

CHARTING New Waters





EDITOR
Nora Williamson
ASSOCIATE EDITOR
Gianluca D’Elia
ART DIRECTOR & DESIGN
Christine Kennedy
FEATURE PHOTOGRAPHY
Gianluca D’Elia John Schlia
Jeff Witherow Matt Wittmeyer
COVER ILLUSTRATOR
John Tomac
CONTRIBUTORS
Bethany Bushen Nicole Cullen
Gianluca D’Elia Emily Gillette
Maureen Malone Nora Williamson
URMC COMMUNICATIONS
B. Chip Partner AVP, Communications
ADVANCEMENT & ALUMNI RELATIONS
Melissa L. Head ’99W (MS) Executive Director for Advancement
Andrea Allen, Senior Director of Advancement and Alumni Relations
Mia Cannon, Senior Director of Alumni Relations and Volunteer Engagement
Rochester Nursing Magazine is published twice a year for alumni, students, and friends of the University of Rochester School of Nursing. It is published by the University of Rochester Medical Center Departments of Communications, Alumni Relations, and Advancement.
WRITE TO
We welcome your letters and feedback concerning stories in the magazine or issues related to the University of Rochester School of Nursing. Send your comments to:
Editor, NURSING Magazine
601 Elmwood Avenue, Box SON
14642
SON-Communications@urmc.rochester.edu
www.son.rochester.edu

Lisa Kitko, PhD, RN, FAHA, FAAN
Dean, School of Nursing Independence Foundation
Chair in Nursing Education
Vice President, University of Rochester Medical Center
Professor of Nursing & Geriatric Medicine
From the Dean
DEAR FRIENDS,
I hope this message reaches you in good spirits and enjoying all the brightness that summer brings. After a rain-soaked spring here in Rochester, the world around us has finally burst into color, reminding us how renewal often follows challenge.
That sense of resilience has echoed throughout our School of Nursing in recent months. We’ve experienced profound loss with the passing of two extraordinary leaders — Dr. Loretta Ford and Dr. Kathy Rideout. Their vision, their compassion, and their unwavering belief in the power of nursing continue to shape who we are. Their legacies don’t just live on. They propel us forward. I truly believe we are honoring them with every step we take.
Across education, practice, and research, our momentum remains strong. You’ll see it in the stories throughout this magazine — especially our cover feature, which spotlights how nurse-led preventive care is creating real impact in the workplace and beyond. Through programs now serving thousands, we’re embedding wellness into the fabric of our communities and measuring the difference it makes.
(Flip to Page 28 for more.)
We’re also looking ahead with clarity and purpose. Our strategic plan through 2030 charts an ambitious but deeply intentional course, focused on making our School a place where people can thrive, innovate, and belong. I couldn’t be prouder of the team working to turn that vision into reality. You can explore the details by scanning the QR code on this page.
This year feels especially meaningful as we stand at the edge of a remarkable milestone: our Centennial. It was September 1925 when Helen Wood Hall first opened its doors to nursing students — a building filled with curiosity, intelligence, and the hope of healing. One hundred years later, that spirit still defines us.
As we prepare to celebrate this momentous anniversary, I invite you to join us for Meliora Weekend this September. We’ll come together to reflect on our roots, honor our legacy, and share what’s ahead. I promise it will be a celebration filled with meaning, memory, and momentum.

In the meantime, I hope you’ll continue to find ways to stay connected — through events, through giving, or even just by flipping through these pages and remembering why this work matters so much.
Wishing you a joyful, restorative summer. WITH GRATITUDE,

UR Nursing has ranked No. 15 among U.S. nursing schools for its master’s programs, and ranked No. 28 among Doctor of Nursing Practice programs, according to U.S. News & World Report.
Eligible New Yorkers can pursue a new nursing career through the 12-month accelerated program, with tuition and fees covered by the NYS Career Pathways Training Program. Graduates commit to three years of service in healthcare settings that serve communities most in need.
Nursing isn’t just about treating an illness or performing procedures. It’s about being present, being patient, and being a steady hand during times of uncertainty. It’s about advocating for those who can’t always advocate for themselves, offering comfort when words fall short, and creating a safe space for healing... I want to extend my heartfelt thanks to the School of Nursing for the incredible work that goes into making the program such a rewarding experience and creating an environment where students can thrive.”
Diyor Mukhammadov ‘24N, UR Nursing Scholar and RN at Wilmot Cancer Institute Student speaker at Dean’s Diamond Circle
The UR School of Nursing ranks among the top nursing schools at No. 32 in research funding from the National Institutes of Health. Nearly 100 UR Nursing Scholars have graduated from the accelerated bachelor’s program over the past year, receiving full tuition coverage through this workforce initiative in exchange for three-years of service at select UR Medicine hospitals.
UR Medicine Employee Wellness, operated out of the UR School of Nursing, has delivered life-changing wellness programs for a decade — surpassing 100,000 biometric screenings completed in its first 10 years.

Since its launch in 2019, the UR Nursing Tuition Grant has helped more than 850 University employees advance their careers. This innovative program supplements existing tuition benefits to offer full tuition coverage for select nursing and healthcare programs. In May, the University announced a two-year extension of the grant. Share this opportunity with others by scanning the QR code.
UR Nursing was re-endorsed through 2030 by the International Nursing Association of Clinical and Simulation Learning (INACSL), recognized for excellence in pre-briefing, debriefing, facilitation and professional integrity in simulation education.

Healthy Students, Bright Futures
UR Nursing and RCSD Transform Student Care at Monroe High School
Six months after its launch, the School-Based Health Center at James Monroe High School is already transforming students’ lives — providing a safe, welcoming space for both physical and mental health care.
Julieann Falu, a senior at Monroe High School, says she and many of her peers are grateful to have mental health counselors available whenever they need support.
“I thought it was amazing to be honest,” Falu says. “When I left school early to go to an appointment, it was difficult for me to catch up with my schoolwork. I’m glad they have a health center here.”
Her sentiments are echoed by many Monroe students, who describe the center as “awesome,” “a safe place,” and “clean and comfortable.” Others highlight the friendly, helpful staff and the relief of knowing care is always close at hand.
These perspectives underscore the real impact since the University of Rochester School of Nursing and Rochester City School District opened the School-Based Health Center at Monroe High School this February. The center now provides comprehensive physical and mental health care to more than 700 students — regardless of insurance status — with no out-of-pocket costs.
Breaking Down Barriers to Care
For many Monroe High School students, accessing healthcare once meant navigating complex systems, missing school for appointments, and facing financial barriers. The new Health Center eliminates these obstacles by bringing services directly to where students spend most of their day.
“Having a school-based health center communicates to our students and our youth that medical and mental health care are important,” explains Nichole Gardea Butler, MS, LCSW-R, director of school-based health centers and
assistant professor of clinical nursing. “We are here to make sure that students are healthy so they can fully participate in their day-to-day school activities.”
Jason Muhammad, principal of Monroe High School, has already noticed positive changes.
“At Monroe, we believe that when students feel their best, they can do their best,” said Muhammad. “Having a school-based health center right here on campus gives our students a safe, welcoming place to address their health needs without missing valuable class time. This is a game-changer for our school community and a powerful investment in our students’ well-being and future.”
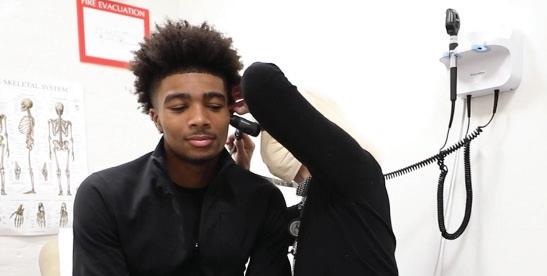
Comprehensive Care Under One Roof
Staffed by nurse practitioners, ambulatory technicians, licensed social workers, and psychiatrists from the UR School of Nursing and Strong Memorial Hospital, the Monroe Health Center offers:
Physical exams and preventive care
Mental health assessments and therapy
Medication management


Treatment for acute and chronic conditions
On-site lab services
Health education and counseling Immunizations
Coordination with primary care providers

who would otherwise need to take time off for their children’s medical appointments.
Gloriann Perez, a senior at East High School, has experienced firsthand the benefits of school-based health centers through East High’s established center.
“The health center has been helpful to me because I’m a multi-sport athlete, so I’m here all the time getting my physicals done when I need to,” Perez said. “Sometimes my mom can’t just take time out of work to go ahead and make that physical, especially with the wait times.”
A Model with Proven Results
The Monroe Health Center builds on three decades of successful school-based healthcare provided by the UR School of Nursing, which opened its first such center at East High School in 1995. Last year alone, the East High clinic served more than 620 students across 3,090 visits.
Research consistently shows that school-based health centers improve attendance, academic performance, and graduation rates while enhancing overall student health. They also reduce lost workdays for parents
By the Numbers
700+ students with access to care at Monroe High School
“By providing high-quality, patient-centered care, our Health Centers have the power to make a lasting impact on adolescents—equipping them with the knowledge and resources to take charge of their health,” says Renu Singh, MS, CEO of the UR Medicine Employee Wellness Program, who oversees the School’s clinical initiatives.
Looking Forward
As the Monroe Health Center approaches the half-year mark, its team continues to build trust with students and develop tailored programs to address the specific health needs of the school community.
Lisa Kitko, PhD, RN, FAHA, FAAN, dean of the University of Rochester School of Nursing, sees the center as fulfilling a core mission:
“We are proud to champion a model that breaks down barriers, ensuring that young people in our community have greater access to essential health care. Our health care providers develop longitudinal relationships with students, which enables earlier intervention and more personalized care planning.”

30 years of UR School of Nursing providing school-based health services
270+ School-Based Health Centers across New York State
0 out-of-pocket costs for students and families
Scan the QR code to watch our behind-the-scenes video featuring interviews with students, staff, and healthcare providers at the Monroe High School Health Center.
Leadership in Motion: Faculty Step Into New Roles
GRADUATE
PROGRAM LEADERSHIP
SUSAN CIURZYNSKI
Interim Director, DNP Program

Professor Susan Ciurzynski, PhD, RN-BC, PNP, VCE, FNAP, will serve as interim director for the DNP Program, ensuring a smooth transition following Lydia Rotondo’s retirement. Ciurzynski brings over 30 years of experience as a pediatric nurse, educator, and leader, and has previously served as the director of the Center for Lifelong Learning and assistant director of the DNP program.
MARIA MARCONI
Director, Leadership Programs & Nursing Education Assistant Professor Maria Marconi, EdD, RN, CNE, expands her leadership role to include leadership of the Clinical Nurse Leader and Leadership in Health Care Systems master’s programs, while continuing to direct Nursing Education programs. Marconi is widely recognized for her expertise in nursing education, curriculum development, academic assessment, and NCLEX preparation.
BETH PALERMO
Interim Director, Nurse Practitioner Programs Assistant Professor Elizabeth Palermo, DNP, RN, ACNP-BC, ANP-BC, now serves as interim director for all Nurse Practitioner programs and
ORGANIZATIONAL LEADERSHIP
CARLA DELUCIA
continues as specialty director for the Adult-Gerontology Acute Care Nurse Practitioner program. Palermo brings extensive experience as a clinician, educator, and curriculum leader, and is recognized for her contributions to advanced practice education, geriatric care, and professional development of nurse practitioners.
MARGARETANN CARNO


Interim Specialty Director, Pediatric Acute Care NP Professor Margaret Carno, PhD, MBA, MJ, RN, PNP-AC/PC, CNE, ATSF, FAAN, steps in as interim specialty director for the Pediatric Acute Care Nurse Practitioner program, following Julie Gottfried’s tenure. Carno was part of the faculty team that developed the advanced certificate program, which launched in 2021.
LAURA PAYTASH & MARIA CHENNELL
Interim Co-Specialty Directors, Family & Adult-Gerontology Primary NP Instructor


Associate Dean for Academic and Student Success Assistant Professor Carla DeLucia, EdD, now also provides oversight of the Center for Lifelong Learning – led by Director Susan Stanek, PhD, MSN/Ed, RN, in addition to the Student Affair’s Office, further strengthening student support services, retention, and enhancing how we meet continuing education needs.
TARA SERWETNYK
Director of Academic Assessment and Academic Innovation Associate Professor Tara Serwetnyk, EdD, RN, FNAP, NPD-BC, now serves in an expanded role overseeing assessment strategies to measure and improve student learning outcomes in alignment with program goals and accreditation standards. She continues to lead the Education

Laura Paytash, DNP, RN, FNP-BC, and Assistant Professor Maria Chennell, DNP, RN, FNP-C, NP-C, RNFA, take on interim co-director roles for these nurse practitioner specialty programs. Both bring significant clinical and educational experience, providing leadership as the programs transition following recent retirements.



Innovation Team, where she played a pivotal role in launching the School’s iROC initiative, earning recognition as an Apple Distinguished School.
JOHN EAVES
Associate Dean for Operations and Finance John Eaves, MBA, now also oversees the Admissions Office – led by Director Kimberly Starken – as associate dean for operations and finance, supporting strategic enrollment efforts and helping the school respond to evolving workforce needs.
LISA BROPHY


Interim Associate Dean for Academic Affairs Associate professor Lisa Brophy, EdD, RN, MSBA, CNE, has been named interim associate dean for academic affairs, where she will oversee both undergraduate and graduate programs.
Kate Valcin Named URMC Chief Nursing Executive

After a nationwide search, E. Katherine Valcin ’18N (PMC) ’20N (DNP) was named the University of Rochester Medical Center’s (URMC) chief nursing executive and chief nursing officer of Strong Memorial Hospital.

“Kate’s extensive experience in nursing, hospital operations, and education and mentorship will be instrumental in propelling URMC forward,” said Kathy Parrinello ’75N, ’83N (MS), ’90W (PhD), CEO of Strong Memorial and Highland hospitals. “Her outstanding performance in the interim role and engagement with the URMC nursing team, coupled with her extensive experience — both within Strong Memorial and across the nursing and healthcare professions more broadly — position her perfectly to lead our nursing teams.”
Valcin is also a preceptor and educator at the School of Nursing. In 2023, she received national recognition as a Fellow of the American College of Critical Care Medicine, an honor typically bestowed upon physicians. She is also the current president of the New York Organization for Nursing Leadership (NYONL).
“The search committee reviewed a variety of strong candidates for this position. Kate stood out as a leader with experience and knowledge that will help URMC grow as it addresses the opportunities and challenges of today’s healthcare environment,” said Lisa Kitko, PhD, RN, FAHA, FAAN, dean of the School of Nursing, who led the search
committee. “Her experience in the academic medical setting, collaborative style, support for nurses, and focus on education make her a great leadership partner for the School of Nursing.”
In her new role, Valcin will oversee all nursing operations at URMC, convene system-wide chief nursing officers in information sharing, and strengthen collaboration across disciplines. She will also serve as assistant dean of clinical practice at the School of Nursing, continuing to bridge clinical care and education.
Valcin completed her undergraduate studies at Roberts Wesleyan University and her master’s in nursing with a concentration in education at Duke, followed by a post master’s certificate in Clinical Nurse Leadership and Doctor of Nursing Practice from the University of Rochester School of Nursing.
“I am incredibly proud of the URMC nursing team and all they have accomplished, particularly through the challenges our profession faced in recent years,” said Valcin. “As we look to the future, I aim to build on this strong foundation by advancing nursing practice and creating a supportive and empowering environment for our staff. Together, we will enhance patient care, while preparing the next generation of nurse leaders to address the growing complexities of healthcare.”
Grant Aims to Strengthen Supports for New Nurses and their Mentors
Retention and recruitment efforts start with building a better beginning for preceptors and trainees alike

Starting a new job can be scary. For nurses who are not only new to the job but new to the profession, a $2 million grant from the New York State Department of Health promises to be a game-changer for the University of Rochester Medical Center. The funds are allowing Nursing Practice and the School of Nursing, with support from the Learning & Development Department, to enhance onboarding and training processes to comprehensively evaluate the existing preceptor program, create a new consultant position to support preceptors, and add “transition-to-practice-unit” pilots to nurse onboarding.
The vision for this multifaceted program, rooted in a strong academic-clinical partnership, was pioneered by School of Nursing Dean Emerita Kathy Rideout, EdD, PPCNP-BC, FNAP.
“Kathy’s vision for this collaborative program embodied the spirit of Meliora where we collaboratively work to give our students a learning experience that opens their eyes to the many paths they can take in nursing,” said SON Dean Lisa Kitko, PhD, RN, FAHA, FAAN.
This academic and clinical partnership directly benefits Nursing Practice, led by Chief Nursing Officer E. Kate Valcin, DNP, RN, NEA-BC, CCRN, CNL, FCCM. A preceptor herself, she knows the importance of the making incoming nurses feel confident in their early days and beyond.
“My first priority as CNO is to recruit and retain nursing staff,” Valcin said, “but this is only possible when we can motivate and engage the nurses we already have. Whatever someone’s reasons for becoming a nurse, it is our job to ensure
they are not only well-trained but that their mentors also have the support they need to thrive and be successful.”
Building a Village
Dean Viggiano, RN is a nurse at Golisano Children’s Hospital. He used to be a science teacher and ran his own tutoring business but switched careers after the pandemic.
For him, nursing combined his interests in science and education, but with the in-person interaction he craved. Viggiano enrolled in SON’s accelerated bachelor’s in nursing program where he began to build a circle of mentors. He later took part in the Nurse Residency Program—a year-long series of facilitator-led monthly forums that allow participants to learn about career paths within nursing.

“Seeing the same people every month for a year helped to create consistency and friendships that transcend the workplace,” he said. “It’s a huge benefit to have those relationships already built-in.”
The mentorship continued on the job at GCH, where he encountered a number of preceptors whom he still works with most days. He remains grateful for the rapport they share to this day.

“My first preceptor quite literally taught me how to be a nurse,” said Viggiano. “I knew my preceptors were always there for me as I navigated the emotional journey of nursing, especially in pediatrics. Our rapport helps us to navigate the challenging situations we face and I know I can go to them for anything, big or small, work-related or not.”
Who Mentors the Mentor?
On the flipside, preceptors don’t always have someone to turn to when they need support. There was internal feedback from preceptors, too, which prompted the creation of a new role—a senior clinical precepting consultant, or SCPC.
Creating this new role also aligns with national standards set forth by the ANCC, the national accrediting institution for nurses. Nurses from Strong recently returned from the national magnet conference, where they learned about ways to better support preceptors in keeping with the national gold standard. The new consultant position, one of several jobs created with grant funding, also offers the chance for nurses in the latter part of their career to transition into a new kind of mentorship role, said Stephanie Von Bacho, EdD, RN, senior director of Learning & Development who is also on faculty at SON.
“You think the preceptor is the go-to, the sage on the stage, but they don’t necessarily have someone themselves to turn to

“This model is another way for us to be synergistic and think about how we can support our nurses holistically,” said Von Bacho. The grant runs through fall of 2026.
when they need help,” said Von Bacho. “Having a preceptor consultant is a win-win for us, not only to support the preceptors but it offers an opportunity for a seasoned nurse with years of experience to do something different.”
The third and final piece of the grant will be used to supplement hands-on training for nursing students by designing and implementing two transition-to-practice units (TPUs) for new graduate nurse orientation.
1,464
5,608 79 RNs & LPNs at URMC Certified Nurses RNs/LPNs hired to Nursing Practice in 2024 By the numbers : 840
New graduates from SON joined URMC in 2024
The TPU model is adapted from the dedicated education unit (DEU) model, which provides clinical experience for nursing students through a partnership with a clinical institution. DEUs have been shown to give students a more realistic and effective learning experience. SON has partnered with URMC affiliates like Highland Hospital for the last decade.
Much like nursing students can get a firsthand look at the clinical environment with oversight from their nurse educator and clinical site instructor, new nurses can have similar experiences as part of their onboarding. The grant will fund a TPU pilot on a medical surgical unit with plans to establish a TPU in psychiatry as well.

Pinning Ceremony
December graduates of the accelerated bachelor’s program celebrate the next step of their careers at their cohort’s pinning ceremony.

“Florence Nightingale said, ‘Were there none who were discontented with what they have, the world would never reach anything better.’ Let us embody that mentality as we begin our careers in nursing,” accelerated bachelor’s class speaker Stephen Foster told his classmates at the December pinning ceremony.



“Let’s set new goals and reach for new heights — not only for ourselves, but also for the patients and communities we will serve,” said RN to BS class speaker Safa Rabah-Muhammad.

Accelerated bachelor’s alumna Nasreen Jaff receives her diploma from Dean Lisa Kitko.
Alumnus Dennis Averin receives his nursing sash and pin from his family.

Laura Paytash, a simulation educator and graduate clinical education co-coordinator, completed her Doctor of Nursing Practice in Spring 2025 and celebrates at the ceremony with fellow instructor
‘A Calling to Serve Others’
UR Nursing Class of 2025 Celebrates Next Steps

Sarah Mullen, chosen by her cohort as the undergraduate student speaker, changed careers to nursing following a previous career in HR. “As much as this program has conditioned us to work hard, it has also reminded us why we work hard. Nursing is a vocation, a calling to serve others when they are most in need,” said Mullen, a UR Nursing Scholar who is beginning her career with Strong Memorial Hospital’s solid organ transplant team this fall.

Graduate speaker Rachael Howe, a nurse manager in the Department of Psychiatry and recent alumna of the Leadership in Healthcare Systems program, shared how her time at UR Nursing has made her a better collaborator and leader. “It’s very easy to keep your head down and silo yourself within your own unit or department when you are in the thick of it,” Howe said. “I feel at the heart of this program is to always make the effort to keep improving, make the change, learn something new, and always try to better your best.”

Assistant Professor of Clinical Nursing Linda Migliore received the annual Dean’s Excellence in Teaching Award. She was recognized for her mentorship of emerging healthcare and nursing leaders through her role as specialty director for the Leadership in Healthcare and Clinical Nurse Leader master’s programs.

The School of Nursing honored more than 250 current and future nurses and healthcare professionals across its bachelor’s, master’s, and doctoral programs Friday, May 16, as they turned their tassels.
Sharon Gilbride.
Campus Events
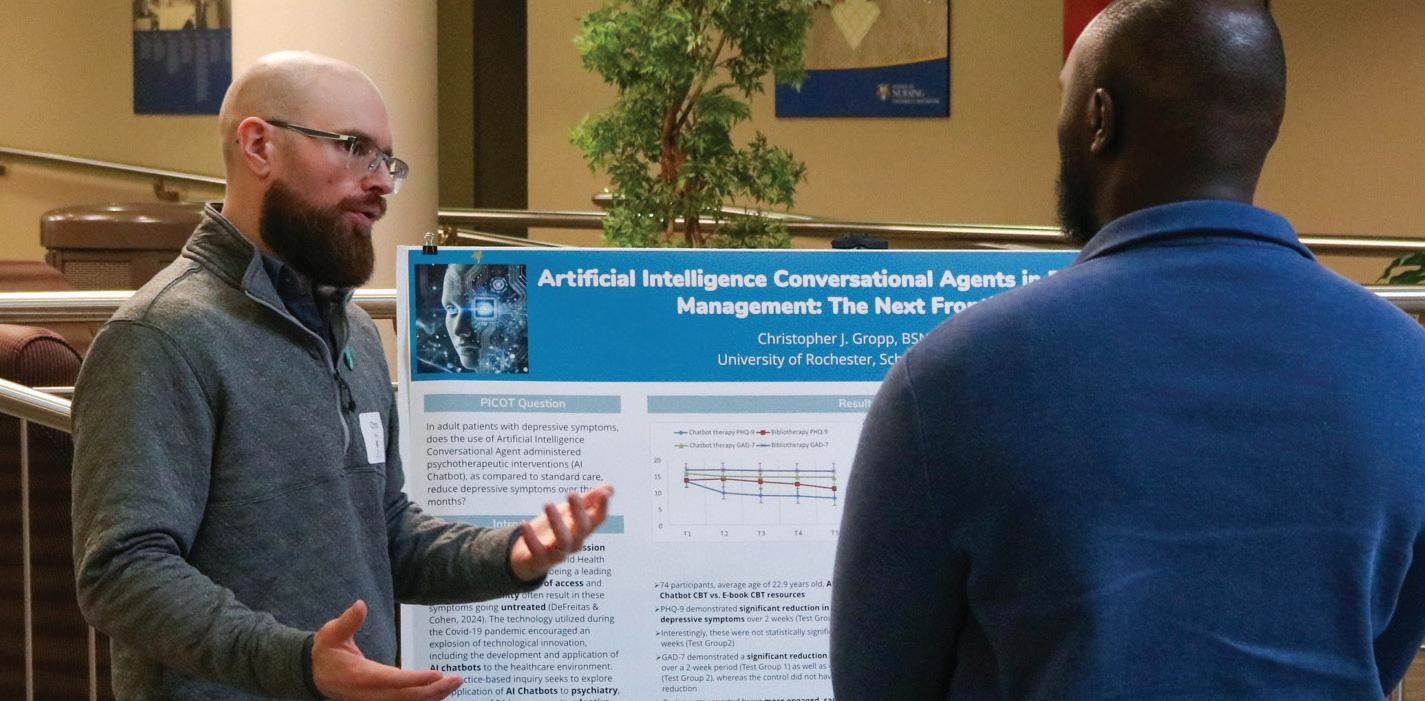
Christopher Gropp, a 2025 alumnus of the Psychiatric Mental Health Nurse Practitioner program, presents his work at the program’s annual capstone celebration.

Accelerated bachelor’s students, under the direction of Assistant Professor of Clinical Nursing Leann Patel, provided hearing and vision screenings for children at elementary schools in Williamson and Gananda, New York, as part of their community health clinical experience.

Psychiatric Mental Health NP students and faculty gather for the program’s annual capstone celebration, wearing green in honor of Mental Health Month.



UR Nursing welcomed students from East High School for its semester-long career exploration program, under the direction of Master’s in Nursing Education students, faculty, and alumni.

The PhD in Nursing & Health Science program held its annual PhD Research Day in May, during which students showcased their areas of research interest to faculty and fellow students, and shared dissertation research in various stages of development.


Allergy Advocates New York volunteers Melissa Mueller-Douglas and Toni Taylor visited the School of Nursing to lead an “Epi Near You” emergency anaphylaxis training for accelerated bachelor’s students.

Assistant Professor Lauren Ghazal, Dean Lisa Kitko, and Senior Associate Dean for Research Sally Norton celebrate the news that the National Cancer Institute (NCI) named Wilmot Cancer Institute as the nation’s 73rd designated cancer center.
At the annual I Heart SON Day, students, faculty, and staff wrote thank-you notes to alumni and supporters and shared their own reasons the School community is special to them.


Congratulations to Susan W. Groth, PhD, WHNP-BC, FAANP, ’93N (MS), ’04N (PhD), newly installed as the Ruth Miller Brody and Bernard Brody Professor, who was recognized for her research expertise in maternal and child health and women’s wellness. Salah Al-Zaiti, PhD, RN, CRNP, ANP-BC, FAHA, was also honored and installed as the Independence Foundation Chair of Cardiovascular Nursing for his groundbreaking work in emergency cardiac care and AI-driven clinical innovation.
Geriatric Workforce Kept Pace with Aging Population,
But Significant Rural Disparities Persist Professorship Installations

A new study in JAMA Network Open finds that the combined workforce of geriatric physicians and nurse practitioners kept pace with the rapidly growing older U.S. population from 2010 to 2020. Led by Ying Xue, DNSc, RN, the Loretta C. Ford Endowed Professor in Primary Care Nursing, the research highlights a dramatic rise in geriatric NPs as a key factor in meeting demand. However, nearly two-thirds of U.S. counties still lack any specialized geriatric professionals, with the greatest shortages in rural areas that have smaller older populations, lower socioeconomic status, and fewer healthcare resources.
“To address geographic disparities in geriatric care access, we must implement targeted policies that both incentivize healthcare professionals to serve rural communities and support the financial sustainability of healthcare facilities in these underserved areas,” said Xue.
With the older adult population expected to grow by 25 million by 2040, underscores the urgent need for strategic workforce development to ensure comprehensive older adult care. The research was supported by the University of Rochester and included co-authors from Columbia University and the University of Gothenburg. Xue received support for the study from the Drs. Jeremy A. Klainer and Pamela York Klainer Endowed Dean’s Discretionary Award in Nursing.
Pictured from left: Sally Norton, senior associate dean for research, President Sarah Mangelsdorf, Sue Groth, Salah Al-Zaiti, Dean Lisa Kitko, and URMC CEO David Linehan.

Associate Professor of Clinical Nursing April Haberyan, PhD, MS, RN, CNE, has been named a distinguished fellow of the National Academies of Practice (NAP).
The NAP’s distinguished fellowship recognizes individuals who have made significant contributions to health care practice, research, education, and public policy. Founded in 1981, the NAP advises governmental bodies on health care, fosters collaboration, and advances patient-centered care. Fellows are elected by peers from various health professions.
Haberyan, who joined the School of Nursing faculty in 2022, is recognized for her extensive experience in behavioral and mental health and as a nationally recognized expert in disaster response.
“Receiving this recognition is truly an honor and a humbling acknowledgment of my work to advance behavioral and mental health, wellness, and disaster response,” Haberyan said. “This recognition motivates me to continue advocating for better mental health support, particularly in disaster response, and to further contribute to developing healthcare practices and policies prioritizing the well-being of first responders and communities in crisis.”
Haberyan earned her bachelor’s in nursing and master’s in adult psychiatric mental health nursing at the University of Rochester, along with a master’s in psychology and PhD in social psychology from the University of Nebraska-Lincoln. She began her career as a staff nurse on an inpatient psychiatric unit at Virginia Commonwealth University Medical Center, and has since served as an administrative director of a hospital mental health unit, health coach, behavioral health nurse educator, and nurse residency program manager.
As a recent Geriatric Faculty Scholar at the University of Rochester Aging Institute, Haberyan identified gaps in curriculum related to older adult care in the School of Nursing’s Accelerated Bachelor’s program, with the goal of developing geriatric educational content that can be nationally
A Champion for Mental Health and Disaster Response
April Haberyan Named Distinguished Fellow of National Academies of Practice
disseminated. In 2024, she earned first place in education posters at the American Psychiatric Nurses Association’s annual conference for a presentation highlighting her work with faculty colleagues to develop older adult mental health simulation for bachelor’s students, using the 4Ms Framework of Age-Friendly Health Systems.
Haberyan has also provided disaster mental health training to students in the U.S. and Macedonia and facilitated critical incident debriefings for first responders, helping them process the emotional toll of their work. At Northwest Missouri State, she helped create a campus-wide suicide prevention program.
As part of the NAP, Haberyan looks forward to extending her national impact.
“Being part of the National Academies of Practice offers a unique opportunity to collaborate with experts across disciplines and contribute to shaping healthcare practice, policy, and education,” Haberyan said. “I am especially excited about the potential to influence disaster response strategies and advocate for more comprehensive mental health care for first responders.”
“I believe my experience in interdisciplinary teamwork, disaster response, and healthcare education will enable me to offer valuable insights. I am eager to work alongside others who share the commitment to improving healthcare for individuals in crisis and the professionals who serve them.” Haberyan shared her gratitude for the faculty, mentors, and leadership who have supported her as a disaster responder, educator, nurse residency program manager, campus suicide prevention program developer, and wellness coach.
“Their guidance, encouragement, and unwavering commitment to the mission have been invaluable,” she said.

Celebrating the impact of Faculty and Staff
Feelings of gratitude filled the room as School of Nursing faculty and staff celebrated the annual End of Year Awards on May 28.
“We graduated more than 200 outstanding students, continued to teach and mentor the next generation of nurses, made new discoveries in how we care for people from all backgrounds, and expanded access to quality care in our communities,” said Dean Lisa Kitko, PhD, RN, FAHA, FAAN “Every one of you has played a part in these achievements, and I am deeply grateful.”
The following faculty and staff members were honored with special awards, recognizing their contributions to education, research, clinical practice, and the School’s overall workplace culture and community:
Drs. Jeremy A. Klainer and Pamela York Klainer Endowed Dean’s Discretionary Award in Nursing:
Assistant Professor Lauren Ghazal, PhD, FNP-BC: “APP-ONC: Advanced Practice Providers Caring for Cancer Survivors Outside of Oncology Settings”
Assistant Professor Dillon Dzikowicz, PhD, RN, PCCN: “Bridging Innovation and Impact: Establishing the Cardiovascular Physiological Nursing Hub”
Mary Dombeck Award: Associate Professor and PhD Program Director Marie Flannery, PhD, RN (faculty)
Peter Bertoldo, MBA (staff)
Most Promising New Investigator: Dillon Dzikowicz
Professional Advancement Award: Lauren Ghazal
Outstanding Scholarly Practitioner Award: Laura Paytash, DNP, APRN, FNP-BC, graduate clinical education co-coordinator and simulation educator
Outstanding Faculty Colleagues: Susan Stanek, PhD, MSN/Ed, RN, director of the Center for Lifelong Learning, and Kathy Hiltunen, MBA, RN, assistant professor of clinical nursing
Outstanding Staff Colleague: Eric Eggert, educational media specialist
Outstanding Staff Member of the Year: Elaina McKie, PhD administrator and manager of academic program support
Dean’s Appreciation Award: Senior Associate Dean for Research Sally Norton, PhD, RN, FNAP, FPCN, FAAN

Recognizing Our Retirees
The following retirees were also celebrated for their years of service, leadership, and lasting contributions and impacts.
Patrick Hopkins, DNP, APRN, C-PNP, NNP, retired after 31 years at the University, and 20 at the School of Nursing. As specialty director of the Neonatal Nurse Practitioner Program, former co-director of our accelerated bachelor’s program, and a beloved teacher and colleague, Patrick brought an energy, humor, and passion to the School that have made a lasting difference for students, faculty, and staff.
Lynne Massaro, DNP, RN, FNP-C, ANP-BC, FAANP, retired after 16 years at the School and 20 years at the University, where she served as Specialty Director for both the Family Nurse Practitioner and Adult-Gerontology Primary Care NP programs. She is recognized for launching the nurse practitioner residency program at Highland Family Medicine, and for her dedication to clinical education, global health initiatives, and mentoring future nurse practitioners.
John McIntyre, MS, RN, CNL, CCRN-K, retired after 43 years at the University and 17 years at the School, where he advanced simulation and experiential learning for nursing students. He played a key role in developing interprofessional education, bringing together nursing and medical students for collaborative, real-world training. McIntyre’s leadership in critical care and commitment to student success have left a lasting impact on the School and its graduates.
Linda Migliore, MS, RN, NPD-BC, CNL, retired after 44 years at the University and five years teaching at the School, where she led the Clinical Nurse Leader and Leadership in Health Care Systems programs. In 2025, she received the Dean’s Teaching Award at Commencement in honor of her dedication to mentoring students and building strong academic-practice partnerships. Her legacy includes shaping

curriculum, inspiring future nurse leaders, and leaving a lasting impact on the School and its community.
Lisa Norsen, PhD, RN, ACNP-BC, retired after an extraordinary 35 years at the School and 48 years with the University. Norsen has been recognized as a true pioneer in nursing, a dedicated leader, and a champion for wellness and innovation.The UR Nursing alumna was one of the nation’s very first nurse practitioners to practice in an acute care setting. Her leadership has shaped our programs, inspired her colleagues, and improved the lives of countless individuals in our community, most recently as she served as the chief wellness officer for our employee wellness programs.
Lydia Rotondo, DNP, RN, CNS, FNAP, who served as the driving force behind UR Nursing’s education mission and graduate programs, is retiring after leading as senior associate dean for graduate education & innovation and director of the DNP program. She launched the annual DNP Summit, guided the School through a successful 10-year reaccreditation, and helped the School earn national honors like the Apple Distinguished School designation and National League of Nursing Center of Excellence status. Rotondo’s leadership brought significant change: she expanded DNP program access for master’s-prepared nurses, championed the use of simulation in clinical education — helping pass new state legislation — and created innovative programs like the iROC mobile learning initiative. Her vision and advocacy have made a lasting difference for our students, faculty, and the future of nursing.
Doctor of Nursing Practice (DNP) candidates and faculty surprised Lydia Rotondo with a cake at the annual DNP Project Day to celebrate her Summer 2025 retirement; Sally Norton received the annual Dean’s Appreciation Award from Dean Lisa Kitko at the annual Faculty & Staff Awards.
Professor Salah Al-Zaiti was an invited speaker at Stanford University’s Think AI healthcare conference, where he shared insights from his experience in designing and deploying intelligent AI-ECG tools in clinical settings.


RBNA Advocacy Day: Kristina Santory and accelerated bachelor’s student Taylor Le Blanc attended the National Black Nurses Association’s New York State Advocacy Day in Albany, where they spoke with local legislators about affordable housing, gun violence, the opioid epidemic, mental health access, and Black maternal health.


Faith Carini-Graves, a psychiatric nurse practitioner and liaison in the AACN Graduate Student Nursing Academy, presented a poster on her DNP scholarly project to design a quality improvement initiative to standardize the workflow of crisis management in a community-based psychiatric setting at the AACN Doctoral Education Conference. She is photographed with Lydia Rotondo, former director of the DNP program, and current interim director Susan Ciurzynski.

Instructor of Clinical Nursing Kristina Santory and Director Assessment and Academic Innovation Tara Serwetnyk presented at the Apple Nursing Education Forum, where they shared how the School is using innovative tools and digital solutions to empower both educators and students, enhance clinical learning, and prepare future nurses for success in a technology-driven world.
Congratulations to PhD student Kofi Gyasi Agyei, who earned third place in the University’s International Graduate Student Research Showcase with the poster presentation “Factors Associated with Knowledge and Attitudes Toward Palliative and Care for the Dying among Undergraduate Nursing Students.”
Faculty and doctoral students from the School of Nursing share their work at the Eastern Nursing Research Society’s annual Scientific Sessions in Philadelphia.
Leading the Way in Cardiovascular and Stroke Care

National Research Innovation Awarded
Professor Salah Al-Zaiti, PhD, RN, CRNP, ANP-BC, FAHA, received the AHA Council on Cardiovascular & Stroke Nursing’s (CVSN) 2024 Research Article of the Year Award. Al-Zaiti is part of a national research team that is developing an artificial intelligence-based (AI) clinical decision-making support tool to better classify chest pain among emergency department patients.
The team developed an algorithm, trained by data from more than 7,000 patients from multiple U.S. sites and who had chest pain without the obvious ST elevation of a heart attack, to identify who might have heart attacks and help providers make diagnoses more quickly and accurately. Their research findings are published in Nature Medicine.
Al-Zaiti is a previous recipient of the CVSN Council’s Martha N. Hill New Investigator Award, and helped develop the AHA’s 2020 guidelines for preventing and mitigating the risk of exercise-related adverse cardiac events.

School of Nursing Faculty and Dean Earn National Honors and Shape the Future of Heart Health at the American Heart Association’s Scientific Sessions
Excellence in Stroke Care Recognized
Ann Leonhardt-Caprio ‘06N (MS) ‘20N (DNP), assistant professor of clinical nursing and program coordinator for the UR Medicine Comprehensive Stroke Center, won the Excellence in Clinical Practice Award.
“Recognition from my peers inspires me to continue striving for excellence, fostering collaboration, and advancing the field of stroke care to benefit patients and the nursing community alike,” Leonhardt-Caprio said.
Locally, she has contributed to efforts to reduce readmissions, evaluate nursing care for stroke patients, and establish a collaborative group across the UR Medicine Health System to address system-wide stroke care needs. Nationally, Leonhardt-Caprio has been an active volunteer in the CVSN Council’s Stroke Nursing Committee. She previously received the 2022 Stroke Article of the Year Award, as well as the AHA New York chapter’s Leadership Legacy Award.
“This award has inspired me to provide mentorship and guidance, helping others advance their careers,” she said. “I see tremendous opportunities to foster clinical scholarship, cultivate the next generation of nurses, and strengthen interprofessional partnerships.”
National Leadership in Palliative Care
Dean Lisa Kitko, PhD, RN, FAHA, FAAN, began her term as chair of the AHA’s CVSN Council and co-authored the AHA’s scientific statement on palliative care and cardiovascular disease in adults.
The statement emphasizes a need for palliative care services and support for both individuals and their care partners, and that effective communication, shared decision-making, age-friendly care principles, and advance care planning can significantly improve quality of life for people living with cardiovascular disease.
“Palliative care isn’t just about the end of life — it’s about improving overall well-being and quality of life for both patients and caregivers,” Kitko said.

Palliative Care and Advanced Cardiovascular Disease in Adults: A Scientific Statement From the AHA
Remembering Loretta C. Ford 1920-2025


Founding
Dean, University of Rochester School of Nursing
Former Director of Nursing, University of Rochester Medical Center
How Loretta Ford’s Vision Continues to Transform Healthcare
When Dr. Loretta C. Ford passed away this January at the age of 104, the nursing world lost not just a pioneer, but a force. A visionary who reshaped the very contours of healthcare, Dr. Ford co-founded the nurse practitioner role and championed the bold idea that nurses could lead, teach, and heal on new frontiers. Her passing stirred a global wave of tributes — from colleagues, students, and the nearly 400,000 nurse practitioners whose careers exist because she dared to ask, “Why not us?” The global coverage of her passing, spanning outlets like the New York Times, BBC, and Wall Street Journal, echoed the reach of her influence and the legacy she leaves behind.
But if her life has come to a close, her legacy remains vividly alive at the University of Rochester and around the world. It pulses through the hospitals and clinics where NPs deliver life-changing care. It resonates in every academic health system shaped by her Unification Model. It lives in the daily practice of nurse leaders who carry forward her vision, integrating research, education, and compassionate care.
This fall, as we prepare to honor Dr. Ford with a special tribute during Meliora Weekend, we look back not only at what she built — but at what she made possible. The voices in this spread are just a glimpse into the deep admiration and gratitude she inspired. Each quote, each milestone, reflects the impact of a woman who didn’t just transform nursing, she transformed lives.
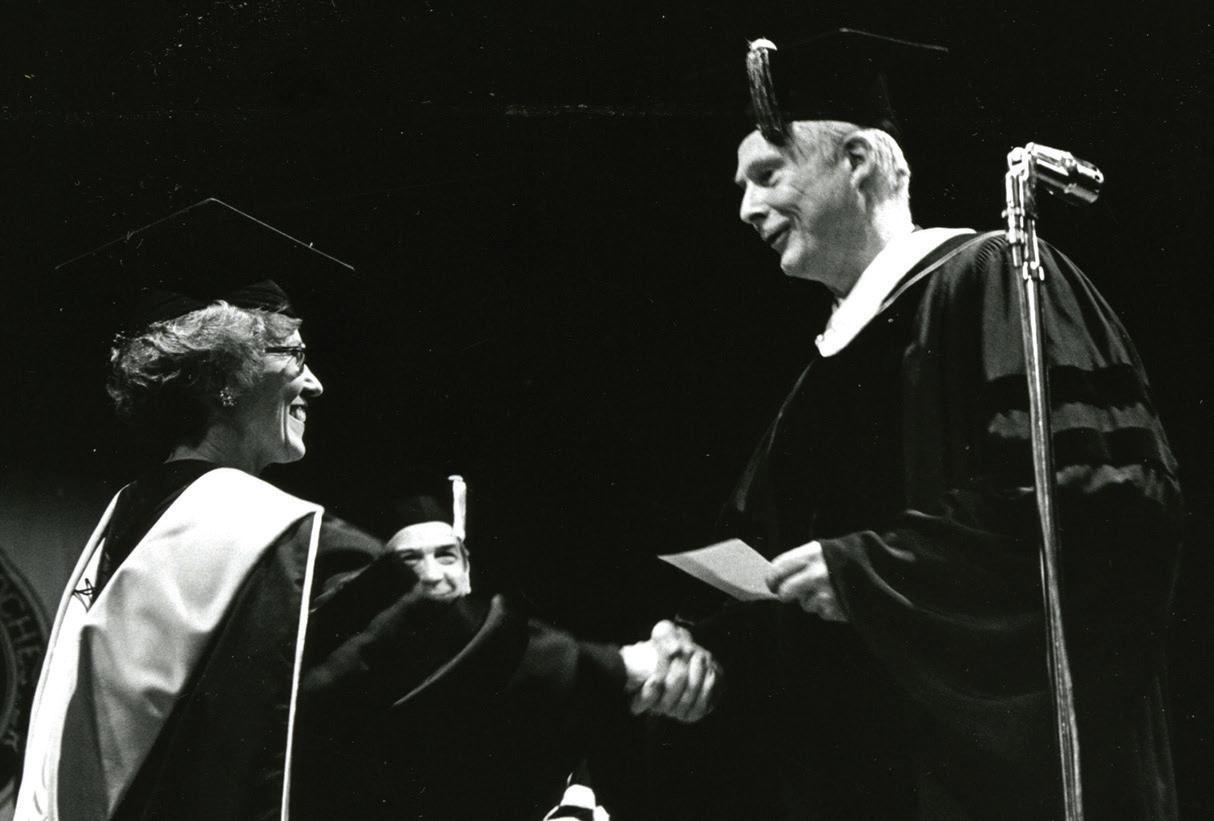
Dr. Ford with W. Allen Wallis at her installation as dean of the School of Nursing in 1972. During her speech, Ford called for a new order for nursing’s direction in education, research, and practice with the University of Rochester School of Nursing in the forefront as a national trend setter for improving the delivery of health care.
“What is new will be an effort to adopt a philosophy of joy in change, to view change as opportunities to gain new insights, to drink deeply into the joys of discovery, and to participate in an adventure. This is truly a day of a ‘new order of things.”
Dr. Ford’s Legacy at Rochester
When Dr. Loretta Ford arrived in Rochester in December 1972, she brought a vision that would forever change nursing education and practice. As the founding dean of the independent School of Nursing at the University of Rochester and director of nursing at Strong Memorial Hospital, Ford championed innovation, collaboration, and a commitment to both scholarship and service. Her leadership came at a pivotal time: the school had just launched pioneering nurse practitioner programs, and the proximity to the Medical Center enabled Ford to foster an environment where interdisciplinary teamwork thrived. The nurse practitioner model she introduced at the University of Colorado found fertile ground at Rochester, quickly becoming a national exemplar.
Ford’s most enduring legacy is the Unification Model, which bridged her dual roles and created a collaborative culture across education, research, and clinical care. This model empowered nurses to conduct their own research and put Rochester in the national spotlight as a leader in nursing education.
Over her 15-year tenure, the school launched the nation’s first acute care nurse practitioner program, developed faculty training in primary care, and was among the first to offer doctoral education in nursing. Today, more than 2,000 nurse practitioner graduates from Rochester—and nearly 400,000 nationwide—trace their professional roots to Ford’s vision.
Dr. Ford’s willingness to challenge the status quo, her curiosity, and her optimism continue to inspire the University of Rochester School of Nursing, setting a standard for excellence that endures more than 50 years later.

Dr. Ford signing a steel beam at an event for the Loretta C. Ford Education Wing. The School of Nursing expansion featured four new classrooms and an auditorium. It opened in 2006.
Impact felt in Rochester and beyond
“As a junior nursing student, at convocation (1973), Dr. Ford told us she was not educating cookies but cookie cutters to lead and shape healthcare. Then we added some baking soda and turned healthcare upside down. What a champion and mentor!”
Susan Terwilliger ’79N (MS)
Clinical Associate Professor at Binghamton University
“I met Lee as a Robert Wood Johnson Nurse Faculty Fellow. Lee was one of the leaders of that RWJF-funded program and was a consistent source of mentorship, support and advocacy for what we were doing. Lee led with her wisdom, her risk taking, her innovative spirit, and her wonderful sense of humor. I was honored to be one of the individuals who signed the beams of her named building there at the University of Rochester. And as we worked at AACN to reshape acute care practice, Lee came and spoke to tell us about her journey to create nurse practitioner education and practice. She said crises are not a bad time to do innovative risk taking. Crises are the exact time to push for innovation and new beginnings. And she did this wearing her wonderful Super Woman outfit as she strode into the room and stood on top of one of the tables. Lee, you were an inspiration, and your warmth and generosity will be sorely missed.”
Geraldine Polly Bednash, PhD, RN, FAAN Former CEO of American Association of Colleges of Nursing
“I had the privilege of knowing Dr. Ford for many years and she was in every way an amazing person. She encouraged me to become one of the first acute care nurse practitioners and inspired me to advance my career through education and exploration — never to be afraid to try something new or think in a different way. She touched so many people in so many ways. Her wisdom, energy and spirit shaped nursing as we know it today and her legacy will guide us for years to come.”
Lisa Norsen, `77N, `83N (MS), `07N (PhD), `92N (PMC) Former Chief Wellness Officer, UR Medicine Employee Wellness Professor of Clinical Nursing, University of Rochester School of Nursing
“In January 1972, I was hired as assistant chairman for graduate studies in the Department of Nursing and six months later transitioned to assistant dean for graduate studies, when Lee Ford became founding dean of the new School of Nursing and director of nursing in the Medical Center. We had a small, regional master’s program at the time and, under Lee’s leadership, we rapidly developed master’s-level NP degree programs from the existing pediatric and medical NP certificate programs led by Harriet Kitzman and Evan Charney and Barbara Bates and Joan Lynaugh. We also had the model of the Rochester Regional Medical Program that included outstanding faculty who were clinical nursing leaders as well as educators and early clinical researchers. Lee worked hard to link the nursing education with the clinical side in her unifying vision.
Those first years under Lee’s leadership were a whirlwind experience. Change was always in the air. Lee’s vision of unification kept her on the road a lot, bringing visibility to her vision and funding to develop programs. She propelled all of us into a tripartite set of individual expectations-research, teaching and clinical roles. She stayed ‘on task,’ determined to realize her vision of unification and, I think, she had more confidence in faculty ability to realize that vision with her than we had ourselves. Those first five years were very demanding [and that’s not to say the later years of her Deanship were not…. In 1979, we opened one of the early PhD programs in nursing].
As a young, untenured assistant professor, I was asked to lead her first five-year Dean’s review for the University. I did, and she never held it against me! In fact, the last time I wrote her was this past Christmas. Thank you, Lee, for bringing us all along with you on this amazing visionary nursing journey. You remain in my heart.”
Madeline Schmitt, PhD, RN, FAAN, FNAP
Professor Emeritus, University of Rochester School of Nursing
Ford during a 2015 visit to the University’s School of Nursing to celebrate the 50th anniversary of the nurse practitioner profession.


CHANGERS GAME for


Loretta Ford transformed the nursing profession by establishing the nurse practitioner role, linking education, research, and clinical practice.
This fall, celebrate her groundbreaking vision and 100 years of the University of Rochester School of Nursing at Carrying the Vision Forward: A Tribute to Loretta Ford’s Legacy in Nursing and Healthcare—a special event honoring her impact and the bold future of nursing.
Don’t miss this and other unforgettable events during Meliora Weekend. Registration opens this summer.
Learn more at rochester.edu/melioraweekend
SEPTEMBER 18-21, 2025
#melioraweekend
Honoring the Legacy of Kathy Rideout: A Visionary Leader Who
Led with Heart
Celebrating a life of compassion, innovation, and a deep commitment to the future of nursing.

Kathy Rideout, EdD, PPCNP-BC, FNAP, former professor of clinical nursing and pediatrics and dean emerita, passed away February 28 at the age of 67. For more than 35 years, she served the University of Rochester community as a nurse practitioner, educator, scholar, and beloved dean. Kathy was a visionary leader, a compassionate clinician, and a steadfast champion for her students, colleagues, and patients. Her influence extended far beyond the University, inspiring generations to lead with empathy, excellence, and purpose.

Her Enduring Impact
As dean, Kathy Rideout guided the School of Nursing through a time of tremendous growth and transformation. She championed groundbreaking research, expanded the school’s facilities, and built a culture that embraced every student, colleague, and patient with openness and respect.
She helped establish the UR Medicine Center for Employee Wellness, led a major expansion of Helen Wood Hall, and launched the Dean’s Diversity Scholarship—



making the path to a nursing career more accessible for future generations. Her leadership was deeply personal: she greeted students by name, mentored with care, and never lost sight of the patient as the center of it all.
Kathy’s commitment to diversity, equity, and inclusion helped shift the conversation in nursing—not only at Rochester, but nationally. She broke barriers by example, and her impact continues to shape the profession in powerful ways.
Remarkably, even while leading at the highest level, Kathy remained a practicing pediatric ostomy nurse. Her clinical work was more than a responsibility—it was a reflection of her belief that great leaders stay close to the heart of the work.
“She built a culture of excellence, compassion, and inclusion — one that continues to guide us every day. The School of Nursing will honor her legacy by carrying forward the vision she so thoughtfully established.” — Lisa Kitko, PhD, RN, FAHA, FAAN, Dean of the UR School of Nursing
“Kathy helped me to realize that my intellect, drive, and life experiences were valued contributions. That moment changed my life because it set me free to act as a full member of the University community, and I have since thrived.” — LaRon Nelson, ’02N, ’04N (MS), ’09N (PhD), Yale University
“Even as dean, she remained deeply connected to clinical practice, providing consults for NICU patients with complex wounds and ostomies. Her dedication to increasing the diversity of the student body has strengthened the diversity of nursing practice across our medical center.” — E. Kate Valcin, DNP, RN, Chief Nursing Executive, URMC
“Kathy embodied the true integration of nursing education and practice, showing us all that leadership means never

forgetting why we entered this profession in the first place.”
– Jill Halterman, MD, MPH, chief of pediatrics at Golisano Children’s Hospital
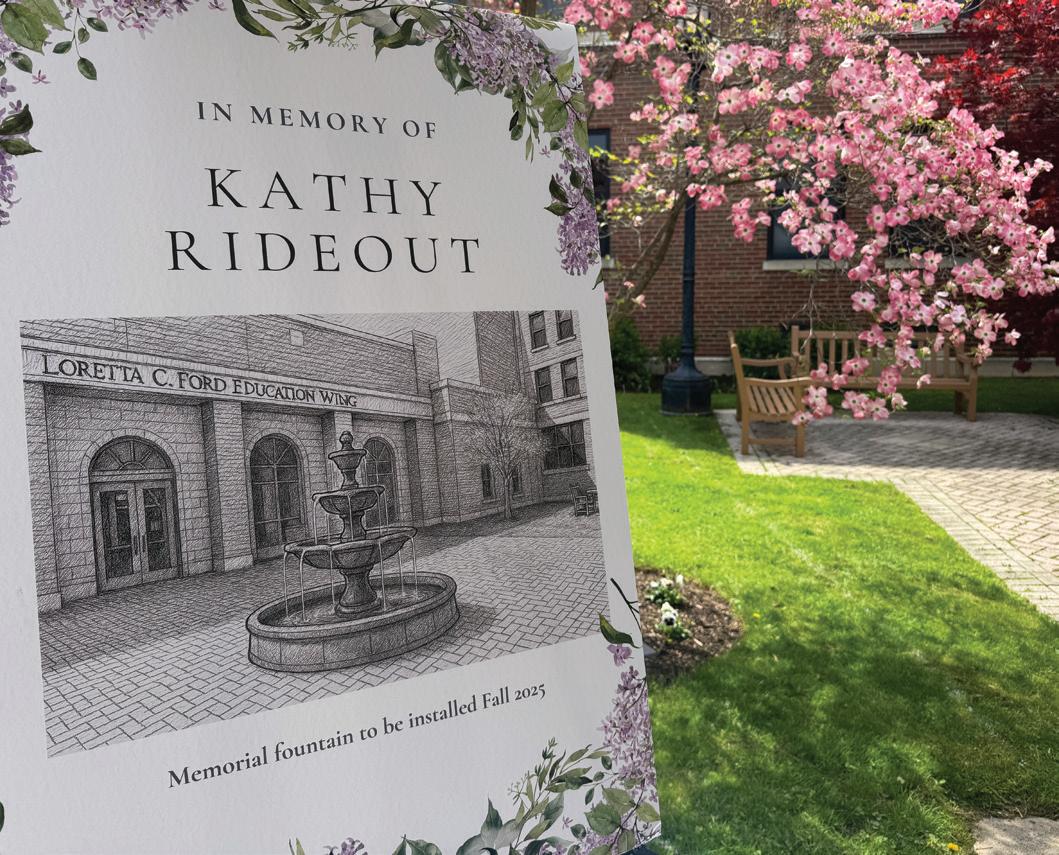
In May, the School of Nursing community gathered to honor Kathy’s life with a celebration full of memories, laughter, and gratitude. Colleagues, former students, and friends shared stories that reflected her extraordinary warmth and the countless lives she uplifted.
This September, a new fountain will be dedicated in the School of Nursing courtyard—a permanent tribute to a leader whose compassion and vision continue to ripple outward.

Read the full tribute and explore personal stories of Kathy’s lasting legacy.
Charting New Waters

How a nurse-led workplace wellness program is changing the course of preventative care.
Every year, Calvin Cole, PhD, takes 20 minutes for a biometric screening appointment with UR Medicine Employee Wellness to stay ahead on his health.
The assistant professor and cancer researcher has a family history of diabetes and pays special attention to his blood glucose levels. The Employee Wellness program, founded and housed at the School of Nursing, is distinguished by its screenings with point-of-care testing, personalized online wellness portal with access to year-over-year results, and robust catalog of lifestyle and condition management coaching.
“I love that I can track my numbers year after year,” he said after a recent screening at Strong Memorial Hospital. “My screenings have given me the knowledge to adjust my lifestyle in real-time.”
Cole is among more than 30,000 University of Rochester employees who are eligible to utilize the nurse-led Employee Wellness program. The reach extends beyond the University community too: the Center for Employee Wellness is now celebrating its tenth anniversary of delivering life-changing programs to external clients. It has grown to serve 85 organizations throughout Western New York, ranging
from school districts to manufacturers, impacting nearly 70,000 individuals.
Recent research shows that the program has significant health and financial benefits for those who participate.
A December study in the journal Healthcare found that across all levels of cardiovascular disease risk, cost-savings for individuals participating in Employee Wellness programming were $1,224 per person, or a $4.90 return on investment for every $1 spent. Among employees with a
moderate to high cardiovascular disease risk who


participated in Employee Wellness, 48 percent improved their risk compared to the predicted risk, and 33 percent improved by a full category.
“Being able to quantify the impact of Employee Wellness through a peer-reviewed journal is a reaffirmation that we are effectively meeting the needs of the populations we work with,” said Renu Singh, MS, CEO of UR Medicine Employee Wellness. “There is no cookie-cutter approach when it comes to wellness. We are embedded in the communities we serve and passionate about making wellness work through personalized, tailored programming.”
The Rochester-based Smola Consulting, a benefit and wellness consulting firm, is among the organizations whose employees have been impacted by the programming UR Medicine Employee Wellness offers.
“By addressing key issues such as stress management and chronic disease prevention, and by empowering individuals to take charge of their health, these programs are steadily becoming a must-have service at workplaces,” wellness consultant Dan Justis said of the program in an interview with Rochester Business Journal. “The result is a healthier, more connected, and more resilient community for all.”
In addition to partnering with other organizations, the School of Nursing is also looking to incorporate its model for workplace wellness and value-based care into UR Medicine’s primary care system, bolstering access to preventative care through disease management coaching and enhanced patient education.
“This project will help to remove barriers and fill gaps in care by identifying patients at risk and connecting them to comprehensive disease management services that have
a demonstrated impact in improving health, reducing the cost of care and risk of cardiovascular disease,” Singh said. “Our coaching program is primary prevention, which addresses modifiable risk factors and promotes healthy lifestyles.”
Saving Money, Saving Lives
Evidence of Employee Wellness’ return on investment is good news for both workers and employers, given that about one-sixth of annual healthcare spending is attributed to the treatment of cardiovascular disease, and nearly half of adults in the U.S. have it, according to the Centers for Disease Control and Prevention.
Overall, chronic disease affects 60 percent of adults, accounting for three-fourths of healthcare spending – but many of these conditions are linked to lifestyle choices. That’s where Employee Wellness steps in, aiming to empower individuals to take charge of their health with the right support.
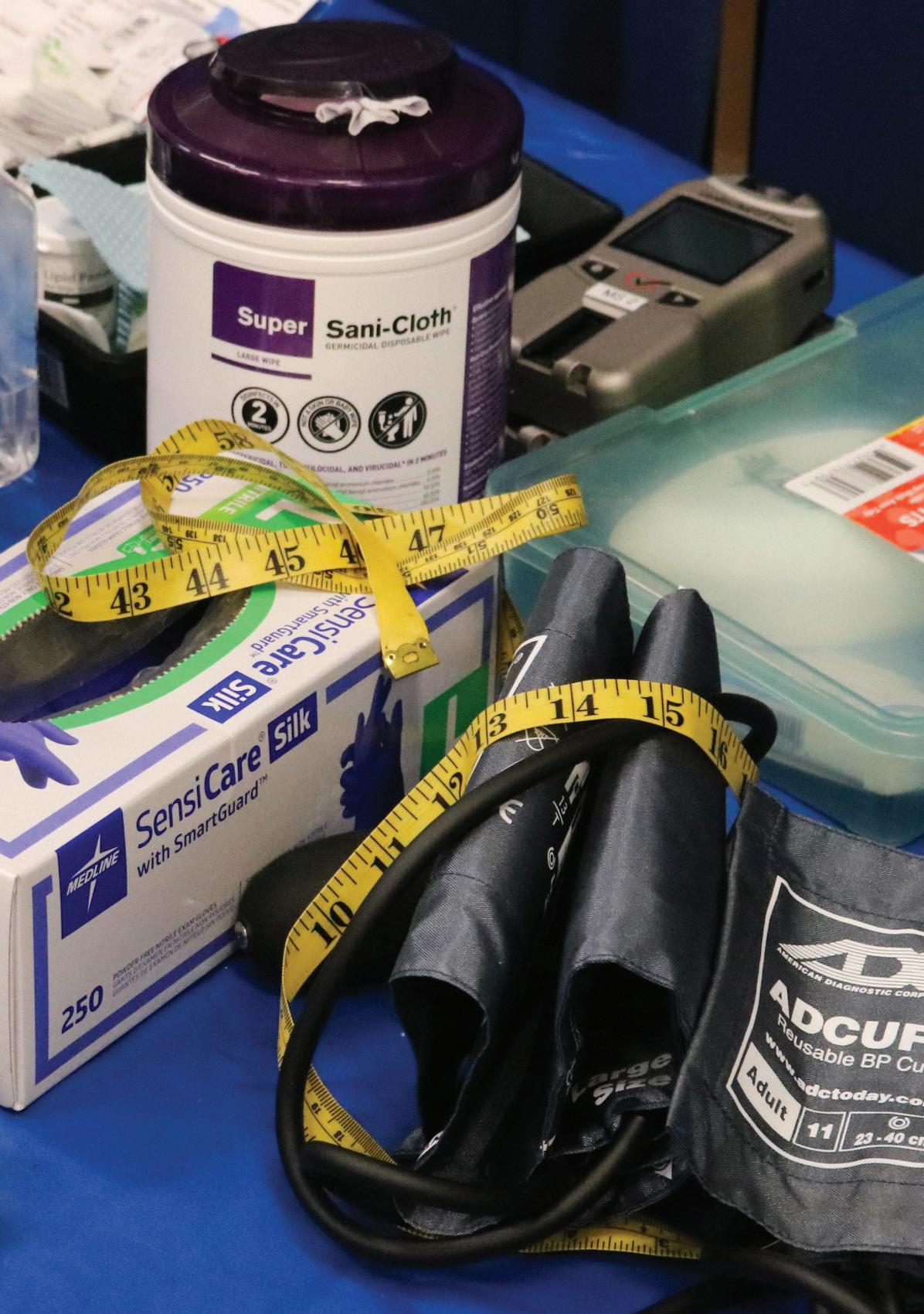
Signing up for a biometric screening is often the first step, as it helps identify risks and determine next steps. At these 20-minute appointments, a registered nurse measures patients’ blood pressure, heart rate, abdominal girth,

and BMI. They also take a small sample of blood through a finger stick to measure cholesterol, triglyceride, and blood glucose numbers within minutes. Eligible employees can receive $125 for completing both a screening and an online personal health assessment.
S. Craig Rooney, PhD, chief wellbeing officer at the University of Rochester Medical Center, emphasized the importance of the program after completing a biometric screening earlier this year.
“Wellness starts with each of us. It’s fantastic to have an opportunity right at work where taking just a few minutes for yourself is simple, incentivized, and effective. When we prioritize our health, we bring our best selves to work and life,” he said.
Charting CEW’s Next Steps
Employee Wellness continues to expand its programming and evolve to proactively address Western New Yorkers’ various healthcare needs today. In 2024, the Wellness team added two new disease management programs for irritable bowel syndrome/disease and osteoarthritis, and a one-on-one coaching program for women experiencing menopause and perimenopause.
“We see over 13,000 people a year in our biometric screenings, the majority of whom are women. These women often talk about their unique health needs as a female, especially as they experience perimenopause and menopause,” explained Lisa Norsen, PhD, RN, ACNP, the recently retired chief wellness officer for Employee Wellness. “Although this is a normal part of a woman’s life, women often express awkwardness, embarrassment, or confusion or about their symptoms or think they just have to ‘suffer through it.’”
Norsen is confident that the new coaching program will offer the right support to help navigate menopause successfully and improve their quality of life, utilizing the latest evidence and best approaches for nutrition, exercise, sleep, sexuality, emotions, and medications.
“We want every woman to know how to be their best as they enter this phase of life,” she said.
The program is reflective of the Employee Wellness team’s overall goal for the decade ahead: to continue providing programs that are current, innovative, and responsive to emerging health needs in the Rochester region.
“While there is no way to predict where we’ll be in 10 years, what we can do is promise to continue to hold ourselves to the highest standards as we raise the bar for employee wellness programs and give lifestyle medicine and prevention the spotlight they deserve,” Norsen said.
UR Medicine Employee Wellness is currently hiring wellness nurses. If you’re a licensed RN who is passionate about preventative care, health coaching, and empowering others, visit urson.us/join.

The Finger Prick That Saved My Life
Why You Shouldn’t Skip Your Biometric Screening
A simple decision to sign up for the biometric screening may have saved my life. Without the screening, I might not have discovered that I’m a type 2 diabetic until it became a serious, life-threatening emergency. My hope is that my experience inspires you to take proactive steps for your health as well.
Initially, I signed up to get an extra $125 in my paycheck. Who doesn’t love a little extra money in their bank account?
I saw the screening as an easy way to get healthier and lean into self-care while earning a bonus. Before the screening, I hadn’t had any blood work or appointments in a while. The pandemic made it easy to neglect regular check-ups, and being neurodivergent, I didn’t recognize many physical signs and symptoms of type 2 diabetes that might have been red flags for my primary care provider (PCP).
The Screening
I did my screening on a Saturday morning at the YMCA close to home. The screening was simple enough—step on a scale, take some measurements, prick your finger—but that little drop of blood changed everything. My fasting glucose was alarmingly high for someone who didn’t have diabetes—over 300. That number meant nothing to me at the time, but I could sense a shift in the nurse who was educating me about each of my results in real time. She asked if I was diabetic. I said, “I don’t think so.” She was concerned and taught me about the signs and symptoms of hyperglycemia before recommending that I call my doctor first thing Monday morning.
Determined to be proactive, I went to the pharmacy on the way home and bought a glucose meter. I tested over the weekend, hopeful that the high reading at my screening was just a fluke. Unfortunately, it wasn’t. I was on the phone with my primary care provider’s office first thing Monday to schedule an appointment for later that week.
The ER Visit
Monday night, my blood sugar spiked into the 400s. I didn’t feel right, and my husband recognized some of those hyperglycemia symptoms the nurse had shared at the screening. I was scared, so we made our way to the ER. I met
Ashley M., copywriter at URMC

with several doctors, nurses, and a diabetes educator throughout the night. I learned that damage to the blood vessels can start with A1C levels above 7 percent, and the risk of significant long-term complications like blindness, nerve damage, heart disease, stroke, and kidney failure. My A1C was 11.4.
I received numerous insulin shots, but my sugar levels just weren’t responding, and I was admitted as soon as a bed was available.
After a short stay at Strong, I went home and felt immediately overwhelmed by my new routine: multiple daily insulin shots, a weekly Trulicity shot, metformin pills, and a continuous glucose monitor implanted in my arm. I was assigned a provider at the endocrinology office at URMC and signed up for the diabetes management program with Employee Wellness. I felt raw, both physically and emotionally.
The Results
Reflecting on this experience, I realize that I was in a dangerous place with my blood sugar. If not for the screening, I worry I could have gone to the ED in the back of an ambulance in a far more dangerous state, or that my health may have simply continued to deteriorate until permanent damage was done.
It’s been about two years, and my A1C is now 5.7, exactly half of where I started. I no longer need insulin and my monitoring continues to look awesome. I’ve lost weight and am better educated about carbs, protein, fat, and sugar. My experience spurred a shift in the way I experience my body and how I care for it.
I’m grateful for the biometric screening and the Well-U diabetes management program. They didn’t just change my life; they likely saved it. If you’ve been putting off your screening, I urge you to reconsider. It might just be the best decision you make for your health.

Celebrating Excellence
The 2025 Dean’s Diamond Circle Awards celebrate alumni, faculty, and supporters whose work is transforming healthcare, research, and communities worldwide. The UR School of Nursing handed out some of its highest honors at the annual Dean’s Diamond Circle awards dinner on April 11.

Distinguished Alumnus Award
Rita F. D’Aoust, ’76N, ’84N (MS), ’94N (PMC), ’06N (PMC), ’08W (PhD)
A trailblazer in nursing education, Rita D’Aoust is renowned for her leadership in curriculum innovation and workforce development. As an associate professor in nursing at Johns Hopkins, she advances nurse practitioner education nationwide and champions career pathways for veterans. Her legacy includes launching the UR School of Nursing’s Accelerated Bachelor’s program and pioneering high-fidelity simulation and technology in nursing.
Humanitarian Award
Orlando Harris ’10N (MS), ’14N (PhD)
Orlando Harris, associate professor of nursing at the University of California, San Francisco, is a global leader in health equity for sexual and gender minorities. His groundbreaking research and advocacy address stigma, violence, and climate justice, while his mentorship and policy work are shaping more inclusive health care for communities in California and worldwide.



Dean’s Medal
Nancy Dianis ’85N (MS)
A leader in global clinical research, Nancy Dianis has dedicated more than 45 years to advancing health initiatives on HIV, cancer, and chronic diseases. As vice president and associate director at Westat, she played a pivotal role in major international trials and epidemiologic studies. Deeply committed to the UR School of Nursing, Dianis co-chairs the School’s National Council and also serves on the University’s Campaign Planning Committee.
The annual celebration honored the significant contributions of School of Nursing alumni, former faculty, and supporters, from left: Orlando Harris, recent alumnus and speaker Diyor Mukhammadov, URMC CEO David Linehan, doctoral student and speaker Jamie Feingold, Rita D’Aoust, Debbie Kamarck, and in the front, Dean Lisa Kitko, Nancy Dianis, and University President Sarah Mangelsdorf.
Legacy Award
Debbie R. Kamarck and Michael E. Kamarck, PhD, P’12, P’13
Debbie and the late Michael Kamarck, PhD, have dedicated their lives to advancing science, healthcare, and education, while fostering a deep commitment to family and community. Today, Debbie continues to champion access to healthcare and education for women and children, supporting scholarships and nursing programs. Their shared legacy continues through their family, philanthropy, and enduring commitment to service.

From Mentee to Mentor
Through nursing education, Sarah Corsette gives back to future nurses

Sarah Corsette ’22N (MS), RN, MEDSURG-BC, has known since high school that she wanted to pursue a career in nursing.
A program at her high school offered an opportunity to shadow nurses for college credits, and wise advice from her mother affirmed her choice. “Sarah, you would always have a job,” she remembers her mom telling her.
At the time, Corsette was a reserved, observant kid, but growing up playing sports taught her early on that she could thrive in a team environment. She envisioned herself working at the bedside, not knowing at the time how many doors a registered nurse role would open — or how much a career in nursing would shape her confidence and leadership skills. Corsette began her career as a medical-surgical nurse at the University of Rochester Medical Center (URMC), but she felt an urge to expand her role.
She found inspiration for what to do next in her own unit: Acute Medicine colleagues and fellow alumnae Courtney Hallmark ’18N (MS), ’22N (MS), ’24N (DNP) and Chanea Dougherty ’18N (MS) influenced Corsette to consider a Master’s in Nursing Education.
“Chanea was teaching at the School of Nursing, and Courtney was the nurse educator on my floor. As I interacted with the students on my floor and saw how my own mentors functioned in their roles as educators, that became my biggest reason to want to go back to school,” Corsette said.
“Now, my former students are nurses on my floor, and they’re charge nurses and preceptors. It’s amazing to mentor students and see their growth, and to remember that I have been mentored at some point too,” she said.
In addition to her work as an RN, the master’s-prepared nurse educator is serving as the Unit Shared Governance Council leader on URMC’s Professional Nursing Council, secretary of the Finger Lakes Organization for Nursing Leadership, and an adjunct clinical instructor at Nazareth University. She shares her journey into nursing, education, and leadership:

Can you tell us what your role in the Professional Nursing Council is like?
I spend 24 hours per week on my floor as a bedside nurse, and 12 in my PNC role. As the unit-based shared governance leader, I oversee all of URMC’s unit councils. It has been exciting to break out of my med-surg bubble and connect with people across the University. I hold monthly meetings where council chairs can present on the work their units are doing, practice public speaking, and learn foundational skills like how to navigate conflicts or run a meeting.
What was your experience as a Nursing Education master’s student like?
When I first knew I wanted to pursue my master’s, I thought, “I need a buddy to do this with.” Three friends and I started the program together, and we all supported each other through school and watched each other grow. All of the professors have been great, such as Maria Marconi, Lauren Lee, Sue Stanek, and Deanna Drexler, who helped me feel confident as an educator. Dee Dee Rutigliano has been an incredible mentor to me; she supported me throughout the program and encouraged me to pursue certifications.
What helped you balance work and school?
I took it slow. I finished my degree over three years, taking one course a semester while working part-time. I had a supportive leadership team, and Strong has been supportive of higher education and nurses going back to school. My nurse manager was flexible with my schedule, classes, and assignments, and that made a big difference.
What tips would you share with nurses who might be considering a leadership role?
Say yes to new opportunities (and recognize when you need to start saying “no”). Leaning into the uncomfortable has always paid off for me in the long run!
What’s something you wish you knew before you started nursing?
Don’t do too much at first. Then, get involved. I know it can be intimidating and overwhelming jumping into nursing. I always tell new employees to take at least six months before joining a committee, to understand what it is to just be a nurse.

Finding Purpose in Psychiatric Nursing
A career change to nursing led Faith Carini-Graves on a path to community-based care

Faith Carini-Graves ’22N (MS), ’25N (DNP) began her journey into nursing when she took on her first healthcare job as a home health aide. The former photographer was seeking a career change, and instantly felt a deep connection to the caregiving role.
Today, Carini-Graves is a psychiatric nurse practitioner and recent alumna of the Doctor of Nursing Practice program, and just recently finished a term as a liaison in the American Association of Colleges of Nursing’s Graduate Nursing Student Academy, through which she helped foster new professional development opportunities for fellow students.
While practicing in the community at the Hillside Family of Agencies, Carini-Graves utilized her DNP Scholarly Project to find ways to improve both provider and patient outcomes. Through Project CCRISIS – short for Community-based Crisis Response Intervention Strategies for Interdisciplinary Standardization – she designed a quality improvement initiative to standardize the workflow of crisis management for her multidisciplinary team of colleagues.
Carini-Graves shares insights on her career so far, and the power of the nursing role.
How did you discover an interest in nursing?
During high school and initially in college, I was aiming to be a photographer. I quickly realized that I didn’t want to connect with people primarily as a salesperson. I started out in healthcare as a home health aide and found the role of a healer to be much more my style. I enjoyed being creative to meet each unique patient’s needs.
Can you describe your current role in nursing and what makes it rewarding?
I absolutely love being a nurse on a healthcare team. We nurture unique relationships with patients and other professionals on our team strategically to meet the needs of the patients. Currently, I work on two interdisciplinary teams that provide psychiatric care to youth in the community. I use my relational skills, which are critical to the nursing approach, to show them that they can trust me and that we can work together. I also use clear communication and collaboration with my team so that we are providing coordinated and holistic care.
What is the most powerful part of being a nurse for you?
The most amazing thing about being a nurse, for me, is being in those human moments — even the difficult ones. We have such amazing access to key human experience moments. The power of nurses is knowing what to do in those intense human moments.

1970s
University of Rochester School of Nursing National Council member Diane R. Lauver ʼ78N (MS), ʼ87N (PhD) will receive the Lulu Wolf Hassenplug Alumni Award for Distinguished Career in Nursing from Vanderbilt University. This prestigious honor recognizes exceptional leadership, advancement of the nursing field, and lasting contributions to patient care, education, and research.
1980s
Retired Susan A. Flow ʼ81N writes that her journey in healing continues, inspired by the University of Rochester’s generosity bestowed on her. She continues to be inspired by the school’s leadership and contributions to the nursing profession as well as across the board collegial cooperative efforts. She’s designated the University as the recipient of her legacy, trusting its dedication to creating scholarship pathways for deserving students.

1990s
Bridgett C. Langstaff ʼ98N graduated with an MS in Nursing Administration from Empire State University in December 2023 and became the pediatric patient safety coordinator in February 2024. After four years as a clinical leader in the Pediatric ICU, she now works to ensure the safest, evidence-based nursing practices at a 71-bed children’s hospital, which serves 22 counties plus parts of Pennsylvania and Vermont. In March 2024, Langstaff accepted the Franny Award for Volunteer of the Year from the TSC Alliance. Inspired
by her son Jude, born with tuberous sclerosis complex (TSC), Langstaff has volunteered since 2009 to raise awareness and advocate for research funding. In 2024, she joined the March on Capitol Hill with Dr. Derek Bauer, co-director of the TSC Clinic at the University of Rochester.
2000s
Julie A. Berkhof ’01N, ’03N (MS) was named Bay College’s 2025 Distinguished Alumni of the Year. Berkhof is Director of Nursing at the University of Rochester Medical Center’s Wilmot Cancer Institute, where she has advanced oncology nursing, enhanced nurse practitioner roles, and fostered collaboration across the health system. Berkhof earned her LPN in 1995 and her ADN in 1996 from Bay College before pursuing her bachelor’s and master’s in nursing from the University of Rochester and a Doctor of Nursing Practice from St. John Fisher University. She has received multiple honors, including the Excellence in Leadership Award and URMC’s Meliora Award, and has contributed widely to research in geriatric oncology.

Susan Matthews Bezek ʼ06N (MS) was named director of cardiopulmonary services at UR Medicine Thompson Health, overseeing Cardiology, Cardiac Rehab, Respiratory Therapy, and Clinical Nutrition. She brings extensive experience in critical care, education, and leadership to her new role.
Kathryn Violet Edwards ʼ08N (MS) was a pediatric nurse practitioner at Stony Brook Pediatrics and Golisano Children’s Hospital. She earned her bachelor’s degree from the University at Buffalo and her master’s from the University of Rochester. Recently, she completed a post-master’s dual certification in Family Nurse Practitioner at St. John Fisher University.
Amanda Avery ʼ09N (MS), PNP has joined Bassett Healthcare Network as a Pediatric Nurse Practitioner at Oneonta Fox Pediatrics. She provides a full range of healthcare services for infants to young adults. Amanda earned her master’s degree as a Pediatric Nurse Practitioner from the University of Rochester School of Nursing and is certified by the Pediatric Nursing Certification Board.

2010s
Kamila J. Barnes ʼ11N (MS), ʼ13N (DNP) was inducted as a Fellow into the New York Academy of Medicine in December 2024.
Rebecca Rayburn ʼ18N, ʼ21N (MS) was named the 2024 Ambulatory Nursing Leader of the Year by OR Manager. This prestigious award recognizes excellence in nursing leadership, dedication, compassion, and commitment to patient care. Rayburn was praised for her expertise, kindness, and collaborative spirit in her role as a nurse manager at Surgery Center at Sawgrass.
2020s
Ariane Bianchi ʼ23N is currently working at Golisano Children’s Hospital Pediatric Cardiac Care Center and has been a pediatric clinical instructor for Genesee Community College (GCC). She earned an associate degree in Nursing from GCC and a bachelor’s degree from the University of Rochester. She plans to pursue a master’s degree in nursing education this coming year.
1950s

June Allen ’50N, ’59W passed away on Feb. 9, 2025.
Lois McKenzie ’51N passed away on Oct. 14, 2024.
Jo Anne Duke ’53N passed away on Jan.9, 2025.
Sandra Riley ’55N passed away on Oct. 30, 2022.
Beverly Bixby ’56N passed away on Dec. 16, 2024.
Anne Valery ’58N passed away on Feb. 9, 2025.
Deanna Warren ’58N (DPL), ’72N passed away on Dec.25, 2024.
Eva Pan ’59N (DPL) passed away on March 12, 2025.
1960s
Gloria Hagopian ’64N, ’70N (MS), ’79W (EdD) passed away on Oct.3, 2024.
Kathleen Neuner ’69N (MS) passed away on March 19, 2025.
1970s
Carol Hondorf ’78N (MS) passed away on April 20, 2025.
Bonnie Vaughn ’78N passed away on March 21, 2025.
1980s
Marlene Dohr ’80N (MS) passed away on Nov. 10, 2024.
Charlyne Hickey ’81N (MS) passed away on Dec. 13, 2024.
Paul Archibald ’84N passed away on Feb. 28, 2025.
Diane Alliet ’86N passed away on Dec. 2, 2024.
2000s
Barry Evans ’04N (MS) passed away on March 17, 2025.
Steven Richard Young, 67, of Austin, Texas passed away at his home on June 29, 2024. He established, with his sister Susan, the Anna Bater Young Endowed Scholarship Fund at School of Nursing. This fund was established in memory of their mother, Anna Bater Young, to provide opportunities for future students to gain excellent preparation in the field of nursing. Anna came to the University of Rochester in 1938, received her diploma from the School of Nursing in 1941 and received her bachelor’s degree from the University of Rochester College of Arts and Sciences in 1952.
Fay W. Whitney ’60, ’61N, PhD, RN, FAAN passed away in August 2024. Fay Wadsworth Whitney was a trailblazer in nursing education, practice, and policy whose legacy continues to impact students and patients alike. A proud graduate of the University of Rochester School of Nursing, Fay earned her bachelor’s degree in 1961 and went on to an accomplished career as a clinician, educator, researcher, and advocate. She held leadership roles at the University of Pennsylvania and the University of Wyoming, where she helped establish the Whitney Health and Wellness Center and advanced access to care in rural communities.
A passionate supporter of nursing education, Fay and her husband Roy Whitney ’57, ’73S (MBA), generously gave back to their alma mater. Their $1 million gift in 2011 created the Ralph R. and Fay Wadsworth Whitney Endowed Gift Fund to support aspiring nurse practitioners and advanced practice nurses at Rochester. Fay also co-chaired the School’s Meliora Challenge campaign and served on several advisory councils.
In recognition of her leadership and lifelong commitment to advancing nursing, the University of Wyoming renamed its School of Nursing in her honor in 2003. Her legacy of generosity, scholarship, and service will continue to inspire generations of nurses to come.















Did you receive a promotion? Move to a new city?
Publish your research findings? We want to hear from you! Submit your news and we will share it with your classmates and the UR Nursing community in the next Rochester Nursing Magazine. Fill out the alumni class notes form online or mail to:
Name
Address City
Occupation
Employer
(include maiden name, if applicable)


Family information (Spouse, children’s names)


Wilmot Breakaway Ride Warrior Walk + Run
The Wilmot Warrior Weekend is our premier charity event, offering cycling, a walk, and a run in the Finger Lakes region.
Sept 27–28, 2025
Our warriors come together and raise money for the Wilmot Cancer Institute to find advances which move us toward more cures. Start a team or join HereComesTheSON. Register today!

Permit No. 780 Rochester, NY
601 Elmwood Avenue, Box 643 Rochester, New York 14642
Change Service Requested
The Arts and Observation program, a collaboration with the Memorial Art Gallery, helps accelerated nursing students sharpen their observational skills and challenge their assumptions.

“
Kristina Santory, RN, ’06, ’14W (MS), instructor of clinical nursing
In a field that is so focused on physical assessments, lab values, and what to do next, this act of careful looking helps nursing students to pause and think: Are we seeing the whole picture?”
