IOWA VISION





With the current academic year coming to a close, I would like to take an opportunity to provide you with a brief update on the department and share a few highlights from this past year.
We remain proud of our tradition of excellence and our commitment to patients and the ophthalmology profession. Iowa’s program continues to be well-regarded by our peers—once again ranking in the top ten in the U.S. News & World Report’s annual ranking of top-ranked hospitals for Ophthalmology. This ranking is one measure of the reputation our department has developed and a reflection of the overall consistency we have in our faculty and staff.
Thanks to the hard work and dedication of our faculty and staff, the department continues to provide exceptional clinical care. Patient volumes continue to grow and so does the number of faculty. We’ve added Dr. Kanwal Matharu to our cornea team, Dr. Marc Toeteberg to our glaucoma team, and Dr. Ryan Diel joins our comprehensive team. Dr. Michael Wall, Dr. Karen Gehrs, Dr. Tim Johnson, and Dr. Scott Larson are departing from the department. We wish them all the best in their retirement and further pursuits.
Education, excellence, and innovation remain a cornerstone for Iowa’s eye program. We continue to be passionate about training and shaping future ophthalmologists into leaders within the specialty and in practice. In July of 2023 we welcomed our second class with six residents. As the 2026 and 2027 resident classes move through their training, we anticipate continued growth within our program. Increasing from five to six residents, will help us keep up with the demand for our graduates nationally and in our referring region. Most importantly, this change has allowed us to expand educational offerings, mitigate our risk of fatigue issues, and better meet the demand for our graduates.
Due to the efforts of our faculty and staff, our program has an excellent reputation as evidenced by being the #2 ranked Ophthalmology Residency Program and #5 ranked Ophthalmology Department in the country by Ophthalmology Times, as well as moving up to the #6
spot in US News & World Report’s 2023 rankings. This is reflected by our graduates being in high demand for fellowship and practice positions.
Related to our training programs, we started a fund to help continue Operation HawkEyeSight, a resident run endeavor at the free clinic in Iowa City that provides exams and surgeries at no cost. We are also funding a Diversity Visiting Student Scholarship, which was previously awarded to Adetayo Oladele-Ajose when she was completing a rotation at Iowa—and now Adetayo is now a second-year resident with us! We’ve completed work on our new simulation lab, which was funded by alum Dr. John Graether, and it is up and running. This new space will provide new opportunities for our department’s trainees.
Clinical research activity continues to expand as we explore new treatments and potential cures for eye diseases. We have nearly 30 trials taking place that involve new devices and treatments. Some of the clinical trials and studies underway involve Thyroid eye disease, cornea transplant preservation, Radiation Retinopathy in Uveal Melanoma, Bardet-Biedl Syndrome 10, X-linked retinoschisis, Orbital Adnexal Tumors, Retinoblastoma, Sepofarsen in Leber Congenital Amaurosis, and 3D Image Analysis Approach to Determine Severity and Cause of Optic Nerve Edema. Perhaps most exciting is our continued progress with gene and stem cell therapy research. It certainly is exciting to lead and participate in so many studies to treat eye disease and potentially restore vision!
Our research efforts, in the department, at the Institute for Vision Research , and at the V.A. Center for Prevention & Treatment of Visual Loss , continue to garner attention and funding support. All of this continued success is a reflection of the interdisciplinary research and collaborative spirit among our faculty, researchers, and staff.
While healthcare seems to be shifting in different ways, one area of uncertainty is the incredibly generous support we receive from our many alumni and donors. In FY23, we were fortunate to have received over $14 million,
“State of the Department” continues on page 6
WRITTEN BY: ELLA J. GEHRKE
For Kasen Cochran, a 17-year-old high school junior from Winterset Iowa, wrestling is not just a passion—it’s part of his identity. From earning a varsity spot as a freshman to competing at team state and nationals, Kasen is a gifted athlete.
Kasen also has Juvenile X-linked Retinoschisis (JXLR), a rare genetic eye condition that poses a constant threat to his vision. The condition causes cysts to form within his retina, disrupting the transmission of light signals to the brain and significantly impacting his sight.
Like many patients with rare health disorders, Kasen’s road to diagnosis was not straightforward. It wasn’t until he was 12 years old and struggling to track flyballs on his baseball team that his parents realized something was amiss. “We wondered if he just needed glasses at that time and took him to an optometrist who thought he might have lazy eyes,” says Kasen’s dad, Brad Cochran. After a series of visits to optometrists and ophthalmologists, Kasen eventually received the diagnosis of JXLR, and was told of his increased risk of eye damage and the potential for partial or complete vision loss, even from mild eye trauma. This devastating news meant he would likely have to give up any sports where there’s potential to be hit in the eye. Juvenile X-linked retinoschisis is a challenging condition that currently does not have a known cure. Individuals with JXLR are often advised to take precautions such as avoiding contact and ball sports and wearing protective eyewear in high-risk settings.
At just 12 years old, Kasen had already developed a strong passion for competition, which made this news particularly difficult for him. “Up until this point, he was very chill about the diagnosis, but when he was told he had to give us sports, that’s when it really set in for him” says mom, Mindy Cochran, “we knew this would really change his life, because sports are what he loves most.”
Ultimately, the Cochran family was referred to Arlene V. Drack, MD, a pediatric ophthalmologist who specializes in genetic eye diseases at the University of Iowa, located two and a half hours away from the Cochran’s home. From the moment they met Dr. Drack, Kasen and his parents felt that his diagnosis wasn’t the end of his story. Dr. Drack quickly reassured them that Kasen’s well-being was her top priority, and she was determined to help him find a way to continue pursuing his passions while safeguarding his eyesight. “She gave us hope,” recalls Mindy.
Although a no cure for JXLR has been identified yet, Dr. Drack and her team are dedicated to several ongoing research efforts. When she is not in the clinic, Dr. Drack leads a laboratory on campus, conducting in-depth studies to expand what is known about this disease. The Drack Lab’s primary focus is gene therapy, with the aim of repairing the gene responsible for causing JXLR, along with exploring additional therapies that are specifically designed to benefit children, like Kasen.
What was initially seen as a disability now simply represents Kasen and his abilities as a wrestler. The goggles have become a unique and integral part of his wrestling gear.
After Kasen’s diagnosis, his parents diligently searched for effective ways to safeguard his eyes from trauma. They exhaustively tried different types of athletic goggles, including mesh goggles, but none proved satisfactory. Some goggles were plagued by fogging issues, while others were easily dislodged during wrestling matches. However, a chance encounter with a fellow JXLR patient and wrestler from Michigan opened new possibilities. Mindy, Kasen’s mother, reached out for advice and connected with the family from Michigan. It was here that they discovered a unique solution: women’s lacrosse goggles. These goggles, now iconic in the Iowa wrestling community because of Kasen, fit snugly against Kasen’s face without gaps and are secured in place with specialized wrestling headgear.
When Kasen first started wearing goggles at wrestling tournaments, he would often catch people looking at him and his goggles. But as he continued to excel in the sport, pictures of Kasen in his goggles started appearing throughout the wrestling community and he (and his signature goggles) began to gain notoriety. In the closeknit world of wrestling, goggles became synonymous with Kasen. Even when he competed out of state, people
recognized him, and the questioning glances stopped. What was initially seen as a disability now simply represents Kasen and his abilities as a wrestler. The goggles have become a unique and integral part of his wrestling gear.
Throughout the wrestling season, Kasen’s mom, Mindy, receives regular inquiries from other parents. On average, she is contacted at least once a week by parents of children who are curious about the goggles. They reach out seeking advice on how to protect their kids’ eyes from potential injuries, so that they can continue to wrestle. It’s not just parents of children with JXLR who approach her, but also those whose children have had previous eye injuries and are looking for ways to ensure their safety while participating in the sport.
Kasen’s athletic talent and unwavering resilience have undoubtedly captured the attention of his wrestling community. Wrestlers, coaches, and fans alike have been inspired by his story, and now easily recognize him by the distinctive goggles. His unique journey has made him a standout figure in the wrestling community, drawing admiration for his wrestling talent as well as his determination and spirit.

“State of the Department” continues from page 2
in philanthropic donations for innovative research, patient care, and scholarly pursuits. These new funds were contributed by over 1,275 donors, including alum Dr. Randy Brenton (‘87R) who pledged $500,000 to support resident, fellow and med student research at Iowa. Funds like this provide a tremendous boost in what we can, and do, accomplish together. If you are interested in investing in our success, please contact me or visit givetoiowa.org/eye
Finally, I can proudly say that I’m grateful to lead and be among such an extraordinary team of dedicated people. On behalf of the department and our Iowa Eye family, thank you for your continued support of the University of Iowa and your partnership in eye care!
Sincerely,
Keith D. Carter, MD Chair and Department Executive Officer
Lillian C. O’Brien and Dr. C.S. O’Brien
Chair in Ophthalmology
After a pair of complex surgeries, alumna Christi Eldred is thankful for a UI medical team’s collaborative expertise.
BY JOSH O’LEARY
When Christi Eldred (93BA) learned she had a fistula behind her right eye—a dangerous condition that threatened her vision and, potentially, her life—she could have traveled anywhere for treatment.
She and her husband, former Hawkeye and Major League Baseball pitcher Cal Eldred, had medical connections around the nation from his days as a player and coach. But the Eldreds knew Christi would receive unparalleled care at University of Iowa Hospitals & Clinics, just a half-hour drive from their home in Mount Vernon, Iowa.
Thanks to a quick-acting team of UI neurologists and ophthalmologists—and after two marathon surgeries—Christi Eldred’s decision to stay in her home state for treatment turned out to be the right game plan. “I just knew they were going to take care of me—and they did,” she says.
The first signs of trouble surfaced in fall 2021, when Eldred began noticing a prism-like distortion in her vision’s periphery. Eldred had been fighting a recent sinus infection and headaches, but this seemed different. Her right eye became swollen and red, and an uncomfortable pressure built up behind it, keeping her awake at night.
Eldred’s family physician and eye doctor were stumped. They referred her to UI Hospitals & Clinics, where she underwent a battery of tests in the Emergency Department, including an MRI scan. The images ruled out an abscess or tumor, but a closer look by ophthalmologists and further testing the following day revealed the problem: carotid cavernous fistula. Simply put, there was an abnormal connection between a carotid artery and a vein called the cavernous sinus, creating a backflow of blood and putting pressure on the back of Eldred’s eye. Left untreated, there was a chance the fistula could rupture and cause bleeding in the brain.

UI neurointerventional surgeon Santiago Ortega-Gutiérrez examined Eldred and put her on a fast track to the operating room. In an initial procedure, which lasted about five hours, the clinical associate professor of neurology performed an angiogram through an artery in her arm to map out the path to the problem area between her brain and eye. He then attempted to embolize the fistula using a catheter inserted into the femoral vein in her thigh but was ultimately unable to reach it because the usual pathways were clotted. Knowing they’d need to take a more direct route, Ortega-Gutiérrez brought in an orbital surgeon, clinical professor of ophthalmology Erin Shriver (06R), to help him access the superior ophthalmic vein—a small blood vessel that travels from the front of the eye socket to the cavernous sinus.
Shriver consulted with colleagues through the North American Society of Academic Orbital Surgeons before devising a new plan with Ortega-Gutiérrez and practicing the technique with her oculoplastics team. Once Shriver was prepared for the surgery, she spoke with Eldred and explained that, while she hadn’t performed this exact procedure before, she was confident in this territory.
“I thought it was important that I be open and upfront with her because she had a very serious condition, and I wanted her to have the best outcome possible,” Shriver says. “We discussed the option of her getting a second opinion or going elsewhere for her surgery, but she stressed that she felt comfortable with

With Eldred’s symptoms progressing rapidly, she gave the go-ahead for the orbitotomy early the following week. In the operating room, Shriver made an incision just above Eldred’s right eyelid crease, dissecting into
the orbit, or eye socket, and navigating through the fat and tissues to isolate the superior ophthalmic vein. She then stabilized the delicate vein and elevated it for placement of the microcatheter, giving Ortega-Gutiérrez an open pathway to the fistula.
After the second five-hour surgery—which at times required improvisation and trial and error with different instruments—Shriver, Ortega-Gutiérrez, and the Iowa team successfully sealed off the abnormal connection. Shriver credits the unique teamwork between surgeons, fellows, technicians, nurses, and anesthesiologists for the successful outcome. “There were several times during the case that we could have easily given up,” she says. “We knew that neurosurgery was her only other option, however, and so we persisted.”
Ortega-Gutiérrez says the unique surgery was only possible because of the UI’s multidisciplinary expertise in neurointerventional surgery and ophthalmology. Because of that collaboration, Eldred did not have to undergo a more aggressive, invasive brain surgery.
“In specialized centers like ours, we have the luxury of having a great deal of endovascular and oculoplastic expertise,” says Ortega-Gutiérrez. “Working together with Dr. Shriver allowed us access into the small veins located within the orbit to open the pathway for me to get into the brain.”
With the pressure relieved from her ocular nerves, Eldred’s vision soon corrected itself, and she made a full recovery. The radiation from imaging resulted in temporary hair loss, and it took her a few weeks to fully get back on her feet, but Eldred was thankful that doctors were able to attack the issue in a way that minimized the trauma to her body. Two years later, she has 20/20 vision, and follow-up testing has given her a clean bill of eye health.
“For people like me, whose situations are complicated, you need doctors who are not afraid to try complicated things,” says Eldred, a mother to five adult children and two grandkids. “They saved my eye, so there’s no better outcome.”


On October 13th we officially opened the new Dr. John M. Graether Ophthalmology Simulation Laboratory. This new simulation lab is an ophthalmology-dedicated space and includes seven stations—one teaching station and six learning stations. Each station includes a tabletopmounted operating microscope with a foot pedal to control the scope. Each station also has a monitor that shows what is seen through the microscope and each monitor can be projected to the large screen at the front of the room. In addition to these stations there is also an Eyesi surgical simulator with retina and phaco capabilities, as well as an Eyesi slit lamp simulator.
This new simulation lab was made possible by the generous gift of Dr. John Graether, who was on hand at the dedication of the new lab. Dr. Graether was a resident and fellow at Iowa and wanted to add resources that allow trainees to get hands-on experience. Below is part of what Dr. Graether shared at the opening of the new lab that is named after him.
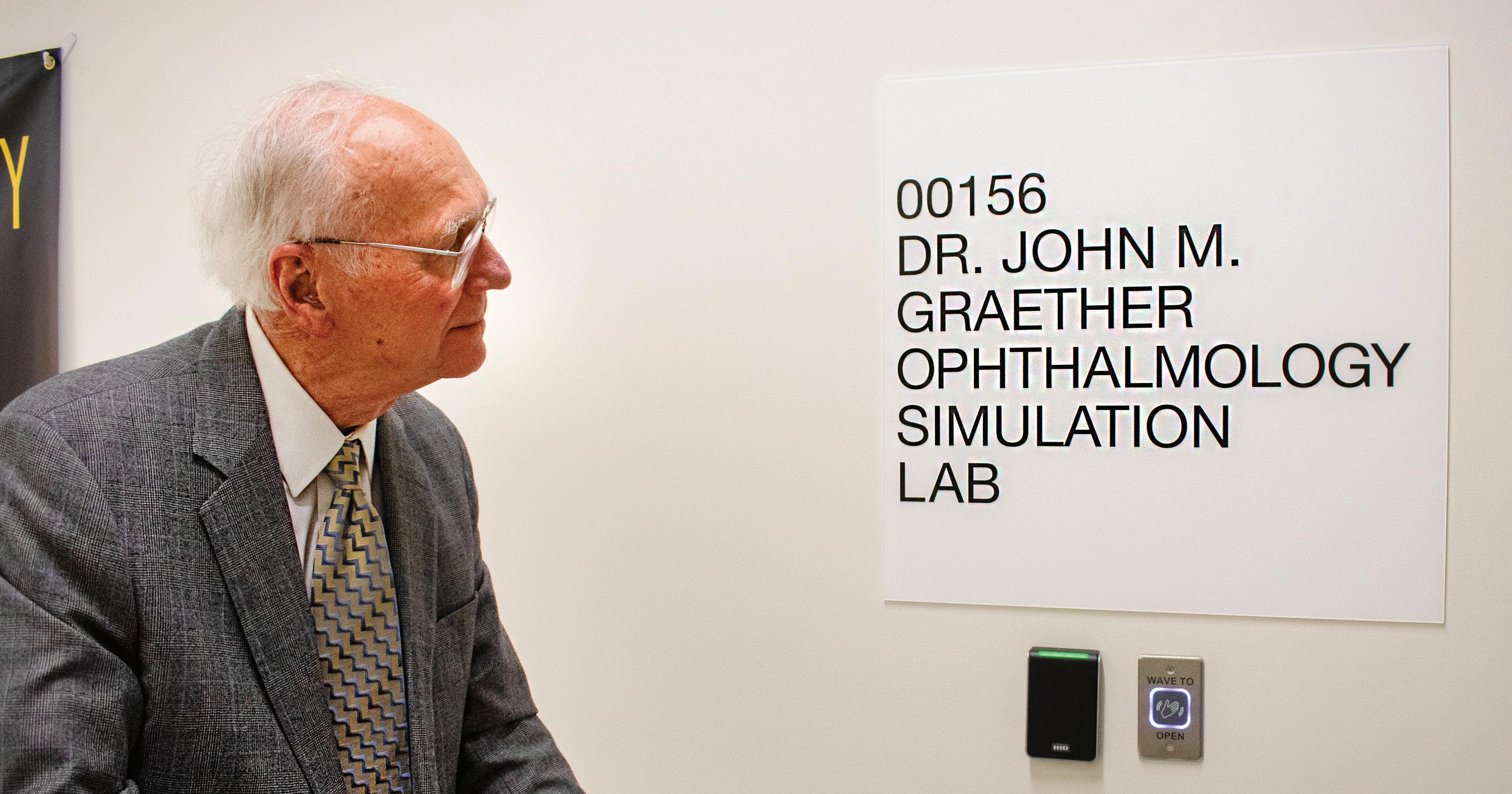
“I feel privileged to be involved in the acquisition of this simulation lab for our consistently highly rated University of Iowa Eye Department where I trained as a resident and fellow.
Changes in our medical delivery system have resulted in limited availability of hands-on operating room experience. With the delft skills now required to handle the delicate tissues of the retina and cornea in many microscopic procedures, simulation laboratories have become essential for recruiting the best resident and fellow candidates and train them both in and outside the operating room.
I have also enjoyed promoting and funding innovation by other surgeons, such as my good friend and former colleague Donny Suh, now head of Ophthalmic Pediatrics at UC-Irvine, and others so that they could have a similar career experience during this period of enormous changes in our specialty in the treatment of many eye diseases. I consider this laboratory a fitting legacy that I believe will continue to advance our shared surgical growth.”
Dr. Jaclyn Haugsdal, Director of Simulation Education, also shared some thoughts on the new sim lab.
“The main question I get asked a lot is “why does ophthalmology need our own space if the shared hospital simulation space works well for our purposes?” My response is that our space will have adjustable tables and chairs and a microscope foot pedal at each station so ergonomics and microscope management can be appropriately practiced. Additionally, the other departments that use the shared sim lab space do lots of bone drilling and the space gets dusty and dirty, which is a non-issue in our new space that is ophthalmology specific. Additionally, having our own space means we have control of storage and availability. The shared space is in high demand, and we often ran into scheduling issues.
The goal of the Dr. John M. Graether Simulation Lab is to provide a training space that is easy to come down to practice at any point without having to reserve space or get special access or having to find supplies from various locations.”
The P. J. Leinfelder award was inaugurated in 1982 by alumni who wished to pay tribute to Dr. Leinfelder -- scholar, teacher, and physician. Dr. Leinfelder served on the staff of the Department of Ophthalmology from 1936 to 1978. A faculty committee presents awards each year to the resident and fellow physicians who have made significant contributions in preparing and delivering seminars.
Resident Winner:
Joanna Silverman
“Is Suction-based Tectonic Stabilization Protective Against Endothelial Loss?”
Fellow Winner: Margaret Strampe
“Quality of Life Improves After Strabismus Surgery”
Randall S. Brenton, M.D. (83MD, 83F, 88R) and Cheryl J. Brenton established the Brenton Research Award through a generous gift provided in 2023. This award acknowledges outstanding research endeavors by residents and fellows dedicated to furthering the field of ophthalmology.
Resident Winner: Mahsaw Mansoor
“Cost Savings in Multidose Protocol for Cataract Surgery: A Pilot Study at UIHC”
Fellow Winner: Giulia Steuernagel Del Valle
“Flash Visual Evoked Potential in Pediatric Inherited Eye Disease”








Judith Brody, MD
Ophthalmology Residency, Department of Ophthalmology, Rabin Medical Center, Petach Tikva, Israel
Lindsay Chun, MD
Ophthalmology Residency, Department of Ophthalmology and Visual Sciences, University of Chicago
Kyle Green, MD
Ophthalmology Residency, University of Rochester, Flaum Eye Institute, Rochester, NY
Christian Mays, MD
Ophthalmology Residency, Virginia Commonwealth University Health System, Richmond, VA
Taariq Mohammed, MD
Ophthalmology Residency, University of Maryland Medical Center, Baltimore, MD
Rupin Parikh, MD
Ophthalmology Residency, Dean Mcgee Eye Institute, Oklahoma City, OK
Marina Peskina, MD
Ophthalmology Residency, Jamaica Hospital Medical Center, Richmond Hill, NY
Margaret Strampe, MD
Ophthalmology Residency, Department of Ophthalmology and Visual Sciences, University of Iowa, Iowa City, IA






Oladipupo Anibire, MD MD, Meharry Medical College
Donavon Dahmer, MD MD, Frederick P. Whiddon College of Medicine, University of South Alabama
Marshall Henrie, MD MD, Spencer Fox Eccles School of Medicine, University of Utah
Paige Noble, MD MD, Roy J. and Lucille A. Carver College of Medicine, University of Iowa
Adetayo Oladele-Ajose, MD MD, Jacobs School of Medicine and Biomedical Sciences, SUNY - Buffalo
Zachary Richards, MD MD, Texas A&M Health Science Center















Salma Dawoud, MD
Oculoplastics Fellowship, Medical College of Wisconsin, Milwaukee, WI
Beau Fenner, MD, PhD
Consultant in the Department of Medical Retina, Singapore National Eye Centre, Singapore
Christopher Fortenbach, MD, PhD Faculty, University of Washington, Seattle, WA
Natasha Gautam, MBBS, MS Glaucoma Fellowship, Mayo Clinic Rochester, MN
H. Douglas Jin, MD Northwest Retina, Everett, WA
Jamie Keen, MD Loyola Medical Center and Private Practice, Chicago, IL
Edward Linton, MD
Neuro Ophthalmology Faculty, University of Iowa, Iowa City, IA
Guneet Mann, MBBS, MS
Pediatric Ophthalmology Fellowship, Texas Children’s Hospital, Houston, TX
Araniko Pandey, MBBS
Uveitis Fellowship, Bascom Palmer Eye Institute, Miami, FL
Sean Rivera, MD
Eye Associates of New Mexico, Albuquerque, NM
Adriana Rodriguez Leon, MD Neurology Faculty VA Medical Center, Coralville, IA
Emily Witsberger, MD
Pediatric Cornea and External Disease Fellowship, Hospital for Sick Children, Toronto, Ontario
Matthew Field, MD, PhD
Cornea/Anterior Segment Fellowship, Minnesota Eye Consultants Minneapolis, MN
Zachary Mortensen, MD
Eye Associates of Colorado Springs Colorado Springs, CO
Tirth Shah, MD Georgia Eye Clinic Atlanta/Athens, GA
Margaret Strampe, MD
Pediatric Ophthalmology Fellowship, University of Iowa, Iowa City, IA
Caroline Yu, MD
Oculofacial Plastic Surgery Fellowship, Mayo Clinic, Rochester, MN
Old colleagues reconnected this February at the annual Macula Society meeting. It wasn’t by chance though. Steve Russell, MD nominated Andrew Lotery, MD for the annual Paul Henkind Memorial Lecture and Award. This annual award lecture recognizes a Macula Society member for their exceptional contributions to retina research. When Dr. Lotery was named as this year’s winner, it was Dr. Russell who introduced him at the meeting. “I nominated Andrew because he has performed research and published on the cause of a number of monogenetic and polygenetic (such as AMD) ocular diseases, while also leading many multicenter trials—the most recent of which was to evaluate the treatments for central serous choroidopathy, a puzzling condition that can mimic AMD,” Dr. Russell explained. “On top of his research and trials, he’s also built an ophthalmology department, including a training program, from scratch at the University of Southampton.” Although an ocean separates them these days, over 20 years ago, they both served on faculty at Iowa.
Dr Lotery’s connection to Iowa goes back to 1998 when he came to Iowa City for fellowships in medical retina and molecular ophthalmology. He made such an impression that he was offered a faculty position in 2000 when he finished his second fellowship. As he moved from fellow to faculty, Dr. Russell went from trainer to colleague. In addition to time spent learning from Dr. Russell while at Iowa, Dr. Lotery also worked closely with Dr. Ed Stone (among others). His time with Dr. Stone was where his interest in the molecular basis of ophthalmic diseases grew. After serving on faculty at Iowa for two years, Dr. Lotery was offered a position at the University of Southampton and felt it was best for him and his family to return to the UK.
When he arrived at the University of Southampton, he established their first vision research group, and the ophthalmology clinical trials group at University Hospital Southampton. He also developed an anti-VEGF treatment (treatment that prevents the growth of new blood vessels in affected eyes) and photodynamic therapy for age-related macular degeneration. Despite being separated by an


ocean, Drs. Lotery and Russell continued to collaborate. “Since Andrew left, we have collaborated on the testing of our Low-vision Enhancement Optoelectronic (LEO) project,” Russell said. “This is an electronic device that uses a camera and vibration signals to inform the user of hazardous or desirable objects in their path. We are still developing a more user-friendly and reliable device.”
Dr. Lotery is currently leading a UK multi-center clinical trial evaluating photodynamic laser treatment for central serous chorioretinopathy funded by the National Institute for Health and Care Research (NIHR), as well as an international research project funded by the Wellcome Trust evaluating machine learning as a tool to better understand age related macular degeneration (AMD). He is also participating in several clinical trials at different stages evaluating novel treatments for AMD and inherited retinal diseases. Current laboratory work includes developing cell models of AMD and assessing the value of gene therapy in AMD.
Beau Fenner, MD, PhD grew up enjoying the beautiful waters off the southwestern coast of Australia – yet his pursuit of the best education led him to some of the top institutions around the world, including in Ireland and Singapore. During ophthalmology and medical retina fellowship at the National Eye Centre in Singapore, he developed an interest in inherited retinal diseases (IRD). Seeing an opportunity to create a leading ocular genetics center in Asia, he sought the best training in IRDs he could find. “I was looking for somebody who not only knew inherited retinal diseases inside and out—but who was also prepared to spend time training me,” described Dr. Fenner. “As fate would have it, Dr. Ed Stone at University of Iowa had recently initiated an IRD fellowship that was intended for people who wanted to make IRDs a central part of their career.”
Leaving behind the urban bustle of Singapore for the cornfields of Iowa City, Dr. Fenner served as the inaugural Mina Chung Fellow in Inherited Retinal Disease from 2022-23. Moving his family in the midst of a pandemic was no trivial decision, but one made simpler thanks to the strong reputation of the University of Iowa and the opportunity to experience life in the Midwest. “In addition to the fellowship itself, location was an important part of my decision,” said Dr. Fenner. “I have 3 young children who have grown up in a large and densely populated city, so the opportunity for them to experience more of the outdoors, much like where I myself grew up in Western Australia, was just too good to pass up.”
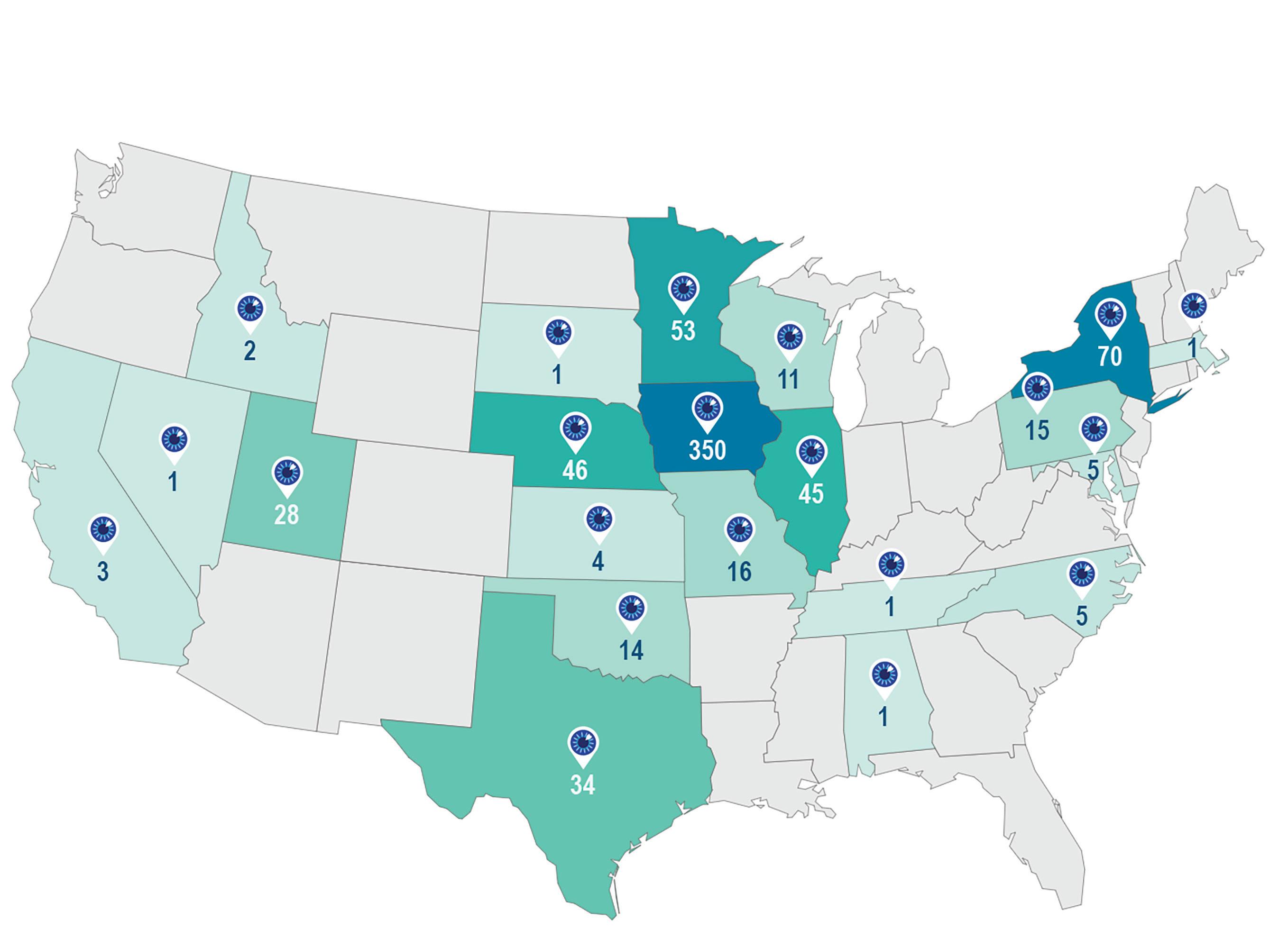
Iowa’s unique environment, which balances intense, world-class training with a welcoming, family-friendly setting, has attracted many of the brightest minds in ophthalmology for decades. Over the past 60 years, the University of Iowa has trained over 120 retina fellows who have become go-to physicians in their community and leading examples of excellence in clinical care, teaching, and research. Iowa retina fellows currently practice in over 30 states in the US and numerous places internationally, including Canada, England, China, and New Zealand. Prominent alumni include Dr. Andrew Lotery, featured on page 11 as this year’s prestigious Paul Henkind Award winner from the Macula Society.
“The fact that Beau moved his family halfway around the world speaks to the strength of Iowa’s global reputation and the relatability of our collegial culture, including through visionary leaders like Ed Stone, a guiding figure in inherited retinal disease for decades” says Dr. Ian Han, Director of the Retina Service, who worked closely with Dr. Fenner for the year. “It was a joy to have Beau at Iowa – he quickly wove himself into the fabric of our department and was an exemplary doctor for our patients, as well as an influential teacher to the residents.”
Dr. Fenner remembers his time in the department fondly and found the family atmosphere at Iowa especially unique. “I was consistently surprised by how warm and welcoming the clinical faculty and trainees were. It’s
really something that stood out to me, especially when compared to other large teaching hospitals where there are limited opportunities to spend quality time with teaching faculty.”
For Dr. Fenner, fellowship in Iowa was a springboard to leadership and innovation back home. “Within a few months of returning to Singapore, I was given the opportunity to create and lead an Ocular Genetics Service at the Singapore National Eye Centre,” Dr. Fenner notes. “On the research side, I’ve recently formed some strong collaborations with basic scientists from our affiliated eye research institute and we are now developing targeted therapeutics that are relevant to IRD patients here in Singapore.”
For Dr. Fenner and other Iowa fellows, the time spent in training is just part of a lifelong relationship. “We miss Beau a lot,” says Dr. Han, “but I’m glad that we still get to work together on research collaborations. During his time at Iowa, Beau authored multiple papers, including a landmark paper representing the largest clinical case series ever published for ABCA4-associated retinal disease (see QR code below). We are currently meeting regularly for online lab meetings as part of a multicenter collaboration studying artificial intelligence-based image analysis for inherited retinal disease.”
Dr. Fenner also remains closely connected with Dr. Stone and the Institute for Vision Research, including through monthly virtual didactic sessions on inherited retinal disease for Singapore and Malaysia. These case-based sessions (https://stonerounds.org/teaching/schedule) are attended by participants worldwide and reflect Iowa’s strong reputation internationally, as well as Dr. Fenner’s rising stardom in the field.
Although Dr. Fenner’s time in Iowa was relatively brief, the lessons learned have been enduring. “The time spent in Iowa has played an important role for me when considering what treatment approaches are more likely to be useful for my patients. It’s one of the most challenging areas in ophthalmology, but the potential rewards for patients are incredible,” says Dr. Fenner. “I’m incredibly grateful for the time I got to spend with the UI Retina faculty.”
Read Dr. Fenner’s landmark research paper: https://www.aaojournal.org/article/S01616420(24)00096-4/fulltext

Kanwal Singh Matharu, MD joined the department in 2023 as an Assistant Professor and member of the Cornea Service. After finishing medical school at McGovern Medical School in Houston, Dr. Matharu stayed in Houston for his residency at Baylor’s Cullen Eye Insitute. After residency, Dr. Matharu completed a cornea fellowship at the University of Pittsburgh Medical Center before heading to Stanford University for a fellowship in Global Ophthalmology. We asked Dr. Matharu some questions about his vision for global eye care at Iowa.
Interviewer: Tell me about your background in global eye care.
Matharu: My background in global eye care, most specifically, is that I did a global ophthalmology fellowship this past year based out of Stanford, and the Himalayan cataract project which is a major nonprofit in the space of global eye care.

Interviewer: Was that your first experience as a physician overseas?
Matharu: Yes, that was my first direct patient care and first experience with in-depth research abroad.
Interviewer: What made you apply for that global ophthalmology fellowship at Stanford?
Matharu: I think having family living abroad, specifically in India, and having that exposure and parents who encouraged me to look beyond my borders and recognize my privilege here at home, instilled in me specific values and interests. In college I had a minor in global health and health policy, but, at that time, I wasn’t able to have any global patient care experiences. In the long run it paid off because I was able to go abroad when I had more tangible skill sets, and I felt like I had much more to offer after having completed a residency and fellowship than I did as a naive undergrad.
Interviewer: Is there a specific moment when you felt like you saw your career encompassing not just your own local practice but a much larger, global network?
Matharu: Since I’ve been at Iowa I keep pinching myself because in a very neat and tidy way, all the different things I’ve been studying are coming to fruition and coming together in synergistic ways. I’ve had incredible mentors, both before I got here and here, who have helped show me how I can tie together these different threads.

Interviewer: Based on your desire to participate in global eye care, why did you choose Iowa?
Matharu: It’s actually an addendum to the previous answer, which was, the more I learned about global health and health policy, from a theoretical perspective at first and then going abroad and seeing how Iowa fits perfectly with all the things I’d studied. Global eye care isn’t just about eyes, it is critically important to have good relations with the local politicians. It is critically important to engage in their community festivals because that is what builds these long-term partnerships. I couldn’t see myself focused on just direct patient care globally. Direct patient care could be the best way for someone else, but for me, I was looking for a more academically focused way to pursue global eye care. In academia, there are kind of three parts: direct patient care, research, and education. What I saw during my global ophthalmology fellowship was the global yearning for more education, and Iowa has been one of the best educational institutions—not only for ophthalmology, but also in terms of our eye banking and just the ethos here—it’s second to none.
Interviewer: In your short time here in Iowa, what are some things that have been coming onto your radar as far as ways to expand our global eye care?
Matharu: During the past year, I have been incredibly amazed at how much global ophthalmology was already happening. I think we just haven’t had a nice, codified expression of it, but people here have been working with Orbis (a nonprofit that works to build eye care systems that cover the full range of eye care services) for a long time. Building out that relationship and sharing our resources is low hanging fruit. With all of the resources we have here, like morning rounds, all these incredible surgical resources, the simulation lab and Stone Rounds (StoneRounds.org), all it took was to send a couple emails to people who I ‘d previously met—program directors in Ghana, Tanzania, India, and Nepal. I shared the link to Stone Rounds and suddenly, we started seeing participation from new people in those locations. It’s already what’s been happening at Iowa, and there are already people here doing things that are innovative and could easily translate to ophthalmic education globally. Same thing with the Iowa Lions Eye Bank—our eye bank is world renowned for teaching on a one-to-one level. There are simple things happening regularly here that we can easily share—from surgical techniques, to research, to clinic management.
Interviewer: What would you like global eye care to look like at Iowa in five, ten or twenty years? Do you have a vision for that far down the road?
Matharu: Definitely! In five years, I’d like to have physicians from low- and middle-income countries routinely coming to Iowa to learn from our teams, not just the physicians but also the nurses and techs, etc. and for us to have built out a robust library of videos so that we can export all that information cleanly and efficiently.
At ten years, it would be great if we had identified a partner institution or partner practice in a low- or middle-income nation with the goal being to raise the level of care in a region such that everyone else in the region—private practices, government, hospitals—also raise their volume and quality of care to build out a really robust relationship between that entire region and our institution.
The twenty-year vision would be that we have figured out how to do all of this as an institution and we can share our best practices with other institutions that want to create their own global eye care program. I think we’re on that path and it’s perfect timing because the American Academy of Ophthalmology is now really invested in global ophthalmology because so many young ophthalmologists are excited about it. Because of the prestige and experience and reputation of Iowa’s ophthalmology department, we were invited to participate in the Global Ophthalmology Consortium. So even though we are just starting to organize our own efforts, we are already participating at the national level.
Interviewer: Any other thoughts you have on global eye care?
Matharu: I think the one thing I’d really like to highlight is that global does not mean International. Global means looking everywhere and seeking to reduce health disparities no matter if they exist on another continent or just across town. I’m really proud to be part of the Iowa ophthalmology department because they’ve already been taking care of our local population with initiatives like Operation HawkEyeSight and being the safety net hospital for the whole state of Iowa. So I think that emphasis has always been a part of the ophthalmology department at Iowa and I’d like to continue to encourage that and figure out how we can teach others how we’ve been doing that. And I think that’s a very important part of our global ophthalmology experience here.

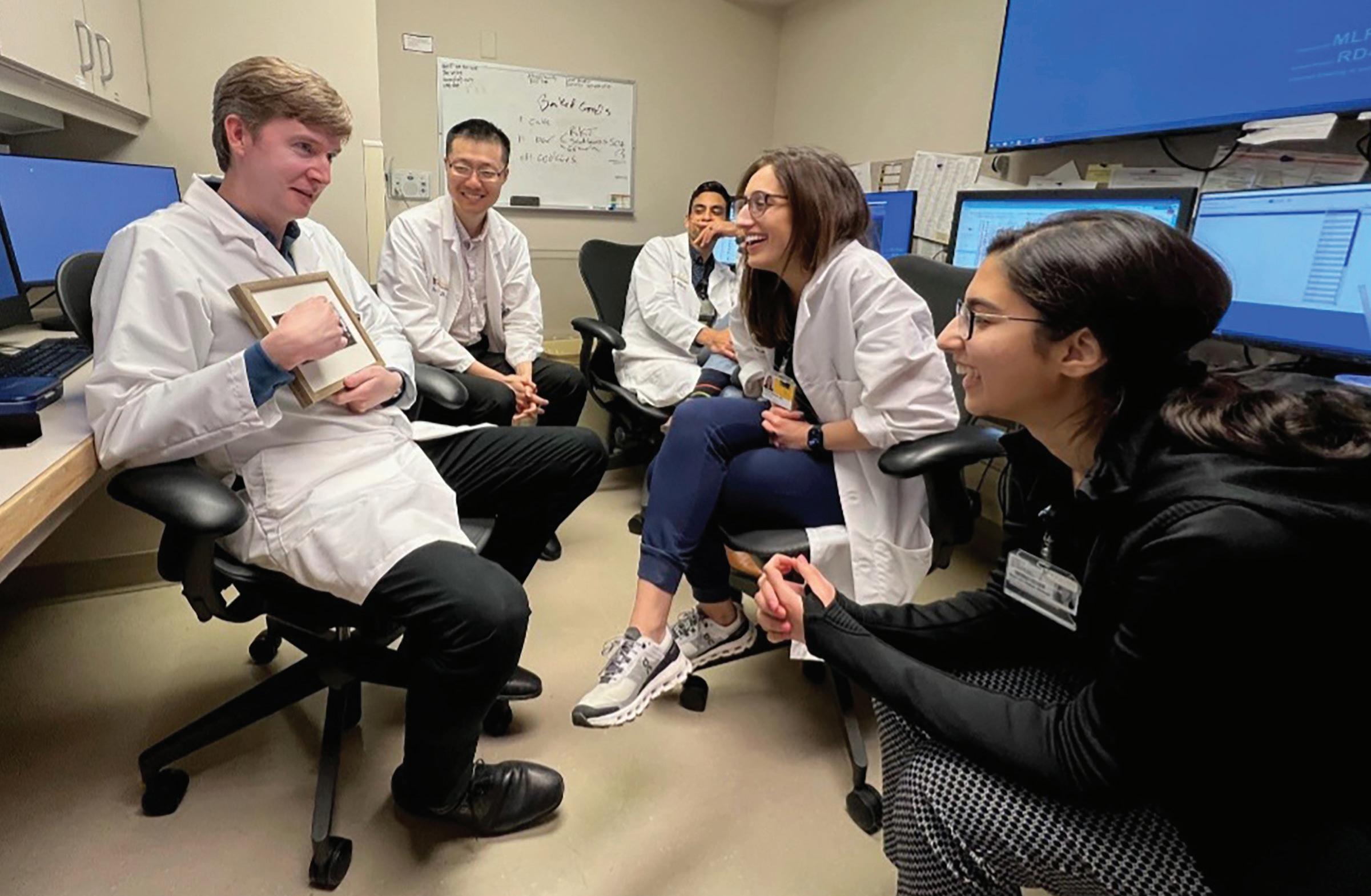
UI ophthalmology residents treat eye conditions such as cataracts and diabetic retinopathy through their volunteer work with Operation HawkEyeSight.
While also working to serve people across the globe, the Ophthalmology Department at the University of Iowa knows that global outreach must also reach those in our own community.
ARTICLE BY SHELBI THOMAS
For years, a patient of the Iowa City Free Medical and Dental Clinic found joy in lovingly preparing pupusas—a traditional El Salvadorian dish of corn griddle cakes—for family and friends. But over time, her eyesight deteriorated so much from cataracts that the delight of cooking became a struggle.
University of Iowa ophthalmology residents who volunteer at the clinic regularly saw her and other lowincome and uninsured patients whose vision could be restored—if only they had access to the proper treatment. Despite a strong desire to expand the services offered, resident volunteers were restricted to diagnosing patients and prescribing eyeglasses or eye drops due to the cost of vision restoring procedures.
To further break down barriers to accessing local health care, resident volunteers identified cataracts and diabetic retinopathy as two of the most common causes of major vision loss that they could address at the free medical clinic. “Those diseases tend to affect these patients worse and to a greater degree, just because they don’t have as good of access to care to keep those things under control,” says Andrew Pouw, an ophthalmologist and UI clinical assistant professor of ophthalmology and visual sciences who advises the clinic’s resident volunteers. “And they can be permanently blinding.”
For the past two years, the resident volunteers have secured a $100,000 UI Carver College of Medicine grant addressing health disparities to purchase the necessary equipment for diagnosing and treating eye diseases. They worked with UI Health Care leadership for administrative clearance and to schedule cataract surgeries at the Iowa
River Landing facility twice a year. With the purchase of portable equipment, the laser treatment for diabetic retinopathy can be performed at the free medical clinic in Iowa City every other month.
Already, the resident volunteers have helped dozens of patients restore their sight—and they are continuing to seek ways to extend their reach. That includes plans to offer more treatments for other eye diseases, spread awareness of the program to optometrists across Iowa, and find additional funding to help maintain equipment, expand services, and manage cataract surgery costs. Sean Rodriguez, one of the resident volunteers who leads the effort, says he’s encouraged to see more than 50 volunteers—from ophthalmology and anesthesia faculty, fellows, and residents to medical students—join Operation HawkEyeSight. “Getting involved in this helps keep a great perspective on what’s important, which is taking care of the patient—regardless of the cost,” he says.
In August 2022, the pupusa maker became one of the first free medical clinic patients to benefit from cataract surgery. “It was a very touching moment when she came out and was able to see again for the first time in a long time,” says Pouw. “A lot of tears were shed. That’s why our resident volunteers do this.”
During a postoperative visit to the clinic, the woman could finally clearly see the faces of the volunteers who restored her sight. Able to return to her livelihood of making pupusas, she brought a cooler of her specialty dish to the clinic to thank her healers for helping her return to the cooking she loves.
A northwest Iowa family launches Brews for Blindness to spread hope to those affected by vision loss.
BY TYLER STRAND
Rob Hage struggles to hold back the tears. Every day he thinks about his grandkids facing the same inherited eye disease that afflicts him and his son. These aren’t tears of grief, however. They’re tears of joy.
Hage is overcome with hope and gratitude, because he has reason to believe his grandchildren will never have to experience the fear of blindness that he and his son have faced. He knows firsthand that the University of Iowa Institute for Vision Research has discovered a potential cure and preventative treatments for rare heritable conditions like retinitis pigmentosa and one of the most common forms of vision loss, macular degeneration. The IVR aims to make these treatments widely affordable and available within a matter of years.

Rob Hage (second from left, back row) and his family gather at Coralville’s Backpocket Brewing to celebrate the launch of the pilot beer for Brews for Blindness.
To help expedite that process, Hage’s family is raising awareness and money for the IVR through craft beer. In September 2021, the Hages started their own brewery, Blind Butcher Brewing, in Inwood, Iowa, and raised more than $42,000 within a year. Earlier this summer, the family launched Brews for Blindness—a nonprofit that’s organizing other community-minded breweries to join its mission. Each partner can designate a new or existing beer to the cause, allocating a portion of sales to the IVR. Together, these efforts will spread hope and empower others to help cure blindness, one beer at a time. “There’s no reason we have to leave anybody behind in this disease; we can help everyone,” says Hage. “That’s our mission—and until this disease is gone, we’re just going to keep plugging at it.”
Hage has witnessed the IVR’s “leave no one behind” mentality at work. Fourteen years ago, Hage traveled across the state to see IVR director and ophthalmologist Ed Stone (89R, 90F, 92F) in the UI Department of Ophthalmology and Visual Sciences. Hage was diagnosed with retinitis pigmentosa, a rare genetic disorder that involves a breakdown and loss of cells in the retina that steadily narrows his central vision. Despite the discouraging diagnosis, Hage still left Iowa City with a glimmer of hope. Stone told him that his team wouldn’t quit until they found a cure.
In December 2020, that potential cure came to light. Hage watched a webinar in which Stone described a promising vision-restoring treatment that was positioned to undergo clinical trials in the coming years. The challenge was making it affordable. That’s where Hage’s vision for starting a brewery came into focus.
Soon after Blind Butcher Brewing opened, Hage’s son was diagnosed with retinitis pigmentosa. The news came as a shock, though it wasn’t nearly as daunting for the family as his own diagnosis. “Things were surprisingly a lot easier,” says Hage. “We’re just so confident in what’s being done [at the IVR]. We know it’s going to work. It’s just a matter of time, awareness, fundraising, and this grassroots effort that we’re involved with here in Iowa.”
This past May, Brews for Blindness took flight with the canning of its pilot beer, Sight for the Blind. Two and a half years in the making, the hazy IPA was brewed by Coralville’s Backpocket Brewing. The can’s label features a QR code with information about the nonprofit’s mission and a link to donate online to a vision research fund. Hage has shared his mission with the brewers’ guilds in Iowa and South Dakota and aims to partner with more than 100 Iowa craft brewers later this year. Once the nonprofit is well-established in Iowa, Hage will begin seeking partnerships with breweries beyond the state.
“The culture of craft beer brings people together,” says Hage, who was inspired by Sierra Nevada Brewing Company’s worldwide campaign that raised millions to support those affected by the 2018 California wildfires. “The industry is just perfectly aligned to raising awareness in communities across Iowa and the country.”
Blind Butcher Brewing is located a few miles northwest of Inwood, Iowa, in the middle of nowhere. But most who walk in the doors don’t find it by accident. Every weekend, Hage meets people who have lost hope, need more of it, or want to know how they can help. The Hages’ family story demonstrates how a vision, a community, and a belief can transform lives—one person at a time.
“We’re shining a light on how we can bring this cure to people from around the world,” says Hage. “It doesn’t matter who you are, where you’re from, or how old you are. We signed on to the mission of leaving no one behind. That’s what we’re going to do.”





Publication highlights in 2023
140
TOTAL FACULTY PUBLICATIONS IN 2023
81 CITATIONS OF 2023 FACULTY PUBLICATIONS
2023 faculty publication that has been the most highly cited:
Groth, S. L., Linton, E. F., Brown, E. N., Makadia, F., & Donahue, S. P. (2023). Evaluation of Virtual Reality Perimetry and Standard Automated Perimetry in Normal Children. Translational vision science & technology, 12(1), 6. https://doi.org/10.1167/tvst.12.1.6
Most highly cited publication of all time from current faculty:
Cited 12,966 times
“Image processing with imageJ,” published in 2004 by Abramoff M.D., Magalhaes P.J., Ram S.J.,
Our top five most cited articles in 2023:
Cited 654 times, published in 2004
“Image processing with imageJ” by Abramoff M.D., Magalhaes P.J., Ram S.J.
10,401
2023 CITATIONS OF FACULTY PUBLICATIONS FROM ANY YEAR
Cited 222 times, published in 2004
Cited 167 times, published 2018
Cited 141 times, published 2016
Cited 111 times, published 2010
“Ridge-based vessel segmentation in color images of the retina” by Russell S., Bennett J., Wellman J.A., Chung D.C., Yu Z.-F., Tillman A., Wittes J., Pappas J., Elci O., McCague S., Cross D., Marshall K.A., Walshire J., Kehoe T.L., Reichert H., Davis M., Raffini L., George L.A., Hudson F.P., Dingfield L., Zhu X., Haller J.A., Sohn E.H., Mahajan V.B., Pfeifer W., Weckmann M., Johnson C., Gewaily D., Drack A., Stone E., Wachtel K., Simonelli F., Leroy B.P., Wright J.F., High K.A., Maguire A.M.
“Pivotal trial of an autonomous AI-based diagnostic system for detection of diabetic retinopathy in primary care offices” by Abramoff M.D., Lavin P.T., Birch M., Shah N., Folk J.C.
“Improved automated detection of diabetic retinopathy on a publicly available dataset through integration of deep learning” by Abramoff M.D., Lou Y., Erginay A., Clarida W., Amelon R., Folk J.C., Niemeijer M.
“Retinal imaging and image analysis” by Abramoff M.D., Garvin M.K., Sonka M.
To see a full list of our faculty’s publications visit ttps://medicine.uiowa.edu/eye/research/recent-publications or scan the QR code


Dr. Alson Braley, who was department chair at the time, established Iowa Lions Eye Bank (ILEB) in 1955 with support from the Iowa Lions Clubs. Since its establishment, ILEB has been affiliated with the University of Iowa Department of Ophthalmology and Visual Sciences, and as the only eye bank in the state, serves all 99 counties. Today, ILEB staff work at the BioVentures Center in Coralville, as well as a satellite office within the Iowa Donor Network headquarters in Altoona.
Eye bank staff members recover, medically evaluate, process, and distribute ocular tissue donated by generous individuals for use in corneal transplantation, research, and education. ILEB also honors donors and their loved ones for the gift of sight and provides outreach and education to the public.
Transplantable tissue is available to surgeons not only in Iowa but across the country and internationally. ILEB recovers ocular tissue from approximately 1,000 donors each year. In most cases, just the cornea is recovered for transplantation. ILEB will also recover whole eyes for research purposes.
Before recovery, all next of kin must complete a medicalsocial history of the donor. Although recovery of ocular
tissue must take place within hours of a death, ILEB can preserve a cornea for up to 14 days. However, most transplants occur within the same week after recovery. Some corneas also go into long-term storage for use in other procedures.
ILEB is an innovative leader in eye banking, constantly adjusting and adding processes to better serve surgeons’ tissue needs. Staff provide a variety of tissue preparations, including but not limited to DMEK, DSAEK, LSK/IEK/ IEALK and DALK processing. They work to ensure the needs of surgeons and their patients are met using thorough communication, adjusting processing and donor parameters accordingly while also honoring donors.
Cornea donation is regulated by the FDA. ILEB also follows the medical standards set by the Eye Bank Association of America and undergoes accreditation by EBAA every three years.
In 2025, ILEB will celebrate its 70th anniversary.
Stay updated on its plans to celebrate, as well as its latest work, by subscribing to the bimonthly newsletter and learn how you can help support ILEB’s commitment to restoring and preserving sight at IowaLionsEyeBank.org.
Although he was born in Ann Arbor, Michigan, Dr. James “Jim” Hersey was shaped by his upbringing in Independence, Iowa. And even though he moved to Colorado shortly after finishing his ophthalmology residency, Iowa still held a special place in his heart. Before his death in 2019, Dr. Hersey and his wife of 65 years, Phyllis, still felt such a strong connection to Iowa that they decided to include a gift to the University of Iowa Department of Ophthalmology in their estate planning.
Having grown up in Independence, Dr. Hersey stayed close to home for college and attended Cornell College in Mount Vernon, Iowa. After growing up with a father who was a doctor, and with the University of Iowa just down the road, Dr. Hersey came to Iowa for medical school (1954-1957) and for his ophthalmology residency (1961-1965). Phyllis remembers this time as an intense period of training for Dr. Hersey and growth for the couple. “All our friends were in the middle of medical training also. We didn’t do anything terribly exciting except go to the football games. There wasn’t really time for much else.”

Iowa football remained a touch point for the couple as, even after moving to Denver after residency, they remained devoted Iowa Hawkeye fans. The Hersey’s also adopted the Dever sports teams after moving—becoming avid Colorado Rockies and Denver Broncos fans.
When asked what made her and Dr. Hersey want to give back to the University of Iowa, Phyllis said, “the university is what made our life really. It really set us up for the future.” One the Hersey’s daughters recalled her father’s belief in the importance of education and reiterated, “it was the foundation for everything, and we’ve had such a wonderful life. Even though he lived most of his adult life outside of Iowa. I think he always considered Iowa his home. His parents had both gone to Iowa and they were so connected with the university. You know, it’s part of the family heritage to take care of what has supported you.”
The support the University of Iowa provided for Dr. Hersey and his family led to a long career where he practiced in Denver for 35 years. In 1985 Dr. Hersey was one of the founding partners of Denver Eye Surgeons, one of the first outpatient surgery centers of its kind in Denver. It was always the people that kept Dr. Hersey so engaged with his practice and his community. “He was interested in so many different things and could really talk to people about almost anything and as Mom said, he just loved people so he could put them at ease and reassure them and he just made them feel comfortable,” said Susan Carmody , another of the Hersey’s daughters. His love of people continued after he retired and led him to regularly volunteer at the homeless shelter in downtown Denver, as well as taking him on two medical mission trips to the Philippines.
Through all the twists and turns of life, the Hersey’s always felt a connection to Iowa. This connection is part of what makes the Ophthalmology Department at Iowa so special, and it’s what led to the Hersey’s philanthropic support. Their support will have lasting effects on all the future ophthalmologists that will come through the department, just like Jim from Independence did all those years ago.
“The restaurant business kind of gets in your blood; you can do this for a long time and continue to really enjoy it,” said Jeff Brands, who heads up Edotto Brands, a family of restaurateurs in central Iowa. This past year, he and his family found a way to serve their customers while also serving children impacted by eye diseases.
With nearly two decades of experience operating several Taco John’s locations in Iowa, their restaurant group recently expanded by adding two Slim Chickens restaurants to their portfolio— one located in Ankeny and the other in Grimes. Jeff’s daughters, Kristen Sandhurst, CFO, and Kelli Langfitt, VP of Marketing, work alongside their dad in running the newly established Slim Chickens franchises.
This past year, they launched a “round up” campaign at their Slim Chickens locations, where customers were asked to consider rounding up their bill to help raise funds and awareness for vision research taking place at the University of Iowa. Using their business to help raise funds for meaningful causes is nothing new for the family, as they’ve used this platform to support a variety of charitable organizations over the years. Their passion in advancing vision research came shortly after meeting Dr. Arlene Drack, a clinicianresearcher at the University of Iowa. Once learning of her efforts to advance research for X-linked retinoschisis, a rare progressive eye disease often found in childhood, they knew they had to do more.
“A few years back, we changed our mission and core values so that our mission statement now reads, ‘To serve others as we would like to be served,’ and so we really felt like this was an opportunity to live out our mission statement,” Jeff said. This past November, they saw this mission in action when countless Slim Chickens customers stepped up to join them in giving back to support an area of research that is often in need of resources, due to the rarity of these conditions.

TOTAL GIVING FOR FY2023
$14,432,573
NUMBER OF GIFTS: 1,204
AVERAGE GIFT SIZE: $11,987
GIFTS FROM: 41 STATES
To learn more about how philanthropic support helps advance the work of the University of Iowa Department of Ophthalmology and Visual Sciences and UI Institute for Vision Research, please contact:
Matt Kuster Executive Director of Development matt.kuster@foriowa.org 319-467-3720
Katie Sturgell Senior Director of Development katie.sturgell@foriowa.org 319-467-3756
Frank Descourouez Associate Director of Development frank@foriowa.org 319-467-3672
Jedd Spidell Assistant Director of Development jedd.spidell@foriowa.org 319-467-3342
The University of Iowa Center for Advancement, P.O. Box 4550, Iowa City, IA 52244-4550 319-335-3305 or 800-648-6973
The UI acknowledges the University of Iowa Center for Advancement as the preferred channel for private contributions that benefit all areas of the university. For more information or to donate in support of the eye program, visit the secure website at Givetoiowa.org/eye
In 2023, Iowa Lions Eye Bank recovered corneas from 1,015 donors in Iowa, 63 percent of whom were registered. The average donor age was 64 and 60 percent of donors were male. The eldest donor was 98 years old and the youngest donor was 10 years old. There were 732 people who received transplanted corneas from Iowa Lions Eye Bank. Corneas from Iowa Lions Eye Bank went to recipients in 21 states, Puerto Rico and 7 other countries.
IOWA VISION is published for alumni, colleagues, and friends of the University of Iowa Department of Ophthalmology and Visual Sciences.
Editor-in-Chief
Keith D. Carter, MD, FACS
Editors
Matt Browning, MFA
Caroline Allen, MLIS Kelsey Hunold, BFA
Design
Benson & Hepker Design
Photography
Kelsey Hunold, Kevin Caldwell Photography and other University of Iowa Health Care sources
Contributors
Jen A. Miller and Molly Rossiter (University of Iowa Health Care Marketing and Communications), Josh O’Leary (UI Center for Advancement)
Please direct comments and inquiries to Matt Browning 319-384-8529 matt-browning@ uiowa.edu
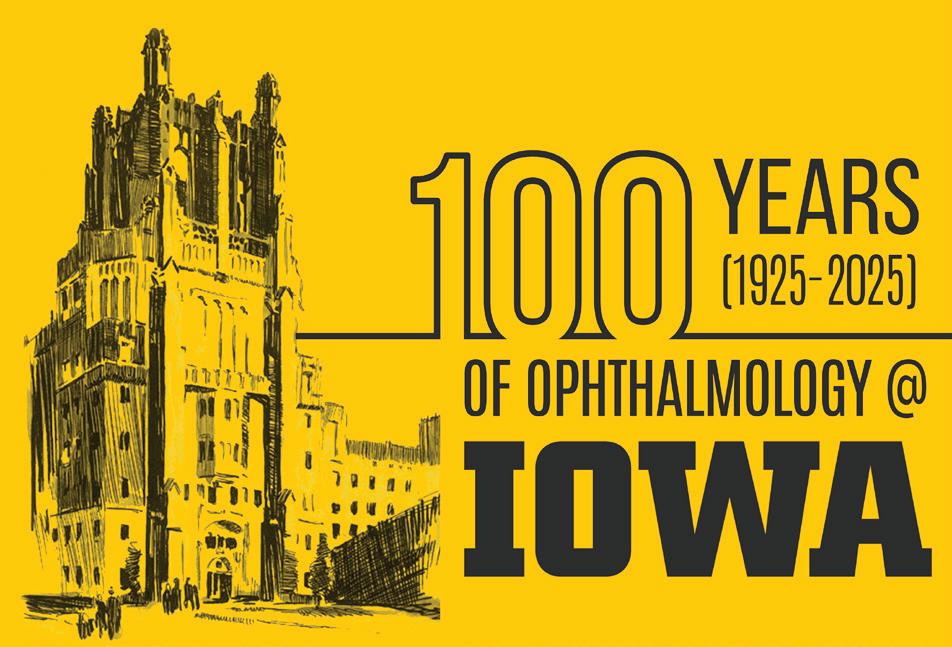
2025 marks the centennial of the University of Iowa hiring Dr. C.S. O’Brien to start the ophthalmology department, the first west of the Mississippi. Through 2025 we will be sharing the history, accomplishments and stories of the department from its inception to today. We will also be hosting a centennial celebration in June of 2025 in conjunction with our annual Iowa Eye meeting and alumni reunion. Be on the lookout for more on our centennial.
Brian Privett turned his childhood curiosity about ophthalmology into a career-long commitment to community leadership and service to Iowans.
STORY CELINE ROBINS; PHOTOGRAPHY TIM SCHOON
For Brian Privett, MD, serving a close-knit community as an ophthalmologist has been a lifelong ambition—but doing so in Cedar Rapids, Iowa, came as a bit of a surprise.
Privett, who completed his residency program at the University of Iowa in 2011, grew up in Kennett, a small town in the Missouri Bootheel. Kennett did not have many specialty physicians, but one of the few was an ophthalmologist who was a neighbor of Privett’s. At an early age, he took notice of the doctor’s effect on the small community and began to see himself in the ophthalmologist’s shoes someday.
“I wanted to work with my hands. I wanted to do something that really seemed to have an impact,” Privett remembers. “People value their vision, and I noticed that people really seemed to appreciate his work.”
The idea stuck. Privett attended medical school at the University of Missouri and became the first in his family to earn a medical degree. When it came time to choose a residency training program, he asked his fellow eye docs for advice.
“A lot of other ophthalmologists I considered mentors during medical school suggested that I look at the University of Iowa,” Privett says. “Later I learned that Iowa is one of the top-ranked ophthalmology residency programs in the country.”
After his interview at the University of Iowa Carver College of Medicine, he was confident his mentors had steered him in the right direction.
“It had great faculty and a tradition of innovation in our field across the entire world,” Privett says.
‘Everyone had those Midwestern values’ Privett remembers his residency training at Iowa as a time when he was exposed to fascinating cases, the like of which he has rarely seen since.
“There are so many things that you see coming through Iowa, as the tertiary care center in the state, that you’re never going to see in the rest of your career,” he says. “Those three years in residency were the most academically interesting years of probably my entire life.”
He found Iowa to be a nurturing training environment.
“Everyone had those Midwestern values,” Privett remembers. “The faculty had high expectations, and they pushed me, but they did it in a respectful and missiondriven way. They made everyone feel like they were a part of the team, so that you wanted to step up and continue that high-quality tradition that Iowa had come to be known for. It was a very kind place to learn.”
During residency training, he met his wife, Julia, a 2007 graduate of Iowa’s physician assistant program.
“She would tell you that her program is even higher ranked than the ophthalmology program is,” he jokes.
The couple began to think about where to settle down. Brian wanted to find a place with the small-town charm of Kennett; Julia wanted to live someplace with the bustling energy of her home near Detroit.
“We never really planned on staying in Iowa. We looked all over the country,” he says. “I knew I wanted to join a group that was going to be fair and not take advantage of me, and we needed to find a place that still had that small-

town feel but also the amenities and entertainment that you might find in a city.”
Privett consulted his friends and mentors who were faculty at the University of Iowa to ensure he was making the right decision.
“That’s another advantage of practicing near where you train,” he says. “I was able to get recommendations from my faculty mentors. You can get the inside scoop before you actually sign a contract and join a practice.”
Ultimately, they decided to put down their roots in Cedar Rapids. The Privetts now have two children, ages 9 and 6.
“Privitt” continues on page 28
“It’s like I had always hoped for. When I’m out and about in town, I’ll see patients at community events, and they’ll come up and say ‘hi.’ It’s just kind of nice to feel that sense of being a part of the community.”
BRIAN
PRIVETT, CARVER COLLEGE OF MEDICINE ALUMNUS WHO PRACTICES OPHTHALMOLOGY IN CEDAR RAPIDS, IOWA
“Privett” continues from page 27
“Cedar Rapids seemed like a great place to raise children, and that’s turned out to be true,” Privett says.
In addition to his roles as a father of two and an ophthalmologist, he also leads two local Cub Scout dens and serves as Cubmaster of the local pack.
Physician as advocate
Privett has practiced at the Iowa Eye Center in Cedar Rapids for 11 years. He appreciates that the job allows him both to develop rapport with patients that he cares for year after year, and to perform procedures like LASIK and cataract surgery.
“It’s like I had always hoped for,” Privett says. “When I’m out and about in town, I’ll see patients at community events, and they’ll come up and say ‘hi.’ It’s just kind of nice to feel that sense of being a part of the community.”
The ability to use advanced technology, or what Privett calls “toys and gadgets,” is another draw of the field.
“Obviously the eyes are very small, so a lot of our work involves microscopes, lasers, and technology for measuring the eye and doing diagnostics in the office,” he says. “I would say that the majority of ophthalmologists do have some interest in technology.
“There’s also an interesting number of ophthalmologists that are interested in photography; we have a very visual field. We look at images a lot in our learning, and a lot of the knowledge of how optics work goes well into learning the hobby of photography.”
As for Privett, his interests lie elsewhere: his career has been defined by advocacy. In his first year of practice, he joined the Iowa Medical Society (IMS).
“We advocate for physicians, but we also advocate for patients and for health care in general,” he says. “Not everyone who’s making decisions about health care knows a lot about health care. Legislators need to hear from physicians, and we can serve our patients better if we’re advocating on their behalf.”
He served on the board of the IMS for nine years and served a one-year term as president of the statewide organization, starting in April 2020.
“The beginning of the pandemic was a challenging time to be the leader of that group,” Privett says. “We were very involved with communicating between various public health entities, hospitals, and physicians. But I think it was an important time to make sure that physicians’ voices were being heard at all levels.
“We pivoted to doing a lot more public health initiatives than what IMS had done in the past. We had to be nimble, and we had to change the way we communicated, and who we communicated with. We were able to help physicians, whether they were a part of a big system or an independent physician in rural Iowa, communicate back to the Statehouse, and in some instances at the federal level.”
The experience has taught him the importance of advocacy in medicine—in short, that “advocacy does work.” He is motivated to impress that message upon other Iowa physicians.
“When you start working in advocacy, you meet other physicians that are like-minded and have the passions that you have,” Privett says. “Once you get involved with it, you wish every physician would be involved in advocacy because you’ve become more optimistic that when we come together in an organized way, we can create change.”
He has continued to share his optimistic message after his presidential term ended through hosting the monthly IMS podcast, Doc 2 Doc. In the podcast, he interviews physicians from across Iowa about topics related to advocacy and to health care more broadly. Recent episodes have included a highlight on the opioid epidemic in Iowa with an addiction medicine psychiatrist and a special feature on physician workforce issues.
“I find it really intellectually interesting, but I also get to communicate with different physicians across the state of Iowa, which I enjoy,” he says. “It’s something I plan to continue doing as long as people keep listening.”
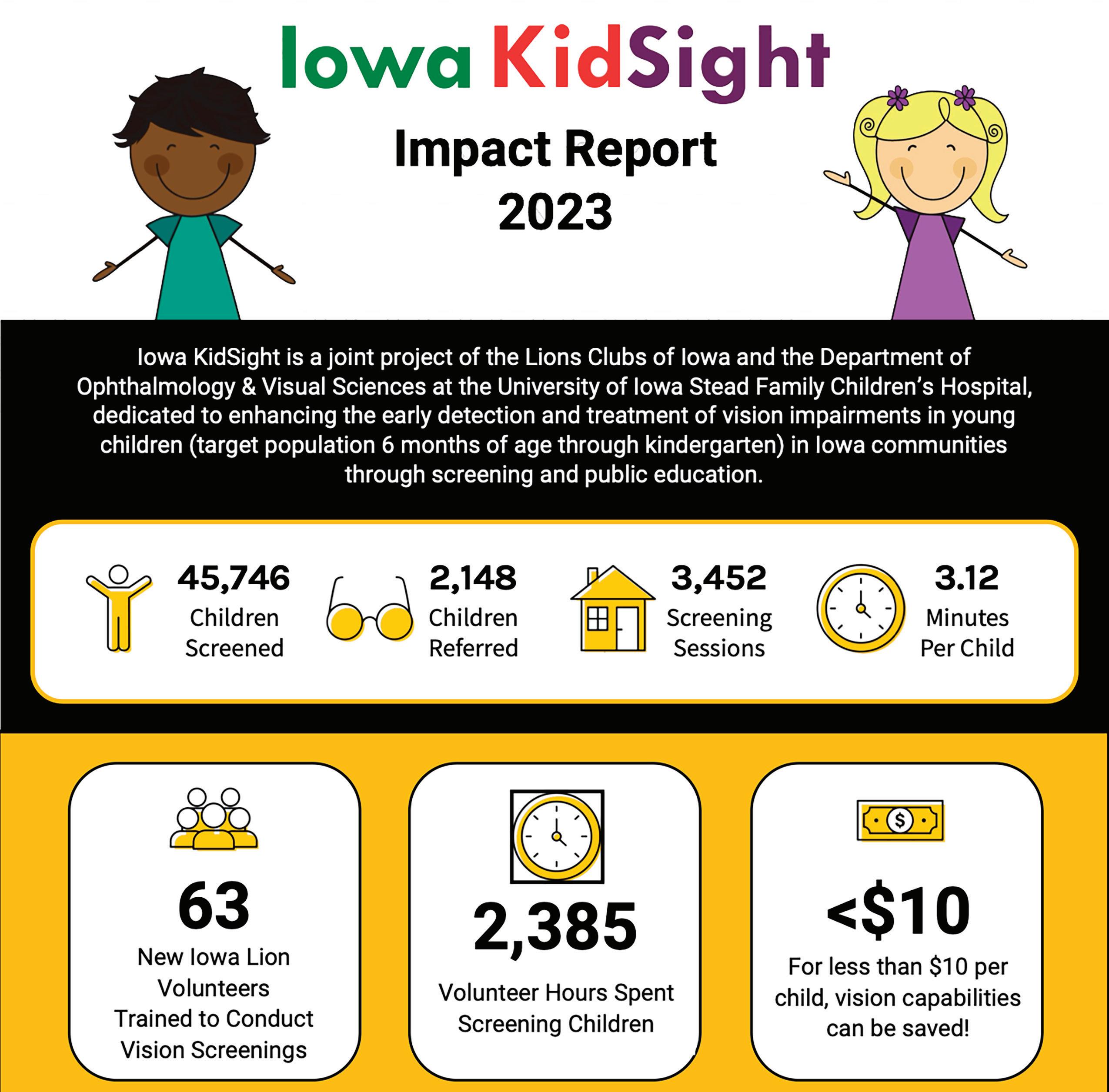
Meet Monroe. She was screened by Iowa KidSight this past year. Through this screening, Monroe and her parents found out that she needed glasses. Below is a conversation with Monroe and her parents after she had gotten her new glasses.
Q&A with Monroe:
Q. Tell us about your glasses:

Q. What changes did you notice in your child since receiving her glasses?
A. “I really like my glasses because they are rainbow and glow in the dark. My doctor put eye drops in my eyes and looked at my eyes. They covered up one eye and put little dots to see if I could see them. My doctor helped me a lot and it was a pretty good day…”
Q. What is your favorite thing to look at?
A. “I like to look at myself in the mirror and animals that are far away and even airplanes. I couldn’t see things far away before glasses.”
Q&A with Monroe’s parents:
Q. Did you know your child wasn’t seeing well?
A. “We did not and had no indication that she was having trouble seeing things far away.”
A. “She would describe objects, people, animals in greater detail than she did before. She could see intricacies of the world around her that she couldn’t see or describe before. It was wonderful!”
Q. Thinking back to before your child received his/her glasses, were there things she did or didn’t do?
A. “She couldn’t describe things in detail—which at the time, we thought was due to her developing language and now we realize it was her vision.”
Q. Are there any other comments you’d like to share regarding your child?
“The eye screening helped both my daughter and my son. Because of this screening, we took her to an eye doctor who diagnosed and treated her vision impairment. The doctor then recommended we get our son screened. He also has the same vision impairment and now has corrective lenses at a very young age. We are so grateful for this screening and the opportunity to set our children up for developmental success without vision being an obstacle. Thank you so much!”
Patient’s Choice Awards | Top 10% Providers
• Elaine Binkley
• H. Culver Boldt
• Sara Downes
• Ian Han
• Pavlina Kemp
• Andrew Pouw
• Erin Shriver
• Edwin Stone
Dr. Michael Abramoff was recognized on the Carver College of Medicine Wall of Scholarship for his paper, “Retinal Imaging and Image Analysis”.

Dr. Lee Alward recently gave the inaugural Donald Minckler Doheny Glaucoma Lecture at the UCLA 5th Annual Glaucoma Symposium.
Dr. Elaine Binkley and Dr. Budd Tucker were awarded a $1.3M grant from the Gilbert Family Foundation as principal investigators for research related to neurofibromatosis type 1 (NF1).

Dr. Timothy Boyce was inducted as a new member of the American Uveitis Society.

Dr. Keith Carter was awarded the American Society of Ophthalmic Plastic and Reconstructive Surgery Outstanding Contribution Award for his contributions to the Mentoring in Ophthalmology Program.

Dr. Alina Dumitrescu received the Chakraborty Family Professorship in Pediatric Genetic Retinal Diseases. She was also presented with the Board of Directors’ Honor Award for her distinguished service to the American Association for Pediatric Ophthalmology and Strabismus.

Dr. Jaclyn Haugsdal was awarded the inaugural Lee Alward Teaching Award. She was also named as the department’s Ophthalmic Simulation Director.
Dr. Marcus Noyes was promoted to the chair elect for the Fellowship of Scleral Lens Society.
Dr. Chau Pham was selected to participate in the American College of Surgeons’ Certificate in Applied Surgical Education Leadership (CASEL) program, as well as the University of Iowa Teaching Scholars program.
Dr. Stephen Russell was honored on the UI Carver College of Medicine Wall of Scholarship for his paper, Efficacy and safety of voretigene neparvovec (AAV2hRPE65v2) in patients with RPE65mediated inherited retinal dystrophy: a randomised, controlled, open-label, phase 3 trial, being cited over 1,000 times by at least two of three academic citation indices (Google Scholar, Scopus, and Web of Science)
Dr. Christopher Sales was elected to join the University of Iowa Chapter of the National Academy of Inventors. Dr. Sales, along with Noah Healy (Design Engineer), were also the winners of the Tippie School of Business and Iowa John Pappajohn Entreprenurial Center Innovation Challenge Award, which came with a $20,000 prize. He was also Selected for the Stanford BioDesign Global Faculty in training program and will serve as the co-chair of the Cornea Society Fellows Summit.
Dr. Erin Shriver was given the Secretariat Award by AAO for service on state affairs. She was also named “Outstanding Champion for Veterans’ Eye Care”, by AAO for her “Protect Veterans’ Eyesight: Defending Quality Surgical Care” fundraising achievements. In addition, Dr. Shriver is also serving a 3-year term as a Trustee-at-Large to the American Academy of Ophthalmology Board of Trustees.

Chelle Lehman, MS was named Iowa KidSight’s new program director, replacing Lori Short who stepped down this year.
Mike Bray, COA, assistant clinic manager, received an Exceptional Performance Award from the department for his invaluable contributions and dedication to outstanding patient care at UIHC.
Dr. Noor-Us-Sabah Ahmad was selected for the ARVO Science Communication Fellowship. This is a competitive, one-year program for ARVO members-in-training to develop science communication and advocacy skills for engagement with the public, media, and legislators.

Dr. Aaron Dotson (PGY-4) was selected as one of the National Minority Quality Forum’s 40 Under 40 Leaders in Minority Health! This award recognizes accomplishments in the healthcare field and potential to continue positively
impacting minority communities. He was also named the 2024 recipient of the Robert A. Copeland Jr. Advocacy Education Award.
Dr. Arnulfo Garza (PGY-3) was recently selected as one of ten aspiring retina specialists to attend the Annual Duke Fellows Vitrectomy Course.

Dr. Mahsaw Mansoor (PGY-4) was one of only 10 residents in the nation to receive the 2024 American Society of Cataract and Refractive Surgery (ASCRS) Residence Excellence Award.
Dr. Rupin Parikh (Oculoplastics Fellow) was selected as the 2024 ASOPRS Advocacy Ambassador for AAO Mid-Year Forum.
1. Meghan Menzel, CRA’s photo, “Nevus on the Nerve” was featured on the cover of the September 2023 Ophthalmology Science journal. It was the second-place winner in the Color Fundus normal stereo division at the Ophthalmic Photographers’ Society 2021 Scientific Exhibition (www.opsweb.org). Equipment: Topcon 50DX.
2. Meghan Menzel, CRA, and Dr. Elliott Sohn had an image featured on the cover of the September 2023 Ophthalmology journal with their photo, “Best Disease”. It was the Honorable Mention winner in the Color Fundus Photography Normal 30-40[1] Field category at the Ophthalmic Photographers’ Society 2022 Scientific Exhibition.
3. Sarah Skiles, CRA, and Dr. Ian Han had an image featured on the cover of the September 2023 Ophthalmology Retina Journal with their photo, “Pseudohypopyon in Best Vitelliform Macular Dystrophy.” It was the first-place winner in the Color Fundus Photography Wide Angle field division at the Ophthalmic Photographers’ Society 2022 Scientific Exhibition.
4. Jody Troyer, CRA, and Dr. Elliott Sohn were featured on the cover of the August 2023 Ophthalmology Retina Journal with their photo, “Macular Neovascularization in Boy.” It was the Second Place Winner in the wide-angle category at the Ophthalmic Photographers’ Society 2022 Scientific Exhibition.
Department of Ophthalmology and Visual Sciences
University of Iowa Health Care 200 Hawkins Drive, 11136 PFP Iowa City, IA 52242-1091
319-356-2864
319-356-0363 (fax) iowaeyecare@uiowa.edu
Appointment scheduling: 319-356-2852 – Adult 319-356-2859 – Pediatric
UI Health Access for the general public: 800-777-8442
UI Consult for referring providers: 800-322-8442
Department news, events, and information: medicine.uiowa.edu/eye
/UIowaEye
/UIowaEye

@UIowaEye

Ruth Fisher was named as the first Executive Director of the Iowa Lions Eye Bank in 1955. Previously, Ms. Fisher had been diagnosed with Keratoconus and required a donor cornea transplant. Her cornea replacement surgery was performed by Dr. Alson E. Braley in 1954, about a year before she became Executive Director of the Iowa Lions Eye Bank.
200 Hawkins Drive, 11136 PFP Iowa City, IA 52242
IOWA EYE MEETING INFORMATION
• What: The Iowa Eye Annual Meeting is a chance to hear from some of the top eye doctors in the country speaking on relevant topics, earn CME credit, and reconnect with old friends and colleagues.
• Where: University of Iowa Hospital, Iowa City
• When: June 2025