Decision Medicine
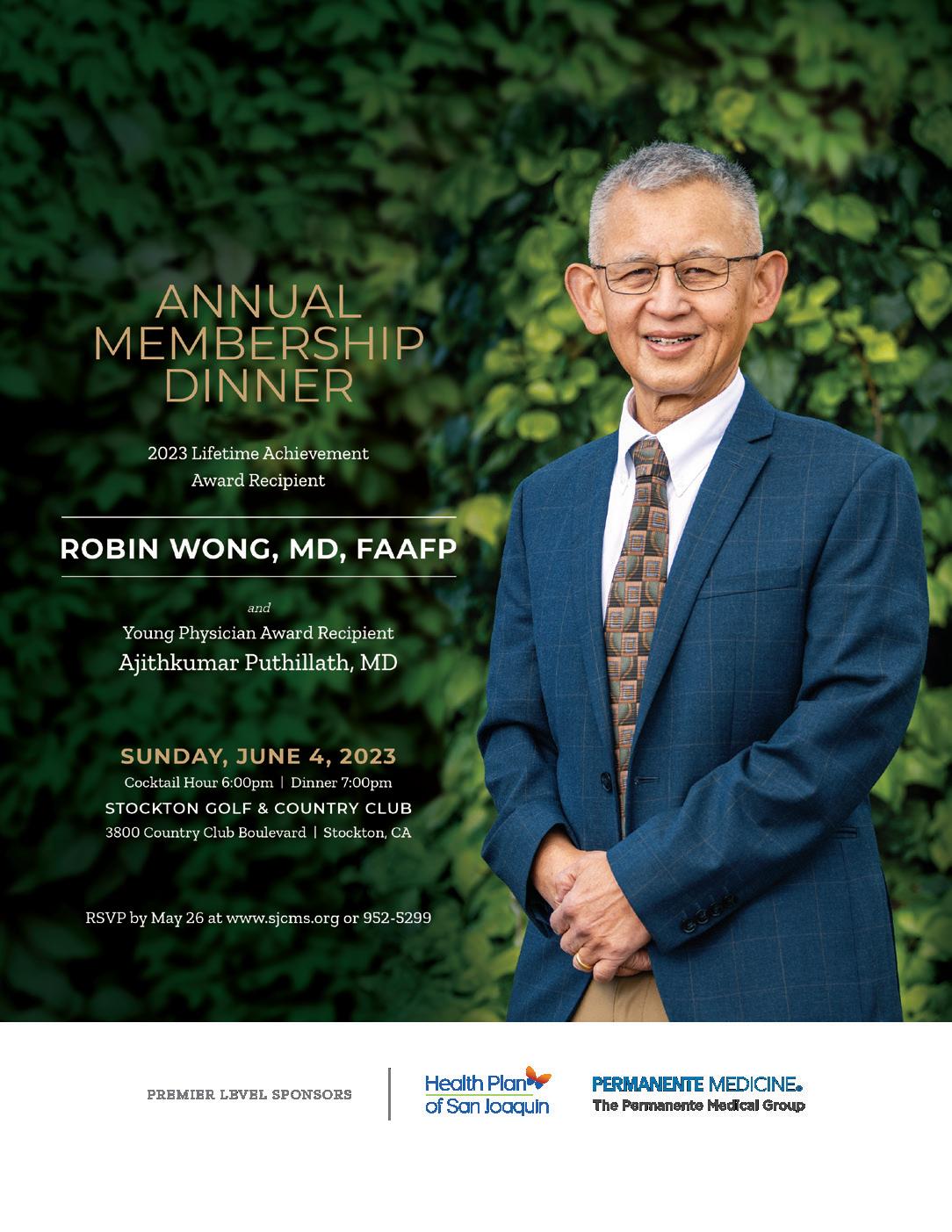
Annual Membership Dinner

A Note to My Patients


Poor documentation during intake resulted in a

Decision Medicine
Annual Membership Dinner

A Note to My Patients


Poor documentation during intake resulted in a
causing permanent damage to a good knee.
The Joint Commission data reveals that wrong-site incidents are the fourth most frequently reported sentinel event.
To minimize surgical errors, practices insured by ProAssurance can access annual risk assessments to learn how well their surgical teams and protocols are working. Risk consultants gather and review the data, note potential weak spots, and deliver recommendations based on former claims.
Helping our insureds assess their patient safety procedures and sharing strategies learned from our closed claims history helps them mitigate risk and be prepared if they ever need to face a malpractice claim.


PRESIDENT Cyrus Buhari, DO PRESIDENT ELECT Neelesh Bangalore, MD TREASURER Sujeeth Punnam, MD
BOARD MEMBERS Stephen Tsang, MD, Maggie Park, MD, Alain Flores, MD, Manreet Basra, MD, Sanjeev Goswami, MD, Kinnari Parikh, MD, Inderpreet Dhillon, MD and Bhagya Nakka, MD, Sunny Philip, MD, Ripudaman Munjal, MD
MEDICAL SOCIETY STAFF
EXECUTIVE DIRECTOR Lisa Richmond
MEMBERSHIP COORDINATOR Jessica Peluso
COMMITTEE CHAIRPERSONS
CMA AFFAIRS COMMITTEE Larry Frank, MD
DECISION MEDICINE Kwabena Adubofour, MD
MEDICAL EDUCATION PROGRAMS Kelly Savage, MD
SCHOLARSHIP LOAN FUND Gregg Jongeward, PhD
CMA HOUSE OF DELEGATES REPRESENTATIVES
Robin Wong, MD, Lawrence R. Frank, MD
James R. Halderman, MD, Raissa Hill, DO Richelle Marasigan, DO, Ramin Manshadi, MD
Philip Edington, MD , Sujeeth Punnam, MD
Sunny Philip, MD, Ripudaman Munjal, MD
SAN JOAQUIN PHYSICIAN MAGAZINE
EDITOR Lisa Richmond
EDITORIAL COMMITTEE Lisa Richmond, Cyrus Buhari, DO
MANAGING EDITOR Lisa Richmond
CREATIVE DIRECTOR Sherry Lavone Design
CONTRIBUTING WRITERS Jo Ann Kirby, Cyrus Buhari, DO, Alex Dingess, MPH, Gwen Callaway, MPH
THE SAN JOAQUIN PHYSICIAN MAGAZINE
is produced by the San Joaquin Medical Society
SUGGESTIONS, story ideas are welcome and will be reviewed by the Editorial Committee.
PLEASE DIRECT ALL INQUIRIES AND SUBMISSIONS TO:
San Joaquin Physician Magazine
3031 W. March Lane, Suite 222W Stockton, CA 95219
Phone: (209) 952-5299 Fax: (209) 952-5298
E-mail Address: lisa@sjcms.org
MEDICAL SOCIETY OFFICE HOURS:
Monday through Friday 8:30am-4:30pm
Closed for Lunch between 12pm-1pm




celebratory banquet this year. I know you’ll enjoy reading more about her story!

Dr. Armendariz is the perfect example of the goal of Decision Medicine and Bridge to Medicine; to encourage high achieving students to go on to medical school and return to serve the communities in which they grew up. We know it’s not that simple, and there is no doubt it takes a long time to see the return on investment, but stories like Vanessa’s make it all worth it.
When I started at SJMS is Spring of 2013, I inherited two awesome staff members, Jessica Peluso, Membership Coordinator and Vanessa Armendariz, Community Relations Manager. Vanessa had recently graduated from Johns Hopkins University and was taking a break before applying to medical school. Her mentor, Dr. Adubofour, and my predecessor, Mike Steenburgh, worked to create a position at the medical society for her to gain meaningful experience.
Vanessa’s primary responsibility was to facilitate Decision Medicine, of which she was a participant in 2005! She knew firsthand the impact the program made on her and was passionate about elevating it during her in time at SJMS. Throughout medical school and training, many have been rooting for her from home and anxiously awaiting her return to the community. As promised, Vanessa is back and recently started a position as a family medicine physician with Community Medical Centers. As if to tie it up in a neat little bow, she was the keynote speaker at our Decision Medicine
Beyond the program s themselves, once a student is in the “BTM/DM family” we work to stay in touch, notifying them of opportunities and serving as a resource at any point along their path. Through those efforts, I am excited to report that we currently have 26 students in medical school, 10 in residency and 3 practicing physicians. There are 75 students currently in undergrad in pre-med/stem majors and others that went into (or plan to go into), equally important health careers as mid-level providers, nurses, physical therapists, and dentists.
As we move into Fall, we begin our annual membership campaign. Whether it is our pipeline programs, leadership opportunities, social events, reimbursement assistance, access to legal experts or local, state, and federal advocacy, we hope that you recognize the value of membership in SJMS/CMA. Please encourage your colleagues to join you in organized medicine.

I can’t believe I’m saying this……… but please Save the Date for the Holiday Party on Thursday, December 14.
Happy Fall,
Lisa Richmond



The Affordable Care Act (ACA) of 2010 brought about monumental changes in the way medicine is practiced in the United States of America. Whether you were a proponent for change or a booster for the status quo, we were all left somewhat disappointed. The area’s most concerning to physicians, who on a daily basis, attempt to deliver high-quality care to the patients of our communities, were left unaddressed despite trillions of tax dollars of “investment” in healthcare initiatives.
Unfortunately, the hopes of meaningful tort reform and insurance reform quickly dashed. So was the fate of the wonder and marvel of a new era with a connected Electronic Health Record (EHR) that could streamline the sharing of information and improve care for patients. The law was basically molded, shaped, and rubber stamped by the malpractice attorney lobby and the insurance companies among many special interests.
ABOUT THE AUTHOR
Cyrus Fram Buhari, DO is the current president of the San Joaquin Medical Society and practices at the San Joaquin Cardiology Medical Group
While remaining in favor of our current private and employer-based healthcare insurance system, I can recognize why there would be the lure of a single-payer system. What I continue to urge for is incremental improvements that will grant patients the best of both worlds. Perhaps incremental change to the system in 2010 would have been more advisable but politics knows little of prudence or foresight. Either way, here is where we are. I endured insufferable lectures from guest-speaker US Congressmen at society meetings. I sat quietly while physician attorneys gave sad presentations on the new way medicine would be practiced in the future. From the tantalizing talk of new payment models to the shame of the current cost of healthcare trajectory in the US, I sat there in fear of what was to come. Nowhere

in any of the tales we were told was there mention of the things I hold dear in my daily practice. Where was the talk of the doctor-patient relationship? Where was the talk of reducing burdens to healthcare delivery for independent physician practices? Where was the talk of prescription drug pricing reforms? The list goes on and on. Oh, what could have been… What a missed opportunity.
When this law first began implementation, it seemed as though you needed to hire 10 new employees just to be able to comply and not face stiff financial penalties. My suspicion is that whoever backed the law’s passage did not think far enough in advance to envision the chaos it would create. That is how legislation works. Just pass it and deal with the fallout through a multitude of amendments and regulatory changes. Like it or not that’s the way it’s done.
Okay… enough waxing poetic about what wasn’t done right. It’s time to get down to what we can do now.
physician staff (who are designated to deal with this daily). And please, do not make me bring up the “Bizarro World” conversations we have to endure during peer-to-peer phone calls where I have to hear how “new technologies” experimental despite being FDA and CMS approved for years.
We must as physicians inform our colleagues and our patients on all pending legislation that is aimed at improving healthcare and removing burdens to its delivery.
SB598 is a big step in the right direction. Your San Joaquin Medical Society board and staff, along with CMA have spearheaded efforts to educate legislators of the current state of affairs and the benefit of reform. We must as physicians inform our colleagues and our patients on all pending legislation that is aimed at improving healthcare and removing burdens to its delivery. I urge you to get out and support your society by encouraging our colleagues to join and get involved in SJMS.
I urge you to get out and support your society by encouraging our colleagues to join and get involved in SJMS.
SB598 is our new target for advocacy. This is the proposed legislation to reform the prior authorization process in California. As I have previously stated, prior authorization is a valuable tool to ensure that appropriate tests are performed for the appropriate patient. All physicians recognize this. Unfortunately, (and predictably) it has become a tool to deny access to care for patients. It is utilized by insurance providers as a cost-saving (and hence profit-generating) tool that ends up denying stateof-the-art diagnostics, procedures, and advanced pharmaceutical therapy for our patients. It has become a source of frustration for physicians and
Our SJMS and CMA are focused in the future on stopping cuts to physician reimbursement and trying to get the shortsightedness out of the legislative system at all levels of government. If we fail to stand up to these challenges, we risk succumbing to far worse. Already the ugly head of capitated insurance plans have reared their foul stench in our community after a peaceful hiatus.
The most effective weapon in the fight for delivering the highest quality care to the patients of our community is our support of the San Joaquin Medical Society and its efforts in fighting for us all.
Every patient is made for more. That’s why we bring together the latest breakthroughs and the most advanced experts in more than 40 medical specialties at over 20 convenient locations throughout San Joaquin and Sacramento counties. We offer more health, more wholeness and more hope to everyone we serve. For every age, every stage of life and every diagnosis, we’re neighbors providing compassionate support.
Adventist Health offers:

- Cardiology
- Gastroenterology
- Orthopedics
- Urology
- Occupational medicine
- Maternity
- Pediatrics
- Surgery
- Intensive care
- Emergency services
Learn more about our services at AdventistHealthLodiMemorial.org
- Oncology
- Neurology
- Bariatrics
- Home-health services
- Outpatient therapy services
- Advanced imaging services, featuring board-certified radiologists
- Coordinated care with primary-care physicians












LEADING VOICE IN HEALTH CARE: Through expert political and regulatory advocacy, CMA has positioned itself as one of the most influential stakeholders in the development and implementation of health policy. CMA also gives members direct access to our state’s and nation’s legislative leaders so they can shape the practice of medicine in California.
ADMINISTRATIVE BURDENS: CMA works hard to reduce administrative burdens in physician practices, so physicians can spend more time caring for patients. CMA is fighting to streamline prior authorization at both the state and federal level, prevent unfair payment practices, stop duplicative reporting requirements and more.

LEGAL EXPERTS: CMA’s Center for Legal Affairs provides members with information about laws and regulations that impact the practice of medicine. Our health law information specialists—with the help of CMA legal counsel—will help you find information on a multitude of health-law related issues.
PHYSICIAN WORKFORCE: CMA is committed to ensuring California is training enough physicians to meet current and future demand. Our CalMedForce GME grant program to date has allocated over $189 million to 143 GME programs across California to retain and expand residency programs in primary and emergency medicine.
REIMBURSEMENT ASSISTANCE: Members receive one-on-one assistance from CMA’s reimbursement experts, who have recouped $40 million from payors on behalf of CMA physicians since 2008.
LOAN FORGIVENESS: CMA’s CalHealthCares program provides loan repayment on educational debt for California physicians and dentists. Eligible physicians can receive up to $300,000 in exchange for a fiveyear service obligation. To date, 1,077 California providers have received a combined total of $256 million to pay down student debt.
TELEHEALTH: Through CMA’s advocacy, both public and private payors were pushed to expand their coverage of and reimbursement for services provided via telehealth. CMA in 2022 also successfully pushed to extend the COVID-19 telehealth waivers into 2023 and to permanently extend key Medi-Cal telehealth payment parity.
“Membership in CMA allows me to make a long-lasting difference in the lives of my patients and protect and enhance the practice of medicine in California.”
Bradford Anderson, M.D. Physical Medicine/Rehabilitation Member since 1991
TOBACCO TAX: CMA has fought tirelessly for decades to decrease the harmful impacts of tobacco, including passing the Prop. 56 tobacco tax in 2016. Prop. 56 provides $2.7 billion a year dedicated to increasing access to quality health care by improving Medi-Cal provider payments and addressing the critical physician workforce shortage. CMA also passed a 2021 bill to impose a 12.5% tax on e-cigarettes to reduce their use and generate revenue for important health care initiatives.
MICRA MODERNIZATION: Facing another statewide ballot proposition that would have effectively eliminated MICRA’s cap on non-economic damages, CMA seized an opportunity to end one of the longest running political battles in California. The legislative deal (AB 35), which modernizes MICRA while preserving its underlying principles, has ushered in a new and sustained era of stability around malpractice liability.
CMA provides many avenues to get involved with federal, state and local opportunities. Impact
Be a physician advocate and have a direct impact on the future of medicine in California. Connect

Connect, network and learn with physician colleagues from across the state.
REPRODUCTIVE RIGHTS: California has a long history of protecting and defending reproductive health care rights. CMA strongly believes that medical decisions—including those around abortion and contraception—should be made by patients in consultation with their health care providers.
COVID-19: CMA supported and informed physicians throughout the COVID-19 pandemic. Support included distributing more than $100 million worth of PPE across the state at no cost to physician practices to ensure they could serve California’s patients safely. CMA continues to advocate at the local, state and national levels to ensure that the interests of physicians and their patients are considered, as governments respond to the COVID-19 pandemic and other future public health threats.
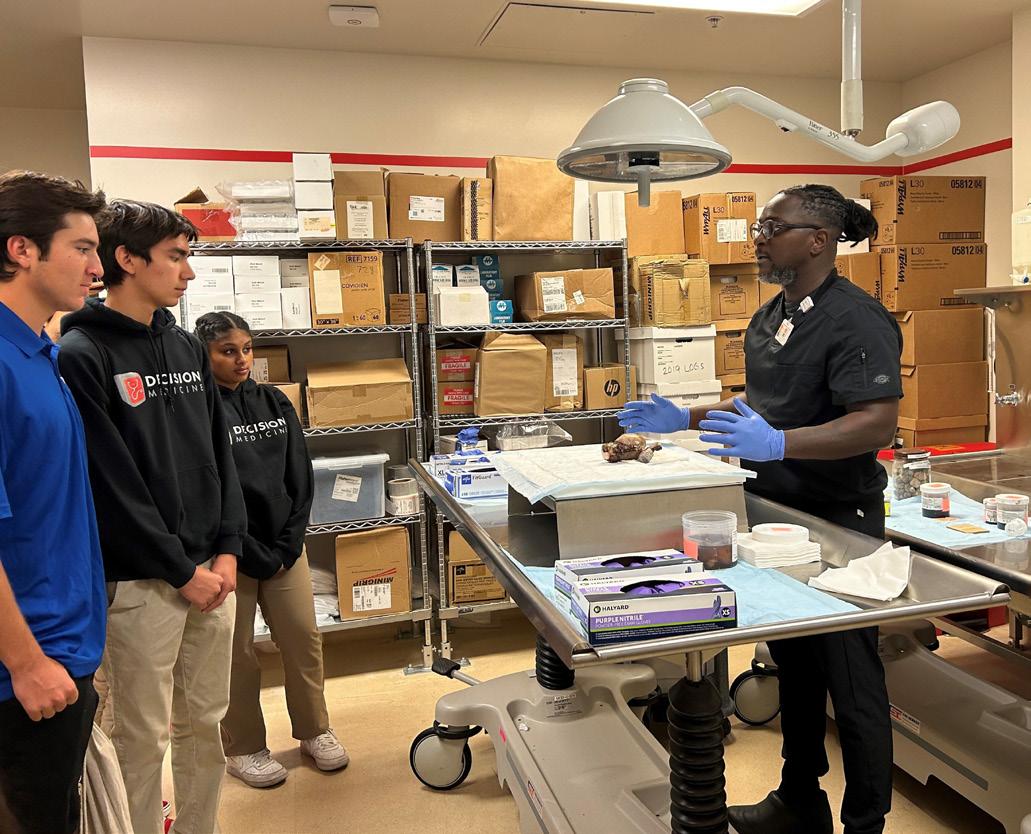
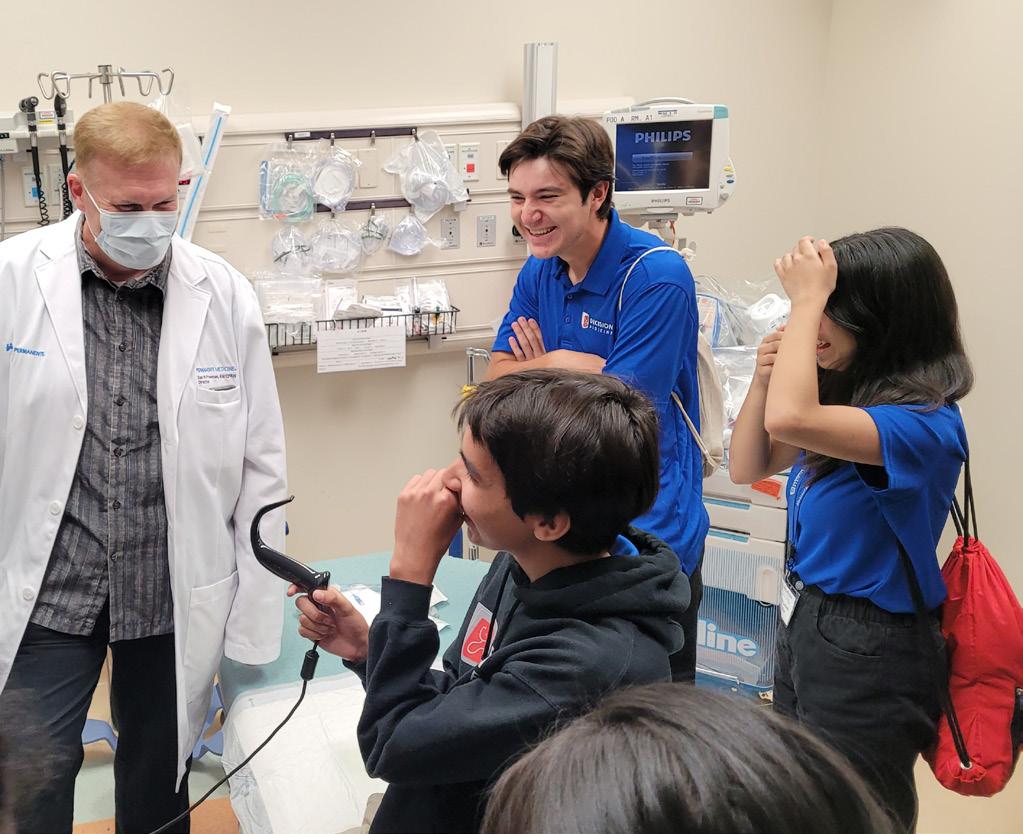
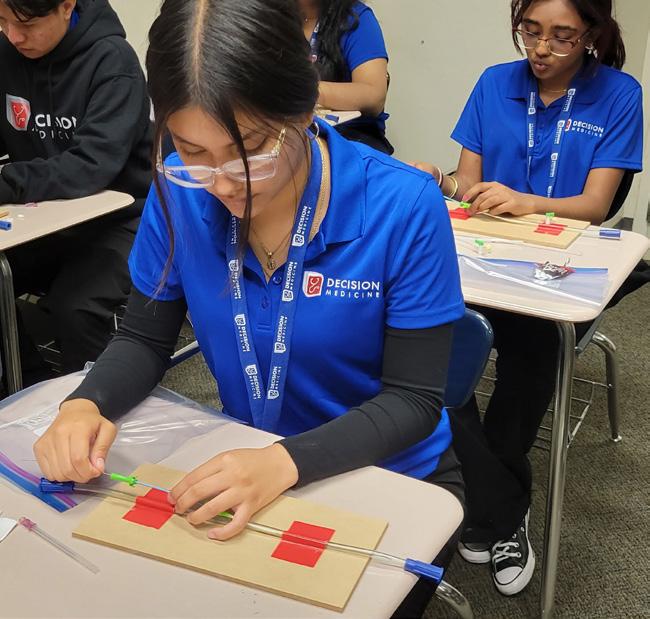
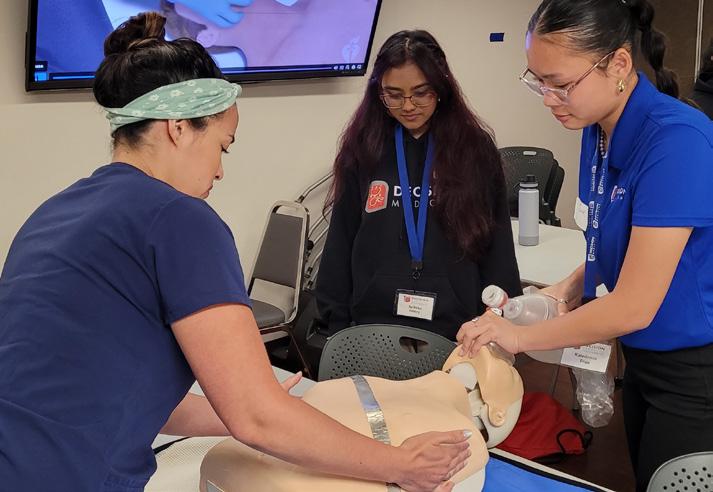
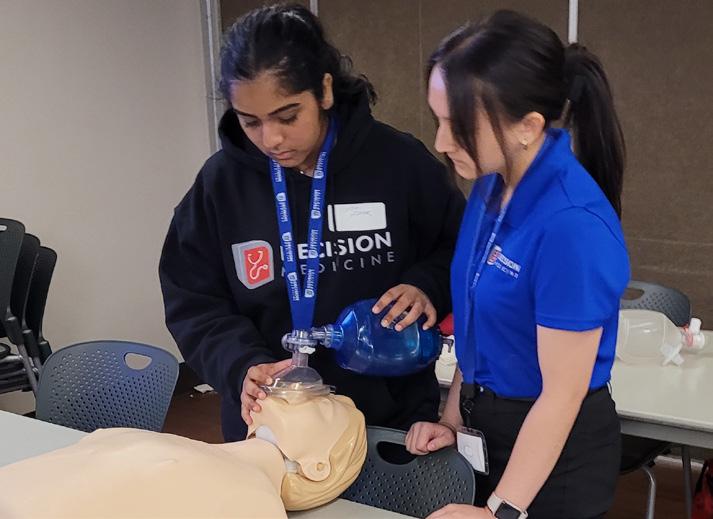
The 23 high school juniors and seniors chosen to participate in the San Joaquin Medical Society’s 2023 Decision Medicine program already have learned lifesaving skills that they will take with them into their communities. The students became certified in Basic Life Support at St. Joseph’s Medical Center in Stockton where instructors taught them to recognize several life-threatening emergencies, how to give highquality chest compressions and even how to deliver appropriate ventilations. Over the course of two weeks, they shadowed doctors, took part in team-building activities, learned about a myriad of health care professions, were educated in topics such as infectious disease, visited UC Davis Medical School as well as area hospitals, learned about what is being done to address the health of the county’s homeless population and more. >>
 BY JO ANN KIRBY
BY JO ANN KIRBY
TEENS LEARN WHAT IT TAKES TO SAVE LIVES

Nearly 100 students from 27 high schools applied to take part in the program, which is designed to expose high achieving students to careers in medicine and provide them support and mentorship in the hopes that they further their education and come back to San Joaquin County to serve as physicians or in other vital medical field careers, thus alleviating a dire shortage of health-care professionals in our area. From there, 48 were chosen to be interviewed and 24 were offered spots in the program. The opportunity is a big one for these students, many of whom come from families where their annual household income is below the poverty line.
“I’d always been interested in medicine, especially my biology classes. So, when I heard about this program from my sister who had participated in it, I applied,” said Alina Sanchez, as she and a classmate took a break from learning how to administer chest compressions. During the session, she asked questions of instructors to ensure she understood the assignments and listened attentively during a demonstration. She will be a senior at Cesar Chavez High School and shared that her sister was so inspired by Decision Medicine that she is studying public
health at University of California, Berkeley. Another student, Victor Carcamo of Franklin High School, said he found the visit to St. Joe’s very compelling. “I want to be a cardiac surgeon,” he said. “It feels good to be able to experience this especially since just 24 were chosen. It’s an honor.”
Dr. Marina Castillo, a pediatrician at Sutter Health and a mom, said she enjoys taking part in the program. She helped interview applicants and read their essays. “As a pediatrician, I’m committed to helping young people create a mindset that helps them realize their potential,” she said. “It’s a great group of students all around. They are all high achieving. They all want to give back to the community. Your goal with Decision Medicine is to provide these opportunities.” Dr. Castillo was paired up with a teen who shadowed her for a day. The teen sat in on patient visits and went out to lunch where they had a conversation about a career in pediatrics. “It was nice for her to see I have a life and a family,” she said.
The opportunity for these incredibly smart and talented students from underrepresented backgrounds to meet health professionals who look like them, witness medical

“ IT’S A GREAT GROUP OF STUDENTS ALL AROUND. THEY ARE ALL HIGH ACHIEVING. THEY ALL WANT TO GIVE BACK TO THE COMMUNITY. YOUR GOAL WITH DECISION MEDICINE IS TO PROVIDE THESE OPPORTUNITIES.”
- DR. CASTILLO
Decision Medicine (DM) was created by the San Joaquin Medical Society to inspire high achieving, under-represented students to consider a career in medicine and encourage them to return to the Central Valley to serve our diverse community.
Health Plan of San Joaquin (HPSJ), the county’s local Medi-Cal Managed Care Plan, and long-time supporter of the DM program, provides scholarships through their “Health Careers Scholarship Program” to local students who are committed to pursuing careers in healthcare. This year, HPSJ increased the number of Health Careers Scholarships, including nine Decision Medicine Students, an investment of $27,000 in young adults who have successfully completed the DM program.
For scholarship recipient, Stacy Hui Du, this program has helped in her long-term pursuit of going to medical school. Du states, “While this scholarship will be of great assistance in relieving my parents’ worries about the cost of attending college, it will also make my dream of becoming a physician and returning to serve my community much more attainable. As a daughter of refugees from Vietnam, education has always been emphasized in our home. While attending UC Berkeley, I hope to continue efforts to promote health equity among underserved and vulnerable populations.”
HPSJ attended the 2023 Decision Medicine (DM) Celebration Banquet to present Health Careers Scholarships to this year’s DM alumni. Pictured, from right to left, HPSJ Member Development Representative, Julia Valdez alongside DM graduates: Anthony Luna who will attend California State University Monterey Bay (CSUMB) to major in biology, plans to earn BS and MS degrees before attending medical school. Anthony hopes to return

to the area to work for Community Medical Centers (CMC); Ashley Peterson will be a neuroscience major at UCLA and aspires to serve in San Joaquin County as a pediatric neurologist. Dayanara Flores plans to major in Public Health and minor in Chicano/Chicana studies and become a pediatrician; Gurleen Sharma wants to become a Licensed Vocational Nurse (LVN) and work towards a Bachelor’s in nursing (BSN) to become a Nurse Practitioner; Harmandeep Singh Batth will attend UCLA to earn an undergraduate degree in Biological Sciences, then a degree in medicine to become a doctor that can help underserved communities; Jessica Ximena Alcala has committed to UC Irvine to study public health and desires a career as a cardiothoracic surgeon; Prabhnoor Dhillon plans to attend UCLA and make an impactful change as a practicing vascular surgeon in her community; Shelby Miller will attend UC Irvine with a double-major in biological sciences and psychology, and plans to return to San Joaquin County to practice internal medicine; Stacy Hui Du plans to attend UC Berkeley and become a physician who can create local health clinics which uninsured individuals and families can receive affordable medical care; HPSJ’s Chief Medical Officer, Dr. Lakshmi Dhanvanthari pictured far right, presented each scholarship awardee with a certificate.
Dr. Dhanvanthari said, “We believe in the importance of fostering relationships that will improve health equity and access to quality healthcare in our community. Investing in students who have a connection to this area and can relate to the people they will eventually care for is a motivator and we couldn’t be prouder to support them on this journey.”

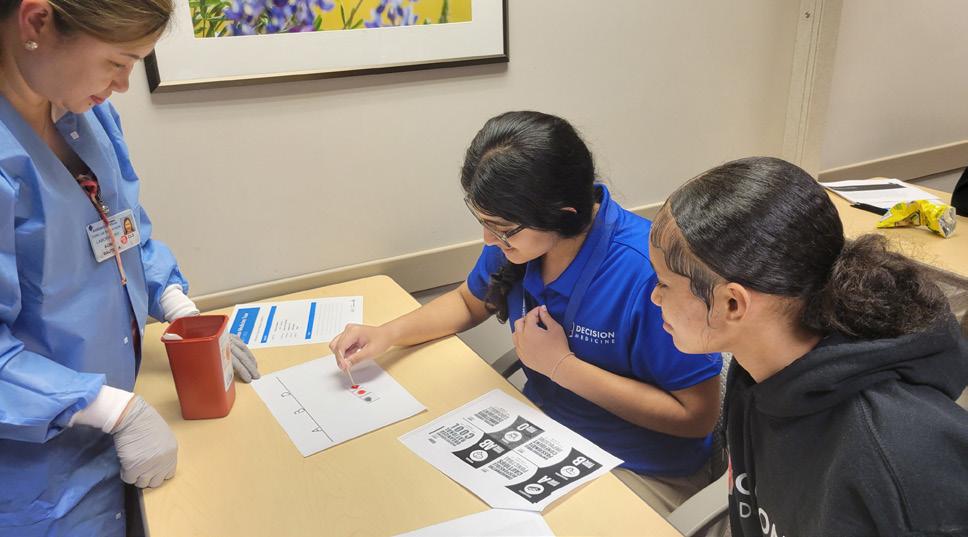
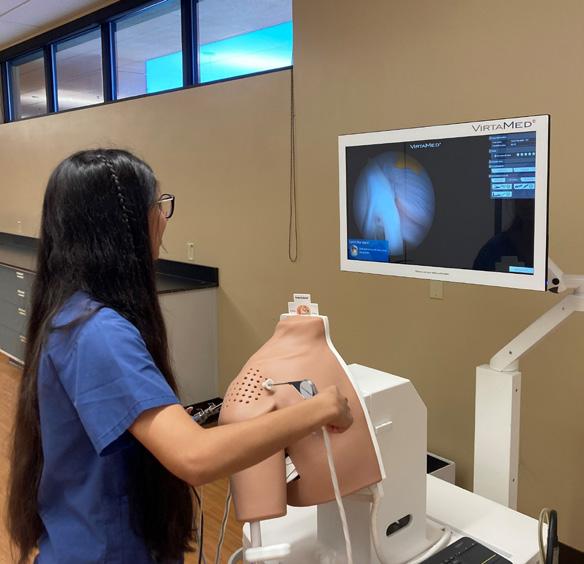

procedures, learn more about what it takes to get into medical school, and to make connections with potential mentors is invaluable for students whose parents may not have graduated college or worked in medicine. At a banquet to celebrate the completion of the program, students arrived with family members and were treated to a dinner at the Stockton Golf & Country Club. The evening included a highlight video of their experiences, a speech by a former Decision Medicine student who is now starting her career as a physician in Stockton, and a ceremony where they donned white coats and received a certificate.
The co-founder of Decision Medicine, Dr. Kwabena Adubofour, exhorted the students to stay focused and appreciate the love and support of family. He was most adamant that they come back and serve as medical professionals in their hometown, stressing the need for primary care physicians is great. Dr. Vanessa Armendariz, who has returned to Stockton to start a career in family medicine with California Community Centers’ new adolescent clinic, encouraged the teenagers. “I know how jam-packed these two weeks have been,” she said. “Eighteen years ago, I was sitting where you were sitting. During the program, I was introduced to physicians who looked like me.” She explained that in college, studying at John Hopkins University, which is known for its rigor and excellence, she struggled academically for the first time in her life. She reached out to Dr. Adubofour, who she met when she took part in Decision Medicine, and he jokingly threatened bodily harm if she didn’t persevere. When those moments occur, she told her audience “reach out to your family and mentors, to your village.” They will keep you motivated and supported, she said.
Decision Medicine and its many partner institutions also benefit from the hard-working physicians and health professionals who volunteer with Decision Medicine to light a flame in the next generation of potential healers. “I try to participate as much as I can.
I appreciate being included in this,” Dr. Castillo said. “I think it’s important to be a familiar face and have someone who they can bounce ideas off of. This is a field where it definitely is delayed gratification. It takes a long journey to get there. If I can be an inspiration, that would mean the world to me.”


SUNBAL DILSHAD Noorda College of Osteopathic Medicine

Scholarship Loan Fund
BRIDGE TO MEDICINE
Mentor: Kelly Savage, DO

AMIT GREWAL, DO University of ChicagoNorthshore Internal Medicine

DECISION MEDICINE 2013
HYOSUNG “DAVID” HAN Michigan State University College of Medicine
BRIDGE TO MEDICINE
Mentor: Howard Young, MD

JAZZMIN WILLIAMS, MD UCSF Dermatology Program
DECISION MEDICINE 2012

ALEYAH BLAKE
Stockton Collegiate International Schools
VICTOR CARCAMO
Franklin High School
MAGGIE CHEUNG
Stockton Collegiate International School
GIANNAH CORTEZ
Benjamin Holt College Prep Academy
RAFAEL CUEVAS
Lincoln High School
ALESSANDRA DE LA O
Stockton Early College Academy
KATHLEEN EMPERADOR
Health Careers Academy
GURNEET KAUR
Tokay High School
SAMIHAH KHAN
Weston Ranch High School
APIKSHA MISTRY
Stockton Early College Academy
ABIGAIL MUNOZ
Stockton Collegiate International School
SANYA NATH
John C. Kimball High School
DIEGO PALACIOS
Langston Hughes academy
NICOLE PETERSON Health Careers Academy

MELODIT PIEDRA Health Careers Academy
PRIYANKA PRABHAKAR
Saint Mary's High School
ALINA SANCHEZ
Cesar Chavez High School
HARMONY SANDHU
Tokay High School
SANTHOSH SENTHIL
Mountain House High School
KATEDENCE TRAN
Bear Creek High School
JC VERA Health Careers Academy
THRISHIKA VUPPALANCHI
Mountain House High School
MARISOL ZARAGOZA
Edison High School






Premier Financial Sponsor
• Health Plan of San Joaquin
Community Partners
• Adventist Health Dameron Hospital

• Community Medical Centers
• Kaiser Permanente
• San Joaquin General Hospital
• San Joaquin Public Health Services
• Shriners Children’s
• St. Joseph’s Medical Center
• St. Mary’s Dining Room
• UC Davis School of Medicine
• UCSF School of Medicine
DM Committee & Shadow Day Mentors
• AJ Putillath, MD
• Alain Flores, MD
• Bhagya Nakka, MD
• Cyrus Buhari, DO
• Dheeraj Nandanoor, MD
• Gentry Vu, MD
• George Khoury, MD
• Hyma Jasti, MD
• Jaicharan Iyengar, MD
• John Canzano, MD
• Kinnari Parikh, MD
• Kwabena Adubofour, MD
• Kyle Natsuhara, MD
• Linda Sakimura, MD
• Marina Castillo, MD
• Mohammad Pathan, MD
• Nathan Kludt, MD
• Raissa Hill, DO
• Randeep Bajwa, MD
• Richard Waters, MD
• Richelle Marasigan, DO
• Roland Winter, MD
• San Tso, DO
• Sanjeev Goswami, MD
• Sunny Philip, MD
And so many more who contributed their time and expertise!
Originally published in the San Francisco Chronicle and SFChronicle.com
Dear Patient:
I know now what I didn’t know then. My 16-month-old son died unexpectedly last summer, and I experienced life on the other side of the exam table, in horrid slowmotion technicolor. I sat on the other end of a 911 call. I rode in the ambulance as a caregiver, not a first responder. I waited outside the emergency room as I heard the doctor call out for vital signs and medications, and most tellingly to my ears, a social worker. I experienced the silence after the gloves came off and the team walked wearily out of the room. This time, I was the one to wail.
The truth is, Patient, I am not unfamiliar with death. I am a palliative care physician, a branch of medicine focused on quality of life for those living with serious illness. I came to this specialty because it helped me preserve the heart of why I went to medical school in the first place and touched on a tender part of my soul that was already marked by loss, having seen my mom live with and then die of cancer when I was a teenager. As a doctor, I lived on the margins of grief daily, handling it with as much care as I could while still tucking it neatly away when I walked out of the office each day.
But in this moment, living daily with grief and pain and longing, feeling rage and fear and dread seemingly in the same instant, I find my mind wandering to you, dear

Patient, and seeing you in a whole new light.
I am so sorry that I didn’t know. I sat across the room from you, and you did such a good job of hiding your suffering with silence or anxiety or anger, that I didn’t see your broken, beautiful core there. I offered words that I thought were empathy like, “This must be so hard,” or “I can’t imagine what it is you’re going through,” and I went home and patted myself on the back for being there for you, for being a beacon in a medical system that attempts to automate and quantify the most precious parts of the life experience. In reality, you left our visit feeling more alone. For that, I am so sorry.
I didn’t see how your description of abdominal pain held multitudes. Yes, there is a tumor in your liver and, yes, it may be helped by pills or heat or any number of handy solutions that I used to reach for with earnest self-satisfaction. What I did not acknowledge was that in your breathless descriptions, begging to be heard because I might cut you off at any moment, there was also a plea to be seen. That is the thing about grief that I know now — it is so lonely. The cut is so thoroughly deep that you cannot believe the world doesn’t see the pulsating flood pouring out of you — and yet you walk among people who seem fully oblivious. It is as if I am saying silently all of the time, “Don’t you know? How can you not know?” all the while smiling cheerfully and speaking of the mundane. I see now, Patient, that you were saying that, too, underneath it all, asking me to see.
Here’s what I’d say to you today instead: I don’t know if I can fix your abdominal pain, but I will try. I will look for answers and seek out solutions and no matter the outcome, I will be there. I will walk with you all the way. I promise to be one of the few who will walk with you all the way.

I see you, beautiful, grieving Patient. I honor the fact that in the face of the insurmountable task of making it to the next day, of getting out of bed, of living this unbidden life, you chose to come to my office
and explain what you are going through and ask for help. I am so sorry for all of the times that I failed to honor your request, where I shoved your deep questions under the rug because the 20-minute visit was over, or where I relegated your suffering to the realm of someone else’s job. I am so sorry that you stepped into the vulnerable place of being a patient who seeks counsel from an expert, and in return, I did not honor that sacred marvel of a moment, that gift of authenticity that you extended to me. I can see clearly now.
I do not have all the answers, even for myself — perhaps most of all for myself. I do not have pat advice for how to move through grief and sorrow, Patient. It is so fresh, so jagged, so consuming. (Maybe you have advice for me? I am all ears.) I only know that my weeping heart reaches into the past to those days when I sat with you and out into the future to when I hope to sit with you again, and this time I name myself as your companion. I grieve with you. I am with you. May we all feel less alone, even as we bleed.
Love, Your Doctor
Bonnie Chen is a palliative care physician in Oakland.
 BY JO ANN KIRBY
BY JO ANN KIRBY
Fulfilling a promise she made as a high school student in San Joaquin Medical Society’s Decision Medicine program, Dr. Vanessa Armendariz is back home and ready to serve her community as a family physician who will be part of a team developing programming and services for the new Adolescent Health Center that Community Medical Centers is launching in downtown Stockton. Her story is one of resilience, compassion and determination, the plot of which features an important supporting cast of family, friends and mentors who cheered her on when she felt the odds seemed insurmountable. >>



“When I did Decision Medicine, I made a commitment to come back to our community because there is this huge shortage of medical providers,” Dr. Armendariz said. “I’ve always had that yearning to come back to the community who raised me and supported me and now I’m making that promise come true.”
It was a promise she made as a young Franklin High School student when she was chosen to be part of Decision Medicine, a two-week program for high achieving high school juniors and seniors from underrepresented backgrounds who are chosen for a hands-on introduction to the field of medicine with the goal of inspiring them and assisting them on their path to medical school. The hope is that they will come back to San Joaquin County to launch their career. Growing up, it wasn’t until she participated in Decision Medicine that she saw medical providers who looked like her. “Decision Medicine really helped me see that I could do this,” she
“ When I did Decision Medicine, I made a commitment to come back to our community because there is this huge shortage of medical providers. I’ve always had that yearning to come back to the community who raised me and supported me and now I’m making that promise come true.”
- Dr. Vanessa Armendariz
said. “Our community is very much a melting pot, and we have such diverse patients. I feel like a lot of patients will connect more to medical professionals who understand their culture.”
Through Decision Medicine she met with mentors who would offer her support when she needed it most. Dr. Kwabena Adubofour was one such guide. As an undergrad student on a full ride to John Hopkins University in Baltimore, she might as well have been in an entirely different universe. The unfamiliar setting featured classmates who were from a far different background. “Not even just race-wise, but financially and educationally, it was all a huge difference,” said Dr. Armendariz, a firstgeneration college student. “I just wanted to quit. I felt like I couldn’t do it anymore.” At the end of her sophomore year, she reached out to Dr. Adubofour, who cajoled, threatened, challenged, and even demanded that she stick it out. “Look around the lecture hall and name one

student who is more resilient than you,” he told her when she thought an organic chemistry class was getting the best of her. “I get teary-eyed when I think about her. The resilience, persistence, the grace with which she carries herself, the brilliant person she is to have a full ride to John Hopkins, the ability to carry through with her dreams — I think she has taught me more than I’ve taught her,” Dr. Adubofour said.
After successfully graduating from the university with a degree in public health, she took a break from her studies but gained valuable work experience as a community relations manager for the San Joaquin Medical Society. Fittingly, one of her duties included facilitating the Decision Medicine program that had inspired her as a teen. A few years later, when she felt it was time to apply for medical school, another SJMS physician gifted her a book titled “The Medical School Interview: Winning Strategies from Admissions Faculty.” She landed at the University



of Kansas School of Medicine, far from home again. Along her journey, she made a point to volunteer in organizations that provided her with the chance to be a mentor. Through groups such as the Latino Medical Student Association, the Student National Medical Association, the Family Medical Interest Group, and other councils, she was able to provide the support her connections at Decision Medicine gave her. This past June, she was closer to home when she wrapped up a stint as a resident physician with Sutter Santa Rosa Family Medicine Residency.
Today, she and her supportive husband Joseph, along with their ginger cat Ed Sheeran, are back in Stockton where they are making a home

and planning for the future. The cat, like the popular singer it is named after, has its own Instagram account where it can be seen dressed up like a physician in one fun post. Dr. Vanessa, as she invites patients to call her, has come full circle. Even her new job came at the suggestion of her longtime mentor, Dr. Adubofour. At Community Medical Centers, Chief Medical Officer Dr. Benjamin Morrison said the anticipation is that she will be a valuable member of the adolescent health team in its mission to improve health and well-being in the communities CMC serves. “She will help improve access and increase medical education and preventative medicine availability for our adolescent population,” he said of her new position at the Adolescent Health Center, slated to open in 2025. “As she settles in, she will also take on a teaching role to help share her knowledge with family medicine residents who are still in training,” he said. The new center’s objective is to provide a location and a health home to better meet the unique needs of our adolescents in the community. It will focus on primary and preventative care while offering outpatient behavioral health and substance use disorder

“As she settles in, she will also take on a teaching role to help share her knowledge with family medicine residents who are still in training,” - Dr. Ben Morrison
treatment as well as other services. As a physician, she said she hopes to speak to her patients on a level they understand and to make sure they have a clear knowledge of the medical plan for their care.

Coming back home isn’t the end of her story. According to her biggest champion, her mother, it’s just the beginning. “I am so grateful to Dr. Adubofour for inspiring her and taking her under his wing and bringing her back home,” Gerri Armendariz said of her youngest child and only daughter. “I knew when she was born that she was going to do great things. She’s going to be an excellent doctor. She is so caring, and she has the biggest heart. Stockton is going to be happy to have her home.”
Recently the new physician spoke to the newest cohort of Decision Medicine students. As the keynote speaker at a banquet celebrating the students for successfully completing the program, she encouraged them to believe in themselves. “I want you to be aware of a syndrome called imposter syndrome,” she said, referring to a psychological occurrence in which people may doubt their skills or accomplishments and fear being exposed as frauds. “We have to remind ourselves that we do belong, and you do deserve to be here. This is your life. This is your story. The changes we all want to see in medicine starts with us.”

“ We have to remind ourselves that we do belong, and you do deserve to be here. This is your life. This is your story. The changes we all want to see in medicine starts with us.”
- Dr. Vanessa Armendariz

U.S. News & World Report Names St. Joseph’s Medical Center Among Nation’s Best Hospitals for 2023-2024
Dignity Health St. Joseph’s Medical Center has been named by U.S. News & World Report as its 2023-2024 Best Hospitals, in addition to being recognized as High Performing in nine common procedures and conditions.
St. Joseph’s Medical Center was ranked Best Regional Hospital in the Stockton Metro Area and is tied for 43rd in the state of California in the 2023-2024 Best Hospitals rankings. High Performing areas include Congestive Heart Failure, Colon Cancer Surgery, Diabetes, Heart Attack, Hip Fracture, Kidney Failure, Leukemia, Lymphoma and Myeloma, Pneumonia, and Stroke.
U.S. News evaluated more than 4,500 hospitals across 15 specialties and 21 procedures and conditions; only 12% of evaluated hospitals earned a Best Hospitals ranking. Hospitals awarded a “Best” designation excelled at factors such as clinical outcomes, level of nursing care and patient experience.

On July 24th, an unprecedented partnership to address the homeless crisis in Stockton was announced at a press conference with St. Mary’s Dining Room, City of Stockton, San Joaquin County, Health Plan of San Joaquin, and Dignity Health St. Joseph’s Medical Center. Through a collaborative effort that resulted in more than $16 million in funding, St. Mary’s Dining Room will soon have low-barrier space for hundreds of individuals in Stockton who are unsheltered, including women, seniors, and individuals with disabilities.
St. Mary’s Dining Room – one of the largest homeless service agencies in San Joaquin County – received $6.5 million from the Board of Supervisors through the City of Stockton that propelled its unique homeless shelter project forward, an additional $3.6 million from the City of Stockton, $5.4 million from the Health Plan of San Joaquin, and $2 million from Dignity Health.
Providing staff, physicians, and patients with relevant & up to date information
St. Joseph’s Medical Center launched its inaugural Orthopaedic Residency Program, the newest addition to their growing Graduate Medical Education (GME). In preparation of the new cohort of residents, an Arthroscopy Simulator was added to the lineup in the Surgical Simulation Laboratory.

Program Director, Dr. Jaicharan Iyengar said, “Our arthroscopy simulator…is an incredible tool to allow our residents to practice minimally invasive joint surgery and train at the highest level with current techniques, which I think will translate to producing skilled surgeons for our community in the longterm”.
The arthroscopy simulator was funded by St. Joseph's Foundation of San Joaquin. The Foundation was and continues to be instrumental in the growth of St. Joseph's GME program
Unifying under one brand promotes the continuity of care provided for patients across the three hospitals and their affiliated entities.
The three hospitals have worked as a network for decades and continue to do so under this new brand. The network offers advanced, quality care – from preventative and routine healthcare to highly specialized services – to everyone. The facilities serve many diverse communities throughout the Central Valley, enabling patients to access a wide range of services at convenient locations close to home.
Tenet Healthcare announced the launch of Central Valley Doctors Health System, a single, identifiable name and brand that reflects the integration of its healthcare system across the Central Valley, including its three acute care hospitals: Doctors Medical Center in Modesto, Emanuel Medical Center in Turlock and Doctors Hospital of Manteca.
Continuing to work together as Central Valley Doctors Health System gives the facilities the opportunity to enhance care coordination and access to the specialized services they bring to the region, benefiting patients in all aspects of healthcare.
Learn more about the Central Valley Doctors Health System at cvdoctorshealthsystem.com.
Doctors Hospital of Manteca and Emanuel Medical Center appointed Rob Giorgiani, MBA, MEng, CPA, as the new Chief Financial Officer (CFO) over both facilities.
Giorgiani comes to the Central Valley from Richmond, Virginia, where he served as CFO of St. Mary’s Hospital and Richmond Community Hospital. Prior to his role as CFO, he served as Assistant CFO over seven acute care facilities in the greater Richmond area.
St. Joseph’s Medical Center offers comprehensive interventional radiology (IR) services to treat many conditions that once required surgery. By utilizing minimally invasive techniques, IR procedures generally result in decreased risks, less pain, and shorter recovery times for patients when compared to traditional surgery. Whether your patients are experiencing back pain, chronic kidney disease, heart and vascular conditions, cancer, or men’s or women’s health issues, IR treatments are available to address many health concerns.
St. Joseph’s interventional radiologists have a wealth of experience and expertise in leading-edge, minimally invasive procedures. Featured services and treatments include:

• Angiography for vascular malformation
• Balloon kypohoplasty for vertebral compression fractures
• Cryoablation for kidney cancer
• Pain management to treat nerve pain (pain blocks)
• Percutaneous transhepatic biliary drainage (PTBD)
• Peripheral arterial and venous disease
• Prostate artery embolization (PAE)
• Radioembolization for liver cancer (Y90)
• Uterine artery / uterine fibroid embolization (UAE / UFE)
For more information, visit dignityhealth.org/stockton/IR or call IR scheduling at (209) 467-6323.
Giorgiani earned his Bachelor of Science degree in Chemical Engineering from Virginia Tech, Master of Systems Engineering degree from the University of Virginia and Master of Business Administration degree in Management and Finance Specialty from Indiana University.

Doctors Hospital of Manteca and Emanuel Medical Center, sister facilities in Manteca and Turlock, are both part of the Central Valley Doctors Health System.
“This initiative goes hand-in-hand with our mission of providing quality, compassionate care in the communities we serve, and we are proud to help provide healthy meals for those in need in our community.”
Doctors Hospital of Manteca donated 3,530 servings of cereal and $160 to Second Harvest of the Greater Valley, during its annual Healthy Over Hungry Cereal Drive in June.

The donations collected will help provide local children and adults struggling with hunger with a healthy breakfast. Good nutrition is essential to good health, and summer is a particularly tough time for many food-insecure families because children can no longer rely on schools for nutritious meals, putting an added burden on families. Whole-grain cereal, when part of a healthy, balanced breakfast, is a popular food item that experts say can help address the hunger gap during the summer months when children are not in school.
“The Cereal Drive has been a longstanding tradition at our hospital and we are so appreciative for the support we receive,” said Eleze Armstrong, CEO of Doctors Hospital of Manteca.
Doctors Hospital of Manteca is proud to announce that Amy Mou, day shift charge nurse, has been honored by Tenet Healthcare as part of its annual recognition program. Amy has been named a Tenet Hero for her outstanding contributions in 2022.

“Amy is a true inspiration who continues to make a positive and meaningful impact in our community each day,” said Eleze Armstrong, CEO of Doctors Hospital of Manteca. “We are deeply grateful to Amy for her dedication, selfless efforts, and commitment to our mission of making sure we provide quality, compassionate care in the communities we serve, which Amy fully embodies.”
The Tenet Heroes program celebrates those who make a meaningful impact within their communities and go above and beyond their daily responsibilities. Nominated by leadership and/or fellow colleagues, Tenet Heroes exemplify the company’s core values and commitment to its mission.
life specialists and dieticians, Shriners Children’s can handle the most medically complex patients.
The rapid adoption of high-resolution manometry reflects how useful it is proving to be, Dr. Hassan says.
Adventist Health Lodi Memorial Welcomes
Dr. Sartaj Sandhu, Internal Medicine
Dr. Sartaj Sandhu is an accomplished, board-certified physician specializing in Internal Medicine, with a particular focus on general outpatient and geriatric care. With over a decade of experience and fluency in English, Punjabi, Hindi, and Urdu, he is well equipped to treat common conditions within our diverse
The number of pediatric motility centers – where children can be tested and treated for achalasia, gastroparesis, chronic intestinal pseudo-obstruction, and the like – has been growing statewide and nationally.
A new study in the Journal of Pediatric Gastroenterology and Nutrition says that, where there were only 31 such centers nationally in 2015, there are 54 today.
Shriners Children’s Northern California has had motility specialist, Maheen Hassan, M.D., since 2020, when she was amongst the first of these pediatric specialists in Northern California.
In fact, the hospital has an entire functional GI and bowel management program, which Dr. Hassan says is key to the care the hospital can provide.
With a team that includes colorectal surgeons as well as child
Providing staff, physicians, and patients with relevant & up to date information
Sartaj Sandhu, MD
















community. Dr. Sandhu’s expertise extends to the treatment of various common conditions such as diabetes, hypertension, obesity, osteoporosis and dementia, among others. His passion for medicine is driven by a profound love for health, well-being, and the human body. He states, “I want to give patients the tools and education to create healthy changes in their own bodies and allow them to live more full and prosperous lives.”
Originally from Canada, Dr. Sandhu has recently married and chosen Lodi as the home for his family. He looks forward to becoming an integral part of the community in which he serves. When he is not practicing medicine, you can find him in the gym, playing soccer, drawing, reading, traveling and meeting new people.
Dr. Rabeep Grewal, Rehabilitation Medicine
Rabeep Grewal, MD, is a highly experienced physician certified by the American Board of Physical Medicine and Rehabilitation. With fluency in English, Punjabi and Hindi, she provides exceptional care to our diverse range of patients in the Acute Physical Rehabilitation department. Dr. Grewal’s expertise greatly enhances the county’s longest running APR department, which has served the Lodi community for over 30 years.
Dr. Grewal’s focus lies in restoring health and function to our inpatient rehabilitation patients who have experienced strokes, multiple traumas, fractures, debility, brain injuries or other life-changing events. She embarked on a career in medicine to fulfill a genuine desire to see others regain independence after suffering a major health event. When she is not caring for the community, Dr. Grewal enjoys traveling, reading and cooking.

The Adventist Health Lodi Memorial sleep laboratory offers diagnostic testing that includes diagnostic polysomnography, titration polysomnography and home overnight oximetry monitoring. They can safely diagnose conditions that include snoring, sleep apnea, hypersomnia, and parasomnia.
Their sleep laboratory team has extensive training and experience to help people with sleep disorders improve their quality of life through better sleep and rest. The staff works closely with primary care providers to provide timely, accurate test results for their patients that enable them to develop an effective treatment plan.
Conditions currently treated:
• Insomnia
• Narcolepsy
• Nocturnal panic attacks
• Other disruptive sleep disorders
• Periodic limb movement
• Sleep apnea
• Sleep terrors
• Sleep walking
• Types of seizures and epilepsy
Procedural/Interventions
• Diagnostic polysomnography –in sleep lab
• Diagnostics polysomnography – in home
• Titration polysomnography
• Home overnight oximetry monitoring
Patient Referrals
Fax: 209-333-5138
Phone: 209-333-5167

In response to advocacy by the California Medical Association (CMA), the U.S. Department of Education (DOE) now allows eligible California physicians to participate in the Public Loan Service Forgiveness (PSLF) program, despite state prohibitions on physician employment by private non-profit hospitals, clinics, foundations, and other health care entities.
To assist physicians in applying for the PSLF program, CMA developed a guide, “Public Service Loan Forgiveness: What California Physicians Need to Know.” CMA has made important updates to the guide. There is a new FAQ regarding qualifying employers (pg. 3-4) and a significantly updated section related to loan eligibility and qualifying loans (pg. 12-13). As previously reported, not all direct loans must be consolidated.
Under the new rules, which launched on July 1, 2023, California physicians who have qualifying loans, make 120 qualifying payments, and provide services 30 hours/week in a non-profit health care facility (hospital, foundation, clinic, or other organization) may qualify for the new federal PSLF program. Physicians who are in for-profit sole proprietorships or partnerships or are employed by for-profit medical groups or other professional corporations still qualify under the new rules as long as 30 hours of services per week are provided in a non-profit facility through a written agreement with the facility or health care entity, which can include a letter granting medical staff privileges.
Some loan payments made as early as 2008 may qualify under the new rules. To be eligible for the PSLF program and to have past loan payments count toward the program requirements, physicians must have Direct Loan Program loans that are not in default. If you already have a qualifying loan, you do not need to consolidate your loans. If you do not have a qualifying loan, you have until December 31, 2023, to consolidate your loans to be eligible for PSLF.
It is imperative that physicians review page 6 of the application form for more information about loan eligibility. Physicians are also encouraged to contact their loan servicers for advice about their personal loan eligibility. A new section of the CMA guide, “Qualifying Loans and Loan Consolidation” (pg. 12-13), provides additional details about loan eligibility and qualifying repayment plans for PSLF. If you are unsure whether you have Direct Loans, you can verify by logging into your account on https://studentaid.gov/.
CMA urges interested physicians to check our PSLF guide for periodic updates. CMA will be updating the guide regularly to clarify issues as we get more information from the DOE and to answer questions that we receive from physicians, foundations, clinics, and hospitals. The most up-to-date version of this guide will always be posted at cmadocs.org/pslf.
From delicate robotic and catheter procedures to precision therapeutics, we’re proud to offer diagnostic and treatment options for adult and pediatric referring providers across Northern California and the Central Valley.
Your referred patients benefit from shorter drives, less traffic, affordable lodging, and more. We also offer robust telehealth and telemedicine options, for both initial consultations and follow up care.
Maxwell A. Fung, M.D. Director, UC Davis Dermatopathology Service Professor of Clinical Dermatology and Pathology Specialty: Dermatology, Dermatopathology
at Shriners Children’s Northern California


Shriners Children's Northern California is the only children's hospital to be designated as a Special Care Center for colorectal and urology care by California Children's Services. Our Pediatric Colorectal Center brings together a multidisciplinary team of specialists to evaluate, diagnose and solve colorectal health issues, including:
Anorectal malformations
Bladder extrophy
Caudal regression syndrome/ sacral agenesis
Chronic constipation
Cloaca/cloacal anomaly
Cloacal extrophy
Encopresis
Fecal incontinence
Hirschsprung disease
Idiopathic constipation
Megacolon
Neurogenic bladder
We offer advanced diagnostics, including:
Neurogenic bowel
Pseudo-obstruction
Rectal prolapse
Rectal trauma
Spina bifida
VATER/VACTERL association
Now at St. Joseph’s Cancer Institute, the TrueBeam Linear Accelerator combines imaging, radiation beam delivery and sophisticated motion management to accurately and precisely target tumors with speed.
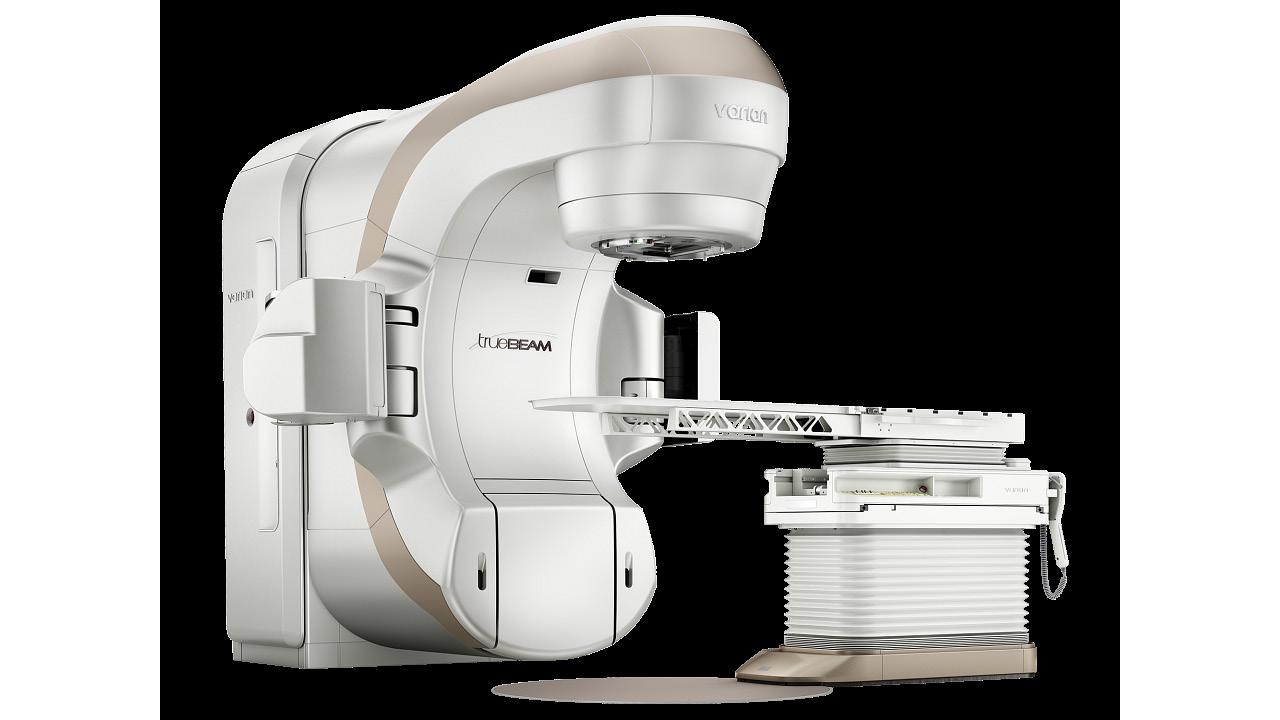
The TrueBeam provides breakthrough technologies that allow our experts to treat more challenging cancers with precisely targeted, highly concentrated doses of radiation, given in less time, and with less impact on healthy tissue.

Learn more at dignityhealth.org/stockton/cancercare

The Office Managers Forum empowers physicians and their practice manager staff with valuable tools via expert led educations sessions from industry professionals who are committed to delivering quality healthcare. This quarterly forum is normally held on the second Wednesday of March, June, September and December at Papapavlo's.
Registration is required!
If you don’t receive an invitation via E-Mail, please email Jessica@sjcms.org
September 13th, 2023: 11:00AM to 1:00PM
This workshop provides up-to-date changes and practice requirements to meet the Annual OSHA mandates. Topics included: Bloodborne Pathogens, Aerosol Transmissible Disease Guidelines, Violence in the Workplace, as well as several other OSHA related topics.
Carrie Champness, RN, BSN Safety Compliance Specialist- Carrie has been an OSHA compliance specialist for over 35 years and provides up-to-date information about changes and practice requirements to meet all OSHA mandates.

December 13th, 2023: 11:00AM to 1:00PM
Join us for our annual Medicare Update workshop for physicians and office staff. This 2 hour seminar will cover relevant information about current, future and proposed changes for the coming year!
Cheryl Bradley- Associate Director of CMA’s Center for Economic Services
UHC delays Designated Diagnostic Provider program in CA until Jan. 1, 2022
At the end of 2022, the California Department of Health Care Services (DHCS) reached an agreement with five commercial managed care plans (MCP) to deliver Medi-Cal services in 21 counties across the state starting in January 2024. As a result, approximately 1.2 million Medi-Cal patients will be required to transition to a new a new health plan, and in some counties Medi-Cal patients will have the ability to select from more than one plan.
DHCS recently updated its 2024 MCP Transition Policy Guide to include a table that lists Medi-Cal managed care plan changes slated to take effect January 1, 2024, and relevant transition-related policies by county. Physicians are encouraged to review the table to see what changes are coming to their counties.
The policy guide also contains DHCS policy and plan requirements, including:
• Member Enrollment and Noticing
• Continuity of Care requirements
• Enhanced Care Management and Community Supports Transition requirements
The California Medical Association (CMA) is also hosting a free webinar with DHCS on August 10, 2023, to help physicians understand and prepare for the transition. DHCS will present an overview of the transition, including health plan changes by county, work underway to ensure a smooth transition, the enrollee continuity of care policy, and physician and patient resources available. DHCS will be available for a question-and-answer session and would like to hear feedback from physicians about how to ensure a smooth transition for Medi-Cal enrollees and providers.
When the COVID-19 public health emergency expired on May 11, 2023, the U.S. Health and Human Services Office for Civil Rights (OCR) announced the end of flexibilities that allowed physicians to utilize remote communication technologies for telehealth services that did not fully comply with HIPAA rules.
OCR provided a 90-calendar day transition period for covered health care providers to come into compliance with the HIPAA rules for telehealth. The transition period will expire at 11:59 p.m.
on August 9, 2023, at which time physicians will be expected to utilize only HIPAA-compliant communication tools.
The HHS website offers a list of some platforms that advertise they provide HIPAA-compliant video communication products.
For more information about the current state of telehealth in California, the California Medical Association (CMA) has published a Telehealth Policy Update. Although the pandemic-era telehealth waivers have ended, many telehealth flexibilities will extend beyond the end of the pandemic due in large part to CMA advocacy at the state and national levels.
Doctors Hospital of Manteca is now part of the Central Valley Doctors Health System, expanding your access to services close to home.

From emergencies and screenings to surgical and procedural services, we deliver quality healthcare and compassionate care.
Doctors Hospital of Manteca offers:
• 24-Hour Emergency Care and Convenient Online Check-Ins
• 24/7 Critical Care Coverage Led by Intensivists
• Advanced Orthopedics for Knee and Hip
• Weight Loss Surgery Center of Excellence
• Imaging Services, Including Open MRI and PET/CT
• Surgical Services
• Women’s Health, Including 3-D Mammography
• Wound Care Center
To refer a patient, call (844) 632-5727 or visit DoctorsManteca.com

Triple-digit heat, wildfire smoke, and flooding are just a few examples of emergencies that San Joaquin County residents experience on a regular basis; however, older adults and those with access and functional needs (AFNs) may face greater health risks during disasters than others. These populations often live alone, rely on medication and/or medical equipment, have a disability that limits their mobility or cognitive abilities, possible limited English proficiency, inadequate access to transportation, and/or restricted financial resources that make it difficult to respond to and recover from an emergency. For these and many other reasons, this high-risk group is the focus of September’s National Preparedness Month. During this celebration you can encourage your patients to take three actions to prepare in case of a disaster: Make a Plan, Build a Kit, Stay Informed.
Making a plan, and involving friends, family, and neighbors in that plan, can help reduce anxiety and ensure better safety and well-being in the event of a disaster. Encourage patients to create a communication plan that details the patient’s trusted network of individuals, including medical providers, that can be called upon during an emergency. Patients should base their plan on the lowest anticipated level of functioning (1). Back-up plans for medication, medical equipment, electricity-dependent equipment, and
transportation should be made. Electric-dependent patients should contact their utility companies, who can prioritize power and advise on backup power plans (2). Additionally, people with disabilities may want to register with the local fire or police station so they can receive quick care during an emergency.
Building a kit can seem daunting, but many people already have the supplies that are needed. FEMA details a basic disaster supplies kit on its website (3). This is a good place to start, but special considerations might be required for older adults and those with AFNs. Extra medication and copies of prescriptions, glasses, batteries, medical equipment, copies of insurance policies/cards, ID cards, and contact information for doctors, friends, and relatives should be considered. For those with durable or electric medical equipment, including operating instructions in the kit can be helpful. A patient may consider labeling their items with their name, which can help during an emergency. Since decisions surrounding pets can also be a challenge during a disaster, also consider sharing FEMA’s list of emergency pet supplies. Once assembled, store the kit in a place where it can be grabbed easily and quickly. It may be a good idea for your patient to store extra medical items at their school, workplace, or a neighbor’s home in case the kit at home is not accessible.
Staying informed about potential emergencies means knowing the disasters that affect where we live, work, and play. Encourage your patients to be ready for various scenarios. It is important to have multiple avenues for receiving information about extreme events. Radio, TV, Wireless Emergency Alerts (WEA), smart phone apps, as well as local emergency services offices like SJReady.org can be helpful to make sure patients are getting information specific to their area.
Because older adults and those with AFNs are especially vulnerable to the health effects that disasters can cause, it is important that healthcare professionals engage their patients in the discussion of emergency preparedness. Start by asking your patient if they have an emergency plan in place. If not, suggest a resource, like Ready.gov, to help them get started. Address your patient’s needs, such as illness or disability, and how they might go about preparing for emergencies that may affect their health or access to medical care. Finally, remember that preparing for emergencies can be a sensitive topic for some patients. Taking the time to Make a Plan, Build a Kit, and Stay Informed can significantly reduce the stress and anxiety patients may feel during emergencies, and hopefully lead to better health outcomes should disaster strike.
SJReady.org is the website of our county’s Office of Emergency Services. Find any local emergency information here, as well as information on San Joaquin County’s Emergency Alert Notification System.
Weather.gov is the website of the National Weather Service. Active alerts, safety information, and educational pages can be found here.
Ready.gov has pages specific for older adults, those with AFNs, kids, and many populations to prepare for, respond to, and mitigate emergencies.
The FEMA App can be installed for IOS or Android. The FEMA app will ask for location services, so it can alert if any disasters or declarations depending on location. In addition, the application has engaging articles on how to better prepare for disasters.
Citations
"Disaster Safety for People with Disabilities." Redcross.Org, Accessed 27 Jul. 2023, Inclusive Preparedness Resources | American Red Cross "Emergency Power Planning for People Who Use Electricity and Battery-Dependent Assistive Technology and Medical Devices." Adata.Org, Accessed 27 Jul. 2023, Emergency Power Planning for People Who Use Electricity and Battery-Dependent Assistive Technology and Medical Devices | ADA National Network (adata.org)
"Build a Kit." Ready.Gov, Accessed 27 Jul. 2023, www.ready.gov/kit
1929 - 2023
Dr. Bryant Bennett Williams, 93, of Stockton California, peacefully passed away at home on July 20, 2023. He was a beloved father, Pediatrician, cherished friend and faithful servant of God.
Dr. Williams was born on September 24, 1929, to Bryant Bennett Williams, Sr and Luella Smith Williams in San Antonio, Texas. He was very active in High School including being Senior Class president and co-captain of the football team. It was at this time he realized his true calling to be a pediatrician. He even quoted in his yearbook that was his future ambition.
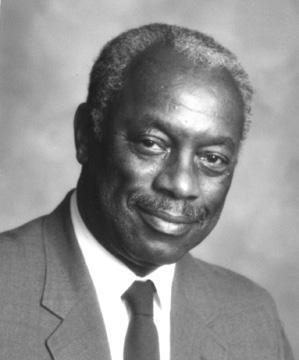
After graduating from High School, he moved to Nashville, Tennessee to attend college at Fisk University. He then
continued on to Meharry Medical School where he earned his Doctor of Medicine. While attending Meharry he met his beloved wife, Janice Huffman who was attending college at Fisk at the same time. He moved to Oakland, CA to complete his residency at Highland Hospital so he could be closer to Janice who had previously moved to California to be with her sister after college. Bryant and Janice married in 1960 and decided to build their life in Stockton, California.
Dr. Williams started his medical practice in Stockton that would span over 50 years. During this time, he received numerous accolades for his work in the community, including the San Joaquin Medical Society’s Lifetime Achievement Award in 2012.
He was predeceased by his parents, and two siblings Rosalyn and Gwendolyn. He is survived by his wife of 62 years, Janice, his children, Bryant (Daughter-in-law Antoinette) Brett, Jonathan and Jana (Son-in-law Warren). Grandchildren; Ryan, Joseph, Ava and nieces and nephews.
1930 - 2023
Beloved father, family physician, and friend, Dr Robert T Browne, 93, passed away at home in Stockton on June 30, 2023. As someone who always went the extra mile to care for and support those around him, usually with quick wit or a funny story, he left the world a better place and will be deeply missed. With Evelyn, his wife of 60 years (now deceased), they are survived by their two daughters, Kathleen Rosing (Gary) and Anne Marie Ott, his brother Leo of Melbourne, FL, and their grandchildren Jordan, Sara, and Colby Ott. Extended family includes his sister-in-law, Doris Piasecki and many nieces and nephews on the east coast, Kathleen’s stepchildren Laura Rosing, Michele and Kelly Bohren, and grandchildren, Jaidyn and Gianna Bohren.
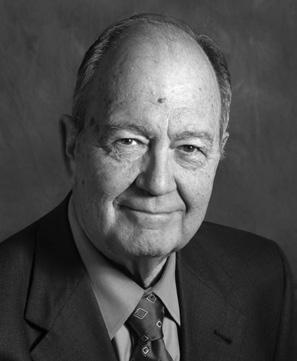
Dr. Browne practiced family medicine for over 60 years in Stockton and was the founding medical director of the Hospice of San Joaquin. As a physician, he was dedicated to providing medical services to the underprivileged, and was a champion for the profession of medicine, serving as president of the San Joaquin Medical Society in 1980, with membership spanning his career. Additionally, he was active in sports medicine as a team physician for Stagg High School and the Stockton Ports baseball teams.
Bob continued in private practice until this year when he retired from working with Dr Kirti Solanki, Jennifer Hasselbach, FNP, and his “family” of employees who have
been together for years. Although retired, he couldn’t help but stop by the office to socialize and help when he could.
Over the years, he and his family enjoyed travelling around the United States and other countries. An avid wine “connoisseur”, Bob was part of a cohesive group of friends who would get together weekly to share wines, meals, and stories. They would sometimes travel locally to wineries as well as to France for wine-tasting.
He was a eager supporter of local arts and could frequently be seen at symphony concerts, musicals, fund-raisers and philanthropic organization functions.
1934-2023
Gerald Charles Barnes, MD passed away peacefully on Sunday, August 6. Jerry, as he was known by friends, will be greatly missed for his intelligence and good humor. Born in Sioux Falls, South Dakota in 1934, Jerry was a resident of San Joaquin County for decades, beginning with an internship/residency at San Joaquin General Hospital in 1965. He served in the US Marine Corps from 1954-57. He was a proud graduate of the University of Wisconsin, Madison, where he studied medicine and started his family with his wife Darlene, of Lodi, Wisconsin. A BoardCertified Orthopedic Surgeon,
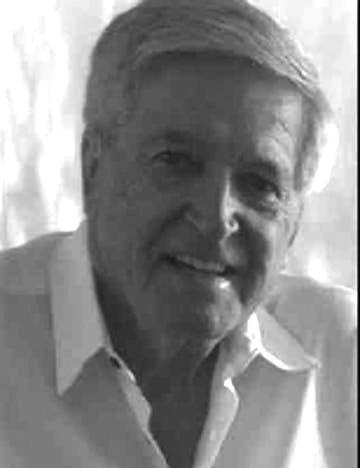
Jerry joined Stockton Orthopedic Medical Group in 1970, and later worked with Kaiser Permanente in Stockton & Modesto. In the mid-70s he was a team physician for high school football (Franklin and Stagg). He was an active member of the San Joaquin Medical Society, serving on multiple committees throughout his career.
One of his greatest passions outside medicine was his love of thoroughbred horses. Jerry was an owner-breeder of several horses - "The Sport of Kings." He and Darlene made it to the winner's circle, and also enjoyed the races at The Kentucky Derby.
Upon retirement, they hit the road in their American Dream, celebrated each wedding anniversary at Lake Tahoe, and finally after he really retired, Jerry got to golf more and improve his game of duplicate bridge. He is survived by brothers Marshall and James, wife Darlene and their 3 children: Jerry, Susan and Karen, as well as 4 grandchildren: Jade, Jackson, Galan and Sarra.
San Joaquin Medical Society
3031 W. March Lane, Suite 222W
Stockton, California 95219-6568
The Medi-Cal redetermination process is still underway for over 14 million California enrollees. This includes approximately 600k San Joaquin and Stanislaus County residents.
The Department of Health Care Services (DHCS) is asking Medi-Cal beneficiaries to update their contact information at BenefitsCal.com. This will ensure that beneficiaries receive their renewal packets and are able to respond to requests for information that will help determine their eligibility.
You can continue to communicate the details of the renewal process to your Medi-Cal patients and let them know they will receive a letter or envelope in the mail. Encourage them to take action to keep their coverage by:
• Visiting BenefitsCal.com to update their personal information
• Returning renewal forms as quickly as possible in person to their local Medi-Cal office, by mail, or online at BenefitsCal.com
You may have patients that did not turn in renewal forms or have experienced loss of coverage and have questions:
“I did not turn in my renewal form or information. I got a notice that my Medi-Cal is ending. What can I do?”
“I got a notice that I no longer get medical. I think I still should get it. What can I do?”
You can find answers to those questions and more at dhcs.ca.gov/keep-yourMedi-Cal/Pages/faqs.aspx
Encourage your patients to get vaccinations and boosters during their routine visits. HPSJ rewards Members for completing certain wellness exams. Find more information at www.hpsj.com/myrewards
www.hpsj.com/provider
