2022 – 2023 EMPLOYEE BENEFITS GUIDE Phone | 888.836.5100



• • • • • • • • • • • • • • 1

• • • • • 2
Default Password


Password

Site Access
3
LOCAL HEALTH CARE. TEXAS-SIZED BENEFITS. TRS-ActiveCare Plan Highlights 2022-23
From the North Texas plains to the Gulf Coast, TRS-ActiveCare is where you live and work. We have more Texas doctors than any other plan and more ways to make your health plan yours.




Learn the terms.
• Premium: The monthly amount you pay for health care coverage.
• Deductible: The annual amount for medical expenses you’re responsible to pay before your plan begins to pay its portion.
• Copay: The set amount you pay for a covered service at the time you receive it. The amount can vary by the type of service.








• Coinsurance: The portion you’re required to pay for services after you meet your deductible. It’s often a specified percentage of the costs; i.e. you pay 20% while the health care plan pays 80%.
• Out-of-Pocket Maximum: The maximum amount you pay each year for medical costs. After reaching the out-of-pocket maximum, the plan pays 100% of allowable charges for covered services.
758429.0322
4
This plan is closed and not accepting new enrollees. If you’re currently enrolled in TRS-ActiveCare 2, you can remain in this plan. 2022-23 TRS-ActiveCare Plan Highlights Sept. 1, 2022 –Aug. 31, 2023 Things to Know •TRS’s Texas-sized purchasing power enables access to broad networks without county boundaries. •Specialty drug insurance means you’re covered, no matter what life throws at you. Monthly Premiums Employee Only$364$ $457$$376$ Employee and Spouse$1,026$$1,117$$1,058$ Employee and Children$654$$735$$675$ Employee and Family$1,228$$1,405$$1,265$ Total PremiumTotal PremiumTotal Premium Your PremiumYour PremiumYour Premium Total PremiumYour Premium $1,013$ $2,402$ $1,507$ $2,841$ How to Calculate Your Monthly Premium Total Monthly Premium Your District and State Contributions Your Premium Ask your Benefits Administrator for your district’s specific premiums. All TRS-ActiveCare participants have three plan options . Each includes a wide range of wellness benefits. TRS-ActiveCare 2 • Closed to new enrollees • Current enrollees can choose to stay in plan • Lower deductible • Copays for many services and drugs • Nationwide network with out-of-network coverage • No requirement for PCPs or referrals TRS-ActiveCare PrimaryTRS-ActiveCare Primary+TRS-ActiveCare HD Plan Summary • Lowest premium of all three plans • Copays for doctor visits before you meet your deductible • Statewide network • Primary Care Provider (PCP) referrals required to see specialists • Not compatible with a Health Savings Account (HSA) • No out-of-network coverage • Lower deductible than the HD and Primary plans • Copays for many services and drugs • Higher premium • Statewide network • PCP referrals required to see specialists • Not compatible with a Health Savings Account (HSA) • No out-of-network coverage • Compatible with a Health Savings Account (HSA) • Nationwide network with out-of-network coverage • No requirement for PCPs or referrals • Must meet your deductible before plan pays for non-preventive care Wellness Benefits at No Extra Cost* Being healthy is easy with: •$0 preventive care •24/7 customer service •One-on-one health coaches •Weight loss programs •Nutrition programs •Ovia TM pregnancy support •TRS Virtual Health •Mental health benefits •And much more! *Available for all plans. See the benefits guide for more details. Plan Features Type of CoverageIn-Network Coverage OnlyIn-Network Coverage OnlyIn-NetworkOut-of-Network Individual/Family Deductible$2,500/$5,000$1,200/$3,600$3,000/$6,000$5,500/$11,000 CoinsuranceYou pay 30% after deductibleYou pay 20% after deductibleYou pay 30% after deductibleYou pay 50% after deductible Individual/Family Maximum Out of Pocket$8,150/$16,300$6,900/$13,800$7,050/$14,100$20,250/$40,500 NetworkStatewide NetworkStatewide NetworkNationwide Network PCP RequiredYesYesNo In-NetworkOut-of-Network $1,000/$3,000$2,000/$6,000 You pay 20% after deductibleYou pay 40% after deductible $7,900/$15,800$23,700/$47,400 Nationwide Network No Prescription Drugs Drug DeductibleIntegrated with medical$200 brand deductibleIntegrated with medical Generics (30-Day Supply/90-Day Supply)$15/$45 copay; $0 copay for certain generics$15/$45 copayYou pay 20% after deductible; $0 coinsurance for certain generics Preferred BrandYou pay 30% after deductibleYou pay 25% after deductibleYou pay 25% after deductible Non-preferred BrandYou pay 50% after deductibleYou pay 50% after deductibleYou pay 50% after deductible Specialty $0 if PrudentRx eligible; You pay 30% after deductible $0 if PrudentRx eligible; You pay 30% after deductible You pay 20% after deductible Insulin Out-of-Pocket Costs$25 copay for 31-day supply; $75 for 61-90 day supply$25 copay for 31-day supply; $75 for 61-90 day supplyYou pay 25% after deductible $200 brand deductible $20/$45 copay You pay 25% after deductible ($40 min/$80 max)/ You pay 25% after deductible ($105 min/$210 max) You pay 50% after deductible ($100 min/$200 max)/ You pay 50% after deductible ($215 min/$430 max) $0 if PrudentRx eligible; You pay 30% after deductible ($200 min/$900 max)/ No 90-day supply of specialty medications $25 copay for 31-day supply; $75 for 61-90 day supply Doctor Visits Primary Care$30 copay$30 copayYou pay 30% after deductibleYou pay 50% after deductible Specialist$70 copay$70 copayYou pay 30% after deductibleYou pay 50% after deductible $30 copayY ou pay 40% after deductible $70 copayY ou pay 40% after deductible Immediate Care Urgent Care$50 copay$50 copayYou pay 30% after deductibleYou pay 50% after deductible Emergency CareYou pay 30% after deductibleYou pay 20% after deductibleYou pay 30% after deductible TRS Virtual Health-RediMD (TM) $0 per medical consultation$0 per medical consultation$30 per medical consultation TRS Virtual Health-Teladoc ® $12 per medical consultation$12 per medical consultation$42 per medical consultation $50 copayYou pay 40% after deductible You pay a $250 copay plus 20% after deductible $0 per medical consultation $12 per medical consultation $ $ $ $ $ $ $ $ $ $ $ $ $ $ $ $ 5
REMEMBER:
Compare Prices for Common Medical Services
Log into Blue Access for MembersSM at www.bcbstx.com/trsactivecare to use the cost estimator tool. This will help you find the best prices through different providers.
*Pre-certification for genetic and specialty testing may apply. Contact a Personal Health Guide at 1-866-355-5999 with questions.
www.trs.texas.gov
Revised 05/03/22 Benefit TRS-ActiveCare Primary TRS-ActiveCare Primary+ TRS-ActiveCare HDTRS-ActiveCare 2 In-Network OnlyIn-Network OnlyIn-NetworkOut-of-NetworkIn-NetworkOut-of-Network Diagnostic Labs* Office/Indpendent Lab: You pay $0 Office/Indpendent Lab: You pay $0 You pay 30% after deductible You pay 50% after deductible Office/Indpendent Lab: You pay $0 You pay 40% after deductible Outpatient: You pay 30% after deductible Outpatient: You pay 20% after deductible Outpatient: You pay 20% after deductible High-Tech Radiology You pay 30% after deductible You pay 20% after deductible You pay 30% after deductible You pay 50% after deductible You pay 20% after deductible + $100 copay per procedure You pay 40% after deductible + $100 copay per procedure Outpatient Costs You pay 30% after deductible You pay 20% after deductible You pay 30% after deductible You pay 50% after deductible You pay 20% after deductible ($150 facility copay per incident) You pay 40% after deductible ($150 facility copay per incident) Inpatient Hospital Costs You pay 30% after deductible You pay 20% after deductible You pay 30% after deductible You pay 50% after deductible ($500 facility per day maximum) You pay 20% after deductible ($150 facility copay per day) You pay 40% after deductible ($500 facility per day maximum) Freestanding Emergency Room You pay $500 copay + 30% after deductible You pay $500 copay + 20% after deductible You pay $500 copay + 30% after deductible You pay $500 copay + 50% after deductible You pay $500 copay + 20% after deductible You pay $500 copay + 40% after deductible Bariatric Surgery Facility: You pay 30% after deductible Facility: You pay 20% after deductible Not CoveredNot Covered Facility: You pay 20% after deductible ($150 facility copay per day) Not Covered Professional Services: You pay $5,000 copay + 30% after deductible Professional Services: You pay $5,000 copay + 20% after deductible Professional Services: You pay $5,000 copay + 20% after deductible Only covered if rendered at a BDC+ facility Only covered if rendered at a BDC+ facility Only covered if rendered at a BDC+ facility Annual Vision Exam (one per plan year; performed by an ophthalmologist or optometrist) You pay $70 copayYou pay $70 copay You pay 30% after deductible You pay 50% after deductible You pay $70 copay You pay 40% after deductible Annual Hearing Exam (one per plan year) $30 PCP copay $70 specialist copay $30 PCP copay $70 specialist copay You pay 30% after deductible You pay 50% after deductible $30 PCP copay $70 specialist copay You pay 40% after deductible 6
TRS also contracts with HMOs in certain regions of the state to bring participants in those areas additional options. Not all HMOs are available in all regions. Please verify your eligibility.
You can choose this plan if you live in one of these counties: Austin, Bastrop, Bell, Blanco, Bosque, Brazos, Burleson, Burnet, Caldwell, Collin, Coryell, Dallas, Denton, Ellis, Erath, Falls, Freestone, Grimes, Hamilton, Hays, Hill, Hood, Houston, Johnson, Lampasas, Lee, Leon, Limestone, Madison, McLennan, Milam, Mills, Navarro, Robertson, Rockwall, Somervell, Tarrant, Travis, Walker, Waller, Washington, Williamson
You can choose this plan if you live in one of these counties: Cameron, Hildalgo, Starr, Willacy
You can choose this plan if you live in one of these counties: Andrews, Armstrong, Bailey, Borden, Brewster, Briscoe, Callahan, Carson, Castro, Childress, Cochran, Coke, Coleman, Collingsworth, Comanche, Concho, Cottle, Crane, Crockett, Crosby, Dallam, Dawson, Deaf Smith, Dickens, Donley, Eastland, Ector, Fisher, Floyd, Gaines, Garza, Glasscock, Gray, Hale, Hall, Hansford, Hartley, Haskell, Hemphill, Hockley, Howard, Hutchinson, Irion, Jones, Kent, Kimble, King, Knox, Lamb, Lipscomb, Llano, Loving, Lubbock, Lynn, Martin, Mason, McCulloch, Menard, Midland, Mitchell, Moore, Motley, Nolan, Ochiltree, Oldham, Parmer, Pecos, Potter, Randall, Reagan, Reeves, Roberts, Runnels, San Saba, Schleicher, Scurry, Shackelford, Sherman, Stephens, Sterling, Stonewall, Sutton, Swisher, Taylor, Terry, Throckmorton, Tom Green, Upton, Ward, Wheeler, Winkler, Yoakum
Remember that when you choose an HMO, you’re choosing a regional network. 2022-23 Health Maintenance Organization (HMO) Plans and Premiums for Select Regions of the State REMEMBER: www.trs.texas.gov Total Monthly Premiums Total PremiumYour PremiumTotal PremiumYour PremiumTotal PremiumYour Premium Employee Only$491.55$ N/A $$ Employee and Spouse$1,232.58$ N/A $$ Employee and Children$789.39$ N/A $$ Employee and Family$1,418.42$ N/A $$ Central and North Texas Baylor Scott & White Health Plan Brought to you by TRS-ActiveCare Blue Essentials - South Texas HMO Brought to you by TRS-ActiveCare Blue Essentials - West Texas HMO Brought to you by TRS-ActiveCare
Revised 05/03/22 Prescription Drugs Drug Deductible$200 (excl. generics)N/A$150 Days Supply30-day supply/90-day supplyN/A30-Day Supply/90-Day Supply Generics$12/$30 copayN/A$5/$12.50 copay; $0 for certain generics Preferred BrandYou pay 30% after deductibleN/AYou pay 30% after deductible Non-preferred BrandYou pay 50% after deductibleN/AYou pay 50% after deductible Specialty You pay 25%/35% after deductible (perferred/non-preferred) N/AYou pay 15%/25% after deductible (preferred/non-preferred) Immediate Care Urgent Care$45 copayN/A$50 copay Emergency Care $500 copay after deductibleN/A $500 copay before deductible + 25% after deductible Doctor Visits Primary Care$15 copayN/A$20 copay Specialist$70 copayN/A$70 copay Plan Features Type of CoverageIn-Network Coverage OnlyN/AIn-Network Coverage Only Individual/Family Deductible$1,900/$4,750N/A$950/$2,850 CoinsuranceYou pay 20% after deductibleN/AYou pay 25% after deductible Individual/Family Maximum Out of Pocket$8,000/$15,000N/A$7,450/$14,900 $ $ $ $ N/A N/A N/A N/A N/A N/A N/A N/A N/A N/A N/A N/A 7
*ActiveCare 2 is only available to those currently under the plan, not available to new enrollees.

8
If you were hospitalized today, how much do you think your out-of-pocket expenses would be?

Your total expense, including deductible & coinsurance, could be as high as $6,250 or more!
Benefit Connection is a low-cost program designed to help you pay for covered out-of-pocket expenses you may incur while you are either confined in a hospital or being treated as an out-patient for an injury or an illness.

San Marcos Consolidated Independent School District has chosen a plan design that offers you an optimal offset of expenses due to high deductibles and high out-of-pocket maximums.
Plan Benefits offered to employees of San Marcos C - LOW PLAN
Hospital Confinement Benefit* - This benefit is designed to offset the cost you incur as an in- patient in the hospital when your primary comprehensive major medical policy applies such expenses to your deductible or coinsurance maximum, up to the $1000 plan year maximum per insured person.
Out-Patient Benefit* - This benefit offsets the cost you incur for out-patient treatment when your primary major medical policy applies such expenses to your deductible or coinsurance maximum, up to the $500 benefit limit, and up to a maximum of three out-patient occurrences per family per plan year. An “occurrence” is the treatment, or the series of treatments, for a specific injury or illness within a plan year Expenses related to physician office visits are not included in this benefit. Covered expenses include:
Surgery in an Out-Patient Facility or a Physician’s Office
Emergency Room visits
Diagnostic testing, Lab & X-ray at a diagnostic or hospital out-patient facility or at a Physician’s office if the cost is not included in the global office visit fee and is not part of wellness/preventive care
*For expenses to be eligible under this plan they must be medically necessary for the treatment of an injury or illness. Expenses not covered by your group major medical plan are not covered.
How to File a Claim
When you enroll in the Benefit Connection plan, you will receive an ID card, along with specific instructions on how to file a claim. This form outlines the procedures you should follow to obtain a claim form, what you need to file a claim, and where you should send your claim. Simply stated, you will need to submit a completed claim form, itemized bills (NOT balance due statements), and EOB’s that correspond to the itemized bills.
Claims may be filed at any time, but must be filed no longer than 12 months from the date of service in order to be eligible for coverage.
This information sheet highlights the important features of the product. The policy has limitations and exclusions. The exact provisions governing the insurance are contained in the master policy issued to each group on form number GAPP-4200, policy series G4200. Your carrier representative can supply you with costs and complete details of coverage.
Arranged/Administered By: Special Insurance Services, Inc.
2740 Dallas Parkway, Suite 100
Plano, Texas 75093
(972)788-0699 (800) 767-6811
Fax: (972) 960-0377
Offered to Employees of: San Marcos CISD
Offered By: US Employee Benefits Services Group





Monthly Cost Plan Selection Employee Only Employee & Spouse Employee & Child(ren) Employee & Family Ages 39 & Under $ $ $ $ Ages 40 through 49 $2 $ $ $ Ages 50 & Above $5 $9 $ $1
9
If you were hospitalized today, how much do you think your out-of-pocket expenses would be?

Your total expense, including deductible & coinsurance, could be as high as $6,250 or more!
Benefit Connection is a low-cost program designed to help you pay for covered out-of-pocket expenses you may incur while you are either confined in a hospital or being treated as an out-patient for an injury or an illness.

San Marcos Consolidated Independent School District has chosen a plan design that offers you an optimal offset of expenses due to high deductibles and high out-of-pocket maximums.
Plan Benefits offered to employees of San Marcos C
Hospital Confinement Benefit* - This benefit is designed to offset the cost you incur as an in- patient in the hospital when your primary comprehensive major medical policy applies such expenses to your deductible or coinsurance maximum, up to the $2000 plan year maximum per insured person.
Out-Patient Benefit* - This benefit offsets the cost you incur for out-patient treatment when your primary major medical policy applies such expenses to your deductible or coinsurance maximum, up to the $ 1000 benefit limit, and up to a maximum of three out-patient occurrences per family per plan year. An “occurrence” is the treatment, or the series of treatments, for a specific injury or illness within a plan year Expenses related to physician office visits are not included in this benefit. Covered expenses include:
Surgery in an Out-Patient Facility or a Physician’s Office
Emergency Room visits
Diagnostic testing, Lab & X-ray at a diagnostic or hospital out-patient facility or at a Physician’s office if the cost is not included in the global office visit fee and is not part of wellness/preventive care
*For expenses to be eligible under this plan they must be medically necessary for the treatment of an injury or illness. Expenses not covered by your group major medical plan are not covered.
How to File a Claim
When you enroll in the Benefit Connection plan, you will receive an ID card, along with specific instructions on how to file a claim. This form outlines the procedures you should follow to obtain a claim form, what you need to file a claim, and where you should send your claim. Simply stated, you will need to submit a completed claim form, itemized bills (NOT balance due statements), and EOB’s that correspond to the itemized bills.
Claims may be filed at any time, but must be filed no longer than 12 months from the date of service in order to be eligible for coverage.
This information sheet highlights the important features of the product. The policy has limitations and exclusions. The exact provisions governing the insurance are contained in the master policy issued to each group on form number GAPP-4200, policy series G4200. Your carrier representative can supply you with costs and complete details of coverage.
Arranged/Administered By: Special Insurance Services, Inc. 2740 Dallas Parkway, Suite 100 Plano, Texas 75093
(972)788-0699 (800) 767-6811
Fax: (972) 960-0377
Offered to Employees of: San Marcos CISD
Offered By: US Employee Benefits Services Group





Monthly Cost Plan Selection Employee Only Employee & Spouse Employee & Child(ren) Employee & Family Ages 39 & Under $ $ $ $ Ages 40 through 49 $ $ $ $ Ages 50 & Above $ $ $ $
10
Dental
Metropolitan Life Insurance Company
Network: PDP Plus
Child(ren)’s eligibility for dental coverage is from birth up to age 26.
* Negotiated Fee refers to the fees that participating dentists have agreed to accept as payment in full for covered services, subject to any copayments, deductibles, cost sharing and benefits maximums. Negotiated fees are subject to change.
** Reimbursement for out-of-network services is based on the lesser of the dentist’s actual fee or the Maximum Allowable Charge (MAC). The out-of-network Maximum Allowable Charge is a scheduled amount determined by MetLife. ***
R&C fee refers to the Reasonable and Customary (R&C) charge, which is based on the lowest of (1) the dentist’s actual charge, (2) the dentist’s usual charge for the same or similar services, or (3) the charge of most dentists in the same geographic area for the same or similar services as determined by MetLife.
†Applies to Type A, B and C Services
PLAN OPTION 1 High Plan PLAN OPTION 2 Low Plan Coverage Type In-Network % of Negotiated Fee * Out-of-Network 80% of R&C Fee *** In-Network % of Negotiated Fee * Out-of-Network % of Scheduled Amount ** Type A: Preventive (cleanings, exams, X-rays) 100% 100% 80% 80% Type B: Basic Restorative (fillings, extractions) 80% 80% 50% 50% Type C: Major Restorative (bridges, dentures) 50% 50% 40% 40% Type D: Orthodontia 50% 50% 50% 50% Deductible† Individual $50 $50 $50 $50 Family $150 $150 $150 $150 Annual Maximum Benefit Per Person $1,000 $1,000 $1,000 $1,000 Orthodontia Lifetime Maximum Per Person $1,500 $1,500 $750 $750
11
San Marcos Consolidated ISD
M o n t h l y C o s t
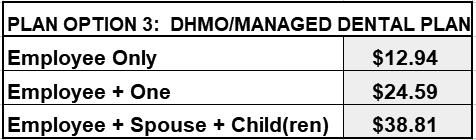
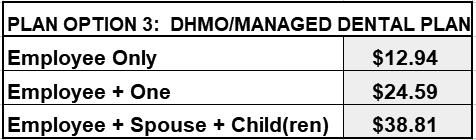
The following monthly costs are effective through August 31st, 202 Your premium will be paid through convenient payroll deduction. The Monthly costs shown below for “Employee + Spouse + Child(ren)” include the cost for all eligible children.
Plan Option 1: High Plan Plan Option 2: Low Plan
Employee Only
$3 Employee Only $
Employee + One Employee + One $
Employee + Spouse + Child(ren) $ Employee + Spouse + Child(ren) $
List of Primary Covered Services & Limitations
The service categories and plan limitations shown represent an overview of your Plan Benefits. This document presents the majority of services within each category, but is not a complete description of the Plan.
Plan Option 1: High Plan Plan Option 2: Low Plan
Type A –Preventive How Many/How Often
Prophylaxis (cleanings)
Oral Examinations
Topical Fluoride Applications
X-rays
Sealants
Type A –Preventive How Many/How Often
Two per calendar yearProphylaxis (cleanings)
Two exams per calendar yearOral Examinations
One fluoride treatment per calendar year for dependent children up to his/her 14th birthday
Full mouth X-rays; once per 5 years
Bitewings X-rays; one set per calendar year
One application of sealant material every 60 months for each non-restored, nondecayed 1st and 2nd molar of a dependent child up to his/her 14th birthday
Topical Fluoride Applications
X-rays
Two per calendar year
Two exams per calendar year
One fluoride treatment per calendar year for dependent children up to his/her 14th birthday
Full mouth X-rays; once per 5 years
Bitewings X-rays; one set per calendar year
Sealants
One application of sealant material every 60 months for each non-restored, nondecayed 1st and 2nd molar of a dependent child up to his/her 14th birthday
Type
Fillings
Fillings
Simple Extractions Simple Extractions
Crown, Denture and Bridge
Repair/ Recementations
Oral Surgery
General Anesthesia
Space Maintainers
When dentally necessary in connection with oral surgery, extractions or other covered dental services
Space maintainers for dependent children up to his/her 14th birthday.
Crown, Denture and Bridge
Repair/ Recementations
Oral Surgery
General Anesthesia
Space Maintainers
When dentally necessary in connection with oral surgery, extractions or other covered dental services
Space maintainers for dependent children up to his/her 14th birthday.
Restorative How Many/How Often
B – Basic
–
Restorative
Many/How Often
Type B
Basic
How
12
Type C – Major Restorative How Many/How Often
Type C – Major Restorative How Many/How Often
Endodontics Endodontics
Implants
Bridges and Dentures
Replacement once every 10 years
Initial placement to replace one or more natural teeth, which are lost while covered by the plan Dentures and bridgework replacement; one every 10 years
Replacement of an existing temporary full denture if the temporary denture cannot be repaired and the permanent denture is installed within 12 months after the temporary denture was installed
Implants
Bridges and Dentures
Replacement once every 10 years
Initial placement to replace one or more natural teeth, which are lost while covered by the plan Dentures and bridgework replacement; one every 10 years
Replacement of an existing temporary full denture if the temporary denture cannot be repaired and the permanent denture is installed within 12 months after the temporary denture was installed
Crowns, Inlays and Onlays
Replacement once every 10 years
Periodontics Periodontal scaling and root planing once per quadrant, every 24 months
Periodontal surgery once per quadrant, every 36 months
You, your spouse and your children, up to age 26, are covered while Dental insurance is in effect
All dental procedures performed in connection with orthodontic treatment are payable as Orthodontia
Payments are on a repetitive basis
20% of the Orthodontia Lifetime Maximum will be considered at initial placement of the appliance and paid based on the plan benefit’s coinsurance level for Orthodontia as defined in the plan summary
Orthodontic benefits end at cancellation of coverage
Crowns, Inlays and Onlays
Replacement once every 10 years
Periodontics Periodontal scaling and root planing once per quadrant, every 24 months
Periodontal surgery once per quadrant, every 36 months
Type
Your children, up to age 19, are covered while Dental insurance is in effect.
All dental procedures performed in connection with orthodontic treatment are payable as Orthodontia
Payments are on a repetitive basis
20% of the Orthodontia Lifetime Maximum will be considered at initial placement of the appliance and paid based on the plan benefit’s coinsurance level for Orthodontia as defined in the plan summary
Orthodontic benefits end at cancellation of coverage
The service categories and plan limitations shown above represent an overview of your plan benefits. This document presents the majority of services within each category, but is not a complete description of the plan.
Type D –Orthodontia How Many/How Often
D –Orthodontia How Many/How Often
13
Frequently Asked Questions
Who is a participating dentist?
A participating dentist is a general dentist or specialist who has agreed to accept negotiated fees as payment in full for covered services provided to plan members. Negotiated fees typically range from 30%-45% below the average fees charged in a dentist’s community for the same or substantially similar services. †
How do I find a participating dentist?
There are thousands of general dentists and specialists to choose from nationwide --so you are sure to find one that meets your needs. You can receive a list of these participating dentists online at www.metlife.com/mybenefits or call to have a list faxed or mailed to you. What services are covered under this plan?
The certificate of insurance sets forth the covered services under the plan. Please review the enclosed plan benefits to learn more.
May I choose a non-participating dentist?
Yes. You are always free to select the dentist of your choice. However, if you choose a non-participating dentist your out-of-pocket costs may be higher.
Can my dentist apply for participation in the network?
Yes. If your current dentist does not participate in the network and you would like to encourage him/her to apply, ask your dentist to visit www.metdental.com, or call 1-866-PDP-NTWK for an application. †† The website and phone number are for use by dental professionals only.
How are claims processed?
Dentists may submit your claims for you which means you have little or no paperwork. You can track your claims online and even receive email alerts when a claim has been processed. If you need a claim form, visit www.metlife.com/mybenefits or request one by calling
Can I get an estimate of what my out-of-pocket expenses will be before receiving a service?
Yes. You can ask for a pretreatment estimate. Your general dentist or specialist usually sends MetLife a plan for your care and requests an estimate of benefits. The estimate helps you prepare for the cost of dental services. We recommend that you request a pre-treatment estimate for services in excess of $300. Simply have your dentist submit a request online at www.metdental.com or call 1-877-MET-DDS9. You and your dentist will receive a benefit estimate for most procedures while you are still in the office. Actual payments may vary depending upon plan maximums, deductibles, frequency limits and other conditions at time of payment.
Can MetLife help me find a dentist outside of the U.S. if I am traveling?
Yes. Through international dental travel assistance services * you can obtain a referral to a local dentist by calling +1-312-356-5970 (collect) when outside the U.S. to receive immediate care until you can see your dentist. Coverage will be considered under your out-of-network benefits. ** Please remember to hold on to all receipts to submit a dental claim.
How does MetLife coordinate benefits with other insurance plans?
Coordination of benefits provisions in dental benefits plans are a set of rules that are followed when a patient is covered by more than one dental benefits plan. These rules determine the order in which the plans will pay benefits. If the MetLife dental benefit plan is primary, MetLife will pay the full amount of benefits that would normally be available under the plan, subject to applicable law. If the MetLife dental benefit plan is secondary, most coordination of benefits provisions require MetLife to determine benefits after benefits have been determined under the primary plan. The amount of benefits payable by MetLife may be reduced due to the benefits paid under the primary plan, subject to applicable law.
Do I need an ID card?
No. You do not need to present an ID card to confirm that you are eligible. You should notify your dentist that you are enrolled in the MetLife Preferred Dentist Program. Your dentist can easily verify information about your coverage through a toll-free automated Computer Voice Response system.
14
†Based on internal analysis by MetLife. Negotiated fees refer to the fees that in-network dentists have agreed to accept as payment in full for covered services, subject to any co-payments, deductibles, cost sharing and benefits maximums. Negotiated fees are subject to change.
††Due to contractual requirements, MetLife is prevented from soliciting certain providers.
*AXA Assistance USA, Inc. provides Dental referral services only. AXA Assistance is not affiliated with MetLife, and the services and benefits they provide are separate and apart from the insurance provided by MetLife. Referral services are not available in all locations.
**Refer to your dental benefits plan summary for your out-of-network dental coverage.
Exclusions
This plan does not cover the following services, treatments and supplies: Services which are not Dentally Necessary, those which do not meet generally accepted standards of care for treating the particular dental condition, or which we deem experimental in nature; Services for which you would not be required to pay in the absence of Dental Insurance; Services or supplies received by you or your Dependent before the Dental Insurance starts for that person; Services which are primarily cosmetic (for Texas residents, see notice page section in Certificate); Services which are neither performed nor prescribed by a Dentist except for those services of a licensed dental hygienist which are supervised and billed by a Dentist and which are for:
o Scaling and polishing of teeth; or
o Fluoride treatments;
Services or appliances which restore or alter occlusion or vertical dimension; Restoration of tooth structure damaged by attrition, abrasion or erosion; Restorations or appliances used for the purpose of periodontal splinting; Counseling or instruction about oral hygiene, plaque control, nutrition and tobacco; Personal supplies or devices including, but not limited to: water picks, toothbrushes, or dental floss; Decoration, personalization or inscription of any tooth, device, appliance, crown or other dental work; Missed appointments;
Services:
o Covered under any workers’ compensation or occupational disease law;
o Covered under any employer liability law;
o For which the employer of the person receiving such services is not required to pay; or
o Received at a facility maintained by the Employer, labor union, mutual benefit association, or VA hospital;
Services covered under other coverage provided by the Employer;
Temporary or provisional restorations;
Temporary or provisional appliances;
Prescription drugs;
Services for which the submitted documentation indicates a poor prognosis; The following when charged by the Dentist on a separate basis:
o Claim form completion;
o Infection control such as gloves, masks, and sterilization of supplies; or
o Local anesthesia, non-intravenous conscious sedation or analgesia such as nitrous oxide. Dental services arising out of accidental injury to the teeth and supporting structures, except for injuries to the teeth due to chewing or biting of food;
Caries susceptibility tests;
Initial installation of a fixed and permanent Denture to replace one or more natural teeth which were missing before such person was insured for Dental Insurance, Other fixed Denture prosthetic services not described elsewhere in the certificate; Precision attachments, except when the precision attachment is related to implant prosthetics;
15
Initial installation of a full or removable Denture to replace one or more natural teeth which were missing before such person was insured for Dental Insurance, Addition of teeth to a partial removable Denture to replace one or more natural teeth which were missing before such person was insured for Dental Insurance,
Adjustment of a Denture made within 6 months after installation by the same Dentist who installed it; Implants supported prosthetics to replace one or more natural teeth which were missing before such person was insured for Dental Insurance,
Fixed and removable appliances for correction of harmful habits;
Appliances or treatment for bruxism (grinding teeth), including but not limited to occlusal guards and night guards;
Diagnosis and treatment of temporomandibular joint (TMJ) disorders. This exclusion does not apply to residents of Minnesota;
Repair or replacement of an orthodontic device;
Duplicate prosthetic devices or appliances;
Replacement of a lost or stolen appliance, Cast Restoration, or Denture; and Intra and extraoral photographic images
Limitations
Alternate Benefits: Where two or more professionally acceptable dental treatments for a dental condition exist, reimbursement is based on the least costly treatment alternative. If you and your dentist have agreed on a treatment that is more costly than the treatment upon which the plan benefit is based, you will be responsible for any additional payment responsibility. To avoid any misunderstandings, we suggest you discuss treatment options with your dentist before services are rendered, and obtain a pre-treatment estimate of benefits prior to receiving certain high cost services such as crowns, bridges or dentures. You and your dentist will each receive an Explanation of Benefits (EOB) outlining the services provided, your plan’s reimbursement for those services, and your out-of-pocket expense. Procedure charge schedules are subject to change each plan year. You can obtain an updated procedure charge schedule for your area via fax by calling 1-800-942-0854 and using the MetLife Dental Automated Information Service. Actual payments may vary from the pretreatment estimate depending upon annual maximums, plan frequency limits, deductibles and other limits applicable at time of payment.
Cancellation/Termination of Benefits: Coverage is provided under a group insurance policy (Policy form GPNP99 / G.2130-S) issued by Metropolitan Life Insurance Company (MetLife). Coverage terminates when your membership ceases, when your dental contributions cease or upon termination of the group policy by the Policyholder or MetLife. The group policy terminates for non-payment of premium and may terminate if participation requirements are not met or if the Policyholder fails to perform any obligations under the policy. The following services that are in progress while coverage is in effect will be paid after the coverage ends, if the applicable installment or the treatment is finished within 31 days after individual termination of coverage: Completion of a prosthetic device, crown or root canal therapy.
Like most group benefit programs, benefit programs offered by MetLife and its affiliates contain certain exclusions, exceptions, reductions, limitations, waiting periods and terms for keeping them in force. For complete details of coverage and availability, please refer to the certificate of insurance or contact MetLife.

Metropolitan Life Insurance Company | 200 Park Avenue | New York, NY 10166 L0319512645[exp0520][xNM] © 2019 MetLife Services and Solutions, LLC DN-ANY-PPO-DUAL
16
Facts & Stats
Visits to the dentist can be expensive. From preventive care to major services, dental is a smart way to protect your smile and your pocketbook.
You get coverage for a wide range of services through a network of carefully selected participating dentists who agree to significantly lower costs than typical dental charges.
for example cleanings, x-rays and sealants
At the time of enrollment, you pre-select a participating dentist. Each enrolled family member may select a different participating dentist. Your primary care dentist also helps coordinate specialty care for you.
John’s primary care dentist identifies a molar that failed to erupt and advises that John needs to have it extracted.
for example fillings and extractions
for example crowns and root canals
The cost of an impacted tooth extraction ranges from $225-$600 per tooth in the U.S. By using a participating dentist, John pays the copay only, which depending on his exact plan, could range from just $10-$60
for soft tissue impacted tooth extraction.
What you need to know about a dental HMO/managed care plan:
• Significantly lower costs for dental services through a growing network of participating dentists.
• No deductibles, annual maximums or claims forms to complete.
• fees for materials and procedures requiring multiple services (i.e. root canals and crowns)
• For added convenience, MetLife’s Mobile App is available on the iTunes® App Store and Google Play. After downloading, you can use it to find a dentist, view your claims and access your ID card.
Smiles are free, but they are worth a lot
Range from $225 - $600 $0$100$200$300$400$500$600 $60 max
17
San Marcos Consolidated ISD
Welcome to Davis Vision!
care for your vision and eye health - a key part of overall health and wellness! If you are not currently enrolled, please visit our member site at davisvision.com or call 1.877.923.2847 and enter client code 8100 to locate providers or for additional information.
Just log on to our Member site at davisvision.com and click “Find a Provider,” or call us at 1.800.999.5431.
Make an appointment. Tell your provider you are a Davis Vision member with coverage through San Marcos Consolidated ISD. Provide your member ID number, name and date of birth, and do the same for your covered dependents seeking vision services. Your provider will take care of the rest!
in full. Includes dilation when professionally indicated.
Clear plastic lenses in any single vision, bifocal, trifocal or lenticular prescription. Covered in full. (See below for additional lens options and coatings.)

Covered in Full Frames:
Frame Allowance: VisionworksFrame Allowance:

Any Fashion or Designer level frame from Davis Vision’s Collection/2 (retail value, up to $160).
$125 toward any frame from provider plus 20% off any balance./1 No copay required.
$175 allowance plus 20% off any balance toward any frame from a Visionworks family of store locations./4 No copay required.
From Davis Vision’s Collection/2, up to: Four boxes/multi-packs*
Eight boxes/multi-packs*
$150 allowance toward any contacts from provider’s supply plus 15% off balance./1 No copay required.
Covered in full with prior approval.
*Number of contact lens boxes may vary based on manufacturer’s packaging.
1/ Additional discounts not applicable at Walmart, Sam’s Club or Costco locations
2/ The Davis Vision Collection is available at most participating independent provider locations. Collection is subject to change. Collection is inclusive of select toric and multifocal contacts.
3/ Including, but not limited to toric, multifocal and gas permeable contact lenses.

4/ Enhanced frame allowance available at all Visionworks Locations nationwide. 5/Transitions® is a registered trademark of Transitions Optical Inc.
Please note: Your provider reserves the right to not dispense materials until all applicable member costs, fees and copayments have been collected. Contact lenses: Routine eye examinations do not include professional services for contact may not be exchanged for eyeglasses. Progressive lenses: If you are unable to adapt to progressive addition lenses you have purchased, conventional bifocals will be supplied at no additional cost; however, your copayment is nonrefundable. May not be combined with other discounts or offers. Please be advised these lens
8/18/17
SPCVX01122web
lens types and coatings! Member Price Davis Vision Collection Frames: Fashion | Designer | Premier ..................................$0 | $0 | $25 Tinting of Plastic Lenses.............................................................................................................$0 Oversize Lenses .........................................................................................................................$0 Scratch-Resistant Coating ..........................................................................................................$0 Ultraviolet Coating ....................................................................................................................$12 ..............................................$35 | $48 | $60 Polycarbonate Lenses ...............................................................................................................$0 High-Index Lenses ..................................................................................................................$55 Progressive Lenses: Standard | Premium | Ultra .................................................$50 | $90 | $140 Polarized Lenses .....................................................................................................................$75 Photochromic Lenses (i.e. Transitions®, etc.)/5 ......................................................................$65 Scratch Protection Plan: Single Vision | Multifocal Lenses .............................................$20 | $40 Frequency Once everyIn-network Copay In-network Coverage Eye Examination 12 months$10Covered
Spectacle Lenses 12 months$25
Frame 24 months$0
Contact Lens & Follow Up Care 12 months$0 Davis
Collection Contacts: Specialty Contacts/3: Covered in
15% discount/1 15% discount/1 Contact Lenses (in lieu of eyeglasses) 12 months$0
Contacts:
Replacement Disposable Contact Lens Allowance: :
Vision
full.
Covered in Full
Planned
18
San Marcos Consolidated ISD
Welcome to Davis Vision!
care for your vision and eye health - a key part of overall health and wellness! If you are not currently enrolled, please visit our member site at davisvision.com or call 1.877.923.2847 and enter client code 8101 to locate providers or for additional information. SPCVX01123web
Just log on to our Member site at davisvision.com and click “Find a Provider,” or call us at 1.800.999.5431.
Make an appointment. Tell your provider you are a Davis Vision member with coverage through San Marcos Consolidated ISD. Provide your member ID number, name and date of birth, and do the same for your covered dependents seeking vision services. Your provider will take care of the rest!
in full. Includes dilation when professionally indicated.
Clear plastic lenses in any single vision, bifocal, trifocal or lenticular prescription. Covered in full. (See below for additional lens options and coatings.)

Covered in Full Frames:
Frame Allowance: VisionworksFrame Allowance:

Any Fashion, Designer or Premier level frame from Davis Vision’s Collection/2 (retail value, up to $195).
$150 toward any frame from provider plus 20% off any balance./1 No copay required.
$200 allowance plus 20% off any balance toward any frame from a Visionworks family of store locations./4 No copay required.
From Davis Vision’s Collection/2, up to: Four boxes/multi-packs*
Eight boxes/multi-packs*
$200 allowance toward any contacts from provider’s supply plus 15% off balance./1 No copay required.
Covered in full with prior approval.
*Number of contact lens boxes may vary based on manufacturer’s packaging.
1/ Additional discounts not applicable at Walmart, Sam’s Club or Costco locations
2/ The Davis Vision Collection is available at most participating independent provider locations. Collection is subject to change. Collection is inclusive of select toric and multifocal contacts.
3/ Including, but not limited to toric, multifocal and gas permeable contact lenses.

4/ Enhanced frame allowance available at all Visionworks Locations nationwide. 5/Transitions® is a registered trademark of Transitions Optical Inc.
Please note: Your provider reserves the right to not dispense materials until all applicable member costs, fees and copayments have been collected. Contact lenses: Routine eye examinations do not include professional services for contact may not be exchanged for eyeglasses. Progressive lenses: If you are unable to adapt to progressive addition lenses you have purchased, conventional bifocals will be supplied at no additional cost; however, your copayment is nonrefundable. May not be combined with other discounts or offers. Please be advised these lens
8/18/17
lens types and coatings! Member Price Davis Vision Collection Frames: Fashion | Designer | Premier ....................................$0 | $0 | $0 Tinting of Plastic Lenses.............................................................................................................$0 Oversize Lenses .........................................................................................................................$0 Scratch-Resistant Coating ..........................................................................................................$0 Ultraviolet Coating ......................................................................................................................$0 ..............................................$35 | $48 | $60 Polycarbonate Lenses ...............................................................................................................$0 High-Index Lenses ..................................................................................................................$55 Progressive Lenses: Standard | Premium | Ultra .....................................................$0 | $40 | $90 Polarized Lenses .....................................................................................................................$75 Photochromic Lenses (i.e. Transitions®, etc.)/5 ......................................................................$65 Scratch Protection Plan: Single Vision | Multifocal Lenses .............................................$20 | $40 Frequency Once everyIn-network Copay In-network Coverage Eye Examination 12 months$10Covered
Spectacle Lenses 12 months$25
Frame 12 months$0
Contact Lens & Follow Up Care 12 months$0 Davis
Contacts: Specialty Contacts/3: Covered in
15% discount/1 15% discount/1 Contact Lenses (in lieu of eyeglasses) 12 months$0
Contacts: Planned Replacement Disposable Contact Lens Allowance: :
Vision Collection
full.
Covered in Full
19
Frequently Asked Questions
How can I contact Member Services?
Call 1.800.999.5431 for automated help 24/7. Live help is also available seven days a week: Monday-Friday, 8 a.m.-11 p.m. | Saturday, 9 a.m.-4 p.m. | Sunday, 12 p.m.-4 p.m. (Eastern Time). (TTY services: 1.800.523.2847.)
Our Collection offers a great selection of fashionable and designer frames, most of which are covered in full. No wonder 8 out of 10 members select a Collection frame. Log on to our member Web site at davisvision.com and take a look!
When will I receive my eyewear?
Your eyewear will be delivered to your network provider generally lens coatings, provider frames or out-of-stock frames may delay the standard turnaround time.
Claim forms are only required if you visit an out-of-network provider. Claim forms are available on our member Web site.
eyeglasses or contact lenses on different dates or through different provider locations. Complete eyeglasses must be obtained at one time, from one provider. You may not split between a network recommend that all services be obtained from a network provider.
Yes; however, you receive the greatest value by staying in-network. If you go out-of-network, pay the provider at the time of service, then submit a claim to Davis Vision for reimbursement, up to the following amounts: eye exam - $35 | single vision lenses - $25 | bifocal - $40 | trifocal - $45 | lenticular - $80 | frame - $55 | elective contacts - $65 | visually required contacts - $150.
Your vision plan does not cover medical treatment of eye disease or injury; vision therapy; special lens designs or coatings, other than those described herein; replacement of lost eyewear; nonprescription (plano) lenses; contact lenses and eyeglasses in the two pair of eyeglasses in lieu of bifocals.
DAVIS VISION EXTRAS!
One Year Breakage Warranty Repair or replacement of your plan covered spectacle lenses, Collection frame or frame from a network retail location where the Collection is not displayed. Access a higher frame allowance by visiting a Visionworks family of store locations/6
Additional Savings At most participating network locations, members receive up to 20% off additional eyeglasses, sunglasses contact lenses./7
Mail Order Contact Lenses Replacement contacts (after service ensures easy, convenient, purchasing online and quick, direct shipping to your door. Log on to our member Web site for details.
Laser Vision Correction Up to 25% discount off participating provider’s U&C or 5% off advertised special (whichever is lower). Log on to our member Web site for details and to locate a provider. A One-time/lifetime allowance of $200 is available.
Low Vision Services Comprehensive low vision evaluation
Eye Health & Wellness Log on and learn more about your eyes, health and wellness; common eye conditions that can impair vision; and what you can do to ensure healthy eyes and a healthier life.
For more details… and responsibilities, or more information about Davis Vision, please log on to our member Web site or contact us at 1.800.999.5431.
Davis Vision has made every effort to correctly summarize your vision plan features contract with Davis Vision, the terms of the contract will prevail.
Fully insured product Underwritten by HM Life Insurance Company. Administered by Davis Vision, which may operate as Davis Vision Insurance Administrators in California. 6/ Enhanced frame allowance available at all Visionworks Locations nationwide. 7/Additional discounts not applicable at Walmart, Sam’s Club or Costco locations. 20
Voluntary Long Term Disability Insurance
Standard Insurance Company has developed this document to provide you with information about the optional insurance coverage you may select through San Marcos CISD. Written in non-technical language, this is not intended as a complete description of the coverage. If you have additional questions, please check with your human resources representative.
Employer Plan Effective Date
A minimum number of eligible employees must apply and qualify for the proposed plan before Voluntary LTD coverage can become effective. This level of participation has been agreed upon by San Marcos CISD and The Standard.
Eligibility
To become insured, you must be:
A regular employee of San Marcos CISD, excluding temporary or seasonal employees, full-time members of the armed forces, leased employees or independent contractors
Actively at work at least 15 hours each week
A citizen or resident of the United States or Canada
Employee Coverage Effective Date
Please contact your human resources representative for more information regarding the following requirements that must be satisfied for your insurance to become effective. You must satisfy:
Eligibility requirements
An eligibility waiting period (check with your human resources representative)
An evidence of insurability requirement, if applicable
An active work requirement. This means that if you are not actively at work on the day before the scheduled effective date of insurance, your insurance will not become effective until the day after you complete one full day of active work as an eligible employee.
Benefit Amount
You may select a monthly benefit amount in $100 increments from $300 to $8,000; based on the tables and guidelines presented in the Rates section of these Coverage Highlights. The monthly benefit amount must not exceed 66 2/3 percent of your monthly earnings.
Benefits are payable for non-occupational disabilities only. Occupational disabilities are not covered.
Plan Maximum Monthly Benefit: 66 2/3 percent of predisability earnings
Plan Minimum Monthly Benefit: 10 percent of your LTD benefit before reduction by deductible income
21
Benefit Waiting Period and Maximum Benefit Period
The benefit waiting period is the period of time that you must be continuously disabled before benefits become payable. Benefits are not payable during the benefit waiting period. The maximum benefit period is the period for which benefits are payable. The benefit waiting period and maximum benefit period associated with your plan options are shown below:
Options 1-6: Maximum Benefit Period of To SSNRA for Sickness and Accident
If you become disabled before age 62, LTD benefits may continue during disability until you reach age 65 or to the Social Security Normal Retirement Age (SSNRA) or 3 years 6 months, whichever is longer. If you become disabled at age 62 or older, the benefit duration is determined by your age when disability begins:
62 To SSNRA, or 3 years 6 months, whichever is longer
63 To SSNRA, or 3 years, whichever is longer
64 To SSNRA, or 2 years 6 months, whichever is longer
65 2 years
66 1 year 9 months
67 1 year 6 months
68 1 year 3 months
69+ 1 year
First
Day Hospital Benefit
With this benefit, if an insured employee is hospital confined for at least four hours, is admitted as an inpatient and is charged room and board during the benefit waiting period, the benefit waiting period will be satisfied. Benefits become payable on the date of hospitalization; the maximum benefit period also begins on that date. This feature is included only on LTD plans with benefit waiting periods of 30 days or less.
Preexisting Condition Exclusion
A detailed description of the preexisting condition exclusion is included in the Group Policy. If you have questions, please check with your human resources representative.
Preexisting Condition Period: The 90-day period just before your insurance becomes effective
Exclusion Period: 12 months
Preexisting Condition Waiver
The Standard may pay benefits for up to 90 days even if you have a preexisting condition. After 90 days, The Standard will continue benefits only if the preexisting condition exclusion does not apply.
Own Occupation Period
For the plan’s definition of disability, as described in your brochure, the own occupation period is the first 24 months for which LTD benefits are paid.
Any Occupation Period
The any occupation period begins at the end of the own occupation period and continues until the end of the maximum benefit period.
Option Accidental Injury Other Disability Maximum Benefit Period 1 0 days 7 days To SSNRA for Sickness & Accident 2 14 days 14 days To SSNRA for Sickness & Accident 3 30 days 30 days To SSNRA for Sickness & Accident 4 60 days 60 days To SSNRA for Sickness & Accident
90 days 90 days To SSNRA for Sickness & Accident
180 days 180 days To SSNRA for Sickness & Accident
5
6
Maximum Benefit Period
Age
22
Other LTD Features
Employee Assistance Program (EAP) – This program offers support, guidance and resources that can help an employee resolve personal issues and meet life’s challenges.
Family Care Expense Adjustment – Disabled employees faced with the added expense of family care when returning to work may receive combined income from LTD benefits and work earnings in excess of 100 percent of indexed predisability earnings during the first 12 months immediately after a disabled employee’s return to work.
Special Dismemberment Provision – If an employee suffers a lost as a result of an accident, the employee will be considered disabled for the applicable Minimum Benefit Period and can extend beyond the end of the Maximum Benefit Period
Reasonable Accommodation Expense Benefit – Subject to The Standard’s prior approval, this benefit allows us to pay up to $25,000 of an employer’s expenses toward work-site modifications that result in a disabled employee’s return to work.
Survivor Benefit – A Survivor Benefit may also be payable. This benefit can help to address a family’s financial need in the event of the employee’s death.
Return to Work (RTW) Incentive – The Standard’s RTW Incentive is one of the most comprehensive in the employee benefits history. For the first 12 months after returning to work, the employee’s LTD benefit will not be reduced by work earnings until work earnings plus the LTD benefit exceed 100 percent of predisability earnings. After that period, only 50 percent of work earnings are deducted.
Rehabilitation Plan Provision – Subject to The Standard’s prior approval, rehabilitation incentives may include training and education expense, family (child and elder) care expenses, and job-related and job search expenses.
When Benefits End
LTD benefits end automatically on the earliest of:
The date you are no longer disabled
The date your maximum benefit period ends
The date you die
The date benefits become payable under any other LTD plan under which you become insured through employment during a period of temporary recovery
The date you fail to provide proof of continued disability and entitlement to benefits
Rates
Employees can select a monthly LTD benefit ranging from a minimum of $300 to a maximum amount based on how much they earn. Referencing the appropriate attached charts, follow these steps to find the monthly cost for your desired level of monthly LTD benefit and benefit waiting period:
1.Find the maximum LTD benefit by locating the amount of your earnings in either the Annual Earnings or Monthly Earnings column. The LTD benefit amount shown associated with these earnings is the maximum amount you can receive. If your earnings fall between two amounts, you must select the lower amount.
2.Select the desired monthly LTD benefit between the minimum of $300 and the determined maximum amount, making sure not to exceed the maximum for your earnings.
3.In the same row, select the desired benefit waiting period to see the monthly cost for that selection.
If you have questions regarding how to determine your monthly LTD benefit, the benefit waiting period, or the premium payment of your desired benefit, please contact your human resources representative.
Group Insurance Certificate
If you become insured, you will receive a group insurance certificate containing a detailed description of the insurance coverage. The information presented above is controlled by the group policy and does not modify it in any way. The controlling provisions are in the group policy issued by Standard Insurance Company.
23
Options 1-6
Annual Earnings Monthly Earnings Monthly Disability Benefit Accident/Sickness Benefit Waiting Period Cost Per Month 0-7 14-14 30-30 60-60 90-90 180-180 3,600 300 200 6.26 5.50 4.66 3.02 2.62 1.92 5,400 450 300 9.39 8.25 6.99 4.53 3.93 2.88 7,200 600 400 12.52 11.00 9.32 6.04 5.24 3.84 9,000 750 500 15.65 13.75 11.65 7.55 6.55 4.80 10,800 900 600 18.78 16.50 13.98 9.06 7.86 5.76 12,600 1,050 700 21.91 19.25 16.31 10.57 9.17 6.72 14,400 1,200 800 25.04 22.00 18.64 12.08 10.48 7.68 16,200 1,350 900 28.17 24.75 20.97 13.59 11.79 8.64 18,000 1,500 1,000 31.30 27.50 23.30 15.10 13.10 9.60 19,800 1,650 1,100 34.43 30.25 25.63 16.61 14.41 10.56 21,600 1,800 1,200 37.56 33.00 27.96 18.12 15.72 11.52 23,400 1,950 1,300 40.69 35.75 30.29 19.63 17.03 12.48 25,200 2,100 1,400 43.82 38.50 32.62 21.14 18.34 13.44 27,000 2,250 1,500 46.95 41.25 34.95 22.65 19.65 14.40 28,800 2,400 1,600 50.08 44.00 37.28 24.16 20.96 15.36 30,600 2,550 1,700 53.21 46.75 39.61 25.67 22.27 16.32 32,400 2,700 1,800 56.34 49.50 41.94 27.18 23.58 17.28 34,200 2,850 1,900 59.47 52.25 44.27 28.69 24.89 18.24 36,000 3,000 2,000 62.60 55.00 46.60 30.20 26.20 19.20 37,800 3,150 2,100 65.73 57.75 48.93 31.71 27.51 20.16 39,600 3,300 2,200 68.86 60.50 51.26 33.22 28.82 21.12 41,400 3,450 2,300 71.99 63.25 53.59 34.73 30.13 22.08 43,200 3,600 2,400 75.12 66.00 55.92 36.24 31.44 23.04 45,000 3,750 2,500 78.25 68.75 58.25 37.75 32.75 24.00 46,800 3,900 2,600 81.38 71.50 60.58 39.26 34.06 24.96 48,600 4,050 2,700 84.51 74.25 62.91 40.77 35.37 25.92 50,400 4,200 2,800 87.64 77.00 65.24 42.28 36.68 26.88 52,200 4,350 2,900 90.77 79.75 67.57 43.79 37.99 27.84 54,000 4,500 3,000 93.90 82.50 69.90 45.30 39.30 28.80 55,800 4,650 3,100 97.03 85.25 72.23 46.81 40.61 29.76 57,600 4,800 3,200 100.16 88.00 74.56 48.32 41.92 30.72 59,400 4,950 3,300 103.29 90.75 76.89 49.83 43.23 31.68 61,200 5,100 3,400 106.42 93.50 79.22 51.34 44.54 32.64 63,000 5,250 3,500 109.55 96.25 81.55 52.85 45.85 33.60 64,800 5,400 3,600 112.68 99.00 83.88 54.36 47.16 34.56 66,600 5,550 3,700 115.81 101.75 86.21 55.87 48.47 35.52 68,400 5,700 3,800 118.94 104.50 88.54 57.38 49.78 36.48 70,200 5,850 3,900 122.07 107.25 90.87 58.89 51.09 37.44 72,000 6,000 4,000 125.20 110.00 93.20 60.40 52.40 38.40 73,800 6,150 4,100 128.33 112.75 95.53 61.91 53.71 39.36 24
Options 1-6 (Continued)
Annual Earnings Monthly Earnings Monthly Disability Benefit Accident/Sickness Benefit Waiting Period Cost Per Month 0-7 14-14 30-30 60-60 90-90 180-180 75,600 6,300 4,200 131.46 115.50 97.86 63.42 55.02 40.32 77,400 6,450 4,300 134.59 118.25 100.19 64.93 56.33 41.28 79,200 6,600 4,400 137.72 121.00 102.52 66.44 57.64 42.24 81,000 6,750 4,500 140.85 123.75 104.85 67.95 58.95 43.20 82,800 6,900 4,600 143.98 126.50 107.18 69.46 60.26 44.16 84,600 7,050 4,700 147.11 129.25 109.51 70.97 61.57 45.12 86,400 7,200 4,800 150.24 132.00 111.84 72.48 62.88 46.08 88,200 7,350 4,900 153.37 134.75 114.17 73.99 64.19 47.04 90,000 7,500 5,000 156.50 137.50 116.50 75.50 65.50 48.00 91,800 7,650 5,100 159.63 140.25 118.83 77.01 66.81 48.96 93,600 7,800 5,200 162.76 143.00 121.16 78.52 68.12 49.92 95,400 7,950 5,300 165.89 145.75 123.49 80.03 69.43 50.88 97,200 8,100 5,400 169.02 148.50 125.82 81.54 70.74 51.84 99,000 8,250 5,500 172.15 151.25 128.15 83.05 72.05 52.80 100,800 8,400 5,600 175.28 154.00 130.48 84.56 73.36 53.76 102,600 8,550 5,700 178.41 156.75 132.81 86.07 74.67 54.72 104,400 8,700 5,800 181.54 159.50 135.14 87.58 75.98 55.68 106,200 8,850 5,900 184.67 162.25 137.47 89.09 77.29 56.64 108,000 9,000 6,000 187.80 165.00 139.80 90.60 78.60 57.60 109,800 9,150 6,100 190.93 167.75 142.13 92.11 79.91 58.56 111,600 9,300 6,200 194.06 170.50 144.46 93.62 81.22 59.52 113,400 9,450 6,300 197.19 173.25 146.79 95.13 82.53 60.48 115,200 9,600 6,400 200.32 176.00 149.12 96.64 83.84 61.44 117,000 9,750 6,500 203.45 178.75 151.45 98.15 85.15 62.40 118,800 9,900 6,600 206.58 181.50 153.78 99.66 86.46 63.36 120,600 10,050 6,700 209.71 184.25 156.11 101.17 87.77 64.32 122,400 10,200 6,800 212.84 187.00 158.44 102.68 89.08 65.28 124,200 10,350 6,900 215.97 189.75 160.77 104.19 90.39 66.24 126,000 10,500 7,000 219.10 192.50 163.10 105.70 91.70 67.20 127,800 10,650 7,100 222.23 195.25 165.43 107.21 93.01 68.16 129,600 10,800 7,200 225.36 198.00 167.76 108.72 94.32 69.12 131,400 10,950 7,300 228.49 200.75 170.09 110.23 95.63 70.08 133,200 11,100 7,400 231.62 203.50 172.42 111.74 96.94 71.04 135,000 11,250 7,500 234.75 206.25 174.75 113.25 98.25 72.00 136,800 11,400 7,600 237.88 209.00 177.08 114.76 99.56 72.96 138,600 11,550 7,700 241.01 211.75 179.41 116.27 100.87 73.92 140,400 11,700 7,800 244.14 214.50 181.74 117.78 102.18 74.88 142,200 11,850 7,900 247.27 217.25 184.07 119.29 103.49 75.84 144,000 12,000 8,000 250.40 220.00 186.40 120.80 104.80 76.80 25
San Marcos CISD
Employee Assistance Program (EAP)
AWP is proud to serve as your EAP, offering you and your household valuable, confidential services at no cost to you.


or any issue affecting your quality of life.
YourEAP Benefits:
All benefits can be accessed by calling: toll free 1-800-343-3822
for our deaf and hearing impaired callers, please dial 7 – 1 - 1 teen line
1-800-334-TEEN (8336)
We are available totake your call 24 hours a day,7 days a week.
LawAccess
Legal and Financial services provided by a lawyer or financial professional specializing in your area of concern. Available online or by telephone.
HelpNet


Customized EAP website featuring resources, skill-building tools, online assessments and referrals.

WorkLife
Resources and referrals for everyday needs. Available by telephone.
SafeRide
Reimbursement for emergency cab fare for eligible employees and dependents that opt to use a cab service instead of driving while impaired.
1 to 6 Counseling Sessions
Per problem, per year. Short-term counseling sessions which include assessment, referral, and crisis services. Newsletters
Registration Code: AWP-SMCISD-5478
Alliance Work Partners is a professional service of Workers Assistance Program, Inc. Copyright © 2022 Workers Assistance Program, Inc. Confidential and proprietary. All rights reserved.
Alliance Work Partners is here for you as life happens.
Visit your EAP website at awpnow.com and create a customized account. Go to
Your benefits are designed to help you manage daily responsibilities, major events, work stresses,
https://www.awpnow.com Select “Access Your Benefits”
Training Series
26
Webinar
Tips for Everyday Living
Criteria for Benefits Eligibility
Full Benefits:
• Employee, retiree, married/divorced spouse, partner, significant other
• Any household member, regardless of age or relationship, residing in employee’s home, including significant other and their children
• All covered employees may bring anyone with them to their authorized/covered sessions regardless of relationship to employee.
• Children and grandchildren, age 26 or under, residing in US or Puerto Rico. This includes children and grandchildren of significant other or partner.
• Any person meeting benefit eligibility prior to lay-off or termination of an employee will continue to be eligible for benefits up to 6 months from the date of employee’s lay-off or termination. Benefits are extended for 6 months from date of employee's call within this timeframe.
Assessment & Referral:
• Children and grandchildren age 27 and overof employee, married/divorced spouse, partner, or significant other living outside employee’s home
• Employee instructed by law to receive courtordered counseling

• All crisis cases (suicidal/homicidal, domestic violence, chemical dependence, substance abuse, child/elderly abuse) not otherwise covered
• Any person meeting benefit eligibility prior to lay-off or termination of an employee will continue to be eligible for assessment and referral after 6 months and up to 1 year from the date of employee’s lay-off or termination. Benefits are extended 1 year from date of employee's call within this timeframe.




Information & Referral:
• Anyone contacting Alliance Work Partners regardless of contract status

Children under the age of 18 must have a written, signed release by their guardian who has custody (whether living in the home or not) to attend counseling on their own. This release is given to their affiliate provider. Divorced parents who bring their children in for counseling mustbring a copy of their divorce decree or have signed permission from the other parent before bringing a child into counseling. Grandparents who bring their grandchildren into counseling must have proof of guardianship or written permission from the child’sparents.

Alliance Work Partners is a professional service of Workers Assistance Program, Inc. Copyright © 2022 Workers Assistance Program, Inc. Confidential and proprietary. All rights reserved.
Program (EAP)
Marcos CISD 27
Employee Assistance
San
life insurance you can keep!
purelife-plus


You own it
QUICK QUESTIONS 3

You can qualify by answering just 3 questions – no exams or needles.
DURING THE LAST SIX MONTHS, HAS THE PROPOSED INSURED:
Been actively at work on a full time basis, performing usual duties?
Been absent from work due to illness or medical treatment for a period of more than 5 consecutive working days?

FlexiblePremiumAdjustableLifeInsurancetoage121.PolicyFormICC18PRFNG-NI-18orFormSeriesPRFNG-NI-18.Somelimitationsapply.Seethe PureLife-plusbrochurefordetails.TexasLifeislicensedtodobusinessinthe DistrictofColumbiaandeverystatebutNewYork.


19M016-C1092(exp0321)

Been disabled or received tests, treatment or care of any kind in a hospital or nursing home or received chemotherapy, hormonal therapy for cancer, radiation, dialysis treatment, or treatment for alcohol or drug abuse?
Life insurance can be an ideal way to provide money for your family when they need it most. purelife-plus offers permanent insurance with a high death benefit and long guarantees1 that can provide financial peace of mind for you and your loved ones. purelife-plus is an ideal complement to any group term and optional term life insurance your employer might provide and has the following features: 1. Aftertheguaranteeperiod,premiumsmaygodown,staythesameorgoup. 2. CoveragenotavailableonchildreninWAorongrandchildreninWAorMD. InMD,childrenmustresidewiththeapplicanttobeeligibleforcoverage. 3.

Conditionsapply.
1 2 3
it
you when you change jobs or retire
it through
payroll deductions
You can take
with
You pay for
convenient
cover your spouse, children and grandchildren, too2
can get a living benefit if you become terminally ill3 It’s Affordable 28
You can
You
PureLife-plusispermanentlifeinsurancetoAttainedAge121thatcanneverbecancelledaslongasyoupaythenecessarypremiums.Afterthe GuaranteedPeriod,thepremiumscanbelower,thesame,orhigherthantheTablePremium.Seethebrochureunder”PermanentCoverage”.
monthlypremiums
StandardRiskTablePremiums Non-Tobacco ExpressIssue GUARANTEED MonthlyPremiumsforLifeInsuranceFaceAmountsShown PERIOD IncludesAddedCostfor AgetoWhich Issue AccidentalDeathBenefit(Ages17-59) Coverageis Age Guaranteedat (ALB) $10,000 $15,000 $25,000 $40,000 $50,000 $75,000 $100,000 $125,000 $150,000 TablePremium 15D-1 8.00 83 2-3 8.25 83 4-10 8.50 79 11-16 8.75 75 17-20 10.75 15.85 19.25 27.75 36.25 44.75 53.25 73 21-22 11.00 16.25 19.75 28.50 37.25 46.00 54.75 73 23-25 11.25 16.65 20.25 29.25 38.25 47.25 56.25 71 26 11.50 17.05 20.75 30.00 39.25 48.50 57.75 72 27 11.75 17.45 21.25 30.75 40.25 49.75 59.25 72 28 11.75 17.45 21.25 30.75 40.25 49.75 59.25 71 29 12.00 17.85 21.75 31.50 41.25 51.00 60.75 71 30-31 12.25 18.25 22.25 32.25 42.25 52.25 62.25 70 32 12.75 19.05 23.25 33.75 44.25 54.75 65.25 70 33 13.25 19.85 24.25 35.25 46.25 57.25 68.25 71 34 13.75 20.65 25.25 36.75 48.25 59.75 71.25 72 35 9.60 14.50 21.85 26.75 39.00 51.25 63.50 75.75 73 36 9.90 15.00 22.65 27.75 40.50 53.25 66.00 78.75 73 37 10.20 15.50 23.45 28.75 42.00 55.25 68.50 81.75 73 38 10.65 16.25 24.65 30.25 44.25 58.25 72.25 86.25 74 39 11.25 17.25 26.25 32.25 47.25 62.25 77.25 92.25 75 40 8.65 11.85 18.25 27.85 34.25 50.25 66.25 82.25 98.25 76 41 9.15 12.60 19.50 29.85 36.75 54.00 71.25 88.50 105.75 77 42 9.85 13.65 21.25 32.65 40.25 59.25 78.25 97.25 116.25 78 43 10.55 14.70 23.00 35.45 43.75 64.50 85.25 106.00 126.75 80 44 11.25 15.75 24.75 38.25 47.25 69.75 92.25 114.75 137.25 81 45 12.05 16.95 26.75 41.45 51.25 75.75 100.25 124.75 149.25 82 46 12.85 18.15 28.75 44.65 55.25 81.75 108.25 134.75 161.25 83 47 13.55 19.20 30.50 47.45 58.75 87.00 115.25 143.50 171.75 83 48 14.35 20.40 32.50 50.65 62.75 93.00 123.25 153.50 183.75 84 49 15.25 21.75 34.75 54.25 67.25 99.75 132.25 164.75 197.25 85 50 16.35 23.40 37.50 58.65 72.75 108.00 86 51 17.65 25.35 40.75 63.85 79.25 117.75 87 52 19.25 27.75 44.75 70.25 87.25 129.75 88 53 20.85 30.15 48.75 76.65 95.25 141.75 90 54 21.95 31.80 51.50 81.05 100.75 150.00 90 55 22.95 33.30 54.00 85.05 105.75 157.50 91 56 23.95 34.80 56.50 89.05 110.75 165.00 91 57 25.05 36.45 59.25 93.45 116.25 173.25 91 58 26.25 38.25 62.25 98.25 122.25 182.25 91 59 27.35 39.90 65.00 102.65 127.75 190.50 91 60 28.05 40.95 66.75 105.45 131.25 195.75 91 61 29.55 43.20 70.50 111.45 138.75 207.00 91 62 31.15 45.60 74.50 117.85 146.75 219.00 92 63 32.85 48.15 78.75 124.65 155.25 231.75 92 64 34.65 50.85 83.25 131.85 164.25 245.25 92 65 36.55 53.70 88.00 139.45 173.75 259.50 92 66 38.65 92 67 40.95 92 68 43.45 92 69 46.05 93 70 48.65 93
Non-Tobacco
PureLife-plus
29
Form:18M049-ICCEXP-A-M-1AD
PureLife-plusispermanentlifeinsurancetoAttainedAge121thatcanneverbecancelledaslongasyoupaythenecessarypremiums.Afterthe GuaranteedPeriod,thepremiumscanbelower,thesame,orhigherthantheTablePremium.Seethebrochureunder”PermanentCoverage”.
Tobacco monthlypremiums
GUARANTEED MonthlyPremiumsforLifeInsuranceFaceAmountsShown PERIOD IncludesAddedCostfor AgetoWhich Issue AccidentalDeathBenefit(Ages17-59) Coverageis Age Guaranteedat (ALB) $10,000 $15,000 $25,000 $40,000 $50,000 $75,000 $100,000 $125,000 $150,000 TablePremium 15D-1 83 2-3 83 4-10 79 11-16 75 17-20 15.00 22.65 27.75 40.50 53.25 66.00 78.75 70 21-22 15.50 23.45 28.75 42.00 55.25 68.50 81.75 70 23-25 16.25 24.65 30.25 44.25 58.25 72.25 86.25 69 26 16.50 25.05 30.75 45.00 59.25 73.50 87.75 69 27 16.75 25.45 31.25 45.75 60.25 74.75 89.25 68 28 17.00 25.85 31.75 46.50 61.25 76.00 90.75 68 29 17.25 26.25 32.25 47.25 62.25 77.25 92.25 68 30-31 19.25 29.45 36.25 53.25 70.25 87.25 104.25 69 32 19.75 30.25 37.25 54.75 72.25 89.75 107.25 69 33 20.00 30.65 37.75 55.50 73.25 91.00 108.75 69 34 20.25 31.05 38.25 56.25 74.25 92.25 110.25 68 35 13.80 21.50 33.05 40.75 60.00 79.25 98.50 117.75 69 36 14.25 22.25 34.25 42.25 62.25 82.25 102.25 122.25 69 37 15.00 23.50 36.25 44.75 66.00 87.25 108.50 129.75 70 38 15.45 24.25 37.45 46.25 68.25 90.25 112.25 134.25 70 39 16.35 25.75 39.85 49.25 72.75 96.25 119.75 143.25 70 40 12.55 17.70 28.00 43.45 53.75 79.50 105.25 131.00 156.75 72 41 13.25 18.75 29.75 46.25 57.25 84.75 112.25 139.75 167.25 73 42 14.15 20.10 32.00 49.85 61.75 91.50 121.25 151.00 180.75 74 43 15.55 22.20 35.50 55.45 68.75 102.00 135.25 168.50 201.75 76 44 16.35 23.40 37.50 58.65 72.75 108.00 143.25 178.50 213.75 77 45 17.45 25.05 40.25 63.05 78.25 116.25 154.25 192.25 230.25 78 46 18.45 26.55 42.75 67.05 83.25 123.75 164.25 204.75 245.25 79 47 19.45 28.05 45.25 71.05 88.25 131.25 174.25 217.25 260.25 79 48 20.45 29.55 47.75 75.05 93.25 138.75 184.25 229.75 275.25 80 49 22.05 31.95 51.75 81.45 101.25 150.75 200.25 249.75 299.25 82 50 23.15 33.60 54.50 85.85 106.75 159.00 82 51 24.85 36.15 58.75 92.65 115.25 171.75 83 52 26.95 39.30 64.00 101.05 125.75 187.50 85 53 28.65 41.85 68.25 107.85 134.25 200.25 87 54 30.05 43.95 71.75 113.45 141.25 210.75 87 55 31.45 46.05 75.25 119.05 148.25 221.25 87 56 33.05 48.45 79.25 125.45 156.25 233.25 87 57 34.55 50.70 83.00 131.45 163.75 244.50 87 58 36.35 53.40 87.50 138.65 172.75 258.00 87 59 37.85 55.65 91.25 144.65 180.25 269.25 87 60 38.85 57.15 93.75 148.65 185.25 276.75 87 61 41.45 61.05 100.25 159.05 198.25 296.25 88 62 43.85 64.65 106.25 168.65 210.25 314.25 88 63 46.15 68.10 112.00 177.85 221.75 331.50 88 64 48.45 71.55 117.75 187.05 233.25 348.75 89 65 50.85 75.15 123.75 196.65 245.25 366.75 89 66 53.45 89 67 56.25 89 68 59.15 89 69 62.25 89 70 65.55 90
PureLife-plus StandardRiskTablePremiums Tobacco ExpressIssue
30
Form:18M049-ICCEXP-A-M-1AD
San Marcos Consolidated Independent School Districtprovides this valuable benefitat no cost to you.


Safeguard the most important people in your life.
AT A GLANCE: Accident PlusLifeKeys TravelConnect
ADDITIONAL DETAILS
Conversion:
Continuation of Coverage:
Benefit Reduction:
EmployeeConnect LifeKeys TravelConnect
31

Supplemental Life and AD&D Insurance The Lincoln Term Life and AD&D Insurance Plan: LifeKeys TravelConnect San Marcos Consolidated Independent School District Benefits At-A-Glance Employee
/ Domestic Partner
Children 32
Spouse
Dependent
What your benefits cover
Employee Coverage
Guaranteed Life and AD&D Insurance Coverage Amount
Maximum Life Insurance Coverage Amount
Spouse / Domestic Partner Coverage -
Guaranteed Life and AD&D Insurance Coverage Amount
Maximum Life Insurance Coverage Amount
Dependent Children Coverage -
Guaranteed Life Insurance Coverage Options:
33
Additional Plan Benefits
Benefit Exclusions

Questions?
LifeKeys
TravelConnect
34
Note: Rates are subject to change and can vary over time. Group
Note: Rates are subject to change and can vary over time.
Monthly Supplemental Life and AD&D Insurance Premium Here’s how little you pay with group rates.
Rates for You =
Group
Rates for Your Spouse / Domestic Partner =
Dependent Children Monthly Premium for Life Insurance Coverage Group Rates for Your Dependent Children 35

The following is not an exhaustive list of terms and conditions but only serves as a depiction of benefits and exclusions. Interested parties should consult the contract for a complete listing of terms and conditions. Toll Free: 1-800-366-8354 A Promise A New Dimension in Supplemental Cancer Insurance Toll Free: 1-877-523-0176 36
BASE POLICY BENEFITS
BENEFIT PROVISIONS. We will pay the benefits described in the Certificate for the treatment of an Insured Person’s Cancer, provided he or she is covered under an issued Certificate which remains in force. Payment will be made in accordance with all applicable policy provisions. Benefits are payable for a positive diagnosis that begins after the Effective Date. The positive diagnosis must be for Cancer as defined in the policy.
1.POSITIVE DIAGNOSIS BENEFIT. We will pay the Actual Charge but not to exceed $300 per Calendar Year for one test that confirms the Positive Diagnosis of Cancer in an Insured Person. This benefit is not payable for multiple diagnoses of the same Cancer or for Cancer that metastasizes or for recurrence of the same Cancer.
2.NATIONAL CANCER INSTITUTE DESIGNATED COMPREHENSIVE CANCER TREATMENT CENTER EVALUATION/CONSULTATION BENEFIT We will pay the Actual Charge, but not to exceed a lifetime maximum of $750 , if an Insured Person is diagnosed with Internal Cancer and seeks evalu ation or consultation from a National Cancer Institute designated Comprehensive Cancer Treatment Center. If the Comprehensive Cancer Treatment Center is located more than 30 miles from the Insured Person’s place of residence, We will also pay the transportation and lodging expenses incurred but not to exceed a lifetime maximum of $350 . This benefit is not payable on the same day a Second or Third Surgical Opinion Benefit is payable and is in lieu of the Non-Local Transportation and Lodging Expense Benefits of the Policy. This benefit is payable one time during the lifetime of the Insured Person.
3.SECOND AND THIRD SURGICAL OPINION EXPENSE BENEFIT We will pay the Actual Charge for a written second surgical opinion concerning the recommendation of Cancer surgery and if the second surgical opinion is in conflict with that of the Physician originally recommending the surgery and the Insured Person desires a third opinion, We will the Actual Charge for a written third surgical opinion. The Physician providing the second or third surgical opinion cannot be associated with the Physician who orig inally recommended the surgery. This benefit is not payable the same day the National Cancer Institute Evaluation/Consulting Benefit is payable.
4.MEDICAL IMAGING, TREATMENT PLANNING AND MONITORING EXPENSE BENEFIT We will pay the Actual Charge, but not to exceed $1,000 per Calendar Year, for laboratory tests, diagnostic X-rays, medical images, when used in Cancer treatment plannings related to Radiation Treatment, Chemotherapy or Immunotherapy.
5. ANTI-NAUSEA MEDICATION EXPENSE BENEFIT We will pay the Actual Charge for anti-nausea medication, but not to exceed $150 per calendar month , when an Insured Person is prescribed such medication as the result of Radiation Treatmen t, Chemotherapy or Immunotherapy treatments for Cancer.
6. COLONY STIMULATING FACTOR OR IMMUNOGLOBULIN EXPENSE BENEFIT We will pay the Actual Charge but not to exceed $1,000 per Calendar Month for Colony Stimulating Factor Drugs or Immunoglobulins presc ribed by a Physician or Oncologist during an Insured Person’s Cancer treatment regimen for which benefits are payable unde r the Radiation, Chemotherapy and Immunotherapy Benefit of this Policy or rider attached to it.
7.OUTPATIENT HOSPITAL OR AMBULATORY SURGICAL CENTER EXPENSE BENEFIT We will pay the Actual Charge from an Ambulatory Surgical Center or Outpatient department of a Hospital for the use of its facilities for the performance of a surgical procedure covered under this Policy but not to exceed $350 per day.
8.PROSTHESIS
EXPENSE BENEFIT
(A.) Surgically Implanted Breast Prosthesis We will pay the Actual Charge for a surgically implanted prosthetic device required and prescribed to restore normal body contour lost as the direct result of an Insured Person’s breast removal for the treatment of Cancer. The Surgically Implanted Breast Prosthesis Benefit does not include coverage for breast reconstruction surgery which may be covered under the Surgical Schedule within the Surgical and Anesthesia Benefits Rider.
(B.) Non-Surgically Implanted Prosthesis We will pay the Actual Charge incurred not to exceed $2,000 per amputation for an artificial limb
or other non-surgically implanted prosthetic device that is prescribed and required to restore normal body function lost as the direct result of an Insured Person’s amputation for the treatment of Cancer . We will pay a lifetime maximum of $2,000 per amputation The cost of replacement of a prosthetic device is not covered. Hairpieces or wigs are not covered under this benefit.
9.NON-LOCAL TRANSPORTATION EXPENSE BENEFIT We will pay the Actual Charge, but not to exceed the coach fare on a Common Carrier for the Insured Person and one adult companion’s travel to a Hospital, Radiation Therapy Treatment Cen ter, Chemotherapy Treatment Center, Oncology Clinic or any other specialized treatment center where the Insured Person receives tr eatment for Cancer. This benefit is payable only if the treatment is not available Locally but is available Non-Locally. The adult companion may include the live donor of bone marrow or stem cells used in a bone marrow or stem cell transplant for the Insured Person. At the option of the Insured Person, We will pay a single private vehicle mileage allowance of $.50 per mile for Non-Local transportation in lieu of the common carrier coach fare.
37
10.LODGING EXPENSE BENEFIT We will pay the Actual Charge not to exceed $75 per day for a room in a motel, hotel or other appropriate lodging facility (other than a private residence), when an Insured Person receives treatment for Cancer at a Non-Local Hospital, Radiation Therapy Treatment Center, Chemother apy Treatment Center, Oncology Clinic or any other specialized treatment center. The room must be occupied by the Insured Person or an a dult companion which may include the live donor of bone marrow or stem cells used in a bone marrow or stem cell transplant for the Insured Person. This benefit is not payable for lodging expense incurred more than 24 hours before the treatment nor for lodging expense incurred more than 24 hours following treatment. This benefit is limited to 100 days per Calendar Year
11.INPATIENT BLOOD, PLASMA AND PLATELETS EXPENSE BENEFIT We will pay the Actual Charge not to exceed $300 per day for the procurement cost, administration, processing and cross matching of b lood, plasma or platelets administered to an Insured Person in the treatment of Cancer while an Inpatient.
12.OUTPATIENT BLOOD, PLASMA AND PLATELETS EXPENSE BENEFIT We will pay the Actual Charge not to exceed $300 per day for the procurement cost, administration, processing and cross matching of blood, plasma or platelets administered to an Insured Person in the treatment of Cancer while an Outpatient.
13.BONE MARROW DONOR EXPENSE BENEFIT We will pay the Daily Hospital Confinement Benefit shown on the Certificate Schedule for each day a live donor, other than the Insured Person, is confined in a Hospital for the harvesting of bone marrow or stem cells used in a bone marrow or stem cell tr ansplant for the treatment of an Insured Person’s Cancer.
14.BONE MARROW OR STEM CELL TRANSPLANT EXPENSE BENEFIT We will pay the Actual Charge not to exceed a lifetime maximum of $15,000 for surgical and anesthesia procedures (including the harvesting and subsequent re-infusion of blood cells or peripheral stem cells) performed for a bone marrow transplant and/or a peripheral stem cell transplant for the treatment of an Insured Person’s Cancer. This benefit will be paid in lieu of the Surgical Expense Benefit and the Anesthesia Expense Benefit which may be described in a rider attached to an issued Certificate.
15.AMBULANCE EXPENSE BENEFIT We will pay the Actual Charge for ambulance service if an Insured Persons is transported to a Hospital where he or she is admitted as an inpatient for the treatment of Cancer . The ambulance service must be provided by a licensed professional ambulance company or an ambulance owned by the Hospital.
16.INPATIENT OXYGEN EXPENSE BENEFIT We will pay the Actual Charge not to exceed $300 per Hospital confinement for oxygen prescribed by a Physician and received by an Insured Person while confined in a Hospital for the treatment of Cancer
17.ATTENDING PHYSICIAN EXPENSE BENEFIT We will pay the Actual Charge not to exceed $40 per day for the professional services of a Physician or Oncologist rendered to an Insured Person while he or she is confined in a Hospital fo r the treatment of Cancer. This benefit is payable only if the Physician or Oncologist personally visits the Hospital room occupied by the Insured Person and the amount stated is the maximum amount that will be payable for each day of Hospital confinement regardless of the number of visits made by one or more Physicians or Oncologists.
18.INPATIENT PRIVATE DUTY NURSING EXPENSE BENEFIT We will pay the Actual Charge not to exceed $150 per day for the full time service of a Nurse that is required and ordered by a Physician when an Insured Person is confined in a Hosp ital for the treatment of Cancer. The Nurse must provide services other than those normally provided by the Hospital and the Nurse may not be an employee of the Hospital or an Immediate Family Member of the Insured Person.
19.OUTPATIENT PRIVATE DUTY NURSING EXPENSE BENEFIT We will pay the Actual Charge not to exceed $150 per day limited to the same number of days of the prior Hospital confinement for the full time service of a Nurse that is required an d ordered by a Physician when an Insured Person is confined indoors at home as the result of Cancer . This benefit is not payable if the services of the Nurse are custodial in nature or to assist the Insured Person in the activities of daily living. This benefit is not paya ble when the Nurse is a member of the Insured Person’s Immediate Family. Charges mus t begin following a period of Hospital confinement for which benefits are payable under this Certificate.
20.CONVALESCENT CARE FACILITY EXPENSE BENEFIT We will pay the Actual Charge not to exceed $100 per day for an Insured Person’s confinement in a Convalescent Care Facilit y. The maximum number of days for which this benefit is payable will be the number of days in the last Period of Hospital Confinement that immediately preceded admission to a Convalescent Care Facility. The Convalescent Care Facility Confinement must: be due to Cancer ; begin within 14 days after the Insured Person has been discharged from a Hospital for the treatment of Cancer ; be authorized by a Physician as being medically necessary for the treatment of Cancer.
21.RENTAL OR PURCHASE OF MEDICAL EQUIPMENT EXPENSE BENEFIT We will pay the lesser of the Actual Charge not to exceed $1,500 per Calendar Year for either the rental or purchase of covered medical equipment designed for home use, required and ordered by the Insured Person’s attending Physician as the direct result of the treatment of Cancer. Covered medical equipment includes wheel chair, oxygen equipment, respirator, braces, crutches or hospital bed .
38
22.HOME HEALTH CARE EXPENSE BENEFIT We will pay benefits for the following Covered Charges when a Insured Person requires Home Health Care for the treatment of Cancer.
1. Home Health Care Visits - We will pay the Actual Charge for Home Health Care Visits not to exceed $75 for each day on which one or more such visits occur. We will not pay this benefit for more than 60 days in any Calendar Year.
2. Medicine and Supplies - We will pay the Actual Charge not to exceed $450 in any Calendar Yea r for drugs, medicine, and medical supplies provided by or on behalf of a Home Health Care Agency.
3. Services of a Nutritionist - We will pay the Actual Charge not to exceed a lifetime maximum of $300 for the services of a nutritionist to set up programs for special dietary needs.
23.HOSPICE CARE EXPENSE BENEFIT We will pay the Actual Charge for Hospice Care not to exceed $100 per day , when such care is required because of Cancer . This benefit is payable whether confinement is required in a Hospice Center or services are provided in the Insured Person’s home by a Hospice Team. Eligibility for payments will be based on the following conditions being met:(1) the Insured Person has been given a prognosis as being Terminally Ill with an estimated life expectancy of 6 months or less; and (2) We h ave received a written summary of such prognosis from the attending Physician. We will not pay this benefit while the Insured Person is confined to a Hospital or Convalescent Care Facility. The lifetime maximum benefit is 365 days of Hospice Care
24.HAIRPIECE EXPENSE BENEFIT We will pay the Actual Charge not to exceed a lifetime maximum of $150 for the purchase of a wig or hairpiece that is required as the direct result of hair loss due to Cancer treatment
25.PHYSICAL,
SPEECH, AUDIO THERAPY AND PSYCHOTHERAPY EXPENSE BENEFIT
We will pay the Actual Charge not to exceed $25 per therapy session for:
1.Physical therapy treatments given by a license Physical Therapist, or
2.Speech therapy given by a licensed Speech Pathologist/Therapist; or
3.Audio therapy given by a licensed Audiologist; or
4.Psychotherapy given by a licensed Psychologist. These sessions may be given at an institute of physical medicine and rehabilitation, a Hospital, or the Insured Person’s home. These treatments must be given on an Outpatien t basis unless the primary purpose of a Hospital confinement is for treatment of Cancer other than with physical, speech or audio therapy or psychotherapy. Benefits may not exceed $1,000 per Calendar Year.
26.WAIVER OF PREMIUM. We will waive the premiums starting on the first premium due date following a 60 day period of Total Disability of the Named Insured due to Cancer. The Named Insured must: (a) be receiving treatment for such Cancer for which benefits are payable under this Certificate; and (b) remain disabled for 60 consecutive days. We will waive premiums for as long as the Named Insured remains Totally Disabled.
THIS IS A CANCER ONLY POLICY, which should be used to supplement your existing health care protection.
RENEWABILITY. Coverage will terminate when the Group Master Policy terminates or when required premium remains unpaid after expiration of the Grace Period.
PREMIUM RATES. We may change the premium rates for coverage only if we also change the rates for all other Certificates issued under the Group Master Policy.
EXCLUSIONS AND LIMITATIONS. No benefits will be paid under the Certificate or any attached riders for: 1. any loss due to any disease or illness other than Cancer, or a listed covered Specified Disease; 2. care and treatment received outside the territorial limits of the United States; 3. treatment by any program engaged in research that does not meet the criter ia for Experimental Treatment as defined; 4. treatment that has not been approved by a Physician as being medically necessary; or 5. losses or medical expenses incurred prior to the Certificate Effective Date of an Insured Person’s coverage regardless of the Date of Positive Diagnosis.
PRE-EXISTING CONDITIONS LIMITATION. Relative to any Insured Person, We will not pay benefits for expenses resulting from Pre-existing Conditions during the 12 months after coverage becomes effective for such Insured Person.
“Pre-existing Condition” means Cancer, or a listed Specified Disease if that optional rider is issued, which was diagnosed by a Physician or for which medical consultation, advice or treatment was recommended by or received from or sought from a Physician within 1 year prior to the effective date of coverage for each Insured Person.
Insurance coverage is provided by form number series LG- 6040 and associated riders. This advertisement highlights some features of the Certificate and riders, but is not the insurance contract. An is sued Master Group Policy, Certificate and riders set forth, i n detail, the rights and obligations of both the insured and the insu rance company. Please read the policy, certificate and riders for detailed coverage information.
39
ANNUAL CANCER SCREENING BENEFIT RIDER (form LG-6041) A.Basic Benefit B.Additional Benefit
FIRST OCCURRENCE BENEFIT RIDER (form LG-6043)
ANNUAL RADIATION, CHEMOTHERAPY, IMMUNOTHERAPY and EXPERIMENTAL TREATMENT BENEFIT RIDER (form LG-6045)
SURGICAL BENEFIT RIDER (form LG-6048) Surgical
the
issued.
DAILY HOSPITAL CONFINEMENT BENEFIT RIDER (form LG-6042)
Confinements of 30 Days or Less
Confinements of 31 Days or More
Benefits for an Insured Dependent Child under Age 21 double the Daily Hospital Confinement benefit
ADDITIONAL BENEFITS AMOUNTS LEVEL A Maximum LEVEL B Maximum
$100 Per Calendar Year $200 Per Calendar Year $100 Per Calendar Year $200 Per Calendar Year
$1,000 Once per Lifetime $1,500 Once per Lifetime $3,000 Once per Lifetime $4,500 Once per Lifetime
$5,000 Per Calendar Year $20,000 Per Calendar Year
$1,500 Procedure Maximum $3,000 Procedure Maximum Anesthesia Expense $375 Procedure Maximum $750 Procedure Maximum Breast Reconstruction $900
$1,350 Procedure Maximum Per Procedure $2,700 Procedure Maximum Per Procedure
Expense
per $1,000 of
Surgical Benefit
Skin Cancer Surgery Expense ($125 to $750 depending on the procedure)
$200 Per Day $400 Per Day $400/ $800 Per Day $300 Per Day $600 Per Day $600/ $1,200 Per Day 40
Specified Disease Benefit
SPECIFIED DISEASE BENEFIT RIDER (form LG-6052)
COVERS THESE 38 SPECIFIED DISEASES
Addison’s Disease
Amyotrophic Lateral Sclerosis
Botulism
Bovine Spongiform Encephalopathy
Lupus ErythematosusRocky Mountain Spotted Fever
MalariaSickle Cell Anemia
MeningitisTay-Sachs Disease
Multiple SclerosisTetanus
Budd-Chiari SyndromeMuscular DystrophyToxic Epidermal Necrolysis
Cystic Fibrosis
Diptheria
Encephalitis
Epilepsy
Hansen’s Disease
Myasthenia GravisTuberculosis
Neimann-Pick DiseaseTularemia
OsteomyelitisTyphoid Fever
PoliomyelitisUndulant Fever
Q FeverWest Nile Virus
Histoplasmosis Rabies
Legionnaire’s Disease
Lyme Disease
Reye’s Syndrome
Rheumatic Fever
BENEFITS
Whipple’s Disease
Whooping Cough
coverage
rates. Initial Hospitalization Benefit $1,500 per unit of coverage Hospital Confinement Benefit $300 per day per unit of coverage double per day beginning with
31st
of continuous confinement. Individual Coverage Single Parent Family Coverage 41
Oneunit of
is included for the premium
the
day
Optional Rider – Hospital Intensive Care Unit Benefit Rider
*Additional Limitations and Exclusions for the Hospital Intensive Care Unit Benefit Rider
ALL BENEFITS CONTAINED IN THIS HOSPITAL INTENSIVE CARE UNIT BENEFIT RIDER REDUCE BY ONE -HALF AT AGE 75.
Hospital Intensive Care Unit Rider $500 Daily ICU Benefit $1,000 Daily ICU Benefit Individual Single Parent Family Family
INTENSIVE CARE
BENEFIT
(form LG-6047)* Intensive Care Unit Benefit Double Intensive Care Unit Benefit Step Down Unit Benefit $500 Per Day $1,000 Per Day $250 Per Day $1,000 Per Day $2,000 Per Day $500 Per Day
HOSPITAL
UNIT
RIDER
42
Critical Illness Insurance Plan Summary
COVERAGE OPTIONS
Employee$10,000 or $20,000
Spouse/Domestic Partner1
Coverage is guaranteed provided you are actively at work.3
100%of the employee’s Initial Benefit Coverage is guaranteed provided the employee is actively at workand the spouse/domestic partner is not subject to a medical restriction as set forth on the enrollment form and in the Certificate.3
Dependent Child(ren)2 100%ofthe employee’s Initial Benefit Coverage is guaranteed provided the employee is actively at workand the dependent is not subject to a medical restriction as set forth on the enrollment form and in the Certificate.3
BENEFIT PAYMENT
Your Initial Benefit provides a lump-sum payment upon the first diagnosis of a Covered Condition. Your plan pays a Recurrence Benefit4 for the following Covered Conditions: Heart Attack, Stroke, Coronary Artery Bypass Graft, Full Benefit Cancer and Partial Benefit Cancer. A Recurrence Benefitis only available if an Initial Benefit has been paid for the Covered Condition. There is a Benefit Suspension Period between Recurrences.
The maximum amount that you can receive through your Critical Illness Insurance plan is called the Total Benefit and is 3 times the amount of your Initial Benefit. This means that you can receive multiple Initial Benefit and Recurrence Benefit payments until you reach the maximum of 300% or $30,000or $60,000.
Please refer to the table below for the percentage benefit amount for each Covered Condition.
22 Listed Conditions
MetLife Critical Illness Insurance will pay 25% of the Initial Benefit Amount for each of the 22 Listed Conditions until the Total Benefit Amount is reached. A Covered Person may only receive one payment for each Listed Condition in his/her lifetime. The Listed Conditions are Addison’s disease (adrenal hypofunction); amyotrophic lateral sclerosis (Lou Gehrig’s disease); cerebrospinal meningitis (bacterial); cerebral palsy; cystic fibrosis; diphtheria; encephalitis; Huntington’s disease (Huntington’s chorea); Legionnaire’s disease;malaria; multiple sclerosis (definitive diagnosis); muscular dystrophy; myasthenia gravis; necrotizing fasciitis; osteomyelitis; poliomyelitis; rabies; sickle cell anemia (excluding sickle cell trait); systemic lupus erythematosus (SLE); systemic sclerosis (scleroderma); tetanus; and tuberculosis.
Example of Initial & Recurrence Benefit Payments
The example below illustrates an employee who elected an Initial Benefit of $10,000 and has a Total Benefit of 3 times the Initial Benefit Amount or $30,000.
IndividualInitial Benefit
Critical Illness Insurance Eligible
Requirements
Covered Conditions Initial Benefit Recurrence Benefit Full Benefit Cancer5 100% of Initial Benefit50%of Initial Benefit Partial Benefit Cancer5 25% of Initial Benefit12.5%of Initial Benefit Heart Attack100% of Initial Benefit50%of Initial Benefit Stroke6 100% of Initial Benefit50%of Initial Benefit Coronary Artery Bypass Graft7 100% of Initial Benefit50%of Initial Benefit Kidney Failure100% of Initial BenefitNot applicable Alzheimer’s Disease8 100% of Initial BenefitNot applicable Major Organ Transplant Benefit100% of Initial BenefitNot applicable 22 Listed Conditions25% of Initial BenefitNot applicable
43
SUPPLEMENTAL BENEFITS
MetLife provides coverage for the Supplemental Benefits listed below. This coverage would be in addition to the Total Benefit Amount payable for the previously mentioned Covered Conditions.
Health Screening Benefit10After your coverage has been in effect for thirty days, MetLife will provide an annual benefit* of $50or $100 per calendar year for taking one of the eligible screening/prevention measures. MetLife will pay only one health screening benefit per covered person per calendar year. For a complete list of eligible screening/prevention measures, please refer to the Disclosure Statement/Outline of Coverage.
INSURANCE RATES
MetLife offers competitive group rates and convenient payroll deduction so you don’t have to worry about writing a check or missing a payment! Your employee rates are outlined below.
Illness – Covered ConditionPaymentTotal Benefit Remaining Heart Attack – first diagnosis Initial Benefit payment of $10,000 or 100% $20,000 Heart Attack – second diagnosis, two years later Recurrence Benefit payment of $5,000 or 50% $15,000 Kidney Failure – first diagnosis, three years later Initial Benefit payment of $10,000 or 100% $5,000
Monthly Premium/$1,000 of Coverage(Non-Tobacco) Attained Age Employee Only Employee + Spouse Employee + Children Employee + Spouse + Children <25 $0.65 $1.14 $1.05 $1.54 25–29 $0.65$1.18$1.05$1.57 30–34 $0.83 $1.47 $1.23 $1.87 35–39 $1.07$1.91$1.47$2.30 40–44 $1.56 $2.72 $1.96 $3.12 45–49 $2.14$3.71$2.54$4.11 50–54 $2.89 $4.99 $3.29 $5.39 55–59 $3.84$6.65$4.24$7.05 60–64 $5.42 $9.24 $5.81 $9.64 65–69 $7.45$12.56$7.85$12.96 70+ $10.43 $17.20 $10.83 $17.60 44
How do I enroll?
QUESTIONS & ANSWERS
Enroll for coverage at USB School Groups-San Marcos Employer website.
Who is eligible to enroll?
Regular active full-time employees who are actively at work along with their spouse/domestic partnerand dependent childrencan enroll for MetLife Critical Illness Insurance coverage.3
How do I pay for coverage?
Coverage is paid through convenient payroll deduction.
What is the coverage effective date?
The coverage effective date is 09/01/2018.
If I Leave the Company, Can I Keep My Coverage? 11
Under certain circumstances, you can take your coverage with you if you leave. You must make a request in writing within a specified period after you leave your employer. You must also continue to pay premiums to keep the coverage in force.
Who do I call for assistance?
Contact a MetLife Customer Service Representative at 1 800-GET-MET8 (1-800-438-6388), Monday through Friday from 8:00 a.m. to 8:00 p.m., EST. Individuals with a TTY may call 1-800-855-2880.
Footnotes:
1 Coverage for Domestic Partners, civil union partners and reciprocal beneficiaries varies by state. Please contact MetLife for more information.
2 Dependent Child coverage varies by state. Please contact MetLife for more information.
3 Coverageis guaranteed provided (1) the employee is actively at work and (2) dependents are not subject to medical restrictions as set forth on the enrollment form and in the Certificate. Some states require the insured to have medical coverage. Additional restrictions apply to dependents serving in the armed forces or living overseas.
4 We will not pay a Recurrence Benefit for a Covered Condition that Recurs during a Benefit Suspension Period. We will not pay a Recurrence Benefit for either a Full Benefit Canceror a Partial Benefit Cancer unless the Covered Person has not had symptoms of or been treated for the Full Benefit Cancer or Partial Benefit Cancer for which we paid an Initial Benefit during the Benefit Suspension Period
5 Please review the Disclosure Statement or Outline of Coverage/Disclosure Documentfor specific information about cancer benefits.Not all types of cancer are covered. Some cancers are covered at less than the Initial Benefit Amount.For NH-sitused cases and NH residents, there is an initial benefit of $100 for All Other Cancers.
6 In certain states, the covered condition is Severe Stroke.
7 In NJ sitused cases, the Covered Condition is Coronary Artery Disease.
8 Please review the Outline of Coveragefor specific information about Alzheimer’s disease.
10 The Health Screening Benefit is not available in all states. See your certificate for any applicable waiting periods.There is a separate mammogram benefit for MT residents and for cases sitused in CA and MT.
11 Eligibility forportability through the Continuation of Insurance with Premium Payment provision may be subject to certain eligibility requirements and limitations. For more information, contact your MetLife representative.
Monthly Premium/$1,000 of Coverage(Tobacco) Attained Age Employee Only Employee + Spouse Employee + Children Employee + Spouse + Children <25 $0.88 $1.48 $1.28 $1.88 25–29 $0.88$1.54$1.28$1.94 30–34 $1.19 $2.04 $1.58 $2.44 35–39 $1.59$2.78$1.99$3.18 40–44 $2.43 $4.16 $2.83 $4.56 45–49 $3.41$5.84$3.81$6.23 50–54 $4.68 $8.00 $5.08 $8.40 55–59 $6.27$10.83$6.67$11.23 60–64 $8.96 $15.30 $9.35 $15.70 65–69 $12.52$21.17$12.91$21.56 70+ $17.86 $29.52 $18.26 $29.92
45
METLIFE’S CRITICAL ILLNESS INSURANCE (CII)IS A LIMITED BENEFIT GROUP INSURANCE POLICY. Like most group accident and health insurance policies, MetLife’s CII policies contain certain exclusions, limitations and terms for keeping them in force. Product features and availability may vary by state. In most plans, there is a preexisting condition exclusion. In most states, after a covered condition occurs there is a benefit suspension period during which most plans do not pay recurrence benefits. Attained Agerates are based on 5-year age bands and will increase when a Covered Person reaches a new age band. A more detailed description of the benefits, limitations, and exclusions can be found in the applicable Disclosure Statement or Outline of Coverage/Disclosure Document available at time of enrollment. For complete details of coverage and availability, please refer to the group policy form GPNP07-CI or GPNP09-CI, orcontact MetLife for more information. Benefits are underwritten by Metropolitan Life Insurance Company, New York, New York.
MetLife's Critical Illness Insurance is not intended to be a substitute for Medical Coverage providing benefits for medical treatment, including hospital, surgical and medical expenses. MetLife's Critical Illness Insurance does not provide reimbursement for such expenses.

Metropolitan Life Insurance Company | 200 Park Avenue| New York, NY 10166 L1216486089[exp0321][All States] NW 3.5AA
46
San Marcos Consolidated Independent School District
47
Accident Insurance Plan Summary
48
49
50
51
52
53

54


Valuable pre-tax benefits with convenient tools Employee Education Pre-Tax Savings Example Without FSA With FSA Net Increase in Take-Home Pay = $166/mo! Carryover puts your mind at ease!
it
The more you contribute to these accounts, the more you reduce your taxable gross salary. And with less taxes taken, your take-home pay increases! Online Enrollment and Contributions The TASC Card Convenience Flexible Spending Account (FSA) 55
How
Works
How to Access Your FSA Funds
Multiple self-service tools available to easily manage your FlexSystem account(s) and TASC Card transactions:
MyTASC Online: www.tasconline.com
MyTASC Mobile App: www.tasconline.com/mobile
MyTASC Text Messaging (SMS)

Eligible Expenses
any
Important Considerations
FSA Funds do not Rollover:
FX-4245-060118
56
403(b) UNIVERSAL AVAILABILITY NOTICE
The Opportunity.
You have the opportunity to save for retirement by participating in the School District’s 403(b) plan We recommend that all employees view a brief, 3minute video presentation explaining what a 403(b) plan is, and how to contribute.

The video can be reached at www.403bwhyme.com
If there are any questions, you may contact The OMNI Group at 877-544-6664.
How Can I Participate?
You can participate in the Plan with pre-tax contributions by completing and submitting a Salary Reduction Agreement (“SRA”) online at http://www.omni403b.com/, or by submitting a completed SRA form, which can be found on the same website, to The OMNI Group either by facsimile to (585) 672-6194 or by mail at 1099 Jay St., Bldg F, Rochester, NY, 14611 (“OMNI”).
How Much Can I Contribute Annually?
You may contribute up to $ 00 in 20 ; this amount is subject to change annually. If you have at least 15 years of service with your employer or you are at least 50 years old, you may also be able to make additional catch-up contributions. For appropriate limits for your particular circumstances, please contact OMNI’s Customer Care Center at 1-877-544-6664.
What If I Already Have An Account?
If you are already contributing to the Plan, and you want to change your contribution amount or service provider, simply complete and submit a new SRA. See directions above for on-line and paper submission options.
What If I Do Not Want To Contribute?
If you do not want to take advantage of this program, simply submit an SRA with the option “I do not wish to participate at this time” selected. See directions above for on-line and paper submission options.
How can I get more information?
You can access further information at www.omni403b.com or www.403bwhyme.com.
57






MEDICAL TRANSPORT MASA
enrolled in a medical plan to sign up for MASA! 58
You do NOT have to be
EMERGENCY TRANSPORTATIONCOSTS







MASA MTS is here toprotect its members and their families from the shortcomings of health insurance coverage by providing them with comprehensive financial protection for lifesaving emergencytransportationservices, bothathome andaway fromhome.
ManyAmericanemployersandemployees believethattheirhealthinsurancepolicies covermost,ifnotallambulanceexpenses. The truth is, they DONOT!

Even after insurance payments for emergency transportation, you couldreceive abillupto$5,000forgroundambulanceand as high as $70,000 for air ambulance. The financial burdens for medical transportation costs are veryreal.

HOW MASA ISDIFFERENT
AcrosstheUStherearethousandsofground ambulance providers andhundreds of air ambulance carriers. ONLY MASA offers comprehensive coverage since MASA is a PAYER andnotaPROVIDER!




ONLY MASA provides over 1.6million members with coverage for BOTH ground ambulance and air ambulance transport, REGARDLESS ofwhich provider transportsthem.


Members are covered ANYWHERE in all50 states andCanada!
Additionally, MASA provides arepatriation benefit:ifamemberishospitalizedmorethan 100miles from home, MASA can arrangeand pay tohave them transported toahospital closer totheir place ofresidence.
EmergentGround Transportation Emergent Air Tr ans port ation Non-EmergentAir Transportation Repatriation U.S./Canada U.S./Canada U.S./Canada U.S./Canada EmergentPlus A MASA Membership prepares you for the unexpected and gives you the peace of mind to access vital emergency medical transportation no matter where you live, for aminimal monthlyfee.
One low fee for the entire family
NO deductibles
NO healthquestions
Easy claims process For more information, pleasecontact Your Broker or MASA Representative EVERYFAMILY DESERVES AMASAMEMBERSHIP OURBENEFITS Benefit* Any Ground. Any Air. Anywhere.™ * Please refer to the MSA for a detailed explanation of benefits and eligibility, 59
•
•
•
•
60
6