






In late 2020, Ginny Clements, a breast cancer survivor and advocate, donated $8.5 million to establish the Ginny L. Clements Breast Cancer Research Institute at the University of Arizona Cancer Center. Breast cancer is one of the Cancer Center’s top five priority cancers, as identified through data gathered by the Center’s Office of Community Outreach and Engagement about the catchment area population. The mission of the Ginny L. Clements Breast Cancer Research Institute is to provide the best cancer care for breast cancer patients in the state of Arizona and beyond through cutting edge research.
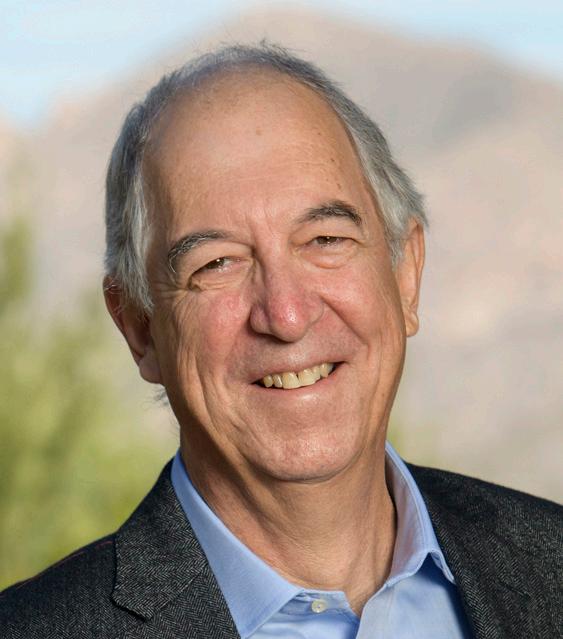
“The Ginny L. Clements Breast Cancer Center is internationally renowned for its comprehensive cancer research and clinical care, and our talented team of investigators and researchers continue to make an impact for communities throughout our state. I am incredibly proud of how the Center serves as an innovation powerhouse to create positive impact for patients, their families and communities around the world.”
Robert C. Robbins, MD President, University of Arizona

“We’re excited about expanding translational research through the Ginny L. Clements Breast Cancer Research Institute. The work we do will advance our understanding of breast cancers and help people throughout the nation.”
Joann Sweasy, PhD Director, University of Arizona Cancer Center
“Working together, WE can make a difference. As I have often said “it takes a village”- the clinicians, the researchers, and donors. This research and new knowledge are helping those who are fighting the fight and hopefully creating a world that is free of breast cancer.”
Ginny L. Clements Breast Cancer Survivor and Philanthropist
THE
ARIZONA CANCER CENTER
ONLY NATIONAL CANCER INSTITUTE DESIGNATED COMPREHENSIVE CANCER CENTER HEADQUARTERED IN THE STATE OF ARIZONA.
In addition to being part of the University of Arizona Cancer Center, which is the only NCI designated Comprehensive Cancer Center in the state of Arizona, the Cancer Center’s breast program is NAPBC accredited (National Accreditation Program for Breast Centers), which involves meeting a rigorous set of standards to assure the highest quality care for our patients.


Some of the most exciting work being done at the Ginny L. Clements Breast Cancer Research Institute is now having a positive impact in the lives of cancer patients and their caregivers. The research of Terry Badger, PhD provides one example of this. Dr. Badger’s work makes use of supportive care interventions by telephone to help patients better cope with their symptoms and maintain a positive outlook, which is known to be a key piece in survivorship and maintaining quality of life while being treated for breast cancer.
“We’ve developed very effective supportive care interventions that have worked for thousands of cancer patients and their caregivers to manage their symptoms and reduce psychological distress.” Badger’s team has developed a program for providing supportive care to patients by phone, and this innovation predates the telehealth trends that came with the COVID-19 pandemic. Badger said that these interventions cater specifically to the needs of the Cancer Center’s catchment area.
“Everything we do can be done in both English and Spanish,” Badger said. “We can provide this service to people in rural areas. The majority of participants report very positive experiences associated with this kind of supportive care.”
Our Breast Cancer Clinical Research Team uses a multidisciplinary approach to breast cancer diagnosis and treatment. In addition to a team of doctors and specialists, we have a breast cancer nurse navigator who works closely with each patient to provide education, support and guidance from diagnosis, through treatment, and ultimately survivorship.
Our clinic also offers genetic counseling and testing through our certified genetic counselors, and we have a robust clinical trials program for access to the newest breast cancer treatments. At the University of Arizona Cancer Center, we strive to provide complete care through our integrated breast cancer team. Breast cancer is diverse. Some patients can safely be treated with surgery alone. Other patients may benefit from up-front chemotherapy, surgery and then radiation. Deciding which approach is best in your situation requires a team of specialists who have access to all of the available treatment options.
Each member of the University of Arizona Cancer Center breast cancer treatment team is exclusively dedicated to treating patients with breast cancer. In the rapidly changing world of breast cancer research, this specialization allows our doctors to provide individualized care to every patient, every day. As an NCI designated comprehensive cancer center, our team has access to, and is actively conducting, the newest research. Clinical Research Team Members are also part of the Innovative Working Group.
The Breast Cancer Innovative Working Group translates discovery about fundamental breast cancer mechanisms to the clinical setting. Its three goals are (1) to investigate the cellular and molecular mechanisms of breast cancer metastasis, (2) to promote collaboration among scientists and clinicians with diverse expertise to enhance discovery, diagnosis and treatment, and (3) to promote the translation of discoveries to clinical application in the form of new targeted therapies, biomarkers, and diagnostics.
Dr. Ehsani serves as the Breast Clinical Research Team leader at the Cancer Center. Her clinical expertise is breast oncology, treatment of breast cancer, and management of related complications. She is a member of City of Hope Clinical Cancer Genomics Community of Practice, and she sees women in the High-Risk Clinic for counseling and management of their increased risk for breast cancer. She also has an interest in breast cancer survivorship, cancer prevention, and genetic risk assessment of cancer.
 Sima Ehsani, MD*
Sima Ehsani, MD*

Dr. Erdrich is a surgical oncologist and assistant professor with the Division of Surgical Oncology at the University of Arizona Department of Surgery who specializes in melanoma, sarcoma, and breast cancers. Dr. Erdrich also researches Native American cancer disparities and works with tribal partners to improve cancer education, prevention, and treatment.
 Jennifer Erdrich, MD, MPH, FACS*
*Clinical Research Team Members are also part of the Innovative Working Group listed after this section.
Jennifer Erdrich, MD, MPH, FACS*
*Clinical Research Team Members are also part of the Innovative Working Group listed after this section.
Dr. Foster’s clinical focus is exclusively on the management of breast cancer and breast disease. She has a special interest in the multidisciplinary management of breast cancer. She is an expert in all aspects of breast cancer surgery, benign breast disease, and in management of patients at high risk for breast cancer.


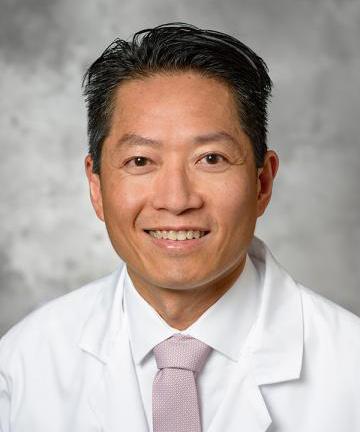
Dr. Jiralerspong is recognized for his research on metabolism in breast cancer, with presentations at national oncology meetings in obesity in breast cancer, and the role of the highly promising diabetes drug metformin in the treatment of breast cancer.
Dr. Rozell assists patients in treatment decisions regarding chemotherapy, hormonal therapy, targeted therapy, second opinion consultation and survivorship.


Dr. Segar’s primary clinical and research focus is on breast cancer and precision medicine. She leads the early phase clinical trial program at the Cancer Center involved in developing new therapuetics. Her key interests include studying the breast cancer tumor microenvironment, understanding the role of the immune system, and improving management of toxicities related to therapies administered to treat breast cancer, including peripheral neuropathy.
Dr. Weihs researches psychosocial interventions and maintains an active clinical practice of psychiatric care for cancer patients embedded with her multidisciplinary team. She collaborates with intervention scientists to test innovative psychosocial interventions for breast cancer patients. She has conducted three prospective longitudinal studies to determine the impact of emotional and interpersonal processes on medical, psychiatric, functional, and quality of life outcomes.
Umbreen Arshad Rozell, MD* Nova M. Foster, MD, FACS* Sao Jiralerspong, MD* Jennifer Segar, MD* Karen L. Weihs, MD*
Dr. Badger’s team investigates symptom management to decrease psychological distress and symptom severity for English and Spanish-speaking survivors and their families. Dr. Badger has tested telephone-delivered interventions to improve access to care. Her current symptom management and supportive care research includes survivors/families who are currently in or completing cancer treatment.
Dr. Chow’s team conducts translational research to understand metformin’s effects on human breast tissue and the potential of using it for breast cancer prevention. She also collaborates with imaging scientists to assess the use of breast CT to determine breast density, a surrogate biomarker of breast cancer risk, in Hispanic women with high adiposity. The goal is to develop safe, effective treatments for breast cancer prevention.
Bone metastases affecting most women with stage IV breast cancer are a major focus of study in Dr. Janet Funk’s research group. Current work clarifies the importance of bone specific metabolism of dietary compounds for bioactivity, and the development of unique and more clinical relevant (ER+) models of breast cancer bone metastases.


Dr. Gurtner is an internationally known plastic surgeon, scientist, inventor and entrepreneur. His focus is on improving the quality of life for patients with breast cancer. Dr. Gurtner has published 350+ papers, received over $27 million in federal grants, and been awarded 60 patents. His work has led to the formation of venture backed companies producing innovative products, many of which have been acquired by industry.

Dr. Kim’s research focuses on oncogenes and tumor suppressors that play a role in the emergence and therapyresistant recurrence of breast cancer. One of her main projects is to characterize the ING4 tumor suppressor related to its functions in chromatin remodeling, transcriptional regulation, and tumor immune microenvironment modulation metastasis.

 Terry Badger, PhD, RN, FAPOS, FAAN
Hsiao-Hui (Sherry) Chow, PhD
Geoffrey Gurtner, MD, FACS
Janet Funk, MD
Suwon Kim, PhD
Terry Badger, PhD, RN, FAPOS, FAAN
Hsiao-Hui (Sherry) Chow, PhD
Geoffrey Gurtner, MD, FACS
Janet Funk, MD
Suwon Kim, PhD
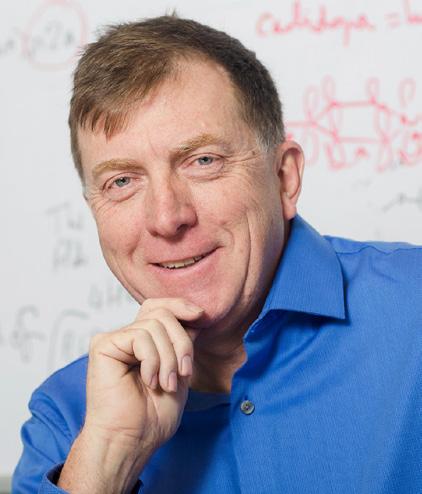
Dr. Montfort’s research concerns the link between protein structure and function, including how drugs bind to their targets and influence activity. One focus is on nitric oxide signaling, and nitric oxide driven breast cancer. His group is studying how excess nitric oxide production in breast cancer drives an aggressive tumor phenotype and has identified novel targets for therapeutic intervention.
In collaboration with breast oncologists, pathologists, biophysicists, and biomedical engineers, Dr. Mouneimne’s team is tackling the problem of breast cancer metastasis from diverse angles, rationales, and training backgrounds, broadening their approach to include basic, translational, and patient-oriented research strategies.



Dr. Paek investigates how cancer cells decide between transient and terminal cell fates following cell stress from chemotherapy treatment. His lab develops fluorescent reporters to track the dynamics of key transcription factors involved in cell-fate decisions. Their goal is to alter the activation of these proteins in order to increase cancer cell death and enhance treatment efficacy.
Dr. Thatcher’s research has resulted in two novel drugs that have completed Phase 1/2 clinical trials in estrogen receptor positive breast cancer and further exploitation of epigenetic mechanisms to confront endocrine-resistance in combination with checkpoint inhibitors. New research in triple negative breast cancer is exploring targets associated with cancer cell metabolism, inflammation, and the tumor microenvironment.
Dr. Schroeder’s lab studies drivers of metastatic breast cancer and differences between the function of receptor tyrosine kinases (RTKs) in normal verses transformed epithelium. Many RTKs are involved in cancer progression, especially the ERBB or HER family, including the Epidermal Growth Factor Receptors (EGFR), HER2, ERBB3 and ERBB4. The team wants to understand the non-canonical role of these receptors in cancer progression and develop novel therapeutics.
The University of Arizona Cancer Center’s Ginny L. Clements Breast Cancer Institute is home to the only accredited breast cancer program in Arizona.

Game-changing basic scientific research at the Ginny L. Clements Breast Cancer Research Institute is presenting researchers with opportunities to collaborate and translate discovery into innovation. Cancer Center member, Ghassan Mouneimne, PhD, has discovered that breast cancer cells become more aggressive when they encounter tissue stiffening. This discovery and collaboration with fellow Cancer Center member, Casey E. Romanoski, PhD, has led to the development of a “MeCo Score” which measures tissue stiffness and may one day be used as a predictor for best, individualized intervention strategies for breast cancer patients. “Unfortunately, bone metastasis is normally not identified until an advanced state when it’s not reversible,” Dr. Mouneimne, said. “What’s really exciting is one day being able to take a sample from the patient’s primary tumor and predict who is at high risk for bone metastasis. Then we could intervene with a prevention strategy that we are now validating in the lab.”

Dr. Vanderah’s laboratory investigates metastatic breast cancer utilizing a syngeneic murine model to reduce cancer-induced bone pain while also trying to reduce bone wasting. We have found that a novel type of non-psychotropic cannabinoid as well as increasing endogenous cannabinoids (endocannabinoids) can significantly reduce cancer-induced pain and improve bone integrity.

Dr. Vedantham’s research interests are in the design, development and clinical translation of novel x-ray imaging systems and imaging techniques with particular focus on oncological and interventional imaging. He has made major contributions to breast cancer imaging research and is currently developing advanced tomographic techniques and systems for breast imaging and its clinical translation.

Dr. Lora Wang is an Associate Professor of Radiation Oncology specializing in breast cancer and lymphoma cancers. Her primary research interests are in breast cancer and individualizing care for patients. She also researches health disparities in minority populations as they pertain to cancer diagnosis, prevention, and treatment.
Dr. Yao’s research is primarily focused on investigating the gene network “switches” that control cancer cell dormancy and growth. By combining single-cell and omics measurements with mathematical and machine learning models, he seeks to unravel the intricate and heterogeneous biological systems underlying breast cancer dormancy, drug resistance, relapse, and metastasis.
Dr. Zohar’s lab works on development of microfluidicbased in vitro human models of several aspects of metastatic breast cancer. Two major projects are development of organ-on-a-chip platforms to: (1) investigate organ-specific extravasation of circulating tumor cells from blood vessels to the bone microenvironment, and (2) study stromal interactions and dormancy of metastatic cancer cells in the lung microenvironment.
 Yitshak Zohar, PhD
Todd W. Vanderah, PhD
Lora Wang, MD
Srinivasan Vedantham, PhD
Guang Yao, PhD
Yitshak Zohar, PhD
Todd W. Vanderah, PhD
Lora Wang, MD
Srinivasan Vedantham, PhD
Guang Yao, PhD

Dr. LoRusso brings more than 25 years of expertise in medical oncology, drug development, and early phase clinical trials. Prior to her Yale appointment, she served in numerous leadership roles at Wayne State University’s Barbara Karmanos Cancer Institute, most recently as director of the Phase I Clinical Trials Program and of the Eisenberg Center for Experimental Therapeutics.


Anne Marie Mercurio is a patient research advocate primarily in oncology, who helps empower patients to be partners with their doctors and encourage disruptive innovation in areas of cancer research. She aspires to see that “meaningful change” is the end result of all efforts and not simply a buzzword or a catch-phrase.
Dr. Arteaga is an internationally recognized expert in breast cancer with more than 350 publications in the areas of oncogenes and breast tumor initiation and progression, targeted therapies and biomarkers of drug action and resistance, and investigator-initiated clinical trials in breast cancer.


Dr. van ‘t Veer is a world-renowned Molecular Biologist, and Leader of the Breast Oncology Program and Associate Director Applied Genomics at the UCFS Helen Diller Family Comprehensive Cancer Center. She’s also the former Head of Diagnostic Oncology of the Netherlands Cancer Institute, and inventor of MammaPrint. Her research focuses on personalized medicine.
Barbara A. Pockaj, MD, is a surgical oncologist with a strong clinical and research interest in breast cancer and malignant melanoma. Dr. Pockaj’s research focuses not only on clinical studies but also translational science.
 Patricia LoRusso, DO
Anne Marie Mercurio
Carlos Arteaga, MD
Laura J. van ‘t Veer, PhD
Barbara A. Pockaj, MD
Patricia LoRusso, DO
Anne Marie Mercurio
Carlos Arteaga, MD
Laura J. van ‘t Veer, PhD
Barbara A. Pockaj, MD




Your donations to our cancer center and the Ginny L. Clements Breast Cancer Research Institute support advances in innovative clinical and supportive care, education, early detection, and can help us recruit and retain the best researchers and clinicians in the fields of cancer research and care.
The University of Arizona Cancer Center is a National Cancer Institute Designated Comprehensive Cancer Center and accredited by the National Accreditation Program for Breast Cancers.


