THEIMPOSSIBLE INTO THE
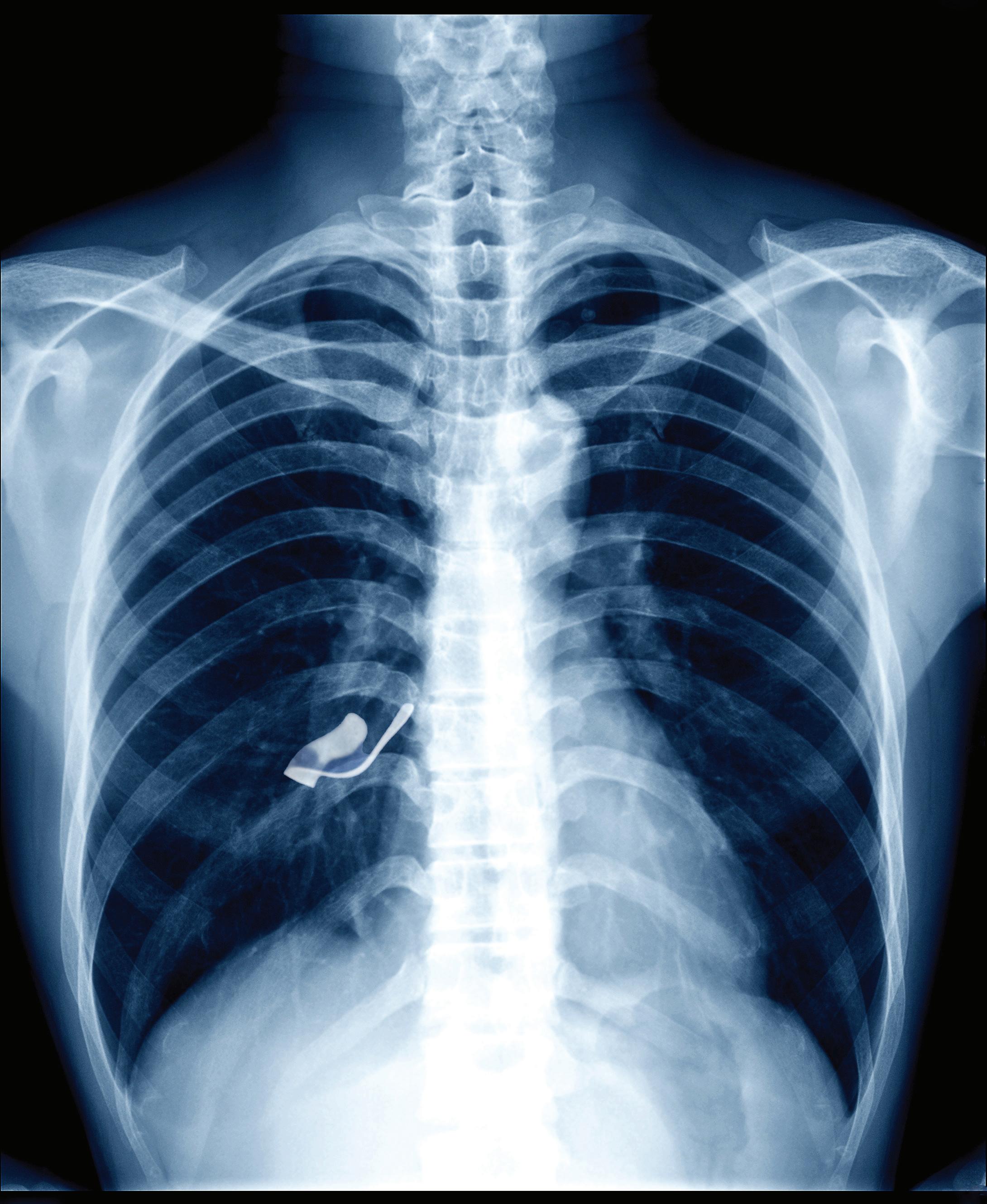
11 days after appendectomy, tests for acute abdominal pain revealed a
11 days after appendectomy, tests for acute abdominal pain revealed a
left inside the patient.
Surgical miscounts are considered never events because they are usually preventable by following established procedures.
ProAssurance offers risk assessments designed to help practices minimize errors by establishing and evaluating safety procedures and communication protocols.
With reliable procedures in place, our insureds are more likely to reduce errors in their medical practice, avoid claims, and make claims more defensible if they do occur.



PRESIDENT Sujeeth Punnam, MD
PRESIDENT ELECT Stephen Tsang, MD
TREASURER Sanjeev Goswami, MD
BOARD MEMBERS Maggie Park, MD, Alain Flores, MD, Manreet Basra, MD, Kinnari Parikh, MD, Bhagya Nakka, MD, Sunny Philip, MD, Rahuljit Bajwa, MD, Neelesh Bangalore, MD and Dheeraj Nandanoor, MD
MEDICAL SOCIETY STAFF
EXECUTIVE DIRECTOR Lisa Richmond
MEMBERSHIP COORDINATOR Jessica Peluso
COMMITTEE CHAIRPERSONS
CMA AFFAIRS COMMITTEE James Halderman, MD
CMA TRUSTEE Ramin Manshadi, MD
DECISION MEDICINE Kwabena Adubofour, MD
MEDICAL EDUCATION PROGRAMS Kelly Savage, MD
SCHOLARSHIP LOAN FUND Alexander Fodor, MD
CMA HOUSE OF DELEGATES REPRESENTATIVES
Aisha Chaudhry, MD, Dheeraj Nandanoor, MD, James R. Halderman, MD, Raissa Hill, DO, Richelle Marasigan, DO, Philip Edington, MD, Sujeeth Punnam, MD, Ripudaman Munjal, MD, Stephen Tsang, MD, Alberto Del Pilar, MD
SAN JOAQUIN PHYSICIAN MAGAZINE
EDITOR Lisa Richmond
EDITORIAL COMMITTEE Lisa Richmond, Sujeeth Punnam, MD
MANAGING EDITOR Lisa Richmond
CREATIVE DIRECTOR Sherry Lavone Design
CONTRIBUTING WRITERS Jo Ann Kirby, Sujeeth Punnam, MD, Joan Duwve, MD, MPH, King Lomotos, MPH, CIC, Theresa Fournier, MPH
THE SAN JOAQUIN PHYSICIAN MAGAZINE is produced by the San Joaquin Medical Society
SUGGESTIONS, story ideas are welcome and will be reviewed by the Editorial Committee.
PLEASE DIRECT ALL INQUIRIES AND SUBMISSIONS TO:
San Joaquin Physician Magazine 3031 W. March Lane, Suite 222W Stockton, CA 95219
Phone: (209) 952-5299 Fax: (209) 952-5298
E-mail Address: lisa@sjcms.org
MEDICAL SOCIETY OFFICE HOURS: Monday through Friday 8:00am - 4:00pm


The 2025 Mercedes-AMG SL 55 is more than a roadster it’s a celebration of performance and refinement. Whether you’re winding through wine country or arriving in style at a summer festival, every mile is a sensory experience. Crafted for those who savor the journey as much as the destination.



Back in 2013, I facilitated my first Decision Medicine class as Executive Director of SJMS. I was immediately struck by the students’ enthusiasm and the friendships they built so quickly—an experience that has stayed with me throughout the past 13 summers. One of the most rewarding aspects of Decision Medicine is watching like-minded students form lasting friendships and, in many cases, professional networks that continue well beyond the program.
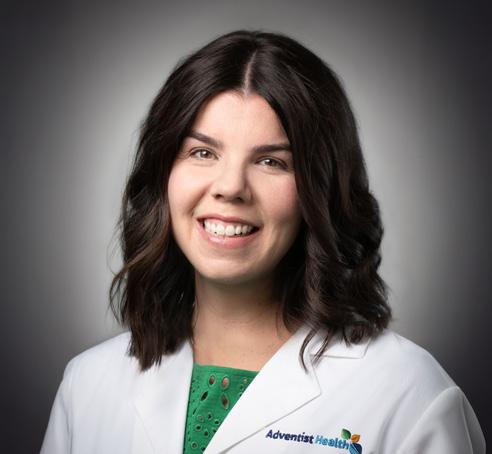
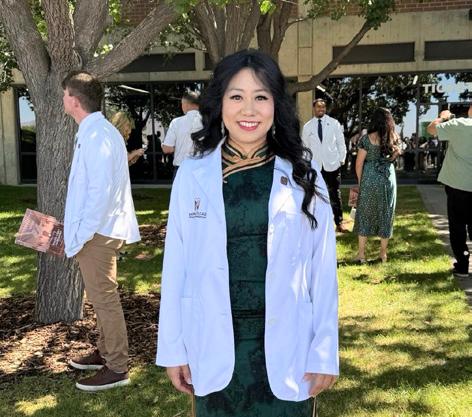
In this issue, we are especially proud to highlight Dr. Farwa Feroze, a member of that 2013 class. Dr. Feroze attended Touro University College of Osteopathic Medicine, completed her residency at San Joaquin General Hospital, and is now joining Sutter Gould Medical Group in Manteca as a family medicine physician—and soon to be SJMS member. We could not be prouder of her! Remarkably, four additional members of that cohort are currently in medical school or residency.
In her original Decision Medicine application, Dr. Feroze wrote, “My dream is to become a hard-working physician, who will make a difference in someone’s life.” We have no doubt she will do exactly that. You may read more of her story on page 45.
Each year, I survey our alumni to track the program’s long-
term impact. I am thrilled to report that among Decision Medicine graduates there are now at least 9 practicing physicians, 38 in medical school, 8 in residency or fellowship, and more than 100 undergraduates pursuing pre-med and STEM majors. Many others are following paths into nursing, physician assistant programs, physical therapy, dentistry, and other vital healthcare careers.
There are so many people involved in contributing to the success of our pipeline programs—staff, physician volunteers, community partners, and sponsors. It truly takes a village! We know that you will enjoy a glimpse into this year’s program toward the middle of the issue, as well as celebrating all the new medical school admissions and residency matches.
Finally, for my planners out there, please save the date for our Holiday Party on Thursday, December 11, at Stockton Golf & Country Club. We look forward to celebrating with you!
Warm Regards,
Lisa Richmond

Doctors Hospital of Manteca offers:
• 24-Hour Emergency Care and Convenient Online Check-Ins
• 24/7 Critical Care Coverage Led by Intensivists
• Bariatric Center of Excellence
• Blue Distinction Center for Hip and Knee Replacement
• Imaging Services, Including Open MRI and PET/CT
• Surgical Services
• Women’s Health, Including 3-D Mammography
• Wound Care Center
From emergencies and screenings to surgical and procedural services, Doctors Hospital of Manteca delivers quality healthcare and compassionate care close to home. To refer a patient, call



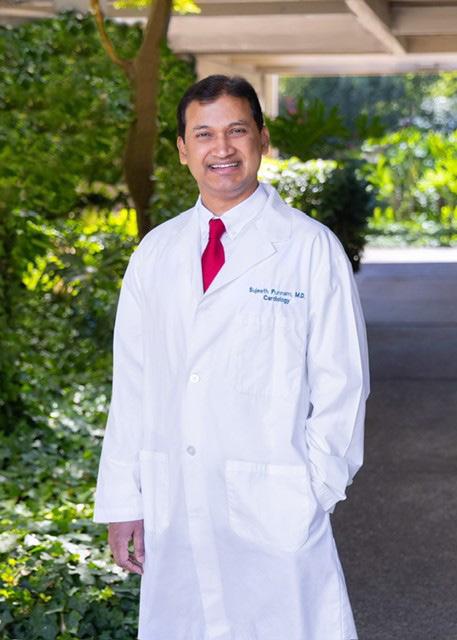
Sujeeth Punnam, MD is the current president of the San Joaquin Medical Society and practices interventional cardiology at Sutter Gould Medical Group
It is with a profound sense of honor and gratitude that I come to you today to communicate with you as the President of this esteemed organization. SJMS is the 4th oldest serving medical society in the state of California. And for an IMG hailing from a small town in India, son of a teacher, it’s very special for me to be nominated for this position. Even more humbled!
I would like to express my sincere appreciation to all those who have contributed to the continued success of this society, especially the board members and the outgoing president, Dr Bangalore. I thank my wife, Aparna and our 2 beautiful kids, Son Aneesh and Daughter Sarayu. Without their love and support and the sacrifices they make, I would not have been able to serve our physician community. Thank you!
SJMS represents about 700+ dues paying physicians in the counties of San Joaquin, Calaveras, Amador and Alpine counties. We conduct monthly board meetings, publish a quarterly magazine called San Joaquin Physician and functions as networking platform for local peers. SJMS hosts 2 main events, the Winter gala and awards gala. We recently had the Awards Gala and we got a chance to celebrate two woman physicians, Dr. Param Gill for Lifetime Achievement Award and Dr Manreet Basra for Young Physician Award for excellence in medicine. I fondly reminisce myself being one of the beneficiaries of the young physician award 6 years ago.
The SJMS encourages the professional growth of our members
by offering opportunities to serve on the Board of Directors, committees, SJMS’s delegation to the CMA House of Delegates, and other leadership positions. Through the larger network of the California Medical Association (CMA), SJMS represents the interests of organized medicine to policymakers in San Joaquin County and the state legislature. Advocacy is one of the biggest values these professional bodies bring to the members. Ever since third-party reimbursement has become the norm of doctor-patient relationship, advocacy has become the necessity of doctors to safeguard their interests, by way of collaborating with lawmakers. Think of membership dues as insurance we pay for cars or homes. Practice of medicine has faced lots of challenges before and will do so in the future. So, stay involved.
well-being and empowerment of its members and the communities we serve. We must continue to foster a culture of excellence in medical education, and clinical practice.”
We will work towards collaboration by engaging with the members. As your president, I commit to serving with integrity, passion, and dedication. I will work tirelessly to achieve our shared goals and to ensure that our society continues to thrive and make a positive impact on the community. And I believe in servant leadership!
“I envision a society that remains at the forefront of medical advancements, while also prioritizing the well-being and empowerment of its members and the communities we serve.
As your president, I commit to serving with integrity, passion, and dedication so our society continues to thrive and make a positive impact.”
Apart from these, San Joaquin Medical Society, runs Scholarship Loan Fund, Bridge to Medicine and Decision Medicine programs as charitable initiatives aiming to encourage local academically talented students to study medicine and return to practice in the area.
I envision a society that remains at the forefront of medical advancements, while also prioritizing the
As part of member engagement, we on the board sensed a need for continuing medical education for members, and SJMS has decided to work on this. We are going to have a Fall CME Healthcare symposium, with the first edition slated for Sep 27th. American Medical Association president, Dr Bobby Mukkamala has graciously accepted to deliver a keynote speech for the event as part of his grass roots reach. Please mark your calendars for an educational feast on wide range of topics on cardiology ppdates for primary care physicians and noncardiologists. We have some excellent speakers lined up from Stanford, UCSF and UC Davis delivering talks. You will be hearing about the details very soon.
To sum it up, I am deeply honored to lead this incredible group of individuals, and I am excited about the possibilities that lie ahead.

As we reach the midpoint of 2025, the California Medical Association (CMA) remains a leading voice for physicians and the patients they serve – championing policies that protect the practice of medicine and prioritize patient safety. Over the past six months, we’ve worked closely with lawmakers, regulators and key stakeholders to push back against inappropriate scope expansions, reduce unnecessary administrative burdens and uphold the integrity of physician-led care.
Our efforts this year have focused on ensuring that legislative and regulatory changes support – rather than hinder – the delivery of high-quality, evidence-based care. From testifying on critical bills to mobilizing grassroots physician engagement, we’ve amplified the voices of our members to make meaningful progress on the issues that matter most to physicians and the patients they serve.
This report provides an overview of our advocacy efforts so far this year, the challenges we’ve confronted and the victories we’ve secured. Together, we continue to protect the future of medicine.
CMA has protected physician decision-making and patient safety by successfully opposing or negotiating amendments to legislation that posed significant risks to clinical care. CMA stopped AB 1450 (HOOVER), which would have allowed advanced practice providers, such as nurse practitioners, physician assistants and certified registered nurse anesthetists, to practice independently within the California Children’s Services program, an inappropriate shift for this complex, high-risk patient population. CMA also secured amendments to AB 1196 (GALLAGHER), preserving critical surgical team standards for cardiac procedures and ensuring alignment with current professional guidelines for safe, high-quality care.
In negotiations over AB 970 (MCKINNOR), CMA protected physician discretion in mandatory child abuse reporting, ensuring that clinical judgment remains central in navigating these sensitive and consequential decisions.
CMA-sponsored SB 351 (CABALDON) also continues to advance through the legislative process and is currently on the Assembly Floor and enjoys bipartisan support. As private equity firms continue to gain influence in our health care system – leading to rising costs and undermining the quality of care – the bill empowers the Attorney General to investigate and take action against those that unlawfully interfere in the patient-physician relationship.
CMA also continues to push for reforms to California’s broken prior authorization system. Three bills from CMA’s Prioritizing Patients, Empowering Physicians legislative package – AB 512 (HARABEDIAN), AB 539 (SCHIAVO) and SB 306 (BECKER) – have advanced out of their houses of origin in the State Legislature. These measures aim to streamline burdensome prior authorization processes that delay and deny medically necessary care and bury physicians in red tape.
So far this legislative session, CMA has made meaningful progress in protecting the physician-patient relationship and reinforcing the critical role of physician oversight and evidence-based standards in delivering safe and effective health care.
On the pages that follow, you will find an overview of the bills CMA has opposed or successfully negotiated so far this year, as well as a look at the status of CMA’s sponsored and priority support bills.
AB 396 (Tangipa) Needle and Syringe Exchange
This bill would have required every needle provided through a needle exchange program to carry a unique identifier and required all needles provided through exchange programs to be properly disposed of. Any needle that had not been properly disposed of could be traced back, with the offending entity that donated the needle fined $10,000 per needle. This bill would have created significant costs that threaten the existence of needle exchange programs.
Status: Held in the Assembly Health Committee.
AB 1215 (Flora) Hospitals:
This bill would have required that dentists, podiatrists, clinical psychologists, nurse practitioners, nurse anesthetists, nurse midwives and other non-physician health care professionals be admitted to a hospital’s organized medical staff. This bill failed to account for the diverse circumstances and requirements of different health care facilities and would have put physician licensure at risk by linking enforcement of this bill to disciplinary actions by the medical board.
Status: Held in the Assembly Business and Professions Committee.
AB 1453 (Tangipa) Contraception Information
This bill would have required California State University campuses – and requested that University of California campuses – provide all students with adoption information any time they access contraception or emergency contraception through campus health services. This was an inappropriate mandate that would have undermined efforts to provide students with the reproductive health care they need.
Status: Held in the Assembly Higher Education Committee.
This bill would have allowed the California Department of Health Care Services to approve advanced practice providers, including nurse practitioners, physician assistants and certified registered nurse anesthetists, to practice independently within the California Children’s Services program. Allowing advanced practice providers to practice independent of physician supervision is inappropriate and dangerous and at odds with delivering the safest and most effective patient care.
Status: Held in the Assembly Health Committee.
This bill would have required the Government Operations Agency to appoint a working group to study the impacts and role of artificial intelligence in mental health treatment environments, but did not require a physician to be appointed. CMA requested amendments to ensure that the working group include a physician. However, the bill was held before amendments could be taken.
Status: Held in the Senate Appropriations Committee.
This bill would have required a “covered employer” to report confidential behavioral health employee and medical-surgical employee compensation information to the Department of Industrial Relations. This bill would have diverted resources away from patient care and posed privacy and data security concerns.
Status: Held on the Senate Floor.
AB 277 (Alanis) Behavioral Health Centers, Facilities and Programs: Background Checks
This bill requires any person providing behavioral health treatment to undergo a background check. CMA ensured that this would not apply to physicians holding a current and valid license, as the California physician licensure process includes a fingerprint-based background check.
Status: Held in Assembly Human Services Committee.
AB 290 (Bauer-Kahan) Emergency Services: Physician Fines
This bill would have increased penalties for physicians that fail to provide emergency health care by increasing monetary penalties for violations of existing state law from $5,000 per violation to $1 million per violation, and by establishing additional civil liability for physicians who violate injunctions related to a prior failure to provide emergency health care. Due to opposition, the bill was ultimately gutted and amended and no longer pertains to the practice of medicine – moving CMA to a neutral position.
Status: Currently in Senate Appropriations Committee.
AB 348 (Krell) Full-Service Partnerships
This bill establishes criteria for serious mental illness to presumptively be eligible for a full-service partnership through their county and funded by the Mental Health Services Act. CMA collaborated with the California State Association of Psychiatrists to address concerns and ensure those with behavioral health conditions would also be presumptively eligible.
Status: Currently in Second House: Senate Floor.
AB 360 (Papan) Menopause Survey
This bill would have created a menopause training survey, to be provided to all physicians and surgeons upon license renewal, to determine the level of menopausal training they have received. While the survey would have been anonymous and optional, mandating the creation of an overly broad survey to be conducted at license renewal was an inappropriate avenue to gather such information. Amendments were taken that instead create a study on menopausal training to be conducted by the California Department of Health Care Access and Information and the Medical Board of California, removing CMA opposition.
Status: Held in Assembly Appropriations Committee.
AB 432 (Bauer-Kahan) Menopause CME Mandate
This bill would have required physicians in several specialties – including general internal medicine, family medicine, OB-GYN, cardiology, endocrinology, and neurology – to complete continuing medical education (CME) specifically on menopause if 25% or more of their patient population consisted of adult women under age 65.
CMA agrees that menopause is a critical health issue and supports efforts to improve access to education on the topic. However, CMA opposed the bill’s original mandate, as physicians are best positioned to determine what CME content is most relevant to their practice. The bill also applied too broadly, capturing many specialists who do not diagnose or manage menopause.
The bill has since been amended to create an incentive program, allowing physicians to receive double CME credit for menopause education, which removed CMA’s opposition.
Status: Currently in Senate Appropriations Committee.
This bill introduces a variety of changes to mandated reporting for general neglect, including establishing an alternative response approach and creating a new standardized curriculum for mandated reporters that is required to be completed within the first three months of employment. CMA worked to ensure that physicians, who already undergo mandated reporting training, were exempted from this new training requirement, moving us to neutral.
Status: Currently in Senate Appropriations Committee.
This bill prohibits concurrent or retrospective review of medical necessity for the first 28 days of an inpatient substance use disorder stay during each plan or policy year. However, the bill also granted psychologists the ability to prescribe drugs. CMA moved to neutral after psychologists were removed from the list of those who can prescribe drugs.
Status: Currently in Senate Appropriations Committee.
970
This bill proposes a pilot program to evaluate a new model for mandatory child abuse reporting. The program would incorporate internet-based tools and decision support systems to assist mandated reporters in assessing whether a report should be made. Amendments clarify that participation in the program is voluntary and affirm that mandated reporters – particularly physicians – retain full authority and discretion in making reporting decisions.
Status: Held in Assembly Public Safety Committee.
AB 1196 (Gallagher)
This bill would have changed the requirements for cardiac surgical teams performing extracorporeal bypass to consist of a minimum of one surgeon and two additional medical staff persons, down from three surgeons. CMA coordinated with the California Society of Cardiologists to narrow the bill and ensure that requirements reflect the current professional standards of care.
Status: Held on the Assembly Appropriations Suspense File.
This bill would have required the California Department of Public Health to track and identify regions with Valley fever and mandate that adult patients receiving primary care services in high-incidence regions be offered a Valley fever screening test in a culturally competent and linguistically appropriate manner. CMA opposed this testing mandate as it overrides a physician’s clinical judgment in determining whether testing is appropriate for a given patient. Amendments were negotiated that remove the mandate that every adult patient be offered a test –instead clarifying that patients in high-risk areas need to be screened according to current clinical standards. Amendments were also made to ensure physicians are not subject to any licensing actions if, based on their professional judgment, they decide not to screen or offer a test for Valley fever.
Status: Currently in Assembly Appropriations Committee.
AB 408 (Berman) Physician Health and Wellness Program
This bill would establish a physician health and wellness program under the Medical Board of California to support physicians’ health and protect patients. The bill would align California with national best practices to address mental health and burnout issues. This bill will protect patients by connecting impaired or at-risk physicians with treatment.
Status: Currently in Senate Business, Professions and Economic Development Committee.
AB 489 (Bonta) Health Care Professions: Deceptive Terms or Letters: Artificial Intelligence
This bill would ban companies from marketing artificial intelligence (AI) chatbots as licensed medical professionals. AI can be a useful tool for physicians and for patients. However, patients need to know when they’re talking to an AI chatbot versus a trained health care professional.
Status: Currently in Senate Appropriations Committee.
AB 510 (Addis) Prior Authorization: Same or Similar Specialty
This bill would have required that appeals of prior authorization delays, modifications or denials be performed by a provider of the same or similar specialty. This would have helped ensure that providers can discuss prior authorization denials with a professional peer who understands the recommended treatment and underlying condition.
Status: This bill was held in Assembly Appropriations Committee and will not move forward this session.
AB 512 (Harabedian) Prior Authorization: Shortened Timelines
This bill would shorten urgent prior authorization request timelines from 72 hours to 24 hours for electronic submission and 48 hours for non-electronic submission. For non-urgent requests, the timeline would be shortened to three business days for electronic submission while maintaining the existing five business days for non-electronic submission. This change will ensure more patients can receive care or appeal denials in a timely fashion.
Status: Currently in Senate Appropriations Committee.
AB 539 (Schiavo) Prior Authorization: One-Year Duration
This bill would extend the validity of an approved prior authorization to one year (current industry standard is 60 to 90 days). This will provide patients with a longer window of time to receive medically necessary care and avoid the cumbersome prior authorization review and appeal processes.
Status: Currently in Senate Health Committee.
AB 967 (Valencia) Physicians and Surgeons: Licensure: Expedite Fee
This bill would streamline the process for licensing outof-state physicians looking to practice in California. This will ensure that physicians can be recruited to move to California and have certainty that they will have an active license to practice when they relocate.
Status: Currently in Senate Business, Professions and Economic Development Committee.
SB 32 (Weber Pierson) Health Care Coverage: Timely Access to Care
This bill would enhance access to maternity care services by requiring the California Department of Health Care Services, the California Department of Managed Health Care and the California Department of Insurance to establish unique time and distance standards for perinatal units in collaboration with stakeholders.
Status: Currently in Assembly Appropriations Committee.
SB 306 (Becker) Prior Authorization: Volume Reduction
This bill would authorize the California Department of Managed Health Care (DMHC) to eliminate prior authorization requirements for most services and lowertier prescription drugs that are routinely approved. Health plans would be required to submit prior authorization data to DMHC, which would use that information to identify and remove certain requirements. The goal is to reduce administrative burdens, minimize delays in care and allow physicians to spend more time with patients.
Status: Currently in Assembly Appropriations Committee.
SB 351 (Cabaldon)
Private equity firms are gaining influence in our health care system, leading to rising costs and undermining the quality of care. This bill empowers the Attorney General to hold private equity groups accountable for interfering with the practice of medicine, allowing the Attorney General to investigate and take action against private equity firms that unlawfully interfere in the patient-physician relationship. The goal is to restore trust in the health care system, ensuring that medical decisions are made in the best interest of patients, not financial shareholders.
Status: Currently in Second House: Assembly Floor.
CMA is proud to introduce CMA Capitol Insights, a new members-only email newsletter designed to keep physicians informed and engaged in the state and national policy decisions that impact the practice of medicine and the patients they serve.
Delivered straight to your inbox, CMA Capitol Insights offers timely updates on health care legislation, budget proposals, regulatory changes, and CMA’s advocacy efforts in Sacramento, D.C., and beyond. Each issue highlights what’s at stake, what CMA is doing, and how members can take action.
In an era of rapidly shifting political and policy landscapes, CMA Capitol Insights helps ensure that you have the information you need to protect your profession and your patients. Subscribe now at cmadocs.org/subscribe.








Celebrating 60 years of excellence and unwavering commitment to businesses and families in California’s Central Valley and East Bay communities


May 21, 1965.

Luke Simon, DO
Zeiter Eye Medical Group is excited to announce Dr. Luke Simon as their newest ophthalmologist. Dr. Simon grew up in Lodi and was a three-sport athlete at Lodi High School before entering college at Cal Poly San Luis Obispo as a pre-med student. He then spent four years at Western University of Health Sciences-College of Osteopathic Medicine of the Pacific. Next, Luke matched in Ophthalmology, spending 4 years at New York Medical College, followed by a one-year fellowship in Tampa, Florida honing his skills in anterior segment surgery. We welcome Dr. Luke Simon back to his roots in Lodi as a board-certified ophthalmologist with expertise
Providing staff, physicians, and patients with relevant & up to date information
in comprehensive eye care, LASIK, cataract surgery, and corneal conditions.
Dr. Simon enjoys getting to know his patients on a personal level to better understand their lifestyle, hobbies, and visual needs. This allows him and his patients to work together to address any concerns they have regarding their vision within the context of the patients’ lives.
When not seeing patients, Dr. Simon enjoys outdoor activities and spending time with his wife and three young children. Dr. Simon is looking forward to joining our community and will be caring for patients in Zeiter Eye’s Stockton, Lodi, Manteca, Jackson, and Sutter Creek locations.
In June 2025, Lynn Watson, RN, MSN, NEA-BC, joined St. Joseph’s Medical Center as Chief Nursing Officer. Lynn joined St. Joseph’s from Tenet Healthcare as the Market Chief Nursing Officer for Carondelet Health Network. While with Tenet, she oversaw nursing operations at two hospitals, a critical access hospital and two free-standing emergency centers, totaling over 800 beds. With over 10 years’ experience as a Chief Nursing Officer, Lynn has achieved success at a variety of different hospitals, leaving a legacy at each institution. Additionally, Lynn has shared her expertise with those looking to start a career in healthcare as an Associate Professor at Lewis University (Romeoville, IL) and Maricopa Community College (Phoenix, AZ).
With over 25 years of progressive healthcare leadership,


Lynn is recognized for transforming clinical operations through innovative, data-driven strategies that enhance patient safety, elevate quality metrics and optimize efficiency.
St. Joseph’s Medical Center recently announced the appointment of Alicia Howe, MHA, as St. Joseph’s Medical Center’s new Chief Operating Officer. Alicia joins St. Joseph’s from Orlando Health where she served in leadership at their Health Central Hospital. In her leadership role, she oversaw daily operations of Health Central Hospital, focusing on quality initiatives, patient satisfaction and continuous improvements across allied health and operational support services. Alicia led a large ancillary staff, emphasizing engaging, supporting and motivating her teams through team building, training opportunities and career development.
Alicia is no stranger to Northern California, having worked with Kaiser Permanente, South Sacramento Medical Center for nearly a decade, and she additionally worked at UC Davis Medical Center. With a background in Imaging Services, Alicia holds her Master of Healthcare Administration from Ashford University and Bachelor of Arts in Radiography from Laroche College.
St. Joseph’s Recognized as High Performing Among Four Procedures and Conditions by U.S. News & World Report
St. Joseph’s has been named among U.S. News & World Report’s 2025-2026 Best Hospitals as a High Performing hospital for Heart Attack, Heart Failure, Kidney Failure, Leukemia, Lymphoma and Myeloma. This is the highest distinction a hospital can earn as part of U.S. News’ Best Hospitals Procedures & Conditions ratings. U.S. News’ annual Procedures & Conditions ratings are designed to assist patients and their health care providers in making informed decisions about where to receive care for challenging health conditions or elective procedures.
New Cancer Diagnostic Equipment Arrives at St. Joseph’s Medical Center
In June 2025, St. Joseph’s Medical Center welcomed the Phillips EPIQ Elite Ultrasound System into the hospital. This piece of equipment, along with the Mammotome MRI-Guided Breast Biopsy System, was fully funded through St. Joseph’s Foundation of San Joaquin’s 2025 Fun Run/Walk for Wellness. Both of these machines will greatly benefit local cancer patients, providing precise and minimally invasive diagnostic capabilities and imaging. Each year, St. Joseph’s Foundation of San Joaquin, in
Let us help you regain control and take your life back. At St. Joseph’s Behavioral Health Center, we are committed to providing compassionate, quality care, in an environment that fosters communication, trust, and personal growth. Our inpatient and outpatient programs are dedicated to helping those we serve to achieve their goals and improve their quality of life. In addition, we have a Medication-Assisted Treatment Program designed to meet the needs of adults who are uninsured or underinsured with a history of opioid or stimulant use dependency. Whether you need assistance dealing with depression, anxiety, or substance dependency, or are seeking counseling, we can help.







Learn more at dignityhealth.org/stockton/behavioralhealth



































partnership with hospital leadership and physicians, selects specific equipment to purchase with funds raised through the annual community event. This partnership allows us to tap into physician expertise on community needs and the latest technology to improve healthcare outcomes in the San Joaquin region.
Gould Medical Group now the majority orthopedic provider in San Joaquin County, helping improve access to high-quality care
More San Joaquin County residents can now gain access to highly specialized orthopedic care closer to home thanks to efforts by Sutter Health and Gould Medical Group. Nine orthopedic specialists joined Gould in July, making the group the majority orthopedic provider in San Joaquin County.
“We welcome this group of physicians who share our passion for clinical excellence and continuous improvement, which help patients achieve their best care outcomes and experiences,” said Dr. David Peterson, chief medical officer of Gould Medical Group.
The new providers include surgeons specializing in injuries and ailments of the foot, ankle, knees and hips, as well as sports medicine and trauma. Two interventional pain management specialists are also part of the team. Formerly of Alpine Orthopedic Medical Group, the providers join 38 other orthopedic specialists who are part of Gould. For more than 75 years, Gould Medical Group — one of Central Valley’s premier physician-led medical groups aligned with Sutter Health — has been recognized for its high-quality care.
“Our group is honored to join a team whose culture mirrors our own, one that places patients first and is deeply rooted in compassion and community,” said Dr. Jeffrey MacLean, a surgeon specializing in trauma and one of the doctors joining Gould Medical Group. “We appreciate the bold vision and forward-thinking strategy setting this team apart, and we look forward to helping build on its legacy of providing high-quality care.”
Sutter’s latest care expansion in Stockton is another example of how the integrated, not-for-profit organization is bolstering its highly regarded and revered orthopedic and sports medicine program with the latest treatments and technologies. Teams across the system are pioneering

The teams marked the occasion with a ceremonial ribbon-cutting on Friday, July 25 at a care center located at 2488 North California St. in Stockton. The clinic joins the existing care center at 2545 West Hammer Lane offering orthopedic care, helping expand access and convenience for patients.
orthopedic advancements for patients and ushering in the latest complementary therapies like sports psychology and sports nutrition.

San Joaquin General Hospital Welcomes
Dr. Philip Cheng as New NICU Director San Joaquin General Hospital (SJGH) proudly announces the appointment of Dr. Philip Cheng as our new Director of the Neonatal Intensive Care Unit (NICU). Trained in Pediatrics, Neonatology, and Pediatric Cardiology, Dr. Cheng brings exceptional expertise in newborn and pediatric heart care to the hospital and the greater San Joaquin County community.
Dr. Cheng completed his residency in General Pediatrics in Fresno, followed by a Neonatology fellowship at the University of California, San Diego, and most recently, a Pediatric Cardiology fellowship at the University of California, San Francisco.
Prior to joining SJGH, Dr. Cheng served as the Medical
Providing staff, physicians, and patients with relevant & up to date information
Director of the NICU at St. Joseph’s Medical Center, where he also held the role of Chief of Pediatrics. He played a pivotal role in developing the hospital’s first pediatric hospitalist program.
Dr. Cheng’s appointment reflects SJGH’s ongoing commitment to ensuring that families in San Joaquin County have access to world-class medical care close to home.
Welcoming Dr. Campbell, OB/GYN
Dr. Molly K. Campbell is a board-certified fellow of the American College of Obstetrics and Gynecology. She provides routine care for women in all stages of life with simple and complex concerns.
Dr. Cambell earned her medical degree at St. George’s
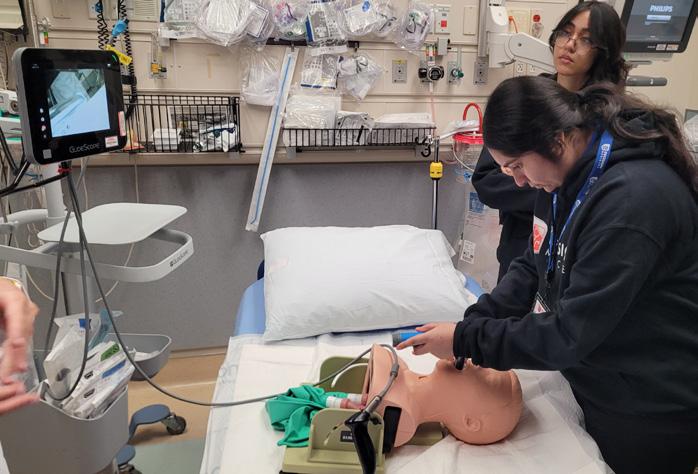
St. Joseph’s Medical Center leads the region in education, medical innovation, technology, and clinical research. We provide nine robust residency programs and four fellowships* focused on training highly-skilled, compassionate, and wellrounded physicians who will graduate prepared to care for any individual in a diverse range of emergent, urgent, and ambulatory care settings. St. Joseph’s is relentless in delivering health care with humankindness, and it starts with teaching the next generation of physicians.
St. Joseph’s offers residency and fellowship programs in:
•Anesthesiology
• Cardiovascular Disease*
• Critical Care Medicine*
•Emergency Medicine
•Family Medicine
• Internal Medicine
• Medical Simulation*
• Neurology
•Orthopedic Surgery
•Psychiatry
• Transitional Year
• Ultrasound*
•Urology
To learn more, visit dignityhealth.org/stockton/residency.

University in Grenada and completed her residency at Newark Beth Israel Jersey City Medical Center.
Before attending medical school, Dr. Campbell worked as a research assistant in the emergency department. There, she realized how many women lack high-quality gynecologic treatment in their reproductive years. She believes she has a responsibility to help counsel and encourage women to continue well-woman care throughout their lives.
Dr. Campbell is married to her college sweetheart, and they have two children and a sheepadoodle together. Both Dr. Campbell and her husband were collegiate NCAA Division I swimmers. Now, her personal life revolves around attending her kids’ swim meets, as well as riding bikes, hiking, going to the beach and kayaking.
Adventist Health Lodi Memorial receives Get With The Guidelines ® Stroke and Diabetes Award
Adventist Health Lodi Memorial received the American Heart Association/American Stroke Association’s 2025 Get With The Guidelines®-Stroke Gold Plus Quality Achievement Award.
The prestigious award recognizes the hospital’s commitment to ensuring stroke patients receive the most appropriate treatments, according to nationally recognized, research-based guidelines.
To receive the Gold Quality Achievement award, Adventist Health Lodi Memorial had to receive 85 percent or higher adherence to all Get With The Guidelines-Stroke achievement indicators for at least 24 consecutive months. The Gold Plus Quality Achievement is an even more advanced level of recognition, acknowledging the hospitals’ consistent
Providing staff, physicians, and patients with relevant & up to date information
compliance with quality measures.
Adventist Health Lodi Memorial earned further recognition for Target: Stroke Honor Roll Elite, which means 75 percent or more of acute ischemic stroke patients who were treated with IV tPA, received thrombolytic therapy within 60 minutes.
Additionally, Adventist Health Lodi Memorial received the Association’s Target: Type 2 Diabetes Honor Roll award. To qualify for this recognition, hospitals must meet quality measures developed with more than 90 percent of compliance for twelve consecutive months for the “Overall Diabetes Cardiovascular Initiative Composite Score.”
Adventist Health Lodi Memorial recognized with Hospital Week proclamation
Adventist Health Lodi Memorial was recently recognized by Lodi’s Mayor Bregman, who officially proclaimed May 11–17 as Hospital Week in Lodi. During the proclamation, Mayor Bregman acknowledged the hospital’s ongoing commitment to improving the health and well-being of the Lodi community—a meaningful affirmation of the work done each day.
The proclamation was presented to Adventist Health Lodi Memorial President, Brooke McCollough. in a special moment of recognition and appreciation for the hospital’s decades of care for the residents of Lodi.
“This proclamation is not just a recognition of our hospital—it’s a celebration of the people behind it,” said McCollough. “I’m incredibly proud of the work our team does each day to care for our community with excellence and heart.”

Kaiser Permanente Modesto and Manteca Hospitals Recognized for Commitment to High-Quality Stroke and Cardiovascular Care Kaiser Permanente clinicians follow up-to-date, research-based guidelines for the treatment of heart disease and stroke, aiming for better patient outcomes and more lives saved
The American Heart Association is recognizing Kaiser Permanente’s Modesto and Manteca hospitals for its commitment to providing stroke and cardiac patients with the most appropriate treatment founded in the latest scientific evidence, leading to more lives saved, shorter recovery times, and fewer hospital readmissions.
Kaiser Permanente Modesto hospital received the 2025 Get With The Guidelines®-Stroke Gold Plus with Target; Stroke Honor Roll and Target; and Type 2 Diabetes Honor Roll. Kaiser Permanente Manteca hospital received the 2025 Get With The Guidelines®Stroke Gold Plus with Target and Stroke Honor Roll Elite Plus.
In the United States, heart disease is the leading cause of death for men and women and people of most racial and ethnic groups, according to the Centers for Disease Control and Prevention (CDC). In addition, the CDC says one person dies every 34 seconds from cardiovascular disease and someone in the U.S. has a stroke every 40 seconds.
















AWARD RECIPIENT PARAMPAL K. GILL, MD




By Jo Ann Kirby
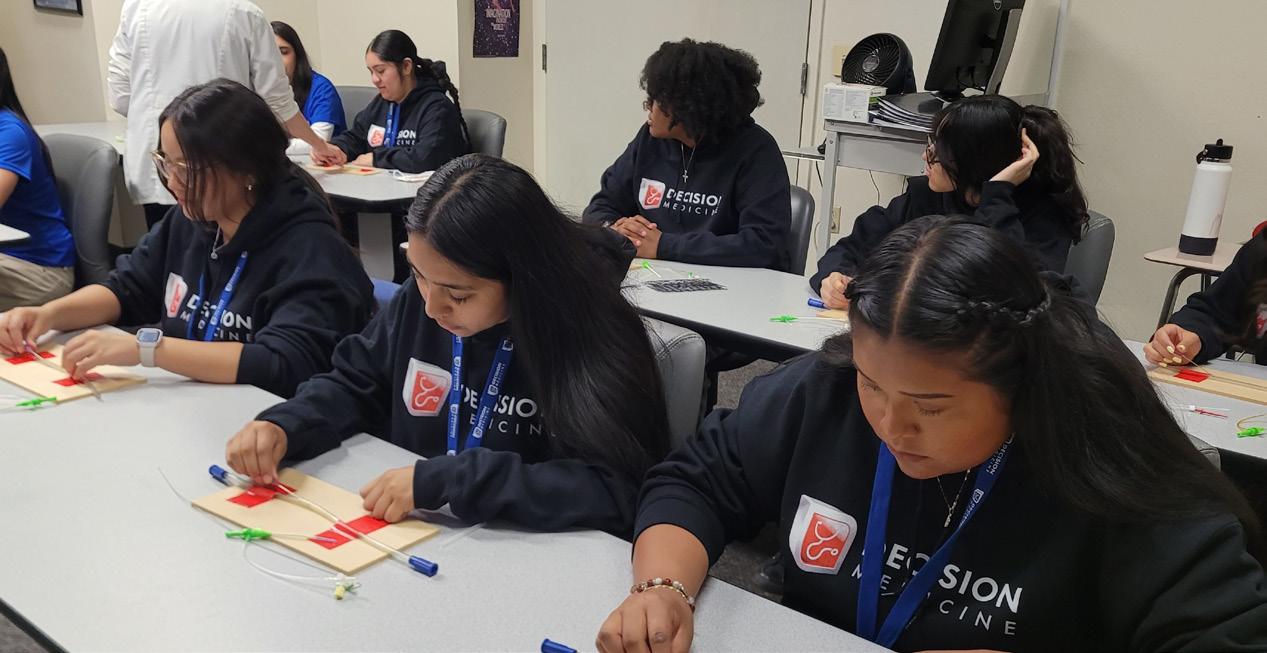
Becoming a physician can seem like an unsurmountable goal for students hoping to be the first in their family to attend college. But now, maybe not so much for the 24 high school juniors and seniors who applied, interviewed and were ultimately selected to take part in the 2025 Decision Medicine program.
“This was everything I was looking for coming from an under-resourced community. I’ve always known the medical field is something I wanted to pursue but Decision Medicine instilled the confidence I need and has shown me the steps I need to take and the path I need to take to pursue my goals,” said Mehar Boparai, who attends Sierra High School in Manteca.

In its 24th year, Decision Medicine was conceived
by Dr. Kwabena Adubofour and Dr. George Khoury as a way to introduce students to the field of medicine through mentoring opportunities and site visits to clinics, public health organizations, a medical school, hospitals, surgery centers and nonprofits that serve the homeless. The San Joaquin Medical Society program aims to encourage high achieving, underserved students, who would not otherwise have these opportunities, to consider a career in medicine and eventually come back to work in our community. They are able to meet health care professionals who share their valuable time with the students to offer a glimpse at their career. >>

“This was everything I was looking for coming from an under-resourced community. I’ve always known the medical field is something I wanted to pursue but Decision Medicine instilled the confidence I need and has shown me the steps I need to take and the path I need to take to pursue my goals.” -
MEHAR BOPARAI, SIERRA HIGH SCHOOL STUDENT


The opportunity was like a gift to 17-year-old Mehar. “I was over the moon,” she said of how she felt when she found out she was accepted into the program. “This gave me the opportunity to get that exposure that I’ve wanted.”
Being with like-minded peers who share a passion for science and math made the experience even more rewarding, she said. “It made me realize, I do fit in,” she said of the new friends and connections she’s made over the two-week program that took place this summer. “I felt comfortable and happy. It was great to be with students who praise each other. We got along so great and I learned about opportunities from them as well.”
Lisa Richmond, executive director of the San Joaquin Medical Society, said this year’s cohort stood out. “They have been especially engaged throughout the program, really paying attention and asking great questions,” she said. “The group clicked right away, and it’s clear they’re passionate about becoming doctors.”
In a Q&A session with medical residents at St. Joseph’s Medical Center, the students asked in-depth questions and took copious notes.
“How do you make your medical school application stronger?” one student asked the medical residents. They were advised to get involved in their community, conduct research or volunteer. One student realized he was







DM Committee & Shadow Day

Health Plan of San Joaquin
COMMUNITY PARTNERS
Adventist Health Lodi Memorial
Community Medical Centers
Kaiser Permanente
San Joaquin General Hospital
San Joaquin Public Health Services
St. Joseph’s Medical Center
St. Mary’s Community Services
UC Davis School of Medicine
And so many more who contributed their time and expertise!
Adnan Khan, MD
Alain Flores, MD
Cyrus Buhari, DO
David Araiza, MD
Dheeraj Nandanoor, MD
Diego Ferro, MD
Gentry Vu, MD
George Khoury, MD
Hyma Jasti, MD
John Canzano, MD
John Zeiter, Jr., MD
Kinnari Parikh, MD
Kwabena Adubofour, MD
Linda Sakimura, MD
Manreet Basra, MD
Marina Castillo, MD
Neelesh Bangalore, MD
Richelle Marasigan, DO
Ruby Gill, MD
San Tso, DO
Sanjeev Goswami, MD
Sunny Philip, MD
Tarandeep Kaur, MD
Vanessa Armendariz, MD
Ashlynn Urteaga
MANTECA HIGH SCHOOL
Brittney Garcia
LINDEN HIGH SCHOOL
Czandhie Corpuz
STOCKTON COLLEGIATE
INTERNATIONAL SCHOOL
Daniela Munoz
HEALTH CAREERS ACADEMY
Emmanuel Reyes
LATHROP HIGH SCHOOL
Eshal Maqsood
Middle College High School
Hafsa Hina
MIDDLE COLLEGE HIGH SCHOOL
Janessa Arredondo-Avila
WESTON RANCH HIGH SCHOOL
Jasmine Faith Johnson
EDISON HIGH SCHOOL
Jolene Cisneros
TRACY HIGH SCHOOL
Keerat Sandhu
BEN HOLT COLLEGE PREPARATORY
ACADEMY
Layla Amon Foster
FRANKLIN HIGH SCHOOL
Lesly Nemecio
LODI HIGH SCHOOL
Mehar Boparai
SIERRA HIGH SCHOOL
Mirian Perez
STOCKTON EARLY COLLEGE
ACADEMY
Ryan Nguyen
JOHN C. KIMBALL HIGH SCHOOL
Sebastian Munoz
FRANKLIN HIGH SCHOOL
Skyler Vang
HEALTH CAREERS ACADEMY
Sophia Samaniego EDISON HIGH SCHOOL
Syrell Gatan
STAGG HIGH SCHOOL
Tanish Dutta
MOUNTAIN HOUSE HIGH SCHOOL
Tanya Momand LATHROP HIGH SCHOOL
Thao Nguyen
MOUNTAIN HOUSE HIGH SCHOOL
Victoria Rodriguez
LINCOLN HIGH SCHOOL
already doing just that, by volunteering as a translator between patients and health professions. They heard a message of hope and were encouraged to never give up just because the path isn’t always straight. Sometimes there are detours or obstacles that can and must be overcome. They also learned the importance of empathy and compassion. One student asked, “How do you keep from becoming desensitized?”
“At the end of the day, it grounds me to get to know the patient,” Dr. James Garcia, a resident at St. Joseph’s, said. “Think of this patient as someone in your own family and how would you want your family to be treated?”
For teenagers who would be the first in their family to attend college, the application process can seem overwhelming. But the writing workshop and a “Jump Start to College” session with a high school counselor explained the process and gave valuable information and tips that students were encouraged to remember.
“You have to make every university feel like it’s your first-choice school,” Johnna Gheradi advised. “And how do you do that? You research.”
Sebastian Munoz, a 17-year-old student at Franklin High School said the program made him see the possibilities and potential for a future in medicine. “I think it’s really meant the whole world to me. It’s opened up so many doors,” he said. “I’ve struggled with imposter syndrome, like I don’t really belong. It’s been hard for me to see myself in the medical field.”
It helps that the students were able to meet and speak with a diverse group of physicians and health care professionals who came from similar backgrounds. That detail was driven home when the students and their families attended a celebration banquet that celebrated their participation in the program.
The keynote speaker, Dr. Amanda Panh, graduated from Bear Creek High School and University of the Pacific before being accepted into the UC Davis School of Medicine. Today, she is a physician at Community Medical Centers in Stockton and she had nothing but words of encouragement for students who may have also felt like Sebastian. “You guys all belong in medicine. Being from Stockton
should never limit you, it should only fuel you.”
Dr. Panh confessed that she didn’t always make good grades but she turned her life around when she realized a minimum wage job wasn’t going to give her the future she wanted for herself.
“Being a doctor isn’t just about grades it’s about grit, curiosity, compassion and the ability to bounce back when things don’t go as planned,” she said. “Barriers exist but so do bridges. You belong in every single room no matter where you’re from. Your zip code doesn’t define your destiny. Medicine needs you. Your voice, your story, your heart, that’s what healthcare is missing.”
Dr. Panh shared her cell phone number in hopes that she can be a source the students can count on when they need advice, information on resources or a nudge in the right direction.
Celebrating the students was a proud moment for the teens and their families at a banquet where the students said their goodbyes to each other and the program facilitators but promised to keep in touch. They were beaming with joy, knowing that they had been part of something very special and newly secure in the knowledge that the program had shown them the path forward.
“This year we had 140 applications, and we interviewed 45 students selected by a panel of doctors,” Richmond said, explaining how the group was narrowed down to the 24 ultimately chosen for the 2025 cohort. They represented 18 high schools throughout the county and had a combined GPA of 4.1. “Once you’re in, your part of the family; we want to stay in touch and be here to support you.”
So far, she estimates the program has resulted in 9 practicing physicians, 39 in medical school, 9 in residency, two in fellowship and at least 100 students attending college in pre-med or pre-health majors.
“We are just really proud of you,” she told them.
For the students, the future is now a bit brighter. “This experience has opened my eyes to what I can bring to the field and solidified my passion for serving my community,” Sebastian said.

















Health Plan awards scholarships and honors
Decision Medicine students
Decision Medicine (DM), a program founded by the San Joaquin Medical Society, inspires high-achieving students from underrepresented backgrounds to explore careers in medicine and motivate them to return to the Central Valley to serve its richly diverse communities.
Health Plan of San Joaquin/Mountain Valley Health Plan (“Health Plan”), the region’s local Medi-Cal Managed Care Plan, has been a proud supporter of DM for many years. Through its Health Careers Scholarship Program, the Health Plan awards scholarships to local students dedicated to entering healthcare professions.
This year, ten DM graduates were among the recipients
of Health Careers Scholarships—representing a $30,000 investment in the future of healthcare and in young leaders who have completed the DM program and are committed to makinga difference.
Scholarship awardee, Sehaj Gill, shares, “To me, medicine is both a clinical and civic responsibility. I want to serve my hometown of Stockton as a neurosurgeon—not just with a scalpel, but by working to change the healthcare system and bridge the equity gap between patients of different socioeconomic backgrounds. My goal is to ensure that quality healthcare is accessible to all.”
Health Plan is proud to honor this year’s Decision Medicine program graduates and scholarship awardees—remarkable students dedicated to serving their communities through careers in medicine. Each recipient embodies resilience, compassion, and a deep commitment to improving health care in the Central Valley.
Alessandra De La O – Pursued profession: Internal or Family Medicine. A first-generation college student, Alessandra has dreamed of becoming a doctor since childhood. She is determined to overcome barriers and serve her community as a compassionate physician. Anicia Ortiz – Pursued profession: Pediatric Surgeon. Guided by faith, resilience, and her mother’s example, Anicia is pursuing a career in pediatric surgery. She is currently building her academic foundation at the University of the Pacific. Celene Limon – Pursued profession: OB-GYN. Celene’s passion for medicine stems from her desire to care for people in her hometown of Stockton. She hopes to return as a licensed OBGYN to serve local families. Gabriela Ochoa – Pursued profession: Pediatrician. Proud of her Mexican-American heritage, Gabriela aims to become a pediatrician and address children’s health needs in underserved communities like Stockton. Jaisleen Kaur – Pursued profession: Pediatrician or Cardiothoracic Surgeon. Quietly determined, Jaisleen discovered her calling during hospital shadowing experiences and is pursuing a future as a physician specializing in pediatrics or cardiothoracic surgery. Janae Mya Butler – Pursued profession: Dermatologist. Personal struggles with eczema and psoriasis inspired Janae to become a dermatologist, helping others overcome skin conditions with confidence and care. JC Yandel Vera – Pursued profession: Cardiac Surgeon. JC is passionate about breaking cultural barriers in medicine and currently volunteers as a hospital interpreter to ensure all patients feel understood and respected. Jose Martinez – Pursued profession: Gastroenterologist. Inspired by his mother’s work as a GI technician, Jose is committed to becoming a gastroenterologist to improve and save lives through advanced medical care. Sanya Nath –Pursued profession: Pediatrician. A childhood asthma scare and the compassion of her care team led Sanya to pursue pediatrics, with a goal of serving Central Valley children and
families. Sehaj Gill – Pursued profession: Neurosurgeon. Sehaj plans to return to Stockton as a neurosurgeon, dedicated to bridging health equity gaps and ensuring access to quality care for all patients.
Says DM program graduate and scholarship awardee, Jose Martinez, “Ever since my mother introduced me to the medical field through the stories she shared from her work as a GI technician, I’ve been inspired by the life-changing power of medicine. Seeing how patients could come in critically ill and leave with their lives transformed made me realize that becoming a physician was my calling. I want to impact lives and help others in need, just as I saw happening in those stories.”
Jose’s story is just one example of the passion and purpose driving these scholarship recipients. Each student brings a unique perspective shaped by personal experiences, cultural roots, and a shared commitment to serving others—qualities that align closely with the Health Plan’s mission to strengthen the healthcare workforce in the Central Valley.
By fostering this connection between education and community service, the Health Plan is helping to shape a new generation of healthcare leaders. These students carry not only academic promise, but also a deep understanding of the unique needs of the Central Valley—making them wellpositioned to return as skilled, compassionate providers who can make a lasting impact.
“Supporting the next generation of healthcare professionals is one of our highest priorities as a community health plan,” said Health Plan’s Chief Medical Officer, Dr. Lakshmi Dhanvanthari.
“By growing the size and scope of our scholarship program, we’re not just funding education, we’re investing in the future of the youth and expanding access to health care in the communities we serve. We truly can’t wait to see these bright, determined students return to share their talents.”
Lisa Lim
DECISION MEDICINE 2009

Saba Khan
WESTERN HEALTH SCIENCES UNIVERSITY
BRIDGE TO MEDICINE
MENTOR: JENNIFER GRAY, MD

MIDWESTERN UNIVERSITY CHICAGO
BRIDGE TO MEDICINE
MENTOR: R. GRANT MELLOR, MD

A.T. STILL UNIVERSITY SCHOOL OF OSTEOPATHIC MEDICINE
DECISION MEDICINE 2018
BRIDGE TO MEDICINE
MENTOR: JENNIFER GRAY, MD

NOORDA COLLEGE OF OSTEOPATHIC MEDICINE
BRIDGE TO MEDICINE
MENTOR: AMIR ASSADI-RAD, PHD

Arshdeep Gill
ALICE WALTON SCHOOL OF MEDICINE
DECISION MEDICINE 2021
BRIDGE TO MEDICINE
MENTOR: KELLY SAVAGE, DO

TCU BURNETT SCHOOL OF MEDICINE
BRIDGE TO MEDICINE
MENTOR: JOHN ZEITER, MD
SCHOLARSHIP LOAN FUND

MAYO CLINIC COLLEGE OF MEDICINE
BRIDGE TO MEDICINE
MENTORS: HYMA JASTI, MD & R. GRANT MELLOR, MD
SCHOLARSHIP LOAN FUND

UCLA DAVID GEFFEN SCHOOL OF MEDICINE
DECISION MEDICINE 2017
SCHOLARSHIP LOAN FUND

Christian Labasan
CALIFORNIA HEALTH SCIENCES UNIVERSITY
COLLEGE OF OSTEOPATHIC MEDICINE
DECISION MEDICINE 2019

UC DAVIS SCHOOL OF MEDICINE DECISION MEDICINE 2019

Julia Tang
MEDICAL COLLEGE OF WISCONSIN DECISION MEDICINE 2018

Kiana Mikami
UC DAVIS SCHOOL OF MEDICINE
DECISION MEDICINE 2019

Kartik Goswami
KAISER PERMANENTE SANTA CLARA
INTERNAL MEDICINE
DECISION MEDICINE 2016

ADVOCATE LUTHERAN FAMILY MEDICINE
BRIDGE TO MEDICINE

Natalie Pearlman
UCSF FAMILY & COMMUNITY MEDICINE
RESIDENCY
DECISION MEDICINE 2012
BRIDGE TO MEDICINE

BY JO ANN KIRBY
What if there was a program that would inspire, mentor and show youth the path to become health care providers so that they would return home to practice medicine in their underserved hometowns? There is and they are!
Dr. Farwa Feroze, D.O., is a Decision Medicine success story who is a shining example of how the San Joaquin Medical Society’s two-week summer program can energize and support underprivileged but highly motivated high school students to seek out an education in medicine. The program’s ultimate goal is that these students come back to practice medicine in our community. And Dr. Feroze, like other DM success stories, has done just that.
“Decision Medicine played a pivotal role in shaping my path to a career in medicine. It helped me see a future for myself in healthcare and emphasized the importance of coming back to serve the community that raised me,” said Dr. Feroze, who recently graduated from San Joaquin General Hospital’ Family Residency Program.
As a junior at Tracy High School, Farwa Feroze was one of 24 students selected for the 2013 Decision Medicine program. Initially she was considering a medical profession because of the empathy and care her family encountered obtaining medical care for her nonverbal, autistic sister. Taking part in Decision Medicine that summer, she would tour community health centers and see firsthand how the local homeless population was receiving care.
“One of the most impactful aspects of the program was the integration of healthcare with local community support systems,” she said. “In just two weeks, we saw how hospitals, clinics, social services, and public health initiatives worked together to support the health of underserved populations. That holistic perspective has stayed with me throughout my training and continues to influence how I approach patient care today.”
She would go on to study public health at the University of California, San Diego, before attending medical school at Touro University College of Osteopathic Medicine.
During Decision Medicine, each student receives a one-on-one mentoring experience with a local physician in their practice. She also met Dr. Kwabena Adubofour, one of the program’s co-founders, and later reconnected with him during her clinical rotations in Stockton. He even attended her hooding ceremony at medical school graduation. >>





“I will soon begin my role as a Family Medicine Physician at Sutter Health’s South Manteca Care Center.”
- Dr. Feroze
Fulfilling the goal of Decision Medicine, she came back to San Joaquin County where she matched as a resident in San Joaquin General’s Family Medicine Residency Program. That full-circle moment meant something special to her. “It affirmed that my journey had come to fruition, and I felt a deep sense of purpose and fulfillment in being able to serve the same community that had inspired my path into medicine,” she said.
Today, she continues on her career path. “I will soon begin my role as a Family Medicine Physician at Sutter Health’s South Manteca Care Center,” she said. “In this position, I will be providing comprehensive outpatient primary care to all patients, ranging from adolescents to older adults.”
She said a typical work week will involve managing both chronic and acute medical conditions, offering preventive care services, and practicing holistic, patientcentered care. “I am looking forward to building longterm relationships with patients and continuing to serve the diverse healthcare needs of our community,” Dr. Feroze said.
“My family is proud and deeply grateful that I am now serving as a physician in the community where we have lived, grown, and built our lives.”- Dr. Feroze
Dr. Kwabena Adubofour, who co-founded Decision Medicine along with Dr. George Khoury, said the Decision Medicine program has been successful. The two physicians remain committed to Decision Medicine and are heartened to see the impact it has made on its participants “It’s an absolute joy to see our students come back to practice.”
Dr. Feroze is one of nine practicing physicians who took part in Decision Medicine. She said Decision Medicine was a strong
foundation that she could build on as she kept her ultimate goal in sight. “My advice to current students is to work hard, stay humble, and never forget where you came from,” she said. “Your roots will keep you grounded. Do what you love, and focus on building genuine relationships—with your patients, your peers, and your mentors. You have the opportunity to make a real difference in your community, and that’s a privilege worth striving for.”
Today, she remains committed to the core mission of Decision Medicine — to support and encourage San Joaquin County students to pursue health careers and come back to serve in their community. “I intend to remain local and continue practicing medicine within this community,” she said. “I am committed to working hard and serving this community that has given me so much, honoring the values I have been taught, and contributing to the well-being of the community I call home.”
And what do her parents thing of all she has accomplished?
“My family is proud and deeply grateful that I am now serving as a physician in the community where we have lived, grown, and built our lives,” she said.

The new Sutter Alpine Care Center is bringing more top-quality orthopedic care to the Stockton and San Joaquin County community. Gould Medical Group is delighted to welcome the Alpine Orthopedics Group, a trusted name in orthopedics with deep roots in the community. Sutter is committed to delivering more access to timely, state-of-the-art care to help our patients feel their best.
See how we care at sutterhealth.org/alpine
2488 N California St., Stockton, CA 95204





A PLACE FOR ALL NEWS HIGHLIGHTING RESIDENTS AND GRADUATE MEDICAL EDUCATION
The Resident’s Report is dedicated to all the good news related to our hard-working residents training at San Joaquin General Hospital and St. Joseph’s Medical Center. Please email your submissions, written in third person with accompanying photo to Lisa@sjcms.org.
In July, St. Joseph’s welcomed its new class of residents and fellows, with 90 new members of the Graduate Medical Education program in nine residencies and four fellowships for the 20252026 Academic Year. For the incoming class, St. Joseph’s welcomes 59 Californians, including 16 from the Central Valley area, 20 Northern Californians, and 18 previous medical student rotators and two former residents.

St. Joseph’s rapidly-growing Graduate Medical Education program, which was launched in 2018, helps train and retain physicians in San Joaquin Community and to maintain and expand services we offer to our community. Current Residency and Fellowship specialties include Anesthesiology, Cardiovascular Disease, Child and Adolescent Psychiatry, Critical Care Medicine, Emergency Medicine, Family Medicine, Internal Medicine, Medical Simulation, Neurology, Orthopedic Surgery, Psychiatry, Transitional Year, Ultrasound, and Urology. Ultimately, St. Joseph’s will have over 300 residents and fellows by 2028.

St. Joseph's Internal Medicine Residency Program proudly recognizes the recent graduates and celebrates their accomplishments. The following physicians have chosen to continue serving in the San Joaquin Valley or to further their training through fellowship programs here in the Central Valley.
Onkar Mudhar, MD
CLASS OF 2023
Dr. Mudhar is currently working at Doctors Medical Center in Modesto, Emanuel Medical Center in Turlock and Doctors Hospital of Manteca, CA.
Manpreet Bains, MD
CLASS OF 2023
Dr. Bains is currently working at Adventist Health Lodi Memorial in Lodi, CA
Misael Betancourt Flores, MD
CLASS OF 2024
Dr. Betancourt Flores is currently working at Adventist Health Lodi Memorial in Lodi, CA.
Madalyn Rivas, MD
CLASS OF 2024
Dr. Rivas is currently working at Adventist Health Lodi Memorial in Lodi, CA
Urooj Zahid, DO
CLASS OF 2024
Dr. Zahid will be working as Academic hospitalist in a Teaching Hospital in Central Valley, CA
Caroline Tashdijan, MD
CLASS OF 2023
Dr. Tashdijan is currently pursuing a Critical Care Medicine Fellowship at St. Joseph’s Medical Center.
Arshi Jha, DO
CLASS OF 2024
Dr. Jha is currently pursuing a Cardiovascular Disease Fellowship at St. Joseph’s Medical Center.
Shubani Singh, MD
CLASS OF 2025
Dr. Singh is currently pursuing a Critical Care Medicine Fellowship at St. Joseph’s Medical Center.














Free to SJMS/CMA Members!

The Office Managers Forum empowers physicians and their practice manager staff with valuable tools via expert led education sessions from industry professionals who are committed to delivering quality healthcare. This quarterly forum is normally held on the second Wednesday of March, June, September and December at Papapavlo's in Stockton.
Registration is required!
If you don’t receive an invitation via E-Mail, please email Jessica@sjcms.org
September 10, 2025: 11:00AM to 1:00PM
This workshop provides up-to-date changes and practice requirements to meet the Annual OSHA mandates.
Topics included: Bloodborne Pathogens, Aerosol Transmissible Disease Guidelines, Violence in the Workplace, as well as several other OSHA related topics.

Carrie Champness, RN, BSN Safety Compliance SpecialistCarrie has been an OSHA compliance specialist for over 35 years and provides up-to-date information about changes and practice requirements to meet all OSHA mandates.
December 10th, 2025: 11:00AM to 1:00PM

Join us for our annual Medicare Update workshop for physicians and office staff. This 2 hour seminar will cover relevant information about current, future and proposed changes for the coming year!
Cheryl Bradley- Associate Director of CMA’s Center for Economic Services
UHC delays Designated Diagnostic Provider program in CA until Jan. 1, 2022
What You Need to Know: Anthem Blue Cross is
now enforcing a policy requiring physicians to include the appropriate gestational age ICD-10 Z3A diagnosis code on all professional maternity delivery claims. Many practices—unaware of the rule—are now facing retroactive repayment demands, adding significant administrative strain through appeals, claim corrections and repayment processing.
Anthem Blue Cross recently began enforcing a maternity claims policy that is creating significant administrative and financial burdens for physicians. The policy outlined in the Anthem California Facility and Professional Provider Manual, requires physicians to report the gestational age at delivery on all professional maternity claims by including the appropriate ICD-10 Z3A diagnosis code. Many practices—unaware of the requirement—are now receiving repayment demands on previously paid claims, triggering time-intensive dispute resolution, rebilling and payment reconciliation work.
This requirement applies to the following CPT® delivery procedure codes: 59400, 59409, 59410, 59510, 59514, 59515, 59525, 59610, 59612, 59614, 59618, 59620, and 59622.
While Anthem updated its provider manual in January 2020 to include this requirement, the California Medical Association (CMA) has raised concerns that the change was not clearly communicated to physicians. If the policy had been properly enforced, impacted claims should have been denied upon submission rather than paid and later subject to recoupment. Instead, Anthem just recently began enforcing the policy, applying it retroactively, and forcing practices to absorb the administrative burden of appeals, corrected claim submissions and repayment demands. The lack of timely notice and clear guidance on how to address these recoupments has left many practices scrambling to resolve claim issues and ensure proper payment.
CMA is seeking clarification from Anthem on the five-year lapse in policy enforcement, the lack of clear notice to physicians and the steps practices should take to submit corrected claims to ensure proper reimbursement.
Given the potential financial and operational impact of overpayment recovery efforts, it is essential for affected physicians to respond promptly and appropriately to overpayment notices. Under California law, physicians who disagree with an overpayment request must initiate a dispute within 30 working days from receipt of the notice. Failure to do so may result in Anthem withholding funds from future payments.
Fully insured health plans may request refunds within 365 days from the date of payment, except in cases of fraud or misrepresentation. When attempting to recoup, health plans are required to issue a written request that clearly identifies the claim in question, including the patient’s name, date of service, and a detailed explanation of the reason for the overpayment. Physicians then have 30 working days to dispute this request.
For providers dealing with ERISA self-insured plans, contracted providers have up to four years to pursue refunds, while non-contracted providers have two years.
If a health plan attempts to recover funds outside of these timeframes, or if the plan fails to provide the necessary notice and opportunity for dispute, physicians are encouraged to challenge the request in writing.
CMA’s reimbursement experts are available to support practices as they navigate the challenges posed by Anthem’s enforcement of this policy. Members can contact the CMA Center for Economic Services at economicservices@cmadocs.org or (800) 786-4262.
Additionally, physicians may find valuable information on their rights and options for handling health plan refund requests in CMA health law library document #7512, “Plan Requests for Refunds from Physicians.” This document is available free of charge to CMA members, and nonmembers may purchase it for $3 per page.
What You Need to Know: A federal antitrust lawsuit against MultiPlan and several major insurers is moving forward, alleging a price-fixing scheme that systematically underpaid out-of-network physicians. The case could result in substantial financial recoveries for affected providers, and CMA is hosting a webinar to help practices determine eligibility and protect their rights.
A sweeping federal antitrust case against MultiPlan, Inc. and several major payors is moving forward after a significant win for plaintiffs in June. The MultiPlan multidistrict litigation (MDL No. 3121), pending before
Judge Matthew F. Kennelly in the Northern District of Illinois, alleges that MultiPlan and other major insurers including Aetna, Cigna, UnitedHealth, and Blue Cross Blue Shield conspired to systematically underpay out-of-network health care providers through price-fixing and other anticompetitive practices.
According to the complaints, these payors outsourced rate-setting to MultiPlan, which used proprietary pricing to artificially suppress out-of-network payment rates. By pooling sensitive pricing data and imposing common methodologies and price caps, the defendants allegedly eliminated market competition, depriving physicians of fair payment for services and generating profits from administrative fees tied to the underpayments.
In April 2025, the U.S. Department of Justice filed a Statement of Interest supporting the plaintiffs’ legal theory—underscoring that coordination among competitors through a third-party intermediary can violate antitrust laws. In June, Judge Kennelly denied the defendants’ motion to dismiss, allowing the case to proceed to discovery. Physicians who have received out-of-network payments priced by MultiPlan could be eligible for damages—potentially tripled under federal law—and injunctive relief to end the alleged practices.
The plaintiffs are seeking compensation equal to the difference between actual payments and the fair market value of the services provided. If successful, the case could lead to significant reimbursements for participating providers and drive changes in how outof-network rates are determined nationwide.
Physicians may not always know whether MultiPlan priced their claims. Clues can often be found in explanations of benefits or remittance advice showing references to “MultiPlan,” “Data iSight,” “Viant,” “NCN,” “ProPricer,” or “MARS.” All such claims— including those negotiated or paid under the No Surprises Act—may be eligible to participate in the MDL.
The California Medical Association is hosting a free webinar on Tuesday, Sept. 16, 2025 – Navigating the MultiPlan Litigation: What Physician Practices and Facilities Need to Know. Presented by AGG Healthcare Litigation partner Matt Lavin, a member of the Executive Committee for direct-action plaintiffs in the case. Lavin will walk through the origins of the litigation, key legal developments, strategies for joining the case, and why now is the time to act.





UC Davis Health is an extraordinary place to further your career. You’ll experience being part of an academic medical center that’s committed to advancing pioneering research, promoting a sense of belonging through an inclusive work environment, and fostering continuous learning to develop health care leaders.
UC Davis Health offers robust benefits, including:
■ Competitive compensation
■ Retirement and savings investment plans, including UC’s defined-benefit pension plan
■ An emphasis on work-life balance
■ Access to wellness programs, state-of-the-art facilities, and more

BY JOAN DUWVE, MD, MPH; KING LOMOTOS, MPH, CIC; THERESA FOURNIER, MPH
Seasonal influenza remains a major public health concern, contributing to significant morbidity and mortality each year. According to the World Health Organization (WHO) and the Centers for Disease Control and Prevention (CDC), influenza causes an estimated 290,000 to 650,000 respiratory deaths globally each year. In the United States, the CDC classified the 2024-25 flu season as high severity overall across all ages, with preliminary estimates of at least 47 million flu-related illnesses, 21 million medical visits, 610,000 hospitalizations, and 27,000 deaths.
Of those deaths, 266 were pediatric deaths, the highest number reported in any non-pandemic flu season since pediatric flu deaths became nationally notifiable in 2004. More than 40% of the children who died had no known high risk underlying medical conditions. Nine out of 10 pediatric deaths attributed to influenza occurred in children eligible for flu vaccination who were not fully vaccinated.
National Syndromic Surveillance Program data and corresponding data from one participating hospital in San Joaquin County show a significant increase in the percentage of emergency department visits for children younger than 5 years of age during the 2024-25 influenza season while Laboratory-Confirmed Influenza Hospitalizations in California were notably higher for those 65 years of age and older.
According to national U.S. Outpatient Influenza-like Illness Surveillance Network (ILINet) data, the percentage of outpatient visits for respiratory illness attributable to young and school-aged children remained significantly higher than those for all other age groups throughout the 2024-25 flu season.
Vaccination remains the cornerstone of influenza prevention and everyone 6 months of age and older should receive a flu vaccine every year. Although some people who get a flu vaccine will still get the flu, the vaccine reduces the risk of severe illness, hospitalization, and death due to flu and its complications - especially among those at high risk, including young children, adults 50 years and older, people with chronic diseases or who are immunocompromised, and individuals who are pregnant.
In California, more than 72% of adults over 65 received a flu vaccine during the 2023-24 flu season. Yet only 46% of adults 50-64 were vaccinated, despite one-third of the people in this age group living with underlying medical condition that put them at higher risk for flu-related complications.
Influenza vaccination significantly lowers the risk of influenza-associated hospitalizations and severe respiratory illness in pregnant individuals and reduces the risks of influenza-related preterm birth and low birth weight. Maternal antibodies are transferred through the placenta, providing passive immunity to the infant during the first 6 months of life, before the baby is old enough to be vaccinated. The inactivated influenza vaccine (IIV) can be administered anytime during pregnancy, has an excellent safety profile during any trimester and is not associated with increased risk of congenital anomalies.
The 2024-25 flu season was also severe in San Joaquin County. As of July 25, 2025, the 2024-25 influenza season was listed as a cause of death for 1607 Californians, 30 of whom were under the age of 18. Twenty-seven of those deaths were San Joaquin County residents, 81% of whom were over the age of 50 and 19% were between the ages of 19 and 49.,
Despite advancements in prevention and treatment, rates of influenza illness and death continue to place a strain on communities, healthcare systems, schools, and families. Fortunately, healthcare providers are uniquely positioned to change the trajectory of these impacts on our county by promoting influenza immunization to their patients.
Cocooning infants by vaccinating parents, siblings, and grandparents is the best way to keep the entire family healthy. Children who attend daycare or school are frequently exposed to respiratory illnesses and are often the source of influenza virus transmission within households. Children under 5 years of age and those with underlying conditions such as asthma, diabetes, or congenital heart disease, are more susceptible to influenza and its complications.
Annual influenza vaccination is recommended for everyone, 6 months of age and older. For children under 9 years receiving the vaccine for the first time, two doses (at least 4 weeks apart) are required for the vaccine to be effective. Yet, according to the CDC National Immunization Survey-Flu of households with children ages 6 months -17 years conducted between October 2024-June 2025, only half of California children had received a flu
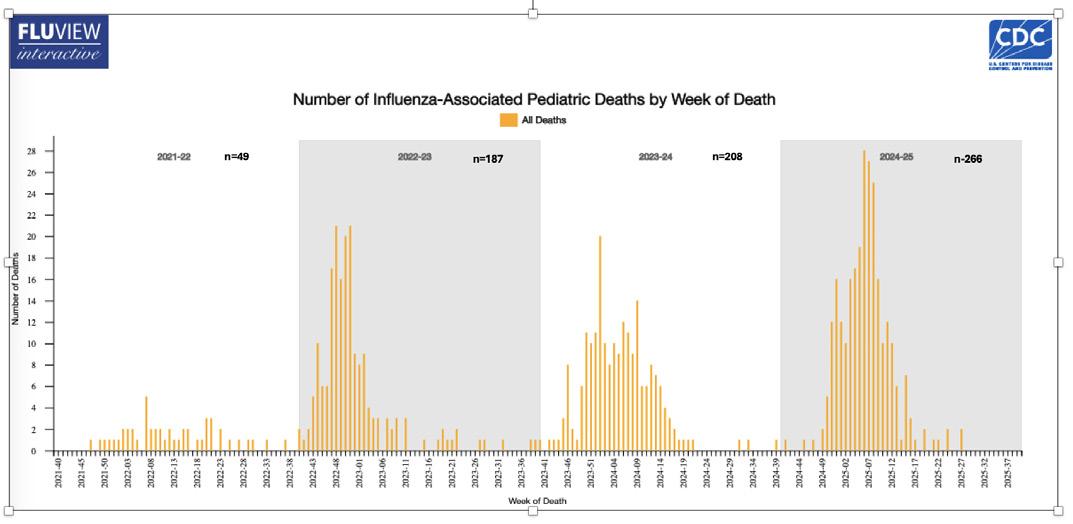
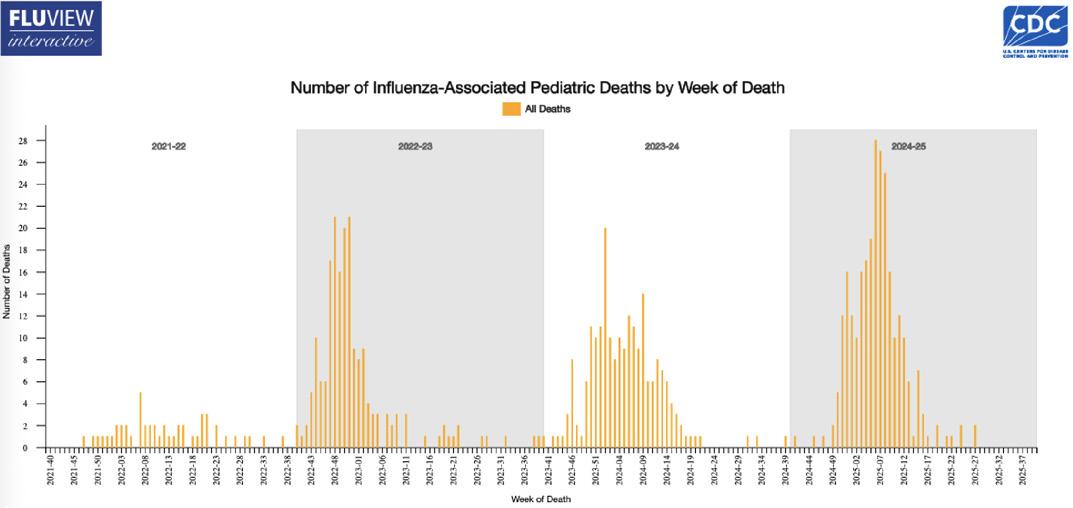
shot during that period. This mirrored the vaccination rate of children nationally and reflects a 14.5% decrease in childhood flu vaccinations since 2020.
In California, more than 72% of adults over 65 received a flu vaccine during the 2023-24 flu season. Yet only 46% of adults 50-64 were vaccinated, despite one-third of the people in this age group living with underlying medical condition that put them at higher risk for flu-related complications. Influenza vaccination prevents millions of illnesses and thousands of hospitalizations in adults aged 50-64.,
As a health care provider, your strong recommendation is a critical factor in helping your patients decide to get a flu vaccine. Research indicates that most adults are likely to get their flu vaccine or have their children vaccinated if their doctor or health care professional recommends it to them.A CDC survey found that flu vaccination was highest among those with a provider offer or referral for vaccination (62.3%) compared with those who reported receiving a provider recommendation but no offer or referral (31.8%) and no recommendation (12.2%).
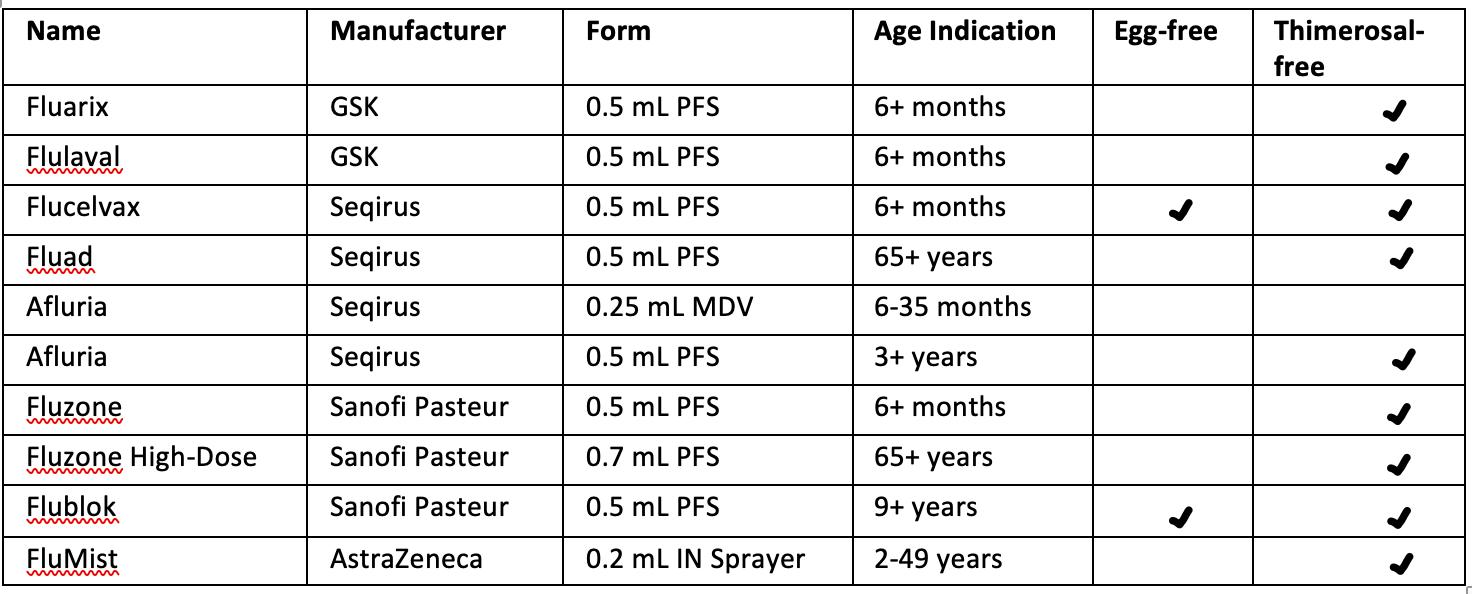
FluMist is a Live attenuated influenza vaccine and is contraindicated during pregnancy.. For a list of contraindications to influenza vaccine, please go to the CDC website.
Influenza vaccines available during the 2025-26 flu season (Table 1) will now all be trivalent. The influenza A (H3N2) component has been updated, while the influenza A (H1N1) and influenza B Victoria lineage components are unchanged.
Conclusion
Seasonal influenza remains a significant clinical and public health challenge, particularly for vulnerable populations such as pregnant individuals, children, and older adults. As trusted sources of information, a strong recommendation for flu vaccination by physicians in San Joaquin County will help increase vaccination rates, and decrease the incidence of flu illness, transmission, hospitalization, and death among the most vulnerable members of our community.