magazıne WINTER 2022
Martha Jefferson PLUS: Better Surgery Through Technology Genetic Counseling: Knowledge is Power | At the Ready for Student Athletes STEP-BY-STEP SUCCESS HOW THREE NURSES BUILT THEIR CAREERS
Sentara
Rita Bunch
President, Sentara Martha Jefferson Hospital
SENTARA MARTHA JEFFERSON BOARD
Carol Hurt | Chair
Lillian BeVier
Robert Broermann
Rita Bunch, President Joshua Fischer, MD
Paul Gaden Michael Gentry John Ligush, MD Lawrence Martin Douglas Moyer E. Ray Murphy
SENTARA MARTHA JEFFERSON ADMINISTRATORS
Rita A. Bunch, MPH, FACHE President
Amelia S. Black DNP, RN, NEA-BC Vice President, Chief Operating Officer
Johnsa Morris, MHA, MBA, RN, NEA-BC Vice President of Patient Care & Chief Nursing Officer

Paul Tesoriere, MD , FHM, FACP Vice President, Chief Medical Officer
SENTARA MARTHA JEFFERSON MAGAZINE
EDITOR
Alyssa Pacheco
CONTRIBUTORS
Luanne Austin Kristen Kirk Preston Knight Lisa Smith Jennifer Stover
PHOTOGRAPHY
Andrew Shurtleff
Tommy Thompson
DESIGN
Picante Creative
A Multitude of Blessings
As we close out 2022 and I approach the end of my first year with Sentara Martha Jefferson, I find myself reflecting even more on the things for which I am grateful. Anyone who knows me knows that gratitude is fundamental to who I am, and when I take a moment to consider the work of our team and how we all contribute to our mission to improve health, it is easy for me to identify so many blessings.
Every team member at Sentara Martha Jefferson fosters a culture of gratitude and support by passionately putting our Caring Tradition into action, through exceptional teamwork, our supportive caregiving environment and our patient outcomes. We also work to strengthen the Caring Tradition by supporting the growth of our team members, including the encouragement of career advancement from within, as you’ll see on page 24.
The passion of our team members is also evidenced in the accolades Sentara Martha Jefferson continues to receive. This year we were honored with a five-star quality rating from the Centers for Medicare and Medicaid Services, a grade of A in both the spring and fall 2022 Leapfrog Hospital Safety assessments, and several other awards and accreditations, as you’ll see on page 4. Without the dedication of our team members, none of these achievements would be possible.
As you may recall from our spring 2022 issue, colleagues from numerous Sentara Martha Jefferson departments recently came together to introduce robotic-assisted surgery to the hospital. Thanks to the efforts of those who led the charge to introduce such state-of-the-art techniques and procedures, our team is now able to make fundamental transformations in patients’ lives. On page 19, you’ll read about the successful outcomes of two patients who benefited from this new technology.
Beyond the important work our team members carry out inside the hospital, though, we also strive to keep an eye on the well-being of our community as a whole. Along with our community partners, including the Blue Ridge Health District and UVA Health, we recently completed the Community Needs Health Assessment (CHNA). This assessment, which takes place throughout our health district every three years, results in a data-driven analysis of our community’s health needs, as well as recommendations for where we should be concentrating our efforts. The current assessment identified three crucial policy targets:
• Transportation, including working to ensure that our community members can get to the health services they need
• Digital access and literacy, allowing individuals to bypass transportation limitations in favor of telehealth visits
• Healthcare and mental healthcare access, including:
○ Workforce (increasing the number of providers)
○ Medicaid, health insurance and payment
○ Referral and communication networks
As you’ll read on page 28, our community health team, which is highly engaged in the CHNA process, works diligently to align its strategies with these focus areas. This team, operating through the Sentara Starr Hill Health Center, has grown significantly over the past decade, offering an increasing array of services to help community members make wiser choices that lead to healthier, more fulling lives. In 2020, for example, the team pivoted in response to the COVID-19 pandemic to provide free online classes and continue chronic disease prevention education through the First Tuesday Educational Series, which covers a wide variety of topics.
And as grateful as I am for our team, I want to also thank you, our community, for everything you do to support our local hospital. Together we can continue to build a solid, caring, successful legacy of quality health care that will serve the needs of our community for many years to come.
Wishing you a healthy, happy holiday season!
Rita Bunch
President, Sentara Martha Jefferson Hospital
PRESIDENT’S
LETTER

WINTER 2022 CONTENTS Features 19 Better Surgery Through Technology Taking minimally invasive procedures to the next level 24 Step-by-Step Success How three nurses built their careers 28 A Community Success Story Sentara Starr Hill Health Center takes aim at chronic diseases 28





2 | WINTER 2022 CONTENTS Departments President’s Letter Inside front cover 3 The Best Medicine 4 New & Noteworthy 6 Provider’s Perspective 9 On-Call Advice 11 Improve Health Every Day 14 Eat Well, Live Well 17 Sentara Cares 33 Clinical Excellence Genetic Counseling: Knowledge is Power 36 Health Matters Colon Cancer: Early Detection is the Best Protection 37 La Salud Importa Cáncer de Colón: La detección temprana es la mejor protección 38 Sentara in the Community At the Ready for Student Athletes 41 Caring Tradition 14 36 41 33 x 38
Staying Safe in Your Winter Wonderland
My previous column, which provided summer health tips, was a huge success—and by “huge success,” I mean nobody threatened to sue me after following my advice. So I thought I would now share my wisdom related to the upcoming winter months and the holiday season.
Let’s start with the topic of food. Tip #1: When you sit down to eat your big holiday meal, try not to take the names of the dishes literally. Take stuffing, for example. Unless you’re a taxidermist working on yourself, it’s not an invitation to literally stuff your body full of this tasty treat, despite the temptation to do so. And please, if there are peas on the table, do not take this as a literal directive.
Which brings us to New Year’s Eve and tip #2. For many, the top health risk on Dec. 31 isn’t foodrelated, but drink-related. Many people assume the physical laws of the human body don’t apply on holidays and assume it’s not possible to drink too much on New Year’s Eve—because, you know, it’s New Year’s Eve. But I’m here to tell you, alcohol is not known for keeping a calendar. Even if it did, it would probably forget what day it was—since, you know, it’s alcohol.
Now, I’m not one who tends to overimbibe. A wild night for me, in fact, is two glasses of wine. One New Year’s Eve, however, I ate at a restaurant where they paired a cocktail with each course of dinner. That would have been fine if I were at my favorite fast-food chicken place, since a chicken dinner is just one course (or, at least, it comes in one box). But this restaurant had so many courses that after I drank the accompanying cocktails, I walked down a flight of steps in the restaurant and literally couldn’t figure out how to get back up.
Steps are pretty straightforward and rarely require an instruction manual, but for whatever reason, I was completely befuddled. I tried calling out, “but it’s New Year’s Eve,” and that’s when I realized that the alcohol didn’t care.
Moving from culinary concerns to weather, winter often brings with it a snowfall or two (or several). When the forecast calls for a lot of heavy snow, I often shovel my driveway when it’s only partially covered, even if it’s still snowing. My neighbors laugh at me as I’m shoveling while the flakes are still coming down—but when the heavy stuff is over, the remaining accumulation is much more manageable for me, whereas they’re now stuck dealing with dangerously heavy piles. Personally, I would rather shovel the equivalent of two light snowfalls than struggle with one that could injure my back. So who’s laughing now, neighbors? (Actually, they probably still are, because I usually fall down while shoveling, and not because I’ve been drinking.)
Which brings me to the topic of black ice. The ninja of weather risks, black ice can be right in front of you, and you won’t even know it’s there. It may not technically know karate, but black ice can throw you to the ground quicker than Bruce Lee in combat with Humpty Dumpty. Since you don’t want to have doctors trying to put you back together again, remember that if it has been below freezing outside, be extra careful where you step. You know the saying, “Dance like no one is watching”? My advice with black ice is to walk like your neighbors are watching. Because they always are.
Have a wonderful—and safe—winter!
sentara.com | 3
THE BEST MEDICINE BY MICHAEL CORDELL
new & noteworthy
To get connected with one of our providers, or for more information on any caregiver at Sentara Martha Jefferson, please call 1-800-SENTARA.
Get with the Guidelines
Sentara Martha Jefferson has received the American Heart Association/ American Stroke Association’s Get With the Guidelines®–Stroke Gold Plus/Target: Stroke Honor Roll Elite/Target: Stroke Advanced Therapy/ Target: Type 2 Diabetes Honor Roll Award. The award recognizes Sentara Martha Jefferson’s commitment to ensuring that stroke patients receive the most appropriate treatment, according to nationally recognized, research-based guidelines using the latest scientific evidence. Congratulations, and thank you to our team members! It takes highly committed teams to achieve such levels of recognition.
National Accreditation for Rectal Cancer Treatment
Sentara Martha Jefferson Hospital earned a three-year accreditation from the National Accreditation Program for Rectal Cancer (NAPRC), a quality program of the American College of Surgeons.
Arthur Bender Quality Award

Congratulations to Dr. Erika Struble, recipient of the 2022 Arthur Bender Quality Award. This award is given annually to a physician on the medical staff of Sentara Martha Jefferson Hospital who has provided outstanding service to our community, improving the quality of care we offer our patients.

Thank you for your continued care for and dedication to our community!
To achieve voluntary NAPRC accreditation, a rectal center must demonstrate compliance with the NAPRC standards addressing program management, clinical services and quality improvement for patients. Centers are required to establish a multidisciplinary rectal cancer team that includes clinical representatives from surgery, pathology, radiology, radiation oncology and medical oncology.
“We are proud to be among the leaders in the field of rectal cancer who have earned the rigorous NAPRC accreditation,” says Zachary Gregg, MD, who led the team through the multiyear accreditation process. “This accreditation helps to showcase that our team has the necessary tools to get our patients through a difficult disease process.”
Accreditation by the NAPRC is granted only to those programs committed to providing the best possible care to patients with rectal cancer.
“This accreditation is a testament to our commitment to multidisciplinary rectal cancer care and our team’s dedication to ensuring that we provide the best patient care for our community,” says Laura Kavanagh, regional director for oncology for Sentara Healthcare. “Accreditations such as NAPRC help patients gain an extra level of comfort from knowing they’re being treated by an accredited site of excellence for rectal cancer.”

4 | WINTER 2022
Sentara Martha Jefferson Cardiology Program Among Nation’s Top-Performing Hospitals for Heart Attack Patients
Sentara Martha Jefferson has received Platinum recognition by the American College of Cardiology’s NCDR Chest Pain-MI Registry Performance Achievement Award for 2022. Seven Sentara Healthcare hospitals received the Platinum Award—the highest achievement, which is bestowed upon just 240 hospitals nationwide.

This is the 10th-consecutive year the American College of Cardiology has recognized Sentara Martha Jefferson’s commitment to and success in implementing a higher standard of care for heart attack patients.
Serenity Garden Dedicated to Team Members

The Serenity Garden, made possible by a leadership gift from The Joseph and Robert Cornell Memorial Foundation and donations through the Martha Jefferson Hospital Foundation COVID-19 Emergency Response Fund, is a purpose-built space where staff, patients and patient family members can rest and reflect, just a few steps from the Intensive Care and Cardiac units at Sentara Martha Jefferson. A major goal of the new garden is to help reduce burnout and boost health and wellness for our professional caregivers. Since the start of the pandemic, community philanthropic support has made possible many new investments in staff wellness and resiliency at Sentara Martha Jefferson.
The Sentara Martha Jefferson Intensive Care Unit (ICU) recently installed an electronic intensive care unit (eICU) system known as Equum Medical. This telemedicine technology will assist the caregiving team by adding another layer of care for all of the hospital’s ICU patients.
ICU Gains Assistance with eICU Monitoring
Using the technology, the Equum Medical eICU team receives and analyzes patient information such as vital signs, laboratory results and X-rays to help determine and provide the very best possible care. The system enables Equum team members to view and speak with Sentara Martha Jefferson providers, patients and family members at the ICU bedside via a special monitor mounted in the patient’s room.
In addition, the eICU team uses the system to make rounds multiple times each night to check on patients. Importantly, however, the cameras face inward toward a wall when not in use, and no temporary or permanent recordings are made from the camera or microphone. As well, several additional measures have been taken to ensure patient privacy, including the encryption of all medical information, which is transmitted over secure, private data lines (not over the Internet).
sentara.com | 5
Melodious Speech:
A Valuable Health Goal
Along with Western medicine, I regularly practice yoga to help me improve my health and well-being. More than just stretching, yoga also addresses more complex and seemingly unconnected functions like speech—specifically, according to ancient texts, “melodious” speech. The first time I read about this concept, I was perplexed. I thought: “Melodious? To speak like a melody in a song?”
But when I learned the science behind the connection between body and voice, I realized how much sense it made. Yoga helps us achieve and maintain an upright spine, allowing the neck to give ample support to the throat. As a result, the muscles of the mouth and face are able to relax, and the breath to flow more evenly. The result? A more pleasant-sounding voice.
Give this a try: If you grimace or scowl, what tone does your mouth make when you speak? How about when you

smile in a relaxed way? Take note of the important differences in your voice.
According to John Hopkins University, “Your voice is the sound that air makes when forced out of your lungs and passes over your vocal cords … The vocal cords can be stressed by using too much tension when speaking

PROVIDER’S PERSPECTIVE
Alex McGee, MDiv, BCC Sentara Martha Jefferson Hospital
6 | WINTER 2022
… Vocal misuse is anything that strains or harms the vocal cords, such as too much talking, shouting, or coughing.”
Now, even with all of my decades of practicing yoga, I still have room for improvement. During the pandemic, I have been challenged in new ways, struggling to feel peaceful or centered and often finding it difficult to speak in soothing ways.
One major challenge I have experienced during the pandemic has to do with wearing masks. Masks tend to squeeze my face and don’t fit as well when I smile. As a result, I realized that I had largely given up smiling. Naturally, that tendency backfired in terms of my speech, since the muscular act of smiling tends to make one’s voice gentler. Further, even though the masks cover the mouth’s smile, other people were missing out on the “smile” in my eyes.
A second challenge I have faced involves the use of safety measures in the hospital. In
order to project through the multiple layers of equipment— the N95 mask, the procedure mask and the face shield, when needed—I’ve had to strain my vocal cords and enunciate in an exaggerated manner in order to be heard. In fact, sometimes I’ve had to resort to “barking,” which causes the vocal cords to be strained while I am trying to communicate clearly.
A third challenge has been the stress involved with certain topics of conversation and the many unknowns surrounding the pandemic. Whether in the grocery store or in the often stressful hospital environment, many of us have often felt on guard during the more deadly times of the pandemic. And with many differing beliefs and behaviors, some topics of conversation have led to interpersonal tension.
These three challenges illuminate some truths about the
basic human needs to be heard, feel safe and relate to others. During the pandemic, these three needs have often been in conflict. For instance, wearing masks has made it harder to feel heard, easier to feel safe and harder to relate to others. As is so often true, our physical and psychological health overlap.
Medical scholars around the world have also been exploring these challenges during the pandemic. The Journal of Voice, which publishes peer-reviewed international research, recently published an article on “Vocal Health and Stress” by Dr. Carillo-Gonzalez, who pointed out: “the prolonged use of the mask could represent a risk for developing voice disorders due to vocal misbehavior, such as speaking very loudly or with poor intelligibility, having to constantly repeat messages, and consuming fewer glasses of water as a result
sentara.com | 7
of having the mouth region under restraint.”
Medical leaders have noticed particular challenges for people whose jobs require them to use their voice frequently. To address the issue, Carillo-Gonzalez suggests that people who need to speak a lot during their workday “must receive training support, instructions that help them speak slower during communicative interaction, muscle relaxation and mindfulness techniques.”
In response to these challenges, many organizations are now developing ways to help employees adapt.

The good news is that establishing and practicing healthy voice habits can help. Western medicine, along with other sources of wisdom, encourages:
• Hydration: Although drinking fluids is difficult to do regularly while wearing a mask, sipping water or herbal tea frequently can help you feel better.

• Using a moderated voice: Even though masks and COVID safety measures present challenges, try to make adjustments to avoid
yelling, or speaking so loudly that the vocal cords become strained.
• Vocal rest: Taking a break from speaking may require trade-offs, such as doing less of a particular activity, in order to preserve your voice in the long run.
• Exercises: Try a “yawnsigh,” in which you spread your mouth wide and let out a long exhale, or try the yoga practice of chanting mantras.
The intersection of physical, emotional and mental health is becoming even clearer to me. Ease in one area leads to ease in the other areas. And ease in the mind, emotions and body leads to a voice that feels better. So, my lesson going forward is to double down on practicing my gentle speech—both for my health and the well-being of those around me.
8 | WINTER 2022
PROVIDER’S PERSPECTIVE
Please explain what diverticulitis is and how it’s treated.
Diverticulitis refers to inflamma tion or infection of the small pouch-like recesses, called diverticula, that can form in the digestive tract— especially in the lining of the colon, the lower portion of the large intestine. No one knows why these marble-sized pouches form, but a low-fiber diet may be one cause. Lack of fiber makes the colon work harder to eliminate waste, and this may cause diverticula to form in weak areas of the colon wall. Most people form diverticula at some point—especially after middle age—and most of the time they cause no serious problems.
The cause of diverticulitis is not fully understood, either, but doctors think the condition may arise from bacteria caught in pouches that happen to tear. Risk factors associated with a higher incidence of diverticulitis include age; obesity; lack of exercise; a low-fiber diet; smoking; and taking certain medications like ibuprofen, naproxen, steroids and opioids.
Diverticulitis can be very painful. Typical symptoms include persistent abdominal pain— especially in the lower left side—which may get

worse with movement; rectal bleeding; bloating; abdominal tenderness; constipation or, less commonly, diarrhea; nausea or vomiting; loss of appetite; and fever or chills. Diagnosis is typically based upon a history of symptoms, as well as blood tests and X-rays or computed tomography
Treatment depends upon the severity of the condition. Mild cases usually can be treated with rest, diet modifications, antibiotics and over-the-counter pain medications. In the majority of mild cases treated by these means, symptoms are successfully resolved.
Severe cases may lead to complications that include blockage of the colon; abscess, or the collection of pus in the diverticula; and peritonitis, or rupture of a diverticulum that releases its toxic contents into the abdominal cavity. Peritonitis is a medical emergency that requires immediate attention. Severe cases of diverticulitis may be treated by the insertion of a drainage tube in the case of an abscess, or by surgery if there is blockage, or if there is presence or significant risk of peritonitis.
The best way to avoid diverticulitis is to exercise regularly, eat a high-fiber diet and drink plenty of fluids to help your body handle the increased fiber intake.

sentara.com | 9
Blue Ridge Region physicians of Sentara Martha Jefferson Hospital and Sentara RMH Medical Center answer your health and wellness questions
ON-CALL ADVICE
What is laryngitis, and what causes it?
What treatments are recommended?
Laryngitis is an inflammation of the larynx, the “voice box” that contains the vocal cords. It can be either acute (of short duration), or chronic (of long duration). Laryngitis typically results in a change of vocal quality, often described as hoarseness or a weak voice. Associated symptoms can include dry throat, cough, a tickling sensation that leads to repeated clearing of the throat, and/or a sore throat.
cords and experience laryngitis. Voice changes also may be caused by benign or malignant growths on the vocal cords. Frequently effective self-treatment measures for acute laryngitis include the following: Rest your voice and avoid talking as much as possible to give the inflammation a

Avoid smoking or drinking alcohol or caffeine, since those agents can dry out and
Drink plenty of water and use a humidifier to maintain moisture and lubrication in

Cover your mouth with a scarf or mask when going out in extremely cold weather. Moisten your throat by sucking on lozenges
A healthcare provider should be seen in cases where there is difficulty swallowing or breathing, or if you develop a high fever with laryngitis. Voice change that persists for longer than 3 weeks should be evaluated by a physician to determine the underlying cause.
10 | WINTER 2022 ON-CALL ADVICE
Blue Ridge Region physicians of Sentara Martha Jefferson Hospital and Sentara RMH Medical Center answer your health and wellness questions
Safe Travel During Winter
Winter weather can present serious challenges and dangers to travelers. Avoiding dangerous driving conditions is always a good policy, so as much as possible, stay off the roads when the weather is bad or predicted to be dangerous. If you must venture out, be extra cautious and follow these safe driving tips.
General Advice
• Know your route and keep informed on road conditions and the weather forecast.
• Travel with a fully charged cell phone, and keep family or friends advised of your route, as well as your departure time and estimated arrival time.
• Keep your tires properly inflated, and keep your gas tank at least half-full to avoid frozen gas lines.
• Do not use cruise control when driving in slippery conditions (heavy rain, ice or snow).
Create a Winter Safety Kit

• Keep blankets and extra jackets, gloves and head coverings in your vehicle during cold weather, in case you get delayed or stranded in the cold.
• Take extra snacks, drinks and any necessary medications in your vehicle when traveling in winter.
• Keep a working flashlight and extra batteries in your vehicle at all times, along with a good ice scraper, snow brush and can of lock deicer.
• Take a bag of cat litter in your vehicle for use in gaining traction if your wheels start spinning on ice or packed snow.
While Driving in Adverse Conditions
• Drive slowly, and keep an eye on other vehicles around you.
• Accelerate and slow down slowly and evenly. When on slippery roads, give yourself plenty of room and time to slow down and stop.
• If you start to skid, don’t hit your brakes—instead, gently steer the vehicle in the direction you want to go.
If You Get Snowbound or Stranded
• To conserve gasoline, run the engine just long enough to remove the chill.
• Stay with your vehicle, rather than trying to walk in deep or blowing snow— your vehicle can provide shelter and make it easier for you to be spotted. Tie a colored piece of cloth around your antenna or place it in your window to help make you more visible.
• Make sure your exhaust pipe is not clogged with snow, ice or mud, and keep something in the vehicle that will allow you to unclog the exhaust pipe, if needed.
sentara.com | 11 IMPROVE HEALTH EVERY DAY
Are You Getting Enough Calcium?
You may know that our bodies need calcium to maintain strong bones and teeth, but did you know that calcium also helps our nerves transmit messages throughout the body and helps our blood clot? Since the body loses calcium every day through perspiration, urination and other means—and because the body can’t make its own calcium—we need to replace the calcium we lose each day by eating calcium-rich foods.
How Much Calcium Do You Need?
1,000 mg per day: Women 50 and younger Men 70 and younger
Salmon Sardines Shrimp Soybeans Spinach
Most people probably think of dairy products as good food sources of calcium, but you can also get this essential mineral by regularly eating these calcium-rich foods: Broccoli Collard greens Figs, dried Kale Okra Oranges

1,200 mg per day: Women 51 and older Men 71 and older
Also be sure also to get plenty of vitamin D each day. The body needs vitamin D to help it absorb calcium.
Managing or Avoiding High Blood Pressure
Here are six things you can do to lower high blood pressure or avoid it altogether:

• Lose weight.
• Get regular physical activity— at least 30 minutes most days of the week.
• Don’t smoke.
• Reduce your sodium (salt) intake.
• Drink alcohol in moderation, or not at all.
• Take blood pressure medication, if prescribed, as your doctor indicates. If you have high blood pressure, make sure you take care of it. Not doing so can lead to heart disease, stroke, kidney failure and other serious problems.
IMPROVE HEALTH EVERY DAY
12 | WINTER 2022
TIPS FOR RELIEVING DRY SKIN
As the temperature outside gets colder, we tend to crank up the heat in our homes. But heaters remove moisture from the air, causing our skin to get dry. To prevent dry skin, fine lines and wrinkles, the American Academy of Dermatology recommends a modified skin care routine during colder weather:


Baths and showers. Limit baths and showers to 5-10 minutes, and use warm water rather than hot. Wash with a gentle, fragrancefree cleanser, and lightly blot skin with a towel to dry.
Moisturize immediately. Applying a moisturizer will trap much-needed moisture to help soothe dry skin.
Wear gloves. The hands often are the first place dry skin appears, so be sure to wear gloves while going outside in the winter, performing tasks that may require hands to get wet, and exposing hands to chemicals and greases.
Humidify. During winter the humidity in the air drops, and using a humidifier puts moisture back into the air, helping to fight against dry skin. A simple remedy? Vaseline is an excellent moisturizer, and one of the most economical. It should be applied regularly after a warm bath or shower. And for dry, cracked hands or feet, apply Vaseline liberally before bed and cover with white cotton gloves or socks.
If, despite your best efforts, your dry winter skin doesn’t start to feel better, see a dermatologist, as you may require a prescription ointment or cream. A dermatologist can examine your skin and explore treatment options with you.
sentara.com | 13
IMPROVE HEALTH EVERY DAY
Plant-Based Eating
FOR A HEALTHY HEART
Do you have to become a vegetarian or vegan to benefit from plant-based eating?
Of course not! Introducing a plant-based diet merely means increasing your intake of whole grains, cereals and cereal products, fruits, vegetables, legumes, nuts, and seeds while trying to limit intake of animal products like meat, fish and dairy.
BY SHILA RAJBAHAK, RDN
Why Plant-Based Eating?
For starters, a plant-based diet rich in fruits, vegetables and whole grains can help you increase your fiber intake, which in turn can help improve cholesterol levels by increasing high-density lipids (HDL or “good” cholesterol) and lowering lowdensity lipid levels (LDL or “bad” cholesterol). Additionally, the naturally low cholesterol content of plant foods contributes to a reduction in overall dietary cholesterol intake.
Fruits and vegetables are also abundant in antioxidants, which are thought to protect cells against harmful substances known as free radicals that can play a role in causing cancer and heart disease. Plant-based eating also can help with weight management. In addition, studies have shown that vegetarians generally have higher intake than nonvegetarians of vitamins A, C and E, as well as thiamine, riboflavin, folate, calcium, magnesium and iron.
To help improve heart health, the American Heart Association encourages adopting a Mediterranean-style diet, which is abundant in minimally processed plant-based foods such as

14 | WINTER 2022 EAT WELL, LIVE WELL
fresh fruits and vegetables, nuts and whole grains; rich in monounsaturated fat from olive oil; lower in saturated fat, meats, dairy products, sugary sweets and processed foods; and higher in fish and other seafood. Review of multiple studies from 2019 has shown better cardiovascular health outcomes from Mediterranean and plant-based diets, including reduced rates of coronary heart disease, ischemic stroke and overall cardiovascular disease.
Tips for Implementing a Plant-Based Diet:

Get creative with fruits and vegetables:
• Use fresh fruit as a topping on oatmeal or as a side with toast or pancakes.
• Eat fresh vegetables as a snack or in a salad.
• Use fresh vegetables like spinach and fresh or frozen fruits to prepare a smoothie, and top with nuts and seeds.
Explore different ways to prepare vegetable dishes:
• Boiling and simmering: Make vegetable soups and broth to eat during the colder months.
• Steaming is one of the best cooking methods for preserving nutrients, as it leads to less loss of the water-soluble B vitamins. Steam vegetables like broccoli, spinach, lettuce, corn and green beans to accompany your meal.

• Microwaving is an easy and convenient way to cook vegetables when you’re short on time. Choose a microwavable frozen vegetable bag without sauce, to keep sodium levels down.
• Grilling and broiling: While grilling meat in your backyard or on a camping trip, throw in vegetables like zucchini, tomatoes and peppers—rather than packaged foods like chips—to serve as sides.
• Roasting and baking: Roast vegetables when you don’t have much time to prepare. Throw chopped vegetables of your choice on a baking sheet with plant oil (olive or canola) and spices, and let the oven do the work.
• Stir-frying: Taking less time and using less fat, stir-frying is better for heart health than other methods like deep frying. Use a small amount of plant oil to stir-fry with vegetables, meat and a starch of your choice.
Spices and aromatics: The American Heart Association recommends consuming no more than 2,300 milligrams of sodium per day. Instead of salt, use seasonings like garlic powder, onion powder, lemon juice and pepper to flavor vegetables and make them more appetizing. Freshly minced garlic, chopped onions, celery, tomatoes, carrots, mushrooms, parsley, thyme and cilantro also can help enhance flavor without sodium.
Meatless Mondays: Setting aside a day each week to have meatless meals is a great way to eat more fresh vegetables. On these days (Monday or any other day you prefer), you can also use meat substitutes like tofu, chickpeas and seitan (made of wheat gluten) to increase your protein intake.
Alternatives to Dairy Instead of whole milk, dietitians advise using 2% or 1% milk for better heart health. In addition, there’s a wide selection of plant-based milk products available that naturally have lower cholesterol levels and are great alternatives for those who are lactose intolerant. Here’s a quick overview of some plant-based milk options:
• Soy milk: Highest in protein among all alternatives to cow’s milk
• Oat milk: Good fiber content but low in protein
• Rice milk: Comparable in calories to cow’s milk but rich in carbohydrates
• Almond milk: Lower in calories but higher in fiber than cow’s milk
• Coconut milk: Low in calories but rich in saturated fat
sentara.com | 15
Vegan Mushroom Stroganoff

Ingredients
2 tablespoons olive oil
1 large onion, chopped
4 garlic cloves
9 ounces cremini mushrooms, sliced 1 tablespoon flour
1 teaspoon thyme
2 teaspoons Dijon mustard
½ teaspoon black pepper
4 cups vegetable stock
1 teaspoon lemon juice
8 ounces uncooked rotini pasta
Fresh parsley
Directions
1. Heat the olive oil in a pot on medium-high heat, then add the onions and garlic. Saute for 2 minutes.
2. Add the mushrooms and saute for 5-6 minutes until the mushrooms are golden brown.
3. Add in the flour, thyme, Dijon pepper, vegetable stock and lemon juice. Mix everything together and bring the mixture to a boil.
4. Add the pasta, cover the pot and cook on medium-low heat for 8-10 minutes until the pasta is cooked through.
5. Top with fresh parsley and serve immediately.
Nutrition:
Serving size: ¼ of recipe. Calories 269, fat: 9 grams, carbohydrates: 38 grams, fiber: 2 grams, protein: 10 grams
Butternut Squash Soup

Ingredients
2 tablespoons extra-virgin olive oil
1 large yellow onion, chopped ½ teaspoon sea salt
1 (3-pound) butternut squash, peeled, seeded and cubed
3 garlic cloves, chopped 1 tablespoon chopped fresh sage ½ tablespoon minced fresh rosemary 1 teaspoon grated fresh ginger 3-4 cups vegetable broth
Freshly ground black pepper Chopped parsley
Directions
1. Heat the oil in a large pot over medium heat. Add the onion, salt and black pepper to taste. Saute until soft, 5-8 minutes.
2. Add the squash and cook until it begins to soften, stirring occasionally for 8-10 minutes.
3. Add the garlic, sage, rosemary and ginger. Stir and cook for 1 minute, until fragrant. Then add 3 cups of vegetable broth. Bring to a boil, cover and reduce heat to simmer. Cook until squash is tender, 20-30 minutes.
4. Let cool slightly and pour soup in a blender, working in batches as necessary. Blend until smooth. If soup is too thick, you can add an additional 1 cup of vegetable broth.
5. Top with parsley and serve.
Nutrition:
Serving size: 1 cup. Calories: 80, fat: 3 grams, carbohydrates 11 grams, fiber: 2 grams, protein: 3.5 grams.
Like regular cow’s milk, plant-based milk can be consumed plain or added to coffee, smoothies and other recipes. While each type of plant-based milk has its own advantages, soy milk can be a good choice if you’re concerned about not getting enough protein in your diet.
While we’re on the topic of soy and soy milk, I would also like to address some myths and misconceptions about the consumption of soy products. Many people believe—mistakenly—that soy isoflavones have harmful health impacts, including thyroid and breast cancer. However, studies have shown that there is no cause-andeffect link between eating foods like soy milk, tofu, or edamame and getting breast cancer. On the contrary, research has shown that, since soy is high in both protein and fiber, consuming soy products actually can help prevent breast cancer and can have benefits for women with breast cancer.
Reap the Rewards
Working more plant-based foods into your diet isn’t as challenging as you might think! Going totally vegetarian or vegan isn’t necessarily to take advantage of the benefits of a plant-based diet—making just a few small changes to the types of foods you eat can make a big difference and help lead to a lifetime of health benefits. To get you started on the road to healthier eating, try the delicious plant-based recipes on the left.
16 | WINTER 2022
WHO WE ARE
As an organization, we’re driven to improve health every day. And while we meet that mission through the healthcare services we provide to our patients and the coverage we provide to our health plan members, we know that truly improving health every day requires a much deeper commitment within our communities.
WHAT WE DO










Through our grassroots partnerships with organizations throughout Virginia and Eastern North Carolina, we work to:
• Ensure greater access to behavioral health services for children, families and adults.












• Secure consistent, equitable access to nutritious food.
• Support targeted training for skilled careers in high-demand fields.
• Develop emergency and scattered housing solutions.






• Eliminate barriers to care and strengthen the cultural fabric of our communities.

sentara.com | 17
SENTARA CARES
Bringing about long-lasting change locally


entara held two grant cycles in 2022, providing investments to organizations working to advance health equity and create healthier communities. Most recently, 17 organizations in the Charlottesville area received funding totaling more than $400,000. These investments expand on Sentara’s long-standing commitment to address social determinants of health and promote equitable access to care in traditionally underserved communities—efforts strengthened through numerous grassroots partnerships with community and faith-based organizations.


“Addressing the most pressing needs of our communities and improving overall health and wellness are the foundation of our mission at Sentara,” says Sherry Norquist, MSN-RN, Sentara director of community engagement and impact. “We are hopeful that through our ongoing investments and collaboration with community partners and faith-based leaders who share our mission, together we will continue to create opportunities to advance health equity and eliminate disparities in the communities where we live, work and play.”
Sentara prioritizes funding for community partners and initiatives that align with our primary focus areas. The 17 local community partners receiving funding from the fall 2022 Sentara Cares grant cycle include:

All Blessings Flow Inc.
Central Virginia Legal Aid Society

Charlottesville Free Clinic City of Promise
Community Climate Collaborative County of Greene, Virginia Elk Hill

Greene Care Clinic Health Brigade Local Food Hub
On Our Own Charlottesville Piedmont Housing Alliance Piedmont Virginia Community College Educational Foundation

ReadyKids
Restoration and Hope House The Bright Stars Program Virginia Institute of Autism
The Sentara Cares program strives to foster sustainable community partnerships around social determinants of health—specifically housing, food security, behavioral health services, skilled career training and equitable access to care—and we cannot do this work alone.
Our 2023 grant cycles will be open in February for the spring session and June for the fall session. Visit SentaraCares.com to learn more.

18 | WINTER 2022 SENTARA CARES
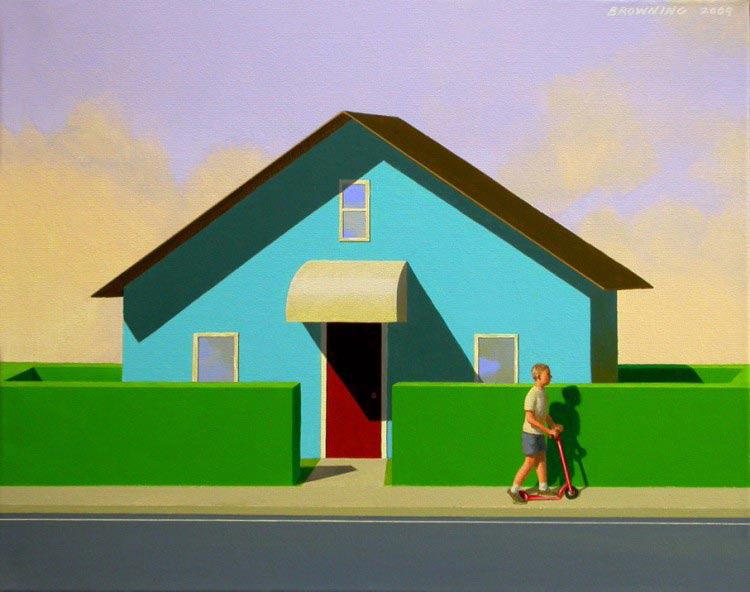
BETTER SURGERY
THROUGH


An advanced new robotic-assisted surgery system, known as da Vinci Xi, is enhancing the surgical care provided at Sentara Martha Jefferson Hospital. Installed in January 2022, this system has already benefited numerous patients, enabling surgeons to carry out complex minimally invasive procedures with greater precision and control, while offering less postoperative pain and faster recovery times.





Sophisticated Robotic System Takes Minimally Invasive Procedures to the Next Level sentara.com | 19
Relief from Reflux






David Jones had suffered from severe heartburn and GERD (gastroesophageal reflux disease, or chronic acid reflux) for years—so severe, in fact, that he had to carry Tums antacid tablets with him everywhere he went. “I had Tums in my vehicle, in my file cabinet at work and next to my bed,” he says. “I had Tums all over the place.”
About 20 years ago, a doctor recommended that Jones have surgery. However, Jones chose not to have the procedure, and his condition gradually worsened. “It would wake me up at night, and I’d end up in my recliner until it subsided,” Jones recalls.

Finally, a gastroenterologist referred him to Mary Vinson, DO, a thoracic surgeon at Sentara Martha Jefferson Medical & Surgical Associates who specializes in robotic surgery. Dr. Vinson recently joined Sentara after an advanced robotics fellowship at St. Joseph’s Hospital in Tampa, Fla., and five years of practice as a robotic surgeon.
Tests revealed that Jones had a hiatal hernia, along with reflux. He also had developed Barrett’s esophagus, a complication of GERD in which the normal lining of the esophagus changes to tissue that is more like the lining of the intestines. Such a diagnosis can be a warning sign, since about 10% of

20 | WINTER 2022
David Jones
people with Barrett’s esophagus go on to develop esophageal cancer. Learning about his condition was a wake-up call for Jones, who lost one of his sisters to esophageal cancer six years ago.

A retired law enforcement officer, Jones, 67, now drives a school bus in Nelson County. Thankfully, he was able to schedule his surgery to take place during the summertime, to avoid missing work as much as possible. During the procedure, Dr. Vinson repaired Jones’ hernia and performed a Toupet (or partial) fundoplication, which tightens the area between the esophagus and the stomach to prevent stomach acid from entering the esophagus.
During robotic surgery, a small 3D camera and tiny surgical instruments are placed inside the








patient using very small incisions. Importantly, the robotic system doesn’t actually perform the surgery—the surgeon controls the instruments during the entire procedure and can view the inside of the patient’s body via a computer screen with close-up 3D images.
Robotic surgery typically results in fewer incisions and quicker recovery times. Following his procedure, Jones returned home after spending just one night in the hospital. He healed quickly and didn’t require any postoperative pain medication—outcomes he attributes to a strong will and good genes. “I think stubbornness had a lot to do with it,” he says. After following a limited diet during his recovery, Jones has since tried pizza, spaghetti
sentara.com | 21
Mary Vinson, DO
sauce and other foods with no issues. Today he’s back to cutting his grass, washing his school bus and enjoying daily walks.
Vinson. “He’s done wonderfully and has no symptoms of reflux. He has been able to advance his diet with ease and bounced back incredibly fast.”
would take up to 25 Tums tablets a day, but now he doesn’t need them at all. In fact, he gave away his last bottle to a co-worker who
was experiencing heartburn. “I ran out to my truck, got the bottle and gave it to her,” he says. “And that was the end of it.”
A few weeks after school started this fall, Jones was back driving his bus. “I’ve got a great group of kids,” he says proudly. “They missed me, and they let me know it.”
Although it took years for him to finally decide on having surgery, Jones is happy he went through with the procedure. “Oh, my Lord, I love Sentara Martha Jefferson Hospital,” he says. “Both my sons were born there, and it is my go-to place. The people are wonderful, from the check-in staff to the nurses, anesthesiologists and doctors.”
Precise Surgery, Great Results




When Mike Tuso needed surgery for inguinal hernias, he had a lot of questions. He got his answers— and a positive outcome—at Sentara Martha Jefferson.

Tuso, 71, and his wife have an active lifestyle, frequently enjoying biking, hiking, traveling and spending time with family. When the hernias first developed, he wasn’t sure what they were and tried to ignore them. Also called a groin hernia, an inguinal hernia occurs when abdominal tissue juts through an opening in the abdominal wall, which separates the abdomen from the groin. “It was a year or two before I realized the hernias were getting bigger, although they weren’t painful,” he recalls. “But obviously there was something going on.” His primary care doctor recommended surgery.
Tuso went to Timothy S. Snow, DO, a surgeon at Sentara Martha Jefferson Medical & Surgical Associates, in early April 2022. Dr. Snow,




22 | WINTER 2022
Before the surgery, Jones would take up to 25 Tums tablets a day, but now he doesn’t need them at all.
David Jones
who was involved in acquiring the da Vinci robot at Sentara Martha Jefferson, had received extensive training on da Vinci sys tems during his fellowship and residency.



Robotic surgery appealed to Tuso, a semiretired electrical engineer who helped design motion-control systems for factories. “I was interested and fasci nated by the capabilities of the da Vinci robotic system,” he says.





That engineering-oriented mind led to a lot of questions for Dr. Snow, who took the time to explain the technical details of the procedure to Tuso. “It was obvious he was really comfortable doing the sort of surgery I needed, and he had done plenty of them before—which is good because experience counts,” Tuso says. “Dr. Snow was confident in the whole process and the outcomes he has had. It was really comforting and wonderful to have that level of commu nication with him.”
Since it was Tuso’s first experience with a surgical procedure requiring general anesthesia, he was somewhat nervous about that aspect of the procedure. To help alleviate Tuso’s concerns, Dr. Snow also put him in touch with the anesthesiologist, who answered all his questions about the anesthesia equipment and procedures. “The doctors and the staff did everything they could to make me comfortable and not worried,” Tuso says.
Tuso had surgery in late April. During the procedure, Dr. Snow inserted mesh into the abdominal wall to strengthen the tissue and prevent the hernias from recurring. “The da Vinci system is a tool that helps enhance the operation,” explains Dr. Snow. “It makes it easier for the surgeon to perform the procedure in a safe manner. Thankfully, it also decreases postoperative pain and is far superior in terms of recovery time.”
While Tuso did experience some pain during his recovery, it was manageable. He had to take it easy and couldn’t lift anything heavy at first, but he started going on short walks one week after his surgery. Six weeks after surgery, he was riding his bike again. “The biggest thing was that for the first month, I had to be careful about the position of my body while I was sleeping,” Tuso says. “If I tried to twist or turn on my side, I could feel a sort of pulling and a bit of pain. You just learn not to do those things, and it slowly gets better.”
Tuso believes it’s important for patients who are facing surgery to do their homework. “Don’t be afraid to ask questions about the number of surgeries they’ve done and the outcomes,” he says. “My wife and I felt like God was with us in our first meeting with Dr. Snow. It seemed like he was the perfect person to do this. Plus, I really appreciated Dr. Snow’s personal empathy, patience and willingness to explain and answer questions.”
sentara.com | 23
Timothy S. Snow, DO
Step-by-Step

 Luis Morales, BSN, RN, CCRN, CMC, was eight months into his nursing career, working in the Med-Surg/Oncology Unit at Sentara Martha Jefferson, when he decided it was time to walk down to the Intensive Care Unit (ICU). His goals for that trip were to speak with the ICU manager, make a solid first impression and explain why he wanted to become a Wendel 1 ICU team member.
Luis Morales, BSN, RN, CCRN, CMC, was eight months into his nursing career, working in the Med-Surg/Oncology Unit at Sentara Martha Jefferson, when he decided it was time to walk down to the Intensive Care Unit (ICU). His goals for that trip were to speak with the ICU manager, make a solid first impression and explain why he wanted to become a Wendel 1 ICU team member.
Success How three Sentara Martha Jefferson nurses have progressed in their careers Luis 24 | WINTER 2022
“I believe I made a good impression,” Morales says. “The ICU manager told me, ‘The pins on your badge speak to your commitment to nursing,’ referring to the pins I had received for DAISY nominations, as well as the pin I received for winning the DAISY award. Then she added, ‘Let’s go ahead and start working on your transfer.’”

Since considering a nursing career, Morales had been interested in getting experience in critical care nursing—a must for being accepted into graduate-level programs in his desired specialty of nurse anesthetist.
Morales had first spoken to Sentara Martha Jefferson ICU leaders at a job fair prior to his graduation in 2016 from Piedmont Virginia Community College (PVCC). While earning his associate’s degree at PVCC, he had thrived during a clinical rotation at the hospital, and the genuine kindness and friendliness of the staff had convinced him that Sentara Martha Jefferson was the place to launch his career.
Just a few years earlier, Morales had been working at a retail department store, stocking shelves and selling electronics. He didn’t have a college degree at that point, and he knew something needed to change. His wife, whom Morales describes as the best nurse he knows, inspired a new path for him. The power of her passion and commitment had always wowed him.
“I thought to myself, ‘You know what? Things will only improve for me if I decide to take charge,’” he remembers. “I decided that getting a college degree was my pathway to a better future.”
So Morales quit his job, enrolled at PVCC and later graduated with
an award for academic excellence in nursing. Three years later, with help from Sentara Martha Jefferson’s tuition reimbursement initiative, he earned his Bachelor of Science in Nursing (BSN) degree online—all while working full time and building a reputation as a dedicated clinician who always advocates for his patients.
Striving Toward a Dream Morales’ nurse manager, Tiffany Fick, RN, has supported him during every step of his career advancement.
In fact, Fick has already written a recommendation supporting Morales’ pursuit of a doctor of nurse anesthesia practice (DNAP) degree—a highly competitive three-year program toward earning the DNAP and CRNA (certified registered nurse anesthetist) designations.
Fick’s encouragement for Morales isn’t a surprise, given her penchant for lending a hand. Morales frequently sees her in scrubs, taking patients to the restroom, covering lunches and watching the monitors when other nurses have to go off the unit with patients. Also impressive to Morales is Fick’s willingness to lend an ear.
“She’s always looking to help her staff in any way she can, and not just from a professional standpoint,” he says. “Tiffany is a great listener. Anytime you approach her with a work concern, it gets addressed—but she’s also willing to step outside her manager role if you want to vent to her about general stuff.”
Once Morales is accepted into a CRNA program, he will likely need to leave his full-time position at Sentara Martha Jefferson, due
to the program’s demanding pace of study, but he will still aim to work part time on an as-needed basis. He hopes to be back at Sentara Martha Jefferson full time someday.
“It’d be an honor to work alongside the surgeons who have known me since I was a new graduate nurse,” he says. “To serve our community as an anesthesia provider at the hospital where I have grown as a professional would be a dream come true.”
Finding the Right Path

Some hospitals would call Amy Hunt, BSN, RN, a charge nurse instead of a unit coordinator, the title to which she was promoted five years ago. During her shifts in the Emergency Department (ED) at Sentara Martha Jefferson, Hunt frequently takes charge, making important decisions swiftly and efficiently.
Following the hospital’s split-flow model, she prioritizes patient care and tracks timelines. With precision and positivity, she diligently works to wipe out the old-school stereotype of the packed, plodding hospital ED.
The irony behind her current level of skill and expertise, though, is that Hunt once lacked the clarity and confidence that now serve her— and her patients—so well.
Fifteen years ago, she took some nursing school prerequisite courses, although she was unsure of her future at the time. Some of her family members were nurses, so she thought it might possibly be a good career path for her. To get some experience in a healthcare setting, Hunt applied for a position as unit secretary at the Sentara Martha Jefferson Urgent Care Center, where she met a nurse named Mary Wolfe.
“Mary pushed me to be a nurse more than I probably would have pushed myself,” Hunt recalls. “She could see that nursing should be my career choice, even if I didn’t know it yet.”
sentara.com | 25
Wolfe kept her eye on Hunt as she grew from support staff to ED technician to full-time ED technician and a full-time nursing student. Hunt’s talent for problemsolving and interacting with patients at the bedside hinted strongly at her potential in the field.


Watching and Learning
Even when a nursing school waitlisted Hunt on two different
occasions, Wolfe told her not to give up and to keep applying. She helped Hunt with applications and letters of recommendation.
As Hunt continued to gain experience, observing the patient care given by veteran Sentara Martha Jefferson nurses like Wolfe was invaluable to her. When she was finally accepted into nursing school, Hunt attended full time, driving two hours roundtrip each
class day. After classes, she would work an eight-hour shift.
Hunt’s follow-up to her associate’s degree in nursing was made possible with a Sentara Martha Jefferson scholarship. Paying little out of pocket, she completed an online RN-to-BSN program while working as an ED nurse. Then she became a preceptor, guiding new grads and new hires. Through years of hard work and dedication, the student had become the teacher.
Flexibility continues to be key for Hunt in maintaining her work-life balance. While pregnant, she switched from night shift to day shift, and then was promoted to unit coordinator following her maternity leave. Over the last five years, she has maintained a good balance, even as she is currently working toward her CEN (certified emergency nurse) certification.
Perhaps when her little one is in school, Hunt will be tempted to pursue a higher management role. She sees others climbing the ladder. Her boss, Courtney Lambert, stepped up from manager to director. A former nurse co-worker earned an educator role. And another staff nurse rose to unit coordinator, educator and finally manager.
“Maybe one day,” Hunt says about the idea of another promotion. “Who knows what the next five to 10 years will hold. For now, I like being a constant for the department—that person who’s fair and consistent. This role itself is meant to grow you.”
Growing Pains and Possibilities

“Nursing can feel very challenging,” Ryan Thompson, MSN, RN, CNL, says.
That’s how he describes his new job as Cardiac Intermediate Care Unit team coordinator, which he started a few weeks earlier. He’s also serving as
Amy
acting manager while the regular manager is out on maternity leave. So, temporarily, Thompson has two roles to fill.
Thompson’s previous manager for 10 years, Dana Graves, continues to check in on him and provide guidance when needed. Graves has witnessed much of his professional journey—from a nursing student in the ICU, to a newly minted floor nurse in cardiac care, to a charge nurse, to unit coordinator, to team coordinator. Under Graves’ tutelage, Thompson received invitations to serve on committees dealing with diversity and inclusion, as well as shared governance. He was also asked to join an aspiring leaders program and become a preceptor.
Five years ago, Thompson’s department welcomed an influx of new hires, so he began orienting nurses about every three months.
“If I’m able to instill in new nurses the things I find most important,” Thompson says, “I find I end up with the best workers.”
His list of imperatives: Be present. Find humor. Connect with patients. Prioritize relationships.
“Building friendships that you can engage with outside of work allows you to feel accepted and bring

more of yourself to your job,” Thompson observes.
For instance, Thompson has biked to work with a co-worker who has become a friend. This year, the floor celebrated three baby showers together. One nurse even had three fellow nurses as bridesmaids and four more team members as guests.
Bonds and Betterment
As important as co-worker relationships is the nurse-patient bond. At one time, Thompson wanted to be a doctor, so he earned a bachelor’s degree in biology to set himself off in that direction. Then he decided to alter his path, with the idea that nurses more often interact with and educate patients.


“Talking to people is one of the things I do well,” Thompson says. “I let people know they’re being
Ryanheard. You don’t always have a lot of time with a patient, but you can still have a meaningful conversation. Just looking a patient in the eye lets that person know that I’m listening.”
Down the road, Thompson might go back to school. For his second go-round as a student, he benefited from a Sentara Martha Jefferson scholarship to earn his master’s degree. In the future, he might tap into tuition reimbursement to earn a doctoral degree that would enable him to teach in nursing school.
“We don’t have enough people in the profession,” Thompson says, “and we also don’t have enough teachers for aspiring nurses.”
Until then, he’ll tackle his new job—a mix of administrative tasks, nurse education and direct patient care—with the same dedication he has given during his 10-year career. He remains focused on making continual progress and, for the moment, wants to concentrate on helping his unit perform as efficiently and effectively as possible.
“Other career opportunities may lie ahead for me,” Thompson adds, “but for now I want to improve some of the processes on our floor and focus on making things better for patients in the here and now.”
sentara.com | 27
A community Success Story
Through free services, Sentara Starr Hill Health Center takes aim at chronic diseases
Since Sentara Martha Jefferson established the Sentara Starr Hill Health Center more than a decade ago, the facility’s free services have been helping community members make wiser choices and lead healthier, more fulfilling lives.

28 | WINTER 2022

sentara.com | 29
Located in Charlottesville’s Jefferson City Center, the Starr Hill Health Center focuses on supporting sustainable lifestyle changes to help prevent and manage chronic diseases like heart disease, diabetes and obesity. Clients can attend cooking classes, group sessions and other supportive services, all free of charge. The center team also offers a five-week class focusing on chronic disease prevention and nutrition.
“I’ve found Sentara Starr Hill is a good way to learn about different things,” says Ruth Williams, a Starr Hill Health Center client who also helps lead a crocheting group at the facility. It’s a great resource, and everything is free for the community. They’re helping me improve and keep up with my health.”
A lot of attention goes toward nutrition, teaching clients how to eat healthier and develop a more sensible meal plan. Clients can even take part in live cooking demonstrations of healthy foods with a local chef— a program that started in early 2022 with about 10 students, including Williams.

“The students really loved the classes, says Setour Dillard, RN, integrated care manager at Sentara Starr Hill. “Each one had his or her own cooking area. They learned about spices, planning, and how to use less salt and fat during food preparation.”
Williams says she appreciates the broad scope of Sentara Starr Hill’s approach to making people healthier.
“I find myself eating more fruit, drinking more water and exercising more these days,” she says. “It’s all been really helpful. I’ve enjoyed it a lot.”
Partnering Up for a Bigger Impact
The first Tuesday of each month, Sentara Starr Hill hosts an online chronic disease education program via Zoom featuring a guest speaker. The program was launched during the pandemic,
as the facility sought innovative ways to continue to be part of clients’ lives, in spite of social distancing needs. The monthly program strives to feature innovative topics, such as acupuncture and meditation, to pique clients’ interests.
30 | WINTER 2022
Additionally, during the height of the pandemic, Sentara Starr Hill assisted more than 1,000 people in receiving COVID-19 vaccinations at the Jefferson School.
“We try to cover all aspects of healthy living to keep people at

their best,” Dillard notes.
Sentara Starr Hill team members aren’t alone in their efforts to improve community health, either—partnerships are paramount to success. That’s why Sentara Starr Hill provides clients with free 30-
day guest passes to the local YMCA and free chair yoga classes at the Jefferson School through the Charlottesville Parks and Recreation Department. The center also partners with the local pastors association to host in-person classes on
sentara.com | 31
chronic diseases and nutrition at area churches.
Dillard says Sentara Starr Hill is far from finished in its quest to connect with the community. While some physicians do refer patients to the center, Sentara Starr Hill relies heavily on word of mouth to increase awareness of its services. Recently, the center has been working to increase its presence in neighborhoods and at various events—bringing its services to clients, rather than waiting for clients to take the initiative. One of the emerging target areas for these outreach efforts has been at local barber shops and salons.
“We have learned that it’s challenging to get people to come here and seek us out,” Dillard says. “We’re trying to be more present and visible in the community. So, for instance, we work with the Local Food Hub to provide fresh fruit and vegetables to the community. Food insecurity is still out there. We’re always trying to adapt and respond to our community’s current needs. To maximize our impact, we’ll basically partner with anyone and everyone.”
She emphasizes, though, that the center’s services are always available to community members looking to improve their health. “You can walk in any time,” she adds.
Breaking Through Barriers to Change
One of the challenges faced by the Sentara Starr Hill team has to do with human nature. Even when something as important as health is at stake, humans often can be woefully stubborn about making better choices.
Unlike more obvious health issues, such as a broken bone, chronic disease prevention requires the client’s willingness to change and actively engage with the center’s services.
To address this challenge, Sentara Starr Hill strives to help clients feel comfortable and encouraged in their journeys toward better health. One past program that’s about to have a rebirth is a tour of a grocery store, which aims to help people learn how to read food labels and make healthier choices.
“It can be very, very hard to change eating habits and other lifestyle aspects,” Dillard says. “It takes time, and it doesn’t happen overnight. It takes commitment on the part of the individual. If they stumble, we help get them back on the right track. We’re here to support them and get them through it. We don’t turn anybody away. No one is perfect—you can always come back and keep trying to improve your lifestyle.”

Reflecting on her experiences with the center’s cooking
programs, Williams admits that not every new food option presented to her has been well received. She laughs when recalling the class she attended on meatless meal preparation.
“That was different for me,” she recalls. “Some things I liked, some things I didn’t. But it was a good way to try different things and find some new options.”
At the end of the day, having opportunities to change and improve is one of the big selling points for Sentara Starr Hill. Clients have access to numerous tips for leading healthier lives and many opportunities to find what truly works for them.
“Our goal is to get you into a healthier place,” Dillard says. “It’s all about helping the community in any way we can. Even if we’re just able to help one person on a given day, that’s still an important success story.”
If you’re interested in learning more about the services at the Sentara Starr Hill Health Center, please call Setour Dillard, RN, at 434-984-6220.
32 | WINTER 2022
Knowledge Power
ISGenetic Counseling for Cancer Helps Patients Make More Informed Health Decisions

Are you or your doctor concerned that cancer might run in your family? Or do you currently have cancer and would like to understand your risk for other cancers, as well as help your family members learn about their own cancer risks? If so, you could be a good candidate for genetic counseling.
Trained in both genetics and psychological counseling, genetic counselors can help patients understand genetic conditions, as well as talk them through any emotional impacts that may arise from the findings in their genetic profiles.
Paul Kwon, MS, LCGC, who has worked as a genetic counselor for both Sentara RMH Medical Center and Sentara Martha Jefferson
sentara.com | 33 CLINICAL EXCELLENCE
Hospital since June 2022, serves as an invaluable resource for patients when making decisions about their health.
“I really love working in this field,” he says. “I’m interested in helping patients understand how their family history affects their cancer risks.”
Kwon didn’t start out in genetic counseling, however. After earning his bachelor’s degree in biology at the University of Richmond, he first worked in vaccine development. However, he ultimately wanted to interact more with patients, so he began shadowing genetic counselors and found the specialty enjoyable. Kwon then returned to

school to get his graduate degree in counseling at Virginia Commonwealth University.
Today, Kwon works as a healthcare provider alongside primary care providers, oncologists and other physicians in the cancer field. When a physician recognizes that a patient’s personal or family history of cancer may point to certain higher-risk “red flags,” the patient is often referred to Kwon.
Based in Richmond, Va., Kwon’s clinic typically has a full slate of patients, providing services via telemedicine four days per week.
Watching for Warning Signs
Many physicians try to keep an eye out for general types of red flags that might indicate a patient who is at high risk for certain types of cancer, or whose cancer is hereditary. Such warning signs include:
• Early-onset cancer (i.e., most types of cancer occurring before age 50)

• A strong family history of cancer
• Multiple primary cancers (i.e., separate instances of primary cancer)
Genetic counseling, which usually occurs over several sessions, involves gathering information from the patient, educating the patient and discussing genetic testing results. Kwon starts by learning about the patient’s personal and family history.
“For instance, if I’m seeing a patient in her 50s with breast cancer, I would start from her children’s generation, then her siblings, her parents, and her

34 | WINTER 2022 CLINICAL EXCELLENCE
Paul Kwon, MS, LCGC
grandparents on either side,” Kwon explains. “We would go over the cancer histories of each relative, including aunts and uncles, and then cousins. The process does take some time.”
After gathering all this information, Kwon looks for specific types of patterns of cancer in the family history—patterns that may indicate the presence of particular conditions. He also assesses whether the patient’s cancer might be hereditary.
“Notably, only about 5-10% of cancer cases are hereditary,” he says.
If Kwon sees evidence of certain types of cancer in a patient’s family history, but the patient doesn’t have cancer, he discusses whether the patient might be at an increased risk and what can be done to mitigate that risk.
“I’ll talk with them about their family history, talk about hereditary cancer in general and then discuss any red flags I see in their history,” he explains.
Once Kwon has covered the topic of risk factors thoroughly with patients, he then talks with them about whether or not they would like to pursue genetic testing to receive more information about their individual cancer risks, and potentially about cancer risk factors for family members.
As a side note, data generated by this kind of genetic testing is protected by law and must conform to regulations established in the Genetic Information Nondiscrimination Act (GINA). This federal legislation, enacted in 2008, protects individuals against discrimination based on their personal genetic information, as it applies to health insurance (with a few exceptions) and employment. These protections are intended to encourage Americans to take advantage of genetic testing as part of their medical care.
For patients who opt to go ahead with the testing, the process usually involves a simple blood draw. Once results are returned, Kwon schedules another appointment to discuss the patient’s specific profile and determine any needed next steps.
“I think I’m good at explaining things in such a way that my patients understand,” he says. “I want them to understand what it all means.”
With his counseling degree, Kwon also can help patients deal with the emotional aspects of receiving difficult information. He takes the time to answer any questions and reassures the patient
that he will work with their caregiving team to ensure the best possible cancer treatment and surveillance management.
“Depending on the patient, there can be a sense of guilt, sadness or other natural emotional reactions,” he says. “I do my best to discuss any feelings or thoughts the patient may have during post-testing counseling and remind them they’re not at fault for their genetic profile.”
Family Ties
While genetic counseling can have a significant impact on an individual patient’s outcomes, it can also play a larger role in the overall health of the patient’s family.
If the patient has an inherited cancer risk, Kwon will write a letter for the patient to share with family members, if desired.
“In such cases, it’s crucial for the rest of the family to receive genetic testing,” Kwon says.
For instance, if a patient presents with a personal and/or family history of breast or ovarian cancer, Kwon talks with them about BRCA1 and BRCA2, two well-known genes linked to increased risk for breast cancer and other related types of cancer. (He notes that there are also many other genes associated with increased risk for breast and ovarian cancers.)
“If a disease-causing mutation is in a family’s BRCA gene, I can clarify whether the patient and his or her family are at risk for other types of cancers,” Kwon says. “In these cases, women in the family might have an increased risk for breast cancer and ovarian cancer, and men in the family might have an increased risk for prostate cancer, pancreatic cancer and melanoma.”
For patients and family members, being armed with information about specific risk factors can lead to positive health impacts down the road.
“If we find a disease-causing mutation in one of the BRCA genes, for instance, we can make medical management recommendations,” Kwon says.
Ultimately, patients and family members must decide which, if any, genetic testing options are right for them.
“Genetic counseling is all about patient education,” Kwon adds. “The information we provide gives patients power to make informed decisions, be proactive with their health and lead the best possible lives.”

sentara.com
“I’m interested in helping patients understand how their family history affects their cancer risks.”
— Paul Kwon, MS, LCGC
COLON CANCER: Early Detection is the Best Protection

Cancer of the colon and rectum (colorectal cancer) is one of the leading causes of cancer death among men and women in the United States, according to the American Cancer Society. The organization estimates that more than 106,180 new cases of colon cancer and more than 44,850 new cases of rectal cancer will be diagnosed in the U.S. in 2022.
Colorectal cancer usually starts as a polyp, or small growth, in the lining of the colon or rectum. Although not all polyps are cancerous, over time some of them can develop into cancer. The key to successful treatment is to catch the colon or rectal cancer in its earliest stages—or, better still, to screen for and remove any polyps.
Symptoms
In its earliest stages, colorectal cancer usually produces no symptoms. At more advanced stages, colorectal cancer can cause abdominal discomfort and cramps; blood in the stool; and changes in bowel habits, such as frequent constipation or diarrhea that may last several days.

Risk Factors
Risk factors for colorectal cancer include the following:
• Age
• Diet high in red meat and fat
• Family history of colorectal cancer
• Lack of physical activity/sedentary lifestyle
• Obesity
• Smoking
Screenings
A number of colorectal cancer screening tests are available. Your healthcare provider can help you decide which method is best for you.
Colonoscopy is an outpatient screening procedure that allows the physician to examine the lining of the large intestine and rectum directly. Using a thin, flexible tube with a small camera and light on the end, the doctor looks for changes and growths like polyps. If any suspicious growth is found, the physician usually can remove it during the colonoscopy procedure, and the growth is then examined for the presence of cancer.
The patient is placed in a lightly sedated state during the colonoscopy, which lasts about 30-60 minutes. Most patients are asked to take it easy for the remainder of the day on which the colonoscopy is performed, and are able to return to normal activities the day after their procedure.
The American Cancer Society generally recommends that people should have their first colonoscopy at age 45 and then repeat it about every 10 years. For African Americans, the recommended starting age is 40. If you have a personal history of cancer or a family history of colorectal cancer, your doctor may recommend you have a colonoscopy more frequently than every 10 years.
If you are 45 or older (40 for African Americans), or if you are younger but have risk factors for colorectal cancer, ask your doctor about colonoscopy and the other screening tests.
36 | WINTER 2022
HEALTH MATTERS
CÁNCER DE COLÓN:
La detección temprana es la mejor protección
El cáncer de colon y recto (cáncer colorrectal) es una de las principales causas de muerte por cáncer entre hombres y mujeres en los Estados Unidos, según la Sociedad Americana contra el Cáncer. La organización estima que se diagnosticarán más de 106 180 nuevos casos de cáncer de colon y más de 44 850 nuevos casos de cáncer rectal en Estados Unidos en 2022.
El cáncer colorrectal generalmente comienza como un pólipo, o crecimiento pequeño, en el revestimiento del colon o recto. Aunque no todos los pólipos son cancerosos, con el tiempo algunos de ellos pueden convertirse en cáncer. La clave para un tratamiento exitoso es detectar el cáncer de colon o recto en sus primeras etapas o, mejor aún, detectar y eliminar cualquier pólipo.
Síntomas
En sus primeras etapas, el cáncer colorrectal generalmente no produce síntomas. En etapas más avanzadas, el cáncer colorrectal puede causar
molestias abdominales y calambres, sangre en las heces y cambios en los hábitos intestinales, como estreñimiento frecuente o diarrea que puede durar varios días.
Factores
de riesgo
Los factores de riesgo para el cáncer colorrectal incluyen los siguientes:
• Edad
• Dieta rica en carne roja y grasa
• Antecedentes familiares de cáncer colorrectal
• Falta de actividad física/estilo de vida sedentario
• Obesidad
• Tabaquismo
Exámenes
Hay varios exámenes de detección del cáncer colorrectal disponibles. Su proveedor de atención médica puede ayudarle a decidir qué método es mejor para usted.
La colonoscopia es un procedimiento de detección ambulatorio que permite al médico examinar el revestimiento del intestino grueso y el recto directamente. Usando un tubo delgado y flexible con una pequeña cámara y luz en el extremo, el médico busca cambios y crecimientos como pólipos. Si se encuentra algún crecimiento sospechoso, el médico generalmente puede extirparlo durante el procedimiento de colonoscopia y luego se examina el crecimiento para detectar la presencia de cáncer.

Se coloca al paciente en un estado ligeramente sedado durante la colonoscopia, que dura entre 30 y 60 minutos. A la mayoría de los pacientes se les pide que no realicen esfuerzos durante el resto del día en que se realiza la colonoscopia y pueden volver a las actividades normales al día siguiente.
La Sociedad Americana contra el Cáncer generalmente recomienda que las personas se realicen su primera colonoscopia a los 45 años y que luego la repitan cada 10 años. Para los afroamericanos, la edad de inicio recomendada es a los 40 años. Si tiene antecedentes personales de cáncer o antecedentes familiares de cáncer colorrectal, el médico puede recomendarle que se realice una colonoscopia con una frecuencia mayor a 10 años.
Si tiene 45 años o más (40 para los afroamericanos), o si es más joven pero tiene factores de riesgo de cáncer colorrectal, consulte con su médico sobre la colonoscopia y otros exámenes de detección.
sentara.com | 37 LA SALUD IMPORTA
Student Athletes AT THE READY FOR
Athletic Trainers
Play Vital Role in Treating Sports Injuries
As a freshman at Orange County High School (OCHS) in Orange, Va., Bree Squiers was thrilled to earn a spot on the varsity volleyball team—not just because she’s passionate about the sport, but also because her older sister, Brooke, was on the team.

Unfortunately, Bree’s season came to a heartbreaking halt after an accident during her first week of practice.
“I was going up for the ball, and my sister dove for it at the same time, sliding into both of my legs,” Bree recalls. “I heard a loud pop when she hit me, and I fell to the ground.”
A Pathway to Care
OCHS athletic trainer Jenna Fincham swiftly scooped Bree off the ground, with the help of her coach and manager, and examined Bree’s knee. Suspecting that Bree had sprained a major knee ligament during the collision, Fincham called Bree’s mom, Suzie, to give her the news and offer advice for follow-up care.
“When parents aren’t sure what the next steps should be, I offer to reach out to Sentara Martha Jefferson for orthopedic care,” says Fincham, who
38 | WINTER 2022 SENTA RA IN THE COMMUNITY
has been an athletic trainer at OCHS for more than seven years. “I have good rapport and a direct line of contact with the athletic trainers at Sentara Martha Jefferson.”
Fincham contacted John Walker, an athletic trainer at Sentara Martha Jefferson Orthopedics and Sports Medicine, asking for his help in facilitating an appointment with sports medicine and orthopedic surgeon Matthew Panzarella, MD. Before considering surgery, Dr. Panzarella recommended holding off for a few weeks to see how Bree’s knee healed.
The Role of Athletic Trainers
Thousands of students in the Blue Ridge region participating in a wide range of activities, from youth recreational leagues through college sports teams, benefit from the support of athletic trainers at Sentara Martha Jefferson Hospital and Sentara RMH Medical Center.
While collegiate and high school teams often have an orthopedic surgeon and athletic trainer on the sidelines for high-contact games, you can also find athletic trainers at practices for a wide range of high school sports. The trainers often oversee multiple practices and games, focusing on sports with the highest risk of injuries.
“Athletic trainers provide care on the spot, first assessing an injury and then providing initial treatment,” explains Scott Powers, a certified athletic trainer and the athletic trainer program coordinator at Sentara RMH. “After an athlete has seen an orthopedic physician and, if needed, had surgery, we also help the athlete rehabilitate so they can get back on the field.”
For athletes with more serious injuries, rehab may mean coming to a clinic, but athletic trainers
try to make the process as convenient. In less severe cases, they can guide students with a rehab program at school while their team is practicing.

“For some students, getting to appointments after school is tough,” Walker notes. “Working with athletic trainers at school is more convenient, and they can still get a high level of treatment.”
Community Outreach
Several schools in Central Virginia, including OCHS, employ athletic trainers through their school district budgets rather than contracting out with a healthcare system. Walker’s goal is to build partnerships with those trainers to help provide a conduit to care.
He also hopes to offer seminars focusing on “prehab,” which would cover tips for coaches, athletic trainers and athletes to help them warm up properly and improve form, thereby reducing the chances of getting hurt.
Right now, Sentara Martha Jefferson has two full-time athletic trainers, including Walker, who works at the sports medicine clinic. The athletic trainers meet with patients to perform initial assessments before Dr. Panzarella sees them.
Sentara RMH employs 13 full-time athletic trainers: four in the orthopedic clinic, six in high schools, and three in the James Madison University (JMU) recreational sports program. Powers has expanded the athletic training program during his six years in the position.

Peace of Mind for Parents
Recently, the Sentara RMH athletic trainer team helped coordinate an appointment for Zechariah Stuhlmiller, a 9th-grade varsity football player at Broadway High School in Rockingham County.
“We were doing hitting drills, and I got hit high from behind,” recalls the freshman defensive back,
sentara.com | 39
known as “Z” by his friends and family. “My cleat got stuck in the ground, and my knee twisted as I came down. The coach called our athletic trainer to check on me right away.”
Knowing there’s an athletic trainer nearby is comforting to athletes’ parents.
“It’s definitely given me peace of mind and made the process easier,” says Z’s dad, Jason Stuhlmiller, who has coached baseball at the high school and collegiate levels. “The athletic trainer got in touch with orthopedics, and we were able to get an appointment the next day.”
Thomas Weber, MD, co-medical director for the Sentara RMH Orthopedics and Sports Medicine program, determined that Z had strained his medial collateral ligament. Z was able to rehab with the athletic trainer at school and get back on the field a couple weeks later.
High school athletic trainers attend meetings at the beginning of each sports season to make sure parents know they are available for questions or concerns about an injury.

“When Bree and her siblings went to practices, it was comforting knowing Jenna would be there,” says Suzie Squiers. “As a parent, you want to know someone is there for your child, and Jenna absolutely was that.”
Health Care Away From Home
For young adults at college, dealing with an injury experienced while working out, playing intramurals
or participating in other activities on campus can be daunting.
Thankfully, JMU students can rely on the advice of Sentara RMH athletic trainers, who staff a full-service athletic training room at the university’s recreation center, which is open to all JMU students.

“We see a lot of 18- and 19-year-olds making healthcare decisions for the first time,” Powers explains. “They need counseling and guidance. They need to know if they should see a doctor, and that’s what we do with our evaluations.”
JMU students can see the athletic trainers free of charge for an initial assessment. If indicated, the athletic trainer will recommend that the student seek follow-up care with a physician. Students can also return and rehab for free.
Powers recalls a case in which a student took a fall while skateboarding. When the student came in to get checked for a concussion, he reported experiencing considerable neck pain. The athletic trainer on duty referred him to Sentara RMH, and X-rays revealed two cervical fractures. In such cases, having an athletic trainer on hand can help students get the treatment they need more quickly and conveniently, potentially helping them avoid more serious injury.
Looking Out for Athletes
Seeing students back on the field following an injury is rewarding for athletic trainers.
“We’re certainly on the athlete’s side,” Walker says. “We want them to stay in the field, and it’s our job to help them get back out there as soon as possible.”
A few months after her accident on the volleyball court, Bree had surgery to reconstruct the major ligament that keeps the kneecap in place. However, COVID school shutdowns and a subsequent snowboarding injury delayed her return to the court. Now a senior, Bree serves as a team captain and has aspirations of becoming an orthopedic surgeon.
“Jenna’s work as our athletic trainer has had a positive impact on our entire team,” Bree remarks. “She’s been like a mom to us, and we truly appreciate all she’s done. I hope to make a difference like that someday, too.”
40 | WINTER 2022
SENTARA IN THE COMMUNITY
TheHealing
Massage Therapy Brings Comfort
at Sentara Martha Jefferson
Few experiences in life are scarier and more stressful than intensive cancer treatment.
Carolyn Dawson knows this all too well, having fought both lung and breast cancer at Sentara Martha Jefferson Hospital’s Phillips Cancer Center over the past decade. In addition to surgery and chemotherapy, she has endured twicedaily radiation treatments, which required her to lay completely immobile on a steel table, staring
up at the machines that were blasting her body with radiation.
To calm the anxiety caused by her illness and treatments, Dawson often timed her appointments around the schedule of Sentara Martha Jefferson’s massage therapist team, whose gentle, healing touch helped to quiet her mind and ease her bodily tension.
“Having 15 minutes to sit down and take a breath after treatment made such a difference,”

mjhfoundation.org | 41 CARING TRADITION
Touch
Safe, therapeutic touch extends the Caring Tradition to patients, families and staff.
Dawson recalls. “Sometimes you just sit there and don’t say anything, or you want to talk about what’s going on, and the massage team is so sympathetic and understanding. It’s an incredibly valuable service, and I’m so grateful for the community support that makes it possible.”
Thankfully, Dawson is now cancer-free, although she still grapples with osteoarthritis and other aftereffects of treatment. “It’s been a long road, and they’ve been there the whole time,” she says.
Rebeccah T. Getz, RN, LMT, architect of the massage program and a 43-year Sentara Martha Jefferson veteran, has become a friend to Dawson over the years. “We chat, and she gets a knot out of my neck, and I leave feeling rejuvenated after my 15 minutes of ‘Becky time.’ Her wonderful attitude and compassion are infectious. She’s just the person you need in this type of situation.”

The Heart of the Caring Tradition Community generosity through the Martha Jefferson Hospital Foundation makes it possible for Getz and her team of four part-time massage therapists—Kate Hall, Cora Houghton, Alexa Matthews and Cecilia Mills—to provide 280 hours of free massage monthly to patients, families and hospital staff.
“It really is the heart of the Caring Tradition,” says Sylvia Hendrix, MD, a Sentara Martha Jefferson radiation oncologist. “You don’t need massage therapy to get accredited or to achieve wonderful outcomes, but the patient experience is so integral to care. When you’re in Becky’s chair, she’s taking care of you, and you feel like your life is a little lighter.”
That appreciation led Dr. Hendrix and other forward-looking hospital leaders and physicians to champion massage at the hospital back in the 1990s, before quantitative
research had demonstrated the therapeutic power of safe touch to ease pain and anxiety, and to support other medical interventions.
Getz’s irresistible warmth, humor and dedication make her a powerful advocate for the program as well. Massage and other holistic modalities helped her beloved husband, Brad, fight lymphoma, so she knows firsthand how important healing touch can be for those going through cancer treatment.
Today the massage program is an essential component of the hospital’s commitment to caring for the whole person. Getz’s team members take their time with patients, listening to and supporting them as they work out the knots and tension in sore shoulders and clenched hands.
The impact of their efforts is often visible and immediate. “Being in a constant state of fight-orflight, as patients and families so often are, isn’t supportive to healing,” observes Peggy Bishop, NP, palliative care team coordinator. Bishop’s team supports some of the sickest patients in the system, as well as some of the oldest, working closely with family members to create a holistic plan that helps improve patient quality of life.
42 | WINTER 2022 CARING TRADITION
Sentara Martha Jefferson’s massage therapists have helped Carolyn Dawson manage pain and anxiety during her decade-long battle with cancer.
“Aging people with serious illness often become disenfranchised,” says Bishop, noting that massage takes on added importance when “tender, loving touch is otherwise absent from patients’ lives.”
Even a few minutes with a skilled therapist can be remarkably restorative, bringing down the level of fear to a place where patients and families can have necessary conversations about quality of life. Getz and her teammates often attend palliative care team meetings, recognizing that family members frequently share important information with them that would otherwise go unreported.
Healing the Healers
Getz and her teammates are also beloved among Sentara Martha Jefferson’s staff, who rely on massage to relieve sore muscles, cure headaches and find a few minutes of respite. Thanks to community support through the Staff Resiliency and Wellness Fund, the team now has the funding to provide monthly massage events for staff, as well as round on all hospital departments and Sentara medical offices.
The unique perspective of the massage team gives them a true appreciation for the challenges of frontline medical work. “For instance, radiology team members have to wear heavy lead protective gear for hours each workday, and you can see the toll that weight takes on their shoulders over time.”

Imaging techs also feel the effects of the physical nature of their daily work, spending hours putting strain on their hands, wrists, shoulders and neck muscles while reaching over wide beds and torquing their bodies into uncomfortable positions. Many longtime sonographers, unfortunately, deal with pain on a daily basis.
Ann Brown, RVT, RDMS, RDCS, team coordinator for general and vascular ultrasound and a 19-year veteran of the Sentra Martha Jefferson imaging team, considers massage vital for managing pain and maintaining the physical flexibility she needs in order to do her job. Brown, who pays for regular massages outside of work, considers the on-site therapy provided by Getz’s team to be an important supplement.
“The community’s support of this program helps to keep me working,” Brown says. “Massage helps keep me and other members of our team from having to be out on worker’s comp. It’s amazing how much 10 minutes of massage a week can do to help your muscles and joints stay loose and prevent injuries.”
For her part, Getz sees it as a calling to share her gift for healing touch with as many people as she can. “I give a lot, but I get it back tenfold,” she says. “I feel like I’ve found my niche. You should see the difference it makes.”
mjhfoundation.org | 43 CARING TRADITION
Community support enables Becky Getz and her team to provide regular massage therapy to help hospital staff manage stress and prevent workplace injury.
Exhibiting Compassion
VISUAL
Jacquelyn Ragland, a retired Charlottesville educator, knows firsthand the healing power of art and beauty. Five years ago, diagnosed with aggressive non-Hodgkin’s lymphoma and facing down an intensive course of chemotherapy and radiation, she signed up for an art therapy class at the Sentara Martha Jefferson Phillips Cancer Center.
“In the midst of the procedures and treatments and blood tests, creating something felt so healthy and healing,” Ragland recalls. “I don’t remember what I even made, but I do remember how the process made me feel. It was absolutely a direction that my soul wanted and needed to go. The class was so therapeutic.”

44 | WINTER 2022 CARING TRADITION
ARTS INSPIRE COMFORT AND HEALING AT SENTARA MARTHA JEFFERSON
Cancer survivor Jacquelyn Ragland drew on the beautiful art of the Phillips Cancer Center to find a sense of calm and balance during her cancer journey.
Healing, Calming Spaces
Recognizing that healing comes in many forms, Sentara Martha Jefferson’s leadership team makes an intentional effort to integrate beauty and art into the hospital campus. From the colors on the walls to the quiet beauty of the surrounding mountains, the facility is situated in a healing environment designed to provide a sense of comfort and caring.
This focus on thoughtful design puts Sentara Martha Jefferson in good company, as more than half of America’s hospitals are now infusing art therapy into their design and programming by brightening hospital walls, offering classes and in other ways. According to the World Health Organization, infusing art into the healthcare setting benefits patients’ loved ones and healthcare providers, in addition to helping patients navigate the emotional journey of battling an illness.
“Having something beautiful to look at when you’re sick is a wonderful thing,” says Matalie Deane, who worked at Sentara Martha Jefferson as a respiratory therapist for 34 years. Now a professional artist herself, Deane leads the hospital’s Art Committee.

Comprised of board members, physicians, staff and volunteers, the committee is charged with selecting original art and media, and determining where that artwork will be placed in the hospital. The 1,200-piece permanent collection includes large works that can be appreciated from across



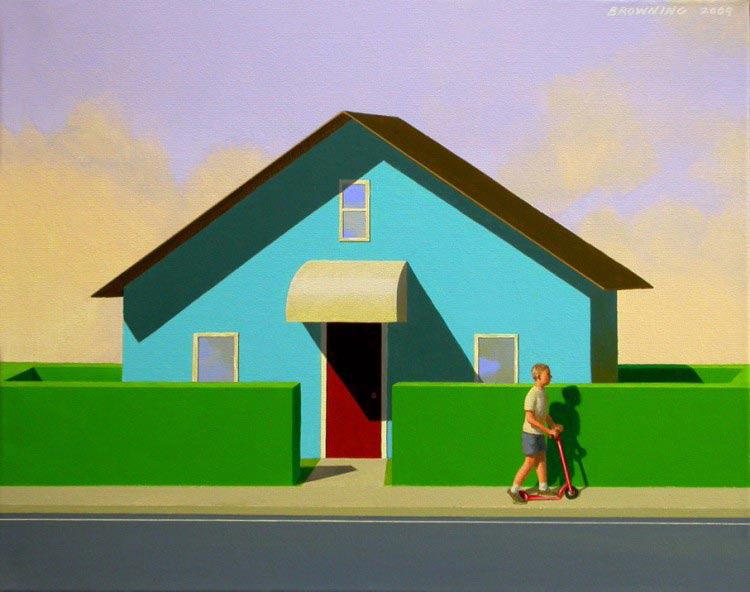
mjhfoundation.org | 45
The hospital’s 1,200 piece permanent collection includes the Elm Street series by Virginia artist Rob Browning.
Art Committee chair and artist Matalie Deane enjoys sharing the hospital’s art with her young granddaughter.
the lobby, as well as others that beg one to approach and marvel at small details.
“What they all have in common is an ability to divert attention, engage the mind and lift spirits,” says Carol Hurt, chair of the Sentara Martha Jefferson Hospital Board of Directors. “All of the pieces are also created locally, from a community of artists that is so vibrant, we rarely need to look outside of Charlottesville to find pieces that intentionally connect patients, visitors and staff with our beautiful surroundings.”
The hospital’s permanent collection is supplemented by rotating art exhibits that are thoughtfully assembled and kept fresh in the maternity ward, the lab testing area and the cancer center—higher-traffic areas where patients and visitors might feel the most anxiety. Also keeping in mind how many hours hospital staff members put in, the Art Committee regularly rotates art in busy hospital corridors.
Support This Work
Visit mjhfoundation.org to download a walking tour and support the art collection through the Kitty Stroud Fund.
Sharing Your Love Through Art: Special Exhibitions
Showcase Local Artists
“My art is my passion,” says figurative artist Bryan Trent Fair, a Central Virginia native who honed his craft studying with well-known artists on the East and West Coasts before moving home to Buckingham County and joining the Sentara Martha Jefferson Hospital team as an executive assistant.

Fair, who currently serves on Sentara Martha Jefferson’s Art Committee, was recently featured in a hospital exhibition of portraits that paid homage to classic Hollywood icons. The paintings hung in the second floor Phillips Cancer Center hallway in one of three rotating exhibit spaces, all of which were designed to be accessible as a source of comfort for anxious patients and families.
The Art Committee looks for two-dimensional work (no sculpture) that is bright, engaging and uplifting. Exhibitions rotate every few months and typically include five to 10 works. Art is available for purchase.
“This is a great opportunity for local artists to display their work for the community, in a way that really makes a difference,” Fair says.
To find out more about exhibiting your artwork, contact Renee Dinwiddie at rmwalker@sentara.com.
“The intentional art creates a more calming space for patients—and also for staff walking between units,” says Sentara Martha Jefferson hospitalist Mark Mandichak, MD.

Art also adorns the walls in many of the staff spaces, including a recently dedicated hospitalist conference room honoring the memory of Nicholas C. Brandt, MD. The space features two beautiful landscape paintings by regional artist Susan McAllister that were gifted to the hospital by Dr. Brandt’s family.
Choosing Joy
When Jacquelyn Ragland first received her frightening diagnosis, her doctor told her, “It’s a bad cancer, but you don’t have a lot of it, so I think we might be OK.”
Today, Ragland is cancer-free, feeling healthy and enjoying retirement, grateful every day for the team of doctors who saw her through her diagnosis, treatment and recovery. She also remembers the healing power of the art on Sentara Martha Jefferson’s walls.
“I recall several times when I would stand in front of one of those paintings to have a personal ‘mini-retreat’ before a treatment,” she says. “The beauty and the calming scenes balanced out the more difficult parts of my healing process. They gave me an opportunity to choose light, joy and creation.”
46 | WINTER 2022
CARING TRADITION
A generous gift from Marty and Ann Meth enabled the purchase of beautiful art pieces by regional artist Susan McAllister for a hospitalist conference space dedicated to the memory of their beloved son-in-law, Nicholas C. Brandt, MD.
Addressing Mental Health and Substance Abuse: The Women’s Initiative
For more than a century, Sentara Martha Jefferson Hospital has worked to improve the health of friends and neighbors in our community, providing compassionate care for all who walk through our doors and reaching outward to work for greater health equity in our community.
Every three years, Sentara Martha Jefferson partners with colleagues at UVA Health and the Blue Ridge Health District to create a comprehensive study of the most pressing health issues in our community. The most recent Community Health Needs Assessment identified four priority areas:
• Reduce health disparities and improve access to care.
Promote healthy eating and active living.
• Address mental health and substance abuse.
Foster a healthy and connected community for all ages.
Through the support of the Martha Jefferson Hospital Foundation, our Community Benefit team closely collaborates with community healthcare partners to address these urgent needs. This piece is the final in our year-long series highlighting a few of the partners and programs we support and work with to improve the health of our community.
Shelly Wood (right) directs Sister Circle, an affinity group for women from across the African diaspora, with grant funding and support from Sentara Starr Hill colleagues, including Integrated Care Manager Setour Dillard (left).

“Everyone goes through challenges and struggles—it’s part of being human,” observes Elizabeth Irvin, executive director of The Women’s Initiative. “Sometimes we think we’re not supposed to reach out, that we’re supposed to get better on our own. But that’s a fallacy. People need each other, and we need help sometimes.”
In such moments, The Women’s Initiative offers a safe space for women to share experiences of depression, anxiety, substance abuse and other behavioral challenges—many of which women experience at higher rates than men. More than 2,500 women find compassion, guidance and support at The Women’s Initiative every year. All services are free or offered on sliding scale, including more than 6,700 individual counseling sessions annually that cost $5 or less.
More than 20 therapists work out of The Women’s Initiative’s two locations downtown, including donated office space in the Jefferson School City Center adjoining Sentara’s Starr Hill Health Center. The shared location and longstanding partnership between the two organizations make for a seamless transition for clients.
mjhfoundation.org | 47
CARING TRADITION
The Women’s Initiative therapist
To connect with Latina women, who often have difficulty accessing culturally responsive care, The Women’s Initiative hosts outreach efforts at Latinx communities, such as Charlottesville’s Southwood.


“It’s like going from the living room to the kitchen,” says Setour Dillard, Starr Hill’s integrated care manager. Clients partner with Dillard and other Starr Hill staff for regular health checks, cooking classes and other services to help manage chronic illnesses, including diabetes, heart disease and obesity.
When necessary, clients can also go next door to The Women’s Initiative office to access walk-in clinics, individual counseling, resources and social support from their peers.
“The partnership with Sentara is so important in helping us make the connection between mental and physical health in someone’s overall well-being,” says Shelly Wood, therapist and director of one of The Women’s Initiative’s affinity-based healing programs, Sister Circle, which is supported by Sentara grant funds.

The need for behavioral health services in our region is huge. While more than 250,000 people live in the Blue Ridge Health District, there are only 25 adult psychiatric beds—and zero child or adolescent psychiatric beds—in our community. Importantly, this longstanding shortage of behavioral health services disproportionately impacts people of color, who are more likely to experience issues of anxiety and depression than their white counterparts, but less likely to be taking medications or receiving treatment.
Also, in light of the existing gap in racial and ethnic diversity among trained clinicians and the fact that more than 40% of The Women’s Initiative’s clients are people of color, Wood and her colleagues are all
An easily accessible Women’s Initiative office in the Jefferson School, adjacent to Sentara’s Starr Hill Health Center, encourages clients to care for both their physical and mental well-being.
trained to work with members of the LGBTQIA+ community, and many therapists are multilingual. Special affinity programs—including Bienestar for Latina women and Sister Circle for people who identify as women from across the African diaspora— also provide spaces of cultural understanding.
The Women’s Initiative also recognizes that people heal in different ways, providing a diverse offering of services including yoga, chair massages, West African dance classes and writing classes that focus on storytelling as healing. This diversity allows the organization to focus on what Irvin calls “culturally responsive care” that is designed to redress mental health disparities for Black, Latinx and other people of color in our community.
“We’re a smaller community place for people to go, where it feels more accepting,” Wood says. “People look for a place they feel they can trust.”
That trust, and the openness it enables, makes all the difference. “The Women’s Initiative believes in the innate capacity for healing and growth in all women. We’ve seen so many people come here and get better.”
Our mission to improve health everyday drives everything we do to keep individuals, families and the community we serve healthy. We do this by establishing partnerships that create a positive impact in our communities.
Through the support of the Martha Jefferson Hospital Foundation and the Sentara Healthier Community Fund, Sentara Martha Jefferson Hospital provides grant funding to community health partners, like The Women’s Initiative, located in the Blue Ridge Health District and surrounding counties. Find out more at sentaracares.com.
48 | WINTER 2022
CARING TRADITION
Meet Ryan.
Sentara Martha Jefferson Hospital is dedicated to improving the health of our community and it shows through the compassionate care provided by the people that work within our walls.

Ryan Thompson, RN, BSN, is one of those people. From the moment you meet Ryan, you know that you are in the hands of a dedicated caregiver focused on helping you feel better.
“When you serve in the community in which you live, these people stop being strangers but people you will see again.”
Hear more from Ryan in his own words at Sentara.com/MarthaJeffersonPeople.
Hear more of Salinda’s story
SENTARA MARTHA JEFFERSON HOSPITAL
Sentara Martha Jefferson Hospital 500 Martha Jefferson Drive Charlottesville, VA 22911 Sentara.com Change service requested
SENTARA MARTHA JEFFERSON HOSPITAL
SENTARA MARTHA JEFFERSON HOSPITAL IS A COMPREHENSIVE STROKE CENTER

Sentara Martha Jefferson Hospital is recognized as a Comprehensive Stroke Center by DNV GL Healthcare. This is the highest level of certification available, and it signifies our ability to provide advanced stroke care 24/7. We are proud to serve Central Virginia with quality stroke care in a warm, caring setting.

For more information, visit www.Sentara.com/Stroke
Follow us on Facebook @SentaraMarthaJeffersonHospital, and T witter @MarthaJefferson.
Non-Profit Org.
U.S. Postage
PAID
Sentara Martha Jefferson Hospital



















































































 Luis Morales, BSN, RN, CCRN, CMC, was eight months into his nursing career, working in the Med-Surg/Oncology Unit at Sentara Martha Jefferson, when he decided it was time to walk down to the Intensive Care Unit (ICU). His goals for that trip were to speak with the ICU manager, make a solid first impression and explain why he wanted to become a Wendel 1 ICU team member.
Luis Morales, BSN, RN, CCRN, CMC, was eight months into his nursing career, working in the Med-Surg/Oncology Unit at Sentara Martha Jefferson, when he decided it was time to walk down to the Intensive Care Unit (ICU). His goals for that trip were to speak with the ICU manager, make a solid first impression and explain why he wanted to become a Wendel 1 ICU team member.