Spring 2024 SERVING SAN JOAQUIN, OPERATION ACCESS PAIRS UP WITH SUTTER 'S STOCKTON SURGERY CENTER Healthy Living in San Joaquin County CalMedForce Funding Protect Access to Healthcare Act

















SPRING 2024 SAN JOAQUIN PHYSICIAN 3 VOLUME 72, NUMBER 1 • MARCH 2024 6 A MESSAGE FROM EXECUTIVE DIRECTOR 8 A MESSAGE FROM OUR PRESIDENT 12 HEALTHY LIVING IN SAN JOAQUIN COUNTY 16 HOLIDAY PARTY 18 CHARTING A HEALTHY COURSE 26 PROTECT ACCESS TO HEALTHCARE ACT 28 CALMEDFORCE FUNDING 30 OPERATION ACCESS PAIRS UP WITH SUTTER’S STOCKTON SURGERY CENTER 36 IN THE NEWS 46 RESIDENTS REPORT 48 PRACTICE MANAGEMENT 52 PUBLIC HEALTH 56 IN MEMORIAM 57 NEW MEMBERS
PRESIDENT Cyrus Buhari, DO
PRESIDENT ELECT Neelesh Bangalore, MD TREASURER Sujeeth Punnam, MD
BOARD MEMBERS Stephen Tsang, MD, Maggie Park, MD, Alain Flores, MD, Manreet Basra, MD, Sanjeev Goswami, MD, Kinnari Parikh, MD, Inderpreet Dhillon, MD, Bhagya Nakka, MD, Sunny Philip, MD, and Ripudaman Munjal, MD
MEDICAL SOCIETY STAFF
EXECUTIVE DIRECTOR Lisa Richmond
MEMBERSHIP COORDINATOR Jessica Peluso
COMMITTEE CHAIRPERSONS
CMA AFFAIRS COMMITTEE Larry Frank, MD
DECISION MEDICINE Kwabena Adubofour, MD
MEDICAL EDUCATION PROGRAMS Kelly Savage, MD
SCHOLARSHIP LOAN FUND Gregg Jongeward, PhD
CMA HOUSE OF DELEGATES REPRESENTATIVES
Robin Wong, MD, Lawrence R. Frank, MD
James R. Halderman, MD, Raissa Hill, DO
Richelle Marasigan, DO, Ramin Manshadi, MD
Philip Edington, MD , Sujeeth Punnam, MD
Sunny Philip, MD, Ripudaman Munjal, MD
SAN JOAQUIN PHYSICIAN MAGAZINE
EDITOR Lisa Richmond
EDITORIAL COMMITTEE Lisa Richmond, Cyrus Buhari, DO
MANAGING EDITOR Lisa Richmond
CREATIVE DIRECTOR Sherry Lavone Design
CONTRIBUTING WRITERS Jo Ann Kirby, Cyrus Buhari, DO, Deepa Singh, MPH, Nadeja M. Steager
THE SAN JOAQUIN PHYSICIAN MAGAZINE is produced by the San Joaquin Medical Society
SUGGESTIONS, story ideas are welcome and will be reviewed by the Editorial Committee.
PLEASE DIRECT ALL INQUIRIES AND SUBMISSIONS TO:
San Joaquin Physician Magazine
3031 W. March Lane, Suite 222W Stockton, CA 95219
Phone: (209) 952-5299 Fax: (209) 952-5298
E-mail Address: lisa@sjcms.org
MEDICAL SOCIETY OFFICE HOURS:
Monday through Friday 8:30am-4:30pm
Closed for Lunch between 12pm-1pm
4 SAN JOAQUIN PHYSICIAN SPRING 2024


ACCESS IS KEY
As I was compiling stories for this issue, I noticed the common thread was access to care; whether it is a direct or indirect result of the initiatives we highlight and champion through the San Joaquin Medical Society and the California Medical Association.
A few years ago, the SJMS Board of Directors was approached by a non-profit organization, Operation Access (OA). They organize medical volunteers and arrange surgical and specialty care for patients in need. Elective, outpatient procedures are provided free of charge to the patient in specialties such as GI, General Surgery, GYN, Head & Neck, Ophthalmology, Orthopedics and Urology. For years, patients from San Joaquin County were being referred to the Bay Area for surgery and the organization was working to network and expand to our community.
Through OA’s partnership model, volunteers/facility determine the quantity of referrals accepted in a predetermined period, and cases are integrated into their schedule or organized in a block of donated care. Operation Access manages logistics and case manages patients to maximize efficiency for partners. When I learned the first surgery in our area was being performed by Dr. Patrick Manookian at Sutter’s Stockton Surgery Center, I knew we needed to feature it here. Learn more about the organization and how to get involved on page 30
Physicians for a Healthy California, the non-profit arm of CMA, announced more than $38 million in CalMedForce awards across the state to support medical training and residency programs and help grow the physician workforce. In this sixth round of funding, programs in San Joaquin County were awarded a total of $960,000! As we know, physicians who train here are far more likely to stay and serve the community, where they are desperately needed to improve access to care for patients.
The California Medical Association and the Coalition to Protect Access to Care have launched the Protect Access to Healthcare Act and are working to place it on the November 2024 ballot to ensure that millions of Californians have great access to affordable, high-quality, lifesaving healthcare. Historically, California has used the Managed Care Organization (MCO) Tax- a tax on health insurance companies- to draw down federal funding and help support the State’s General Fund. The last MCO Tax expired at the end of 2022. The proposed ballot initiative will use MCO Tax revenue to make critical and meaningful investments in the Medi-Cal system. Please look for more information in coming months.
Finally, please save the date for our annual Young Physician and Lifetime Achievement Award dinner on Sunday, June 9, where we will be honoring Drs. Adnan Khan of San Joaquin Cardiology and Dr, Edward Schneider, retired family practice physician.
Be well,
 Lisa Richmond
Lisa Richmond
6 SAN JOAQUIN PHYSICIAN SPRING 2024
EXECUTIVE DIRECTOR’S REPORT
LISA RICHMOND


SPRING 2024 SAN JOAQUIN PHYSICIAN 7 EQUIPMENT LOANS 5.99% *Advertised as low as interest rate is accurate as of February 1, 2024 and is subject to change. All rates and terms are subject to credit approval. Some restrictions may apply. Speak with a bank representative for details. (209) 944-1516 Locally Owned and Locally Managed Since 1965 2023 WINNER Best Bank and Best Business Loans
It has been an honor

ABOUT THE AUTHOR
Cyrus Fram Buhari, DO is the current president of the San Joaquin Medical Society and practices at the San Joaquin Cardiology Medical Group
During the past 2 years I have had the honor of serving as the San Joaquin Medical Society Board President. Past Presidents held the reigns during times that brought us together as a group and times that highlighted our differences. Some examples were COVID-19 and the efforts that the SJMS made to ensure the safety of our physician community as well as the fight against outside forces who sought to dissolve the MICRA protections altogether. My tenure has been slightly rocky, however I feel that during this time our SJMS was as engaged, as passionate, and as effective as at any other time in our history.
We oversaw the extension of COVID telehealth waivers that were so vital to maintaining and expanding patient access to care while extending the Medi-Cal telehealth payment parity. We led the charge to continue to reduce administrative burdens on physician practices. We continue to fight against scope of practice infringements scoring victories along the way.
Our fight is not done. We, along with CMA, are pushing with full force to lobby congress to stop and reverse CMS payment cuts to physician practices. Should they remain, we will see dire consequences for patient access and overall care for our already underserved community. We are much stronger in this fight when we are together and advocating with one voice.
For my next-to-last editorial piece as President of your SJMS I have decided to keep it short and sweet. Our success has been achieved due to the hard work of the Executive Director and Membership Coordinator. For doing the job they do with a sense of pride and ownership they force us all to shoot for the best in advocacy and clinical practice. SJMS is currently in and has maintained an excellent financial position. Together we strive to increase our membership through offering value to our physician community through various advocacy, educational and social opportunities. Pipeline programs like Bridge to Medicine and Decision Medicine, aimed at encouraging talented, local students to go in to medicine, are prime examples of addressing the physician shortage in absolute service to our community.
There will be one more editorial piece from me after this as I start to transition to the role of immediate Past-President of the San Joaquin Medical Society. I have the utmost confidence that the integrity of the Society and its membership are represented flawlessly by the board. We must continue to grow the membership and we must keep a goal of having all of our community physicians involved as members of our SJMS.
Thank you for the continued opportunity to serve the San Joaquin Medical Society and its membership.
8 SAN JOAQUIN PHYSICIAN SPRING 2024
from our
> Cyrus
Buhari, DO
A message
President
Fram
HealthCare is Better Together.








Central Valley Doctors Health System
Three Trusted Hospitals, One United Team
We believe together, we can do so much good. Serving as one health system allows us to enhance patient care coordination, access to our hospitals and the many specialized services and resources our facilities provide. And, Central Valley Doctors Health System Transfer Center provides a seamless patient experience. One call provides direct access to our hospitals.
• Level II Trauma Center
• Central Valley’s only Comprehensive Stroke Center
• Bariatric Center of Excellence
• Blue Distinction Center for hip and knee replacement
• Robotic-assisted surgery
• Comprehensive Oncology Center
• Heart Care
• Premier Obstetrics and Neonatal Intensive Care (NICU)
We are always your Community Built on Care.

SPRING 2024 SAN JOAQUIN PHYSICIAN 9
To learn more, call 855-631-5673 or visit CVDoctorsHealthSystem.com

Leading cardiovascular care, with heart.
Your heart might be something you’ve always taken for granted. But it’s the whole reason we’re here. St. Joseph’s Medical Center is one of the nation’s 50 Top Cardiovascular Hospitals, bringing not only clinical expertise, but a passion to heal. We are renowned for our advanced diagnostic and treatment options, supported by comprehensive rehabilitation services that help get patients back to feeling their best. From routine checkups to lifesaving procedures, our team has the expertise and the dedication to care for your heart—and the person around it. Learn more about our innovative services at dignityhealth.org/stockton/heart.


SPRING 2024 SAN JOAQUIN PHYSICIAN 11

Healthy Living in San Joaquin County
BY NADEJA M. STEAGER
The Community Health Leadership Council (CHLC), in its 24th year, continues to help shape the future of healthcare in the Northern San Joaquin Valley. Key leaders across healthcare, education, and business come together regularly to discuss and identify critical health risks needing to be addressed, lessened, and where possible removed. The council has focused on healthcare economics, the workforce, youth behavioral and mental health, and most recently, community health and improving access and utilization to services programs and resources.
chronic diseases, offer valuable insights into behaviors and lifestyles that promote community health. The forum brought together multi-sector leaders, stakeholders, and community members across healthcare, education, and business, to connect and learn about Blue Zones and consider the possibilities of San Joaquin County becoming a Blue Zone.
Keynote speaker, Danny Buettner Jr., brought a
message of fostering healthier lifestyles that can result in increased longevity and vitality.
In November of 2023, the CHLC hosted its 23rd Annual Community Health Forum with a keynote message on Blue Zones, a concept originating from research by Dan Buettner, which identifies regions around the world where people live significantly longer and healthier lives. These areas, characterized by high levels of well-being and low rates of
Keynote speaker, Danny Buettner Jr., brought a message of fostering healthier lifestyles that can result in increased longevity and vitality.
Danny highlighted successful implementations of Blue Zones in other regions, illustrating the potential benefits for our county. One notable example is the transformation of Loma Linda, California, where residents have embraced Blue Zone principles with remarkable results. Through initiatives such as promoting plant-based diets, creating walkable neighborhoods, and fostering strong social connections, Loma Linda has seen






reductions in obesity rates, chronic diseases, and healthcare costs. With healthy lifestyle behaviors and a focus on traditional diets rich in fruits, vegetables, and fish, along with regular physical activity and a strong sense of community, some have achieved some of the highest life expectancies.
Danny was joined by a panel of local experts, Erin Garica, Community Medical Centers, Nick Lee,
Attendees were immersed in a Blue Zone world where healthy living is natural and yields happiness, fulfillment, and the potential for long life, Local healthcare professionals and stakeholders expressed enthusiasm about the potential impact of Blue Zones in our county.
The Edible Schoolyard, Barb Alberson, San Joaquin County Public Health Services, and Melissa Flores, Collins Electrical Company Inc. and MC and Moderator, Brian Jensen, Hospital Council Northern and Central California. Collectively they highlighted the connection between Blue Zones concepts and

CHLC Members
Dr. Lisa Aguilera-Lawrenson Superintendent/President
SAN JOAQUIN DELTA COLLEGE
Barb Alberson
Sr. Deputy Director/Interim Director
SAN JOAQUIN COUNTY PUBLIC HEALTH SERVICES
Troy Brown Superintendent of Schools
SAN JOAQUIN COUNTY OFFICE OF EDUCATION
Paul Canepa Supervisor, District 2
SAN JOAQUIN COUNTY BOARD OF SUPERVISORS
Greg Diederich Agency Director
SAN JOAQUIN COUNTY
HEALTH CARE SERVICES AGENCY Interim CEO
SJ Health
Dr. Gretchen Edwalds-Gilbert Provost and Executive Vice President
UNIVERSITY OF THE PACIFIC

Alain Flores, MD Assistant Physician-in-Chief
THE PERMANENTE MEDICAL GROUP
Matt Garber Assistant Director
SAN JOAQUIN COUNTY HEALTH CARE SERVICES AGENCY
SPRING 2024 SAN JOAQUIN PHYSICIAN 13



local initiatives and efforts, such as Healthy Eating and Active Living (HEAL), that align with two of the Blue Zones Power 9; Plant Slant and Move Naturally.
Attendees were immersed in a Blue Zone world where healthy living is natural and yields happiness, fulfillment, and the potential for long life, Local healthcare professionals and stakeholders expressed enthusiasm about the potential impact of Blue Zones in our county. And, with an emphasis on fostering healthier lifestyles to increase longevity, the initiative sparked optimism and excitement.
If adopted, Blue Zone implementation in the county could bring forth numerous benefits. From improved physical health and vitality to enhanced social connections and community engagement, the initiative holds the promise of a holistic wellness revolution. With improved health reducing healthcare costs associated with preventable diseases, Blue Zones could
If adopted, Blue Zone implementation in the county could bring forth numerous benefits.
offer long-term economic advantages for the county.
As discussions continue, stakeholders remain committed to ensuring that efforts will be focused on initiatives like Blue Zone principles of healthy eating and active living and will be tailored to the unique needs and culture of our communities. The implementation of Blue Zones concepts could change the trajectory of our community’s health for generations to come.
With the support and guidance of the Community Health Leadership Council and the collective commitment of residents, San Joaquin County has the opportunity to create a vibrant community where improved well-being is the standard, chronic diseases are lessened, and longevity becomes the norm. Gleaning from successful Blue Zone implementations worldwide and infusing the community’s unique cultural identities into every initiative, we can work together to develop a culture of health and vitality.


Lizeth Granados
Chief Executive Officer
HEALTH PLAN OF SAN JOAQUIN
Brian Jensen
Regional Vice President
HOSPITAL COUNCIL OF NORTHERN & CENTRAL CALIFORNIA
Sanjay Marwaha, MD Physician in Chief THE PERMANENTE MEDICAL GROUP
Brooke McCollough President
ADVENTIST HEALTH, LODI MEMORIAL HOSPITAL
Christine Noguera
Chief Executive Officer COMMUNITY MEDICAL CENTERS
Thomas Pogue
Director of the Center for Business and Policy Research UNIVERSITY OF THE PACIFIC
CHLC Members

Lisa Richmond
Executive Director
SAN JOAQUIN MEDICAL SOCIETY
Nadeja Steager
Executive Director
COMMUNITY HEALTH LEADERSHIP COUNCIL SAN JOAQUIN Director
SAN JOAQUIN PATHWAYS COMMUNITY HUB
Sarah Sweitzer
Dean, Stockton Campus STANISLAUS STATE UNIVERSITY
Don Wiley
Chief Executive Officer and President
DIGNITY HEALTH, ST. JOSEPH’S MEDICAL CENTER
Betty Wilson Executive Director
BUSINESS COUNCIL OF SAN JOAQUIN COUNTY
Moses Zapien, Chief Executive Officer & President SAN JOAQUIN COMMUNITY FOUNDATION
SPRING 2024 SAN JOAQUIN PHYSICIAN 15









Holiday Party


CMA’s 2023 Areas of Focus Recap
In January of 2023, CMA’s physician leaders met to take stock of California’s current health care landscape and decide where to focus the organization’s efforts in the coming year.
These physician leaders identified the following four key areas of focus for 2023 and made significant progress in each:
+ Advancing health equity and access to care
+ Assuring professional autonomy
+ Reducing wasteful administrative burdens
+ Growing membership


Advancing Health Equity and Access to Care
CMA’s top priority in 2023 was our campaign for health access and equity. The California Legislature and Governor Gavin Newsom have taken tremendous steps to expand Medi-Cal eligibility to all income-eligible Californians, covering more than 14 million Californians. Over the last decade, eligibility expansions have led to millions of Californians enrolling in the Medi-Cal program.
CMA proudly supports this expansion and the goal of universal access, but we believe it must be coupled with true access to care. Public health insurance programs cannot be an empty promise.
Historic Medi-Cal Rate Increase: In 2023, CMA and a broad coalition of health care providers, hospitals, emergency responders, community health centers, Planned Parenthood and health plans advocated to improve Medi-Cal access to care. As a result, Governor Newsom signed budget legislation in July 2023 to provide the largest Medi-Cal rate increase in California history. A historic win for physicians and patients, the signed legislation dedicates a portion of funds raised through the reinstatement of the Managed Care Organization (MCO) Tax, which expired late last year, to help sustain and increase investment in the MediCal program.
The first phase of Medi-Cal provider rate increases, which takes effect January 1, 2024, is targeted to primary care, obstetric, and non-specialty mental health services to raise the reimbursement rates in these areas to at least 87.5% of Medicare. Also included in the first phase will be budget increases that will make it possible to train hundreds of additional physicians each year by expanding graduate medical education residency slots.
In 2025, the level of funding committed to Medi-Cal rate increases is slated to grow substantially. A second phase of rate increases, effective January 2025, will provide additional investments in primary care, obstetric care, and non-specialty mental health services as well as specialty care services and emergency department care.
“CMA physicians have been sounding the alarm that health equity and health care access in the Medicare program are deteriorating and we need Congress’s leadership to restore the promise of Medicare to our patients.”
Additionally, CMA and the Coalition to Protect Access to Care, a broad and diverse group of health care organizations, have filed a statewide ballot initiative with the California Attorney General’s office that will build upon and make permanent the victories secured in the 2023-24 budget deal for patients and providers. CMA is working closely with the other members of the coalition to gather the hundreds of thousands of signatures needed to place the initiative on the 2024 November ballot.
In Washington, D.C., CMA is fighting for Medicare payment reform by urging lawmakers to support H.R. 6683, the “Preserving Seniors’ Access to Physicians Act,” by Representatives Gregory Murphy, M.D. (R-NC), Jimmy Panetta (D-CA), Brad Wenstrup (R- OH), and Danny Davis (DIL). This bipartisan legislation will stop the 3.37% Medicare physician fee schedule payment cut set to take effect on January 1, 2024.
SAN JOAQUIN PHYSICIAN 19
CMA is also seeking a long-overdue annual inflation update for Medicare physicians. When adjusted for inflation, physician payments have declined 26% since 2001, while practice costs have risen 47% over the same period.
CMA is working to pass H.R. 2474, the “Strengthening Medicare for Patients and Providers Act.” The measure was introduced by California physician Congressional representatives Raul Ruiz, M.D. (D-CA), Ami Bera, M.D. (D-CA), and their Republican partners Larry Bucshon, M.D. (R-IN) and Mariannette Miller-Meeks, M.D. (R-IA). If enacted, the bill would provide an automatic, annual inflation update to the Medicare Physician Fee Schedule tied to the Medicare Economic Index (MEI) – thereby granting physicians inflation updates all other Medicare providers already receive. By tying physician fees to the MEI, the bill will bring much-needed stability to physician practices and protect patients’ access to medical care in California, particularly in our underserved areas and lowincome communities of color.
“CMA physicians have been sounding the alarm that health equity and health care access in the Medicare program are deteriorating and we need Congress’s leadership to restore the promise of Medicare to our patients,” said CMA President Tanya Spirtos, M.D. A 2022 CMA survey showed that nearly half of physicians are contemplating early retirement
Assuring Professional Autonomy
due to low Medicare payments, and two-thirds are considering limiting their Medicare patients or dropping out of the program entirely.
CMA is also working with the American Medical Association (AMA) and others in organized medicine to pass additional Medicare payment reform legislation this year that will create exemptions to the current budget neutrality requirements in the Medicare fee schedule that forces cuts on some services to provide updates for others. Legislation is also being crafted to reduce the administrative burdens in the Merit Incentive Payment System (MIPS).
Public Service Loan Forgiveness Program (PSLF): In response to advocacy by CMA, the U.S. Department of Education (DOE) will now allow eligible California physicians to participate in the PSLF program, despite state prohibitions on physician employment by private non-profit hospitals, clinics, foundations and other health care entities.
The fix is a major win for California and Texas physicians, hospitals, and patients as it ensures physicians in California and Texas will have equal access to this important loan forgiveness program. To assist physicians in applying for the PSLF program, CMA developed a guide, “Public Service Loan Forgiveness: What California Physicians Need to Know,” which can be found at cmadocs.org/pslf.
In California and across the country, unlicensed or lay entities – such as private equity funds, hospital systems, staffing management companies and other corporate organizations that are owned or controlled by non-physicians – are working to expand their reach from hospitals and nursing facilities, into physician practices. CMA is working to address this practice in a number of ways.
Protecting the Corporate Bar: The corporate bar is a broad and robust law that touches on nearly every aspect of the delivery of medical care by physicians and other licensed health care professionals. It springs from a fundamental public policy to protect and preserve the independence of physicians’ professional judgment in the care of their patients, free from external forces that can interfere with the physician-patient relationship. CMA is committed to supporting this California law, which bars lay individuals, organizations and corporations from practicing medicine. However, there continue to be attempts to chip away at California’s corporate bar. Legislation introduced this year, Senate Bill 784 (Becker), would have created permanent exemptions to the corporate bar for health care districts.
Supporters of the bill argued it would help address the physician shortage and increase access to care by authorizing health care districts that own or control a general acute care hospital to directly

20 SAN JOAQUIN PHYSICIAN

employ physicians and surgeons. However, CMA argued that the bill would undermine long-standing patient protections, and the bill was held in committee until 2024.
CMA has also been active in protecting the corporate bar in the courts. Last year CMA filed an amicus brief in support of emergency physicians in American Academy of Emergency Medicine Physician Group (AAEMPG) v. Envision Healthcare Corp. In the suit, AAEMPG alleges that Envision violated California laws barring corporations from practicing medicine when it took over staffing of the emergency department at Placentia-Linda Hospital. CMA’s amicus brief provides the court with a thorough picture of how Envision’s business model not only threatens the physicians involved in the lawsuit, but how, if left unchecked, Envision’s business model provides a roadmap for corporate entities to similarly disempower physicians throughout the state.
Envision Healthcare announced in May that it filed for bankruptcy protection, but AAEMPG has vowed to continue the federal lawsuit. CMA will continue to monitor and provide support as needed.
Addressing Consolidation in Health Care: CMA is also supporting efforts to reduce consolidation in health care. In 2022, Governor Newsom signed legislation establishing the Office of Health Care Affordability (OHCA), which will set health care spending targets for health insurers and providers. This board could have significant implications for physician practice viability and consolidation. The board members have been seated and include pediatrician and former state senator Richard Pan, M.D. CMA has built a team that is engaging with the new office and has played a critical role both legislatively and through the regulatory process to ensure OHCA’s growth targets do not unjustly focus on physician practices that are not the true cost drivers in health care.

“CMA’s amicus brief provides the court with a thorough picture of how Envision’s business model not only threatens the physicians involved in the lawsuit, but how, if left unchecked, Envision’s business model provides a roadmap for corporate entities to similarly disempower physicians throughout the state.”
Reducing Wasteful Administrative Burdens
Reducing or eliminating administrative burdens is another top priority for CMA. We hear regularly from CMA members that unnecessary administrative tasks are a waste of time and resources, take valuable time away from patients, are a critical driver of excess health spending, and are a major contributor to physician burnout. We have been pursuing efforts at both the state and federal level to help reduce that burden.
Right-Sizing Prior Authorization: CMA sought to reduce harmful prior authorization burdens through Senate Bill 250 (Pan) in 2021- 2022. While the bill faced strong opposition from the health plans, it progressed further in the legislative process than any previous attempts to address the problem.
In 2023, physicians and patients once again came together to fix the broken prior authorization system with legislation authored by Senator Nancy Skinner. While health plans mounted an aggressive effort to kill Senator Skinner’s original bill, SB 516, which carries many of the same provisions to reform the prior authorization process, will advance in 2024 when it is heard in the Assembly Appropriations Committee in the New Year.
“CMA has heard no shortage of stories from members and their patients about prior authorization-related delays that have led to prolonged patient suffering, unnecessary trips to hospitals, patient endangerment, permanent injury and even death.”
At the Federal Level, CMA is urging the Centers for Medicare and Medicaid Services (CMS) to finalize regulations that bring meaningful improvements to Medicare Advantage plan prior authorization programs. The CMS regulations reflect CMA-supported bipartisan legislation authored by California physician Congressman Dr. Bera – H.R. 3173/S. 3108, the “Improving Seniors’ Timely Access to Care Act” – that unanimously passed the U.S. House of Representatives in September 2022 and has more than 375 bipartisan House and Senate cosponsors. The proposed regulations require payors to implement more timely and transparent prior authorization programs and incentive gold-carding programs.
Fixing Physician Credentialing: CMA has also heard from members that the redundant and inefficient credentialing process must be modernized to better meet the needs of physicians.
Current credentialing processes require that each insurance plan independently verify physician credentials. Because of this redundancy, a physician must repeatedly seek approval for credentials from each health plan they contract with, no matter how many hospitals a physician has worked in or how many insurance plans they have previously contracted with. This process impacts access to care by significantly delaying the time between a physician’s acceptance of a position and when they can see patients and/or bill for services.

22 SAN JOAQUIN PHYSICIAN

CMA is working with Assemblymember Jim Wood to correct this problem. Assembly Bill 815 would create a one-stop-shop for the credentialing process by requiring the California Health and Human Services Agency to create a provider credentialing board tasked with certifying private and public entities to credential health care providers. Under the bill, if a physician chooses to be credentialed by an entity approved by the board, health plans must accept the physician’s credential. AB 815 cleared its house of origin in 2023 and will move forward in the legislative process in 2024.
Fighting Burdensome Payor Policies: More than a year ago, Cigna announced it would implement a policy requiring the submission of medical records with all Evaluation and Management claims with CPT 99212-99215 and modifier 25 when a minor procedure is billed. CMA mounted opposition to the policy and outlined our concerns to Cigna, urging the payor to rescind the policy that effectively penalized physicians for providing efficient, unscheduled care to patients.
In May, Cigna announced it was pausing implementation to re-evaluate the policy and indicated it would work to optimize the provider experience before any future implementation of the policy. Cigna also said it will work with key national medical associations to educate providers to ensure modifier 25 is used appropriately and in alignment with national guidelines and industry standards.
Growing Membership
Being a member of CMA means being a part of a powerful and active physician community. As a member, your voice and that of all your colleagues are amplified at the local, state and national levels to ensure decision-makers hear and understand the unique challenges facing physicians. CMA not only works hard on your behalf with state and federal policymakers, but also delivers specialized benefits to physicians at every stage of their career.
To drive membership growth in 2024, CMA will continue to work hard for every member and deliver value – regardless of your mode or location of practice. We know the work we do is only possible thanks to the collective strength of our physician members, and we will continue to offer members access to valuable programs and expertise and seek new opportunities to expand membership by demonstrating all that CMA has to offer.
CMA was also successful in advocating for change to UnitedHealthcare’s plans to significantly expand the number of gastroenterology endoscopy services requiring a prior authorization. CMA expressed concern that this was yet another unnecessary administrative burden that would simply delay patient access to medically necessary diagnostic services. As a result of pushback from CMA and others in organized medicine, UnitedHealthcare announced it would pause the prior authorization requirement and instead implement an optional prior notification process.
Stopping Burdensome Legislation: Through our advocacy, we were able to stop several bills that would have been harmful to patients from advancing this year. Assembly Bill 1751 (held in committee) would have forced physicians to inform patients about nonpharmacological treatments for pain, including chiropractic, acupuncture and mental health services; AB 616 (vetoed) would have required audited financial reports and statements from medical groups to be released to the public; SB 524 (held in committee) would have allowed retail chain pharmacists to furnish medications treating conditions identified through CLIA-waived tests performed by a pharmacist; and AB 1570 (held in committee) would have allowed optometrists to perform delicate eye surgeries..

SPRING 2024 SAN JOAQUIN PHYSICIAN 23
cmadocs.org

Here are just some of the benefits ... San Joaquin Medical Society Resources: • Annual Directory • Quarterly Magazine • Social Events • Office Managers Forum • Leadership Opportunities • Patient Referrals CMA Resources: • Legal Help • Contract Analysis • Billing Assistance • Education Resources • News Updates • Practice Resources • Member Discounts Federal, State, and Local Advocacy: Dues support advocacy efforts to protect the profession of medicine and your patients Serving the counties of San Joaquin, Calaveras, Alpine, and Amador (209) 952-5299 www.sjcms.org BECOME A MEMBER OF SJMS/CMA
The California Medical Association and the Coalition to Protect Access to Care have launched the Protect Access to Healthcare Act and are working to place it on the November 2024 ballot to ensure that millions of Californians have greater access to affordable, high-quality, life-saving health care.
BACKGROUND
+ Medi-Cal provides essential health coverage to one in three Californians and is foundational to the state’s health care delivery system and economy. In fact, 15 million Californians and nearly 50% of children get their health care through the Medi-Cal program, making it essential for preventive and routine care for California kids.
+ Medi-Cal provider rates have not increased in more than a decade, and for most physicians it’s been more than 25 years – leaving millions of patients insured, but without meaningful access to health care. Patients with Medi-Cal coverage routinely wait weeks or months for appointments, and oftentimes must travel long distances to receive care.
THE MCO TAX
+ Historically, California has used the Managed Care Organization (MCO) Tax – a tax on health insurance companies – to draw down federal funding and help support the state’s General Fund. The last MCO Tax expired at the end of 2022.
+ Recognizing that we have a generational opportunity to improve health outcomes for millions of Californians, this ballot initiative will use MCO Tax revenue to make critical and meaningful investments in the Medi-Cal system.
THE BALLOT INITIATIVE
The Protect Access to Healthcare Act will increase reimbursement rates for Medi-Cal providers – some of which have not been increased in decades – and expand our state’s graduate medical education and training to create more physician residency programs and funding for more residency positions within those programs. Additionally, there will be funding for loan repayment for physicians, dentists and other allied health professionals. These actions will bring more providers to areas across California where they are needed most.
26 SAN JOAQUIN PHYSICIAN SPRING 2024
Specifically, the initiative will:
+ Make the Medi-Cal provider rate increases that were included in the 2023-24 state budget permanent for generations to come
+ Expand access to health care for Medi-Cal patients, which will result in less use of emergency rooms and decrease wait times for all Californians
Increase funding for mental health programs that care for children and Medi-Cal patients
+ Allow California to manufacture its own insulin and other prescription drugs for Californians at much lower prices than currently exist
In addition to funding Medi-Cal rate increases for primary care, specialty care, mental health care and emergency physician care, the measure will ensure that Medi-Cal patients have more access to preventive medicine, which will reduce expensive and timely emergency room usage, benefiting everyone.
FUNDING CATEGORIES
The Protect Access to Healthcare Act will raise $4.3 billion in annual, ongoing revenue that will be distributed in the following areas:
+ Primary Care - 22%
+ Specialty Care - 22%
+ Emergency Department Access - 8.75%
+ Mental Health Facility Access - 7%
+ Outpatient and Clinic Access - 5.75%
+ Family Planning - 5.5%
+ Graduate Medical Education - 4.5%
+ Health Care Workforce - 4.5%
+ Improved Clinic Quality - 3.5%
+ Public Hospitals - 3.5%
THE COALITION
+ Specialty Dental Services - 3.5%
+ Ground Emergency Transport - 3%
+ Emergency Room Physicians - 2.5%
+ Abortion Access - 1.25%
+ Advance Practice Cllinician and Allied Health Loan Repayment - .75%
+ CalHealthCares Physician and Dental Loan Repayment - .75
+ Community Health Care Workers - .75%
+ Affordable Prescription Drugs - .5%
+ The Coalition to Protect Access to Care consists of of physicians, dentists, health care workers, hospitals, community health centers, Planned Parenthood and emergency responders working together to support a ballot measure to permanently use dedicated funding to support Medi-Cal providers such as physicians, hospitals, women’s health, and community clinics and health centers.
+ The coalition’s goal is to ensure that Medi-Cal enrollees have the same access to care as those with commercial insurance, and that providers can afford to treat their communities as they present themselves – without worrying about the financial solvency of their practices.
cmadocs.org/access
SPRING 2024 SAN JOAQUIN PHYSICIAN 27
9-8-23
31 of California’s 58 counties lack the number of primary care providers recommended by national health experts. The scarcity of residency positions, especially in underserved communities, has further exacerbated the state’s physician shortage.
Millions in grant funds went to community clinics, medical centers and hospitals throughout California.
$40 million1 in Proposition 56 funding is allocated annually through CalMedForce to sustain, retain and expand graduate medical education (GME) programs in underserved communities, thus increasing California’s physician workforce and improving access to quality health care.
Eligibility:
+ Located in CA
+ Licensed as allopathic or osteopathic
+ Provide primary care
+ Accredited by the Accreditation Council for Graduate Medical Education
+ Provide care in medically underserved areas
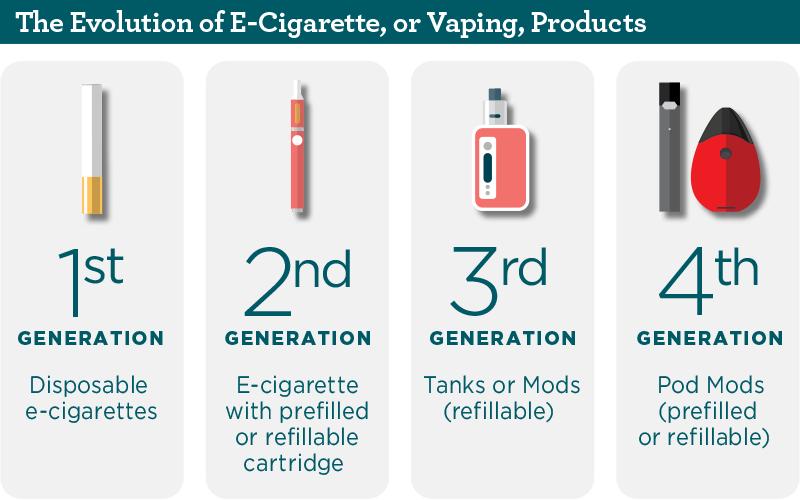
CalMedForce All Cycles Award Summary 2018–2024*
2018–2019
2019–2020
Total Amount Awarded: $227,755,000
*The amount may fluctuate slightly, based on the administration fee and year to year carryover. Award data listed represents original award numbers. Award data is subject to fluctuation for various reasons such as award reductions or loss of residency program accreditation.
28 SAN JOAQUIN PHYSICIAN SPRING 2024
Number of Awardees Number of Resident Positions
Total Awarded: $37,220,000
Total Awarded: $37,740,000 2020–2021 Total Awarded: $37,710,000 2021–2022 Total Awarded: $38,415,000 2022–2023 Total Awarded: $37,955,000 2023–2024 Total Awarded: $38,715,000 217 138 210 129 212 112 201 102 196 88 147 69
State tobacco tax-funded program awards $38 million to expand state’s health care workforce
Demand for CalMedForce GME funding at all time high with over $121.9M requested
Physicians for a Healthy California (PHC) announced more than $38 million in CalMedForce awards across the state to support medical training and residency programs and help grow the physician workforce.
The sixth round of CalMedForce funding, generated by the voter-approved Proposition 56 tobacco tax of 2016 and administered by PHC, supports 217 residency positions in 138 graduate medical education (GME) programs at hospitals and clinics, with an emphasis on those serving medically underserved groups and communities. This cycle marks the largest applicant pool to date, with 155 programs requesting over $121.9 million in funding to support 698 resident positions.
The California Future Health Workforce Commission estimates that California will need an additional 4,700 primary care clinicians by 2025 and 4,100 more by 2030 to meet demand. PHC, in partnership with the University of California (UC), established the CalMedForce grant program to help address California’s physician shortage by supporting residency programs where medical school graduates continue their training prior to obtaining a medical license and caring for patients independently.
“The continued increase in applications over the last six years demonstrates the high demand and need for graduate medical education funding in California to close our physician shortage gap,” said PHC President and CEO Lupe Alonzo-Diaz, MPA.
“CalMedForce funds provide essential support to residency program to continue to grow the physician workforce and ensure access to care for all Californians.”
UC is the designated recipient of Proposition 56 funding and has contracted with PHC to administer CalMedForce. All accredited residency programs in the state that meet guidelines are eligible to apply for funding. Of this year’s CalMedForce awardees, approximately 22 of the 138 awarded GME programs are sponsored by UC.
To date, CalMedForce has allocated over $226.6 million for 638 awards to 167 GME programs across California to retain and expand residency slots in primary care (family medicine, internal medicine, pediatrics, and obstetrics and gynecology) and emergency medicine.
“The increasing demand for funding reflects the importance of this program in supporting the health workforce of California and improving the access to high quality care, particularly for medically underserved groups and communities.” said Deena McRae, MD, Associate Vice President for Academic Health Sciences in the University of California’s Office of the President. “Funding of these residency programs helps the state make critical steps towards achieving health equity.”
“This year’s funding is another crucial step towards strengthening our physician workforce to meet the demands and address access to care challenges in California’s growing and changing patient population,” said Alonzo-Diaz.
SPRING 2024 SAN JOAQUIN PHYSICIAN 29
San Joaquin Programs Awarded $960,000 San Joaquin General Hospital Family Medicine Residency . . . . . $330,000 San Joaquin General Hospital Internal Medicine Residency . . . $330,000 St. Joseph’s Medical Center Emergency Medicine Residency . . $150,000 St. Joseph’s Medical Center Family Medicine Residency . . . . . . $150,000


30 SAN JOAQUIN PHYSICIAN SPRING 2024

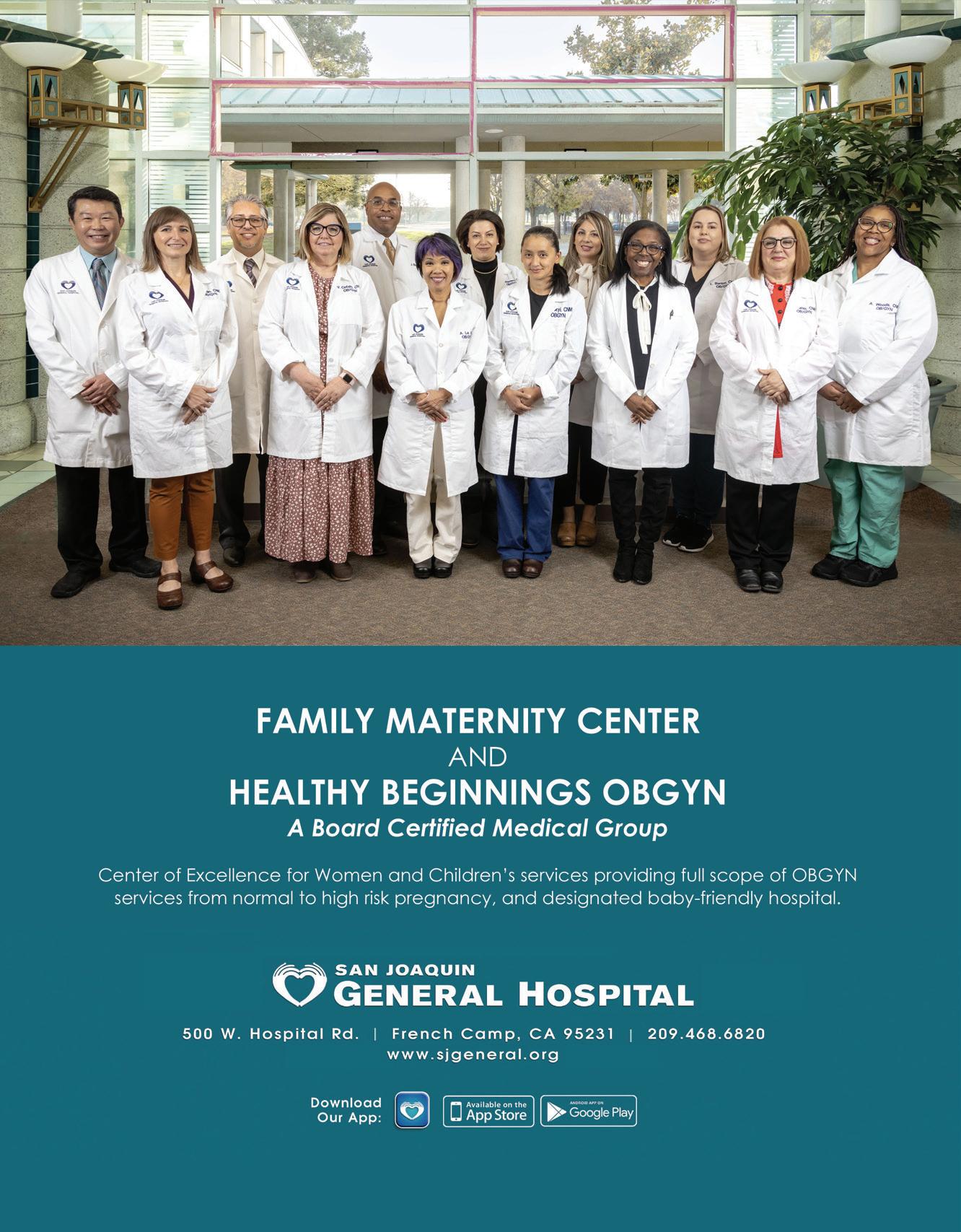
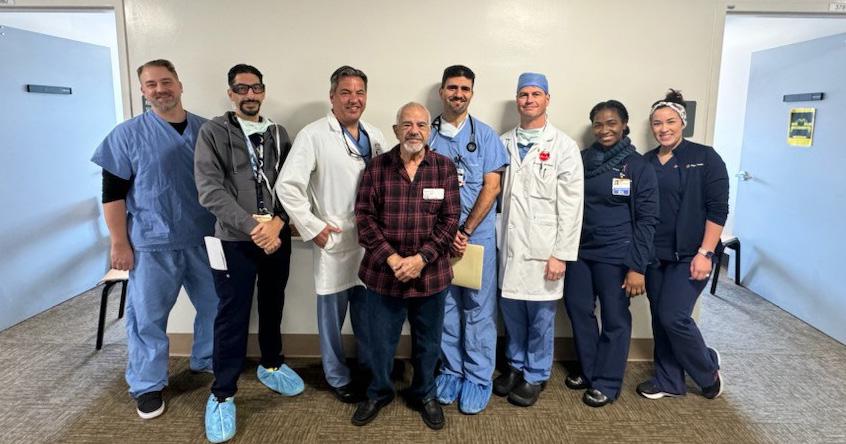
OPERATION ACCESS PAIRS UP
WITH SUTTER 'S STOCKTON SURGERY CENTER

SPRING 2024 SAN JOAQUIN PHYSICIAN 31
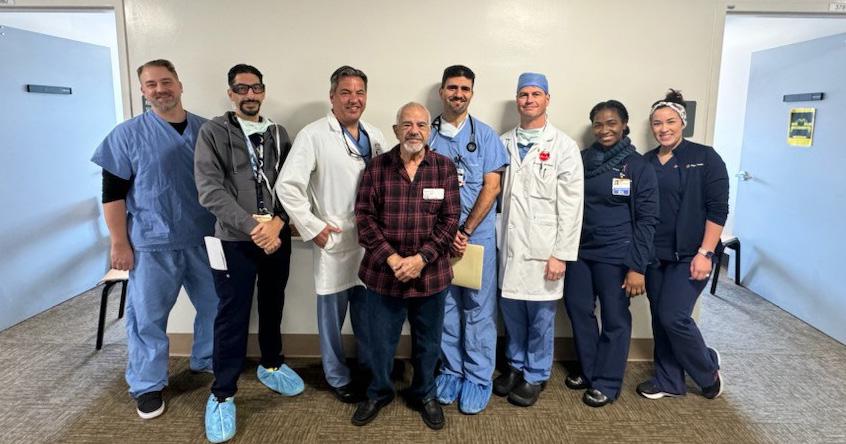
NEW PARTNERSHIP MEANS PATIENTS CAN GET HELP CLOSER TO HOME
BY JO ANN KIRBY
Operation Access, a nonprofit that connects uninsured, low-income patients with donated surgical and specialty care, is now enabling its San Joaquin County clients in need to receive services in Stockton instead of traveling outside the county for care. The organization has formed new partnership with Sutter Gould Medical Foundation that allows qualified clients to have procedures performed at the Sutter’s Stockton Surgery Center.
The first patient to receive care through this new collaboration was Pablo Galan, a 66-year-old Tracy man who found out about Operation Access through Community Medical Centers in Tracy. The uninsured construction worker was suffering from a hernia that was so painful he visited an emergency room and eventually was forced to quit working when he could no longer lift heavy objects.


The inaugural patient to benefit from the new collaboration was matched with Dr. Patrick Manookian, a Stockton surgeon, who performed the surgery at the Sutter’s Stockton Surgery Center in January. “The first procedure was a robotic ventral hernia repair, which went great.” Dr. Manookian said. The patient had his follow up visit and is doing fantastic. He was extremely appreciative and excited to finish recovering from surgery so he can work again,” Dr. Manookian said. “This is the reason I went into medicine, to help those in the most need. I’m sharing my experience with this program with all of my colleagues. I’ve told them there is an opportunity to make a huge difference with these individuals who need our help.”
Over the past 16 years, a total of 462 Operation Access patients residing in San Joaquin County had to travel to the Bay Area or other regions to receive services


32 SAN JOAQUIN PHYSICIAN SPRING 2024

READY TO GET INVOLVED?
Operation Access accepts monetary donations and the nonprofit is looking for medical professionals to volunteer their services. They also seek new partnerships with local hospitals and outpatient surgery centers. For more information, visit www.operationaccess.org/get-involved and take quick survey.
because the nonprofit didn’t have a partnership with local facilities, said Dennise Garcia Leon, an Operation Access program manager. She hopes that other local surgery centers, hospitals, and volunteers will partner with Operation Access so that more patients can be served locally. Leaving their hometown for medical care can be very expensive for Operation Access patients to travel back and forth to the Bay Area for care. “We can provide transportation but often they would have to miss an entire day of work or if they didn’t work, maybe the family member accompanying them would be forced to miss work,” Leon said.
Operation Access has long partnered with Sutter in other locations to provide outpatient surgical and specialty care for the underserved and underinsured

across the greater Bay Area. Johnny Russell, Regional Director of Operations within Sutter Health’s Division of Ambulatory Surgery, said “we’re happy to expand our partnership to care for people in San Joaquin County.” Sutter’s Stockton Surgery Center will be able to provide qualifying Operation Access patients with a variety of outpatient elective procedures. “Patients receive followup care through the referring community health clinics where they already receive their primary care. The surgeons work closely with the patients, the patients’ families and the patients’ primary care doctors to ensure a smooth transition to follow up care.”
Dr. Manookian said volunteering to perform the first Operation Access surgical procedure in Stockton didn’t require him to come in on his day off, the patient was
SPRING 2024 SAN JOAQUIN PHYSICIAN 33
scheduled for the procedure on a normal workday, just like any other patient. “The time spent with these patients is 100 percent volunteered time, which would ordinarily be spent attending to other business,” he said. “The time I spend is within my schedule, but is time I’m giving to the project, which then must be made up elsewhere.” But it is a very gratifying way to give back. “It feels amazing,” Dr. Manookian said. “To me this is an application of my abilities in the purest form,” he said. “I get a great deal of fulfillment from my profession in general. But most patients have choices where they can go for their healthcare — if they don’t see me, they’re probably going to see someone else. With the Operation Access patients, I know if they don’t see me, they’re probably left without an option to get the help they need. That makes it special.”
Russell said both surgeons and medical teams at Sutter-affiliated ambulatory surgery centers are glad to volunteer their time and expertise to offer life-changing elective surgeries to patients who wouldn’t otherwise be able to afford it. “The team is so happy to be a part of the care for patients that need our services and may not have
For Love...
NOT PROFIT
Your trusted local non-profit serving Stanislaus, San Joaquin, Merced and surrounding counties since 1979.
NOT ALL HOSPICES ARE THE SAME.
Make sure to ask for Community Hospice, the longest standing accredited Medicare and Medi-cal certified hospice, palliative and health services organization.
Hospice Care
Palliative Care
Pediatric Care

2431 W. March Lane
Suite 100
Stockton, CA 95207 209.477.6300
hospiceheart.org
received the care otherwise,” he said. “It is a way they feel they can give back to the community.” It’s also a way they can help make a positive change in the overall health of their community.
Leon said Operation Access helps clients who fall through the cracks. People who earn under 200 percent of the federal poverty level are eligible for services through the local partnership at the Sutter’s Stockton Surgery Center. These are low-income people who are financially unable to pay the out-of-pocket cost of specialty care, are unable to obtain insurance or earn too much to qualify for Medi-Cal. People who earn up to 400 percent of the FPL and connect with Operation Access will still have to travel for care to facilities in the East Bay, San Francisco or the Peninsula where they do accept patients over 200 percent of FPL.
Common procedures that Operation Access helps clients find care for are elective, out-patient, medically necessary and low-risk procedures only. Specialists donate their time for procedures in urology, orthopedics, gynecology, gastroenterology, general surgery, ophthalmology, ENT, and other specialties.

Alexander Cohen
Hospice House
The only hospice inpatient and respite facility in Stanislaus County
Hope Counseling
Grief and mental health support services
CommunityHospiceCV
Chi_CommunityHospice
HospiceHeart
Community Hospice
Children’s
Grief Support
School based and Camp Erin® of the Central Valley
Community Education
Hope Chest Thrift Stores
“We are looking to grow and want to work with other centers in order to continue serving uninsured San Joaquin County residents locally,” Leon said. She has a welcome packet for surgeons and other health professionals who would want to get involved. More information on how to get involved or donate, can be found at operationaccess.org.
“I am so grateful for everything and for everyone who has been so kind to me,” Galan said through Leon, who interpreted from Spanish to English for him. “Thank you everyone for helping me. You are my angels.”
Leon said it was a moving experience to help Galan receive care closer to his home. “I love the mission so much,” she said.” Working with doctors who see medical care as a human right is so gratifying.”
34 SAN JOAQUIN PHYSICIAN SPRING 2024





SPRING 2024 SAN JOAQUIN PHYSICIAN 35 The California Medical Association has partnered with Lockton Affinity to administer the CMA Insurance Program. Whether you operate independently or as part of a group practice, are beginning your career or considering retirement, this program offers key benefits to help protect you through all stages: The Lockton Affinity CMA Insurance Program is administered by Lockton Affinity, LLC d/b/a Lockton Affinity Insurance Brokers LLC in California #0795478. Coverage is subject to actual policy terms and conditions. Policy benefits are the sole responsibility of the issuing insurance company. The California Medical Association will receive a royalty fee for the licensing of its name and trademarks as part of the insurance program offered to the extent permitted by applicable law. Not available in all states. Available policies To meet your exact needs, Lockton Affinity offers extensive policy options. BUSINESS COVERAGE Workers’ Compensation Cyber Liability Business Owner’s Policy Business Overhead Expense Employment Practices Liability insurance Affinity Small Group Health Plans PROFESSIONAL COVERAGE Medical Malpractice PERSONAL COVERAGE Individual Health insurance Dental Group Level Term Life insurance Long-Term Care insurance Long-Term Disability insurance Travel Assistance Using group purchasing power, CMA members get exclusive, comprehensive coverage at discounted rates. Discover unique coverage offerings to safeguard yourself, your loved ones, your business and your livelihood. Newly available: CMA members can access Medical Malpractice insurance. Begin your partnership today. Contact Lockton Affinity’s dedicated representatives to select the policies you need to build your insurance package. Info@LocktonAffinityCMA.com | (800) 278-8130 Customized insurance solutions for physicians and health care organizations
IN THE NEWS
Providing staff, physicians, and patients with relevant & up to date information
Save the Date!
The San Joaquin Medical Society will be holding its’ annual membership dinner on Sunday, June 9 at Stockton Golf & Country Club. This year SJMS is excited to present the Young Physician and Lifetime Achievement Awards to Drs. Ajithkumar Puthillath and Robin Wong, respectively. Additionally, we will celebrate the installation of new officers and board members. This festive event is always highly attended by our physician membership and entire medical community.
Healthgrades Names Dignity Health St. Joseph’s Medical Center One of America’s 250 Best Hospitals
Dignity Health St. Joseph’s Medical Center has been announced for the second consecutive year as one of America’s 250 Best Hospitals for 2024, according to new research released by Healthgrades, the leading resource consumers use to find a hospital or doctor. This achievement puts SJMC in the top 5% of hospitals nationwide for overall clinical performance. Additionally, SJMC received Healthgrades America’s 100 Best Hospitals for Critical Care™ for two years in a row (20232024), reflecting St. Joseph’s commitment to exceptional patient care.
St. Joseph’s Medical Center Completes
Milestone of 500th Minimally Invasive TAVR Procedure
Dignity Health St. Joseph’s Medical Center has reached the milestone of completing 500 transcatheter aortic valve replacement (TAVR) procedures, led by Dr. Richard Waters, TAVR team cardiologist. TAVR is a minimally invasive procedure that focuses on replacing a thickened aortic valve that has difficulties fully opening, due to either aortic valve stenosis or aortic valve regurgitation, both of which cause reduced blood flow from the heart to the rest of the body.
St. Joseph’s Cardiovascular Surgery Program has been ranked by Society of Thoracic Surgeons as the highest category for quality and successful outcomes in both coronary artery bypass grafting (CABG) and Aortic Valve Replacement (AVR) procedures.
36 SAN JOAQUIN PHYSICIAN SPRING 2024
In The News
500th TAVR Procedure

St. Joseph’s Medical Center Begins New Lymphedema Prevention Program to Improve Care for Cancer Patients
Dignity Health St. Joseph’s Medical Center, a provider of comprehensive cancer care to the San Joaquin community, announced an innovative new program to reduce the impact of secondary lymphedema in breast cancer patients and survivors. The new program will assist breast cancer patients who are at risk of developing lymphedema from surgery, radiation, or taxane-based chemotherapy treatments.
The new lymphedema prevention program utilizes the latest lymphedema detection technology called L-Dex. L-Dex is a measurement of fluid buildup in an at-risk limb compared to a healthy limb and is measured on the SOZO® system,
graciously funded by the St. Joseph’s Foundation of San Joaquin, which uses a sophisticated technology called bioimpedance spectroscopy (BIS). The SOZO test is non-invasive, takes less than 30 seconds to complete, and provides results immediately after the test. At-risk patients receive a baseline measurement and then are measured regularly after treatment.
St. Joseph’s Medical Center Employees Donate over 1,300 Toys to Children in Need
Dignity Health St. Joseph’s Medical Center held its annual Adopt-a-Child toy drive on December 14th, with 1,332 toys and 31 bikes collected for local children. For more than 40 years, employees at SJMC have donated gifts through the annual event that is organized and carried out entirely by employee volunteers.
Through partnering with nonprofits such as Child Abuse Prevention Council, Human Services Agency, PREVAIL, Children’s Home of Stockton, Haven of Peace, and Stockton Shelter for the Homeless, the toys will be distributed to over 500 local children in the San Joaquin community prior to Christmas.
“We are humbled by the generosity of our employees who continue to make Adopt-a-Child an astounding success year after year,” said President and CEO Donald J. Wiley. “This truly exemplifies St. Joseph’s Medical Center staff’s dedication and commitment to our local community, and I am grateful that we are able to give back in such a meaningful way during the holiday season.”

SPRING 2024 SAN JOAQUIN PHYSICIAN 37
St. Joseph’s Community Health team at the annual toy drive
New SOZO® system at SJMC

since 1899.
Dignity Health - St. Joseph's Medical Center opened its doors as St. Joseph’s Home and Hospital in December of 1899. Its founder, Father William B. O'Connor, collaborated with the Dominican Sisters of San Rafael to assist a local group of physicians in finding a suitable place to treat their medical and surgical patients with specialized care. As the population of Stockton and the surrounding towns increased, St. Joseph's grew alongside the community to meet the complexities and challenges of delivering quality health care—leading the way with firsts in cardiac, cancer, maternity, pediatrics, and emergency care services.
Celebrating 125 years, St. Joseph's Medical Center is proud to serve the Stockton community. For more information, please visit dignityhealth.org/stockton.




38 SAN JOAQUIN PHYSICIAN SPRING 2024


15th Annual St. Joseph’s Fun Run/Walk for Wellness Exceeds Goal, Aiding in Purchase of New Breast Cancer Diagnosis Equipment
The 15th annual St. Joseph’s 5K Fun Run/Walk for Wellness was held on January 27, 2024, and with the generous support of the community, they exceeded their $110,000 goal, raising $110,536 in 2024.
Each year, funds raised from the Fun Run/Walk for Wellness goes to a specific need at St. Joseph’s, keeping all donations local to the Stockton community. In 2024, revenue from the event will aid in purchasing St. Joseph’s Cancer Institute’s new breast cancer diagnosis equipment, a Pristina Serena 3D Biopsy Unit.
“With the continued support of our local community through the Fun Run/Walk for Wellness, we are able to make incredible strides in providing the latest equipment and technology upgrades at St. Joseph’s Cancer Institute to help improve the overall health of the San Joaquin community,” said Julie Eckardt-Cantrall, VP and Chief Philanthropy Officer with St. Joseph’s Foundation of San Joaquin.
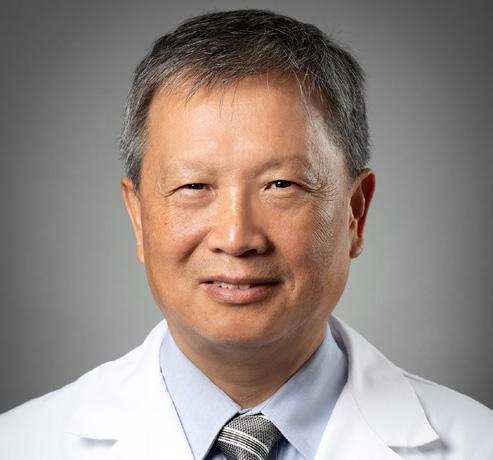
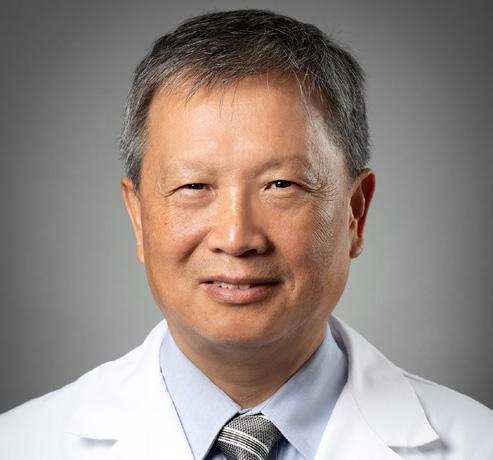
Dameron Hospital Welcomes Dr. Minghui Liu, Cardiothoracic and Vascular Surgery
Dameron Hospital welcomes Minghui Liu, MD, PhD, an experienced cardiothoracic and vascular surgeon, who recently joined the Dameron Hospital Cardiac Surgery Program.
Dr. Liu comes to Dameron from Central Valley Medical Group, a well-established cardiothoracic and vascular practice in Modesto, California, where he has been practicing since 2011. He completed his cardiothoracic surgery residency at UC Davis Medical Center and his general surgery residencies at Lahey Clinic Medical Center in Burlington, Massachusetts and Oregon Health & Science University in Portland, Oregon. Dr. Liu also earned his cardiothoracic surgery fellowship from the StarrWood Group of Cardiothoracic Surgery at St. Vincent Hospital and Medical Center in Portland, Oregon.
With 30 years of experience that includes performing more than 5,000 complex cardiac, thoracic and vascular surgery procedures, his expertise across several surgical specialties has established him as a sought after, highly respected surgeon in the Central Valley.
Referrals can be made by contacting the AHPN Stockton Surgical Specialties Department at Dameron at 209-242-7098 or by fax at 209-461-7579.
SPRING 2024 SAN JOAQUIN PHYSICIAN 39
2024 Fun Run/Walk for Wellness
Minghui Liu, MD, PhD
IN THE NEWS
Adventist Health Lodi Memorial and Dameron Hospital Receive Get With The Guidelines ® Stroke Awards
Adventist Health Lodi Memorial and Dameron Hospital both received the American Heart Association/American Stroke Association’s 2023 Get With The Guidelines®-Stroke Gold Plus Quality Achievement Award.
The prestigious awards recognize both hospitals’ commitment to ensuring stroke patients receive the most appropriate treatments, according to nationally recognized, research-based guidelines.
To receive the Gold Quality Achievement award, Adventist Health Lodi Memorial had to receive 85 percent or higher adherence to all Get With The Guidelines-Stroke achievement indicators for at least 24 consecutive months. The Gold Plus Quality Achievement is an even more advanced level of recognition, acknowledging the hospitals’ consistent compliance with quality measures.
Adventist Health Lodi Memorial earned further recognition for Target: Stroke Honor Roll Elite, which means 75 percent or more of acute ischemic stroke patients who were treated with IV tPA, received thrombolytic therapy within 60 minutes.
Additionally, both hospitals received the Association’s Target: Type 2 Diabetes Honor Roll award. To qualify for this recognition, hospitals must meet quality measures developed with more than 90 percent of compliance for twelve consecutive months for the “Overall Diabetes Cardiovascular Initiative Composite Score.”
Providing staff, physicians, and patients with relevant & up to date information
Adventist Health Lodi Memorial and Dameron Hospital receive Geriatric Emergency Department Accreditation
Adventist Health Lodi Memorial and Dameron Hospital have achieved Geriatric Emergency Department Accreditation from the American College of Emergency Physicians. This accreditation means that the hospitals’ emergency services are equipped with the necessary expertise, resources and staff to provide excellent care, specifically tailored to older patients. “As we see a rise in our geriatric population in the coming years, it is of the utmost importance that our hospitals can provide the highest level of specialized care to our community’s elders,” says Adventist Health Lodi Memorial president Brooke McCollough. “This accreditation is a testament to both Emergency Departments’ unwavering commitment to elevating the standard of care for our elderly, ensuring their well-being and dignity are upheld throughout their healthcare journey.
To achieve accreditation, emergency department staff focused on standardizing approaches to care for common geriatric issues; ensuring optimal transitions of care from the emergency department to other settings, including inpatient units, home or rehabilitation and long-term care centers; and accomplishing a series of geriatric-focused quality improvements.
Older adults visit the emergency department at higher rates than other age groups and often arrive with multiple chronic conditions. Seniors who visit hospitals accredited by the American College of Emergency Physicians can be confident that they have enhanced staffing, education and geriatricfocused policies and protocols to provide appropriate care and help get older patients back to their daily lives after an emergency occurs.
40 SAN JOAQUIN PHYSICIAN SPRING 2024
In The News

Medical Malpractice insurance for CMA members
About Medical Malpractice
Medical Malpractice insurance is crucial in protecting your practice and livelihood. Beyond paying the high cost of legal fees and judgments, Medical Malpractice insurance from the CMA Insurance Program, administered by Lockton Affinity, includes many benefits:
Coverage for common practice activites
Specialized customer service support
Regular updates from Lockton Affinity
Tailored coverage for all practice types
Medical Malpractice FAQs
What is the difference between Medical Malpractice and Professional Liability coverage?
• These policies are the same coverage with different names. This coverage may also be referred to as Errors and Omissions or E&O.
Do I need a separate policy if I am working at multiple locations?
• Malpractice coverage follows you wherever you work, so there is no need to have a separate policy.
How do I get a quote and apply for Medical Malpractice coverage?
• Contact Lockton Affinity’s team of highly trained, licensed insurance professionals.

SPRING 2024 SAN JOAQUIN PHYSICIAN 41
Scan the QR code to protect your practice today or contact Lockton Affinity's team directly at Info@LocktonAffinityCMA.com or (800) 278-8130. The CMA Insurance Program is administered by Lockton Affinity, LLC d/b/a Lockton Affinity Insurance Brokers LLC in California #0795478. Coverage is subject to actual policy terms and conditions. Policy benefits are the sole responsibility of the issuing insurance company. The California Medical Association will receive a royalty fee for the licensing of its name and trademarks as part of the insurance program offered to the extent permitted by applicable law. Not available in all states.
IN THE NEWS
“We are incredibly proud to provide two locations in San Joaquin County that are ready and able to provide leading geriatric care,” says McCollough. “While we hope they never need emergency care, we hope our older neighbors can rest a little easier knowing that quality care is available, close to home.”
Health Plan of San Joaquin/Mountain Valley Health Plan appoints Liz Le as new Chief Operations Officer
Health Plan of San Joaquin/Mountain Valley Health Plan (HPSJ/ MVHP) announced that Liz Le joined the organization as Chief Operations Officer (COO). Le brings a wealth of experience as an accomplished and forward-thinking health care leader. Her extensive background includes operations and progressive management, which encompasses program implementation and development; provider network management, expansion, and contracting; member enrollment and outreach; delegated plan services; regulatory program audits; and government contracts compliance.
For over 20 years, Le has held several key roles at Optum/United Health Group and CalOptima. Among her notable achievements, Le oversaw the development and implementation of Optum/United Health Group’s CalAIM program. During her tenure at CalOptima, she led the health plan’s Network Management efforts to successfully launch the Health Homes Program and Whole-Child Model program.
Le’s impact extends to her significant contributions to the establishment of CalOptima’s Program for All-Inclusive Care and Cal MediConnect program, which is California’s Dual Eligible Demonstration Project. Additionally, Le served as a leading contributor for the launch of CalOptima’s Medicare Advantage Special Needs Plan for dual eligible members and the integration of the Long-Term Care Services program.
Providing staff, physicians, and patients with relevant & up to date information

Le stated, “I have always been interested in health care and that passion has continued throughout my career. I am grateful for the Medi-Cal and Medicare experience I have gained, particularly in regulations and operations. This role of COO allows me to apply my knowledge of government programs and utilize my experience with operations. I understand the member populations we serve because my family was served by the public health system. I am so grateful for the opportunity to make a difference in the service that we deliver to our members.”
In her new role, Liz will operationalize HPSJ/MVHP’s strategic initiatives and enhance opportunities to support our provider partners in the delivery of care as we continuously improve health access, quality, and equity for our members. This includes leading initiatives to broaden our provider network in San Joaquin and Stanislaus Counties, as well as in our new service areas of Alpine and El Dorado Counties.
42 SAN JOAQUIN PHYSICIAN SPRING 2024 In The News
Liz Le
Health Plan of San Joaquin/Mountain Valley Health Plan appoints Betty Clark as new Chief Legal and General Counsel Health Plan of San Joaquin/Mountain Valley Health Plan announced that Betty Clark joined the organization as Chief Legal and General Counsel.
With extensive healthcare legal experience, Clark has previously worked as an attorney for the Department of Managed Health Care (DMHC) and as in-house counsel for San Francisco Health Plan and Alameda Alliance for Health. She brings knowledge and expertise in health plan licensing, particularly related to the Knox-Keene Health Care Service Plan Act and contractual requirements for Medi-Cal managed care plans.
Throughout her career, Clark has served as a liaison between health plans and key stakeholders that include DMHC, Department of Health Care Services, Local Health Plans of California, and California Association of Health Plans. She has been involved in drafting amendments and material modifications to health plans’ Knox-Keene licenses, overseeing regulatory filings and reports, leading projects on the implementation of new statues and regulations, providing legal counsel on compliance issues, and advocating on behalf of health plans before regulatory agencies.
In her capacity as Chief Legal and General Counsel at HPSJ/MVHP, Clark is responsible for providing strategic and operational legal advice to the health plan’s executive team, their designees, and governing board, the San Joaquin County Health Commission. Clark’s role encompasses a broad spectrum of legal considerations, focusing on issues such as statutory and regulatory compliance, new business development, employment matters, risk exposure mitigation, and legal compliance. She will additionally oversee legal issues impacting HPSJ/MVHP, lead litigation and regulatory strategies, manage outside counsel, and support the organization in operationalizing newly enacted laws.
Clark holds a Juris Doctor with a Technological Innovation: Generating Economic Results (TI:GER) Program Certificate from Emory University School of Law in Atlanta, Georgia. She graduated from the University of California, Los Angeles, receiving a Bachelor of Science in Psychobiology with a Minor in Spanish. Clark is an active member of the State Bar of California and the California Society for Healthcare Attorneys.
Expressing enthusiasm for returning to her hometown, Clark

stated, “I grew up in Stockton, CA. I am excited to return to the place where I was raised give back to the community that was instrumental in shaping the person I am today.”
Kaiser Permanente Northern California Receives Nationally Recognized Health Equity Accreditation
Kaiser Permanente Northern California is being recognized by the National Committee for Quality Assurance (NCQA) for providing high-quality, equitable care.
The NCQA awarded Kaiser Permanente Northern California the Health Equity Accreditation, which focuses on building an internal culture that supports the organization’s external health equity work; collecting data that helps the organization create and offer language services and provider networks mindful of individuals’ cultural and linguistic needs; and identifying opportunities to reduce health inequities and improve care.
Kaiser Permanente Northern California’s Health Equity accreditation covers all lines of business including its Commercial HMO, Exchange HMO, Medicaid HMO, and Medicare HMO health care plans.
“As a health care organization, we are committed to providing culturally responsive, equitable care to our members, patients and the communities we serve,” said Carrie Owen Plietz, FACHE, president of Kaiser Permanente’s Northern California region. “We believe everyone should have access to high-quality, affordable health care. This is core to our mission, and we are continually working to reduce barriers and eliminate health care inequities.”
SPRING 2024 SAN JOAQUIN PHYSICIAN 43
Betty Clark
IN THE NEWS
Some of these efforts include:
• In 2022, a study published in the New England Journal of Medicine showed that Kaiser Permanente Northern California has eliminated colorectal cancer disparities between Black and white adults. This study looked at colorectal cancer screening participation, incidence, and death rates for Black and white KP Northern California members ages 50 to 75. The study covered a 19-year period in which our screening rate increased from approximately 40% to 80%.
• In 2022, Kaiser Permanente Northern California invested $1.1 billion in the health of the communities it serves in Northern California. A significant part of the investments supported access to quality care through participation in the Medi-Cal program and Medical Financial Assistance.
• Kaiser Permanente Northern California remains focused on addressing the root causes of health disparities, such as economic opportunity, affordable housing, health and wellness in schools, and a healthy environment.
• Kaiser Permanente embeds practices to identify and eliminate inequities across operations — from how we design buildings to how we conduct research and deliver care. Kaiser Permanente is dedicated
Providing staff, physicians, and patients with relevant & up to date information
to delivering culturally responsive care, with multilanguage outreach, call center staff fluent in more than 140 languages, and medical facilities uniquely focused on the needs of specific communities.
• Kaiser Permanente’s integrated care model, which provides both care and coverage, and our coordinated approach to delivering care make us a leader in addressing health disparities among our members and communities. Because Kaiser Permanente takes care of nearly all our members’ needs and records all patient care interactions in an electronic health record, Kaiser Permanente can identify health disparities among different groups.
• Kaiser Permanente employees and physicians reflect and embrace the diverse communities we serve. This allows Kaiser Permanente to provide culturally responsive, equitable care for our members and patients.
“Advancing health equity is a foundational commitment of Kaiser Permanente, because everyone deserves access to highquality health care,” said Maria Ansari, MD, FACC, chief executive officer and executive director of The Permanente Medical Group. “This NCQA accreditation reflects our ongoing commitment to creating and maintaining a culture focused on providing equitable care to our members and patients, which is essential to improving the health and wellbeing of the communities we serve.”
HAVE SOMETHING TO SHARE?
Send your files to lisa@sjcms.org one month prior to publication (February 1st for the Fall issue, May 1st for the Fall issue, August 1st for the Fall issue and November 1st for the Fall issue).
44 SAN JOAQUIN PHYSICIAN SPRING 2024
In The News



















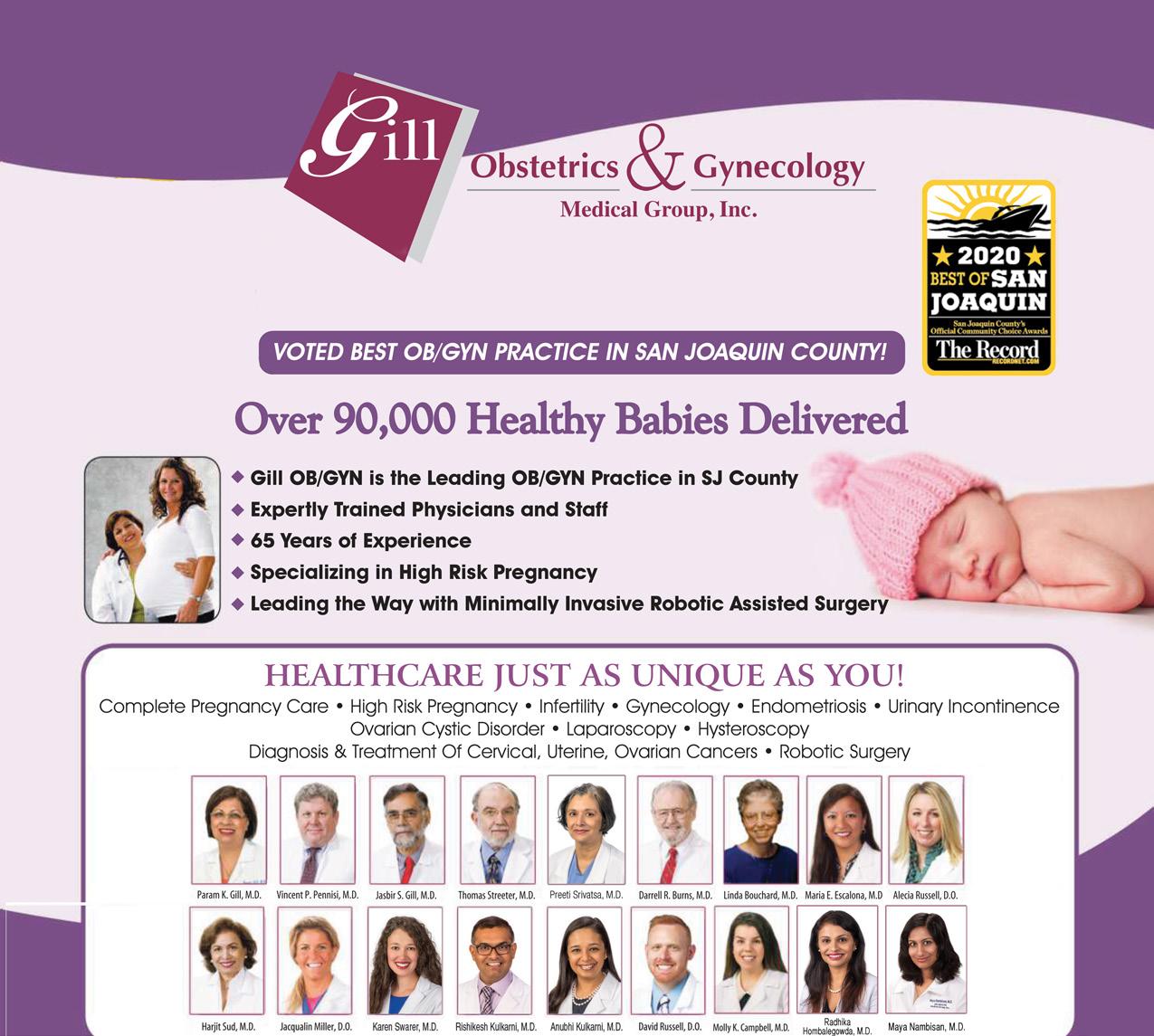
SPRING 2024 SAN JOAQUIN PHYSICIAN 45 GILLPRIMARYCARE.COM • ACCEPTING NEW PATIENTS Stockton Stockton Lodi 1503 E. March Lane, Suite A Phone: (209) 446-4455 123 S. Commerce Street, Suite D Phone: (209) 467-6825 835 S. Fairmont Avenue Phone: (209) 365-9331 THE KEY TO A BETTER YOU IS RIGHT NEXT DOOR. Dedicated to Family and Internal Medicine PROVIDERS Guido Abellera, M.D. Vincent B. Pennisi, M.D., Internal Medicine Dominic Pennisi, M.D., Internal Medicine Complete Women’s Healthcare HEALTHCARE JUST AS UNIQUE AS YOU! Complete Pregnancy Care • High Risk Pregnancy • Infertility • Gynecology • Endometriosis • Urinary Incontinence Ovarian Cystic Disorder • Laparoscopy • Hysteroscopy • Diagnosis & Treatment of Cervical, Uterine, Ovarian Cancers • Robotic Surgery Parampal K. Gill, MD Vincent Pennisi, MD Jasbir S. Gill, MD Darrell Burn, MD Maria Escalona, MD Jacqualin Miller, D.O. Alecia Russell, D.O. David Russell, D.O. Molly Campbell, M.D. Radhika Hombalegowda, M.D. James P. Maganito, D.O. Armita Bakhtmand, PA-C Magegan Sakhizada, PA-C
RESID ENTS' REPORT

A PLACE FOR ALL NEWS HIGHLIGHTING RESIDENTS AND GRADUATE MEDICAL EDUCATION

The Resident’s Report is dedicated to all the good news related to our hard-working residents training at San Joaquin General Hospital and St. Joseph’s Medical Center. Please email your submissions, written in third person with accompanying photo to Lisa@sjcms.org.

46 SAN JOAQUIN PHYSICIAN SPRING 2024

THE SAN JOAQUIN MEDICAL SOCIETY WAS PROUD TO HOST RESIDENTS FROM SAN JOAQUIN GENERAL HOSPITAL AND ST. JOSEPH’S MEDICAL CENTER AT THE ANNUAL HOLIDAY PARTY.
IT WAS A FESTIVE EVENING OF NETWORKING, FELLOWSHIP AND FUN!

SPRING 2024 SAN JOAQUIN PHYSICIAN 47
Practice News and Resources
Free to SJMS/CMA Members!

The Office Managers Forum empowers physicians and their practice manager staff with valuable tools via expert led education sessions from industry professionals who are committed to delivering quality healthcare. This quarterly forum is normally held on the second Wednesday of March, June, September and December at Papapavlo's in Stockton.
Registration is required!
If you don’t receive an invitation via E-Mail, please email Jessica@sjcms.org
48 SAN JOAQUIN PHYSICIAN SPRING 2024
March 13th, 2024: 11:00AM to 1:00PM
"2024 Employment Law Updates”

Discover how to navigate complex employment law changes and stay on track for a successful year. This will help businesses navigate California’s challenging employment and labor laws.
Jamie Bossuat, a shareholder and employment lawyer at Kroloff will present an update on the most pressing issues in employment law and will offer practical suggestions for reducing liability. Issues will include recent changes in wage and hour requirements, updates to leave of absence laws, and current litigation trends.
June 12, 2024: 11:00AM to 1:00PM
“Know Your Rights: How to Identify and Stop Unfair Payment Practices”

• Claim submission deadlines
• How much time does a payor have to pay my claim?
• What are the interest and penalty requirements for late payment?
• What are my appeal rights and how much time do I have to appeal?
• How do I get my contracted fee schedule?
• What are my rights regarding notices of overpayment?!
Mark Lane, Associate Director in the CMA’s Center for Economic Services, began his career as a claims processor for plans such as Blue
Shield and Health Net. Over the next 18 years, his experiences in claim operations, customer service, provider relations and contracting have allowed him to get a unique vantage point on the relationship between physicians and payors. Having experienced the physicianpayor relationship from both ends, Mark is able to understand the needs and positions of the respective sides, making him an ideal candidate to educate providers on overcoming the ever-changing challenges of the healthcare landscape.
CMA PRACTICE RESOURCES
CMS refreshes Open Payments data
UHC delays Designated Diagnostic Provider program in CA until Jan. 1, 2022
The Centers for Medicare & Medicaid Services (CMS) recently refreshed Open Payment to reflect changes to the data that have been made since the last update in June 2023. The updated dataset is now available for viewing at openpaymentsdata.cms.gov.
What is the Open Payments database?
Under federal law, drug and medical device manufacturers are required to report their financial interactions with physicians – including consulting fees, travel reimbursements, research grants and other gifts. Any payments, ownership interests and other “transfers of value” are reported to the Centers for Medicare and Medicaid Services (CMS) for publication in the public Open Payments database.
Open Payments data is updated twice a year in January and June. The prior year’s data is published initially by June 30, and physicians are able to preview the data attributed to them during a 45-day, pre-publication review and dispute period that runs from April 1 to May 15.
CMS then refreshes the Open Payments data in January to include updates from disputes and other data corrections made since the initial publication of the data.
The recently refreshed Open Payments Data Set includes:
Record Updates: Changes to non-disputed records made on or before November 15, 2023, are published.
SPRING 2024 SAN JOAQUIN PHYSICIAN 49
Disputed Records: Dispute resolutions completed on or before December 31, 2023, are displayed with the updated information. Records with active disputes that were not resolved by December 31, 2023, are displayed as disputed.
Record Deletions: Records deleted before December 31, 2023, were removed from the Open Payments database. Records deleted after December 31, 2023, remained in the database, but will be removed during the next data publication in June 2024.
Some Medicare telehealth claims not being paid correctly
Noridian—California’s Medicare Administrative Contractor—recently issued an alert about a Medicare system issue that has resulted in Place of Service 10 telehealth claims being priced at the facility rate regardless of the provider specialty. The Centers for Medicare and Medicaid Services (CMS) has indicated it is aware of the issue and is looking into the matter. As of now, there is no action needed. CMA will provide an update when additional information is available.
Feds finalize significant prior auth reform regulation
The Centers for Medicare and Medicaid Services (CMS) recently finalized comprehensive prior authorization reform regulations. These meaningful reforms apply to Medicare Advantage plans, state Medicaid and Children’s Health Insurance Program (CHIP) fee-for-service programs, Medicaid and CHIP managed care plans, and Qualified Health Plan issuers on the federally-facilitated Exchanges (FFE).
These regulations reflect the bipartisan legislation supported by the California Medical Association (CMA) and authored by California physician Congressman Ami Bera, M.D. and others – HR 3173/S 3108 “Improving Seniors’ Timely Access to Care Act” that unanimously passed the U.S. House of Representatives in September 2022 with more than 375 bipartisan House and Senate cosponsors.
The final rule requires electronic prior authorization processes, shortens the time frames to respond to prior authorization requests, requires the public reporting of certain prior authorization metrics and establishes policies to make the
prior authorization process more efficient and transparent.
The rule will require impacted payors (not including QHPs on the FFE) to send prior authorization decisions within 72 hours for urgent requests and seven calendar days for standard requests. For some payors, this new timeframe for standard requests cuts current decision timeframes in half. The rule also requires payors to include a specific reason for denying a prior authorization request, which will help facilitate resubmission of the request or an appeal when needed.
These operational or process-related prior authorization policies are being finalized with a compliance date starting January 1, 2026, and the initial set of metrics must be reported by March 31, 2026.
Other highlights of the final rule include:
-Allows payors to exempt physicians with a history of high prior authorization approval rates.
-Mandates appropriate and public clinical evidence to substantiate prior authorization decisions.
-Requires plans to establish Utilization Management Committees with physicians.
-Increases public transparency of approvals, denials, overturned decisions and response times.
CMS estimates that efficiencies introduced through these policies will save physician practices and hospitals over $15 billion over a 10-year period.
CMA will be working with the American Medical Association on federal legislation to achieve our remaining prior authorization goal – real time decisions. CMA also continues to support statelevel legislation to reform prior authorization, process to ensure that patients receive the care they need — when they need it.
50 SAN JOAQUIN PHYSICIAN SPRING 2024




Public Health Update
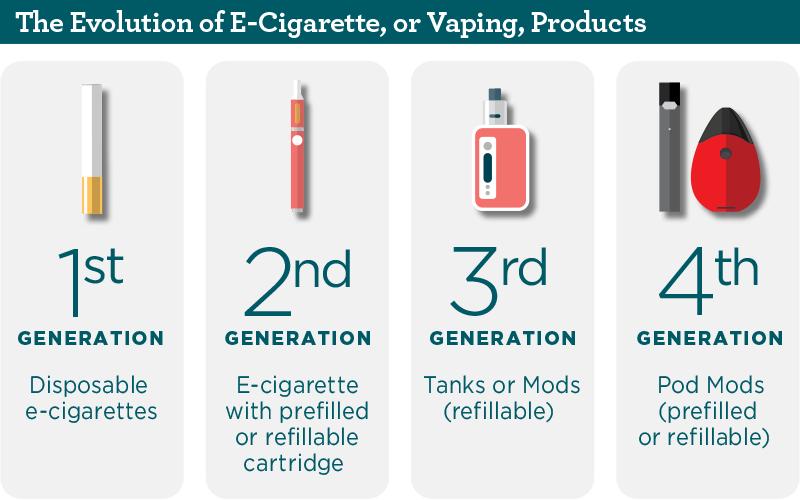
Unveiling the JUUL Settlement: Navigating the Complex Landscape of Youth Vaping
BY DEEPA SINGH, MPH, PUBLIC HEALTH EDUCATOR
A MAJOR VICTORY!
In September 2023, a $462 million multistate settlement agreement with electronic cigarette maker, JUUL Labs, Inc. (JUUL), was negotiated by the California Department of Justice (DOJ) and six other states: New York, Colorado, the District of Columbia, Illinois, Massachusetts, and New Mexico.1 This settlement comes after a two-year investigation into JUUL’s marketing practices attracting youth towards their e-cigarette products. 1 JUUL is now permanently prohibited from activities that include using cartoons
52 SAN JOAQUIN PHYSICIAN SPRING 2024

or persons under age 35 in advertisements, funding education programs and materials, targeting youth with direct or indirect marketing, using billboards to advertise, and using paid influencers to market products.2
On this monumental achievement towards a tobacco-free generation, California Attorney General Rob Bonta stated, “Today is another step forward in our fight to protect our kids from getting hooked on vaping and nicotine.” 1 Of the entire settlement, California will receive $175.8 million allocated toward funding research, education, and enforcement efforts related to e-cigarettes.
More locally, the City of Stockton in June 2023 passed an ordinance banning the sale of flavored tobacco products, prohibiting the proximity of new tobacco retailers to youthsensitive areas, and regulating the growth of smoke and vape shops in Stockton. Additionally, all businesses that sell tobacco products now need to obtain and maintain a valid local Tobacco Retail License (TRL). The ordinance adoption is a significant step toward strengthening California’s Senate Bill (SB) 793, which prohibits the sale of most tobacco products, e-cigarettes, and menthol cigarettes. Although SB 793 was passed in August 2020, Big Tobacco’s challenges resulted in Proposition 31, a ballot measure put forth to California voters in the November 2022 election. Upon passing, Proposition 31 upheld SB 793 and went into effect in December 2022. 3
VAPING IN YOUTH
JUUL devices are a type of e-cigarette, or vape, that has grown popular among youth. It is important to note that “vaping” is the act of heating chemicals from an e-cigarette/vaping device and breathing in the aerosol created by the process, which is not harmless water “vapor”.4 As a case in point, Stanford’s Tobacco Prevention Toolkit found that one JUUL pod (approx. 41.3 mg of nicotine) is equivalent to almost 41 cigarettes, or a little over two packs of cigarettes! 4
One out of five high school students reported that they used e-cigarettes in the past 30 days in 2020.5 Most youth credit the reason for trying an e-cigarette as “a friend used them”, and the most common reason for continuing to use e-cigarettes is “feeling anxious, stressed, or depressed.” 6
In examining data around vaping in youth, a 2023 school-based survey by the National Youth Tobacco Survey (NYTS) looked at both middle and high school students, and found that among youth who reported current use of e-cigarettes, more than one in four use e-cigarettes daily, and almost nine out of ten use flavored e-cigarettes. 7 Nationally, NYTS reported that there was a decline in current e-cigarette use among high school students from 14.1% to 10.0% in 2023. 7 It should be noted that e-cigarettes are still the most popular flavored tobacco product among youth. This indicates that public health and preventative healthcare measures are starting to work, but more actionable steps are still required to eradicate the use of e-cigarettes among youth.
SPRING 2024 SAN JOAQUIN PHYSICIAN 53
THE PHYSICIAN’S ROLE
When asked about the negative health effects of vaping on youth and what more healthcare providers can do, Dr. Maggie Park, San Joaquin County Public Health Officer, and boardcertified pediatrician, emphasizes that “nicotine in e-cigarettes is addictive, and along with the myriad of other chemicals found in these products, it can have lasting effects on developing brains. Clinicians need to understand that youth are being targeted by the tobacco industry and we need to do our best to make sure that our adolescents and young adults understand that vaping is not harmless. Even secondhand vape exposure puts our children at risk of brain, heart, and lung disease.”
EDUCATION IS THE KEY
You may have an adolescent patient who is using e-cigarettes or a parent who may be concerned about their child using them. The following resources are designed just for clinicians and can help you prepare to have these conversations.
Stanford Medicine’s Vaping Information, Solutions, and Intervention Toolkit (VISIT) provides comprehensive resources for providers on how to address vaping, prevention, and intervention in the clinical setting. VISIT was created for adolescent and young adult health professionals by clinicians, educators, and researchers. Review https://med.stanford.edu/ visit.html for more information regarding VISIT.
Kick IT California is a great resource to recommend to patients who are ready to quit vaping. Kick It CA will connect your patients with a “quit coach” who will work with them to create a personalized quit plan. Tell your patients to call 1-800-3008086 or text “Quit Smoking” to 66819 to get started. Refer patients to https://kickitca.org/
San Joaquin County Public Health Services Smoking and Tobacco Outreach/Prevention Program (STOPP) website is a resource to revisit often to get information on local activities and refer patients to more information about local and inperson cessation resources. Visit STOPP.sjcphs.org for more information.
The conversation doesn’t have to end here. If you are interested in joining the fight toward a tobacco-free community, learn how to get involved with the Coalition for Tobacco-Free San Joaquin by emailing stopp@sjcphs.org.
References:
Attorney General Bonta announces $462 million Multistate settlement with e-cigarette maker Juul. State of California - Department of Justice - Office of

the Attorney General. April 12, 2023. Accessed January 29, 2024. https:// oag.ca.gov/news/press-releases/attorney-general-bonta-announces-462million-multistate-settlement-e-cigarette.
Juul Settlement - Wisconsin Department of Health Services. Accessed January 29, 2024. https://www.dhs.wisconsin.gov/publications/p03445.pdf.
Long J. 11/9/22 - Proposition 31 in California Passed! Now What? | Public Health Law Center. www.publichealthlawcenter.org. Published November 9, 2022. https://www.publichealthlawcenter.org/ commentary/221109/11/9/22-proposition-31-california-passed-nowwhat
Vaping Information SIT. The Essentials. Vaping Information, Solutions<br>& Interventions Toolkit. Accessed January 29, 2024. https://med.stanford.edu/visit/the-details/HealthEffects.html.
Youth and tobacco use. Centers for Disease Control and Prevention. November 2, 2023. Accessed January 29, 2024. https://www.cdc.gov/ tobacco/data_statistics/fact_sheets/youth_data/tobacco_use/index.htm
Tobacco product use and associated factors among middle and high school students - national youth tobacco survey, United States, 2021. Centers for Disease Control and Prevention. March 10, 2022. Accessed January 29, 2024. https://www.cdc.gov/mmwr/volumes/71/ss/ss7105a1.htm?s_ cid=ss7105a1_w.
Results from the Annual National Youth Tobacco Survey (NYTS). U.S. Food and Drug Administration. Accessed January 29, 2024. https://www. fda.gov/tobacco-products/youth-and-tobacco/results-annual-nationalyouth-tobacco-survey.
Image reference:
Photo credit: https://www.zcisd.org/apps/pages/index.jsp?uREC_ ID=364688&type=d&pREC_ID=2068845
54 SAN JOAQUIN PHYSICIAN SPRING 2024


SPRING 2024 SAN JOAQUIN PHYSICIAN 55
In Memoriam
DANIEL RICHARD FISHER, MD
1935 - 2023
On the morning of Friday, December 15th, 2023, Dr. Daniel Richard Fisher passed away in his sleep due to congestive heart failure. He is survived by his life partner of 20 years, Beverly Bradley, his children Steven Fisher, Alice Goodman, and William Fisher, his five grandchildren, and his two greatgrandchildren.
Daniel was born on July 6th, 1935, in Urich, Missouri to Daniel Frank Fisher and Rosemonde Geraldine Outwater. His family moved to Sandwich, Illinois. He trained and competed as a boxer, earning his Golden Gloves. He received his bachelor’s degree from Albion College in 1957 and continued his education to earn his medical doctorate at the University of Illinois at Urbana-Champaign in 1961.
While on a break from school, he met his future wife, Margaret Jane Lowden (later Jane Lowden Fisher) of Hinsdale, Illinois. They married in 1960 and had three children: Steven, Alice and William. They later divorced.
Daniel fulfilled his military service duty through the United States Public Health Service. He was initially based in New Orleans, where Steven was born. At the end of his service in New Orleans, the family moved to Albuquerque, where Daniel completed his internship and Alice was born.The family moved to San Francisco in 1960s, where Daniel completed his residency at the University of California at San Francisco. During his residency, Daniel visited his uncle Clarence and aunt Muriel in nearby Stockton; Daniel and Jane then decided to settle there in 1960’s.
In Stockton, Daniel initially worked at the San Joaquin County Hospital and later became part of the obstetrics and gynecology team working at both Dameron Hospital and St. Joseph’s Medical Center. While working at the county hospital, Daniel read about defibrillators, a new technology at the time, and had one built from parts he ordered through the mail. This was the first defibrillator at the county hospital, and it saved many lives.
Daniel was certified as a specialist by the American Board of Obstetrics and Gynecology in 1969 and admitted as a Fellow in the American College of Surgeons in 1971.
Throughout his practice, Daniel diligently researched emerging medical technologies and techniques, often becoming
an early adopter of them. He was quick to acquire an ultrasound machine and also adopted laparoscopic surgical techniques when these technologies emerged in the 1980s and 1990s.
Daniel also became an Assistant Clinical Professor in the Department of Obstetrics and Gynecology at the University of California at Davis in 1994 and was certified by the Medical Board of California as an Expert Medical Reviewer in 1996.

During the 1980s, Daniel became interested in the field of infertility and transitioned his practice away from obstetrics to focus more on this emerging field of medicine. He found tremendous personal satisfaction in helping couples who were having trouble conceiving a child to overcome their difficulties and to create the families they wanted.
Daniel was an avid skier and ski racer, earning a NASTAR gold medal in the early 1980s. He later enjoyed cycling and mountain biking. Daniel was also passionate about investing and he followed the markets and daily economic news with great interest.
After his divorce, Daniel moved to Reno, where he lived a largely solitary life. While on a ski trip in Sun Valley in 2003, Daniel met Beverly Bradley. He fell deeply in love, moved to her home in San Diego and spent the rest of his life with her.
After struggling with issues in his lumbar vertebrae, an irregular heartbeat and neuropathy in both of his feet, Daniel finally succumbed to congestive heart failure. He valued love above all else in life – not only the love between friends and family, but also the universal love shared by all people. He also placed great value on both health and education. And he valued freedom – most of all, the freedom from fear, an emotion which he saw as the polar opposite of love. For many years, he maintained a license plate that read LIVFREE as an encouragement to all.
56 SAN JOAQUIN PHYSICIAN SPRING 2024
In Memoriam
21
NEW SJMS MEMBERS THIS WINTER! ...and even more on the way.
Syed Umer Ali, MD
Cardiovascular Disease
2800 N California St, Ste 14A Stockton, CA 95204
AGA Khan University, 2009
John Zeiter Jr., MD
Opthalmology
255 E Weber Avenue Stockton, CA 95202
Baylor College of Medicine, 2017
Andrew Fong, MD
Pathology
2131 N California Street Stockton, CA 95204
Wright State University
Boonshoft, 2015
Glenmore Lasam, MD
Cardiovascular Disease
415 E Harding Way, Ste D Stockton, CA 95204
Cagayan State University, 2000

Ali Reza Mirhosseini, MD
Cardiovascular Disease
415 E Harding Way, Ste D Stockton, CA 95204
Shiraz University of Medical Sciences, 2005
Nadia Shaikh, MD
Cardiovascular Disease
415 E Harding Way, Ste D Stockton, CA 95204
University of Massachusetts, 2014
Haytham Aljoudi, MD
Cardiovascular Disease
1801 E March Ln, Ste D400 Stockton, CA 95210
University of Jordan, 2001
Bader Abu Ghalyoun, MD
Cardiovascular Disease
1801 E March Ln, Ste D400 Stockton, CA 95210
University of Jordan, School of Medicine, 2003
Sandeep Mann, MD
Addiction Medicine
2216 N California St., Ste A Stockton, CA 95204
American University of the Caribbean
Minghui Liu, MD
Cardiovascular Surgery
530 W Acacia St., #1 Stockton, CA 95203
Hunan Medical University
Chude Anagor, MD
Internal Medicine
200 Mission Blvd
Jackson, CA 95642
University of Nigeria College of Medicine
Olexander Barchan, MD
200 Mission Blvd
Jackson, CA 95642
French Camp, CA 95231
Kiev Medical Institute
SPRING 2024 SAN JOAQUIN PHYSICIAN 57
New Members
21 NEW SJMS MEMBERS THIS WINTER! ...and even more on the way.

Nanying Li, MD Internal Medicine
200 Mission Blvd Jackson, CA 95642
Guangzhou Medical Univ, China
Chrystal Rhea, DO Family Medicine
200 Mission Blvd Jackson, CA 95642
Kansas City Univ of Medicine & Biosciences
Prabjit Singh, MD Internal Medicine
200 Mission Blvd Jackson, CA 95642
Baba Farid University of Health Sciences
Felicia Tang, MD Family Medicine
9279 Locust St Plymouth, CA 95669
CASE Western Reserve University School of Medicine
Sunil Kumar Thaghalli Siddegowda, MD Internal Medicine
200 Mission Blvd Jackson, CA 95642
Kempegowda Institute of Medical Sciences
Erik Wiele, DO Family Medicine
200 Mission Blvd Jackson, CA 95642
Touro University College of Osteopathic Medicine
Christopher Li, MD Urology
1789 W Yosemite Manteca, CA 95337
Boston University Medical Center
Suma Nagaraj, MD Pediatrics
2185 W Grant Line Rd Tracy, CA 95377
Karnataka Institute of Medical Sciences
Christopher Doria, MD
Pediatrics
7373 West Lane
Stockton, CA 95210
French Camp, CA 95231
Fac of Medical Surg-University of Santo Tomas
58 SAN JOAQUIN PHYSICIAN SPRING 2024
New Members


• Complimentary Dark Web Compromise Credential Report
✓ Over 11 billion accounts have been compromised – Has yours?
• Complimentary Phone System Assessment
✓ Is your phone bill higher than you would like? Does your phone system allow you to work from anywhere?
• Complimentary Security and Risk Assessment
✓ Have you conducted you r Risk Assessment yet? Call Mark Williams @ 209-623-1023 or email mark@ce-technology.com
SPRING 2024 SAN JOAQUIN PHYSICIAN 59
Member
Benefits
San Joaquin Medical Society
Only
RETURN SERVICE REQUESTED

True to our mission, we are improving access for people who qualify for Medi-Cal.
HPSJ is proud of the reputation we have built from strong community partnerships and a commitment to preserving the safety net of providers who provide quality health care to our diverse population with growing needs.
As we kick off a new year, we are setting out to build on HPSJ’s foundation and are prepared to engage in new initiatives that will improve quality, address health inequities, and ensure that members receive access to the best care possible. We will accomplish this through a framework that focuses on:
Operational Excellence and Growth
Skilled and Stable Workforce
Community Partnerships
Financial Stewardship
Take a look at our 2023-2026 Strategic Roadmap for opportunities to partner and collaborate toward achieving a vision of equitable access to quality care.

As of January 1, 2024, we have expanded our service area to El Dorado and Alpine counties as Mountain Valley Health Plan (MVHP).
Our team at HPSJ/MVHP remains more committed than ever to partnership, community, and wellness.
60 SAN JOAQUIN PHYSICIAN SPRING 2024 San Joaquin Medical Society
W. March Lane, Suite 222W Stockton, California
3031
95219-6568
PRSRT STD. U.S. POSTAGE PAID Permit No. 60 Stockton, CA
(7526) www.hpsj-mvhp.org
1-888-936-PLAN























 Lisa Richmond
Lisa Richmond