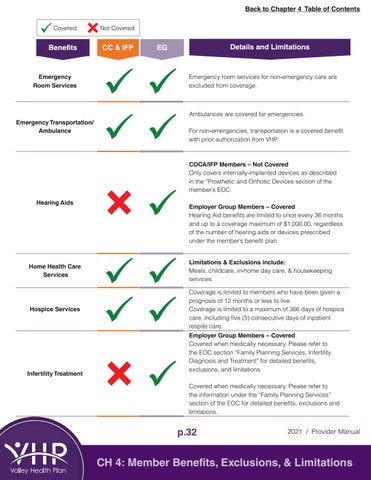
Back to Chapter 4 Table of Contents Covered
Not Covered
Benefits
CC & IFP
Emergency Room Services
Details and Limitations
EG
Emergency room services for non-emergency care are excluded from coverage.
Ambulances are covered for emergencies. Emergency Transportation/ Ambulance
For non-emergencies, transportation is a covered benefit with prior authorization from VHP.
COCA/IFP Members – Not Covered Only covers internally-implanted devices as described in the “Prosthetic and Orthotic Devices section of the member’s EOC. Hearing Aids
Employer Group Members – Covered Hearing Aid benefits are limited to once every 36 months and up to a coverage maximum of $1,000.00, regardless of the number of hearing aids or devices prescribed under the member’s benefit plan.
Home Health Care Services
Limitations & Exclusions include: Meals, childcare, in-home day care, & housekeeping services.
Hospice Services
Coverage is limited to members who have been given a prognosis of 12 months or less to live. Coverage is limited to a maximum of 366 days of hospice care, including five (5) consecutive days of inpatient respite care.
Infertility Treatment
Employer Group Members – Covered Covered when medically necessary. Please refer to the EOC section “Family Planning Services, Infertility Diagnosis and Treatment” for detailed benefits, exclusions, and limitations. Covered when medically necessary. Please refer to the information under the “Family Planning Services” section of the EOC for detailed benefits, exclusions and limitations.
p.32
2021 / Provider Manual
CH 4: Member Benefits, Exclusions, & Limitations