THE PUBLICATION OF UMASS MEMORIAL HEALTH November 2022 Paradigm Shift Enhances Effectiveness of Complex Aortic Aneurysm Repair Page 12 THE PURSUIT
UMass Memorial Health
UMass Memorial Health, the clinical partner of UMass Chan Medical School, is the largest not-for-profit health care system in Central Massachusetts. We employ more than 16,500 people, and many of our 2,100 physicians are part of UMass Memorial Medical Group and Harrington Physician Services.
Together, we make health and wellness services available to people of all ages in our region and beyond. Our physicians provide care at the bedside, in the clinic or community, and in patients’ homes, advocating for social equality, providing economic stability and opportunity, and improving health and well-being. There are many ways to heal. We pursue them all. Relentlessly. Visit ummhealth.org for more information.
UMass Memorial Medical Group
UMass Memorial Medical Group is a dedicated, multispecialty network. One of the largest group medical practices on the East Coast, we also are the clinical partner of UMass Chan Medical School. Our academic connections enable us to be on the leading edge of innovative patient care. As members of the UMass Memorial Health system, our doctors offer patients both day-to-day and specialty health care in areas such as cancer, cardiology, pediatrics, orthopedics, surgery and women’s health. Visit ummhealth.org/umass-memorial-medical-group for more information.
Contents
HEALTH EQUITY
04 Interventions Reduce Racial Gaps in Pediatric Well-Visit Rates

Real-time analytics dashboards helped stakeholders identify and mitigate barriers to well-visit adherence, without making judgements or assumptions about patients and families.
08 Health Equity Project
Wins Tyson Award Team continues to identify barriers caused by structural racism and discrimination — and find better strategies for equitable implementation of social determinants of health interventions.
09 Building on Pandemic Collaborations and Community Data to Address Health Equity Issues
With a UMass Memorial donation for health equity efforts, the City of Worcester hired a vendor to integrate and manage public health data — data that could help improve health in the city.
DISCOVERY
12 Paradigm Shift Enhances
Effectiveness of Complex Aortic Aneurysm Repair
Minimally invasive endovascular repair makes for safer and more effective repair of complex aortic aneurysms, especially those that include the arteries branching to the brain, arms, intestines and kidneys.
19 Key Takeaways for Managing Abdominal Aortic Aneurysms
NEJM study identifies the benefits of endovascular repair rather than open surgery, as found in randomized, controlled trials.
CLINICIAN EXPERIENCE
21 Reducing physician burnout with wellness coaching
Physician-to-physician coaching model offers support for the challenges of being a health care provider.
24 Prevalence of burnout among clinicians
15 FORS Technology Enhances
Visibility and Reduces Radiation Exposure during EVAR
Light refracted through optical fibers generates real-time images of endovascular devices.

CARE DELIVERY
THE PURSUIT
The Pursuit is published by UMass Memorial Health to share innovations and advances — in care delivery, technology, population health and more — with physicians and other health care leaders. To have the newest articles delivered directly to your inbox, email pursuit@ummhealth.org, or subscribe at pursuit.ummhealth.org.
All content has been reviewed by physicians and administrators. Publisher: Judy Taylor Patel; Executive Editor: Nicole Lucey; Managing Editor and Writer: Marguerite Paolino; Graphic Design: Dominika Schmid © 2022. Visit our website at pursuit.ummhealth.org.
17 Patient Journey: After Long
Denial Period, a Short Road from EVAR to Recovery
‘It’s terrifying when your doctor tells you that you have a life-threatening condition, and it’s terrifying to think of having such a complex surgery.’
Ongoing negative experiences can be detrimental to well-being and have serious and long-lasting effects that are not easily remedied.
25 Supporting Peers through Difficult Situations
A peer-to-peer interaction after an incident can be a chance to vent some of the stress immediately.
DIGITAL MEDICINE
27
Risk assessment algorithm predicts level of care patients will need
First developed for a COVID-19 field hospital, this predictive analytics tool shows how data can drive health care innovation.
THE PURSUIT November 2022 | 3
RESEARCH
Facebook.com/xxxxx @xxxxxx pursuit@umassmemorial.org
Interventions Reduce Racial Gaps in Pediatric Well-Visit Rates
Real-time analytics dashboards helped stakeholders identify and mitigate barriers to well-visit adherence, without making judgements or assumptions about patients and families.
Well-child visits are among the most essential tools for maintaining and improving children’s health and wellbeing. Yet an examination of UMass Memorial Health pediatric data revealed that adherence rates for these routine appointments varied significantly by race and ethnicity, with Black and Latino patients attending at lower rates than white patients.
An interdisciplinary UMass Memorial Health team took an innovative next step by using the data to specifically address the disparities revealed, said Arvin Garg, MD, MPH, a pediatrician and Associate Chief Quality Officer for Health Equity at UMass Memorial.
“Our data analytics team created robust dashboards with real-time, practice-level data to illustrate the disparities, highlight the need for change, and help clinicians and staff design and implement interventions — and then keep track of their progress,” he said.

The multistakeholder project — called “Prioritizing Child Health: Promoting Adherence to Well-Child Visits in an Urban, Safety-Net Setting, During the Height of the COVID-19 Pandemic” — helped close the gaps and improved well-child visit adherence among all groups. In 2021, it won the inaugural Bernard J. Tyson Award for Excellence in Pursuit of Healthcare Equity (see page X). Results were published in the Joint Commission Journal on Quality and Patient Safety in April 2022.
“Without the data to show us where we’re improving, we’d just be guessing,” Garg said. “With the data, we can identify specific barriers and identify potential solutions. Improving adherence to well visits among patients of color represents a unique opportunity to improve the health of children, address social determinants of health, reduce racial/ethnic disparities in health care access, and promote population health.”
Making advances in health equity in care and outcomes
The project originated in 2020. After the murder of George Floyd and the Black Lives Matter protests that followed, Eric Dickson, MD, President and CEO of UMass Memorial, charged leadership with identifying opportunities to promote equity in health care access and outcomes across the system.
“When it comes to health equity, pediatrics is critically important, and we wanted to focus on an area with potential to have a significant impact on health,” said Lawrence Rhein, MD, MPH, Chair, Department of Pediatrics, and Associate Professor, UMass Chan Medical School.
Pediatrics also offered a significant amount of data to explore. The 53 Central Massachusetts practices associated with UMass Memorial serve 40,000 patients ranging from infants to 21-year-olds.
“We always had data on children’s well visits,” said Tracey Wilkie, Senior Director, Population Health Reporting & Analytics, Office of Clinical Integration, UMass Memorial. “But we hadn’t examined it based on race and ethnicity.”
During the year leading up to October 2020, which was used as a baseline, only 58% of Black patients and 64% of Latino patients had their annual well-child visit, compared with 72% of white patients. With clear evidence of a health equity gap, the team set a goal of increasing the numbers of well-child visits to 64% for Black patients and 69% for Latino patients.
By September 2021, teams in pediatrics and family medicine had conducted well-child visits with 72% of Black patients and 74% of Latino patients, far exceeding the initial goals. The effort also narrowed the overall disparity between Black, Latino and white children.
(See chart on the right.)
An analysis of UMass Memorial Health patient data revealed disparities in pediatric well-visit adherence rates, based on race and ethnicity. During the 12-month span used as a baseline, 58% of Black patients and 64% of Latino patients had their annual well-child visit, compared with 72% of white patients. Multifaceted interventions effectively reduced the gaps between white, Black and Latino children. As of September 2021, teams in pediatrics and family medicine had conducted well-child visits with 72% of Black patients and 74% of Latino patients, far exceeding initial goals and narrowing the overall disparity between Black, Latino and white children.
THE PURSUIT November 2022 | 54 | THE PURSUIT November 202 2
HEALTH EQUITY
“We haven’t completely closed the gap yet,” said Eric Alper, MD, UMass Memorial’s Chief Quality Officer and Chief Informatics Officer. “But we’ve made significant progress, and we can improve further by continuing to focus on this issue.”
Identifying obstacles to well-child visit adherence
As a safety-net hospital system, UMass Memorial serves many low-income families and families of color who face challenges related to social determinants of health. The presence of racial and ethnic disparities in adherence to well-child visits didn’t come as a surprise to stakeholders.
“We didn’t know the full range of issues that could lead to missed appointments and feed these disparities,” said Josephine Fowler, MD, Clinical Vice Chair, Department of Family Medicine, UMass Memorial Health, and Professor, Family Medicine and Community Health, UMass Chan Medical School.
The team decided to survey families to find out. To recruit patient/family volunteers to participate in the project, the UMass Memorial team enlisted the support of researchers at Massachusetts Health Quality Partners (MHQP), an independent, nonprofit organization dedicated to improving patient care experiences in the state. MHQP was tasked with surveying 30 people from a list of 3,000 provided by UMass Memorial.
Two senior MHQP researchers conducted interviews in English, and MHQP contracted two bilingual researchers with a background in public health to schedule and conduct interviews in Spanish. They conducted one-onone interviews with 15 English speakers and 15 Spanish speakers. Twenty-eight of the interviews were with parents/ guardians; two were with young adult patients.
The survey results confirmed the anecdotal reports from physicians and staff across the UMass Memorial system. The most frequently reported obstacles to parents bringing their children to well visits included:
• Transportation
• Cost of parking
• Competing demands (e.g., lack of time off from work)
• Inconvenient office hours and availability of appointments
• Language barriers
• Patients becoming young adults (ages 18-21)
“The interviews showed us exactly what our patients and
families are dealing with,” Fowler said. “Parents have other children who can’t come to appointments with their sibling because of COVID, and there’s no one to care for them at home. Parents need to work and don’t have the option for taking an afternoon off. They often lack transportation.
While many of us think of $7 for parking or $12 for a taxi as nominal fees, those are significant costs for people without a lot of financial resources. If they have to choose whether to put food on the table or go to a well visit, they’re going to choose food.”
Equal care means everyone gets the same amount of care. To have equitable outcomes, we need to go beyond equal care.
— Josephine Fowler, MD
Recommending ways to improve access to care
After identifying the reasons for the discrepancies in well-child visit adherence, the team focused on developing interventions, without making judgements or assumptions about a family or patient.
“What if someone says they can’t get to an appointment. I might assume it’s because there isn’t enough parking or parking is too expensive,” Rhein said. “But what if they don’t have a car? We can give out parking vouchers all day and it won’t make a difference. Instead, we can look at bus routes, and alternate transportation such as a taxi or ride services.”
The UMass Memorial team made a variety of recommendations for improving access and family participation in well-child visits both during and after the COVID-19 pandemic. Practices were free to take the ideas and adapt them, or come up with solutions better suited to their patient population.
• Schedule the next well-visit at the time of the current visit
• Develop an information sheet on the importance of preventive care visits
Distribute to patients and families at acute-care appointments
Post in exam rooms, in myChart (patient portal) and on the UMass Memorial website
Provide translations in languages relevant to the patient population
• Encourage follow-through on recommended care by implementing a reminder system and call process
• Consider staff calls in addition to automated reminder options
• Conduct well-child exam during acute-care visits, for patients who are behind on the recommended well-child visits or who don’t have a future visit scheduled

• Use telehealth for well-child visits when in-person exams are not feasible
• Develop a template specifically for well-child visits
• Implement a missed-appointment letter system that highlights the importance of preventive care visits
• Expand or extend office hours to align with family scheduling needs, including possible staggered shifts to accommodate expanded office hours and weekend hours
• Provide a voucher for free parking or arrange for curb-tocurb transportation through Medicaid
“Some of these interventions, even if they seem simple, require investment and cooperation from everyone from front-line office staff to physicians to executive leadership,” Garg said. “They require all of us — across the whole health care system — to come together and work toward a common goal of improving care for all children in our communities.”
THE PURSUIT November 2022 | 76 | THE PURSUIT November 202 2
HEALTH EQUITY HEALTH EQUITY
Pellentesque pharetra quam elit, a iaculis lorem lobortis at. Fusce ac mattis urna. Duis quis commodo enim, at mollis massa.
Photo by Matt Wright
Health Equity Project Wins Tyson Award

Team continues to identify barriers caused by structural racism and discrimination — and find better strategies for equitable implementation of social determinants of health interventions.
A data-driven UMass Memorial Health project — designed to identify and address racial gaps in adherence to pediatric well-visits — received the inaugural Bernard J. Tyson National Award for Excellence in Pursuit of Healthcare Equity in 2021. The award recognizes health care organizations leading initiatives that result in measurable, sustained improvements in health equity.
“UMass Memorial Health’s success in reducing health care disparities among Black and Latino pediatric patients is well deserving of the first Tyson Award,” said David W. Baker, MD, MPH, FACP, Executive Vice President, Healthcare Quality Evaluation, at The Joint Commission, which established the award in tandem with Kaiser Permanente. “The project team was able to make a significant improvement in well-child visit adherence in less than a year, showing all health care leaders that health care disparities can be improved with even small changes and must be taken seriously.”
The late Bernard J. Tyson was named CEO of Kaiser Permanente in 2013 and Chairman of its Board of Directors in 2014. Throughout his 30 years at the company, he was committed to addressing the health care inequities that persist in the U.S. health care system.
“I’m proud that The Joint Commission and Kaiser Permanente have recognized our team’s work and how much significant progress we’ve made,” said UMass Memorial Health Chief Quality Officer and Chief Informatics Officer Eric Alper, MD. “While we took on this project during the height of the pandemic, we are working toward closing the gap even further as we continue to focus on this issue. Our team is excited about addressing other areas where we identify health care inequities.”
The UMass Memorial project was chosen, in part, because of its sustainability. The project team is continually refining the evaluation and implementation efforts for improving visit adherence, identifying how structural racism and discrimination act as barriers, and finding better strategies to ensure equitable implementation of social determinants of health interventions.
“I’m so pleased that the Tyson Award selection committee recognized this work.” said Lawrence Rhein, MD, MPH, Chair of the Department of Pediatrics at UMass Memorial Health and Associate Professor at UMass Chan Medical School. “Since we’re an academic institution, part of our mission is to share our work and outcomes within our organization, regionally and nationally. I’m proud of the fact that our leadership at UMass Memorial recognizes the value of pediatrics and supports our department’s efforts to make health care more equitable for our patients and their families.” ◼
The project team went through multiple plan-do-study-act (PDSA) cycles to improve interventions incrementally. The Lean model of continuous quality improvement, which relies heavily on PDSA cycles, to achieve iterative gains is widely used at UMass Memorial.
“With the real-time analytics dashboards and front-line staff able to see what’s working or not working in individual practices, we have the opportunity to try different approaches and keep moving ahead with more and more effective solutions,” Rhein said.
While the project team was able to reduce the gap in well-child visits significantly, the work to close it entirely continues.
Fowler emphasized that achieving positive outcomes depends on adapting approaches to individual situations to ensure that care is not just equal, but also equitable.
“Equal care means everyone gets the same amount of care. To have equitable outcomes, we need to go beyond equal care,” she said. “We need to make sure our approach is the best one for the individual patient to achieve a positive outcome, and that can be different for different people.” ◼
Building on Pandemic Collaborations and Community Data to Address Health Equity Issues
With a UMass Memorial Health donation for health equity efforts, the City of Worcester hired a vendor to integrate and manage public health data — data that could help improve health in the city.
It’s not easy to find a silver lining in a catastrophic global pandemic. Yet,
Matilde (Mattie) Castiel, MD, sounds almost nostalgic when she describes how over 20 organizations in her Worcester, Massachusetts, community came together to fight COVID-19. She sounds energized when she explains how the same organizations could work together to tackle other public health problems — if they shared and consolidated their data. Now, a $1 million donation from UMass Memorial Health will be used to purchase that data, the first step in a larger effort.
To be an agent for positive change in this region, we have to expand our work beyond the walls of our great hospitals and clinical offices.
— Eric Dickson, MD
The donation established the Worcester Health Equity Fund to help the City of Worcester improve health equity and reduce health disparities among residents. The amount is equivalent to five years of real estate taxes on a local property UMass Memorial purchased to add capacity amid the ongoing bed shortage. Because UMass Memorial is a nonprofit, the property will become tax exempt beginning in 2023.
“To understand where the city is today, you have to go back to the
THE PURSUIT November 2022 | 98 | THE PURSUIT November 202 2
HEALTH EQUITY HEALTH EQUITY
Some of these interventions, even if they seem simple, require investment and cooperation from everyone from front-line office staff to physicians to executive leadership.
— Arvin Garg, MD, MPH
pandemic,” said Castiel, who serves as Commissioner of Health & Human Services in Worcester. She is one of three city-appointed members of the Health Equity Advisory Group, which is responsible for disbursing monies in the Worcester Health Equity Fund. Two additional group members are appointed by UMass Memorial.
“It was a time of extraordinary collaboration between health care and public health organizations in the city — and it started with the connection between the City of Worcester and UMass Memorial Health.”

Coming together against COVID-19
While UMass Memorial and the City of Worcester have worked together in multiple capacities over the years, the spread of COVID-19 brought the two organizations into a new era of collaboration. In 2020, they created a COVID-19 Equity Task Force to address the fact that local minority groups were feeling the impact of the pandemic disproportionately. Twenty other organizations joined the task force’s efforts to provide prevention and education information, launch public testing programs, and implement a low-barrier vaccination program for at-risk populations.
Having all these organizations working together had an enormous impact on outcomes in our community. And we didn’t want to go back to the siloed way we functioned before.
— Matilde (Mattie) Castiel, MD
rates in Worcester and surrounding communities, broken down by age, sex/ gender and race/ethnicity.






















































“The data made it clear that we needed to make sure those neighborhood resources were in place — not just during the pandemic but for the future,” Shirshac said. “This was an opportunity for us to improve health care access for everyone in our communities. And we learned a lot that we can apply to other public health issues.”
“Being able to act on the data UMass Memorial provided was amazing,” Castiel said. “Having all these organizations working together had an enormous impact on outcomes in our community.”


The Health Equity Advisory Group decided to apply the funds specifically to a project that will bring together data from the different electronic medical record systems used by UMass Memorial, St. Vincent Hospital and community health centers into a common format. With that data, they will have a fuller picture of how specific health issues — opioid use disorder or diabetes, for example — are affecting people in the community. Then they can use that information to identify opportunities for improvement and change.
“We can look at race and ethnicity. We can do some geomapping. We can examine the touchpoints for people with different health conditions. What happens during the time a patient who uses opioids is engaged with the health care system? How do we make the health care system more welcoming for them? Are A1C levels higher among people with diabetes who are certain ages or ethnicities?” Castiel said. “With access to real-time data over the course of a
year and Jeanne Shirshac’s amazing dashboards pulling it all together, we’ll begin to have the information we need to answer questions like these and determine how we can make the most impact in the community.”
While COVID-19 presented extraordinary circumstances, Eric Dickson, MD, President and CEO of UMass Memorial Health, prioritizes continuing the partnership with the City of Worcester and other community partners to address health inequities and improve health for all.
“To be an agent for positive change in this region, we have to expand our work beyond the walls of our great hospitals and clinical offices,” he said. “We’re committed to improving the health and well-being of the community while working hard to minimize the social determinants of health that persist as barriers to underserved populations. Part of that commitment is pivoting as necessary and providing support for the urgent health needs of our community.” ◼
Wave 1 of Covid-19 - City of Worcester Positive Cases















































UMass Memorial’s data analytics team used geospatial mapping analysis to identify areas with the most COVID-19 cases. Jeanne Shirshac, Vice President of Health Policy and Public Programs at UMass Memorial, and her team generated weekly reports on the infection

Using data to identify effects of opioid use


As the need for testing and vaccination sites waned, Castiel wanted to find a way to keep the organizations that had been involved in the city’s COVID-19 response from going their separate ways. The donation from UMass Memorial and the creation of the Worcester Health Equity Fund seemed the perfect opportunity to renew and expand efforts to work together.

THE PURSUIT November 2022 | 1110 | THE PURSUIT November 202 2
HEALTH EQUITY HEALTH EQUITY
Pellentesque pharetra quam elit, a iaculis lorem lobortis at. Fusce ac mattis urna. Duis quis commodo enim, at mollis massa.
Photo by Matt Wright
Pellentesque pharetra quam elit, a iaculis lorem lobortis at. Fusce ac mattis urna. Duis quis commodo enim.
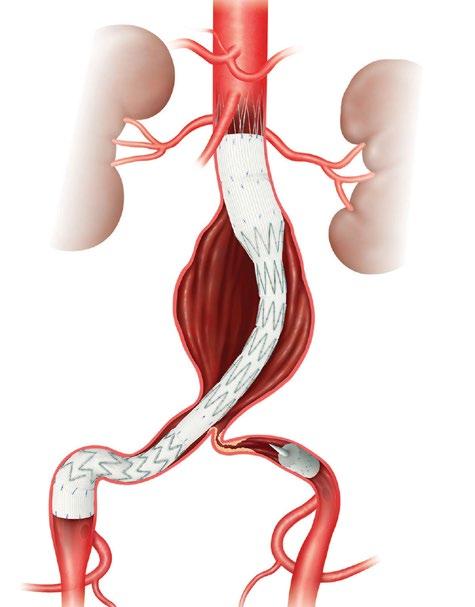
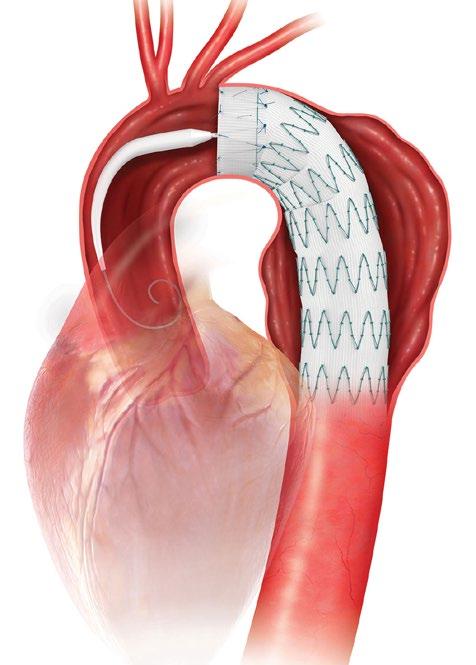
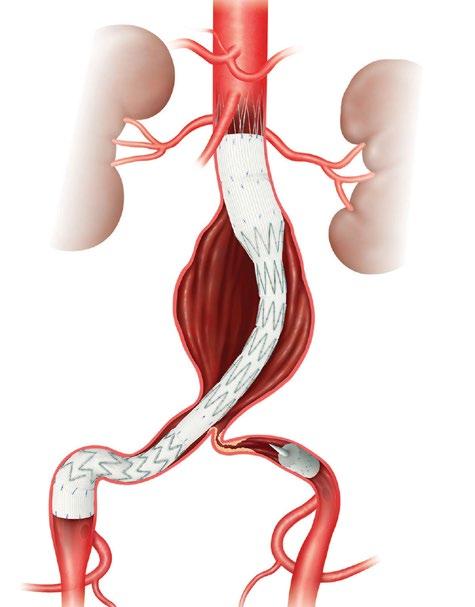
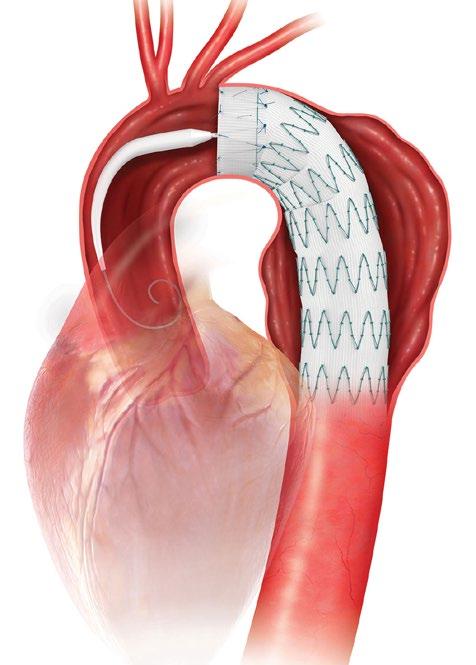
Paradigm Shift Enhances Effectiveness of Complex Aortic Aneurysm Repair
Minimally invasive endovascular repair makes for safer and more effective repair of complex aortic aneurysms, especially those that include the arteries branching to the brain, arms, intestines and kidneys.
Surgeons at UMass Memorial Health’s Center for Complex Aortic Disease are advancing both fenestrated and branched forms of endovascular aortic repair (EVAR) techniques. These involve only two groin needle punctures, rather than open surgical repair, making the procedures safer and recovery faster for patients.
By the time patients meet Andres Schanzer, MD, FACS, they have been through cardiac workups with their own cardiologists and vascular surgeons already. They know the size and complexity of their abdominal aortic aneurysm, and they are acutely aware of the risk of rupture. They come to UMass Memorial Medical Center in Worcester looking for new treatment possibilities and the potential to improve and extend their lives. They come looking for hope.
“Many of my patients have been living with this for several years before I see them, and they may have been told there’s no repair strategy available for them,” said Schanzer, Chief of the Division of Vascular and Endovascular Surgery and Director of the Center for Complex Aortic Disease at UMass Memorial Medical Center, one of 10 U.S. sites using custom-made endografts for complex fenestrated/ branched endovascular aortic aneurysm repairs. He is also Director of the UMass Memorial Health Heart and Vascular Center and a Professor at UMass Chan Medical School.
“In many of these cases, endovascular repair may be a good option. It provides a minimally invasive alternative to an open repair, with faster recovery and less pain. It’s the most transformational technology we’ve had in vascular surgery in decades, and it’s a tremendous benefit when there’s a more complex aneurysm present.”
The Center for Complex Aortic Disease is one of the busiest in the nation when it comes to minimally invasive endovascular aortic repair (EVAR), a procedure that has fundamentally altered treatment for thoracic and abdominal aortic aneurysms. Many of the center’s patients, who come from across the U.S. as well as from other nations, would not be able to tolerate the traditional open surgical repair because of comorbidities, advanced age, or location or complexity of the aneurysm.
“Open thoracoabdominal repair is the most invasive surgery you can do to a human,” Schanzer said. After making a midline transabdominal or retroperitoneal incision to access and then clamp the aorta and iliac arteries, the surgeon replaces the section of the artery that has the aneurysm with a tubular or bifurcated prosthetic graft. Most aortic aneurysms develop below the renal
DISCOVERY
arteries and become increasingly complex when they involve blood supply to the kidneys and the intestines, a situation that requires the fenestrated endovascular aortic repair (FEVAR) procedure.
A minimally invasive alternative
During a minimally invasive repair of an aortic aneurysm, an expandable stent graft is delivered to the area of the aneurysm through blood vessels using wires and catheters. When it’s in place, the surgeon expands the stent graft into position, leaving the aneurysm intact while constructing the device. At UMass Memorial, a new fiber optic imaging technology is used to enhance visibility and reduce the amount of radiation exposure to patients and the clinical team.
“Endovascular repair is a complete paradigm shift in how quickly people can be treated and recover. I’ve never seen a
technology move a field forward so rapidly,” Schanzer said. “We can do the procedure through small needle punctures. We introduce the device into the artery and then essentially build the device inside the patient’s blood vessels.”

The minimally invasive FEVAR technique makes for safer and more effective repair of complex aortic aneurysms that include the arteries branching to the kidneys and intestines. The stent graft is designed to accommodate more complex aortic anatomy. Small holes in the endograft are configured at the exact location of the branch arteries to accommodate the addition of smaller stent grafts to those arteries. The fenestrated endograft must align with the patient’s particular anatomy. Schanzer has completed more than 450 FEVAR procedures, a number that puts him among the top three U.S. surgeons who perform the procedures.
Vascular surgeon Jessica P. Simons, MD, MPH, DFSVS, has partnered with him in many of those procedures. In addition to her role in the Center for Complex Aortic Disease, Simons is Associate Professor of Surgery and Program Director, Vascular Surgery Residency, UMass Chan Medical School.

In August 2022, Schanzer and his team became the first in the world to repair a diseased aortic arch using a retrograde three-vessel device custom-made for a patient’s anatomy. A prototype of the device was first manufactured and deployed in a 3D printed model of the patient’s aorta to establish technical feasibility.
“The configuration for this device was the first of its kind to use three branches to the arteries supplying the arms and brain in such a way that all could be accessed from a single groin puncture,” Schanzer said, adding that the patient recovered well and went home after a short hospital stay.
Faster recovery for patients
The fact that endovascular repairs are so much less invasive means that speed of treatment increases and the recovery period decreases. Even a complex FEVAR procedure involves only three to five hours of surgery and one to three days in the hospital’s cardiovascular unit.
“I tell my patients they’ll be back to normal in one to three weeks,” he said. In comparison, patients who have an open repair spend three to seven days in intensive care, 10 to 20 days on the cardiovascular floor, and some time in a rehabilitation facility. Their recovery at home typically continues for a minimum of six months.
Schanzer said he and his team achieve technical success — that is, placing the device, maintaining the patient’s
THE PURSUIT November 2022 | 1312 | THE PURSUIT November 202 2
DISCOVERY
Andres Schanzer, MD, FACS, has completed more than 450 FEVAR procedures, a number that puts him among the top three U.S. surgeons who perform the procedures.
Photo by XXX
Photo by Matt Wright
stability and stopping blood flow to the aneurysm — in 97% of FEVAR cases. Mortality rate within 30 days of the procedure is less than 4%.
“Given the complexity of the procedures and the multiple comorbidities of our patients, that is excellent,” Schanzer said. Conventional open repairs have mortality rates ranging from 5 to 20%.
The team also takes a collaborative approach to working with patients and families, as well as with referring physicians and surgeons. Standard practice at the center is to invite physicians to observe their patient’s procedure and keep them apprised of the patient’s journey — which is lifelong. Patients must commit to having follow-up imaging on an annual basis.
FORS Technology Enhances Visibility and Reduces Radiation Exposure during EVAR
It’s the most transformational technology we’ve had in vascular surgery in decades, and it’s a tremendous benefit when there’s a more complex aneurysm present.
— Andres Schanzer, MD, FACS
Schanzer said it’s essential for patients to have their care fully understood by their local physicians. That ensures that the information about their procedure, recovery and ongoing progress is readily available to the referring provider when the patient is home.
“We tell our referring physicians about everything — clinical visits, our concerns, any complications that arise, follow-up needs,” said Robichaud.
Leadership in the Aortic Research Consortium
Light refracted through optical fibers generates real-time images of endovascular devices.
Patient-centered, team-based approach
To meet the needs of patients who are undergoing these complex endovascular procedures, every member of the center’s team must have expertise beyond what is usually expected in their professional areas. That begins with Lindsey Carr, an administrative assistant and patient care coordinator who helps patients get to the hospital, schedule scans and navigate insurance challenges. Nurse practitioners on the team provide essential clinical care and ensure that patients understand the risks and benefits of the procedures. Devon Robichaud, MSN, ACNP, Clinical Coordinator, sees patients in person or remotely before their surgeries, follows them post-surgery throughout their lives, and manages issues that can arise at any time during the process. Like Robichaud, Shauneen Valliere, NP, Research Coordinator, provides clinical care, and she also ensures that the center follows the latest FDA regulations.
Support of the clinical team continues throughout the patient experience. Vascular anesthesiologists, who specialize in these types of procedures, place essential lumbar drains to remove excess cerebrospinal fluid and prevent paralysis. The cardiovascular ICU is staffed with nurses who are experienced in taking care of these complex patients.
UMass Memorial’s Center for Complex Aortic Disease is one of 10 sites participating in a physician-sponsored investigational device exemption study. Each site functioned independently until coming together as the U.S. F/BEVAR Aortic Research Consortium in 2018. The consortium is evaluating custom-made and physicianmodified FDA-approved devices for treatment of patients with complex abdominal or thoracoabdominal aneurysms.
Schanzer serves as Medical Director. Together, the 10 sites have completed more than 2,500 cases, making it the largest trial of its kind in the world.
“Having such a large data set helps as we examine the issues we encounter. For example, the best types of device designs, different types of anatomical challenges, rates of recovery, need for reinterventions, etc.,” Schanzer said. “A single site doesn’t have enough data to draw conclusions on these types of issues. Now the data we are drawing from is orders of magnitude greater.”
He believes the consortium and its large dataset of fenestrated and branched EVAR procedures will be essential in advancing endovascular repair to greater efficacy.
“The consortium will provide the infrastructure and the agile regulatory pathway to enable large-scale testing of emerging technologies,” he said, adding that the amount of data will facilitate more randomized trials to study the technology and bring it to new heights. “We can push the field much further by all working together.” ◼
Endovascular repairs are done in a hybrid cardiovascular operating room with advanced imaging equipment, a fluoroscopy unit and traditional operating suite. At UMass Memorial Medical Center, the hybrid OR is also equipped with Fiber Optic RealShape (FORS) technology. Surgeons there were the first in the nation to use FORS for a complex endovascular aortic aneurysm repair (EVAR). The technology gives operators better imaging and more flexibility in maneuvering endovascular guidewires and catheters for EVAR, while also reducing dependence on fluoroscopy.
Most vascular surgeons rely on two-dimensional, grayscale fluoroscopy imaging to visualize endovascular devices. For the patient, the radiation exposure can be significant, although the need for the procedure outweighs that risk. For surgeons and other members of the clinical team who conduct the procedures repeatedly, the radiation exposure has the potential to become more consequential as it accumulates during training programs and the procedures themselves.
A new technology developed by Philips dramatically improves visibility while also reducing dependence on fluoroscopy. In 2021, UMass Memorial Medical Center vascular surgeons became the first in the nation to use FORS, a technology that generates realtime images of endovascular devices by refracting light through optical fibers. Only two other hospitals in the U.S. and three outside the country are currently using it.
Reducing radiation exposure
“Radiation continues to be an essential tool for us, but we all know it can pose a threat to the health of a patient and to everyone on the treatment team,” said Andres Schanzer, MD, FACS, Chief, Division of Vascular and Endovascular Surgery, Director, Center for Complex Aortic Disease at UMass Memorial Medical Center, Director, UMass Memorial Health Heart and Vascular Center, and Professor, UMass Chan Medical School.
Instead of the ionizing radiation of fluoroscopy, FORS technology uses light refracted through optical fibers to provide 3D tracking of endovascular guidewires, catheters and devices. FORS technology has the potential to reduce

THE PURSUIT November 2022 | 1514 | THE PURSUIT November 202 2
DISCOVERY DISCOVERY
Photo xxxx
Pellentesque pharetra quam elit, a iaculis lorem lobortis at. Fusce ac mattis urna. Duis quis commodo enim, at mollis massa.
a patient’s radiation exposure by as much as 75% during endovascular complex aortic aneurysm repair.
“FORS technology gives us the opportunity to protect our patients and colleagues from radiation exposure, while providing safe, effective, minimally invasive repairs with even greater accuracy,” Schanzer said.

Imaging advantages
In addition to reducing the need for fluoroscopy, FORS technology enhances the visibility as the operator moves devices through the arteries. The real-time images produced are three dimensional, so the EVAR team can view progress and movement from any angle. The technology also allows for zooming in and having multiple projections on-screen at once.
“This enables me to always keep the full extent of the guidewire in my field of vision,” Schanzer said. “Then I can advance the FORS catheter over the wire to get it in position. The FORS system shows which portion of the
guidewire or catheter is in front of the other, making all endovascular interventions easier and safer.”
The FORS images are displayed on top of, and in alignment with, anatomical patient images created through digital subtraction angiography (DSA) or computed tomography (CT), both of which are black and white. With DSA or CT
images alone, it can be difficult to determine the exact placement of the catheter, but with FORS technology, it can be seen in color in the foreground.
“The system is very intuitive and truly represents a new era in device guidance,” Schanzer said, adding that having a color image has an additional benefit. “Until I started using FORS, I hadn’t realized how much operator fatigue there is when you’re only looking at different shades of gray to visualize everything. It’s become very apparent to me that the bright yellow and blue on top of the gray background really decreases that strain, especially when you’re looking at previous stent grafts and wires.” ◼
Patient Journey: After Long Denial Period,
a Short Road from EVAR to Recovery
‘It’s terrifying when your doctor tells you that you have a life-threatening condition, and it’s terrifying to think of having such a complex surgery.’
Jawan Betts likes to save time by booking multiple medical appointments on the same day. But in the autumn of 2017, her usual plan went awry when two of her doctors heard a new heart murmur. Instead of going home on time, she went for an ultrasound and a CT scan at her community hospital in upstate New York. The results revealed she had two aortic aneurysms.
“I was so scared that day,” said Betts, who was 59 at the time and working full-time as a supervisor in a medical practice. “I knew it meant that they’d have to open me up, all the way down. And that did not appeal to me one bit.”
Patient wants wait-and-see approach
The doctors at her local community hospital sent her to the University of Rochester Medical Center, where vascular surgeon, Michael Stoner, MD, told her endovascular surgery for a situation as complex as hers would be coming to Rochester soon, and in the meantime, she might be a good candidate for a study he was working on.
Betts was fine with waiting and monitoring the aneurysms. She didn’t have any symptoms.
“It was easy to ignore it for a while,” she said. “In hindsight, I know it wasn’t a smart thing to do, given the risks, but I was in denial for a long time. You really don’t know how you’ll react to something like this.”
Eighteen months later, she learned she didn’t qualify for the study after all. And a third aneurysm had developed. Stoner referred her to Andres Schanzer, MD, FACS, Chief, Division of Vascular and Endovascular Surgery, Director, Center for Complex Aortic Disease at UMass Memorial Medical Center, Director, UMass Memorial Health Heart and Vascular Center, and Professor, UMass Chan Medical School.
She drove the six hours from her home outside Rochester to Worcester to find out whether she would be a good candidate for the minimally invasive endovascular aortic repair (EVAR). She was impressed by Schanzer, but she didn’t feel ready to have the surgery.
I woke up with no pain at all and spent the night in the step-down unit.
The care was phenomenal. I went home the next day and went back to work on Monday.
— Jawan Betts, patient
“It’s terrifying when your doctor tells you that you have a life-threatening condition, and it’s terrifying to think of having such a complex surgery,” said Devon Robichaud, MSN, ACNP, Clinical Coordinator for the Center for Complex Aortic Disease. “Sometimes it takes patients a while to come to terms with it. If their aneurysms aren’t yet very large, they can take some time, but the risk increases as time goes by and the aneurysms grow.”
Ready to defuse ‘ticking time bomb’
For a while, Betts was satisfied with having the aneurysms monitored, but over time, she recognized the danger of not
THE PURSUIT November 2022 | 1716 | THE PURSUIT November 202 2
DISCOVERY CARE DELIVERY
FORS technology has the potential to reduce a patient’s radiation exposure by as much as 75% during endovascular complex aortic aneurysm repair.
Photo by Matt Wright
Pellentesque pharetra quam elit, a iaculis lorem lobortis at. Fusce ac mattis urna. Duis quis commodo enim, at mollis massa.
Pellentesque pharetra quam elit, a iaculis lorem lobortis at. Fusce ac mattis urna. Duis quis commodo enim, at mollis
touch.”
The first surgery was Tuesday, February 4, 2020, when COVID-19 was “just a little rumble,” Betts said. “The surgery itself was a breeze. I woke up with no pain at all and spent the night in the step-down unit. The care was phenomenal. I went home the next day and went back to work on Monday.”
Fear of pandemic, not surgeries
The second surgery was more complex, but Betts’s fear about returning to the hospital was due to the pandemic rather than the procedure.
“Around March 17, the world basically had to shut down. I was physically sick from the stress. I thought, ‘Am I crazy to walk into a hospital in this situation?’ I asked my PCP for advice, and she made me realize it was life or death. I chose life. Once I made up my mind, there was no going back.”
On March 23, there was so little traffic that they made it to Worcester in record time. Her husband and son dropped her off at the hospital entrance, which was eerily quiet. She was one of only a few patients in the waiting room, which had been crowded with dozens of people the month before.
“Jawan’s surgery was the first we had scheduled since the shutdown,” Robichaud said. “COVID was causing so much uncertainty and fear at that time. Very few surgeries were taking place anywhere in the hospital.”
Home three days after more complex surgery
The surgery went exactly as planned, and although Schanzer had told Betts to expect to spend five to eight days at the hospital, she was well enough to go home after three.
“I was almost disappointed,” Betts said. “I kind of liked having the call button, and the nurses were amazing.”
Her recovery was smooth and rapid.
repairing them. She scheduled two endovascular surgeries with Schanzer, both in 2020.
“I was something of a ticking time bomb,” Betts said. She had a Type 2 thoracoabdominal aortic aneurysm that measured more than 6 cm. This is the most extensive type of aneurysm, as it involves the majority of the thoracic aorta and abdominal aorta.

“Devon was my shining star. She held my hand from my first appointment through my recovery. We still keep in
“On day 13 after the surgery, I woke up to a beautiful sunny day,” she said. “I drove myself to the area where we like to camp and went on a little hike. I felt great.”
[Subhead] ‘A gift’ to have this surgical option
Betts, now 64, is followed by Stoner close to home, and Schanzer and his team review her annual CT scan to ensure the stents are all working as expected.
“It was a gift that Dr. Schanzer was doing this type of surgery,” Betts said. “It was exactly what I needed, and I got there at exactly the right time — in spite of COVID.” ◼
Key Takeaways for Managing Abdominal Aortic Aneurysms
NEJM study identifies the benefits of endovascular repair rather than open surgery, as found in randomized, controlled trials.
A 2021 New England Journal of Medicine (NEJM) article on managing abdominal aortic aneurysms provided evidence in support of endovascular aortic aneurysm repair (EVAR) over open repair, as well as a review of formal guidelines and clinical recommendations. The study was authored by Andres Schanzer, MD, FACS, Chief of the Division of Vascular and Endovascular Surgery and Director of the Center for Complex Aortic Disease at UMass Memorial Medical Center, and Gustavo Oderich, MD, Professor and Chief of Vascular and Endovascular Surgery at McGovern Medical School, UTHealth Houston.
“There is the need to balance the risk of observing an aneurysm against the risk of repair,” said Schanzer, who is also Director of the UMass Memorial Health Heart and Vascular Center and a Professor at UMass Chan Medical School. “Then there’s the need to evaluate the risk of open repair or EVAR.”
Common risk factors
A variety of factors increase risk for abdominal aortic aneurysm: advanced age, family history, previous or current use of tobacco, hypercholesterolemia and hypertension. Patients with diabetes mellitus, on the other hand, have a lower risk.
Men are at higher risk than women, and recommendations for when to repair an aneurysm differ for the sexes. An aneurysm with a diameter of 5.5 cm or more makes a man a candidate for repair. For women, a measurement of 5.0 cm or greater should be repaired. Smaller aneurysms may be watched over time to see whether and how much they are expanding and evaluated for level of increased risk.
Benefits of EVAR over open surgery
The NEJM study identifies the benefits of repairing via EVAR rather than open surgery, as found in randomized, controlled trials.
• There’s a lower risk of perioperative complications and death.
• It’s advantageous for the first two to three years after surgery. Longer term survival is comparable to open surgical repair.
THE PURSUIT November 2022 | 1918 | THE PURSUIT November 202 2
CARE DELIVERY RESEARCH
massa. Photo provided
by Jawan Betts
• Reinterventions may be more necessary after EVAR, but they usually involve minor endovascular procedures. There is higher risk of a need for laparotomy after open repair.
EVAR patients must be followed long-term with duplex ultrasonography or computed tomographic angiography.
Limits to the procedure
While EVAR patients have a better survival rate than open repair patients at first, the study shows that the gap in the survival rate closes after two to three years. Several reasons are given:
• Underlying cardiovascular risk
• Lack of adherence to follow-up care recommendations
• Ongoing inflammation due to the fact that the aneurysm stays intact with EVAR
• Sac pressurization
• Failure of the stent graft device
In many EVAR cases — 18 to 63% — the patient’s anatomy did not match the manufacturer’s guidelines for appropriate use. While the majority of aortic aneurysms are now treated with EVAR procedures, there are limits to when and how the stent grafts can be used. The devices must match the anatomy of the specific patients to ensure the aorta has healthy areas above and below the aneurysm to ensure the stent graft can be sealed to its wall. The diameter of the femoral and iliac arteries must be large enough for insertion of devices. To avoid the risk of embolization, the patient cannot have excessive plaque and must have vessels that branch within the angle that can be accommodated by the device.
The size, shape, and fenestrations must match the patient anatomy exactly, which can be a challenging goal to achieve with physician-modified stent grafts.
“In my opinion, if an appropriate company-manufactured device is available, that is likely the best option,” Schanzer said, adding that the manufacturer’s quality assurance capabilities are much greater than what can be done when a physician is modifying a device. When working with a stent manufacturer, he and his team make a 3D model of the patient’s aorta and look at other images in comparison to the model. They measure each angle to ensure they understand how the stent graft will interact with the aorta. Then the information is sent to engineers who develop a final model for the manufacturer. He cautions against pushing the limits of the devices too far, a situation he sees becoming more common in recent years.
“About 25% of our patients are referred to us after failure of their prior EVAR or TVAR [transcatheter aortic valve replacement] procedures,” he said. ◼
Reducing physician burnout with wellness coaching
Physician-to-physician coaching model
offers support for the challenges of being a health care provider.
As head of the Clinician Experience Office, Steven Bird, MD, FACEP, FACMT, spends many of his waking hours advocating for clinical staff to take better care of themselves and studying ways to enhance their wellbeing, including developing and launching a free wellness coaching program for them. Yet when he looked at his own calendar in early November 2021, he saw he had not planned for a single day off through the end of the calendar year. The irony was not lost on him.
A 12-month clinical trial of a one-on-one wellness coaching program for clinicians reduced participants’ burnout scores by 31% and improved their overall wellness, as measured by a validated self-assessment tool.
with being a health care provider, and it can be helpful to work with someone who has deep understanding of the situation and environment you’re working in.”
Study: Coaching has significant impact
“I’m like many of my fellow clinicians — not always the best model for self-care and at risk for burnout,” he said. Bird divides his time equally between roles as an emergency physician at UMass Memorial Health and as Clinician Experience Officer supporting clinicians throughout UMass Memorial Health and UMass Chan Medical School, where he also serves as Professor of Emergency Medicine. The Clinician Experience Office, established in 2019 by UMass Memorial Medical Center, UMass Memorial Medical Group and the UMass Chan Medical School, is designed to advance clinician wellness and professional fulfillment.
“We typically think that we should have compassion for others — for our patients and their families — but it can also be for us,” Bird said. “Wellness coaching for physicians by physicians works. Sometimes we need support to manage the difficult circumstances and feelings that come

To offer his colleagues that support, Bird developed a one-on-one wellness program and recruited five UMass Memorial and UMass Chan physicians to join him for a nine-month coaching training program. In January 2021, the team began offering the free coaching program, which was set up as a 12-month clinical trial, largely based on a 2019 JAMA Internal Medicine article, “Effect of Professional Coaching Intervention on the Well-being and Distress of Physicians” by Lotte N. Dyrbye, MD, and Tait D. Shanafelt, MD, at the Mayo Clinic. Bird also drew on data from the Healthcare Professional Well-being Academic Consortium (PWAC), which uses assessment, program evaluation and scholarship to advance well-being among health care professionals. UMass Memorial/UMass Chan Clinician Experience Office is one of 22 U.S. academic medical centers and affiliates that are members of PWAC.
During 2021, 66 clinicians signed up for the wellness coaching program, and 54 completed three-months sessions.
Now, the results of the trial are in. As measured by the Well-Being Index (WBI), a validated self-assessment tool created by the Mayo Clinic, participant burnout scores decreased by 31% compared to those who were in the
20 | THE PURSUIT November 202 2
RESEARCH CLINICIAN EXPERIENCE
Randomized, controlled trials show that, compared to open repair, EVAR has a lower risk of perioperative complications and death.
— Tara Kumaraswami, MD, MPH
CLINICIAN EXPERIENCE
control group. There are separate WBI assessment tools for physicians and advanced practice providers.
“The coaching had a statistically significant impact on those who completed all sessions with their coaches,” Bird said. The program has been well-received and now has more applicants than the coaching program can serve, since it’s limited by the number of coaches available. He hopes to grow the program and reduce the dropout rate.
Success requires time commitment
“A wellness coaching program is based on positive psychology, but it’s a two-way street. It takes work,” Bird said, adding that some of those who dropped out of the 2021 session found they didn’t have the time to devote to the work. “Our coaches facilitate participants finding what will help them feel well. It’s not necessarily going to address burnout directly. They can institute behavioral change to help achieve what they want in life and in their career.”
Program participants, 80% of whom were women, included physicians, advanced practice providers, residents and fellows. All were asked to:
• Commit to a three-month coaching cohort
• Complete a well-being assessment
• Identify goals to improve their personal and professional lives
• Virtually meet with their wellness coach every two weeks
Giving back: From coachee to coach
For Tara Kumaraswami, MD, MPH, Obstetrics and Gynecology Residency Program Director and Assistant Professor of Obstetrics and Gynecology, the program was worth the time and effort. When she found herself struggling with the isolation of practicing medicine during a pandemic, she requested coaching.
“There’s something to be said for taking care of yourself. And we often don’t do that. The coaching program offers the opportunity to take the time — an hour — to focus on what’s going on in your life, with someone at your side to guide you through the experience,” she said, adding that she was matched with a coach she had been acquainted with in medical school. “Sometimes you need someone to listen — someone who knows what you’re going through. So you know you’re not the only one having that experience.”
Kumaraswami worked with her coach to focus on what she was accomplishing as a residency program director and OB/GYN generalist and to add more physical activity to her life.

“It was good to talk about the positives, not only the negative things that were happening at the time,” she said.
“It’s not about venting or complaining. My coach helped me find the direction I wanted to go, but truly the answers are within the coachee.”
In 2022, she joined the program as a coach and is now helping colleagues find their own answers, just as her coach helped her.
Continued need to address mental health
While Kumaraswami is open about her own need for coaching, she recognizes that there’s continued stigma around mental health care among clinicians and appreciates that the program protects the identities of participants.
A 2017 study, published in Mayo Clinic Proceedings, reported that close to 40% of physicians would be reluctant to seek mental health care — out of concern for possible repercussions to their medical licensure.
“It’s important for people to feel secure in talking about their stresses and concerns, and that’s not always easy for health care professionals,” said Bird. “While there is less stigma in seeking help for mental health, it still exists. And the fear of being subjected to that stigma is very real.”
He believes there is a long-term need for wellness coaching among clinicians. He gives his own experience as an example. In the emergency department, he often sees the effects of stress on his colleagues and on himself. When hospital beds were most scarce at the height of the Omicron wave, for example, he found himself coming up short in the care he could provide for a patient.
“I called 39 hospitals in New England to find a bed for one patient, and I could not find one. That’s not the kind of medicine I ever wanted or envisioned practicing. When you can’t get the patient the care they need and deserve, you feel a decreased sense of personal accomplishment, but even more than that, you could experience moral distress,” he said. “And that’s a lot to carry.” ◼
Physicians and medical students throughout the U.S. can receive free, confidential emotional support via the Physician Support Line, which is staffed by a volunteer network of psychiatrists. Call 1 (888) 409-0141, 8:00 a.m. to 1:00 a.m. ET, seven days a week.

My coach helped me find the direction I wanted to go, but truly the answers are within the coachee.
Photo by Matt Wright
Prevalence of burnout among clinicians
Ongoing negative experiences can be detrimental to well-being and have serious and long-lasting effects that are not easily remedied.
Physician burnout was on the rise in the years leading up to 2020, and the COVID-19 pandemic exacerbated the trend.
When wellness is framed as being easily achieved via a list of things you ‘should’ be doing, it’s perceived that the problem is with the individual.
— Steven Bird, MD, FACEP, FACMT
In its 2021 survey of 2,504 U.S. physicians, The Physicians Foundation found that 61% of physicians reported often experiencing feelings of burnout, compared to 40% in the organization’s 2018 survey.

While the term burnout is applied to many groups, medical professionals may experience it as emotional exhaustion, depersonalization of the patient, decreased efficacy or decreased sense of personal accomplishment
Steven Bird, MD, FACEP, FACMT, believes the lack of appreciation clinicians experience is also one of the many contributing factors.
“While at the beginning of the pandemic we were viewed as health care ‘heroes,’ the weariness and frustrations of the pandemic have led to increasing verbal and physical abuse of physicians and other health care workers,” said Bird, who is an emergency medicine physician at UMass Memorial Health and Clinician Experience Officer supporting clinicians throughout UMass Memorial and UMass Chan Medical School, where he is Professor of Emergency Medicine.
For example, a survey conducted by Bird and his colleagues found that, of system clinicians reporting on-the-job verbal mistreatment or abuse, 85% of abuse came from patients and families. Ongoing negative experiences like this can be detrimental to well-being and have serious and long-lasting effects that are not easily remedied. While many articles suggest ideas for maintaining and restoring mental calm in the face of such experiences, Bird cautions against offering over-simplified self-care remedies or activities.
“When wellness is framed as being easily achieved via a list of things you ‘should’ be doing, it’s perceived that the problem is with the individual. ‘If only you’d do this, you’d be well,’” he said. Like many other clinicians he knows, he doesn’t want to be told to meditate and write a gratitude journal.
“While those types of activities can be helpful for some people, it’s totally valid when a physician rejects advice like that and asks for system-level supports, like providing onsite childcare, increasing staffing, promoting widespread vaccination and opening more patient beds.”
Supporting Peers through Difficult Situations
A peer-to-peer interaction after an incident
can be a chance to vent some of the stress immediately.
This established, confidential program offers clinicians same-day support from a peer during difficult or crisis situations. Whether formal or informal, peer connections can help clinicians manage the emotional effects of trauma and stress.

Intense and unexpected circumstances are routine for those involved in health care, yet ignoring the emotional effects of trauma and stress can contribute to burnout, psychological distress and career dissatisfaction. Talking with a peer, whether formally or informally, can help clinicians reduce or avoid the possibility of a difficult event negatively affecting their professional and personal lives.
At UMass Memorial Health and UMass Chan Medical School, the Clinician Experience Office supplements those informal peer interactions with its organized 28-member Peer Support Network. For the last 15 years, this free, confidential program has been available to physicians, nurses, administrators and any other clinicians who ask for help, although often a colleague or supervisor will alert the CXO of someone who may need assistance. The trigger is usually an unanticipated or poor patient outcome, a lawsuit, traumatic personal event or other negative circumstance that an individual is having difficulty dealing with.
“After more than two years of being on the front lines of the pandemic, PTSD, burnout and suicidality are alarmingly common among health care professionals,” said Steven Bird, MD, FACEP, FACMT, Clinician Experience Officer. “One of the biggest challenges is that people are generally bad at asking for help, even when they need it most. And physicians are often even worse at it. Because of that, we reach out to people when we become aware of a difficult situation, so they don’t have to ask for assistance. We go directly to them with this support.”
Offering support proactively
While one-on-one wellness coaching for physicians requires a big commitment from both coaches and participants (see page 21), the Peer Support Network is a different model.
The Clinician Experience Office pairs the person with peer support within a day, ideally within a couple of hours of a difficult situation arising. Typically, it’s a one-time meeting, although there may be a check-in to follow up. If the person is having difficulty at that time, the peer support volunteer can help identify next steps and assist in finding appropriate resources. The Clinician Experience Office doesn’t track who has requested or received support.
Having that peer-to-peer interaction — and having it quickly on the heels of an incident — offers the chance to vent some of the stress immediately.
— Steven Bird, MD, FACEP, FACMT
“Having that peer-to-peer interaction — and having it quickly on the heels of an incident — offers the chance to vent some of the stress immediately. And the connection can make a difference in someone’s willingness to seek ongoing assistance when it’s needed,” Bird said. “When you’re talking with another clinician, you know they’re just as steeped in the day-to-day struggles of being in health care as you are. They understand what it’s like to be in similar types of crisis situations.”
24 | THE PURSUIT November 202 2 CLINICIAN EXPERIENCECLINICIAN EXPERIENCE
◼
Noticing warning signs
A clinician providing peer support, whether as part of a program or not, should be an active listener and ask questions to give the person an outlet for self-expression, Bird said. This can also help assess whether additional support may be needed and what that might look like. The National Alliance on Mental Illness recommends seeking more assistance if you or a colleague experience warning signs such as:
• Feeling irritable or angry
• Experiencing anxiety, depression, loneliness or constant sadness
• Having thoughts of harming yourself
• Reliving traumatic events
• Isolating yourself
• Lacking trust in others
• Experiencing compassion fatigue, burnout or moral injury
• Getting too much or not enough sleep
• Adding or increasing use of alcohol or other substances
• Experiencing physical issues such as digestive or appetite problems, more aches and pains, sexual or reproductive issues, and executive function and memory problems
Bird emphasizes that it’s important to check in with a colleague who has experienced a traumatic incident — there’s no need to wait for warning signs. Encourage the person to take advantage of a formal peer support program if it’s available. While Bird has seen a decrease in referrals to his office as the pandemic has waned, requests continue on a steady basis. In the last three months of 2021, his office received requests for a peer counselor at least once per week. Earlier in the pandemic, requests were coming in every day.
“The effects are hard to measure since the program affects a small number of people and is designed to be a check-in rather than a full counseling program,” Bird said. “There are no records kept. It’s simply an opportunity to talk with someone within a few hours of a potentially upsetting or disturbing situation — and it can make a tremendous difference.”
Physicians and medical students throughout the U.S. can receive free, confidential emotional support via the Physician Support Line, which is staffed by a volunteer network of psychiatrists. Call 1 (888) 409-0141, 8:00 a.m. to 1:00 a.m. ET, seven days a week


Risk Assessment Algorithm Predicts
Level of Care Patients Will Need
First developed for a COVID-19 field hospital, this predictive analytics tool shows how data can drive health care innovation.
A cross-functional team developed a predictive analytics tool to help emergency room physicians predict whether COVID-19 patients would continue to have mild or moderate symptoms that could be safely addressed in UMass Memorial Health’s field hospital. After being successfully used in the field hospital environment, the same predictive analytics tool has been deployed to assess patient risk elsewhere in the hospital system.
With all the COVID-19 information amassed since the start of the pandemic, it can take a moment of reflection to remember just how little was known about the virus in early 2020. As people flooded hospitals, staff members scrambled to figure out ways to treat patients while avoiding getting sick themselves. There seemed no rhyme or reason as to who would overcome the illness and who would succumb.
When David McManus, MD, talks about those early days of the pandemic, he emphasizes the lack of knowledge and extreme conditions hospitals were confronting all day, every day.
“We were making decisions without data,” said McManus, Chair, Department of Medicine, UMass Memorial Medical Center, and Professor, UMass Chan Medical School. That was an untenable idea for him, because he knew that at least some data could be extracted from the Medical Center’s electronic medical records (EMR) system. And he wanted to figure out how to tap into it to benefit patients.
To start, McManus and Apurv Soni, MD, PhD, Physician Champion for Digital Health at UMass Memorial Health, and Assistant Professor, UMass Chan Medical School, brought together a multidisciplinary group — which included physicians, hospital administrators, medical
Everyone started referring to [DECOMP scores] during our noon calls when we would discuss eligible patients: ER docs, nurses, the field hospital team and case managers.
Even now, ER docs refer to DECOMP scores when making decisions.
— John Broach, MD
students, and experts in digital medicine and clinical informatics. The team abstracted the EMR information of 1,000 COVID-19 patients who had been seen at the Medical Center.
“Then we asked 50 of our UMass Chan Medical School students to validate data on each patient’s symptoms, history and outcomes,” he said. “The next step was teaching a computer to look at the charts, go back into the information that would be available to an emergency room doctor, and predict whether individual patients would be OK or whether they would decompensate.”
Predicting risk for COVID-19 patients
Co-developed by McManus and Soni, the resulting proprietary predictive analytics tool — Decompensation
THE PURSUIT November 2022 | 27
◼
CLINICIAN EXPERIENCE DIGITAL MEDICINE
DIGITAL MEDICINEDIGITAL MEDICINE
Electronic COVID Observational Monitoring Platform Triage (DECOMP-Triage) — calculated a risk score based on factors such as vital signs, lab results, age, medical history and diagnosis of type 2 diabetes.
The DECOMP-Triage tool identified patients who were
the best match for UMass Memorial’s COVID-19 field hospital, which had capacity to care for patients with mild or moderate symptoms. The UMass Memorial DCU Center Field Hospital opened in a Worcester arena and convention center on April 9, 2020, when the state of Massachusetts was dealing with its initial surge of

COVID-19 cases. It was the first field hospital in the state. A total of 161 patients had been treated at the hospital by the time it closed in May 2020, although the facility would need to be reopened later in the year.
Since the field hospital did not have an intensive care unit, it was especially important to make sure only the patients
least likely to decompensate were admitted for care.
“We programmed the tool directly into our medical records system to make it available for all hospital teams to use,” McManus said. A patient’s risk score was instantly accessible to the entire care team, without adding extra steps to an already-busy workflow.
Photo by Joseph Prezioso
— David McManus, MD
Building on DECOMP-Triage’s success
The team continues to explore new ways to learn from and apply the predictive analytics algorithm in other care environments in the hospital system.
“The success of using the DECOMP-Triage tool in our field hospital taught us a lot about how data could be a driver of innovation in our health care system,” McManus said. “We’re building on our predictive modeling algorithms.”
Using risk scores in the field hospital
To ensure accuracy and usefulness of risk scores, the predictive modeling tool calculated them every time a patient’s vital signs or lab data were entered in the EMR and refreshed them every 15 minutes. Categorizing the scores with a DECOMP-Alert of green, yellow or red made it easy for staff to use them. When UMass Memorial reopened the field hospital with capacity for 240 patients in December 2020, case managers had already created guides to instruct team members how to use risk scores as part of existing clinical workflows. (The field hospital stayed open until mid-March 2021.)
Recommendations were based on probability of respiratory failure requiring mechanical ventilation remaining below 5% throughout the hospitalization. A patient with a DECOMP-Triage score of:
• 0–3 could be considered for the field hospital on day 0
• 4–5 could be considered for the field hospital after 24 hours, if DECOMP-Alert was green or yellow
• 6–7 could be considered for the field hospital after 72 hours, if DECOMP-Alert was green or yellow
• 8 and higher were not considered for the field hospital because their probability of respiratory failure was greater than 50%
“A big reason why DECOMP scores were so helpful with the field hospital was because there was a common language that was associated with it,” said John Broach, MD, Director, Division of Emergency Medical Services and Disaster Management, UMass Memorial Medical Center, and Director, UMass Memorial DCU Center Field Hospital. Broach also serves as an Associate Professor at UMass Chan Medical School.
“Everyone started referring to them during our noon calls when we would discuss eligible patients: ER docs, nurses, the field hospital team and case managers. Even now, ER docs refer to DECOMP scores when making decisions.”
The UMass Memorial team has grown rapidly and expanded the algorithms developed for the field hospital and applied them in radiology, gastroenterology, homebased acute care and chronic disease management.
These algorithms will be used throughout UMass Memorial to predict outcomes in areas such as:
• Inpatient mortality
• COPD exacerbation that could lead to emergency department visits
• Prodrome of COVID-19, before the onset of specific signs and symptoms
In UMass Memorial Health’s Hospital at Home program, which provides hospital-level care to eligible patients in their own home environments, the predictive analytics tool has become especially important. It takes data from wearable devices, radiology and other imaging, and other EHR information to provide clinical decision support.
“Everything about the patient is uploaded to a portal. We’ve saved 1,000 patient days through Hospital at Home,” McManus said. “The field hospital broke the model of how we’ve been practicing medicine. It forced us to innovate — to build a hospital where there wasn’t one before and to use data and statistical algorithms in ways we hadn’t used them before. Now we’re keeping that innovation going.”
McManus founded two new entities to help facilitate and accelerate digital innovation. The Medical School’s Program in Digital Medicine, directed by Soni, focuses on research and innovation, while the Center for Digital Health Solutions at UMass Memorial Health focuses on implementing and following through on the innovation.
“The partnership between these entities is critical,” said Soni, who serves on the leadership board of the Center for Digital Health Solutions. “By leveraging the Program in Digital Medicine’s ability to develop innovative tools like DECOMP-Triage and the Center for Digital Health System’s ability to systematically implement them, we can be at the forefront of medicine.”
30 | THE PURSUIT November 202 2 DIGITAL MEDICINE
◼
The field hospital broke the model of how we’ve been practicing medicine. It forced us to innovate.
I NNOVATION HEALS
is at the core of who
are and how we
our
to serve. Innovation leads to discoveries and creates new ways to cure.

provides
and gives peace of mind. Innovation leads to better health and more care for more people.
saves lives and helps us heal, relentlessly.
Marketing and Communications Department 100 Front Street Worcester, MA 01608 NONPROFIT ORG. U.S. POSTAGE PAID WORCESTER, MA PERMIT NO. 176 Innovation
we
fulfill
mission
It
hope
Innovation