



Poor documentation during intake resulted in a





Poor documentation during intake resulted in a
causing permanent damage to a good knee.

The Joint Commission data reveals that wrong-site incidents are the fourth most frequently reported sentinel event.
To minimize surgical errors, practices insured by ProAssurance can access annual risk assessments to learn how well their surgical teams and protocols are working. Risk consultants gather and review the data, note potential weak spots, and deliver recommendations based on former claims.
Helping our insureds assess their patient safety procedures and sharing strategies learned from our closed claims history helps them mitigate risk and be prepared if they ever need to face a malpractice claim.

PRESIDENT Cyrus Buhari, DO
PRESIDENT ELECT Neelesh Bangalore, MD
TREASURER Sujeeth Punnam, MD
BOARD MEMBERS Stephen Tsang, MD, Maggie Park, MD, Alain Flores, MD, Manreet Basra, MD, Sanjeev Goswami, MD, Kinnari Parikh, MD, Inderpreet Dhillon, MD, Bhagya Nakka, MD, Sunny Philip, MD, and Ripudaman Munjal, MD
MEDICAL SOCIETY STAFF
EXECUTIVE DIRECTOR Lisa Richmond
MEMBERSHIP COORDINATOR Jessica Peluso
COMMITTEE CHAIRPERSONS
CMA AFFAIRS COMMITTEE Larry Frank, MD
DECISION MEDICINE Kwabena Adubofour, MD
MEDICAL EDUCATION PROGRAMS Kelly Savage, MD
SCHOLARSHIP LOAN FUND Gregg Jongeward, PhD
CMA HOUSE OF DELEGATES REPRESENTATIVES
Robin Wong, MD, Lawrence R. Frank, MD
James R. Halderman, MD, Raissa Hill, DO
Richelle Marasigan, DO, Ramin Manshadi, MD
Philip Edington, MD , Sujeeth Punnam, MD
Sunny Philip, MD, Ripudaman Munjal, MD
SAN JOAQUIN PHYSICIAN MAGAZINE
EDITOR Lisa Richmond
EDITORIAL COMMITTEE Lisa Richmond, Cyrus Buhari, DO
MANAGING EDITOR Lisa Richmond
CREATIVE DIRECTOR Sherry Lavone Design
CONTRIBUTING WRITERS Jo Ann Kirby, Cyrus Buhari, DO, Jessica Freeman, MPH
THE SAN JOAQUIN PHYSICIAN MAGAZINE is produced by the San Joaquin Medical Society
SUGGESTIONS, story ideas are welcome and will be reviewed by the Editorial Committee.
PLEASE DIRECT ALL INQUIRIES AND SUBMISSIONS TO: San Joaquin Physician Magazine
3031 W. March Lane, Suite 222W Stockton, CA 95219
Phone: (209) 952-5299 Fax: (209) 952-5298
E-mail Address: lisa@sjcms.org
MEDICAL SOCIETY OFFICE HOURS:
Monday through Friday 8:30am-4:30pm
Closed for Lunch between 12pm-1pm



In early April SJMS physicians attended the 50th Annual California Medical Association’s (CMA) Legislative Advocacy Day in Sacramento. The event brought together over 400 physicians, medical students, and resident members from across the state to advocate for important health care issues affecting Californians. In addition to hearing from physician leadership and keynote speaker, SJMS representatives met with our local legislators at the Capitol to discuss issues such as protecting historic investments in Medi-Cal, critical prior authorization reform and CMA’s sponsored bill to institute guardrails on the use of artificial intelligence. The energy and passion were palpable through the sea of white coats in the room, and along our walk over to the Capitol.

Although we understand the difficulty in taking time out of your busy practice, there is no one better suited to advocate for the medical profession and patients, than physicians. We will need all hands-on deck as the California Medical Association and the Coalition to Protect Access to Care, a broad and diverse group of health care organizations, have submitted enough signatures to qualify a statewide ballot initiative for the November 2024 ballot that will expand access to health care for millions of Californians. More information about this initiative is included in this issue.
SJMS has remained steadfast in its commitment to encouraging and assisting the bright, talented youth of our community to pursue a career in medicine via our Decision Medicine (DM) pipeline program. This year, the committee scored 98 applications before interviewing 40 students and ultimately selecting the final 24 in the class of 2024. A huge thank you to Drs. George Khoury, Hyma Jasti, Kwabena Adubofour, Lily Pang Marina Castillo, Neelesh Bangalore, Stephen Tsang, and Vanessa Armendariz (DM ’05) for their engagement in this process. We welcome new volunteers for both our Bridge to Medicine and Decision Medicine programs. Contact me at Lisa@sjcms.org for more information.
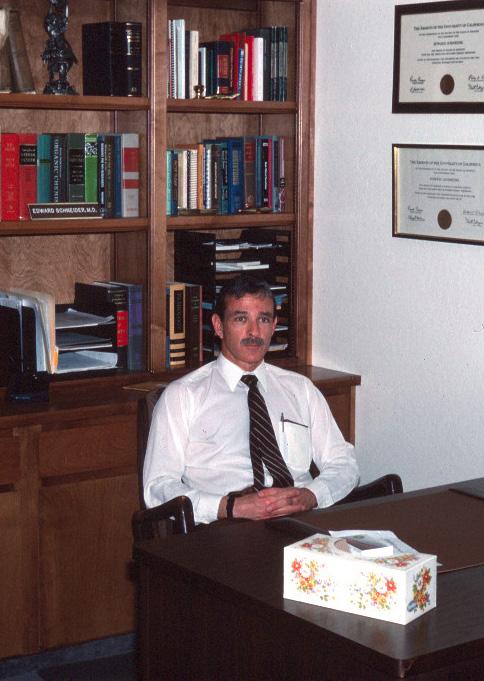
We are looking forward to our June 9 membership dinner honoring the 2024 Young Physician and Lifetime Achievement award recipients, Drs. Adnan Khan of San Joaquin Cardiology and retired family physician, Edward Schneider. We know you’ll enjoy learning more about them personally and their dedication to their patients, colleagues, and community! Additionally, we will celebrate the passing of the gavel from Cyrus Buhari, DO to Neelesh Bangalore, MD. We are so grateful for Dr. Buhari’s leadership and commitment to the medical society and his extended, two-year term as president. Hope to see you there. : -)
Have a wonderful summer, Lisa Richmond

Your heart might be something you’ve always taken for granted. But it’s the whole reason we’re here. St. Joseph’s Medical Center is one of the nation’s 50 Top Cardiovascular Hospitals, bringing not only clinical expertise, but a passion to heal. We are renowned for our advanced diagnostic and treatment options, supported by comprehensive rehabilitation services that help get patients back to feeling their best. From routine checkups to lifesaving procedures, our team has the expertise and the dedication to care for your heart—and the person around it. Learn more about our innovative services at dignityhealth.org/stockton/heart.


Fram Buhari, DO is the
current president of the San Joaquin Medical Society and practices at the San Joaquin Cardiology Medical GroupMy tenure as President of the San Joaquin Medical Society is at an end. I am now making the transition to immediate-past president. The SJMS staff used pliers to pry the gavel from my unwilling hand in order to pass it to the incoming President, Dr. Neelesh Bangalore. My last article stated how honored I have been to lead one of the oldest medical societies in California. I look at the wall of past presidents and am shocked to see my own face wearing a suit and tie. This society has been led by distinguished physician leaders throughout its over 150-year history. It is truly something for all our physician community to be proud of. The SJMS along with the California Medical Association work diligently to support physician practices and healthcare in our community. This joint effort is on full display every political season. Unfortunately, the California legislature often tries to inject themselves between doctors and patients in an effort to pass headline-grabbing laws and regulations. They are often misguided and have so many unintended consequences that they must be constantly amended. Often this is despite and not along with advice from physicians.
During my 2 years as president of the SJMS there have been efforts to fight infringement on our scope-of-practice, streamline the prior authorization process, stave off cuts in vital Medi-Cal programs, and preserve access for our aging Medicare population. SJMS and CMA have had some successes and some challenges. We are constantly fighting to eliminate cuts to physician reimbursement that are built into very poorly thought-out budgets from the Federal Government. That fight seems endless and sometimes pointless, but we will continue to fight it and I urge all the physicians in our community to fight ridiculous cuts that will only serve to diminish access and care for the vulnerable of our community.
As teaching programs in our community expand to address the need for a stable for future young physicians and physician talent the San Joaquin Medical Society continues to answer the call to support by what resources they have available. We have seen the development and expansion of
programs in Surgery, Primary Care fields, and Specialty medicine. With a unified physician membership these programs will flourish and there will be no lack of resources to assist and guide our young physicians. A strong SJMS is a draw for graduating physicians to feel accepted into the community and they will feel as if their success is our goal as well.
The SJMS Board of Directors is stacked with talent. A very diverse group of physicians from our community, who are actively practicing and delivering care, represent the members of the SJMS. They represent not only the current members, but all physicians in our community and we strive to have them join us. The Board members’ participation and direction creates value for all of us and I continue to encourage the membership to try to expand. It is the only way that our voices can be heard and taken seriously. As a Board, we meet with legislators and candidates to discuss our interests and the interests of our patients. Some listen and
earn our support.
As one of the stewards of our fine San Joaquin Medical Society, I have confidence in the Board of Directors and the incoming President to grow the society’s membership and push forth its mission. Our Board looks like the membership… diverse, talented, and full of altruism. As this is my final opinion piece, I would like to thank the Board’s Executive Director, Lisa Richmond, and our Membership Coordinator, Jessica Peluso. They are the backbone of the Society and the key to its success, and I owe them a debt of gratitude for all they have done to ensure that my time on the Board was fruitful and meaningful. I will be the Immediate Past President of the San Joaquin Medical Society and I am very proud of what we have accomplished together and will continue to accomplish moving into the future.
Thank you all so very much.
-Cyrus Fram Buhari, DO

Doctors Hospital of Manteca offers:
• 24-Hour Emergency Care and Convenient Online Check-Ins
• 24/7 Critical Care Coverage Led by Intensivists
• Bariatric Center of Excellence
• Blue Distinction Center for Hip and Knee Replacement
• Imaging Services, Including Open MRI and PET/CT
• Surgical Services
• Women’s Health, Including 3-D Mammography
• Wound Care Center
From emergencies and screenings to surgical and procedural services, Doctors Hospital of Manteca delivers quality healthcare and compassionate care close to home. To refer a patient, call
Physician practices are still in crisis and continue to experience issues with multiple operations due to the Change Healthcare cyberattack, according to the American Medical Association’s (AMA) most recent follow-up survey on the impact of the cyberattack outages.
The findings of the survey, which was conducted from April 19 to April 24, 2024 and included responses from California physicians, dispute UnitedHealth Group’s claim that their systems are nearly back to their pre-cyberattack levels and claims are again flowing.
Specifically, the survey of physician practices found that:
85% continue to experience disruptions in claim payments
79% still cannot receive electronic remittance advice
75% still face barriers with claim submission
63% are losing revenue due to the inability to charge patient co-pays or remaining obligation
60% continue to face challenges in verifying patient eligibility
Survey respondents continue to experience significant financial strain from the cyberattack fallout, with 62%
reporting that they used personal funds to cover practice expenses, 42% unable to purchase supplies, and more than a third reporting that they are unable to meet their payroll obligations following the cyberattack.
Physician practices are reminded that temporary funding assistance is available to those affected by the Change Healthcare cyberattack. Assistance is available in the form of advanced payments from the Centers for Medicare and Medicaid Services (CMS), as well as short-term, no-cost loans from the Optum Temporary Funding Assistance Program. If you find that the funds available through the Optum “check funding eligibility” tool are insufficient, practices can submit a request through the “temporary funding assistance inquiry form” or contact Optum directly at (877) 702-3253.
The California Medical Association (CMA) is committed to supporting physician practices during this difficult time. We have developed a grid that lists a summary of known impacts, workarounds, and guidance from payors, which is available free to CMA members. CMA members can reach out to us at (800) 786-4262 or economicservices@cmadocs.org.
Additionally, the American Medical Association (AMA) has curated resources and provided tips for physicians and health care staff to protect patient health records and other data from cyberattacks.


pushes the bar pusheshigher the bar pusheshigher bar pusheshigher the bar pusheshigher the bar pusheshigher the bar pusheshigher the bar pusheshigher bar pusheshigher the bar bar pusheshigher the the bar pusheshigher the bar pusheshigher the bar pusheshigher pusheshigher the bar pusheshigher the bar pusheshigher the the bar pusheshigher bar pusheshigher the bar pusheshigher the bar pusheshigher pusheshigher the bar pusheshigher bar pusheshigher the bar the bar pusheshigher bar pusheshigher the bar pusheshigher the bar pusheshigher the pusheshigher the bar pusheshigher bar pusheshigher bar pusheshigher the bar pusheshigher the bar pusheshigher the bar pusheshigher bar pusheshigher the pusheshigher bar pusheshigher pusheshigher the bar the bar pusheshigher the the bar pusheshigher bar pusheshigher the bar pusheshigher the bar pusheshigher pusheshigher the bar pusheshigher bar pusheshigher the pusheshigher bar pusheshigher the bar pusheshigher the bar pusheshigher bar pusheshigher the pusheshigher the bar pusheshigher the bar pusheshigher the bar pusheshigher bar pusheshigher the bar pusheshigher the bar pusheshigher the the bar pusheshigher bar pusheshigher the bar the bar pusheshigher pusheshigher the bar pusheshigher the bar pusheshigher the the bar pusheshigher bar pusheshigher the bar pusheshigher the bar pusheshigher the pusheshigher the bar bar higher

Dr. Adnan Khan, medical director for the Cardiac Catheterization Laboratory at St. Joseph’s Medical Center and an interventional cardiologist with San Joaquin Cardiology Medical Group, hadn’t even turned 40 when he learned he was chosen as the recipient of the San Joaquin Medical Society’s Young Physician Award. From his early years, he established himself as a goal setter who always challenges himself to a new intention once he has completed an objective.
He has achieved great success in a relative short amount of time since completing his internal medicine residency in 2014 and the second of two specialized cardiology fellowships in 2018, all at the University of Texas Medical Branch in Galveston, Texas.
For a teen who immigrated to the United States from Pakistan at the age of 16, his singular focus was obtaining the education he needed to become a successful cardiologist. That meant making up a lot of credits in order to graduate high school. “I went to Delta College before transferring to UC Davis, and there was no discernable difference in instruction,” he said. “Delta was very convenient and affordable, just a short drive for me, which meant more time I could dedicate to studying. If they had offered a bachelor’s degree, I would have stayed.”

He was laser focused on becoming a cardiologist. “There was extreme clarity in my mind. I always knew what I wanted to do,” he said.
Dr. Khan said one unique obstacle he endured was the fact that no one among his family or friends were in the medical field. “I didn’t have anyone to guide me. I had to figure out each step on my own or ask the counselor for help. The Delta College counselor helped me a lot and I utilized that resource. I just kept working towards the next stop in my journey.”
He is very close to his parents and siblings, he and his wife, Mahrukh , whose name means “moonlight” along with their daughters Namal and Suhan, and son Muhammad, live with his extended family in north Stockton. “My parents supported me a lot, also my brother was a great moral and financial support to me. He is two years older than me and was working full-time,” he said of his family’s help while he was studying his way through college, medical school, residency and subsequent fellowships. The ever-changing
profession means that he is still studying. His research with colleagues has been published and he is constantly looking to improve the outcome of his patients. His next innovative goal is to establish a cardiogenic shock team at St. Joe’s. Such a team could help with the immediate evaluation and treatment of cardiogenic shock patients when their heart is unable to pump enough blood to meet the needs of their body. Khan said another mission is to add an interventional cardiology fellowship. It all adds up to improved patient care for the local community.
Friends and colleagues say Dr. Khan is deserving of this Young Physician of the Year accolade and it is one of a half dozen he has received in his career, including the George R. Herrmann Scholarship Award he received as Cardiology Fellow of the Year.
“He is whole heartedly serving patients in this community for the last six years, providing top-notch cardiac care,” Dr. Muhammad Choudhry, a colleague at San Joaquin Cardiology Medical Group who has known Dr. Khan since
their cardiology fellowship training days in Texas, said.
Dr. Cyrus Buhari, who nominated Dr. Khan, says he is an absolute fixture in the community in terms of caring for heart patients. “He worked very hard to become the cardiac cath lab director at St. Joseph’s Medical Center and his opinion is always highly valued. He has successfully brought multiple new technologies to our community on the interventional side.”
Khan was finishing up with his interventional cardiology fellowship in Texas when the partners at San Joaquin Cardiology Medical Group recruited him six years ago.
“Other physicians could learn a lot from Dr. Khan. They can learn to always act professionally in every meeting and in every interaction with other physicians and with patients,” Dr. Choudhry said. “His opinions are all well thought out and measured. He always has the best interest of the patient in mind.”
Dr. Khan is also a man of deep faith as a practicing Muslim. “I actually went to Saudi Arabia for two weeks. We went for the pilgrimage. My wife hadn’t done if and I wanted my kids to experience it,” he said. “It’s one thing to read about something, but it’s another thing to see it firsthand because it starts to make more sense and helps with your belief. I think my faith also helps me in my work.”
Dr. Khan enjoys playing cricket when he can. “He is a cricket fanatic,” Dr. Choudhry said, adding that he will even sneak peaks at cricket games on his phone during departmental meetings. He is also a basketball fan and enjoys taking his kids to the movies. The family man hopes to visit Hawaii or a historic place such as Turkey on their next vacation.
If he hadn’t been so laser focused on becoming a cardiologist, he said he might have wanted to be a fighter pilot “for the adrenaline rush.” However, as cardiologist, he practices visualization before a procedure — mentally walking himself visually through each step that will result in a successful outcome and reciting a prayer.
“One has to be humble, extremely humble,” he said. “I know in my mind how each step will go and what to do if there is a complication because things can take a turn for the good or the bad.”





Diagnosis

















your future with UC Davis Health


UC Davis Health is an extraordinary place to grow your career. You’ll experience being part of an academic medical center that’s committed to advancing pioneering research, promoting a sense of belonging through an inclusive work environment, and fostering continuous learning to develop health care leaders.

Join our team as we strive to provide world-class care in the Northern California region. Offering a competitive compensation and benefits package, flexible schedules, access to wellness programs, and more.

The California Medical Association (CMA) recently celebrated a milestone with its 50th Legislative Advocacy Day, held on April 10, 2024, in Sacramento. The event brought together over 400 physicians, medical students and resident members from across the state to advocate for important health care issues affecting Californians.
Attendees received updates from CMA President Tanya W. Spirtos, M.D., and CMA’s chief lobbyist Stuart Thompson, Senior Vice President of Government Relations, and Political Operations,
about key health care issues before the legislature this year. Attendees then lobbied their legislators in support of some of CMA’s priority issues, including:
• The protection of the historic investments in Medi-Cal in Governor Gavin Newsom’s proposed budget. These investments are vital for maintaining access to quality health care for all Californians. Physicians urged lawmakers to safeguard this funding and ensure its continued support through the legislative process.
• The critical need to reform the prior authorization process: CMA’s sponsored bill, SB 516, authored by Senator Nancy Skinner, aims to




address the challenges and delays caused by the current prior authorization system. Physicians shared personal stories and insights, highlighting the urgent need for reform to ensure timely access to care for patients.
• CMA’s sponsored bill to institute guardrails on the use of artificial intelligence (AI) in health care settings was also a central focus of meetings. Senator Josh Becker’s SB 1120, known as the “Physicians Make Decisions Act,” would require physician oversight of utilization review decisions made or assisted by a health plan’s AI decisionmaking tools or algorithms. Recent news reports have highlighted instances and allegations of health plans using AI algorithms to wrongly deny medically necessary care.
“CMA’s advocacy day provides a unique opportunity for physicians to directly influence health care policy and ensure that the voice of medicine is heard in Sacramento,” Thompson said. “Flooding the halls with white coats and meeting with legislators and their staff is a powerful
demonstration of the dedication and passion of California physicians.”
CMA CEO Dustin Corcoran also provided an update on the Protect Access to Healthcare Act, a ballot initiative filed by CMA and coalition partners that would permanently expand access to health care for millions of Californians who rely on Medi-Cal.
“By building on and making permanent the historic investments to Medi-Cal that the Governor and the Legislature made last year, we can ensure equitable access to care and allow physicians to take on Medi-Cal patient loads reflective of their communities,” Corcoran said.
As the legislative year progresses, CMA remains committed to advocating for policies that prioritize patient care and support physicians in providing the best possible health care for Californians.
Legislative Advocacy Day attendees also enjoyed hearing from keynote speaker California Senate President pro Tempore Mike McGuire, who commended CMA and its members for their dedication to improving health care in California.




AB 1070 (Low) – Physician Assistants: Physician Supervision: Exceptions
CMA Position: Neutral
Permits a physician and surgeon to supervise up to 8 physician assistants at one time if all the physician assistants are focused solely on performing in-home health evaluations to gather patient information and perform annual wellness visits or health evaluations that do not involve direct patient treatment or prescribing medication.
(Amends Business and Professions Code §3516)
AB 716 (Boerner) – Ground Medical Transportation
Requires the Emergency Medical Services authority to annually report the allowable maximum rates for ground ambulance transportation services in each county. Limits the amount an enrollee or insured owes a noncontracting ground ambulance provider to the in-network cost-sharing amount, and prohibits a ground ambulance provider from billing an uninsured or self-pay patient more than the established Medi-Cal payment or Medicare fee-for-service amount, whichever is greater. Prohibits a noncontracting ground ambulance provider from sending a higher amount to collections. Require a plan or insurer to directly reimburse a noncontracting ground ambulance provider for ground ambulance services the difference between the in-network cost-sharing amount and an amount described, as specified, unless it reaches another agreement with the noncontracting ground ambulance provider.
(Adds Health and Safety Code §§1371.56, 1797.124, and 1797.233; Repeals Health and Safety Code §1367.11; Adds Insurance Code §10126.66; Repeals Insurance Code §10352)
CMA Position: Support
Extends the Emergency Medical Services System and the Prehospital Emergency Medical Care Personnel Act until January 1, 2031. Expands the allowable community paramedicine services program specialties to include providing short-term, post discharge follow-up for persons recently discharged from a hospital due to a serious health condition, including collaboration with, and by providing referral to, home health services when eligible.
(Amends Health and Safety Code §§1797.273, 1815, 1834, 1836, 1841, 1842, and 1857)
Specifies that a licensed speech-language pathologist who holds a written verification that was issued before January 1, 2023, by a board-certified otolaryngologist stating that the licensed speech-language pathologist has performed a minimum of 25 supervised flexible fiber optic transnasal endoscopic procedures and is competent to perform those procedures, shall be deemed to meet specified requirements regarding flexible fiber optic transnasal endoscopic procedures, as provided.
(Amends Business and Professions Code §2530.2;
SB 43 (Eggman) –
CMA Position: Support Expands the definition of “gravely disabled” for purposes of either placing a person on an involuntary psychiatric hold or conservatorship. The new definition of “gravely disabled” includes individuals with either a severe substance use disorder or a co-occurring mental health disorder and a severe substance use disorder, and individuals who, due to a mental health disorder or one of the two above conditions, are unable to provide for their personal safety or necessary medical care.
(Amends Health and Safety Code §1799.111; Amends Welfare and Institutions Code §§5008, 5350, 5354, 5402; Adds Welfare and Institutions §5122)
SB 326 (Eggman) – The Behavioral
CMA Position: Support
If approved by the voters at the March 5, 2024, statewide primary election, this bill will recast the Mental Health Services Act (MHSA) renaming it the Behavioral Health Services Act (BHSA), expanding it to include treatment of substance use disorders, changing the county planning process, and expanding services for which counties and the state can use funds. This will revise the distribution of MHSA moneys, including allocating up to $36,000,000 to the department for behavioral health workforce funding.
(Amends, repeals, and adds Education Code §99277; Amends, repeals, and adds Health and Safety Code §131315; Amends, repeals, and adds Revenue and Taxation Code §19602.5; Amends, repeals, and adds Unemployment Insurance Code §1095.5; Amends Welfare and Institutions Code §§4090, 4094, 4096.5, 5675, and 5813.6; Amends and repeals Welfare and Institutions Code §§5840.5, 5840.8, 5846, 5847, 5848, 5878.2, 5895, and 5899; Amends, repeals, and adds Welfare and Institutions Code §§5604, 5604.1, 5604.2, 5604.3, 5604.5, 5610, 5613, 5614, 5664, 5771.1, 5805, 5806, 5813.5, 5830, 5835, 5835.2, 5840, 5840.6, 5840.7, 5845, 5845.5, 5848.5, 5849.1, 5849.2, 5849.3, 5852.5, 5868, 5878.1, 5878.3, 5881, 5886, 5890, 5891, 5891.5, 5892, 5892.1, 5892.5, 5893, 5897, 5898, 14197.7, and 14707.5; Adds Welfare and Institutions Code §§5831, 5845.1, and 14197.71; Adds Welfare and Institutions Code Part 4.1 (commencing with Section 5887),Division 5; Adds Welfare and Institutions Code Part 7,Division 5, Chapter 3 (commencing with Section 5963); Adds and repeals Welfare and Institutions Code §5892.3; Repeals Welfare and Institutions Code §5963.06)
Expands the criteria for a qualified autism service professional to include a psychological associate, an associate marriage and family therapist, an associate clinical social worker, or an associate professional clinical counselor, as specified. Requires those positions to meet the criteria for a Behavioral Health Professional, as provided.
(Amends Health and Safety Code §1374.73; Amends Insurance Code §10144.51; Adds 4686.4 Welfare and Institutions Code §4686.4)
AB 352 (Bauer-Kahan) – Health Information
CMA Position: Support
Requires specified businesses that electronically store or
maintain medical information on the provision of sensitive services on behalf of a provider of health care, health care service plan, pharmaceutical company, contractor, or employer to develop capabilities, policies, and procedures, on or before July 1, 2024, to enable certain security features, including limiting user access privileges and segregating medical information related to gender affirming care, abortion and abortion-related services, and contraception, as specified. Prohibits a provider of health care, health care service plan, contractor, or employer from cooperating with any inquiry or investigation by, or from providing medical information to, an individual, agency, or department from another state or, to the extent permitted by federal law, to a federal law enforcement agency that would identify an individual or that is related to an individual seeking or obtaining an abortion or abortion-related services that are lawful under the laws of this state, unless the request for medical information is authorized in accordance with specified existing provisions of law. Exempts a provider of health care from liability for damages or from civil or enforcement actions relating to cooperating with, or providing medical information to, another state or a federal law enforcement agency before January 31, 2026, if the provider of health care is working diligently and in good faith to comply with the prohibition.
(Adds Civil Code §56.110; Amends Civil Code §56.101 and §56.108; Amends Health and Safety Code §130290)
AB 1697 (Schiavo) – Uniform Electronic Transactions Act
Permits use of electronic signatures to authorize disclosure of medical information by a provider of health care, health care service plan, pharmaceutical company, or contractor. Permits electronic signatures for the disclosure of genetic test results contained in an applicant’s or enrollee’s medical records, by a health care service plan. Permits electronic signatures for an employer to disclose medical information and genetic test results. for electronic signatures to be valid, these authorizations must expire on the occurrence of a specified date or event.
(Amends Civil Code §§56.05, 56.11, 56.17, 56.21, and 1633.3)
AB 1029 (Pellerin) – Advance Health Care Directive Form
CMA Position: Neutral
Confirms that a voluntary standalone psychiatric advance directive, as defined, may be executed in addition to or instead of a traditional advance health care directive. Clarifies long standing law to reflect prescribed limitations of the powers of a health care agent, conservator, or surrogate by expressly stating that a “health
care decision” under an advance health care directive does not include consent by an individual’s agent, conservator, or surrogate to convulsive treatment, psychosurgery, sterilization, or abortion, and by modifying the statutory advance health care directive form to reflect that the individual’s agent may not consent to a mental health facility or consent to convulsive treatment, psychosurgery, sterilization, or abortion for the individual.
(Adds Probate Code §4679; Amends Probate Code §§4617, 4701)
CMA Position: Support
Removes the requirement that a minor seeking to consent to mental health treatment or counseling on an outpatient basis, or to residential shelter services, must present a danger of serious physical or mental harm to themselves or to others or be the alleged victim of incest or child abuse.
(Amends, repeals, and adds Family Code §6924)
CMA Position: Support
Authorizes a minor who is 16 years of age or older to consent to replacement narcotic abuse treatment that uses buprenorphine at a physician’s office, clinic, or health facility, by a licensed physician and surgeon or other health care provider, as specified, whether the minor also has the consent of their parent or guardian. Authorizes a minor 16 years of
Your trusted local non-profit serving Stanislaus, San Joaquin, Merced and surrounding counties since 1979.
NOT ALL HOSPICES ARE THE SAME. Make sure to ask for Community Hospice, the longest standing accredited Medicare and Medi-cal certified hospice, palliative and health services organization.
Hospice Care
Palliative Care
Pediatric Care

Alexander Cohen Hospice House
The only hospice inpatient and respite facility in Stanislaus County
Hope Counseling
Grief and mental health support services
Children’s Grief Support
School based and Camp Erin® of the Central Valley
Community Education
Hope Chest Thrift Stores
age or older to consent to any other medications for opioid use disorder from a licensed narcotic treatment program as replacement narcotic therapy without the consent of the minor’s parent or guardian only if, and to the extent, expressly permitted by federal law.
(Amend Family Code §6929; Add Family Code §6929.1)
AB 48 (Aguiar-Curry) – Nursing Facility Resident
Informed Consent Protection Act
Expands the rights of every resident in nursing facilities and intermediate care facilities to receive information that
is material to an individual’s informed consent decision concerning whether to accept or refuse the administration of psychotherapeutic drugs. Includes the right to be free from psychotherapeutic drugs used for the purpose of resident discipline or convenience, or used as a chemical restraint except in an emergency. All residents of skilled nursing facilities, intermediate care facilities, and hospice facilities would have the right to appeal an involuntary transfer or discharge through the appeal process, as specified, regardless of a resident’s payment source or the Medi-Cal or Medicare certification status of the facility in which the resident resides.
(Amends Health and Safety Code §1599.1; Adds Health and Safety Code §1599.15)
AB 242 (Wood) – Critical Access Hospitals: Employment
Eliminates the sunset date on the exception to the prohibition on charging for professional services for federally certified critical access hospitals that employ licensees and charge for professional services rendered by those licensees to patients under specified conditions, including that the medical staff concur by an affirmative vote that the licensee’s employment is in the best interest of the communities served by the hospital.
(Amends Business and Professions Code §2401)

AB 1021 (Wicks) – Controlled Substances: Rescheduling
CMA Position: Support States that if any Schedule I controlled substance is federally rescheduled or exempted from the Controlled Substances Act, it will automatically become lawful for health professionals to prescribe, furnish, or dispense under California law.
(Adds Health and Safety Code §11150.3)
From delicate robotic and catheter procedures to precision therapeutics, we’re proud to offer diagnostic and treatment options for adult and pediatric referring providers across Northern California and the Central Valley. Your referred patients benefit from shorter drives, less traffic, affordable lodging, and more. We also offer robust telehealth and telemedicine options, for both initial consultations and follow up care.
Our physician referral liaisons are here to help navigate referrals and:
■ Facilitate access to our secure EMR system, PhysicianConnect
■ Assist with UC Davis Health clinical trials and telemedicine
■ Keep you abreast of new services, providers and research programs
■ Arrange meetings and webinars, and share information about CME and events
Your local Physician Referral Liaison: Joaquin Muñoz | 916-701-7161 | joamunoz@ucdavis.edu
Shirin Jimenez, M.D.
Associate Professor, Division of Cardiovascular Medicine
Specialties: Cardiology, Advanced Heart Failure


Your patients deserve faster access to a top cardiothoracic surgeon.
Adventist Health has brought together a team of cardiothoracic experts to quickly give your patients the attention they need. Led by Dr. Minghui Liu, a board-certified cardiothoracic surgeon with more than 30 years of experience and more than 5,000 complex cardiothoracic and vascular procedures, we are staffed to get your patients into surgery faster than any other hospital in San Joaquin County, keeping you fully advised every step of the way. When every beat and breath matters, immediate expertise is vital for your patients.
Scan the QR code to learn more, or visit AdventistHealthLodiMemorial.org/CardiothoracicCare



The California Medical Association has partnered with Lockton Affinity to administer the CMA Insurance Program. Whether you operate independently or as part of a group practice, are beginning your career or considering retirement, this program offers key benefits to help protect you through all stages:
Using group purchasing power, CMA members get exclusive, comprehensive coverage at discounted rates.

Discover unique coverage offerings to safeguard yourself, your loved ones, your business and your livelihood.

available: CMA members can access Medical Malpractice insurance.
To meet your exact needs, Lockton Affinity offers extensive policy options.
Communication failures among members of the healthcare team can lead to patient harm, which can prompt malpractice lawsuits. Common scenarios in these suits include refusing requests to examine patients and not exchanging adequate patient information during report and hand-off. Another example is assuming patient well-being despite information
available that indicates a problem. The case study below highlights the need for healthcare team members to develop effective communication strategies, especially during team conflict. (Although the setting of the case study is labor and delivery, the communication issues highlighted can occur in any healthcare setting.)
A patient at 34 weeks gestation presented to labor and delivery (L&D) reporting decreased fetal movement. The L&D nurse noted minimal variability in the fetal heart monitor (FHM) tracing and no response on vibroacoustic stimulation (VAS). She contacted the on-call OB, who ordered an ultrasound and Lactated Ringer’s but dismissed the nurse’s suggestion of a biophysical profile (BPP). The nurse obtained a BPP anyway and reported the 4/10 results to the OB, who admonished her for not following the original order. The nurse expressed her concern for fetal wellbeing and requested the OB’s immediate presence at bedside. Two hours later the OB arrived. He ordered betamethasone and continued observation. The infant was delivered via C-section two hours later. Apgars were 0/2/5 at one, five, and 10 minutes. The child was later diagnosed with cerebral palsy and profound intellectual disability.
• Address conflicts with team members in a private area.
• Change your communication style if it is likely to be regarded as dismissive or confrontational.
• Participate in team communication and collaboration training.
failures among members of the healthcare team can lead to patient harm, which can prompt malpractice lawsuits.
The parents’ lawsuit, which focused on the OB, alleged the delivery delay caused the infant’s injuries. Defense experts were not supportive of the OB due to several issues. One issue was the OB’s delay in examining the patient in response to the nurse’s communication of concerning FHR, VAS, and BPP results. The OB’s defense was also complicated by finger-pointing between him and the nurse, who blamed each other for the poor outcome. Further, the plaintiffs witnessed the nurse’s telephone conversations with the OB in which she urged him to examine the patient. The finger-pointing and testimony about the telephone calls were expected to reflect poorly on the OB in front of a jury. The case was ultimately settled due to these various issues, which would have made prevailing at trial unlikely.
To prevent similar incidents and improve patient safety, consider the following strategies: 1,2
• Proactively monitor patient progress.
• Thoughtfully consider challenges to your treatment plans.
• If attempts to resolve conflict fail, take steps to address them within the hospital’s organizational framework.
Although organizational factors can frustrate communication, in many malpractice claims communication failures can be traced to individuals on the plaintiff’s healthcare team. A common theme in these claims is passive attitudes toward obtaining patient information. This manifests as failure to evaluate patients with adequate frequency, ask questions, provide information, and voice safety concerns, among other things. Why these failures occur is not always apparent, but they can often be attributed to causes such as distraction, fatigue, over-commitment, fear, and over-confidence. Communication is a team endeavor, which often requires team training to achieve proficiency. It requires the individual and collective commitment of every team member and the institution in which the healthcare takes place.
1. Agency for Healthcare Research and Quality, Pocket Guide: TeamSTEPPS 3.0, Revised May 2023, https://www.ahrq.gov/ sites/default/files/wysiwyg/teamstepps-program/teamsteppspocket-guide.pdf.
2. Gary L. Sculli et al, “Effective Followership: A Standardized Algorithm to Resolve Clinical Conflicts and Improve Teamwork,” Journal of Healthcare Risk Management 35, no. 1 (July 30, 2015):21-30. https://doi.org/10.1002/jhrm.21174.
The information provided in this article offers risk management strategies and resource links. Guidance and recommendations contained in this article are not intended to determine the standard of care but are provided as risk management advice only. The ultimate judgment regarding the propriety of any method of care must be made by the healthcare professional. The information does not constitute a legal opinion, nor is it a substitute for legal advice. Legal inquiries about this topic should be directed to an attorney.



A career as a family physician was not the only vocation the 2024 recipient of the San Joaquin Medical Society’s Lifetime Achievement Award pursued. After 28 years in practice, Dr. Edward Schneider went on to transition into not one but two professions — as a surgical assistant and a college instructor. Even in retirement, he is still actively helping the next generation of eager students fulfill their dreams of getting into medical school.
Dr. Edward Schneider, the son of a Jewish tailor, dreamed of one day becoming a family doctor, even though no one in his family had attended college. In fact, he feels a certain pride in knowing that his father’s talent with a needle and thread was passed down to him — a talent he used to stitch up patients while assisting in surgeries. His father, who immigrated from Poland, and his mother, who fled anti-Jewish programs in Ukraine prior to the Holocaust, raised two sons who would become the first in their family to attend college.
Today, Dr. Schneider is still helping others by mentoring first-generation college students navigate their journey in the San Joaquin Medical Society’s Bridge to Medicine program. One such student said Dr. Schneider’s words of support have helped him during times of hardship. >>



“From his mentorship, I was able to gain more confidence in not only myself, but my belief in being worthy of attending medical school,” D’Angelo Martinez said, of meeting Dr. Schneider during his undergraduate studies at UC Davis. His hopefulness and positivity helped me to stay focused and not lose sight of the goal of getting into medical school. He always advised me to never worry about how long it may take me to attend medical school because as long as I stay dedicated, I will eventually reach that goal.”

grade science teacher to encourage him to become a doctor. The gifted student graduated at the mere age of 16 from an accelerated program at Grant High School in Los Angeles and graduated from UCLA in 1966, commuting from his parent’s home to his university classes as they could not afford the cost of college room and board.
Dr. Schneider didn’t have a program like Decision Medicine or Bridge to Medicine to guide him back when he was a young student, but his aptitude for biology prompted his 8th grade science teacher to encourage him to become a doctor.
Martinez did reach that goal. Today, he is working as a medical assistant at a pulmonary and primary care office and will begin medical school this summer.
Dr. Schneider didn’t have a program like Decision Medicine or Bridge to Medicine to guide him back when he was a young student, but his aptitude for biology prompted his 8th
“My happiest moment in life at that time was opening the acceptance letter to University of California San Francisco Medical School,” he said. In San Francisco, he would meet his partner in life Nancy was an assistant head nurse in oncology at UCSF when they met at a medical clinic in the Haight-Ashbury neighborhood. After they were married and he had graduated from medical school at the age of just 23, he spent a year in surgical residency at the University of Minnesota Medical School with the intention of becoming a surgeon. But the draft would intervene, and he joined the Navy, serving his country at Great Lakes Naval Hospital for two years.


An opening at San Joaquin General Hospital in a new residency program in 1973 led him to practice family medicine in Stockton.
Dr. Paul Waters, in nominating Dr. Schneider for the Lifetime Achievement Award, says he is “totally dedicated to the care and wellbeing of patients in this community.” Dr. Waters would launch Dr. Schneider’s career as a family physician in Stockton by inviting the young doctor to work with him when he finished his residency. “I was his preceptor when he was in his residency and I felt strongly about his skills,” Dr. Waters said.

Soon enough, Dr. Waters would encourage his protégé to strike out on his own.
“I didn’t have to put out a penny to start my practice,” Dr. Schneider said. “Within a year, it started getting crowded and he told me it was time to start my own practice. I opened up across the hall and we were colleagues and friends ever since.”
Nancy says she and her husband worked as a team in the practice and didn’t bring their work home with them. They raised two sons; Paul is the head of a civil engineering firm in Stockton and Adam is an orthopedic surgeon in Arizona. The couple now enjoy spending time with their four grandchildren — three boys and a girl — and indulging in hobbies, visiting with friends, and attending the symphony.





He serves on the artistic committee of the Stockton Symphony board. In his late 70s, he still runs four miles twice a week to keep fit and also enjoys golfing. On a recent spring day, he and his wife had a giant puzzle of the human skeletal system on a table in their Lincoln Village home that was nearly complete.

Looking back, the couple said they it was gratifying that multiple generations, four in some cases, chose Dr. Schneider to be their family physician. “I admire the dedication he had for his patients,” Nancy, who ran the office, said.
He said he really believes he helped people live healthier lives and was touched by the reaction of his patients when he decided to sell his practice due to frustrations with insurance companies and the overall hectic pace. “When my patients found out I was leaving, they said they were sorry, but they were happy for me as well,” he said.
After retiring from his practice of 28 years, Dr. Schneider changed course and became a college instructor, teaching at San Joaquin Delta College to share the excellent education he had received from the UC system and to give back to his community. He would teach sex ed, intro to human anatomy and physiology, and human anatomy. Many of his students were nursing school applicants. He also reconnected with his first love and began assisting in surgery with specialists in Stockton. He retired from Delta in 2011 and from surgical assisting in 2014.
Thankfully, he still finds time to mentor and also volunteers in elementary classrooms for STEM education projects.
“We need more physicians in Stockton and the Valley,” he said. “That’s the main goal but it’s also gratifying to me to help these students and guide them on the path in taking the right classes, preparing for the MCAT and applying to medical school.”
It’s guidance that his Bridge to Medicine mentees value.
“When I think of Dr. Schneider, the first thing that comes to mind is the level of optimism he radiates,” Martinez said. “Following each of our discussions, I always left the conversation feeling reassured in myself. Dr. Schneider’s true desire to help others in the community serves as a beacon of hope.”




Dignity Health - St. Joseph's Medical Center opened its doors as St. Joseph’s Home and Hospital in December of 1899. Its founder, Father William B. O'Connor, collaborated with the Dominican Sisters of San Rafael to assist a local group of physicians in finding a suitable place to treat their medical and surgical patients with specialized care. As the population of Stockton and the surrounding towns increased, St. Joseph's grew alongside the community to meet the complexities and challenges of delivering quality health care—leading the way with firsts in cardiac, cancer, maternity, pediatrics, and emergency care services.
Celebrating 125 years, St. Joseph's Medical Center is proud to serve the Stockton community. For more information, please visit dignityhealth.org/stockton.
 Doug Long
Doug Long
Adventist Health has appointed Doug Long as president of Dameron Hospital in Stockton. Long is responsible for the day-to-day operations of the hospital, ensuring that quality patient care is provided, and that the financial integrity of the hospital is maintained. Dameron Hospital is currently managed by Adventist Health.
Long, who began his new role in February, is returning to Adventist Health. He previously served as Business Development Executive, contracting with vendors, establishing partnerships, and coordinating integration into system operations. Prior to his work at Adventist Health, Long held leadership roles at West Hills Hospital and Medical Center in Los Angeles and Riverside Community Hospital.
Long will work with Brooke McCollough, current president of Adventist Health Lodi Memorial Hospital, to transition into the role of Dameron Hospital president.
“We welcome Doug to the Dameron Hospital leadership team,” said Eric Stevens, President, Adventist Health
Providing staff, physicians, and patients with relevant & up to date information
Northern California Network. “Together, Terri Day and Brooke McCollough have navigated the complex healthcare challenges facing Dameron and Adventist Health Lodi Memorial in recent years. This new leadership model adopting the “network” approach will keep both Adventist Health Lodi Memorial and Dameron Hospital working closely together. We are excited to develop a new leadership model with a dedicated executive at Dameron Hospital as it continues to grow to best serve our community.”
Adventist Health Lodi Memorial Pacific Heart and Vascular is thrilled to welcome Dr. Alaa Gabi, a board-certified Interventional and Structural cardiologist specializing in arterial and vascular diseases along with more complex cardiac and peripheral vascular Interventions. His extensive studies and authorship of over 30 publications have prepared him to deliver excellent care for our community with confidence.
Fluent in English and Arabic, his deep experience and board certifications position him as a strong addition to our robust cardiology team in Lodi and Stockton. Dr. Gabi’s philosophy of care comes from his desire to keep your heart, the most important organ in the body healthy and strong. He was drawn to cardiology after watching the happiness of many families after successful recovery of their loved ones from heart attacks.
Dr. Dwayne Wilson is board-certified in preventive medicine and joins Adventist Health Lodi Memorial with over a decade of clinical experience. Originally from New York, he served as a Navy Corpsman specializing in naval warfare and combat medicine. During his service, his pursuit of a career in medicine took him to Tennessee and Florida where he specialized in public health and then occupational medicine. He is currently seeing patients at our Occupational Medicine clinic offering DOT and pre-employment physicals along with workplace injury treatment.
Dr. Wilson was inspired to pursue medicine after spending time with his grandmother who had multiple sclerosis. He now cares for each patient he encounters with passion and enjoys contributing to a patient’s health and healing. He states, “It feels great to make a difference in a person’s life as they navigate through difficult times.”
Dameron Hospital is thrilled to welcome Dr. Gamel Marey to their team of surgeons. Dr. Marey is double American board-certified in both general surgery and cardiothoracic surgery. He has received six medical recognitions and sits on 11 different professional societies.
Originally from Egypt, he relocated to New York and Massachusetts for his general surgery and cardiothoracic surgery residencies. His training continued in advanced aortic surgery




Medical Malpractice insurance is crucial in protecting your practice and livelihood. Beyond paying the high cost of legal fees and judgments, Medical Malpractice insurance from the CMA Insurance Program, administered by Lockton Affinity, includes many benefits:
Coverage for common practice activites
Specialized customer service support
Regular updates from Lockton Affinity
Tailored coverage for all practice types
What is the difference between Medical Malpractice and Professional Liability coverage?
• These policies are the same coverage with different names. This coverage may also be referred to as Errors and Omissions or E&O.
Do I need a separate policy if I am working at multiple locations?
• Malpractice coverage follows you wherever you work, so there is no need to have a separate policy.
How do I get a quote and apply for Medical Malpractice coverage?
• Contact Lockton Affinity’s team of highly trained, licensed insurance professionals.
Scan the QR code to protect your practice today or contact Lockton Affinity's team directly at Info@LocktonAffinityCMA.com or (800) 278-8130.

at the Cleveland Clinic and congenital cardiac surgery at the University of Minnesota Children’s Hospital.
He has been practicing cardiac surgery since 2015 and offers expert medical care at Dameron Hospital with robust experience in providing a full spectrum of cardiac surgery, which includes coronary bypass, valve repair and replacement, septal myectomy, aortic root surgery and aortic aneurysms.
Joseph’s Medical Center Celebrated 125 Years of Caring for the Stockton Community

On March 19th, St. Joseph’s Medical Center hosted an anniversary celebration to honor the laying of the cornerstone and founding of St. Joseph’s Home and Hospital 125 years ago. In addition to an anniversary mass and ceremony, hospital leadership, staff, physicians, donors and dignitaries witnessed the unveiling of the Hospital’s Legacy Wall commemorating SJMC’s 125th year of serving our community.
“The history of St. Joseph’s is an integral part of the Stockton community, and I am grateful for the continued support we receive from our community every day,” said Donald J. Wiley, President and CEO of St. Joseph’s. “I could not be more proud and more humbled of all we have accomplished over the last 125 years, from becoming a nationally-recognized medical center in quality care to instituting our Graduate Medical Education program. Among many other achievements, these would not be possible without the support of our physicians, nurses, staff, volunteers and the Dominican Sisters.”
Dignity Health’s grant program helps to improve community health and health equity, and enhance local service systems, via restricted charitable contributions for defined projects. St. Joseph’s Medical Center and St.
Joseph’s Behavioral Health Center’s $334,922 funding for local nonprofits is part of Dignity Health California’s statewide total of $5.2M that was provided via community grants to nearly 100 organizations. The 2024 local grant funding benefits five community-based organizations seeking to provide health and human services to residents most in need in San Joaquin County.
The following five projects were awarded funding this year, with each grant recipient working in partnership with other community organizations: APSARA, Community Health Improvement Grants; San Joaquin Community Foundation, San Joaquin Pathways Community HUB; Second Harvest of the Greater Valley, Fresh Food 4 Kids; St. Mary’s Community Services, Health Ambassadors
Matthew Kiefer, MD, was recognized at the 2024 Community Philanthropy Summit as this year’s Outstanding Volunteer Fundraiser. Dr. Kiefer, an Emergency Medicine doctor at Dignity Health St. Joseph’s Medical Center, serves as the Simulation Lab Director for St. Joseph’s Graduate Medical Education Program. Through donor tours and showcase events, Dr. Kiefer curates experiences for guests to understand how crucial the SIM Lab is for development and growth of SJMC’s resident physicians. He is thoughtful in planning, months in advance, for each potential donor.
“From his first introduction to philanthropy at St. Joseph’s,

St. Joseph’s presents grant to Second Harvest
Dr. Kiefer effortlessly shifted from focusing on cost to addressing impact,” said Julie Eckardt-Cantrall, Vice President & Chief Philanthropy Officer of St. Joseph’s Foundation of San Joaquin.
Kaiser Permanente’s Modesto and Manteca hospitals earn an “A” for limiting patient injuries, reducing medical errors, and preventing infections, according to the Leapfrog Group
Reinforcing Kaiser Permanente’s commitment to health care quality excellence, Kaiser Permanente’s Modesto and Manteca hospitals are recognized with “A” grades for patient safety, according to The Leapfrog Group’s biannual Hospital Safety Grades report.
Leapfrog reviews hospital clinical data and assigns hospitals grades based on approximately two dozen
Providing staff, physicians, and patients with relevant & up to date information
measures that analyze patient injuries, medical and medication errors, and infections.
“As we focus on providing high-quality care to our patients, members, and the communities we serve, safety is always our top priority,” said Aphriekah DuhaneyWest, senior vice president and area manager for Kaiser Permanente Central Valley. “We are proud of this top rating for patient safety and will continue to ensure our patients are cared for in a safe and comforting environment.”
This spring, 13 Kaiser Permanente hospitals in Northern California received A grades from Leapfrog including: Antioch, Fresno, Manteca, Modesto, Oakland, Roseville, San Francisco, San Jose, San Rafael, Santa Clara, Santa Rosa, South Sacramento, and South San Francisco.
“Providing safe patient care is paramount to the work we do each and every day,” said Sanjay Marwaha, MD, physician in chief for Kaiser Permanente Central Valley. “We are honored to be recognized once again by the Leapfrog Group as a leader in patient safety as we continue to deliver exceptional care to our patients.”
A top-100 hospital – and a great place to work
UC Davis Medical Center has received a Healthgrades America’s 100 Best Hospitals Award for 2024, placing it among the top 2% of hospitals nationwide for overall clinical performance. Meanwhile, UC Davis Health has ranked No. 51 among 600 listed institutions on the 2024 Forbes list of America’s Best Large Employers, based on an independent survey of approximately 170,000


participants from a wide range of companies with 1,000 or more U.S. employees. The publication also listed UC Davis Health as a Best Employer for Diversity 2024, and a Best Employer for Women 2023 (the most recent rankings as of this writing). Newsweek recently ranked UC Davis Health among America’s Greatest Workplaces for Women 2024 in organizations with more than 5,000 employees and recognized us as one of America’s Greatest Workplaces for Parents & Families based on an evaluation of categories such as work-life balance, working environment, and corporate culture.
Health Plan of San Joaquin/Mountain Valley Health Plan Invests $100M in a Three-Year Community Reinvestment Program
As part of Health Plan’s 2023-2026 strategic roadmap to improve health for residents in San Joaquin, Stanislaus, El Dorado and Alpine counties, we have launched our Community Reinvestment Program. Through an investment of $100M over the next three years, Health Plan aims to transform care delivery, expand provider access, and improve the quality of health care in our communities.
Principles for the Community Reinvestment Program:
• Access to barrier-free quality care
• Support for local innovation
• Strategic & Transparent Spending
• Beneficial to our Members
Providing staff, physicians, and patients with relevant & up to date information
• Partnership with community
• Integrity
Some of the initial investments include:
• Community Health Worker Recruitment Workforce
• Community Health Worker Training Certification Program
• HIE Grants Incentive Program
• Mobile health clinics
…..and more to come in the future months.
Lizeth Granados (CEO) states, “Combining technology and meaningful solutions to improve health care quality and access for our members is an integral part of HPSJ/ MVHP’s mission. The Community Reinvestment Program supports our mission in two folds: 1) improve health outcomes by expanding capacity for and supporting the use of Community Health Workers and Doulas; and 2) make it easier for providers to access patient data so they can deliver care more efficiently and effectively. Through the collaboration of our providers and community partners, we continue to look for opportunities where our Community Reinvestment Program funding can positively impact the healthcare experience for our members, providers, and the community.
Health Plan looks forward to partnering with providers, clinics, hospitals, community-based organizations, and our members to improve community health while furthering Health Plan’s mission and vision.














Initiative will expand access to health care services and improve care for all Californians
The California Medical Association and the Coalition to Protect Access to Care, a broad and diverse group of health care organizations, have submitted enough signatures to qualify a statewide ballot initiative for the November 2024 ballot that will expand access to health care for millions of Californians.
The initiative builds on the historic investment that the Governor and Legislature made earlier this year to dedicate additional funding to the Medi-Cal program. The Protect Access to Healthcare Initiative is critical to ensuring the accessibility and affordability of health care services for all Californians, as well as recognizing the critical role that physicians play in achieving this vision.
Without raising taxes on individuals, the measure will bring more federal funds back to California and improve access to critical health care services. This initiative includes targeted rate increases for primary care and specialty care to make it easier for Medi-Cal patients to find a physician. In addition, the measure includes funding for graduate medical education to create more residency slots and new residency programs and loan repayment for those who agree to treat Medi-Cal patients.
Specifically, the initiative will:
Expand access to preventive health care for Medi-Cal patients, leading to fewer costly emergency room visits and shorter wait times for all Californians.;
Increase funding for mental health, including for those who need in-patient care;
Help California to manufacture its own insulin and other prescription drugs for much lower prices than exist currently.
Expand California’s education and training to create a pipeline of physicians and other health care providers to help alleviate shortages in underserved areas of the state.
Now more than ever, it is important that the 15 million Californians who rely on Medi-Cal for health coverage have access to care. Equally as important is ensuring that emergency room wait times are reduced for ALL Californians, that there is more funding for mental health care across the state and that we help reduce the cost of life-saving prescription drugs.
The support and engagement of the physicians of California will be invaluable in driving this initiative forward. In the coming weeks and months, we will reach out to you with opportunities to assist in outreach and education efforts and keep you updated on the progress of this initiative.
Please visit accesstohealthcareca.com for more information.

A PLACE FOR ALL NEWS HIGHLIGHTING RESIDENTS AND GRADUATE MEDICAL EDUCATION
SJMS Physicians Job Fair & Mixer
Thursday, September 19 6pm-8pm
Mercedes-Benz of Stockton
Please join us for the inaugural SJMS Physicians Job Fair & Mixer. This is a perfect opportunity to enjoy refreshments, while networking with physician members and senior residents from our local graduate medical education programs. Exhibitors will be providing services to or hiring for positions in the San Joaquin Medical Society service areas of Alpine, Amador, Calaveras, San Joaquin, and Tuolumne counties.
The Resident’s Report is dedicated to all the good news related to our hard-working residents training at San Joaquin General Hospital and St. Joseph’s Medical Center. Please email your submissions, written in third person with accompanying photo to Lisa@sjcms.org.
U S


San Joaquin General Hospital’s Internal Medicine Residency Program is excited to announce Dr. Jae Keum’s acceptance to the Geriatric Medicine Fellowship at Washington University, St. Louis after graduation in June 2024.
The program would like to also extend congratulations to 2023 grad and current faculty Dr. Arenja Shafeque for her acceptance to the Infectious Disease Fellowship at UC Davis, Sacramento.

The SJMC Internal Medicine residency program kicked off our joint mentoring venture with the San Joaquin Medical Society’s Decision Medicine students last month. There was plenty of food, fun, and encouraging conversations on advocating for yourself and finding what makes you happy. We all had a great time with these enthusiastic future physicians and can’t wait to keep working with them!





































St. Joseph’s rang in the New Year with receiving initial accreditation for two new fellowships – Cardiovascular Disease Fellowship and Critical Care Medicine. Drs. Cyrus Buhari and Loui Abdelghani will welcome three fellows each to their respective programs in July 2024. Additionally, St. Joseph’s anticipates a Child and Adolescent Psychiatry Fellowship submitted for review by November 2024.
All nine residency program successfully filled during The Match for a total of 72 new residents. Additionally, the Internal Medicine Residency Program received a temporary complement increase in April 2024. The incoming class will be 20 interns with three on a dedicated Primary Care track with Dr. Kwabena Adubofour and Community Medical Center East Main Clinic. St. Joseph’s will welcome 82 new residents in July 2024.

Free to SJMS/CMA Members!

The Office Managers Forum empowers physicians and their practice manager staff with valuable tools via expert led education sessions from industry professionals who are committed to delivering quality healthcare. This quarterly forum is normally held on the second Wednesday of March, June, September and December at Papapavlo's in Stockton.
Registration is required!
If you don’t receive an invitation via E-Mail, please email Jessica@sjcms.org
June 12, 2024: 11:00AM to 1:00PM
• Claim submission deadlines
• How much time does a payor have to pay my claim?
• What are the interest and penalty requirements for late payment?
• What are my appeal rights and how much time do I have to appeal?
• How do I get my contracted fee schedule?
• What are my rights regarding notices of overpayment?!

Mark Lane, Associate Director in the CMA’s Center for Economic Services, began his career as a claims processor for plans such as Blue Shield and Health Net. Over the next 18 years, his experiences in claim operations, customer service, provider relations and contracting have allowed him to get a unique vantage point on the relationship between physicians and payors. Having experienced the physician-payor relationship from both ends, Mark is able to understand the needs and positions of the respective sides, making him an ideal candidate to educate providers on overcoming the ever-changing challenges of the healthcare landscape.

Carrie Champness, RN, BSN Safety Compliance Specialist- Carrie has been an OSHA compliance specialist for over 35 years and provides up-to-date information about changes and practice requirements to meet all OSHA mandates.
Medi-Cal Rx implements utilization management criteria for Code 1 diagnosis restricted drugs
UHC delays Designated Diagnostic Provider program in CA until Jan. 1, 2022
Effective April 30, 2024, the California Department of Health Care Services (DHCS) has turned on claim utilization management edits for Reject Code 80 – Diagnosis Code Does Not Meet Drug Coverage Criteria for beneficiaries 22 years of age and older.
When submitting a prescription for a drug on the Code 1 diagnosis restricted list, prescribers must now demonstrate that the diagnosis restriction is met by completing one of the following actions:
• Submitting a qualifying diagnosis from the Code 1 diagnosis restricted list with the electronic prescription;
• Submitting a prior authorization request through an approved Medi-Cal Rx submission method establishing the Code 1 diagnosis restriction is met or establishing medical necessity for an alternative diagnosis; or
• Providing a qualifying diagnosis verbally to the pharmacy provider.
September 11, 2024: 11:00AM to 1:00PM
This workshop provides up-to-date changes and practice requirements to meet the Annual OSHA mandates.
Topics included: Bloodborne Pathogens, Aerosol Transmissible Disease Guidelines, Violence in the Workplace, as well as several other OSHA related topics.
DHCS also advised that Medi-Cal Rx will utilize diagnosis codes from the patient’s medical record, if available, to meet the requirement. However, absent a clear way to identify whether a qualifying diagnosis is on file, this method could result in duplicative work and delays patient access to medications.
Code 1 restricted drugs that do not meet one of the above requirements will be denied coverage with Reject Code 80 – Diagnosis Code Submitted Does Not Meet Drug Coverage Criteria.
Although California has several laws that protect
patient privacy related to disclosure of reproductive health, gender-affirming care and mental health services, DHCS has elected to keep some medications associated with these services on the Code 1 restricted drug list. Practices concerned about privacy issues associated with submitting a diagnosis to a pharmacy may wish to seek a prior authorization from Medi-Cal Rx rather than submitting a diagnosis code to the pharmacy.
New health care worker minimum wage takes effect June 1; IPAs and small physician practices exempt
On June 1, 2024, a new state law takes effect that phases in minimum wage increases for health care workers (SB 525 – Durazo). As of that date, physician groups with 25 or more physicians, and other types of health care facilities that meet certain criteria regardless of their size—such as urgent care clinics, community and other licensed clinics, ambulatory surgical centers and hospitals—must comply with the new minimum wage requirements. (Practices are encouraged to consult the complete list of covered health care facilities in the law to confirm whether it applies to them.)
Through California Medical Association (CMA) advocacy, SB 525 was amended to exempt medical group practices of 24 or fewer physicians and IPAs. CMA’s advocacy also ensured that physician practices would not face more drastic and immediate wage increases proposed or passed in some local jurisdictions and statewide that would be more difficult to weather.
With a gradual implementation, the ramp-up more closely aligns with wage trajectories that
are anticipated to occur naturally due to economic pressures outside of SB 525, including existing law that requires an annual assessment and adjustment of the minimum wage to reflect inflation. SB 525, which was signed into law in October 2023, ended efforts to move the fight to local and state ballot measures across the state, many of which sought immediate, rather than phased-in, minimum wage increases to $25, as well as limits on the pay of health care executives. CMA will be closely monitoring how the new law impacts physician practices and patient care, especially small and rural practices, hospitals and clinics.
The following chart shows when SB 525 wage increases would go into effect for each category of covered health care employers:
The Centers for Medicare and Medicaid Services (CMS) recently finalized comprehensive prior authorization reform regulations. These meaningful reforms apply to Medicare Advantage plans, state Medicaid and Children’s Health Insurance Program (CHIP) fee-for-service programs, Medicaid and CHIP managed care plans, and Qualified Health Plan issuers on the federally-facilitated Exchanges (FFE).
These regulations reflect the bipartisan legislation supported by the California Medical Association (CMA) and authored by California physician Congressman Ami Bera, M.D. and others – HR 3173/S 3108 “Improving Seniors’ Timely Access to Care Act” that unanimously passed the U.S. House of Representatives in September 2022 with more than 375 bipartisan House and Senate cosponsors.
3.5% annually until it reaches $25 in 2033
The final rule requires electronic prior authorization processes, shortens the time frames to respond to prior authorization requests, requires the public reporting of certain prior authorization metrics and establishes policies to make the prior authorization process more efficient and transparent.
The rule will require impacted payors (not including QHPs on the FFE) to send prior authorization decisions within 72 hours for urgent requests and seven calendar days for standard requests. For some payors, this new timeframe for standard requests cuts current decision timeframes in half. The rule also requires payors to include a specific reason for denying a prior authorization request, which will help facilitate resubmission of the request or an appeal when needed.
These operational or process-related prior authorization policies are being finalized with a compliance date starting January 1, 2026, and the initial set of metrics must be reported by March 31, 2026.
Other highlights of the final rule include:
-Allows payors to exempt physicians with a history of high prior authorization approval rates.
-Mandates appropriate and public clinical evidence to substantiate prior authorization decisions.
-Requires plans to establish Utilization Management Committees with physicians.
-Increases public transparency of approvals, denials, overturned decisions and response times.
CMS estimates that efficiencies introduced through these policies will save physician practices and hospitals over $15 billion over a 10-year period.
CMA will be working with the American Medical Association on federal legislation to achieve our remaining prior authorization goal – real time decisions. CMA also continues to support state-level legislation to reform prior authorization, process to ensure that patients receive the care they need — when they need it.
CMS signals additional prior auth reforms for Medicare Advantage, prescription drugs
The Centers for Medicare and Medicaid Services (CMS) recently suggested that the agency may implement additional prior authorization reforms in the Medicare Advantage program.
Recently, CMS Administrator Chiquita BrooksLaSure said CMS was evaluating whether the agency needed to take further action to crack down on health plans’ use of prior authorization and signaled that prescription drugs were a potential area for action.
A U.S. Department of Health Human Services Office of Inspector General (HHS OIG) report from 2022 found that Medicare Advantage Organizations delayed or denied enrollees’ access to necessary services via prior authorization.
Following the 2022 OIG report, CMS implemented a number of meaningful prior authorization reforms to Medicare Advantage and Medicaid plans. These reforms, from regulatory changes finalized in April 2023 and January 2024, will decrease delays in care and prevent inappropriate denials. Both of the regulations were consistent with changes advocated for by the California Medical Association (CMA). CMS estimates that efficiencies introduced through these policies will save physician practices over $15 billion over a 10-year period.
“I think that we have taken some really important steps in our rules. We’ve done the rules that are broad across the industry and also specific to Medicare Advantage. But we want to continue to look and hear about how things are operating. I’ve been hearing a lot about prescription drugs,” LaSure said.
CMA continues to work with Congress on federal legislation to achieve our remaining prior authorization goals and we are urging CMS to include drugs. CMA is also supporting state-level legislation to reform prior authorization to ensure that patients receive the care they need — when they need it.
CMA physicians have staunchly advocated for prior authorization reform by sharing personal stories and stories from patients about harmful care delays and denials; speaking to local media about the need for prior authorization reform; and submitting video testimonies about the impact of prior authorization. Patient witnesses also shared harrowing testimony in legislative hearings and through media outlets about the devastating impacts prior authorization delays have had on their lives and their loved ones.
CMA urges physicians to continue to share stories about the harms of prior authorization delays – both from your own experiences and practices, as well as from your patients. Together, we can win this fight and create a better system that prioritizes patients over profits.
As the summer months approach, physicians play a crucial role in ensuring their patients are wellinformed and prepared to safeguard their health against seasonal challenges. From sun safety to insect-borne illnesses, a proactive approach to patient education can mitigate risks and promote a safe and enjoyable summer. Here are some essential topics you may want to discuss with your patients.

When temperatures soar past 100º F during the San Joaquin Valley summer, heat-related illnesses like heat stroke and heat exhaustion are common. Urge patients to look for symptoms such as headache, dizziness, or confusion, since taking swift action can prevent serious complications.
A hot car can be lethal for young children. Remind caregivers that a child’s body temperature rises three to five times faster than an adult's. It can take as little as 15 minutes in a hot car for a child to begin to suffer life-threatening effects.
Mosquitoes, often viewed as mere nuisances, can transmit severe illnesses. Discussing protection against mosquito bites through the use of repellents and appropriate clothing is crucial to prevent mosquito-borne diseases.
Exposure to the sun's UV rays can lead to sunburns and increase the risk of skin cancer. Reinforce that applying sunscreen and wearing protective clothing are essential precautions against these dangers.

Water-related injuries peak during summer months. Safety measures such as life jackets and supervision, particularly for children, can prevent accidents in lakes, rivers, pools, and oceans. That said, life jackets are essential for everyone while in bodies of water. Whether staying on shore or making a splash, adults should also limit their alcohol intake.
Supervision is paramount in preventing playground injuries, which tend to rise during the summer. Parents need to closely monitor children and consider their own limitations e.g., to be able to step quickly in if a child takes a tumble. Trampolines can also cause severe injuries; nets around trampolines are recommended for safety.
The summer is a perfect time to get child wellness visits, dental checkups, and receive immunizations for the new school year. Taking advantage of the time children are not in school can lead to children missing less school and prevents having to squeeze in appointments at the beginning of fall.
Valley fever, a respiratory infection caused by soil fungus, is on the rise, particularly in San Joaquin Valley’s outdoor workers, such as those working in construction, landscape, and farming. Recognizing symptoms such as fatigue, cough, and fever is essential for early diagnosis and treatment. The California Department of Public Health urges providers to “Think Valley Fever” (couldbevalleyfever.org)

Warmer temperatures increase the risk of foodborne illnesses. Educating your patients on proper food handling and storage practices can prevent conditions like salmonella poisoning. For example, utilizing a food thermometer ensures food safety. For beef, pork, veal, or lamb, ensure the internal temperature reaches 160º F. Poultry dishes like turkey and chicken require a minimum internal temperature of 165º F. Seafood cooking temperatures vary; fish should reach 145º F, while shrimp, lobster, and crabs are done when their flesh turns pearly and opaque. Clams, oysters, and mussels should be cooked until the shells open. When in doubt, patients can visit the U.S. Food and Drug Administration website for guidance.
Hydration is key to staying healthy throughout the summer. Making sure children and adults consume an adequate amount of water is crucial in preventing illnesses and injuries. Emphasizing the importance of hydrating with beverages low in sugar is key. Suggest infusing water with fresh fruit such as strawberries and lemons as this can provide a refreshing incentive to increase water intake. Carrying a reusable water bottle promotes consistent hydration habits during the summer.
Summer vacations often involve travel to different regions. Discussing necessary immunizations for specific destinations can prevent travel-related illnesses and ensure a safe journey.
By addressing these key topics, physicians can empower their patients to enjoy a safe and healthy summer season.
1931 - 2023
John Brownell Irish, MD passed away on Wednesday, April 3rd in Stockton, CA at the age of 92. He was born on October 28, 1931, to John and Carolyn Irish in Washington, DC.
John attended the University of Iowa and pursued a career in Radiology. He married his college sweetheart, Peggee Lutz in 1954 and they were happily married for 49 years.
In 1962, he moved his family to Stockton, California where he practiced as a successful Radiologist with Radiology Medical Consultants Group for 30 years.
John was involved in a wide variety of nonprofit organizations including the Stockton Symphony and San Joaquin Medical Society. In addition, he thoroughly enjoyed his 35 years on the board of the Haggin Museum, serving as both Treasurer and President. His ultimate passion was traveling and learning about the
different cultures throughout the world. In his free time, John enjoyed playing golf and tennis and was a Bridge Life Master.
John is survived by his children Sara Gyorke (Andy), Susan Irish (Ed Marrone), Shari Pedroncelli (Frank), and John Irish. His grandchildren Clare Gyorke, Drew Gyorke (deceased), Angela Pedroncelli, Cristina Pedroncelli, Stephen Marrone and Amiri Irish. Also, Fran Meredith, his loving partner for the last 20 years.




San Joaquin Medical Society
3031 W. March Lane, Suite 222W
Stockton, California 95219-6568
RETURN SERVICE REQUESTED

Health Plan is proud of our commitment to preserving the safety net, in partnership with our community and providers to provide quality health care to our diverse population with growing needs.
Over the next three years, Health Plan will continue to build on our foundation by investing $100M in new initiatives that will improve quality, address health inequities, and ensure that members receive access to the best care possible. We will accomplish this through a framework that focuses on:
