PROGRAMMING
“Programming is problem-seeking, and design is problem-solving.”
These five steps are essential to the programming process. The first four steps do not need to be followed in a consistent order and two or more steps may need to be developed at the same time. Each project is unique, and programming should capture that. The fifth step is addressed only after the information is gathered in the previous steps.
ESTABLISH GOALS
Create a space that feels welcoming and has a sense of community
Reduce cultural stigma associated with doctors and encourage people to find care
Increase the independence of the user regardless of their language or any disabilities
COLLECT AND ANALYZE FACTS
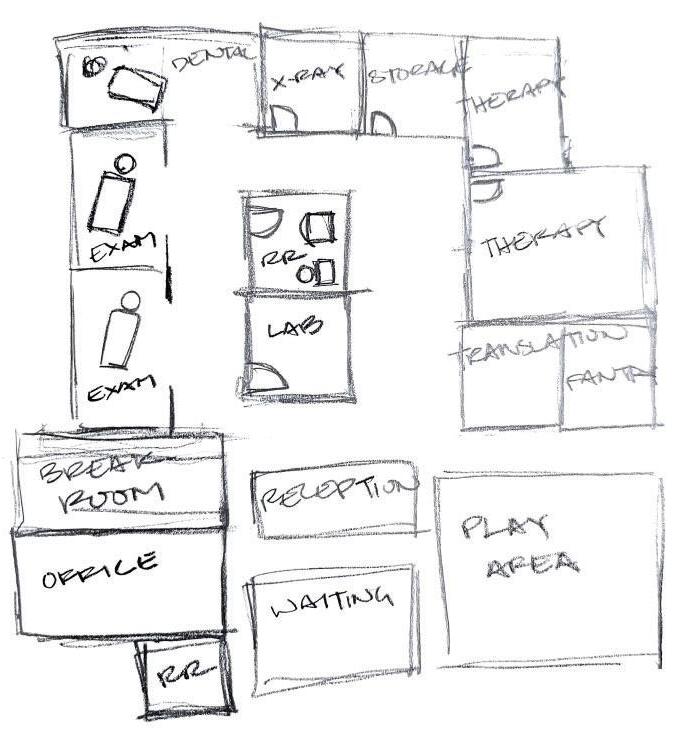
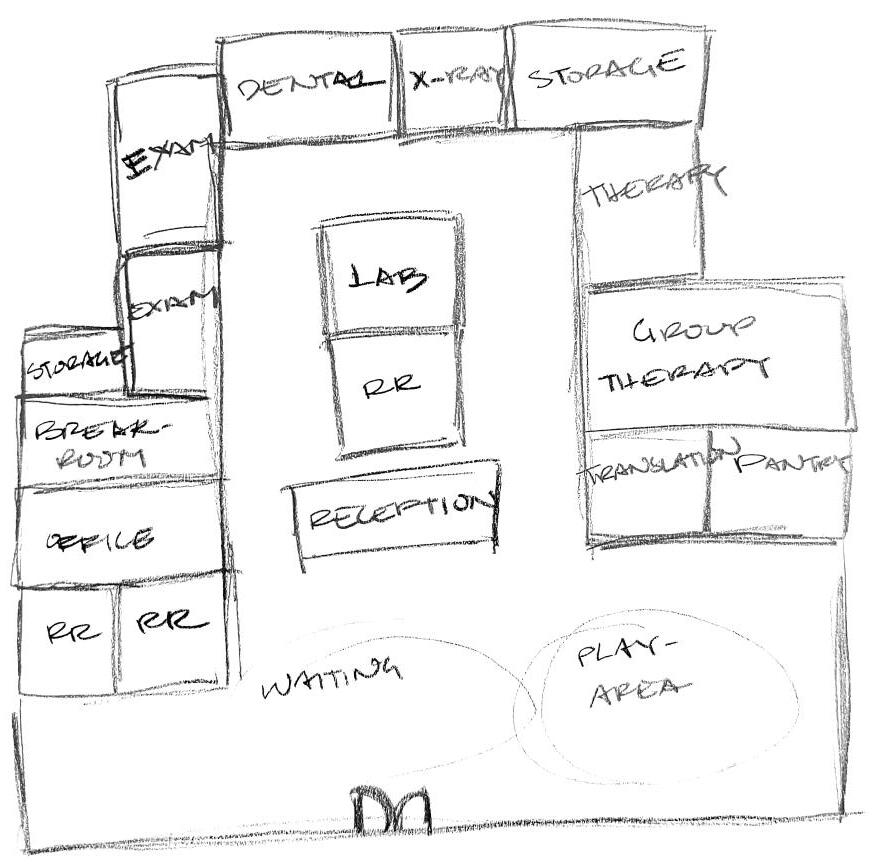
2 doctors, 1 dentist, 2 therapists, 1 x-ray tech, 1 lab tech, 1 receptionist, and 1 or more translators
Requires medical equipment storage, an employee office, and employee breakroom
Located near Bud Bailey Apartments
UNCOVER AND TEST CONCEPTS
Provide a medium level of security to ensure both the privacy and safety of all patients
Locate the children’s play area away from doors and within view of the reception lounge
Specify locking doors and appropriate STC ratings in the walls of all rooms where medical information will be discussed
Provide simple wayfinding to increase the independence of the user
Implement bright colors on paths in the floor and on the doors, with each color associated with different rooms/procedures
Provide incentives for local refugee communities seek out care from doctors and therapists
Create a space for food donations that can be picked up when a patient receives care in that office. Allow methods for donations to be dropped off and picked up discreetly to protect patient privacy and the overall security of the office
DETERMINE NEEDS
High quality, medical grade materials and FFE
Both individual and group therapy options
Space for professional translators to meet with patients
4
STATE THE PROBLEM
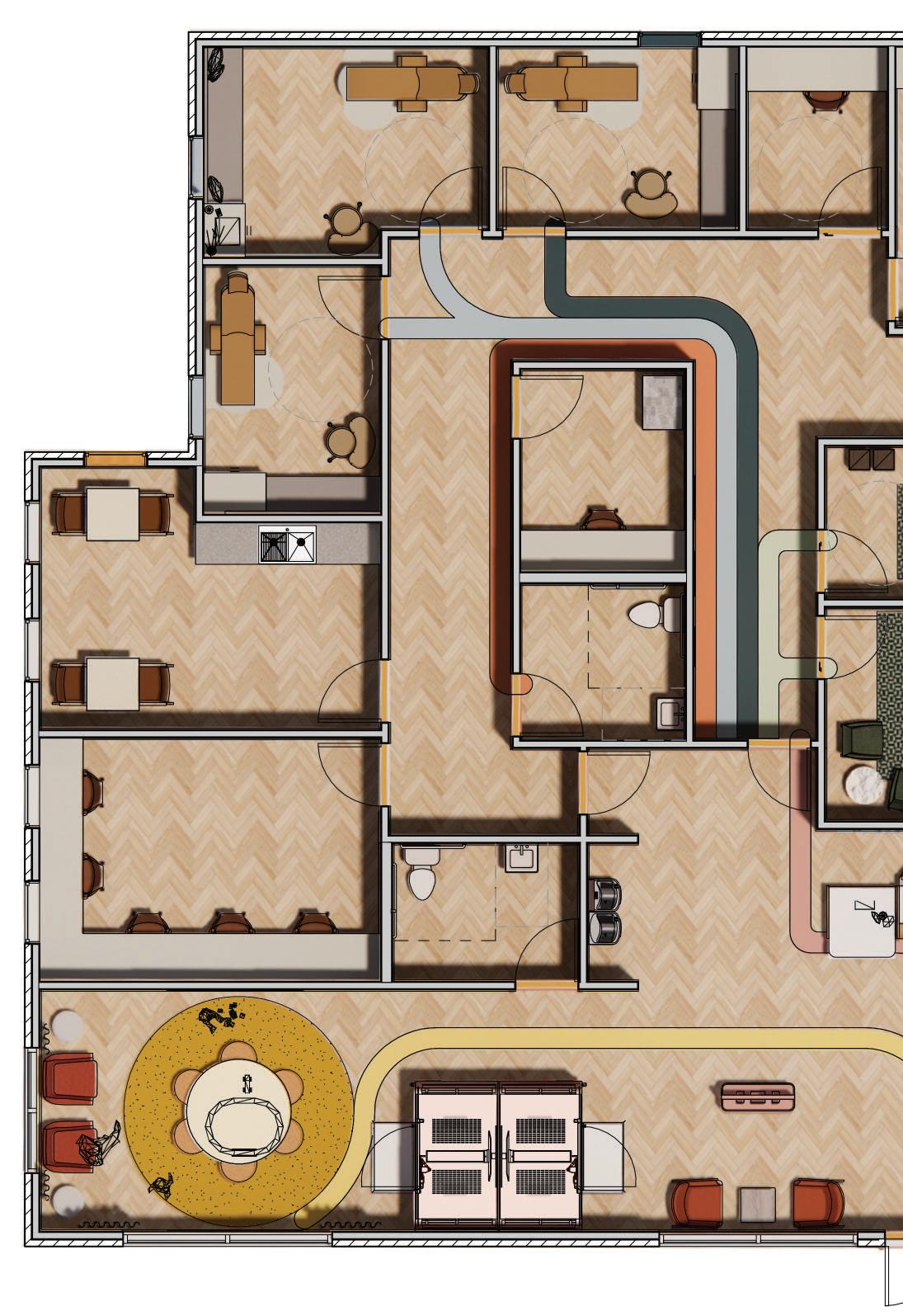
Bud Bailey Family Medical needs to provide a welcoming and communityfocused office because it will help break down cultural barriers and make medical care a more comfortable process. The reception desk is placed directly in front of the entrance to welcome clients. The waiting space is laid out similarly to a living room with a conversation area to promote the community and support system they provide each other.
Bud Bailey Family Medical requires easy wayfinding and accessibility options to support the independence of all patients and caregivers. Colorful LVT will be placed in the wood LVT flooring to create paths throughout the office. These paths will correlate with different specialties (i.e.: general doctor, dentist, therapist), and will lead to a matching-colored door.
Bud Bailey Family Medical needs a space for children to safely play within the office because refugee families often have several young children. A play area with a single path of entry will be located away from the entrance doors to provide safety and give the parents easy visibility to their children.
5
David Suisse volunteered for two years at the Federal Refugee Center in Twin Falls, Idaho. His knowledge and expertise drove many design decisions in this project.
I: What was your role at the refugee center in Idaho?
D: I worked there for two years. During the first year, I taught English, helped them build resume skills, and helped them apply for jobs. Then, in the second year, I went back and helped them with the same things and offered my experience with healthcare stuff. They put me on health and medical training. The refugee centers have community mentors who are refugees that have been in the US for longer than a year or two and have their feet under them, they have a sense of what’s going on, they have an apartment, and are off the federal funding. Those mentors act as liaisons whenever new refugees need help, and they get a small stipend from the government. I basically put together medical and health training, and other general training like banking and driving for these mentors and did assessments on where they’re at.
I: So, were you training these mentors?
D: Yeah, I was training the mentors. Then I had to do assessments, they basically wanted to know where these people are at. I showed them a first aid kit, and what they should and should not call 911 for. It’s a lot of memorizing and things that they’re not familiar with. There are also some cultural norms, especially around time keeping that make it really difficult for a lot of refugees from certain countries to keep appointments very well because they’re used to time and deadlines being a little more fluid. That’s something to keep in mind for a center serving a lot of refugees. *sighs* It’s hard because I definitely come from a point of view that there is no right or wrong way to view anything no matter where you’re from. If time is more fluid and the party is at eight, that really means the party is from four to ten and you can show up whenever that’s chill. But when insurance is involved and they start missing appointments, it can be really difficult. So, for their sake, I have to get frustrated when they don’t do it properly because they can be penalized for that if they keep doing it. So, I did a lot of training with that sort of thing.
I: What are the goals of the federal refugee centers?
D: The way that the US government places refugees, like the refugee center in Twin Falls only had access to those funds and resources for a year, sometimes two or three years. The goal is for them to have an apartment, a job, a car, and a driver’s license after a year, then they (the government) cut the funding and they go to places like Salt Lake City. They go to other places that are not federal refugee centers, more like community refugee centers or non-profits to provide continued support and resources. They won’t pay stipends like the federal refugee center did the first year.
I: So that would be the kind of center that Bud Bailey apartments are?
D: Yes, as far as I know, most first-year refugee centers are in more rural/ suburban areas, I don’t think they have a ton in place in Salt Lake. That’s just where they congregate when they have jobs and for a sense of community after they’re a little more stable.
6 SPECIALIST
INTERVIEW
I: Did you ever see any medical needs? A lot of research I’ve seen shows that they benefit from therapy because of abusive situations, torture, rape, and all this terrible stuff. What kind of medical needs were really common that you saw?
D: My health communication capstone paper was about mental illness in refugee populations in Southern Idaho and Utah. It was one of the most frustrating projects that I’ve ever done. There are a lot of health issues, and when you have a marginalized community, they’re going to be seeing more of everything. It’s hard for them to work jobs and take care of kids because they’re working more hours and they have less time to make healthy meals, so you see higher diabetes and hypertension. If they come over from a particularly war-torn area or high abuse situation, I had refugees that I would take to the doctor with old gunshot and stab wounds that had started to bleed again. There is physical care that’s needed but I would say that’s not nearly as common as mental illnesses like heavy PTSD, anxiety, and depression. My paper is very comprehensive of what I understand from the situation in just Idaho and Utah. When I first spoke to the director of the federal refugee center, a refugee himself of about fifteen years, I said “I’ve noticed that mental illness is a big issue and the literature side is a big issue, so what is the process like?” so I did some work with a couple of experts there. Basically, when they come over from another country, they’ll have a really brief psychological screening, super brief, not great, not intensive at all. Sometimes it doesn’t even happen because the goal is to just get them here. Then the priority is to get them a job, get them a car, get them an apartment.
I: So that mental health becomes a secondary thing?
D: yeah. It was frustrating to me, and I was kind of villainizing the system a little bit. I was talking to the director about it and saying “what can we do to fix this?” and he said, “don’t you dare”. He was pretty blunt with me, not mean though. He basically said “don’t you dare bring up mental illness or mental health with any of my refugees because most of the time, they don’t know they have an issue. If you trigger something then they can’t hold a job, they can’t get funding and it makes it worse”. So, the solution may be easier to use in Salt Lake rather than in a rural area like Twin falls because there are not many nearest therapists who can actually deal with refugee levels of PTSD, there are a lot of levels to PTSD and refugee level is the worst, are hours away in Salt Lake. So, we can set up regular appointments, but they can’t hold a job because you’re traveling to Salt Lake every week and they can’t take care of their kids, and the federal government can’t help pay for it because there’s not enough funding. It’s a huge wicked and complex problem that would be easier in Salt Lake City for sure. The conclusion that we made together is that the year the refugees are under federal help was to not do mental health but give them a choice once they relocate to a place like Salt Lake. If they would like to pursue help, that’s a more appropriate time to do it because they’re a little more stable.
I: So they would get the help once they are in a community-based support system?
D: Yep, just like they would be there (Bud Bailey Apartments). Make sure they have community support, make sure they have housing if they have some sort of relapse or really triggering event that they’re stable and can handle the aftershock.
7
I: That makes a lot of sense, I never would have even thought of that.
D: When I wrote my paper I cried a lot, it’s a deeper dive than people might be ready for.
I: Oh no! Can I ask you how you think interior design and architecture play a role in those things you’re involved in like community health and medical support? Interior design can have a big impact on your mental health, when you were at the refugee center did you see examples of this? Were the buildings well taken care of and helpful to the people there?
D: There’s definitely a funding issue there. It’s old and pretty cluttered. The first year I was there, I had to get a certain number of hours so when I wasn’t teaching, I was cleaning. We chucked so many old school supplies, and people would donate trash, I like to think they just didn’t know and were just trying their best to help. Any sort of new building would be nice. I felt like classroom settings were where a lot of them excelled, which might be hard to get in a doctor’s office, but that would help. When I would tutor, a lot of my students didn’t succeed as well as they did in a classroom setting.
I: Like sitting at a desk with pencil, paper, and notebooks?
D: Well, just sitting with other students like a classroom versus tutoring. Even when they weren’t from the same place at all and didn’t speak the same language, they were more successful. So, I’m kind of biased towards larger spaces because it allows for more of a community feel that is hard to get in a medical office. But in a rec center or community events, it would be really popular. They love that sort of thing, it’s really important.
I: Well, I’ve started some work on the lobby of this medical center, do you think a variety of seating arrangements for people to sit together like in a living room would be an effective design?
D: Yeah, I think I would even be more comfortable in a situation like that. I would take clients to the hospital when they had doctor’s appointments and be with some of those who had a hard time understanding what was going on and walk them through insurance. I don’t know if there was any sort of visceral reaction that I noticed to any sort of structural thing in a doctor’s office. I will say that a higher proportion of refugees compared to the American public have children, multiple children, and young children. A lot of the ones I worked with that were getting regular checkups because of lower health quality had accessibility issues, had a really hard time with stairs, and that sort of thing. Sometimes it was because of a stab wound, or sometimes it was just polio because they didn’t have access to a vaccine when they were growing up.
I: Do you think it would be effective to set up a center with multiple doctors’ offices and therapy offices for people to come and volunteer at?
D: A lot of doctors do a certain number of volunteer hours a week, not everyone, but there are a lot who do. Salt Lake is a great place for it because they come to Salt Lake to serve generally marginalized communities. If you come to an urban area like this, you’re more experienced with the homeless population, there are several organizations that specialize in this area and would be interested in
8
this sort of thing. AHEC, UPHA, and a couple of non-profits in Salt Lake are literally just physicians that donate their time to serve homeless populations. I’m not sure if there is anything specifically geared toward refugees, but they focus a lot on people without housing. But obviously, there’s a larger proportion in Salt Lake City than in other cities in Utah.
I: How do you communicate with people who struggle with English in important situations like when you discuss insurance or train them on how to call 911?
D: First off, there are several interpretation services that are used in hospitals like Intermountain, and Utah in general, I think they’re required by law to provide you service in a language you can understand. So, you call a number and they say “what language do you want?” and you tell them and they’ll connect you with someone. That’s what they’ll use a lot of the time if they don’t have anyone on hand. Medical interpretation is a pretty big deal because a lot of the time doctors will just ask the kids to translate for the parents. But that’s super inappropriate and should never happen. That will mess kids up and won’t be as accurate and is just not a good thing to do. We mostly used professional interpreters on the phone. For insurance stuff that can be a little bit different because they’re dealing with that at home, so we tried to always have someone who spoke each of the languages of the population. You’ll get waves of refugees, for a while we were getting refugees from Eastern Europe like Serbia and so we’d have people that spoke all those languages. Now we’re mostly getting them from Sudan and Congo, so I got to use my French, there are also people who speak Swahili and Arabic. We just try to always have someone at the refugee center so that people can come in and say “hey, I got this bill. I don’t know what it says, and I don’t know what to do with it.” we have someone to speak their language to sit down with them and go through it.
I: Are those people mostly other volunteers or other refugees that have “graduated”?
D: Sometimes both. We had some of those community mentors, and we also just gave stipends to some people who worked as translators. When one of my best friends was in a refugee camp for a while was hired at the camp somewhere in North Africa because he spoke six languages. So, they just hired him to interpret at the camp. He didn’t tell me about it when I was helping him put together his resume, I had to dig for that information. I was like “what do you mean you speak six languages? Where else have you worked?” and he would say “oh yeah, I worked for the UN”. I said, “what do you mean you worked for the UN? That should have been the first thing out of your mouth!”. So, people like that, speak way more languages than most Americans. But it would have to be somebody who had been here for a while because obviously, they have to understand the ins and outs of insurance. So, we’d do that. That’s what people would come into the office the most for, bill help when they didn’t understand the English or the system. Our insurance and medical system are so complicated that it’s as much of a resource to have someone sit down and help with insurance as it is to have a medical appointment.
I: Do you think it would be helpful to have a meeting room within the clinic just dedicated to insurance help and translation?
D: That would be so cool. That would be so cool. If you had limitless funding and could have full-time
9
staff there, that would be so cool. Volunteering is cool too though. What’s nice about Salt Lake City is that you’re so close to the University where everyone needs volunteer hours, I would come in and help with French sometimes. The translation is a big deal, which would suck when we’d get to that point in the medical training and I’d say “I have no clue how to explain to you in a way that you’ll understand and remember and retain in a way that I understand even how to do insurance. All I can tell you is that you should get a job that provides it and work with them to get it figured out. Beyond that, just come in (to the refugee center office) because I don’t know how to do it sometimes.” There’s also a big difference between most doctors and doctors that work with refugees, if only because they’re used to the way that they just won’t show up to appointments or be late or won’t pay their bills because they don’t understand how it works. A lot of doctors in Twin Falls had a no-refugee policy because they had too much to do, and they didn’t feel like they could deal with that. So, there were six physicians that we worked with that we would always send our refugees to or that would always take appointments because they were just stellar and would always have a spot open. That’s why it’s hard to pull from a general physician population to serve a refugee population.
D: I also want to say that working through mental illness is obviously a huge deal, but PTSD is a learning disorder, so it affects English learning.
I: Really?
D: Yes. So, if you have PTSD, it makes it much more difficult to learn. There were people who had some of the worst learning disabilities that I would ask my supervisor (the director of the English center) about. I asked, “Why is everyone having such a hard time?” and she said, “they all have PTSD.” it can be really hard to focus and it gives you almost ADHD-like symptoms sometimes. So, they can’t get a job, they can’t get stable, and they can’t get mental help.
I: Do you think group therapy might be more effective than one-on-one? Just because they excel better in a classroom setting.
D: I think in general, when you’re learning English, it might be different for something like PTSD. I’m not a therapist so I don’t know the ethics behind doing group therapy for serious trauma. I also know, our refugees were awesome and incredible, and some of the nicest/chillest people ever, but there were a couple of times when people were from areas or family lines or clans that did not get along well. So, there were a couple of times when we couldn’t put people in the same classes because even accents could tip it off and cause some aggression.
10
ABSTRACT
Background
Refugee populations have the highest rates of complex PTSD and depression. Financial limitations, educational limitations, cultural stigmas, and the inconvenience of travel are all factors of why a conflict-affected person would not seek medical attention.
Objective
The purpose of this exercise was to propose interior and architectural design solutions to make medical care more easily accessible and available to refugees and other low-income families.
Approach
A computer-simulated model was designed to showcase the proposed solutions.
Results
The location provides easy access and convenience to the clinic. The design enables all patients the ability to advocate for themselves and provides a comfortable space to receive treatment.
Conclusions
These design solutions can be easily implemented near refugee neighborhoods and promotes good health and general well-being in an accessible way.
11
“Health is a fundamental human right for all… refugees should have access to the same or similar healthcare as host populations”
“Health is a fundamental human right for all… refugees should have access to the same or similar healthcare as host populations”. The UN Refugee Agency works hard to make sure healthcare is always available (UNHCR, 2023). However, just because healthcare is available does not mean it is always accessible.
When something is accessible, whether it be a product, building, or service, it can be used by anyone. Most accessibility laws and guidelines are geared toward those who have a disability or several, but accessibility can benefit all users (Interaction Design Foundation, 2023). Closed captions, elevators, and press-to-open-door buttons are all examples of accessibility that everybody uses.
When refugees arrive in the U.S., they live in a Federal Refugee Center for about a year. In those centers, they work towards getting an apartment, a car, and a job. Once those three criteria are met, they are transferred to a community-based support system and no longer receive funding from the Federal centers (Suisse, 2022). A single year is not a lot of time to learn the American healthcare and insurance systems, while simultaneously becoming fluent in English. Because of constraints on a refugee’s time and money, the healthcare they receive in this first year is somewhat limited. Major physical wounds are treated, but there is rarely any mental health treatment given. “Basically, when they come over from another country, they’ll have a really brief psychological screening, super brief, not great, not intensive at all. Sometimes it doesn’t even happen because the goal is to just get them here. Then the priority is to get them a job, get them a car, get them an apartment.” (Suisse, 2022). These goals are the main reason why mental health is a secondary priority in the Federal Refugee Centers. “Most of the time, they don’t know they have an issue. If you trigger something then they can’t hold a job, they can’t get funding, and it makes it worse.” (Suisse, 2022). Rebuilding your life in a new country is an uphill battle, and you must strictly prioritize your needs. Unfortunately, mental healthcare usually falls low on that priority list.
When refugees leave the federal centers and relocate to a new community, it’s really their first opportunity to receive mental healthcare. But this is when cultural differences and accessibility begin to play a major role in this complicated situation. Researchers in Switzerland found that “language, gatekeeper-associated problems, lack of resources, lack of awareness, fear of stigma and a mismatch between the local health system and perceived needs of Syrian refugees and asylum seekers [are] key barriers to accessing care.” (Kiselev, et al., 2020). These are the same kinds of barriers that refugees are facing in the U.S. The goal of the Bud Bailey Family Medical project is to break down those barriers and encourage people to seek healthcare that can be life-changing. Because of the affordability of the Bud Bailey Apartments in Salt Lake City, they are popular locations for refugees to relocate to after they have “graduated” from the Twin Falls Federal Refugee Center. Right next to apartments is a small vacant lot, perfect for a medical center intent on helping the people who live next door. This vacant lot is the proposed site for the Bud Bailey Family Medical center.
12
RESEARCH
The design focus of Bud Bailey Family Medical is to create a welcoming space, increase the independence of the users, and reduce the cultural stigmas surrounding healthcare. To make the office feel welcoming, furniture and architectural finishes often found in a residential setting were selected. The waiting area of the lobby was arranged with a sofa and armchairs like a living room to create a sense of safety and home. Away from the doors, but within view of the waiting area is a children’s play area. A small table with soft poufs is an obvious signal that this space is for children and will be a safe area for them to play. Each room in the center is painted with calming pastels and lit with warm light to help people feel as comfortable as they possibly can at a doctor’s visit.

13
Many cultures have negative stigmas surrounding mental health and the care of mental illnesses. Finding ways to incentivize people to go around these stigmas can be extremely helpful in getting them the care they need. At Bud Bailey Family Medical, a food pantry is used as that incentive. “When you have a marginalized community… it’s hard for them to work jobs and take care of kids because they’re working more hours and have less time to make healthy meals, so you see higher diabetes and hypertension” (Suisse, 2022). Giving patients access to the food pantry incentivizes them to receive medical care and provides them with more healthy food options they may not otherwise have. Keeping in mind the privacy of patients and the negative stigma they want to avoid, the food pantry can be accessed from both the lobby and the back door of the facility.
Wayfinding was one of the most critical keys to increasing the independence of Bud Bailey Family Medical users. Wayfinding is an information system that helps guide people through a space, like street signs, or maps at the mall. In this medical center, color is used as a guide. “Patients and families who visit healthcare campuses are often under stress. Wayfinding systems can help reduce their stress by providing easy-to-follow signage and legible directions to their destinations. In some settings, reliance on text-based messaging is minimized and systems rely heavily on non-text cues such as colors and symbols.” (SEGD, 2023). Using paths of color, each being associated with a different element of the center, the user can easily guide themselves to where they need to go. Yellow is assigned to the children’s space of the area, and a bright yellow path embedded in the flooring leads to the play area. Orange is assigned to the waiting space and restrooms; a path leads from the doors to the lounge and restroom doors are painted in a matching shade. Pink is assigned to the reception; it also has a path from the door to the reception desk and continues through the door to the exam rooms. Green is assigned to therapy, dark blue is assigned to dentistry, and light blue is assigned to general physicians. White is assigned as a “background” color and is used to hide away rooms like the lab and medical storage.
14
Providing space for a patient to meet with a medical interpreter is key to breaking down the language barrier that prevents many from finding healthcare. “Medical interpretation is a pretty big deal because a lot of the time doctors will just ask the kids to translate for the parents. But that’s super inappropriate and should never happen. That will mess kids up and won’t be as accurate” (Suisse, 2022). Using soundproof meeting booths both encourages the use of professional translation services and allows children to play in the easy view of their parents. Framery Pods were specified because of their many customizable and accessible features. Speech levels are reduced, meaning you can’t hear conversations outside the pod, and private conversations won’t be overheard. Innovative ventilation systems always provide fresh air to the pod. Lighting and power sources to connect phones and video conference technology are easily accessible in the pod. Fold-up furniture and a small ramp make it more accessible for wheelchair users and other disabled people (Framery, 2023). Bud Bailey Family Medical is just the beginning of finding more solutions to help refugees in need of healthcare. Locating it near refugee communities makes it just that much easier for them to access. Many similar clinics can easily be located across the country. The initial goals of this clinic to create a welcoming space, promote the independence of the user, and reduce cultural stigmas associated with mental healthcare are just a start. The solutions proposed here may not be the most effective in achieving these goals, but the clinic provides the perfect place to study and innovate new ideas making healthcare truly accessible.

15




















 1.
2.
3.
10.
11.
12.
13.
15.
14.
16.
17.
1.
2.
3.
10.
11.
12.
13.
15.
14.
16.
17.









