















Overwhelmed with managing your human resources and payroll tasks?
Don’t let these complexities hinder your practice growth and operational efficiencies.
Let HR&P tailor a solution providing you the freedom to focus on patient care and scale your business.






• Scalable and flexible administrative models
• Reliable payroll administration & tax services
• Comprehensive benefits administration
• Regulatory compliance and human resource management
• Affordable Care Act (ACA) compliance
• Advanced, proprietary human resource technology (HRIS)
• Houston-based designated support team in each discipline


As a dentist, you face unique challenges every day. That’s why at MedPro Group, we created an industry-leading malpractice policy that keeps you safe. Here’s what else you can expect with MedPro on your side.
Get unmatched coverage. Practice more safely. Protect your good name.
You’ll get great coverage at a great price. We also offer policy options that others don’t — including Occurrence and a pure consent clause, which gives you more control during a claim.
With 24/7 access to our free risk resources and on-staff experts, you and your practice will be better prepared for every day challenges. We don’t just defend claims, we help you avoid them.
The average dentist is sued at least once in their career, which is why we’re in your corner when it matters most. We lead the industry with a 95% dental trial win rate (plus 8 out of 10 claims close without payment).




ADDRESS TO THE 2025 TEXAS DENTAL ASSOCIATION HOUSE OF DELEGATES
Glen D. Hall, DDS
190 TDA OUTGOING PRESIDENT’S ADDRESS TO THE 2025 TEXAS DENTAL ASSOCIATION HOUSE OF DELEGATES
Georganne P. McCandless, DDS
15TH DISTRICT TRUSTEE, AMERICAN DENTAL ASSOCIATION, ADDRESS TO THE 2025 TEXAS DENTAL ASSOCIATION HOUSE OF DELEGATES
Rita M. Cammarata, DDS
SELF-ASSEMBLING P11-4 PEPTIDE FOR BIOMIMETIC REMINERALIZATION OF INCIPIENT ENAMEL LESIONS: A REPORT OF 2 ADOLESCENT CASES
Priyanshi Ritwik, BDS, MS
Brian P. LeSage, DDS
Oded Bahat, BDS, MSD
Guest Editor Rade D. Paravina, DDS, MS, PhD
210 Value for Your Profession: Are You Writing Prescriptions on Paper? Here’s Why This Is a Problem— And Why You and Your Patients Will Be Happier When You ePrescribe
213 Oral and Maxillofacial Pathology: Case of the Month
214 Oral and Maxillofacial Pathology: Case of the Month Diagnosis and Management
217 In Memoriam
218 Classifieds
223 Index to Advertisers
Errata: The May 2025 Texas Dental Journal featured an article from the November 2022 issue without proper acknowledgment of republication and reprinting: Surgical Repositioning of Intrusive Luxation Injury with 15-Year Follow-up: A Case Report.
Jacqueline M. Plemons, DDS, MS, Editor
Juliana Robledo, DDS, Associate Editor
Nicole Scott, Managing Editor
Barbara Donovan, Art Director
Lee Ann Johnson, CAE, Director of Member Services
Ronald C. Auvenshine, DDS, PhD
Barry K. Bartee, DDS, MD
Patricia L. Blanton, DDS, PhD
William C. Bone, DDS
Phillip M. Campbell, DDS, MSD
Michaell A. Huber, DDS
Arthur H. Jeske, DMD, PhD
Larry D. Jones, DDS
Paul A. Kennedy, Jr., DDS, MS
Scott R. Makins, DDS, MS
Daniel Perez, DDS
William F. Wathen, DMD
Robert C. White, DDS
Leighton A. Wier, DDS
Douglas B. Willingham, DDS
The Texas Dental Journal is a peer-reviewed publication. Established February 1883 • Vol 142 | No. 4
Texas Dental Association 8701 W Hwy 71, Ste 201-M, Austin, TX 78735 Phone: 512-443-3675 • FAX: 512-443-3031 Email: tda@tda.org • Website: www.tda.org
Texas Dental Journal (ISSN 0040-4284) is published monthly, except January-February, March-April, July-August, and November-December, which are combined issues, by the Texas Dental Association, 8701 W Hwy 71, Ste 201-M Austin, TX 78735, 512-443-3675. Periodicals Postage Paid at Austin, Texas, and at additional mailing offices. POSTMASTER: Send address changes to TEXAS DENTAL JOURNAL, 8701 W Hwy 71, Ste 201-M, Austin, TX 78735. Copyright 2025 Texas Dental Association. All rights reserved. Annual subscriptions: Texas Dental Association members $17. In-state ADA Affiliated $49.50 + tax, Out-of-state ADA Affiliated $49.50. In-state Non-ADA Affiliated $82.50 + tax, Out-of-state Non-ADA Affiliated $82.50. Single issue price: $6 ADA Affiliated, $17 Non-ADA Affiliated. For in-state orders, add 8.25% sales tax. Contributions: Manuscripts and news items of interest to the membership of the society are solicited. Electronic submissions are required. Manuscripts should be typewritten, double spaced, and the original copy should be submitted. For more information, please refer to the Instructions for Contributors statement at tda.org. All statements of opinion and of supposed facts are published on authority of the writer under whose name they appear and are not to be regarded as the views of the Texas Dental Association, unless such statements have been adopted by the Association. Articles are accepted with the understanding that they have not been published previously. Authors must disclose any financial or other interests they may have in products or services described in their articles.
Advertisements: Publication of advertisements in this journal does not constitute a guarantee or endorsement by the Association of the quality of value of such product or of the claims made.
Two ways to register: Call us at 214-384-0796 or e-mail us at sedationce@aol.com Visit us on the web: www.sedationce.com NOW Available: In-Office ACLS & PALS renewals; In-Office Emergency Program Live Programs Available Throughout Texas
Two ways to Register for our Continuing Education Programs: e-mail us at sedationce@aol.com or call us at 214-384-0796
OUR GOAL: To teach safe and effective anesthesia techniques and management of medical emergencies in an understandable manner. WHO WE ARE: We are licensed and practicing dentists in Texas who understand your needs, having provided anesthesia continuing education courses for 34 years. The new anesthesia guidelines were recently approved by the Texas State Board of Dental Examiners. As practicing dental anesthesiologists and educators, we have established continuing education programs to meet these needs.
Two programs available (satisfies rules 104.1 and 111.1)
Live Webcast (counts as in-class CE) or Online (at your convenience)
All programs can be taken individually or with a special discount pricing (ask Dr. Canfield) for a bundle of 2 programs:
Principles of Pain Management
Fulfills rule 104.1 for all practitioners
Use and Abuse of Prescription M edications and Provider Prescription Program
Fulfills rules 104.1 and 111.1
Nitrous Oxide/Oxygen Conscious Sedation Course for Dentists:
Credit: 18 hours lecture/participation (you must complete the online portion prior to the clinical part)
Level 1 Initial Minimal Sedation Permit Courses:
*Hybrid program consisting of Live Lecture and online combination
Credit: 20 hours lecture with 20 clinical experiences
SEDATION REPERMIT PROGRAMS: LEVELS 1 and 2
(ONLINE, LIVE WEBCAST AND IN CLASS)
ONLINE LEVEL 3 AND 4 SEDATION REPERMIT AVAILABLE!
(Parenteral Review) Level 3 or Level 4 Anesthesia Programs (In Class, Webcast and Online available):
American Heart Association Advanced Cardiac Life Support (ACLS) and Pediatric Advanced Life Support (PALS) Initial and Renewal Programs
NOTE: ACLS or PALS Renewal can be completed by itself at any combined program Combined ACLS-PALS-BLS and Level 2, 3 and
WEBCASTING and ONLINE RENEWALS AVAILABLE! Live and archived webcasting to your computer in the comfort of your home. Here are the distinct advantages of the webcast (contact us at 214-384-0796 to see which courses are available for webcast):
1. You can receive continuing education credit for simultaneous live lecture CE hours.
2. There is no need to travel to the program location. You can stay at home or in your office to view and listen to the course.
3. There may be a post-test after the online course concludes, so you will receive immediate CE credit for attendance
4. With the webcast, you can enjoy real-time interaction with the course instructor, utilizing a question and answer format
OUR MISSION STATEMENT: To provide affordable, quality anesthesia education with knowledgeable and experienced instructors, both in a clinical and academic manner while being a valuable resource to the practitioner after the programs. Courses are designed to meet the needs of the dental profession at all levels.
Our continuing education programs fulfill the TSBDE Rule 110 practitioner requirement in the process to obtain selected Sedation permits. AGD Codes for all programs: 341 Anesthesia & Pain Control; 342 Conscious Sedation; 343 Oral Sedation This is only a partial listing of sedation courses. Please consult our www.sedationce.com for updates and new programs. Two ways to Register: e-mail us at sedationce@aol.com or call us at 214-384-0796

¥ Available for consultation by phone or email
¥ Color histology images on all reports
¥ Expedited specimen shipping with tracking numbers
¥ Reports available online through secure web interface Professional, reliable service with hightechnology solutions so that you can better serve your patients. Call or email for free kits or consultation. jkjpathology.com 281-292-7954 (T) 281-292-7372 (F) johnkacher@jkjpathology.com

PRESIDENT Glen D. Hall, DDS 325-698-7560, abdent78@gmail.com
PRESIDENT-ELECT Elizabeth Goldman, DDS 214-585-0268, texasredbuddental@gmail.com
PAST PRESIDENT Georganne P. McCandless, DDS 281-516-2700, gmccandl@yahoo.com
VICE PRESIDENT, SOUTHEAST Matthew J. Heck, DDS 512-280-8800, matthewjheckdds@gmail.com
VICE PRESIDENT, SOUTHWEST Melissa Uriegas, DDS 956-800-1625, meluriegas@gmail.com
VICE PRESIDENT, NORTHWEST Adam S. Awtrey, DDS 325-672-2794, awtrey.adam@gmail.com
VICE PRESIDENT, NORTHEAST Drew M. Vanderbrook, DDS 214-821-5200, vanderbrookdds@gmail.com
SENIOR DIRECTOR, SOUTHEAST Ron Hill, DDS 713-626-8343, rhilldds@gmail.com
SENIOR DIRECTOR, SOUTHWEST Austin Lee, DDS 210-496-1919, austinvincentlee@gmail.com
SENIOR DIRECTOR, NORTHWEST Annie C. Wilson, DDS 817-860-4343, annie@anniewilsondds.com
SENIOR DIRECTOR, NORTHEAST Shane A. Ricci, DDS 972-381-1888, riccidds@hotmail.com
DIRECTOR, SOUTHEAST Jennifer Hathaway, DDS 979-776-6884, jp.hathaway@yahoo.com
DIRECTOR, SOUTHWEST Kenneth Gonzales, DDS 361-992-2421, bikerdent@yahoo.com
DIRECTOR, NORTHWEST Kevin Altieri, DDS 817-294-5513/817-991-1835 altdent@yahoo.com
DIRECTOR, NORTHEAST Celeste Latham, DDS 214-351-1500, drclatham@yahoo.com
SECRETARY-TREASURER* Oshmi Dutta, DDS 210-888-0700, odutta@gmail.com
SPEAKER OF THE HOUSE* Gregory W. Rashall, DDS 936-336-5171, rashdent@sbcglobal.net
PARLIAMENTARIAN** Jodi D. Danna, DDS 972-377-7800, jodidds1@gmail.com
EDITOR** Jacqueline M. Plemons, DDS, MS 214-507-0815, drplemons@yahoo.com
LEGAL COUNSEL** Carl R. Galant
INTERIM EXECUTIVE DIRECTOR** Duc M. Ho, DDS 281-395-2112, ducmho@sbcglobal.net
*Non-voting member **Non-voting



TDA Awards Committee members include Dr Matthew J. Heck, chair, Dr Adam S. Awtrey, Dr Melissa Uriegas, and Dr Drew M. Vanderbrook. Awards were presented at the TDA House of Delegates during the TDA Meeting in San Antonio in May 2025.

Dr Carmen P. Smith received the Gold Medal for Distinguished Service Award, presented by Dr Georganne McCandless. This is the association’s highest award, given to a dentist who represents the best of the TDA, dedicating his or her life to the Association and profession, advancing both through his or her commitment, strength, and vision.


Dr Glen D. Hall received the Incoming President’s Award.

Dr Tanya Sue Maestas received the Rising Star of the Lone Star Award, presented by Dr Georganne McCandless.

Dr Georganne P. McCandless, who served the association as president-elect and president, receives the Outgoing President’s Award, presented by Glen D. Hall.

Drs Mark A. Camp (not pictured), Laji J. James, Krystelle Anaya, and Stephen A. Sperry (not pictured), who served the Association as directors, senior directors, and vice presidents. Presented by Dr Melissa Uriegas and Dr Adam Awtrey.
The TDA Outstanding Senior Dental Student Award recipients were Laura Fernandez for the Texas A&M University College of Dentistry, Stanton Pruitt for the University of Texas School of Dentistry at Houston, Mira Lavallee for the University of Texas Health Science Center at San Antonio School of Dentistry, and Betsaida Delgado for the Woody L. Hunt School of Medicine, El Paso.



President’s Awards were presented to Dr Ensy A. Atarod (accepted on her behalf by Dr Shaliee Gupta), Ms Charlotte Bolls of Greater Houston Dental Society, and Dr Jerry J. Hopson (accepted on his behalf by Dr Shane Ricci).

Drs Ronald Lee, Kathleen Nichols, Adam Shisler, Katie E. Stuchlik, Elizabeth D. Jaynes, David A. Slaughter (not pictured), and Travis Campbell (not pictured), who served the Association as Council Members. Presented by Drs Melissa Uriegas (left), Adam Awtrey (right), and Drew Vanderbrook (far right).
Certificates of Merit were presented to Everyone for Veterans, in recognition of its efforts to serve the dental health and welfare of the disadvantaged veterans in the Lubbock area; Ms Mitzi Robers, in recognition of her efforts to serve the dental health and welfare of the disadvantaged population of San Antonio.
TDA SERVICE RECOGNITION AWARDS



Service Recognition Awards were presented to Dr Duc “Duke” M. Ho for his unwavering dedication and exceptional contribution to the TDA; Mr Carl Galant for his outstanding achievement in facilitating the successful sale of the TDA building and the acquisition of the TDA Financial Services Insurance Program; and Ms Jane Evans for her years of tireless dedication to the Dallas County Dental Society and exceptional commitment to the TDA Smiles Foundation and the Texas Mission of Mercy.
Mrs Gloria A. Morales receives the award for her leadership as president of the Alliance of the Texas Dental.


TDA Incoming President’s Address to the 2025 Texas Dental Association House of Delegates may 10, 2025
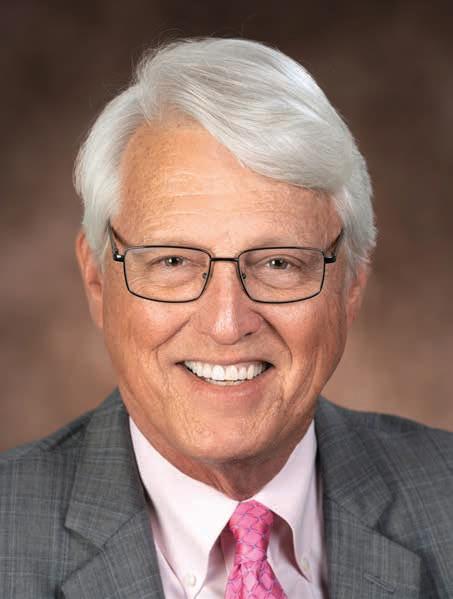
Glen D. Hall, DDS Incoming TDA President

I feel it’s a great responsibility to stand before you as the incoming president of this esteemed organization—an organization through which many of my friends have mentored me.
Today, I want to share a vision for: (1) strengthening our membership, and (2) shaping the future of our profession—a future rooted in unity, innovation, and purpose. My remarks will take us on a journey through:
• the challenges we face,
• the strategies to overcome them, and
• a personal reflection on what it means to lead.
Let’s begin with a reality we cannot ignore: our declining membership market share. This isn’t just a Texas issue or a dentistry issue—it’s a trend across professional associations. But for us, the stakes are high. Fewer members mean:
• less advocacy power,
• fewer resources, and
• a weaker voice in shaping the future of dental practice.
It’s not just about numbers. It’s about our ability to represent you—to protect your practice, and advance our profession.
You may ask, “Why is this happening”? Research tells us the answer lies in the changing landscape of dentistry. Newer dentists face unprecedented challenges: crushing student debt, the rise of employee dentist roles, and a reliance on digital tools for education and networking. For many, the traditional model of association membership feels disconnected from these realities.
Some question the value of their dues, asking, “What’s in it for me?”
This is our challenge—but it’s also our opportunity to adapt, innovate, and redefine what membership means.

Dr Hall’s Sister, Vicki Daughdrill, visits from Atlanta, Georgia.

To rebuild and strengthen our market share, we must focus on 3 key strategies.
First, we must clearly communicate our value proposition. When we poll our members, one word traditionally rises above all others: advocacy. Advocacy is the heartbeat of the TDA. Through tireless efforts in the state legislature, we’ve protected you from burdensome regulations and advanced laws that benefit both patients and providers.
Take Senate Bill 1090 from this session, which tackles dental insurance reforms, ensuring fair compensation for dentists, and transparency for patients. This isn’t abstract—it directly impacts your ability to practice profitably. Our Council on Legislative and Regulatory Affairs, dedicated staff, and lobby team work year-round to monitor and influence legislation. You, as delegates and officers, know this value best. It’s our job to be the light in the darkness of membership doubt, reminding every dentist that their

membership fuels this critical work.
But we can’t stop there. We must ensure every member understands the full scope of what their dues unlock.
Second, we must invest in modern, flexible member engagement. Today’s dentists are busy, balancing practice management, family, and professional growth. To meet them where they are, our engagement must be:
• mobile-friendly,
• relevant, and
• accessible.
We’ve made strides here. In our most recent poll, continuing education was the #1 value of membership. Our Dental Concierge app offers on-demand CE, with affordable courses on digital dentistry, regulatory compliance, and patient care—many of which are available 24/7.
But we can do more.
Expanding these platforms will ensure education fits into members’ lives, not the other way around.
We must also deepen our support for early-career dentists. With your help, initiatives from our Council on Membership, New Dentists, and students seek to provide tailored resources for navigating private practice, DSOs, large group practices, or academia. By connecting new dentists with mentors and expert guidance, we’re not just helping them succeed— we’re cultivating the next generation of leaders. Engagement like this builds loyalty and shows we’re invested in their future.
Third, we must foster a stronger sense of community and belonging. Membership isn’t just about perquisites—it’s about feeling connected to something bigger.
• The TDA Leadership Institute equips emerging leaders with tools, networks, and confidence to contribute to our profession. These experiences create lifelong bonds among peers across Texas.

• Our annual meeting is another cornerstone—blending education, networking, and camaraderie. This year’s “Totally ‘80s Party,” with arcade games, roller-skating, and prizes, reminded us of the joy in being together.
These moments recharge us, reinforcing that we’re part of a vibrant, supportive community.
Looking at the present, let’s talk about a specific issue tied to membership: dues and market share.
In 2019, the ADA changed its dues structure for new members, moving from no dues to full dues in 3 years instead of 5. The impact was stark. Texas licenses about 900 dentists annually. Before the change, our retention rate was 60%. After that change, it dropped to 30%. In 2000, our market share was 74%. Last year, it was 42%. This doesn’t mean we are losing members, it means that fewer dentists join than don’t join, or fewer renew than those that let their membership expire. Over the years that difference becomes significant.
So let us imagine a third-year dental student—they’re not yet ready to practice independently. Similarly, a third-year member, just hitting full dues, often lacks the experience to fully appreciate the value of membership. Too many leave before they see the full picture. We must rethink how we onboard new members, helping them understand the long-term benefits of their investment.
Now, looking ahead, let’s consider a transformative tool: artificial and augmented intelligence. AI is already reshaping how associations deliver value. Imagine personalized outreach that recognizes your practice specialty or special interest and suggests tailored CE courses or events. AI-driven platforms can adapt content in real time based on your learning needs, making education more effective and engaging. AI won’t replace human leadership, nor do we want it to—but it will amplify our ability to serve, understand, and connect with members. Paired with a bold strategy, AI can drive innovation and keep us ahead of the curve.

As I close, let me share a personal reflection. Becoming president of the Texas Dental Association is one of the greatest honors of my life—a role I didn’t seek but embraced when my colleagues entrusted me with it. My journey began years ago in Abilene, where my landlord, a pediatric dentist and member of the Council on Insurance, invited me to a local component meeting. That moment opened my eyes to the power of collective action. At my first TDA House of Delegates meeting where I was to serve as an alternate delegate, the first person to speak to me was Dr Rene Rosas from El Paso. He introduced himself to me in his usual humble manner and befriended me on the spot, and continued to mentor me and many other over his active years.
From there, I served on committees and councils at the TDA and ADA, learning that leadership isn’t about titles—it’s about service. I’ve seen it first-hand: from pioneers who have created programs helping millions of underserved and needy, to colleagues who bridged the past with the future. They all embody the same characteristics: listening, stepping forward, and asking how we can do better for our members, patients, and communities.
As your president, I carry that philosophy forward. My goal is to unite us around shared purpose, supported by a strong board and an engaged membership. Simply, I want to hear from you, understand your different needs and work alongside each of you to better our profession. Together, we can lead Texas dentistry into a future defined by innovation, collaboration, and excellence.
Before I conclude, allow me to thank those who’ve walked this journey with me. First, my wife Carol whose unwavering support has been the backbone of my practice and leadership. Two of my 3 children are here today: my son Eric, his wife Christina, and their children Morgan, Matthew, and Christopher, from Dripping Springs; and my daughter Andrea Leggett, who works in customer relations at my office, her husband Zack, and their children Jackson and Laura from Abilene. My son Brian, his wife Elizabeth, and their children Caleb, Joshua, and Daniel, couldn’t join us from El Paso, but they’re with me in spirit.
Thank you for your trust and for joining me in this mission to strengthen our association and shape the future of our profession. Let’s do this together.

TDA outgoing President’s Address to the 2025
Texas Dental Association House of Delegates May 9, 2025


It is my honor to be speaking to you today as your Texas Dental Association president. It has been my distinct privilege to represent you and our beloved profession this past year. It has been an incredibly busy and productive year. I’ve traveled from Amarillo to Corpus Christi. I’ve gone from El Paso (my heart and where I grew up) all the way to east Texas and everywhere in between. My many journeys have highlighted how special our dental component societies in Texas are. Between myself, Dr Hall and Dr Graves, we managed to visit 22 local component dental societies.
Your kindness when hosting me in your components was greatly appreciated. You offered up your homes for me to stay in, you picked me up from the airport, you spent the afternoons away from your offices to have extended meals with me. I also received all kinds of gifts along the way: chocolates, wine, Red Raider Texas steaks and tons of personal and heartfelt handwritten notes.
In public, you greeted me in many ways. Most of the time, it was Dr McCandless, often it was Madam President. But on occasion, it was Ms TDA. The Rio Grande Valley dental society and TDA board member Dr Melissa Uriegas presented me with a special gift: a sparkly Ms TDA sash. The TDA vice presidents completed the ensemble by gifting me a customized crown. I wear them both with pride…in the hope that I could also bring world peace as TDA president.




As I traveled the state proudly representing you as your president, one thing has been apparent: membership matters. It’s having membership in organized dentistry but it’s also the importance of our shared experiences as essential health care providers. These are the things that continue to matter. You tell me and show me all the time how much this matters.
Last year in my House of Delegates speech, I talked a lot about our shared experiences. I talked about my own shared experiences with colleagues during various stages of my career. Those shared experiences kept me engaged in organized dentistry and defined my career path.
I asked each of you, “What is your shared experience with your colleagues?” I challenged you to define those shared experiences with our members and especially our nonmembers. Defining and focusing on those shared experiences was what I highlighted everywhere I went. In fact, I talked about it so much that you all started saying it back to me.
During our visits you all asked the hard questions.
• What is the status of our declining membership in the tripartite?
• What is TDA doing to guard against third-party payor interference?
• How is TDA dealing with the unwarranted expansion of scope of practice?
• What can we do about depression and suicide among dental professionals?
While I answered these questions to the best of my ability and we had the most thoughtful discussions surrounding these challenging issues, we didn’t always have an immediate solution.
But what I asked you in response was just as important.
• Are you participating in your local components?
• Are you inviting nonmember friends to these local meetings and sometimes paying for them?
• Are you saying yes to a leadership position?
• Are you offering to be an ear to listen to our younger colleagues?
• What sacrifices are you making?
As mental health and well-being in our profession has moved to the forefront of our discussions, membership in our association is even more important today. One is but the loneliest number, but by growing our membership, we can band together and be more than just one.



Dentistry can be hard, but in the best of ways. When dental professionals come together in an organized way with one big voice, the dividends are innumerable. The benefits of membership in a professional association have long been reported on. It can improve personal and professional growth, but can also lead to opportunities unseen. Opportunities such as:
• Opening yourself up to new professional possibilities— like becoming TDA president!;
• Being part of a larger community that not only understands you, but can support you in every way;
• Providing avenues for mentorship and fellowship;
• Having the ability to influence and direct the future of our profession;
• Gaining access to tangible benefits like health insurance, CE opportunities and partnerships with endorsed vendors.
The Texas Dental Association continues to work hard for our members. This year our CLARA team put together a robust 2025 legislative agenda that includes:
• Requesting a long overdue increase in Medicaid reimbursements;
• Protecting patients and dentists through dental insurance reform;
• Urging the legislature to reinstate funding for the Dental Education Loan Repayment Program;
• Improving oral health access and;
• Protecting Texans by expanding Botox administration for enhanced patient care and advocating for a commonsense patient protection bill as it relates to DIY clear aligners.
Shout out to our very own TDA members Drs Matt Roberts, Shailee Gupta, Brooke Elmore, and Alex Otto for giving of their time and testimonies at the Texas Capitol on behalf of TDA.
In addition, TDA has recently acquired the TDA Financial Services Insurance Program. This new, member-owned insurance business offers a full range of insurance products to benefit you, your staff, your family and your dental practice. In addition to these multiple insurance offerings, TDA members also have access to a healthcare member benefits program that utilizes a national PPO network.
The work of our Council on Annual Meetings and Continuing Education Programs goes forward at a full pace. Their work all year long is reflected in this annual meeting. Along with the


continued expansion of our CE concierge, they are answering a member need: bringing continuing education to you.
And our Council on Public Health and Access to Care did the heavy lifting this year after they identified an administrative downcoding policy by Dentaquest that reclassified multisurface posterior restorations without interproximal surfaces to a Class I. TDA disagreed with this and immediately filed a formal complaint with the Texas Human Health Services Commission. TDA’s advocacy efforts were successful and this was reversed.
My deepest thank you goes out to our TDA Board. Their generosity of time and deliberate debate and discussion helped guide our Association forward. I’ve said it before and I will say it again, our TDA staff are a dedicated group of individuals that work tirelessly on our behalf.
A big thank you goes to my staff. They jumped through hoops this year to make my schedule work and allow me to serve in this capacity. And to my best friends Rita and Dottie, thanks for always being my biggest cheerleaders.
I would like to say a very special thank you to my husband Skip Fortune. You have been my driver, my valet, and my photographer. No one wants for my success more than you do. Ms TDA and her sparkly sash and crown could not have done the year without you. You are simply the best!
Before my crown slides off, I would like to show you the shared experiences we had this year (starts slide presentation).
Dentistry has been good to me and that’s in large part due to organized dentistry. I have loved doing this job, and I hope to have left something behind that you all can build on. Working on behalf of our profession with my friends and colleagues never felt like work.
TDA is invested in the success of every dentist, and I will continue educating people that we are the trusted source for dentists across their careers, no matter the practice setting, no matter if they are just starting out or have helped make smiles brighter over a long career. Our members are the ties that bind this association together, and I have truly benefited from our shared experiences.
Thank you!
















Running a dental practice shouldn’t feel like juggling HR, billing, marketing, and 87 phone calls a day.





Meet Jaza, your AI-powered office sidekick that:
Fills unscheduled treatment slots with confirmed appointments
Re-engages patients who haven’t visited in years
Converts Instagram, Facebook, & Google leads into paying patients
Handles your marketing like a pro
Manages HR tasks and operations without the drama
It’s like hiring five extra staff members — without the payroll.
Ridiculously Smart. Faster Growth.
www.jaza.ai


15th district trustee, american dental association, Address to the 2025 Texas Dental Association House of Delegates may 9, 2025


Mr Speaker, Madame President, Colleagues, and Distinguished guests. Thank you for taking the time to address you all this morning, and Mr Speaker, congrats on your first House. I wish you good luck, because this crowd can be pretty rowdy.

So, I am into my second year as the 15th District Trustee to the ADA from Texas and to say it has been uneventful would be an understatement. Building sales, software changes, credit unions, Forsythe acquisition, research lab consolidations, Foundation Veteran events, financial operating plans, and Strategic Forecasting, and then there were more events I never would have imagined.
I want to walk you through the past year, focusing on a few main things. I know we are in May and the beginning of the summer heat in Texas, but think back to a “Christmas Morning.” Picture in your mind the presents wrapped neatly under the tree, all is quiet, and then the kids wake up, unwrapping everything with unabandon fury begins, and all of the boxes and unassembled pieces of toys are scattered on the floor, no one is sure which piece goes where. Then, later in the aftermath, Mom is starting to clean up and organize all the pieces back into the boxes so the toys can be assembled and played with. This is where we are currently at the ADA.
Before Christmas, there is always the wish list. Initially, at ADA, there were predictions of large amounts of income from non-dues revenue offsetting increasing expenses; there was a thought that a new membership model was needed, and great hope that it would spark an increase in market share. And there was “investing” of reserves because “you can’t stop progress”, and “get on board or get out of the way”, these were mantras we were hearing. But ADA does not belong to any one person; it belongs to all of us, and there are checks and balances in place to protect this mindset; they should not be sidestepped, and they need to be strengthened.
Now let’s start to unwrap those presents under the tree, and we’ll start with the big shiny present in the back of the tree, the one all the kids hope has their name on it, but alas, it’s for your brother! In September,



In September, we made the switch to a new AMS (Association Management Software), and we bought Salesforce Fontiva. It went live on September 10th and has really been full of issues ever since. Membership data is the lifeblood of any Association, just like the data in your recare system drives your practice, member data maintains our Tripartite.
we made the switch to a new AMS (Association Management Software), and we bought Salesforce Fontiva. It went live on September 10th and has really been full of issues ever since. Membership data is the lifeblood of any Association, just like the data in your recare system drives your practice, member data maintains our tripartite. Since September, I have talked to Linda and Lee Ann, Sara from CADS, and Jane from DCDS, trying to be the liaison between Texas and the IT department at ADA. We owe Rachael Daigle a debt of gratitude for all the hours she has put into managing and protecting our membership data and for transferring the data over as cleanly and correctly as possible into Fontiva. Rachael is here, please stand up and let’s give her a round of applause, it is well deserved.
Working toward a solution, ADA brought in an IT company called Datazoom to start lining out the problems that developed as the conversion started. It was found that this out of the box system, Salesforce Fontiva, which cost $36MM and was designed to be utilized at 90% out of the box and 10% customizing to State and Local needs was currently at 60% out of the box and 40% custom, these change orders have cost the ADA another $17MM.
Can the system be what we need it to be? Yes. Should we have picked a different system? Maybe. Should we scrap it and start over? No, too costly. And what will it cost to fix? That is still being determined, but not nearly as much as we thought.
When you start to question these costs, remember this: first, Aptify was no longer a secure system to use (remember our data breach a few years back), and second, it could no longer be upgraded; a new system had to be put in place. Also, remember this new system is required to work for approximately 553 different entities across the country. All asking for different nuances and changes to the original out-of-the-box system. All of these costs were shouldered by the ADA. One can argue that maybe we should have had a member assessment, maybe we should have had the State or Local pay for their customizing requests. But that is not what has happened, and those costs were paid through the ADA Long Term Reserves.
So why did this all happen? We brought the system online too early, and the data incoming from those 553 entities was not uniform, hence, it did not transfer over into the correct fields during the conversion, and that’s a simple version of it. Plus, during all of this transitioning, a separate system called Broadcast Med was brought online, which took IT resources away from the conversion, further adding to the wrapping paper and toy pieces on the floor, maximizing the clutter and chaos of change.
But where are we now? We are currently working through stabilizing the system and getting us to an MVP (a Minimal Viable Product) by October of this year, that’s our renewal season. This ensures we can enroll new and renewing members and we have an operating UMA (a Universal Member Application) and can accept and transfer monies and have it assigned to the correct member. Now maybe you’re happy the big shiny present wasn’t for you but for your brother, he probably deserves it!!
Finally, we unwrapped our first present from under the tree, and it equated to getting a pack of socks for Christmas. At the May Board meeting, it was presented to the trustees that all states would move to the Membership Pilot because if not, we would continue to lose market share and never be able to regain the loss if we did not change course now. Despite this presentation, the trustees asked the then-president to ensure we would continue with the Pilot program as it was, on a voluntary basis only. This was a good decision as the state of the AMS has affected the new Membership Engagement Model
from truly being able to live up to its potential. The same 5 states that started in the new model are the only ones in the pilot, and we are pausing the inclusion of NEW states into the MEM at this time. Although it has shown a small bit of positive change, it has been hampered by the new AMS system.
Back to Christmas, and we get to “the stockings hung by the chimney with care”. What’s in them, a few envelopes from your grandparents, and you know there is cash in them. Well, some of your siblings have thrown their bills of money on the floor to be caught up with the wrapping paper and toy pieces. But there is always that one brother or sister who understands finances and squirrels their money away, while you’re still wondering where yours went. Could this sibling be our own Dr Cody Graves, ADA treasurer? He has been able to get answers to the questions the Finance Committee and BOT had been asking all along, but received answers along the lines of “stay in your lane”, or we were given financial data that supported the narrative being told at the time. Currently, the finances are being presented in a manner more consistent with which we are familiar, the FOP will be discontinued, and an annual budget with quarterly revisions will be implemented.
Just like the day after Christmas, our extended family leaves to go home, and we have to find room for the new toys and clothes. At ADA, we have to manage new situations and a different set of financial reports. Let me be clear, we have challenges ahead of us in Chicago, our coffers aren’t as full as they once were, but NO monies were lost.
But, just before Christmas day ends, your favorite Aunt rings the doorbell, and as usual, she comes with a smile, great positive energy, and the perfect present you had been hoping for. In February, Dr Betsy Shapiro was hired to be the Interim Executive Director of the ADA. The search for a new executive continues, but not at the pace at which it started. Betsy is beloved by many members of the Association. She is smart, fair, thoughtful, and introspective, and is an excellent representative of the ADA. She was at the White House on Monday, but most importantly, she is trusted by all. And at this point, ADA needs consistent, positive change to keep and regain that trust, that is the gift she brings to us today.
It’s now a few days after the holidays, and we’re heading for the ski trip, so we need to clean the house, put away the new stuff, and get packed to go to the mountains. That is where ADA is now: we are putting our house in order before the ED position is publicized, and then we can look to the future.
I know I haven’t given you a ton of details, Dr Graves and I will do an update on the state of the ADA today at 3:00 in Room 304C for questions you may want to ask ADA-related.
Also, we have two of my fellow trustees with us this weekend, both are candidates for the president-elect position of the ADA. Dr Michele Tulak-Gorecki from Michigan, representing the 9th District, and Dr Jim Boyle from Pennsylvania, representing the 3rd District. They will be the headliners today for the Candidates Forum, which we are doing today at 4:00 here in this room after the Reference Committee hearings. It will be a new format, podcast style.
Thank you to our Madame President, Dr McCandless, and our incoming President Dr Hall, and to all of you for everything you do for organized dentistry. Remember, we are better together as a tripartite, and the ADA must succeed for the profession to succeed. My pledge to you is to continue to do my best to make that happen. Have a good House and thank you all.

At ADA, we have to manage new situations and a different set of financial reports. Let me be clear, we have challenges ahead of us…

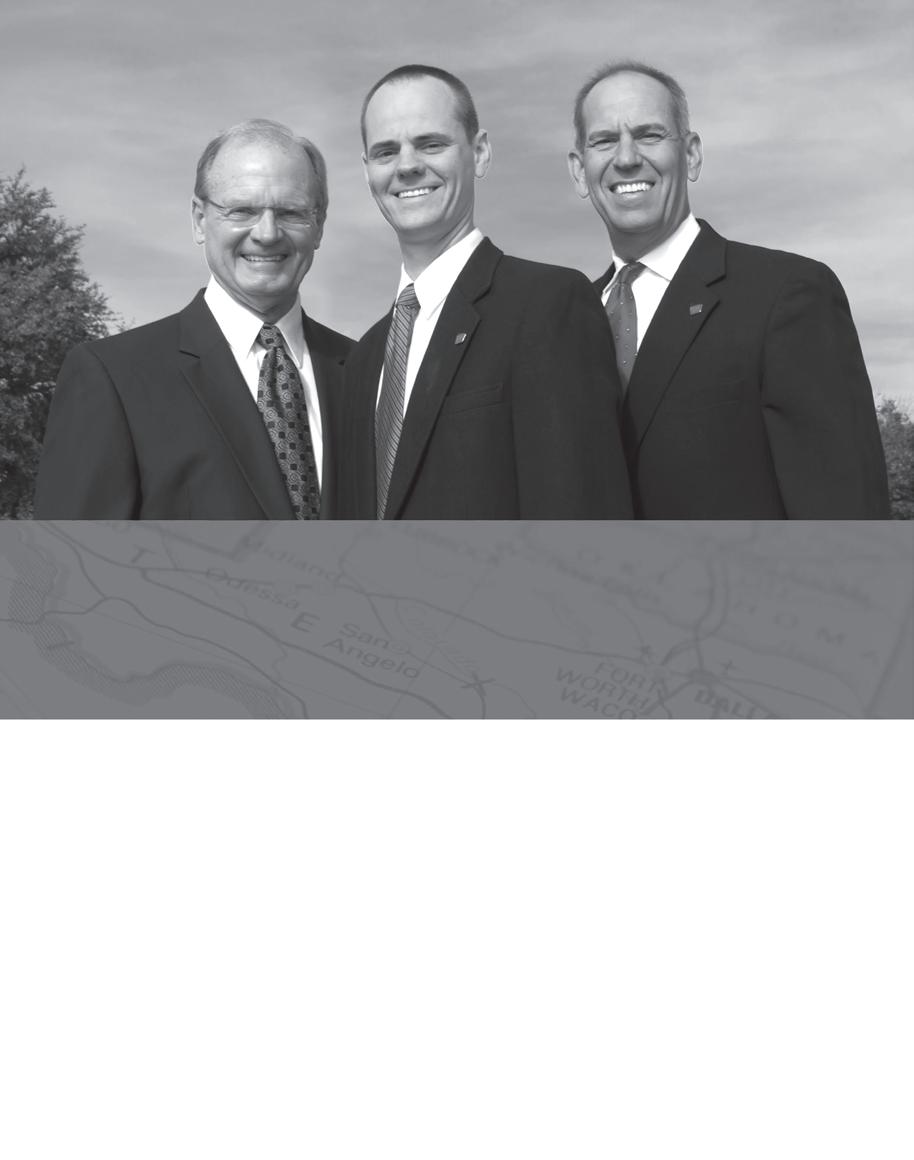
Your dental practice is more than a business—it’s your legacy. At Henry Schein Dental Practice Transitions, we specialize in helping practice owners with seamless, stress-free transitions tailored to personal, professional, and financial goals.
Why Choose Us for Your Practice Transition?
• Unlock your practice’s true value with expert, data-driven valuations to unlock your practice’s true value
• Gain access to 36,000+ purchasers
• Full-service support from your first consultation to final closing
• Unmatched expertise backed by local insights and deep industry connections
• Over 500 closings with over $400MM in sales price since 2023.

Start your journey to a rewarding retirement today. Contact us or scan the QR code to schedule a complimentary consultation.
800-988-5674
DPT@henryschein.com

Priyanshi Ritwik, BDS, MS
Professor, University of Texas Health Science Center at Houston School of Dentistry, Department of Pediatric Dentistry, Houston, Texas

Initial caries lesions (ICL) are noncavitated demineralized areas of enamel due to acid dissolution, which become clinically apparent when enamel is air-dried. Clinical management of ICL focuses on remineralization to prevent cavitation. Fluorides are widely utilized for remineralization of ICL, but fluoride only penetrates the outer 30 um of enamel surface, leaving the subsurface lesion in a demineralized state. Selfassembling P11-4 peptide (SAP) is a remineralizing agent that can permeate to the subsurface lesion and form a scaffold for remineralization. This article documents the indications, clinical steps, limitations and outcomes with SAP in 2 adolescent patients. In vitro studies and systematic reviews support the use of SAP for remineralizing ICL. All 5 teeth with ICL treated with SAP in the 2 patients did not exhibit clinical progression after 6 months but only 2 of the teeth showed esthetic improvement in the appearance of the treated ICL.
Key words
Incipient enamel lesions, self-assembling peptide, noninvasive treatment
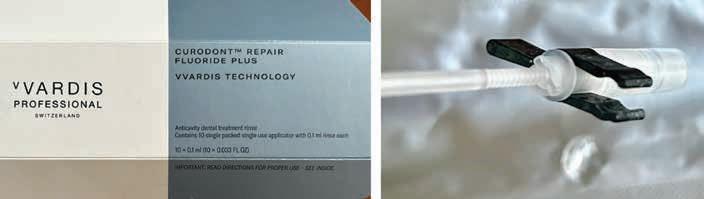
An in vitro study reported that CR led to guided remineralization in 2 weeks.10 Another in vitro study showed that SAP led to an increase in microdensity, hardness, and elastic modulus in artificially created ICL.1 A recent systematic review assessing the effectiveness of SAP showed that its use led to clinical arrest of ICL (relative risk [RR], 1.82 [95% CI, 1.32 to 2.50] and a 32% decrease in lesion size. It also led to a decrease in the incidence of cavitation (RR, 0.32 [95% CI, 0.10 to 1.06]; NNT, 6.9).9
There is limited case-based information on SAP and CR in pediatric patients due to it being a newer material and technique. In vitro studies and clinical trials have shown better remineralization with CR than fluoride varnish, which has led to an interest in utilizing this treatment modality for children with ICL.1,6,8,11 This publication aims to highlight the indications, clinical steps, limitations and outcomes of CR for the management of ICL in 2 adolescent patients.
A 15-year-old female presented for a routine recall appointment. She had been suffering from dry eyes for a few months. Her physician evaluated her for Sjogren’s syndrome (SS) because her mother had SS. Evaluations confirmed the presence of antinuclear antibodies but a diagnosis of SS was not established unequivocally due to the patient not meeting all the clinical diagnostic parameters.
Dental examination revealed good oral hygiene and periodontal health.
Facial ICL were noted on the maxillary central incisors (Figure 2). Due to the possibility of SS, risk of xerostomia) and the clinical presence of ICL, CR was presented to the patient and her parent as a preventive option. Following assent from the patient and informed consent from the parent, oral prophylaxis was performed with rubber cup and dental prophy paste. CR was applied to the facial surfaces of the maxillary central incisors according to the steps listed in Table 1, except for the use of sodium hypochlorite. A cheek retractor was used for isolation. The steps in the application of CR for this patient are shown in Figure 3. The patient returned


for her scheduled 6-month periodic dental examination. Her medical history remained unchanged. Dental examination showed good oral hygiene without progression or clinical changes in the extent of ICL. The lesions at the 6-month recall appointment are shown in Figure 4. Esthetic changes in ICL were not noted during the visual examination at the recall appointment.

A 14-year-old male presented for a routine dental recall appointment. He had recently completed orthodontic treatment. He presented with cervical decalcifications on multiple teeth, gingivitis and edematous gingival margins. ICL on the maxillary right premolars and maxillary left central incisor were most prominent (Figure 5). The option of guided remineralization with CR for the 3 teeth was presented to the patient and the parent. Following assent from the patient and informed consent from the parent, oral prophylaxis was performed with rubber cup and dental prophy paste. CR was applied to the facial surface of the maxillary left central incisor and buccal surfaces of the maxillary right premolars according to the steps listed in Table 1, except for the use of sodium hypochlorite. DryShield was used for isolation. The application steps for this patient are shown in Figure 6. When the patient returned for his scheduled 6-month periodic dental examination, the ICL remained stable without progression or cavitation (Figure 7). Esthetic improvement was noted on the buccal surfaces of the maxillary premolars.
Both patients were provided with a prescription for 1.1% sodium fluoride toothpaste for use at home and counseling for dietary and oral hygiene practices for caries prevention. They tolerated the procedure well without side effects or adverse events.



ICL on permanent teeth in adolescent patients are important to recognize and manage. The clinical focus on noninvasive methods to facilitate remineralization aims to prevent the breakdown of enamel and the subsequent need for restorations.8,12 Limited clinical trials have evaluated the efficacy of SAP on ICL.11 A recent systematic review identified 6 clinical trials that could be included in the analysis with a follow-up duration of 6-12 months in the included trials.9 The paucity of clinical trials and shortterm follow-up data is expected for a newly available material. Curodont™ received approval from the US Food
and Drug Administration in 2019 for the treatment of white spots.13 The ADA approved the D2991 CDT code for the application of hydroxyapatite regeneration medicament in January 2024, which can be used for teeth treated with SAP or CR.14
These case reports highlight clinical scenarios in pediatric dentistry where the use of a material such as CR may be considered, along with an assessment of the limitations of the material.
Identification of at-risk patients and at-risk tooth surfaces by the dentist is the preliminary step. Chronic health conditions, medications, dietary habits, inadequate oral hygiene measures, and dental appliances contribute to the risk
for 20 seconds, lesions after etching,
for ICL.4 The clinician and the patient/ guardian should be collaboratively vested in the noninvasive management of the diagnosed ICL. It is the author’s opinion that the autonomy of the adolescent should be respected and engaged to promote active participation from the patients in preventive care. This is the reason for soliciting assent from the minor prior to the use of CR.
The benefits of CR include ease of use, noninvasiveness, short chair time (5 minutes of CR contact time) and minimal post-treatment restrictions. It is nonstaining and does not adversely impact esthetics. However, the material has some limitations. The treated teeth need to be kept dry for 5

minutes to facilitate absorption of the material into ICL. Hence, it cannot be used for uncooperative patients who may not be able to hold still or keep their mouths open for 5 minutes. Another important limitation is that using CR does not significantly improve the esthetics of ICL. This is important for the patient and the guardian to understand so that realistic expectations are established. However, CR is a valuable, noninvasive option for cervical ICL in premolars and molars, where esthetics are not critical. An in vitro evaluation of CR in artificially created ICL showed improvement in the color of the treated surfaces.15 However, the current author noticed clinical improvement in esthetics of only 2 of the 5 teeth treated with CR.
An inherent limitation in weighing scientific evidence for clinical use of SAP is the inability to provide evidence of in vivo remineralization within the body of ICL in clinical trials. Evaluations of ICL in patients are typically performed by visual and tactile assessment and standardized photographs.4 While these methods are easy, they are not quantitative for laboratory analysis of optical changes, microdensity, and hardness.4 Hence, data from in vitro studies and clinical trials must be collated to determine the best utilization in clinical practice. The clinical outcome of ICL treated by SAP can be difficult to measure objectively. Standardized photographs can help clinicians assess lesion progression and optical changes.8 An in vitro study utilized DIAGNOdent 2095 and QLF-D Biluminator, SEM-EDS (KaVo Dental, Charlotte, NC, USA) to study remineralization and optical changes in artificial ICL treated with SAP.2 However, these methodologies may not be clinically applicable due to the cost of the equipment and their unavailability in pediatric practices.
The case reports highlight the benefit of treatment of ICL with CR in 2 high-risk patients. The clinical outcome of this noninvasive approach after 6 months was a lack of clinical progression of the treated lesions. Two of the 5 treated teeth showed clinically observable optical improvement. There were no side effects or adverse events related to the treatment.
The author is thankful to Grand Parkway Pediatric Dental for the ability to provide care for these patients. The author is grateful to Anoushka Debnath for assistance with editing and graphics.
References
1. Nath SJC, Fu Y, Li KC, Loho T, Loch C, Ekambaram M. A comparison of the enamel remineralisation potential of self-assembling peptides. Int Dent J. 2024;74(2):187–194. doi: 10.1016/j. identj.2023.07.003.
2. Firinciogullar EC, Urdinc AM. Effects of fluoride-containing biomimetic agents on remineralization and color change of enamel white spot lesions: An in vitro study. Oper Dent. 2025;50(1):78–92. doi: 10.2341/24-048.
3. Torres PJ, Phan HT, Bojorquez AK, Garcia-Godoy F, Pinzon LM. Minimally invasive techniques used for caries management in dentistry. A review. J Clin Pediatr Dent. 2021;45(4):224–232. doi: 10.17796/1053-4625-45.4.2.
4. Rathore K, Patnana AK, Chugh VK, Chugh A, Kumar P. Self-assembling peptides for managing white spot lesions: A systematic review and meta-analysis. Eur Arch Paediatr Dent. 2023;24(5):519–531. doi: 10.1007/s40368-023-00821-2.
5. Young DA, Novy BB, Zeller GG, et al. The american dental association caries classification system for clinical practice: A report of the american dental association council on scientific affairs. J Am Dent Assoc. 2015;146(2):79–86. doi: 10.1016/j.adaj.2014.11.018.
6. Kobeissi R, Badr SB, Osman E. Effectiveness of self-assembling peptide P(11)-4 compared to tricalcium phosphate fluoride varnish in remineralization of white spot lesions: A clinical
randomized trial. Int J Clin Pediatr Dent. 2020;13(5):451–456. doi: 10.5005/jpjournals-10005-1804.
7. Schmidlin P, Zobrist K, Attin T, Wegehaupt F. In vitro re-hardening of artificial enamel caries lesions using enamel matrix proteins or self-assembling peptides. J Appl Oral Sci. 2016;24(1):31–36. doi: 10.1590/1678775720150352.
8. Broseler F, Tietmann C, Bommer C, Drechsel T, Heinzel-Gutenbrunner M, Jepsen S. Randomised clinical trial investigating self-assembling peptide P(11)4 in the treatment of early caries. Clin Oral Investig. 2020;24(1):123–132. doi: 10.1007/ s00784-019-02901-4.
9. Keeper JH, Kibbe LJ, Thakkar-Samtani M, et al. Systematic review and meta-analysis on the effect of self-assembling peptide P(11)4 on arrest, cavitation, and progression of initial caries lesions. J Am Dent Assoc. 2023;154(7):580–591.e11. doi: 10.1016/j. adaj.2023.03.014.
10. Kind L, Stevanovic S, Wuttig S, et al. Biomimetic remineralization of carious lesions by self-assembling peptide. J Dent Res. 2017;96(7):790–797. doi: 10.1177/0022034517698419.
11. Shaalan O, Fawzy El-Sayed K, Abouauf E. Evaluation of the remineralization potential of self-assembling peptide P11-4 with fluoride compared to fluoride varnish in the management of incipient carious lesions: A randomized controlled clinical trial. Clin Oral Investig. 2024;28(8):438–z. doi: 10.1007/s00784-024-05822-z.
12. Innes NPT, Schwendicke F. Restorative thresholds for carious lesions: Systematic review and meta-analysis. J Dent Res. 2017;96(5):501–508. doi: 10.1177/0022034517693605.
13. US Food and Drug Administration. FDA report. https://fda.report/ DailyMed/76207c03-eb76-4c28-8645ecc13f4aa852. Updated 2025.
14. Carequest Institute for Oral Health. Minimally invasive care in oral health dental and medical billing codes. https://www.carequest.org/topics/ minimally-invasive-care/dental-andmedical-billing-codes-minimallyinvasive-care#:~:text=Dental%20 Codes%20(CDT),Application%20of%20 hydroxyapatite%20regeneration%20 medicament. Updated 2025.
15. Albar N, Basheer SN, Moaleem MMA, et al. Color masking ability of guided enamel regeneration with a novel self-assembling peptide and resin infiltration on artificial enamel lesions under various challenges: An in vitro spectrophotometric analysis. Biomimetics (Basel). 2024;9(12):764. doi: 10.3390/biomimetics9120764. doi: 10.3390/biomimetics9120764.
HUGE OPPORTUNITY FOR GROWTH: GP in a well-located professional building with 3 ops in good condition. Currently paper-based and non-digital, operating 4 doctor days per week. Growth potential by adding a hygienist, expanding services, marketing, or extending hours. Over 1,200 active patients (10% FFS, 50% PPO, 40% Medicaid). Ideal for a satellite office or first practice. Call AFTCO today! Opportunity ID: TX-02453
Luis O. Regueira, Sr., D.M.D.
Zayd M. Hashmi, D.M.D.
Asra S. Hashmi, D.D.S. and has acquired the practice of has acquired the practice of Frisco, Texas Cleveland, Texas We are pleased to have assisted in these transitions. Benjamin C. Edmunds, D.D.S.
FANTASTIC LOCATION: GP is in a bustling retail center with great visibility. The office is equipped with 3 ops, digital X-ray, and paperless patient charts. The practice has over 1,200 active patients that are a mixture of 20% FFS and 80% PPO. The seller refers out most specialties, and the practice operates on 3.5 doctor days and 4 hygiene days, leaving ample room for growth. Don’t wait, call AFTCO today! Opportunity ID: TX-02459
Alexandre R. Canevet, D.D.S.
GREAT LOCATION: Thriving GP generating $841K annually with 8 doctor days and 4 hygiene days per week. Serves 1,400+ active FFS/PPO patients with 25+ new patients monthly. Located in a busy medical complex, the 1,320 sq. ft. office has 5 ops and is fully digital. Growth potential by keeping referrals in-house. Don’t miss out—call AFTCO today!
Opportunity ID: TX-02493
EXCELLANT RETAIL LOCATION: GP that is highly visible in a retail center. This practice operates with the owner and 1 PT associate, is open 7 days a week and provides regular dental care as well as emergency services. The practice has over 1,750 active patients who are ~20% FFS, ~70% PPO, and less than 10% Medicaid. The office opened just 6+ years ago, has 4 ops fully equipped, and is in excellent condition. This is a great opportunity for growth by capitalizing on the existing patient base and expanding services. Don’t wait, call AFTCO today! Opportunity ID: TX-02419
Go to our website or call to request information on other available practice opportunities!

J. Hanna JD Former General Counsel, Texas Dental Association

Guest Editor Rade D. Paravina, DDS, MS, PhD
Brian P. LeSage, DDS, Oded Bahat, BDS, MSD
Read this article in full at: https://onlinelibrary.wiley.com/doi/epdf/10.1111/jerd.13417
Objective
To briefly review and summarize significant clinical, functional, esthetic, and periodontal characteristics that are essential to multidisciplinary case analysis and treatment planning for single-tooth replacement in the esthetic zone with an implant-supported prosthesis.
A patient’s preoperative condition (e.g., bone quality/quantity, gingival biotype, macro-/ microesthetic features) significantly affects the stability, function, and esthetics of the anticipated implant-supported prostheses and, therefore, must be comprehensively evaluated after acquiring thorough diagnostic data. Understanding the immediate and long-term implications of diagnostic findings before undertaking any procedures enables critical assessment and step-by-step execution of the most appropriate interventions, surgeries, and prosthetic designs for greater esthetic and functional treatment predictability.
Collaborative and interdisciplinary treatment planning among the restorative dentist, implant surgeon, and laboratory ceramist is the foundation for achieving successful outcomes when undertaking a single-tooth replacement with an implant-supported prosthesis in the esthetic zone. It enables the identification and skilled execution of specific procedures, selection and sequencing of dental implant-related surgeries and temporization techniques, and design and delivery of the ideal implant-supported prosthesis to satisfy the patient’s and team’s treatment objectives.

Preoperative smile view of a female patient presenting with a high smile line that would influence pink/white esthetics, failing all-ceramic crown on her maxillary right central incisor, and a fracture line in her maxillary left central incisor due to initial trauma. Canines exhibit moderate wear faceting and visual tension.

Posttreatment smile view of the definitive, implant-supported restoration that achieved the patient’s esthetic expectations.
Critically informed differential treatment planning through multidisciplinary collaboration enhances treatment predictability, esthetic outcomes, and functional success while simultaneously reducing potential immediate and delayed complications, thereby helping to ensure the feasibility of achieving anticipated results.
Provided by: PERKS


Here’s Why This Is a Problem— And Why You and Your Patients Will Be Happier When You ePrescribe
By Robert McDermott President & CEO, iCoreConnect
Even with the switch to EHRs and digital transformation over the last decade, some providers still rely on paper prescriptions. Are you one of them? If so, this article will highlight why using paper prescriptions is not a best practice and how ePrescribing can significantly help you and your patients.
Quickly, let’s add the backdrop of patient experience—which encompasses every interaction a patient has with your practice—because ePrescribing is germane to it.
Why is providing a positive patient experience so important?
It leads to better health outcomes. This is foremost. A positive patient experience encourages patients to actively participate in their care. It encourages engagement with patient education efforts, following treatment plans, and adhering to medication regimens.
It influences patient satisfaction and loyalty. Patients who feel valued and supported are likely to recommend the practice to others and return for future needs. Word-of-mouth endorsements can enhance a practice’s reputation, which attracts new patients and bolsters community trust.
Patient experience is significantly impacted by the effectiveness and efficiency of care delivery. Your practices processes—including the way you create prescriptions— impact your patients.
What’s wrong with writing paper prescriptions?
When you make prescriptions on paper, you are less inefficient, increase the likelihood of mistakes, and are likely inconveniencing your patients.
• Illegible handwriting can result in medical errors. At best, it may require time on the phone to obtain clarification.
• Patients may have privacy and security concerns regarding their medical information.
• Traveling to a dental appointment and then to a pharmacy is inconvenient for most people. It’s also time consuming to wait at a provider’s office and pharmacy.
• Patients could easily misplace or lose their paper prescription, the result could be delayed or missed medication refills.
• Travel to the office or pharmacy—and possibly lost time at work—may require expenses or lead to lost wages.
• Getting to a dentist office or pharmacy to obtain a paper prescription may present challenges to those with limited mobility.
Investing in ePrescribing software can significantly improve patient experience.
• Patients will enjoy the convenience of not having to drop off and pick up paper prescriptions at the pharmacy.
• Patients can more easily access their prescriptions and obtain refills because ePrescriptions are stored in a pharmacy’s database. Pharmacists can also keep track of their prescription interactions.
• Your patients will have shorter wait times at the pharmacy because pharmacists can start preparing medication as soon as they receive it.
• The risk of adverse drug events or contraindications are minimized because ePrescriptions can include checks for drug interactions and allergies.
• There’s no risk of unwanted eyes on prescriptions because they’re transmitted directly.
Prescribing electronically streamlines the prescribing process and increases accuracy.
• ePrescription software is tailored to preferences of each dentist, so prescriptions are a quick process. Prescribers can use ePrescription software to customize medication regimens based on their preferences; and factors such as allergies, drug interactions, and patient preferences. And don’t forget that ePrescribing enables providers to send prescriptions directly to pharmacies electronically.
• A simplified prescription process contributes to improved medication adherence, which helps patients stay on track with treatment plans.
• PMP/PDMP integration improves safety and saves lives. Efficiency and accuracy are paramount when it comes to checking prescription data. Having a single source of information regarding controlled substances is a powerful tool.
• Illegible handwriting, inaccurate information, and abbreviations—some of the primary causes of prescription errors—can be avoided through ePrescribing.
In short, ePrescribing improves patient experience, the accuracy of prescriptions, and efficiency in creating prescriptions.
iCoreRx cloud ePrescribing software improves the efficiency and safety of prescription management while significantly enhancing patient satisfaction and trust; and TDA members receive substantial discounts on iCoreRx and other endorsed services from iCoreConnect. Learn more at tdaperks.com (Compliance & Supplies) or call (888) 810-7706.

Designed for dentists, with dentists, the new ADA Member App is here and ready to put the resources you need in the palm of your hand.

• Chat 1:1 or with your network
• Newsfeed customized to your interests
• Digital wallet to store your important documents
• Stream the new “Dental Sound Bites” podcast
Tap into possibility at ADA.org/App









A 34-year-old male presented to the Baylor University Medical Clinic on January 13, 2025, with a chief complaint of gingival swelling and tooth mobility in the right maxillary region. The clinical and radiographic assessment revealed a suspicious lesion warranting further investigation. Radiographically, the lesion presents as a mixed radiolucent-radiopaque area, often containing variable-sized calcified components. The borders may range from well-circumscribed to ill-defined, and the internal structure can appear unilocular or multilocular depending on the stage and nature of the lesion. In our case, the lesion was located in the right posterior maxilla, extending superiorly into the right maxillary sinus. It demonstrated a mixed radiolucentradiopaque internal pattern, characterized by patchy and coarse internal calcifications, some of which appear irregular and nodular, consistent with Liesegang ring-type mineralization. The lesion was expansile, showing outward displacement and thinning of the cortical plates. There was destruction of the floor and walls of the right maxillary sinus, indicating aggressive behavior. There was involvement of adjacent teeth, with at least one tooth demonstrating root resorption. An incisional biopsy was performed at the time of the initial presentation. The patient returned after a 4-month interval for definitive surgical management of the lesion.
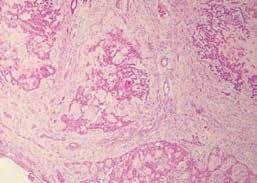
Histopathologic examination revealed a tumor composed of discrete islands, strands, and sheets of polyhedral epithelial cells in a fibrous stroma. Large areas of amorphous, eosinophilic, hyalinized (amyloid-like) extracellular material were also present.
Calcifications were present within the amyloid-like material which fused and formed large, complex masses.
See page 214 for the answer and discussion.

Ashim Raj Shrestha, BDS, MPH, MS Resident, Department of Diagnostic Sciences, Texas A&M University College of Dentistry, Dallas, Texas.

Haiying Zhang, MD Department of Pathology, Baylor Scott and White Health, Dallas, Texas.

Ajay Shakya, BDS, MDS, PhD Intern, Maxradpath, Georgetown, Texas.

Karan Dharia, BDS, MS Director, Maxradpath, Georgetown, Texas.

Madhu Shrestha, BDS, MDS, MS, PhD Department of Diagnostic Sciences, Texas A&M University College of Dentistry, Dallas, Texas. (Corresponding author)
diagnosis and management—from page 213
odontogenic
Discussion
Based on the clinical and radiographic findings, the top 3 differential diagnoses for this case included calcifying odontogenic cyst (COC), desmoplastic ameloblastoma (DA), cemento-ossifying fibroma (COF), and calcifying epithelial odontogenic tumor (CEOT).
Originally described by Gorlin in 1962, the calcifying odontogenic cyst (COC) is a rare jaw lesion characterized by an ameloblastoma-like epithelial lining with calcifications and ghost cells, which are also seen in a dentinogenic ghost cell tumor(de Arruda et al., 2018). While COC can occur throughout the jaws, it shows a clear predilection for the anterior regions (Kler et al., 2009a). COC affects both the maxilla and mandible with equal predilection for males and females (Moradzadeh Khiavi et al., 2021). The lesions are most often seen in the second decade of life (Li & Yu, 2003). Mandibular COC lesions often extend across the midline,

unlike their maxillary counterparts which typically remain confined (White & Pharoah, 2005). Radiographically, most of these lesions present as well-defined, unilocular radiolucencies with a sclerotic margin, though a small percentage (around 5–13%) may appear multilocular. They may also show considerable variation ranging from completely radiolucent lesions to mixed radiolucentradiopaque patterns with scattered, irregular calcifications, and in some cases, they may form dense, cloud-like opacities (Altini & Farman, 1975). Histologically, COC show a cystic epithelial lining with basal cells that are cuboidal to columnar, often resembling ameloblasts, while the overlying suprabasal layers exhibit a stellate reticulum-like appearance, closely mirroring the structure of the enamel organ (Kler et al., 2009b). A microscopic hallmark feature of COC is the presence of eosinophilic, anucleate ghost cells. Over time, these ghost cells often undergo calcification, gradually losing their cellular detail and giving rise to discrete areas of calcified keratin within the lesion (Irani & Foroughi, 2017). For central cystic COC lesions, enucleation is generally the treatment of choice, though rare recurrences have been reported. In contrast, neoplastic variants warrant en bloc resection along with close, long-term follow-up to monitor for recurrence or progression (Buchner et al., 1990).
Desmoplastic ameloblastoma (DA) is an uncommon subtype of ameloblastoma, distinguished by its dense, collagen-rich stroma. It most often presents in patients in the fourth to fifth decades, without any significant gender predilection
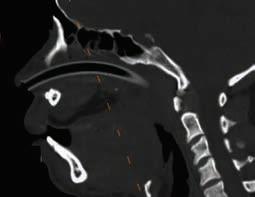
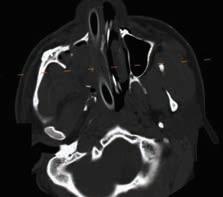
Figure 1A-C: Above are axial, sagittal and coronal sections of a mdeical CT without contrast depicting a lesion with an isodensity of soft tissue within the right maxilla. The lesion extends into, and involves most of, the right maxillary sinus as seen on the axial and coronal sections with focal loss of the posterolateral wall of the sinus (1A and 1C). There is radiographic loss of adjacent alveolar bone and extension of the lesion into the palate as seen on the sagittal section (1B).
(Beckley et al., 2002). This condition typically manifests in the anterior region of the jaws, with no significant difference in prevalence between the maxilla and mandible. The primary clinical feature is painless swelling, which often results in buccal expansion and displacement of adjacent teeth (Kaffe et al., 1993). The desmoplastic variant of ameloblastoma most commonly presents radiographically as a multilocular radiolucency. However, when associated with increased sclerosis, the lesion often exhibits a mixed radiolucent-radiopaque pattern, which can closely resemble the appearance of a fibro-osseous lesion (Effiom & Odukoya, 2011). Histologically, desmoplastic ameloblastoma is characterized by a densely collagenized stroma, referred to as desmoplasia, within which scattered, irregularly shaped islands and strands of odontogenic epithelium are embedded (Manikandan et al., 2023). Due to its infiltrative nature, desmoplastic ameloblastoma is best managed by resection with wide margins, which significantly lowers recurrence rates compared to conservative approaches like enucleation or curettage (Sharma et al., 2021).
Cemento-ossifying fibroma (COF) is an uncommon benign odontogenic neoplasm believed to arise from the periodontal ligament, characterized histologically by a fibro-cellular stroma interspersed with varying amounts of mineralized material resembling bone and/or cementum (Kaur et al., 2021). Clinically, cemento-ossifying fibroma presents as a slowly enlarging intraosseous lesion, typically affecting the jaws of young to middle-aged adults, with a distinct female predilection (More et al., 2011). Radiographically, the appearance of cemento-ossifying fibroma is largely influenced by the degree of mineralization. In its early stages, it is often presented as a well-defined unilocular or multilocular
radiolucency. As the lesion matures, progressive deposition of mineralized tissue results in a mixed radiolucentradiopaque pattern. A characteristic feature is the presence of a well-demarcated border with a sclerotic rim, indicative of a peripheral reaction in the surrounding bone (Waldron & Giansanti, 1973). Histologically, cemento-ossifying fibroma reveals a heterogeneous admixture of mineralized components such as woven bone, lamellar bone, and cementum-like calcifications embedded within a background of fibrovascular connective tissue, often arranged in a disorganized pattern (Aravindan et al., 2023). Management of cemento-ossifying fibroma typically involves enucleation for smaller lesions, while larger lesions may require bloc resection with subsequent bony reconstruction. Given its radio-resistant nature and potential for post-radiation complications, radiotherapy is generally not recommended. The overall prognosis is fair; however, maxillary lesions tend to show a higher recurrence rate than mandibular ones, largely due to their larger size at diagnosis and the anatomical challenges associated with complete surgical excision (White & Pharoah, 2005b).
Calcifying epithelial odontogenic tumor (CEOT) is an uncommon benign tumor of odontogenic origin, representing roughly 1% of all odontogenic tumors (Buyukkurt et al., 2014). It was first described by Pindborg and is therefore also known as the “Pindborg tumor” (Baral et al., 2020). There are differing opinions regarding the origin of CEOT. Some pathologists suggest that it arises from the stratum intermedium of the enamel organ during tooth development, while others believe it may originate from remnants of the primitive dental lamina present in the early stages of odontogenesis (Maria et al., 2010). CEOT can occur across a broad age range but is most
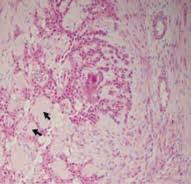
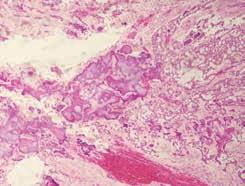
2A. Low power view (4X) of the photomicrograph revealed tumor mass composed of closely packed sheets of polyhedral cells. The tumor cells had a well-defined border with eosinophilic cytoplasm and central round nucleus. 2B. Medium power view (10x) showing the presence of islands and sheets of polyhedral cells and focal areas of homogenous amorphous pink matrix representing amyloid material (represented by black arrows) are seen with polyhedral epithelial strands. 2C. Multiple concentric calcifications that are fused as large masses are seen.
often seen in individuals between their 30s and 60s with equal predilection for male and female (Angadi & Rekha, 2011). Approximately 52% of CEOT cases are associated with impacted or unerupted teeth, or odontomas and mostly involves the mandibular molar region (Deboni et al., 2006). In the present case, the lesion was located in the right posterior maxilla.
Radiographically, the lesion presents as a mixed radiolucentradiopaque area, often containing variable-sized calcified components. The borders may range from well-circumscribed to ill-defined, and the internal structure can appear unilocular or multilocular depending on the stage and nature of the lesion. In our case, the lesion was located in the right posterior maxilla, extending superiorly into the right maxillary sinus. It demonstrated a mixed radiolucent-radiopaque internal pattern, characterized by patchy and coarse internal calcifications, some of which appear irregular and nodular, consistent with Liesegang ring-type mineralization. The lesion was expansile, showing outward displacement and thinning of the cortical plates. There was destruction of the floor and walls of the right maxillary sinus, indicating aggressive behavior. There was the involvement of adjacent teeth, with at least one tooth demonstrating root resorption.
In the final interpretation, although varying differential diagnoses such as calcifying odontogenic cyst, desmoplastic ameloblastoma, and cemento-ossifying fibroma were initially considered based on the clinical presentation and radiographic features, the histopathologic features in our case revealed a final diagnosis of calcifying epithelial odontogenic tumor (CEOT). The surgical management of CEOT may range from conservative enucleation to marginal or segmental resection, with partial resection reserved for lesions demonstrating extensive involvement or aggressive behavior (Sedghizadeh et al., 2007). Given the indolent growth pattern of this tumor, a long-term follow-up period of 5 to 10 years is advised to monitor for potential recurrence (Patiño et al., 2005). In the present case, we acknowledge the importance of extended follow-up to ensure complete resolution and to monitor for any potential recurrence of the lesion. Although rare in occurrence, CEOT must be included in the differential diagnosis of a mixed radiolucent-radiopaque lesion in the jaw with some aggressive changes. Accurate diagnosis of CEOT relies on a thorough correlation of clinical, radiographic, and histopathologic features. Appropriate surgical intervention and long-term follow-up is essential to minimize the risk of recurrence and ensure an optimal patient outcome.
References:
Altini, M., & Farman, A. G. (1975). The calcifying odontogenic cyst. Oral Surgery, Oral Medicine, Oral Pathology, 40(6), 751–759. https://doi.org/10.1016/0030-4220(75)90444-2. Angadi, P. V., & Rekha, K. (2011). Calcifying Epithelial Odontogenic Tumor (Pindborg Tumor). Head and Neck Pathology, 5(2), 137–139. https://doi.org/10.1007/s12105-011-0250-6. Aravindan, V., Kumar, S. P., Murugan P, S., Krishnan, M., & Sneha, A. (2023). A Rare Case of Cemento-Ossifying Fibroma: A Case Report. Cureus. https://doi.org/10.7759/cureus.38685. Baral, R., Bajracharya, D., Ojha, B., & Karn, G. (2020). Calcifying Epithelial Odontogenic Tumor: A Case Report. Journal of Nepal Medical Association, 58(223), 174–177. https://doi. org/10.31729/jnma.4842.
Beckley, M. L., Farhood, V., Helfend, L. K., & Alijanian, A. (2002). Desmoplastic ameloblastoma of the mandible: a case report and review of the literature. Journal of Oral and Maxillofacial Surgery : Official Journal of the American Association of Oral and Maxillofacial Surgeons, 60(2), 194–198. https://doi.org/10.1053/joms.2002.29822. Buchner, A., Merrell, P. W., Carpenter, W. M., & Leider, A. S. (1990). Central (intraosseous) calcifying odontogenic cyst. International Journal of Oral and Maxillofacial Surgery, 19(5), 260–262. https://doi.org/10.1016/S0901-5027(05)80414-X.
de Arruda, J. A. A., Schuch, L. F., Abreu, L. G., Silva, L. V. O., Monteiro, J. L. G., Pinho, R. F., Silva, L. P., de Sousa, S. C., de Andrade, B. A. B., Romañach, M. J., de QC Lourenço, S., Batista, A. C., de Mendonça, E. F., Martins, M. D., Rados, P. V, Rivero, E. R., de Souza, L. B., Pinheiro, M. das G., Gomes, A. P. N., Mesquita, R. A. (2018). A multicentre study of 268 cases of calcifying odontogenic cysts and a literature review. Oral Diseases, 24(7), 1282–1293. https://doi.org/10.1111/odi.12906.
Deboni, M. C. Z., Naclério-Homem, M. da G., Pinto Junior, D. S., Traina, A. A., & Cavalcanti, M. G. P. (2006). Clinical, radiological and histological features of calcifying epithelial odontogenic tumor: case report. Brazilian Dental Journal, 17(2), 171–174. https://doi. org/10.1590/S0103-64402006000200017.
Effiom, O. A., & Odukoya, O. (2011). Desmoplastic ameloblastoma: analysis of 17 Nigerian cases. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontology, 111(1), e27–e31. https://doi.org/10.1016/j.tripleo.2010.06.021.
Irani, S., & Foroughi, F. (2017). Histologic Variants of Calcifying Odontogenic Cyst: A Study of 52 Cases. The Journal of Contemporary Dental Practice, 18(8), 688–694. https://doi. org/10.5005/jp-journals-10024-2108.
Kaffe, I., Buchner, A., & Taicher, S. (1993). Radiologic features of desmoplastic variant of ameloblastoma. Oral Surgery, Oral Medicine, Oral Pathology, 76(4), 525–529. https://doi. org/10.1016/0030-4220(93)90023-W.
Kaur, T., Dhawan, A., Bhullar, R. S., & Gupta, S. (2021). Cemento-Ossifying Fibroma in Maxillofacial Region: A Series of 16 Cases. Journal of Maxillofacial and Oral Surgery, 20(2), 240–245. https://doi.org/10.1007/s12663-019-01304-y.
Kler, S., Palaskar, S., Shetty, V., & Bhushan, A. (2009a). Intraosseous calcifying cystic odontogenic tumor. Journal of Oral and Maxillofacial Pathology, 13(1), 27. https://doi. org/10.4103/0973-029X.48753.
Kler, S., Palaskar, S., Shetty, V., & Bhushan, A. (2009b). Intraosseous calcifying cystic odontogenic tumor. Journal of Oral and Maxillofacial Pathology, 13(1), 27. https://doi. org/10.4103/0973-029X.48753.
Li, T.-J., & Yu, S.-F. (2003). Clinicopathologic Spectrum of the So-Called Calcifying Odontogenic Cysts. The American Journal of Surgical Pathology, 27(3), 372–384. https://doi. org/10.1097/00000478-200303000-00011.
Manikandan, S., Vijayakumar, G., Parthiban, B., & Kumarasamy, B. (2023). Desmoplastic Ameloblastoma—A Case Report. Journal of Pharmacy and Bioallied Sciences, 15(Suppl 1), S814–S816. https://doi.org/10.4103/jpbs.jpbs_44_23.
Maria, A., Sharma, Y., & Malik, M. (2010). Calcifying Epithelial Odontogenic Tumour: A Case Report. Journal of Maxillofacial and Oral Surgery, 9(3), 302–306. https://doi.org/10.1007/ s12663-010-0068-x.
Moradzadeh Khiavi, M., Mahdavi, N., & Awudu, A. (2021). Developing odontoma arising from calcifying odontogenic cyst: A case report. Clinical Case Reports, 9(11). https://doi. org/10.1002/ccr3.5011.
More, C., Thakkar, K., & Asrani, M. (2011). Cemento-ossifying fibroma. Indian Journal of Dental Research, 22(2), 352. https://doi.org/10.4103/0970-9290.84296.
Patiño, B., Fernández-Alba, J., Garcia-Rozado, A., Martin, R., López-Cedrún, J. L., & Sanromán, B. (2005). Calcifying Epithelial Odontogenic (Pindborg) Tumor: A Series of 4 Distinctive Cases and a Review of the Literature. Journal of Oral and Maxillofacial Surgery, 63(9), 1361–1368. https://doi.org/10.1016/j.joms.2005.05.302.
Sedghizadeh, P. P., Wong, D., Shuler, C. F., Linz, V., Kalmar, J. R., & Allen, C. M. (2007). Multifocal calcifying epithelial odontogenic tumor. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontology, 104(2), e30–e34. https://doi.org/10.1016/j. tripleo.2006.06.050.
Sharma, A., Ingole, S., Deshpande, M., & Meshram, D. (2021). Retrospective analysis of Desmoplastic Ameloblastoma: Clinical review. Medicina Oral Patología Oral y Cirugia Bucal, e246–e255. https://doi.org/10.4317/medoral.24152.
Waldron, C. A., & Giansanti, J. S. (1973). Benign fibro-osseous lesions of the jaws: A clinicalradiologic-histologic review of sixty-five cases. Oral Surgery, Oral Medicine, Oral Pathology, 35(3), 340–350. https://doi.org/10.1016/0030-4220(73)90072-8.
White SC, Pharoah MJ. Cysts of the jaws. In: White SC, Pharoah MJ, editors. Oral Radiology: Principles and Interpretation. 5th ed. Missouri: Mosby-Elsevier; 2005. pp. 399–400.
Eugene M. Allen Sr
Aubrey
11/30/32–11/7/23
Good Fellow: 1991
Life: 1997 • Fifty Year: 2016
Russell S. Barnett Jr
Austin 1/5/39–7/4/23
Good Fellow: 1989
Life: 2004 • Fifty Year: 2014
Gene Norman Barry Nome
8/24/43–3/30/25
Good Fellow: 2000 • Life: 2008
Jerry D. Black
Brady
4/12/36–12/27/23
Good Fellow: 2000
Life: 2001 • Fifty Year: 2016
Ernest Dick Butler
Navasota
1/24/39–8/27/20
Good Fellow: 1990
Life: 2004 • Fifty Year: 2015
Charles E. Cavin
Garland 10/30/25–11/27/20
Good Fellow: 1982
Life: 1990 • Fifty Year: 2006
Charles Rogers Clark Flatonia
2/7/32–10/3/22
Life: 1997 • Fifty Year: 2011
Larry A. Cooper
Dallas 12/4/31–8/6/24
Good Fellow: 1984
Life: 1996 • Fifty Year: 2010
Jerry S. Dickson
Dallas 6/18/37–5/24/24
Good Fellow: 1988
Life: 2002 • Fifty Year: 2013
Richard Gene Dyck Conroe
8/28/30–10/11/24
Good Fellow: 1988
Life: 1995 • Fifty Year: 2013
Scott Alan Ervin Terrell
5/22/64–5/3/25
Good Fellow: 2014 • Life: 2021
Tommy Wilton Gage Rockwall
10/6/35–5/23/25
Good Fellow: 1994
Life: 2000 • Fifty Year: 2018
Wallace Gerald Haney Lubbock
3/21/21–10/29/24
Good Fellow: 1975
Life: 1986 • Fifty Year: 2000
Marion E. Harrell
Wichita Falls
11/17/41–5/26/25
Good Fellow: 1991
Life: 2006 • Fifty Year: 2016
E. Penn Jackson
San Antonio
10/10/31–11/10/24
Good Fellow: 1989
Life: 1996 • Fifty Year: 2014
Millard Julian Kimery Sr Abilene
3/30/32–5/3/25
Life: 1998 • Fifty Year: 2018
Jose A. Lomba
San Antonio
2/4/37–1/24/24
Life: 2010
Robert Burnard Moseley
Paris 6/26/49–3/26/18
Good Fellow: 1999
Life: 2014
Robert Franklin Pickard Sr
Groves 12/22/26–11/21/24
Good Fellow: 1977
Life: 1991 • Fifty Year: 2003
Robert McLain Reed Hondo 1/23/32–4/25/25
Good Fellow: 1988
Life: 1997 • Fifty Year: 2013
Ollie Bob Rominger Kerrville 12/20/29–8/14/23
Good Fellow: 1987 Life: 1993 • Fifty Year: 2012
Corinne R. Scalzitti
Austin 7/14/50–5/20/25 Life: 2015
Fredrick Irwin Silverman
Asheville, NC 3/11/46–8/1/22 Life: 2011
Andrew Henry Smith III
Mission 1/11/54–5/27/25 Life: 2019
Robert C. Sproull
Boerne 11/5/20–4/8/25
Life: 1986 • Fifty Year: 2006
James Pryor Stanley
Atlanta 10/25/29–6/6/24
Good Fellow: 1992
Life: 1997 • Fifty Year: 2017
John Wellington Truitt Jr
Gainesville 6/15/43–9/8/24
Good Fellow: 1994 • Life: 2008 Fifty Year: 2018
Roger Martin Weed
San Antonio 2/26/43–4/29/22
Good Fellow: 1998 • Life: 2008
DEADLINE
Copy text is due the 20th of the month, 2 months prior to publication (ie, January issue has a due date of November 20.)
MONTHLY RATES
PRINT: First 30 words—$60 for ADA/TDA members and $100 for non-members. $0.10 each additional word.
ONLINE: $40 per month (no word limit). Online ads are circulated on the 1st business day of each month, however an ad can be placed within 24 business hours for an additional fee of $60.
SUBMISSION
Ads must be submitted, and are only accepted, via www.tda.org/MemberResources/TDA-Classified-Ads-Terms. By official TDA resolution, ads may not quote specific incomes or revenues and must be stated in generic terms (ie “$315,000” should be “low-to-mid-6 figures”). Journal editors reserve the right to edit and/or deny copy.
ALL TEXAS LISTINGS FOR MCLERRAN & ASSOCIATES. AUSTIN (ID #729): Legacy GD office located in the heart of Austin in a high visibility location. Majority PPO patient base, 1,300+ active patients, 15 new patients visit the office per month, and an impeccable reputation online and in the community. The 2,050 sq ft office space contains 6 total operatories (4 equipped), computers throughout, digital x-ray sensors, and intra-oral cameras. They generated revenue of mid-six figures during each of the past 3 years with abundant upside potential.
AUSTIN (ID #743): Legacy GD office located in a suburb just north of Austin. 100% FFS patient base, 1,500+ active patients, and a robust hygiene recall program. The office contains 5 equipped operatories, with computers throughout, digital x-rays, CBCT, and a digital scanner. The practice offers opportunities for additional growth via expanding current marketing activities and keeping additional specialty procedures in-house. DALLAS (ID #728): Well-established GD office in a growing suburb southeast of Dallas. This practice has an impeccable reputation, treats a majority FFS patient base with 1,700+ active patients. The 1,800 sq ft facility features 4 fully equipped
operatories (with a 5th plumbed and ready to be equipped), computers throughout, digital x-ray sensors, digital panoramic x-ray, digital scanner, CAD/CAM milling unit, dental laser, and intra-oral cameras. This turn-key office has strong net cash flow and significant upside potential.
SURGERY (ID #711): Legacy, oral surgery practice in a bustling suburb between Dallas and Fort Worth. A heavily tenured team, large patient base, and a fantastic reputation in the local community. 3,300 sq ft office in an easily accessible medical office park, 4 fully equipped operatories, two plumbed operatories for future expansion, computers throughout, digital x-ray sensors, and a 3D Cone Beam CT. With over 7 figures in 2023 revenue and profit margins trending at 50%, the foundation for a successful future has already been laid out with abundant upside potential available. DALLAS/ FORT WORTH (ID #744): Well-established
GD office located in a growing suburb of DFW. Impeccable reputation in the community, treats a majority PPO patient base with 1,900+ active patients. The 2,500 sq ft, high-visibility retail location contains 5 fully equipped operatories (with the opportunity to expand into a 6th) with computers throughout, digital x-ray sensors, panoramic x-ray, digital scanner, and intra-oral
cameras. EL PASO (ID #733): Fast-growing GD practice in a modern, high visibility location in El Paso. The well-equipped, 2,400 sq ft office has 4 fully equipped operatories with 2 available for future expansion, digital x-ray sensors, a digital pano, digital scanner, laser, intra-oral cameras, and paperless charts. They serve a large, diverse patient base. HOUSTON-SOUTH (ID #682): Established, multi-specialty dental office in a suburb approximately 20 miles south of Houston. Large (4,000 sq ft), easily accessible office condo with 13 equipped operatories, computers throughout, CBCT, and
McLerran & Associates is the largest dental practice brokerage firm in Texas. When it’s time to buy or sell a practice, we’ve got you covered.
PRACTICE SALES
DSO C S
PRACTICE APPRAISALS
Austin 512-900-7989
DFW 214-960-4451
Houston 281-362-1707
San Antonio 210-737-0100
South Texas 361-221-1990
Email: texas@dentaltransitions.com
www.dentaltransitions.com
digital scanner. Massive PPO/FFS patient base (3,000+) with over 50 new patients visiting the office per month. The practice revenue averages over 7 figures annually with strong net cash flow, and there is room for expansion through enhancing the hygiene recall and focusing on standardizing the procedural mix. With approximately 55% of the dentistry being restorative, 25% pediatrics, 10% ortho, and 10% OMS, the office is on a stable foundation with the opportunity to take it in whatever direction you choose.
(ID #724): Legacy GD office located southwest of Houston. Majority PPO patient base, 2,000+ active patients, great online reputation with 100+ reviews. 5 total operatories (4 equipped), with computers in each, digital x-rays, digital Pano, a CAD/CAM milling unit, and a digital scanner. The practice realized revenue of over seven figures in 2024 with robust net cash flow margins (>40%) and a robust hygiene recall program. HOUSTON-CENTRAL (ID #734):
Well-established GD practice in a modern, high visibility location in Houston. Beautiful modern office, 2,600 sq ft, 7 fully-equipped operatories, computers throughout, digital x-ray sensors, 3D cone beam CT, digital scanner, dental laser, intra oral cameras and paperless charts. The practice
treats a FFS/PPO patient base with nearly 2,000 active patients, adds 30 new patients per month, and boasts a near-perfect Google rating across 400+ reviews. HOUSTON-NORTH (ID #737): Well-established, GD office located 30 miles north of Houston. The practice occupies 4,300 sq ft in a standalone building, with only one additional tenant. Four fully-equipped operatories with four additional prepped for future expansion. Well equipped with computers throughout, digital x-ray sensors, a 3D Cone Beam CT, digital scanner, intra oral cameras, and paperless charts. The practice has a robust hygiene recall program and incredible growth potential. SAN ANTONIO-TX
HILL COUNTRY (ID #685): Well-established dental practice and real estate nestled in the hill country north of San Antonio. The office relies mostly on word-of-mouth referrals with limited marketing/advertising activities, has a robust hygiene recall program with over 40% of total office production coming from the hygiene department, and refers out many specialty procedures leading to upside potential for an incoming buyer. The practice saw strong revenue growth in 2023, and the trend continued into 2024. SAN ANTONIO-EAST (ID #716): Legacy GD practice and real estate in a
rural community east of San Antonio. The large office space offers ample room for expansion and features 5 fully equipped operatories with computers in each op, digital x-ray sensors, a digital Pano, a digital scanner, intraoral cameras and paperless charts. This practice has strong profit margins and serves a large, multigeneration 100% FFS patient base. TO REQUEST MORE INFORMATION ON MCLERRAN & ASSOCIATESí LISTINGS: Please register at www.dentaltransitions.com or contact us at 512-900-7989 or info@dentaltransitions. com.
ARLINGTON: Second generation medical space available in Arlington. Looking to establish your dental practice or open an additional location in a thriving retail shopping center? This welllocated medical space is the perfect spot for your healthcare business! Features: high visibility, foot traffic, and 41,500 vehicles per day through the intersection. Situated in a bustling shopping center with established retail stores. Spacious layout designed to accommodate medical offices, dental clinics, or specialized healthcare services. Includes 5 patient rooms with sinks included. Convenient accessibility, ample parking and easy access for patients
and staff. Customizable interiors—tailor the space to suit your practiceís needs. Tenant finish out and financing options. The landlord is willing to assist with a generous tenant finishout allowance. Our lending partner offers 90%+ financing options available for approved healthcare practices. Location: 6201 Matlock Rd, Ste 139, Arlington, a community with strong demand for quality healthcare services. Call Christy Jordan at 817-371-1670; Email cjordan@ realtyappreciation.com.
CENTRAL TEXAS HILL COUNTRY: For sale by owner, thriving fee-for-service general dental practice. Established rural four operatory dental practice for sale in the heart of the beautiful Texas hill country. This all-digital practice with a new pano produces mid-6 figure income with just 2 days per week of operation, offering great room for expansion and growth. The recently renovated real estate which offers a modern, welcoming environment for patients is also for sale. This is a perfect opportunity for a dentist looking to step into a successful, modern and established dental practice with plenty of room to expand. Contact dentalofficesale2024@gmail. com for more information and showings.
HOUSTON: General practice (reference: “Southwest”) in the southwest area practice near a main highway in Houston. Collections in mid-6 figures. Production is growing. Practice in a strip shopping center. The office is 1,475 sq ft with 3 total operatories: 2 for dentistry and one for hygiene. Please let me know if you need anything else from me. A fourth operatory area is plumbed. Contains reception area, dentist office, sterilization area, lab area. Majority of patients are 30 to 65 years old. Practice has operated at this location for over 35 years. Practice sees patients about 16 to 19 days per month. Collection ratio of 99%. Practice is a fee-for-service and PPO practice. Contact Christopher Dunn at 800-930-8017 or Christopher@DDRDental.com.
NEW BRAUNFELS: Dental practice for sale in high traffic area and very visible building. Beautifully renovated recently, with 3 operatories, move-in ready, with 1,250 sq ft. No HMO or DMO. If interested, please email to salemydentalpractice@yahoo.com or leave message on landline, 830-606-4544.
BROWN
Practices for sale in Texas and surrounding states, For more information and current listings please visit our website at www. adstexas.com or call us at 469-222-3200 to speak with Frank or Jeremy.
TYLER: Perfect location for dental office at one of the top intersections in Tyler; Troup & Loop 323. 70,000 cars per day providing unmatched visibility to both highways. Benefits from the tallest (35’) freestanding pole sign and electronic reader board at the intersection and would be impossible to get approved today. Ready for immediate occupancy. Please call Rick, 937-3676656
MIRROR AND EXPLORER, WILL TRAVEL:
Sick leave, maternity leave, vacation, or death, I will cover your general or pediatric practice. Call Robert Zoch, DDS, MAGD, at 512-517-2826 or drzoch@yahoo.com.
