

Taking care of care
How AI is powering eCase for better care outcomes.
On hearing the term Artificial Intelligence, one would be excused for immediately thinking of ChatGPT –the natural language processing tool that has generated a lot of publicity recently.
However, AI, in general terms, is much broader than this – providing the ability for machines and computer programs to learn from experience, adjust to new inputs and perform human-like tasks. These range from predictive analytics to voice and facial recognition and robotics.
Using AI technologies, computer and software programs can be trained to accomplish specific tasks by processing large amounts of data and recognising patterns in the data. According to Nina Combe – chief product officer at Health Metrics – rather than being something off in the far distant future, these technologies exist now and offer opportunities for aged care providers to unlock greater efficiencies for managers and staff.
“The AI technology that currently exists for potential use by aged care providers can be split into two key categories,” Combe tells Australian Ageing Agenda, “those that can address the current business challenges and support the sustainability of aged care organisations and
those that can provide an improved experience for residents or staff.”
Supporting business sustainability
The first category includes technology such as predictive analytics, which allows aged care providers to realise the business value of their data. Data is one of an aged care provider’s most valuable and important assets. However, accessing all of the data available can be labourintensive and time-consuming.
Predictive analytics can help solve data complexity through automated and action-based dashboards that provide greater understanding and context. eCase software’s analytical dashboards, for example, organise and display important information at a glance to help providers understand their data and unearth answers to critical questions.
“Providing operational and clinical insights for aged care management and staff, eCase retrieves, analyses and reports on key industry metrics as well as other informational requirements an aged care provider may have,” says Combe.


“By connecting dashboards to specific metrics or key performance indicators, aged care providers can gain vital business
 Glen Hegner
Glen Hegner
intelligence along with the ability to dive deep into specific pieces of information to continually monitor progress.”
Visual insights for clinical teams
Visualising data via dashboards can benefit and assist clinical managers in identifying patterns and highlighting important issues in multiple ways. Falls, for example, remain a leading cause of hospitalised injuries and injury deaths among older Australians, making up 77 per cent of all injury hospitalisations and 71 per cent of injury deaths in people aged 65 and over.
Residential aged care quality indicator data from 2021-22 shows that almost a third of aged care residents experienced a fall each quarter, with over 2 per cent of falls causing a major injury.
Combe says that while the approach to fall prevention is multifactorial, dashboards can provide a visual evaluation of the effectiveness of current prevention strategies.
“By collating and analysing valuable data such as current medications, mobility status, time and location, providers can form the foundation of trend analysis,” she tells AAA. “By analysing variables, clinical managers can gain a more comprehensive understanding of fall incidents and adjust strategies as required.”
Combes adds that the power of AI is, essentially, driven by the access to the data it has. “The more data that can be integrated, the more powerful insights can be drawn,” she says. “This is why, when it comes to selecting a software system, it’s important to choose one that is interoperable and easy to connect with other systems via APIs.”
Interoperability is key
Glen Hegner, chief information officer at Fresh Hope Communities, says that if providers “go down a road with disparate software systems” it will be much harder to reach a “single pane of glass” that is managing a complex digital system from a single executive dashboard. He also warns that integrations can be more costly than the original cost of the software.
“Operators should choose their software partners carefully, and ensure that the systems chosen have easy access to an API,” Hegner explains, “which means you can export the
data into other systems, such as a business intelligence platform.”

Hegner says that integrated data should also be “cleansed”, referring to the process in which data that is incomplete, incorrect, improperly formatted, duplicated, or irrelevant to the task at hand, is removed prior to sharing.
“eCase integrates with My Health Record, sharing resident data, but only in a cleansed format,” says Hegner. “This is important from a cybersecurity standpoint, as you are only sharing information that is necessary to the task.”
“Fresh Hope Communities is also currently working with Health Metrics on an API to a survey tool platform that will assist us with the star rating function. Again, being able to only export the relevant resident data is key,” he says. Improving resident and staff experience The second category includes items such as medical sensors and assistive technologies. Wearable medical sensors can be used to analyse and model data in regard to age, medications, conditions and health telemetry (for example, temperature, blood pressure and ECG).
Over a period of time, care staff and general practitioners can obtain a better understanding of how aged care residents are responding to their treatment and care.
A number of aged care facilities have started to adopt AI and machine vision to detect falls and monitor pain. Camera and visual monitoring streams can be used to gauge pain levels based on facial expressions. PainChek, for example, uses AI technology to identify the presence of pain even when it’s not obvious.
Using the PainChek app via a smartphone camera, the platform analyses images using AI-driven facial recognition. This is particularly beneficial for residents with dementia and other conditions where they are not able to communicate their pain or their level of pain.
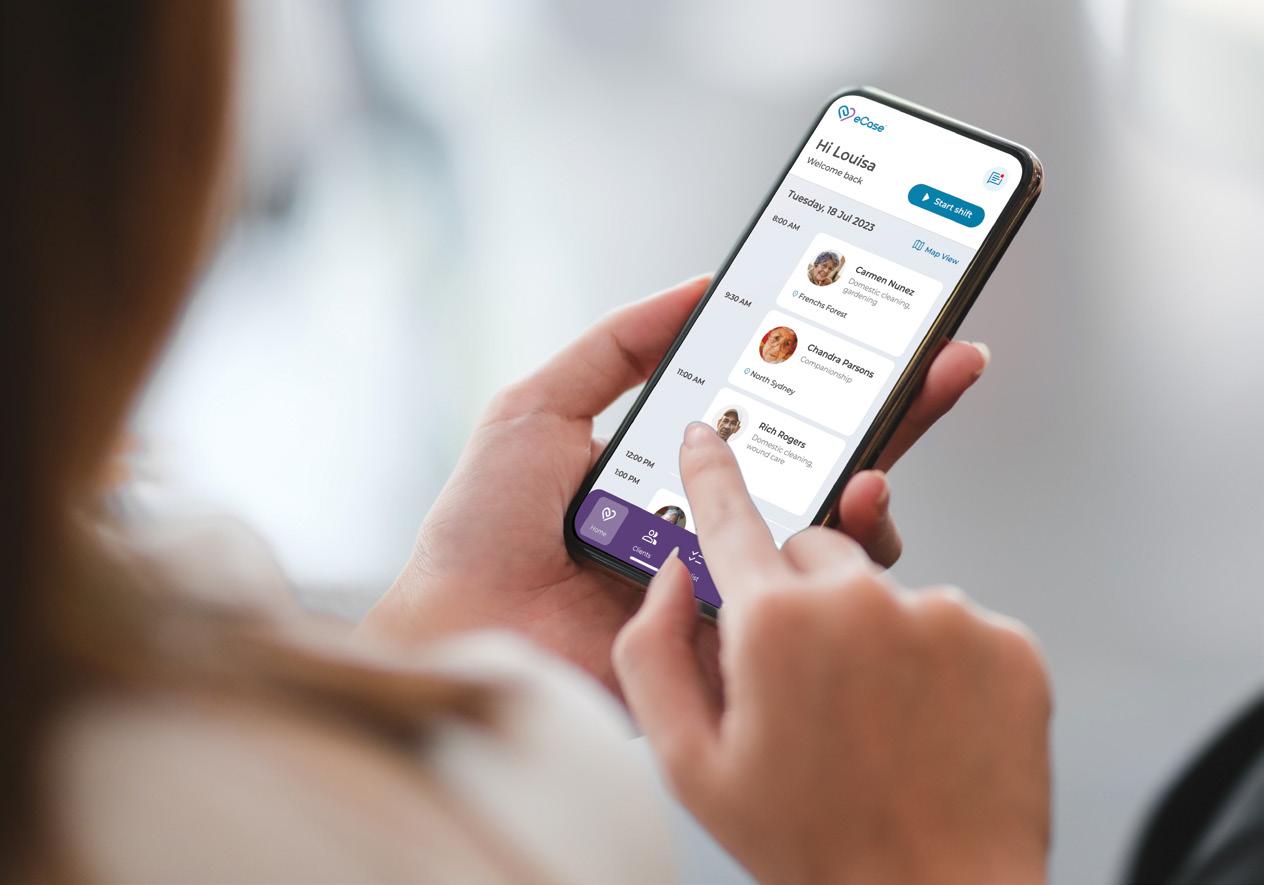

eCase provides operational and clinical insights for aged care management andstaff
“It’s important to choose software that is interoperable and easy to connect with other systems via APIs.”
St Andrews is a community-based, not-for-profit aged care organisation providing residential aged care, retirement living and community care services to over 600 people in the Ballina, Northern Rivers and the Far North Coast region of New South Wales.
Joining St Andrews as chief executive officer in January 2022, Todd Yourell quickly discovered he was unable to access information or reports about the daily activities of care in the residential facility. Although there was an existing care management system in place, it was not providing the oversight he required nor the functionality required by care staff.
“It had gotten to the point where records of showers or Activities of Daily Living for residents were being put on a whiteboard, informing staff of what they needed to do that day,” says Yourell.
At this point, it was clear that St Andrews needed to decommission their existing care management system and undertake a tender process. Adding to the urgency were the disappointing mid-year results of an Aged Care Quality and Safety Commission audit.
“The feedback from the commission was that, although it was very obvious that our carers were providing great care to residents, we were unable to produce the documentation to back that up,” says Yourell.
In addition to managing the reporting requirements and general functions of their residential aged care facility, Yourell required a software system that would also work across St Andrews’ retirement villages and community care operations.
“I wanted a system that would work across all three,” says Yourell, “because residents move into our retirement living, get home care or viceversa, and eventually track through to the aged care facility.”
“One of the early things that came to my attention was a potential resident who had left our retirement-living village and had gone to another organisation as they didn’t know we had an aged care facility. The admissions team in the aged care facility also didn’t know that people who were enquiring to come into the facility had been with us in another format, as we had no history of them,” he says.
Closing the information gap
Once the decision was made to go to tender, Yourell started to actively research and speak to suitable software vendors in the aged care industry.


Twelve organisations were invited to tender, resulting in six responses that were shortlisted to three, including eCase software by Health Metrics.

“I knew eCase because I’ve used it during a prior role at Tricare,” says Yourell. “Our facility manager at the time we were reviewing the different systems with, was familiar with it as well,” says Yourell.
St Andrews decided to go with eCase as they identified the software was an advanced system to manage and document resident care. It also provided a better user experience that was easy for staff to follow. In addition, as a personcentred care management system, eCase is able to track the resident journey from home care to retirement living through to residential care.
“We really wanted a system that would manage residents within one single record architecture, which I didn’t know existed until I spoke to Health Metrics. I wanted one system that would track people across our entire organisation and eCase provided that,” says Yourell, adding: “There was also great enthusiasm from the Health Metrics team and I knew there was going to be ongoing support put in place.”
Wanting to avoid having multiple systems that didn’t speak to each other, eCase’s interoperability was considered another key advantage. eCase will
“I wanted one system that would track people across our entire organisation and eCase provided that.”Delegates are taken through new features at the two-day eCase Customer Conference in Melbourne in July “We’re refreshing our look to better reflect our commitment to enabling better care,” says Health Metrics CEO Paul Brindle
integrate to PainChek and Checked In Care, a downloadable app available to residents’ families to keep them informed of their loved one’s activities and care.
“That’s a real positive,” says Yourell. “When your mum comes into our facility, you can log into Checked In Care and see their care plan, what activities they’ve been involved in and you can communicate directly with us. We also use PainChek for non-verbal communicators. It provides great historical data for residents which you can compare over time to view progress.”
Implementing the solution
St Andrews’ most pressing need was to implement eCase into their residential aged care facility.
eCase was then introduced into St Andrews’ retirement villages – 101 independent living units over four sites – and scoping was undertaken to provide St Andrews with the ability to generate eContracts and eQuotes as well as to easily undertake billing for services across their aged care facility and retirement villages. This included additional billing for services such as hairdressing, newspapers, taxis and escorts to medical appointments.
“This will make things so much easier, as we can put in a note saying this person receives the newspaper, five days out of seven, and add the cost one time. Previously we have had to make individual entries on the financial system, which is not productive,” says Yourell. “We want everything to work in the one system so we can see a complete record of people’s financial records.”
Next on the horizon, is the rollout of eCase across the organisation’s home care operations. St Andrews Community Care provides Home Care Packages, DVA Community Nursing, Veterans’ Home Care and private services such as meal preparation and clinical care.

Their extensive team includes registered nurses, enrolled nurses, certified personal care workers, gardeners and domestic assistants and cleaners, available to provide services seven days a week.
Yourell believes that the implementation will make significant changes to the back-end
Changing the face of care
Building on a history of over 15 years, we’re refreshing our look to better reflect our commitment to
We’re drawing a line in the sand between the Health Metrics of the past, with the delivery of a new future for eCase, for our customers, our users and our partners.
Our new branding provides the foundational elements of some transformational design changes that will be implemented into eCase as part of our investment into our User Interface (UI) and
Paul Brindle, chief executive officer of Health Metrics
corporate services office. “Just for community care alone, with tracking staff, rosters and billing appropriately, we’ve got a full-time equivalent looking just after that, whereas eCase will do it all at the push of a button,” he says. “It’s not just how it’s helping on the care side of things, it’s how it helps in the corporate services back-end office that will also make a huge impact,” he said.
Showing compliance made easy
With eCase in place, St Andrews is ready for the Aged Care Quality and Safety Commission to return for another audit.
“In a matter of only a couple of months with eCase in place, I can say I’d be really happy for the commissioners to come in now because I can give them any documentation that they want to see,” says Yourell.
“With the systems in place, the work logs, the care plans and assessments in place, we’re compliant, which is what we were not able to show previously. Now I can tell you what time people are having showers, what activities have occurred, things that I wouldn’t have been able t o tell you with the previous system.”
Yourell adds that making the change to eCase has made the work of the care staff easier and people are getting “through what they need to do”.
Where once care staff had been waiting until the end of shift before writing up their notes for the day, they’re now doing point-in-time care reporting directly to eCase via tablets.
“They click on the resident’s image, see their tasks and tick completed. It’s a lot easier,” says Yourell. “Staff have commented to me that it’s really good we’ve got this accountability.”
When asked if the whiteboard is still in place, Yourell says: “There’s no more whiteboard. That’s a very good sign.” n
“With eCase in place, I’d be really happy for the commissioners to come in now because I can give them any documentation that they want to see.”
