Back to Chapter 4 Table of Contents
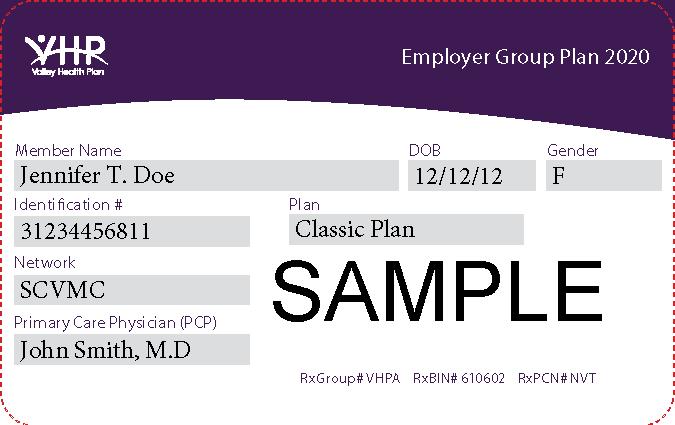
VHP network providers render a variety of health care services pursuant to the benefit limitations and exclusions reflected in the member’s Evidence of Coverage (EOC). You can find the EOCs for the Covered California/IFP and the Employer Group Lines of Business on the VHP website at https://www. valleyhealthplan.org/sites/m/mm/Pages/evidenceofcoveragebookletanddisclosureform.aspx. For specific benefits questions or assistance, please contact Member Services at 1.888.421.8444. Providers need to validate VHP Commercial Employer Group, Covered California and Individual & Family Plan member eligibility and benefits prior to rendering services to VHP members. To confirm a VHP member’s eligibility, please refer to the Valley Express online eligibility system available at https://www.valleyhealthplan.org/sites/p/fr/auths/Pages/home.aspx or contact VHP’s Member Services Department Monday through Friday, 8 am to 5 pm (Pacific) at 1.888.421.8444. If you do not have access to the online system, and you wish to obtain access to Valley Express to verify eligibility, please call Provider Relations at 1.408.885.2221. A copy of the VE Access Form is included in the Appendix. Disclaimer: Members must present their VHP identification card whenever they seek services. Providers must check eligibility at each visit. Possession of a VHP ID card does not guarantee eligibility or payment.
Member Benefit Plans Employer Group Plan (Classic and Preferred): Members are not responsible for any cost sharing for covered services unless specified (e.g., cost share applies to acupuncture and chiropractic care). Refer to the member’s EOC at https://www.valleyhealthplan.org/sites/m/ mm/Documents/VHP-Employer-Group-EOC-2020-Final.pdf Covered California and Individual & Family Plan: Members are responsible for deductibles, coinsurance, and copayments, which apply to many covered services. Refer to the member’s EOC at https://www.valleyhealthplan.org/sites/m/mm/Documents/2021-CoveredCalifornia-IFP-EOC.pdf The following list is not intended to be an all-inclusive list of covered and non-covered benefits. All services are subject to benefit coverage, limitations, and exclusions as described in the EOC. Some services require prior authorizations before services are rendered. For more information on services requiring prior authorization, see Chapter 17, “Utilization Management” for additional information.
p.29
2021 / Provider Manual
CH 4: Member Benefits, Exclusions, & Limitations