

PREFACE
The SNMA National Service Protocol Handbook is designed for use by local SNMA chapters as they seek to implement the National Service Protocols. The mission of SNMA is to "support current and future underrepresented minority medical students, address the needs of underserved communities, and increase the number of clinically excellent, culturally competent, and socially conscious physicians." Community service is at the heart and sould of that mission. In order for us to successfully and effectively implement the national service protocols, it is vital that we understand the purpose of each protocol and its importance to our communities. This handbook aims to provide that knowledge.
Since its inception, SNMA has been committed to reducing morbidity and mortality in underserved communities and, to this end, our programs are focused on educating communities and empowering their members to make healthy lifestyle choices. Originally created in the 1980's, our National Service Protocols are designed to ensure each of our local chapters are advancing the mission of the SNMA while addressing the health disparities that plague underserved communities. In addition to benefiting the communities where the protocols are implemented, the National Service Protocols play a vital role in preparing future physicians to have an active role in health promotion and disease prevention. Participation in community service programs also serves to help medical students develop the interpersonal skills necessary to have productive and healthy relationships with patients while providing opportunities for cultural sensitivity and competency enrichment.
We hope that with the use of this handbook, each and every SNMA member becomes a culturally competent, socially conscious physician.
ROLE OF THE LOCAL COMMUNITY SERVICE LIAISON
The SNMA Local (Chapter) Community Service Liaison/Coordinator is responsible for the oversight & coordination of SNMA National Service Protocol programs at the chapter level. Any chapter officer or chapter member may hold this role. He/she/they must be able to communicate effectively with others, possess excellent time management skills and demonstrate strong leadership skills.
ADMINISTRATIVE DUTIES: Local Community Service Liaisons/Coordinators should contact their Regional Community Service Liaisons at the beginning of their term and obtain the most recent edition of the SNMA National Service Protocol Handbook, the Intro to SNMA National Service Protocols and Service Protocol specific PowerPoint presentations. Community Service Liaisons/Coordinators should familiarize themselves with these resources. The primary goal of the SNMA National Service Protocols is to effect change in underserved communities across the nation. In order to effectively evaluate the impact of our programs and seek funding for future programs, it is vital that chapters document their service activities. Community Service Liaisons/Coordinators should use the Community Service Program Report* form included in this handbook to track their chapter’s activities, which can be utilized to assist in completing quarterly Chapter Report Forms.
PROGRAMMATIC DUTIES: Implementing SNMA’s National Service Protocols is the primary responsibility of the local (chapter) Community Service Liaison/Coordinator. He/she/they should:
Promote chapter implementation of the National Service Protocols
Assist the chapter president in creating a community service calendar for the year Plan member training sessions
Develop a Work Plan* for each program’s implementation
Maintain regular communication with the Regional Community Service Liaison & the National Community Service Committee
FISCAL DUTIES: While National Service Protocol programs are generally funded by the local chapter, the National Community Service Committee has established a grant program to provide assistance to our chapters. Applications can be downloaded from snma.org. The deadline to receive applications for the Fall cycle is December 13th and March 15th for the Spring Cycle.
A WORD ON CULTURAL COMPETENCY
WHAT IS CULTURAL COMPETENCY?
Of cultural competency, the Office of Minority Health (U.S. Department of Health & Human Services) says, “Cultural and linguistic competence is a set of congruent behaviors, attitudes, and policies that come together in a system, agency, or among professionals that enables effective work in crosscultural situations.” “Culture” refers to integrated patterns of human behavior that include the language, thoughts, communications, actions, customs, beliefs, values, and institutions of racial, ethnic, religious, or social groups “Competence” implies having the capacity to function effectively as an individual and an organization within the context of the cultural beliefs, behaviors, and needs presented by consumers and their communities (Adapted from Cross, 1989)”.
HOW DOES CULTURAL COMPETENCE DIFFER FROM CULTURAL AWARENESS?
Cultural Knowledge is familiarization with selected cultural characteristics, history, values, belief systems, and behaviors of the members of another ethnic group (Adams, 1995). Cultural Awareness is developing sensitivity and understanding of another ethnic group This usually involves internal changes in terms of attitudes and values. Cultural awareness must be supplemented with cultural knowledge (Adams, 1995). Cultural Sensitivity knows that cultura differences as well as similarities exist, without assigning values, i e , better or worse, right or wrong, to those cultural differences (National Maternal and Child Health Center on Cultura Competency, 1997). Cultural Competence in health refers to being aware of cultural differences among diverse racial, ethnic, and other minority groups, respecting those differences, and taking steps to apply that knowledge to professional practice
WHY IS THIS IMPORTANT?
Cultural competency is one the main ingredients in closing the disparities gap in health care It’s the way patients and doctors can come together and talk about health concerns without cultural differences hindering the conversation but enhancing it. Health care services that are respectful of and responsive to the health beliefs, practices and cultural & linguistic needs of diverse patients can help bring about positive health outcomes
WHAT ARE THE COMPONENTS OF CULTURAL COMPETENCE? The
Process of Cultural Competency in the Delivery of Healthcare Services, a practice model developed by Josepha Campinha-Bacote, PhD, identifies 5 central constructs: Desire, Knowledge, Awareness, Skill and Humility, with desire being the key construct.
Desire: The motivation of the healthcare provider to "want" to engage in the process of cultural competence. Characteristics of compassion, authenticity, humility, openness, availability, and flexibility
Knowledge: Obtaining a sound educational foundation concerning the various world views of different cultures.
Awareness: Self-examination of one's own prejudices and biases toward other cultures An indepth exploration of one's own cultural/ethnic background.
Skill: The ability to collect culturally relevant data regarding the client's health history and presenting problem. Ability to conduct culturally based physical assessments. Conducting these assessments in a culturally sensitive manner
Humility: A lifelong commitment to self-evaluation and self-critique. Developing mutually beneficial partnerships with communities on behalf of individuals and defined populations. The journey towards cultural competence is a dynamic process that is based on understanding culture. So, the question becomes
WHAT IS CULTURE?
While no absolute definition of “culture” exists, it can be described as an innate but learned, cumulative, dynamic perspective of the world shared by a group of people Its primary components are Values & Beliefs, Behaviors and Language. It is important to keep these components in mind as you first examine your own culture and later strive to understand different cultures.
Values & Beliefs
Values are ideas of right & wrong while beliefs are a view of reality shared by a group. Key components of values & beliefs that affect health care delivery are Health Beliefs & Religion. These constructs may be mutually exclusive in one culture while inextricably linked in another
Health Beliefs
Health beliefs seek to create a context of meaning surrounding health, illness & disease. While the germ theory of disease- that microscopic organisms, such as bacteria & viruses, are the cause of many diseases is nearly universal accepted in the U.S., other cultures may subscribe to a different theory. Personalistic theories of illness contend that illness is caused by the intervention of a sensate agent who may be a supernatural being (a deity or dead ancestor) or a human being with special powers (a witch or a sorcerer) The sick person's illness is considered to be a direct result of the malign influence of these agents in retaliation for a transgression of moral and spiritual nature. Naturalistic theories of disease tend to view health as a state of harmony between a human being and the environment Illness results when the balance is upset Vitalist theories are based on the idea that when vital forces within the body flow in a harmonious pattern, a positive state of health is maintained. Illness results when this smooth flow of energy is disrupted.
Health beliefs have a very real impact on medical care and treatment. While a person who subscribes to the germ theory may seek an antibiotic for his illness,
recovery from an illness arising from personality causes usually involves the use of ritual and symbolism- most often by practitioners who are specially trained in these arts, illness due to naturalistic causes may be treated with vast pharmacopoeia of preparations made from herbs & minerals and dietary advice and therapeutic measures for disruptions in vital force are aimed at restoring a normal flow of energy in the body. As future physicians, we must be prepared to elicit and manage health beliefs.
Religion: Religion refers to a specific set of beliefs & practices regarding the spiritual realm beyond the visible world. As future physicians, general knowledge of various religious practices & customs is useful. However, general respect for one’s belief system lies at the core of cultural competency. Medical decisions and spiritual/religious beliefs are often not exclusive of each other and may conflict. It is vital to remember that the ultimate decision of treatment is a patient’s right and must be respected Respect will create an open & honest physician-patient relationship.
Behaviors
Behaviors are observed patterns of actions that are acceptable when they fall within the cultural norms- the range of permissible behavior established by the group. The key components of behavior that affects health care delivery are Family Relationships.
Family Relationships: The family is the primary unit of society in which children learn acceptable social behaviors & roles and parents impart cultural attitudes, beliefs, behaviors & values. It is paramount for physicians to understand the structure & role of family in health care. For some, the cultural expectation is that family members will address health concerns autonomously; while for others, decisions are made as a family. Understanding the role of family and working within its dynamic will facilitate more successful clinical encounters. Health care providers must also respect each family unit as presented
Language
Language represents the verbal and non-verbal patterns of communication that are common to a group of people. Health care professionals and managers must have a basic understanding of the impact of language on health care delivery in order to efficiently organize services that meet the needs of both the institution and a diverse patient population. Limited English proficiency (LEP) is a barrier to linguistic competence while lack of awareness of social customs of communication may hinder the physician-patient relationship
Limited English Proficiency: Even though most health care providers want to offer them the same attention and concern as to any other patient, LEP patients encounter obstacles at every turn They may delay making an appointment because of the difficulty communicating over the telephone. Misunderstandings about the time, date, and location of appointments are more likely to occur if the
patient does not understand English. Even when patients arrive at the facility on time, they may be late for appointments because of difficulty communicating with registration staff Furthermore, the medical interview and examination present unlimited possibilities for confusion and potential serious misunderstanding can occur since complete and accurate medical history is crucial to an accurate diagnosis Sophisticated technology and diagnostic procedures are not substituting for clear patientprovider communication. Even when tests are necessary, if patients are not given instructions in a language they can understand, they may not be adequately prepared physically or psychologically. Likewise, if patients are to comply with a treatment plan, they must have a clear understanding of what is required of them It is our responsibility to find a way to effectively communicate with all patients
Social Customs of Communication: While verbal communication may present a problem particularly in the case of regional word choice or colloquialisms, non- verbal communication is more frequently the source of misunderstandings Non- verbal communication includes bodily proximity, gestures, facial expressions, eye contact, touching and body position. While they are too numerous a few examples include:
Posture: Hands in your pocket is disrespectful in Turkey; Sitting with legs crossed is considered offensive in Ghana; showing the soles of your feet is considered offensive in Thailand. Facial Expressions: Many Asian cultures suppress facial expression as much as possible while many Mediterranean cultures exaggerate grief or sadness and most American men hide grief or sorrow Some see “animated” expressions as a sign of a lack of control while too much smiling is viewed in as a sign of shallowness.
Touch: Indians don’t typically touch with the left hand as to do so may be considered a social insult. Islamic cultures generally don’t approve of any touching between genders. Cultures with high emotional restraint concepts generally have little public touch while those, which encourage emotion, accept frequent touches.
It is impractical to attempt to learn all the social customs of communication As future physicians, it is vital to be alert to cues that a communication may be present and subsequently seek to address it. Effective communication requires awareness of verbal & non-verbal communication and identification of the best way to share information with the patient
WHAT'S IN A HEALTH FAIR?
HOW DO I PLAN FOR ONE?
KEYS TO SUCCESS

A I R S
S
The purpose of a health fair is many-fold. A health fair serves to bring members of a community together to provide health care information and screening with the objective of encouraging a healthier lifestyle among individuals and communities. The way an organization goes about accomplishing this goal varies from group to group. Thus, this document is by no means the absolute blueprint to executing a successful health fair. Rather, it is a starting point that hopefully allows organizations to inject their own creative ideas to better meet the specific needs and goals of their community and health fair, respectively.
03 04 05 08 12
Health Fair Objectives
What's In a Health Fair
The Timeline & The Planning
The Nuts & Bolts
Health Fair Checklist
H E A L T H F A I R
O B J E C T I V E S
. . .
It should come of no surprise to you, being an SNMA member, that we have a great commitment to meet the needs of underrepresented/underserved communities across the world. In the United States alone, minorities, namely Blacks and Latinos, continue to be disproportionately affected by preventable and/or treatable medical conditions such as obesity, diabetes, hypertension, HIV/AIDS, and preventable infections. Many of this can be attributed to minorities’ decreased access to care and to the persistent racial/ethnic biases that plague many of America’s health care providers. According to SNMA’s mission, the health fair conducted by your chapter should strive to meet the following goals as a minimum:
1) Provide health screenings, counseling, education, and RESOURCES for those with limited access to care
2) Promote healthy living in our communities
3) Facilitate the connection between the residents and resources of our communities.
In summary, in accordance with the overarching mission of SNMA, our health fairs should strive to “address the needs of underserved communities
Think of a health fair as a central resource for the promotion of healthy living – where it all comes together. Below is a list of some of the functions that a health fair should have.
Screening: There should be screening for basic physiological diseases that can be diagnosed in a primary care setting. In addition, free immunizations for children and adults may be offered.
Blood Pressure, Cholesterol, Bone Density, Glucose, Glaucoma, Immunizations
Preventative Health Counseling: In the same vein as basic screening, the organization putting on the health fair should be very conscious about providing EDUCATION. That is education in terms of knowledgeable educators and informative sessions, pamphlets, etc. Remember, someone can be screened for diseases and provided immunizations - however, if there is no lasting education, you have to question the utility and validity of your health fair. For example, …
Have local preventative cardiologists educate about the metabolic syndrome and its relation to heart disease.
Provide trained smoking cessation specialists to provide education and counseling.
AIDS awareness/prevention
Nutritional Eating Alternatives in the midst of communities where healthy eating options are minimal
Prenatal care and Teen pregnancy prevention
Social Work Counseling: The psychosocial/behavioral aspect of an individual/family is intricately intertwined with their health and influences how they manage their health. For example, if one is depressed, one is less likely to monitor their blood sugars and control their diabetes. Thus, a health fair is in perfect position to provide social services such as….
Signing up the uninsured to Medicaid or other local low-cost health plans
Providing information on domestic violence and substance abuse
Mental Health Education: Information on depression, stress management, schizophrenia, alcoholism, bipolar disorder
Much more: There are many other things that you can add to your health fair. Your health fair should include things that meet the needs of the community you are serving at the time. For example, Healthy Eating/Exercise – Is obesity a huge problem in your community? If you’re in America, it probably is? Provide a menu detailing healthier ways to cook some of the favorite/common foods in that specific community. Provide creative ideas on how people can use their communities to their advantage for exercise
Needle/Gun Exchange Programs – Are drugs a big problem? Set up a drive to have people turn in their needles. If guns are a problem, maybe set up a gun exchange program with the help of a qualified lawenforcement agency
CPR demos and class-sign ups
Asthma program information
Provide a free risk factor checklist, information on health-related services available in the community and how to obtain follow-up care
Don’t forget the KIDS: face painting, water games, clowns
And of course, you’ll need food and refreshments
This part of the health fair is the most critical. As the saying goes, if you fail to plan, you plan to fail. The planning and timing should follow the following guideline in general:
1. Getting Started: Start planning as early as possible. In general, 3-5 months prior is more than enough time. Definitely, NO LATER than 2 months before the event. For the purposes of this document, we will use a 3-month timeline. Set a date! Find out if any other health fairs are being put on around that time.
Secure SNMA Protocol Kit
Brainstorm and Decide on a theme that provides some focus and uniqueness to your fair
Create potential Committees: Peoples roles/ responsibilities should be clearly defined and articulated. Committees should include
Site logistics – set-up/clean-up, volunteer management, equipment/materials, floor plan, check-in, information with materials on follow-up care/clinics, etc
Publicity/Promotion – Press releases, media, website, emails Building community attendance through grassroots outreach at churches, schools, grocery stores, etc
Participation recruitment and management – Soliciting organizations and speakers to provide services and information
Finance/Budgeting Committee
Directors/Chairpersons
Most importantly, begin drafting proposals/budgets necessary for funding
Identify advisor(s) (preferably a physician and/or public health official) and community organizations/hospitals/clinics to be your sponsors. You will probably need some sort of invitation letter for this step (most likely similar to the proposals written for funding)
2. More than 2 months before the fair
Secure Location: Examples include churches with large congregations, high schools, shopping center parking lot, housing development, etc.
Attempt to locate space free of charge, since it may be available in most communities You should also consider your target group when deciding on location, since some places are not easily accessible for people of all ages and helpful to find those with physical disabilities The location needs to be large enough to accommodate all the displays Tables must be available for the displays, as well as appropriate lighting and enough electrical outlets at the site Ensure that there is enough parking at the location, and it is out if there is anyone like a custodian who will be available at the site Be sure the location has enough power sources for possible booth participants
Have budget and proposals finished
Order materials and supplies
Apply for Community Service Grant from National Community Service Committee
Set schedule for regular (e.g., weekly or biweekly) meetings or conference calls. Make a contact sheet for all those involved in the planning and execution of the fair.
Brainstorm on prominent national and local representatives to attend your health fair and thus provide it with some status and legitimacy (not to say that it isn’t legitimate without them)
Have a general idea on the resources/services/providers you want to invite to the fair
3. Two Months before Fair
Contact providers (e g HIV mobile truck, local insurance agencies, immunization services) Begin to identify possible organizations and health care providers to host booths at the health fair, especially in the context of your theme
Contact other allied health field students (e g dental, nursing, public health) to provide perception and help with your fair
Begin advertising strategy
Confirm location and any compliance obligations
4. Six to Seven Weeks months before Fair
Confirm providers coming to the fair.
Finalize the list of participants. Review the list to ensure that a range of basic services and health care information is provided.
Determine follow-up services for uninsured participants in case any medical problems are uncovered during the screenings.
Begin organization of pamphlets, resources, and goods to be handed out at Fair
Ensure that committees are on task
5. Four to Six Weeks before fair
Advertise, Advertise, Advertise on the front lines! Have fliers printed Churches, schools, libraries, grocery stores, community centers, shelters, YMCA, soup kitchens, public housing, barbershops/salons, record stores, etc
Do not forget to reach out to media such as local news and radio and newspaper
Re-confirm materials and providers: Finalize contracts with any possible vendors, such as event venue, equipment rental company, printers, transportation, etc.
Design floor plan and logistics and review this with representatives from that event venue
Identify food and drink providers
6. Three to Four Weeks before Fair
Confirm everything again (providers, supplies, food, advertising)
Schedule a date for representatives from each participating organization to walk through the site. Send confirmation letters to all participants/providers with details of your event including suggested arrival time, contact info, site limitations, parking, etc.
Print out floor plan and design and send it out to all participants and volunteers. Make sure you’ve included things like bathrooms, food stations, power sources, play stations, parking, etc.
Order food and drink (have plenty of water and snacks for volunteers)
Organize set-up and clean-up crews
7. One to Three Weeks before the Fair
Make sure everyone is on task and up to date with their responsibilities
Finalize all information with participants/sponsors/resource providers, etc
Create a checklist for the day of the event
Keep the foot on the pedal with advertising Revisit schools, after-day programs, Hospital ERs, grocery stores, etc
8. ONE week before the Fair
Walk through the event venue with the venue representative to confirm any specific participant requests such as power, a certain booth location or extra equipment. Confirm arrangements and details with all vendors.
Buy film or disposable cameras to document the event. Consider assigning a planning committee member with few event-day responsibilities to photograph the health fair You may want to use the photos in a newsletter, as a thank you for speakers or to show a potential funder your organizing success.
Assign planning committee members specific duties for the day of the event. Assignments may include information booth, check-in registration, setup/clean-up
Create a full-day timeline for the day of the health fair with committee member and volunteer assignments, times, responsibilities and contact information
9. WEEK of the Health Fair
Make sure advertising/publicity push is in full swing
Make sure pamphlets and all printed resources are secured
Re-confirm attendance of key attendees, booths, and media/publicity outlets
Schedule planning meeting to make sure all last-minute details are taken care of
10. Day of the Health Fair: It’s Game Time
Arrive early! Do a quick run-through and refer to “day of event” checklist
Set-up and make sure everyone knows their tasks
Stay CALM!
Have FUN!
11. Week Following the Health Fair
Send thank you notes to all participants, volunteers and sponsors
Process evaluations and follow-up on news coverage of the event
Have a celebration/party!
N U T S A N D
E X T R A !
Health Fair Components: (* Denotes the minimum)
Registration*
Height and weight*
Nutrition and fitness
Immunizations*
Oral health*
Kids Corner or Children’s health*
Women’s Health*
Men’s Health*
Blood pressure*
Sexual Health and Awareness*
Vision and Hearing
Cholesterol screening and literature*
Glucose Screening and literature*
Physician review*
Alcohol, drug, and tobacco
awareness
HIV/AIDS and STDs
Breast Self-exam demonstration
Poison control
Bone marrow registry
Social services
Evaluation*
E X T R A !
Suggested Materials/Equipment Checklist: Arrange for donations
Literature
Gloves, Sharps container
Scale and Vision chart
Sphygmomanometers and Stethoscopes
Glucometers and Lancets and Test strips
Band-Aids, Alcohol swabs, and Cotton balls
Station identification signs
Biohazard containers and bags
Health fair programs
Evaluations
Coloring books or activities for children’s corner
Innovation and Creation:
Don’t be scared to do something different. Take a stance and followthrough. Set big goals. If you have statistics on the insured status of your community, make a goal to get x number of families or individuals insured.
During the health fair, you can work to enroll uninsured children in Medicaid or the State Children’s Health Insurance Program (SCHIP). When parents or guardians inquire about children’s health care coverage, it is also a great opportunity to inquire about their insurance status and, if appropriate, explain the adult coverage available to them. Be creative with how you market and eventually document your event.
TIPS on having a successful FAIR
Partner with another organization to increase attendance and participation
Try to tie the fair to another event that targets the same population
Make your fair stand out:
Invite fire department and ask them to bring a fire engine or smoke house to practice escaping from a fire.
Invite well-known radio host/personality or entertainment artist/celebrity if possible
Have prizes (e.g. restaurant certificates, record store certificates, heart healthy cookbooks, clothing from an apparel store, sports equipment etc.) such as a dance-competition, spelling-bee, jumprope competition, poetry etc. Have a learning corner where kids can learn about their bodies and basic hygiene
Invite the police department and ask them to bring McGruff the Crime Dog or to provide child identification cards.
Invite health department to provide the immunizations
Ensure that all participants complete health fair survey before leaving so that you can evaluate the success of the fair.
Make sure that EVERY participant in the fair leaves with SOMETHING. Remember, education, education, education…it’s all about health promotion here!
Solicit donations from local businesses to give away as door prizes.
Involving the Local Media in Your Health Fair (adapted from various online sources)
Local health fairs provide compelling visuals for stories and offer opportunities for effective feature stories. You will want to focus the media on the problems and issues your fair is addressing such as poor nutritional options, poor access to care, insurance status, overcrowded ERs, etc. Offer reporters opportunities to interview families with children enrolled in the programs along with local health care providers. If your health fair is at a school, you may want the school’s principal, superintendent or a school board leader to discuss the relevance of health and health care to learning. As always, you will want to select your spokespersons with care and provide media training. You may wish to have a media table at the fair with spokespersons available throughout the day. Remember to indicate that the fair is FREE to all.
Below are suggested tips for engaging the media in your health fair activities. Promote the event in advance through television, radio, newspaper, community calendars and school communications outlets.
Ask reporters who cover health and metro news to attend.
Alert photo editors to the photo opportunities available.
Explain the range of coverage opportunities to local television producers. These include preview stories on early morning news shows; live reports during noontime newscasts; live reports during “Live at Five” newsmagazine programs; and summation stories during the nightly and evening news. Keep in mind that each of these shows, although broadcast by the same local network, may involve a different producer.
Offer radio reporters opportunities to report live from the event or offer them sound bites recorded during the event.
Offer to have an on-air television reporter take part in the health screenings offered at the fair in order to demonstrate the value of health care coverage
B E S I T Y

E V E N T I O N
I D S A N D T E E N S
GOALS, TARGET GROUPS AND MINIMUM
REQUIREMENTS
ABOUT THE OBESITY AND PREVENTION PROTOCOL
FOUR KEY PRINCIPLES FOR GETTING FIT AND STAYING HEALTHY HELPFUL WEBSITES
INTRODUCTION
3 0 4 0 5 0 9
ABOUT OBESITY AND PREVENTION PROTOCOL
TOPICS
HELPFUL WEBSITES
I N T R O D U C T I O N
According to the Centers for Disease Control and Prevention (CDC), the prevalence of obesity in American children and adolescents is about 18.5% (about 13.7 million) children and adolescents. Minorities, particularly African Americans and Latinos, are significantly more overweight than European Americans. The prevalence of obesity is highest amongst African Americans and Hispanics compared to Caucasian and Asian children and adolescents.
GOALS
Disseminate information regarding healthy eating and physical activity to educate the community Encourage healthy lifestyle modification and weight loss where appropriate in adults
TARGET GROUP(S)
Children and teens
MINIMUM REQUIREMENTS
No minimum number of sessions. Topics can be covered sequentially or combined, depending on resources available and target group.
A B O U T T H E O B E S I T Y
P R E V E N T I O N P R O T O C O L
According to the Centers of Disease Control and Prevention, the prevalence of obesity among 2-to 5-year-olds is 13.9%, 6to 11-year-olds is 18.4%, and 12- to 19-year-olds is 20.6%.
The American Obesity Society defines overweight and obesity as follows:
Overweight = being at or above the 85th percentile for BMI
Obesity = being at or above the 95th percentile for BMI
**See CDC growth charts, found at http://www.cdc.gov/growthcharts/
The obesity-prevention protocol hinges on the idea that for kids and teens, getting fit and staying healthy require four key principles: Making healthy food choices
Making healthy beverage choices (staying away from highcalorie drinks)
Getting at least 30 to 60 minutes of physical activity everyday
Avoiding overeating by learning appropriate portion sizes and listening to their bodies
H E A L T H Y L I F E S T Y L E *
Define “healthy weight”
Discuss the obesity epidemic in America and its impact on minority populations in an age-appropriate manner
Give statistics that highlight the specific group you are targeting (children, teenage girls, etc.)
Discuss the sequelae of obesity (diabetes, osteoarthritis, heart disease, cancer)
Emphasize the importance of everyday lifestyle choices in preventing obesity
Introduce the “4 Keys to Staying Fit and Healthy”
*See section entitled “Topics for Teens” for additional topics/activities.
F O O D C H O I C E S
*Use diagrams, figures and handouts in Be Smart, Be Healthy! Booklet. Activity pages are designed for kids under 12, but similar activities can be made for teens.
Part I Understanding calorie Balance
Explain that calories are units of energy that we gain from food and burn through physical activity (give examples) Understanding the MyPlate Dietary Guidelines Reading food labels
Part II
Understanding portion sizes
Provide copies of portion sizes handout to each participant. Emphasize the importance of listening to your body and stopping when you’re full.
Activity: Making healthy choices activity page.
Healthy recipes and snacks (give handout)
Activity: Healthy snacks taste test (participants can vote for the best- tasting snack).
Homework: food journals
Have participants complete a week-long food journal and discuss at the next session.
P H Y S I C A L A C T I V I T I E S
Aim for 30 to 60 minutes of physical activity every day
Activity: Finding fun physical activities handout
Limit TV/video game and internet time to no more than 1-2 hours a day (not including homework time)Physical activity guide
Activity: Have someone lead participants in a 30-minute session of a fun moderate physical activity such as kickball, dance aerobics or taking a walk as a group outside. Be sure to include proper warm up and stretching.
F I T A N D H E A L T H Y
Make healthy food choices
Follow the MyPlate Dietary Guidelines, choose fried foods and sweets less often, and eat lots of fruits and vegetables.
Choose healthy drinks
Make water and milk your #1 choices. 100% fruit juice is okay in appropriate amounts. Soda and fruit punch taste good, but just add lots of calories and not many nutrients.
Be active every day
Aim for at least 30 minutes to an hour of physical activity a day.
Physical activity burns calories and helps you stay at a healthy weight.
Don’t overeat
Learn to stop when you’re full.
Kids Health
www.kidshealth.org
USDA Choose My Plate
https://www.choosemyplate.gov/
Health Hoping
https://web.extension.illinois.edu/hopping/onerope.html
Super Healthy Kids
https://www.superhealthykids.com/
CDC Child and Teen BMI Calculator
https://www.cdc.gov/healthyweight/bmi/calculator.html
The following websites have helpful guidelines and statistics as well as handouts:
The Obesity Society, Information for Healthcare Providers and Patients
https://www.obesity.org/information-for-patients/
National Heart, Lung, and Blood Institute: Aim for a Healthy Weight
www.nhlbi.nih.gov/health/public/heart/obesity/lose wt/
USDA Dietary Guidelines for Americans: How much are you eating?
https://www.dietaryguidelines.gov/
The Diabetes Prevention Project
https://dppos.bsc.gwu.edu/
Weight Watchers Website, Body Mass Index Explained
http://www.weightwatchers.com/health/asm/calc healthywei ght.aspx
American Heart Association Website
https://www.heart.org/
CDC Body Mass Index
Informationhttps://www.cdc.gov/healthyweight/assessing/bmi/index .htm
National Institute of Health, Serving and Portion Sizes
https://www.nia.nih.gov/health/serving-and-portion-sizes-howmuch-should-i-eat
Calorie Calculator
https://www.calculator.net/calorie-calculator.html
Centers for Disease Control and Prevention Website
https://www.cdc.gov/nchs/products/databriefs/db360.htm
USDA ChooseMyPlate
https://www.choosemyplate.gov
Bar-on ME. The effects of television on child health: implications and recommendations. Arch Dis Child. 2000;83(4):289-292. doi:10.1136/adc.83.4.289https://www.ncbi.nlm.nih.gov/pmc/articles /PMC1718503/
O B E S I T Y
D U L T
GOALS, TARGET GROUPS AND MINIMUM REQUIREMENTS
ABOUT THE OBESITY AND PREVENTION PROTOCOL
FOUR KEY PRINCIPLES FOR GETTING FIT AND STAYING HEALTHY HELPFUL WEBSITES

03 04
05
11 TOPICS
HELPFUL WEBSITES INTRODUCTION
ABOUT OBESITY AND PREVENTION PROTOCOL
I N T R O D U C T I O N
According to the Centers for Disease Control and Prevention (CDC), the prevalence of obesity in American children and adolescents is about 18.5% (about 13.7 million) children and adolescents. Minorities, particularly African Americans and Latinos, are significantly more overweight than European Americans. The prevalence of obesity is highest amongst African Americans and Hispanics compared to Caucasian and Asian children and adolescents.
GOALS
Disseminate information regarding healthy eating and physical activity to educate the community Encourage healthy lifestyle modification and weight loss where appropriate in adults
TARGET GROUP(S)
Adults
MINIMUM REQUIREMENTS
No minimum number of sessions. Topics can be covered sequentially or combined, depending on resources available and target group.
A B O U T T H E O B E S I T Y
P R E V E N T I O N P R O T O C O L
According to the Centers of Disease Control and Prevention, the prevalence of obesity among 2-to 5-year-olds is 13.9%, 6to 11-year-olds is 18.4%, and 12- to 19-year-olds is 20.6%.
The American Obesity Society defines overweight and obesity as follows:
Overweight = being at or above the 85th percentile for BMI
Obesity = being at or above the 95th percentile for BMI
**See CDC growth charts, found at http://www.cdc.gov/growthcharts/
The obesity-prevention protocol hinges on the idea that for kids and teens, getting fit and staying healthy require four key principles: Making healthy food choices
Making healthy beverage choices (staying away from highcalorie drinks)
Getting at least 30 to 60 minutes of physical activity everyday
Avoiding overeating by learning appropriate portion sizes and listening to their bodies
H E A L T H Y L I F E S T Y L E *
Goals
Discuss the obesity epidemic in America and its impact on minority populations
Give statistics that highlight the specific group you are targeting
Discuss the sequelae of obesity (diabetes, osteoarthritis, heart disease, cancer)
Define Overweight and Obesity
Explain the calculation of the Body Mass Index
Activity: What is My Body Mass Index?
Body Shape and Health (for women)
Emphasize the importance of everyday lifestyle choices in preventing obesity
F O O D C H O I C E S
*Use diagrams, figures and handouts in Be Smart, Be Healthy! Booklet.
Goals
Calorie Balance
Explain that calories are units of energy that we gain from food and burn through physical activity (give examples)
Regardless of diet program, weight gain and weight loss are determined by calorie balance
Understanding the MyPlate Dietary Guidelines
Reading food labels
Serving sizes
Emphasize the importance of listening to your body and stopping when you’re full Healthy recipes and snacks
Activity: Food Journal
.Goals Breaking the cycle between our thoughts, our feelings and our weight
Activity: Problem Solving Worksheet
Shutting down negative thoughts
Activity: Turning Negatives to Positives Worksheet
Managing stress
Activity: Stress Busters Worksheet
P H Y S I C A L A C T I V I T I E S
Goals
Aim for 30 minutes of moderate PA on most days of the week
Define “moderate PA” and give examples as well as caloric expenditure for different activities
Hand out physical activity guide
Activity: Have someone lead participants in a 30-minute session of a fun moderate-intensity physical activity such as dance aerobics or taking a walk as a group outside. Be sure to include proper warm up and stretching.
W E I G H T L O S S A N D
M A I N T E N A N C E
Goals Review BMI and Healthy Weight information
Have each participant calculate their BMI
Discuss Popular Diets
Emphasize that all diets work by creating a calorie deficit
Tipping the calorie balance for healthy weight loss
Healthy weight loss means going at a slow and steady pace, losing at a rate of 1-2 pounds per week
Activity: Have participants review their food journals and identify areas where they can cut out 500-1000 calories per day
Activity: Review Physical Activity guides
Goal Setting
Activity: Weight Loss or Weight Maintenance Goal Sheets
Goals
Taking it one day at a time
Emphasize the importance of positive thinking and not giving up.
Overcoming barriers
Discuss building a support circle.
Managing stress
Activity: Have participants discuss their current stressors. Review stress management techniques from Topic 3 and have participants help each other strategize ways to apply those techniques to their everyday lives.
Planning Ahead
Discuss the importance of knowing what situations make it hard to eat healthy and finding healthy alternatives.
Closing Activity: Healthy recipes Pot-Luck supper (or lunch).
The following websites have helpful guidelines as well as handouts:
National Heart, Lung, and Blood Institute: Aim for a Healthy Weight www.nhlbi.nih.gov/health/public/heart/obesity/lose wt/USDA
USDA Dietary Guidelines for Americans 2015-2020 https://www.dietaryguidelines.gov/
Weight Watchers Website, Body Mass Index Explained http://www.weightwatchers.com/health/asm/calc healthyweight.aspx
American Heart Association Website
https://www.heart.org/
CDC Health & Physical Activity Website, Adult BMI Calculator http://www.cdc.gov/nccdphp/dnpa/bmi/bmi-means.htm
Northwestern Memorial ® Hospital Patient Information. Modify your lifestyle to reduce the risk of heart and vascular disease. https://www.nm.org/conditions-and-care-areas/treatments/lifestylechanges-for-heart-and-vascular-disease
Waist Hip ratio calculator. https://www.thecalculatorsite.com/health/whr-calculator.php
National Institute of Health, Serving and Portion Sizeshttps://www.nia.nih.gov/health/serving-and-portion-sizes-howmuch-should-i-eat
The Diabetes Prevention Project
https://dppos.bsc.gwu.edu/
Calorie King Website. http://www.calorieking.com
USDA ChooseMyPlate
https://www.choosemyplate.gov/
FDA Interactive Nutrition Facts Label
https://www.accessdata.fda.gov/scripts/InteractiveNutritionFactsLa bel/#intro

S E X U A L H E A L T H & L G B T Q I A + A W A R E N E S S
BASIC ANATOMY
HIV AND OTHER STI'S
TEEN SEXUALITY, RELATIONSHIPS, AND CHOICES
The Basics Introduction
HIV and Other STI's
Teen
Sexuality, Relationships, and Choices 2 0 2 0 - 2 0 2 1
I N T R O D U C T I O N
The following “Teaching and Reference Guide Draft” is the first step in bringing the HIP Corps Prevention Program into a protocol format. This document is not intended as a hard and fast curriculum, but truly a “Guide” for SNMA students who are interested in providing sexual health awareness education, emphasizing HIV/AIDS prevention. Students and their advisors, along with school officials, parents, and the local community may decide to censor some topics addressed in this document. Some of the information contained here is more technical than needed for the typical outreach, but this document is intended to inform SNMA volunteers of the various concerns of today’s teens Those concerns (sex, relationships, peer-pressure) constitute the very real life context within which young people make their decisions. Our intent is to ensure that information is easily available to students, so when a copy of this document is sent via electronic transfer, numerous hyperlinks (shown in blue or violet) will take the reader to additional sources of information Hard copies of this document will be made available to any interested parties. The majority of the information contained in this document was taken from the following three sources and are cited throughout the text:
www.pamf.org (Palo Alto Medical Foundation)
http://health.howstuffworks.com/aids.htm
http://www.cdc.gov/hiv/pubs/facts/condoms.htm
http://www.cdc.gov/hiv/dhap.htm
https://www cdc gov/hiv/dhap/about html
For additional information and activities, please go to:
http://www unicef org/lifeskills/index 14926 html
There are many resources here available for download. The Life Skills Manual is very comprehensive and deals with behavior change and decision making.
http://www.peacecorps.gov/wws/guides/looking/contents.html#grade35
Again, many, many solid resources here are available for download. My Future is My Choice is subtitled “Protecting Our Peers from HIV Infection”; very relevant, indeed.
O B J E C T I V E S
Goals
Examine the body and its functions
Understand reproduction and contraception
Explore HIV and other STIs
Define sexual expression and sexual orientation
Compare healthy and unhealthy relationships
Target Group(s)
Young people in high school
I N T R O D U C T I O N
The following “Teaching and Reference Guide Draft” is the first step in bringing the HIP Corps Prevention Program into a protocol format. This document is not intended as a hard and fast curriculum, but truly a “Guide” for SNMA students who are interested in providing sexual health awareness education, emphasizing HIV/AIDS prevention. Students and their advisors, along with school officials, parents, and the local community may decide to censor some topics addressed in this document. Some of the information contained here is more technical than needed for the typical outreach, but this document is intended to inform SNMA volunteers of the various concerns of today’s teens Those concerns (sex, relationships, peer-pressure) constitute the very real life context within which young people make their decisions. Our intent is to ensure that information is easily available to students, so when a copy of this document is sent via electronic transfer, numerous hyperlinks (shown in blue or violet) will take the reader to additional sources of information Hard copies of this document will be made available to any interested parties. The majority of the information contained in this document was taken from the following three sources and are cited throughout the text:
www.pamf.org (Palo Alto Medical Foundation)
http://health.howstuffworks.com/aids.htm
http://www.cdc.gov/hiv/pubs/facts/condoms.htm
http://www.cdc.gov/hiv/dhap.htm
https://www cdc gov/hiv/dhap/about html
For additional information and activities, please go to:
http://www unicef org/lifeskills/index 14926 html
There are many resources here available for download. The Life Skills Manual is very comprehensive and deals with behavior change and decision making.
http://www.peacecorps.gov/wws/guides/looking/contents.html#grade35
Again, many, many solid resources here are available for download. My Future is My Choice is subtitled “Protecting Our Peers from HIV Infection”; very relevant, indeed.
T H E B A S I C S
M A L E S E X O R G A N S
From the outside, the male has two visible sex organs, the testes and penis. The testes (singular: testis) are the primary male sexual organs in that they make sperm and produce testosterone. The sperm cell is the male sex cell (gamete). Testosterone is the hormone that causes male secondary sex characteristics such as facial and pubic hair, thickened vocal cords and developed muscles.
The testes are housed outside of the main part of the male's body, in a sac called the scrotum. This location is important because in order for the sperm to develop properly, they must be kept at a slightly lower temperature (95 to 97 degrees Fahrenheit, 35 to 36 degrees Celsius) than normal body temperature (98.6 F, 37 C).
The immature sperm travel from each testis to a coiled tube on the outer surface of each testis called the epididymis, where they mature in about 20 days. The sperm exits the body through the penis.
The penis is made of soft, spongy tissue (see How Viagra Works for details). When engorged with blood during sexual excitation and intercourse, the spongy tissue stiffens and causes the penis to become erect, which is important for the penis's main function -- to place the sperm inside the female.
T H E B A S I C S F
All of the female's sexual organs are located within her body except the vulva. The vulva consists of two sets of folded skin (labia major, labia minor) that cover the opening to the reproductive tract, and a small nub of sensitive, erectile tissue (clitoris), which is the remnant of the fetal penis.
The two ovaries are the major female sex organs, the counterpart of the male testes. The ovaries make the eggs, or oocytes, which are the female gametes, and produce estrogen, the female sex hormone. Estrogen causes female secondary sexual characteristics such as pubic hair, breast development, widening of the pelvis and deposition of body fat in hips and thighs. The ovaries are located in the abdomen.
Eggs develop inside the ovary and are released upon ovulation into a tube (the oviduct or Fallopian tube) lined with fingerlike projections. The egg travels through the Fallopian tube, where fertilization can take place, to a muscular chamber called the uterus.
The uterus is where the baby develops. It is made of smooth muscle and is normally about the size and shape of a small pear turned upside down. During pregnancy, it can stretch to about the size of a basketball to hold the developing baby. The base of the uterus (neck of the pear) is a muscular wall called the cervix. In the cervix is a tiny opening, about the size of a pinhead, called the external os. The external os is filled with a thick plug of protein (mucus) that serves as a barrier to the entrance of the uterus. The cervix leads into a smooth-muscle-walled tube called the vagina, or birth canal.
T H E B A S I C S
F E M A L E S E X O R G A N S
The vagina connects the uterus to the outside of the body, and its opening is covered by the labia. The vagina receives the male's penis during sexual intercourse and delivers the baby during childbirth. The vagina is normally narrow (except around the cervix), but can stretch during intercourse and childbirth.
Finally, two sets of glands, the greater vestibular gland (Bartholin's gland) and the lesser vestibular gland, are located on either side of the vagina and empty into the labial folds of skin. The secretions from these glands lubricate the labial folds during sexual excitation and intercourse.
T H E B A S I C S
Two other organs, not located in the reproductive system, are important for sexual function in both males and females:
The hypothalamus in the brain
The hypothalamus has nerve cells that secrete a hormone called gonadotropin releasing hormone (GnRH) into the blood vessels leading to the anterior pituitary gland.
The anterior pituitary gland just beneath the brain
GnRH causes the anterior pituitary cells to release two hormones, luteinizing hormone (LH) and follicle stimulating hormone (FSH), into the general blood circulation.
LH and FSH act on the testes/ovaries to stimulate the making and maturation of the sex cells and the production of sex hormones (testosterone, estrogen, progesterone).
The nerve cells time-release small, low-level spurts of GnRH every 90 minutes, which causes the anterior pituitary to secrete small pulses of LH and FSH. The sex hormones from the testes/ovaries give feedback to the hypothalamus and anterior pituitary to regulate the secretion of GnRH, LH and FSH -- this interplay is called the negative feedback control system. The chemical interplay between the hypothalamus, anterior pituitary gland and the testes/ovaries is important for sexual development, maintaining sexual function and sexual reproduction. An error in this chemical interplay can be a cause of infertility.
T H E B A S I C S
From the time of puberty on, men make sex cells (in the form of sperm cells) continuously. In contrast, by the time a female is born, she has made all of the eggs that she will ever have.
As she reaches puberty, the eggs begin to develop and get released, and this process continues until menopause. In both males and females, the production of sex cells involves meiosis, a type of cell division whereby our two sets of genetic instructions are reduced to one set for the sex cell
Each cell in your body contains a set of chromosomes from your mother (her egg) and your father (his sperm). When you look at human chromosomes, they are X-shaped, except for the male Y chromosome. When your body produces sex cells (sperm or egg, depending on whether you are a male or female), your body must reduce the number of chromosomes by half to go into the sex cells. To do this, it randomly sorts chromosomes from both sets in one cell division and then reduces them by half in another. Therefore, each sperm or egg that your body produces is unique and different -- it contains a different mix of your mother's and father's genes. This is why two brothers in the same family can look and act totally different from one another even though they come from the same parents -- it all depends on which genes (chromosomes) were randomly chosen when producing the sex cells of the mother and father.
T H E B A S I C S
Remember that, biologically, the main goal of sexual reproduction is to have the sperm combine with the egg to make a baby. With respect to the man, age is not critical. Men are capable of producing sperm that can fertilize an egg at any time from the onset of puberty until they die (there have been many cases in which men in their 70s and 80s have conceived children with younger women). In contrast, women typically can release fertilizable eggs from the time of puberty until their late 40s or early 50s. After that time, their ovaries stop releasing eggs and they undergo various biochemical and physiological changes, the sum of which is called menopause.
Although women are capable of conceiving a child from puberty to menopause, the timing of sexual intercourse is critical to the success of sexual reproduction. Women have an ovulatory cycle, or menstrual cycle, made up of complex physiological and biochemical changes that are linked to the timing of reproduction.
In the first phase of the menstrual cycle, a follicle (the cell complex that surrounds and nurtures the egg) grows in the ovary, while the lining of the uterus builds up to receive a fertilized egg. At mid-cycle, when the egg is ready, the ovary releases the egg. This stage is called ovulation and is the optimum time for fertilization to take place. The egg enters the Fallopian tube on its way to the uterus. In the last phase of the menstrual cycle, one of two things happens: If the egg is fertilized, it continues on to the uterus, attaches to the lining and pregnancy begins; if the egg is not fertilized, the uterus sheds its lining (and the now-dead egg), menses begins and another menstrual cycle ensues.
T H E B A S I C S
When a man and a woman engage in sexual activity, each goes through an arousal phase. In both the man and the woman, nerve impulses from the brain cause their heart rates to increase and dilate peripheral blood vessels. They feel warm, and they begin to sweat. The Cowper's glands in the man and the vestibular glands in the woman secrete fluid that lubricates the man's urethra and the woman's labial area and vagina.
The man's brain sends nerve impulses to the blood vessels in his penis and tells the arterioles to dilate and the venules to constrict. The blood flow engorges the spongy tissue of his penis, causing it to become erect. As the couple engages in intercourse, the man inserts his erect penis into the woman's vagina. As intercourse continues, the man reaches a point at which muscle contractions in the epididymis, prostate and seminal vesicles propel semen from the penis into the woman's vagina (ejaculation) at the base of the uterine cervix.
In men who have sex with men, the man inserts his erect penis into the man’s rectum. The man reaches a point at which muscle contraction happens as previously stated. In women, who have sex with women, the vagina is not normally penetrated with sex organs but the body’s response to stimulation is the same.
Muscle contractions in the woman's body periodically dip her cervix into the semen.
Once the semen is deposited at the base of the uterus, the sperm begin a long journey to fertilization.
T H E B A S I C S
S E X U A L I N T E R C O U R S E :
F E R T I L I Z A T I O N
The long journey to fertilization must be completed within 12 to 48 hours, before the sperm die. They must first cross the barrier of the cervix, which will be thin and watery if the woman has just ovulated (for our purposes, we will assume that sexual intercourse has occurred within a couple of hours after ovulation).
Once the sperm have traversed the cervical mucus, they travel up the moist lining of the uterus into the Fallopian tubes (only one of the Fallopian tubes contains an egg, so many sperm travel in the wrong direction). Fewer than 1,000 sperm out of the millions in the semen actually reach the Fallopian tubes.
Many sperm surround the egg in the Fallopian tube The head of each sperm (acrosome) releases enzymes that begin to break down the outer, jelly-like layer of the egg's membrane, trying to penetrate the egg Once a single sperm has penetrated, the cell membrane of the egg changes its electrical characteristics (depolarizes) This electrical signal causes small sacs just beneath the membrane (cortical granules) to dump their contents into the space surrounding the egg The contents swell, pushing the other sperm far away from the egg (cortical reaction) The other sperm die within 48 hours The cortical reaction ensures that only one sperm fertilizes the egg
The fertilized egg is now called a zygote The depolarization caused by sperm penetration results in one last round of division in the egg's nucleus, forming a pronucleus containing only one set of genetic information The pronucleus from the egg merges with the nucleus from the sperm Once the two pronuclei merge, cell division begins immediately
The dividing zygote gets pushed along the Fallopian tube By approximately four days after fertilization, the zygote has about 100 cells and is called a blastocyst. When the blastocyst reaches the uterine lining, it floats for about two days, finally implanting in the uterine wall by the sixth day after fertilization. Once implanted, the blastocyst secretes HCG, which rescues the corpus luteum and signals that a successful pregnancy has begun.
The implanted blastocyst continues developing in the uterus for nine months As the baby grows, the uterus stretches until it is about the size of a basketball
T H E B A S I C S
As you can see from the process of sexual reproduction, there are several ways to prevent sperm and egg from coming together, which is known as contraception.
What is abstinence?
The act of not having sex, which can range from no sexual contact to everything but intercourse.
How does it work?
You refrain from all forms of sexual intercourse.
Does it protect against sexually transmitted infections (STIs)?
Yes! It's the best protection against STIs and the only guarantee against them.
Does it protect against pregnancy?
Yes. It's the best protection and the only guarantee (as long as no semen enters the vagina).
What are the chances of getting pregnant while using abstinence?
There is no chance of getting pregnant as long as semen is kept out of the vagina.
What are the advantages of using abstinence?
There are no hormonal or medical side effects.Abstinence is a good way to REALLY get to know your boyfriend or girlfriend without the complications of sex.
Remember: Abstinence is the only sure way to prevent pregnancy or sexually transmitted diseases, including HIV.
T H E B A S I C S
If you do decide to engage in sexual intercourse, here are some methods to prevent pregnancy. See FDA: Birth Control Guide for details.
Birth control pills - Preventing an egg follicle from developing
Condoms (male/female)
Cervical caps
Sponges
Diaphragms
Placing a barrier between sperm and egg
Spermicides
Killing the sperm
Tubal ligations (in women)
Vasectomies (in men)
Surgical procedures which block the sperm or egg (IUDs)
Timing - avoiding intercourse during the period of maximum fertility
T H E B A S I C S

H I V A N D O T H E R S T I ' S
Sexual activity carries certain risks of diseases caused by the following organisms:
Bacteria (gonorrhea, syphilis, chlamydia)
Protozoa (trichomoniasis)
Viruses (genital herpes, HIV/AIDS)
Sexually Transmitted Infections (STIs) Some 56 million Americans have an STI other than HIV/AIDS, and many more are infected each year. The causative bacterial, viral, or parasitic agents are spread primarily by sexual contact, but may also be spread by the use of infected needles. Some STIs are chronic infections, but many can be cured. Quick diagnosis and treatment are often the keys to cure. The only 100% prevention is abstinence. Maintaining faithful monogamous relations with one's spouse is effective, provided both partners are free of STIs. Safe sex (use of a condom) with a monogamous partner is the next best protection against STIs. Always remember that prevention is better than therapy.
H I V A N D O T H E R S T I ' S
B A C T E R I A L S T I ' S
Gonorrhea ("clap"), a common disease worldwide, is caused by the bacterium Neisseria gonorrhoeae. There are over 650,000 new cases in the U.S. each year. 82% of cases of gonorrhea occur in teenagers and young adults, and females are twice as likely to become infected after one act of intercourse with an infected male as males are after one act of intercourse with an infected female. Gonorrheal infections may be asymptomatic in both sexes. Symptoms of exposure include urethral or vaginal discharge and frequent and painful urination. Bacterial culture confirms the diagnosis. Gonorrhea requires antibiotics to resolve, so see your doctor for appropriate diagnosis and treatment. Penicillin used to be the drug of choice, but many strains have become resistant. Sexual partners should be treated, and intercourse avoided until the infection is cured. Untreated gonorrhea can damage the heart or cause a form of arthritis.
Chlamydia is caused by the bacteria Chlamydia trachomatis.
Infection with chlamydia is often concurrent with gonorrheal infections. Chlamydia is the most frequently reported and fastest-spreading STI in the United States. More than 3 million men and women in the U.S. are diagnosed each year. Infection without symptoms and latent disease is not uncommon.
Males typically experience painful and frequent urination and a urethral discharge 7- 21 days after exposure. Females often do not have any symptoms and the infection is discovered in conjunction with a gonorrheal infection. Chlamydia requires antibiotics to resolve. A physician should be consulted for appropriate diagnosis and treatment. Sexual partners should be treated, and intercourse avoided until the infection is cured.
Pelvic inflammatory disease is a complication of gonorrhea or chlamydia. It is an infection that generally involves the uterus, fallopian tubes, or pelvic area. Symptoms vary but usually include abdominal pain and tenderness, fever, and vaginal discharge.
This is a very serious infection and requires antibiotics to treat and may also require hospitalization. A doctor should be consulted for appropriate diagnosis and treatment. If untreated or inadequately treated, it may result in infertility and/or sterility.
H I V A N D O T H E R S T I ' S
B
A C T E R I A L S T I ' S
Syphilis - There are more than 70,000 new cases of syphilis each year in the U.S. caused by the spirochete bacteria Treponema pallidum.
The risk of infection with syphilis after a single exposure is ~50%. Syphilis has four clinical stages -- primary, secondary, tertiary, and congenital (passed from mother to baby).
The primary stage occurs between 10 and 90 days after infection and causes an ulcer at the site of infection. The primary stage is highly infectious. Secondary syphilis occurs about 6 weeks after the primary stage and causes a rash all over the body, fever, headache, loss of appetite, and joint pain. The tertiary form of syphilis has many different forms and may present without any external signs or symptoms. If untreated, the third stage can affect the heart, brain, or other vital organs.
Syphilis is usually diagnosed by a blood test, The disease can cause many problems in all areas of the body including the heart, brain, skin, bone, upper respiratory tract, and liver. Syphilis requires antibiotics to resolve. Consult a doctor for appropriate diagnosis and treatment.
Bacterial Vaginosis is a vaginal bacterial infection caused by several bacteria that are normally harmless. Signs and symptoms include malodorous vaginal discharge, but you may or may not be symptomatic This infection requires antibiotics to treat Consult a doctor for appropriate diagnosis and treatment.
H I V A N D O T H E R S T I ' S
Trichomoniasis is a readily curable infection caused by the protozoa Trichomonas vaginalis.
Common signs and symptoms include a mild to severe malodorous vaginal discharge, intense itching, and painful urination; males may not have any symptoms. Trichomoniasis requires antibiotic therapy, so see your doctor for appropriate diagnosis and treatment The drug of choice is metronidazole (Flagyl®) It is very effective but may produce several side effects. Both partners should be treated.
H I V A N D O T H E R S
What is Genital Herpes?
The Herpes Simplex Virus (HSV) causes a recurrent, incurable viral disease that has two forms, HSV-1 and HSV-2. HSV-1 generally appears as cold sores around the face-especially the mouth. HSV-2 generally is a sexually transmitted disease that manifests as genital lesions. Herpes zoster, shingles, is a re-manifestation of chickenpox which is herpes varicella.
Can I know when I'm infectious?
No, as many as 50% of patients with genital herpes are shedding the virus without experiencing any of the symptoms. Many cases are transmitted during this time.
Signs and Symptoms
The first episode, initial infection: this presents with flu-like symptoms, clusters of lesions on the genitalia that can ulcerate and spread. It may take 2-3 weeks before the lesions scab over and heal. After the initial infection, the virus settles in the nerve root ganglia -- heads of nerves that run parallel to the spinal cord -- and remains dormant until stress or other factors reactivate it. Recurrent infections begin in about 50% of patients with a "prodrome" pre- reactivation flu-like symptoms and tingling around the area where the lesions will be.
Treatment
There is no cure for herpes, however, there are a few drugs that will help shorten the duration of the symptoms and relieve the discomfort associated with herpes. These are antiviral drugs and they are available by prescription only. Therefore, see your doctor for appropriate diagnosis and treatment.
H I V A N D O T H E R S T I ' S
Acyclovir(Zovirax®)
Once acyclovir enters the body, it is modified to look exactly like a natural nucleotide (nucleotides make up RNA and DNA). It then competes with the natural nucleotides to make the viral RNA. When acyclovir is incorporated into the viral RNA instead of the natural nucleotide, replication of the virus is stopped. Some of the common side effects encountered with acyclovir include headache, nausea, vomiting, dizziness, and loss of appetite.
Valacyclovir(Valtrex®)
Valacyclovir is converted to acyclovir in the body. It acts exactly the same way and has the same side effect profile as acyclovir.
Penciclovir(Denavir®)
Penciclovir, like acyclovir, is modified once it enters the body to look exactly like a natural nucleotide. It then competes with the real nucleotides and when it is used instead of the normal nucleotides, it stops replication of the viral RNA It is available only as a cream and is used to treat herpes sores on the face and lips. Common side effects include dulled sensitivity to touch, altered taste sensation, skin irritation or itching, and skin rash.
Famciclovir(Famvir®)
Famciclovir is nearly identical to Penciclovir except that it has to be altered in the body to Penciclovir first It is the oral form of Penciclovir and comes as tablets With the exception of the fact that is an oral drug, it otherwise acts exactly like Penciclovir. Common side effects include diarrhea, dizziness, headache, tiredness, and nausea.
H I V A N D O T H E R S T I '
V I R A L S T I ' S : H P V
What is Human Papilloma Virus (HPV)?
Some 5 5 million new cases of HPV infection are reported each year in the U S Twenty million Americans, men and women alike, are infected with this virus. HPV is a doublestranded DNA virus that is the causative agent of genital warts. There are more than 65 types of the virus. Infection with specific types of HPV can lead to neoplastic changes in genital epithelia. The lesions are usually papules or plaques that may be hard to see. In women, the infection may be intravaginal or cervical. If the cervix becomes affected, cervical cancer can result Because of the contagious and possibly neoplastic nature of the infection, treatment is necessary. Destructive treatment includes removal of warts by the use of lasers, freezing, or burning. Some medications may be applied by a physician (podophyllin, trichloracetic acid) or the patient with proper training (podofilox, imiquimod), but there are some side effects. These include pain, burning, inflammation, skin erosion, scarring, erythema, and medications that should not be used during pregnancy There is no cure and warts may recur at any time Patients with genital warts are also at risk for other STDs.
H I V A N D O T H
Human Immunodeficiency Virus (HIV) is the virus that causes Acquired Immunodeficiency Syndrome (AIDS). Some 1,000,000 Americans are estimated to be infected with HIV with 40,000 being added each year. Half of these cases are in those under 25 years of age. Those at highest risk have unprotected sex with multiple partners and/or are injection drug users who share needles.
HIV is a virus that affects the human immune system, specifically T-helper cells that have a CD4+ marker on their surface. These T-helper cells normally function to protect against infection.
When HIV enters one of these cells, it is protected by a capsule This capsule breaks open and a single strand of RNA is released along with an enzyme called reverse transcriptase. Reverse transcriptase than converts the single strand of RNA into a double strand of DNA. This DNA is then incorporated into the normal cellular DNA. The rest of the immune system does not respond because the virus is inside the cell. The HIV virus has taken over the cellular machinery and forcing the immune system to make millions of copies of the HIV virus. Infected persons frequently succumb to opportunistic infections
Clinically, HIV presents with flu-like symptoms, and then the symptoms go into dormancy, but the virus continues to replicate. As the amount of HIV virus in the body increases, the immune system is further impaired and opportunistic infections become more common. Some of the most common infections include thrush (fungal infection), Kaposi's Sarcoma (cancer), pneumonia, recurrent herpes infections, and in later stages severe bacterial, protozoal or fungal bloodstream infections. There are many medications available to help slow the progression of HIV, however, no cure is currently known and many infections are drugresistant. Clearly prevention of infection is rational and desirable. Talk to a doctor if you have questions and/or you need diagnosis and treatment.
H I V A N D O T H E R S T I ' S
Unique Features of HIV
The thought of contracting HIV is frightening, and there is a good reason for that fear--the disease is presently incurable, it has a high mortality rate, it spreads quickly, and there is no vaccine to protect against it. In today's world, that combination is rare. For example, smallpox is often fatal, but the disease has been completely contained through vaccinations. Tuberculosis is often fatal but can usually be cured with antibiotics if caught early.
AIDS has been able to infect and kill so many people because of its unique makeup. Let's look at some of the features that make this disease so unusual: HIV spreads by intimate contact with an infected person. Forms of intimate contact that can transmit AIDS include sexual activity and any sort of situation that allows blood from one person to enter another. Especially when you compare it with the many viruses that spread through the air, it would seem like the intimacy involved in the transmission of AIDS would be a limiting factor.
A person can carry and transmit the HIV virus for many years before any symptoms show themselves. A person can be contagious for a decade or more before any visible signs of disease become apparent. In a decade, a promiscuous HIV carrier can potentially infect dozens of people, who each can infect dozens of people, and so on.
The last feature in this list is the one that is truly unique. HIV invades and destroys the immune system -- the system that would normally protect the body from a virus. HIV corrupts and disables the system that should be guarding against HIV
H I V A N D O T H E R S T I ' S
V
I R A L S T I ' S : H I V
How AIDS Works
AIDS (Acquired Immunodeficiency Syndrome) is one of the worst pandemics the world has ever known. HIV (Human Immunodeficiency Virus), the virus that causes AIDS, was first discovered in 1981 in a remote area of central Africa. It has since swept across the globe, infecting millions in a relatively short period of time. AIDS has killed 28.1 million people that we know of, with 3 million people dying in the year 2002 alone. While many cases go unreported, the prevalence of the disease is increasing. See below for some comparisons:
The flu pandemic of 1918 killed approximately 20 million people worldwide. World War II killed approximately 40 million people.Clearly the AIDS pandemic has and will continue to have a significant and global impact.
How HIV Enters the Body
In the United States, given the current distribution of HIV in the population, there is better than a one in 1,000 chance of contracting HIV during an unprotected heterosexual encounter, according to the Centers for Disease Control and Prevention (CDC). In some locations, the chances are even higher. Unprotected sex is the most common way of transmitting HIV. Your chances for infection increase with each new partner. Here is a list of ways in which HIV can be transmitted:
Sexual contact
Sharing contaminated intravenous needles
Breastfeeding (mother to baby)Infected mother to fetus during pregnancy or birth
Blood transfusions (rare in countries where blood is screened for HIV antibodies)
There is also a slight chance of transmission through open-mouth kissing and biting. However, there have been very few cases of HIV being transmitted through either method. In fact, the CDC has investigated only one case in which HIV infection was attributed to open-mouth kissing.HIV does not transmit through the air or surface contact like cold and flu viruses do. HIV is a fragile virus and doesn't survive well outside the human body. This fragility makes the possibility of environmental transmission very remote. Outside of a host cell, HIV doesn't survive for very long. In laboratory studies, the CDC has shown that once the fluid (blood, sweat, tears, etc..) containing the HIV virus dries, the risk of environmental transmission is nearly zero.
H I V A N D O T H E R S T I ' S
V I R A L S T I ' S : H I V
HIV and Its Transmission
Research has revealed a great deal of valuable medical, scientific, and public health information about the human immunodeficiency virus (HIV) and acquired immunodeficiency syndrome (AIDS). The ways in which HIV can be transmitted have been clearly identified. Unfortunately, false information or statements that are not supported by scientific findings continue to be shared widely through the Internet or popular press Therefore, the Centers for Disease Control and Prevention (CDC) has prepared this fact sheet to correct a few misperceptions about HIV.
How HIV is Transmitted HIV is spread by sexual contact with an infected person, by sharing needles and/or syringes (primarily for drug injection) with someone who is infected, or, less commonly (and now very rare in countries where blood is screened for HIV antibodies), through transfusions of infected blood or blood clotting factors. Babies born to HIV-infected women may become infected before or during birth or through breast-feeding after birth.In the health care setting, workers have been infected with HIV after being stuck with needles containing HIV-infected blood or, less frequently, after infected blood gets into a worker’s open cut or a mucous membrane (for example, the eyes or inside of the nose). There has been only one instance of patients being infected by a health care worker in the United States; this involved HIV transmission from one infected dentist to six patients.
Investigations have been completed involving more than 22,000 patients of 63 HIV-infected physicians, surgeons, and dentists, and no other cases of this type of transmission have been identified in the United States.
H I V A N D
Some people fear that HIV might be transmitted in other ways; however, no scientific evidence to support any of these fears has been found. If HIV were being transmitted through other routes (such as through air, water, or insects), the pattern of reported AIDS cases would be much different from what has been observed. For example, if mosquitoes could transmit HIV infection, many more young children and preadolescents would have been diagnosed with AIDS.
All reported cases suggesting new or potentially unknown routes of transmission are thoroughly investigated by state and local health departments with the assistance, guidance, and laboratory support from CDC No additional routes of transmission have been recorded, despite a national sentinel system designed to detect just such an occurrence
The following paragraphs specifically address some of the common misperceptions about HIV transmission
HIV in the Environment
Scientists and medical authorities agree that HIV does not survive well in the environment, making the possibility of environmental transmission remote.HIV is found in varying concentrations or amounts in blood, semen, vaginal fluid, breast milk, saliva, and tears. (See page 3, Saliva, Tears, and Sweat.) To obtain data on the survival of HIV, laboratory studies have required the use of artificially high concentrations of laboratory-grown virus. Although these unnatural concentrations of HIV can be kept alive for days or even weeks under precisely controlled and limited laboratory conditions, CDC studies have shown that drying of even these high concentrations of HIV reduces the amount of infectious virus by 90 to 99 percent within several hours. Since the HIV concentrations used in laboratory studies are much higher than those actually found in blood or other specimens, drying of HIV- infected human blood or other body fluids reduces the theoretical risk of environmental transmission to that which has been observed--essentially zero. Incorrect interpretation of conclusions drawn from laboratory studies has unnecessarily alarmed some people.
H I V A N D O T H
Results from laboratory studies should not be used to assess the specific personal risk of infection because (1) the amount of virus studied is not found in human specimens or elsewhere in nature, and (2) no one has been identified as infected with HIV due to contact with an environmental surface. Additionally, HIV is unable to reproduce outside its living host (unlike many bacteria or fungi, which may do so under suitable conditions), except under laboratory conditions, therefore, it does not spread or maintain infectiousness outside its host.
Households Although HIV has been transmitted between family members in a household setting, this type of transmission is very rare. These transmissions are believed to have resulted from contact between skin or mucous membranes and infected blood. To prevent even such rare occurrences, precautions, as described in previously published guidelines, should be taken in all settings "including the home" to prevent exposures to the blood of persons who are HIV infected, at risk for HIV infection, or whose infection and risk status are unknown. For example,
Gloves should be worn during contact with blood or other body fluids that could possibly contain visible blood, such as urine, feces, or vomit
Cuts, sores, or breaks on both the care giver’s and patient’s exposed skin should be covered with bandages
Hands and other parts of the body should be washed immediately after contact with blood or other body fluids, and surfaces soiled with blood should be disinfected appropriately
Practices that increase the likelihood of blood contact, such as sharing of razors and toothbrushes, should be avoided Needles and other sharp instruments should be used only when medically necessary and handled according to recommendations for health-care settings. (Do not put caps back on needles by hand or remove needles from syringes. Dispose of needles in puncture-proof containers
H I V A N D O T H E R S T I ' S
Businesses and Other Settings
There is no known risk of HIV transmission to co-workers, clients, or consumers from contact in industries such as food-service establishments (see information on survival of HIV in the environment). Food-service workers known to be infected with HIV need not be restricted from work unless they have other infections or illnesses (such as diarrhea or hepatitis A for which any food-service worker, regardless of HIV infection status, should be restricted. CDC recommends that all food-service workers follow recommended standards and practices of good personal hygiene and food sanitation.
In 1985, CDC issued routine precautions that all personal-service workers (such as hairdressers, barbers, cosmetologists, and massage therapists) should follow, even though there is no evidence of transmission from a personal-service worker to a client or vice versa. Instruments that are intended to penetrate the skin (such as tattooing and acupuncture needles, ear-piercing devices) should be used once and disposed of or thoroughly cleaned and sterilized. Instruments not intended to penetrate the skin but which may become contaminated with blood (for example, razors) should be used for only one client and disposed of or thoroughly cleaned and disinfected after each use. Personal-service workers can use the same cleaning procedures that are recommended for health care institutions.
CDC knows of no instances of HIV transmission through tattooing or body piercing, although Hepatitis B virus has been transmitted during some of these practices. One case of HIV transmission from acupuncture has been documented. Body piercing (other than ear piercing) is relatively new in the United States, and the medical complications for body piercing appear to be greater than for tattoos. Healing of piercings generally will take weeks, and sometimes even months, and the pierced tissue could conceivably be abraded (torn or cut) or inflamed even after healing. Therefore, a theoretical HIV transmission risk does exist if the unhealed or abraded tissues come into contact with an infected person’s blood or other infectious body fluid.Additionally, HIV could be transmitted if instruments contaminated with blood are not sterilized or disinfected between clients.
H I V A N D O T H E R S T I ' S
Kissing
Casual contact through closed-mouth or "social" kissing is not a risk for transmission of HIV. Because of the potential for contact with blood during "French" or open-mouth kissing, CDC recommends against engaging in this activity with a person known to be infected However, the risk of acquiring HIV during open-mouth kissing is believed to be very low. CDC has investigated only one case of HIV infection that may be attributed to contact with blood during open-mouth kissing.
Biting
In 1997, CDC published findings from a state health department investigation of an incident that suggested blood-to-blood transmission of HIV by a human bite. There have been other reports in the medical literature in which HIV appeared to have been transmitted by a bite. Severe trauma with extensive tissue tearing and damage and the presence of blood was reported in each of these instances Biting is not a common way of transmitting HIV In fact, there are numerous reports of bites that did not result in HIV infection.
Saliva, Tears, and Sweat
HIV has been found in saliva and tears in very low quantities from some AIDS patients. It is important to understand that finding a small amount of HIV in body fluid does not necessarily mean that HIV can be transmitted by that body fluid. HIV has not been recovered from the sweat of HIV-infected persons. Contact with saliva, tears, or sweat has never been shown to result in the transmission of HIV.
Insects
From the onset of the HIV epidemic, there has been concern about transmission of the virus by biting and bloodsucking insects. However, studies conducted by researchers at CDC and elsewhere have shown no evidence of HIV transmission through insects--even in areas where there are many cases of AIDS and large populations of insects such as mosquitoes.Lack of such outbreaks, despite intense efforts to detect them, supports the conclusion that HIV is not transmitted by insects.
The results of experiments and observations of insect biting behavior indicate that when an insect bites a person, it does not inject its own or a previously bitten person’s or animal’s blood into the next person bitten. Rather, it injects saliva, which acts as a lubricant or anticoagulant so the insect can feed efficiently. Such diseases as yellow fever and malaria are transmitted through the saliva of specific species of mosquitoes. However, HIV lives for only a short time inside an insect and, unlike organisms that are transmitted via insect bites, HIV does not reproduce (and does not survive) in insects. Thus, even if the virus enters a mosquito or another sucking or biting insect, the insect does not become infected and cannot transmit HIV to the next human it feeds on or bites. HIV is not found in insect feces.
There is also no reason to fear that a biting or bloodsucking insect, such as a mosquito, could transmit HIV from one person to another through HIV- infected blood left on its mouth parts. Two factors serve to explain why this is so--first, infected people do not have constant, high levels of HIV in their bloodstreams and, second, insect mouth parts do not retain large amounts of blood on their surfaces. Further, scientists who study insects have determined that biting insects normally do not travel from one person to the next immediately after ingesting blood. Rather, they fly to a resting place to digest this blood meal.
H I V A N D O T H E R S T I ' S
Effectiveness of Condoms
Condoms are classified as medical devices and are regulated by the Food and Drug Administration (FDA). Condom manufacturers in the United States test each latex condom for defects, including holes, before it is packaged. The proper and consistent use of latex or polyurethane (a type of plastic) condoms when engaging in sexual intercourse--vaginal, anal, or oral--can greatly reduce a person’s risk of acquiring or transmitting sexually transmitted diseases, including HIV infection
There are many different types and brands of condoms available--however, only latex or polyurethane condoms provide a highly effective mechanical barrier to HIV. In laboratories, viruses occasionally have been shown to pass through natural membrane ("skin" or lambskin) condoms, which may contain natural pores and are therefore not recommended for disease prevention (they are documented to be effective for contraception) Women may wish to consider using the female condom when a male condom cannot be used.
For condoms to provide maximum protection, they must be used consistently (every time) and correctly. Several studies of correct and consistent condom use clearly show that latex condom breakage rates in this country are less than 2 percent. Even when condoms do break, one study showed that more than half of such breaks occurred prior to ejaculation.
When condoms are used reliably, they have been shown to prevent pregnancy up to 98 percent of the time among couples using them as their only method of contraception
Similarly, numerous studies among sexually active people have demonstrated that a properly used latex condom provides a high degree of protection against a variety of sexually transmitted diseases, including HIV infection.In the next section, you will learn what happens once the HIV virus enters the body, and how it attacks the immune system.
H I V A N D O T H E R S T I ' S
The Lifecycle of HIV
Like all viruses, HIV treads the fine line that separates living things from nonliving things. Viruses lack the chemical machinery that human cells utilize to support life. So, HIV requires a host cell to stay alive and replicate. To replicate, the virus creates new virus particles inside a host cell and those particles carry the virus to new cells. Fortunately, the virus particles are fragile
Viruses, like HIV, don't have cell walls or a nucleus. Basically, viruses are made up of genetic instructions wrapped inside a protective shell An HIV virus particle, called a virion, is spherical in shape and has a diameter of about one 10,000th of a millimeter.
HIV infects one particular type of immune system cell. This cell is called the CD4+T cell, also known as a T-helper cell (see How the Immune System Works for details on T cells) Once infected, the T-helper cell turns into an HIV-replicating cell. T-helper cells play a vital role in the body's immune response. There are typically 1 million T-cells per one milliliter of blood. HIV will slowly reduce the number of T-cells until the person develops AIDS.
H I V A N D O T H E R S T I ' S
How HIV Infects the Body
To understand how HIV infects the body, let's first look at the virus's basic structure. Here are the basic parts of the HIV virus:
Viral envelope
This is the outer coat of the virus. It is composed of two layers of fatty molecules, called lipids. Embedded in the viral envelope are proteins from the host cell. There are also about 72 copies of Env protein, which protrudes from the envelope surface. Env consists of a cap made of three or four molecules called glycoprotein (gp) 120, and a stem consisting of three to four gp41 molecules. p17 protein
The HIV matrix protein that lies between the envelope and core
Viral core
Inside the envelope is the core, which contains 2,000 copies of the viral protein, p24. These proteins surround two single strands of HIV RNA, each containing a copy of the virus's nine genes. Three of these genes--gag, pol and env-- contain information needed to make structural proteins for new virions.
HIV is a retrovirus, which means it has genes composed of ribonucleic acid (RNA) molecules. Like all viruses, HIV replicates inside host cells. It's considered a retrovirus because it uses an enzyme, reverse transcriptase, to convert RNA into DNA.
H I V A N D O T H E R S T I ' S
Once the HIV virus enters the body, it heads for the lymphoid tissues, where it finds T-helper cells. Let's look at how the HIV virus infects immune system cells and replicates:
Binding
The HIV attaches to the immune cell when the gp120 protein of the HIV virus binds with the CD4 protein of the T-helper cell The viral core enters the T- helper cell and the virion's protein-membrane fuses with the cell membrane.
Reverse transcription
The viral enzyme, reverse transcriptase, copies the virus's RNA into DNA.
Integration
The newly created DNA is carried into the cell's nucleus by the enzyme, viral integrase, and it binds with the cell's DNA HIV DNA is called a provirus
Transcription
The viral DNA in the nucleus separates and creates messenger RNA (mRNA), using the cell's own enzymes. The mRNA contains the instructions for making new viral proteins.
Translation
The mRNA is carried back out of the nucleus by the cell's enzymes The virus then uses the cell's natural protein-making mechanisms to make long chains of viral proteins and enzymes.
Assembly
RNA and viral enzymes gather at the edge of the cell. An enzyme, called protease, cuts the polypeptides into viral proteins.
Budding
New HIV virus particles pinch out from the cell membrane and breakaway with a piece of the cell membrane surrounding them. This is how enveloped viruses leave the cell. In this way, the host cell is not destroyed.
H I V A N D O T H E R S T I ' S V
The World Context of HIV
No one dies from AIDS or HIV specifically. Instead, an AIDS-infected person dies from infections, because his or her immune system has been dissipated. An AIDS patient could die from the common cold as easily as he or she could from cancer. The person's body cannot fight off the infection, and he or she eventually dies
To understand the devastation of AIDS, you have to understand the high mortality rate of people who develop the disease. If you counted every person in the city of Chicago, which is about 3 million, you would get the idea of how many people died worldwide from AIDS in 2002. Basically, that means that each year AIDS kills the same number of people that populate the third-largest city in the United States.
More than 44 million people are infected with the HIV virus worldwide, with as many as 29.58.2 million of those cases in sub-Saharan Africa. Additionally, another 1.75.3 million new HIV infections occurred in 201802, which represents almost 15,000 new cases per day. The regions with the greatest number of people living HIV/AIDS, according to the World Health Organization, include:
Sub-Saharan Africa - 29.54million
South and Southeast Asia – 4.96
million
Latin America - 1.5 million
North America - 980,000
Americas – 3.5 million
Eastern Europe/Central Asia - 1.2
million
H I V A N D O T H E R S T I ' S
V I R A L S T I ' S : H I V
AIDS is clearly one of the worst health crises facing the world today. Without any truly effective treatment, most health experts are putting an emphasis on prevention to stop the spread of HIV. To learn more about HIV and AIDS, go to the next section.
H I V A N D O T H E R S T I ' S
Male Latex Condomsvand Sexually Transmitted Diseases
In June 2000, the National Institutes of Health (NIH), in collaboration with the Centers for Disease Control and Prevention (CDC), the Food and Drug Administration (FDA), and the United States Agency for International Development (USAID), convened a workshop to evaluate the published evidence establishing the effectiveness of latex male condoms in preventing STDs, including HIV. A summary report from that workshop was completed in July 2001 (http://www.niaid.nih.gov/dmid/stds/condomreport.pdf). This fact sheet is based on the NIH workshop report and additional studies that were not reviewed in that report or were published subsequent to the workshop (see “Condom Effectiveness” for additional references). Most epidemiologic studies comparing rates of STD transmission between condom users and non-users focus on penile-vaginal intercourse.
Recommendations concerning the male latex condom and the prevention of sexually transmitted infections (STI's), including human immunodeficiency virus (HIV), are based on information about how different STI's are transmitted, the physical properties of condoms, the anatomic coverage or protection that condoms provide, and epidemiologic studies of condom use and STI risk.
The surest way to avoid transmission of sexually transmitted diseases is to abstain from sexual intercourse, or to be in a long-term mutually monogamous relationship with a partner who has been tested and you know is uninfected.For persons whose sexual behaviors place them at risk for STI's, correct and consistent use of the male latex condom can reduce the risk of STI transmission. However, no protective method is 100% effective, and condom use cannot guarantee absolute protection against any STI. Furthermore, condoms lubricated with spermicides are no more effective than other lubricated condoms in protecting against the transmission of HIV and other STI's. In order to achieve the protective effect of condoms, they must be used correctly and consistently. Incorrect use can lead to condom slippage or breakage, thus diminishing their protective effect.Inconsistent use, e.g., failure to use condoms with every act of intercourse, can lead to STI transmission because transmission can occur with a single act of intercourse.
While condom use has been associated with a lower risk of cervical cancer, the use of condoms should not be a substitute for routine screening with Pap smears to detect and prevent cervical cancer.
H I V A N D O T H E R S T I ' S
Sexually Transmitted Infections, Including HIV
Latex condoms, when used consistently and correctly, are highly effective in preventing transmission of HIV, the virus that causes AIDS. In addition, consistent and correct use of latex condoms can reduce the risk of other sexually transmitted infections (STI's), including discharge and genital ulcer diseases. While the effect of condoms in preventing human papillomavirus (HPV) infection is unknown, condom use has been associated with a lower rate of cervical cancer, an HPV-associated disease.
There are two primary ways that STDs can be transmitted. Human immunodeficiency virus (HIV), as well as gonorrhea, chlamydia, and trichomoniasis – the discharge diseases – are transmitted when infected semen or vaginal fluids contact mucosal surfaces (e.g., the male urethra, the vagina or cervix). In contrast, genital ulcer diseases – genital herpes, syphilis, and chancroid – and human papillomavirus are primarily transmitted through contact with infected skin or mucosal surfaces.
Laboratory studies have demonstrated that latex condoms provide an essentially impermeable barrier to particles the size of STD pathogens.
The theoretical basis for protection. Condoms can be expected to provide different levels of protection for various sexually transmitted diseases, depending on differences in how the diseases are transmitted. Because condoms block the discharge of semen or protect the male urethra against exposure to vaginal secretions, a greater level of protection is provided for the discharge diseases. A lesser degree of protection is provided for the genital ulcer diseases or HPV because these infections may be transmitted by exposure to areas, e.g., infected skin or mucosal surfaces, that are not covered or protected by the condom.
Epidemiologic studies seek to measure the protective effect of condoms by comparing rates of STDs between condom users and nonusers in real-life settings. Developing such measures of condom effectiveness is challenging. Because these studies involve private behaviors that investigators cannot observe directly, it is difficult to determine accurately whether an individual is a condom user or whether condoms are used consistently and correctly. Likewise, it can be difficult to determine the level of exposure to STDs among study participants. These problems are often compounded in studies that employ a “retrospective” design, e.g., studies that measure behaviors and risks in the past.
H
As a result, observed measures of condom effectiveness may be inaccurate. Most epidemiologic studies of STDs, other than HIV, are characterized by these methodological limitations, and thus, the results across them vary widely--ranging from demonstrating no protection to demonstrating substantial protection associated with condom use. This inconclusiveness of epidemiologic data about condom effectiveness indicates that more research is needed--not that latex condoms do not work. For HIV infection, unlike other STDs, a number of carefully conducted studies, employing more rigorous methods and measures, have demonstrated that consistent condom use is a highly effective means of preventing HIV transmission.
Another type of epidemiologic study involves the examination of STD rates in populations rather than individuals. Such studies have demonstrated that when condom use increases within population groups, rates of STDs decline in these groups. Other studies have examined the relationship between condom use and the complications of sexually transmitted infections. For example, condom use has been associated with a decreased risk of cervical cancer – an HPV associated disease.
The following includes specific information for HIV, discharge diseases, genital ulcer diseases, and human papillomavirus, including information on laboratory studies, the theoretical basis for protection, and epidemiologic studies.
H I V A N D O T H E R S T I ' S
HIV/AIDS
AIDS is, by far, the deadliest sexually transmitted disease, and considerably more scientific evidence exists regarding condom effectiveness for the prevention of HIV infection than for other STDs. The body of research on the effectiveness of latex condoms in preventing sexual transmission of HIV is both comprehensive and conclusive. In fact, the ability of latex condoms to prevent transmission of HIV has been scientifically established in “real-life” studies of sexually active couples as well as in laboratory studies.
Laboratory studies have demonstrated that latex condoms provide an essentially impermeable barrier to particles the size of STD pathogens.Theoretical basis for protection. Latex condoms cover the penis and provide an effective barrier to exposure to secretions such as semen and vaginal fluids, blocking the pathway of sexual transmission of HIV infection.
Epidemiologic studies that are conducted in real-life settings, where one partner is infected with HIV and the other partner is not, demonstrate conclusively that the consistent use of latex condoms provides a high degree of protection.
Discharge Diseases, Including Gonorrhea, Chlamydia, and Trichomoniasis
Gonorrhea, chlamydia, and trichomoniasis are termed discharge diseases because they are sexually transmitted by genital secretions, such as semen or vaginal fluids. HIV is also transmitted by genital secretions.
Laboratory studies have demonstrated that latex condoms provide an essentially impermeable barrier to particles the size of STD pathogens.
Theoretical basis for protection. The physical properties of latex condoms protect against discharge diseases such as gonorrhea, chlamydia, and trichomoniasis, by providing a barrier to the genital secretions that transmit STD- causing organisms.
Epidemiologic studies that compare infection rates among condom users and nonusers provide evidence that latex condoms can protect against the transmission of chlamydia, gonorrhea and trichomoniasis. However, some other epidemiologic studies show little or no protection against these infections. Many of the available epidemiologic studies were not designed or conducted in ways that allow for accurate measurement of condom effectiveness against the discharge diseases. More research is needed to assess the degree of protection latex condoms provide for discharge diseases, other than HIV.
H I V A N D O T H E R S T I ' S
Genital Ulcer Diseases and Human Papillomavirus
Genital ulcer diseases and HPV infections can occur in both male and female genital areas that are covered or protected by a latex condom as well as in areas that are not covered. Consistent and correct use of latex condoms can reduce the risk of genital herpes, syphilis, and chancroid only when the infected area or site of potential exposure is protected. While the effect of condoms in preventing human papillomavirus infection is unknown, condom use has been associated with a lower rate of cervical cancer, an HPV associated disease.
Genital ulcer diseases include genital herpes, syphilis, and chancroid. These diseases are transmitted primarily through “skin-to-skin” contact from sores/ulcers or infected skin that looks normal. HPV infections are transmitted through contact with infected genital skin or mucosal surfaces/fluids. Genital ulcer diseases and HPV infection can occur in male or female genital areas that are, or are not, covered (protected by the condom).
Laboratory studies have demonstrated that latex condoms provide an essentially impermeable barrier to particles the size of STD pathogens.
Theoretical basis for protection. Protection against genital ulcer diseases and HPV depends on the site of the sore/ulcer or infection. Latex condoms can only protect against transmission when the ulcers or infections are in genital areas that are covered or protected by the condom. Thus, consistent and correct use of latex condoms would be expected to protect against transmission of genital ulcer diseases and HPV in some, but not all, instances.
Epidemiologic studies that compare infection rates among condom users and nonusers provide evidence that latex condoms can protect against the transmission of syphilis and genital herpes. However, some other epidemiologic studies show little or no protection. Many of the available epidemiologic studies were not designed or conducted in ways that allow for accurate measurement of condom effectiveness against the genital ulcer diseases. No conclusive studies have specifically addressed the transmission of chancroid and condom use, although several studies have documented a reduced risk of genital ulcers in settings where chancroid is a leading cause of genital ulcers. More research is needed to assess the degree of protection latex condoms provide for the genital ulcer diseases.
While some epidemiologic studies have demonstrated lower rates of HPV infection among condom users, most have not. It is particularly difficult to study the relationship between condom use and HPV infection because HPV infection is often intermittently detectable and because it is difficult to assess the frequency of either existing or new infections. Many of the available epidemiologic studies were not designed or conducted in ways that allow for accurate measurement of condom effectiveness against HPV infection.
A number of studies, however, do show an association between condom use and a reduced risk of HPV-associated diseases, including genital warts, cervical dysplasia, and cervical cancer. The reason for the lower rates of cervical cancer among condom users observed in some studies is unknown. HPV infection is believed to be required, but not by itself sufficient, for cervical cancer to occur.Co-infections with other STDs may be a factor in increasing the likelihood that HPV infection will lead to cervical cancer. More research is needed to assess the degree of protection latex condoms provide for both HPV infection and HPV- associated diseases, such as cervical cancer.
More Information www.HowStuffWorks.com Articles
How Human Reproduction Works
How Viruses Work
How Your Immune System Works
How Blood Works
How Cells Work
More Information for Research purposes
AIDS101.com
Aids Action Committee
AIDS Education Global Information System
World AIDS Day
The Body: An AIDS and HIV Information Resource
CDC: Division of HIV/AIDS Prevention
CDC National Prevention Information Network: HIV/AIDS
CNN - AIDS: 20 Years of an Epidemic
The HIV Life Cycle
HIV Sequence Database
HealingWell.com: HIV/AIDS Resource Center
JAMA - HIV/AIDS Resource Center
UNAIDS
State Criminal Statutes on HIV Transmission
NY Times: Selected articles and timeline
fightAIDS@home:Go to battle against AIDS with your computer
T E E N S E X U A L I T Y ,
R E L A T I O N S H I P S , A N
Everyone is sexual. What that means, exactly, is the purpose of this section of our site. You may have questions about how your body is changing into that of an adult, or about the feelings and emotions you have. It's natural, and your reactions to these changes are under your control To make it all easier, learn what you can Talk to your parents, other adults you trust, friends, or your doctor. Make safe decisions about how you express your sexuality, and you will be fine. If you do not find the answers to your questions on this Web site, talk to your parents or a doctor.Sexuality is an important aspect of life, and adolescence is a critical period in the development of sexual values, attitudes, and behavior. The advent of puberty, the power of peer-group expectations, and the communication of mixed messages about sex make dealing with sexuality a difficult but exciting challenge for adolescents
Pleasure, Virginity, and Sexual Responsibility
The question, "Am I ready to have sex?" doesn't have an easy answer. There are many things to consider and many responsibilities that come with having sex. We encourage you to talk with a parent, guardian, doctor, teacher, older sister, or older brother; someone with knowledge that might help you to think your decision through. We do understand that talking about sex may be uncomfortable for you. But having someone available to answer your specific questions and having someone who understands you can be a tremendous help when deciding "if" to have sex.
Masturbation
There is no doubt about it, sexual pleasure is one of the best feelings in the world. Most people's first experience with sexual pleasure and orgasm is through masturbation. There are many feelings and opinions about "getting off" through masturbation (sometimes referred to as solo sex).
Most people's first experience with sexual pleasure and orgasm is through masturbation. There are many feelings and opinions about "getting off" through masturbation (sometimes referred to as solo sex).
Humans can become sexually aroused and reach orgasm without partners, and at any age Orgasm without a partner may occur involuntarily while the person is asleep, or it may be brought about voluntarily. Masturbation refers to the second type - any deliberate bodily selfstimulation that produces a sexual response.
Self-stimulation is also known as autoerotic or solitary sexual behavior. Besides masturbation, self-stimulation includes erotic fantasy and nocturnal emissions (also called wet dreams), with erotic fantasy being the most common.
T E E N S E X U A L I T Y ,
R E L A T I O N S H I P S , A N D
Common Questions about Masturbation
What positive functions do fantasies fulfill in an adolescent's erotic life?
They are a source of pleasurable sexual arousal. They act as a substitute for the satisfaction of unattainable or inappropriate sexual needs or goals. They provide an opportunity for adolescents to recognize their sexual needs and preferences, and to rehearse these in a way that is non-threatening.
What negative effects can fantasies have on an adolescent's erotic life?
They can provoke anxieties and guilt about sexual feelings, which may be perceived as perverted or forbidden.
What do we know about boys' wet dreams or nocturnal emissions?
Although wet dreams are involuntary, they can cause a great deal of embarrassment, and even guilt, in the morning. It's important to remember, however, that nocturnal emissions are a normal and healthy part of adolescence.
What are the facts about masturbation?
Masturbation is tension-relieving and enjoyable and does not cause physical harm. Many cultures accept it as a normal part of sexuality, although ours does not. Masturbation is the most common source of orgasm for both males and females, and for two out of three boys, the source of their first ejaculation. Girls seem to start masturbating earlier than boys but are less likely to admit to it. Is it normal to masturbate?
What do we know about boys' wet dreams or nocturnal emissions?
Although wet dreams are involuntary, they can cause a great deal of embarrassment, and even guilt, in the morning. It's important to remember, however, that nocturnal emissions are a normal and healthy part of adolescence.
What are the facts about masturbation?
Masturbation is tension-relieving and enjoyable and does not cause physical harm. Many cultures accept it as a normal part of sexuality, although ours does not. Masturbation is the most common source of orgasm for both males and females, and for two out of three boys, the source of their first ejaculation. Girls seem to start masturbating earlier than boys but are less likely to admit to it. Is it normal to masturbate?
Is it normal to masturbate?
Yes. Many people do -- but it is also normal not to masturbate. Children frequently masturbate and should be encouraged to do it privately.
Can a person masturbate too much?
Yes, if it interferes with other aspects of your life, such as relationships, school or work. What about sexual activity with someone else?
Whether it is your first kiss, touching, oral sex or "going all the way," sexual activity with a partner is a powerful experience. There are choices to be made about how far you go and what responsibility you have to protect your partner and yourself from disease or pregnancy. This section deals with these complex issues.
R E L A T I O N S H I P S , A N D C H O I C E S
Virginity
What does "virginity" really mean?
The definition has changed greatly from the origination of the word, with its transformation to a sexual term in medieval times and today’s adaptation of the word. Below is some history about "virginity" you might find of interest.
Virgo – Origination of "Virgin"
"Virgin" originated from the Greek and Latin word "Virgo," or maiden. It was used often in Greek mythology to classify several goddesses such as Artemis (also known as Diana) and Hestia. Virgin was a label of strength and independence -- it described the goddesses who were immune to the temptations of Dionysus, Greek god of seduction and wine. Artemis is the Greek virgin goddess of the moon and the hunt; she protects women in labor, small children and wild animals. Hestia is the Greek virgin goddess of the hearth. She never takes part in the struggle of men and gods. Virginity was once a term of power.
Medieval Transformation of Virgin
In medieval times, virginity became a sexual term for a heterosexual woman in a physical state of not having had been penetrated by a penis. "Virginity" was classified as a gift from the Christian God only to be released by a "husband." It was expected for a woman to remain chaste until marriage; a woman broke her family’s honor if she was not chaste and was often punished. Tests of chastity, both medical and mystical, were used on women to verify their status. One such test was checking for a hymen, or thin flap of skin located ½ inch inside most women’s vaginas upon birth. If the hymen was still intact, the woman was said to be "virgin." This test had been developed or adopted by various other cultures as well. T E E N S
R E L A T I O N S H I P S , A N D C H O I C E S
Today’s Interpretation
n the last few decades, the term or label "virgin" has become confusing as we try to label persons of both genders -- as well as trans-gendered persons and all persons of sexual orientations (straight, gay and bisexual).
The old concept of checking for a woman’s hymen to determine if she is a virgin is being thrown out as more is understood about the hymen. Not all women are born with hymens, some are born without fully intact hymens, and the membrane is so thin that it often breaks with normal physical activity such as running, gymnastics or horseback riding.
Today it’s assumed that "virgin" means not having had been penetrated sexually. But what is considered "de-virginizing" penetration is still unclear -- does it mean penetration by a penis, finger, tongue or experience alone? Even more confusing is how society judges a "virgin."
Sometimes the name is used condescendingly, sometimes in high regard and sometimes simply just as a fact. So, there you have it -- the history and confusion of the word "virgin." It still leaves a question as to what "virginity" really means. As society is still confused, it’s up to us to develop our own personal interpretation of the word. Many would like to regain the association of the word "virgin" with power, extending to all persons However, you decide to personalize the term, don’t force your interpretation on others. If your potential partner discusses "virginity" versus "non-virginity" make sure you are clear on your definitions.
The First Time
Sometimes it seems like "everyone" your age is having sex Forget It! What other people do doesn't matter Only you can answer the question: Is this the right time for me?
Asking questions of yourself and your partner, talking to people with experience, getting prepared and understanding what the first time might be like can help you decide whether you are ready for sex. What won't help you is making the choice while under the influence of alcohol, drugs or pressure from a partner or peers.
Question Yourself
What are your own attitudes toward sex, and what do you really know? Getting to the heart of that answer can be harder than it seems. Figure out how you feel first, even before you talk to your partner. As a guide, run through the following questions and write down your responses.
What do you know about sexually transmitted infections (STIs)?
What do you know about pregnancy?
Do you know how to lower the chance of pregnancy and STIs?
Can you and your partner talk openly about sex, and prevention of pregnancy, STIs and HIV?
If you or your partner has an STI, can you discuss the infection and how to prevent passing it?
How does having sex fit in with your personal values?
How does sex fit in with the values of your culture, family and religion?
Do you trust and respect your partner?
Does your partner trust and respect you?
Do you or your partner feel pressured about sex?
How well do you know how your partner likes to be touched and what your partner likes and dislikes?
How well does your partner know how you like to be touched and what you like and dislike?
What will you and your partner do if sex results in pregnancy and/or disease?
R E L A T I O N S H I P S , A N D C H O I C E S
When Sex Turns Ugly
Sex, in itself, is not a bad thing -- in fact sex can feel really good. But some bad things can happen if you have unsafe sex or sex when you are not emotionally ready to handle the responsibility of having sex. The consequences of having sex that is unsafe (i.e., allowing exchange of bodily fluids) or sex that is not based on respect and mutual readiness (i.e., both people have thought and talked about it) include:
Sexually transmitted infections (STI's)--Catching a bug (see section above on STI’s and HIV)
Rape, Sexual Assault, and Sexual harassment--Unwanted advances
T E E N S E X U A L I T Y ,
R E L A T I O N S H I P S , A N D C H O I C E S
S E X U A L O R I E N T A T I O N
As people pass from childhood into their teen years and beyond, their bodies develop and change. So do their emotions and feelings.
Adolescence Is a Time of Change
During the teen years, the hormonal and physical changes of puberty usually mean people start noticing an increase in sexual feelings. It's common to wonder and sometimes worry about new sexual feelings.
It takes time for many people to understand who they are and who they're becoming Part of that involves better understanding of their own sexual feelings and who they are attracted to.
What Is Sexual Orientation?
Sexual orientation is the emotional, romantic, or sexual attraction that a person feels toward another person There are several types of sexual orientation; for example:
Heterosexual.
People who are heterosexual are romantically and physically attracted to members of the opposite sex:
Heterosexual males are attracted to females, and heterosexual females are attracted to males. Heterosexuals are sometimes called "straight."
Homosexual
People who are homosexual are romantically and physically attracted to people of the same sex:
Females who are attracted to other females are lesbian; males who are attracted to other males are often known as gay. (The term gay is sometimes used to describe homosexual individuals of either sex.)
Bisexual
People who are bisexual are romantically and physically attracted to members of both sexes.
Asexual.
People who are asexual may not be interested in sex, but they still feel emotionally close to other people.
S E X U A L O R I E N T A T I O N
During the teen years, people often find themselves having sexual thoughts and attractions For some, these feelings and thoughts can be intense and seem confusing That can be especially true for people who have romantic or sexual thoughts about someone who is the same sex they are "What does that mean," they might think "Am I gay?"
Being interested in someone of the same sex does not necessarily mean that a person is gay just as being interested in someone of the opposite sex doesn't mean a person is straight. It's common for teens to be attracted to or have sexual thoughts about people of the same sex and the opposite sex. It's one way of sorting through emerging sexual feelings.
Some people might go beyond just thinking about it and experiment with sexual experiences with people of their own sex or of the opposite sex. These experiences, by themselves, do not necessarily mean that a person is gay or straight.
What Is LGBT?
You may see the letters "LGBT" or ("LGBTQ") used to describe sexual orientation. This abbreviation stands for "lesbian, gay, bisexual, and transgender" (or "lesbian, gay, bisexual, transgender, and questioning").
Transgender isn't really a sexual orientation it's a gender identity. Gender is another word for male or female. Transgender people may have the body of one gender, but feel that they are the opposite gender, like they were born into the wrong type of body.
People who are transgender are often grouped in with lesbian and gay as a way to include people who don't feel they fit into the category of being "straight "
Do People Choose Their Sexual Orientation?
Why are some people straight and some people gay? There is no simple answer to that. Most medical experts, including those at the American Academy of Pediatrics (AAP) and the American Psychological Association (APA), believe that sexual orientation involves a complex mix of biology, psychology, and environmental factors. Scientists also believe a person's genes and hormones play an important role.
Most medical experts believe that, in general, sexual orientation is not something that a person voluntarily chooses. Instead, sexual orientation is just a natural part of who a person is.
There's nothing wrong about being LGBT. Still, not everyone believes that. These kinds of beliefs can make things difficult for LGBT teens.
T E E N S E X U A L I T Y ,
R E L A T I O N S H I P S , A N D C H O I C E S
S E X U A L O R I E N T A T I O N
What's It Like for LGBT Teens?
For many LGBT people, it can feel like everyone is expected to be straight. Because of this, some gay and lesbian teens may feel different from their friends when the heterosexual people around them start talking about romantic feelings, dating, and sex.
A 2012 survey by the Human Rights Campaign found that 92% of LGBT teens had heard negative things about being lesbian, gay, bisexual, or transgender
LGBT teens might feel like they have to pretend to feel things that they don't in order to fit in with their group, family, or community. They might feel they need to deny who they are or that they have to hide an important part of themselves
Fears of prejudice, rejection, or bullying can lead people who aren't straight to keep their sexual orientation secret, even from friends and family who might support them.
Some gay or lesbian teens tell a few close friends and family members about their sexual orientation
This is often called "coming out " Many LGBT teens who come out are fully accepted by friends, families, and their communities They feel comfortable about being attracted to someone of the same gender
But not everyone has the same good support systems. Even though there is growing acceptance for LGBT people, many teens don't have adults they can talk to about sexual orientation. Some live in communities or families where being gay is not accepted or respected.
People who feel they need to hide who they are or who fear discrimination or violence can be at greater risk for emotional problems like anxiety and depression. Some LGBT teens without support systems can be at higher risk for dropping out of school, living on the streets, using alcohol and drugs, and trying to harm themselves.
Everyone has times when they worry about things like school, college, sports, or friends and fitting in In addition to these common worries, LGBT teens have an extra layer of things to think about, like whether they have to hide who they are
This doesn't happen to all gay teens, of course. Many gay and lesbian teens and their families have no more difficulties than anyone else.
The Importance of Talking
For people of all sexual orientations, learning about sex and relationships can be difficult. It can help to talk to someone about the confusing feelings that go with growing up whether that someone is a parent or other family member, a close friend or sibling, or a school counselor.
It's not always easy to find somebody to talk to But many people find that confiding in someone they trust (even if they're not completely sure how that person will react) turns out to be a positive experience.
In many communities, youth groups can provide opportunities for LGBT teens to talk to others who are facing similar issues. Psychologists, psychiatrists, family doctors, and trained counselors can help them cope confidentially and privately with the difficult feelings that go with their developing sexuality. They also help people find ways to deal with any peer pressure, harassment, and bullying they might face.
Whether gay, straight, bisexual, or just not sure, almost everyone has questions about physically maturing and about sexual health like if certain body changes are "normal," what's the right way to behave, or how to avoid sexually transmitted infections (STIs). It's important to find a doctor, nurse, counselor, or other knowledgeable adult to be able to discuss these issues with.
Beliefs Are Changing
In the United States, and throughout much of the world, attitudes about sexual orientation have been changing Although not everyone is comfortable with the idea of sexual orientation differences and there's still plenty of prejudice around, being gay is getting to be less of a "big deal" than it used to be.
Although we often associate gender development with puberty and adolescence, children begin showing interest in their gender early in life This article discusses how gender identity typically develops and how parents and caregivers can promote healthy gender development in children It's important to remember that each child is unique and may develop at a different pace
What we mean by gender?
Assigned sex: When children are born, they are assigned “male” or “female” based on their external sex organs When a child has a penis, the assigned sex is male When a child has a vulva, the assigned sex is female In rare cases, a child is born with external sex organs that are not clearly male or female Gender identity: Gender identity is “who you know yourself to be” While gender has generally been used to mean male or female, we now understand that gender exists on a spectrum A person’s gender identity may be man, woman, boy, girl, non-binary, etc
Gender expression: This is how you express your gender to others, whether through behaviour, clothing, hairstyle, or the name you choose to go by Words to describe someone’s gender expression could be “masculine,” “feminine,” or “androgynous” Sexual orientation: This refers to the gender of the people to whom you are typically sexually and/or romantically attracted A person can be attracted to those of the same gender and/or different gender(s) Your gender identity does not define your sexual orientation Transgender: When a person’s gender identity is not the same as their assigned sex at birth, they may be referred to as “transgender” (often shortened to “trans”) For example, a child born with female body parts may say that they are a boy A child may also say that they are not a boy or a girl, but just “themselves” because they don’t want their sexual characteristics to define who they are Indigenous people may use the term “two-spirit” to represent a person with a combination of masculine and feminine characteristics
Gender dysphoria: Describes the level of discomfort or suffering associated with the conflict that can exist between a person's assigned sex at birth and their true gender Some transgender children experience no distress about their bodies, but others may be very uncomfortable with their assigned sex, especially at the start of puberty when their body starts to change T
T E E N S E X U A L I T Y ,
R E L A T I O N S H I P S , A
N
Gender Identity
Gender identity is how a person feels and who they know them self to be when it comes to their gender. There are more than two genders, even though in our society the genders that are most recognized are male and female (called the gender binary) and usually is based on someone’s anatomy (the genitals they were born with). This is gender assignment and it is based on an assumption that someone’s genitals match their gender. However, gender isn’t about someone’s anatomy, it is about who they know them self to be. There are many different gender identities, including male, female, transgender, gender neutral, non-binary, agender, pangender, genderqueer, two-spirit, third gender, and all, none or a combination of these.
There are many more gender identities then we’ve listed. Gender can be complex and people are defining themselves in new and different ways as we gain a deeper understanding of identities. Some terms may mean different things to different people. There are certain terms some folks may not like to use or call themselves and some terms that they may like to use or call themselves. If you’re not sure what to call a person, it’s best to ask the person what they would like to be called. It is always up to us to decide how we identify, and how we express our gender. However you decide or identify deserves to be respected and supported.
R E L A T I O N S H I P S , A N D C H O I C E S
Some (But Not All) Gender Identity Terms
Transgender
Someone whose gender identity is different from the one they were assigned at birth might identify as transgender. Sometimes trans or transgender gets used as an umbrella term for gender diverse people. However, not everyone uses it to describe themselves. When in doubt ask, and always honor someone’s personal terms when it comes to gender identities. What do we mean assigned at birth? Think about one of the first things the doctor (or midwife) says when someone is born, “It’s a girl” or “It’s a boy.” This is gender assignment and it is based on an assumption that someone’s genitals match their gender. However, we know this isn’t always the case and that each of us gets to decide what gender we know our selves to be. It may not align with the genitals we are born with or be part of the gender binary (male-female). For example, someone may be born with a vagina but know themselves to be male.
Two-Spirit
A modern English term that an Indigenous person might identify as that comes from the traditional knowledge of Indigenous peoples in Canada/Turtle Island/North America. It can mean a person who walks between genders; one who carries the gifts of both males and females, or one who is gender unique (not specific to any gender) and/or as a way to identify as 2STLGBQ+. When Europeans arrived in North America, they introduced homophobia and transphobia to many Indigenous nations and dishonored the idea of what it means to be Two- Spirit. Today, many Indigenous Peoples are reclaiming the ancient understanding that there are more than two genders.
Cisgender
Cisgender is a term to describe someone whose gender matches what they were assigned at birth. For example, they were assigned female at birth based on being born with a vagina and know themselves to be female.
Non-Binary
Someone who does not identify as a man or a woman, or solely as one of those two genders. It’s often used as an umbrella term for identities that fall outside the male/female gender binary. Being non-binary means different things to different people, so this definition is purposely broad.
T E E N S E X U A L I T Y ,
R E L A T I O N S H I P S , A N D C H O I C E S
Genderqueer
Someone may identify as genderqueer if their gender identity is neither male nor female, is between or beyond genders, or is some combination of genders. This identity is often related to or in reaction to the social construction of gender, gender stereotypes and the gender binary system.
Gender Expression
Gender expression is about how someone acts and presents themselves to world. For example does someone wear makeup? Do they wear dresses? Do they prefer to only wear pants? Gender expression is not related to someone’s gender or sex, but rather about personal behaviors and interests. A cis man may wear nail polish or a trans woman may not like wearing dresses. Sometimes people don’t express their gender in the way they would like to because they don’t feel safe to do so. This is why it’s important to not assume someone’s gender just based on how they look, but rather by checking in with them. Gender expression is also deeply tied to culture. What Euro- Canadian culture codes as being either ‘male’ or ‘female’ can be different than what other cultures may code as being ‘male’ or ‘female’.
Gender Fluid
Gender fluid may refer to a gender which varies over time. Someone who identifies as gender fluid may fluctuate between genders or express multiple genders at the same time. Their gender may also vary at random or vary in response to different circumstances.
Gender Neutral
Someone who feels they are neither male or female may identify as gender neutral.
T E E N S E X U A L I T Y ,
R E L A T I O N S H I P S , A N D C H O I C E S
How does gender identity develop?
Most children have a strong sense of their gender identity by the time they are 4 years old Here is what you can typically expect at different ages:
2 to 3 years old
At around 2 years old, children are aware of physical differences between boys and girls Most children can identify themselves as a “boy” or “girl”, although this may or may not match the sex they were assigned at birth Some children’s gender identity remains stable over their life, while others may alternate between identifying themselves as “boy” or “girl”, or even assume other gender identities at different times (sometimes even in the same day) This is normal and healthy
4 to 5 years old
While many children at this age have a stable gender identity, gender identity may change later in life Children become more aware of gender expectations or stereotypes as they grow older For example, they may think that certain toys are only for girls or boys Some children may express their gender very strongly For example, a child might go through a stage of insisting on wearing a dress every day, or refusing to wear a dress even on special occasions
6 to 7 years old
Many children begin to reduce outward expressions of gender as they feel more confident that others recognize their gender For example, a girl may not feel that she has to wear a dress every day because she knows that others see her as a girl no matter what she wears Children who feel their gender identity is different from the sex assigned to them at birth may experience increased social anxiety because they want to be the same as their peers, but realize they don’t feel the same way
8 years old and up
Most children will continue to identify with their sex assigned at birth Pre-teens and teens continue to develop their gender identity through personal reflection and with input from their social environment, like peers, family and friends Some gender-stereotyped behaviors may appear You may notice your teen or pre-teen making efforts to “play up" or "play down" some of their body’s physical changes Others are more confident in their gender identity and no longer feel like they have to portray a perfectly masculine or feminine appearance. As puberty begins, some youth may realize that their gender identity is different from their assigned sex at birth. Because some children’s gender identification may change, especially around puberty, families are encouraged to keep options open for their child.
T I
How do most children express their gender identity?
Younger children may express their gender very clearly. For example, they may say “I am a she, not a he!”, “I am not your daughter, I am your son.”
Children may also express their gender through their:
Clothing or hairstyle
Choice of toys, games, and sports
Social relationships, including the gender of friends
Preferred name or nickname
Remember: Gender expression is different from gender identity. You can’t assume a child’s gender identity based on their gender expression (for example, their choice of toys, clothing, or friends).
What does gender-creative mean?
Gender-creative children express their gender differently from what society may expect. For example, a boy who loves to wear pink or a girl who insists on wearing her hair very short might be considered “gender-creative”. Society’s expectations for gender constantly change and vary in different cultures and at different times in history.
Relationships
We first learn about loving and caring relationships from our families. Ideally each child is nurtured and respected and grows up to care for others and develop strong and healthy relationships with others. This does not mean that it is always easy to make and keep friends, it just means that we share the goal of having strong relationships.
Tips for Building Positive Relationships
Respect others
Be kind and caring
Be a good listener
Do projects together
Learn to compromise
Avoid gossip
Cooperate
Talk about your feelings
Say nice things
Friendship
Everyone needs friends, and you probably have always had at least one. As you get older, some of your friendships will start to change, and may grow deeper. You might also begin to know many more people, although not all of them will be your close friends. Chances are you will also start to spend more time with your friends, and maybe talk on the phone more. Changes in relationships are natural, but not always easy.
Making and keeping friends can be particularly tough if you are shy or unsure of yourself. The best way to make new friends is to be involved with activities at school, and in the community where there are other people your age. Another way to make friends is to be friendly and helpful to other people. Talk to people, get to know them, find out if you have something in common with them.
Tips for Keeping Friends
Be supportive
Be encouraging
Do not tease or belittle
Cooperate
Compromise
Be considerate
Talk openly about disagreements
Apologize when you hurt them
Relationships with Friends
It is important to all of us that we feel like we belong somewhere or fit in with other people. Hopefully, your home is a place where you can always feel like you belong and that the members of your family like you. Having friends, or peers, that are like you, and who you can count on to listen to you, support you through tough times, or just spend time with you is important, too. This pressure we feel to fit in, and have people like us, is called peer pressure.
Peers can have a positive or negative influence on your thoughts, decisions, and behavior. If your friends encourage you to "do the right thing," reach your goals, work hard, or do anything else that is good for you, they are having a positive influence. If on the other hand, you know something your peers are saying or doing is wrong, and you keep your opinion to yourself and do things you know you should not, that influence is negative.
There are things you can watch out for that should make you think about whether your friends are having a negative influence on you. Do your friends do any of the things below?
Criticize you?
Make fun of how you feel?
Dare you to do things?
If they truly accepted you, then they would not do these things.
E E N S E X U A L I T Y ,
R E L A T I O N S H I P S , A N D C H O I C
Unhealthy relationships will often depend upon one person’s power and control over another. Do you see the behavior of yourself or your partner or a friend in the diagram below?
E E N S E X U A L I T Y , R E L A T I O N S H I P S , A N D C H O I C E S
On the other hand, the attributes of a healthy relationship include mutual respect, honesty and accountability, trust and support, and the ability to compromise. Do you see any of your relationships in the diagram below?
T.O.D.E.R
SHARING THE GREATEST GIFT OF ALL
NATIONAL STATISTICS PROGRAM OBJECTIVES

National Statistics A Personal Story Program Objectives
U C A T I O N R E C R U I T M E N T P R O G R A M
. O . D . E . R
It is with sincere appreciation that the Student National Medical Association thanks the National Minority Organ Tissue Transplant Education Program and the National Marrow Donor Program for their assistance with the development of the Tissue and Organ Donation and Education Recruitment (TODER) Protocol.
R I
A L L - - L I F E
As of March 2020, more than 112,000 patients in the United States are on the national transplant waiting lists for an organ or tissue transplant Every 10 minutes, someone is added to the national waiting lists. Everyday, 20 persons will die waiting for an organ or tissue transplant. Because certain diseases that affect the kidneys, heart, lung, pancreas, and liver that could eventually require a patient to need a transplant are found more frequently in minority populations than in the general public, minorities make up a disproportionate number of those awaiting organ transplants. The problem is compounded by the fact that matching organs between members of the same ethnic and racial groups often enhances successful transplantation. While nearly half of those waiting on the transplant list are of minority origin, only 25% of the available donor pool represents minority donors Minorities wait twice as long for a transplant because of this shortage of organs donated by minorities The longer the wait, the greater the risk of death.
Each year, over 30,000 patients in the United States are diagnosed with life threatening blood diseases such as leukemia and aplastic anemia For many of these patients, a bone marrow or stem cell transplant is their only chance for survival Even though tissue types are inherited, approximately 70% of patients must search for a donor outside of their immediate family. The chances of finding an unrelated donor depend on the rarity of the patient’s tissue type. Generally, minorities have a lower chance of locating a match because minorities are currently underrepresented on national donor registries.
A very similar story is found with regards to blood donations It is estimated that 95% of the population will need some form of blood transfusion during their lifetime. Yet, only 5% of the medically eligible population donate blood. With the high incidences of sickle cell disease, injuries, cancer, diabetes and cardiovascular disease among minorities, the need for blood within communities of color continues to rise However, minorities donate blood at a proportion significantly lower than their percentage in the population
It is without a doubt that increasing the number of minority organ, tissue, and blood donors is a paramount concern As future medical leaders of our communities and nation, the Student National Medical Association must take an active role in addressing the shortage of minority donors and the needless death that results from minority donors waiting for transplants because of this lack of minority donors. By forming alliances within the African American and other communities of color, the Student National Medical Association can increase its accessibility to minority donors and its visibility within these communities
P R O G R A M
O B J E C T I V E S
C O M M U N I T Y S E R V I C E
The objective of the Tissue and Organ Donation and Education
Recruitment Program is to:
Increase the number of minorities who donate organs and tissues.
Educate minority communities on the facts about organ/tissue transplantation.
Emphasize the importance and need for minorities to donate organs/tissue/blood.
Encourage minorities to enroll in organ and tissue donation programs.
Develop culturally sensitive recruitment strategies with an emphasis on donor education.
Provide prevention education that focuses on the importance of healthy lifestyles to reduce the possible need for a transplant.
N A T I O N A L
I. SAMPLE ACTIVITIES
Community-based organ/tissue/blood drive School-based organ/tissue/blood drive Panel discussions/forums with transplant recipients Workshops on the legalities of organ donations including living will information Panel discussions on the ethical and religious issues surrounding organ donation Combined Health Fair/Donor Drive Green ribbon awareness campaigns Walk-A-Thon to increase awareness
II. SUGGESTED STEPS FOR IMPLEMENTATION
With each step, SNMA should be guided by the “golden rule” for community outreach: Community meetings involving local people should employ their leaders, on their territory, with their customs, speaking their language about their concerns
1 Identify community organizations willing to serve as sponsor of donor/blood drive These organizations could include colleges and universities, fraternities, sororities, civic groups and churches
2 Hold a training session with sponsoring group to cover:
a.the need for organ/tissue/blood donations from minority donors
b.myths surrounding donation
c.recruitment strategies
3 Establish organizing committees within sponsoring group
a.Publicity Committee
b.Incentives Committee
c.Recruitment Committee
4 Have individuals from sponsoring group make presentations (written or oral) to the organization:
a.Utilize individuals from within the organization community who have benefited from donation as a spokesperson for testimonials
b Emphasize the special need for minority donors
c Address myths surrounding donation
d Utilize education material targeted toward minority donors
e Request program participants to sign pledge cards
f Request assistance with recruitment of others
5 For campus-based drives, have students make public service announcements and challenges to classes and campus organizations.
6.For blood drives, get a list of previous donors from the American Red Cross and call previous donors and request their participation in the blood drive
7 Use campus and local media (newspapers, radio, and television, etc ) to help publicize drive
8 Arrange with local vendors to provide food, gifts and other small promotional items for donors as incentives
9 For campus-based drive, plan with the college/university administration for students to receive community service hours/credit for planning, organizing, implementing, and participating in the drive
10 The day of the drive, have donors fill out surveys assessing their experience with the drive and recruitment efforts Use feedback to make changes for the next drive
III. SAMPLE DOCUMENTS
Materials Available from Student National Medical Association:
Get the Facts on Donation and Transplantation
Why Minorities Should DonateUnderstanding the Donation Process
Understanding the Transplant Process
Religious Views on Organ Donation and Transplantation
Giving the Gift of Life: What Organs/Tissues Can Be Donated
Do You Know Our History? Interesting Facts about African Americans and Blood Donation
African Americans and Organ Donation A Personal Story
TODER Session Evaluation Form
Blood Drive Evaluation Form
Material Available from the Minority Organ Tissue Transplant Education Program: What Everyone Should Know About Kidneys and Kidney Diseases
Family Discussion Certificate
Uniform Donor CardMiracles Can Happen Make It A Family Affair
Frequently Asked Questions on Organ/Tissue Donation and Transplantation
Material Available from the American Red Cross: Fact Sheet (DRD Form 224812)
Who May Recycle Life (DRD Form 224412)
Answers to Most Often Asked Questions (DRD Form 521212)
Lifesaver Within You (DRD Form 223712 )
Blood Donor Pledge Sheet (DRD 306)
Primer for Volunteers (DRD 319)
Taking Care of Our Own: Sickle Cell Anemia (DRD Video)
Share the greatest gift (DRD Flier 519212)
Graduate with Mother (DRD Poster 518612)
Birthday Girl (DRD Poster 518712)
Martin Luther King (DRD Poster 519112)
Sheridan Church Bulletin Stuffer (DRD Form 521112)
Overcoming Objections (DRD Form 224012)
Nutrition and Iron (DRD Form 223612)
Recruiting Donors (DRD Form 224712)Autumn (DRD Video)
Material Available from the National Marrow Donor Program:
NMDP Fact Sheet (890)
NMDP Fact Sheets (Spanish) (890)
The Need for African American Volunteer Stem Cell Donors (844)
The Need for Native American Volunteer Stem Cell Donors (837)
The Need for Hispanic Stem Cell Donors (839)
Stem Cell Donation (346)
Questions and Answers About Cord Blood Donation (405)African Americans Uniting for Life AAUL Brochure (420)
Keep the Circle Strong Brochure (Native American) (#426)
Hispanics Giving Hope/Hispanos Dando Esperanza Bilingual Brochure (465) Chance of A Lifetime (410)
A Medical Professional’s Guide to Unrelated Donor Stem Cell Transplantation: The Services and Resources of the NMDP 2nd Edition (441)
NMDP Education and Recruitment Guide (822)
IV. Additional Contact Information
National Minority Organ Tissue Transplant Education Program (MOTTEP) 2041 Georgia Avenue, NW, Suite 3100 Washington, DC 20060 (202) 865-4888 (800) 393-2839 (202) 865-4880 fax http://www nationalmottep org/
National Marrow Donor Program (NMDP) 3001 Broadway Street, NE Minneapolis, MN 55413 (800) MARROW2 http://www marrow org/
National Marrow Donor Program (for SNMA use only)
Isaac A Fordjour 7910 Woodmont Avenue, #1103 Bethesda, MD 20814 (800) 573-6667 ifordjou@nmdp org
American Red Cross (800) GIVE-LIVE http://www.redcross.org/
United Network for Organ Sharing (UNOS) 1100 Boulders Pkwy, Suite 500 Richmond, VA 23225-8770 (804) 330-8541 http://www.unos.org/
Minority Organ Donation Education Program (MODEP) William Minniefield 156 Madison Avenue Lackawanna, NY 14218 (716) 822-6104
wjm5@acsu buffalo edu
O
F A C T S
Minorities & Donation
End-stage renal disease (ESRD), a very serious and life-threatening kidney disease, is far more common among certain ethnic groups. Asian-Americans and Hispanics are three times more likely; and African Americans are twice as likely as Caucasians to develop ESRD Certain diseases of the kidney, heart, lung, pancreas, and liver are also more common in minority communities. These include hypertension among African Americans and diabetes among Hispanics. These diseases damage organs, often leading to the need for transplantation. Since genetic similarities are much stronger, transplantation works better between people with the same ethnicity. A shortage of organs donated by members of a specific minority community results in longer waiting periods and fewer transplants for those of the same ethnicity.
Health Care Crisis / Statistics
Advancements in technology have resulted in successful organ transplants for individuals with life threatening diseases. Many more have their sight, hearing, and mobility restored and health regained through cornea, bone tissue, and skin transplants.
The national list of patients waiting for vital organs increases each year There are currently more than 1,000 patients in South Florida with life-threatening diseases awaiting transplant. Every 1014 minutes the name of a patient with end stage organ failure is added to the national waiting list.
2017 patients waiting for a life saving organ die every day. Over six thousand people died last year waiting for a suitable organ for transplantation.*
N A T I O N A L S T A
Minorities & Donation
End-stage renal disease (ESRD), a very serious and life-threatening kidney disease, is far more common among certain ethnic groups. Asian-Americans and Hispanics are three times more likely; and African Americans are twice as likely as Caucasians to develop ESRD Certain diseases of the kidney, heart, lung, pancreas, and liver are also more common in minority communities. These include hypertension among African Americans and diabetes among Hispanics. These diseases damage organs, often leading to the need for transplantation. Since genetic similarities are much stronger, transplantation works better between people with the same ethnicity. A shortage of organs donated by members of a specific minority community results in longer waiting periods and fewer transplants for those of the same ethnicity.
Health Care Crisis / Statistics
Advancements in technology have resulted in successful organ transplants for individuals with life threatening diseases. Many more have their sight, hearing, and mobility restored and health regained through cornea, bone tissue, and skin transplants.
The national list of patients waiting for vital organs increases each year There are currently more than 1,000 patients in South Florida with life-threatening diseases awaiting transplant. Every 1014 minutes the name of a patient with end stage organ failure is added to the national waiting list.
2017 patients waiting for a life saving organ die every day. Over six thousand people died last year waiting for a suitable organ for transplantation.*
N A T I O N A L S T A T I S T I C S
On June 4,2020, the Organ Procurement and Transplantation Network (OPTN) national patient waiting list for organ transplant included the following:**
Type of Transplant
Kidney transplant
Liver transplant
Pancreas transplant
Pancreas islet cell
Patients Waiting for Transplant 122,240 12,714 894 894
Kidney-pancreas transplant 1,813
Intestine transplant.
Heart transplant.
Heart-lung transplant.
Lung transplant. Total: 248 3,557 50 1,162 122,240
NOTE: OPTN/UNOS policies allow patients to be listed with more than one transplant center (multiple-listing), thus the number of registrations is greater than the actual number of patients Some patients are waiting for more than one organ; therefore the total number of patients is less than the sum of patients waiting for each organ.
N A T I O N A L S T A T I S T I C S
Number of Transplants Performed in 2019
Type of Transplant
Kidney alone
Liver transplants.
Pancreas alone
Kidney-pancreas
Intestine
Heart alone
Heart-lung lung
Total.
Number of Donors in 2020 Type of
Resource: United Network for Organ Sharing
Resource: United Network for Organ Sharing
Based on OPTN data as of June 4, 2020September 20, 2002. Double kidney, double lung, and heart-lung transplants are counted as one transplant. NOTE: Data subject to change due to future data submission or correction.
A single organ donor can save the lives of up to eight people by donating the heart, lungs, liver, kidneys, pancreas, and intestines. One tissue donor can improve the lives of more than 50 people by donating eyes, bone, soft tissue, heart valves, veins, and skin.

How does the physician determine if a patient has actually died?
The physician performs a series of tests to determine if death has occurred. Death is indicated if the patient:
Cannot breathe without assistance
Has no pupil response to light
Has no response to pain
What does the term “brain dead” mean?
When someone is brain dead, it means there is no blood flow or oxygen to their brain and that their brain has ceased functioning in any capacity. It does not mean that other organs, such as the heart, kidneys, or liver are dead, although they may function for only a few days. Unless damaged by injury or disease, these organs may be donated to another individual for an organ transplant.
Why doesn’t the heart stop beating if a person is brain dead?
The heart has its own pacemaker independent of the brain. As long as it has oxygen, it continues to beat. The heart could actually be removed from the body, placed in a saline solution, given oxygen, and still continue to beat. Therefore, the brain can be dead, and the heart may continue to beat.
What part does medication play in the body of the brain-dead patient?
In case the family wishes to donate the organs and/or tissues, medications are usually continued until the time the patient is officially declared brain dead. These medications help keep the blood pressure and heart rate under control, and some reduce swelling in the brain.
Would removing the respiratory support equipment be the same as causing the death of my family member or not giving him or her all possible chances?
Once the patient is brain dead, he or she is already dead; consequently, you cannot cause death by removing respiratory support The respiratory support equipment only keeps the heart beating.
What is the recorded time of death for a brain-dead patient, when the patient is declared brain dead or when the heart actually stops beating?
The recorded time of death is when the physician actually pronounces the patient dead. The patient can be pronounced dead on the basis of brain death (with the heart still beating). Medically and legally, the patient is dead at that point.
Does the body of a brain-dead patient sometimes start to deteriorate even if the patient is still on life support?
The failure of many organs begins to occur soon after brain death.
Are there any clinical documented cases where a patient was declared brain dead and later restored to a normal life?
No. When you hear about patients who were brain dead and recovered, they were not actually brain dead. They were in a deep coma or vegetative state with slight brain activity.
M Y T H V S F A C T
The public’s understanding of donation and transplantation is often based more on myth than reality. The instinctive fear of the unknown, combined with those superstitions surrounding death, may decrease donation and limit the lifesaving potential of transplantation medicine. Broad-based public understanding and acceptance of organ donation is essential to provide transplantation to those in need.
Myth: A doctor might take organs before someone is really dead.
FACT: The declaration of death must be made and consent from the donor family must be obtained before donation can occur. Cadaveric organ donation is only possible when brain death is diagnosed and declared. Tissue donation is possible when death results either from cardiac arrest or neurological cessation. After brain death, the body’s organs can be maintained with ventilator and circulatory support for a short period before losing viability for transplantation. Even though death has occurred, the body may appear to be alive for a short period of time because of this support. Medical personnel may mistakenly refer to the mechanical support as “life support”. Mechanical maintenance of a dead body is not the same as providing and removing support from a living patient. Brain death and the maintenance process should be clearly understood by donor families. Health care professionals can help by precisely explaining death and the donation process.
Myth: Doctors might let one patient die so that they can save others with transplants.
FACT: The physician who attends a patient at the time of death is not involved with the transplant programs operations or administration or with potential recipients This is both required by law and ethical medical practice.Procurement coordinators serve as intermediaries between donor hospital/attending physicians and transplant programs and teams The donor hospital notifies the procurement organization when a possible donor is identified. The attending staff is fully focused on the care of the patient. Donation is considered only after all efforts have been made to save the patient’s life. At this point, there may be some interaction by the attending staff with procurement coordinators.
M Y T H V S F A C T
Myth: If I am in an accident and the hospital knows that I want to be a donor, the doctors will not try to save my life.
FACT: Organ and tissue recovery takes place only after all efforts to save your life have been exhausted and death has been legally declared. The medical staff treating you is completely separate from the organ recovery agency and the transplant team. This is both required by law and ethical medical practice. The organ recovery agency does not notify the transplant team until your family has consented to donation.
Myth: Donation will increase the hospital charges billed to the donor families.
FACT: Donation costs the donor family nothing. All costs associated with the donation procedures are charged to the procurement organization and then passed on to the transplant center which bills the transplant recipient and his/her insurer. The donor family is responsible for the costs of all medical care not related to the donation and for funeral expenses - as they would be in any case.
Myth: Donation disfigures the body. It won’t be possible to have an open casket funeral.
FACT: Donation does not disfigure the body. Donation is a surgical procedure performed in a sterile operating room The donor’s body is treated with the same care and respect as any surgical patient. When bone is donated, synthetic prostheses are implanted to maintain skeletal structure Skin donation may give the appearance of a light sunburn but is usually not apparent. Because there is no disfigurement and no obvious suturing, donation does not interfere with the family’s choice of funeral plans, including open casket.
M Y T H V S F A C T
Myth: Donation takes a long time and will delay the funeral.
FACT: Donation occurs within a few hours of the family giving consent. The time available between declaration of death and donation is 12 to 24 hours for most organs and tissues. After donation surgery, the body is immediately released to the funeral service, and funeral and visitation plans can proceed. When the case involves the medical examiner’s office, the medical examiner, with the consent of next of kin, will release the body to the procurement organization for retrieval of organs and tissues. After the autopsy, the medical examiner will release the body to the funeral home.
Myth: Transplants are still experimental procedures with questionable outcomes. FACT: Transplantation of vital organs, in most cases, is regarded as therapeutic, standard medical practice. Kidney transplantation in 2002 has a one-year patient survival rate of better than 97 percent; heart transplants, 84 percent; and liver transplants, 85 percent. Even the relatively new pancreas transplant procedures offer a one-year patient survival rate of 83 percent. Tissue transplants can restore sight, mobility, heart action, circulation, and hearing; repair damaged skin, bone, and muscle; and help speed the healing process.
Myth: People can sell organs to make a lot of money.
FACT: It is against the law to sell organs under the Federal National Organ Transplant Act (Public Law 98-507) and under state statutes. Anyone convicted of violating the federal law is subject to a maximum of five years imprisonment Violation of the state statute is a second-degree felony carrying a penalty of up to 15 years in prison and up to $10,000 fine.Organ procurement organizations (OPOs), such as LAORA, coordinate all activities associated with donation, including distribution and nonprofit services certified and monitored by the U.S. Government’s Health Care Financial Administration. While the sale of organs is prohibited, state statutes do permit the recovery of reasonable costs associated with removal, storage, and transplantation of organs and tissue.
M Y T H V S F A C T
Myth: Wealthy people or those with celebrity status get the donated organ. It's not fair to those with fewer resources.
FACT: A person becomes eligible to receive a donated organ or organs by getting on the national list of transplant candidates. The decision to proceed with transplant as a medical treatment is made by the patient and his or her doctor. The patient is evaluated for transplant based on a variety of medical, psychological, and financial criteria. When the patient meets the evaluation criteria, his or her name and needs are entered on the national waiting list. Publicity about fundraising for transplants often leaves the inaccurate impression that individuals are raising money to pay for organs. In fact, these are generally uninsured patients and their families who are seeking funding to satisfy the financial requirements of the transplant program before they can be included on the waiting list. The waiting list is maintained by the United Network for Organ Sharing (UNOS), a non-profit service headquartered in Richmond, Virginia. UNOS was established under the National Organ Transplant Act of 1984 and serves transplant centers, physicians, and procurement organizations nationwide. The role of UNOS is to match available organs with potential recipients, based on strict criteria that include medical urgency, tissue and blood type, time on the waiting list, and geographic proximity. The system is designed to assure fairness Once a patient is on the waiting list, he or she is guaranteed that every effort is being made to locate the needed organ or organs as quickly as possible There is no way a person can “buy” higher priority on the waiting list. The only exception to the listing process is direct donation, such as a donation between living relatives
Myth: Donation is against our religion.
FACT: Most major organized religions support donation as a humanitarian act in keeping with religious doctrine. The Roman Catholic Church, Protestant faiths, Judaism, Islam, Buddhism, and Hinduism all regard donation as a personal decision for individual members. Families who have religious questions are advised to consult with their personal spiritual advisors. Life Alliance Organ Recovery Agency (LAORA) works with clergy members to help clear up misunderstandings and provide appropriate counsel on religious viewpoints.
M Y T H V S F A C T
Myth: If I donate, my organs will probably not benefit someone in my local community.
FACT: Geographical proximity is a key criterion in organ distribution. When a donation is made, the procurement organization first attempts to place the organ in the immediate area or within the state. If a qualified recipient is not found locally, the search then turns to the national list. Every effort is made to find recipients as close as possible to the donation site.
Myth: I’ve heard about a business traveler who is heavily drugged, then awakes to find that he or she has had one kidney (or sometimes both) removed for a black-market transplant.
FACT: This tale has been widely circulated over the internet. There is absolutely no evidence of such activity ever occurring in the U.S. or any other industrialized country. While the tale may sound credible, it has no basis in the reality of organ transplantation.
Myth: Signing a donor card is meaningless. My family will be making all the decisions when I’m gone. FACT: Signing a donor card, combined with family discussion of donation, is the most certain method of having one’s wishes carried out A signed and witnessed donor card is a legal document It is a positive statement to family and physicians that the individual wants to consent to be a donor Consent to donation is required from the donor’s legal next of kin. This decision must be made quickly. A signed donor card tells the next of kin that their loved one has thoughtfully considered donation and made his or her own decision.
D O N A T E
Organs/Tissue
There are over 112,000 persons in the United States waiting for organ transplants.
A new name is added to the transplant waiting list every 10 minutes.
Matching organs between members of the same ethnic and racial groups often enhances successful transplantation.
Minorities wait twice as long for a transplant because a shortage of organs donated by minorities. The longer the wait, the greater the risk of death.
20 persons per day die waiting for transplants. Nearly half of those who die while on the transplant waiting list are minorities.
One person can donate organs or tissues than can potentially benefit as many as 50 people.
Bone Marrow/Stem Cells
Each year over 30,000 patients are diagnosed with a life-threatening blood disease and their only chance for survival is a bone marrow or stem cell transplant.
At any given time more than 3,000 patients are actively searching for a marrow/stem cell donor.
70% of these patients must search for an unrelated donor.
Since minorities are currently underrepresented on donor registries, the chances of a minority patient finding an unrelated donor are lower.
Blood
One in 10 persons entering the hospital needs blood. Each unit of blood you donate can help up to four people.
95% of the population will need a blood transfusion during their lifetime. Only 5% of the medically eligible population donate blood.
Less than 1% of African Americans donate blood.
D O N A T I O N A N D T R A N S P L A N T
When considering organ and tissue donation and transplantation individuals often wonder if the religion approves such an act. Research conducted by the American Council on Transplantation and the New York Regional Transplant Program has found that the majority of religions permit and support donation and transplantation.
Amish: Approve if there is a definite indication that the health of the recipient would be improved, but reluctant if the outcome is questionable.
Buddhism: Donation is a matter of individual conscience.
Catholicism: Transplants are ethically and morally acceptable to the Vatican, and donations are encouraged as an act of charity, fraternal love, and selfsacrifice
Christian Science: Does not take a specific position on transplants or organ donation. The decision to donate organs is left to the individual.
Greek Orthodox: No objection to procedures that contribute to restoration of health, but donation of the entire body for research experimentation is not consistent with tradition.
Hinduism: Donation/transplantation is an individual decision.
Islam: Approve donations provided that the donor’s consent is written in advance Organs cannot be stored in organ banks, but must be transplanted immediately.
Jehovah’s Witness: Do not encourage donation, but believe it is a matter of individual conscience. All organs and tissues must be completely drained of blood.
Judaism: A direct transplant is preferred but encourages donation even if the beneficiary will not be known. Donor must be brain dead in accordance with set standards.
Mennonite: Do not prohibit organ donation and transplantation The decision is an individual one.
Mormon: Donation/transplantation is an individual decision.
Protestantism: Encourage and endorse organ donation.
Quakers: Donation/transplantation is an individual decision.
Seventh-Day Adventist: Organ donation and transplantation are acceptable practices for members. The decision is an individual one.
95% of the population will need a blood transfusion during their lifetime.
Dr. Charles Richard Drew developed the system of storing and preserving blood and blood plasma, which revolutionized the medical profession.
Dr. Daniel Hale Williams performed the first successful open-heart surgery.
Type O blood is commonly used to treat trauma patients.
Mr. Vivien Theodore Thomas assisted with research that led to the use of blood and plasma treatment for traumas during World War II.
Within specified limits, high blood pressure will not prevent you from donating.
Dr. Michael Croslin developed the computerized blood pressure device.
An hour of your time can mean a lifetime to someone else
1 donation can save up to 3 lives
Blood cannot be manufactured; it can only come from donors 16% of all blood used goes toward the treatment of heart disorders.
Add your name to the above list of contributions made by African Americans by sharing the greatest gift of all--LIFE.
Please, donate blood today!
A P E R S O N A L
My name is William Minniefield I am an African American whose family has been touched by end stage renal disease Some years ago, my younger brother died while waiting for a kidney My brother’s name was Ronald and he was one year younger than I was He was diagnosed at an early age with high blood pressure that eventually caused kidney damage, requiring a transplant. Ronald had also developed an enlarged heart that is associated with long term dialysis that led to cardiac arrest. When Ronald died, he left a wife and two very young children behind His birthday was August 8, and mine is August 6 Seeing his children, my niece and nephew, at family gatherings is a painful reminder that my brother is gone On my birthday I’m reminded even more so that he is gone, and how much I miss him On the day of his funeral I put a small jar of red dirt (we are from Atlanta, GA) in his coffin and a note in his suit pocket letting him know that we will always be with him. During the first few months after his death, I visited his grave two or three times a week and on his birthday for the next three years. Ronald was on dialysis for five years before his death and those were not good years for him He was plagued with constant infections and was in a lot of pain I remember too clearly taking him to some of his dialysis appointments and watching him struggle and feeling so helpless Near the end of his life I would carry him to his wheelchair and put him in the car. The saddest part of all is, he did not need to die.
As fate would have it, I now have an older brother Curtis who has been on dialysis for four years Curtis developed diabetes in 1990 that led to his end stage renal disease In 1996 his doctor told him that it was time to go on dialysis Curtis must go on dialysis three times a week, four hours each time. Eleven months ago, Curtis was placed on the national transplant waiting list, but my family and I wonder if there will be a kidney available for him. We pray that he won’t have to endure what Ronald did.
My family has always believed in and supported organ donation. Two years ago, my niece (Dee Dee) died two weeks before her fourth birthday from cancer. Even with all the grief her mother was enduring she did not hesitate to donate Dee Dee’s corneas to the tissue bank. Three weeks later she received a letter informing her that two children had received Dee Dee’s corneas. This is the type of unselfish act that we must practice so others may live or have a better quality of life African Americans must educate themselves concerning organ donation and learn how this disease affects us. We must also learn how to live and eat better to minimize our chances of developing diabetes and hypertension. Education must become a large part of the total package for preventing and minimizing diabetes and hypertension.
Why must we wait until after the fact? Please think about becoming an organ donor because this story could be about your family.

S M O K I N G

GOALS AND OBJECTIVES
TRAINING MODELS
ADDITIONAL ACTIVITIES AND GENERAL FACTS
0 3 0 4 3 6 3 9 4 0
C O N T E N T S
GOALS AND OBJECTIVES
TRAINING MODELS
SURVEY
FACTS ABOUT SMOKING 2 0 2 0 - 2 0 2 1
ADDITIONAL ACTIVITIES
I S S U E
P R O G R A M G O A L S A N D
O B J E C T I V E S
To empower the youth to say "NO" to tobacco products.
To educate and motivate the youth to choose a healthy lifestyle.
To encourage the involvement and interaction of SNMA with the community that we serve.
To motivate the youth to educate others about the health effects of smoking tobacco products.
To encourage medical students to educate and motivate their patients smoking cessation and prevention.
S K I L L S ( T R A I N I N G M O D E L 1 )
Setting up the Program
As suggested by the Surgeon General, the program should target children in the sixth or seventh grade Contact a middle or junior high school in your area to arrange class time for the program. Find out what smoking prevention/educational programs the school already has in place so that the sessions best serve the students.
Training Facilitators
Each session should have at least two members of the SNMA chapter participating. Remember that the sessions must be in a non-lecture format whenever possible. For the ‘20-’21 academic year, if the school distinct is doing non-traditional learning at home, consider creative pre-activity and post-activity videos
Emphasize discussions, experiments, role-playing, films, etc. Get the students involved and keep their interest. Try to involve parents, by giving homework assignments for example. Experiments should be tried before a session is conducted to ensure that it will work and is safe Please consider that this protocol is written for an audience of medical school students, not sixth and seventh graders. Facilitators must present important concepts and information in a manner that can be comprehended. Also, recall the Surgeon General’s eighth element: “the program should be socially and culturally acceptable to each community” (4). That is, it is the duty of each facilitator to make him- or herself aware of the reality that their audience faces inside, and especially, outside the classroom
Lesson Outline
Below are essential topics to be dealt with over the course of the program. A typical program would run for five weeks with one one-hour session each week plus a booster session to follow some months later as a means of follow-up. Due to the emphasis of social skills training, a holistic approach combining this protocol with other protocols, such as Teen Health and Sexuality and Violence Prevention, could be a very effective way to present this information It is left up to the individual chapters to determine the final format for their smoking prevention program.
S E S S I O N 1
: A C T I V E L I S T E N I N G
Facilitators introduce themselves and share a little bit about who they are and why they are participating in the program. Explain the purpose of the program (to encourage a smoke-free lifestyle through social skills training) and give a brief outline of the program’s activities. Facilitators should use this session to begin learning the names of the students and to appreciate the dynamics between students in the class and between the students and the teacher.
Ask students what it means to be an active listener Ask students to tell you ways that you can listen actively. Explain importance of active listening. Let students know that this is what you expect from them during every session
Now is also a good time to establish ground rules for the sessions, such as no talking while someone else is talking, no one shall put down anyone else’s ideas or comments, no question is a dumb question, all questions are welcomed and the facilitators will try to answer questions to the best of their ability or will direct students to an appropriate resource, etc.
Students should be asked to complete a self-evaluation about their experience with smoking (questions that may be included in the evaluation are listed below). Facilitators should encourage students not to complete the evaluation if they feel they cannot answer all the questions honestly. Evaluations should be collected in a manner to ensure that responders remain anonymous (students can place folded evaluations in a closed box). Students should not put their names on the evaluations. Facilitators should explain that the purpose of the evaluations is to determine the impact of the program and ways to improve the program.
S E S S I O N 2 : C O U R S E O F
T O B A C C O U S E A N D
C O N S E Q U E N C E S
Short-term consequences should be emphasized. Students should also learn about long term effects of smoking. Such information can be found in the Smoking Prevention Position Paper or in the listed references and resources. A copy of the American Cancer Society program “Don’t Choke on Smoke” has been included as a resource because it provides helpful information, illustrations, and experiment designs for this session.
Students should realize the effect of carbon monoxide on oxygen carrying capacity and what this implies about their performance in sports and other activities. Also, reduced oxygen tension can promote the onset of sickle cell painful crises.
An example of a simple experiment: cover the unlit portion of a cigarette with a filter or tissue, attach a piece of tubing and create suction with a pipette bulb, show the student the stain that is created on the filter (5)
S
E S S
I
O N 3 : P E E R P R E S S U R E
Students learn how to deal with peer pressure and recognize what peer pressure is. Students should realize that peer pressure is only as powerful as they allow it to be and that compliance with peer pressure is the opposite of being independent.
Students should practice different ways of dealing with peer pressure. Facilitators can use role-playing: present a situation to the class and ask the students to come up with ways to handle the situation in a positive manner, small groups of students can get together to develop their ideas and come up with a brief skit to present to the rest of the class. Alternatively, the facilitators can play the pressuring peers and have a student play the role of the peer who does not succumb to the pressure.
Self-esteem: Students practice ways to improve or reinforce selfesteem by acknowledging their positive characteristics. This should be an ongoing process during the program A homework assignment could involve the parents and allows parents to provide a supportive role: have students get their parents or guardian to tell them five characteristics that they admire about their child while the child writes them down. These assignments do not have to be shared in class, but facilitators should get a general idea of whether or not the class did the assignment at the next session.
S E S S I O N 4 : I M A G E S
Students learn the ways in which the media portrays tobacco “social images” and influence people to use tobacco. Students should come away with an understanding of how some adolescents may use tobacco to improve self-image. Facilitators should explain the importance of children as a market for cigarette manufacturers in search of new impressionable consumers. An excellent module on decoding tobacco advertising can be found in A Manual on Smoking and Children (5).
Social Activism: Students begin to learn what it means to be a social activist. As a homework assignment, students can practice writing letters advocating tobacco-free lifestyles or design antitobacco/pro-nonsmoking posters.
S E S S I O N 5 : P U B L I C
C O M M I M E N T U S I N G V I D E O T A P E
A N D C O N C L U S I O N
Students can perform a skit or make a video using a news program format to summarize what they have learned, answer questions from their peers, and share their commitment regarding tobacco. The posters and letters assigned to promote social activism can be used in the video. For example, the posters can be used for a backdrop or samples from letters can be shared. Students should be given the option to participate or not. A student should not be made to make a commitment that he or she does not intend to keep. Students can identify a friend or friends in the class to make the non-smoking commitment with (the buddy system) and sign a contract that they write out themselves.
Students should be given a true/false quiz or play a quiz game to be sure that they learned the important points of each session. The results of such quizzes can also help facilitators decide which points need to be better emphasized (Possible questions are listed below). Facilitators should explain that this will not be graded but is to show how well the facilitators did.
Students should be asked what they liked and did not like about the program so that it can be improved. Students can write down comments if they do not feel comfortable expressing them orally Facilitators should remain in touch with the class to see how they are doing and to provide support
B O O S T E R S E S S I O N
Since the effects of smoking prevention programs have been shown to be short lived in the absence of follow-up and reinforcement, it is recommended that at least one booster session is conducted (4). This session can be planned by each chapter depending on the dynamics between the class and the facilitators during the previous sessions.
The session should be held the following year or after a few months have passed. The session can be a discussion about how they have used what they learned during the earlier sessions or problems or pressures that they have encountered. Another suggestion might be to assemble the class for a less formal smoke-free gathering outside the classroom setting. Selfevaluations should be completed again, compiled, and compared to results of the initial evaluations.
S U G G E S T E D S E L F - E V A L U A T I O N
A N D Q U I Z T O P I C S
Suggested Questions:
ever tried cigarette smoking age when first smoked a whole cigarette ever smoked cigarettes regularly (one cigarette a day for 30 days)age when first smoked regularly number of days during past month that cigarettes were smoked number of cigarettes smoked per day during past month number of days during past month that cigarettes were smoked on school property ever tried to quit smoking cigarettes during past six months any use of chewing tobacco or snuff during past month any use of chewing tobacco or snuff during past month on school property
Suggested Quiz Topics:
a drug is a chemical that changes how the body works all forms of tobacco contain a drug called nicotine, which is addictive tobacco contains other harmful substance in addition to nicotine tobacco use includes cigarettes and smokeless tobacco tobacco use had short-term and long-term physiologic and cosmetic consequences tobacco use during pregnancy has harmful effects on the fetus stopping tobacco use has short-term and long-term benefits many people who use tobacco have trouble stopping some advertisements try to persuade people to use tobacco
A N D Q U I Z T O P I C S
Suggested Quiz Topics continued
tobacco advertisement is often directed toward young people personal feelings, family, peers, and media influence decisions about tobacco use
young people can resist pressure to use tobacco most young people and adults do not use tobacco people who choose to use to tobacco are not bad people environmental tobacco smoke is dangerous to health there are laws, rules, and policies that regulate the sale and use of tobacco community organizations have information about tobacco use and can help people stop using tobacco
schools and community organizations can promote smoke-free environmentssmoking cessation programs can be successful (3)
D O N ' T C H O K E O N S M O K E
This program can also be used for as a single session program versus the more comprehensive five session program. A self evaluation should be distributed and collected to the students before the day of the program and a quiz should be left with the class’ teacher to assess the effectiveness of the session. A booster session is recommended Activities #2 and #3 are great additions to this program.
OUTLINE
Introduction (5 minutes)
Presenter introduces self w/o reference to American Cancer Society or topic of program. “We’re going to discuss a serious topic today, but we’re going to have fun doing it.”
Pictionary Game
The presenter encourages students to guess the name of the program through a series of pictures drawn by the presenter. Each picture represents a word or part of a word. (Answer: Don’t Choke on Smoke)Brief (2-3 minutes) intro to topic (i.e., Today, we’re going to talk about smoking, how it’s bad for your health, and how you can avoid getting hooked.)
Smoking and Your Body (10 minutes)
“Non-lecture” presentation on smoking and how it affects your body (experiment, several games, and visuals accompany this)“Rank the Killers” game.
Brief intro of smoking statistics, followed by “1 in 4 game”
Brief outline of all the various body parts affected by smoking
How the lungs work - description of how the lungs get oxygen to the body via the circulatory system and how tobacco smoke interferes with this process.
Smoking Bottle Experiment. Use this as an opportunity to talk about secondhand smoke.4700 compounds in cigarettes.
Short-term/social effects of smoking (Q & A style)
D O N ' T C H O K E O N S M O K E
Role Playing (30 minutes)
Break the class into two groups.
One (group of 3 or 4 kids) will be responsible for applying the pressure tactics. The other group will practice techniques for saying no.
One presenter directs discussion for each group The pressure group is given scenarios to play out. The “Say No” group discussed general techniques for saying NO to a variety of situations
The groups come back together to practice their situations. Each situation should take only 2 or 3 minutes with 5 minutes for discussion and Q & A.
After the performances, the presenter can summarize additional situations that may confront students.
Conclusion Reminder of how to say no! It’s your choice. It’s your power.
O U T L I N E D E T A I L S : P I C T I O N A R Y
The presentation will begin with a game of Pictionary based on the theme: “Don’t Choke on Smoke”
All the kids will know is that medical students will be talking to them The reason for this is to get them engaged in the presentation before they realize it’s about smoking. In other words, they should never have the chance to think of this as a lecture and tune us out.
We’ve chosen a theme that rhymes, that is easy to remember, and that accurately represents the presentation topic. Be sure to repeat this theme often throughout the presentation, so that they’ll remember it.
Finally, you’ll be doing the drawing to make this activity as interactive as possible. Be sure to practice so that what you’re drawing is recognizable to the kids; we want to make this puzzle relatively easy for them to solve.
Okay. The Pictionary game is over, and all the kids are having fun and they have guessed the topic. The next major part of the presentation is the “nonlecture” and we have to make sure that we don’t lose their attention. Prior to this game, no mention will be made of the topic of the presentation.
It’s a good idea at this point to 1) provide a short introduction to the topic, 2) Outline the major parts of the presentation, and 3) set the ground rules for the next 45 minutes or so.
O U T L I N E D E T A I L S : P I C T I O N A R Y
Here is a sample of what you might say Today, we are going to talk about smoking, what it does to you body and how you can avoid getting hooked. It’s a very serious topic, but I hope we’re going to have fun with it! First, (presenter 2 name) will give you a few quick smoking and medical facts and tell you more about some of the ways that smoking hurts your body
Pay close attention to what (presenter 2 name) tells you because next we are going to act out some situations where people might pressure you to have a cigarette. We’ll teach you different ways to say no and you’ll have a chance to practice them.
We hope you learn a lot from this presentation. If you have any questions any time, raise your hand and we’ll try to answer them.
The most important thing to remember is that we just got the kids attention with a fun game. And, we want the rest of the presentation to be just as fun, so don’t lecture them…
A N D Y O U R B O D Y ( A N O N -
L E C T U R E )
The purpose of the “NON-lecture” portion of the presentation is to teach the students why they should not smoke. This is not intended to be the main part of the overall presentation; ideally, it should only last 10 minutes. This information can and should be used in the role-playing segment of the presentation. When reviewing this information with the students, the process should be as interactive as possible. Ask the kids questions and let the kids ask questions of you at any time. Feel free to use any interactive tactics which come to mind.
Remember, you’re talking to 9- to 12-year-olds, not medical students. Keep it simple. Keep it fun!
“Rank the Killers” Game
This game is similar to one of the games on “The Price is Right” game show. Five of the top killers (i.e., smoking, accidents, pneumonia, AIDS, and guns) will be written/drawn individually on cards to be given to 5 students that you choose. All 5 of the students will go to the flip chart at once to match their card to the correct number of annual deaths, which will be listed in order, on the chart
The students will have to collaborate (the actual players and those watching) so that all the cards are finally matched up to the correct numbers. The facilitator will tell them only how many cards are correct each time they think they have it right (not which ones are correct). The students will continue trying until all of the cards are matched up to their correct number of deaths.
A N D Y O U R B O D Y ( A N O N -
L E C T U R E )
RANK THE KILLERS
1 - 434,0002
2 - 86,0003
3 - 75,0004
4 - 33,0005
5 - 26,000
These are the number of people who die each year from these causes. The correct order is:
1) Smoking 2) Accidents 3) Pneumonia 4) AIDS 5) Guns
“What
Happens to Smokers?”
1. Most smokers will die 5-8 years earlier than non-smokers. 2. 1 in 4 smokers will die early.
3. 2 or more of these 4 will suffer from diseases caused by smoking: emphysema, lung cancer, chronic cough, etc.4. “1 in 4 Game” - have the students count off 1 through 4 until everyone has a number. Have all the 1’s in each group lie down to represent the ones who will die; have the 2’s and 3’s cough and get sick. This will get the kids involved and demonstrate how drastic these statistics are.
5. Ask the kids why they think smokers get sick and die.
How the Body is Affected by Smoking
Use drawing on the easel pas to point to different body parts Make this a quick run-down of the list of organs, with very little details. We want to emphasize that smoking affects more than just the heart and lungs This can be done by Facilitator 1.
.
A N D Y O U R B O D Y ( A N O N -
L E C T U R E )
Normal Breathing Process
Facilitator 1 will be setting up the smoking water bottle experiment while F2 is speaking.
1. Breathing In (Refer to graphic on flip chart)
a. Air fills your lungs, where blood cells absorb oxygen.
b. Blood carries oxygen from the lungs to the heart, and the heart pumps it throughout your body.
c. Oxygen helps your cells do their job, and lets your body function the way it should.
2. Breathing Out
a. Blood cells carry away carbon dioxide from body cells back to the lungs.
b. When you breathe out, you force the carbon dioxide out of your body.
3. How Smoking Affects this Process ( refer to experiment in Progress; have kids come up and watch)
a. If you smoke, you breathe in chemicals like tar and carbon monoxide, which can’t be breathed out.
b. These chemicals stay behind and can cause cells to change, which may become cancer.
c. Tell them that carbon monoxide is in the pollution that comes from the tailpipes of cars it keeps oxygen from getting to the cells in your body, and can cause headaches, dizziness, and lack of energy
A N D Y O U R B O D Y ( A N O N -
L E C T U R E )
1. Second-hand smoke is produced by the burning cigarette between puffs. This is different from the smoke that smokers inhale directly into their lungs.
2. Second-hand smoke contains MORE of some chemicals, like carbon monoxide
3. People who smoke hurt others around them as well as themselves
. Second-Hand Smoke (F1)Show the students what second-hand smoke is while the experiment is smoking the cigarette.
.
W A T E R B O T T L E E X P E R I M E N T
Materials Needed
Clear Glass bottle, 1 gallon, such as used for bleach, apple cider, vinegar, etc.
Two-hole rubber cork that will fit the bottle red
Clear glass or plastic tubing - ¼” diameter by 4” long (to be flared at one end and bent as a mouth and throat piece)Rubber or plastic hose - 3/16” diameter, 4’ long
Gallon bottle or bucket (to catch water)Matches or lighter
Ash tray
Solid rubber cork (for shaking up water and smoke)
Pipe cleaner
Assembling Instructions
Insert the 4-foot-long tubing in one hole of the cork long enough to reach about 1” from the bottom of the bottle. This will be the siphon tube. Bend and flare a ¼” by 4” long glass tubing. The bend should be 45 to 90 degrees and the end flared to accommodate a cigarette. This can be done by heating with a Bunsen burner, bending or flaring and then cooling the tubing. Insert this mouth and throat piece through the other hole in the cork extending about ½ inch into the bottle. Fill the bottle full of water.
W A T E R B O T T L E E X P E R I M E N T
Demonstration
Blow into the short tube thereby creating a positive pressure and starting the siphon. Put a cigarette into the short tube and light it. As the water goes out, the smoke from the cigarette will be drawn in. Call attention to the smoke streaming into the bottle. This is one of the reasons smokers have congested lungs and don’t live as long.
Take a cigarette butt out before it burns to the filter. When the water level reaches about 2”, remove the cork with siphon tube and mouthpiece. Place a solid cork or hand on the bottle. Shake the contents in the bottle. Let the audience “try” smelling it.
Take a pipe cleaner, wipe out the mouth and throat piece and paint the hands of the on-lookers with the tar from the cigarette. These tars cause cancers.
Compounds in Cigarettes/Tobacco
Ask the students to guess how many different compounds can be found in one cigarette. Then show the list on the easel pad >4700 chemical compounds, including carbon monoxide, cyanide, formaldehyde, nicotine, and arsenic are found in tobacco.
Nicotine is one of the chemicals in cigarettes. Nicotine is a DRUG. It is more addictive than cocaine.
.
O U T L I N E D E T A I L S : S M O K I N G
W A T E R B O T T L E E X P E R I M E N T
Short Term Effects
Make this a Question/Answer exercise. Tell the students that smoking does bad things to the outside of your body, too. Ask them what they notice about people who smoke and list their answers on the flip chart. Add any of the following which are not mentioned.
1. Speeds up your heart rate and gives you higher blood pressure.
2. Irritates your eyes.
3. Makes you tired.
4. Stains your teeth and fingers yellow.
5. Gives you bad breath; odor in hair, clothes.
6. Gives you a constant sore throat and cough.
7. Reduces blood flow to the extremities: cold hands and feet.
Transition
It will be important to make an effective transition between the “non-lecture” and the role-playing portion of the presentation. Now, we want the kids to learn about saying NO when someone offers them a cigarette. But we also want them to make use of the information they just received as ammunition.
An example of how you might word this transition is: Now that you know why smoking is so bad for you, let’s put what you’ve learned to use. We are going to act out some situations where some of you will pressure others to smoke. You know how dangerous smoking can be, so use these new facts to say no to smoking.
Remember, the role-playing portion of this presentation is really the most important part. This is where the kids will internalize our message on not smoking; this is where the kids will learn to put the preceding information to use The role-playing is the real test of how successful we are in getting our message across.
I N S T R U C T I O N F O R R O L E -
P L A Y I N G E X E R C I S E
The main message we are trying to get across in this presentation is just to “SAY NO TO SMOKING!” In the role-playing exercise, we are arming them with a variety of ways to say no, which will hopefully help them to deal with different types of pressure.
The purpose of Role-playing is to give the kids a chance to practice saying “no” in situations that they might be faced with in the future (or in the present) and to understand what it feels like to say “NO”. It is a fun way for them to interact with other kids, while reinforcing the “just say NO to smoking” message.
Facilitators should meet/talk with the group leader or teacher prior to the presentation to learn more about the composition of the class (i.e., personalities, characteristics, ability to focus on a project, cliques, etc.)
On the following couple of pages, you’ll see three options for conducting a role-playing exercise. For each option, you should begin with this step. Discuss the cards on “levels of Pressure” and “Techniques for Saying No” with the total class before dividing into subgroups. Inform children that these are suggested techniques to use in their role-playing scenarios. However, they should create their own dialogue, so collect all the cards before you split the class into groups.
Facilitators should observe whether or not children actually use these techniques in their role-play. Give this information to group leaders or teachers so they can utilize this for any post-presentation classes.
I N S T R U C T I O N F O R R O L E -
P L A Y I N G E X E R C I S E
OPTION ONE
1. Divide the class into two groups. The group size will depend on the size of the class.
2. One presenter will direct discussion in one group, while the other presenter directs discussion in the second group.
3. In each subgroup, there will be 4-6 children as role-players and the rest will be observers/critiquers. If time allows, the players and observers can switch tasks.
4. Role players will consist of pressurers and those who say “NO.”
Suggestions for selecting role players include:- consider the more outgoing children to play a reverse role of those who say “NO”- consider the more outgoing children to do the critiquing- the quieter, more passive children should be given the role of pressurerThese suggestions allow children to understand and feel what it is like to put themselves in another character, develop confidence or humility by playing a role opposite their own personality.
5. Place scenarios in a hat or box and let the children pick them at random to add suspense.
6. Facilitators explain the characters of each scenario. You can use the character cards provided for each scenario to help you do this. Give the children 5 minutes to prepare their scene (a time limit must be set to keep them focused). Collect the cards before the scene begins.
I N S T R U C T I O N F O R R O L E -
P L A Y I N G E X E R C I S E
7. Facilitators should meet with the observers/critiquers to discuss the importance of listening while the role players are preparing their scene. 8. Allow each scenario 2-3 minutes to play out before the critique phase begins within each subgroup. There is no need to bring the whole class back together for the critique session. Encourage them to discuss what happened, get their feedback, and talk about other ways they might have dealt with that situation differently.
I N S T R U C T I O N F O R R O L E -
P L A Y I N G E X E R C I S E
OPTION TWO
This option should be used with kids who are “acting out” or who may have trouble focusing on the task at hand. This option gives the facilitators much more control over the situation and the children’s response to the material.
1. Again, split the class into two smaller groups. Try to break up any cliques and try to distribute the more difficult children between the two groups.
2. One presenter will direct discussion in one group, while the other presenter directs discussion in the second group.
3. The role playing in this option consists of the facilitator who acts as the pressurer and all of the children who say “NO.” Suggestions for selecting these role players include.
4. Place the scenarios in a hat or box and let the children pick them at random to add suspense.
5. Facilitators should explain the scenario. You can use the character cards provided for each scenario to help you do this. However, since you are the only pressurer here and all of the children are trying to say “NO” you will have to modify the scene slightly.
6. Allow 3-5 minutes for each scenario, then spend a few minutes talking about ways they might have dealt with that situation differently. Repeat while you have time left in the period.
I N S T R U C T I O N F O R R O L E -
P L A Y I N G E X E R C I S E
OPTION THREE
This option gives the kids much more freedom to create their own situations, situations that have more relevance to their own lives. This option, however, requires that the children are very mature about this topic and are highly focused on the task at hand.
1. Divide the class into two groups. The group size will depend on the size of the class.
2. One presenter will direct discussion in one group, while the other presenter directs discussion in the second group.
3. Begin a short discussion with the children about situations they have encountered where they have been pressured to smoke. Have the children choose one of these situations to act out.
4. For each situation, there should be 4-6 children as role-players and the rest should be observers/critiquers. If time allows, the children can choose another situation and the players and observers can switch tasks.
5. Role players will consist of the pressurers and those who say “NO.” If the children are very focused and mature, they can self-select their roles. However, you can still make some suggestions, including:- the more outgoing children to play a reverse role of those who say “NO”- or, the more outgoing children to so critiquing- the quieter, more passive children can be encouraged to take the role of pressurer These suggestions allow children to understand and feel what it is like to put themselves in another character, develop confidence or humility by playing a role opposite their own personality. 6. Give the children 5 minutes to prepare their scene (a time limit must be set to keep them focused).
P L A Y I N G E X E R C I S E
OPTION THREE
7. Facilitators should meet with the observers/critiquers to discuss the importance of listening while the role players are preparing their scene.
8. Allow each scenario 2-3 minutes to play out before the critique phase begins within each subgroup. There is no need to bring the whole class back together for the critique session. Encourage them to discuss what happened, get their feedback, and talk about other ways they might have dealt with that situation differently.
I N S T R U C T I O N F O R R O L E -
S A M P L E R O L E P L A Y S I T U A T I O N S
1.Marco is a handsome, macho football player who gets good grades. He goes out on a date with Jasmine who is a smart “fly girl.” She offers Marco a cigarette and he refuses.
2. Mary Lou is your regular type of high school girl on the cheerleading squad. She wants to fit in at her new school. When the leader of the cheerleading squad offers her a cigarette in front of all the other girls, she wants to say no.
3. Luis hangs out with his friends. One day his best buddy passes half of his cigarette to Luis. Luis wonders what it feels like to smoke, but he also wants to say no. He has seen how yellow his father’s teeth are from smoking and has second thoughts.
4. Donna is a naïve girl, unsure if herself, and comes from a family of smokers. Luckily none of her friend’s smoke. One day a cool girl offers Donna a cigarette. Donna wants the girl to think she’s cool too, and starts to take the cigarette, but Donna’s friends talk her out of it.
5. Tyrone hates cigarettes and is familiar with smoking facts. His parents both smokes. They feel Tyrone is too fanatical about second-hand smoke; but they respect his position and do not smoke in his presence. Recently, Tyrone learned that his younger sister, Channel, had been experimenting with cigarettes. He decided to talk to her. Channel felt it was okay to smoke since her parents did nothing to discourage it.
I
S A M P L E R O L E P L A Y S I T U A T I O N S
CONCLUSION
Once all of the role-playing is over, your job is to tie everything together for the kids and to reinforce again the main messages.
1. Smoking hurts your body and can even kill you
2. Summarize the techniques for saying NO
3. Don’t Choke on Smoke
Also, quickly summarize for the kids some of the major points of the presentation. Use the flip chart to write these down.
1. Kill over half a million people every year.
2. They make it harder to breath.
3. Cigarettes stink.
4. They can make you sick.
If you have time, you can use this conclusion as a chance to quiz the kids to see what they have learned. Giving them the opportunity to repeat some of the key phrases and information can also help reinforce our message.
End the program by handing out some of the brochures and book markers so that the children have something “tangible” after the program is over.
Finally, we will be sending curriculum book to all of the program directors so that they can follow up with additional anti-smoking exercises and activities. While you are there, you should talk with the program director to encourage them to follow up regularly. The more positive messages the kids are exposed to, the more likely they will be to just say “NO” to cigarettes.
T R A I N I N G M O D E L 2
This model uses the Smoke Screeners program created by the Centers for Disease Control and Prevention. It is an educational program to aid young people in being more aware of the negative messages that are portrayed in movies and videos by educating young people on how to be more media literate
Duration: 1 hour (Additional sessions can be administered for more intense activities. These activities are explained in the moderator’s guide)
Materials: Video and Moderator’s Guide (These can be obtained for free by calling the CDC – 770-488-5705 option 3, publications department or www.cdc.gov/tobacco, please allow up to 6 weeks for delivery)
T R A I N I N G M O D E L 3
This model uses the program Secrets Through the Smoke This is an excellent educational program that speaks about the history of the tobacco industry, the harmful effects of tobacco use, and the effects of tobacco advertising
Duration: 90 – 105 minutes
Materials: Video and Teacher’s Guide (These can be obtained for free by calling the CDC – 770-488-5705 option 3, publications department or www.cdc.gov/tobacco, pleas allow up to 6 weeks for delivery)
T R A I N I N G M O D E L 4
This program, Test Your Lungs, is intended for use on college campuses by setting up a table/booth. The purpose is to target smokers and place them on the path to cessation as well as to prevent others from beginning smoking
Duration: Unlimited
Materials: Display board, white t-shirts, picture of a smoker’s teeth (a picture can be obtained from http://www.sunnetwork.com/azdental/smoke.htm)delete , picture of a smoker’s lungs (http://www.presmark.com/htmlfile/pictures.htm), facts about smoking, what is in cigarette smoke information, survey, smoking cessation information/pamphlets
Instructions: On the display board, arrange the picture of the smoker’s teeth, lungs, and facts about smoking. Place the title (Test Your Lungs) in large, visible letters on the display board or table. Below the pictures place phrases such as (or make up your own): See the beautiful smile smoking can get you; Who would want to kiss a mouth like this?; You may look great on the outside, but this is what smoking is doing to you on the inside; Imaging breathing with lungs like these. Make sure that all information is displayed in a large and visible fashion to attract the attention of individuals walking by.
As students come to the display, have them complete the survey. If he/she is a smoker then they can ‘Test their Lungs.
’How to test lungs: Have the individual light one of their cigarettes/cigars. After the individual inhales the smoke, have him/her place a white t-shirt on his/her mouth and blow the smoke out of his/her mouth onto the t-shirt. The t-shirt will show the effects of what smoking is doing to their lungs.
Follow up with individuals who tested their lungs
T R A I N I N G M O D E L 4
This program, Test Your Lungs, is intended for use on college campuses by setting up a table/booth. The purpose is to target smokers and place them on the path to cessation as well as to prevent others from beginning smoking
Duration: Unlimited
Materials: Display board, white t-shirts, picture of a smoker’s teeth (a picture can be obtained from http://www.sunnetwork.com/azdental/smoke.htm)delete , picture of a smoker’s lungs (http://www.presmark.com/htmlfile/pictures.htm), facts about smoking, what is in cigarette smoke information, survey, smoking cessation information/pamphlets
Instructions: On the display board, arrange the picture of the smoker’s teeth, lungs, and facts about smoking. Place the title (Test Your Lungs) in large, visible letters on the display board or table. Below the pictures place phrases such as (or make up your own): See the beautiful smile smoking can get you; Who would want to kiss a mouth like this?; You may look great on the outside, but this is what smoking is doing to you on the inside; Imaging breathing with lungs like these. Make sure that all information is displayed in a large and visible fashion to attract the attention of individuals walking by.
As students come to the display, have them complete the survey. If he/she is a smoker then they can ‘Test their Lungs.
’How to test lungs: Have the individual light one of their cigarettes/cigars. After the individual inhales the smoke, have him/her place a white t-shirt on his/her mouth and blow the smoke out of his/her mouth onto the t-shirt. The t-shirt will show the effects of what smoking is doing to their lungs.
Follow up with individuals who tested their lungs
F A C T S A B O U T S M O K I N G -
A D A P T E D F R O M A M E R I C A N
C A N C E R S O C I E T Y
Smoking is the most preventable cause of death in our society430,700 deaths per year were attributed to smoking between 1990-1994Smoking is the cause of about 30% of all cancers Smoking is responsible for more than 87% of lung cancer cases overall
In addition to the long-term negative effects of smoking - such as increased incidence of cancer, heart disease, ulcers, and emphysema - smoking can cause numerous short-term negative effects including: increased heart rate and blood pressure, eye irritation, yellow stains on teeth, reduced stamina, and throat irritation; all of which can be seen in teenage smokers
Smoking has made lung cancer the #1 cancer killer of American women
Smoking has been implicated as a risk factor in cancers if the mouth, pharynx, larynx, esophagus, pancreas, uterine cervix, kidney and bladder
Cigarette smoking increases the risk of cancer if the larynx, oral cavity, and esophagus by about seven-fold and contributes to cancer of the kidney, urinary bladder, and pancreas
Other forms of tobacco are not safe alternatives to smoking cigarettes
Cigar use causes cancer of the larynx, mouth, esophagus, and lungBidis (small, brown, flavored cigarettes) are a significant health hazard to users, increasing the risk of coronary heart disease and cancer of the mouth, pharynx and larynx, lung, esophagus, stomach, and liver
F A C T S A B O U T S M O K I N G -
A D A P T E D F R O M A M E R I C A N
C A N C E R S O C I E T Y
Cigar use causes cancer of the larynx, mouth, esophagus, and lung
Bidis (small, brown, flavored cigarettes) are a significant health hazard to users, increasing the risk of coronary heart disease and cancer of the mouth, pharynx and larynx, lung, esophagus, stomach, and liver
W H A T I S C I G A R E T T E S M O K I N G ?
Tobacco smoke contains over 4,000 substances; 47 of them are known to cause cancer. Between 70% and 90% of non-smokers are regularly exposed to secondhand smoke It is estimated that only 15% of cigarette smoke is inhaled by a smoker. The remaining 85% lingers in the air for everyone to breath.
What is in the air? Here, the amount of toxins from one cigarette that a smoker breathes in through a filtered tip versus the amount of toxins released into the air of the end of the same cigarette.
Smoking Cessation Information: These can be obtained for free from the American Cancer Society (www.cancer.org) or the American Lung Association (www.lungusa.org) https://www.lung.org/. Allow ~2 weeks for delivery. The American Lung Association has an online smoking cessation program that anyone can participate in for free.
Pamphlets from the American Lung Association: Facts about Cigarette Smoking; Yes, you can quit smoking For Good; Becoming a Successful Quitter. Pamphlets from the American Cancer Society: Set Yourself Free: A smoker’s guide

A D D I T I O N A L A C T I V I T I E S
Activity #1: Warning Labels
Adapted from the Tobacco-Free Sorts Playbook. Department of Health and Human Services, Centers for Disease Control and Prevention www.cdc.gov/tobacco
There are four different warning labels, which appear on cigarette packs. Go to the store of look at advertisements. Write the four warnings below: 1. 2. 3. 4.
Can you do better than these? Try writing your own warning label and tell it the way you think it should be said:
A D D I T I O N A L A C T I V I T I E S
Activity #2: The Cost of Smoking
Adapted from the Tobacco-Free Sorts Playbook. Department of Health and Human Services, Centers for Disease Control and Prevention www.cdc.gov/tobacco
Smoking is a habit, which is not only unhealthy, it is very costly. Find out the average price for a pack of cigarettes (Marlboro, Camel and Newport are the tree brands purchased by over 80% of all teens – they are also the most expensive). Using the formula below figure what a pack-a-day habit would cost you through your teen years (from age 13-20)
$ (cost per pack) x 365 (days per year) x 7 (years) = $Now list at least five things you hope to own at age 20 that cost about the same amount of money: 1. 2. 3. 4. 5.
Which would you rather have, one of the things listed above, or a head start on health problems, which will ruin your looks, kill your sports performance, and follow you the rest of your life?
A D D I T I O N A L A C T I V I T I E S
Activity #3: Smoking Takes Your Breath Away
Adapted from the Tobacco-Free Sorts Playbook. Department of Health and Human Services, Centers for Disease Control and Prevention www.cdc.gov/tobaccoWarning: Do not attempt this exercise if you have asthma, bronchitis, or any condition, which affects your breathing Do only with your parent’s permission.
The problem with smoking is that it damages your body gradually, and it is sometimes difficult to feel the damage right away. Try this one with a friend.
Get a drinking straw (cut in half) and two small coffee stirrers that look like a miniature straw. Take the large diameter straw; place it in your mouth. Now run in place or jump rope for 2-3 minutes while breathing only through the straw. Do you feel different than normal? This is how your breathing would feel as a young person when it is damaged by only a few years of light smoking.
While you are still out of breath, try breathing through the small diameter straw. Can you feel the difference? You may feel pressure in your chest and a panicky feeling. You may not be able to do this without breathing through your nose. That is how it feels to have emphysema, a breathing disease caused by many years of smoking. Simple acts such as standing up or walking across the room could make you feel that way. Only with emphysema, you could not go back breathing normally. Eventually, most people with emphysema have to use an oxygen tank for a few hours a day.
A
Activity #4 - Jeopardy Game
Adapted from: American Cancer Society, 1599 Clifton Road, N E Atlanta, GA 30329
All age groups like games. It is something that will be effective for third graders to high school seniors. As a follow up to ensure that you educated the kids, the Jeopardy Game can be integrated into the "Don't Choke on Smoke" program. It's a fun way of reviewing the information that was learned during the session. The idea is to take approximately thirty to forty-five minutes educating the students about the effects of cigarette smoking and the importance that they say “No” to this drug (nicotine). You can divide the group by sex (boys against girls), geography (right side of the room versus the children on the left side), or any pre-set division that the students may have in existence. Then, you can test their knowledge of the subject by playing Jeopardy.
The more creative SNMA members of your chapter can create a Jeopardy board. The board will consist of four columns and five rows for a total of twenty questions. The questions will increase in difficulty and simultaneously the point total will increase. Below you will find an example and you may alter the question, categories, etc. to suit your students, but be creative and integrate your own questions, too. Please make sure that you ask questions that were covering during the "Don't Choke on Smoke" sessions which means that if you use the examples below, you must incorporate more education into the sessions that covers all of the topics. At the end of this protocol, you will find some additional smoking facts that may help you with this activity.


G
E N E R A
L S M O K I N G F A C T S
General comments about smoking:
Smoking is the single most important preventable cause of death in our society
Smoking is related to about 434,000 premature deaths each year About 250 million people now living in developed countries will die as a result of smoking.
The estimated annual excess mortality is about 350,000 more than the total number of American lives lost in World War I, Korea, and Vietnam combined. The magnitude of the risk incurred by cigarette smokers is correlated with cumulative exposure.
In addition to the long-term negative effects of smoking - such as increased incidence of cancer, heart disease, ulcers, and emphysema - smoking can cause numerous short-term negative effects including: increased heart rate and blood pressure, eye irritation, yellow stains on teeth, reduced stamina, and throat irritation; all of which can be seen in teenage smokers.
G E N E R A L S M O K I N G F A C T S
Smoking and cancer:
Smoking is the cause of about 30% of all cancers.
Smoking is responsible for more than 87% of lung cancer cases overall
Smoking increases the risk of lung cancer over tenfold.
Smoking has made lung cancer the #1 cancer killer of American women
Smoking has been implicated as a risk factor in cancers if the mouth, pharynx, larynx, esophagus, pancreas, uterine cervix, kidney and bladder.
Cigarette smoking increases the risk of cancer if the larynx, oral cavity, and esophagus by about seven-fold and contributes to cancer of the kidney, urinary bladder, and pancreas.
Cigarette smoking compounds the likelihood of cancer in those exposed to other carcinogenic influences.
Smoking and Other Health Effects
Smokers have twice the risk of dying of heart attacks.
Smoking increases the risk of developing emphysema and chronic bronchitis over five-fold.
Smoking is a major risk factor for coronary atherosclerosis underlying coronary heart disease (CHD), especially myocardial infarction. CHD causes about 560,000 deaths annually, of which it is estimated that 30% or 170,000 are attributable to smoking. One pack of cigarettes per day increases the risk of CHD two-fold.
Smoking is a major risk factor for peripheral vascular disease. This disease is a narrowing of blood vessels that carry blood to the leg and arm muscles. If a blood clot blocks an already narrowed artery, the result could be the damage or even loss of an arm or leg.
G
E
N E R A L S
M O K I N G F A C T S
Compounds in cigarettes
Tobacco smoke contains more than 4700 chemical compounds, including carbon monoxide, nicotine, sulfur dioxide, ammonia, vinyl chloride, hydrogen cyanide, formaldehyde, benzene, and arsenic. According to the EPA, many of these compounds are treated as hazardous when emitted into outdoor air by toxic waste dumps and chemical dumps.
Forty-three compounds in tobacco smoke are known to cause cancer. Some substances it contains can cause permanent and often harmful changes in the genetic material of cells.
Nicotine
Nicotine addiction is “the most widespread example of drug dependence in our country” according to the US Public Health Service.
Nicotine is a toxic and addictive drug, and in combination with the tars and carbon monoxide found in cigarette smoke, it is a serious risk factor for lung disease, various cancers, heart disease, and other illnesses.
Central nervous system effects of nicotine include irritability and tremors. Nicotine may cause intestinal cramps, diarrhea, and increased heart rate and blood pressure.
Physical dependence on nicotine develops rapidly and is severe. A craving for tobacco is accompanied by irritability, anxiety, restless.
G
E N E R A L S M O K I N G
F A C T S
Teenagers and Tobacco
Teenagers who plan to complete four years of college have smoking rates less than half of those without similar plans (Remember, for those who want to be professional basketball or football players, attending college is necessary )
Most teenagers prefer to date nonsmokers, according to a survey conducted for the American Lung Association. Among boys aged 12-17, 78% said they’d prefer to date someone who doesn’t smoke cigarettes. Of the girls, 69% said they’d prefer a date with a nonsmoker. Only 1% preferred to date a smoker.
Sources:
“ACS Cancer Response System” Robbins Pathological Basis of Disease
Lippincott’s Illustrated Reviews -- Pharmacology
INTRO TO MENTAL HEALTH AWARENESS
MENTAL HEALTH ACTIVITIES

HELPFUL RESOURCES
INTRODUCTION
MENTAL HEALTH ACTIVITIES
HELPFUL RESOURCES 2 0 2 0 - 2 0 2 1
I S S U E
I N T R O D U C T I O N
The burden of mental illness on health and productivity in the United States and throughout the world has long been underestimated. Data developed by the massive Global Burden of Disease study, conducted by the World Health Organization, the World Bank, and Harvard University, reveal that mental illness, including suicide, ranks second in the burden of disease in established market economies, such as the United States. Moreover, minorities, particularly African Americans bear a disproportionate amount of this burden.
Here are some interesting facts from the Department of Health and Human Services’ report on Mental Health:
Approximately 12% of the U.S. population – 33.9 million people – identify themselves as African American. The African American population is increasing in diversity as immigrants arrive from many African and Caribbean countries. In 1997, nearly one-fourth of all African American earned more than $50,000 a year. Yet, as a whole, when compared to other racial and ethnic groups living in the U.S., African Americans continue to be relatively poor. In 1999, about 22% of African American families lived in poverty, compared to 13% for the United States as a whole and 8% for nonHispanic white Americans.
I N T R O D U C T I O N
Need for Mental Health Care
Whether African Americans differ from whites in the rate of mental illness cannot be answered simply For African Americans living in the community, overall rates of mental illness appear to be similar to those of non-Hispanic whites Differences do arise when assessing the prevalence of specific illnesses. For example: African Americans may be less likely to suffer from major depression and more likely to suffer from phobias than are nonHispanic whites. Somatization is more common among African Americans (15%) than among whites (9%).
Moreover, African Americans experience culture-bound syndromes such as isolated sleep paralysis, an inability to move while falling asleep or waking up, and falling out, a sudden collapse sometimes preceded by dizziness. While non-Hispanic whites are nearly twice as likely as African Americans to commit suicide, suicide rates among young black men are as high as those of young white men. Moreover, from 1980 - 1995, the suicide rate among African Americans ages 10 to 14 increased 233%, compared to 120% of comparable non-Hispanic whites.
I N T R O D U C T I O N
Need for Mental Health Care
African Americans are over-represented in high-need populations that are particularly at risk for mental illnesses:
People who are homeless While representing only 12% of the U S population, African Americans make up about 40% of the homeless population. People who are incarcerated. Nearly half of all prisoners in State and Federal jurisdictions and almost 40% of juveniles in legal custody are African Americans. Children in foster care and the child welfare system. African American children and youth constitute about 45% of children in public foster care and more than half of all children waiting to be adopted People exposed to violence. African Americans of all ages are more likely to be victims of serious violent crime than are non-Hispanic whites. One study reported that over 25% of African American youth exposed to violence met diagnostic criteria for posttraumatic stress disorder (PTSD). Among Vietnam War veterans, 21% of black veterans, compared to 14% of non-Hispanic white veterans, suffer from PTSD, apparently because of the greater exposure of blacks to warzone trauma.
I N T R O D U C T I O N
Availability of Mental Health Services
The public mental health safety net of hospitals, community health centers, and local health departments are vital to many African Americans, especially to those in high-need populations African Americans account for only 2% of psychiatrists, 2% of psychologists, and 4% of social workers in the United States
Use of Mental Health Services
Overall, only one-third of Americans with a mental illness or a mental health problem get care. Yet, the percentage of African Americans receiving needed care is only half that of non-Hispanic whites. One study reported that nearly 60% of older African American adults were not receiving needed services. African Americans are more likely to use emergency services or to seek treatment from a primary care provider than from a mental health specialist. Moreover, they may use alternative therapies more than do whites. African Americans of all ages are underrepresented in outpatient treatment but overrepresented in inpatient treatment. Few African American children receive treatment in privately funded psychiatric hospitals, but many receive treatment in publicly funded residential treatment centers for emotionally disturbed youth.
I N T R O D U C T I O N
Appropriateness and Outcomes of Mental Health Services
While few clinical trials have evaluated the response of African Americans to evidence-based treatment, the limited data available suggest that, for the most part, African Americans respond favorably to treatment. However, there is cause for concern about the appropriateness of some diagnostic and treatment procedures. For example, when compared to whites who exhibit the same symptoms, African Americans tend to be diagnosed more frequently with schizophrenia and less frequently with affective disorders. One study found that 27% of blacks compared to 44% of whites received antidepressant medication. Moreover, the newer SSRI medications that have fewer side effects are prescribed less often to African Americans than to whites. Finally, even though data suggest that blacks may metabolize psychiatric medications more slowly than whites, blacks often receive higher dosages than do whites, leading to more severe side effects. As a result, they may stop taking medications at a greater rate than whites with similar diagnoses.
SNMA needs to play a major role in correcting these inequalities in diagnosis, treatment and education of mental illnesses in the minority community. In addition, we should be at the forefront of the drive to minimize stigma surrounding mental illness. “T-A-P INTO MENTAL HEALTH!”
M
N T A L H E A L T H A C T I V I T I E S
1 - Student-Based Initiatives
Each chapter must complete five (5) student-based activities in order to fulfill the protocol These activities should focus on the student population and/or medical community. At least one activity from each T-A-P (Treatment Awareness Prevention) initiative should be completed Here are some suggestions
Treatment
Screening for depression, schizophrenia, eating disorders, and anxiety disorders on college campuses (Make sure you have instructions for follow-up and numbers for campus treatment centers)
Partner with your school’s student counseling service to conduct mental health screens for medical students and allow them to self-refer for treatment. (Forms for various screenings as well as national screening day material can be obtained through: https://www.mindwise.org
Awareness
Participate Alzheimer’s) Write an article for your school or local paper about a specific mental illness and where to find resources on mental health Host a seminar which features speakers from the community or your medical school faculty on a mental health topic. Host a debate session that will address controversies in mental health. (treatment of children with medications, psychologists’ prescribing in walk-a-thons for specific mental illnesses (i.e.,
rights, use of seclusion and restraint) Invite students and local psychiatrists to be on the panel.
M
E N T A L H
E A L T H A C T I V I T I E S
Prevention
Invite local ministers to a forum to discuss mental health & religion/spirituality
Lobby your local politicians to maintain and/or improve current mental health resources including area mental health centers, substance abuse centers, and other psychiatric resources
Create an assessment form to measure stigma regarding mental health at your school. Hold a workshop to address the most common myths and to decrease stigma.
Hold information sessions for medical students on how to manage stress as a precursor to major exams.
Promote mental fitness by hosting a guided meditation or relaxation session during exam week.
I E S
2 - Community-Based Initiatives
Each chapter must complete five (5) community-based activities in order to fulfill the protocol To maximize effectiveness, chapters may complete these as a joint activity with other chapters. At least one activity from each T-A-P initiative should be completed
Treatment
Volunteer with a local battered women’s shelter (manning hotlines, donating clothes and toiletries, etc)
Volunteer with a rape crisis shelter
Sponsor a “Gym/Game night” and donate collected proceeds to a local mental health organization
Volunteer at a mental health hospital or program with mentally ill patients
Tutor and/or mentor children and adolescents with learning disabilities (i.e., dyslexia, ADHD, autism, etc.)Work with the homeless population to screen for mental illness and identify available resources (this can be done on the streets or at homeless shelters)
M
N T A L H E A L T H A C T I V I T I E S
Awareness
Conduct a Health Fair that includes booths for various psychiatric illnesses
Hold a small forum for local youth groups (church youth groups, Boys and Girls Clubs, etc) about their exposure to or questions about suicide
Be sure to have local suicide hotline information if you identify someone at risk for suicide.
Educate parent groups about the warning signs of suicide in their children
Educate parents about eating disorders in adolescent females (predominantly) and males
Hold a workshop at a local church, mosque, and synagogue to discuss common misconceptions of the mental health field. Provide information about local faith-based treatment facilities or counseling networks
.Prevention
Hold a self esteem workshop for youths at a local school
Hold a workshop for parents to discuss violence prevention and helping your child cope with bullying
Hold a workshop at a local school about suicide prevention.
1 - www.nami.org
On Campus- mental health programming for use by undergraduate students
Multicultural Outreach Center
SNMA has access to benefits such as: access to information
co-sponsorship of our events
collaboration on community projects
Provider information
Each state has its own site (i.e., www.naminc.org) which has online brochures about mental illness available to download and links, both at the state & natl’ level.
Partnership to Open Doors- a national collaboration between NAMI, National Mental Health Association, & Habitat for Humanity formed to provide safe, affordable housing for people who have a mental illness provides toolkit that have suggestions, ideas, and resources to contact when considering building homes for people with mental illness
Break the Silence (www.btslessonplans.org) – a program that includes lesson plans for grades 4-12 designed to remove the stigma of mental illness which promotes tolerance, anti-bullying, and character development
2 - www.nimh.nih.gov
printed materials on mental illness available
3 - www.mentalhealth.samhsa.gov
Substance Abuse & Mental Health Services Administration National Mental Health Info Center
free publications on mental illness referral sources
health information specialists available at hotline
Children’s Campaign: provides coloring books & posters in English & Spanish about mental illness betterhttps://www.samhsa.gov/homelessness-programs-resources/grantprograms-services/path
4 - https://www.mindwise.org
Information for National Screening Days, including depression, alcohol, anxiety, eating disorders, & suicide will send out kits to perform screening activities
High School SOS Suicide Prevention Program
College Response- education & screening
5 - http://www.bpaincpsych.org/index.php, BPA resource for potential speakers and/or mentors
6 - www.psych.org, American Psychiatric Association Committee of Black Psychiatrists (APA) fact sheets & publications hotline numbers
7 - www.nmanet.org, NMA Psychiatry & Behavioral Sciences Section resource for mentorship, speakers, and information
8 - www.aacap.org, American Academy of Child & Adolescent Psychiatry publications links to regional organizations links to resources
9 - https://www.cdc.gov/healthyyouth/data/yrbs/index.htm, National Youth Risk Behavior Surveillance System
Information and statistics about high school students and suicide
10 - https://www.nami.org/Home, National Alliance of Mental Health state contacts list of 6 effective prevention programs & the 5 core components to these programs educational materials referral sources PSA & brochure specific to BPAD
11 - https://mhaok.org/teen-mental-health-screening
YOUTH SCIENCE ENRICHMENT PROGRAM
HEALTH PROFESSIONS RECRUITMENT AND EXPOSURE PROGRAM
BROTHERHOOD ALLIANCE FOR SCIENCE & EDUCATION

I N T R O D U C T I O N A N D O V E R V I E W
T O P I P E L I N E M E N T O R I N G
I N S T I T U T E
The Student National Medical Association (SNMA) addresses the needs and concerns of medical students of color and provides services to underserved communities. Established in 1964 by medical students from Howard University School of Medicine and Meharry Medical College, SNMA boasts over 40 years of service to underserved communities and medical students. As an independent and student-run non-profit organization, SNMA has over 6,000 members composed of pre-medical and medical students, residents, and licensed physicians from 135 medical schools, colleges, and universities in the U.S. and the Caribbean. The organization advocates for policies that will improve health care services for underserved populations and that will increase the enrollment and retention of medical students of color
Although one-fourth of the nation’s population is of color, less than 10% of its physicians represent that diversity Evidently, there is an unmet need stemming from three general weaknesses:
- Active recruitment and targeted exposure of underrepresented minority (URM) students to this field of study
- Adequate preparation of URM students for the rigorous pursuit of careers in medicine
- A lack of a multi-faceted support structure for students already embroiled in these undertakings.
I
T O P I P E L I N E M E N T O R I N G
I N S T I T U T E
In order to create a diverse healthcare system, students’ preparation should begin very early in their academic careers. The SNMA prioritizes exposure and education starting in elementary school with continued support throughout the trajectory of medical training Such programs are beneficial and necessary, especially in communities where the disparities are great and the number of students pursuing careers in healthcare is disproportionately low.
The Pipeline Mentoring Institute (PMI) exists within the SNMA to address three of the aforementioned weaknesses. Recognizing that many of the barriers to greater diversity within the medical profession lie within the continuum of elementary through undergraduate education, the PMI seeks to close the gap in preparing URM students for a career in medicine and other health-related professions. Specifically, the PMI will focus on establishing pipeline programs that improve general study skills, standardized test-taking skills, and science preparation, promoting age-appropriate, cross-cultural experiences and assessing success, sustainability, and opportunities for growth for pipeline programs across the SNMA Further, the PMI will facilitate students’ exposure to health careers and professional meetings in their chosen field of interest.
The PMI provides the framework and programmatic support for pipeline work within the SNMA. Its primary programs include the Health Professions Recruitment and Exposure Program (HPREP), Brotherhood Alliance for Science Education (BASE), and the Youth Science Enrichment Program (YSEP) The PMI works to foster academic and scientific interest in elementary students and mentor participants as they progress through middle and high school. Through these efforts, the PMI ultimately aims to increase the number of culturally sensitive and capable health professionals.
I
M A N A G E M E N T
Pipeline Mentoring Institute Fellow
The PMI Fellow bears ultimate responsibility for the overall implementation and management of the Pipeline Mentoring Institute. The Fellow is responsible for setting a plan for PMI programming each administrative year. The Fellow will supervise and coordinate all PMI activities The Fellow will work closely with the National Board of Directors and convey information from national leadership to the committee This position is available for both pre-medical and medical student members of the SNMA.
Pipeline Mentoring Institute Director
The PMI Director is appointed by the PMI fellow each year to assist with meeting logistics and grant application/management This position is available for both pre-medical and medical student members of the SNMA
Pipeline Mentoring Institute Advisory Council
The Advisory Council will serve as the primary programmatic planning body for the PMI. The Council will be the main resource for the PMI Fellow for the programmatic structure of the Academy. Based on its experience with pipeline programs, the Council will develop and revise the Academy guidelines and curricula, offer suggestions and advice for individual programs, and will maintain regular communication with the PMI Chair The Council will include, but not be limited to:
●
●
●
●
● Regional Director Representative
National Vice President National Pre-Medical Board
Member SNMA-Kaiser Permanente Fellow
Community Service Committee chair
PMI Director
A professional board member may choose to sit in on Council meetings and engage with the leadership. Should a Future Leadership Project fellow(s) wish to complete a project centered around pipeline work, they may also sit on the Council
Subcommittees/Workgroups
● Research/Quality & Improvement: led by KP fellow
-Coordinates with membership, diversity research, and community service committees to evaluate pipeline work being done across the SNMA
● Strategic Planning subcommittee
Works closely with the national president, PMBM, MAPS leadership to set a strategic plan for each administrative year
-The MAPS Internal Affairs Chair would be recommended to serve on this subcommittee/workgroup
-Ensures completion of PAIR reports, annual reports to the NVP, CSC subcommittee reports, and transition documents
● Webinars/Academy Oversight subcommittee
-Offers region and chapter-based support for the Academy programs (HPREP, YSEP, and BASE)
-Pre-medical student representatives from each region are encouraged to sit on this subcommittee to ensure they have the resources to support the work in their regions
-Responsible for regional and chapter-based training and education around the PMI as a whole and Academy programs
I N S T I T U T E D E S I G N
Goals
● Increase the recruitment of URM and disadvantaged students in grades K-12 for careers in medicine and other health-related professions through the Pipeline Academy.
● Increase cultural humility in academic environments through regional workshops focusing on the need for the diversity of the medical and other health-related professions
● Increase the academic and social preparedness of URM and disadvantaged students for careers in medicine and other health-related professions.
- To provide age and culturally appropriate academic and social skills that will assist their retention in the pipeline to the health professions
-To provide access to and mentorship from health professionals and medical students To provide exposure to the daily activities and environment of health professionals through interactive, hands-on experiences.
- To provide parents and advisors with background information on the health professions and the advice and guidance necessary for their children to become successful health professionals
Facilitated by medical and pre-medical chapter sites, SNMA will carry out these goals through focused programs: YSEP for grades 4 through 8, BASE for male-identifying students, and HPREP for grades 9 through 12. Each Academy program will act with five focuses in mind Education, Exposure, Parent/Advisor Preparation Mentorship, and Cultural Humility The PMI suggests these programs span for the duration of the school year to ensure retention and longitudinal engagement however program length and implementation is at chapters’ discretion.
1. Education Standardized curricula will be created and used for each of the targeted grade groupings Academic and social preparation will focus on age and culturally appropriate science education, standardized test preparation, critical thinking skills, and professional development. The SNMA community service health prevention protocols leveraged to create standardized curricula with a specific focus on mental health awareness, smoking cessation, violence prevention, obesity prevention, and sexual health awareness SNMA medical and pre-medical students will conduct all workshops with assistance from chapter/institutional faculty, academic counselors, and/or school teachers.
I N S T I T U T E D E S I G N
2. Exposure
Interactive and innovative exposure to local healthcare offices, hospitals, research laboratories, academic facilities, community centers, and public health agencies should be provided Age and culturally appropriate tours may be led by SNMA medical and premedical students and include presentations that demonstrate current medical technology, various aspects of clinical medicine, interesting medical/basic science research, public health concerns, and current issues facing URM communities.
3. Parent/Advisor Preparation
Parents and advisors of Academy students will be invited, but not required, to take part in the Academy in order to provide them with insight on higher education, the pipeline into the health professions, psychosocial needs of students, financial aid, and overall career development. SNMA medical students, in partnership with school teachers, will conduct the parent and advisor preparation workshops based on a standardized curriculum
4. Mentorship
SNMA medical students and pre-medical members will serve as mentors to Academy students. Mentorship may include one-on-one discussions between SNMA members and the Academy students, workshops for Academy students, group events, and other initiatives concerning the career and personal development and long-term strategies of success Mentorship shall always be at the center of Academy programming
5. Cultural Humility
Workshops will be organized and held regionally that focus on cultural humility, diversity of the health professions, and the importance of mentoring. Local faculty, community health professionals, academicians, medical students, other health professional students, advocacy organizations, and community members will be invited to participate through targeted outreach Partners of the SNMA, such as the National Medical Association, will be asked to assist in the creation of a workshop curriculum and its presentation.
F I N A N C I A L C O N S I D E R A T I O N S
The PMI Committee will utilize funds awarded through the KP fellowship and outside grants to support its work and programming. The following initiatives may be funded through the fellowship as allowed by current contractual language and obligation and with the expressed consent of the KP fellow, Kaiser-Permanente leadership, and the Chair of the Board of Directors.
PMI Grant Program
Each year, ten awards will be given out to chapters that submit appropriate application materials Award amount will be determined by the PMI Council and approved by the National Treasurer. The PMI council will be the primary body responsible for grant management and resource allocation once chapters have been awarded.
HPREP, BASE, YSEP
The PMI may financially assist chapters demonstrating program success throughout the year to support their program endeavors per the financial guidelines
Research
Funds may be used to purchase assessment tools, contract statisticians to evaluate data, offer work stipends for students completing assessments or other needs contributing to research and Q&I.
Training and Education
Annual Medical Education Conference (AMEC): workshops speakers honorariums, travel stipends for MAPS members and Academy students looking to attend AMEC and other needs related to AMEC planning and workshop implementation.
Regional workshops: focused training around Academy program protocols, chapter report form submission and other elements of the PMI
Chapter Report Forms (CRFs) should be completed online for review by the National Board of Directors and Pipeline Mentoring Institute Committee. CRF templates can be found https://snma org/page/crf CRFs will be due on January 15, April 15, July 15, September 15 to report on the 3 months prior to the due date Reports will include:
● ● ● ● ● number of students who applied number of participants accepted racial, gender, the ethnic makeup of participants description of sessions funding used dates of the program thoughts, comments, and concerns about the activity (can include medical student feedback forms)
P R O G R A M ( H P R E P
)
INTRODUCTION
The aim of the HPREP program is to provide an added foundation and experience to those students interested in pursuing a career in the health professions. By seeing and hearing minority physicians lecture on issues at the forefront of medicine, as well as having minority medical students interacting with them, high school students would have essential role models and interaction opportunities rarely experienced by the minority high school student. The exposure to the educational institution and hospital would allow the student to envision him/herself within a setting of this nature 6-7 years ahead into the future, encouraging him/her to overcome the academic challenges and hurdles that he/she will encounter
This program is not an educational remedial program that would provide assistance with coursework. This program targets underrepresented minority high school students (grades 9-12) who have demonstrated an ability to perform satisfactorily in their course work as well as shown an interest in the sciences
The Health Professions Recruitment & Exposure Program is designed:
- To promote interest and increase awareness in the health professions among underrepresented minority high school students
- To increase the number of minorities entering the health professions, allied health fields, and graduate sciences.
- To facilitate interactions between under-represented high school students, medical students, and faculty of health science institutions.
- To Increase high school student awareness of the unique needs of the minority and economically disadvantaged communities.
- To strengthen high school student's knowledge base of scientific, sociopolitical, and cultural factors that affect health
- To counsel serious college-bound minority high students on college survival skills and the premedical curriculum.
S T U D E N T
NATIONAL MEDICAL ASSOCIATION HEALTH PROFESSIONS RECRUITMENT EXPOSURE PROGRAM (HPREP)
The Student National MedicalAssociation (SNMA) was established because of a need to produce an increasing number of particularly sensitive and excellent physicians to serve minority and indigent communities. The communities suffer disease, illness, and deprivation which, in comparison to the majority community, is both appalling and unacceptable From the realization of the unique concerns, generally non-academic, endured by minority medical students, and the lack of a mechanism by which to address these problems, the SNMA was generated.
In light of this, the SNMA chapter of [YOUR SCHOOL NAME] is searching for motivated minority high school students (9th through 12th grade) who are interested in the sciences to participate in its Health Professions Recruitment Exposure Program The Program consists of [NUMBER] 2-hour seminars once a week during the months of [DATES]. During this time, students will hear lectures on different issues in medicine, participate in group activities and discussions, and receive information concerning college and other program opportunities. Participants will also be required to write a 35 page paper and give an oral presentation on any issue in medicine, and cannot miss more than two (2) sessions to avoid being dismissed from the program
To apply, To apply, please send the following application materials by [DEADLINE] to the address below: ●
Application page
< 300-word essay
Signed contract agreeing to comply with program requirements
Copy of high school transcript (if applicable)
Signed liability waiver to be completed by parents and students
Letter of recommendation from a teacher or counselor








Y
E N R I C H M E N T P R O G R A M
INTRODUCTION
One of the major challenges facing America today is the education status of people of color. As minority medical students and members of the Student National Medical Association, we are dedicated to addressing the disparity, exposure to health professions, that exists within our public school system. Since 2009, the average national science score for African-American students has declined as they matriculate from elementary to high school (Nat 17) This issue will continue to affect the evolving scientific field. According to the Institute of Medicine Committee on Educating Public Health Professionals, schools are faced with the need to evolve because of scientific advances and the increased understanding of the determinants of health, their linkage, and their interactions The Youth Science Enrichment Program (YSEP) provides early, targeted exposure to health professions for elementary and middle school students. As a national body of future physicians, our hope is that YSEP will be an experience that positively influences students’ perception of science
YSEP aims to...
●
● To provide a scientific teaching model that is enjoyable and captivating
To serve as a conduit to increase the number of minority students seeking careers in science
● To increase retention, graduation, and college matriculation among participating students
●
● To improve students’ performance in science courses
To introduce the students to positive role models in the science field
O N L I N E R E S O U R C E S
http://www how-to-study com/
Interactive online study skills curricula for elementary, middle, and high school students
http://www.bls.gov/k12/
The Bureau of Labor Statistics provides students with resources to find careers that relate to their interests
http://stemcareer com/
This site provides STEM career information, videos, research, and learner resources for students, counselors, and teachers
http://explorehealthcareers.org/en/home
For students interested in health careers and would like to explore various career choices
http://afsc.org/sites/afsc.civicactions.net/files/documents/itsmylife.pdf
A brochure that provides students with alternative career choices after high school
http://www engineeringk12 org/
Sponsored by the American Society for Engineering Education, this site seeks to gather and promote engineering education resources available to K-12 students
http://www pathwaystoscience org/programs aspx?u=K8Students K8%20Students&r=&s=&sa=either&p=either&c=either&f=&dd=&ft=&submit=y&adv=adv
A list of science programs for K-8 students
http://www.wikihow.com/Set-SMART-Goals
Explains how to set SMART goals
B R O T H E R H O O D A L L I A N C E F O R
S C I E N C E E D U C A T I O N ( B A S E )
INTRODUCTION
Health disparities often affect minorities the most by way of perception of health, the healthcare system, and access to care (Smedley, Stitch, Colburn, et al., 2001). For half a century, the 25,000 Blacks or African-Americans that have graduated from medical school, were more likely to work in underserved communities than their white peers (Xierali, Nivet,2018). Black and African Americans are not just necessary to perform their medical roles, they are also necessary for establishing quality care. According to the National Academies of Sciences, Engineering, and Medicine, minorities receive a lower quality of care despite age, income, and insurance status which partly contributes to their rising death rates (The National Academies of Sciences, Engineering, and Medicine, 2002). Unfortunately, from birth Black and African American men have the lowest life expectancy than their female and white male and female counterparts (Bond, Jermane, Herman, 2016).
In the context of these statistics, the Brotherhood Alliance for Science and Education (BASE) was developed to respond to the many factors that impede the educational development of minority men including the lack of educational opportunities, lack of encouragement, lack of positive role models, and misguided messages about manhood and achievement. This program aims to address these and other factors with the aforementioned goals and the following objectives in mind:
- To strengthen current ties between underrepresented minority medical students and undergraduates with an emphasis on mentoring undergraduate men
- To collaborate with Minority Association of Pre-medical Student (MAPS) chapters to achieve the above objectives
- To target young males in elementary, middle, and high school and expand relationships with middle and high schools engaged with HPREP and YSEP programs
- To foster continued community/parental support and participation by engaging parents at each level of the planning and preparation stages
- To collaborate with local National Medical Association chapters/faculty as a source of guidance, support, and mentoring relationships for all levels.
The BASE program is designed to engage young people that identify as men and boys from primary education through the undergraduate level and offer them tangible skills and intangible support by medical students, residents, and faculty Additionally, the BASE protocol is designed to utilize the SNMA’s existing pipeline programs such as HPREP, YSEP, or programs embedded within the MAPS structure in order to further, offer them mentorship and guidance.
BASE programming is designed to
● Increase the number of underrepresented minority males (Black, Latino, Native American) advancing through grade school and higher education, with the ultimate goal of increasing their representation in medicine.
● Foster and develop mentoring relationships among members of the pipeline and those beyond to provide a personal source of guidance and support at each level.
● Present higher education, professional development, and health careers as attainable and worthwhile goals for young men and their parents. To instill the importance of community service, community empowerment, and “giving back” in the target population
A P P E N D I X










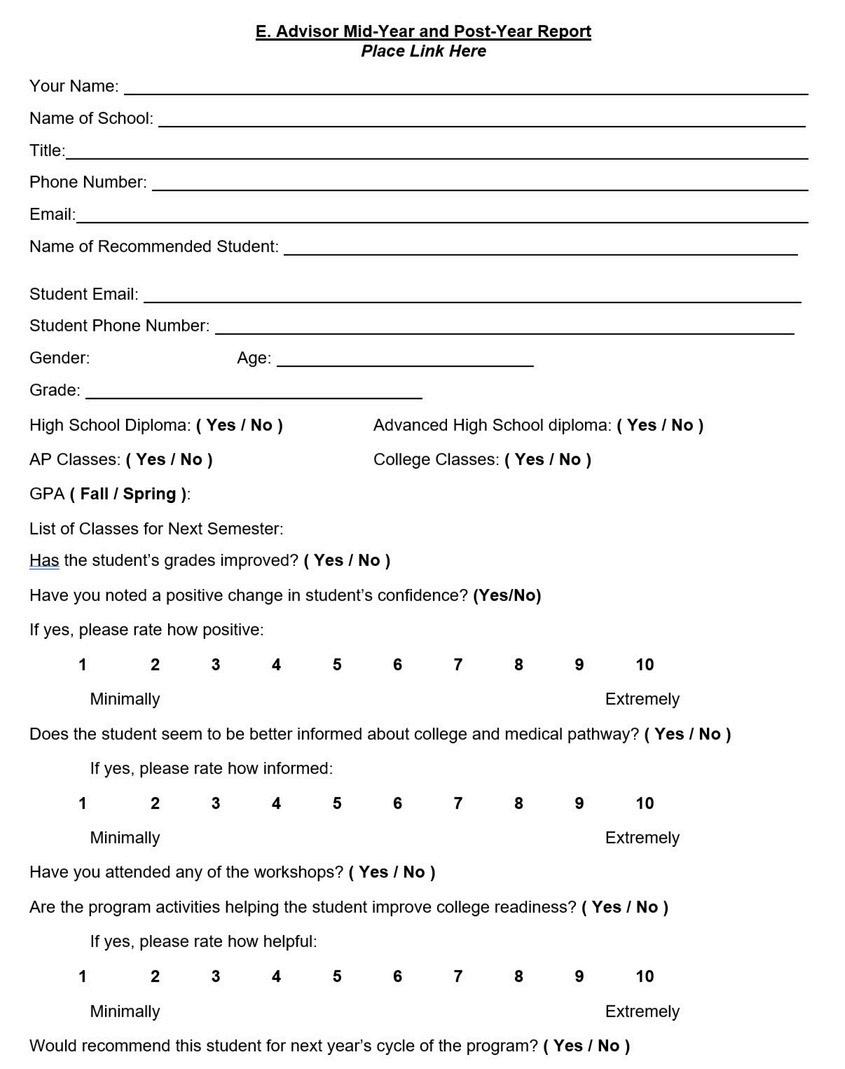



Aspiring Docs (An AAMC Campaign to Increase Diversity in Medicine: www.aspiringdocs.org
Boys Scouts of America / Girl Scouts of America: www.scouting.org / www.girlscouts.org
Boys & Girls Clubs of America: www bgca org
Hip Hop 4 Life: www hiphop4lifeinc org
YMCA / YWCA: www.ymca.net / www.ywca.org
SNMA Pipeline Mentoring Institute: https://snma org/page/programspipeline (Under programs ->Pipeline)
American Medical Student Association: www.amsa.org/members/amsa-premeds
Be The Match® Registry / Cord Blood Donation: www.marrow.org
American Red Cross: www redcross org
National Minority Organ Tissue Transplant Education Program: www.nationalmottep.org
Organ Procurement and Transplantation Network (OPTN): www optn transplant hrsa gov
Organ Donor: www.organdonor.gov
CDC Healthy Living: www cdc/healthyliving
CDC Division of Nutrition, Physical Activity & Obesity: www.cdc.gov/nccdphp/dnpao
CDC Division for Heart Disease & Stroke Prevention: www.cdc.gov/dhdsp/
WISEWOMAN – Well–Integrated Screening and Evaluation for Women Across the Nation: www.cdc.gov/wisewoman
Smart Nutrition 101: www.nutrition.gov
National Diabetes Education Program: www ndep nih gov
Weight-control Information Network: www.win.niddk.nih.gov
Surgeon General’s Vision for a Healthy & Fit Nation: www surgeongeneral gov/library/obesityvision
The State of Obesity: A project for The Trust for America's Health and the Robert Wood Johnson Foundation: www.stateofobesity.org/disparities/blacks
U.S. Department of Health and Human Services Office of Minority Health: www.minorityhealth.hhs.gov/omh/browse.aspx?lvl=4&lvlid=25
Tar Wars: www tarwars org
American Lung Association: www.lung.org
American Public Health Association Tobacco Control and Prevention: www apha org/programs/resources/tobacco
CDC Smoking & Tobacco Use: www cdc gov/tobacco
CDC Youth Tobacco Prevention: www.cdc.gov/tobacco/youth
National African American Tobacco Prevention Network: www.naatpn.org
American Legacy Foundation: www legacyforhealth org
Campaign for Tobacco-Free Kids: www.tobaccofreekids.org
The Truth® Campaign: www.thetruth.com
CDC Sexual Health: www cdc gov/sexualhealth
CDC HIV/AIDS and African Americans: www.cdc.gov/hiv/topics/aa
Advocates for Youth: Lesson Plans: www.advocatesforyouth.org/lessonplans/index.htm
Teens Health: Sexual Health: www kidshealth org/teen/sexual health
Girls Inc.: Fact Sheets & Resource Sheets: www.girlsinc.org/resources
AVERTing HIV & AIDS: www avert org
The Sexual Health Network: www.sexualhealth.com
STI testing locators: www gettested cdc gov
The Family Planning Association: www.fpa.org.uk/resources/leaflet-and-bookletdownload
Great website resources with event suggestions, supplies, and resources for LGBT awareness programs for medical students: http://www.amsa.org/AMSA/Homepage/About/Committees/GenderandSexuality/LGBT PIB .aspx
CDC; Lesbian, Gay, Bisexual, and Transgender Health website: http://www cdc gov/lgbthealth/
US Department of Health and Human Services; Gay, Bisexual and Transgender Health website: http://www.healthypeople.gov/2020/topicsobjectives2020/overview.aspx?topicid=25 Primary Care of LGBT Patients
PowerPoint, courtesy of the American Medical Students Association: http://www.amsa.org/AMSA/Libraries/Committee Docs/LGBT PrimaryCare1.sflb.ashx
Southern Comfort Documentary, which tells the story of Robert Eads, a female-to-male transsexual who was diagnosed with ovarian cancer and turned down for treatment by physicians out of fear that treating such a patient would hurt their reputation This film has a powerful message and can be shared with your chapter The film is separated into 6 short videos; consider showing a clip or the entire film: https://www.youtube.com/watch?v=awxN TecaII
Transgender Community Health Project (TCHP) quantitative study performed by the San Francisco Department of Public Health, generating statistical data on the transgender community of San Francisco: http://hivinsite ucsf edu/InSite?page=cftg-02-02#S5 6X
National Alliance on Mental Illness (NAMI) Multicultural Action Center: www nami org/multicultural
Mental Health America: www nmha org
Mental Health - A Report of the Surgeon General: www surgeongeneral gov/library/mentalhealth/home
National Institute of Mental Health: www.nimh.nih.gov
Break the Silence: A program that includes lesson plans for grades 4-12 designed to remove the stigma of mental illness which promotes tolerance, anti-bullying, and character development: www.btslessonplans.org/
Screening for Mental Health: www mentalhealthscreening org/
High School SOS Suicide Prevention Program: www nais org/Articles/Pages/SOS-(Signsof-Suicide)-High-School-Suicide-Prevention-Program- 144960 aspx
Stop Bullying Now: www.stopbullyingnow.com
National Sexual Violence Resource Center: www.nsvrc.org
National Crime Prevention Council (NCPC): www ncpc org
Family Violence Prevention Fund: www.endabuse.org
Celebrate Safe Communities – An NCPC Program: www ncpc org/programs/celebratesafe-communities
CDC Injury Prevention & Control: Violence Prevention: www.cdc.gov/violenceprevention
V I O L E N C E

YOUTH VIOLENCE
HUMAN RIGHTS
DISOBEYING THE LAW
3 0 4 0 7 0 9
Youth Violence Program Objectives Disobeying the Law 2 0 2 0 - 2 0 2 1
O N T E N T S I S S U E
Human Rights
O B J E C T I V E S
Goals
Explore causes of violence
Explore ways to prevent violence
Educate on the consequences of violent acts
Target Group(s)
Young people from elementary to high school
The local Boys and Girls
Club in your city is a recommended site.
Y O U T H V I O L E N C E
Overview
Violence is defined as “the intentional use of physical force or power, threatened or actual, against oneself, another person, or against a group or community, that either results in or has a high likelihood of resulting in injury, death, psychological harm, maldevelopment or deprivation” (Krug et al. 2002).
Youth violence includes aggressive behaviors such as verbal abuse, bullying, hitting, slapping, or fist fighting Youth violence also includes serious violent and delinquent acts such as aggravated assault, robbery, rape, and homicide, committed by and against youth
In addition to causing injury and death, youth violence undermines communities by increasing the cost of health care, reducing productivity, decreasing property values, and disrupting social services (Krug et al. 2002).
Facts
Nearly 1 in 5 high school students reported being bullied on school property in the last year, and about 1 in 7 were electronically bullied (texting, Instagram, Facebook, or other social media) (CDC 2020)
Homicide is the 3rd leading cause of death for young people ages 1024 Each day, about 13 young people are victims of homicide and about 1,100 are treated in emergency departments for nonfatal assaultrelated injuries (CDC 2020). Youth violence has serious and lasting effects on the physical, mental, and social health of young people. It is a leading cause of death for young people and results in more than 400,000 nonfatal injuries each year (CDC 2020).
Y O U T H V I O L E N C E
Risk Factors
The first step in preventing youth violence is to identify and understand the risk factors A risk factor is anything that increases the likelihood of a person suffering harm. Risk factors are not necessarily causes. Research has identified the following risk factors for youth violence (DHHS 2001; Lipsey and Derzon 1998):
Individual
Attention deficits/hyperactivity
Antisocial beliefs and attitudes
History of early aggressive behavior
Involvement with drugs, alcohol, or tobacco
Early involvement in general offenses
Low IQ
Poor behavioral control
Family
Exposure to violence and family conflict
Harsh, lax, or inconsistent disciplinary practices
Lack of involvement in the child’s life
Low emotional attachment to parents or caregivers
Low parental education and income
Parental substance abuse and criminality
Poor family functioning
Poor monitoring and supervision of children
Peer/School
Association with delinquent peers
Involvement in gangs
Social rejection by peers
Lack of involvement in conventional activities
Poor academic performance
Low commitment to school and school failure
Neighborhood/Community
Diminished economic opportunity
High concentrations of poor residents
High levels of family disruption
Low community participation
Socially disorganized neighborhoods
Y O U T H V I O L E N C E
Web Chart Activity
Solicit participants' comments on their beliefs about the causes of violence by utilizing a web chart
Divide the group evenly into teams.
You will need have one medical student volunteer for each group.
In a center of a large piece of paper, write the word “Violence.”
Ask the students to think about what causes violence and list the causes around the outside of the paper
Draw arrows from the “causes” to the word Violence
The following topics should be discussed in this session:
Racism
Money and power
Lack of opportunities
Poor schools
Few jobs
Insufficient after-school programs or sports teams, etc
Limited access to resources
No food
Poor access to health care
Poor housing, etc
Drugs
Fights between friends, family or strangers
War
The media
TV
Movies
Music
Music videos
Video games, etc.
Being “dissed” (disrespected) or being shamed (violations of one’s dignity)
In order to facilitate the discussion, the session leaders must be prepared to introduce these examples if the students do not mention them and should be able to discuss how he/she feels these issues contribute to violent behavior.
H U M A N R I G H T S
"Universal Declaration of Human Rights"
All humans are born free and equal in dignity and rights and should treat one another in a spirit of brotherhood.
Everyone has the right to life, liberty and security of person
No one shall be held in slavery
No one shall be subjected to torture or cruel, inhuman or degrading treatment.
Everyone is equal before the law and has equal protection by the law.
Everyone is entitled to an effective remedy when his or her fundamental rights are violated.
Everyone has the right to a standard of living adequate for the health and well being of him/herself and of his/her family, including food, clothing, housing, medical care and necessary social services.
No one shall be subjected to arbitrary arrest, detention or exile.
No one shall be subjected to arbitrary interference with his/her privacy, family, home or correspondence, or to attacks upon his/her honor or reputation.
Everyone is free to move
Everyone has a right to visit other countries with full access to human rights
Everyone has a right to a nationality.
Everyone has the right to marry and found a family.
Everyone is allowed to own property.
Everyone has the right to freedom of thought, conscience and religion.
Everyone has a right to freedom of opinion and expression
Everyone has the right to peaceful assembly and association
Everyone has the right to take part in government and to serve his/her community or country.
Everyone has the right to work in his or her choice of employment.
Everyone has the right to social security, including economic, social and cultural rights for the development of his/her personality and dignity Everyone has the right to work in his or her choice of employment
Everyone has the right to rest and leisure, including limits and assistance.
Everyone has the right to education. Furthermore, education shall be free in the elementary stages and should be directed to the full development of the human personality and to the strengthening of respect of human rights and fundamental freedoms
Everyone has the right to freely participate in the cultural life of his or her community.
Everyone has duties to the community in which alone the free and full development of his personality is possible.
H U M A N R I G H T S
Human Rights Activity
Solicit participants' comments about a list of "rights" in a document of human rights
Divide participants into groups of 3 or 4
Ask participants to compile a list of “Rights” they would include in a document of human rights.
Have each group present the rights they included and why they thought they were important.
In a large group, pass out a list of rights included in the United Nations “Universal Declaration of Human Rights” document
Ask participants to compare this list to the rights they listed for their document
When presenting the Human Rights Declaration, it is important for session leaders to be prepared to discuss why human rights violations may make someone become violent.
D I S O B E Y I N G T H E L A W
County Jail Field Trip
Contact your local county jail and state you are requesting a tour for minority students of local elementary, middle, and high schools as part of a violence prevention program. Identify that you are with the SNMA and inform them of the purpose of the visit.
Fill out the necessary paperwork and make sure all students have parental consent, if needed.
Guest Speaker
Contact either a deputy sheriff from your local police department, a juvenile justice corrections officer, or a local county judge and request their time as a guest speaker as part of a violence prevention program, targeting minority students in the area.
Identify that you are with the SNMA and inform the potential speaker of the purpose of the exercise. Inform the potential speaker the list of topics to be covered can range from but is not limited to The demographical make-up of prisons and juvenile correction facilities (age, sex, race, average time of imprisonment) The most common crimes resulting in imprisonment he role drugs and alcohol play in committing crimes The civil rights lost after committing felonies/misdemeanors The importance of staying in school and higher education Personal experiences
It is our hope that this session will serve as a constant reminder to our students of the repercussions of disobeying the law. Likewise, we anticipate the impact of this exercise will deter students from committing violent acts and further advance our mission of violence prevention.
