






 from Louise Barnett, Chief Executive
from Louise Barnett, Chief Executive
Welcome to the latest edition of Impact magazine. It is feeling very autumnal outside and with winter just around the corner, plans are under way to ensure that our hospitals are as prepared as they can be so that we can continue to provide the best quality care we can to our patients.
Despite the challenges that we in the NHS are facing, it really is fantastic to see that you are continuing to make improvements that will really benefit our patients and their experience of care.
A really wonderful example of this is the ITU Patient Diary – an important and effective communication tool that is helping our patients and their families. A huge thank you to the teams involved in creating this, and as you will be able to poignantly read on page 8, it has made an incredible difference as described by one of our patients.
Another area of focus is end of life care and making sure that we are providing the very best care and support we can to patients and their loved ones. It is so important that we get this right for every patient, and you will be able to read about the changes that are being put in place by our Palliative and End Of Life Care Team to help and support colleagues on page 6

Finally, it is important that we all have the time to catch up, reflect and prepare so I want to introduce no corporate meetings on a Friday. This is an attempt to reduce the number of meetings that take place, free you up to meet in person where possible, increase the visibility of leaders at all levels and help us to prepare further for the weekend and weeks ahead. It is important to apply this sensibly in your areas and please do seek guidance from your
manager if helpful. I would really welcome your feedback through the Cascade process about how this going over the coming months
Of course it is really important that you do meet regularly as teams and colleagues and talk through any issues or plans to make continuous improvement in your area. I know we are all very focused on the challenges that we face and the significant pressure on our services so, it is really is fantastic to see your ideas and improvements coming to life.
We know we have much more to do. If you have an improvement idea or need support to tackle an issue or get it off the ground, please speak to our colleagues in the Improvement Hub who can help you – sath. improvementhub@nhs.net
And if you would like to feature in a future edition, please do contact me or our Communications Team –sath.commsteam@nhs.net
Thank you.
Louise Barnett Chief Executive
Dear colleague,
We continue to make good progress on our threeyear Getting to Good improvement journey. I know that so many of you are doing incredible work to help get us to where we all want to be. Thank you for all your commitment in helping us to drive forward these improvements.
As you will be aware, there are nine programmes within Getting to Good – pictured – each of which are led by an Executive Director and within each of these programmes are a number of transformational projects.


The aim is to deliver and embed sustainable change that will support our aim to improve our CQC ratings for care across all of our services and help us to achieve our vision to provide excellent care to the communities that we serve.
One area of recent success has been within Governance, and the transition to DATIX from 4Risk which is now complete. We’re striving to
embed an open and aware risk culture within the Trust, supported by a clear and robust ‘risk reporting, approval and escalation structure’. This transition will help to ensure that we’re working together as an organisation to respond to risk. More on this, and the difference it will make for colleagues and patients, in the next Impact.
Finally, congratulations to our maternity colleagues who were finalists in the Patient Experience Network National Awards (PENNA) for their UX Experience System which we featured in the last edition of Impact. The really great initiative enables our teams to capture the feedback of women, families and colleagues to help shape the improvements in our maternity services. The team has also produced and
introduced a birth preferences card - you can find out more about this innovative card on page 8.
If you would like help or support with your improvement ideas, please contact our Improvement Team via sath. improvementhub@nhs.net
Thank you.
Ensuring that all our patients receive high quality, safe care is a key priority on our Getting to Good journey.
We are just about to embark on a three-year improvement programme in our Emergency Departments, driven by the Emergency Care Transformation Programme.

Similar to the Maternity Transformation Programme, which is heading up improvements in our Maternity Services, there are five work streams, each with a lead. The work streams are:
Work Stream 1 - Clinical Quality, Outcomes and Co-ordination of Care
This work stream will ensure that we are delivering high quality care and supporting our staff with the skills they need to effectively lead our department, putting patients at the heart of what we do.
understand how we could have prevented or lessened the harm that these incidents have caused.
This work stream will help us to develop systems and processes that lessen that risk of harm and ensure we learn from our mistakes and prevent them from happening again. It is important that we set high standards for ourselves and for the care we deliver, we monitor how we are doing against these standards and continuously learn, develop and improve.
Work
The focus for this work stream is to ensure that the workplace is an enjoyable and safe place for all of our colleagues, that we value each other and that our behaviours are respectful and consistent with the values of SaTH.
We want our Trust to be a place where colleagues want to work and experience excellent support from each other and encourage others to join our well-trained and enthusiastic teams delivering the best care we can.
One of the areas of concern highlighted by the CQC was our lack of learning from incidents and complaints. We need to find an effective way to make sure that colleagues recognise when things go wrong, report this and then
We need to ensure we have a supportive culture and processes in place so colleague feel able to raise concerns, report incidents, and feel supported when things do not go to plan so that we can learn and continuously improve care for our patients for the future.
Work Stream 4 - Communication, Compassion and Engaging Communities
We must ensure that we provide services that meet the needs of our population and that we listen to and engage our patients and community to ensure we provide the best possible care now and in the future.
Work stream 4 will focus on how we engage with our communities, how we meet their needs and that of their relatives and families. Tackling health inequalities, listening and embracing an inclusive approach with care and compassion is critical to service delivery and development.
Our vision is to provide excellent care for the
communities that we serve and this means we need to have clear pathways in place for our patients both in terms of the care that we provide but also, working with our external partners and our community, to ensure that people receive the care and treatment that they may need in the community rather than in a hospital setting, where this is appropriate.
Our aim is to achieve timely ambulance handovers and for patients not to have to wait in ED for an inpatient bed thus ensuring patients are in the right place at the right time. This work stream will be closely aligned to the Flow Improvement Group and Urgent Emergency Care Programme across Shropshire.
We are putting in place a number of interventions to improve the patient journey, and their experience of care in our hospitals, when they arrive in our Emergency Departments.
Funding has been secured to create an acute floor area on the RSH site. Based on Ward 22, there will be a medical assessment area to receive direct GP admissions which means that these patients no longer have to go to A&E. It will also provide direct admission for trauma orthopaedic and oncology patients.
A number of ward moves have taken place to create the new floor, which is expected to be operational by the end of November.

Clinical Quality, Outcomes and Co-ordination of Care Staff Culture, Resilience and Health & Wellbeing
Governance, Risk & Safety
Communications and Engaging Communities
Environment, Pathways and Flow
The new acute floor area will not only provide a new medical assessment area, but wider ambulatory care capacity, meaning patients will be able to receive a diagnosis, observation, consultation, treatment and intervention and rehabilitation services, reducing the need for hospital admission.
Sara Biffen, Acting Chief Operating Officer, said: “We are putting in place a number of interventions to improve the flow at the ‘front door’ so that we can improve both patient safety and their experience of care. The new acute floor should improve both, whilst also reducing waiting times, crowding in our ED department and ambulance handovers.
“It is important that wherever possible patients go directly to see a specialist who can deal with their condition and the creation of the acute floor should address this.
“Thank you to everyone who has been involved in this programme, it has been hard work moving wards around - but it will have enormous benefits for our patients and for our ED colleagues as we move towards winter."
An important part of the Getting to Good programme is the delivery of high quality palliative and end of life care for our communities.
A crucial aspect in achieving this is our delivery of palliative and end of life care. Our latest CQC report, published in November 2021, identified improvements needed in our end of life services and our Palliative End of Life Care (PEOLC) team has been working hard to deliver and embed this change across the Trust.
End of life care is everyone's responsibility and we have one chance to get this right. A key component has been the merging of our Palliative Care team and End of Life Care team, the introduction of a central joint contact number, a triage tool for referrals and the expansion of the specialist palliative care service to operate seven days a week across both hospital sites.
The team has also introduced an innovative new way of working to support our ward teams through a project called Supportive Ward Visits, led by the End of Life Care nurses and facilitator supported by the Palliative Care nurses and doctor, which provides intensive support to wards across RSH and PRH to empower them to provide good and excellent end of life care to patients and their relatives.
The project, which began over the summer, sees our Palliative and End of Life nurses and a Palliative Care doctor work intensively with a ward for
anywhere from four to eight weeks to provide one-to-one teaching, group teaching, training, ward manager support and much more.
The visits centre around individual ward needs, and once finished, the team comes back and revisits each ward three to four months later to support the team to be able to maintain the level of care embedded during the visits.
Angie Cooper, Matron for Oncology and Haematology, Palliative & End of Life Care, spoke of the project: “The ward visits raise the profile of how we can deliver excellent end of life care in these individual wards and with ward teams, which helps the teams to focus on how to naturally improve the care they deliver.
“We have received excellent feedback around the Supportive Ward Visits from patients, relatives and ward staff who have told us the impact they have made on how the ward provides effective end of life care for their patients. The wards involved have also seen an improvement in audit results, communication, and pain control and training compliance.”
The PEOLC team aims to continue its improvement journey by expanding the Supportive Ward Visits, raising the profile of the team and end of life care, ensuring their service is
"Delivering high quality palliative and end of life care is of huge importance. This is an area of care that all staff need to be skilled in. Our improvements are aimed at supporting all our staff to be confident to provide this excellent care. So often the focus is put on preventing dying, which is appropriate, but when that is no longer possible it is so important for that to be recognised and for the patient and those important to them to be involved in planning their care and feel supported. This is what we hope to achieve."
Dr Emma Corbett Clinical Lead for Palliative and End of Life Care
sustainable moving forward.
Angie added: “End of life care really matters and we want to make sure our patients but we want to make sure these patients are well cared for, and we want to make sure our patients are well cared for, pain free, supported and that we are having the right conversations with them and their relatives.”
induction process, our HCA colleagues are staying with us - they are being given a real flavour of what being an HCA is like before they work on a ward. This training was never provided before and makes such a difference.”
The Healthcare Support Workers (HCSW) Academy, which was launched alongside our partners last January, provides a solid foundation for Healthcare Assistants (HCA) who are joining our organisation. And as a result, the number of HCA vacancies at SaTH is now at its lowest for some time.
Rachel Armstrong, Head of Non-Medical Education, says she believes this is because our HCAs feel supported and invested in through the training delivered by the new Academy, and the ‘Buddy’ programme which runs alongside it.
More than 200 HCAs have so far been through the Academy at Telford College with about 90% of those being from SaTH.
The first two weeks of training are in the classroom when students complete all their statutory and mandatory training. At the end of six months, if successful, candidates will receive their Care Certificate.

Rachel said: “As a result of a much better
“If we give our colleagues the best start, then they are more likely to stay with us and go on to do further training, which is great for the HCAs and our teams and importantly our patients.
“Now, when HCAs arrive in wards they understand better the impact they have on patient care and that is really important. It is better for our patients. By keeping patients at the centre of what we are doing and by giving people the right training, we are ensuring patient safety and that is key.”
She added that the Academy was a healthy pipeline for our workforce with many HCAs aiming to become midwives, nurses and nursing associates.
The collaborative approach with other partners within the Shropshire, Telford & Wrekin Integrated Care System (ICS) means all HCAs will have the same training as everybody else with further training in their specific roles as needed.
We are always looking for new ways to invest in, and develop, a sustainable workforce and this is a key priority on our Getting to Good programme.
Patient Paul Foster is an advocate of the ITU patient diary – this is his story:
After a second chemotherapy treatment, Paul acquired an infection while recuperating at home and was taken to A&E. He remembered going into A&E and signing in but nothing after that until the rehab team got him up, put him in a wheelchair and took him outside.
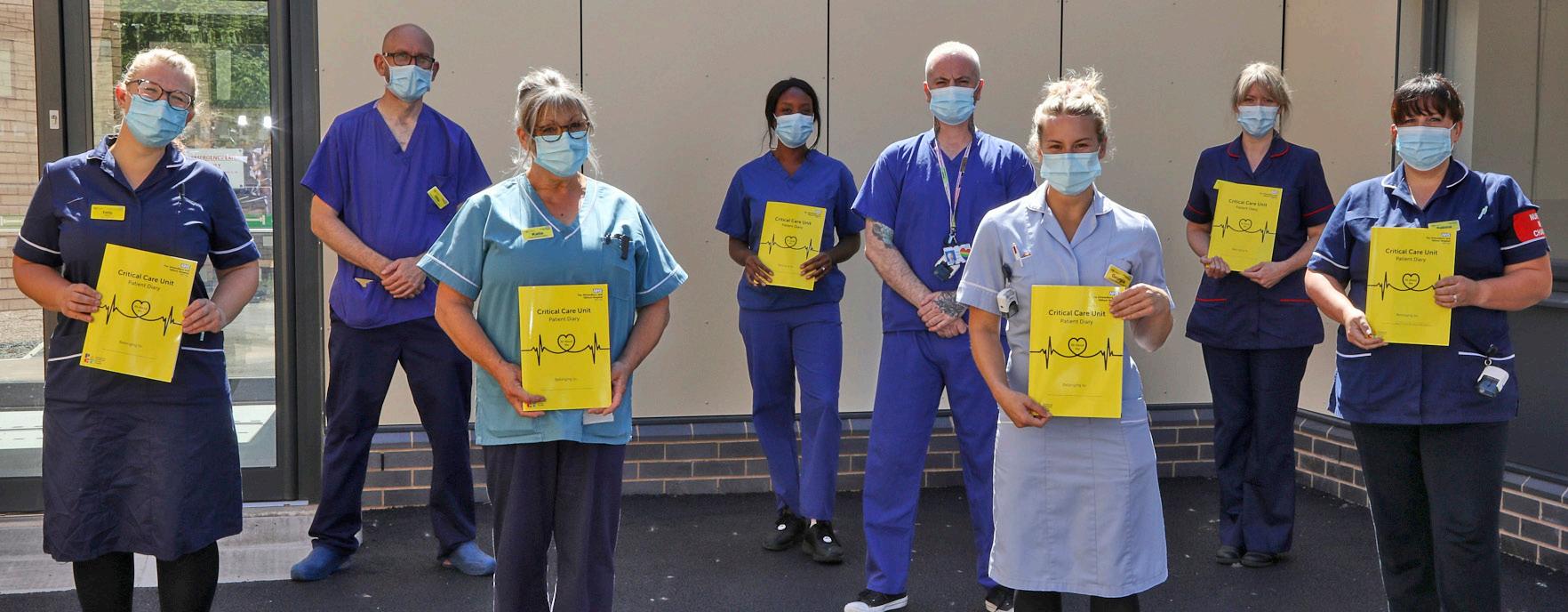
One of our key improvement priorities is ensuring that we are providing the best possible care and experience of care for our patients every single day. Colleagues from across our organisation are driving some really important improvements so that we can achieve this, including in critical care.
Pre-pandemic, a small group of critical care nurses introduced a patient diary for our ITU patients. A lot of work went into researching and writing a proto-type diary, and whilst it was in this developmental stage, a blank exercise book (similar to a school exercise book) was issued to patients. However, there was no structure to guide staff in writing diary entries, and then the pandemic hit, and the diary lost its impetus.
When Katie Craft joined the Critical Care Therapy team as
a therapy assistant practitioner, she felt strongly that our ITU patients could benefit enormously from a well-kept patient diary.
Katie, who previously worked as a registered mental health nurse for 23 years, said: “The diary helps patients to attain a better understanding of the chronological events of their illness and fills the inevitable gaps in their memory. It can help with orientating patients who have struggled with ITU-acquired delirium and is also an invaluable tool for setting realistic rehab goals for recovery.
“The Critical Care Therapy Team wanted the patients to be able to easily identify major landmarks in their recovery as they looked back through their diaries, and we decided that stickers showing their achievements would be a good idea. At this point, I sought the support of the
He said: “I was still really confused. I didn’t really know where I had been or what had happened to me.” When Paul was moved to a ward, he said he became aware of the patient diary.
“I started to read the diaries, this was quite an emotional time for me because I found out that I had lost about five weeks of my life in between being in ITU and back on a ward. I really had no idea of the anguish and stress that I had caused my wife and how much hard work the nurses and doctors had put in to keep me alive. It really was humbling. Without the diary, I would not have known that any of this had taken place.
“In the latest version of the diary there is a section where you can put down significant events like the first time I stood up, the first steps I took and the first time that I took a shower. I have been able to monitor my progress using this part of the diary……it is invaluable to patients like me.”
Our vision is to provide excellent care for the communities that we serve, and we are striving to achieve this through our Getting to Good programme.
Improvement Hub and I am so glad I did. They harnessed my enthusiasm and supported me in further developing our diaries. I spent time talking to the Critical Care team about their experience of the diary as a working document and took what they said to help rework the diary into its lovely new format.”
She added: “I understood from conversations that I had, that some colleagues actively avoided writing to the patient in case what they wrote distressed them. After considering this, I decided to write to the famous children’s author, Michael Rosen, to ask him if he would consider writing a foreword for our diary based on his own experience. He had been in critical care for 48 days with COVID-19 and, following his discharge, he wrote a book based almost entirely on his own patient diary called Many Different Kinds of Love.
“He was delighted to have been asked and wrote us a beautiful and heartfelt foreword which is printed on the inside cover. His words have not only inspired our clinicians to write to their patients, but it has positively encouraged fearful patients to bravely read about the events of their critical illness.”
The multidisciplinary team, family and visitors are encouraged to write in the diary what has happened each day. The diary stays with the patient and can include information that led up to the admission to critical care, how they are progressing, events throughout the day and messages from home.
SaTH Charity has funded the printing of the patient diaries, and Katie has now developed a training presentation to target clinicians who were new to critical care; the presentation includes a video recording that one of our patients sent us extolling the benefits of the diary.
Louise Barnett, Chief Executive, said: “A huge thank you to Michael Rosen and well done to Katie and the Critical Care and ITU teams for developing the ITU Patient Diary which is really wonderful and which is making a real difference for our patients and families.”
 By Michael Rosen (Author of ‘We’re Going on a Bear Hunt’ and ‘Many Different Kinds of Love’).
By Michael Rosen (Author of ‘We’re Going on a Bear Hunt’ and ‘Many Different Kinds of Love’).
“I was in intensive care for 48 days in 2020. Most of that time I was in an induced coma. As a result, I hardly remember any of it. What’s more when I ‘came round’, it was rather slowly and for several weeks, I was confused and disoriented. I couldn’t explain to myself what had happened. I was lucky enough not to experience many nightmares though I did have a series of recurring dreams which made me feel lost or sad.
I was extremely fortunate in that the nurses and ‘helpers’ who looked after me in intensive care wrote a Patient Diary for me and about me. To tell the absolute truth, to start off with, I didn’t dare read it. I can’t exactly explain this. I just felt that I didn’t want to look at myself through the eyes of the nurses and see how helpless I was.
My mistake, I should have looked straightaway. In fact, it took me several months to really read what those ‘letters’ in my diary said and when I did, I was overwhelmed by the kindness, care, and thoughtful treatment the nurses gave me. I love the way they ‘unfold’ in front of me, relating how I’m struggling to stay alive, how the nurses keep wishing me to fight to get better, how I’m progressing and all the details of the things they do for me, like proning me, shaving me (!), telling me stories, playing me the playlist that my family sent me and much, much more. And then at the end, they wish me well, giving me advice about how to take it day by day and how to be patient.
Now I can go back and look at the letters, read them, pore over them and take great comfort from the fact that people worked day and night, to keep me alive. I was a complete stranger to them and yet they treated me with the kind of care that we parents give our children. For all this, I am supremely grateful and it’s especially wonderful to have this record of what those fine people did for me.”
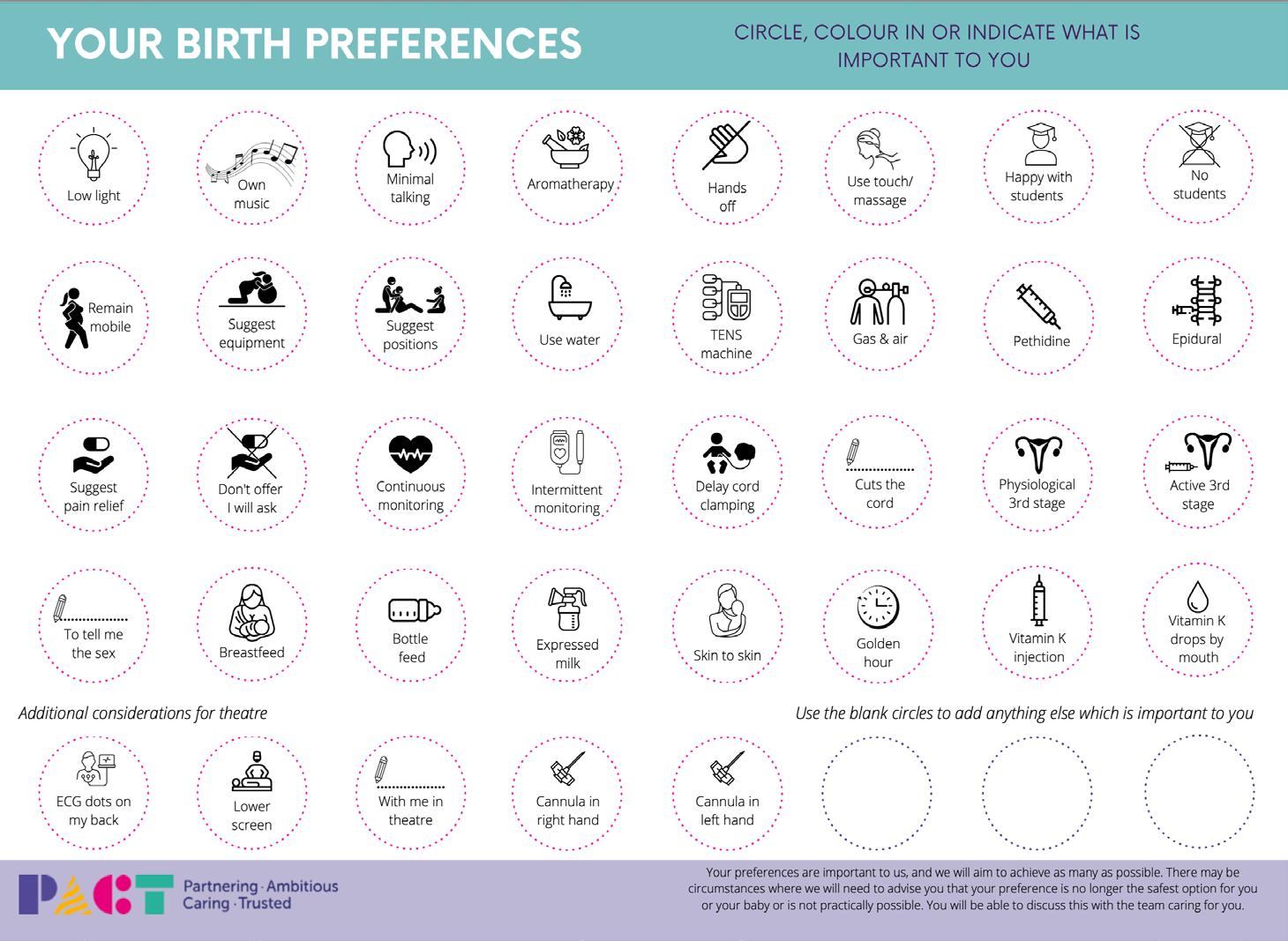
A birth preferences card was devised following feedback from service users through our User Experience (UX) card, an initiative unique to SaTH that shapes developments in our Maternity Services by ensuring that their voices are heard through a structured format of suggestion, feedback and collaboration.
The card is an easy-to-understand visual guide which is displayed in a large format in every birthing room in the Delivery Suite and MLU for expectant mums and maternity staff to view and complete together. The card has been further developed to ensure that women’s choices are understood and acted upon leading up to, and during labour.
The card was co-produced by our Maternity team and the Shropshire and Telford & Wrekin Maternity Voices Partnership.
It is given to service users at their 28-week appointment to take home and reflect on, before completing it with their midwife at their 32-week appointment. The card will then stay with them throughout their birthing journey to ensure their preferences are always clear to their care team.
Skye Rolfe, a midwife on Delivery Suite, said: “Having the birth preference cards on the wall is great, it opens up discussion about birthing options ensuring preferences are valued and respected. I love that they can be filled in by women and their partners or by their midwife on their behalf. We’ve had great feedback so far with some good suggestions as to how they can be further developed to encapsulate more potential preferences.”

Emily Evans, Service User Chair for the Shropshire and Telford & Wrekin Maternity Voices Partnership, said: “This
latest development of the birth preferences card is fantastic for our local service users. Having them in birthing rooms means midwives can act on preferences quickly to ensure the desired environment for labour. The large-scale versions also include space for the birthing person’s name and the name of those supporting them, making it easy for staff entering the room to see.”
We continue to listen to expectant mums and their families to help us to drive improvements in our maternity services.
As part of our Getting to Good improvement programme, we are committed to improving our maternity services so that we can provide the best care for the communities that we serve.
Both the first and final reports from the Independent Review of Maternity Services, chaired by Donna Ockenden, include ‘Local Actions for Learning’ for SaTH, and ‘Immediate and Essential Actions’ to be implemented across all maternity providers in England. We are completing these actions in a thorough and timely manner, running alongside our Maternity Transformation Programme which is driving sustainable change in our maternity services. Our progress
The First Independent Review of Maternity Services, chaired by Donna Ockdenden at SaTH, published in December 2020.
85% of all actions, which equates to 44 out of 52 actions, from Donna Ockenden’s first report have now been delivered at SaTH.
Of these actions, 42 have been 'evidenced and assured', and three 'delivered, not yet evidenced' following our reverse RAG (red-ambergreen) rating system and assurance processes.
With the exception of one internal action, all 13% (seven) of the 'not yet delivered' actions lie outside of the Trust’s control, and rely on external dependencies, for example NHSE, for them to be implemented fully.
The Final Report, presenting Findings, Conclusions and Essential Actions from the Independent Review of Maternity Services, chaired by Donna Ockdenden, published in March 2022.

41% of all actions, which equates to 64 out of 158 actions, from Donna Ockenden’s final report have now been delivered at SaTH.
Of these actions, 50 have been 'evidenced and assured', and 14 'delivered, not yet evidenced' following our reverse RAG rating system and assurance processes.
Good, continued progress has been made against the 63% (100) actions 'not yet delivered', with 45 out of 100 actions listed as being 'on track'.
There are 22 remaining actions to analyse from the final report - these actions either have
"We are continuing to make progress across actions from Donna Ockenden’s Review of our maternity services and we are pleased that this has been recognised by both internal and external groups, including the Care Quality Commission (CQC). However, we know that there is more to be done, and we are determined to continue the good work carried out by our teams in a visible, measurable and sustainable manner.”
 Annemarie Lawrence Director of Midwifery
Annemarie Lawrence Director of Midwifery
external dependencies (20) or more complex actions (two).
A number of multidisciplinary team ‘away days’ have been planned to analyse and plan work on these actions.
The Ockenden Report Assurance Committee (ORAC) continues to meet monthly and is live streamed to the public. This meeting considers not only the progress being made with the actions, but also the positive impact the changes are having on the services provided to women and families.
As part of our Getting to Good improvement work, we are rejuvenating the way we are recruiting to our workforce.
It has never been more important to inspire, attract and recruit the very best to ensure our Trust is the best it can be for our patients, communities and colleagues.
In order to do this well, and to be more efficient, we have been working to reduce the time it takes to get a new recruit in post meaning fewer vacant roles and earlier onboarding.
Efficiency in recruitment is imperative. To set the scene, in August, 209 jobs were advertised. We currently have 688 applicants in the recruitment system as well as 277 roles at the interview stage. To date we have completed 219 ESR forms in September and expect this to continue to rise. In the last two months, the Recruitment team has also attended 11 events including external career fairs and targeted internal events for areas such as ED, Therapies and Catering.
So what are we doing?
We have introduced the onboarding module on Trac which automates the pre-employment paperwork by populating it from the application. This reduces the time it takes for applicants to complete their paperwork and move onto the next stage.
Social media has always been a great place to find new talent and we are increasing our use of this channel, alongside targeted campaigns, staff stories and videos.
We have introduced a new job pack template to make our job descriptions and person specifications more appealing and competitive. We are going back to basics. We are reviewing each step of the recruitment process,
identifying any blockages and introducing or amending processes to help combat these.
...it is imperative that we attract and retain fantastic people in our Trust.
The recruitment intranet page will soon include a new step-by-step guide, video and FAQs for managers to support them through the recruitment process.
Louise Barnett, Chief Executive, said: “The vital work we do every single day would be impossible without the contribution of a broad range of people, and a diverse and inclusive workforce. This is why it is imperative that we attract and retain fantastic people in our Trust. Thank you to colleagues in recruitment for their hard work in streamlining our processes for our staff and this is a great start, and really encouraging as we know we have much more still to do.”

the right people and having high quality job adverts with clear job descriptions and person specifications is an important part of this. We are seeing significant progress in this area, with an increase in job applications received.
An improvement programme is in progress being driven by our Medical People Services Team. One area of focus is improving our staff rotas. Having robust rotas that offer safe working hours is not only crucial for the health and wellbeing of colleagues, it also impacts on the patients we serve.
We have been reviewing a number of rotas to ensure they are compliant and in line with minimum staffing requirements so that we have the right people with the right skill mix at the right time.
Wendy Mann, Assistant Director for Medical People Services, said: “As a Trust we are overreliant on bank and agency medical staff and we are working to rationalise this. The LMS system (for booking agency doctors) and the managed bank system are helping us to make better use of our resources and improve workforce planning.
“There has also been improved reporting on related spend since August, which allows us to make better informed decisions for our colleagues and patients.”
Enhancing our recruitment resources is another element of this improvement work. We need to make a positive first impression to attract
The Trust has also been successful in recruiting to a number of hard to fill specialities, including Oncology, Anaesthetics, Gastroenterology, Breast Surgery, Paediatrics and Neonates.

A comprehensive training and development programme is in place for the team to further support and build on this work.
We have received specialist advice on the terms and conditions of all our medical and dental contracts. It has involved us reviewing current policies and practices, developing a compliance checklist for all recruitment (substantive and bank) in line with the NHS 6 employment standards, reviewing all medical and dental contracts, and improving the efficiency of our expenses approval process.
Wendy said: “There have been some significant steps forward, and we are grateful to all colleagues involved in bringing these improvements to fruition. A comprehensive training and development programme is in place for the team to further support and build on this work. We know we have a lot more to do and are committed to working with other teams across the organisation to achieve excellence in all we do. Please do get in touch if we can help in anyway."
Strengthening and supporting our medical workforce is one of the priorities within our Getting to Good Programme to ensure that we are able to provide the best quality care for our patients every day.