
7 minute read
Advancing Community Health with Hospital Community Benefit Spending
from RISE No. 2
Devin Miller
As Colorado communities continue to experience health disparities and rising health care costs, increased awareness and accountability for community health promotion is needed. One area currently receiving attention is how nonprofit hospitals can better support and invest in their local communities (Zelinger, 2023). Nonprofit hospitals are uniquely positioned to make significant contributions to advance the health equity of the diverse communities in which they serve, beyond the basic provisions of providing medical care (Carroll-Scott et al, 2017) Research supports that merely relying on improving access to existing medical care resources will not, in and of itself, address the larger health issues that our nation is experiencing (Prybil et al., 2017). An ideal place to create a paradigm shift in community health investment is through the Internal Revenue Service’s (IRS) community benefit spending requirement for nonprofit hospitals.
Advertisement
Since the mid-1900’s, nonprofit hospitals have been required by the IRS to provide a form of community benefit to justify their tax-exempt status (Carroll-Scott et al., 2017). Under this regulation, community benefit spending is traditionally understood by nonprofit hospitals as any activity that would benefit their community. Benefits to the community may include providing financial assistance to uninsured patients, conducting [relevant] research, or offering education and trainings to healthcare professionals (Rosenbaum 2016; Singh et al, 2015) In 2010, changes were made to community benefit spending under the Patient Protection and Affordable Care Act (ACA) These changes required nonprofit hospitals to conduct triennial Community Health Needs Assessments (CHNA) and develop annual implementation plans to address community identified needs through tailored health services and population health initiatives (Internal Revenue Service, 2010).
The ACA encourages nonprofit hospitals to go beyond the traditional community benefits of charity care (e.g., free and reduced health care costs) to focus on the underlying causes of health inequities and to allocate funds to initiatives for social determinants of health (Carroll-Scott et al, 2017; Rosenbaum, 2016)
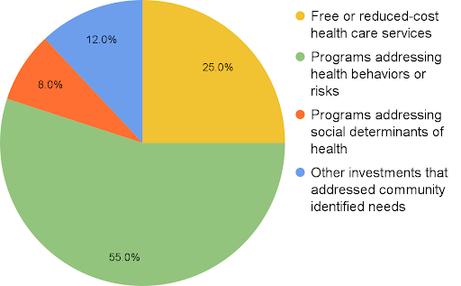
Approximately $100 billion dollars are used for community benefit spending each year in the United States (Chandrashekar et al., 2022). In Colorado, 90% of hospitals are nonprofits and tax-exempt organizations (Colorado Department of Health Care Policy & Financing, 2021). From 2020–2021, Colorado nonprofit hospitals spent $965 million in community benefits (Colorado Department of Health Care Policy and Financing, 2023) These investment categories for Colorado nonprofit hospital community benefit spending include free or reduced-cost health care services, programs addressing health behaviors, programs addressing social determinants of health, and “other investments” that address community needs Based on a recent report, 8% of Colorado community benefit spending is committed to directly addressing social determinants of health (Colorado Department of Health Care Policy and Financing, 2023).
Currently, there are no federal requirements on the amount a nonprofit hospital needs to spend on community benefits, how hospitals identify and prioritize spending initiatives, or what evaluation efforts should be completed to ensure the needs are met by said investments Health advocates argue that the current IRS requirements put loose requirements on nonprofit hospitals and there is only a limited understanding into how community benefit spending is making an impact on the community’s health (Letchuman et al, 2022).
To provide more accountability and transparency on hospital community benefit spending, Colorado passed House Bill (HB) 1320 in 2019. HB 1320 requires nonprofit hospitals to submit a report to the Colorado Department of Health Care Policy & Financing (HCPF) that include: (a) the hospital’s CHNA, Implementation Plan, and the breakout of funding that went to free/reduced-cost health care services, programs addressing health behaviors or risk, and programs addressing social determinants of health, (b) a description of how services and programs address the community identified health needs, (c) details on the public meeting hospitals are required to hold each year to gather feedback on the hospital's community benefit activities With the recent implementation of HB 1320, Colorado nonprofit hospital reporting provides more clarity on their CHNA process and data collection, but advocates continue to push for more requirements and accountability from hospitals.
Limitations
Despite state and federal advancements of CHNA reporting in recent years, advocates continue to highlight the many issues with current CHNA transparency and accountability Table 1 highlights the limitations of the literature One area of focus that remains a concern for community health advocates is the hospital’s methods for employing a meaningful community engagement process for their CHNA The goal of a CHNA is to understand the unique needs of the community, identify the priorities for funding from the community’s perspective, and establish sustainable partnerships (Pennel et al., 2015). Although Colorado made progress when requiring an annual public meeting, this reporting illustrates this approach is still a limited measure of success. Some hospitals do not fully comply with the meeting requirements that are outlined in the statute (Colorado Department of Health Care Policy and Financing, 2023) Hospital reporting shows these meetings are usually limited in attendance and do not provide insight to community priorities For example, one major Colorado hospital did not include a list of participants or organizations that attended the public meeting while other hospitals reported they received “very few questions and comments from public meeting participants” and “none of the questions or comments were actionable”. This reporting does not offer insight due to its inability to determine how community engagement was conducted for the CHNA and determine if the methods for community engagement were grounded in best practices through evaluation.
Similar outcomes for community engagement are found in national community benefit spending reporting Other state's community benefit spending reporting experience similar issues to Colorado Pennel et al use mixedmethods research to describe how authentic community engagement and participation in CHNAs is critical to create effective, equitable, and sustainable programs to improve community health. After analyzing 95 CHNAs and interviewing key informants, they found that while hospitals did have a process for community engagement, these were limited and did not include a broad array of community members or authentic participation in the CHNA process (Pennel et al, 2017) In another qualitative study, Cain et al found that most data used to create the CHNA came from hospital leaders or the board members who are part of the health care organization but do not necessarily speak from personal experience (Cain et al., 2017).
There is currently no framework or guidance provided, by the IRS or other entities, that illustrate a more comprehensive approach to community benefit spending and the importance of community engagement. Authentic community engagement seeks to shift power dynamics and act as a catalyst to create new programs and policies that meet the needs of the community The hospital’s engagement process needs to include active collaboration with communities instead of simply surveying for input on programs that are otherwise designed and led without community participation (Schiavo, 2021) Engaging diverse community partners can help improve “cultural sensitivity, reliability, and validity” in CHNAs while “emphasizing locally relevant problems and approaches to addressing health problems” (Pennel et al., 2017, p. e104). It is essential that CHNAs include community partners to improve health equity in communities. The community collaboration for CHNAs is acknowledged and supported, although the use of them is limited in CHNA development and the prioritization of fund allocations (Ainsworth et al, 2013; Cain et al, 2017; Chandrashekar et al, 2022)
Comprehensive and standardized reporting requirements of nonprofit hospital community engagement efforts would improve data collection, reduce the obfuscation of community initiative planning, and strengthen community partnerships.
Since health inequities are complex and influenced by factors outside of the healthcare system, strategies to improve them should include sectors outside of the traditional health care framework such as faith-based organizations, transportation agencies, and housing authorities Community benefit spending has the potential to create a substantial impact on community health If hospital and community leaders dedicate the time and resources, “needs assessments can become the catalyst whereby transformative change occurs within communities” (Ainsworth et al., 2013, p. 869). The impact and applicability of community benefit spending could be farreaching and greatly improve community health.










