s presentation has made an impact.
“All the staff have been so appreciative of her perspective, because they don’t often get to speak to patients after they leave and hear about their experiences and hear what was helpful and what wasn’t helpful,” she said.
While the instructors have made VPQHC’s course their own, it originated at the University of Vermont Medical Center, where, in McQuiggan’s telling, the pediatric psychiatrist Haley McGowan and the pediatric emergency medicine physician Christian Pulcini developed it for their staff. Through the Vermont
Rutland Regional Medical Center received the training on May 8. Several nurses, medical technicians, and others attended, but the hospital’s priority was to train its emergency psychiatric technicians, according to Thera Blehar, the nurse manager of the ED’s psychiatric east wing.
“I think that the training and hearing from Kristy and her experiences, her perception of things – it just helps staff kind of take a breath before they respond and realize that not everything works for every person. And sometimes you have to be creative,” Blehar said.
Blehar noted that the training didn’t just tell the workers what they were doing wrong – it also told them what they were doing right.
“It was just nice to have that reminder for staff that, also, our patients do remember the good work that we do. You remember someone sitting and taking the extra five minutes talking to you or listening to you or playing a game with you or getting you that cup of water. It can be the little things that we do that have a huge impact on the patient’s experience when they visit us.”
Retreat Aims to Reopen Residential Program
The Brattleboro Retreat, Vermont’s largest psychiatric hospital, has convinced the Green Mountain Care Board that it shouldn’t have to navigate a lengthy regulatory process before reopening an adolescent residential treatment program that shut down during the pandemic.
According to a letter sent by the Retreat to state regulators in August, the program operated from the 1970s until 2021, when a worker shortage, among other factors, led to its closure. The Retreat also runs two inpatient units for adolescents.
In May, the Vermont Department for Children
and Families issued a request for proposals in the hope of contracting a vendor to launch a psychiatric residential treatment facility for adolescents. By its own account, the Retreat responded.
A spokesperson from the Vermont Agency of Human Services told Counterpoint that they couldn’t provide information about other possible bidders or about the selection of a winning bid before the finalization of an agreement. The RFP anticipates a start date of Oct. 1 for the contract.
If the Retreat’s bid wins, it will be able to
begin operations without first having to earn a Certificate of Need, as new healthcare projects in Vermont typically do. In its letter, the Retreat argued that a reopened residential program “doesn’t constitute a ‘new health care project.’”
The restarted program wouldn’t occupy the same location on the Retreat’s campus as its previous iteration, but by repurposing an old inpatient unit, it wouldn’t require the construction of a new facility, either. The Retreat estimated startup costs at $98,999.
The GMCB ruled in the Retreat's favor on August 25.
NEWS . 7 Fall 2018
NEWS Fall 2023
Kristy Hommel (Counterpoint file photo)
Massachusetts Legislator Proposes Peer Respites
The Massachusetts General Court will soon consider legislation to establish 14 or more peer-run respite centers in the Bay State, with a minimum of one in each county. Rep. Lindsay Sabadosa, alongside Rep. Smitty Pignatelli, introduced the bill in the lower chamber in March.
Unlike the Vermont General Assembly, Massachusetts’s legislature doesn’t adjourn after passing the budget for the new fiscal year in July. Sabadosa expects the Mental Health, Substance Use and Recovery Committee’s hearings on H.3602 to begin in the fall.

Representing Northampton, Sabadosa drafted the legislation in partnership with the Wildflower Alliance, a local organization that opened the state’s first peer respite, Afiya.
“After I was elected, they came and sat down with me to tell me about the work that they were doing,” Sabadosa told Counterpoint. “I was very in love with the concept that you could have a sort of non-medicalized response to a crisis and that that could be really successful, building off of the experience of peers who actually have understanding of the situation.”
But “the thing that absolutely cemented” Sabadosa’s commitment to expanding the approach was testimony about Afiya from constituents, who “talked about how much peace it brought them and what a good experience it had been.”
Her bill would instruct the Massachusetts Department of Mental Health to contract peerrun organizations to establish and operate “voluntary, short-term residential programs that provide community-based, trauma-informed,
person-centered support and prevention on a 24/hour basis in a homelike environment to adults, age 18 or older, who are experiencing emotional or mental distress either as an immediate precursor to or as a part of a crisis.”
Staff would consist of “individuals who are formally trained in the provision of peer support services, and who have psychiatric histories and/or have faced and navigated similarly life interrupting challenges.”
Two of the respites, in Hampden and Suffolk counties, would dedicate themselves specifically to “serving LGBTQIA+ individuals,” with a workforce from the same community. The Wildflower Alliance calls these “affinity peer respites.”
By Sabadosa’s account, the legislation has the support of the Department of Mental Health. “The biggest roadblock is always the question of money,” she said.
According to Sabadosa, the state pays $450,000 annually to support Afiya. Calling it “a significant investment,” she pointed out that peer respites typically operate out of singlefamily homes, “and so the cost of leasing or renting those properties can be very high in Massachusetts.”
In the budget for fiscal year 2024, Sabadosa proposed an unsuccessful amendment to allocate funding for two new peer respites. The 2025 budget, starting next July, would fund H.3602 if it passed.
Between now and then, Sabadosa aims to convince other legislators that peer respites can eliminate pricier stays at emergency departments. The other key, she believes, will be
to bring in witnesses who’ve experienced peer respites themselves.
“Those firsthand stories really are invaluable in situations like this,” she said. “I mean, I can sit there and tell you all day that it’s a great idea, but someone who’s actually stayed at Afiya is going to give you a much better idea of what that really meant in their life.”
Ephraim Akiva, the director of Afiya, told Counterpoint that he envisioned the Wildflower Alliance submitting a bid to run the entire network of new peer respites in the event of H.3602’s passage. But he also described the statewide expansion proposed by the bill as a “long-term goal.”
In the short term, he wants DMH to fund one of the aforementioned LGBTQIA+ respites out of its current budget, before any legislative action that would compel it to do so. He intends to site the facility in Holyoke.
Akiva described Sabadosa’s legislation as, in part, a “strategy” to “put more pressure” on DMH to take initiative.
“It’s getting more interest out there,” he said. “People who had no idea what peer respite was now know what it is.”
Akiva, who identifies as queer and trans, came up with the idea for the affinity respite, which he claimed would be the first of its kind anywhere.
“I see my people suffering all of the time,” he said. “We’re seeing unprecedented attacks on trans folks in particular right now.”
In addition to Afiya, Massachusetts currently hosts two other peer respites, operated by Kiva Centers, in Worcester and Bellingham, called Karaya and Juniper.
Union at Soteria House Wins First Contract
Workers at Soteria House in Burlington ratified their first collective bargaining agreement with their employer, Pathways Vermont, in late August.
Soteria House is a peer-run therapeutic residence. Its staff unionized in the summer of 2022, joining Local 1343 of the American Federation of State, County and Municipal Employees. Pathways voluntarily recognized the union.

According to an announcement by the Vermont State Labor Council, AFL-CIO, the new three-year contract at Soteria House boosts pay for all its employees. For instance, it immediately increases the base wage for a full-time worker with one year or more of service from $16.32 to at least $20.50 per hour. Employees will receive additional 3.5% and 3% raises in the second and third years of the contract, respectively.
The agreement guarantees staffing ratios and imposes just cause termination standards. It also gives workers a stronger voice in the operations of the facility: the union’s steward will have an opportunity to join management’s weekly meetings, and the workers will have a right to
form a joint labor-management committee. They’ll have a seat on hiring committees as well.
Eryn Sheehan, a peer support staffer and former resident at Soteria House, told Counterpoint that employees’ desire for more control over their workplace had been a major reason for unionization.
“One of the big things that people wanted was more say in decision-making at the house, so it doesn’t always feel like the decision is being made elsewhere,” she said.
By Sheehan’s account, bargaining began in November 2022.
“It's just been like a lot of back and forth with going over our proposal and then counter-proposals from their side and agreeing to certain elements, but the language needs to change. It’s a lot of details and minutia,” she said.
Unlike the nearby AFSCME-affiliated Howard Center Union, the union at Soteria House will be able to collect “fair share” fees, which means that all workers, whether they choose to join the union or not, will pay dues.
The contract also paves the way for potential unionization for the rest of the Pathways workforce, who, it appears, will enjoy the same relatively uncomplicated process that their colleagues at Soteria House did. Pathways has reportedly committed in writing to continuing to recognize AFSCME organizing efforts through “card check,” forgoing the additional requirement for a secret ballot election administered by the National Labor Relations Board.
“I've been really optimistic that the only reason there wasn't already a union in place was because it's just a young agency, and they hadn't gotten around to it yet,” Sheehan said.
NEWS . 8 Fall 2018 NEWS Fall 2023 8
Soteria House (Counterpoint photo)
Feds Publish National Standards on Peer Certification As Work Continues in VT
More than a year ago, in connection with President Joe Biden’s 2022 State of the Union address, the White House announced a “national mental health strategy to strengthen system capacity,” including the peer workforce.
This June, the Substance Abuse and Mental Health Services Administration, a branch of the U.S. Department of Health and Human Services, described its new National Model Standards for Peer Support Certification as a product of this effort.
“These new national standards will help advance President Biden’s strategy to tackle the nation’s behavioral health crisis,” HHS Secretary Xavier Becerra said in a press release. “Getting help from a person who has been successful in the recovery process can be lifechanging.”
According to the 28-page document, 49 states already have established peer certification programs of some kind. The 2023 national standards “are not intended as a substitute for any state certifications but instead have been developed as guidance for states, territories, tribes, and others, to promote quality and encourage alignment and reciprocity across often disparate state peer support certifications.”
SAMHSA’s Office of Recovery began work last fall. The process first “convened a diverse set of technical experts with a range of identities, lived experience, and professional expertise” and then “employed a public comment process to solicit and incorporate additional feedback and expertise from the peer workforce, states, and others.”
A potential certification program for mental health peers in Vermont remains under active development. The National Model Standards for Peer Support Certification reveal areas of both alignment and disagreement between the policy preferences of SAMHSA and the suggestions put forward for the Vermont Department of Mental Health by its Peer Workforce Development Initiative.
The national standards, for instance, recommend requiring an “attestation of lived
experience” for peers while advising against formal education requirements (such as a high school diploma) and against automatic disqualification on the basis of a criminal conviction. Vermont’s prospective program appears unlikely to diverge from any of this guidance.
But while SAMHSA advises states not to demand more than 120 hours of supervised work experience for peers seeking certification, a draft screening application for Vermont cites a requirement for “250 hours of supervised, paid, or volunteer peer support in the two years before applying for certification.” Vermont would, however, allow applicants with insufficient hours to earn a “provisional status”

from New York wouldn’t instantly receive certification upon moving to Vermont. Instead, they’d “learn Vermont’s system and peer support values and principles” first.
But for SAMHSA, it seems, the purpose of developing national standards was to obviate the need for such a period of adjustment as much as possible.
“SAMHSA is recommending that state certification entities strengthen collaboration efforts and implement additional processes for expanding reciprocity, and strongly encourages state certification entities to utilize this document to revise, strengthen, and align their peer support certifications with other states,” the document states.

Suggestions include creating an “interstate compact” or “a reciprocity board or committee made up of certified peer workers.” States might also “connect with a national reciprocity organization to discuss strategies for implementing reciprocity” or, on their own, “develop a simple certification process for peer workers that are certified in another state.”
that would permit them to practice peer support temporarily, before satisfying the requirements for full certification.
For training, SAMHSA recommends a course that would take peers 40 to 60 hours to complete.
A report delivered to the Vermont Department of Mental Health last year by the Peer Workforce Development Initiative advised DMH to contract a peer-run entity to administer four existing training programs – Intentional Peer Support, Wellness Recovery Action Plan, Alternatives to Suicide, and Hearing Voices, which together would add up to a minimum of 66 hours – as well as a “state-specific curriculum”: all in all, “at least 80 hours,” per the draft application.
The Vermont report also discourages DMH from granting automatic reciprocity to other states: in other words, peer support workers
DMH Deputy Commissioner Alison Krompf told Counterpoint that the department hasn’t yet finalized reciprocity standards for Vermont’s upcoming certification program for mental health peers.
“I think with the staffing crisis and Vermont’s demographics and how much we’ve got an aging population, we need a way to encourage people to come to the state,” Krompf said. “I think the peer community has a voice in, ‘OK, we want reciprocity, but maybe there’s two or three things that we really feel strongly about that you have to have in Vermont.’ But making that seamless and not painful is going to be really important so that we don’t put up barriers to people doing the work.”
According to Krompf, the Peer Workforce Development Initiative will begin “phase three” of its planning work in September. She predicted that the certification program would begin operations next year between May and August.
DMH: Statewide Mobile Crisis Services Delayed, Other Projects Mostly on Track
Vermont’s statewide mobile crisis response program will not launch – in full or in part – on Sept. 1 as planned, according to the Department of Mental Health. Deputy Commissioner Alison Krompf named Jan. 1 as a likelier start date.
DMH contracted Health Care & Rehabilitation Services of Southeastern Vermont to lead the project, which, with the involvement of the state’s nine other community mental health centers, will send mental health workers into homes and other community settings at callers’ request. Krompf attributed the delay to July’s floods.
“HCRS got hit with some of the most significant flooding, so there’s been a bit of a pause for some of this,” Krompf told Counterpoint on Aug. 15. “We were in the final stages of finalizing that contract when that happened. And they had to stop because they’re out there working with all
sorts of people in the community.”
The mobile crisis service isn’t the only new program intended to reduce visits to Vermont’s emergency departments for psychiatric needs. Alongside four other community mental health centers, HCRS also received a grant earlier this
year to establish a new mental health urgent care clinic.
But owing again to the flood, Krompf expected to see its opening date “pushed back a few weeks,” possibly. She anticipated that the new urgent care clinics at Lamoille County Mental Health Services, Washington County Mental Health Services, and Howard Center would launch in September.
The new program at Counseling Service of Addison County, called Interlude, has already begun operations at 99 Maple Street #16 in Middlebury. Using the so-called Living Room Model, it offers a “voluntary, homelike” environment as the agency put it, for people experiencing mental health crisis. Staffers reportedly use “trauma-informed approaches, including Intentional Peer Support and Open Dialogue.”
Fall 2018 NEWS 9 Fall 2023
The Hubert H. Humphrey Building houses the U.S. Dept. of Health and Human Services in Washington, D.C.
Burlington Goes Mad Again
Psychiatric survivors celebrated Vermont Mad Pride 2023 on July 15. For the second year in a row, the event took place in Burlington, starting with a march between the Hood Plant and Battery Park – this time, without a police escort.






With a megaphone in hand, Life Intervention Team Executive Director Karim Chapman, formerly of Vermont Psychiatric Survivors, led attendees up Church Street. Signs and chants helped bring their message of civil rights for psychiatrically labeled people and neuroinclusivity to the public.
A 14-person planning committee had invited journalist Robert Whitaker and Massachusettsbased nonprofit director Sera Davidow to give keynote addresses following the march and a free outdoor lunch. They joined four other speakers (Hilary Melton, Calvin Moen, Chris Hansen, and Wilda White), two poets (Rajnii
Eddins and Zenni Muhammad), and the band Flashback under Battery Park’s bandshell. Ericka Reil emceed.
Sponsors included Intentional Peer Support, Pathways Vermont, and Disability Rights Vermont, all of which set up tents and tables inside the park alongside other organizations and local artists.




NEWS 10 Fall 2018 News 10 Fall 2023
Photos by Brett Yates.
Neuroinclusive Health Clinic Reports Growth in Montpelier at Open House
All Brains Belong VT, a Montpelier-based nonprofit founded during the pandemic, garnered attention last year thanks to its unusual COVID-19 vaccination clinics. Outdoor settings (including the Statehouse lawn), calming features, and specially trained staff allowed neurodivergent children, who may struggle to enter traditional medical settings, to get the shot for the first time.
Neuroinclusive healthcare isn’t just for kids. Led by a physician who has cited her own diagnoses of autism, attention-deficit/ hyperactivity disorder, dyslexia, dyspraxia, and discalculia, All Brains Belong’s medical team delivered care to 252 patients of all ages in 2022, according to its own annual report.
Now, amid what Executive Director Mel Houser called “a lot of growth this year,” the count has risen to 330. On August 2, All Brains Belong held an open house on Zoom to help introduce the public and prospective new patients to its unique offerings.
“Our scope of practice is very specific,” Houser said.
It starts with a theory: the “social model of disability,” a term coined by a British professor of disability studies in 1983. According to this understanding, “it’s not deficits on the part of the person. The issue is an inaccessible world,” Houser explained.
“So what we try to do here is, we try to offer everything that we’re doing in multiple different ways,” she said. “All of our patients complete a customized menu, where it’s really about a co-created experience where you let us know: this lighting, this furniture, these executive functioning and communication supports.”
All Brains Belong’s primary care office offers a sensory-friendly environment. Ahead of time, patients can ask for adjustments with respect to the physical space or to how much (or how little) interaction they may prefer in the waiting room.
“We can make a lot of stuff feasible, which is the nice part about being a small practice,” said Sierra Miller, a nurse practitioner. “It’s intentionally not set up to look like a traditional healthcare setting, partly because a lot of people we serve have a lot of healthcare trauma.”
The office’s COVID-19 precautions remain non-negotiable, however, owing to an abundance of immunocompromised patients who, in Houser’s telling, “don’t have anywhere
else they can get healthcare with this level of risk mitigation.” Maskless or unvaccinated patients can schedule outdoor appointments.
Services include not just regular checkups but also specialized care for a small set of illnesses that particularly affect the neurodivergent population, such as Ehlers-Danlos syndrome, postural orthostatic tachycardia syndrome, mast cell dysfunction, and Long COVID.
“Even if someone does not identify as neurodivergent, they may be coming here because they have a medical condition that we have expertise in,” Houser said. “We also have folks who come here for
for that child. And then I look at all the different forms that come in and try to make a match with another child that has similar interests.”
Kids Connections can help children find new friends who live nearby or join a virtual “Lego party,” inviting them to engage in what Wilkins called “parallel play” via Zoom. A similar program allows adults who enjoy crafting at home to do so synchronously and “kind of chat with each other or use the chat function, just be with each other in community,” as she put it.
An educational discussion group called Brain Club takes place weekly. Once a month, an author joins the Zoom call to discuss a book.
In 2022, All Brains Belong hosted its first annual Community Health Education Fair on the Statehouse lawn. The flooding in Montpelier delayed plans this summer for the second, which would have included various presentations as well as live music and art.
“Our programs are informed and driven by our community members,” Houser stated.
“We have a community advisory board that informs everything that we do.”
The goal is to foster a sense of inclusion. That’s also why All Brains Belong offers assistance for patients seeking employment.
treatment.”
All in all, most patient visits, in fact, take place online. Houser called All Brains Belong a “telehealth-predominant practice,” but this hasn’t prevented the organization from advancing a mission rooted in a vision of human connection for neurodivergent Vermonters.
Houser referred, for instance, to “group medical appointments” as an option. But “health is so much more than healthcare,” she added.
Accordingly, All Brains Belong functions as much more than just a health clinic. Its free community programs are open to patients and non-patients alike, according to Sara Wilkins, who organizes them.
By Wilkins’s count, more than 120 children have participated in a program “called Kid Connections, where caregivers can fill out a form on the website stating what the child’s interests are and what type of communication style works
“We know that there are lots of barriers to access many things in society. This might be things in the physical environment. This might be things around social interactions or culture,” Houser said. “The consequences of this are exhaustion, anxiety, stress. All of it – it’s all part of health.”
In this way, better health outcomes may depend upon broader social changes. On the political level, All Brains Belong has advocated –unsuccessfully so far – for a state law to restrict restraint and seclusion in schools (see page 17), hoping to make education in Vermont friendlier to students with disabilities.
The organization also provides trainings to companies that want to become more neuroinclusive. The consulting fees help pay for community programs.
“Again, the whole point is: connection is the path to health,” Houser said.
Visit allbrainsbelong.org or call 802-2341098 for more information. The Montpelier primary care clinic accepts “a wide range of insurance carriers,” per Houser.
SVMC To Seek Regulatory Approval, Eventually
Southwestern Vermont Medical Center’s board of directors gave hospital administrators a green light in July to apply for a Certificate of Need from the Green Mountain Care Board for a new adolescent psychiatric inpatient unit in Bennington.
Vermont requires healthcare providers to get permission from state regulators before undertaking any large projects. Director of Planning James Trimarchi said that he expects the filing to take place by the end of 2023.
“Filing for the Certificate of Need requires financial tables that project into the future the five-year impact of starting the mental
health unit,” he said. “In today’s healthcare environment, it’s incredibly challenging to put forward a five-year projection of what the financials are going to look like.”
Trimarchi doesn’t anticipate that the GMCB will render a swift decision once it has the application in hand.
“It is likely that there’ll be some interested parties in both support and not-support of the project that could result in the CON process becoming protracted,” he predicted. “We’re a long, long ways from doing anything.”
In July, the New Hampshire-based multihospital system Dartmouth Health, which
includes Dartmouth Hitchcock Medical Center in Lebanon, acquired SVMC. Trimarchi believes that, when it comes time to staff the new psych unit, the affiliation will offer a major advantage.
“The Dartmouth Department of Psychiatry has agreed to supply the providers for the mental health unit,” he said. “There’s no way that we could get the talent we need in order to run this unit without Dartmouth’s backing and support.”
The Vermont legislature allocated $9.225 million in public funds to pay for the adolescent inpatient unit’s construction in the spring. The Brattleboro Retreat currently operates Vermont’s only inpatient beds for adolescents.
NEWS . 11 Fall 2023
The Arts
Art


Artist Finds More Than One Way To Draw a Cat

At scaredycatart.com, Burlington-based artist Sarah Brunkhorst sells prints and stickers at prices starting as low as $2. Her bright, often humorous digital illustrations, by her own description, contain “a lot of visual gags” while also touching on “subtle social issues” with a hint of “punk and feminism.”

“I try to make things that are fun and colorful and that have to do with disability. I take a lot of inspiration from my cats as well,” she said.
Brunkhorst, who originally moved to Vermont from rural Missouri to attend Champlain College, identifies as autistic.
“Talking about things with other people can be really hard, either important things or even just making that first impression,” she explained. “So being able to kind of create what I want to say at my own pace, in my own time, not in the moment, and having that to put out there and show people – that’s kind of a way for me to communicate that’s less hard and scary.”
Selling her art in 2021 at the Ramble, an annual festival in Burlington’s Old North End, inspired her to start a business, which she called Scaredy Cat Art.

Since then, Brunkhorst has brought her work to Art on Park in Stowe and the Downtown Winooski Farmers Market, where she serves as the market’s manager. Buyers can also find some
of her creations at Thirty-Odd in Burlington’s Soda Plant at 266 Pine St.
“Selling art,” she said, “has been, I think, really therapeutic, being able to connect with people in a way that I never had before. That feeling when someone comes up to my booth
and I can see that they understand and relate to something that I made is just a really amazing experience that can be hard to come by, so I’ve really enjoyed that.”
In July, she tabled at Vermont Mad Pride.

“I feel like there aren’t a lot of events like Mad Pride, unfortunately, and I would love to do more like that,” she said. “I definitely dream of organizing, like, a disability market or something like that.”
Autism affects the way Brunkhorst sees the world, which in turn affects her art.

“I think art is a really sensory-heavy experience, and experiencing sensory input differently because of autism – I think those things are definitely intertwined,” she reflected.
Since 2020, Brunkhorst has worked parttime at Howard Center, where she serves as the Exhibitions and Community Engagement Coordinator for the agency’s Arts Collective. Members of the Arts Collective, according to its website, have “lived experience with mental health and/or substance use challenges” and have worked together to mount shows at the Fleming Museum and the Fletcher Free Library, among other locations.
“Before my autism diagnosis, I was diagnosed with depression and anxiety and PTSD. And now, I don’t know if those were things that really were different experiences or if they were part of being autistic, but they’re still things that I do experience,” Brunkhorst said. “And I think that just being around people that understand what those things are like is really great, and having those experiences definitely helps me understand some – definitely not all – of what the people that I work with are going through.”
The Howard Center Arts Collective’s current exhibition is taking place at the Flynndog Gallery at 208 Flynn Avenue in Burlington from Aug. 4 till the end of September. The Collective will host a reception during the South End Art Hop on Sept. 8 from 4:30 to 6 p.m.
Fall 2023
12
“Sad”
“Building”
“My Place in Things”
by Sarah Brunkhorst.
Photo by Brett Yates.
“Landlord vs. Racoon”
“Mazzy” “Graveyard Ghosts”
Sarah and her partner Sean at Mad Pride
Exhibition Spotlights Stories of Homelessness
by BRETT YATES
Vermont Folklife’s research for In our voices, in our communities, a timely traveling exhibition of portraiture and storytelling with a focus on homelessness, began more than two years ago. When it finally debuted in Burlington this spring, one day after the passage of the state’s annual budget, the legislature’s controversial decision to end Vermont’s pandemic-era emergency housing program had drawn the issue into local headlines as never before.
2023 also brought the statistical revelation that Vermont now ranks second in the nation, after California, in per-capita homelessness. Its official count first skyrocketed following the state’s effort in 2020 to avoid the spread of COVID-19 in congregate shelters by opening the doors to motels across Vermont to all comers, with the feds footing the bill.
But amid a housing shortage that feels more dire by the day, our state reportedly may soon claim the top spot. As advocates push for solutions, In our voices, in our communities offers a glimpse into the lived experiences that underlie what appears to have become Vermont’s most pressing political debate.
Vermont Folklife, a nonprofit staffed by educators and anthropologists, teamed with the Burlington-based photographer Macaulay Lerman and the Champlain Valley Office of Economic Opportunity to produce the project. It takes the form of a one-day public art installation, with rows of lawn-sign wickets creating a portrait gallery of currently or recently homeless Vermonters and of the CVOEO employees who work with them.
On June 10, the exhibition occupied the northwest corner of the St. Albans town green, Taylor Park, from 11 a.m. to 4 p.m., overlapping with the city’s adjacent farmers market. A CVOEO representative was on hand to answer questions.



The back of each photograph displayed quotations from an interview with the subject, along with an individualized QR code linking to lengthy audio clips on the CVOEO website. Bringing earbuds helped.
Insofar as these recordings comprise the meat of the project, the physical installation – which subsequently appeared in Middlebury and Swanton over the summer, with more showings to come – functions more as an advertisement for the online exhibition than it does as a standalone show. In St. Albans, several passersby stopped to take note.
CVOEO bills In our voices as a work of “collaborative ethnography, a method that engages the individuals whose lives are being documented in both shaping the research process
and in determining how their experiences are shared with the public.”
The curators present the narratives of homelessness recorded for In our voices as monologues, but their patterns of autobiographical explication often suggest a set of off-microphone questions structuring the speakers’ reflections. At one point, a social worker named Jess stresses the organic eagerness with which her clients tend to publicize the causes of their circumstances when they ask for help, hinting that the interviewers may not have needed to do much coaxing.
“People really want to give an explanation and a story behind what their request is,” she observes. “I have seven other phone calls to make, but they all take double to ten times longer than just the provision of service, because people want to tell us the story.”
Naturally or otherwise, the accounts here take shape primarily as explanations, tending to invoke addictions or psychiatric labels. But they also draw attention to the randomness of life and its consequences in a system with few state guardrails or social supports, where a workplace accident or a falling-out between family members can change everything.
Some narratives find room for surprising digressions. One man, after mentioning his bipolar diagnosis, recounts his family history, which includes victims of the sinking of the Titanic and the architect of the historic Bronx River Highway.
Another narrates how he spent the last dollars in his checking account to buy a Greyhound ticket for his terminally ill brother in Phoenix, who wanted to die beside him on the streets of Burlington, their hometown. Ultimately, a surgeon at UVM Medical Center saved the brother’s life instead.
We also hear descriptions of the day-by-day content of homelessness. By one account, it is a matter of “only walking or trying to sleep and staying out of the cold and out of the heat. But only that. Walking, carrying things, being, having no shelter. It’s always walking.”
Six of the interviews offer first-person chronicles of this reality; the nine musings by service providers outnumber them. To the extent that the latter constitute secondhand glimpses of the phenomenon in question, the discrepancy undercuts the premise and even the title of the exhibition. But these clips allow the exhibition to address homelessness not just as an experience but as an economic and political problem.
One CVOEO worker points out that, over the course of her 25-year tenure at the agency, the welfare payments that she has disbursed – as
part of the Reach Up program for low-income parents, for instance – have not increased, despite significant inflation. Another notes that Vermont’s extreme housing shortage has rendered tenant voucher programs ineffectual.
“I listed off all of these resources that we have to be able to pay for them to have security deposits and rental assistance. And those programs, we’re not even spending them down. There’s sort of money sitting there, and it’s sitting there because we don’t have homes for people to move into. We have ample funding and resources to be able to get them into them –they just don’t exist,” she says.
Several CVOEO clients still attest to the usefulness of the agency’s offerings. And when a staffer, foreshadowing summer 2023’s sense of crisis, discusses the 2021 closure of the Holiday Inn in South Burlington and the fight to ensure that its residents would receive new placements at other hotels, she foregrounds not only the loss of housing but the loss of access to services.
“We had folks working 24/7 there. And so it was a lot of mental health support, which is the primary thing affecting folks that are homeless,” says Taylor.
But another employee acknowledges the limits of the agency’s abilities, and even of its underlying ideological apparatus.
“The strategy that we have for ending poverty is, we’ll take each of you individuals who have been unfortunate enough to find yourself in it and we’ll fix you. You’re what needs fixing,” Jess says. “I struggle with it because it often feels like, if you’re putting Band-Aids on something and sort of fixing it at that each individual level, you’re allowing it to perpetuate and continue because it’s not getting to the real triage point of forcing that larger change.”
This approach isn’t the only way, even at the level of direct assistance. In our voices also highlights the systems of mutual aid among Vermont’s homeless population.
‘It’s like people who don’t have anything taking care of other people who don’t have anything. It’s so beautiful. It’s sad that it has to happen, but it’s lovely,” says Toni from CVOEO.
Sean, who cites his struggles with alcoholism, depression, anxiety, and PTSD, is one example. Now he plans to become a peer recovery coach.
“I was in a dark place, where I thought maybe I might be better off not here anymore,” he says. “It weighs heavy on my heart seeing other people like that.”
The final days for In our voices, in our communities are Sept. 15 and Oct. 13 at the Alburgh Public Library and Burlington’s Champlain Street Park, starting at 1 p.m. and 11 a.m., respectively. Photos by Brett Yates.
Fall 2018 The Arts . 13 Fall 2023
HONORABLE MENTION
Scott
Norman Rosenthal
Randall Eliot Ingalls
Olivia Parent
Counterpoint held its annual Louise Wahl Memorial Writing Contest over the summer. Psychiatric survivors, mental health consumers, and peers submitted creative work, and the winners and runners-up split a total of $250 in prize money. Eryn Sheehan and Martha Roberts earned first place for poetry and prose, respectively.
Louise Wahl Memorial
Electroshock, Sovereignty.
The rains in December wash the snow away.

Tears from my mother run down her cheeks while words roll off my father’s tongue.
He has found another woman again. This woman spoils him and makes him happy.
He doesn’t have to yell to penetrate Mother’s
crystal armor. She is a tree in his vocal storm. His words are water and wind. His verbs and adjectives of this new woman tear violently into our world, though only the adults are talking. Perhaps Spring will come early this year.
by RANDALL ELIOT INGALLS, Johnson
December Rains Wash the Snow Away Yellow School Bus
The first time I thought about death, I was riding the bright yellow school bus. It was like any other day in sixth grade. I looked out the window, and thought about the pumpkin muffin that was sitting in my lunch box. How could I make my father happy?

I was not planning on eating my pumpkin muffin. It must’ve been there for the whole week.
Going uneaten each day. Squashed flat from what it sustained.
I wanted him to be happy. I wondered why he hated me. I forgot to do my math homework. I make my family so sad. They’d be happier if I was gone. I just want them to be happy. We passed a bridge.
Mount Misery by MARTHA
He had walked down the main road from town that November afternoon, looking for a place he had heard about some time back. As he came to where the main road intersected with Old County Road, he looked ahead off into the overgrowth, searching for a track that would take him into the woods that he could see in the distance. Not seeing anything, he headed off the road into the brush, hoping to find his way as he went.
He felt the branches of scrub and sapling brush his shoulders and catch his feet as he walked, slowly and carefully, not wanting to lose his way. He felt the town where he had lived for more than 40 years slide away behind him as he moved forward. He was headed east toward a place he had never seen, a place where he could maybe feel at home.
The woods grew denser, with larger trees, yellow birches, hemlocks, beeches, as he moved forward, without a path, but believing that before too long, his destination would be in sight.
He had heard tales of Mount Misery, guardian of some unlucky farmer’s attempt to make a holding on a New Hampshire hillside. He thought that he might find peace there in a long-abandoned wood yard with a longer-abandoned farmstead. Mount Misery’s historical reputation as a haven for bootleggers and horse thieves made it seem even more like a place of refuge.
ROBERTS, Montpelier
Ahead of him, the thicker birch and hemlock woods were beginning to thin out. Ferns and woodland grasses sprang up as he moved toward the lighter sky.
He heard the song of a red winged blackbird, sweet and tuneful. The bird sat on a low limb of a yellow birch tree and seemed to invite him closer. As he walked past the tree, the bird stopped its singing as if wary of the stranger, paused and then sang on.
The ground became hillier, and the trees grew smaller and further apart. It was rocky underfoot, and he moved more carefully to keep from stumbling. The forest ferns brushed his knees.
He came into a large open space, which had been mostly clear-cut, with log ends and scrap wood scattered around. Off to the side, due east from where he stood, the ground rose into a small mound, covered with short, spiky grass and small chunks of granite and limestone.
He felt his chest tighten, as he breathed faster with anticipation. In a small cedar tree just north of the clearing, the blackbird sang, inviting him on. He walked toward the far edge of the clearing where the mound appeared.
He thought that this might be the Mount Misery that he was seeking, the place of his longing. He walked slowly around it, trying to take in what he had imagined for so long. As he walked around the side and looked at the eastern face of the mound, he saw, to his
Refuse of stars, hemmed by laboratories. Reaching for skies, untainted. Darkness of mind.
Horror encapsulated.
Your pedestals stifle. Stay on them, we have our own.
We are more than the sum of our naming. Louder, as the sum of our living.
by SCOTT NORMAN ROSTENTHAL, Irasburg
2024 CONTEST DEADLINE: JULY 14

I imagined what it would be like to jump. What I didn’t know was the darkness in me was the same one in him. There was a reason for his actions. And no, there’s no excuse. But it gave me closure. He hated me because he hated himself. He did what he did to fill that gaping hole inside of him.
by OLIVIA PARENT, Middlebury
surprise, a small cave, halfway up the slope, partially filled with jumbled rocks. He climbed up the side of the mound, slipping a little on the damp grass and gravel. The cave was probably fifty feet off the ground, deep enough so that a person, a bear or a family of foxes could be comfortable there.
He thought that bootleggers could easily have hidden stores of whiskey in the cave and left them there for collection by traders on their way to New York State. The cave had rocks and stumps scattered on its floor, but he thought that with a little work it could still be a hideout or a place for some lost person to hole up comfortably.
He sat on the ground and leaned against the grassy slope of the mountain. The sun shone thinly on that November day. The blackbird sang, intermittently. He was weary. His shoulders sagged, his breath was slow, his chest felt heavy. His feet were tired, his eyes strained. He had left behind the people who had no time for him, a life that demanded too much, the indifferent town.
He sank back on the grass. A person could live here, he thought. A person could live in this cave, look out every morning at the sunrise, breathe easily, grow a little corn, and be free of whatever was keeping him from comfort.
The blackbird trilled again at the edge of the clearing, singing his sweet song that promised welcome and home.

Fall 2018 The Arts 14 Fall 2023
prose winner
Got Art?
Share It!
We still can have board meetings
I want the parts of me To convene over tea. The way when I was little, I would invite beings I Looked up to to sit with me and Talk over snacks and The very real pot of tea That would brew.

A place setting for Buddha, Bast, Jesus and Kali, Ganesha, Quan Yin, My ancestors were the regulars At every meeting, others Would drop in periodically.

This is one way to make space In my life for advice and I am ready to bring this Practice of mine to the forefront again.
I want to know that just because One diagnosis exists, it is not Mutually exclusive of others. I Have a scroll of diagnoses and I have multiple personalities I am Finally owning up to even though I always knew, I did not Always remember.
But I’m learning that is probably Tied to the situation and I Hear voices others don’t.
I see the chaos, horror and beauty of my own mythology Played out before me for all to see, But all they see is me.
I may be sitting quietly, so quiet and Still to protect my own serenity In the eye of the hurricane around Me playing out scenes so horrible And detailed, riddled with consequences I will not repeat here. Interspersed With the heart-wrenching beauty Of being human. Just enough to keep me From closing down completely to the Visions and voices who know me in All my wholeness that I struggle To connect to.
I don’t think my other personalities Have schizophrenic catatonia, but they
The annual membership meeting for Vermont Psychiatric Survivors is where we elect the new Board of Directors, catch up with one another, and generally have some fun! We’ll be at the Rutland Free Library from 10:30 to 2:15.
For info: Board President Sara Merrow 802-417-5468 or merrowsara@gmail.com
Are not the body’s first personality, The one born with the body. They did not ask for what I Asked the universe for as individuals. That was before the split.
When I asked for assistance, I Heard voices guiding me. I could only hear them when I Listened and they often gave Very good advice or else a statement Posed that seemed to ask me To take my own stance based on This prompt.
I tried to not let anyone know about the voices because I did Not want a label stuck to me Where everything I did afterward Would be deemed the product of Some illness. I feared losing Ownership of my own experience. Which led me to become more Paranoid than I wanted to be.
I don’t need a diagnosis Of multiple personalities. We can still have board meetings, Or tea!
My mindspace has always been My most powerful asset and Fearing other humans attempting To silence it or take that away From me distanced us to the Point I have a very hard time Claiming to be human. I’m not Sure what being Human would Feel like unless this is it.
What I am fairly certain of, is How much I want to have Conversations with my personalities Amongst ourselves. I want this To be what I need and can Receive or make happen.
My dysphoria isn’t going to Be explained away, but sees A tangential wisp of something That might make sense. I had it before the split and
POETRY winner

Now not all of us are the Same gender, but I believe Our main personality is both genders And beyond gender at the same time. Because of this I chose not to change My body to reflect how I felt.
I am glad because what I have I find beautiful, even when the Body feels borrowed and not reflecting Who I am on the inside.
Part of me is this… Part of me is that… And this is how it is now. Some of me has memories I Can access and some of me someday May show me a glimpse into Our own lives lived separate.

Till then I will continue living our Whole life, talking more and more till The parts that do not know each other Can say hello and sit with one another. Reveling in the still-brightness of our own dreams.
by ERYN SHEEHAN, Burlington
Writing
2023 FIRST PLACE
Contest
Martha Roberts Eryn Sheehan
counterpoint @ vermontpsychiatricsurvivors.org or mail to Counterpoint, The Service Building, 128 Merchants Row, Suite 606, Rutland, VT 05701 Please include name and town
Send it to us at: SAVE THE DATE October 28, 2023 Annual Meeting
The Arts . 15 Summer 2023
Vermont Psychiatric Survivors’
Short Fiction
How ‘America’s Got Talent’ Became a Psychological Catastrophe
 by RON MERKIN, Montpelier
by RON MERKIN, Montpelier
While walking on stage, John reminded himself not to tell the audience any of his stupid jokes.
Then, as he stood in front of 4,000 people, in reply to one judge’s “Are you nervous?” – the most frequently asked question before America’s Got Talent auditions – he blurted, “No, I’m John. I told you that just a second ago.”
No one laughed.
Damn it! John thought. I’m not auditioning as a comedian! So why, instead of resisting my crazy impulses, am I ruining my chances before my act begins?
“I didn’t mean to be a wise guy,” he managed. A pause, then from the same judge, “So... what will you be auditioning as?”
“A pianist,” John answered.
“OK, let’s hear it.”
But while he walked to the piano, another idea occurred to John. Instead of sitting facing the keyboard, he sat down with his back to it. With no understanding about why he was doing this, he reached his arms behind him. “How the hell can I play this way?” he shouted.

There was a little laughter. Stealing a glance at the judges, John noticed sour faces on all four of them. So, thinking they needed something more dramatic to stimulate their interest, he slammed his knuckles wherever they landed on the keyboard behind him.
This made things worse. The judges looked confused. Oh, OK, John thought, and he turned around to begin playing “Somewhere Over the Rainbow.”
Unfortunately, after he’d played two bars, one of the judges raised his hand. That was a way of ending an audition. Not having noticed, John continued playing.
“Enough!“ the judge yelled, bringing John to a stop. “I don’t know what the hell you’re trying to do up there, but it doesn’t resonate with me. ”
And before John could respond – he was searching for an expression more tactful than “Tough luck, Mister!” – the judges voted unanimously to dismiss him from the competition. So, walking off stage, John turned his back to the audience, leaned forward, and wiggled his rear end at them.
How disgusting, one of the judges thought. I’m glad we got rid of him
Unfortunately, they hadn’t.
The next afternoon John sneaked back into the auditorium and, from backstage, crept behind an old man whose singing sounded like Pavarotti. Raising both hands above him, John clasped them in an inverted V position and began improvising a ballet pirouette to the man’s left and right as the audience watched.
Mouths dropped open. Eventually, the crowd burst into laughter.
Thinking he was the target, the man stopped singing. Tears formed in his eyes. This was too much for one of the judges.
“What the hell are you doing here again?” she shouted. “And how’d you get past security?” Then, noticing the singer’s confusion – his humiliation – “I don’t mean you,” she continued. “I mean that despicable... that stupid idiot behind you!”
John stopped dancing. He didn’t say anything. A second later, two security guards walked onstage and escorted him out.
How crazy am I? John wondered. And why can’t I resist these impulses that defeat me every time I try to do anything?
Two days later John’s psychologist offered an explanation.
“You can’t deal with a fear you’ve repressed that a lack of talent may be causing your failures,” he explained, sitting across from John during their weekly therapy session. “It’s easier to blame them on the self-defeating tricks you invent than admit to the flaws you correctly or incorrectly perceive regarding abilities. This is all unconscious, of course. But suspecting that any admission of inferiority would be too devastating, you invent excuses –reasons substituting for the lack of talent you’re convinced you really have.”
What a mouthful!
John was at a loss for words. Then feeling uncomfortable, “But... how... would that explain... my impulse... to... sneak behind a singer on stage and impersonate a ballet dancer!?
John was getting angry. Dr. Harberer paused. Then, “Oh!” – and improvising a hypothesis on the spot – “That’s similar to getting a second COVID booster shot! On the chance that people who have been vaccinated might nevertheless get sick, they decide on yet another preventive measure to ensure that the first one works. In other words, should you audition someday in the future as a pianist at America’s Got Talent a second time, you want to be doubly certain that
the judges would remember your behavior – outlandish enough that it wouldn’t be easily forgotten. It’s like... a back-up dose to guarantee you’ll defeat yourself and continue avoiding a confrontation with the lack of talent you unconsciously believe you harbor.”
What nonsense.
John had never heard such… But could there be something to this? This was only his second session with Dr. Harberer.
“I... guess. I mean... I guess. I’ll have to think about that,” he managed.
Walking home a half hour later, John bumped into Jessica. A friend since adolescence, she’d become adept at reading his moods.
“I’m on my way to lunch at Starbucks,” she said. “Care to join me?”
And fifteen minutes later, seated and waiting for their order, “What’s wrong with you this time?” she asked. “I can always tell when something’s eating you.”
“Oh... it’s my psychologist” and John explained what he’d been told that morning.
A pause, an “Aha.” Then, “Your doctor told you what your motives were?”
“Of course. What else should he do?”
“Well, he might have guided you – to an insight… your own realization, in other words. He might have helped you arrive at this... this understanding... yourself!”
“Why? Is that better?”
“Of course it’s better! If you arrive at an awareness yourself, you’ll be more likely to change your behavior! His telling you what’s in your mind before you’re ready to admit to it could bring on the opposite – it could make you resistant. In that case you’re less likely to do anything about it! Don’t you understand?”
“Not entirely. Anyway, how do you know all this?”
“Everybody knows that.” Then, studying him to evaluate whether her point had sunk in, she squeezed his hand. “John, take my word for it.”
The more John thought about it, the more sense Jessica’s insight seemed to make. So, once home, John left a message on Dr Harberer’s voicemail.
“I’ve decided not to continue my psychotherapy,” he said. Wow! That actually felt good! I have to let Jessica know!
But calling her at work, he heard, “You discontinued your therapy?” She sounded incredulous.
“Well, yes. You said...”
“I didn’t mean you should stop your—” (Was this the same person who so criticized John’s psychologist an hour ago?)
“It was you who told me…” But, overwhelmed, John hung up. Only then did it occur to him that regardless of Jessica’s changed opinion, canceling his therapy validated Dr. Harberer‘s point. An unconscious fear that he was incapable of succeeding in psychotherapy was influencing him to cancel it prematurely!
Confused about what he’d done but worried
(Continued on next page)
Fall 2018 E16 Fall 2023 The Arts
Documentary Pushes Against Restraint and Seclusion in Vermont Schools
by BRETT YATES
According to the national advocacy group Lives in the Balance, Vermont’s public schools use restraint and/or seclusion upon 587 children each year. Kids with disabilities comprise the vast majority of cases.
Recently, Lives in the Balance released a free documentary, Restraint and Seclusion in Vermont Schools: Ending the Trauma, on YouTube. The Montpelier-based nonprofit All Brains Belong VT has worked to promote the 28-minute film.
Dr. Mel Houser, the latter organization’s executive director, appears in the opening scene, discussing a five-year-old Vermonter who, on their first day of school, ended up alone in a windowless, closet-sized room.
“When an adult finally opened the door, after the child had screamed themselves to exhaustion after 90 minutes, they saw that the child had removed all of their clothes, scratched up their tiny, 40-pound body, and urinated all over themselves,” she narrates. “This was their first day, their introduction to public school.”
Restraint and Seclusion in Vermont Schools gathers interviews with parents, doctors, advocates, educators, and a survivor to make the case against such practices, citing the risks they pose to children’s mental and physical health.
“Vermont has made so much effort over the past decade enhancing trauma-informed schools, trauma-informed healthcare, traumainformed everything,” Houser continues. “But being held down, immobilized, with your bodily autonomy violated by an adult with more power than you, is itself a traumatic event.”
An accompanying fact sheet by All Brains Belong points out that Vermont law permits even “supine and prone restraints, the deadliest form of restraints.”
While Vermont has not recorded any deaths by way of such tactics in its public schools, Houser asserts that 30 other states have, with asphyxiation cited as the most common cause.
Many of those states have since outlawed usage of supine and prone restraints.
The documentary casts doubt on the notion that schools use restraint and seclusion for the exclusive purpose of keeping students and teachers safe. It presents accounts where they function instead as disciplinary measures for minor offenses like running in the halls.
“Every single time he was restrained, he was not being violent. He was not being aggressive. He was not being dangerous. He was not harming himself. He was not harming somebody else,” Robyn Freener-Maguire, a parent, says of her child.
“I might have been a little upset, but locking me in that room, that made me even more upset,” a survivor recounts.
Brian Dalla Mura, a special education teacher, acknowledges that he used to employ restraint and seclusion in his classroom, just as his colleagues habitually did.
“I didn’t know there were other methods out there,” he laments.
He recalls instances of restraint as “surprisingly violent. In the trainings, it looks calm, organized, but in reality, it’s fighting, screaming, kicking, biting, punching, people out of breath, and very chaotic, loud, noisy, scary – scary for the children, scary for the teachers, scary for the witnesses. The comparison I make is it’s like somebody being arrested, and oftentimes it looks worse than what you would see the police doing on the streets.”
Dr. Ross Greene, the founder of Lives in the Balance, developed the Collaborative and
Proactive Solutions (CPS) model of intervention for kids with “challenging” behaviors. Learning of alternatives may be enough to persuade some educators to abandon seclusion and restraint.
For others, the documentary argues, legislation is probably necessary.
“We have hard data that shows it takes place in plenty of schools that have already received tons of training in multi-tiered systems of support,”
SHORT FICTION • Continued from previous page that Dr. Harberer wouldn’t take him back if he left another voicemail to indicate a change of mind, John shuffled to his piano. There he began playing the same music he’d begun before the America’s Got Talent judge interrupted him two days earlier. For some reason, remembering the incident made him laugh. In fact, the more he thought about it, the more doubled over with hysterics he became.
Hunched forward, his forehead collapsed on the keyboard: why does this remind me of the time years ago when, before the beginning of a piano lesson, my teacher tested my trust in him by challenging me to fall backward from a standing position into his arms? he wondered. My confidence that he’d catch me was meant to help free creative expression, I guess. But what if he hadn’t caught me and I’d landed on the back of my head?
Then, wait a minute, I’m the teacher now! he remembered.
Glancing at his watch he realized he had less than five minutes before his hopelessly untalented seven-year-old student would be
knocking on his door. The kid’s mother always accompanied him. In fact, every time John glanced in her direction, he couldn’t help noticing that she seemed to be flirting with him.
This discomforted John. But his hint at the beginning of the last week’s lesson – “Should you have some shopping or other chore to do, don’t feel obligated to remain here for the entire lesson” – met only with a smile. All things considered, he would have liked to have canceled these lessons. But so many of his students were dropping out lately. He had no idea why. And John needed the money.
Around halfway through the kid’s lesson –a rendition of the music he’d been assigned to practice the week before - John felt something tapping his shoulder.
Waking up, he couldn’t believe what had happened. “Did I... fall asleep?” he asked.
“I’m afraid so.” Smiling, Leon’s mother leaned into him.
“It’s because of this chair. Too comfortable!” Pulling it away from its place a foot or so left of the piano, John exchanged the cushy seat for a
says Kirsten Murphy, executive director of the Vermont Developmental Disabilities Council.
In 2022, the Harwood Unified Union School District in Washington County garnered critical media attention for its heavy reliance on restraint and seclusion, thanks to whistleblowing by Dalla Mura, a former employee. It changed its internal policies this spring.
Meanwhile, in January, Rep. Theresa Wood introduced a bill to restrict the use of restraint and seclusion in schools throughout Vermont. The bill died after five hearings by the House Committee on Education.

Restraint and Seclusion in Vermont Schools seems designed to function, above all else, as an extended compilation of testimony for legislators, with background music as the only aesthetic flourish. An unbroken stream of somewhat jaggedly spliced interviews, without relief from intertitles or B-roll, it may not possess enough easy digestibility to appear even on local TV.
But with any luck, it’ll find its intended audience online before the next legislative session. Go to allbrainsbelong.org/end-thetrauma/ to access the YouTube upload.
small, barren, uncomfortable folding chair. This he dragged across the room.
“I’m sorry,” he mumbled.
“You’re sorry! I thought you were John,” Isabel answered.
“Where did you hear that joke?”
“On television. I watched your audition for America’s Got Talent last week.”
God, if John thought he’d blushed all the times this woman had flirted with him...
Throughout all this, John’s student had not stopped “playing.”
What John did next was too unprecedented – too shocking – to publish. Suffice to say that instead of admitting we’re lacking in inspiration, some writers struggling with a story’s end may leave it hanging so the rejection notice expected from editors to whom the story was submitted can be blamed on material purposely omitted, not on any lack of talent...
Ron Merkin is a retired psychiatric social worker, journalist, fiction writer and entertainer.
Fall 2018 The Arts 17 Fall 2023
Dalla Murra recalls instances of restraint as “surprisingly violent.”
Voices from Mad Pride 2023

Journalist Robert Whitaker and nonprofit director Sera Davidow traveled to Burlington in July for Vermont Mad Pride, where they served as the keynote speakers. Whitaker, the bestselling author of Anatomy of an Epidemic and the founder of the website Mad in America, spoke about fighting against psychiatry’s “medical model,” and Davidow, whose Wildflower Alliance opened Massachusetts’s first peer-run respite, highlighted concerns of competency and confidentiality at the 988 Suicide & Crisis Lifeline. Excerpts follow. Photos by Brett Yates.
The psychiatric survivor movement is a civil rights movement. And any civil rights movement is a benefit to everyone in society. And that’s what you’re doing here today.

It’s not just fighting for people labeled mad. But it’s also a fight for a better society, a more just society. ...
Our society has organized itself, ever since particularly 1980, around what psychiatry calls a medical model. It’s really a disease model.
And that model is that problems arise within the head of the individual, right? So we heard about chemical imbalances. And we even hear that those things are chronic. If you have something wrong inside your head, you need to be fixed – medications or whatever it might be.
But that is a conception of human beings. It’s so out of odds with everything we know about human beings, but it is this conception that the problem arises only within the individual, and not from the individual’s environment, the environment that we create for people, the experiences.
And it gives society sort of a free pass. We don’t have to do anything to make our society better – about poverty, homelessness, good jobs, all those things – because we say if someone’s struggling with their mind, the problem is in the individual.
And the other problem with that idea is, if you say there’s people here who are mentally ill, and there’s people here who are normal, what happens? What happens with that thought? It encourages stigmatization. It encourages the erosion of civil rights. It makes people the other.
So rather than try to fix the individual, we need an area that says, we don’t know why people are struggling, even with extreme states. We really don’t.
There’s many, many different pathways to extreme states and difficulties. Start with that humility.
And then the second thing is, what do we know about human beings? A) Human beings are responsive to their environment. B) We’re not steady-state creatures.
You know what I mean by that? If you’re depressed one day, or if you’re manic one day, or if you’re having psychotic thoughts one day, it doesn’t mean you’re going to do that for the rest of your life.
We need to celebrate people. We need to celebrate different mind states. And we also have to recognize this: to suffer is to be human. To struggle is to be human. …
Right now, our society still is stuck with that other narrative, which is completely ahistorical. I’m not religious, but go read the Bible. Read the Old Testament. Does that sound like people that are just marching through life all nice and content? Not at all. Go read your Shakespeare. Go read those characters. …
So we run Mad in America, and I’m happy to say, Mad in America now gets about 6 million visitors a year. And here’s the most important thing now: we have 11 affiliates in 11 countries, and we’ve got four more about to be launched. …
What you will see if you come to Mad in America, the website, is a big test narrative for changing how we think about psychiatric services. I’m really proud about what I’m going to say now: the Royal College of Psychiatry had its annual meeting last week. And they named who are the people who are criticizing what we’re doing the most.
And there I was on the web. I’m on one of the slides. Which means they were recognizing that there’s a real challenge to the narrative they have.
SERA DAVIDOW
Part of what I want to talk to you about today is this idea that the thing we most need to do with people like me is to increase access to mental health services.
When I say “people like me,” what I mean is people who have psychiatric histories and in particular some of us who sometimes still bump into those edges of our existence. Like me –sometimes I wake up in a day and I’m like, “Do I really have to brush my hair today and brush my teeth today and do that again and again and again and again?” …
And if you think about access now, what do they mean when they say increased access? What does that look like recently?
Now, I could talk to you about Mental Health First Aid. … Side note about Mental Health First Aid: they say they have all this proof. If you aren’t already aware, the vast majority of the proof they have, the evidence that it works, just says that, if you attend a Mental Health First Aid training, you leave the Mental Health First Aid training more familiar with the Mental Health First Aid training. It doesn’t actually say it works for the most part.
So bear that in mind. But what I actually want to talk to you about is 988.
So I’ve been secret-shopping 988. Some people are freaked out by that. They’re like, “You need to leave it alone so the real people who are calling for real reasons can get through.” And I’m like, I am calling for a real reason: I need to know if it’s a threat to me and my community.
I’ve done this now five times, and when I say “call,” I really mean text. I’ve done the text so far. Now, I have spoken to Sue Ann, Simone, Taylor, Gretchen, and Jen.
Sue Ann taught me something important when she took four minutes every time to reply. That’s when I learned they can text with up to ten people at a time. Simone probably shouldn’t be counted because when she asked me how I was doing and I said, “I’m feeling pretty hopeless,” the call ended.
And then there was Taylor. Taylor was actually the best of the bunch. She was pretty good. She tried really hard, and she even made me my very own safety plan based on what I said
would work for me. I’m kind of condescending, but I could tell she was really, really trying. So I kind of appreciated that call.
But then we got to Gretchen. So with Gretchen, I was talking about self-injury, which I have a long history of myself. And I said I was self-injuring then, and she said, “Can we step away from the things we’re using to self-injure, so we can talk?”
And I said, “Gretchen, are you self-injuring too? You can step away, but I’m not going to.”
After that call, there was Jen. Jen was the most recent. Jen was just about a month ago. And in fairness, I pushed the limits with Jen. I did say I was self-injuring, and I also said I was suicidal. And she asked me again if I would stop self-injury.
This is actually not a helpful thing, by the way.
Never in the history of time has it been helpful to me to just assume it’s bad and try to get me to stop. It’s one of the things that keeps me alive. And I tried to explain that to Jen, so she’d stop. And she sort of did. She asked me if I was bleeding and I said yes.
She said, “Do you need medical care?” I said, “No, I’m fine.” And she let it go, more or less.
And then I said I was really too tired to continue the call. And she said okay. And the last thing she said to me was, “Call back anytime. We’re here 24/7.” So I went home, and two hours later, there were three police cars outside of my house and a cop at my door knocking.
Now, let’s unpack this for just a minute. Had I actually been trying to kill myself, two hours later, I’m not sure what they would have accomplished. But I can tell you, what they did accomplish, in this situation, was really freaking out my 11-year-old. …
So this is what we’re talking about when we’re talking about increased access. It is not what we need. We know here what we need.
I’m so grateful when I hear that there’s a soteria in Vermont. I’m so sad to hear that it’s the only one. We’ve lost the California one. We’ve lost the Alaska one.
We’ve lost some of that progress, and how do we get that back? That’s the conversation I want to be having, not this idea of access.
COMMENTARY 18 Fall 2018
Fall 2023 COMMENTARY
ROBERT WHITAKER
Some Thoughts on Independent Living
By MORGAN W. BROWN
Firstly: what is defined as independent living?
According to The Philosophy of Independent Living from the Westchester Independent Living Center (wilc.org), "Independent Living means being able to exercise the greatest degree of choice about where you live, with whom you live, how you live, where you work, and how you use your time. It means participating in community life and pursuing activities of your own choosing."
Years ago (circa either late 1995 or early 1996), after having been appointed as a member of the board of commissioners of the local housing authority, I attended an open house event for a newly renovated building in the area that would serve as an assisted living facility as well as provide level-three licensed nursing care to residents in need of such.
During the event, due to assumptions they had previously made about my activism and advocacy concerning disability rights and related matters, someone mentioned having been surprised by my being there because of the nature of the facility and so on.
In response, I basically explained my belief concerning independent living as not being defined as an all-or-nothing approach and that one should not have to do everything on one's own in order to live independently.
Furthermore, I stated that, to my way of thinking, independent living is defined instead by one being in charge of one's own decisionmaking concerning how and where one wants to
live as well as what one might need and require in terms of any assistance, services and support to be received (as well as whether one chooses to receive such or not).
This means that, at least as I have come to understand it and concerning all members of the community, there are many different versions of living independently, and other than being a location within a community of one's own choosing, it is not necessarily about where or rather in what setting, but more importantly
do everything on one's own, then the person is unable to live independently and should be sent to an institutional facility where decisions about their care and lives are strictly imposed upon them, oftentimes without their prior informed consent.
Ironically, these attitudes, beliefs and judgments are made by those who would impose something on others that they would more than likely not wish to have imposed upon themselves in such circumstances. When it comes to someone else, however, they do not allow for certain essential considerations to be determined and made.
Those essential considerations include the fact that there are usually other viable and more humane as well as less costly approaches and options in need of being explored rather than what is an ableist, institutional, all-or-nothing mindset and approach.
about how decisions are made and reached as well as who makes the decisions about one's own life. It is not a one-size-fits-all proposition.
In my opinion and speaking for myself only, independent living should not merely begin or end within one's own home or housing situation; but, rather, one should be able to live independently wherever and in whatever preferred home-like setting one resides within the community. The same goes for those who are living unhoused (aka living homeless; i.e., without permanent housing).
Although certain attitudes and beliefs as well as things have changed somewhat within various circles of society since then, unfortunately, there is still much that hasn't.
By way of recent observation, apparently, there are still those – including in positions of power – who seem to believe that if one is not able to
The most important element of which is keeping in mind that the person should always retain the right to make their own decisions (or, otherwise, having enacted an advance directive and appointed someone to act on their behalf to do so should they be found to lack the capacity at some point in the future) and not have decisions imposed upon them by others, no matter how well-meaning.
Indeed, as a society, we still seem to have a long way to go. In closing, when thinking about others in need in these types of circumstances, the question to keep in mind is what would one want for either oneself or a dear member of one's family.
Morgan Brown formerly lived without permanent housing for several years and currently resides permanently housed within Central Vermont. He previously served on the Montpelier Homelessness Task Force.

Editorial: Legislators Should Do Useful Things
Watching the General Assembly’s last-minute scramble in June to figure out how not to kick 2,000 homeless Vermonters out of the motels sheltering them, I thought about all the time that legislators had spent during the winter and spring deliberating over bills that were, from a practical standpoint, essentially pointless.
Until a media frenzy and an outpouring of citizen concern converged on Montpelier in the closing weeks of the legislative session, a significant swath of our elected representatives seemed largely unaware that they’d set a course for crisis. As recently as March, they’d determined to kick the can down the road, changing the termination date for the pandemicera General Assistance Emergency Housing Program from early spring to early summer, but that vote hadn’t come with a plan for what the state should do when the end finally arrived.
By the time the legislature reconvened for June’s veto review session, the Democrats’ budget had become a public relations disaster, and following an unsuccessful attempt to blame Governor Scott, the party had to find a way to save face. Ultimately, Scott helped.
A hastily crafted amendment to H.171, which allocated cash reserves to cover continued motel placements for families that met special criteria until April 2024, may have pacified some distressed voters. It did nothing, however, for the 800 Vermonters whom the state had already evicted by that point.
How did this happen? If legislators can’t devise a reasonable process for winding down a program sustained by temporary federal dollars instead of simply pulling the rug out from under its beneficiaries, what do they do all day?
As a Counterpoint reporter, I follow bills related to mental health. Obviously, these comprise a small subset of the proposed legislation that comes before the General Assembly. But they offer a glimpse at a bigger picture, where Vermont’s part-time lawmakers seem to have few ideas of their own, and in that void, the pet projects of small, well-organized interests manage to command an unwholesome share of the precious hours in which our legislators might otherwise attempt to address the major problems of our state.
These bills are not necessarily sinister. Inevitably, while transacting the business of the people, legislators sometimes have to wade into esoteric topics that don’t cross the average Vermonter’s mind or, in the normal course of events, their own.
Understandably, they may (without a bit of corruption) look to someone else for expertise. But surprisingly often, advocacy groups –especially when they represent institutions or individuals rather than genuine political movements – suggest tweaks to the more obscure sections of state statute that fail, in fairly self-evident ways, to present effective solutions to the narrow problems they purport to address.
Trade associations, for example, have their own internal politics, driven by the concerns of members whose problems may not, in the end, be resolvable via rewrites of the laws that pertain specifically to their sector. Their policy analysts have no choice but to seek solutions within that prism, but legislators, at least theoretically, can recognize in lobbyists’ complaints manifestations of larger social failures and strive to resolve them upstream.
One upstream problem, which affects nearly all the rest, is, of course, housing. Others have more specialized dimensions, but there’s not always a specialized solution at hand.
Consider, for example, S.36, which the legislature passed in May.
With this superficially rational bill, the Vermont Association of Hospitals and Health Systems proposed to amend the third section of the Vermont Rules of Criminal Procedure to include assaults against healthcare workers among the misdemeanor offenses for which a police officer can make an arrest without obtaining a warrant or witnessing the incident directly.
For good reason, Vermont’s hospitals want to defend their staff, particularly during a workforce shortage. Nurses offered startling, painful accounts of attacks by patients. But before the bill’s arrival, Rule 3 had already specified that police could arrest a suspect for (Continued on next page)
COMMENTARY . 19 Fall 2018
COMMENTARY. Fall 2023
It is not necessarily about where or in what setting, but more importantly about how decisions are made.
LEGISLATORS • Continued from page 19 a nonwitnessed “simple assault” against any person in any setting.
The added redundancy aimed, at best, to mark a point of emphasis – to send a signal that emergency department nurses, in particular, require protection amid a reported uptick in violence, and that law enforcement has the power to offer that protection.
But in testimony before the legislature, police made clear that, if they hesitated to arrest ED patients, it was not because they were uncertain about their legal right to do so. On the contrary, their procedures owed to a reasonable and – as long as lawsuits still exist – seemingly immovable reluctance to take patients with potentially pressing medical needs into custody and thereby deny them possibly life-saving care.
This reluctance would likely extend just as much or more to a pair of lower-level offenses that S.36 also added to Rule 3: threats against a hospital employee and disorderly conduct inside a hospital. Vermont Defender General Matthew Valerio argued that, by other names, these crimes, too, already fell within the list of arrestable misdemeanors.
“When it comes down to granting more authority to law enforcement than they already have right now, this bill doesn’t do anything,” he told legislators. “If you’re in healthcare and this bill gets passed, they should not anticipate that they have any more protection than they already have right now.”
Lawmakers listened politely to this testimony and continued to move forward, having already apparently determined that they would do what they could to appease VAHHS, which, for its own part, had evidently determined that it had to do something to appease its own distressed members. The final legislation included a provision preventing police from taking patients into custody if they still need medical evaluation or stabilization – in other words, it codified the existing practice as law, fully defeating the original purpose of the bill, which was to boost arrests.
2023’s pair of forensic mental health bills demonstrated a similar dynamic. Over the years, a handful of violent crimes attributed by police to perpetrators with psychiatric diagnoses –and especially a horrifying 2021 murder in Bennington – had generated a small but militant demand for the state to find new ways to restrain and punish alleged criminals within the mental health system.
When a defendant enters the custody of the Commissioner of Mental Health because a criminal court has found them incompetent to stand trial or not guilty by reason of insanity, there’s only so much the state can do without violating the Constitution. After all, the person in question doesn’t actually have a criminal conviction on their record.
Still, the topic has managed to keep the legislature busy.
S.89 created Vermont’s first segregated facility for psychiatric patients committed by a criminal court. Its sponsors never firmly articulated a rationale for why forensic patients should no longer mingle with patients committed by a civil court, who receive similar or identical care, but the change aimed to have the effect of marking them, for the possible satisfaction of
victims’ family members, as a singularly tainted subgroup.
Without a new building on the horizon, the creation of the “new” forensic facility would itself, under this legislation, amount to little more than a metaphor. An existing nine-bed wing of the locked Vermont Psychiatric Care Hospital, which already houses the patient population under discussion, would receive redesignation as a secure residential facility for forensic patients.
The state would save some money by reducing its quantity of level-one psychiatric beds, but in doing so, it would degrade its own definition of “step-down care,” which in this case would include restraint and seclusion. The patients themselves might hardly notice their own “transfers.”
A related bill, S.91, decoupled competency determinations from sanity evaluations. Until
demands for crackdowns. A legislator with a substantive, independent political vision might possess their own, more legible theory of how to work toward a less violent society. But in Vermont, many appear happy enough simply to look important while somebody else, it seems, instructs them how to vote on bills that don’t obviously concern them very much.
But what happens when, at the crucial juncture, no one is available to tell our lawmakers what to do? This year, they had to make hard decisions about how to wrap up the emergency housing program. They couldn’t ask a workgroup to figure it out for them next year, and the homeless don’t have lobbyists to draft policy on their behalf.
A logical plan would have ended admissions to the pandemic-era program – which, without the legislature seeming to notice it, persisted even after the state’s first round of evictions – with enough cash still on hand to sustain remaining beneficiaries for a period long enough to accommodate their transitions to permanent housing, even in inevitable protracted cases.
recently, upon a judge’s say-so, the Department of Mental Health examined both questions – that of the defendant’s state of mind at the time of the alleged offense (sanity) and that of their ongoing ability or inability to stand trial (competency) – simultaneously.
Following S.91’s passage, DMH’s screening will consider only competency, leaving to the defendant the responsibility to raise the question of sanity if their legal counsel deems it relevant. This move intends to demonstrate to public safety advocates that the state has shed its eagerness to let dangerous criminals permanently off the hook by freely offering diagnoses of insanity.
In reality, S.91 only shifts the expense of the sanity evaluation from one part of the state to another – specifically, to the Office of the Defender General, which of course knows that, in order to represent its clients’ best interests, it must always secure a prompt sanity evaluation, before the loss of any evidence. The court may no longer order DMH to do it, but it’ll happen all the same, and still at the public’s expense.
Together, S.36, S.89, and S.91 required a total of 62 committee hearings before their passage. During this time, the less diligent legislators nodded along, and the more diligent ones worked hard (with some success) to make the bills slightly less bad without visibly questioning the seemingly predetermined imperative to advance them irrespective of their merits.
All three bills constituted reactions to the specter of violence in our society – the fear of which all too often turns psychiatrically labeled people into scapegoats and boogeymen in the popular imagination, prompting periodic
With a little forethought, legislators might have realized the implications of what they’d created in 2020: a change whereupon a full return to the state’s pre-pandemic shelter policy could never happen without some significant pain. Opening the state’s motels to all comers at the start of the pandemic revealed a vast population of previously uncounted homeless Vermonters, or it created an all-new one, depending on whom you ask. But in either case, the state assumed a significant responsibility, and a mass eviction should’ve always remained out of the question.
A proactive government, at that point, might have bought some of the motels for the purpose of creating fiscally sustainable permanent shelters. At market price, they would’ve cost less than a few years’ worth of vouchers.
With even more forethought, legislators might have undertaken the work begun by S.100, the HOME Act, a few decades ago, before the housing crunch got so dire as to turn homelessness into the massive problem it’s become today. We shouldn’t have needed to create a desperate shortage of homes for lawmakers to realize the necessity of permitting new construction and denser living arrangements – to say nothing of more radical approaches to housing production.
Instead, the legislature displayed so little forethought that, even now, we don’t really know what will happen to the 2,000 Vermonters whom the veto session supposedly rescued. The sloppy amendment to H.171 ostensibly ensures that they’ll keep their motel placements until April – unless they fail to “participate in the coordinated entry and case management processes” or to “engage in their own search for alternative housing options” or to avoid “misconduct,” according to unspecified criteria to be enforced by an unspecified entity.

The amendment also gives the Agency of Human Services the right to shift anyone in the program to a congregate shelter – whose limit on lengths of stay may number in days or weeks, not in months – at any point.
Even so, according to the media, the crisis is over. The people who created it, however, are here to stay.
.COMMENTARY COMMENTARY 20 Fall 2023 20
Send your commentary or letter to the editor to: Counterpoint, The Service Building, 128 Merchants Row, Suite 606, Rutland, VT 05701, or to counterpoint@vermontpsychiatricsurvivors.org Please include name, address and email.
Readers Say No to ED Arrests
Twenty-two of 24 respondents (91.7%) voted no on the summer Counterpoint poll: “If you threaten emergency department staff while in a mental health crisis, should you be arrested for a crime?”
The question related to legislation introduced in Montpelier in January with the intention of encouraging police officers to take emergency department patients into custody if they threaten or assault workers or engage in disorderly conduct inside hospitals, even if law enforcement hasn’t witnessed the alleged offense. The bill passed despite concerns that it would serve to criminalize Vermonters seeking treatment during mental health crises.
Eleven respondents submitted anonymous comments, reflecting both sides of the issue, including the following:
• “If your actions or words are truly a part of and because of a mental health emergency, then it should be treated as a symptom, just as symptoms are treated for any other health emergency.”
• “When in a crisis, I have found that the way I’ve been treated in the ED was horrid and thus lashing out and protecting oneself is survival instinct and should not be punished. What happened to compassion? If they back you into a corner, you will come out fighting! People deserve to be treated with Respect, Compassion and Dignity and that is sorely lacking in VT hospitals!”
• “It would depend on the situation. People in the ER [may be] distressed, upset, may be frightened, may have acute symptoms that they can’t control, may have been mistreated there, may not understand what is going on. A more humane approach would be to try to calm the person, find a quiet place for them to be, reassure them, find some support. Arresting someone in this situation is an overreaction to someone’s distress and fear, and is not going to make anything better.”
• “The crime occurs when you go hands-on and assault the staff.”

• “The essential premise of mental health laws is that a person perceived to be in a mental health crisis must be forced into a process that assesses the level of danger present. To charge
someone in this type of situation with a crime because they may appear threatening to others is deeply flawed and damaging because:
“1. The initial detention for evaluation phase is based on an allegation that this person might be dangerous in some way, but regardless of whether or not the person actually poses any real danger to themselves or others they are being stripped of their rights based on the opinion of someone else. If the system was not designed in a way that acknowledges, and empathizes, with the ways in which someone in that situation would feel threatened and/or desperate then the system was not designed to care for them. And if that is the case then legislators must publicly acknowledge that.
“2. If it is believed that the person being forced into this process is impaired in a way that limits their understanding of what’s going on then that must include an acknowledgement that a confused person who feels threatened may respond in ways that seem threatening to others. If the system is not designed in a way that acknowledges this then the assessment process is not actually designed to understand the
“If you threaten emergency department staff while in a mental health crisis, should you be arrested for a crime?”
what you perceive you need, then interest would be warranted.”
• “Y’all, we can’t be threatening or assaulting peoples. They be trying they best to help us in our struggle.”
The fall poll – “Do high housing costs or mental health challenges play a greater role in creating homelessness?” – asks readers to weigh competing theories behind a widely discussed problem in Vermont, where, officially, a staggering 43 residents out of every 10,000 are unhoused (compared to 18 nationally).
person being forced into it. And if that is the case then legislators must publicly acknowledge that this system was not designed for compassion, or care, it was designed for detention.”
• “If you are truly in a mental health crisis and have no mental awareness (valid) of your actions, I believe getting you the mental health that you need would be more beneficial than arresting you for something you did not, or would not, have intentionally done in a sane mind. That being said, if you are there for a perceived mental health crisis, and are fully aware of your actions, because you’re not getting
Hoping to help, advocates of various stripes have urged legislators to eliminate regulatory barriers for the construction of new market-rate housing, to invest additional public dollars into affordable housing, and to improve social services (including mental health counseling) for individuals who struggle to find and retain housing.
Researchers have established a correlation between psychiatric diagnoses and incidences of homelessness, but causation – not to mention its direction – is more difficult to prove. Other scholars have focused on the relationship of homelessness to home prices and rental vacancy rates. Of the latter, Vermont has the second lowest in the country.
As always, Counterpoint wants to know what you think.
21 COMMENTARY. Fall 2023
NO 91.7% YES 8.3% Counterpoint Opinion Poll Do high housing costs or mental health challenges play a greater role in creating homelessness? Results of the poll will be published in the next issue of Counterpoint. OR by going to www.vermontpsychiatricsurvivors.org/counterpoint/ QUESTION: VOTE by scanning this onto your mobile phone:
Burlington Pods Offer Lessons
by BRETT YATES
The Elmwood Emergency Shelter Community, which opened in February, accommodates up to 35 adults in small, modular structures on a former parking lot just outside downtown Burlington. Getting the project off the ground wasn’t easy, according to city officials, who discussed some of the challenges of development and operations with the Montpelier Homelessness Task Force in June.
The City of Montpelier created the Task Force in 2019. Chaired by Another Way Executive Director Ken Russell, it also includes Vermont Psychiatric Survivors Vice President Zack Hughes. At the time of the City of Burlington’s public presentation at the Kellogg-Hubbard Library, it hadn’t identified a potential site or funding source for a pod-based shelter in Montpelier.
The first of its kind in Vermont, Burlington’s 30-unit Elmwood facility makes use of flat-packed, rapidly assembled pods, manufactured primarily by the Washington-based company Pallet. By its own count, Pallet has, across the country, produced more than 100 “transitional shelter villages” since 2016.
Burlington’s commitment to building one of its own emerged out of the controversy around its 2021 decision to shut down the unsanctioned Sears Lane encampment in the city’s South End, in the telling of Assistant Director for Community Works Samantha Dunn.

“People felt like that was a community that they had in place,” Dunn said. “We were able to get them into shelter, but it was recognized that there was a need for additional shelter within the City of Burlington.”
In December of that year, Mayor Miro Weinberger publicized a 10-point “action plan” to address homelessness, which proposed an investment in “approximately 30 shelter pods and related infrastructure to create a new lowbarrier facility for 2022.” The City Council approved funding the following February. Opening day didn’t arrive during the calendar year as planned, but it came close.
Burlington’s federal stimulus from the American Rescue Plan Act covered most of the $1.821 million price of development. The 64-square-foot pods themselves – which have electricity, heat, and air conditioning, but not running water – cost $414,778 in total, including five relatively deluxe, custom-made units from Up End This in Johnson, Vermont.
Another $362,731 brought two larger prefabricated buildings to the site. One operates as a community center with a laundry room and a dining room; the other houses six full bathrooms.
Sewer and water connections and electrical trenching for the city-owned site cost $190,563. The Vermont Agency of Natural Resources chipped in $61,750 for the removal of an underground petroleum tank, but the total expense of the job doubled that figure.
Residents can stay for up to 180 days. Dunn hypothesized that, if necessary, staff could allow a resident to circumvent the limit by transferring them to a new pod, which would, theoretically, qualify as a new stay.
The emergency shelter will occupy the lot on Elmwood Avenue for three years. The pods
themselves have a much longer usable life, and Dunn expects Burlington to find ways to repurpose them once the shelter has closed.
Dunn characterized the facility’s temporariness as “part of a permitting strategy, quite honestly. It was political.”
So, too, was its size: the half-acre site could have accommodated more than 35 placements, a number that Dunn “would have increased” if not for the imperative to win (and hold onto) discretionary approvals from bodies like Burlington’s Development Review Board and Public Works Commission.
“We spent a lot of time having community meetings,” Dunn said. “We had contentious DRB hearings. And the amount of time required to sort of get the community comfortable enough not to appeal the permit and just make people
“The state really wanted to see how does this model work,” she continued. “There was a lot of pressure put on the Champlain Housing Trust to step into this role, and they have kind of said, ‘This is what it costs for us to do it.’ And they’re doing a phenomenal job.”
In Dunn’s view, the privacy of shelter pods offers an alternative to congregate shelters. At the Kellogg-Hubbard Library, a member of the audience noted that, during their own period of homelessness, they’d tried to avoid the latter, where the constant presence of strangers “would drive any sane person batty, if not insane,” as they put it.
At the same time, the Elmwood shelter aims to create a sense of community. A $9,900 “placemaking” grant from the Vermont Community Foundation has helped make the built environment a little friendlier.
Burlington-based artist Liza Phillip designed custom murals for the site. “She’s starting them, and then some of the guests at the site are going to help finish them,” Dunn explained.

The city has also installed garden beds, but in June, residents hadn’t yet stepped forward to tend them.
“I’m going to buy the plants tomorrow,” Dunn said. “The site manager put up a sign to start a garden club. She said no one came. So when I was on site, I had to line all these things with fabric, and we moved the dirt. I think people will [come]. We just need to get the stuff there.”
understand what it was going to be like – that was a very important thing to consider when you’re thinking about the site.”
The shelter’s permit requires 24/7/365 staffing, including two overnight security guards, who account for $417,305 of the $1,368,757 annual operating budget. During the daytime, the Champlain Housing Trust operates the facility, which, without a commercial kitchen (or, for that matter, a kitchen for the residents’ use), serves three meals daily, premade and delivered by Feeding Chittenden.
By Dunn’s calculation, the operational costs break down, on a per-person basis, to the
A person in the crowd asked Dunn whether, in planning the facility, Burlington had involved “people with lived experience” at “every step in the process.”
Dunn replied that the city had solicited input during the development of the operations policy and in the site design, leading to modifications in, for example, the alignment of the pods’ front doors. But she declined to affirm start-tofinish participation, seemingly indicating that homeless Burlingtonians may not have weighed in on the decision to pursue the project in the first place.
Dunn’s slides included a list of “lessons learned” for other cities that might want to build a pod-based emergency shelter. The first one was: “You can do it!”
“It was a little bit of luck that I was hired. My workload hadn’t been determined, and I had development experience,” Dunn recollected. “I think you could hire a consultant, but someone’s really got to drive it. It’s not going to build itself.”
Until the first severe cold spell, she’d worried that the pods, which have little insulation, wouldn’t always stay warm. But the electric heaters proved powerful enough, without unmanageable energy bills.
equivalent of “a motel night” by way of the pandemic-era General Assistance Emergency Housing Program. In this case, it includes services. Per Dunn, the state foots “the majority” of the bill.
“It’s much more expensive than we were anticipating,” she acknowledged. “The city had a very challenging time trying to get someone to operate the site, and there was a very uncomfortable meeting between the city and the state.”
Slides from Special Assistant to End Homelessness Sarah Russell encouraged future shelter operators to adopt some of the policies that seemed to have helped in Burlington, like allowing couples to stay together in a single pod, permitting pets, and encouraging residents to accept case management but not mandating it.
As of June 30, according to city data, the Elmwood Emergency Shelter Community had sheltered 49 people, connecting 43 of them to case management via the Champlain Valley Office of Economic Opportunity.
Thirteen had exited the shelter involuntarily. Two had exited to permanent housing.
NEWS 22 Fall 2018 E COMMENTARY 22 NEWS . Fall 2023
Visitors can’t enter the fenced-in shelter (Counterpoint photo).
Art by Liza Phillip at the shelter (Counterpoint photo)
ISPS-US Gets Ready for Annual Conference
The American chapter of the International Society for Psychological and Social Approaches to Psychosis received a record number of proposals this year for its annual conference, according to ISPS-US Executive Director Leah Giorgini.

The conference, titled Humanity in Solidarity, will take place in person and online from Oct. 27 to 29. Each morning will open with a plenary session featuring one of three keynote speakers: Pat Deegan, Vesper Moore, and Willard Ashley Sr.
Deegan became a disability rights activist after receiving a diagnosis of schizophrenia during adolescence. Giorgini billed him as “a legend in the field” who has “done a lot of work with early intervention in New York State.”
Moore “is an indigenous person with lived experience from the LGBT+ community,” and Ashley Sr. “is a psychoanalyst, a reverend, and also a racial justice organizer,” by Giorgini’s description.
Among the panels that will follow the plenary sessions, Giorgini highlighted one centered on “spiritual understandings of extreme states. “Family panels” will feature conversations between people who identify as having experienced psychosis and their parent or sibling.
After lunch, concurrent “breakout spaces” will cover “a wide variety of topics,” from the war in Ukraine to “social justice to just simply sharing a person’s lived experience,” per Giorgini.
The overarching goal, according to promotional materials, is to work toward “understanding our shared journey through psychosis,” which in turn will help attendees “foster and create systems of care in which human rights and full personhood are held central, replacing approaches that ‘other’ and
reduce experiences to labels of deficit and disease.”
Based on information from ticket sales thus far, Giorgini expects to see among attendees a “50/50” split between clinicians and service providers on one side and mental health consumers, psychiatric survivors, and their families on the other. This, in her view, is “the whole point” of the conference.
“We don’t think that one group working alone is going to move the needle. We need to have those conversations together to expand people’s understanding and really get a realistic idea of how to push the system forward or to tear down
term ‘psychosis,’” Giorgini said, “because it’s medicalized language that’s often used to harm people. Yet it’s still a word that a lot of people use because it’s commonly understood to describe an array of experiences, like hearing voices or experiencing what could be termed delusions or hallucinations. It’s a way for us to talk together about something.”
The US chapter appears to be growing. Its most recent annual report cited a 30% increase in members in 2022 alone, bringing the total to 246. Legally registered in Pennsylvania, ISPSUS operates as a remote organization by way of Zoom and email for most of the year.
Virtual discussions take place via monthly webinars (which non-members can also attend for free), at book clubs, and on advocacy committees, which recently have sought to push back on attempts in New York and California to use coercive psychiatry as a means to combat homelessness.
Giorgini called the annual conference “our main activity of the year.” Registrants will convene at the University of Delaware in Newark, DE, or watch recordings at home. Last year, ISPS-US counted 328 attendees.
the system and rebuild it,” she said.
Founded in 1956 by Swiss psychiatrists looking for humane alternatives to asylums, ISPS originally stood for the International Symposium for the Psychotherapy of Schizophrenia. It now has chapters all over Europe and two in Asia, plus Australia and New Zealand. The one in the United States formed in 1998.
Its mission and membership evolved over time.
“What started out as very psychoanalyticalbased opened up to different professions, to different ways of understanding and working through extreme states,” Giorgini described. “It includes not just talking therapies, but art therapies, occupational therapies, peer support, the hearing voices movement, approaches that morphed into social justice movements, philosophy, spirituality.”
Although it dropped the term “schizophrenia,” the organization’s name still stirs internal debate.
“Lots of people within ISPS reject the
ISPS-US offers reduced prices and scholarships for qualifying ticket buyers, including those with “lived experience,” or free entrance with a six-hour volunteer commitment.
Dr. Martin Cosgro, a California-based psychologist who has attended the annual conference “many” times, praised its “warm and supportive environment” and “opportunities for meaningful dialogue.”
“Old friends reconnect, newcomers are welcomed, and generally there’s a feeling of optimism about these issues, knowing that there are others with similar beliefs and visions of a better future,” he said.
Another previous attendee, Fehmida Iyer Visnagarwala, identified as a psychiatric survivor living overseas.
“It helped me immensely to connect with people who think similarly and to get the support which is not forthcoming normally in India,” she said. “The talks were genuine, raw and meaningful for anyone, be they psychiatric survivors or their kith and kin.”
Visit isps-us.org for more information.
DAIL Seeks Specialized Long-Term Caregivers
According to the Vermont Department of Disabilities, Aging and Independent Living, roughly 110 Vermonters with “complex needs” can’t find placements in Medicaid-funded long-term care facilities. The state is searching for a vendor capable of accommodating this population.
Many of Vermont’s nursing homes, residential care homes, and assisted living residences don’t have sufficient expertise to care for people with particular behaviors resulting from brain injury, stroke, or dementia. Most of all, they struggle to take in residents with mental health diagnoses, who make up 63% of those who meet the state’s eligibility criteria for long-term care but, due to a shortage of specialized providers, don’t yet receive it.
Some end up, in DAIL’s words, “‘stuck’ in an inappropriate setting (e.g., hospital).” Others look for out-of-state options.
DAIL issued a request for proposals on Aug. 9. Bidders will propose adding services to an existing licensed facility or establishing a new one.
In either case, they will aim to offer, as the document puts it, “a reliable, high-quality option for specialized care that promotes dignity and quality of life in a safe, secure setting.”
Proposals will include a “use of restraints plan” and “use of anti-psychotic medication plan,” as well as information about how many residents the contractor can serve.
The RFP closes on Sept. 14. DAIL expects to select a winning bid on Sept. 30 and execute
a contract around Dec. 1. It will offer a twoyear agreement with a renewal option for two additional years.
NEWS 23 Fall 2018 Fall 2023 NEWS 23
Have News To Share? Send it to Counterpoint! The Service Building, 128 Merchants Row Suite 606, Rutland, VT 05701 Email: counterpoint@vermontpsychiatricsurvivors.org COUNTERPOINT DEADLINES FALL (September delivery; submission deadline August 5) WINTER (December delivery; submission deadline November 6) SUMMER (June delivery; submission deadline May 1)
The overarching goal is to “foster and create systems of care in which human rights and full personhood are held central.”
SURVIVOR PEER SERVICES
Vermont Psychiatric Survivors
VPS is a membership organization providing peer support, outreach, advocacy and education 128 Merchants Row, Suite 606, Rutland, VT 05701 802-775-6834 www.vermontpsychiatricsurvivors.org
VPS OUTREACH AND PATIENT REPRESENTATIVES (802) 775-6834 info@vermontpsychiatricsurvivors.org
WARM LINE
VERMONT SUPPORT LINE (STATEWIDE): 833-888-2557; 24 hours, 365 days [833-VT-TALKS]

By call or text
CRISIS RESPITE
Alyssum, 802-767-6000; www.alyssum.org; info@alyssum.org
HOSPITALIZATION ALTERNATIVE
Soteria House, information and online application at www.pathwaysvermont.org/what-we-do/ our-programs/soteria-house/ or call Pathways Vermont Intake Line, 888-492-8212, ext. 140
Peer Centers & Employment Support
ANOTHER WAY
125 Barre St, Montpelier, 802-229-0920; info@anotherwayvt.org; www.anotherwayvt.org; see website for events calendar.
PATHWAYS VERMONT COMMUNITY CENTER
279 North Winooski Avenue, Burlington, 802-777-4633; pvcc@pathwaysvermont.org www.facebook.com/PathwaysVTCommunityCenter; www.pathwaysvermont.org/what-we-do/ our-programs/pvcc
Some Peer Centers and Recovery Centers may have changed hours as a result of COVID-19 crisis. Call to check on up-to-date schedules.
Vermont Recovery Centers
WWW.VTRECOVERYNETWORK.ORG
BARRE, Turning Point Center of Central Vermont, 489 N. Main St.; 479-7373; www.tpccv.org; tpccvbarre@ gmail.com
BENNINGTON, Turning Point Center, 160 Belmont Dr; 802-442-9700; info@tpcbennington.org
BRATTLEBORO, Turning Point Center of Windham County, 39 Elm St.; 802-257-5600; tpwc.1@hotmail.com
BURLINGTON, Turning Point Center of Chittenden County, 179 South Winooski Ave, Suite 301; 802-8613150; www.turningpointcentervt.org or support@ turningpointcentervt.org
MIDDLEBURY, Turning Point Center of Addison County, 5 A Creek Rd; 802-388-4249; info@turningpointaddisonvt.org
MORRISVILLE, North Central Vermont Recovery Center, 275 Brooklyn St., 802-851-8120; JOHNSON, 117 St. John’s St. 802-730-8122; recovery@ncvrc.com
NEWPORT, Journey to Recovery Center, 212 Prouty Dr. 802-624-4156
JOHNSON, Jenna’s Promise, 114 St. John’s Rd, 802343-8741; info@jennaspromise.org
RUTLAND, Turning Point Center, 141 State St; 802-7736010; turningpointcenterrutlandvt.org
SPRINGFIELD, Turning Point Recovery Center of Springfield, 7 Morgan St., 802-885-4668; webadmin@ spfldtp.org; www.spfldtp.org
ST. ALBANS, Turning Point of Franklin County, 182 Lake St; 802-782-8454; contacta@turningpointfranklincounty.org
ST. JOHNSBURY, Kingdom Recovery Center, 297 Summer St; 802-751-8520; recoveryinfo@stjkrc.org; www. kingdomrecoverycenter.com
WHITE RIVER JUNCTION, Upper Valley Turning Point, 200 Olcott Dr; 802-295-5206; www.uppervalleyturningpoint.org; info@secondwindfound.org
SUICIDE & CRISIS LIFELINE 988 24/7 support
Crisis Text Line
Around the clock help via text: send “VT” to 741-741 for ground rules; message routed to a trained counselor.
Vermont Federation of Families for Children’s Mental Health
Statewide support for families of children, youth or young adults in transition who are experiencing or at risk to experience emotional, behavioral or mental health challenges. 800-639-6071, 802-876-7021; www.vffcmh.org
Pride Center of Vermont
LGBTQ Individuals with Disabilities Social and Support: Connections and support around coming out, socializing, employment challenges, safe sex, self-advocacy. For center hours call (802) 860-7812 or go to www. pridecentervt.org
Brain Injury Association
Support Group locations on web: www.biavt.org; support@biavt.org; 802-244-6850
Trans Crisis Hotline
The Trans Lifeline (dedicated to the trans population) can be reached at 877-565-8860.
LGBTQ Youth Crisis Hotline: The Trevor Lifeline, 866-488-7386. TrevorText : 678-678
Hearing Voices Network Online Groups
Opportunities to connect, share experiences, and find mutual support via web-based platforms and by phone specifically for those with personal lived experience with hearing voices, seeing visions, and/or negotiating alternative realities. For questions and for details on how to access the group[s]: info@hearingvoicesusa.org.
NATIONAL ALLIANCE ON MENTAL ILLNESS-VT (NAMI-VT): 802-876-7949 x101, or 800-639-6480; 600 Blair Park Road, Suite 301, Williston, 05495; www.namivt.org; info@namivt.org
Connections Peer Support Groups
Meetings are led by trained Peer Support Leaders. The groups provide a safe place that offers respect, understanding, encouragement, and inspires hope to all who attend. Zoom Meetings: Every Monday 7-8:30 p.m. and 1st & 3rd Tuesday 4-5:30 p.m. In-Person: Every Thursday from 3-4:30 p.m., Cathedral Church of St. Paul, 1st floor, Commons Room, 2 Cherry Street, Burlington. To learn more, visit: www.namivt.org/support-groups/peer-support/
Counterpoint publishes this resource directory to allow readers to seek out choices for support. Counterpoint has not reviewed or evaluated the quality or biases of these resources, and makes no representation about their value for any individual.
Public Community Mental Health
COUNSELING SERVICE OF ADDISON COUNTY, 89 Main St., Middlebury, 05753; www.csac-vt.org; 802-388-6751
UNITED COUNSELING SERVICE OF BENNINGTON COUNTY, PO Box 588, Ledge Hill Dr., Bennington, 05201; 802442-5491; 5312 Main St., Manchester, 802-3623950; www.ucsvt.org
CHITTENDEN COUNTY: HOWARD CENTER, 300 Flynn Ave., Burlington, 05401; 802-488-6000; www.howardcenter.org
FRANKLIN & GRAND ISLE: NORTHWESTERN COUNSELING AND SUPPORT SERVICES, 107 Fisher Pond Road, St. Albans, 05478; 802-524-6554; www.ncssinc.org
LAMOILLE COUNTY MENTAL HEALTH SERVICES, 72 Harrel Street, Morrisville, 05661; 802-888-5026; www.lamoille.org
NORTHEAST KINGDOM HUMAN SERVICES, 181 Crawford Road, Derby; 802-334-6744; 2225 Portland St., St. Johnsbury; 802-748-3181; www.nkhs.org
ORANGE COUNTY: CLARA MARTIN CENTER, 11 Main St., Randolph, 05060-0167; 802-728-4466; www.claramartin.org
RUTLAND MENTAL HEALTH SERVICES, 78 So. Main St., Rutland, 05701; 802-775-2381; rmhsccn.org
WASHINGTON COUNTY MENTAL HEALTH SERVICES, 9 Heaton St., Montpelier, 05601; 802-223-6328; www.wcmhs.org
WINDHAM AND WINDSOR COUNTIES: HEALTH CARE AND REHABILITATION SERVICES OF SOUTHEASTERN VERMONT, 390 River Street, Springfield, 05156; 886-4500; 51 Fairview St., Brattleboro, 05301, 802-254-6028; 49 School St., Hartford, 05047, 802-295-3031; www.hcrs.org
24-Hour Crisis Lines and Involuntary Custody Screening
ADDISON COUNTY: Counseling Services of Addison County 802-388-7641
BENNINGTON COUNTY: United Counseling Service, 802442-5491; (Manchester) 802-362-3950
CHITTENDEN COUNTY: Howard Center, 802-488-7777
FRANKLIN AND GRAND ISLE COUNTIES: Northwestern Coun- seling and Support Services, 802-524-6554; 800834-7793 LAMOILLE COUNTY: Lamoille County Mental Health, Weekdays 8 a.m.-4 p.m. 802-888-5026; Nights and weekends 802-888-8888
ESSEX, CALEDONIA AND ORLEANS: Northeast Kingdom Human Services 802-334-6744
ORANGE COUNTY: Clara Martin, 800-639-6360
RUTLAND: Mental Health Services, 802-775-1000
WASHINGTON COUNTY: Mental Health Services, 802-2290591
WINDHAM,WINDSOR COUNTIES: Health Care and Rehabilitation Services, 800-622-4235
Please contact us if your organization’s information changes: counterpoint@vermontpsychiatricsurvivors.org
Veterans’ Services
TOLL-FREE HOTLINE (24/7) 800-273-8255
CRISIS LINE: Toll-Free: 866-687-8387, press 7
FREE TRANSPORTATION: Disabled American Veterans: Toll Free: 866-687-8387 X5394

HOMELESS PROGRAM COORDINATOR: 802-295-9363, ext 6184
TRANSITIONAL RESIDENCES: Canal Street Veteran’s Housing, Winooski 802-864-7402; Dodge House, Rutland, 802-775-6772; Veteran’s Inc, Bradford, 802-627-7838; The Veteran’s Place, Northfield, 802-485-8874.
VERMONT VETERANS SERVICES: program for homeless veterans with very low incomes: 802-656-3232.
VA Mental Health Services
VA HOSPITAL: Toll Free 866-687-8387
Vermont Veterans Outreach Team
Peer-to-Peer Support: Veteran’s Outreach program staff with very diverse backgrounds including service in different branches of the military.
OUTREACH TEAM LEADER: 802-338-3022
ADDISON COUNTY: 802-338-4313
CALEDONIA/ORANGE/WINDSOR COUNTY: 802-338-4324
CHITTENDEN NORTH: 802-338-3078
CHITTENDEN SOUTH: 802-338-4316
LAMOILLE COUNTY: 802-338-3411
ORLEANS/ESSEX COUNTY: 802-338-4325
RUTLAND COUNTY: 802-338-4315
WASHINGTON COUNTY: 802-338-4318
WINDHAM COUNTY: 802-338-4171
MENTAL HEALTH SERVICES: 802-338-3445
www.MakeTheConnection.net
MENTAL HEALTH CLINIC, White River Jt, Toll Free 866-687-8387 Ext 6132
OUTPATIENT CLINICS: Bennington: 802-440-3300; Brattleboro: 802-2512200; Burlington Lakeside Clinic: 802-657-7000; Newport: 802-6242400; Rutland: 802-772-2300
VET CENTERS: (So. Burlington) 802-862-1806; (White River Jctn) 802-295-2908
Web site sponsored by The Department of Veterans Affairs with testimonials by veterans to help connect with the experiences of other veterans, and with information and resources to help transition from service, face health issues, or navigate daily life as a civilian.

Resources Directory 24 Fall 2023












































 by RON MERKIN, Montpelier
by RON MERKIN, Montpelier