Canadian HEALTHCARE REVOLUTIONIZING
HealthcareFacilities
JOURNAL OF CANADIAN HEALTHCARE ENGINEERING SOCIETY
Artificial intelligence-driven tools transforming facilities management and design
Nova Scotia hospital earns Energy Star
IWK Health's commitment to accessibility
Water for the processing of medical devices
MOBILE MEDICAL DEVICE REPROCESSING AREA
COMPLETE SUPPORT THAT HELPS REDUCE RISK, SAVE TIME, AND POTENTIALLY LOWER COSTS




Whether support is needed during hospital construction, renovation, expansion, or for emergency response, STERIS partners every step of the way.
The Mobile Medical Device Reprocessing Area, supported by your local STERIS team, allows care centres to operate at 100%. The fully equipped and integrated unit supports high standards of performance, compliance, and productivity by:
• Eliminating the need for phased construction
• Meeting procedural needs with instrument reprocessing designed for compliance to the current standards
• Utilizing simple single-point electrical and plumbing connections for turnkey operation


INNOVATION & TECHNOLOGY
Closing the As-built Gap Etobicoke General Hospital adopts webbased living maps to manage space, critical equipment
The Path to Dignity and Respect Washroom upgrade supports IWK Health’s commitment to accessibility
16 A Provincial First L'hôpital Fishermen's Memorial obtient la certification Energy Star
23 A Collaborative Success
Emergency public health relocation in Alberta demonstrates what empowered teams can accomplish under pressure
Transforming Healthcare Together
Empowering teams, inspiring creativity, unleashing knowledge
Real-time Knowledge Integration of computer vision-based AI improves workflows
Twins in Design
data models of physical assets transforming the built world
Water Safety in Device Processing New standard brings critical changes to facility management
Reproduction or adoption of articles appearing in Canadian Healthcare Facilities is authorized subject to acknowledgement of the source. Opinions expressed in articles are those of the authors and are not necessarily those of the Canadian Healthcare Engineering Society. For information or permission to quote, reprint or translate articles contained in this publication, please write or contact the editor.
Canadian Healthcare Facilities Magazine Rate
Extra Copies (members only)
Canadian Healthcare Facilities (non members)
Canadian Healthcare Facilities (non members)
$25 per issue
$30 per issue
$80 for 4 issues
A subscription to Canadian Healthcare Facilities is included in yearly CHES membership fees.
EDITOR/RÉDACTRICE Clare Tattersall claret@mediaedge.ca
PUBLISHER/ Jake Blanchard ÉDITEUR DU GROUPE jakeb@mediaedge.ca
PRESIDENT/PRÉSIDENT Kevin Brown kevinb@mediaedge.ca
SENIOR DESIGNER/ Annette Carlucci CONCEPTEUR annettec@mediaedge.ca
GRAPHIQUE SENIOR
GRAPHIC DESIGNER/ Thuy Huynh-Guinane GRAPHISTE roxyh@mediaedge.ca
PRODUCTION Ines Louis COORDINATOR/ inesl@mediaedge.ca COORDINATEUR DE DE PRODUCTION
CIRCULATION MANAGER/ Adrian Holland DIRECTEUR DE LA circulation@mediaedge.ca DIFFUSION
CANADIAN HEALTHCARE FACILITIES IS PUBLISHED BY UNDER THE PATRONAGE OF THE CANADIAN HEALTHCARE ENGINEERING SOCIETY. SCISS JOURNAL TRIMESTRIEL PUBLIE PAR SOUS LE PATRONAGE DE LA SOCIETE CANADIENNE D'INGENIERIE DES SERVICES DE SANTE.
CHES SCISS
PRESIDENT Jim McArthur
VICE-PRESIDENT Kate Butler
PAST PRESIDENT Craig B. Doerksen
TREASURER Reynold J. Peters
SECRETARY Paul Perschon
EXECUTIVE DIRECTOR Tanya Hutchison
CHAPTER CHAIRS
Newfoundland & Labrador: Colin Marsh
Maritime: Steve Smith
Ontario: Beth Hall
Quebec: Mohamed Merheb
Manitoba: Stephen R. Cumpsty
Saskatchewan: Kendall Rathgeber
Alberta: James Prince British Columbia: Mitch Weimer
FOUNDING MEMBERS
H. Callan, G.S. Corbeil, J. Cyr, S.T. Morawski
CHES
4 Cataraqui St., Suite 310, Kingston, Ont. K7K 1Z7 Telephone: (613) 531-2661 Fax: (866) 303-0626 E-mail: info@ches.org www.ches.org
Canada Post Sales
Product Agreement No. 40063056 ISSN
La reproduction ou l’adaptation d’articles parus dans le Journal trimestriel de la Société canadienne d’ingénierie des services de santé est autorisée à la condition que la source soit indiquée. Les opinions exprimées dans les articles sont celles des auteurs, qui ne sont pas nécessairement celles de la Société canadienne d’ingénierie des services de santé. Pour information ou permission de citer, réimprimer ou traduire des articles contenus dans la présente publication, veuillez vous adresser à la rédactrice.
Prix d’achat du Journal trimestriel
Exemplaires additionnels (membres seulement) $25 par numéro
Journal trimestriel (non-membres) $30 par numéro
Journal trimestriel (non-membres) $80 pour quatre numéros
L’abonnement au Journal trimestriel est inclus dans la cotisation annuelle de la SCISS.
BREATHING EMERGENCIES

GROWING UP IN Toronto, it was unheard-of for wildfire smoke to blanket the city. In mid-July, Environment and Climate Change Canada issued an alert about the layer of haze in the air, blown in from wildfires burning in northern Ontario and the Prairies, and pushing Toronto’s air quality to the second-worst in ranking among major cities around the world. The warning was not the first of the year and will likely not be the last, which is frightening given the potential consequences of inhaling wildfire smoke, ranging from dizziness, difficulty breathing and a cough to premature dementia and long-term lung, heart and kidney problems. Still, Torontonians should count themselves lucky, which, I know, sounds absurd given the health risks. People living in wildfire-prone communities face even greater adverse physical health outcomes on top of the mental anguish of potentially losing their home and livelihood. Then there are those who can’t move themselves because they’re in hospital and therefore must rely on healthcare professionals to successfully execute an evacuation. The disruption represents a risk to the lives of patients, especially those with serious health conditions.
Wildfires aren’t the only emergency to prompt an evacuation order. In the case of Alberta Health Services, the discovery of lead levels in the HVAC system at the Grande Prairie Provincial Building required the rapid relocation of its public health services. A Collaborative Success details the urgent move, including the coordinative effort involved.
But first, to begin this issue is a celebratory story about a Nova Scotia hospital that has earned Energy Star certification. Congratulations to the team that worked diligently to obtain this achievement. A major focus of the summer edition is innovation and technology. Article topics cover web-based living maps, accessible washroom design, artificial intelligence and digital twins.
To close, we look at a new standard for water quality systems in device reprocessing.
Looking to the fall issue, if interested in contributing an article related to facility management and design or sustainable healthcare, please contact me. These are key themes outside the focus on this year’s CHES awards recipients.
Clare Tattersall claret@mediaedge.ca




NEWS, VIEWS AND UPDATES


I HAD THE PLEASURE of attending CHES chapter conferences in Winnipeg (Manitoba chapter), Moncton, N.B. (Maritime chapter), Montreal (Quebec chapter), Kitchener (Ontario chapter) and Penticton (B.C. chapter) this past spring. All conferences set attendance records, thanks to the hard work of their planning committees, exhibitors and sponsors.
I also attended the IFHE-EU Congress in Antwerp, Belgium, in May. There were approximately 1,000 delegates from around the globe and 172 booths in the exhibit hall. Outside of the conference, I went to meetings on International Federation of Healthcare Engineering (IFHE) standing orders, the IFHE Americas Group and IFHE general council meeting.
The CHES corporate advisory council committee meets regularly, with their most recent meeting taking place May 13. Brennan Ficko is committee chair. He will report at the next CHES National board meeting, including on the addition of new committee members.
The CHES National executive and board continue to work on guidelines for our strategic plan, which provides guidance and structure for the activities of the board and its subcommittees. There will be an in-person strategic planning meeting for the board in Calgary, ahead of the 2025 CHES National Conference.
We continually meet with representatives from various organizations to review potential collaboration initiatives. This includes the American Society for Healthcare Engineering, Infection Prevention and Control Canada, Canadian Coalition of Health Leaders and Accreditation Canada.
The CHES National executive meets monthly to review the bylaws, budgets and other activities of CHES, including recommendations to the board.
Jim McArthur CHES National president
EARN CONTINUING EDUCATION CREDITS FROM CHES
Members of the Canadian Healthcare Engineering Society can earn free continuing education units (CEU) by reading the Summer 2025 issue of Canadian Healthcare Facilities and passing a quiz based on articles in the issue. Once you’ve read the issue from cover to cover, simply go online to https://www.surveymonkey.com/r/9Y99THM to take the quiz. CHES members who pass the quiz will be able to claim one contact hour (0.1 CEU) on their CanHCC or CCHFM certificate renewals.









EA HIDDEN CRISIS:



VIOLENCE IN THE HEALTHCARE WORKPLACE
very morning, healthcare workers across the country enter their facilities knowing they face risks that extend far beyond medical emergencies. The stats paint a sobering picture: healthcare professionals are five times more likely to experience workplace violence than employees in any other industry, accounting for 73 per cent of all nonfatal workplace injuries due to violence¹. This isn’t just a security concern; it’s a threat to the very foundation of our healthcare system.
The scope of this crisis became starkly apparent through recent research revealing that 81.6 per cent of nurses have experienced at least one type of workplace violence incident, with nearly half reporting an increase in violence rates². The Canadian Medical Association’s recent National Physician Health Survey found that eight in 10 physicians have experienced intimidation, bullying, harassment, or microaggressions in the workplace at some point in their careers3. These aren’t isolated incidents in troubled facilities; they represent a systemic challenge a ecting institutions from prestigious private medical centres to community hospitals. The human toll is disturbing, but the economic impact is equally shocking, with violence response e orts costing hospitals and health systems approximately billions annually4.
THE HEALTHCARE SECURITY PARADOX
What makes healthcare environments particularly vulnerable is their inherent contradiction: they must remain open,

How smart access control can help protect our caregivers
accessible, and welcoming while protecting vulnerable patients and stressed sta . Traditional security approaches often feel inappropriate in healing environments, creating a complex challenge that demands sophisticated solutions. This is where modern access control technology emerges as a critical component of comprehensive workplace violence prevention.
“Healthcare facilities face a unique security paradox,” explains Kyle Pfei er, Healthcare Industry Solutions Leader at Salto. “They need to maintain the open, healing environment that patients require while protecting sta from increasingly frequent violent incidents. Our approach recognizes that e ective healthcare security isn’t about building barriers, it’s about creating intelligent, adaptive systems that enhance safety without compromising the human connection that’s essential to healthcare.”

MODERN ACCESS CONTROL MAY HOLD THE KEY
Salto has developed an integrated approach that addresses this paradox through features designed specifically for healthcare environments. The foundation of this protection lies in comprehensive audit trails from every access point, creating a permanent record that serves dual purposes: deterring potential bad actors who know their movements are being tracked, and revealing behavioural patterns that can be addressed before they escalate into violence. This invisible shield of documentation transforms access control from a reactive tool into a proactive early warning system.
Sophisticated visitor management and identity verification capabilities allow healthcare facilities to maintain their welcoming atmosphere while ensuring unauthorized individuals cannot access sensitive areas. Real-time threat response and lockdown capabilities provide immediate protection when incidents occur, enabling security teams to isolate threats while protecting both sta and patients. Perhaps most importantly, sta empowerment through mobile access eliminates the vulnerabilities of physical credentials that can be lost, stolen, or used by unauthorized individuals, while seamlessly integrating with broader security ecosystems to create a comprehensive protective environment.
ADAPTING TO HEALTHCARE’S DIVERSE ENVIRONMENTS
The beauty of Salto’s approach lies in its adaptability to di erent healthcare environments. For example, emergency departments, where 85 per cent of physicians report increased violence over the past five years5, benefit from wireless locks that provide immediate access control without disruptive hardwiring. Another area that could be improved is pharmaceutical storage, which is critical for preventing drug theft and protecting sta . Utilizing electronic cylinders that create comprehensive audit trails while enabling time-based access restrictions aligned with sta schedules can help address this issue.
THE ECONOMICS OF PREVENTION
The financial justification becomes compelling when analyzed against violence-related costs. Each percentage point reduction in registered nurse turnover can lower labour costs by $263,000 annually for the average hospital6. When combined with reduced security personnel requirements, insurance premium reductions, and liability mitigation, the return on investment in advanced access control becomes substantial.
Yet the true measure of success extends beyond financial metrics. The underreporting culture that plagues healthcare, where studies suggest 88 per cent of workplace violence incidents go undocumented7, begins to shift when sta feel genuinely protected. Advanced access control systems create an environment where incidents are prevented rather than merely responded to after the fact.

THE FUTURE OF HEALTHCARE WORKPLACE SAFETY
Looking forward, the integration of artificial intelligence and predictive analytics promises even more sophisticated threat assessment capabilities. However, the immediate need remains clear: healthcare organizations must transition from reactive security postures to proactive, intelligence-driven approaches that protect sta while maintaining the accessibility essential to quality patient care.
The crisis of healthcare workplace violence demands more than traditional security measures; it requires thoughtful, technology-enabled solutions that understand the unique challenges of healing environments. Salto’s healthcare solutions o er industry leaders a pathway toward sustainable safety improvements that protect their most valuable assets: the dedicated professionals who serve others during their most vulnerable moments.
Salto is a leading global access solutions provider, developing facility access, identity management, and electronic locking technology providing seamless, reliable, and secure experiences. For more information, please visit saltosystems.ca
Sources:
1. American College of Surgeons, “Violence Escalates against Surgeons and Other Healthcare Workers,” ACS Bulletin, October 2024
2. National Nurses United Survey, 2024
3. Canadian Medical Association, “2021 National Physician Health Survey,” 2021
4. American Hospital Association Report, 2017
5. American College of Emergency Physicians Survey, 2024
6. NSI Nursing Solutions, Healthcare Workforce Analytics, 2023
7. Gillam, S.W., et al., “Impact of an Electronic Incident Reporting System on Workplace Violence Reporting,” International Journal of Healthcare Management, 2015
BRITISH COLUMBIA CHAPTER
CHES B.C. held its spring conference in Penticton, June 1-3. As the demands on healthcare facilities grow increasingly complex, the chapter looked to explore a vital evolution in healthcare infrastructure. Around the theme, Healthcare Facilities Beyond Bricks and Mortar, the conference delved into how healthcare environments extend beyond physical structures to embody comprehensive systems of care, innovation and resilience. It invited industry professionals to reimagine healthcare spaces that serve as pillars of health, safety and environmental stewardship, transforming the landscape of Canadian healthcare for generations to come. The program kicked off with keynote speaker Susan Brown, CEO of Interior Health Authority. After the keynote address, there was a dual track of sessions, which covered pressing issues, such as energy efficiency, carbon reduction, digital integration, patient-centred design and emerging trends in healthcare. Participants explored emerging technologies, best practices and advanced energy solutions that drive operational efficiencies while fostering healthier, more sustainable spaces for patients and staff alike. The trade show was sold-out since January, with a record number of exhibitors. The banquet hall also sold-out slightly over capacity at 600 people. As always, I’d like to thank everyone on the chapter conference committee for their hard work to make the event a success.
The B.C. chapter is currently undergoing the process of incorporation. Our bylaws committee consists of Sarah Thorn, Rick Molnar and Norbert Fischer. Progress is taking longer than expected due to member availability, and timing of back and forth discussions on the extent of the bylaws update that’s required to adhere to the B.C. Societies Act, yet also meet the needs of both CHES National and chapter executives. We are currently moving forward with a blended set of bylaws and trying to keep all parties happy. Due to legislative necessity, the B.C. Societies Act will take precedence.
CHES B.C. has experienced some changes since my last report. Communications committee chair Wesley Fan has resigned, so we are currently seeking a replacement. Norbert has kindly stepped in to fill the void.
CHES National continues to move forward with the website roll out. Recent reviews have been favourable and the platform has worked well for our conference information.
The B.C. chapter will once again host the Canadian Healthcare Construction Course in November.
2026 is an election year for the B.C. chapter. We are actively seeking people to step in and help with various positions. If interested and able to commit time and energy to the chapter, please reach out. I’d be happy to chat to explain the needs and commitment required.
On the education front, CHES B.C. continues to provide a wonderful conference education program designed to help its members excel in their work life. Chapter members also receive complimentary webinar program access, and we offer educational sponsorship of up to $1,000 to help with professional development. Every year we receive some applications but rarely fill up. Check out the B.C. chapter page on the CHES website and hit us up if looking for educational funding. CHES B.C. also has a number of perpetual educational bursaries at various provincial post-secondary institutions to help out the next generation.
—Mitch Weimer, British Columbia chapter chair
MANITOBA CHAPTER
The Manitoba chapter held its annual education day on April 15. It was a rousing success with more than 38 exhibitors and 100 attendees. The theme was Navigating Aging Infrastructure.
Next year’s education day is scheduled for May 15. Thank you to the Maritime and Newfoundland and Labrador chapters for agreeing to the change.
The CHES Manitoba Award for Excellence in Project Management was awarded to Brad Cudmore of Southern Health-Santé Sud. The Award for Excellence in Facilities Management was given to Glenn Shymko from Interlake-Eastern Regional Health Authority.
The Winnipeg Construction Association (WCA) hosted the CSA Infection Control During Construction in Healthcare Facilities course May 21-22, in Winnipeg. The Manitoba chapter will host the Canadian Healthcare Construction Course in collaboration with the WCA Nov. 4-5.
—Stephen R. Cumpsty, Manitoba chapter chair
ALBERTA CHAPTER
Over the past quarter, Alberta chapter executive members have actively participated in provincial CHES conferences in Ontario and British Columbia. The visits were part of a strategic effort to promote the 2025 CHES National Conference, which will be hosted in Calgary, Sept. 14-16, at BMO Centre. These outreach efforts have been met with enthusiasm, and we are seeing growing interest from across the country. The chapter is committed to delivering a high-quality experience for all attendees.
The theme of this year’s national conference is Transforming Healthcare Together: Empowering Teams, Inspiring Creativity, Unleashing Knowledge. Key highlights from the program include the opening reception at Studio Bell, home of the National Music Centre; keynote speaker Ross Bernstein, presenting ‘The Champion’s Code;’ educational sessions on integrated project delivery, infrastructure innovation and sustainability; facility tours of South Health Campus and the Arthur J.E. Child Comprehensive Cancer Centre; Women in CHES brunch and a full companion program; and CHES golf tournament at Kananaskis Country Golf Course.
I am thrilled to report that exhibitor space for the 2025 CHES National Conference is completely sold-out. This milestone is a testament to the hard work of our exhibitor recruitment team and the strong support from industry partners.
While exhibitor booths are fully booked, delegate registration remains open. I strongly encourage members and professionals in healthcare engineering and facility management to register soon. The conference promises to be a dynamic and enriching experience, offering valuable networking, professional development and inspiration.
Submissions for CHES Alberta’s executive elections have officially closed. I’d like to thank all members who submitted nominations and expressed interest in serving. Election results will be formally announced during the chapter’s annual general meeting at the national conference in Calgary.
—James Prince, Alberta chapter chair
CHAPTER
Unlike previous years, this past spring was drier. We were not on the receiving end of much snow during winter, leaving brooks and ponds lower than normal and grounds extremely dry. Several forest fires have erupted and I’m confident many more are to come.
The chapter has moved our annual conference to fall from spring, and next year St. John’s will host the CHES National conference. This makes for busy times within the chapter. To promote the 2026 conference, the chapter executive has voted to send the entire team to the 2025 CHES National Conference in Calgary, along with one member from our paid membership, chosen by draw. As an executive, we decided the chapter should be well-represented at the national conference. Plus, it connects more of our members with their peers across the country.
There has been no change to the executive team. We are all in and moving forward planning the chapter’s fall conference and next year’s national conference. For the past two years, we have experienced a steady uptake in participation at our local conference, so this year we have selected a new venue, NL Health Services’ Health Innovation Acceleration Centre, where we can increase the number of vendor booths. We are predicting this year’s conference to be the largest thus far.
The chapter is sitting in a solid financial position. We are looking at creative ways of spending a portion of this funding and investing in the continual education of our members, either through sponsorships to conferences and/or educational reimbursements.
Our membership has seen an increase over the past year, which is mostly due to the provincial capital planning and engineering group. This is great given the program covers coastto-coast within the province and encompasses all five health zones.
—Colin
MARITIME CHAPTER
The Maritime chapter held its spring conference May 4-6, at the Delta Beausejour in Moncton, N.B. The theme was Healthcare Infrastructure for a Resilient and Safe Environment. By all accounts it was a resounding success with approximately 228 in attendance. The exhibit hall was sold-out. We hosted 130 exhibitors representing a total of 53 vendors/booths. Due to an overwhelming response, registrations had to be closed early at 98 delegates and speakers. As a result, we had to split dinner between two restaurants. I’d like to thank our sponsors, delegates and the conference planning team. The conference success is a direct result of their dedication and volunteerism.
CHES Maritime is planning to host the Canadian Healthcare Construction Course in Halifax, Oct. 22-23. The chapter is planning to host an education day in Truro, N.S., in November. The exact date is to be determined.
While the Maritime chapter has a strong membership base in Nova Scotia and New Brunswick (around 280 members), we notably lack membership and leadership from Prince Edward Island. The chapter is actively seeking members and executive representation from this region.
This year’s Per Paasche educational bursary recipient is Jacob Comeau of Summerville, N.B. Jacob is the son of Helen Comeau from Horizon Health Network/Réseau de santé Horizon, a longstanding CHES member and recent Maritime chapter executive member. The chapter collectively wishes Jacob all the best on his goal to obtain a Red Seal as a millwright/industrial mechanic. The bursary is named after our late colleague Per Paasche. All Maritime CHES members who are in good standing and their immediate family members (daughters, sons, grandchildren, nieces, nephews and spouses) are eligible to apply for the $1,000 educational grant.
The Maritime chapter continues to offer several financial incentives to our members, such as the Per Paasche bursary, contribution to Canadian Certified Healthcare Facility Manager exam fees, and spring and fall education days, among other membership benefits.
—Steve Smith, Maritime chapter chair

Marsh, Newfoundland & Labrador chapter chair
QUEBEC CHAPTER
CHES Quebec continues to build on the momentum established earlier in the year, with a focus on engagement, growth and strategic partnerships.
On May 7, we proudly hosted our chapter conference in Montreal, under the theme Connect, Collaborate, Progress. The event was a success, bringing together more than 100 participants, more than half of whom were hospital-based professionals. We were honoured to welcome CHES National president Jim McArthur, whose presence reinforced the importance of national-provincial collaboration. The four technical sessions were well-received, providing valuable insights and stimulating discussion among our members. Importantly, this event led to a noticeable increase in chapter membership — a testament to the relevance of our mission.
During the conference, a call for new executive members was issued to ensure the sustainability and renewal of our leadership team. I invite all members who are passionate about healthcare infrastructure to consider contributing to CHES Quebec’s future direction. Looking ahead, we are actively working with the Association de la construction du Québec to host another Canadian Healthcare Construction Course session in November or December. This builds on our successful collaboration and supports continued efforts to make high-quality training accessible across the province.
—Mohamed
Merheb, Quebec chapter chair
CHAPITRE DU QUEBEC
La SCISS continue de capitaliser sur l’élan amorcé plus tôt cette année, en mettant l’accent sur l’engagement, la croissance et les partenariats stratégiques.
Le 7 mai, nous avons eu le plaisir d’organiser la deuxième édition de notre conférence du chapitre à Montréal, sous le theme Connecter, Collaborer, Progresser. L’événement a été un véritable succès, réunissant plus de 100 participants, dont plus de la moitié provenaient du milieu hospitalier. Nous avons eu l’honneur d’accueillir le président national de la SCISS, Jim McArthur, dont la présence a renforcé l’importance de collaboration entre les niveaux national et provincial. Les quatre conférences techniques ont été très appréciées, offrant des perspectives précieuses et suscitant des échanges stimulants entre nos membres. Cet événement a également permis une augmentation notable de notre nombre de membres — un reflet clair de la pertinence de notre mission.
Lors de la conférence, un appel a été lancé pour recruter de nouveaux membres au sein de l’exécutif, dans le but d’assurer la pérennité et le renouvellement de notre équipe de direction. Nous invitons tous les membres passionnés par les infrastructures de santé à envisager de contribuer à l’avenir de la SCISS.
En regardant vers l’avenir, nous travaillons activement avec l’Association de la construction du Québec a fin d’organiser une autre session du cours canadien sur la construction en santé en novembre ou décembre. Cette initiative s’inscrit dans la continuité d’une collaboration fructueuse et soutient nos efforts continus pour render la formation de qualité accessible à l’écchelle de la province.
—Mohamed Merheb, chef du conseil d’administration du Québec
As the first female chair of the Ontario chapter, I am inspired to work with such a great group of committed and dedicated individuals and excited for the future of our chapter. I am hopeful I can live up to expectations and help support CHES Ontario to excel and move forward.
For the first time in recent memory, there was notable competition for executive positions during elections, indicating a growing interest and investment in the chapter’s future. I am honoured to work with Chris Mackey (vice-chair), Daniel Neaves (secretary), Rudy Dahdal (treasurer) and John Marshman as he transitions to the position of pastchair. I’d like to acknowledge John for his leadership, guidance and ongoing support. Leaving the Ontario chapter executive are Ken Paradise and Jim McArthur. On behalf of CHES Ontario, I would like to thank both Ken and Jim for their dedication to CHES and many years of service on the chapter executive.
The executive team transition comes on the heels of a tremendously successful spring conference. Held in Kitchener, May 2527, it was expertly led by Ron Durocher and his dedicated team. The event not only showcased CHES Ontario’s commitment to advancing healthcare engineering but also highlighted the chapter’s dedication to excellence framed within the theme, Engineering Intelligence into Healthcare Facilities. After the conference, the chapter hosted the Canadian Healthcare Construction Course, which saw more than 50 people in attendance.
As the new executive team comes together, our focus will include strategies to engage current members while attracting new ones, fostering a vibrant community dedicated to healthcare engineering excellence. This momentum will lead to innovative programs, networking opportunities and professional development resources that benefit all members. The future looks bright for CHES Ontario, as we aim to build on past successes and further strengthen our impact in the healthcare engineering field. Here’s to a year filled with innovation, collaboration and success.
SASKATCHEWAN CHAPTER
CHES Saskatchewan’s executive team has been busy planning the chapter’s 2025 conference and trade show, to be held Oct. 19-21, at TCU Place in Saskatoon. Vendors and delegates have been sent invitations and registration information. We continue to reach out to vendors, sponsors and speakers, as we further develop education topics and the theme of this year’s event. If interested in attending or sponsoring the conference, please e-mail ches.sk@accesscomm.ca.
Melodie Young, now past chair of CHES Saskatchewan, recently stepped down from her role and I have taken over for her. My previous position of vice-chair is in the process of being filled. Through these changes, we’ve gained some new directors to the board. I’d like to extend a warm welcome. We’re excited to work with these new members and continue to grow our chapter.
—Kendall Rathgeber, Saskatchewan chapter chair
—Beth Hall, Ontario chapter chair










FROM WILDFIRE TO WARD
Why Indoor Air Quality (IAQ) Can’t Be Ignored in Healthcare Settings
With wildfires raging once again across Canada, air quality is deteriorating at an alarming rate. Thick smoke is seeping into residential and public spaces, prompting a surge in respiratory-related visits to emergency departments nationwide. As hospitals adapt to this growing strain, the need for fortified clean-air strategies has become critical to ensure patient safety and effective care.
“The critical importance of proactive indoor air quality management in healthcare facilities cannot be overstated,” said Erica Brabon, Senior Director, Energy & Sustainability Services, Black & McDonald. “Robust building systems, including advanced filtration and ventilation, are no longer just about comfort; they are essential lines of defense, safeguarding the
health of patients, staff, and visitors from external environmental threats. The B&M team actively partners with clients to assess vulnerabilities, upgrade infrastructure, and implement innovative technologies—empowering facilities to address immediate challenges while building long-term resilience.”
BREATHING HAZARDS
Forest fires release vast amounts of harmful air pollutants, including smoke and fine particulate matter capable of travelling hundreds or even thousands of kilometres. One of the most concerning components is PM2.5—tiny particles which can penetrate deep into the lungs and even enter the bloodstream. These particles, often composed of organic material, heavy

metals, and other combustion byproducts, are linked to symptoms such as headaches, allergies, fatigue, and other long-term health complications.
The risks are especially pronounced for vulnerable groups, including individuals over 65, pregnant women, and people living with cardiovascular conditions, asthma, or chronic obstructive pulmonary disease (COPD). In addition to PM2.5, wildfire smoke contains other hazardous compounds like carbon monoxide (CO), nitrogen oxides (NOx), and polycyclic aromatic hydrocarbons (PAHs). Together, these pollutants can cause acute symptoms and contribute to serious, chronic effects, including respiratory decline and heart disease.
STEPS TO PROTECT OCCUPANTS
During seasons of poor outdoor air quality, healthcare facilities face heightened risks due to the vulnerability of their patient populations and the critical need for safe clinical environments. To protect occupants and maintain operational resilience, facility teams should prioritize comprehensive IAQ strategies centered around their HVAC systems.
The first step of any good IAQ assessment should include:
• A visual inspection to identify any conditions that may have an impact on IAQ.
• A review of the supply and return air distribution and a review of occupant activities, housekeeping practices, building materials, and furnishings that can contribute to the distribution, accumulation, and/or generation of indoor air requirements.


• Spot measurements for temperature, humidity, CO2 and CO, PM2.5 etc. and air sampling for mould
After the initial assessment, a deeper dive can be explored to eliminate potential inefficiencies within the HVAC system, including:
• Filtration: Are the current HVAC systems using high-efficiency air filters to capture dust, pollen, and other airborne particles? Proper filtration removes contaminants and reduces the presence of allergens in the air to significantly improve IAQ.
• Circulation: Are the HVAC systems set at the proper parameters to ensure proper and clean air circulation throughout the different spaces in the building? When outdoor air quality is poor, HVAC systems should be adjusted to maintain adequate ventilation, without letting in poor air to circulate with clean indoor air.
• Purification: Do the current HVAC systems integrate air purification technologies such as UV-C germicidal lamps or electronic air cleaners? These types of equipment target and offset, or capture dangerous microorganisms, bacteria, and other viruses to improve IAQ.
• Temperature and Humidity Control: Are you monitoring and regulating moisture in the air to stop the growth of mold, mildew, and other issues that can impact IAQ? Properly set up HVAC systems control both the temperature and humidity within spaces to contribute to your occupant’s overall comfort and well-being.
Finally, by partnering with a reputable mechanical facility services provider like Black & McDonald, you will ensure your HVAC systems are routinely monitored, maintained, and cleaned to guarantee consistent and optimal functionality. These systems are often intricate, yet vital to a building’s IAQ, so ensuring they are installed and properly maintained is pivotal to a healthy indoor environment.
Prioritize indoor air quality today by contacting Black & McDonald’s Facility Services at facilityserviceinquiries@blackandmcdonald.com.

A PROVINCIAL FIRST
L'hôpital Fishermen's Memorial obtient la certification Energy Star
By/Par Keith Corcoran
Fishermen’s Memorial Hospital in Lunenburg has become the first hospital in Nova Scotia to earn Energy Star certification.
This achievement places the South Shore facility among an elite group of only seven hospitals nationwide that have met the Energy Star standard.
An Energy Star-certified building is known for its outstanding energy efficiency and environmental stewardship. In 2024, the hospital achieved an Energy Star score of 92, meaning it is more energy-efficient than 92 per cent of similar buildings across Canada. The certification reflects dedication to reducing energy consumption, lowering operating costs and cutting greenhouse gas emissions.
Hospital officials, supporters and staff celebrated the occasion with a ceremony in May, where Nathaniel Schrader of EfficiencyOne presented a commemorative certificate and plaque to hospital site lead and health services manager Troy Routledge.
“This award is a testament to the strong partnership between EfficiencyOne and Nova Scotia Health to implementing these smart
Le premier hôpital de Nouvelle-Écosse, l’hôpital Fishermen’s Memorial de Lunenburg, s’illumine d’une nouvelle reconnaissance: il vient d’obtenir la certification Energy Star.
L’hôpital de la rive sud rejoint le cercle prestigieux des sept établissements canadiens certifiés Energy Star.
L’hôpital affiche fièrement sa nouvelle certification Energy Star — un gage d’efficacité énergétique hors pair et d’une gestion environnementale exemplaire. En 2024, il a récolté une note de 92, signe qu’il surpasse 92 pour cent des établissements similaires à travers le Canada. Cette distinction témoigne d’un engagement résolu: réduire la consommation d’énergie, diminuer les coûts d’exploitation et limiter l’empreinte carbone.
L’équipe hospitalière s’est réunie en mai pour une cérémonie mémorable. Au nom d’EfficiencyOne, Nathaniel Schrader a honoré Troy Routledge, gestionnaire du site et des services de santé, en lui remettant un certificat et une plaque commémorative.
“En unissant leurs forces, Nova Scotia Health et EfficiencyOne ont conçu des solutions durables qui transcendent la simple performance énergétique,” souligne Schrader. “Ces innovations intelligentes
“OUR FACILITY HAD TO BE PROFESSIONALLY VERIFIED THAT WE OPERATE MORE ENERGY
EFFICIENTLY THAN AT LEAST 75 PER CENT OF SIMILAR BUILDINGS NATIONWIDE.”
and sustainable solutions to improving building performance, while maintaining the highest standards of patient care,” said Schrader.
Based in Nova Scotia, EfficiencyOne is a provider of energy efficiency and carbon mitigation services.
The plaque and certificate will be displayed in the hospital entrance, serving as a visible reminder of the site’s dedication to environmental stewardship and a greener future.
“Our facility had to be professionally verified that we operate more energy efficiently than at least 75 per cent of similar buildings nationwide,” John Hann, Nova Scotia Health’s director of maintenance and operations, told those gathered at the event. “We had to confirm the building operates in accordance with industry standards for indoor environmental quality.”
Hann credited the site’s environmental stewardship program, managed by Robert Barss, and the partnership with EfficiencyOne as playing major roles in the program’s success.
“I appreciate your efforts and what you did,” said Hann, noting Nova Scotia Health has been taking steps to improve energy efficiency across all its facilities.
“To date, the hospital’s environmental stewardship program has implemented energy savings projects that have reduced almost 34,000 tons of greenhouse gas emissions and saved nearly $6 million annually,” he
optimisent nos bâtiments sans jamais compromettre l’excellence des soins.”
Implantée au cœur de la Nouvelle-Écosse, EfficiencyOne déploie son expertise pour réduire l’empreinte carbone et maximiser l’efficacité énergétique.
L’hôpital exposera fièrement sa plaque et son certificat dans son hall d’entrée. Ces symboles témoigneront chaque jour de notre engagement envers un avenir plus vert.
John Hann, directeur de l’entretien chez Nova Scotia Health, a fièrement annoncé devant l’assemblée: “Notre établissement surpasse 75 pour cent des bâtiments similaires au pays en efficacité énergétique, comme l’attestent des experts indépendants. Nous nous assurons aussi de respecter les normes de qualité environnementale intérieure.”
Hann a attribué le succès au programme de gestion environnementale du site, géré par Robert Barss, et au partenariat avec EfficiencyOne.
“Vos efforts et vos réalisations m’impressionnent,” a lancé Hann avant de souligner les initiatives d’efficacité énergétique déployées par Nova Scotia Health dans l’ensemble de son réseau.
“Notre programme environnemental a métamorphosé l’hôpital,” souligne-t-il avec fierté. “Chaque année, nous économisons 6 millions de dollars tout en éliminant 34,000 tonnes de gaz à effet de serre — l’équivalent de retirer 7,000 voitures de la circulation. Une modeste initiative qui transforme aujourd’hui Nova Scotia Health.”
Les 220 hôpitaux, centres de santé, cliniques et installations connexes que gère l’organisation font d’elle le plus grand employeur de la province — et un acteur clé dans la responsabilité environnementale. Les hôpitaux consomment des quantités considérables d’énergie, d’eau et de matériaux: c’est pourquoi les initiatives durables sont devenues essentielles.
“L’équipe technique de l’hôpital Fishermen’s Memorial a modernisé ses systèmes d’automatisation: des capteurs intelligents orchestrent désormais le chauffage, la ventilation et la climatisation tout en surveillant l’humidité et le taux de CO2.”
Barss et son équipe d’entretien et d’opérations ont mené une charge environnementale saluée par Troy Routledge, responsable du site. Grâce à leurs engagements verts, ils permettent désormais à l’hôpital d’économiser

LEFT TO RIGHT: Nathaniel Schrader of EfficiencyOne with Robert Barss, John Hann, Tanya Nixon, Troy Routledge, Leslie Oliver and Ruth White Frizzell of Nova Scotia Health.
added. “Our little program has done a lot for Nova Scotia Health, in my opinion.”
As the largest employer in the province, with more than 220 hospitals, health centres, clinics and related facilities, the organization plays a key role in environmental responsibility. Hospitals consume significant amounts of energy, water and materials, making sustainability efforts essential.
“At Fishermen’s Memorial Hospital, the focus on energy improvements took place in areas such as our building automation systems, which manage the programming, scheduling and sensors that detect heating, ventilation, air conditioning, humidity and carbon dioxide.”
Site lead Routledge credited Barss and the maintenance and operations team for leading the environmental charge in helping the hospital save more than $140,000 annually through its green commitments.
“We're protecting both our public health and the environment,” said Routledge. “We are proud to lead by example.”
In line with the mission at Nova Scotia Health — to create healthy communities for generations — the efforts made to earn this recognition also enhances the patient experience and creates better workspaces for healthcare providers.
Self-sufficiency programs are taking shape in major hospital renovations and expansions across the province. At the same time, sites are looking for opportunities to become more environmentally conscious where it makes sense. For example, All Saints Hospital in Springhill has upgraded its laundry facilities, replacing aging washers and dryers with high-efficiency models that support bigger loads, improve workflows and create safer work environments.
Keith Corcoran is a communications advisor for public affairs, content and media relations on the communications and marketing team at Nova Scotia Health.
“NOTRE ÉTABLISSEMENT SURPASSE 75 POUR CENT DES BÂTIMENTS
SIMILAIRES AU PAYS EN EFFICACITÉ ÉNERGÉTIQUE, COMME L’ATTESTENT DES EXPERTS INDÉPENDANTS.”
plus de 140,000 dollars chaque année — un geste concret pour la planète.
“Nous protégeons à la fois notre santé publique et l’environnement,” a déclaré Routledge. “Nous sommes fiers de montrer l’exemple.”
Les professionnels de Nova Scotia Health ont obtenu une reconnaissance prestigieuse. Cet accomplissement s’inscrit naturellement dans leur mission: bâtir des communautés où la santé rayonne de génération en génération. En même temps, ils améliorent l’expérience vécue par chaque patient et créent des lieux de travail plus stimulants pour les soignants — un cercle vertueux qui profite à tous.
Les hôpitaux de la province se transforment pour gagner en autonomie. À Springhill, l’hôpital All Saints montre la voie: sa nouvelle buanderie écologique accueille désormais des machines ultraperformantes. Ces équipements modernes engloutissent des charges plus volumineuses, simplifient le travail du personnel et renforcent leur sécurité. Cette métamorphose illustre une tendance provinciale: partout, les centres hospitaliers conjuguent rénovations majeures et respect de l’environnement.
Keith Corcoran est un conseiller en communications pour les affaires publiques, le contenu et les relations avec les médias au sein de l’équipe des communications et du marketing de Santé Nouvelle-Écosse.



























A COLLABORATIVE SUCCESS
Emergency public health relocation in Alberta demonstrates what empowered teams can accomplish under pressure
By Sabrina McCormack & Tim Holliday

In late April 2025, tenants in the Grande Prairie Provincial Building (GPPB) were evacuated due to air quality concerns. As a tenant in the building, Alberta Health Services (AHS) encountered the challenging task of relocating vital public health services without delay. The initial timeline for displacement was estimated to be six weeks to six months to allow for repairs to air systems.
Amidst the backdrop of the province’s intensifying wildfire season and a concurrent measles outbreak, the relocation was more than a logistical hurdle — it became a true test of system-wide agility, innovation and teamwork.
The Queen Elizabeth II (QEII)
Ambulatory Care Centre was a natural choice for relocation due to its available space and strategic role in the zone’s healthcare system. Since the opening of Grande Prairie Regional Hospital (GPRH) in 2021, the acute care programs previously housed at QEII were transferred to the new facility. As a result, several former inpatient units at QEII were unoccupied and well-suited for rapid conversion into clinic and office space. Its central location, existing infrastructure and proximity to other AHS services made it an ideal site to support the urgent needs of the public health team during the relocation.
INCIDENT COMMAND ACTIVATION
To coordinate the emergency response, an incident command structure (ICS) was activated. This collaborative structure was essential in executing swift and informed decision-making. Within hours of the evacuation notice, plans were underway to re-establish public health services at QEII. The logistics branch, led by capital management, brought together a variety of departments, including space management, property management, facility maintenance and engineering (FM&E), information technology (IT), protective services, contracting procurement and supply management, and environmental services.



CREATIVITY UNDER PRESSURE
When the GPPB was evacuated, teams walked away from nearly all operational tools — medical equipment, supplies, IT devices and even basic furnishings were left behind. With limited time and resources, the logistics branch employed a creative reuse and redeployment strategy. In total, some 3,000 square metres of space were prepared and repurposed to support the rapid deployment of public health services, including clinical rooms, support areas and dedicated vaccine storage. This was accomplished without the allocation of emergency or project-specific funding; all minor renovations, equipment deployments and procurement activities were managed through existing operational budgets, highlighting the resourcefulness and fiscal discipline of the teams involved.
FM&E played a foundational role in preparing QEII spaces for safe and functional occupancy. Their efforts began with essential infrastructure readiness, including patching and painting walls, repairing existing millwork and ensuring all ceiling tiles were in place and compliant. FM&E also addressed non-compliant fixtures, such as removing water fountains and hoppers that did not meet current infection prevention and control (IPC) standards. Following renovations, a construction clean was completed before furniture and equipment was deployed. In addition, FM&E ensured HVAC and building temperatures were adjusted to reflect the increased activity in areas that had previously been dormant, helping to maintain comfort and environmental standards for both staff and clients. Their attention to both clinical function and facility compliance was key to transforming unoccupied space into a fully operational public health environment.
A post-pandemic warehouse provided a key source of furniture and equipment that the logistics branch could draw from. Space management collected department needs and picked suitable furniture and accessories to fit-out clinical and staff spaces. As deliveries arrived at QEII, all items were routed to a central staging area, where they were thoroughly wiped down and inspected prior to deployment. A staging and cleaning system was established to support the safe and efficient outfitting of clinic spaces. Fortunately, the local team had experience with this type of setup,
TOP: Public Health waiting room setup in the elevator lobby. MIDDLE: Laboratorygrade fridges and packing station in the newly established vaccine depot at Queen Elizabeth II Ambulatory Care Centre, supporting cold chain management and distribution to 29 regional sites. BOTTOM: Former quad-patient room converted into a shared workspace.
having executed a similar process during the GPRH move four years earlier — a logistical advantage that helped accelerate setup under tight timelines.
To ensure continuity of care, medical equipment was strategically borrowed from other capital and minor projects across the province. Through existing partnerships and procurement channels, essential items like laboratory-grade vaccine fridges, adult weigh scales and vital signs monitors were redeployed to support the rapid setup of the new clinics and vaccine depot. This approach not only avoided procurement delays but also highlighted the strength of site collaboration and system-wide resource sharing, a key factor in enabling safe, functional care environments within days of the evacuation.
IT played a critical role in enabling clinical operations at the relocated site. The QEII, a 40-year-old facility, lacked data drops in many of the former inpatient rooms, which is a common limitation in legacy infrastructure not originally designed for modern digital workflows. However, the site had recently been upgraded with robust Wi-Fi capabilities during the Connect Care roll out, allowing IT to quickly mobilize Wi-Fi-enabled desktop computers or laptops. Where network cabling for Voice over Internet Protocol (VoIP) connectivity wasn’t possible, the team deployed creative communications workarounds. This included equipment to provide 10 megabits per second power over Ethernet network across older single-pair Cat3 cabling, as well as analog to VoIP adapters. IT also routed incoming calls across the wide area network to the new locations.
To maintain cold chain integrity of vaccines during the transition, a temperature monitored, refrigerated truck was first mobilized and parked directly at the QEII site. This allowed vaccine controllers easy access to support not only the newly relocated clinics but also the 29 sites regularly served by the Grande Prairie vaccine depot. The refrigerated truck remained in use for one week until a fully functional depot was re-established. At that point, 13 mobile laboratory-grade vaccine fridges were delivered and installed in the former pharmacy department. Fridge temperatures were maintained and verified through temperature logs and remote monitoring. While Sensaphones could not
Day 1
Day 3
Day 7
Day 8
Day 14
Day 21
Day 35
RELOCATION TIMELINE
• Evacuation from Grande Prairie Provincial Building initiated
• Incident command structure activated
• Queen Elizabeth II (QEII) Ambulatory Care Centre selected
• First laboratory-grade fridges arrive at QEII
• New vaccine depot begins operational commissioning
• Refrigeration truck with vaccines arrives at QEII and stays on-site until coldchain protocol is established
• Thirteen bay immunization clinics open at QEII auditorium
• Environmental Public Health water drop-off location opens at QEII
• Vaccine depot is officially setup
• Refrigeration truck is released
• Fifteen public health clinic rooms and support spaces open
• Twenty-five additional rooms open
• Staff and clients welcomed from programs, such as chronic disease management, environmental public health, health promotion and Indigenous health
be deployed within the compressed timeline, alternative monitoring was implemented to maintain vaccine safety through the building management system (BMS).
Since the vaccine depot was on a separate floor than public health clinics, a dedicated vaccine storage room was created in a former four-bed inpatient room close to the clinic spaces. The vaccine storage room provides staff with convenient access to vaccines during their shifts. The fridges in this room were connected to existing emergency power and integrated into the BMS for ongoing temperature monitoring.
Prior to occupancy, air and water quality testing was conducted by Workplace Health and Safety and Environmental Public Health, respectively. As the space had been unoccupied for an extended period, it was essential to verify the environment was suitable for staff and clients. Results returned within normal ranges, indicating established preventive maintenance and environmental procedures performed by FM&E had effectively maintained the integrity of the unoccupied space.
Protective services (PS) provided support throughout the relocation process, ensuring both safety and access control during the transition. The PS team coordinated card access for doors, elevators and restricted areas to accommodate the new workflows and staff groupings for more than 100 staff. As many staff were new to the QEII site, PS also conducted site orientations, helping to familiarize individuals with revised travel paths, entry points and emergency procedures. With significantly increased foot
traffic from both staff and clients, PS ensured a safe environment as workflows adapted and unfamiliar areas of the building became active once again. Their involvement helped maintain order and reassurance during a time of rapid change. IPC and CSA standards were followed as closely as possible throughout the relocation and setup process. Given the urgency of establishing functional clinical space within days, a risk-informed approach was taken, with exemptions carefully documented by a multidisciplinary team. For example, existing sink and counter was accepted to be used as a hand hygiene sink in clinic rooms, even though fixtures did not meet current IPC facility design requirements. Additionally, carpet still existed in a few areas on the former inpatient unit. These rooms were closed off with doors, secured and signage clearly posted, as time and resources did not permit full removal of the carpet prior to occupancy. These exceptions were evaluated and approved through the multidisciplinary team.
Sabrina McCormack is a clinical liaison at Alberta Health Services (AHS). Tim Holliday is executive director of capital management, north zone, at AHS.
At time of article submission, only personal belongings and vaccines had been retrieved from the Grande Prairie Provincial Building (GPPB). Operational assets, such as medical equipment, furniture, IT equipment and clinical supplies had not yet been retrieved. Current projections indicate the public health departments will be displaced from the GPPB for one year.
REASONS
TO MONITOR YOUR INDOOR AIR QUALITY
According to the World Green Building Council, we spend 90 percent of our time indoors. Given that statistic, it’s clear the quality of the air we breathe in buildings can dramatically impact our health and well-being. At Reliable Controls we believe sustainable buildings are a key component to reducing the health and environmental impacts of indoor and outdoor air pollution.
Improve comfort and productivity.
Volatile organic compounds (VOCs) form a large group of chemicals commonly found in indoor air. According to Health Canada, exposures to VOCs may affect your health, depending on which VOCs are present, the levels present, and how long you're exposed.
In addition, while you can’t yet monitor the presence of a virus like COVID-19 in the air, you can measure a number of factors that affect the risk of viral transmission: temperature, humidity, and CO2. These air-quality measures are also linked to workplace well-being and productivity, so the better the air in your building, the better your occupants are likely to feel—and perform.
1 2 3 Spot problems.
Save energy.
Excessive ventilation wastes energy. Ideally, a building’s ventilation system provides just the right amount of air. Many ventilation systems, especially older ones, are based on constant air volume, which means they always operate at full capacity. By converting to a variable air volume system, you can optimize your energy efficiency with demand-controlled ventilation. Studies show that a ventilation upgrade from constant air volume to variable air volume can achieve annual energy savings of 10 to 21 percent. Beyond that, with air-quality sensors, you have access to real-time data that informs when and where to efficiently deploy air filtration and temperature control.
Identify trends.
Integrating IAQ sensing technology into your building automation system means you can collect building data that helps you perform preventative maintenance and avoid system failures. By tracking pollutant levels continuously over time, for example, you can easily identify where and when to address changes in air-quality parameters. Long-term trends are almost impossible to detect with periodic spot sampling, which provides only a snapshot of data points at a particular time.
4
Most people know IAQ sensors can warn building managers about safety issues like smoke or carbon monoxide. Did you know they can also tell you how much particulate matter is in the air? Or how many harmful volatile organic compounds are circulating in your space? IAQ data can help you determine where to focus cleaning, when to service equipment, when to change filters, and when to increase or decrease ventilation.
5
Earn building certifications.
IAQ monitoring is essential to achieving healthy building certifications like LEED and WELL. Around the world, certification programs set minimum IAQ standards to protect occupant well-being, preserve ventilation system performance, and uphold comfort in both mechanically and naturally ventilated spaces


You can depend on Canadian-made technologies from Reliable Controls to easily monitor the indoor air quality in your facilities. Learn more reliablecontrols.com/IAQ
CLOSING THE
AS-BUILT GAP
Etobicoke General Hospital adopts web-based living maps to manage space, critical equipment
By Andy Santoro

Accurate, up-to-date drawings and data are an essential requirement in managing day-to-day maintenance and crises in a healthcare facility. With major construction and renovations often occurring at the same time, this requirement becomes even more essential, difficult and costly to achieve.
Facility infrastructure information is usually spread over various drawings and spreadsheets created and modified during renovations and expansions over the lifetime of a facility. Locating critical infrastructure assets can be challenging when most facilities, especially older ones, use aged construction drawings for reference. This can be risky and onerous at best.
At Etobicoke General Hospital, plans
were underway for expansion of the facility involving major changes to the electrical, HVAC and water distribution system. Contractors and staff worked together to gather information on the locations and connections to and from all major maintainable electrical equipment.
Using this data, the hospital, together with Canadian facility engineering and software developer Sansys Inc., created an accurate electrical single-line diagram and water distribution riser along with a database that provided critical attributes and locations for all equipment shown on the diagrams. This was done using conventional programs like AutoCAD and Microsoft Excel.
Because of the numerous infrastructure changes continually taking place, an easier
and more flexible solution was needed to ensure the information’s accuracy. With input from the hospital, Sansys developed a new application, EMMA (electrical/mechanical mapping application). EMMA consolidates all of that information into a single database through a web interface that can be easily viewed, queried and updated. All relevant data, including building/level, type of equipment, condition, system and how the equipment is interconnected, was made available to authorized staff.
This system transforms hard and soft copy drawings and data into a combination of living documents. The main features include cloud-based architecture for access anywhere, anytime; simple browser interface for staff without third-party software; controlled access for staff and contractors, limited to view-only
In this case, you search for equipment, what it connects to and from, and the detail information of the equipment all on one screen. All tags are active and navigation to the equipment location in the main riser is enabled through menus when equipment is selected.
t
or edit; links between equipment location on floor plans and connection on the riser; automatic tracking of who, when and what was changed; ability for staff to edit equipment information and locations quickly and easily from the browser interface through drag and drop; editable panel schedule forms tied into the database to keep branch circuits up-todate; ability to upload notes, images and files for each piece of equipment; output shutdown reports in Excel indicating interconnected equipment affected down to the circuit level; and mobile (phone or tablet) capability to make real-time modifications to the system.
The hospital put the system to use as soon as it was online and immediately began to realize the value generated from these features.
“Our staff uses EMMA almost on a daily basis,” says Scott Payne, facilities coordinator at Etobicoke General Hospital and EMMA administrator. “Our panel schedules can be updated on-site with a tablet and whenever any modifications are made in EMMA, the system logs what was changed, who made the changes and when. I can pull up a report in Excel that provides the change history for a specific piece of equipment or a report for all changes to all equipment based on a date range. Having our panel schedule circuit listing accurate and up-to-date really helps when we have to troubleshoot and find capacity and spare circuits for lighting, receptacles or new equipment.”
Outside contractors who provide maintenance work and troubleshooting also use the system.
“By giving them view-only access, they can find specific equipment on their own,” says Payne. “They really don’t need to rely on help from our staff as much. That’s a good thing.”
SHUTDOWN MANAGEMENT AND PLANNING
As part of the early works project for the large expansion, the hospital installed four new chillers, one new boiler and added a new incoming service transformer. Major shutdowns were required to remove old cooling equipment and to tie in the new transformers. EMMA provided all connection relationships between the equipment and loads served by each. The isolation report option generates a complete report of all equipment affected by the isolated equipment, including connections, locations and service summary, right down to the panel schedule circuit descriptions.

With all equipment located, it was easy to identify alternate power sources when required. The hospital was able to manage risk by running multiple what-if scenarios.
“We estimated it saved us resources and time in the order of 60 per cent of a 300 manhour involvement,” says Payne. “Without EMMA, we need to dedicate staff to investigate all implications of isolating a piece of distribution equipment. We are also able to log notes, pictures and attachments for each equipment item. This saves us time and resources when future shutdowns involve the same equipment. Also, in the event of an unplanned equipment failure, we can act quickly to understand the implications of the crisis, notify all staff and stakeholders affected, and determine the best option to quickly manage risk to patients and staff and mitigate damage.
Using the same principle, the hospital has now implemented EMMA for medical gas distribution, domestic water, storm and sanitary drainage, HVAC, fire suppression, nurse call and site services.
“Since the application protocol is the same for the various systems, we use shutdown management for all systems, especially to isolate leaks without shutting down main water risers,” says Payne.
SPACE MANAGEMENT
The hospital has also implemented EMMA for space management and associated assets.
A dynamic tag is created for each room. Searchable attributes for each space include but are not limited to department, room type, square footage and status (used, vacant or under construction). A simple click generates filtered search results to show rooms graphically on the floor plan or tabular Excel spreadsheets. This provides staff the ability to find new space for staff and better understand the implications of change to space usage.
FLOOR PLAN NAVIGATION ENHANCEMENTS
Working with the hospital, the area type feature was developed to help staff better understand the vertical implications in the building. Areas that are drawn on the floor plans are automatically shown on all levels above and below.
“We had to route a dryer exhaust shaft up through four levels,” says Payne. “It helps when you can see a footprint on every level and know the implications.”
This allows staff to quickly assess implications from water leaks, floor drilling, and infection prevention and control, among other issues.
By making it easy for staff to modify and update, accurate information is kept current during all changes and renovations to the facility. This is the essential foundation in creating living maps to better manage space and the facility infrastructure that supports it.
Sansys is now in the process of implementing AI capabilities that allow users to query data and receive actionable answers, relevant options and intelligent solutions.
Andy Santoro, P.Eng, is president of Sansys Inc., which provides unique, customized cloud-based solutions for healthcare construction and facility management. With the help of the company’s healthcare clients, EMMA (electrical/mechanical mapping application) was created to address the need for accurate facility infrastructure records that would allow staff to understand mission critical components within their facility. Andy can be reached at 519-852-4705 or santoro@sansys.com.
Impact of isolating transfer switch ATS-15. t
THE PATH TO DIGNITY AND RESPECT
Washroom upgrade supports IWK Health’s commitment to accessibility
By Jaime Blenus & Jeff Harding

Located in Halifax, IWK Health serves as a crucial women’s and children’s hospital and children’s trauma centre, offering essential care to families across the Maritimes and beyond. With the passing of the Accessibility Act in 2017, the organization is actively working to improve accessibility to meet Nova Scotia’s mandate to create a barrier-free province by the turn of the decade. Recent facility enhancements include the introduction of two fully accessible washrooms on the main floor, designed to promote dignity for all users.
A BASIC HUMAN RIGHT
Barrier-free access to washrooms transcends mere convenience; it is a fundamental human right that upholds individual dignity. The ability to use a washroom independently, without needing to seek permission, is vital for maintaining self-respect and autonomy.
The new accessible washrooms incorporate many features, including user-friendly gantry systems; bariatric change tables; angled mirrors and paddle taps; colours conducive for the visually impaired; accessibility in design; safety measures and emergency controls; and infection prevention and control (IPAC) considerations. A back support for the toilet is to be installed in accordance with CSA standards once the equipment comes in.
The addition of two washrooms reduces waiting times for users and provides redundancy in case one is out of service.
The bariatric gantry lift systems operate without locks, ensuring no key is needed for access. They charge continuously, preventing battery depletion regardless of their position.
Full-sized bariatric change tables maximize capacity while minimizing pinch hazard risk associated with height adjustments.
Both the bariatric gantry lift systems and change tables facilitate seamless transfers for individuals with mobility challenges. They are regularly inspected and maintained by staff to ensure safe operation.
Mirrors are designed for use from a sitting position and paddle taps ensure warm water is readily available for handwashing and cleanup.
Wall and flooring colours provide visual contrast, delineating the usable space, and enhance usability for individuals with vision impairments. For instance, the contrast between wall and fixtures enables a person with reduced vision to identify locations of fixtures more readily.
The lock system utilizes swipe/button activation to eliminate the need for gripping and twisting, making it easier for users with limited hand mobility.
Insulation prevents pipes burning a seated user who may not sense the heat.
An emergency call button alerts protection services while unlocking the door without triggering a door opener, ensuring quick access in emergencies. Protection services officers are trained in the operation of the gantry lift, including primary and secondary override features, in case of failure.
Surfaces are designed for easy cleaning with approved wipes, ensuring compliance with IPAC standards. The flush levers are strategically positioned to prevent reaching across the bowl.
COLLABORATIVE APPROACH TO DESIGN
IWK Health prioritizes accessibility from the very beginning of every project. Each initiative undergoes a thorough review by the accessibility action group — a multi-disciplinary team that includes members with lived experience and those holding Rick Hansen Foundation accessibility certification. This group not only ensures accessibility standards are met but also conducts on-site evaluations of completed projects, identifying opportunities for future enhancements.
The development of the newly accessible washrooms exemplifies this collaborative approach. Input from the accessibility action group, along with contributions from occupational therapy and in partnership with the Atlantic Provinces Special Education Authority, fostered an atmosphere of curiosity and continuous learning. Effective design requires diverse perspectives; no single individual possesses all the insights necessary for creating truly inclusive spaces.
This project’s impact goes beyond just improving physical accessibility. It has ignited ongoing conversations about disability, inclusion and accessibility within the organization. These discussions are influencing hiring practices and inspiring dialogue about future opportunities to enhance accessibility across all operational practices. The tangible changes made at IWK Health are sparking broader discussions about universal design, challenging the centre to envision new possibilities for accessibility in the facility.
Jaime Blenus is the accessibility health consultant, equity and belonging, at IWK Health Centre. Jeff Harding, P.Eng., is the manager of redevelopment space and leasing services. Jaime and Jeff can be reached at jaime.blenus@iwk.nshealth.ca and jeff.harding@iwk.nshealth.ca, respectively.
Recognize yourself, your department and your staff during Healthcare Engineering Week. Make sure everybody knows the vital role played by CHES members in maintaining a safe, secure and functioning environment for your institution.
*2025 Challenge*
CHES members are challenged to celebrate NHFEW by creating a short video and posting it on LinkedIn or X (formerly Twitter) using #NHFEW. CHES will then like and share it on Linkedln (@CHES National Office) and X (@CHES_SCISS).



















IHigh Performance Modular Construction:











A ROBUST SOLUTION FOR HEALTHCARE
n June 2024, Brockville General Hospital became the first hospital in Ontario to expand their diagnostic imaging department by using modular construction to add a new Siemens MRI. By doing so, the wait time for MRIs at the hospital was reduced by a year and a half.
The timeline for the Brockville project using traditional construction methods was at first anticipated to take two and a half years to complete. SDI Canada was able to deliver the prefabricated Cassette® modules within a year. Given that in one year, approximately 5,000 MRI scans can be completed, this means that just as many patients received care one year earlier than expected.
THE CASSETTE SOLUTION

In Ontario, SDI Canada has worked with five hospitals to date who have chosen modular construction as an alternative to traditional construction. The Cassette solution o ered by SDI is designed to complement traditional infrastructure. Instead of being constructed onsite, the modules are built in a controlled, factory environment, and then transported to their location ready to be set in place and integrated with the existing architecture.
Prefabricated hospital rooms are built from steel and come fully equipped with plumbing, electrical, HVAC, and the essential connections needed for medical gases. Building o -site reduces the inconvenience and noise pollution of building on location. The practice became more widely familiar during the pandemic, when the need to quickly expand medical facilities was highlighted.
The adaptability of modular construction is increasingly being seen as a solution for healthcare facilities across Canada. Winnipeg’s Health Sciences Centre was the first in Canada to introduce SDI Canada’s Prefabricated Modular MRI Cassette® in 2023. Brockville General Hospital’s modular MRI department was constructed in 2024. Since then, the company has worked with Kemptville District Hospital to build a new GE Computed Tomography (CT) scanner and is currently installing Ontario’s third Prefabricated Modular MRI Cassette® at Headwaters Health Care Centre in Orangeville.
The Cassette is a hospital-grade building, fully compliant with the Canadian Building Code, CWB Certified (CSA A660-10 & CSA W47.1), with ‘Site Rating Classification’ for seismic design and ULc Listed components & design. These are fully finished, ready to use buildings designed with ergonomics and workflow in mind.
“This solution is very robust,” explains Toufic Abiad, Founder and CEO at SDI Canada, who says that cost predictability is another advantage when building modular. “But it doesn’t matter if it’s less expensive or even a little more depending on the scenario — it’s much faster. How do you put a price on that?”
PRIORITIZING PATIENT CARE
“A patient’s priority is to get the MRI scan as soon as possible,” Abiad states. “I have a solution that will get this to them early.”
Location barriers are also no issue for modular construction, he says. For facilities in remote areas, high performance medical construction for MRIs and CT scans is expensive to build due to the specialist trades required; trades which may be hard to find in remote regions.
“It’s about e ciency. We build the module and send it to you,” says Abiad, who asserts that building in factories speeds up patient care and reduces backlogs in surrounding facilities.
“We construct it in pieces and put it together to form a full facility without any compromise on quality, or patient care and experience.”
Although SDI o ers di erent dimensions and layouts for di ering clinical requirements, each standard prefabricated Cassette® is between 15 and 16 feet wide and 60 feet long and constructed within a factory in a temperature-controlled environment, making for better conditions and work-life balance for those building them.
“The construction worker who was on a three-month rotation waking up at 4 a.m. to go to the jobsite two hours away, now goes to an air-conditioned building and spends more time with his family,” notes Abiad.
THE “INNOVATION OF WAYS”
Building within a controlled environment ensures speed of production and elevated consistency in the finished product. Abiad describes the “innovation of ways” which keep SDI propelled forward.
“We can deliver a healthcare department in a year. It’s not because we’re smarter than anybody else; technology is helping us. We just have the courage to endorse it.”
SDI Canada takes a collaborative approach with architects and engineers when extending a hospital’s footprint. Each steel modular cassette is between 800 and 900 square feet and is linked together like pieces of Lego to form extensions of current infrastructure.
Rather than completing inspection on a job site, architects and engineers inspect the construction at the factory, assessing the work at three stages: the onset, while being built, and then the finished product.









While SDI o ers both traditional and modular building, Abiad sees the potential growth and resilience of prefabricated hospital departments as worth exploring.
“Within a year we built six departments across Canada in five di erent provinces. This system can only help the Ministry of Health to deploy faster care to patients.”
SDI has recently also secured contracts with the Sioux Lookout, and the Royal Victoria Regional Health Centre in Barrie. Across Canada, Abiad says Ontario is a leader in adopting modular cassette technology, closely followed by British Columbia.
“We’re at our second system in BC. We started with Richmond, and now we’re working on Squamish.”
As an entrepreneur, Toufic Abiad sees modular construction as a way of breaking the mold. He identifies further potential value in reusing MRI machinery in smaller communities once a machine ages.
“Down the line, maybe the MRI can’t keep up with 5,000 scans a year in Brockville, but it could do 2,000 scans a year in a smaller town,” Abiad suggests. “That MRI module can be brought to a community hospital that doesn’t already have a magnet.”
When it comes to innovation, Abiad encourages us all to be entrepreneurs: “Stop talking about the future. Be part of it,” he suggests.
Founded in 2003, SDI Canada is the Canadian leader in the implementation of MRI and biomedical equipment, the design and construction of medical infrastructures and the distribution of specialized accessories. To learn more, visit www.sdicanada.ca or email info@sdicanada.ca
GENERATING REAL-TIME KNOWLEDGE
Integration of computer vision-based AI improves workflows
By Matthew Kjin

Within every healthcare facility, balancing safety and the patient experience is an ongoing initiative. Computer vision technology is being asked to do more to generate not only forensic data but real-time events, enabling relevant parties to make data-driven decisions for those responsible for safety and the patient experience.
In this regard, surveillance systems integrated with computer vision artificial intelligence (AI) can revolutionize how healthcare providers optimize all workflows. By leveraging these technologies, organizations can assume a more proactive approach, resulting in improved care, faster recoveries, quicker service administration and happier patient populations. With its ability to sift through vast amounts of data swiftly and accurately, AI empowers healthcare
providers to forecast, anticipate and prepare for potential medical events before they happen, ensuring urgent interference or ready action as needed.
THE POWER OF ANALYTICS
Predictive analytics, a form of data analytics, is focused on using data, whether it be historical or real-time, to make forecasts or anticipate future outcomes. In the context of surveillance in healthcare facilities, data can come from various sources, such as patient records (medical history or care instructions), live and recorded video feeds, and various environmental sensors in the facility (motion, temperature or sound). Information from these sources is aggregated with the use of AI, helping surveillance systems determine risks or potential
sensitivities that need to be carefully monitored for patients.
Enhancing patient safety and preventing falls in healthcare settings is made possible through the integration of AI-powered surveillance systems, real-time monitoring and advanced analytics. Cameras detect unusual movements, such as attempts to get out of bed unassisted, while machine learning models analyze historical and live data to identify high-risk behaviours like instability or leaning over bed rails. These systems seamlessly combine sensor inputs with patient monitoring platforms to issue immediate alerts and provide audio redirections, such as “Please wait for assistance.” By analyzing video feeds alongside electronic health records (EHR), facilities can identify patterns like falls associated
with the patients’ course of care. This proactive approach ensures timely staff interventions, reducing fall incidents and improving patient care.
Advanced surveillance systems enhance behavioural monitoring and emergency detection in healthcare facilities by analyzing expressions, postures and movement patterns to identify signs of agitation or aggression. Historical data is reviewed to refine predictive models, ensuring greater accuracy in identifying early warning signs of crises. These systems integrate behavioural data with patient monitoring platforms, triggering immediate notifications to nearby personnel for prompt intervention and de-escalation. Multi-camera views further enable tracking of patient movements and mapping of high-risk areas within the facility. This proactive approach empowers staff to intervene before situations escalate, reducing harm and enhancing overall care.
TRAINING AND INTEGRATION
Implementing surveillance systems in healthcare facilities requires careful attention to technological and operational considerations to ensure effectiveness and compliance. Data integration is a key challenge, as information often resides in silos across EHRs, monitoring devices and surveillance systems. Merging these data sources, such as combining video surveillance feeds with patient records, equipment utilization data and Internet of Things sensor readings, is essential for a comprehensive view. This process also involves cleaning and normalizing data to ensure it is standardized for analysis.
Privacy and security are paramount, requiring strict adherence to a combination of federal and provincial laws that govern the protection of personal health information along with the use of encryption and anonymization for data storage and transmission. Proper training and deployment are also critical; staff must be trained to interpret computer vision-based alerts, and systems should be piloted in controlled settings to refine algorithms before full implementation. The most successful programs often route relevant alerts through existing systems within the hospital, such as the emergency medical responder, nurse call and other various forms of unified communication plat-

tEnhancing patient safety and preventing falls in healthcare settings is made possible through the integration of artificial intelligence-powered surveillance systems, real-time monitoring and advanced analytics.
forms. The flatter the alert topology, the better.
HONOURING PATIENT PRIVACY
Integrating patient context with computer vision offers significant advantages like improved service readiness and personalized care in healthcare facilities. However, patient health information is highly sensitive and most individuals prioritize its confidentiality. As a result, sharing such data with personnel beyond immediate caregivers may lead to discomfort and concerns about privacy.
Given this, healthcare facilities must implement strict measures to ensure patient data is handled with the utmost care and confidentiality. Before utilizing sensors, smart surveillance or predictive analytics for patient monitoring, it is essential to obtain informed consent. This consent should clearly outline what devices will be used, how the data will be
stored and its intended purpose. Most systems choose to only use live video and to opt out of retaining video. These steps not only reassure patients about their privacy but also safeguard the organization against potential legal liabilities.
Beyond gaining patient consent, healthcare facilities must also take proactive measures to prevent unauthorized access or misuse. Selecting surveillance solution providers requires careful evaluation to ensure they have robust cybersecurity measures in place. Trusted providers go beyond the initial sale, offering comprehensive support throughout the system’s life cycle, from installation to decommissioning. These providers implement end-to-end encryption to protect data during transmission and remain vigilant against cyber threats, issuing timely patches and updates to address vulnerabilities. Such measures reinforce the facility’s commitment to data security and patient privacy.
Matthew Kjin is the segment development manager for healthcare with Axis Communications. Matthew is a security and healthcare technologist with more than 14 years of experience in healthcare services and life safety interlacements. He is an established thought leader in the healthcare segment for his expertise in solutions for improving the patient experience and overall safety of the enterprise.









MEETING CSA Z317.1:21 PLUMBING STANDARDS FOR HEALTHCARE FACILITIES
To protect both the occupants and surroundings in healthcare settings, the design, construction and operation of plumbing systems must meet specific criteria as identified by the Canadian Standards Association (CSA). Precision, safety and compliance are non-negotiable factors to protect against infectious diseases, imbalances in temperature, and catastrophic plumbing failures in healthcare orientated environments.
The CSA Z317.1:21 standard outlines critical requirements — especially in areas like hot water management and fixture design — to ensure safety and functionality in patient care spaces. Below, we look at various clauses within the Standard for healthcare plumbing components and some of the specially engineered products designed to meet the code.
Section 6.3.3.2 — Safe, stable hot-water delivery
Patient safety begins with consistent water temperatures, and fluctuating hot water creates a serious risk of burns and scalds in care settings. Additionally, insufficient water temperatures can create conditions which encourage bacteria such as Legionella to prosper, leading to a potential risk of Legionnaire’s Disease. Lawler’s custom-built mixing valve piping systems are
engineered for CSA compliance. With real-world reliability, Lawler turns a code requirement into a plug-and-play riskmitigation package featuring:
• Precise ±1 °C control across the full demand curve
• Factory-skidded, pre-tested manifolds sized for any wing or entire facility
• Integrated digital monitoring & failsafe shut-off that satisfies the continuous-temperature-monitoring language of 6.3.3.2
Section 8 — Fixtures & fittings for hygiene, flow control and maintainability
CSA Z317.1:21 Section 8 outlines the specific requirements for plumbing fixtures and fittings in healthcare facilities. Focused on hygiene, safety, and performance, these standards are essential for engineers designing compliant and future-ready systems.
8.3 – Hands-Free Operation: Minimize touchpoints and Maximize safety
Sensor-operated faucets enhance hygiene control by reducing the spread of germs through touchless operation. They also reduce risk of cross-contamination on surfaces, and conserve water by enabling automatic faucet turn-off and water flow optimization.

• 2” inlets and outlet
• Stainless Steel Construction
• ASSE 1017 and NSF 372 (lead free) listed

Neptune EMX 200 MS Electronic Mixing System Eng. No. 943640

Chicago Faucets offers a full range of sensor-operated faucets designed for infection control and are distributed exclusively in Canada through Dobbin Sales. Model H-G61K75ABCPT boasts the following features:
Maximum operating pressure: 150 psi
• Controls water temperature to +/- 2°F when properly installed in a continuous recirculation system


• Angled front corners for user safety
• Factory pre-plumbed configuration for efficient installation
• Programmable high temperature alarm function
• Programmable set point range between 95°F to 180°F (Default set temperature 120°F)
• Emergency Backup Power System (EBPS) to maintain operation during outages
Low Load algorithm keeps temperature steady in low demand periods
• Pair with Sloan Optima hands-free faucets for a complete hygienic package
• Control box supplied with 4 ft. 120 VAC power cord and NEMA 4 enclosure
• Modbus communication standard
• Easy integration into BMS system
• Built-in laminar flow control at the spout base
• Operating Voltage: 24 VDC
8.8 – Emergency Eyewash Stations
• Fails “last position” during power failure
Automatic Hot/Cold water shutoff upon cold/hot water inlet supply failure
• Programmable settings for hygiene flush and applicationspecific modes
• Recommended recirculation pipe size: 1-1/4” or greater System includes recirculation pump, circuit setting balancing valve, thermometers, ball valves, check valves, mounting strut and test connection
• Simple user commissioning and setup
Displays outlet temperature
• Removeable and serviceable thermocouple probe
• This product is Ideal for hand hygiene stations and patient zones
• ASSE 1070 Scald Protection
8.5
Factory Assembled and Tested
• Minimum hot water supply temperature: 2°F (1°C) above set point with equal incoming pressures
– Tempered Water at the Point of Use
Water delivered to fixtures in patient zones must not exceed 43°C (or 38°C in certain applications) to prevent scalding. According to the Canadian Safety Council, water at a temperature of 60°C can cause third-degree burns in most adults in just six seconds, highlighting the importance of acceptable water temperature for patient use. Chicago Faucets offers point-of-use thermostatic mixing and faucet-integrated TMV options to maintain safe temperatures even during system fluctuations.
8.6
– Flow Control
Maintaining effective hand hygiene while conserving water is a key balance.
Chicago’s sensor faucets include adjustable, field-serviceable flow control components to meet 1.9 L/min requirements without sacrificing usability.
8.7 – Sink Design for Hygiene and Durability
Splashing from sinks and drain can spread the risk of accidental pathogen exposure. Healthcare facilities must select sinks which resist corrosion, minimize splash, and be easy to maintain. Sloan’s EHS-1000 Stainless Steel Sink meets these requirements with:
• 14-gauge Type 304 stainless steel construction
• Raised outer rim to prevent water from dripping onto floors

The first 15 seconds following exposure to a hazardous substance are crucial. Especially when the exposure is to a corrosive product, delaying treatment can exacerbate an injury. Emergency showers and eyewash stations offer immediate decontamination, enabling workers to quickly rinse off harmful substances that could cause significant damage. Facilities must provide accessible, immediate-use eyewashes in appropriate locations.
Guardian Safety Equipment offers a full line of eyewash stations that meet a range of applications, featuring:
• Wall-mounted, recessed, countertop, and pedestal models
• Stainless steel or plastic heads
• Manual, foot, or combination-activated options
NO. 943640-A
• Models available with alarms, tempering valves, and ADAcompliant features
Model GBF1735DP from Guardian is a product highly recommended by Dobbin Sales. This model includes a polished, stainless finish which is easy to clean and resistant to contaminants, and a fast-draining design.
Dobbin Sales represent industry-leading manufacturers who deliver solutions that meet the demands of healthcare facilities in ensuring compliance with CSA-Z317.1:21.
READY TO SIMPLIFY COMPLIANCE?
Speak with the Dobbin Sales Team for CSA-Z317.1:21
specification guides, project selection and further details.
1-800-565-8515
info@dobbinsales.com www.dobbinsales.com
Lawler, Chicago Faucets, Guardian and Sloan products are distributed exclusively in Canada by Dobbin Sales.


TRANSFORMATIVE POWER
Artificial intelligence and the future of healthcare systems, spaces
By Dan Chuparkoff

Artificial Intelligence (AI) is creating new possibilities in nearly every industry, but few domains stand to benefit from it more than healthcare. From hospital design to patient care, AI-driven tools are reshaping how people think about space utilization, safety collaboration and operational efficiency. When emerging AI technologies in healthcare facilities are considered, a radical transformation is imagined — one that will optimize patient flow, reduce repetitive workloads, improve communication and empower human expertise. However, understanding the practical aspects of AI in healthcare settings requires a few myths to be dispelled and specifics to be laid.
THE ‘AMBIGUOUS ROBOT’ MYTH
One of the biggest challenges in discussing AI is the popular but misleading image of a humanoid robot who is thinking colourful thoughts and standing in a room with levers and switches so it can control the world. In reality, AI is not a mystical intelligence that magically solves every problem; it is a spectrum of software tools designed to recognize patterns or generate new content under human guidance.
AI adoption will be more successful when the focus is on specific, problem-oriented AI applications, rather than speaking of AI in sweeping, general terms. Using more precise language helps professionals to align on exactly what a tool is designed to do. Whether it’s analyzing wait times in an emergency room or simulating a new layout for a patient intake area, specifying the type of AI ensures the conversation remains grounded in practical, actionable outcomes.
AI HYPE CYCLE AND ITS REAL IMPACT
All emerging technologies move through a ‘hype cycle,’ with inflated expectations. AI is no exception, but recent breakthroughs in computing power and growth in training data have genuinely vaulted generative AI’s capabilities to new heights. It’s not just marketing.
Large language models went from tens of millions of data points to trillions in only a few years. That exponential jump enables AI to propose advanced facility designs, draft patient care protocols and interpret building data for better infection control or energy usage. In practical terms, generative AI will
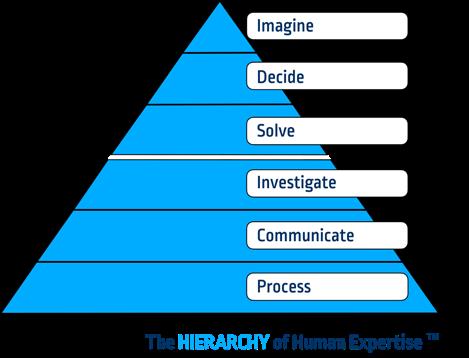
help solve real problems and it’s happening fast.
Still, these AI models are assistants, not replacements. They rely on the data they’ve seen and can be wrong, much like a phone’s auto-correct. Users must validate AI-generated content with expert judgment. By pairing AI’s capabilities with human oversight, healthcare teams can avoid being caught up in unrealistic hype.
OPTIMIZING SPACE UTILIZATION
In large hospitals or clinics, patient and staff movement is vital. AI can analyze the volume of visitors in different areas, identify bottlenecks and propose reconfigurations or staff scheduling tweaks that reduce wait times and cross-contamination risks. By processing vast datasets on patient flow, these tools create insights that improve the overall layout and efficiency of a facility.
ENERGY MANAGEMENT AND SUSTAINABILITY
Healthcare facilities have high energy demands. By spotting patterns in HVAC, lighting and medical equipment usage, AI can recommend strategies for reducing consumption without sacrificing essential conditions. Over time, these findings can inform more sustainable
architectural designs for future expansions or entire facilities.
ROBOTICS FOR OPERATIONAL TASKS
AI-driven robots roaming hospital corridors might feel futuristic but the core technologies are already here. Robots can deliver medications, linens and meals, using AI to detect obstacles or safety issues in real-time. Automating repetitive tasks frees staff to focus on higher-level responsibilities, ultimately improving patient care.
MULTI-LANGUAGE COMMUNICATION
In a healthcare environment that serves diverse populations, communication barriers can degrade patient care. Generative AI tools now translate signage, questionnaires and educational material into multiple languages almost instantly. Real-time transcription and translation services allow clinicians to speak with patients who do not share the same language, advancing health equity while boosting patient satisfaction.
REDUCING ‘MEETING OVERLOAD’
Constant collaboration among doctors, nurses, administrators and facility managers is essential but can be time-consuming. AI-powered
The kinds of work and hierarchy between automatable versus human-centric tasks. Artificial intelligence excels at those at the bottom of the pyramid, while the top layers require human insight.
note-takers produce automatic transcripts and summaries of meetings, highlighting key points and action items so that staff can revisit them quickly. By handling these administrative tasks, AI frees professionals to tackle problem-solving and patient care.
WHY AI WON’T REPLACE HUMANS
One of the most pressing questions for professionals in any industry is whether AI will make human jobs obsolete. The reality is more nuanced. AI will undoubtedly automate certain tasks, often the most repetitive and predictable ones. But this shift allows teams to focus on creative, human-centric work, such as complex problem-solving, decision-making and imagination.
A useful model is to think about a hierarchy or a ‘pyramid’ of workplace tasks: process (the routine tasks that follow a set process); communicate (sharing updates and clarifying progress with team members); investigate (identifying anomalies or inefficiencies); problem-solve (addressing unique issues that arise); decide (choosing the appropriate path forward given many possibilities); and imagine (envisioning a future that does not exist yet, shaped by creativity and hope).
AI excels at the bottom layers — process and a significant portion of communication. Even ‘investigate’ tasks can be streamlined by AI’s ability to sift through data to spot abnormalities. However, the top layers — problem-solving, making complex, context-laden decisions and imagining future scenarios — are domains that require human insight, empathy and ethical considerations. In healthcare, these layers become increasingly

vital. Patients are not just data points; they’re individuals who need holistic, empathetic care. Facility design, too, demands an understanding of patient well-being, workflow integration and future adaptability — facets that depend on human judgment.
A PARTNERSHIP CHANGING WORKFLOWS
It’s important to see AI not as a threat but as a powerful intern or ‘assistant’ that is always learning. When AI is given tasks, the output must be checked (just as an intern’s work would be). Over time, a better sense of its capabilities, limitations and how best to direct AI is gained. This approach aligns with current legal and professional standards in many fields — ultimately, human professionals are responsible for oversight and the final word on significant decisions.
In practice, the translation tools, note-takers and generative design software that are already available can drastically reduce administrative burdens. The result: healthcare professionals and facility planners have more bandwidth to focus on what truly matters — improving patient outcomes, learning about new technologies or treatments, and imagining how to transform healthcare spaces for the next generation of patients.
FROM HYPE TO HABIT
AI has already moved beyond the realm of science fiction. The hype cycle may still lead to sensational claims, but the tools themselves are undeniably powerful and only getting better. Within five years, AI integration will seem as natural as using smartphones today. Hospitals and clinics that adopt AI thoughtfully will
enjoy a competitive advantage: more efficient workflows, better patient communication and reduced operational costs.
Yet, even as AI is embraced, remember artificial intelligence is often just an umbrella term for tools that optimize how vast amounts of data is used. AI can help manage the complexities of modern healthcare, meeting new sustainability goals, addressing changing patient demographics and connecting with global communities in their own languages. Ultimately, humans remain at the heart of this transformation. People still solve the tough problems, imagine new possibilities and empathize with patients in a way that no algorithm can.
The future of healthcare systems and spaces lies in a collaborative partnership between human expertise and AI’s astonishing ability to process data and generate targeted insights. By offloading repetitive tasks to AI, healthcare professionals can devote more energy to real innovation — envisioning hospitals that are safer and more inclusive, sustainable and patient-centric than ever before.
Dan Chuparkoff is an innovation expert from Google, McKinsey and Atlassian, driving global teams to harness technology for growth. With three decades of experience helping teams navigate technological change, he’s one of the world’s leading experts on artificial intelligence (AI), innovation and the future of work. Known as the technology-speaker for non-tech teams, Dan translates complex concepts into simple, accessible ideas. By combining the power of technology with human expertise, he shows organizations how to thrive in the exponential future ahead.
Don’t Let Poor HVAC Performance
Put Patients at Risk
RESTORE. DON’T REPLACE.
With PureAir’s New Life HVAC Restoration Service, hospitals can avoid downtime and extend the life of air handler units.
> Save Up to 70% vs. Replacement
> Improve Indoor Air Quality & Efficiency
> Reduce Downtime & Emergency Repairs
> Restore Performance, Protect Patients
> Ask About Procurement through Kinetic GPO



DIGITAL TWINS IN DESIGN
Dynamic data models of physical assets transforming the built
By Michael Zumpano

world
The intersection of technology and healthcare facility architecture continually redefines modern medical environments’ possibilities. As digital tools become more integrated into design and planning processes, healthcare space conception, construction and management are transforming. These advancements are not merely about keeping pace with innovation; they are reshaping how hospitals, clinics and specialized care centres are built, maintained and monitored to enhance patient care and ensure long-term operational efficiency.
A key example of this technological shift is the adoption of digital twin technology. This tool allows design teams, owner stakeholders and contractors to gain unprecedented visibility into space utilization, maintenance requirements and potential design challenges before they arise. Such technologies pave the way for more informed decision-making and streamlined project execution, setting a new standard for healthcare architecture.
Exploring and embracing emerging technologies is essential for design teams aiming to remain competitive and adaptable. By adopting forward-thinking tools and methods, firms can streamline workflows, deliver better outcomes and keep pace with the rapidly evolving demands of the healthcare design landscape.
3-D SCANS FOR CONCEPTUAL DESIGN
Traditionally, capturing spatial data for conceptual design involved manual measurements with pen and paper or basic laser measuring tools. While effective in their time, these methods were labour-intensive and prone to oversight, often missing critical spatial relationships or hidden conditions within complex healthcare environments.
The adoption of 3-D scanning technology has revolutionized this process, offering precision, speed and comprehensiveness in data collection. Selecting the right tool depends on
A snapshot of the user interface reveals how exterior and interior data are combined to form a full digital building model. The result is a scalable, shareable tool that helps teams collaborate efficiently, whether working within a single building or across a larger campus.
several factors, including training requirements, equipment cost, data capture precision, scanning speed, stealth and accessibility in occupied spaces, and how well the captured data is organized for stakeholder access. These considerations help design teams determine the most effective technology for each project phase, type and size.
COMPLEX CONSTRUCTION HISTORY
Healthcare facilities often evolve over decades, resulting in layered construction histories that can be challenging to unravel. Additions and renovations, sometimes poorly documented, create an intricate tapestry of infrastructure. Traditional as-built drawings frequently lack critical information like the location of furniture, equipment or hidden structural elements.
3-D scanning and digital twin technologies allow design teams to visualize and understand these complexities, providing a realtime, interactive representation of the space. This level of insight significantly reduces risks during renovation and expansion projects by revealing structural interferences and outdated configurations that might otherwise go unnoticed.
OUT-OF-THE-BOX SOLUTIONS
While many scanning technologies are marketed toward industries like construction, agriculture and property management, their application in healthcare design is often over-
IT’S ESSENTIAL TO EVALUATE THE RIGHT TOOL FOR A PROJECT BASED ON THE SPACE’S UNIQUE CONDITIONS, PRIORITIES AND CONSTRAINTS.
looked. This represents a unique differentiation opportunity for both owners and designers in environments where accuracy and efficiency directly impact patient care and operational safety.
Forward-looking design teams are exploring tools not traditionally aimed at architecture, such as DroneDeploy, NavVis and Matterport, to unlock new possibilities in space planning, facility assessment and ongoing facility monitoring. These solutions streamline data capture, enhance spatial understanding and support proactive decision-making throughout the life cycle of healthcare environments, from planning and design to long-term maintenance and operational oversight.
EVALUATING SCANNING TECHNOLOGIES
Different scanning technologies offer distinct advantages depending on project requirements. DroneDeploy allows rapid 360-degree walk-throughs of expansive areas, capturing visual context with minimal setup. NavVis scanners, while heavier and costlier, provide high-precision measurements ideal for pro-

jects requiring exact spatial data. Matterport scanners strike a balance, offering immersive client walk-throughs with clear visuals, though they require a more deliberate setup with a tripod.
The time investment for each method varies. Traditional pen and paper surveys capture around two to four square metres (21 to 42 square feet) per minute, while Matterport can achieve around 7.7 square metres (83 square feet) per minute. DroneDeploy far surpasses these, covering around 92 square metres (1,000 square feet) per minute, and NavVis follows closely at 70 square metres (750 square feet) per minute. Many site-specific factors can cause these estimates to vary.
It’s essential to evaluate the right tool for a project based on the space’s unique conditions, priorities and constraints. For example, a large hospital campus undergoing initial programming may benefit from DroneDeploy’s highspeed, immersive walk-throughs for assessing look and feel across many departments without the need for measurable accuracy. In contrast, a renovation project within an active surgical suite may require the high precision of

LEFT: Choosing the right scanning tool requires multiple considerations: the size of the area, how quickly results are needed and how the data will be used. RIGHT: By visualizing spaces remotely, teams can align quickly, resolve questions on the spot and keep projects moving without stepping foot on-site. Image courtesy Cincinnati Children's Hospital Medical Centre.

track equipment placement and assess compliance with safety standards over time. For example, the models can quickly highlight storage areas where medical supplies or hazardous materials may be improperly placed, or confirm that workstations meet ergonomic and infection prevention guidelines. This continuous oversight contributes to a safer and more organized environment for both staff and patients.
NavVis to verify clearances and compliance with infection control guidelines. Choosing the right scanning solution from the start not only improves workflow efficiency but also ensures the data collected aligns with the project’s intended outcomes and balance of team resources.
FEATURES ENABLED BY DIGITAL TWINS
Digital twins enhance project planning by

validating space characteristics, ensuring compliance with hospital standards and supporting user request evaluations against documented guidelines. They can also be instrumental in identifying discrepancies early in the design process, helping to avoid costly rework or miscommunication.
Beyond design, this technology serves as an ongoing operational tool. Facilities teams can remotely monitor space usage,

Another often overlooked advantage is the ability of models to house critical documentation, such as product cut sheets, operation manuals and equipment data. Traditionally, this information is scattered across physical binders, hard drives or remote storage locations, making it difficult and time-consuming to access. Housing these documents within a centralized, visual model provides users with a much more intuitive way to locate and reference technical data, improving maintenance efficiency and reducing the risk of lost information over time.
Another key benefit is the reduction in repeated physical site visits. In large healthcare campuses, walking across a facility to validate a condition can be time-consuming. This challenge grows in multi-site systems, where


Digital twins enable users to navigate a space remotely, with overlaid floor plans that support quick orientation and spatial understanding, which is especially helpful for off-site teams. Image courtesy Cincinnati Children's Hospital Medical Centre.
travelling to remote locations for basic observations can significantly drain time and resources. With an accurate, interactive environment representation, teams can eliminate this travel burden. This saves hours of labour and enables quicker response times and more informed decision-making, which is especially valuable in the fast-paced world of healthcare operations.
THE FUTURE OF LIVING MODELS
Looking forward, these models are evolving into living, dynamic systems. When paired with real-time sensors and integrated data streams, they can begin to reflect ongoing building performance — monitoring HVAC systems, energy usage and internal conditions like temperature or humidity. This creates a powerful feedback loop for sustainability, helping reduce carbon footprints while improving patient and staff comfort.
Integration with building information modelling, asset tagging and continuous 3-D scan data allows for an always up-to-date model, offering accurate insight for operational adjustments and long-term planning. As the technology matures, these tools are becoming essential components in managing
the full life cycle of healthcare spaces, from design to occupancy to everyday operations. This is reshaping not only how environments are built but also how they are continuously experienced and optimized.
Additionally, the rapid advancement of smartphone technology is democratizing access to spatial data capture. Increasingly powerful mobile devices now support high-resolution light detection and ranging (Lidar) and photogrammetry applications, enabling individuals and smaller teams to generate digital building copies with minimal equipment investment. This accessibility is lowering the barrier to entry for organizations exploring digital twins, making it more feasible to integrate the technology across a broader range of healthcare environments, regardless of scale or budget. In time, these tools may become as ubiquitous as floor plans, serving as foundational resources for day-today operations and strategic planning alike.
EMBRACING THE PARADIGM SHIFT
The integration of 3-D scanning and digital twin technologies is transforming not only how healthcare facilities are designed but also how they are understood, maintained and
optimized long after construction. These tools have shifted from documentation aids to essential platforms for communication, planning and real-time facility oversight.
By enabling remote validation of spaces, streamlining data access and facilitating collaboration among stakeholders, digital replicas reduce inefficiencies and improve responsiveness across departments. As they evolve into living models, their potential to support sustainability, energy management and occupant comfort will only expand.
This convergence of design and operational intelligence is setting a new standard in healthcare architecture, one where facilities are more adaptive, staff are better supported and patient outcomes are prioritized through more intelligent, data-driven environments.
Michael Zumpano is an architect with BHDP Architecture, an award-winning international architectural firm. Michael leverages emerging technologies to improve design outcomes, streamline workflows and support informed decision-making. He equips teams with data-rich tools that enhance collaboration, efficiency and project performance across diverse markets. Michael can be reached at mzumpano@bhdp.com.




When
WATER SAFETY IN DEVICE PROCESSING
New standard brings critical changes to facility management
By Richard L. Parker

As healthcare facilities increasingly focus on patient safety and infection prevention, effective water management has become a critical aspect of medical device processing. To address this, ANSI/ AAMI ST108:2023 was introduced last year as a new, comprehensive standard for water quality systems in device reprocessing. This standard provides a clear framework for healthcare organizations to ensure proper water quality during decontamination, disinfection and sterilization processes.
The journey toward ST108:2023, began with the release of AAMI TIR34: 2014/ (R)2017, which offered initial guidance for managing water quality in medical device reprocessing. Over the past decade, this technical report has evolved into a full-fledged standard with expanded requirements for water system performance, testing and team collaboration, offering healthcare organizations a detailed roadmap for compliance.
STRENGTHENING WATER MANAGEMENT
Healthcare organizations likely have existing water management procedures that align with elements of ST108:2023. However, a thorough review of current practices is essential to identify opportuni-
ties for building upon these systems rather than starting from scratch.
Medical device manufacturers often specify water quality requirements in their instructions for use (IFUs) for different stages of device processing. These requirements should be a cornerstone of any water management plan. Additionally, hospitals must implement strategies to reduce the presence of biological agents like legionella in their water distribution systems.
Key components of an effective water management system include clear roles and responsibilities for the water management team; a comprehensive risk analysis; routine water quality monitoring; and regular system maintenance and performance qualification.
CONSIDERATIONS FOR IMPLEMENTATION
When preparing to implement ST108:2023, healthcare organizations should ask three questions.
Are device and equipment IFUs being followed? Identify the water quality requirements for each stage of the device processing cycle, from decontamination to sterilization. What types of water are defined and required in the facility? Understand the dis-
tinction between utility water, critical water and steam, and ensure each is processed and used according to the standard.
Is the water management team multidisciplinary? Expand the team’s scope to include key personnel involved in device processing, such as central sterilization staff and clinical engineering personnel.
MONITORING AND IMPROVEMENT
To ensure the efficacy of water systems in producing disinfected and sterilized medical devices, organizations must engage in routine monitoring. Meaningful metrics should include checking for corrosion, biofilm buildup, scaling and potential microbial contamination. Monitoring these factors not only protects the integrity of medical devices but also ensures the safety of patients and personnel.
By starting with a gap analysis and expanding the water management team, healthcare organizations can begin taking actionable steps toward full compliance with ST108:2023. Preparing now will enable smoother transitions when upgrades to water systems are required, whether driven by regulatory changes or accreditation standards.
As water quality continues to be a critical factor in effective medical device processing, healthcare facilities have a clear opportunity to strengthen their systems in line with this updated standard. By addressing potential gaps and incorporating cross-functional expertise, organizations can ensure better patient outcomes and safer environments for both staff and those receiving care.
Richard L. Parker is associate director of physical environment and life safety at Accreditation Commission for Health Care Inc. (ACHC), where he provides guidance to customers and surveyors in the ambulatory service centre and hospital programs. Prior to joining ACHC full-time, Richard was an accreditation surveyor while also serving as executive director of facilities for a 615-bed hospital system in Arizona.

Smart Parking Technology Solutions
Overture E-Line
COST-EFFECTIVE. FLEXIBLE. INTELLIGENT. ROBUST .


Ready for Care
Whether you’re managing patient traffic, staff access, or visitor convenience, the Overture E -Line delivers a flexible, future-ready parking solution designed to support healthcare facilities of all sizes
Why choose Overture E -Line?
Wireless – 4G/ WiFi Connection Ready
No trenching. No disruption. With built-in 4G and WiFi capabilities, Overture E-Line makes installation simple and communication seamless ideal for hospitals and clinics where uptime is critical
Safe, Secure & Compliant
Protect your operations with advanced encryption, secure authentication, and reliable transaction logging. Maintain full compliance while preventing unauthorized access and security breaches
Ecological
Designed to provide a seamless and environmentally friendly experience. By utilizing Automatic License Plat e Recognition (ALPR), entry and exit times significantly shorten, reducing the emissions of exhaust gases from idling vehicles. Using paper on roll as a backup, the ticketless system issues digital tickets minimizing waste. The intelligent packaging approach optimizes mat erial use, lowering packaging costs and reducing the overall environmental footprint of the system. These innovations ensure a greener and more efficient solution.

Cost-effective



Invest in a system that delivers top performance and is tailored to today’s needs This parking solution is designed to deliver maximum value, reduce your cost of ownership and improve efficiency. Enjoy the benefits of advanced technology at a competitive price.
Multilingual with Voice
Guidance
AODA-compliant terminals provide voice guidance in English and French, helping visually impaired users navigate more easily Multilin gual screens ensure clarity for patients and visitors from diverse backgrounds
Flexib le – Hybrid with all solutions within the Overture Ecosystem
Open APIs make it easy to connect with third -party apps such as payment processors, hospital systems, or reservation tools creating a smooth, unified experience for operators and users alike.
About Amano Canada
Your Parking Technology Partner since 1987. By streamlining our expertise in Parking Access and Revenue Control Systems (PARCS) , we create holistic, innovative, sustainable and smart mobility solutions that meet the rapidly changing needs of the various stakeholders in organizations in both the public and private sector
Smart Work - Smart Park - Smart Pay