Pediatric Trauma Center at Golisano Children’s Hospital
ANNUAL REPORT • 2024






ANNUAL REPORT • 2024






What is a trauma center? It’s a question we often hear. Is it the emergency department? A separate building? A different part of the hospital?
In essence, a trauma center is a concept—one that began decades ago. It’s the idea that if a hospital dedicates the right resources—skilled caregivers, specialized equipment, and robust support systems—then outcomes for injured patients will improve. It means getting the right care to a child, for any injury, at any time.
Golisano Children’s Hospital at the University of Rochester Medical Center is a cornerstone of pediatric care for Monroe County, the Finger Lakes, and beyond. Our Pediatric Trauma Program is committed to treating the most severely injured children with expert, life-saving care.
We are proud to be the region’s only American College of Surgeons (ACS) verified and New York State designated Level 1 Pediatric Trauma Center. This dual recognition reflects the highest standards in trauma care, education, and research.
Our multidisciplinary team—surgeons, emergency physicians, nurses, and support staff—is available 24/7, every day of the year. From injury through recovery, we provide advanced, compassionate care tailored to each child. We also lead in injury prevention and research, always working to improve safety and long-term outcomes.
Golisano’s Pediatric Trauma Program stands ready to meet the urgent needs of injured children, ensuring access to the highest level of specialized care when it matters most.

Wakeman, M.D.
As the only Pediatric Trauma Center in the Finger Lakes region, Golisano Children’s Hospital is uniquely positioned to provide life-saving care to injured children in our community.

Over the past eight years, since taking on the role of Pediatric Trauma Medical Director, I have had the privilege of witnessing the remarkable growth and maturation of our trauma system and program. What sets us apart today is simple yet profound: we get injured children the care they need faster, supported by a robust process and performance review system that ensures exceptional clinical care is consistently delivered. Our commitment to excellence in clinical care is unwavering. We are equipped to care for any injured child, at any time, with access to all subspecialty services. This comprehensive approach allows us to meet the diverse needs of our patients and their families, ensuring the best possible outcomes.
I am excited to share several updates that highlight the continued evolution of our program:
• Leadership Expansion: Dr. Katie Riera has been appointed as the Pediatric Trauma Associate Medical Director. Dr. Riera will focus on clinical practice guideline creation and performance improvement, particularly for injured adolescents who bridge the pediatric and adult trauma programs.
• Reverification: In 2025, we have been reverified as a Level 1 Pediatric Trauma Center by the American College of Surgeons for another year, affirming our commitment to meeting the highest standards of trauma care.
• Rehabilitation Services: Our Physical Medicine and Rehabilitation team has
opened a new patient floor, now offering rehabilitation care for injured children as young as six years old.
• Whole Blood Program: We are one of the few Pediatric Trauma Centers nationally able to offer whole blood transfusions for children as young as six months old. This innovative approach improves outcomes, including survival from severe injury, while reducing blood product exposures.
• Disaster Preparedness: Additionally, we have significantly enhanced our pediatric disaster preparedness. Through regular meetings and drills, our team ensures we are always ready to respond to emergencies
involving large numbers of children. This proactive approach strengthens our ability to provide coordinated, effective care during mass casualty events, further solidifying our role as a trusted resource for the region.
• Enhanced Facilities: Our new Emergency Department being built will significantly expand the space available to care for injured children, featuring state-of-the-art pediatric resuscitation bays and an adjacent, designated family waiting area.
Our program is also gaining increasing recognition regionally and nationally:
• Regional Outreach: We are actively educating pre-hospital and hospital providers on best practices for stabilizing and caring for injured children, ensuring seamless transfers when needed.
• State Leadership: I serve as Pediatric Subcommittee Co-Chair of the New York State Trauma Advisory Council and Vice Chair of the New York State ACS Committee on


Trauma, with a focus on pediatric readiness.
• Research Excellence: Our team’s research is gaining national attention, with presentations at the Pediatric Trauma Society annual meeting.
These advancements reflect the dedication of our entire team and our shared mission to provide the highest level of care to injured children. I am proud of what we have accomplished and look forward to continuing to grow and innovate in the years ahead.
Thank you for your ongoing support and collaboration as we work together to improve pediatric trauma care in our region and beyond.
Sincerely,
Derek Wakeman, M.D., F.A.C.S.
Pediatric Trauma Medical Director Golisano Children’s Hospital
Surgeons:




Marjorie Arca, M.D.
Professor of Surgery and Pediatrics Surgeon-in-Chief, Golisano Children’s Hospital
Abdelhafeez Abdelhafeez, M.D. Associate Professor of Surgery


David G. Darcy, M.D., F.A.C.S.
Assistant Professor of Surgery and Pediatrics Surgical Director of Neonatal & Pediatric ICUs
Walter Pegoli, Jr., M.D. Professor of Surgery and Pediatrics
TRAUMA PROGRAM TEAM:
Adam Oplinger B.S., R.N., C.E.N., T.C.R.N.
Pediatric Trauma Program Manager
Lauren Pierson D.N.P., C.P.N.P.-P.C.
Pediatric Trauma APP
Riley Youells, E.M.T.-P.
Lead Pediatric Trauma Registrar
Becky Chatt, M.S., R.N. Trauma Program Educator
Sarah Gorman, R.N., B.S.N. Injury Prevention & Outreach Coordinator

Brooke Streiff, M.H.A. Division Administrator
Tamara Englert, B.A.S. Trauma Program Administrative Assistant
SPECIALTY LIAISONS:
Michael A. Vella, M.D., M.B.A., F.A.C.S.
Adult Trauma Program Manager
Neil Blumberg, M.D. Blood Bank
Mitchell Chess, M.D. Pediatric Radiology
Colleen Davis, M.D. Pediatric Emergency Medicine
Derek Wakeman, M.D.
Associate Professor of Surgery and Pediatrics; Pediatric Trauma Medical Director
Katherine M. Riera, M.D.
Assistant Professor of Surgery and Pediatrics; Associate Pediatric Trauma Medical Director
Nicole Wilson, Ph.D., M.D.
Assistant Professor of Surgery, Pediatrics, and Biomedical Engineering; Associate Program Director for Research, General Surgery Residency
Michael Davis, M.D. Pediatric Anesthesiology
Jake Deines, M.D. Pediatric Critical Care
Ann Lenane, M.D. Child Abuse Physician
Susan Nelson, M.D. Pediatric Orthopedic Surgery
Howard Silberstein, M.D. Pediatric Neurosurgery
Lauren Solan, M.D. Pediatric Hospital Medicine
Tina Sosa, M.D. Golisano Children’s Hospital Quality
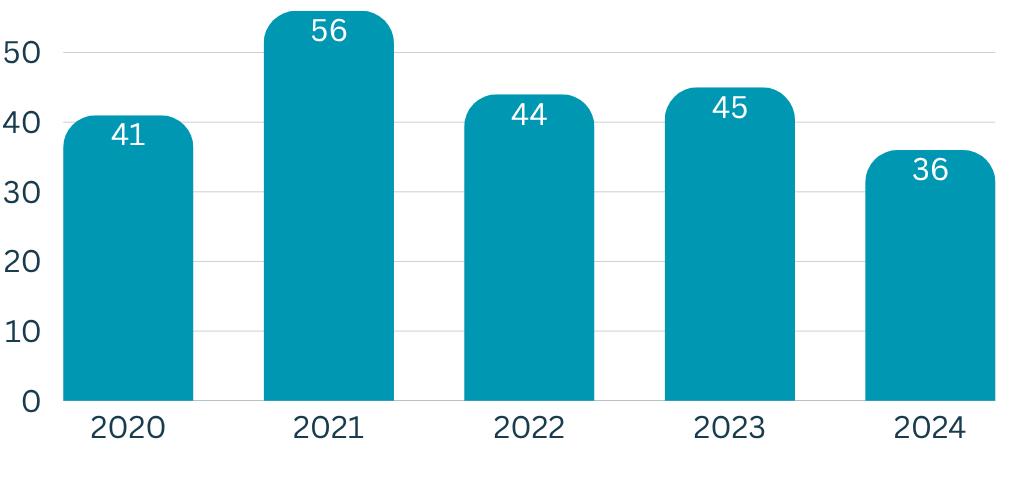
Pediatric ICU Admissions
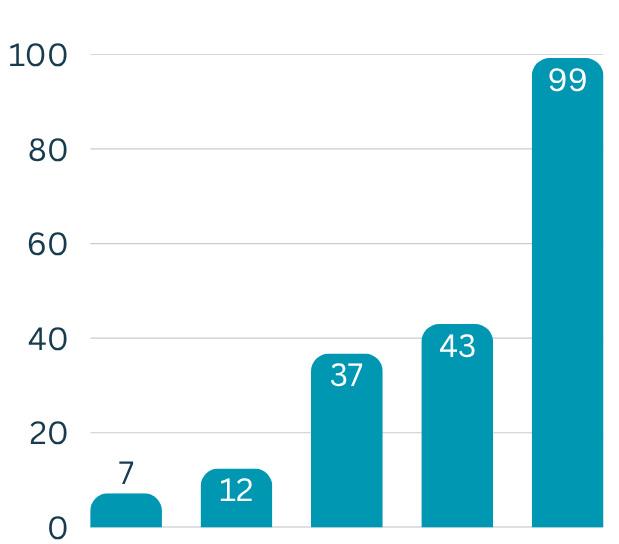
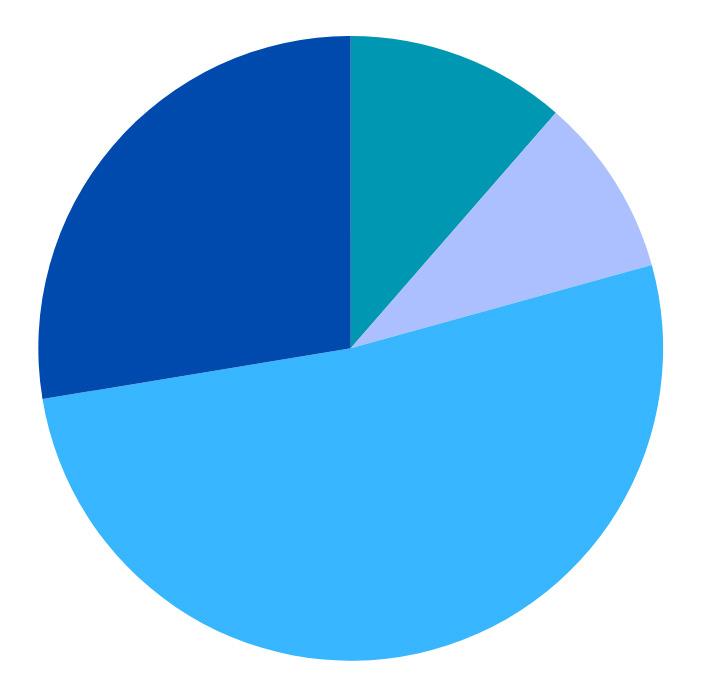
Arrivals to Pediatric Trauma CenterAll Injured Patients

Patient Disposition Following Emergency Department Evaluation
Mechanism of Injury for Trauma Team Activations:

Pediatric Trauma Center Catchment Area Finger Lakes Region 13 counties | population: 1.5 million | 10,000 square miles
Mechanism of Injury Trends for all Injured Patients
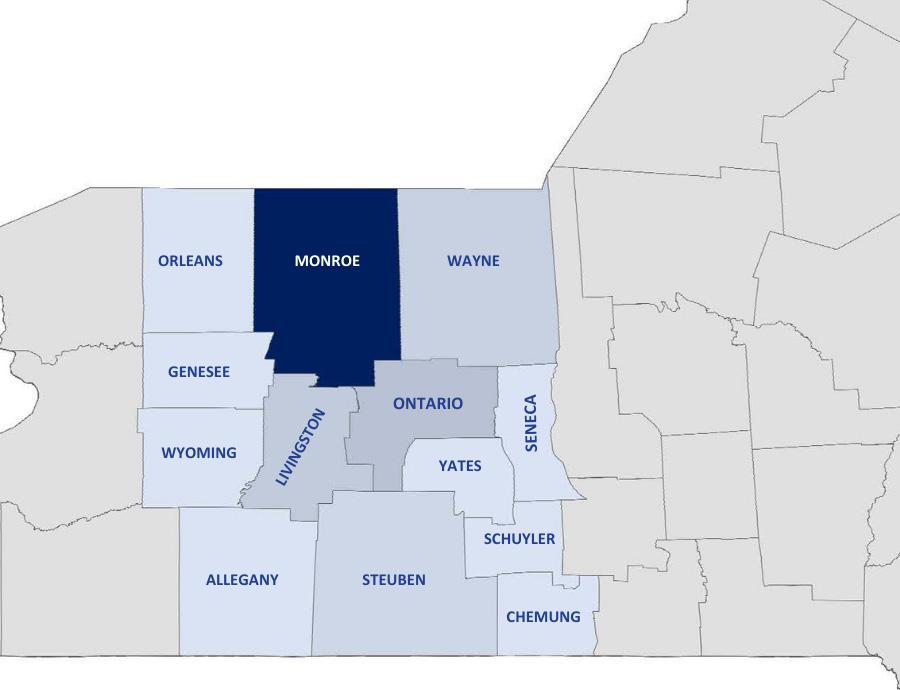
2024 Transfer Patient Data


Total number of patients transferred to the Pediatric Trauma Center 238
Total number of hospitals the Pediatric Trauma Center received patients from 23
Total number of counties Pediatric Trauma received patients from:
Top 5 Counties of Injury (by

At Golisano Children’s Hospital, we believe in providing the best possible care for children who have experienced a serious injury. To do this, our dedicated team is always learning and staying up to date with the latest advancements in trauma care. We are committed to teaching our staff, families, and the community how to manage and care for critically injured children.
Here’s a look at how we continue to enhance our skills and support our patients:
Just like how kids learn and grow every day, our medical team also continuously learns to improve their skills and knowledge:
• Advanced Trauma Care for Nurses (ATCN®): This specialized course helps our nurses
develop advanced skills in managing patients with multiple injuries. It fosters a collaborative, team-oriented approach to trauma care, ensuring our patients receive comprehensive support. Our center has significantly increased this educational
offering to ten times per year, including sessions to train new instructors.
• Advanced Trauma Life Support (ATLS®):
Developed by the American College of Surgeons, this course teaches physicians a systematic and clear approach to caring for trauma patients. It’s designed to help them safely assess and care for the most critically injured patients who arrive at the hospital. Our center now offers this crucial training eight times per year.
• Trauma Education Conference: This monthly conference is open to all staff involved in caring for injured patients. It offers one hour of continuing education on diverse topics such as traumatic brain injury (TBI) and triaging trauma patients, ensuring our team stays informed on current best practices.
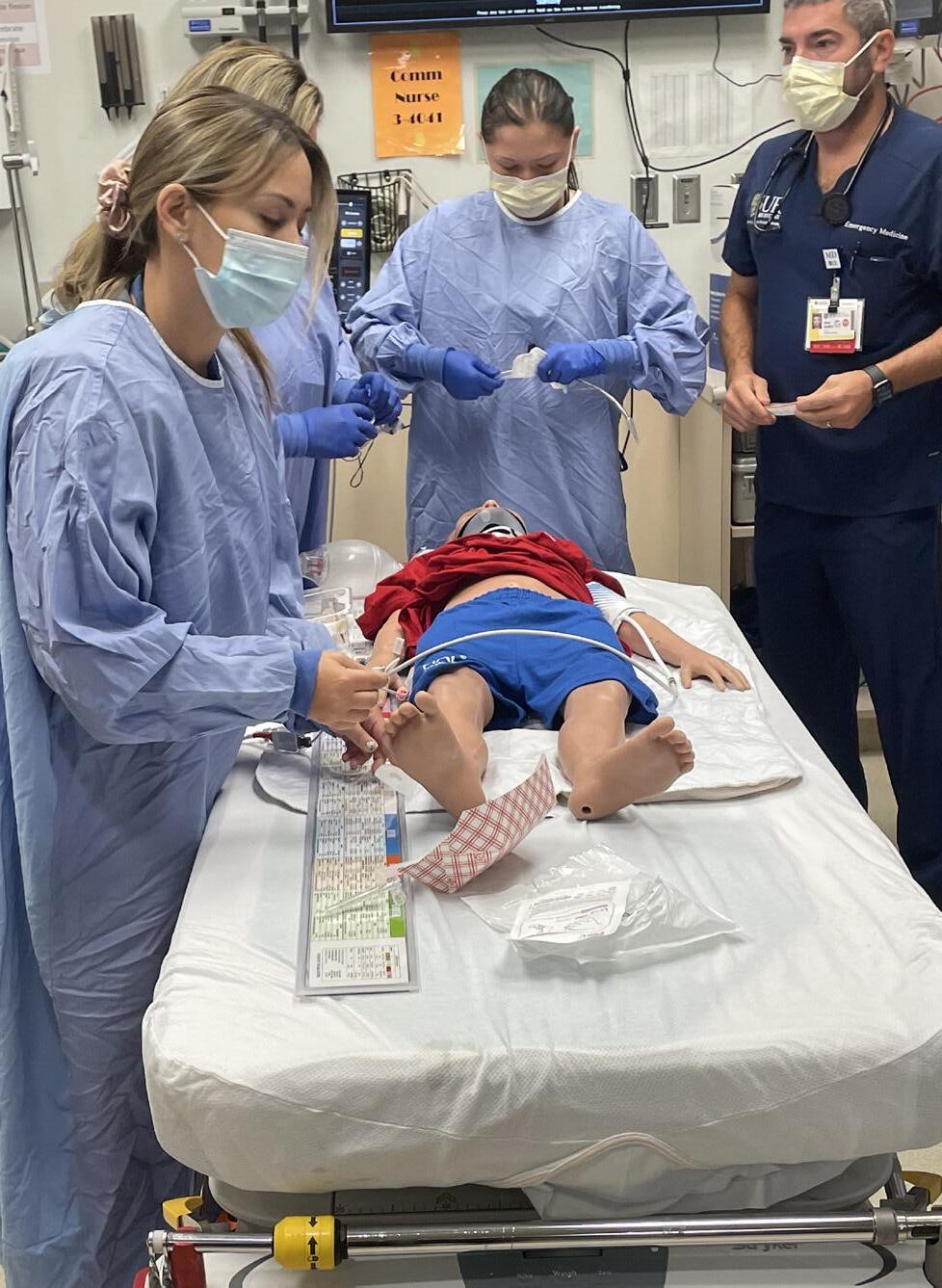
Learning is often best through practice. Our team regularly engages in hands-on training to prepare for real-life situations:
• Trauma Skills Lab: We offer handson training sessions monthly, or more frequently if needed, for all staff involved in trauma care—including physicians, nurses, patient care technicians (PCTs), and respiratory therapists. These sessions allow staff to gain practical experience with essential equipment like rapid infusers, advanced airway tools, and ultrasound, helping them feel more confident and

prepared for real patient care.
• Mobile Trauma Skills Lab: To extend our reach, we also bring our skills lab to regional hospitals and emergency medical service (EMS) agencies. These three-to-four-hour classes offer the same valuable handson experience, ensuring that healthcare providers in our wider community are wellprepared to use various medical equipment when needed.
• Trauma Simulation: Simulation provides a safe and controlled environment for our team to practice skills and enhance communication. Practice through simulation allows for repeated performance and refinement of steps, which research shows optimizes clinical outcomes. Simulated scenarios are based on actual trauma resuscitations in which potential
opportunities for improvement were identified. We offer monthly simulation sessions for staff in the Pediatric Emergency Department. We also collaborate with our partners from the adult trauma center to offer combined simulation sessions with the Pediatric Emergency Department and the Adult Trauma Service.
Our commitment to education extends beyond our hospital walls, preparing our broader community for effective trauma care:
• Rural Trauma Team Development Course (RTTDC®): This course, developed by the American College of Surgeons, focuses on improving trauma care in resource limited settings. It helps smaller facilities develop timely, organized responses for trauma patients. We typically offer this course four times in the spring and four times in the fall, or upon request, to facilities throughout our trauma region.
In October of 2024, our Pediatric Trauma Program, in conjunction with the Department of Prehospital Medicine, took a bold step in advancing pediatric disaster preparedness by hosting a high-impact Disaster Education
Pre-Conference at the New York State EMS Vital Signs Conference in Rochester, New York. This immersive training brought together EMS professionals for a four-hour session of hands-on learning, simulation, and skill-building—focused
specifically on pediatric mass casualty incidents.
The day began with a focused session on SALT Triage—a nationally adopted method that helps emergency responders sort and prioritize patients during large-scale emergencies. SALT stands for Sort, Assess, Lifesaving interventions, and Treatment/Transport, and is designed to streamline decision-making when seconds count and resources are limited.
Participants then put their knowledge into action during a realistic pediatric mass casualty simulation, followed by a tabletop exercise addressing regional transport coordination and hospital surge capacity. The session closed with a fast-paced round of Your Trauma

Triage™, an original card game developed by our team to reinforce triage accuracy in a fun, memorable way.
This innovative program was later showcased on a national stage at the Trauma Center Association of America’s Injury Prevention Conference, where it was recognized as a leading example of creative, effective pediatric disaster education.
Your Trauma Triage™ is a dynamic, scenariodriven card game created by our pediatric trauma program to teach the principles of triage in mass casualty incidents (MCIs). Drawing on deep field experience in both military and civilian trauma care, this tool was developed to simulate the time-sensitive decision-making required in disaster situations.
By placing healthcare providers in a highpressure, game-based environment, the tool fosters quick thinking, reinforces triage accuracy, and encourages reflective learning— all without the risks of a real-world emergency. The game’s structured, repetitive format provides a safe space to build muscle memory, teamwork, and confidence.
In 2025, Your Trauma Triage™ was officially copyrighted by the University of Rochester and is expected to be available to EMS agencies soon. This innovative, scalable, and engaging training resource is poised to make a significant
impact in disaster preparedness education across institutions nationwide.
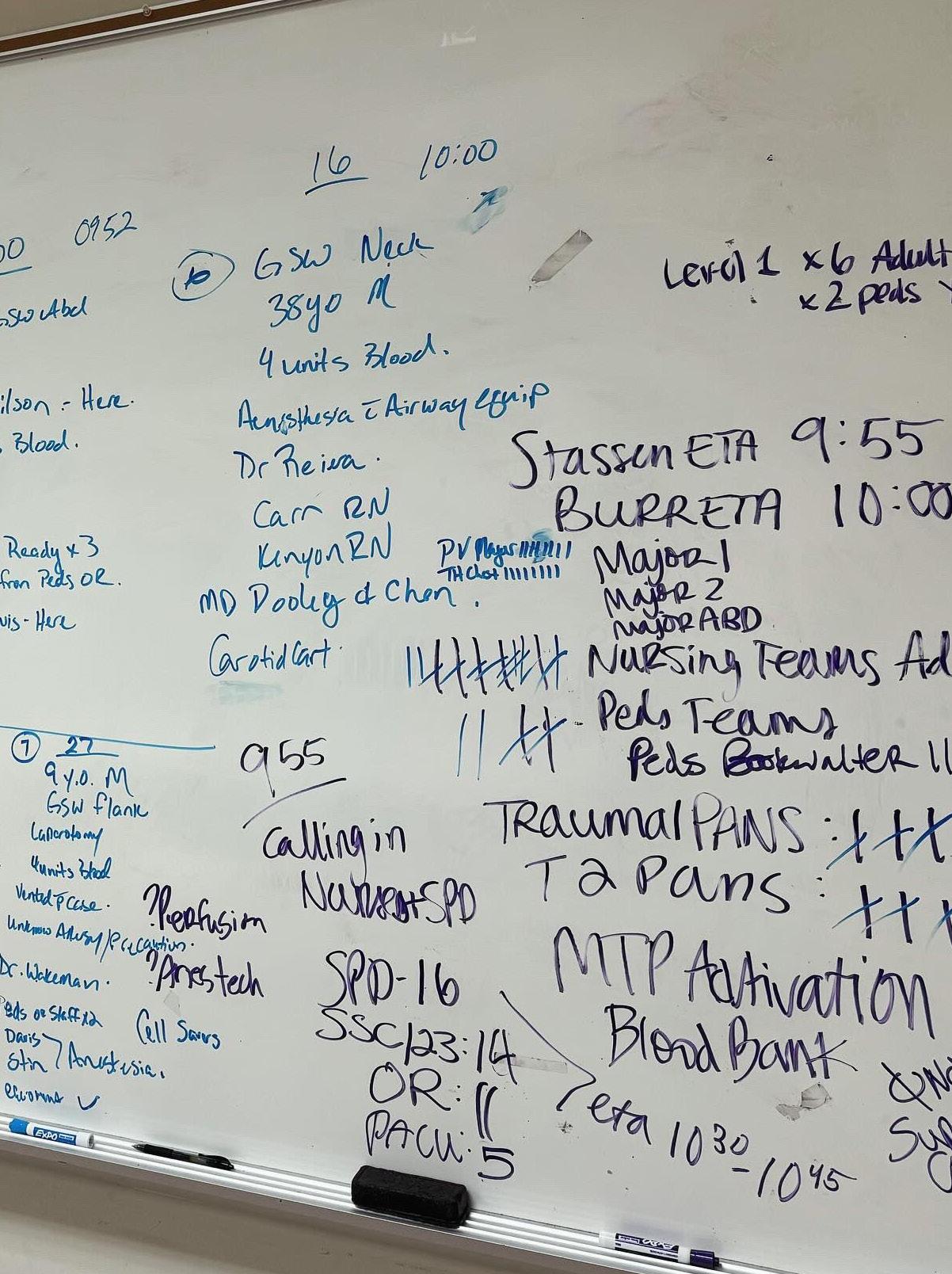
Further highlighting our commitment to pediatric disaster preparedness, in early 2024, our operating room leadership and staff conducted a highly effective disaster preparedness exercise in close collaboration with both the pediatric and adult trauma programs. This comprehensive simulation of a mass casualty incident demanded rapid surgical intervention for multiple severely injured patients, encompassing a wide range of injuries and patient ages. During the drill, our dedicated OR team, alongside our trauma services, brilliantly demonstrated their ability to swiftly convert from routine operations to a full disaster response. This involved efficiently triaging incoming adult and pediatric “patients” and simultaneously managing several complex surgical procedures. The true highlight of this exercise was the exceptional coordinated effort between the operating room, pediatric trauma, and adult trauma services, proving our seamless ability to optimize resource allocation, synchronize with ancillary services, and maintain crystalclear communication under pressure. This collaborative drill underscored our unwavering commitment to preparedness and confirmed our collective capacity to provide immediate, highquality, life-saving care, especially to our most vulnerable pediatric population, even during unforeseen catastrophic events.

Regular trauma-related continuing medical education efforts ensure that all providers remain current with the latest advances in trauma care. The Kessler Trauma Center at Strong Memorial Hospital is committed to teaching staff, and our community partners how to manage critically injured patients.
Whole Blood Transfusion
When a child has a serious injury and loses a lot of blood, we need to replace it quickly and safely. Traditionally, this meant giving several different blood components separately, which could sometimes mean more fluid overall, more exposure to different donors, and other potential complications like temperature changes or electrolyte imbalances.
Now, our pediatric trauma center offers a more
advanced approach: whole blood transfusions. This means we can give all the necessary blood components in one simpler, smaller package. It’s like getting all the pieces of a puzzle together at once, rather than one by one.
This method helps us:
• Minimize the amount of fluid given.
• Reduce a child’s exposure to many different blood donors.
• Lower the risk of complications often seen
with multiple transfusions.
• Streamline the process for our medical team.
We’re proud to share that in 2023, our pediatric trauma center became one of only a few in the nation to regularly use whole blood transfusions for injured children as young as six months old. This practice provides the best possible fluid replacement while reducing risks. Plus, URMC has created a special program to screen type O blood donors specifically for whole blood donations, ensuring we have a ready supply of this vital resource for our trauma patients.
After a serious injury, some children need extra help to get back to walking, talking, or reaching other important milestones. Our hospital is dedicated to helping them fully recover.
We now have a total of thirty-one specialized beds in our inpatient rehabilitation unit,
including a dedicated unit for acute brain injuries. This means more space and support for children who need focused care to improve their abilities and quality of life.
Our teams work closely together, combining the expertise of specialists such as developmental pediatricians, neurologists, neurosurgeons, and physical medicine specialists. We collaborate to create a personalized recovery plan for each child, offering tailored therapies like physical, occupational, and speech therapy, along with custom-made braces and supports. Our goal is to ensure that every child has the resources they need to reach their fullest potential.
We’ve designed our rehabilitation spaces with children and families in mind:
• Crucially, this inpatient rehabilitation unit is located right here on the URMC campus, so children don’t need to be transferred to an unfamiliar facility.

• Rooms are spacious enough for parents to stay overnight, providing comfort and support.
• We have specialized exercise equipment and treatment areas just for kids.
• Children can also get tutoring and help planning their return to school as they continue to heal physically.
We’re committed to helping every child on their unique journey back to health and happiness.
Beyond the physical bumps and bruises, serious injuries can also be tough on a child’s feelings and mind. Sometimes, the emotional recovery takes longer than the physical healing, and it can even impact them later in life.
At our pediatric trauma center, we believe in treating the whole child, which means we pay close attention to their emotional well-being right from the start:
• Early Screenings: For all children aged eight and older who are admitted with an injury, we do a quick check to see if they might be at risk for a condition called acute stress disorder.
• Tailored Support: If a child shows signs of this risk, they immediately receive support from our highly respected pediatric psychiatry team, recognized as one of the best in the nation. If they don’t show immediate signs, we still provide families
with information and resources, just in case concerns pop up later.
• Ongoing Care: Our commitment doesn’t stop when they leave the hospital. We continue to check on their mental health during follow-up appointments, making sure we’re supporting all aspects of their well-being.
This focus on mental health reflects UR Medicine’s dedication to providing top-quality emotional support and treatment for children and teenagers. Our resources include:
• In-hospital support
• Outpatient care (appointments after leaving the hospital)
• Pediatric mental health urgent care for immediate needs.
We’re here to help every child on their journey to complete healing, both inside and out.


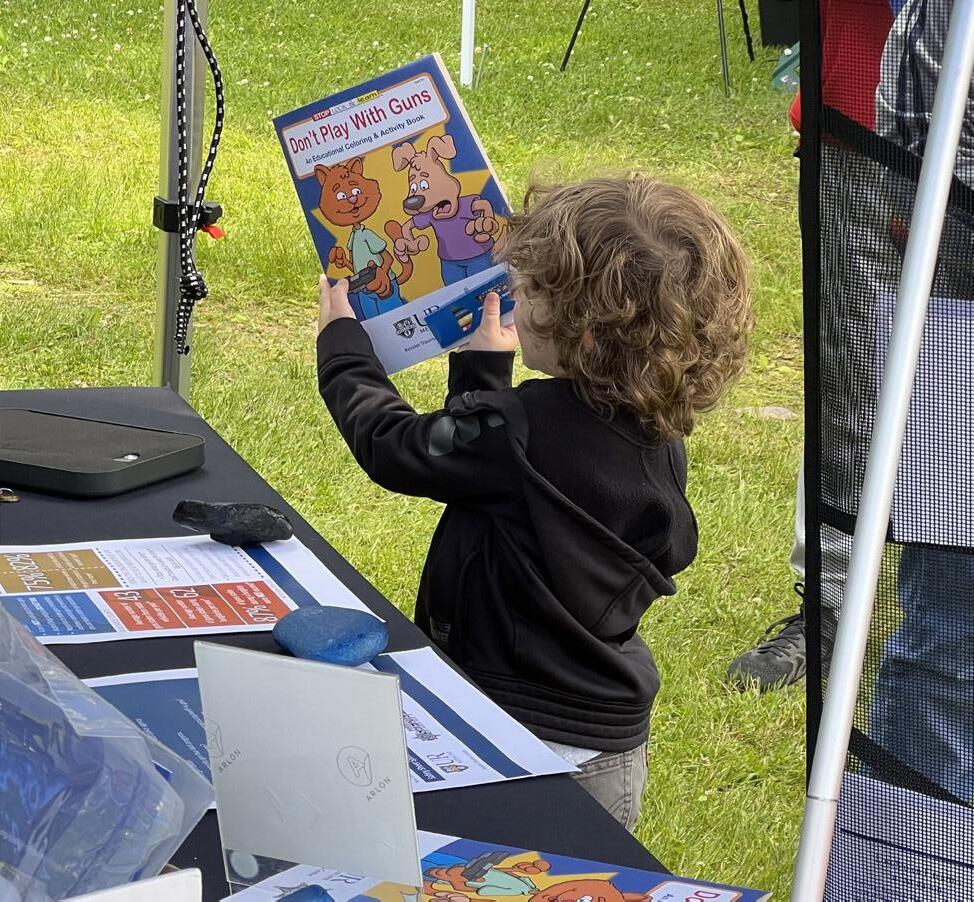
Imagine preventing two-thirds of childhood trauma. It’s not just a dream – it’s a very real possibility, and our pediatric trauma program is making it happen. We work extensively with both community and hospital-based injury prevention programs, leveraging local insights, cutting-edge research, and powerful partnerships to stop injuries before they even start. Key collaborators include the Rochester chapter of Injury Free Coalition for Kids, Impact Teen Drivers, The Rochester Youth Violence Partnership, and the Firearm Injury Prevention Program at the University of Rochester.
Addressing youth violence in our community demands a comprehensive, multi-layered approach. That’s why the Rochester Youth Violence Partnership serves as a vital hospitalbased intervention program. Comprising twenty-eight dedicated local organizations,
this partnership targets victims of violence, immediately working to prevent repeat incidents and provide crucial support after they leave the hospital. By bringing representatives directly to the bedside, we can promptly address concerns and help when it matters most.
Our commitment to safety also extends to preventing unintentional firearm injuries. Many
believe their firearms are safely stored, but, tragically, children often find them. That’s why our trauma program has teamed up with the Monroe County Sheriff’s Office and works with the Firearm Injury Prevention Program at the University of Rochester to deliver essential education on Responsible Gun Ownership, ensuring firearms are inaccessible to children. We also empower parents with guidance and support, encouraging them to ask about firearm access in other homes before playdates –because a child’s safety should be paramount in every environment.
Furthermore, our commitment to safety extends into the schools themselves. When the Rochester City School District prioritized readiness for life-threatening bleeding emergencies, our trauma program responded with intensive Stop the Bleed® training. This crucial didactic and hands-on instruction empowers safety and security officers to provide immediate, life-saving aid.
This training is part of the broader national Stop the Bleed® campaign through the American College of Surgeons. Launched in October 2015 aims to empower civilians with the knowledge to recognize and treat external hemorrhage – the leading cause of preventable death following trauma. While the original curriculum targeted adults, we recognized that children may also witness trauma resulting in severe bleeding and are fully capable of providing initial life-saving care. To address this, a new curriculum, known as Stop the Bleed Kids®, was
developed to teach children as young as five to distinguish a “big bleed” from a “little bleed” and perform hands-on techniques to control it. The Pediatric Trauma Program is the only center in the region to offer this program to kids. This age-appropriate curriculum focuses on helping others, and in a pilot program with 500 children, an impressive 75 percent retention rate of skills and knowledge was observed one year later. This innovative approach ensures even our youngest community members can be lifesavers!
Making our region’s roads safer for our kids and community is one of our top priorities. Working alongside the Injury Free Coalition for Kids of Rochester; we’re using powerful data from sources like the National Highway Traffic Administration and the NYS County Crash
Dashboard to pinpoint exactly where and how to boost traffic safety.
We’re also tackling teen driving risks head-on. With sixteen-year-olds four times more likely to crash than adults, our trauma program, in partnership with Impact Teen Drivers and local school districts, delivers a proven distracted driving prevention program. Teens learn vital strategies, such as how managing passengers can significantly lower crash incidents, preparing them for safer driving futures. Road and car safety for our younger patients is also a priority. Because we know that over half of all car seats are incorrectly installed, we offer vital monthly car seat checks for patients and staff – a simple step that could save a life. Our comprehensive approach also includes bicycle helmet checks and crucial pedestrian safety education.
We are also leveraging cutting-edge data on illegal school bus passing, particularly concerning the staggeringly high numbers of drivers in our area who disregard flashing red lights on stopped school busses. Our pediatric trauma program is using this data to implement
targeted interventions, including community awareness campaigns, and advocating for further action on this issue at the national level to dramatically reduce dangerous incidents and safeguard every child’s journey to and from school.
Recovery from a serious injury can be a challenging journey for both patients and their families. We are dedicated to providing support every step of the way:
• Trauma Survivor’s Network (TSN®): The Pediatric Trauma Center, in collaboration with our Kessler Trauma Center colleagues, is proud to be part of the Trauma Survivor’s Network. TSN helps trauma centers provide essential support and services to patients and their families during recovery. This includes offering support groups and connecting survivors with others who share similar experiences, fostering a sense of community and empowering them to become advocates for injury prevention and improved trauma outcomes.



This is the story of a family’s journey after their son, Penn, was seriously injured, having been struck by a car.
The call came as a gut punch, an abrupt intrusion into an ordinary day. “It was a shock in the deepest sense of the word,” Amy, Penn’s Mom, recalls, her voice still holding a tremor from that moment. “We received a call from the sheriff asking if we were the parents of the injured child, without any update on whether our child was dead or alive. Just that he was being transported to Golisano Children’s Hospital.” The 40-minute drive that followed was a blur of ‘complete emotional numbness, operating on autopilot.” Their son, an energetic boy with autism, had been gravely injured, and the Calverts were hurtling towards an unknown future.
Arriving at Golisano Children’s Hospital, the Calverts were plunged into a world of urgent medical intervention. Their son was still unconscious, and the worry was overwhelming. “As soon as we realized we were at an academic medical center, we felt ourselves breathe—just a little,” Craig explains. “That detail gave us an immediate sense of reassurance that we were in the right place.”
It was the people within that expert environment who truly made the difference. “Josh, an R.N. in
the Pediatric Intensive Care Unit, stood out tremendously,” Amy shares. “When Penn’s oxygen levels were dropping and he kept pulling his mask off, Josh stayed calm and patient, gently holding the mask to his face while soothing him.” Another constant, calming presence was one of the Pediatric Trauma doctors. “They kept us updated regularly and truly cared,” Craig adds. “We even witnessed staff staying past their shifts to continue caring for him. That kind of dedication meant everything.”
Despite the severity of his injuries, Penn displayed an incredible, innate resilience.
“The moment he was conscious, he started giving high-fives to staff—before every surgery, even,” Amy says with a smile. Also, as soon as he could walk again, still within the hospital walls, his determination shone through.
“He started asking when he could return to CrossFit,” Craig laughs.
When asked if they recall any significant milestones marked the road to recovery, Amy immediately exclaimed “Breathing on his own!”, recalling the pivotal moment. Craig states that he has a specific photo of a doctor teaching while Penn was lying in the Hospital bed in the PICU. He states the photo brought him immense relief because in that moment he had thought “If they’re teaching right now, then our son must be okay.”
After discharge, at physical therapy, Penn’s drive was still evident. “He insisted he was ready for CrossFit again—he even did a sit-up that nearly gave the therapist a heart attack,” Amy recounts with humor. She adds that just a month after the injury, Penn proudly walked in his homecoming parade.
Beyond the immediate medical care, the Pediatric Trauma Center at Golisano Children’s Hospital understood the profound impact of trauma on the entire family. “At first, we refused to leave his side,” Amy admits. “But the staff took the time to explain the importance of rest and convinced us to stay at the Ronald McDonald House. That made a huge difference.” Small acts of kindness resonated deeply: “While we were there, two kind men
would regularly stop in just to check on us—to see if we needed anything. Those small acts of kindness made us feel seen and supported.”
Looking back, both parents agree with one another about what saved their son. “Without hesitation: the attentiveness of the staff,” Craig states. “During the ARDS (Acute Respiratory Distress Syndrome) crash, we saw an instant shift in the team’s energy. They didn’t miss a beat and jumped into action”
Their son’s successful recovery has profoundly reshaped the family’s life. “Penn has autism, which means our emotional connection looks a little different than that of many families,” Craig explains. “But through this experience, he was able to see and feel how deeply he is loved. He recognized how his injury affected us and how much we cared. It’s shifted our perspective completely. What we used to think was important no longer is. We now truly understand what matters most.” Added Amy.
For other parents facing similar traumatic experiences, the Calverts offer crucial advice: “Don’t forget to take care of yourself too. The trust that we have in the staff at Golisano Children’s Hospital is without limit. There is no benefit to you or your child’s recovery by going without food or sleep. We didn’t go to the Ronald McDonald house at first because we had the mindset that others need it more. Remember that taking care of yourself doesn’t take away from others” To conclude the interview, the family was asked, “If you could sum up your experience with Golisano Children’s Hospital in one word or short phrase, what would it be?” Craig answered with emotion. “Their staff is not at work. They are doing their calling.”

At our trauma center, our most important goal is to provide the best and safest care for every child. This means we are always looking for ways to improve, ensuring that our practices are based on the latest medical knowledge and meet the highest possible standards for a leading trauma center.
We have a dedicated performance improvement (PI) process that is constantly evaluated and strengthened. Our trauma program leaders meet regularly to review all patient cases that meet
specific criteria for a more in-depth look. This rigorous review helps us confirm that we are following all hospital guidelines and protocols.
Through this proactive approach, we can identify any emerging trends or areas for improvement in our care. This allows us to make necessary adjustments quickly, even before we receive official benchmarking reports from the Trauma Quality Improvement Program (TQIP), a national quality benchmarking program that we also participate in. If a case or a particular trend needs further attention, it is discussed in detail at specialized multi-disciplinary conferences,
where experts from different fields collaborate. Sometimes, a broader hospital-wide review is also conducted.
This thorough and ongoing process highlights our entire hospital’s deep commitment to continuous improvement and to maintaining the absolute highest standards of care for our young patients. It’s how we make sure every child receives exceptional care, every time.
Performance Improvement Initiatives
Supporting Emotional Well-being After Injury
This initiative was launched in response to a new mental health screening requirement set forth by the American College of Surgeons in their “Resources for Optimal Care of the Injured Patient” guidelines. We’ve introduced a special screening process for all injured children aged eight and older admitted to our trauma service. This helps us identify early on if a child might be at risk for developing intense stress reactions, like Post-Traumatic Stress Disorder (PTSD), after their injury.
We use a specific screening tool called STEPP (Screening Tool for Early Predictors of Posttraumatic Stress) to assess a child’s emotional needs shortly after admission. If a child screens positive for emotional distress, we immediately seek parental consent to connect them with our highly skilled pediatric psychiatry team, recognized nationally for its excellence, who then creates a personalized treatment plan. Since launching this important initiative, our pediatric trauma team has maintained an impressive 92 percent compliance rate for

mental health screening. This effort not only ensures comprehensive care but also helps support our dedicated pediatric psychiatry services, allowing them to continue their vital work. Our holistic approach means we’re committed to the complete well-being of every child we treat.
Learn more about our initiative to support the emotional well-being of our patients in the Advances in Pediatric Trauma Care Section of this booklet.
When a child is seriously injured, every second counts. It’s crucial to quickly identify how serious their injuries are so the right medical team can spring into action immediately.
Historically, our hospital used the same criteria to activate the trauma team for both adults and children. To make sure our injured kids get the most precise and rapid response, we explored creating criteria specifically for them.
After reviewing extensive research and looking closely at cases from 2022, we pinpointed two key areas where we could make our trauma team activation even better for children:
• Neurologic Assessment Findings: We noticed that some children with concerning signs in their neurological assessment (how they react and move) weren’t always triggering the highest level of trauma alert. For example, out of fifty-six children
brought in by ambulance with a less-thanfull response, twenty-seven of them needed immediate medical interventions, but twelve of those were initially given a lower-level alert. This meant valuable time could be lost. Now, if an injured child (from birth to fifteen years old) shows any difficulty with movement or response, it automatically triggers the highest level of trauma team activation. This ensures our most specialized team is ready the moment they arrive.
• Penetrating Injuries: In 2022, we treated six children with stab wounds to the torso.
Even though some of their overall injury scores didn’t immediately indicate severe harm, we found that four of these children showed early signs of shock and three needed urgent surgery. This highlighted that these types of injuries can be deceptively dangerous. Based on this review, any child with a stab wound to the torso now automatically receives the highest level of trauma team activation.
These new, pediatric-specific trauma activation criteria were put into practice in July of 2024. We’ve also trained our communication specialists (who take calls from emergency services) to quickly get the right information about a child’s condition and specific injuries like stab wounds. This proactive change has significantly improved our ability to get critically injured children the specialized care they need, precisely when they need it most. Before these changes, about 8.3 percent of seriously injured children might have been initially
underestimated; now, that number has dropped to 5 percent, meaning fewer children are being “under-triaged” and are getting the top-level care they deserve from the very beginning.
For children who suffer a traumatic brain injury (TBI), ensuring the best possible recovery requires precise and consistent care, especially during their time in the Intensive Care Unit (ICU). We noticed in previous national TQIP reports that our pediatric patients with TBI were spending more days in the ICU and on breathing machines compared to other top centers. For instance, our average ICU stay was twelve days compared to a three day average for similar patients elsewhere, and mechanical ventilation averaged 8.5 days versus three days.
After a thorough review of our cases, we discovered that there wasn’t always a standardized way to manage TBI, especially when patients became agitated. We also realized that our rehabilitation specialists weren’t always involved early enough in the ICU stay.
To address this, we developed a comprehensive guideline, working closely with our Pediatric Intensive Care Unit (PICU) team. This guideline is based on the best practices from the American College of Surgeons and provides clear instructions for managing children with severe head injuries in the PICU. It covers everything from initial care to managing brain pressure and ensuring neck stability. Additionally, to further standardize care and
assist our busy resident doctors who often admit these complex patients, we created a Traumatic Brain Injury (TBI) Order Set. This is a pre-filled checklist of medical orders, customized based on the severity of the child’s head injury. It helps ensure that all necessary care, including early consultations with specialists like rehabilitation and neurology teams, is ordered right away. These early consults are crucial for planning the child’s discharge and ensuring smooth ongoing care, including strategies for managing agitation if needed.
The results have been significant! Following the implementation of the TBI Order Set, our Spring 2023 TQIP report showed a dramatic improvement: ICU days decreased to an average of six days (matching the national average), and mechanical ventilation days dropped to 4.5 days (very close to the national average of four days). This improved

care also led to an average cost savings of $16,786 per patient.
To ensure these improvements last, we’ve put measures in place. We’re actively educating new doctors joining our team about the TBI guideline and order set, including it in resident training programs. We also continuously monitor the use of this order set, tracking it on our pediatric trauma dashboard to keep all key stakeholders informed and committed to this best practice.
At Golisano Children’s Hospital Trauma Program, every child’s trauma case tells a story—a story of injury, resilience, and hope. The Pediatric Trauma Registry is the cornerstone of understanding
these stories, capturing comprehensive, highquality data that fuels research and drives improvements in patient care.
This registry goes beyond data and recordkeeping; it is a dynamic tool that allows clinicians and researchers to identify emerging trends, evaluate treatment effectiveness, and refine clinical protocols tailored specifically to children’s needs. The continuous insights gained from the registry have led to measurable improvements in outcomes and recovery for pediatric trauma patients.
Recently, our program has embraced the latest Pediatric Trauma Registry technology from National Quality Systems (NQS). This advanced platform enhances our ability to collect, manage, and analyze data with greater accuracy and speed. Its user-friendly interface and robust analytics tools empower our trauma team to make evidence-based decisions faster, helping to reduce complications and improve survival rates.
The integration capabilities of the NQS system also foster collaboration across care teams and regional partners, promoting a comprehensive, coordinated approach to trauma care. This level of innovation ensures that every piece of data contributes to better protocols, better treatments, and ultimately, better outcomes for children facing traumatic injury.
The ongoing evolution of the Pediatric Trauma Registry exemplifies how data-driven care can revolutionize pediatric trauma treatment, setting new standards and saving lives.

For many years Laurence and Dennis Kessler have dedicated themselves to helping people in their time of greatest need. Through their efforts and those of the managers and employees of the Kessler Group, Inc.,
The Laurence and Dennis Kessler Regional Trauma Unit in Strong Memorial Hospital’s Emergency Department was dedicated in 1997.
In 2003, the Kessler Family, LLC employees joined in fundraising efforts for the first time, initiating a new and generous commitment to name the Burn-Trauma Intensive Care Unit. In 2010, the Kessler Trauma Center was named in honor of the Kessler Family to acknowledge their generosity and extraordinary commitment to injury care in the Finger Lakes region.
Successful businessmen, philanthropists, and individuals dedicated to the health of the region, the Kesslers have built an invaluable legacy for the Rochester community and beyond. The charitable works of their employees exemplify their compassionate and generous spirit.
The Kessler Trauma Center relies on the generous support of past patients and their families as well as friends, health professionals, alumni, and community residents. Gifts to the Center have a tremendous impact. Funds are used to educate the next generation of trauma care providers, improve patient care and to support the development of innovative community outreach programs.
The Kessler Trauma Center, as a part of the University of Rochester Medical Center, is a not-for-profit organization and all gifts made to the Center are deductible according to IRS guidelines.
Please contact Kerrie Merz to learn more about how you can help support this important work. (585) 273-2766 Kerrie_Merz@rochester.edu
As the area’s only Level 1 Trauma Center, the team at Strong is proud to provide state-of-the-art injury care to residents of Rochester, Monroe County and the surrounding region. The new Trauma Resuscitation Unit, a critical part of the expansion project, was designed from the ground up to meet the challenges of modern trauma care. The unit will be significantly larger and will provide immediate access to advanced imaging and treatment modalities.


PEDIATRIC TRAUMA CENTER AT GOLISANO CHILDRENS HOSPITAL
601 Elmwood Avenue Rochester, NY 14642
