


2023 | Issue No 2 BUILDING THE FUTURE OF PUBLIC HEALTH
April
"CPHA: Colorado’s Medicine is a take on the CPHA logo of white mountains, a sun, and fields encircled by blue. In the collage these details have been incorporated to bring the logo to life, connecting it to Colorado’s landscape and reminding the viewer of CPHA’s good work in improving Colorado’s public health."

 CMixed media, acrylic, and paper collage on foam board, 11x14 inches
CMixed media, acrylic, and paper collage on foam board, 11x14 inches
2



"Since RISE Magazine’s launch in May 2022, a new generation of public health leaders and practitioners has joined efforts to advance health, justice, and equity in our communities and legislature."
3
Wivine Ngongo CPHA President
FEATURED PIECES

Assessment of Telemedicine and Access to Care in Rural Areas
Cooking for Health and Pleasure: Beans
COVID-19 Pandemic and Depression Among Children and Adolescents
Improving Health Equity Through Leadership Development
Advancing Community Health with Hospital Community Benefit Spending
COVID-19 and Vaccine Hesitancy: A Literature Review
The Financial and Emotional Costs of a Baby in the United States
Advocacy Day at the Capitol
How a Federal Bill Becomes Law
Interpreter Services in Healthcare: An Untapped Resource in the Broad Area of Public Health
It's Monday, It's Tuesday, It's Another Ozone Alert Day!
Prevention Of Vision Impairments in Colorado Latinx Populations
What’s Gone Wrong?
AI in Healthcare: An Exploration of Health Disparities in Technology
Implementation
The Struggle is Real But So is Our STRENGTH! Legal Precedent in American Courts
Leadership Team Letters from Leadership 6 8 10 12 14 17 26 30 32 36 38 39 42 45 48 49 52 54
4
TABLE OF CONTENTS
OUTSTANDING EMERGING LEADER RECOGNITIONS

Smiles by Siddani: CPHA's Outstanding Leader Spotlight
Outstanding Leader in Our Community: Raeven Clockston

CONTRIBUTORS AND REFERENCES Authors and Artists References 16 22 58 63
5
TABLE OF CONTENTS
RISE LEADERSHIP TEAM
Lisa Peters
Editor-in-Chief & Co-Founder of RISE Associate Director of Membership
Lisa Peters is a Senior Reimbursement Analyst at Centura Health, specializing in data analysis, and state and federal cost reporting. As a Board Member of the Colorado Public Health Association since 2021, Lisa has creative designed, driven, and lead projects using process improvement methodologies, leadership strategies, program evaluation, and change management skills to build programming for students and early careerists. In September 2022, Lisa was awarded the John Muth Award due to her contributions toward cultivating a community for those entering public health that connects them
Hannah Craig Executive Editor

Hannah Craig is a Master of Public Health candidate in the Environmental and Occupational Health Department at the Colorado School of Public Health. She received her bachelor’s in public health and environmental studies from Tulane University in 2018. Her early career experiences have been in food systems, migration, and environmental health research

6
Chelsea Sobczak Executive Editor



Chelsea Sobczak is a Research Services Senior Professional at the University of Colorado School of Medicine She works across projects focused on increasing equitable access to care, and equipping practices to better support their patients in the Department of Family Medicine and the Practice Innovation Program
Chelsea received her bachelor’s in Dietetics with a minor in Global Health (2015), and after working as a nutrition practitioner, chose to focus on healthcare access and education by pursuing her Master of Public Health with a focus in Community and Behavioral Health (2017).
Sami Wilson Executive Editor


Sami is an MPH student in the Global Community and Behavioral Health concentration at CU Anschutz. She is passionate about sexual and reproductive health, and currently works as a Clinical Research Coordinator in the Division of Family Planning at Anschutz She hopes to pursue a career promoting reproductive justice among underserved communities and teens
RISE magazine has been a great opportunity for Sami to utilize her love for both writing and public health after studying English and Environmental Health during her undergraduate degree She is interested in using her interdisciplinary background to draw connections across fields and topics within public health



Outside of work and school, you can find Sami hanging out at coffee shops, enjoying outdoor activities, and reading fantasy novels.

THANK YOU TO OUR RISE EDITORS!
Lexie King
Joanna Garcia Taylor Bostic
Hridith Sudev
Cole Jurecka
Saquib A. Syed
Mckenzie Schrank
7
Cecilia Bedard
LETTERS FROM LEADERSHIP
I am so excited and grateful to celebrate the first anniversary of CPHA’s RISE Magazine with you! In its inception, our Emerging Leaders Committee elevated specific topics, communities, and leaders paving the way towards public health through the collection of academic articles, human stories, and local artwork. RISE’s first Issue personally enhanced my knowledge around diabetes prevention in LGBTQIA+ populations, communityengagement science efforts in predominantly BIPOC* neighborhoods, and policy reform efforts in public health education The Public Health crossword puzzle was a bonus (pg 12)! To current ELC leaders Samantha Bertomen and Jeni Mitchell, I am grateful for your guidance and commitments to not only a healthier Colorado, but a more knowledgeable one

Since RISE Magazine’s launch in May 2022, a new generation of public health leaders and practitioners has joined efforts to advance health, justice, and equity in our communities and legislature. They have joined local and state public health entities to work against COVID-19 vaccine misinformation and disinformation campaigns, targeted racism, increased gun violence, and worsening health disparities experienced by BIPOC, LGBTQIA+, and immigrant/refugee populations Their voices have added to the choir of environmental health champions and their hands elevated to the work that addressed climate change in a world of avid deniers Some of our emerging leaders have joined our public health friends in advocacy to engage policy in birthing rights, public safety, and behavioral health, even in the face of exacerbated political polarizations and sustained public health backlash. And they have supported communities forging new pathways towards collective health and wellness from
within a landscape that continues to push them out We have seen and experienced so much by way of racism, misogyny, heterosexism, xenophobia, antisemitism, ableism, and science denial over the last year To my friends and colleagues new to public health, I am honored to rise above it alongside you.
When love and science prevail in the name of public health, intolerance and misinformation are likely to push back. And because of that, the Colorado public health workforce continues to draw new leaders every day and grow stronger than ever. The following articles honor some of the latest public health efforts and champions our wonderful Editors and Contributors had the privilege to engage Thank you, Emerging Leaders Committee, for showing us where action and science meets humanity And thank you, Colorado Public Health, for sharing this journey of love and science with us
Wivine Ngongo CPHA President
8
LETTERS FROM LEADERSHIP

The field of public health has transformed throughout the past few years, and public health professionals are doing important work within our communities during this shift. As our workforce continues to face new challenges, leaders within public health always rise to the occasion and set forth creative solutions that consider history and systematic disparities while also harnessing the power of existing strengths. This year in the Colorado Public Health Association, we’ve had the pleasure of watching seasoned public health professionals come together with emerging leaders within the field to connect, share knowledge, and provide mentorship This is just one of the many examples of how we see the field of public health growing and reenergizing
Today’s public health emerging leaders are clever, innovative, empathetic, and tenacious. We are humbled to see the enthusiasm, excitement, and dedication that these professionals are bringing to the field of public health In this second edition of RISE Magazine, we hope that our readers can feel this passion and excitement Thank you readers, sponsors, and editors for supporting RISE Magazine over the last year your contributions enable us to continue to elevate the voices and perspectives of Colorado’s emerging leaders who will transform the field of public health!
Samantha Bertomen & Jeni Mitchell Emerging Leaders Committee, CPHA

9
Assessment of Telemedicine and Access to Care in Rural Areas
Garvita Thareja, Eric Cox, Tracey Wood, and Maryssa Yarbrough
Telemedicine is essential because it addresses barriers that individuals may face in rural areas. It conveys many benefits that can be used by individuals unable to regularly commute from their homes Americans living in rural areas tend to experience higher rates of disease, such as high blood pressure and obesity, than those who live in urban areas High rates of poverty and lower rates of physical activity have also been reported among rural dwellers These factors may put rural individuals at higher risk for poor health outcomes (American Hospital Association, 2019). Telemedicine can link individuals to health care services that can prevent or treat various diseases and conveniently connect individuals to physicians. In 2022, when COVID-19 affected the healthcare industry, the growth of telemedicine was remarkable Virtual health care technology has increased health care value and affordability Patients are able to save time and money, and visits to emergency and urgent care centers are reduced with the use of telehealth services In rural America where health care services are significantly harder to access than their urban counterparts, the need for inexpensive and quality care is critical and telemedicine may be the answer to bridging the gap of accessing quality healthcare.
Background
During the COVID-19 public health emergency, reimbursements for telehealth have continued to evolve. Telemedicine substantially increased healthcare affordability leading to many federal policy changes in 2019 and 2020 that have made it easier for healthcare providers to offer this service delivery (Persaud, 2022) The goal of telehealth is to also provide better access to health care while still maintaining medical income for health care organizations One of the
most successful applications of telehealth is the reduction of health care disparities in areas where there is limited access to physicians
Approximately 20% of the US population resides in rural areas, and only 9% of physicians serve these areas (Persaud, 2022) Telehealth aims to eliminate transportation costs, which often burden patients of low socioeconomic status In addition to improved access, it is estimated that telehealth could save the U.S. healthcare system more than $4 billion annually. The use of technology could reduce referrals and wait times, streamline medical evaluations, and decrease the burden of some preventable diseases. As an example, patients who are being treated for chronic diseases account for 75% of medical expenses. Telehealth proposes to lower these medical expenses by monitoring patients at home, ensuring medication adherence through electronic means, and providing expeditious access to a physician In this way, the financial burden of hospital readmissions can be curbed (Persaud, 2022) During the pandemic, the push to make telehealth services widely available was a temporary measure It has now become a common health care service delivery due to its potential to take down barriers in access to critical health care services. Future expansion of healthcare services in rural areas will depend on the continued evolution of telemedicine.
Discussion
In 2020, social distancing due to the COVID-19 pandemic made it essential for healthcare providers to deliver healthcare services in different ways Years after the pandemic, telehealth is still a widely used service tool in healthcare and has become a permanent form of healthcare service delivery in rural areas due
10
to its flexibility in providing services. Telemedicine can support underserved rural Americans with many health care advantages such as increased access to specialists, mental health care, and fewer hospitalizations. Americans who reside in rural areas face many disparities to health care such as the cost of treatment, availability of the physician/specialist, and access to transportation However, to improve healthcare practices, it will be important to understand and conduct research regarding the efficacy and trends of telehealth in rural areas over the years In 2022, a research study was conducted by Kolluri, et al., to understand rural dwellers' experiences with telehealth. The researchers found that participants had significantly positive experiences when using telehealth services. This study allowed researchers to understand how telehealth can bridge gaps in healthcare service delivery for those who reside in rural areas.
Telehealth may be an ideal form of healthcare delivery for rural dwellers, however, internet connectivity is essential to successfully using this service Lack of internet use has been reported in rural areas which can generate another barrier to accessing health care A research study was conducted in 2021, by Holloman, Obermier, and Burger to assess the digital divide in rural areas. Rural areas face inequality when accessing broadband services compared to urban areas. In rural areas internet costs, availability, and packages are limited. As one travels away from a populated area, internet connectivity and speed decreases. Holloman, Obermier, and Burger acknowledge the need for further scientific research to accurately understand trends associated with internet access in rural areas
Even though the research study conducted by Kolluri, et al, saw significantly positive experiences for patients using telehealth in rural areas, other research has found that physicians face challenges when using telehealth services In 2021, a comparative qualitative research study was conducted among 42 physicians in Quebec and Massachusetts. The study found, “the negative
impacts of telehealth on interprofessional work, including reported feelings of isolation due to the absence of interpersonal contacts and the loss of impromptu moments of socialization” (Breton et al., 2021). This study suggests some healthcare professionals who provide telemedicine services may have negative experiences such as feelings of isolation and loss of socialization. Thus, it is important to understand that physicians and patients may have differing perspectives concerning telehealth. Clinical appropriateness may be an essential variable to determine when telemedicine and in-person visits are suitable Despite some research studies finding negative impacts of telehealth services among physicians, it is important to understand that many surveys over the past several years have found using telehealth services to be a positive experience for patients in rural areas
Implications
Individuals living in rural areas can experience various barriers such as limited transportation, poverty, and higher rates of disease. Specialized care and access to health services are essential to breaking down disparities for those who reside in rural areas Telemedicine may be the answer to bridging many gaps and increasing health care services to underserved populations This service delivery mode can be a great option for those who belong to vulnerable populations such as older adults, children, rural dwellers, and minorities Focus group, observational, and experimental studies should be conducted to identify the strengths and weaknesses of telehealth services and delivery. Further research in this area is certainly necessary to understand how telemedicine services affect access to healthcare and health outcomes among rural Americans.
11
"Specialized care and access to health services are essential to breaking down disparities for those who reside in rural areas."
Cooking for Health and Pleasure: Beans


 Amanda Skidmore
Amanda Skidmore
Beans are well-known for their health benefits and have recently gained attention as a foundational component of the diet in “blue zones,” where people tend to lead especially long lives In fact, author Dan Buettner posits that “the cornerstone of a longevity diet is beans”
Not only are beans a good source of fiber, protein, and minerals, but they also taste good and can be a valuable addition to a hearthealthy diet. If you are not familiar with cooking beans, there are several ways to incorporate them into your meals. For instance, you can add a cup of beans to a soup, a salad or grain bowl, or in a burrito, taco, baked pasta, or casserole. If you enjoy hummus, a popular bean dip of pureed chickpeas, olive oil, and tahini, consider pureeing or smashing other beans to use as a ,
dip or spread While darker beans such as black brown, and red have slightly more antioxidants, white beans have a more neutral flavor Therefore, if you want the health benefits of beans but are a bit unsure about the taste, white beans can be a good place to start
Beans tend to have a better taste and texture when cooked from dried, versus canned. They are also most cost-effective when purchased dried, with a pound of dried beans yielding 3-4 cans when cooked. Cooked beans freeze well, so you can prepare a whole pound and freeze them in smaller bags for later use. However, if you don’t have the time or space to cook beans from scratch, canned beans remain a great alternative Do not let the lack of time or space stop you from experimenting with such a nutritious, tasty, and cost-effective food source!
CPHAEmergingLeaderscommitteehosteda volunteereventwithDenverUrbanGardens 12
Pizza Beans: A Recipe
Recipe:
2 tablespoons (30 ml) olive oil
1 large onion, chopped
2 celery stalks, diced
1 large or 2 regular carrots, diced
Salt and freshly ground black pepper or red pepper flakes
2 large garlic cloves, minced
1/4 cup (60 ml) dry white or red wine
(optional)
4 ounces (115 grams) curly kale leaves, chopped or torn
2 1/4 cups (550 grams) crushed tomatoes (28ounce or 800-gram can minus 1 cup; reserve the rest for another use)
1 pound (455 grams) cooked firm-tender giant white beans
Up to 3/4 cup (175 ml) vegetable broth
1/2 pound (225 grams) mozzarella, coarsely grated /
Instructions:
Heat the oven to 475 degrees In a 2 1/2-to-3quart (ideally oven-safe) deep sauté pan, braiser, or shallow Dutch oven, heat the olive oil on medium-high. Add the onion, celery, and carrots.
Season well with salt and black or red pepper. Cook, sautéing, until the vegetables brown lightly, about 10 minutes. Add the garlic and cook for 1 minute more. Add the wine, if using, to scrape up any stuck bits, then simmer until it disappears, 1 to 2 minutes. Add the kale, and cook for 1 to 2 minutes, until collapsed, then add the tomatoes and bring to a simmer Add the beans, and, if the mixture looks too dry or thick (canned tomatoes range quite a bit in juiciness), add up to 3/4 cup broth, 1/4 cup at a time Simmer the mixture together over medium for about 10 minutes, adjusting the seasonings as needed
Bake: Sprinkle the beans first with the mozzarella, then the Parmesan, and bake for 10 to 15 minutes, until browned on top. If you’re

“The cornerstone of a longevity diet is beans." - Dan Buettner
COVID-19 Pandemic and Depression

Among Children and Adolescents
Garvita Thareja, Jessica Chuong, Calina Hilyard, and Thalia Rodriguez
Introduction
The COVID-19 pandemic has impacted society in many ways. This article aims to understand how much these adverse effects of COVID-19 have affected children and adolescents aged 018. Research suggests fear, anxiety, higherstress levels, and depression have risen during this time for most people. However, to what extent are our children and youth impacted? This article investigates how the pandemic period has influenced depression rates among this demographic
The Center for Disease Control and Prevention states that depression diagnoses become more common as children age Depression is a mental health challenge that can lead to other high-risk behaviors such as suicide or self-harm. Research suggests that before the year 2019 (when the pandemic began), approximately 2.7 million children, ages 3-17 years, were diagnosed with depression (Centers for Disease Control and Prevention,
nd) Since the pandemic, one in six children have reported showing daily to weekly symptoms of depression (Zablotsky et al., 2022). Therefore, understanding the relationship between COVID-19 and children and adolescents' mental health is essential to help decrease rates of depression in this population (NSSI) (Thompson, 2008).
For this research, a systematic review was conducted through scientific databases to review the impact of COVID-19 on the mental health of children and adolescents (18 years or younger) This search used the Preferred Reporting Items for Systematic Reviews and Meta-analysis (PRISMA) Through this analysis, articles including similar variables when analyzing the relationship between COVID-19 and children and adolescents' mental health were utilized. Inclusion criteria and key terms were used such as mental health, mental illness, illnesses, stress, suicides, COVID-19, and pandemic to further narrow our search.
14
CPHAEmergingLeadersCommitteeshowstheircommitment totheircommunity,volunteeringwithEkarFarm
Results
The database search resulted in 64 articles eligible for evaluation Of these articles, 12 were eligible for utilization All of the 12 articles were conclusive and each displayed evidence of COVID-19’s impact on depression in children and adolescents 18 years of age and younger. These studies reported environmental factors impacting children and adolescents including lockdown (Nearchou et al., 2020), lack of socialization (Śniadach et al., 2021), financial stresses (Adegboye et al., 2021), and increased social media usage (Listernick & Badawy, 2021).
Future Considerations
Our research analysis displays the importance of continuing research on the relationship between COVID-19 and children and adolescents Currently, this research is limited and therefore needs to continue Additional research will help determine preventable measures against depression risks and other
mental health challenges associated with depression As the United States moves further into a post-pandemic era, understanding the relationship between COVID-19 and children and adolescents will aid in the support efforts of this population.
To combat the impacts of mental health on children and improve those already impacted, education systems will need to consider the depression levels of their students. This will require educators to reassess learning tools used For example, educators may consider reduced use of screen time in the classroom to combat the overuse of technology during the lockdown and virtual learning Children and adolescents' long-term depression will need to be monitored moving forward These initiatives will need to be a combined effort with parents of these populations. Parents will need to be cognizant of their children’s stress levels and how their perceptions of COVID-19 pandemic are perceived by their children. Screening tools can be implemented, such as Pediatric Symptom Checklist (PSC-17) or the Screen for Child Anxiety Related Disorders (SCARED), and they should be required to be used during check-ups to gather data and ensure children exhibiting depression symptoms receive proper intervention and treatment (Listernick & Badawy, 2021) A greater understanding of this relationship will also allow for better preparation and minimization of the mental health consequences of future outbreaks like COVID-19
 Figure 1. PRISMA diagram – data synthesis of 64 articles screened, resulting in 12 articles chosen for review
Figure 1. PRISMA diagram – data synthesis of 64 articles screened, resulting in 12 articles chosen for review
15
"All of the 12 articles were conclusive and each displayed evidence of COVID19’s impact on depression in children and adolescents 18 years of age and younger."
Smiles by Siddani

Oral health is an essential component of overall health, and its importance in public health cannot be overstated Dr Pujitha Siddani is a dentist committed to improving children’s oral health through public health strategies Dr Siddani's journey to becoming a pediatric dentist is an exceptional one that exemplifies the values of hard work, dedication, and passion
Dr. Siddani’s dental career began in India and sparked her interest in public health after she volunteered at a non-profit organization in India that cares for children through orphanages. The unaddressed dental needs of many children in the orphanages highlighted to her the influence and crippling effects of health disparities on children with no healthcare access To address this need, Dr Siddani developed a large-scale oral health program to bring dental services closer to the 7,000 children living in orphanages It was this experience that strengthened Dr Siddani’s resolve to pursue advanced education in the US to become a pediatric dentist competent in public health and with the ability to improve oral health outcomes for children from underserved communities.

Dr. Siddani’s training in public health enabled her to focus on advocacy and policy efforts to have a significant impact on children’s oral health in the US. She worked tirelessly in collaboration with schools and community partners to increase access to oral health services by linking children, youth, and families to no or low-cost dental resources Dr Siddani's advocacy of mandatory annual dental screenings (AB 1433) in California assisted in delivering dental services through school-based health centers to countless students in Los Angeles county Her outstanding contributions to the field of children’s oral health have been of tremendous consequence, especially for children with disproportionately high dental needs.
CPHA'S OUTSTANDING LEADER SPOTLIGHT
Dr. Siddani believes that every child’s well-being is deeply connected to the health and wellness of their community. She incorporates public health strategies and concepts into her practice model to ensure a positive influence at a community level Dr Siddani provides exceptional care for her patients in rural Colorado and offers dental services for special needs children in an environment that accommodates their unique needs She continues to be an advocate for high-quality dental care and its positive impact on children's overall health and their ability to thrive. Dr. Siddani’s commitment to public health and improving access to dental care is commendable and inspirational.

16
p g q y g
Leadership Development
 McKenzie Schrank
McKenzie Schrank
When someone walks into a healthcare setting, there is a wide array of experiences they might have. If they are lucky, they might interact with a provider that has the capacity to listen and have a full conversation, and will dutifully tend to their needs. However, currently, in the American medical system, many providers are stretched thin and burnt out while others, in my experience, do not have the social skills or training to have effective conversations with their patients.
I knew I needed to go into preventative medicine before I even knew what public health was This decision was rooted in personal experiences that exposed the shortcomings of our healthcare system in treating patients
Growing up as a track athlete and the daughter of physical therapists, I was accustomed to attentive and effective care. However, when seeking medical attention as a college athlete and young adult, I found that healthcare professionals often dismissed my concerns and failed to provide adequate treatment. When my symptoms were not easily diagnosable, I had to advocate for myself to receive the care I needed.
Reflecting on my experiences in various healthcare settings, there have been times I’ve felt the provider did not understand me when I explained certain symptoms that could not be definitively seen or diagnosed by whatever test that provider conducted
CPHAEmergingLeadersbuildnewconnections atavolunteereventwithDenverUrbanGardens 17
tIf I had not insisted on a treatment plan aside from “rest and fluids”, several issues could have been way worse than they ended up being. In these situations, I find myself feeling like I did in college in the athletic trainer's office after I knew I had injured my ankle during track practice. I remember trying to convince them that something was truly wrong; as if there needed to be a defined issue in order to be offered anything that would aid my pain or be treated with dignity and respect. As someone who has access to medical insurance and privilege in society, I recognize that those without these advantages face even greater barriers to quality healthcare
Lack of Empathy from Healthcare providers and The Hidden Toll of Racism
An issue that further compounds these communication issues for people of color is systemic racism and microaggressions. In Linda Villarosa’s book Under The Skin: The Hidden Toll of Racism on American Lives and on the Health of Our Nation, she tells the story of a woman who lost her baby due to complications during her pregnancy that medical personnel did not address adequately The patient came to the emergency room with legitimate complaints prior to going into labor, and the medical providers she saw sent her home where she continued to bleed The patient described feeling ignored while doctors downplayed her complaints
Black women across the United States are suffering from mistreatment, racial bias, and toxic stress triggered by discrimination. Villarosa notes that the consequences of this systemic injustice are dire, with rates of maternal death during pregnancy and childbirth increasing at an alarming rate, particularly among black
women even those with higher income and education, which should help protect them against negative outcomes (2). I have been fortunate enough to receive the upbringing and education necessary to advocate for my own health and well-being, and to be heard when I’ve expressed additional concerns. However, the individuals described in these stories were not afforded the same opportunity due to the pervasive impact of structural racism. Healthcare providers who fail to adhere to the principle of "do no harm" are complicit in perpetuating this injustice
So what is the solution?
Awareness and conversation are not enough Community leaders, stakeholders, and medical professionals must be trained, confronted, and ultimately transformed into the leaders and agents of change we need them to be. If healthcare providers had the tools and training to have effective conversations with patients of all backgrounds, many life-threatening medical issues could be prevented, and treatment would be more successful. Then, if truly preventable diseases are circumvented, the medical system will be less burdened Lastly, if we bring people who have experienced the shortcomings of the American medical system into leadership and healthcare provider roles, they would better relate, converse with, and treat patients who are currently underrepresented and marginalized in those roles
As someone with privilege, I feel a responsibility to advocate for those who are marginalized and to shed light on the health inequities that exist in America. It is apparent to me that individuals without these privileges must fight to be heard and receive the care they need and deserve. While the issues I have come across as a patient
“Knowing is not enough, we must apply. Willing is not enough, we must do”
18
– Johann Wolfgang von Goethe
in the American healthcare system have caused inconveniences and frustration, I know marginalized communities suffer severe consequences, both in the short and long term.
To this end, I want to bring attention to a program dedicated to empowering underrepresented voices and equipping communities with the skills needed to address health disparities that exist in America. As public health professionals, we have the platform and an obligation to advocate for those who cannot advocate for themselves
The Colorado Collective Leadership Initiative
People, especially from marginalized communities, should be able to advocate for themselves in a healthcare setting and be heard by the people who are working to prevent and treat their ailments. They should also have the opportunity to be the leaders and agents of change that provide unbiased, equal treatment not just in the healthcare setting, but all over Colorado. That is why I have partnered with the Center for Creative Leadership (CCL) as a Communications Specialist for their newly launched leadership program This program is a partnership with The Colorado Health Foundation (TCHF) and is called the Colorado Collective Leadership Initiative (CLI) The Collective Leadership Initiative was highly informed by community members through interviews with stakeholders such as health and program leaders. The program was designed with the goal of creating better health and wellbeing for all Coloradans. It brings together individuals working in formal and informal leadership roles to tackle real health equity challenges in Colorado communities.
hCo-designed and delivered by the CCL, this program offers a unique experience where participants – regardless of job title, skill level, or experience – can choose how they want to expand their community leadership skills and networks to have a greater impact, free of charge. Dedicated to racial justice, equity, and diverse representation in learning groups, participants work in teams with others across the state and their communities to tackle current, pressing health equity challenges This is achieved through Action Learning Projects During the 2022 program year, projects covered topics such as housing, resource access, food systems, and mental health Types of education provided include experiential leadership development, team coaching, access to the latest leadership development content, and opportunities to learn from experienced individuals, ask questions of panels, and participate in site visits. One alumnus stated she never had access to the type of leadership training she received during the program and learned more about herself and her leadership style just from completing one of the initial assessments.
During the pilot year of the Colorado Collective Leadership Initiative (CLI) in the spring of 2022, 95 leaders completed the program and gave feedback during and after participation Participants cited direct impacts on their personal networks, growth, knowledge, and skills Overall, 91% of responding leaders indicated they were on target or better in the focal leadership capabilities, and 75% indicated they were on target or better in the focal technical capabilities (1). Several leaders acknowledged specific helpful skills they learned during the program such as project management, communication, and time management skills.
19
One expressed, “In CLI, I learned resilience skills, which are beneficial to myself, and as secondary knowledge, I can share with others” Leaders also benefited from the guidance of mentors provided by the program Another leader said, “I learned from my mentor to recognize my bias and then to approach difficult situations from a lens of acknowledging the bias" (Kosovich, 2023) Beyond the leadership development program, these leaders are now part of a leadership collective they can lean on and reach out to send their messages farther and wider than they were able to before.
An initiative ready to learn and evolve as leaders need
Updates will be made to each program to increase the impact of this unique program utilizing feedback from the 2022 participants Leaders gave feedback through formal and informal structures: morning debriefs, daily surveys, and side conversations This feedback changed program structure, content, and various other elements immediately when possible.
Using feedback gathered directly from program participants is just one example of how the CLI is working to increase health equity by providing space for marginalized community members to express how the
initiative should be changed to meet their needs and the needs of future participants In this way, the Colorado Collective Leadership Initiative is not only giving community members a voice, but also gathering leaders from across the state to join together to bring much-needed awareness to health equity and access issues
Lolina, Inc is a healthcare and public health consultancy. They work with clients to strengthen essential components of the healthcare system to achieve improved population health. http://lolina-health.com/

Want to learn more or be involved?
Applications for the 2023 cohort are now closed; however, Individuals who identify with and serve communities of color, women, LGBTQ Coloradans, and those from formal or informal organizations who are passionate about improving health equity for all are strongly encouraged to apply for the 2024 cohort. To stay up to date on all things related to the Colorado Collective Leadership, visit our website at https://cocollectiveleadershipwordpresscom/ and sign up for our newsletter
20

Outstanding Leader in Our Community: Raeven Clockston
Raeven Clockston is an alumna of the Colorado School of Public Health (ColoradoSPH), where she was a leader both in and out of the classroom. Her work towards anti-oppressive practices and leadership in student council has led her to her current position as Equity Specialist in the Office of Equity, Diversity, and Inclusion at the ColoradoSPH
As a student during the 2020 school year, she, like many of us, faced a year of unforeseen challenges and frustration as a multitude of social inequities came to light on a national and global scale The COVID-19 pandemic and deaths of George Floyd and Breonna Taylor, as a result of police brutality, were few of the many examples highlighting the disparities within our systems. During this time, Raeven and her colleagues came together to discuss their frustrations and reflect on their role as public health advocates. These conversations created the opportunity for the group to explore their positionality and involvement in social justice issues Their fundamental belief that racism, discrimination, and social injustice are public health issues fueled the idea that ColoradoSPH has a responsibility to equip its students with

the tools for teaching, supporting, and guiding others to engage in social justice and advocacy efforts Turning these frustrations into action, Raeven helped lead the group as they developed the ColoradoSPH at CSU Anti-Racism Student Action Group. This jump started the efforts that would pave the way for Raeven’s undertaking in leading an anti-oppressive campaign throughout her graduate career. The group created a manifesto and guidance documents to support the implementation of anti-racism, equity, diversity, and inclusion efforts at the ColoradoSPH
Raeven’s leadership in the Anti-Racism Student Action Group influenced her peers to encourage Raeven to join the student council and continue striving for systemic reform Ultimately, she knew her leadership in the student action group had armed her to take on a new position with the student council as vice president. Her role empowered her to advocate for meaningful changes in the school’s curriculum through the incorporation of anti-racist and anti-oppressive values.
Using the manifesto documents as a guide for
Joanna Garcia
22
CPHAstudentsandemergingleaderscome togethertolearnaboutengaginginassociations
systemic change, Raeven continued to promote their vision until it came into fruition. To add value to their tireless effort, the School began investing in the leaders advocating for change. Raeven was one of two students who were hired as the Coordinators of Anti-Racism, Diversity, Equity and Inclusion to focus on the integration of social justice This was the first ever paid position to work collaboratively with faculty in implementing the change demanded by the students Raeven led three student workgroups in executing various objectives to shift the program toward anti-racist practice In addition, she facilitated Black Indigenous and People of Color (BIPOC) focus groups with students within the program to collect, highlight, and elevate their stories and perspectives. The stories that emerged became the directive for future efforts to ensure that these student voices will continue to be heard and centered following her transition out of the student role
Following graduation, Raeven continues to shape the culture of the school by serving as the first ever Equity Specialist in the Office of Equity, Diversity, and Inclusion (EDI) at the ColoradoSPH Her role for the past year and a half has been dedicated to increasing EDI initiatives and making structural changes to move the program in alignment with the core commitment of dismantling structural racism. Currently she is involved in developing the ColoradoSPH Search Advocate Training Program, supporting the ongoing Inclusive Excellence Learning Series, facilitating the ColoradoSPH Campus Community Read book club, and is a leader in the Inclusive Excellence Committee (IEC) Moving forward Raeven will continue to play an integral role in the implementation of ColoradoSPH’s strategic plan in the areas of EDI The goal is to continue strengthening the ColoradoSPH community culture by fostering inclusive excellence, to ensure that diversity, equity, and inclusion are central to the school’s academics, research, practice and service.
Journey into Public Health
Can you describe your personal and professional journey to public health?
I was always interested in equity work, but I took a bit of a winding path into public health At a young age I realized there were striking health inequities between Black, Indigenous, and communities of color compared to their white counterparts, and hoped to use nutrition as a vehicle to address some of these concerns in Colorado During high school I determined that my goal was to work in the nutrition and fitness space to increase food access; I wanted to address food apartheid. In 2015 I went to Colorado State University (CSU) to pursue a Bachelor’s degree in Nutrition and Food Science. During this time I began working as a certified personal trainer, and my lens on physical activity was centered around making movement more accessible. In my last year of undergrad in 2018, I met Dr Chrissy Chard at the Multicultural Undergraduate Research Art and Leadership Symposium (MURALS) where I presented on work I was involved in to combat food insecurity among marginalized communities within northern Colorado During my poster session, Dr Chard mentioned the connection between my research and public health more broadly and brought the ColoradoSPH to my attention.
When did you realize public health was the field you wanted to pursue a career in?
I realized my interests were aligned with public health once I learned of the 10 essential public health services, the social-ecological model framework, and the social determinants of health My path in nutrition was preparing me to influence behavior change at the individual level, but I wanted to examine things at a structural and systemic level to improve the health of populations The pivotal moment was gaining an understanding of what public health was and matching that with my lived
23
experience and goals as a professional. Regardless of where I go in this field, I know this is the profession that will allow me to make a meaningful impact.

As a student at the Colorado School of Public Health (ColoradoSPH)
What was your concentration at ColoradoSPH?
Initially, I entered the ColoradoSPH concentrating in Global Health and Disparities because I was interested in addressing health disparities and inequities as a professional As a student, I took a few epidemiology classes, including a class called Social Epidemiology which focused on the study of social exposures (ie discrimination, racism, ableism) and how they affect the community on an interpersonal level in addition to influencing health outcomes Enrolling this class was a [pivotal] moment in my career that shifted my views on the field as a profession and inspired me to pursue Epidemiology as my graduating concentration.
You played a major role in the creation of the Colorado School of Public Health at CSU Anti-Racism Student Action Group, how did this come about?


In 2020 when COVID hit and the deaths of George Floyd and Breonna Taylor occurred, as a nation we were reckoning with the real impacts of racism at all levels A group of us felt the school had a role in guiding and supporting students to engage in the discussion and become effective advocates The school was silent at a time when we were hoping for them to acknowledge our role in addressing racism as a public health crisis
We soon organized the Anti-Racism Student Action Group which started informally as peers discussing feelings of frustration Through this, we discovered discrepancies in what we should be prepared to do and what the program was preparing us for in terms of curriculum and practicebased learning components. It was validating to have colleagues express similar feelings; it’s important of your colleagues with dominant social identities that show up, engage in the conversation, and learn. It became a more structured group when we had more conversations with faculty about our concerns. The shift making us more formal was when we came together to unify our visions and expectations for the program.
During your time as a student in ColoradoSPH, what inspired you to take on leadership roles in the student council?
I was encouraged to get involved in student council by some peers and a dear mentor and faculty member Up until that point, I hadn’t seen our student council feel empowered to use their voice to push for programmatic changes I went in with the hope that I could work collaboratively to make our curriculum more anti-oppressive and address identified gaps. We expanded the influence of student council in the ColoradoSPH at CSU program and strengthened the relationship between students and faculty.
Youngprofessionalsforgenewconnectionsata CPHAEmergingLeadersnetworkingevent
CPHABoardMembersshowtheirsupportfor publichealthduringPHiR
24
RaevenClockston
Following student council, you were offered a paid position as the Coordinator of AntiRacism Diversity, Equity, and Inclusion to focus on the integration of social justice. How was this experience?
The Anti-Racism Student Action Group created a manifesto document that outlined our vision for the program and the activities that the school could implement to move us in that direction The paid student position came into play when we began working with faculty to change policies and procedures
As a student coordinator, my role required strong facilitation and organizational skills that were necessary to track progress and achieve meaningful change. We had three working groups focused on specific goals and my role was to ensure each group had all the pieces needed to move forward. The workgroups we launched focused on three main areas including (1) the development of a summer work packet that orients incoming students to the importance of EDI, (2) preparing students for their practicum with training to identify structural racism and oppression when they do community work, and (3) asking school applicants to respond to a question about the importance of health equity and their work in that field I served as a connection between the groups and the faculty by organizing meetings to have our ideas heard and implemented
Following graduation, you are now the first ever Equity Specialist for ColoradoSPH. How did you come into this opportunity?
In my last semester of graduate school right before graduation, Dr. Chrissy Chard brought to my attention that the school was looking for a Public Health Equity and Practice Coordinator. I applied and was awarded the position and a large part of the role was to build up the Office of EDI I’ve done this alongside Dr Cerise Hunt, the Associate Dean for Equity, Diversity, and Inclusion at ColoradoSPH
What were some challenges you had to overcome while leading your efforts?
The biggest challenge in a nutshell was shifting
implicit and structural biases. Part of the challenge was initially getting the faculty in our program to broaden their lens and actively engage with the student perspective. Our institution is also interesting to navigate because of the tri-campus model; each campus has its own structure and processes. In order to change something at the school level, it’s important to get all campuses on board and in alignment
What do you think is the most tangible thing that public health as a field could do to improve as a profession?
We could start by acknowledging the ways we’ve been complicit; the ways we’ve participated in these systems that serve to oppress disenfranchised and marginalized groups. Then, with that understanding, consider what the next steps are in changing our systems. We should center community voice and work collaboratively to build creative solutions. I’d like to see public health move beyond credentials to value the power and expertise that comes with lived experience
What advice would you provide to someone interested in public health?
If you feel called to public health, please come, please do it! It comes down to using your voice and the power you have to move us toward achieving health equity; everyone should be able to attain the highest level of health possible. Embrace the change and the unknown, shift as you learn, change your path or your concentration. If the society we deserve doesn’t exist right now, one that is nurturing and just, then it’s our role to dream it into existence.
25
"Embrace the change and the unknown, shift as you learn, change your path or your concentration. If the society we deserve doesn’t exist right now, one that is nurturing and just, then it’s our role to dream it into existence. "
Advancing Community Health with Hospital Community Benefit Spending
Devin Miller
As Colorado communities continue to experience health disparities and rising health care costs, increased awareness and accountability for community health promotion is needed. One area currently receiving attention is how nonprofit hospitals can better support and invest in their local communities (Zelinger, 2023). Nonprofit hospitals are uniquely positioned to make significant contributions to advance the health equity of the diverse communities in which they serve, beyond the basic provisions of providing medical care (Carroll-Scott et al, 2017) Research supports that merely relying on improving access to existing medical care resources will not, in and of itself, address the larger health issues that our nation is experiencing (Prybil et al., 2017). An ideal place to create a paradigm shift in community health investment is through the Internal Revenue Service’s (IRS) community benefit spending requirement for nonprofit hospitals.

Since the mid-1900’s, nonprofit hospitals have
been required by the IRS to provide a form of community benefit to justify their tax-exempt status (Carroll-Scott et al., 2017). Under this regulation, community benefit spending is traditionally understood by nonprofit hospitals as any activity that would benefit their community. Benefits to the community may include providing financial assistance to uninsured patients, conducting [relevant] research, or offering education and trainings to healthcare professionals (Rosenbaum 2016; Singh et al, 2015) In 2010, changes were made to community benefit spending under the Patient Protection and Affordable Care Act (ACA) These changes required nonprofit hospitals to conduct triennial Community Health Needs Assessments (CHNA) and develop annual implementation plans to address community identified needs through tailored health services and population health initiatives(Internal Revenue Service, 2010).
. The ACA encourages nonprofit hospitals to go beyond the traditional community benefits of charity care (e.g., free and reduced health care costs) to focus on the underlying causes of
inthesunshineduringaCPHAOutsideevent 26
CPHAmembersbuildtheirnetworkwhilehiking
health inequities and to allocate funds to initiatives for social determinants of health (Carroll-Scott et al, 2017; Rosenbaum, 2016)

Approximately $100 billion dollars are used for community benefit spending each year in the United States (Chandrashekar et al., 2022). In Colorado, 90% of hospitals are nonprofits and tax-exempt organizations (Colorado Department of Health Care Policy & Financing, 2021). From 2020–2021, Colorado nonprofit hospitals spent $965 million in community benefits (Colorado Department of Health Care Policy and Financing, 2023) These investment categories for Colorado nonprofit hospital community benefit spending include free or reduced-cost health care services, programs addressing health behaviors, programs addressing social determinants of health, and “other investments” that address community needs Based on a recent report, 8% of Colorado community benefit spending is committed to directly addressing social determinants of health (Colorado Department of Health Care Policy and Financing, 2023).
spending is making an impact on the community’s health (Letchuman et al, 2022)
To provide more accountability and transparency on hospital community benefit spending, Colorado passed House Bill (HB) 1320 in 2019. HB 1320 requires nonprofit hospitals to submit a report to the Colorado Department of Health Care Policy & Financing (HCPF) that include: (a) the hospital’s CHNA, Implementation Plan, and the breakout of funding that went to free/reduced-cost health care services, programs addressing health behaviors or risk, and programs addressing social determinants of health, (b) a description of how services and programs address the community identified health needs, (c) details on the public meeting hospitals are required to hold each year to gather feedback on the hospital's community benefit activities With the recent implementation of HB 1320, Colorado nonprofit hospital reporting provides more clarity on their CHNA process and data collection, but advocates continue to push for more requirements and accountability from hospitals.
Limitations
Currently, there are no federal requirements on the amount a nonprofit hospital needs to spend on community benefits, how hospitals identify and prioritize spending initiatives, or what evaluation efforts should be completed to ensure the needs are met by said investments Health advocates argue that the current IRS requirements put loose requirements on nonprofit hospitals and there is only a limited understanding into how community benefit
Despite state and federal advancements of CHNA reporting in recent years, advocates continue to highlight the many issues with current CHNA transparency and accountability Table 1 highlights the limitations of the literature One area of focus that remains a concern for community health advocates is the hospital’s methods for employing a meaningful community engagement process for their CHNA The goal of a CHNA is to understand the unique needs of the community, identify the priorities for funding from the community’s perspective, and establish sustainable partnerships (Pennel et al., 2015). Although Colorado made progress when requiring an annual public meeting, this reporting illustrates this approach is still a limited measure of success. Some hospitals do not fully comply with the meeting requirements that are outlined in the statute (Colorado Department of Health Care Policy and Financing, 2023) Hospital
27
reporting shows these meetings are usually limited in attendance and do not provide insight to community priorities For example, one major Colorado hospital did not include a list of participants or organizations that attended the public meeting while other hospitals reported they received “very few questions and comments from public meeting participants” and “none of the questions or comments were actionable”. This reporting does not offer insight due to its inability to determine how community engagement was conducted for the CHNA and determine if the methods for community engagement were grounded in best practices through evaluation
Theme Limitation
The methods used for collecting data for the CHNA are usually left to the discretion of the hospital As a result, there is wide variation among all CHNAs
Similar outcomes for community engagement are found in national community benefit spending reporting Other state's community benefit spending reporting experience similar issues to Colorado Pennel et al use mixedmethods research to describe how authentic community engagement and participation in CHNAs is critical to create effective, equitable, and sustainable programs to improve community health. After analyzing 95 CHNAs and interviewing key informants, they found that while hospitals did have a process for community engagement, these were limited and did not include a broad array of community members or authentic participation in the CHNA process (Pennel et al, 2017) In another qualitative study, Cain et al found that most data used to create the CHNA came from hospital leaders or the board members who are part of the health care organization but do not necessarily speak from personal experience (Cain et al., 2017).
Reporting
Hospital reporting lacks the robust explanation on how the investments are related to the community’s identified needs
Policy
There is no requirement on the amount hospitals need to allocate for community benefit spending
There is ambiguity for what constitutes as “community benefit”
Health Equity
There is no focus on health equity or the improvement of health inequities
There is currently no framework or guidance provided, by the IRS or other entities, that illustrate a more comprehensive approach to community benefit spending and the importance of community engagement. Authentic community engagement seeks to shift power dynamics and act as a catalyst to create new programs and policies that meet the needs of the community The hospital’s engagement process needs to include active collaboration with communities instead of simply surveying for input on programs that are otherwise designed and led without community participation (Schiavo, 2021) Engaging diverse community partners can help improve “cultural sensitivity, reliability, and validity” in CHNAs while “emphasizing locally relevant problems and approaches to addressing health problems” (Pennel et al., 2017, p. e104). It is essential that CHNAs include community partners to improve health equity in communities. The community collaboration for CHNAs is acknowledged and supported, although the use of them is limited in CHNA development and the prioritization of fund allocations (Ainsworth et al, 2013; Cain et al, 2017; Chandrashekar et al, 2022)
28
Table 2 Issues Raised with Community Benefit Spending
Comprehensive and standardized reporting requirements of nonprofit hospital community engagement efforts would improve data collection, reduce the obfuscation of community initiative planning, and strengthen community partnerships.


Since health inequities are complex and influenced by factors outside of the healthcare system, strategies to improve them should include sectors outside of the traditional health care framework such as faith-based organizations, transportation agencies, and housing authorities Community benefit spending has the potential to create a substantial impact on community health If hospital and community leaders dedicate the time and resources, “needs assessments can become the catalyst whereby transformative change occurs within communities” (Ainsworth et al., 2013, p. 869). The impact and applicability of community benefit spending could be farreaching and greatly improve community health.
For More Information
Nonprofit hospital reporting requirements. Community benefit spending reports, CHNAs, and implementation plans
CPHAEmergingLeadersCommitteeshowstheircommitment totheircommunity,volunteeringwithEkarFarm
Youngprofessionalsforgenewconnectionsata CPHAEmergingLeadersnetworkingevent
COVID-19 and Vaccine Hesitancy: A Literature Review
 Sean Kellogg, Gustavo Tinoco, and Garvita Thareja
Sean Kellogg, Gustavo Tinoco, and Garvita Thareja
Since the beginning of the COVID-19 pandemic, the spread of health misinformation has been rapid and severe. We were interested in examining the rates of vaccine hesitancy as they were related to education, socioeconomic status, and social media use. By discovering what is mainly affecting the U.S. population’s likelihood to get vaccinated, we can aim to reduce vaccine hesitancy rates at the local level. Vaccinations can help develop herd immunity towards current and future harmful coronavirus variants The newest COVID variant XBB 15 is proving not to lead to massive hospitalization or death rates but could cause severe disease in more vulnerable populations, such as the elderly and people with immunocompromising conditions To reduce the chances of experiencing severe disease, a person can opt to receive a booster shot of the vaccine to help minimize negative health outcomes associated with COVID-19 viral infection.
Research question: “How does education level, socioeconomic status, and social media use
relate to COVID-19 vaccine hesitancy”
A Review of the Literature
In Gerretsen et al. (2021), adults ages 18+ from New York, California, Florida, & Texas were analyzed. Despite these being the four most populous states within the U.S., the sample size was not enough to generalize the findings, (N= 7678) In an article written by Kjos et al (2022), the study was conducted to better understand the relationship between health disparities and vaccine hesitancy However, the data was only collected in New York City from February to March 2021 Again, having a small sample size (N = 1584) limits the generalizability of the results In Liu & Li (2021), many limitations were present using data from the Household Pulse Survey (HPS) conducted by the U.S. Census Bureau. For example, the HPS answer choices for why there is vaccine hesitancy within individuals does not consider one’s past experiences with vaccinations, nor one’s philosophical, moral, or religious convictions. These data by the HPS also
30
CPHAmembersenjoyabeautifulColoradosunsethikeduring PublicHealthintheRockies
does not obtain information on the respondent’s ethnicity, making it impossible to examine the heterogeneity within racial groups (Liu & Li, 2021) In Melki et al (2021), a crosssectional phone survey was administered for adults living in Lebanon between March and April 2020. This study found that higher education and trust in the government resulted in less COVID-19 misinformation. Lastly, in a study by Muric et al. (2021), all data were collected from Twitter, demonstrating bias.
Gaps in the research methods of these articles demonstrate the unreliability in being able to generalize these results in the US We decided to conduct a systematic review to better address it
Methods
The literature review was conducted on 9 articles from 2020–2023 using a keyword search strategy including phrases such as “vaccine hesitancy misinformation”, “higher education”, “socioeconomics”,“social media”, and “COVID19”. These keywords were searched on multiple databases including Google Scholar, PubMed, and Auraria library’s website. We ensured all articles were from peer reviewed journals and applicable to the factors associated with vaccine hesitancy Of the selected studies for this review, sample size ranged from 506 to 1,800,000 These data were then analyzed using quantitative and qualitative analysis
What did we find?
We found that the higher education level and lower socioeconomic status study participants had, the less likely they were to have hesitancy towards the COVID-19 vaccine. Additionally, the more the study participants used social media, the more likely it was that they were exposed to misinformation and presented with more vaccine hesitancy. Individuals with a bachelor’s degree and above were likely to get vaccinated even when exposed to social media misinformation Overall, 76% of individuals with a bachelor’s
degree or above indicated that they have received at least one dose of vaccine Social media was shown to be a major contributor to spreading information about the virus and vaccination With the balance of accurate information through platforms such as Youtube, Facebook, Instagram, and Twitter, individuals were less likely to be hesitant towards the vaccine by 75%. Lastly, people with an annual household income of $25,000 or less were 32% less likely to get vaccinated when compared with those above $25,000. However, people of higher socioeconomic status also showed vaccine hesitancy, but at lower rates
What does this mean?
Education, social media messaging, and socioeconomic status can impact vaccine hesitancy Educating the communities about the COVID-19 vaccine, spreading the message through prominent media influencers, and offering incentives like gift cards, educational sessions, and media release campaigns might encourage people to get vaccinated.

31
CPHABoardMember,TheoAbbey,presentsannualawardsat PublicHealthintheRockies
The Financial and Emotional Costs of a Baby in the United States
Garvita Thareja and Andrew Salter
What is parenting? We all know how to define parenting, but how it feels to be a parent can probably best be explained by a parent! As a young parent, I have faced many challenges while supporting a family with limited resources. The resources that my professors connected me to, through academia, helped me manage the cost of my baby and allowed us to thrive through my early parenting years with our given challenges Exploring and sharing these resources will not only help other parents in the community but will also highlight the issues that parents go through emotionally as well as financially to provide the best for their babies
Two years ago, at the young age of 19 years old, my wife (18) delivered our first child, a beautiful girl, born into the world of a novel pandemic and economic uncertainty. Throughout my wife’s pregnancy, we scrambled to figure out a plan a plan that would allow me to continue my education, set us up for success in the coming decades, and allow us to survive and
support our newborn child After struggling for a few months while she was pregnant, I was able to find a position as a dental assistant, utilizing experience from my military job training. Simultaneously, I decided to advance my education and earn a degree in public health. So, I started attending university as a full-time student while working full-time and parenting full-time. To manage the cost of school and the rise in family expenses, I served in the Army Reserves and also became a teaching assistant with the help of my professor In the first semester of my senior year, my wife and I welcomed our second baby girl, a blessing and another important life to care for Yet, there have been numerous sacrifices in order to sustain a family and live independently The cost of having a baby from pregnancy to childbirth is estimated to be about $20,000 (Kaiser Family Foundation, 2022). Further, there is an additional cost of about $18,270 per year for providing a baby (Kaiser Family Foundation, 2022).Due to inflation in recent months, this cost has gone up by 9%. To manage our family’s income, I started

32
Coloradosbeautifullandscapeiseasilyenjoyedduringthe PublicHealthintheRockiesannualconference
tracking budgets tightly with spreadsheets, calculating how many times we could eat out or go out in a month/week, how much gas we could use every week, and even planning on the foods we need to get from the store In order to stay afloat, money and expenses were monitored heavily. Our monthly expenses (Table 1.) include diapers, baby wipes, baby formula, toys, water, childcare, health insurance, doctors visit for the baby, adults' food, mortgage, car insurance, car payments, internet, phone bills, electricity, car fuel, college tuition, clothes, vehicle repairs and services, medicine, and car seats or other essential items
The impact of our current economic uncertainty
Our economy is on the brink of a crash, gas prices are higher than ever, living expenses have inflated, interest rates are at record highs, the prices of essential supplies like food are extreme, and childcare is unattainable for many The Population Bureau notes that households in the United States continue to shift towards multiplefamily and non-family living situations For example, in populations under the age of 25, only 7% of married couples with children live alone, 14% of single parents with children live alone, and 33% of the population live with nonfamily members (U.S. Census Bureau, 2017).
Table 1 Monthly expenses

In early 2022, I was able to start a new position at a local hospital, working with WIC, gaining public health experience, and having access to a flexible schedule My education and mentorship from professors gave me access to resources such as increased income, health literacy, and overall knowledge of the economy, expenses, and society. This has helped me manage some of my expenses, be responsible in my spending, and exposed me to opportunities for success. However, thousands of other young families don’t have the same opportunities and resources. Failure to successfully access resources can be detrimental to physical and mental health outcomes, as well as long-term success There needs to be more help for young families
Data lacks in identifying whether multiple families are living together or not, however, the increasing amount of shared living situations suggest that multiple family living situations are more than likely to increase. This theory is easily supported by recent data suggesting that shared living among young adults has risen to levels not seen since the Great Depression (Fry et al, 2020) The average cost of rent for Colorado in 2021 was $1,437, and the average mortgage cost in Colorado was $1,927
Federal aid programs such as SNAP or food stamps have seen participation numbers increase from 20,487 households in 2020 to nearly 22,000 by the end of 2022 (USDA, 2023). Data suggests that the economic difficulties since the beginning of the pandemic have had a serious stress on families' ability to support
Item MonthlyExpense AdditionalComments Groceries $600 Sam'sClub/Walmart Diapers/Wipes $100 Sam'sClub Mortgage $1,350 2bed1bathCondo Utilities $150 Excel Vehicles $600 2vehicles Phone/Internet $120 2mobilelines Toys/Clothes $200+ Childcare $1590 1Toddler CollegeTuition $385percredithour 20Credithours Total 5,095 WithoutFederalBenefits
(Histogram depicting household makeups, US Census Bureau, 2017)
33
(Graph shows rates of young adults living with parents, Fry et al. 2020)

themselves We know that socioeconomic factors can have a wide variety of impacts on overall health. The state of today's economy is exposing many families especially the young and those in underserved socioeconomic groups to negative health outcomes. These impacts include food insecurity, homelessness, lack of healthcare access, and altered lifestyles. Young families must address these obstacles in order to ensure success, health, and positive outcomes for their children.
The effect goes far beyond just being financially strained
It's equally as important to mention the emotional effects income can have on a family. According to an article published in the Journal of Emotion, high- and low- incomes can be correlated with different emotional feelings. The study analyzed 162 countries and found that families with higher incomes experience positive feelings such as pride, confidence, and determination (Tong et al, 2021) On the other hand, families with lower income experience negative feelings of sadness, fear, and shame (Tong et al, 2021) Additionally, these feelings are
prolonged; a study of 4,000 Americans showed positive or negative feelings related to wealth were observed up to 10 years after the original study (Tong et al., 2021). We can be confident that families experiencing economic hardship are also experiencing negative emotional feelings, which contribute to their overall health and ability to self-advocate. These negative emotional feelings can cause chronic stress and depression, which can contribute to increased rates of Non-Communicable Diseases or NCD Not only are low-income families experiencing degraded health as a result of socioeconomic disparities, but their emotional health is also likely to contribute to poor physical outcomes, such as higher rates of NCD Studies by multiple organizations, including the Johns Hopkins School of Public Health, have found that lowincome individuals experience higher rates of stroke, heart attack, diabetes, and cancer (JHSPH, 2018). This research and data make addressing at-risk, low-income families even more critical, as it can have long-term health effects on members of the family.
Steps to improve outcomes
It's critical that families are given the resources and opportunities to ensure their financial success and, in turn, lower their risk of adverse health impacts Navigating what resources are available to families such as SNAP, TANF, WIC, Child Care assistance, Medicaid, and even educational assistance like FAFSA will be critical in allowing families to quickly address income-related needs. Case navigators specializing in young family success could be highly beneficial for new parents in a complicated world.
Additionally, educational attainment is the key to successful job placement, increased salary, and positive health outcomes Programs should be created to further enhance and provide opportunities for young parents to attend school and earn degrees, certifications, or licensure Creating more programs like the Care Forward Colorado program, which allotted 26 million in funding to provide free community college
34
education to students in certain healthcare positions, can provide many positive economic impacts Families who receive aid in attaining an education and career will experience improved income for families and improved income for economies. In turn, this will also improve shortages in needed careers. Addressing the barriers for families to achieve higher education will improve health outcomes for all family members, support economic development within communities, allow children to grow up in positive environments, and promote mental health.
Assisting young families with case navigators and educational assistance will empower these populations to become successful, thriving, and healthy members of our community These measures will ensure a positive and enriching childhood for their children and positive generational outcomes in health and education. The short-term increase in spending on public programs will have positive long-term economic impacts with families' increased wages. More data and research are needed to assess young families' financial and living situations. Further analysis will increase awareness and emphasize the need for public health measures to promote improved outcomes in these populations
The Rocky Mountain Public Health Training Center (RM-PHTC) provides a variety of trainings to professionals addressing public health issues and works in partnership with subject matter experts to develop a skilled workforce.

Health Equity: A Guide for Public Health Practitioners
Are you serious about applying health equity, but not sure where to start? This course will prepare you to close gaps in health status that result from systemic, avoidable, and unjust policies and practices that create barriers to opportunity for certain people.
Browse additional trainings at: http://rmphtc.org.
35
Advocacy Day at the Capitol

 Brenna Coombs
Brenna Coombs
Walking into the Colorado State Capitol building feels like entering the living center of the state. The feeling is electric and exciting.
I first experienced this while attending the Colorado Public Health Association’s 2023 annual Public Health Advocacy Day there The CPHA Policy Committee organized the event to give public health professionals, students, and community members the chance to meet local legislators and learn about policy and advocacy
CPHA President Wivine Ngongo kicked off the event calling for a moment of appreciation and introspection for public health professionals and others who worked tirelessly throughout the pandemic. Sitting in the audience with other public health students there was a sense of camaraderie and I felt proud to be a part of it.
Following Ngongo, Dean Jonathan Samet of the Colorado School of Public Health urged us to consider the public health implications of climate change, and stressed the importance of advocating for policy changes that reflect the critical health impacts of environmental pollution We also heard from Colorado Representative Jenny Willford, who spoke about the close-hitting consequences of climate change and the pain she felt when air pollution levels made it unsafe for her young son to play outside.
Her powerful anecdote was followed by a presentation from Jon Goldin-Dubois of Western Resource Advocates about the regional impacts of environmental pollution. Goldin-Dubois spoke

36
about Colorado’s history of air pollution and some of the contributing factors. In one example, he explained how emissions from personal vehicles with combustion engines may be reduced in the future by implementing policies that prioritize and incentivize the use of electric vehicles.

Many in attendance seemed excited to start making impactful changes based on the information presented by Goldin-Dubois and the other speakers. Megan Kemp, of Healthy Air & Water Colorado, led an advocacy workshop on how to jump in and get started. In addition to going over different types of engagement, Kemp encouraged people to create an advocacy “elevator pitch” for issues that are the most important to them. Keeping a go-to statement in your back pocket, she told us, can make it easier to navigate interactions with local legislators, when being clear and tothe-point is a must.
After the presentations and scheduled event wrapped up, attendees were encouraged to stick around and speak to local officials or listen to legislative proceedings. Some of my classmates and I went up to the balcony overlooking the house of representatives. We watched as different bills were debated and ruled upon. Getting that close to the legal process, and hearing from policy leaders at the event made it clear just how human our system is and how impactful those of us in public health can be.

37
How a Federal Bill Becomes Law
6 PRESIDENTIAL SIGNATURE PRESIDENTIAL VETO Brieflyelaborateonwhatyouwant todiscuss Senate HOW
SUB-COMMITTEE ASSIGNED FULL COMMITTEE MARKUP BILL SCHEDULED FOR FLOOR ACTION "ON THE FLOOR" BILL DRAFTED BILL IS ASSIGNED NUMBER SB23-XX 2 BUDGET & BILL COMMITTEES ASSIGNED 3 4 5 SUB-COMMITTEE MARKUP HEARINGS TAKE PLACE Markup: formal process to advance bill to the floor 7 8 9 BILL PASSED 10 BUDGET RESOLUTION BILL KILLED 1 FILIBUSTER Includes Budget Committee Markup: formal process to advance bill to the floor CONFERENCE COMMITTEE House of Representatives RULES COMMITTEE Responsible for expediting the passage of bills BILL SCHEDULED FOR FLOOR BILL IS ASSIGNED NUMBER HB23-XX BUDGET & BILL COMMITTEES ASSIGNED SUB-COMMITTEE ASSIGNED ACTION "ON THE FLOOR" HEARINGS TAKE PLACE SUB-COMMITTEE MARKUP Markup: formal process to advance bill to the floor BILL DRAFTED BILL PASSED FULL COMMITTEE MARKUP Includes Budget Committee Markup: formal process to advance bill to the floor 8 9 2 3 4 10 5 6 1 11 7 BUDGET RESOLUTION
A FEDERAL BILL BECOMES LAW
Yesenia Wilson 38
Interpreter Services in Healthcare: An Untapped Resource in the Broad Area of Public Health
 Valeria Pernas and Garvita Thareja
Valeria Pernas and Garvita Thareja
Equitable access to quality health care is a fundamental human right. For people living in the United States who do not speak English, a major barrier to healthcare accessibility is language; however, with reliable access to interpretation services, these patients could have better health outcomes. Understanding medical terminology and treatment plans can be difficult even for those that are English speaking Trying to understand unfamiliar medical terminology with limited-English proficiency (LEP) can add extra strain on achieving successful and satisfactory patient care Language interpretation services have an important role in health care for this population When present, they can help simplify and translate complex medical language to reduce barriers to quality healthcare in diverse communities. In order for someone with LEP to utilize interpretation services they need to have access. Having interpretation services available to LEP increases the chances of effective communication with a health provider,
The United States is a highly diverse country especially in terms of languages spoken, with 67 million people who speak a language other than English at home, as well as many whose proficiency in the English language is low (Camarota, 2014) Proficiency in understanding complex medical terminology and the ability to articulate one’s condition to a healthcare provider is important for patient success This population is also more likely to encounter uninformed consent, inconsistent treatment, and irregular follow ups due to miscommunication (Lang, 2022) Those who
 therefore improving patient outcomes
therefore improving patient outcomes
39
CPHAmembersenjoythebeautifulColoradolandscapeat PublicHealthintheRockies
are in need of interpretation services and do not or are unable to utilize them are at a disadvantage in receiving both equitable and reliable health care. Access to applied interpreting services can make or break the success of a health protocol for a patient in this demographic.
training and briefing of staff on what is available and how patients can use the services A survey conducted in 2020 of staff members at a hospital primarily serving LEP patients sought to gauge the staff member’s knowledge of the facility’s available interpretation services. Questions on the survey covered topics such as hospital staff’s personal training with interpretation services and what they knew about the resources. The results of this survey indicated that the staff at this hospital were severely under-trained in the aspect of interpretation services available for patients The findings from this study show that LEP patients sometimes have limited access to available interpretation services due to poor application or understanding of services by hospital staff (Taira et al, 2020)
There is a gap in the need for interpretation services and resources available. A study looking at 19,627 patients that stayed overnight at a hospital identified that “for 15.7% of episodes of care, a healthcare interpreter was identified as being required at hospital admission. In 3.7% [of patients needing an interpreter], a healthcare interpreter was provided” (Blay et al, 2018) This shows that of the cases that were identified as requiring an interpreter, only a very small percentage received the necessary support Understanding the factors that contribute towards this gap is important to develop solutions that could increase the healthcare experience for the language-diverse communities in the United States.

A problem faced within healthcare is the proper use of resources for linguistic interpretation provided during a health visit, creating barriers that prevent patients from effectively communicating with physicians and receiving adequate care (Al Shamsi et al, 2022) One factor that may decrease the utilization and accessibility of interpretation services is proper
A similar study showed the effects that insufficient use of interpretation services can have on an LEP patient’s experience during hospital visits. Seattle Children’s Hospital has various integrated language interpretation modalities, including over-the-phone interpretation services, touch screen devices with 24-hour access to video online interpreters, as well as one in-person Spanish translator dedicated to the emergency department during its peak hours (Hartford et al, 2019) Patient records showed that interpretation services for LEP patients were underutilized, with only 454% of them receiving the aid (Hartford et al, 2019) As for health outcomes, patients with LEP experienced a decreased likelihood of admittance as well as higher occurrences of unexpected ICU transfers within 24 hours for those who were admitted, compared to patients that were English-proficient (Hartford et al., 2019). The increase in ICU transfers within LEP patients was correlated to findings that showed they were given lower acuity and complexity ratings in terms of their condition during admittance, suggesting that the severity of their symptoms may not have been properly communicated or understood
40
Hartford et al, 2019)

In-person interpretation is commonly thought to be the traditional application of translating resources, but financial and human-resource barriers can make this method inaccessible, as seen in the Seattle Children’s Hospital study, where only one Spanish interpreter was available during peak hours. While hiring more staff dedicated to interpreting roles may not be systemically accessible, implementing easy-touse translation services and properly training staff on their use and indications can be attainable and successful
There are many online, over-the-phone, and digital tools that can be used instead of inperson interpreters, which are available and accepted by LEP patients, such as AT&T interpreter call lines (Lee, L, J, et al., 2002). One survey found that LEP patients that used this AT&T call line had higher satisfaction in their care than when using proxy interpreters such as family or untrained staff (Lee, L, J, et al., 2002). While online and digital services can be more systemically accessible, face-to-face encounters within healthcare are more common and valuable depending on the medical setting, particularly hospitals and emergency departments The diversity within the United States is not only within patients, but medical staff as well Ad hoc interpreters, which are healthcare professionals that are not trained as interpreters, can be common in some settings where trained staff is not available (Lee, L, J, et al, 2002) Allocating funding to provide multilingual healthcare staff with training in medical interpretation could utilize already present human-resource to increase support of LEP patients.
The implementation of medical interpreters throughout a patient’s health encounter ensures that not only are patients able to understand their individual health protocols, but also that the patient's particular needs will also be correctly communicated to and
understood by the provider (Karliner et al, 2010) This can improve patient outcomes, which are a crucial evaluation metric, which could positively affect the bottom line of healthcare systems and the families and communities of those affected.

CPHABoardMembersshowtheirloveandsupportofpublic healthduringPublicHealthintheRockies CPHAmembersconnectwitholdfriendsandforgenew connectionsatPublicHealthintheRockies 41
It's Monday, It's Tuesday, It's Another Ozone Alert Day!
Lyn Riebel and Garvita Thareja
We have all awakened to the alerts on our phones or have seen the signs across the highways as we drive around town, an Ozone Action Day is almost as constant here in Colorado as looking West to see the mountains. Ozone Alerts signify that our Colorado air quality is unhealthy enough that we should limit outdoor activities and be especially cautious if we are among some of the Coloradans who suffer from asthma or have sensitivity to the poor air quality and are vulnerable to developing respiratory issues
Each day we see these alerts we cannot help but think, “again?” Seeing these frequent alerts reminds us of how important healthy air quality really is The cleanliness of our air is indicated by the air quality index (AQI) (Table 1), a scale that measures the levels of air pollutants (National Oceanic and Atmospheric Administration [NOAA], n.d.). This scale measures different aspects of air quality including ground-level ozone, particulates, carbon monoxide, sulfur dioxide, and nitrogen
dioxide on a range from 0 (good) to 500 (hazardous) (United States Environmental Protection Agency [EPA], 2015). To be considered an Ozone Action Day the AQI must be 101 and above (Colorado Department of Public Health & Environment [CDPHE], 2023). In 2021 Colorado set a record for 65 Ozone Action Days (Conservation Colorado, 2022).
As someone living with asthma that is easily triggered by poor air quality, these alerts should be taken very seriously For Coloradans, being outside in nature is a part of the culture and necessary for a healthy lifestyle However, these air quality alerts are now becoming more and more frequent due to the rise in gas wells along the Front Range and the increasing number of vehicles on the roads (Robbins, 2022). This makes it more problematic to be able to get outside and enjoy our beautiful state, not only for individuals who are vulnerable to respiratory issues, but also for young children or adults who regularly spend time outside (Allergy & Asthma Network, 2023).

42
Minimal exposure to poor air quality may cause cough or shortness of breath while prolonged exposure can cause respiratory issues for all individuals (Allergy & Asthma Network, 2023).
Throughout the Front Range, the measure of ozone levels in the air have been consistently above the Environmental Protection Agency (EPA) standard of 0070 ppm (Booth, 2022), with some critical areas trending upwards to more dangerous levels exceeding 0081 ppm in recent years (Booth, 2022; Robbins, 2022) The EPA has even gone as far as potentially classifying nine Colorado counties including Boulder, Denver, Fort Collins, Greely, and Loveland as being “severe” violators of federal ozone standards (EPA, 2022; Robbins, 2022). Healthy levels of ozone are necessary to protect us from the sun’s harmful rays, however, too much ozone creates its own health hazard.
While we have seen increasing trends in the past few years, there have also been some glimpses of hope through legislation In the 2021 legislative session, legislation has been passed to increase electric bus operation as well as to make public transportation free for the month of August, a critical month for ozone alerts (Robbins, 2022). August is a key month for not only higher temperatures that affect ozone, but also because many students are returning to school and vehicle trips are increasing as over 46.6% of children travel to school in a passenger vehicle (Beck & Nguyen, 2017). Increasing the number of electric-powered buses reduces harmful emissions that are typically produced by gas-powered vehicles. Reducing the number of vehicles on the road and ensuring that those vehicles exhibit proper emissions are some steps that can help alleviate dangerous levels of ozone (EPA, 2015) These actions meet some of the objectives for the Healthy People 2020 initiative, specifically the goal to increase the use of public transportation and reduce the effects of major sources of airborne pollutants (Centers for Disease Control and Prevention, 2020).
These actions are a start, but they are not enough to turn our trends in the right direction to improve the air quality of Colorado Currently in Colorado, only motor vehicles registered in Boulder, Broomfield, Denver, Douglas, Jefferson, and parts of the following: Adams, Arapahoe, El Paso, Larimer, and Weld counties require emissions testing, meaning eighty-four percent of Colorado’s 65 counties do not require any emissions testing, leaving many vehicles on the road emitting higher pollutants (Colorado General Assembly, nd) With over 53 million vehicles registered in Colorado (United States Department of Transportation, 2023), requiring emissions testing in all counties, and removing high emission vehicles from the roads, would be a significant step towards addressing our air pollution concerns and would help to reduce the number of Ozone Action Days here in Colorado (Robbins, 2022).
There are other actions that can be taken to help reduce the amount of ozone pollution in Colorado including planting trees, promoting public or shared transportation, or increasing the number of electric vehicles on the road. Colorado is one of many states that offers incentives for purchasing electric vehicles, and organizations such as the Urban Forest Initiative focus on increasing the number of trees planted in Colorado (Downtown Denver Partnerships, 2019) If we all do our part, from turning off lights when not in use, carpooling, using public transportation, or reducing the number of vehicle trips taken, we can see clear blue skies instead of amber lights warning us of another Ozone Alert Day!
43
"If we all do our part, from turning off lights when not in use, carpooling, using public transportation, or reducing the number of vehicle trips taken, we can see clear blue skies instead of amber lights warning us of another Ozone Alert Day!"

44
Table 1. Air Quality Guide for Ozone (retrieved from EPA, 2015).
Prevention Of Vision Impairments in Colorado Latinx Populations
Melissa Scofield
In the US, the Latinx population has disproportionate rates of eye disease and conditions, especially diabetic retinopathy and glaucoma (11) Nationally, 215% of Latinx aged 20 years and older have diabetes and estimates indicate 50% of individuals with glaucoma will be Latinx in 2050 (10, 2). Culturally competent programs acknowledge variances among diverse cultures and design services to meet the needs of distinct populations. Patientcentered health literacy focuses on preventive care to reduce health disparities by providing information and services necessary for individuals to make informed health decisions
As rates of vision impairment among Latinx populations continue to rise, programs must incorporate culturally relevant preventive measures to improve vision health equity. The term Latinx is used to be inclusive to all people of Latin American descent, including those identifying as “Latino, Latina, or Hispanic” In 2021, the US Census Bureau estimated 223% of Colorado’s population identify as Hispanic or Latino Supporting Latinx community members in accessing eye care aims to decrease disparities in the utilization of vision care services and improve vision health outcomes.
Quick Facts
➜ Approximately 8 out of 10 Latinx individuals living with glaucoma are unaware of their deteriorating vision (11).
➜ In the US, 1 in 5 individuals with diabetes is unaware of it (5)
➜ The leading cause of vision loss for individuals aged 18–64 is diabetes (1)
➜ Studies show that the lack of Latinx eye care usage is associated with language barriers/feelings of discrimination, absence of health insurance coverage, poverty, and lower levels of educational attainment (2)
Relevant Information
● There are direct and indirect relationships between vision health and the United Nations Sustainable Development Goals (16)
● Research suggests increased patient satisfaction, reduced health care disparities, and increased seeking of healthcare are all improved by racially concordant health care provider-patient relationships (15).
● A recent study concluded telehealth initiatives benefited racial/ethnic minority groups by reducing disparities related to access to eye care, leading to improved vision health outcomes (13)
● Latinx are more likely to use services once they are aware services exist, while cultural norms place females at the forefront of their family’s health care needs (9)
45
Promoting health equity across all policies and programs is crucial Vision impairments and blindness reduce quality of life and increase economic burden; improving timely detection, management, and treatment is important to preserve vision health (4) Nearly 1 in 4 individuals living with blindness or vision loss is under the age of 40 (12). Adults across their lifespan differ in their perspectives of the importance of vision tests, individuals in their 20’s and 30’s often expressed they did not feel such tests were necessary because they were not experiencing any vision problem (6). As programs aim to address these issues, it’s imperative to implement continuous evaluation and modification processes Effective health promotions require a multi-pronged approach because health behaviors are complex and multi-faceted (7)
Here, the behavioral objective is to increase participation in annual eye exams A 2018 report revealed adults participating in a vision screening study were unaware that they were living with poor vision, even those with very poor vision (ie, 20/50 on the Snellen scale) were often surprised at the results (6) The CDC estimates the number of individuals who are visually impaired or blind in the U.S. will triple by 2050 (3). Diabetic retinopathy early detection and treatment can prevent or delay blindness 90% of the time, however 50% of cases are diagnosed too late for treatment to be effective (3). By providing culturally appropriate vision health knowledge, it’s possible to change awareness and attitudes surrounding the importance of eye exams, leading to a change in cultural norms
The incorporation of Latinx targeted culturally competent vision health literacy is an essential component in increasing eye exam participation Plain language is especially important for individuals with low health literacy. Latinx struggling with health literacy may have less opportunity for disease prevention, leading to delayed diagnosis (14). Reliability tools such as FleschKincaid, can be used to test literacy reading levels prior to finalizing materials,additionally it’s important to not assume that everyone has the same understanding of what may be considered common knowledge (7) Latinx underutilize health screening services, a 2020 study indicated limited health knowledge regarding prevention can be increased with brief tailored education, leading to increased health literacy and motivation to participate in health screenings (8)
Vision Health Belief Model
The above model is adapted from the Health Belief Model. The perceptions, factors, and cues in the model predict health behavior change, illustrating the likelihood of an individual taking action.
Targeted messaging refers to a standardized message created for a defined group, such as demographic targeting to increase vision health literacy. Communication should meet the needs of priority populations and persuade engagement in healthy behaviors, matching the source of information to the target

46
audience’s cultural demographics plays a significant role in establishing credibility (7). Building the bridge over gaps to vision care access involves sharing resources with those who can benefit from the information and the services offered It’s necessary to expand the delivery of culturally sensitive and relevant information to reduce the percentage of Latinx adults who forgo vision health screenings, exams, and/or treatment(s)
Resources


⧫ Prevent Blindness offers vision and eye health Spanish language fact sheets
⧫ NIH offers ¡Ojo con su visión! Toolkits; for diabetes and glaucoma, available in Spanish
⧫ Vision health resources include Health First CO Vision Services Benefits, area agencies, eyeglasses, mobile clinics, and Community Health Centers available across the state

47
CPHAEmergingLeadersCommitteeassembleanddonate blanketsfortheColoradoChildrensHospitalduringtheholidays
What’s Gone Wrong?
Cecilia Bedard
Mixed media, acrylic and paper collage on foam board, 11x16 inches.
What’s Gone Wrong? represents the destruction we humans have caused, climate change, and our apathy towards the results. The imagery in this collage reflects current climate conditions and environmental effects in Colorado and more broadly. It is meant as a warning against inaction or a glimpse into a quickly approaching future.
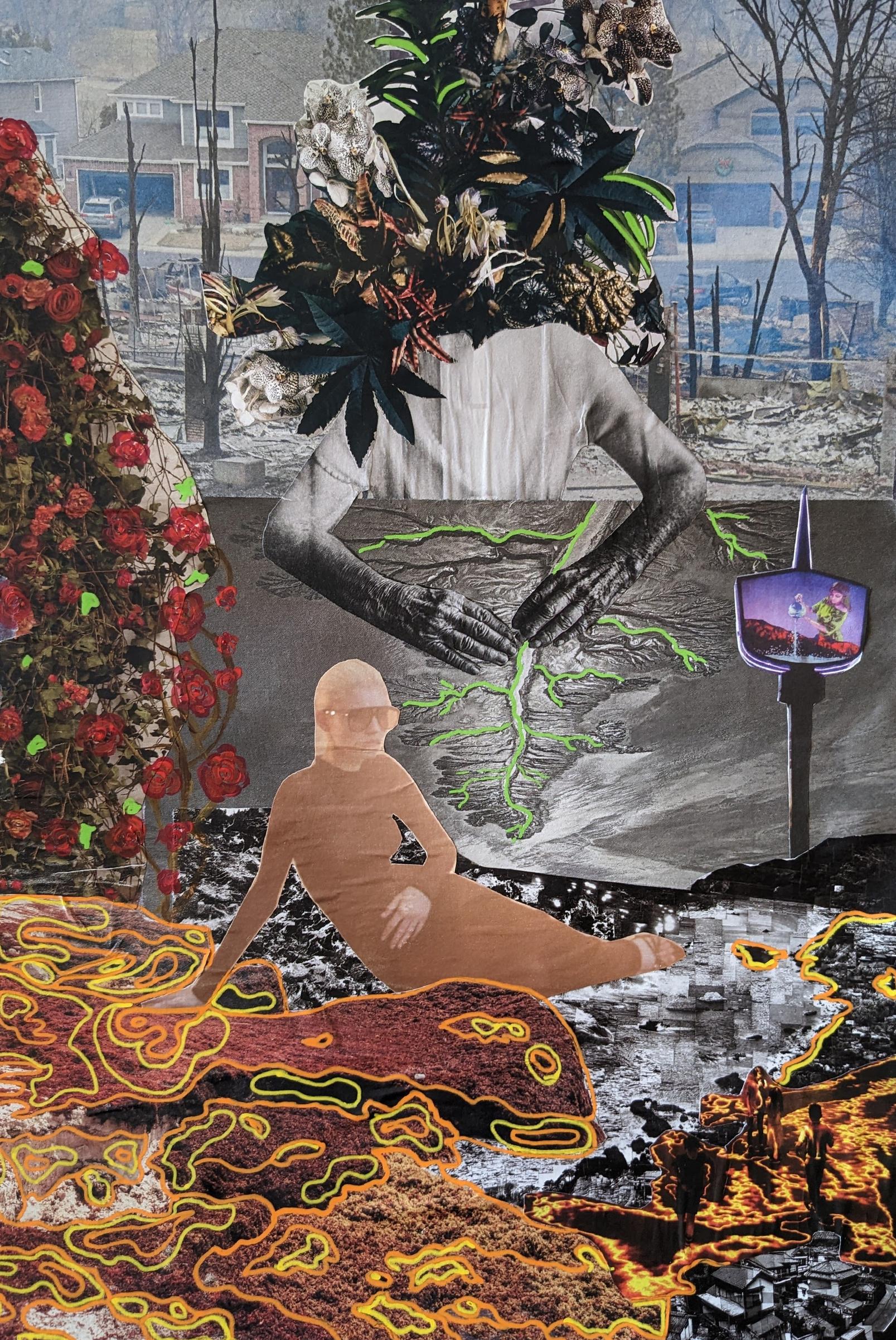
48
AI in Healthcare: An Exploration of Health Disparities in Technology Implementation
 Kailey Osborne, Garvita Thareja, Natalie Bjorklun, and Youssef Eljazouli
Kailey Osborne, Garvita Thareja, Natalie Bjorklun, and Youssef Eljazouli
Aging populations, chronic disease, government-imposed restrictions, rising costs of care, patient billing complications, and shortages in staffing continuously overburden the U.S. healthcare system. Data consistently shows that these systematic burdens disproportionately affect underrepresented and vulnerable populations such as communities with minoritized identities, lower socioeconomic status, and rural communities (7) As a result, these individuals and families suffer from higher health disparities than the general population For the purpose of this article, health disparities are defined as “preventable differences in the burden of disease, injury, violence, or opportunities to achieve optimal health that are experienced by socially disadvantaged populations'' (2). It is important to note that, “while the term disparities is often used or interpreted to reflect differences between racial or ethnic groups, disparities can exist across many other dimensions as well, such as gender, sexual orientation, age,
disability status, socioeconomic status, and geographic location” (5).
The recent COVID-19 pandemic exposed the severity of the challenges faced by the healthcare industry and left many organizations and leaders searching for new models of care and supportive technologies, such as Artificial Intelligence (AI), to provide relief However, do these technology advancements address social determinants of health sufficiently, enabling a reduction in the health disparities and inequities that currently plague the healthcare system rendering it ineffective for many Americans? Or does the integration of AI only further the divide?
The rise of AI in healthcare
Intelligent and complex computer-based models function through algorithms and existed with limited medical functionality as
CPHAsDirectors SamanthaBertomenandLisaPeters presenton engagingGenZandMillennialsduringPublicHealthattheRockies 49
as early as the mid-20th century (4) Although not a novel idea, AI has gained substantial traction over the last decade and has developed many subfields Early prototypes operated “as a simple series of “if, then rules” and have advanced over several decades to include more complex algorithms that perform similarly to the human brain” (4). Whereas the previous technology could attach a diagnosis only if specific symptoms were displayed via a fixed, rigid algorithm, it can now go beyond this effort by identifying patterns and making decisions more individualized to the patient. “Predictive models can be used for diagnosis of diseases, prediction of therapeutic response, and potentially preventative medicine in the future” (4) This refinement allows for more personalized medicine and streamlines modern healthcare delivery
Lack of health equity-focused frameworks for AI implementation
As the US healthcare system becomes increasingly technology-driven, developing a holistic understanding of how technological tools impact healthcare delivery across various socioeconomic groups is imperative. While AI can potentially improve healthcare operations and patient care by simplifying overly convoluted systems, many challenges and ethical concerns must be considered. Over the next decade, health organizations need a clear, targeted pathway for integrating AI technology to impact healthcare disparities and inequities positively Despite the importance of creating a sustainable framework that centers AI integration for health equity, there needs to be more focus on the topic
In addition to AI implementation, a significant concern is reducing the risk associated with the potential bias these AI systems can produce. As sophisticated as these systems and algorithms are, it is essential to remember that they are only as equitable as the humans that
program them Thus, any biases the creators of these systems have will then be (inadvertently) passed on to these systems The biases can be due to the reliability of the instrument managed by AI, such as racial and gender bias. A study reported that pulse oximetry measured different oxygen levels in black patients at risk for hypoxia compared to white patients, thereby creating a racial bias (6). Because there are multiple pathways of how bias can exist in these models throughout their entire lifecycle, the rate of occurrence is more frequent and challenging to eradicate One research gap identified is how much of an effect these biases may have on patients when this technology is scaled and applied more widely Given these uncertainties, it is vital to implement a robust, standardized review process with federal oversight to ensure that AI implementation is thoroughly scrutinized before being approved. The fact that AI technologies have been operational for over 70 years and this does not exist is concerning.
Diving into literature on AI, bias, and healthcare
To explore best practices around AI implementation for reducing health disparities through present healthcare systems, we conducted a qualitative review Search engines such as PUBMED, CINAHL, and Web of Science were utilized Various descriptive elements such as healthcare setting, role of AI in healthcare, regulations, and necessary considerations in implementing healthcare AI, were used to narrow our research focus. In addition, key terms such as “artificial intelligence in healthcare”, “robotics”, “bias in AI”, and “regulatory measures in AI” were applied. The search criteria was limited to studies conducted between 2020-2022 and in peer reviewed publications.
The articles were first reviewed with the title and abstract; and finally full text in-depth reviews of the selected articles were conducted
50
independently by three reviewers (KO, BN & EY) A comprehensive qualitative data review of these five studies was performed by using lineby-line coding by all three reviewers Discrepancies were resolved by mutual discussions, and five articles were selected for the final review The final stage of our complete analysis produced five articles for review.
Article one by Bajwa et al. in 2021 concluded that healthcare systems implementing AI must have in-depth training for employees accessing the technology. Next, an article by Thomasian et al. in 2021 indicated that using regulatory strategies, government oversight, and an established framework is critical in implementing AI in healthcare This will help reduce bias and inconsistency in the usage of AI for measuring parameters such as oxygen levels, blood pressure, etc Further, the article by Troncoso (2020) indicated that a shift to preventative healthcare with active patient participation could use AI technology to facilitate an easier transition from reactive medicine. Gurevich et al. (2022) revealed that AI could be used in health equity. The authors advocated that AI can have positive and negative sides, and both must be explored in depth before adopting it in the healthcare system. The final article in our review by Takshi (2021) indicated that AI is extensively utilized in the healthcare industry but is not regulated. This can cause bias and reliability issues with the patient’s data and healthcare delivery
Looking forward: ensuring equitable impacts
Many obstacles remain for healthcare organizations to use AI health technology to its fullest potential. The relationship between AI technology and health disparities is a new avenue for understanding the impact of technology on healthcare access and equity. The next decade will be critical for implementing and training AI technology in healthcare. As AI grows in complexity and use, best practices state that health organizations need a targeted framework focused on antidiscrimination and human-centered usage to stay on track for AI's proper and equitable incorporation in healthcare
AI improves healthcare delivery and patient turnaround time, reducing day-to-day stress on healthcare providers and ultimately benefiting the workforce shortage. Coming from an overwhelmed world of pandemics and great resignation, AI is a unique resource to tap into and implement. However, the lack of regulatory measures, training, reliability, and data security, in addition to putting the patients' healthcare measurements at risk, still needs to be addressed. Further research is recommended in this area so that AI is integrated appropriately into the future of the healthcare industry
51
"As sophisticated as these systems and algorithms are, it is essential to remember that they are only as equitable as the humans that program them."
EYE For Prevention is a coalition of 14 paid, young leaders from across the Denver-Metro area who have lived experience in substance misuse and/or mental health struggles We came together to create healing spaces for young people to identify their passions and strengths, while growing together as a community We collect and analyze data to better understand the issues that young people are facing and the root causes of those issues. We then mobilize to come up with creative, powerful projects and prevention strategies to make a positive impact. Authentically engaging young people with diverse, lived experience is vital to our process. We train and educate adults working with youth and decision-makers who impact youth, so we can collectively create environments where our current and future generations can thrive
The EYE For Prevention Youth Coalition invited young people to participate in the #EYEsurvive PhotoVoice Project This project specifically looked at substance misuse and mental health by highlighting that the struggle is real but so is our STRENGTH! Youth were asked to participate in this project to bring awareness to their lived experience, use storytelling as a form of social
The Struggle is Real But So is Our STRENGTH!
change and healing, and connect with other young people who are also overcoming struggles through their own strength This was a two-part PhotoVoice project Youth were asked to upload and describe two photos to represent the struggle and strength "The struggle" was defined as causes or contributions to substance misuse (injustices, barriers, social determinants of health, obstacles, and risk factors). "Strength" was defined as elements that help prevent youth substance misuse (resiliency, inspiration, tools that support good mental health and wellbeing, tactics that help overcome challenges, and overall protective factors).
The Youth Leaders developed a PhotoVoice Expo event that uplifted youth voices and resiliency, and they performed qualitative data analysis to create a full PhotoVoice report
Sedona A Morenon-Castelan is the facilitator of EYE For Prevention If you are interested in partnering with EYE For Prevention, please contact SedonaAllen@dhhaorg

here to view the full PhotoVoice report. 52
Click
I am walking through a park and wanted to capture the calmness that nature brings me. My community had never been consistent; the only consistent piece has been movement. Every time I go to the park, I can always be surrounded by trees and foliage. It’s a place for me to detach and heal.

This image was taken of my partner in Fort Collins I cannot say that this image is indicative of a community or of a place, and as a cultural drifter with no sense of place for my community, it's hard to say what part place plays in my life aside from a matter of fact of a specific time But my community is more than a place, and this picture is indicative of that My partner was up in Fort Collins for school, my best friend and brother are out in Atlanta for school, but despite that, my community has been the friends I've made along the way. For any of our lives to be better, we ought to find those worth being around and believing in, and loving them as much as we can.
This photo represents the power of art and expression When I moved to Colorado about 2 years ago, I felt lonely and out of place Art became an outlet for me to safely express how I felt free of judgment and expectations I painted these creation of Adam hands because they represent the fragile yet all-powerful nature of humans as we live and grow with the adversity we face.

This photo was taken during my first day back in the US after studying in Madrid. I was visiting my friend in NYC and we went to a protest. Australia was on fire and every summer since, the US has also been engulfed in flames. It was the very beginning of 2020 which preceded the pandemic, a cause for stress and mental health problems for me and many others This was my first protest of 2020 which became a year of plenty of opportunities to use my voice and bring attention and awareness to injustices

 Justy Robinson
Dakota Perez
Justy Robinson
Dakota Perez
53
Mikaela Kevil
Legal Precedent in American Courts
Eric Wilson
Introduction
Legal precedent is a term strewn about in today’s media, but it is more than just a vague idea. Precedent is a doctrine that has very real consequences in all aspects of life, including health equity. As is seen in Dobbs v. Jackson Women’s Health Organization, when there are no requirements on the use of precedent, it can be applied in any way This use of precedent means that rulings made to benefit health equity can be stripped away later This paper is simply here to provide more information about precedent to the reader and show how its loose definition can be a pitfall for all people

Legal Precedent, also referred to as stare decisis (Latin for to stand by things decided), in American courts has been established as part of the common law system where courts rely on previous judgments rather than deciding
the outcome based on their personal understanding of the law. This is important because it means that rulings made by the courts can actually create laws for American society without having to put forth legislation. Legal precedent also involves the trust that courts will abide by the precedent set by the courts with higher or equal authority to ensure stability within their rulings. Without that trust, the entire idea of precedent falls to pieces While precedent does allow for laws to be created on trust there are reasons for precedent not to be followed and for a new ruling to be administered However, there are no metrics a court has to follow before it can overturn previous rulings All of this seems rather confusing How can you make laws with no legislation? How do courts decide what laws should be thrown out? How can I trust decisions made by courts if they can be overturned just based on an opinion? Some questions have an answer, and some don’t. Leaving those of us who live within American society still scratching our heads.
54
CPHAmembersconnectwithlegislatorsandadvocatesduringDay attheCapitol
Legal precedent itself started back in England with the use of common law in the 13th century A document was written On the Laws and Customs of England that included the written rulings made by the courts in the time leading up to then to try and get future rulings to abide by those rulings that had already been made. The argument is that those preceding rulings had formed the precedent of what should be done. Precedent was then adopted by the United States court system following the United States’ independence A benefit of precedent is that it allows a set standard to be applied to all similar situations brought before the court system
Precedent, though does not have to be followed by a higher court on a ruling by a lower court So, if a ruling is made by a federal judicial court, the federal supreme court is not pressured to follow the same ruling, but if the federal supreme court makes a ruling, then all other federal courts are pressured to adhere to that ruling to follow precedent. This is referred to as vertical stare decisis. Horizontal stare decisis is describing the doctrine that courts should follow their own precedent. So, a 7th circuit court should adhere to the same decisions that court has made in the past This idea of horizontal stare decisis does not apply to situations form one judicial district to another So, if a 13th district court makes a ruling and there is a similar situation where a ruling is being made in a 5th district court, the 5th district court does not have to use the ruling made in the 13th district court While being used in the United States precedent has been used and broken many times in all types of law applications.
Precedent itself is not limited to a specific area of law. It is used in all areas. The fact that it is in every aspect of the shows its great importance, but there is no legal requirement to follow precedent or how to use it Why? Something that is so inherent in our legal system should have some ground rules There should be
bounds on when to follow or break away from precedent to prevent it being used to fulfill an agenda In our current system any judge can break away from precedent by stating that the previous ruling was wrong, didn’t fit in with our society any more, or that the justification of the previous ruling is not strong enough. How can you measure these requirements? How far off does the justification need to be? Our legal system needs to address and create a metric by which reasons for deviating from precedent can be measured to help prevent against misusing the doctrine of precedent
The most well-known and recent case where precedent was rejected was when Roe v Wade and Planned Parenthood of Southeastern Pa v Casey were overturned The opinion of the majority was that “(a) The critical question is whether the Constitution, properly understood, confers a right to obtain an abortion. Casey’s controlling opinion skipped over that question and reaffirmed Roe solely on the basis of stare decisis. A proper application of stare decisis, however, requires an assessment of the strength of the grounds on which Roe was based. The Court therefore turns to the question that the Casey plurality did not consider (Dobbs v Jackson Women’s Health Organization) (b) The doctrine of stare decisis does not counsel continued acceptance of Roe and Casey Stare decisis plays an important role and protects the interests of those who have taken action in reliance on a past decision It “reduces incentives for challenging settled precedents, saving parties and courts the expense of endless relitigation.” Kimble v. Marvel Entertainment, LLC, 576 U. S. 446, 455. It “contributes to the actual and perceived integrity of the judicial process.” Payne v. Tennessee, 501 U. S. 808, 827. And it restrains judicial hubris by respecting the judgment of those who grappled with important questions in the past. But stare decisis is not an inexorable command, Pearson v Callahan, 555 U S 223, 233, and “is at its weakest when [the Court] interpret[s] the Constitution,”
55
Agostini v Felton, 521 U S 203, 235 (c) Casey identified another concern, namely, the danger that the public will perceive a decision overruling a controversial “watershed” decision, such as Roe, as influenced by political considerations or public opinion. 505 U. S., at 866–867. But the Court cannot allow its decisions to be affected by such extraneous concerns. A precedent of this Court is subject to the usual principles of stare decisis under which adherence to precedent is the norm but not an inexorable command If the rule were otherwise, erroneous decisions like Plessy would still be the law The Court’s job is to interpret the law, apply longstanding principles of stare decisis, and decide this case accordingly Pp 66–69 (d) Under the Court’s precedents, rational-basis review is the appropriate standard to apply when state abortion regulations undergo constitutional challenge. Given that procuring an abortion is not a fundamental constitutional right, it follows that the States may regulate abortion for legitimate reasons, and when such regulations are challenged under the Constitution, courts cannot “substitute their social and economic beliefs for the judgment of legislative bodies.” Ferguson, 372 U. S., at 729–730” (Dobbs v Jackson Women’s Health Organization, 2022)
According to this majority opinion there was nothing Constitutionally wrong made by the court in its original opinion of Roe v Wade or in Planned Parenthood of Western Pa v Casey
The only argument made was that the opinion of the previous Supreme Court majority differs from the majority opinion of the current Supreme Court. Then it tries to defend its decision to defy precedent by quoting how stare decisis was used in different cases. Using precedent to defy precedent is an extremely flawed argument.
Precedent has been used to defy precedent, what happens when precedent is used to defy precedent which was used to defy precedent? This is setting the stage to use stare decisis however the interpreter wishes to use it and dilutes its very power in the legal system This demonstrates the need to have clearly defined rules for using precedent and when it can be broken Otherwise, courts will continue to use precedent as an interpretive argument to do whatever they want.
This opinion in Dobbs v. Jackson Women’s Health Organization is only a very high profile case in the United States. Most cases where stare decisis is used in the lower courts and does not receive the media attention that is given to supreme court cases, but use of stare decisis in the lower courts is no less important All decisions made at all levels of the courts both federal and state determine what precedent will be used at that level and those below Those decisions are shaping the very law of our society without having to go through the legislative process of creating new laws. That very idea is circumventing the legislative process that was intended to be the law creating system of the United States. Should the Judicial system have that power to create new law with no oversight from the Legislative powers?
56
"How can we expect that courts will adhere to precedent if the highest court in the land does not adhere to precedent in its own rulings?"
I have found through my research that there are quite a few flaws presented by our current use of the doctrine on precedent We need to change our view of what law is Law is not rigid but fluid, and changes over time Sometimes rapidly without us even knowing through our current system. We also need to have measurements for when to overturn previous rulings so precedent cannot be overturned because of political viewpoints or for any reason that is not firmly rooted within the bounds of law. Once a judgment has been made that establishes a new precedent on the law, I propose that judgement be sent to the legislative brand of government to decide on whether to pass that judgement into law by a majority vote of a certain percentage That way judges can make a decision that cannot be overturned by another court because they disagree with the original decision That way the precedent stands with application of law, and not solely with the judicial interpretation.

 CPHAEmergingLeadersCommitteeassembleanddonate blanketsfortheColoradoChildrensHospitalduringtheholidays
CPHAEmergingLeadersCommitteeassembleanddonate blanketsfortheColoradoChildrensHospitalduringtheholidays
57
RISE Contributor's
Natalie Bjorklun
Natalie Bjorklun lives and works in Denver, Colorado. After earning her undergraduate degree in elementary education from the University of Kansas and teaching, she took her passion for educating to a different field She will graduate in December 2023 with a master's in health administration from MSU Denver, driven to provide accessible, equitable health education to underserved communities
Jessica Chuong
Jessica Chuong was born and raised in beautiful Colorado. She is a current MHA student at Metropolitian State University of Denver and is hoping to continue to pursue her passion in healthcare administration once she graduates. On her free time, she enjoys spending time with family and friends along with her dog, Buttons


Brenna Coombs
Brenna is a graduate student pursuing an MPH at the Colorado School of Public Health. She is also a member of the Colorado Public Health Association’s Emerging Leaders Committee, and currently serves as one of their Public Health Policy Delegates. Being particularly interested in how public health policy intersects with the US legislative and judicial systems, her goal is to help develop and advocate for policies that promote and prioritize health equity at the systemic level.
Eric Cox
Eric Cox is a Health Administration master's student at MSU Denver He completed his undergraduate degree in Health Care Management at MSU Denver in 2021. He am currently in my sixth and final season playing for the MSU Denver baseball team.


Moulay Eljazouli
Youssef Eljazouli is a graduate student perusing his MHA at Metropolitan State University of Denver. In his present role, he serves as an analyst on the operations and strategy team at Quartet health, a tech-enabled mental health startup based in New York. Youssef aspires to leverage technology to improve healthcare as a whole but especially inequities within our healthcare system.
Joanna Garcia
Joanna Garcia is a new addition to the RISE magazine team, joining the CPHA Emerging Leader Committee this past fall She has been eager to jump into the Colorado Public Health community as a first year Master in Public Health student at the Colorado School of Public Health concentrating in Applied Biostatistics. In addition to RISE magazine, she heads the Emerging Leader Spotlight in the monthly ELC newsletter.


58
Calina Hilyard
Calina Hilyard's background is in healthcare sales and exercise science They have a passion for behavioral health and would like work in community and population health after receiving their MHA degree During their off time, they enjoy all the outdoor activities Colorado has to offer!

Sean Kellogg
Sean Kellogg is currently a graduate student studying healthcare administration at Metropolitan State University at Denver and also a Cardiac Sonographer at National Jewish Health. He hopes to stay involved within the clinical side of healthcare after his degree to help both staff and patients have a better experience participating in healthcare services

Devin Miller
Devin Miller is a third year Doctor of Public Health student at the Colorado School of Public Health. Her background is in healthcare management, policy, and population health. She is passionate about enhancing cross-sector collaboration to improve access to care.




Kailey Osborne, BSPH
Kailey Osborne is a Graduate student in the Master of Health Administration program at Metropolitan State University of Denver and currently serves as a Program Manager for the University of Colorado Anschutz Medical Campus. While committing to over a decade in direct patient care as an EMT and later as a Certified Nursing Assistant/Patient Care Technician, she earned a Bachelor of Science in Public Health at the University of Arizona, specializing in community and family health. Kailey is fiercely passionate about advocating for vulnerable populations and improving healthcare systems.
Valeria Pernas
Valeria Pernas is a senior at MSU Denver pursuing a major in Integrative Health with a minor in Pre-Health Care Originally from San Jose, Costa Rica, she is inspired by her country’s recognition by the United Nations as one of the top 20 public health systems in the world. Increasing accessibility and equity within healthcare are the major values that drive her desire to work in healthcare.
Lyn Riebel
Lyn Riebel is a student at Metropolitan State College of Denver studying Public Health. Lyn is also a National Board-Certified Health and Wellness Coach and has been working as a Health and Wellness Coach for over 6 years In the Fall, Lyn is planning on pursuing grad school where she will continue her passion in the Public Health field
RISE Contributor's
59
RISE Contributor's
Thalia Rodriguez
Thalia Rodriguez is an MSU Denver student in the Master of Health Administration program She works for Jefferson Center as an Administrative Project Coordinator and is also a Mental Health First Aid instructor. Her passion for reducing healthcare disparities drives her approach to any project.


Andrew Salter
Andrew Salter is a public health senior graduating in May of 2023 with his bachelors and pursuing his MPH in the coming fall online. Andrew hopes to serve his community after graduation in an impactful and meaningful capacity. Currently, Andrew works at Denver WIC, is a TA at MSU Denver, and serves in the U.S. Army reserves."
Mckenzie Schrank
Originally from Virginia, McKenzie Schrank moved to Colorado in early 2020 to pursue her passions for improving public health through communication and snowboarding. She is a recent Colorado School of Public Health Alumni where she specialized in Community and Behavioral Health as well as Health Communications and currently works as the Communications Specialist for the Colorado Collective Leadership Initiative. McKenzie is a growing writer and editor with two previous publications: one in the journal of the Beta Beta Beta Biological Honor Society (BIOS) and one in the American Journal of Biological Anthropology (AJBA). Her previous work has centered around sharing her experiences in an interesting and relatable way to encourage others to understand the importance of preventative behaviors and medicine
Melissa Scofield, MPH, LDO, CPH, CHES®


Melissa Scofield completed her Master of Public Health (2022) at the University of South Florida. Utilizing her knowledge and experience as a licensed optician, she works to bridge vision health and public health by translating population health data into business models to close care gaps and promote equity. She is open to collaborate on eye care quality improvement efforts, heath promotion development, and public health initiatives.

Amanda Skidmore
Amanda Skidmore is a Board-Certified Ergonomist specializing in the needs of healthcare workers She is a graduate of the Colorado School of Public Health’s Total Worker Health Certificate program and is currently an MPH candidate in Leadership and Public Heath Practices. In her free time, she enjoys cooking, hiking, and engaging in meaningful conversations with her German Shepherd.
60
RISE Contributor's
Garvita Thareja
Dr. Garvita Thareja is an assistant professor at the Department of Health Professions at Metropolitan State University of Denver. Her specialties include public health broadly as well as community health education as she is CHES certified, data analysis, data mining and community health education in the broad area of public health. In her present role, she serves as reviewer for various state, national and international level conference submissions, leads university and community wide professional committees as well as teach undergraduate and graduate students in healthcare management and public health programs Bringing a diverse background, she believes in inter-professional activities and have experience working on cross professional projects
Gustavo Tinoco
Gustavo Tinoco is a Health Center Operations Coordinator at Colorado Community Health Network. Founded in 1982, the Colorado Community Health Network (CCHN) represents the 20 Colorado Community Health Centers, the largest primary network in the state Currently serving more than one in seven Coloradans, CCHN is committed to: Educating policy makers and stakeholders about the unique needs of Community Health Centers (CHCs) and their patients, providing resources to ensure that CHCs are strong organizations, and supporting CHCs in maintaining the highest quality care CCHN’s mission is to increase access to high quality health care for people in need in Colorado The Health Center Operations Division (HCOPS) he works in focuses on growing, strengthening, and sustaining CHCs in Colorado. The HCOPS Division provides technical assistance, training, data analysis, and other resources to CHCs and other partners in the areas of: Health Center Operational and Financial Systems, Health Center Workforce Development Activities, and Health Center Community Development Activities. The Health Center Operations Division maintains effective relationships with partners to promote and support CHCs in Colorado.
Eric Wilson (he/him/his/él)
Bachelor of Science in Mechanical Engineering candidate at Colorado Mesa University/University of Colorado Boulder Engineering (CMU/CU Boulder). Stay at home father. Aspiring to impact legislation in Colorado.


Yesenia Wilson (she/ella)

MPA/MPH candidate at the University of Colorado School of Public Affairs and School of Public Health Colorado Public Health Association Emerging Leaders Committee 2022-2023 Public Health Policy Delegate Disproportionately Affected Populations Liaison for People Experiencing Homelessness and Congregate Settings at the Colorado Department of Public Health and Environment. A Colorado native, Yesenia aspires to influence social, health, and systemic changes through policy and advocacy.

61
RISE Contributor's
Tracey Wood
Tracey Wood is a graduate student at the Department of Health Professions at the Metropolitan State University of Denver. Colorado Native and a mother of two, aspiring for a position in Health Care Administration. Motivated leader with areas of expertise including communication, relationship building, and enhancing efficiency.
Maryssa Yarbrough

Maryssa Yarbrough began her career working with older adults and received her bachelor's degree in social work from Metropolitan State University of Denver, she remains a student as MSU Denver and is currently pursuing her graduate's degree in Health Administration with a prospective graduation in December 2023. Maryssa's interests include advocating for quality health care for underserved populations, representing diversity and inclusion in professional settings, and serving the older adult population. Currently, Maryssa is employed as a Resident Services Coordinator for her local Housing Authority and works closely with lowincome individuals and families to connect them to various resources in the community and ensure they meet their goals related to health, wellness, and housing stability.
THANK YOU!
On behalf of our Leadership Team, contributors, artists, editors, and partners, we wanted to take this moment to say THANK YOU! We appreciate your dedication in supporting the Colorado Public Health Association's emerging leaders, young professionals, and students
We are inspired by your desire to read articles and support artwork created by the next generation of leaders. Your contributions, comments, and readership have kept RISE energized and inspired for another year. Without you, none of this would be possible.
Thank YOU for continuing to help us RISE!
Lisa Peters Editor-in-Chief and Co-Founder of RISE

62
Assessment of Telemedicine and Access to Care in Rural Areas
Breton, M, Sullivan, EE, Deville-Stoetzel, N et al Telehealth challenges during COVID-19 as reported by primary healthcare physicians in Quebec and Massachusetts BMC Fam Pract 22, 192 (2021) https://doiorg/101186/s12875-021-01543-4
Butzner, M, & Cuffee, Y (2021) Telehealth interventions and outcomes across rural communities in the United States: Narrative review. Journal of Medical Internet Research, 23(8). https://doi.org/10.2196/29575
Cacari Stone, L, Roary, M C, Diana, A, & Grady, P A (2021) State Health Disparities Research in rural America: Gaps and future directions in an era of COVID-19 The Journal of Rural Health, 37(3), 460–466 https://doiorg/101111/jrh12562
Centers for Disease Control and Prevention (2017, August 2) About Rural Health Centers for Disease Control and Prevention https://wwwcdcgov/ruralhealth/abouthtml
Christensen, Keith. Telehealth use among rural individuals with disabilities. Center for Persons with Disabilities. (2020). https://rockymountainadaorg/sites/default/files/2020-02/Rural%20Telehealth%20Rapid%20Response%20Reportpdf
Cole, B, Pickard, K, & Stredler-Brown, A (2019) Report on the use of telehealth in early intervention in Colorado: Strengths and challenges with Telehealth as a service delivery method International Journal of Telerehabilitation, 11(1), 33–40 https://doiorg/105195/ijt20196273
Fact sheet: Telehealth: AHA American Hospital Association (nd)from https://wwwahaorg/factsheet/telehealth#: :text=Telehealth%20helps%20increase%20health%2 0care,and%20delivers%20savings%20to%20payers
Hollman, A K, Obermier, T R, & Burger, P R (2021) Rural measures: A quantitative study of the rural digital divide Journal of Information Policy, 11, 176–201. https://doi.org/10.5325/jinfopoli.11.2021.0176
Kolluri, S, Stead, T S, Mangal, R K, Coffee, R L, Littell, J, & Ganti, L (2022, August 20) Telehealth in response to the rural health disparity Health psychology research Retrieved February 4, 2023, from https://wwwncbinlmnihgov/pmc/articles/PMC9392842/
Lane, Megan (December 2017) Making Connections: Telehealth improves access for rural Patients School of Medicine Telehealth for Rural Patients. https://medschool.cuanschutz.edu/deansoffice/cu-med-today/featuresarchives/telehealth-forrural-patients
Sullivan, C, Cazin, M, Higa, C, Zalud, I, & Lee, M-J (2022) Maternal telehealth: Innovations and Hawaiʻi Perspectives Journal of Perinatal Medicine, 51(1), 69–82 https://doiorg/101515/jpm2022-0394
Cooking for Health and Pleasure: Beans
Recipe and image source: https://smittenkitchen.com/2017/09/pizza-beans-cookbook-preview/
COVID-19 Pandemic and Depression Among Children and Adolescents
Adegboye, D, Williams, F, Collishaw, S, Shelton, K, Langley, K, Hobson, C, Burley, D, & van Goozen, S (2021) Understanding why the COVID‐19 pandemic‐related lockdown increases mental health difficulties in vulnerable young children. JCPP Advances, 1(1), e12005-n/a https://doiorg/101111/jcv212005
Centers for Disease Control and Prevention (nd) Data and statistics on children's Mental Health Centers for Disease Control and Prevention Retrieved January 25, 2023, from https://wwwcdcgov/childrensmentalhealth/datahtml
US Department of Health and Human Services (2022) Science update: Youth suicides increased in first year of the pandemic, NIH-funded study suggests. Eunice Kennedy
Shriver National Institute of Child Health and Human Development Retrieved January 19, 2023, from https://wwwnichdnihgov/newsroom/news/042722-COVID-adolescentsuicide
Listernick, Z I, & Badawy, S M (2021) Mental health implications of the COVID-19 pandemic among children and adolescents: What do we know so far? Pediatric Health, Medicine and Therapeutics, 12, 543-549 https://doiorg/102147/PHMTS315887
Luijten, M A J, van Muilekom, M M, Teela, L, Polderman, T J C, Terwee, C B, Zijlmans, J, Klaufus, L, Popma, A, Oostrom, K J, van Oers, H A, & Haverman, L (2021) The impact of lockdown during the COVID-19 pandemic on mental and social health of children and adolescents Quality of life research : an international journal of quality of life aspects of treatment, care and rehabilitation, 30(10), 2795–2804
https://doiorgaurarialibraryidmoclcorg/101007/s11136-021-02861-x
Nearchou, F., Flinn, C., Niland, R., Subramaniam, S. S., & Hennessy, E. (2020). Exploring the Impact of COVID-19 on Mental Health Outcomes in Children and Adolescents: A Systematic Review International journal of environmental research and public health, 17(22), 8479 https://doiorg/103390/ijerph17228479
Samji, H, Wu, J, Ladak, A, Vossen, C, Stewart, E, Dove, N, Long, D, & Snell, G (2022) Review: Mental health impacts of the COVID‐19 pandemic on children and youth – a systematic review Child and Adolescent Mental Health, 27(2), 173-189
https://doiorg/101111/camh12501
Śniadach, J, Szymkowiak, S, Osip, P, & Waszkiewicz, N (2021) Increased Depression and Anxiety Disorders during the COVID19 Pandemic in Children and Adolescents: A Literature Review Life (Basel, Switzerland), 11(11), 1188
https://doiorg/103390/life11111188
Zablotsky, B, Black, L I, Terlizzi, E P, Vahratian, A, & Blumberg, S J (2022) Anxiety and depression symptoms among children before and during the COVID-19 pandemic Annals of Epidemiology, 75, 53-56
https://doiorg/101016/jannepidem202209003
References 63
Advancing Community Health with Hospital Community Benefit Spending
Ainsworth, D., Diaz, H. & Schmidtlein M. (2013). Getting more for your money: Designing community needs assessments to build collaboration and capacity in hospital system community benefit work Health Promotion and Practice, 14(6):868-875 doi:101177/1524839912470445
Cain, C, Orionzi, D, O’Brien, M, & Trahan, L (2017) The power of community voices for enhancing community health needs assessments Health Promotion and Practice, 18(3):437-443 doi:101177/1524839916634404
Carroll-Scott A, Henson RM, Kolker J, Purtle J (2017) The Role Of Nonprofit Hospitals In Identifying And Addressing Health Inequities In Cities Health Affairs (Millwood), 36(6):1102-1109 doi:101377/hlthaff20170033
Chandrashekar, P, Gee, R, & Bhatt, J (2022) Rethinking community benefit programs A new vision for hospital investment in community health Journal of General Internal Medicine, 37(5):1278-1280 doi:101007/s11606-021-07324-0
Colorado Department of Health Care Policy and Financing. Hospital Community Benefit Key Findings. Hosp Community Benefit Rep 2022;1(1):39
Colorado Department of Health Care Policy and Financing (2021) Hospital Cost, Price & Profit Review
https://hcpfcoloradogov/sites/hcpf/files/Hospital%20Cost%20Price%20and%20Profit%2 0Review%20Full%20Report withAppendices-0810acpdf
Colorado Department of Health Care Policy and Financing (2023) Annual Report: Hospital Community Benefit
Accountability https://hcpfcoloradogov/sites/hcpf/files/2023%20Hospital%20Community%20Benefit%2 0Reportpdf
Internal Revenue Service (2010) Requirements for 501(c)(3) Hospitals Under the Affordable Care Act – Section 501(r) https://wwwirsgov/charities-non-profits/charitable-organizations/requirements-for-501c3-hospitals-under-the-affordablecare-act-section-501r
Lutchuman, S, Berry, L, Hole, M, & Bai, G (2022) Revise the IRS’s nonprofit hospital community benefit reporting standard Health Affairs Forefront doi: 101377/forefront20220413829370
Pennel, C, McLeroy, K, Burdine, J, Matarrita-Cascante, D, & Wang, J (2017) A mixed- methods approach to understanding community participation in community health needs assessments Journal of Public Health Management and Practice, 23(2):112-121. doi:10.1097/PHH.0000000000000362
Pennel, C, McLeroy, K, Burdine, D, & Matarrita-Cacante, D (2015) Nonprofit hospitals' approach to community health needs assessment American Journal of Public Health, 105(3): e103-113
Prybil, L, Scutchfield, F, & Dixon, R (2016) The evolution of public health–hospital collaboration in the United States Public Health Reports,131(4):522-525
Rosenbaum S Hospital community benefit spending: Leaning in on the social determinants of health (2016) Milbank Quarterly, 94(2):251-254 doi:101111/1468-000912191
Schiavo, R (2021) What is true community engagement and why it matters (now more than ever) Journal of Community Healthcare, 14(2):91-92 doi:101080/1753806820211935569
Singh, S, Young, G, Daniel Lee, S, Song, P, & Alexander, J (2015) Analysis of hospital community benefit expenditures’ alignment with community health needs: evidence from a national investigation of tax-exempt hospitals American Journal of Public Health, 105(5):914-921 doi:102105/AJPH2014302436
Zelinger, M (2023, January) State, hospital association paint different pictures of Colorado nonprofit hospitals' finances
9News
COVID-19 and Vaccine Hesitancy: A Literature Review
Gerretsen, P, Kim, J, Caravaggio, F, Quilty, L, Sanches, M, Wells, S, & Graff-Guerrero, A (2021) Individual determinants of COVID-19 vaccine hesitancy PLoS One, 16(11), e0258462
King, W C, Rubinstein, M, Reinhart, A, & Mejia, R J (2021) Time trends and factors related to COVID-19 vaccine hesitancy from January-May 2021 among US adults: Findings from a large-scale national survey MedRxiv
Kjos, N, Hendrix, C L, & Thomason, M E (2022) Perceived medical care quality during COVID-19 illness links socioeconomic disadvantage to vaccine hesitancy Preventive medicine reports, 30, 102020
Liu, R, & Li, G M (2021) Hesitancy in the time of coronavirus: Temporal, spatial, and sociodemographic variations in COVID-19 vaccine hesitancy SSM-population health, 15, 100896
Melki, J, Tamim, H, Hadid, D, Makki, M, El Amine, J, & Hitti, E (2021) Mitigating infodemics: The relationship between news exposure and trust and belief in COVID-19 fake news and social media spreading. Plos one, 16(6), e0252830.
Mohammed, F, Al-Kumaim, N H, Alzahrani, A I, & Fazea, Y (2023) The Impact of Social Media Shared Health Content on Protective Behavior against COVID-19 International Journal of Environmental Research and Public Health, 20(3), 1775
Muric, G, Wu, Y, & Ferrara, E (2021) COVID-19 vaccine hesitancy on social media: building a public Twitter data set of antivaccine content, vaccine misinformation, and conspiracies JMIR public health and surveillance, 7(11), e30642
Nguyen, L H, Joshi, A D, Drew, D A, Merino, J, Ma, W, Lo, C H, & COPE Consortium (2022) Self-reported COVID-19 vaccine hesitancy and uptake among participants from different racial and ethnic groups in the United States and United Kingdom Nature communications, 13(1), 636
Wilson, S. L., & Wiysonge, C. (2020). Social media and vaccine hesitancy. BMJ global health, 5(10), e004206.
64
References
The Financial and Emotional Costs of a Baby in the United States
Benchmark employer survey finds average family premiums now top $20,000 Kaiser Family Foundation (2019, September 24) Retrieved March 24, 2023, from https://wwwkfforg/health-costs/press-release/benchmark-employer-survey-findsaverage-family-premiums-now-top-20000/
Care forward Colorado - Colorado Community College System Colorado Community College System - Education that meets students where they are (2022, November 11) Retrieved January 20, 2023, from https://cccsedu/new-students/exploreprograms/care-forward-colorado/
Fry, R., Passel, J. S., & Cohn, D. V. (2020, September 9). A majority of young adults in the U.S. live with their parents for the first time since the Great Depression Pew Research Center Retrieved January 20, 2023, from https://wwwpewresearchorg/facttank/2020/09/04/a-majority-of-young-adults-in-the-u-s-live-with-their-parents-for-the-first-time-since-the-great-depression/ Johns Hopkins Bloomberg School of Public Health (2018, April 5) Poverty increases risk of non-communicable diseases in lower income countries Johns Hopkins Bloomberg School of Public Health Retrieved March 16, 2023, from https://publichealth.jhu.edu/2018/poverty-increases-risk-of-non-communicable-diseases-in-lower-incomecountries#:~:text=Their%20findings%20show%20that%20since,(heart%20attack)%20and%20cancer
SNAP data tables Food and Nutrition Service US Department of Agriculture (2023, January 1) Retrieved January 20, 2023, from https://wwwfnsusdagov/pd/supplemental-nutrition-assistance-program-snap
Tong, E, Reddish, P, Oh, V, Ng, W, Sasaki, E, Diener, E, & Diener, E (2020, September 13) Higher income predicts feelings such as pride and confidence American Psychological Association Retrieved March 16, 2023, from https://wwwapaorg/news/press/releases/2021/03/higher-income-pride-confidence
US Census Bureau quickfacts: Colorado; United States (2022) Retrieved January 20, 2023, from https://wwwcensusgov/quickfacts/CO,US
VanOrman, A., & Jacobsen, L. A. (202AD, February 12). U.S. household composition shifts as the population grows older; more young adults live with parents PRB Retrieved January 20, 2023, from https://wwwprborg/resources/u-s-householdcomposition-shifts-as-the-population-grows-older-more-young-adults-live-withparents/#: :text=While%20only%20one%2Dfifth%20of,parent%20families%20(19%20percent)
Interpreter Services in Healthcare: An Untapped Resource in the Broad Area of Public Health
Bureau of Labor Statistics (2022, September 8th) Department of Labor Interpreters and Translators Retrieved February 1st, 2023, from https://wwwblsgov/ooh/media-and-communication/interpreters-and-translatorshtm
Blay, N, Ioannou, S, Seremetkoska, M et al Healthcare interpreter utilization: analysis of health administrative data BMC Health Serv Res 18, 348 (2018). https://doi.org/10.1186/s12913-018-3135-5
Camarota, S A, & Zeigle, K (2014, October 3) One in five US residents speaks foreign language at home, record 618 million Center for Immigration Studies Retrieved July 2022, from https://cisorg/Report/One-Five-US-Residents-Speaks-ForeignLanguage-Home-Record-618-million
Espinoza, J, & Derrington, S (2021) How should clinicians respond to language barriers that exacerbate health inequity?
Journal of Ethics | American Medical Association Retrieved July 17, 2022, from https://journalofethicsamaassnorg/article/how-should-clinicians-respond-language-barriers-exacerbate-health-inequity/2021-02
Garza, M, Quigg, S M, De Lorenzo, S B, Schroeder, D R, & Takahashi, P Y (2020) Vaccination rates among patients age 65 years and older who require interpreter services in the state of Minnesota Journal of Community Health, 46(4), 703–710 https://doiorg/101007/s10900-020-00927-4
Hartford, E A, Anderson, A P, Klein, E J, Caglar, D, Carlin, K, & Lion, K C (2019) The use and impact of professional interpretation in a pediatric emergency department Academic pediatrics Retrieved July 10, 2022, from https://wwwncbinlmnihgov/pmc/articles/PMC6855248/
Karliner, L S, Kim, S E, Meltzer, D O, & Auerbach, A D (2010) Influence of language barriers on outcomes of hospital care for general medicine inpatients. Journal of hospital medicine, 5(5), 276–282. https://doi.org/10.1002/jhm.658
Lee, L J, Batal, H A, Maselli, J H, & Kutner, J S (2002) Effect of Spanish interpretation method on patient satisfaction in an urban walk-in clinic Journal of General Internal Medicine, 17(8), 641–645 https://doiorg/101046/j1525-1497200210742x
Lang, B (2022, March 10) Using interpreters in Healthcare - Pros & Cons The Language Doctors Retrieved June 29, 2022, from https://thelanguagedoctorsorg/using-interpreters-in-healthcare/ United States Census Bureau (2021, December 16th)About Language Use in the US Population Retrieved February 1st, 2023 from https://wwwcensusgov/topics/population/language-use/abouthtml
65
References
References
It's Monday, It's Tuesday, It's Another Ozone Alert Day!
Allergy & Asthma Network (2023) What do ‘ozone alerts’ really mean? News https://allergyasthmanetworkorg/news/theozone-alert-days-summer/
Beck, L F, Nguyen, D D (2017) School transportation mode, by distance between home and school, United States, ConsumerStyles 2012 Journal of Safety Research, 62, 245–251 https://doiorg/101016/jjsr201704001
Booth, M (2022, August 5) Regional board to approve ozone action plan, but a Colorado coalition wants much more done The Colorado Sun https://coloradosuncom/2022/08/05/ozone-plan-colorado-front-range-air-pollution-failure/ Centers for Disease Control and Prevention. (2020, December 14). Healthy People 2020. https://wwwcdcgov/nchs/healthy people/hp2020htm
Colorado Department of Public Health & Environment (2023, February 10) Colorado air quality https://wwwcoloradogov/airquality/advisoryaspx
Colorado General Assembly (nd) Emissions https://legcoloradogov/content/emissions
Conservation Colorado (2022, March 25) Five reasons Colorado air quality is so bad https://conservationcoorg/2022/03/25/five-reasons-colorados-air-quality-is-so-bad
Cooperative Institute for Research in Environmental Sciences at the University of Colorado Boulder (2014, June 15) Science of smog https://cirescoloradoedu/news/science-smog
Downtown Denver Partnerships. (2019). Urban Forest Initiative. Initiatives & Planning. https://wwwdowntowndenvercom/initiatives-and-planning/downtown-denver-urban forest-initiative/ Friis, RH (2019) Essentials of environmental health Jones and Bartlett Learning (pp 4-5)
National Oceanic and Atmospheric Administration (nd) Air Quality Index National Weather Service
https://wwwweathergov/safety/airquality-aqindex
Robbins, J (2022, July 14) Colorado’s efforts are not enough to solve its ozone problem Rocky Mountain PBS https://wwwrmpbsorg/blogs/news/colorado-ozone-pollution-legislation/
US Department of Energy (2012, September 28) View of Denver skyline from South Table Mountain (STM)[Photograph] Flickr https://wwwflickrcom/photos/departmentofenergy/27040059996
United States Department of Transportation (2023, February 16) Table MV-1 - Highway Statistics 2020 https://wwwfhwadotgov/policyinformation/statistics/2020/mv1cfm
United States Environmental Protection Agency (2015, August) Air quality guide for ozone https://wwwairnowgov/sites/default/files/2021-03/air-quality-guide ozone 2015pdf
United States Environmental Protection Agency (2022, April 13) Determinations of attainment by the attainment date, extension of the attainment date, and reclassification of areas classified as serious for the 2008 Ozone National Ambient Air Quality Standards https://public-inspectionfederalregistergov/2022-07509pdf
American Diabetes Association. (2022). Eye Health.
https://diabetes.org/diabetes/eye-health
Centers for Disease Control and Prevention [CDC] (2020a) Hispanics and Latinos Have Higher Risk for Vision Loss https://wwwcdcgov/visionhealth/resources/features/hispanic-latino-vision-healthhtml
CDC (2020b) Keep an Eye on Your Vision Health
https://wwwcdcgov/visionhealth/resources/features/keep-eye-on-visionhealthhtml
CDC (2020c) Vision and Eye Health Toolkit
CDC (2022) Diabetes Fast Facts
https://wwwcdcgov/visionhealth/programs/vision-toolkithtml
https://wwwcdcgov/diabetes/basics/quick-factshtml
Cohen, Stitz, J, Sangi-Haghpeykar, H, & Williams, S P (2018) Vision Screening in Adults Across the Life Span Southern Medical Journal (Birmingham, Ala), 111(2), 109–112
https://doiorg/1014423/SMJ0000000000000762
Grim, M., & Escoffrey, C. (Eds.). (2022). The health education specialist: A companion guide for professional excellence- 2020 (8th edition) National Commission for Health Education Credentialing, Inc
Kahar, & Negroni, L (2020) Results from brief educational intervention and health screenings: A community health study of Latinos in Southwest Florida Journal of Education and Health Promotion, 9(1), 148–148 https://doiorg/104103/jehpjehp 157 20
Martinez, & Acosta Gonzalez, E (2022) Care v Caring: Obligation, Duty, and Love Among Latino Alzheimer’s Family Caregivers Journal of Applied Gerontology, 41(7), 1744–1751.
https://doi.org/10.1177/07334648221084998
National Committee for Quality Assurance (2022) Health Equity https://wwwncqaorg/health-equity/
National Eye Institute (2022) Eye Health Among Hispanics/Latinos https://wwwneinihgov/learn-about-eye-health/outreachcampaigns-and-resources/eye-health-among-hispanicslatinos
Prevent Blindness (2021) New Study Identifies More People with Vision Loss and Blindness Than Previously Estimated https://preventblindnessorg/new-study-identifies-more-people-with-vision-loss/ Ramsey, Lasalle, C C, Anjum, S, Marx, J L, & Roh, S (2022) Telehealth Encourages Patients with Diabetes in Racial and Ethnic Minority Groups to Return for in-Person Ophthalmic Care During the COVID-19 Pandemic Clinical Ophthalmology (Auckland, NZ), 16, 2157–2166 https://doiorg/102147/OPTHS368972
Shaak, Johnson, M. B., Marsh, J. K., Hansen, S. E., Banerjee, E. S., Stello, B., & Careyva, B. A. (2018). Exploring Health Beliefs Among Hispanic Adults with Prediabetes Journal of Community Health, 43(5), 962–968 https://doiorg/101007/s10900-018-0512-2
Sopeyin, Knight, O J, Green, L K, & Woreta, F (2022) Improving Self-Reported Metrics on Racial/Ethnic Diversity in Ophthalmology Trainee Recruitment: Lessons Learned and Future Directions American Journal of Ophthalmology, 234, A1–A4 https://doiorg/101016/jajo202107001
The International Agency for the Prevention of Blindness (2022, January 3) Eye health services linked to advancing the Sustainable Development Goals https://wwwiapborg/news/eye-health-services-linked-to-advancing-the-sustainabledevelopment-goals/
United States Census Bureau (2021) QuickFacts Colorado; United States https://wwwcensusgov/quickfacts/fact/table/CO,US/RHI725221
Prevention of Vision Impairments in Colorado Latinx Populations 66
AI in Healthcare: An Exploration of Health Disparities in Technology Implementation
Bajwa, J, Munir, U, Nori, A, & Williams, B (2021) Artificial intelligence in healthcare: Transforming the practice of medicine
Future Healthcare Journal, 8, e188-194 https://doiorg/107861/fhj2021-0095
Centers for Disease Control and Prevention (2022, October 4) Health Disparities Cdcgovhttps://wwwcdcgov/healthyyouth/disparities/indexhtm
Gurevich, E, El Hassan, B, & El Morr, C (2022) Equity within AI systems: What can health leaders expect? Forum Gestion Des Soins de Sante [Healthcare Management Forum], 8404704221125368 https://doiorg/101177/08404704221125368
Kaul, V, Enslin, S, & Gross, S A (2020) History of artificial intelligence in medicine Gastrointestinal Endoscopy, 92(4), 807–812 https://doiorg/101016/jgie202006040
National Academies of Sciences, Engineering, and Medicine, Health and Medicine Division, Board on Population Health and Public Health Practice, Committee on Community-Based Solutions to Promote Health Equity, Baciu, A, Negussie, Y, Geller, A, & Weinstein, J N (2017) The state of health disparities in the United States National Academies Press
Sjoding, M W, Dickson, R P, Iwashyna, T J, Gay, S E, & Valley, T S (2020) Racial bias in pulse oximetry measurement The New England Journal of Medicine, 383(25), 2477–2478. https://doi.org/10.1056/NEJMc2029240
Takshi, S (2021, April 28) Unexpected inequality: Dispar unexpected inequality: Disparate-impact fate-impact from Arrom artificial intelligence in healthcare intelligence in healthcare decisions Csuohioedu https://engagedscholarshipcsuohioedu/cgi/viewcontentcgi?article=1580&context=jlh
Thomasian, N M, Eickhoff, C, & Adashi, E Y (2021) Advancing health equity with artificial intelligence Journal of Public Health Policy, 42(4), 602–611 https://doiorg/101057/s41271-021-00319-5
Troncoso, E L (2020) The greatest challenge to using AI/ML for primary health care: Mindset or datasets? Frontiers in Artificial Intelligence, 3, 53 https://doiorg/103389/frai202000053
Legal Precedent in American Courts
Hemmens, C, Brody, D C, & Spohn, C (2021) Criminal Courts (5th ed) SAGE Publications, Inc (US) https://onlinevitalsourcecom/books/9781071833872
“With Roe Overturned, Legal Precedent Moves to Centerstage” Americanbarorg, American Bar Association, 24 June 2022, https://wwwamericanbarorg/news/abanews/aba-news-archives/2022/06/stare-decisis-takes-centerstage/ Sellers, Mortimer N “The Doctrine of Precedent in the United States of America” The American Journal of Comparative Law, vol 54, no suppl 1, 2006, pp 67–88, https://doiorg/101093/ajcl/54suppl167
“Stare Decisis” Legal Information Institute, Legal Information Institute, https://wwwlawcornelledu/wex/stare decisis Molony, Thomas J “Taking Another Look at the Call on the Field: Roe, Chief Justice Roberts, and Stare Decisis” Harvard Journal of Law and Public Policy, vol 43, no 3, 2020, pp 733–814, https://eds-p-ebscohostcom.ezproxy.coloradomesa.edu/eds/detail/detail?vid=5&sid=48a8f964-a5c0-46a0-82098dff08ba03fb%40redis&bdata=JnNpdGU9ZWRzLWxpdmUmc2NvcGU9c2l0ZQ%3d%3d#db=bth&AN=143634837 Accessed 12 Feb 2023
Somin, Ilya “The Rights and Wrongs of Overruling Precedent” Reasoncom, The Volokh Conspiracy, 29 June 2020, https://reasoncom/volokh/2019/06/26/the-rights-and-wrongs-of-overrulingprecedent/#:~:text=The%20Supreme%20Court%20has%20over%20time%20developed%20four,When%20the%20court%20last %20month%20overruled%20Nevada%20v
Mystal, Elie “What Is Stare Decisis, and Why Is It Intellectually Hollow Bullshit?” Balls and Strikes, Demand Justice, 20 Dec 2021, https://ballsandstrikesorg/legal-culture/stare-decisisexplainer/#:~:text=No%20Judges%20adhere%20to%20stare%20decisis%20until%20they,for%20when%20a%20Court%20can%2 0overcome%20stare%20decisis
Douglas, William O “Stare Decisis” Columbia Law Review, vol 49, no 6, June 1949, p 735, https://doiorg/102307/1119147
Schafer, M L (2013) Federal Law, Federal Courts, and Binding and Persuasive Authority New Jersey; The Writing Center, Georgetown University Law Center
DOBBS, STATE HEALTH OFFICER OF THE MISSISSIPPI DEPARTMENT OF HEALTH, ET AL. v. JACKSON WOMEN’S HEALTH ORGANIZATION ET AL (Federal Supreme Court October 2021)
References 67




 CMixed media, acrylic, and paper collage on foam board, 11x14 inches
CMixed media, acrylic, and paper collage on foam board, 11x14 inches























 Amanda Skidmore
Amanda Skidmore


 Figure 1. PRISMA diagram – data synthesis of 64 articles screened, resulting in 12 articles chosen for review
Figure 1. PRISMA diagram – data synthesis of 64 articles screened, resulting in 12 articles chosen for review



 McKenzie Schrank
McKenzie Schrank










 Sean Kellogg, Gustavo Tinoco, and Garvita Thareja
Sean Kellogg, Gustavo Tinoco, and Garvita Thareja






 Brenna Coombs
Brenna Coombs



 Valeria Pernas and Garvita Thareja
Valeria Pernas and Garvita Thareja
 therefore improving patient outcomes
therefore improving patient outcomes









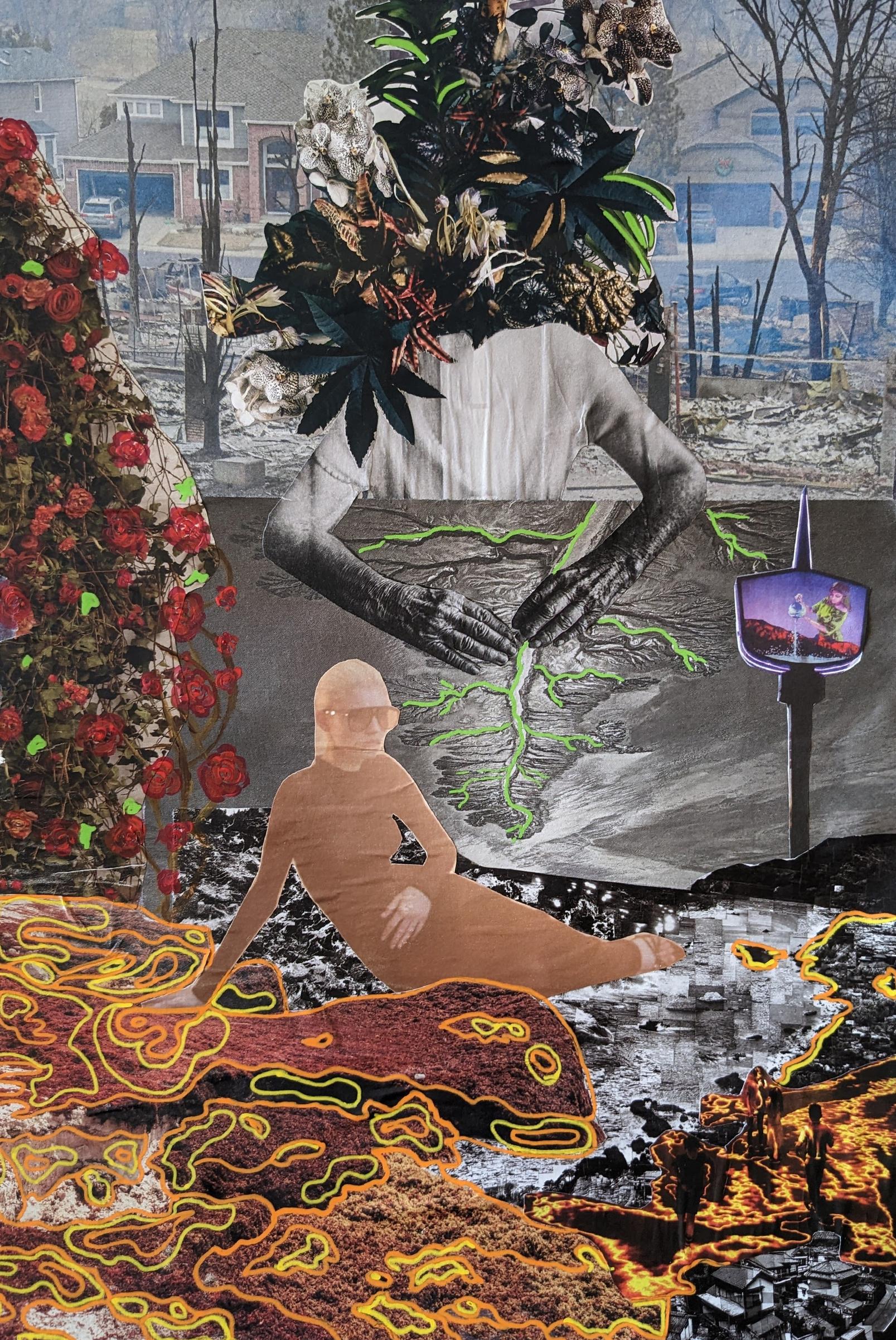
 Kailey Osborne, Garvita Thareja, Natalie Bjorklun, and Youssef Eljazouli
Kailey Osborne, Garvita Thareja, Natalie Bjorklun, and Youssef Eljazouli




 Justy Robinson
Dakota Perez
Justy Robinson
Dakota Perez


 CPHAEmergingLeadersCommitteeassembleanddonate blanketsfortheColoradoChildrensHospitalduringtheholidays
CPHAEmergingLeadersCommitteeassembleanddonate blanketsfortheColoradoChildrensHospitalduringtheholidays





















