










Medical – TRS Activecare
Health Savings Account – EECU
Group Life – Unum

Voluntary Life – Unum
Hospital Indemnity – The Hartford
Dental – Humana
Vision – Eyetopia
Disability – Unum
Accident – American Public Life (APL)
Medical Transportation – MASA
Cancer – American Public Life (APL)
Telemedicine – 1800MD
Legal Services – Legal Shield
Texas Life - Permanent Life
Flexible Spending Account - NBS
Retirement Plans – The Omni Group
Provid great bene t choices to you and your family is justcial welfare of the people who make our district work so well.
Visit last 4 digits of your SSN. (EX: John Sanderson SSN: Complete last name (excluding any special
WHO
insurance at full cost.
Dependent children of any age who are disabled
Children under your legal guardianship
NEW
of the following month.
or cancel coverage during the year if you have a qualifying change in the family or employment status that causes you to include:
Loss or gain of eligibility for other insurance (including

Everyone enrolled in Medical will receive a new Medical Card.
rary ID card or give your provider the insurance company’s phonenumber to call and verify your coverage if you do not havean ID card at the time of service.

Site Access To access your employer online enrollment site, , you can ebsite


mployee ame Robert Smith, SS# 123-45-6789
Default Password
User Name: smith 6789
Password password once you enter the site.
Employee Only
Employee and Spouse
Employee and Child(ren)
Premium: $395.00
District Pay: $395.00
Employee Cost: $0.00
Premium: $1,067.00
District Pay: $395.00
Employee Cost: $672.00
Premium: $672.00
District Pay: $395.00
Employee Cost: $277.00
Premium: $1,343.00
Llano Independent School District 2023-24

Employee and Family
District Pay: $395.00
Employee Cost: $948.00
Premium: $463.00
District Pay: $395.00
Employee Cost: $68.00
Premium: $1,204.00
District Pay: $395.00
Employee Cost: $809.00
Premium: $788.00
District Pay: $395.00
Employee Cost: $393.00
Premium: $1,528.00
District Pay: $395.00
Employee Cost: $1133.00
Premium: $408.00
District Pay: $395.00
Employee Cost: $13.00
Premium: $1,102.00
District Pay: $395.00
Employee Cost: $707.00
Premium: $694.00
District Pay: $395.00
Employee Cost: $299
Premium: $1,388.00
District Pay: $395.00
Employee Cost: $993.00
Premium: $1,013.00
District Pay: $395.00
Employee Cost: $618.00
Premium: $2,402.00
District Pay: $395.00
Employee Cost: $2007.00
Premium: $1,507.00
District Pay: $395.00
Employee Cost: $1112.00
Premium: $2,841.00
District Pay: $395.00
Employee Cost: $2446.00
There are no benefit changes to the BCBSTX West Texas HMO.
Coverage Tier
Premium: $865.00
Employee Only
District Pay: $395.00
Employee Cost: $470.00
Premium: $2,103.16
Employee & Spouse
District Pay: $395.00
Employee Cost: $1708.16
Premium: $1,361.42
Employee & Child(ren)
District Pay: $395.00
Employee Cost: $966.42
Premium: $2,233.34
Employee & Family
District Pay: $395.00
Employee Cost: $1838.34
Coverage Tier 2023 Plan Year Premiums Per Month
Premium: $515.37
Employee Only
District Pay: $395.00
Employee Cost: $120.37
Premium: $1,293.46
Employee & Spouse
District Pay: $395.00
Employee Cost: $898.46
Premium: $828.11
Employee & Child(ren)
District Pay: $395.00
Employee Cost: $433.11
Premium: $1,488.60
Employee & Family
District Pay: $395.00
Employee Cost: $1093.60
*Only available to those who reside outside of Llano County*


• Premium: The monthly amount you pay for health care coverage.
• Deductible: The annual amount for medical expenses you’re responsible to pay before your plan begins to pay its portion.
• Copay: The set amount you pay for a covered service at the time you receive it. The amount can vary by the type of service.
• Coinsurance: The portion you’re required to pay for services after you meet your deductible. It’s often a specified percentage of the costs; i.e. you pay 20% while the health care plan pays 80%.
• Out-of-Pocket Maximum: The maximum amount you pay each year for medical costs. After reaching the out-of-pocket maximum, the plan pays 100% of allowable charges for covered services.
• Individual maximum-out-of-pocket decreased by $650. Previous amount was $8,150 and is now $7,500.
• Family maximum-out-of-pocket decreased by $1,300. Previous amount was $16,300 and is now $15,000.
• Teladoc virtual mental health visit copay decreased from $70 to $0.
• Individual maximum-out-of-pocket increased by $450 to match IRS guidelines. Previous amount was $7,050 and is now $7,500.
• Family maximum-out-of-pocket increased by $900 to match IRS guidelines. Previous amount was $14,100 and is now $15,000. These changes apply only to in-network amounts.
• Family deductible decreased by $1,200. Previous amount was $3,600 and is now $2,400.
• Primary care provider and mental health copays decreased from $30 to $15.
• Teladoc virtual mental health visit copay decreased from $70 to $0.
• No changes.
• This plan is still closed to new enrollees.
*Pre-certification for genetic and specialty testing may apply. Contact a PHG
questions.
TRS contracts with HMOs in certain regions to bring participants in those areas additional options. HMOs set their own rates and premiums. They’re fully insured products who pay their own claims.
You can choose this plan if you live in one of these counties: Austin, Bastrop, Bell, Blanco, Bosque, Brazos, Burleson, Burnet, Caldwell, Collin, Coryell, Dallas, Denton, Ellis, Erath, Falls, Freestone, Grimes, Hamilton, Hays, Hill, Hood, Houston, Johnson, Lampasas, Lee, Leon, Limestone, Madison, McLennan, Milam, Mills, Navarro, Robertson, Rockwall, Somervell, Tarrant, Travis, Walker, Waller, Washington, Williamson
You can choose this plan if you live in one of these counties: Cameron, Hildalgo, Starr, Willacy
You can choose this plan if you live in one of these counties: Andrews, Armstrong, Bailey, Borden, Brewster, Briscoe, Callahan, Carson, Castro, Childress, Cochran, Coke, Coleman, Collingsworth, Comanche, Concho, Cottle, Crane, Crockett, Crosby, Dallam, Dawson, Deaf Smith, Dickens, Donley, Eastland, Ector, Fisher, Floyd, Gaines, Garza, Glasscock, Gray, Hale, Hall, Hansford, Hartley, Haskell, Hemphill, Hockley, Howard, Hutchinson, Irion, Jones, Kent, Kimble, King, Knox, Lamb, Lipscomb, Llano, Loving, Lubbock, Lynn, Martin, Mason, McCulloch, Menard, Midland, Mitchell, Moore, Motley, Nolan, Ochiltree, Oldham, Parmer, Pecos, Potter, Randall, Reagan, Reeves, Roberts, Runnels, San Saba, Schleicher, Scurry, Shackelford, Sherman, Stephens, Sterling, Stonewall, Sutton, Swisher, Taylor, Terry, Throckmorton, Tom Green, Upton, Ward, Wheeler, Winkler, Yoakum
An EECU Health Savings Account (HSA) enables you to save and conveniently pay for qualified medical expenses while you earn tax-free interest and pay no monthly service fees.
Opening an HSA provides both immediate and long-term benefits. The money in your HSA is yours even if you change jobs, switch your health plan, or retire. Your unused HSA balance rolls over from year to year. And, best of all, HSAs allow for tax-free deposits, tax-free earnings and tax-free withdrawals (for qualified medical expenses).1 Also, after age 65, you can withdraw funds from your HSA penalty-free.1
• Save money tax-free for healthcare expenses – contributions are not subject to federal income taxes and can be made by you, your employer or a third party1
• No monthly service fee – so you can save more
• Competitive Dividends paid on your entire HSA balance, so you can earn more
• Free EECU HSA Debit Mastercard® to conveniently pay for your qualified healthcare expenses. (HSA checks are also available upon request.2)
• Free Online & Mobile Banking and Free Bill Pay & Mobile Deposit to manage your account from anywhere, at anytime
• Comprehensive service and support – to assist you in optimizing your healthcare saving and spending
• Federally insured by NCUA – to at least $250,000
Membership in EECU is required - membership information available at eecu.org
1 Contributions, investment earnings, and distributions are tax free for federal tax purposes if used to pay for qualified medical expenses, and may or may not be subject to state taxation. A list of Eligible Medical Expenses can be found in IRS Publication 502, http://www.irs.gov/pub/irs-pdf/p502.pdf As described in IRS publication 969, http://www.irs.gov/pub/irs-pdf/p969.pdf, certain over-the-counter medications (when prescribed by a doctor) are considered eligible medical expenses for HSA purposes. If an individual is 65 or older, there is no penalty to withdraw HSA funds. However, income taxes will apply if the distribution is not used for qualified medical expenses. For more information consult a tax adviser or your state department of revenue. All contributions and distributions are your responsibility and must be within IRS regulatory limits.
2 Call 817-882-0800 or stop-by an EECU financial center to order standard checks at no charge (excludes shipping and handling) or order custom checks - prices vary.
3 Minimum opening deposit and balance of $.01 required. You will receive a Health Savings Account Agreement and Disclosures at enrollment. Please refer to those documents for complete terms and conditions. A free, no annual fee EECU HSA Debit Mastercard® will be sent to you separately. And, an EECU Health Savings Account Specialist is available to assist you with any questions you may have about your EECU HSA.
4 APY (Annual Percentage Yield) is accurate as of April 3, 2020 and is subject to change at any time. Average daily balance is required to earn the disclosed Annual Percentage Yield. Fees could reduce the earnings on the account. Dividend and interest is compounded daily and credited monthly. See Truth-In-Savings for Health Savings Account for more details.

Full Time Employees who regularly work 10 hours per week & Bus Drivers are eligible for insurance on their date of hire.
You keep coverage for a set period of time, or “term.” If you die during that term, the money can help your family pay for basic living expenses, final arrangements, tuition and more. AD&D Insurance is also available, which can pay a benefit if you survive an accident but have certain serious injuries. It can pay an additional amount if you die from a covered accident.
Your employer is offering you this coverage at no cost to you.
What else is included?
If you are diagnosed with a terminal illness with less than 12 months to live, you can request 100% of your life insurance benefit (up to $250,000) while you are still living. This amount will be taken out of the death benefit and may be taxable.

Your cost may be waived if you are totally disabled for a period of time.
You may be able to keep coverage if you leave the company, retire or change the number of hours you work. Employees or dependents who have a sickness or injury having a material effect on life expectancy at the time their group coverage ends are not eligible for portability.
Work-life balance Employee Assistance Program
Get access to professional help for a range of personal and work-related issues, including counselor referrals, financial planning and legal support.
Worldwide emergency travel assistance
One phone call gets you and your family immediate help anywhere in the world, as long as you’re traveling 100 or more miles from home. However, a spouse traveling on business for his or her employer is not covered.
Who can get Term Life coverage?
If you are actively at work at least 10 hours per week, you can receive coverage for:
If you are actively at work at least 10 hours per week, you can receive coverage for:
You: You can receive a benefit amount of $30,000. You can get up to $30,000 with no medical underwriting.
You: You can receive a benefit amount of $30,000. You can get up to $30,000 with no medical underwriting.
Who can get Accidental Death & Dismemberment (AD&D) coverage?
You: You can receive an AD&D benefit amount of $30,000.
No medical underwriting is required for AD&D coverage.
Health Savings Account (HSA) Limits (Pre-tax contributions per calendar year) Single coverage $3,850 Family Coverage: $7,750
Catch up contributions; $1,000
Eligible employees must be actively at work to apply for coverage. Being actively at work means on the day the employee applies for coverage, the individual must be working at one of his/her company’s business locations; or the individual must be working at a location where he/she is required to represent the company. If applying for coverage on a day that is not a scheduled workday, the employee will be considered actively at work as of his/her last scheduled workday. Employees are not considered actively at work if they are on a leave of absence or lay off.
Employees must be U.S. citizens or legally authorized to work in the U.S. to receive coverage. Employees must be actively employed in the United States with the Employer to receive coverage. Employees must be insured under the plan for spouses and dependents to be eligible for coverage.
Exclusions and limitations
Life insurance benefits will not be paid for deaths that are caused by suicide occurring within 24 months after the effective date of coverage or the date that increases to existing coverage becomes effective. This exclusion standardly applies to all medically written amounts and contributory amounts that are funded by the employee including shared funding plans.
AD&D specific exclusions and limitations:
Accidental death and dismemberment benefits will not be paid for losses caused by, contributed to by, or resulting from:
Disease of the body; diagnostic, medical or surgical treatment or mental disorder as set forth in the latest edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM)
while insane
War, declared or undeclared, or any act of war
Active participation in a riot
Committing or attempting to commit a crime under state or federal law
The voluntary use of any prescription or non-prescription drug, poison, fume or other chemical substance unless used according to the prescription or direction of your doctor. This exclusion does not apply to you if the chemical substance is ethanol.
Intoxication – “Being intoxicated” means your blood alcohol level equals or exceeds the legal limit for operating a motor vehicle in the state or jurisdiction where the accident occurred.
Delayed effective date of coverage
sickness, temporary layoff, or leave of absence on the date that insurance would otherwise become effective.
Age reduction
Coverage amounts for Life and AD&D Insurance for you will reduce to 50% of the original amount when you reach age 70. Coverage may not be increased after a reduction.
Termination of coverage
Your coverage under the policy ends on the earliest of:
The date the policy or plan is cancelled
The date you no longer are in an eligible group
The date your eligible group is no longer covered
The last day of the period for which you made any required contributions
The last day you are actively employed (unless coverage is continued due to a covered layoff, leave of absence, injury or sickness), as described in the certificate of coverage
Work-life balance Employee Assistance Program
The Work-life balance Employee Assistance Program, provided by HealthAdvocate, is available with select unum insurance offerings, Terms and availability of service are subjet to change. Service provider does not provide legal advice; please consult your attorney for guidance. Services are not valid after coverage terminates. Please contact your Unum representative for details.
Worldwide emergency travel assistance
Worldwide emergency travel assistance services, provided by Assist America, Inc., are available with select Unum insurance offerings. Terms and availability of service are subject to chance and prior notification requirements. Services are not valid after coverage terminates. Please contact your Unum representative for details.
This information is not intended to be a complete description of the insurance coverage available. The policy or its provisions may vary or be unavailable in some states. The policy has exclusions and limitations which may affect any benefits payable. For complete details of coverage and availability, please refer to Policy Form C.FP-1 et al or contact your Unum representative.
Life Planning Financial & Legal Resources services, provided by HealthAdvocate, are available with select Unum insurance offerings. Terms and availability of service are subject to change. Service provider does not provide legal advice; please consult your attorney for guidance. Services are not valid after coverage terminates. Please contact your Unum representative for details.
Underwritten by: Unum Life Insurance Company of America, Portland, Maine © 2022 Unum Group. All rights reserved. Unum is a registered trademark and marketing brand of Unum Group and its insuring subsidiaries.
Full Time Employees who regularly work 10 hours per week & Bus Drivers are eligible for insurance on their date of hire.
You choose the amount of coverage that’s right for you, and you keep coverage for a set period of time, or “term.” If you die during that term, the money can help your family pay for basic living expenses, final arrangements, tuition and more. AD&D Insurance is also available, which pays a benefit if you survive an accident but have certain serious injuries. It pays an additional amount if you die from a covered accident.
If you buy a minimum of $10,000 of coverage now, you can increase your coverage in the future up to $150,000 to meet your growing needs. There would be no medical underwriting to qualify for coverage.
A ‘Living’ Benefit — If you are diagnosed with a terminal illness with less than 12 months to live, you can request 100% of your life insurance benefit (up to $250,000) while you are still living. This amount will be taken out of the death benefit, and may be taxable. These benefit payments may adversely affect the recipient’s eligibility for Medicaid or other government benefits or entitlements, and may be taxable. Recipients should consult their tax attorney or advisor before utilizing living benefit payments.

Waiver of premium — Your cost may be waived if you are totally disabled for a period of time.
Portability — You may be able to keep coverage if you leave the company, retire or change the number of hours you work. Employees or dependents who have a sickness or injury having a material effect on life expectancy at the time their group coverage ends are not eligible for portability.
If you are actively at work at least 10 hours per week, you may apply for coverage for:
If you are actively at work at least 10 hours per week, you may apply for
Choose from $10,000 to $500,000 in $10,000 increments, up to 5 times your earnings. You can get up to $150,000. This is the amount of coverage you can qualify for with no medical underwriting.
You: Choose from $10,000 to $500,000 in $10,000 increments, up to 5 times your earnings. You can get up to $150,000. This is the amount of coverage you can qualify for with no medical underwriting.
Your spouse: Get up to $250,000 of coverage in $5,000 increments. Spouse coverage cannot exceed 100% of the coverage amount you purchase for yourself.
Your spouse: Get up to $250,000 of coverage in $5,000 increments. Spouse coverage cannot exceed 100% of the coverage amount you purchase for yourself.
Your spouse can get up to $50,000 with no medical underwriting, if eligible (see delayed effective date).
Your spouse can get up to $50,000 with no medical underwriting, if eligible (see delayed effective date).
Your children: Get up to $10,000 of coverage in $2,000 increments if eligible (see delayed effective date). One policy covers all of your children until their 26th birthday.
Your children: Get up to $10,000 of coverage in $2,000 increments if eligible (see delayed effective date). One policy covers all of your children until their 26th birthday.
The maximum benefit for children live birth to 6 months is $1,000.
The maximum benefit for children live birth to 6 months is $1,000.
You: Get up to $500,000 of AD&D coverage for yourself in $10,000 increments to a maximum of 5 times your earnings.
Your spouse: Get up to $250,000 of AD&D coverage for your spouse in $5,000 increments, if eligible (see delayed effective date).
Your children: Get up to $10,000 of coverage for your children in $2,000 increments if eligible (see delayed effective date).
No medical underwriting is required for AD&D coverage.
Actively at work
Eligible employees must be actively at work to apply for coverage. Being actively at work means on the day the employee applies for coverage, the individual must be working at one of his/her company’s business locations; or the individual must be working at a location where he/she is required to represent the company. If applying for coverage on a day that is not a scheduled workday, the employee will be considered actively at work as of his/her last scheduled workday. Employees are not considered actively at work if they are on a leave of absence or lay off.
An unmarried handicapped dependent child who becomes handicapped prior to the child’s attainment age of 26 may be eligible for benefits. Please see your plan administrator for details on eligibility. Employees must be U.S. citizens or legally authorized to work in the U.S. to receive coverage. Employees must be actively employed in the United States with the Employer to receive coverage. Employees must be insured under the plan for spouses and dependents to be eligible for coverage.
Exclusions and limitations
Life insurance benefits will not be paid for deaths caused by suicide occurring within 24 months after the effective date of coverage. The same applies for increased or additional benefits.
AD&D specific exclusions and limitations:
Accidental death and dismemberment benefits will not be paid for losses caused by, contributed to by, or resulting from:
Disease of the body; diagnostic, medical or surgical treatment or mental disorder as set forth in the latest edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM)
Suicide, self-destruction while sane, intentionally self-inflicted injury while sane or self-inflicted injury while insane
War, declared or undeclared, or any act of war
Active participation in a riot
Committing or attempting to commit a crime under state or federal law
The voluntary use of any prescription or non-prescription drug, poison, fume or other chemical substance unless used according to the prescription or direction of your or your dependent’s doctor. This exclusion does not apply to you or your dependent if the chemical substance is ethanol.
Intoxication – ‘Being intoxicated’ means your or your dependent’s blood alcohol level equals or exceeds the legal limit for operating a motor vehicle in the state or jurisdiction where the accident occurred.
Delayed effective date of coverage
Insurance coverage will be delayed if you are not an active employee because of an injury, sickness, temporary layoff, or leave of absence on the date that insurance would otherwise become effective.
Delayed Effective Date: if your spouse or child has a serious injury, sickness, or disorder, or is confined, their coverage may not take effect. Payment of premium does not guarantee coverage. Please refer to your policy contract or see your plan administrator for an explanation of the delayed effective date provision that applies to your plan.
Age Reduction
Coverage amounts for Life and AD&D Insurance for you and your dependents will reduce to 50% of the original amount when you reach age 70. Coverage may not be increased after a reduction.
Termination of coverage
Your coverage and your dependents’ coverage under the policy ends on the earliest of:
The date the policy or plan is cancelled
The date you no longer are in an eligible group
The date your eligible group is no longer covered
The last day of the period for which you made any required contributions
The last day you are actively employed (unless coverage is continued due to a covered layoff, leave of absence, injury or sickness), as described in the certificate of coverage
In addition, coverage for any one dependent will end on the earliest of:
The date your coverage under a plan ends
The date your dependent ceases to be an eligible dependent
For a spouse, the date of a divorce or annulment
For dependents, the date of your death
Unum will provide coverage for a payable claim that occurs while you and your dependents are covered under the policy or plan.
This information is not intended to be a complete description of the insurance coverage available. The policy or its provisions may vary or be unavailable in some states. The policy has exclusions and limitations which may affect any benefits payable. For complete details of coverage and availability, please refer to Policy Form C.FP-1 et al or contact your Unum representative.
Life Planning Financial & Legal Resources services, provided by HealthAdvocate, are available with select Unum insurance offerings. Terms and availability of service are subject to change. Service provider does not provide legal advice; please consult your attorney for guidance. Services are not valid after coverage terminates. Please contact your Unum representative for details.
Unum complies with state civil union and domestic partner laws when applicable.
Underwritten by:
Unum Life Insurance Company of America, Portland, Maine
© 2022 Unum Group. All rights reserved. Unum is a registered trademark and marketing brand of Unum Group and its insuring subsidiaries.
$150,000ISTHEMAXIMUMTHATMAYBEISSUEDWITHOUTANSWERINGHEALTHQUESTIONS
NOTE:FINALRATESMAYVARYSLIGHTLYDUETOROUNDING.
THESEGRIDSAREPRICESOFFREQUENTLYSELECTEDAMOUNTS.YOUMAYCHOOSE ANYINCREMENTOF$10,000UPTO$500,000.(NOTTOEXCEED5TIMESYOURANNUALSALARY) TOPURCHASEANAMOUNTOTHERTHANTHOSELEVELSINDICATEDABOVE,SIMPLY COMPLETETHEFOLLOWING.
SPOUSEAMOUNTCANNOTEXCEED100%OFEMPLOYEESAMOUNT and$50,000isthemostthatcanbeissuedwithoutansweringhealthquestions
CHILD(REN)
$2,000$4,000$6,000$8,000$10,000
NOTE:FINALRATESMAYVARYDUETOROUNDING.
THESEGRIDSAREPRICESOFFREQUENTLYSELECTEDAMOUNTS.YOUMAYCHOOSEANYINCREMENT OF$5,000UPTO$500,000.TOPURCHASEANAMOUNTOTHERTHANLEVELSINDICATEDABOVE, SIMPLYCOMPLETETHEFOLLOWING.
___________________X
#OF5,000UNITSYOURAGECOSTPER5,000UNITMonthlyCost
The average cost for a hospital stay is $2,607 per day1


• Routineoralexaminations(3peryear)
• Bitewingx-rays(2filmsunderage10,upto4films ages10andolder)
• Routinecleanings(3peryear)
• Periodontalcleanings(4peryear)
• Fluoridetreatment(1peryear,throughage16)
• Sealants(permanentmolars,throughage16)
• Spacemaintainers(primaryteeth,throughage15)
• OralCancerScreenin g(1peryear,ages40andolder)
• Emergencycareforpainrelief
• Amalgamfillings(1pertoothevery2years, compositeforanterior/frontteeth)
• Compositefillings(1pertoothevery2years, molarteeth)
• Oralsurgery(toothextractionsincluding impactedteeth)
• Stainlesssteelcrowns
• Harmfulhabitappliancesforchildren(1per lifetime,throughage14)
• Crowns(1pertoothevery5years)
• Inlays/onlays(1pertoothevery5years)
• Bridges(1pertoothevery5years)
• Dentures(1pertoothever5years)
• Denturerelines/rebases(1every3years,following 6monthsofdentureuse)
• Denture repairandadjustments(following 6monthsofdentureuse)
• Implants(crowns,bridges,anddentureseach limitedto1pertootheveryfiveyears)
• Periodontics(scaling/rootplaningandsurgery 1perquadrantevery3years)
• Endodontics(rootcanals1pertoothperlifetime and1re-treatment)
x
Orthodontiaservices
Childorthodontia-Coverschildrenthroughage18.Planpays 50percent(nodeductible)ofthecoveredorthodontiaservices, upto:$1,000lifetimeorthodontiamaximum.
Non-participatingdentistscanbillyouforchargesabovetheamountcoveredbyyourHumanaDentalplan.Toensure youdonotreceiveadditionalcharges,visitaparticipatingPPONetworkdentist.Membersandtheirfamiliesbenefit fromnegotiateddiscountsoncoveredservicesbychoosingdentistsinournetwork.Ifamembervisitsaparticipating networkdentist,thememberwillnotreceiveabillforchargesmorethanthenegotiatedfeeforcoveredservices.Ifa memberseesanout-of-networkdentist,coinsurancewillapplytotheusualandcustomarycharge.Out-of-network dentistsmaybillyouforchargesabovetheamountcoveredbyyourdentalplan.
Employer-sponsoredfunding: 5+enrolledemployees
2 Waitingperiodsdonotapplytoendodonticorperiodonticservicesunlessalateapplicant.
Employee: $31.70
Employee+spouse: $66.18
Employee+child(ren): $72.54
Family: $106.90
*Thisisnotasubstituteforaquote.RatesmustbeapprovedbyHumanaDentalunderwriting.
Regularcleaningscanhelpmanageproblemsthroughout thebodysuchasheartdisease,diabetes,andstroke.*
YourHumanaDentalTraditionalPreferredplanfocuses onpreventionandearlydiagnosis,providingthreeroutine cleanings,orfourperiodontalcleanings,alongwiththree routineperiodicexamspercalendaryear.
*www.perio.org
Takeahealthriskassessmentthatimmediately ratesyourdentalhealthknowledge.You'llreceivea personalizedactionplanwithhealthtips.Youcanprint acopyofyourscorecardtodiscusswithyourdentistat yournextvisit.
x Tipstoensureahealthymouth:

• Useasoft-bristledtoothbrush
• Choosetoothpastewithfluoride
• Brushforatleasttwominutestwiceaday
• Flossdaily
• Watchforsignsofperiodontaldiseasesuchasred, swollen,ortendergums
• Visitadentistregularlyforexamsandcleanings
Didyouknowthat74percentofadultAmericansbelieve anunattractivesmilecouldhurtaperson'schancesfor careersuccess?*HumanaDentalhelpsyoufeelgood aboutyourdentalhealthsoyoucansmileconfidently.
*AmericanAcademyofCosmeticDentistry
WithHumanaDental's TraditionalPreferredplan,youcan seeanydentist.Membersandtheirfamiliesbenefitfrom negotiateddiscountsoncoveredservicesbychoosing dentistsintheHumanaDental TraditionalPreferred Network.TofindadentistinHumanaDental's Traditional PreferredNetwork,logonto Humana.com orcall 1-800-233-4013.
Theothersideofthispagegivesyouasummaryof HumanaDentalbenefits.Yourplancertificatedescribes yourHumanaDentalbenefits,includinglimitationsand exclusions.YoucanfinditonMyHumana,yourpersonal pageat Humana.com orcall1-800-233-4013.
YourHumanaDentalidentificationcardcontainsallthe informationyourdentistneedstosubmityourclaims. Besuretoshareitwiththeofficestaffwhenyouarrivefor yourappointment.Ifyoudon'thaveyourcard,youcan printproofofcoverageat Humana.com .
AfterHumanaDentalprocessesyourdentalclaim,you willreceiveanexplanationofbenefitsorclaimsreceipt.It providesdetailedinformationoncovereddentalservices, amountspaid,plusanyamountyoumayoweyour dentist.Youcanalsocheckthestatusofyourclaimon MyHumanaat Humana.com or by calling 1-800-233-4013.
HumanagroupdentalplansareofferedbyHumanaInsuranceCompany,HumanaDentalInsuranceCompany,Humana InsuranceCompanyofNewYork,HumanaHealthBenefitPlanofLouisiana,TheDentalConcern,Inc.,HumanaMedical PlanofUtah,CompBenefitsCompany,CompBenefitsDental,Inc.,HumanaEmployersHealthPlanofGeorgia,Inc.or DentiCare,Inc.(d/b/aCompBenefits).InArizona,groupdentalplansinsuredbyHumanaInsuranceCompany.InNew Mexico,groupdentalplansinsuredbyHumanaInsuranceCompany.
Thisisnotacompletedisclosureofplanqualificationsandlimitations.Youragentswillprovideyouwithspecific limitationsandexclusionsascontainedintheRegulatoryandTechnicalInformationGuide.Pleasereviewthis informationbeforeapplyingforcoverage.Theamountofbenefitsprovideddependsupontheplanselected. Premiumswillvaryaccordingtotheselectionmade.



Please read carefully the following description of your Unum Educator Select Income Protection Plan insurance.
Eligibility
You are eligible for disability coverage if you are an active employee in the United States working a minimum of 20 hours per week. The date you are eligible for coverage is the later of: the plan effective date; or the day after you complete the waiting period.
Guarantee Issue
Current Employees: Coverage is available to you without answering any medical questions or providing evidence of insurability. You may enroll on or before the enrollment deadline. After the initial enrollment period, you can apply only during an annual enrollment period.
New Hires: Coverage is available to you without answering any medical questions or providing evidence of insurability. You may apply for coverage within 60 days after your eligibility date. If you do not apply within 60 days after your eligibility date, you can apply only during an annual enrollment period.
Benefits are subject to the pre-existing condition exclusion referenced later in this document.
Please see your Plan Administrator for your eligibility date.
Benefit Amount
You may purchase a monthly benefit in $100 units, starting at a minimum of $200, up to 66 2/3% of your monthly earnings rounded to the nearest $100, but not to exceed a monthly maximum benefit of $8,000. Please see your Plan Administrator for the definition of monthly earnings.
The total benefit payable to you on a monthly basis (including all benefits provided under this plan) will not exceed 100% of your monthly earnings unless the excess amount is payable as a Cost of Living Adjustment. However, if you are participating in Unum’s Rehabilitation and Return to Work Assistance program, the total benefit payable to you on a monthly basis (including all benefits provided under this plan) will not exceed 110% of your monthly earnings (unless the excess amount is payable as a Cost of Living Adjustment).

Elimination Period
The Elimination Period is the length of time of continuous disability, due to sickness or injury, which must be satisfied before you are eligible to receive benefits.
You may choose an Elimination Period (injury/sickness) of 0/7, 7/7, 14/14, 30/30, 60/60 or 180/180 days.
If, because of your disability, you are hospital confined as an inpatient, benefits begin on the first day of inpatient confinement. Inpatient means that you are confined to a hospital room due to your sickness or injury for 23 or more consecutive hours. (Applies to Elimination Periods of 14 days or less.)
Benefit Duration
Your duration of benefits is based on your age when the disability occurs.
Plan: SS ADEA: Your duration of benefits is based on the following table:
For disabilities due to a pre-existing condition, Unum will send you a payment each week up to the maximum period of payment. Your maximum period of payment is 4 weeks during the continuous period of disability.
Federal Income Taxation
You may wonder if your disability benefit amount will be taxed. It depends on how your premium — the price of your coverage — is paid.
If your premium is paid with:
Pre-Tax Dollars,* your benefit amount will be taxed
Post-Tax Dollars,** your benefit amount will not be taxed
Both Pre-Tax and Post-Tax Dollars, a portion of your benefit amount will be taxed
The disability benefit amounts you receive will be reported annually on a W-2. It will show any taxable and non-taxable portions separately.
*Pre-Tax Dollars are dollars paid by your employer toward premium that are not reported as earnings on your annual W-2. They are also dollars you pay toward premium through a cafeteria plan.
**Post-Tax Dollars are dollars paid through payroll deductions after taxes and withholdings have been subtracted from your earnings. They are also dollars paid by your employer toward premium that are reported as earnings on your annual W-2 and taxed according ly
Work-life balance is a comprehensive resource providing access to professional assistance for a wide range of personal and work-related issues. The service is available to you and your family members twentyfour hours a day, 365 days a year, and provides resources to help employees find solutions to everyday issues such as financing a car or selecting child care, as well as more serious problems such as alcohol or drug addiction, divorce, or relationship problems.
Services include: toll-free phone access to master’s-level consultants, up to three face-to-face sessions to help with more serious issues; and online resources. There is no additional charge for utilizing the program. Participation is confidential and strictly voluntary, and employees do not have to have filed a disability claim or be receiving benefits to use the program.
However, if you become disabled and are receiving benefits, Unum's On Claim Support can provide additional resources including: coaching on how to communicate effectively with medical personnel, conducting consumer research for medical equipment and supplies, assessing emotional needs and locating counseling resources.
Return
Unum supports efforts that enable a disabled employee to remain on the job or return to work as soon as possible. If you are disabled but working part time with monthly disability earnings of 20% or more of your indexed monthly earnings, during the first 12 months, the monthly benefit will not be reduced by any earnings until the gross disability payment plus your disability earnings, exceeds 100% of your indexed monthly earnings. The monthly benefit will then be reduced by that amount.
Rehabilitation and Return to Work Assistance
Unum has a vocational Rehabilitation and Return to Work Assistance program available to assist you in returning to work. We will make the final determination of your eligibility for participation in the program, and will provide you with a written Rehabilitation and Return to Work Assistance plan developed specifically for you. This program may include, but is not limited to the following benefits: coordination with your Employer to assist your return to work; adaptive equipment or job accommodations to allow you to work; vocational evaluation to determine how your disability may impact your employment options; job placement services; resume preparation; job seeking skills training; or education and retraining expenses for a new occupation.
If you are participating in a Rehabilitation and Return to Work Assistance program, we will also pay an additional disability benefit of 10% of your gross disability payment to a maximum of $1,000 per month. In addition, we will make monthly payments to you for 3 months following the date your disability ends, if we determine you are no longer disabled while: you are participating in a Rehabilitation and Return to Work Assistance program; and you are not able to find employment.
Worksite Modification
If a worksite modification will enable you to remain at work or return to work, a designated Unum professional will assist in identifying what’s needed. A written agreement must be signed by you, your employer and Unum, and we will reimburse your employer for the greater of $1,000 or the equivalent of two months of your disability benefit.
Waiver of Premium
Survivor Benefit
After you have received disability payments under the plan for 90 consecutive days, from that point forward you will not be required to pay premiums as long as you are receiving disability benefits.
Unum will pay your eligible survivor a lump sum benefit equal to 3 months of your gross disability payment.
This benefit will be paid if, on the date of your death, your disability had continued for 180 or more consecutive days, and you were receiving or were entitled to receive payments under the plan. If you have no eligible survivors, payment will be made to your estate, unless there is none. In that case, no payment will be made. However, we will first apply the survivor benefit to any overpayment which may exist on your claim.
You may receive your survivor benefit prior to your death if you are receiving monthly payments and your physician certifies in writing that you have been diagnosed as terminally ill and your life expectancy has been reduced to less than 12 months. This benefit is only payable once and if you elect to receive this benefit, no survivor benefit will be payable to your eligible survivor upon your death. (Note this “Accelerated Survivor Benefit” is not available in Connecticut.)
Dependent Care Expense Benefit
If you are disabled and participating in Unum’s Rehabilitation and Return to Work Assistance program, Unum will pay a Dependent Care Expense Benefit when you are disabled and you provide satisfactory proof that you: are incurring expenses to provide care for a child under the age of 15; and/or start incurring expenses to provide care for a child age 15 or older or a family member who needs personal care assistance.
The payment will be $350 per month per dependent, to a maximum of $1,000 per month for all dependent care expenses combined.
Worldwide Emergency Travel Assistance Services2
Whether your travel is for business or pleasure, our worldwide emergency travel assistance program is there to help you when an unexpected emergency occurs. With one phone call anytime of the day or night, you, your spouse and dependent children can get immediate assistance anywhere in the world3. Emergency travel assistance is available to you when you travel to any foreign country, including neighboring Canada or Mexico. It is also available anywhere in the United States for those traveling more than 100 miles from home. Your spouse and dependent children do not have to be traveling with you to be eligible. However, spouses traveling on business for their employer are not covered by this program.
Other Important Provisions
Pre-existing Condition Exclusion
Benefits will not be paid for disabilities caused by, contributed to by, or resulting from a pre-existing condition. You have a pre-existing condition if: you received medical treatment, consultation, care or services including diagnostic measures, or took prescribed drugs or medicines in the 3 months just prior to your effective date of coverage; and the disability begins in the first 12 months after your effective date of coverage.
4 Week Pre-Existing Condition Benefit
For disabilities due to a pre-existing condition, Unum will send you a payment each week up to the maximum period of payment. Your maximum period of payment is 4 weeks during the continuous period of disability.
Continuity of Coverage
If you are actively at work at the time you convert to Unum’s plan and become disabled due to a pre-existing condition, benefits may be payable if you were: in active employment and insured under the plan on its effective date; and insured by the prior plan at the time of change.
To receive a payment, you must satisfy the pre-existing condition under the Unum policy or the prior carrier’s policy. If you satisfy Unum’s pre-existing condition provision, payments will be determined by the Unum policy.
If you only satisfy the pre-existing condition provision for the prior carrier’s policy, the claim will be administered according to the Unum policy. However,
the payments will be the lesser of the benefit payable under the terms of the prior plan or the benefit under the Unum plan;
the elimination period will be the shorter of the elimination period under the prior plan or the elimination period under the Unum plan; and benefits will end on the earlier of the end of the maximum period of payment under the Unum plan or the date benefits would have ended under the prior plan.
You are disabled when Unum determines that: you are limited from performing the material and substantial duties of your regular occupation due to your sickness or injury; you have a 20% or more loss in indexed monthly earnings due to the same sickness or injury; and during the elimination period you are unable to perform any of the material and substantial duties of your regular occupation.
After benefits have been paid for 24 months, you are disabled when Unum determines that due to the same sickness or injury, you are unable to perform the duties of any gainful occupation for which you are reasonably fitted by education, training or experience. You must be under the regular care of a physician in order to be considered disabled.
Gainful occupation means an occupation that is or can be expected to provide you with an income within 12 months of your return to work, that exceeds 80% of your indexed monthly earnings if you are working or 60% of your indexed monthly earnings if you are not working.
Your disability benefit will be reduced by deductible sources of income and any earnings you have while disabled. Your gross disability payment will be reduced immediately by such items as disability income or other amounts you receive or are entitled to receive from workers compensation or similar occupational benefit laws, sabbatical or assault leave plans and the amount of earnings you receive from an extended sick leave plan as described in Louisiana Revised Statutes or any other act or law with similar intent.
After you have received monthly disability payments for 6 months, your gross disability payment will be reduced by such items as additional deductible sources of income you receive or are entitled to receive under: state compulsory benefit laws; automobile liability insurance; legal judgments and settlements; certain retirement plans; salary continuation or sick leave plans; other group or association disability programs or insurance; and amounts you or your family receive or are entitled to receive from Social Security or similar governmental programs.
Regardless of deductible sources of income, an employee who qualifies for disability benefits is guaranteed to receive a minimum benefit amount of the greater of $100 or 10% of the gross disability payment.
The lifetime cumulative maximum benefit period for all disabilities due to mental illness and disabilities based primarily on self-reported symptoms is 24 months. Only 24 months of benefits will be paid for any combination of such disabilities even if the disabilities are not continuous and/or are not related. Payments would continue beyond 24 months only if you are confined to a hospital or institution as a result of the disability.
Benefits will not be paid for disabilities caused by, contributed to by, or resulting from:
intentionally self-inflicted injuries; active participation in a riot; commission of a crime for which you have been convicted; loss of professional license, occupational license or certification; pre-existing conditions (see definition).
Unum will not cover a disability due to war, declared or undeclared, or any act of war.
Unum will not pay a benefit for any period of disability during which you are incarcerated.
Termination of Coverage
Your coverage under the policy ends on the earliest of the following: The date the policy or plan is cancelled;
The date you no longer are in an eligible group; The date your eligible group is no longer covered;
The last day of the period for which you made any required contributions;
The later of the last day you are in active employment except as provided under the covered layoff or leave of absence provision; or if applicable, the last day of your contract with your Employer but not beyond the end of your Employer’s current school contract year.
Unum will provide coverage for a payable claim which occurs while you are covered under the policy or plan.
How to Apply/ Effective Date of Coverage
Current employees: To apply for coverage, complete your enrollment form by the enrollment deadline.
New Hires: To apply for coverage, complete your enrollment form within 60 days of your eligibility date. Please see your Plan Administrator for your effective date.
If you do not enroll during the initial enrollment period, you may apply only during an annual enrollment.
Delayed Effective Date of Coverage
If you are absent from work due to injury, sickness, temporary layoff or leave of absence, your coverage will not take effect until you return to active employment. Please contact your Plan Administrator after you return to active employment for when your coverage will begin.
Questions
If you should have any questions about your coverage or how to enroll, please contact your Plan Administrator.
This information is not intended to be a complete description of the insurance coverage available. The policy or its provisions may vary or be unavailable in some states. The policy has exclusions and limitations which may affect any benefits payable. For complete details of coverage and availability, please refer to Policy Form( C.FP-1 et.al. or contact your Unum representative.
1,2 The work-life balance employee assistance program, provided by HealthAdvocate, is available with select Unum insurance offerings. Terms and availability of service are subject to change. Service provider does not provide legal advice; please consult your attorney for guidance. Services are not valid after coverage terminates. Please contact your Unum representative for details.
Worldwide emergency travel assistance services, provided by Assist America, Inc., are available with select Unum insurance offerings. Terms and availability of service are subject to change and prior notification requirements. Services are not valid after coverage terminates. Please contact your Unum representative for details. All emergency travel assistance must be arranged by Assist America, which pays for all services it provides. Medical expenses such as prescriptions or physician, lab or medical facility fees are paid by the employee or the employee’s health insurance.
Underwritten by: Unum Life Insurance Company of America 2211 Congress Street, Portland, Maine 04122, www.unum.com
©2022 Unum Group. All rights reserved. Unum is a registered trademark and marketing brand of Unum Group and its insuring subsidiaries.
Costs Effective as of September 1, 2022
Costs below are based on a Monthly payroll deduction (Employer billing mode is based on 12 Payments per year)
*If, because of your disability, you are hospital confined as an inpatient, benefits begin on the first day of inpatient confinement.
Find your Annual/Monthly Earnings above to determine your Maximum Monthly Benefit. If your Annual/Monthly Earnings are not shown, use the next lower Annual/Monthly Earnings and corresponding Maximum Monthly Benefit. Or, you may refer to the Plan Highlights to calculate your Maximum Monthly Benefit based on your earnings.

Costs Effective as of September 1, 2022
Costs below are based on a Monthly payroll deduction (Employer billing mode is based on 12 Payments per year)
*If, because of your disability, you are hospital confined as an inpatient, benefits begin on the first day of inpatient confinement.
Find your Annual/Monthly Earnings above to determine your Maximum Monthly Benefit. If your Annual/Monthly Earnings are not shown, use the next lower Annual/Monthly Earnings and corresponding Maximum Monthly Benefit. Or, you may refer to the Plan Highlights to calculate your Maximum Monthly Benefit based on your earnings.



Are you covered?
Accident Insurance can provide protection to help with the high cost of a covered accidental injury. From a simple physician’s office visit, to x-rays, ambulance transportation or an intensive care admission due to an accidental injury — unexpected expenses can add up.
CHOOSE the benefit options that best protect you and your family from a covered accident. C y
RECEIVE treatment for a covered accident.

Benefit funds are paid directly to you for expenses incurred as the result of a covered accident
You decide how to use the benefit funds—for medical and non-medical expenses
Multiple coverage options for your whole family
FILE your claim online or mail it in. You'll receive a cash benefit to use however you wish.

Cost-effective premiums with convenient payroll deduction
THE INSURANCE POLICY UNDER WHICH THIS CERTIFICATE IS ISSUED IS NOT A POLICY OF WORKERS’ COMPENSATION INSURANCE. YOU SHOULD CONSULT YOUR EMPLOYER TO DETERMINE WHETHER YOUR EMPLOYER IS A SUBSCRIBER TO THE WORKERS’ COMPENSATION SYSTEM.
Dependent Child(ren) Coverage

Continuation Coverage
Based on defined qualifying events defined in your certificate
Spouse benefit amounts are 100% of the insured’s benefit amount, unless otherwise stated.
Dependent child(ren) benefit amounts are 100% of the insured’s benefit amount, unless otherwise stated.
Coverage will be continued for 12 months following the date the insured ceased active employment.
Spouse benefit amounts are 100% of the insured’s benefit amount, unless otherwise stated.
Dependent child(ren) benefit amounts are 100% of the insured’s benefit amount, unless otherwise stated.
Coverage will be continued for 12 months following the date the insured ceased active employment.
Post-Accident Time Frame Requirement
Unless otherwise defined, confinement, stay, treatment, therapy, diagnosis, surgery, paralysis, dismemberment, death or prescription of covered items must occur within the defined number of days after a covered accident.

Hospital Benefits
Hospital Admission
Pays only once per day, even if the confinement or observation long stay is the result of more than one injury.
365 days
365 days
$500/5 days
$500/5 days
Pays only once per day, even if the confinement is the result of more than one injury.
Coma and Paralysis Benefits
Coma
Must continue for at least 30 days before a benefit is payable. Pays once per covered accident.
Must continue for at least 60 days before a benefit is payable
$50,000
Spouse - $50,000
Dependent Child(ren) - $50,000
Dismemberment Benefits
Dismemberment - Single, Double, Finger/Toe$500 to $10,000
Dislocation Benefits
Dislocation (open reduction) - based on joint involved $225 to $3,000
Insured - $100,000
Spouse - $100,000
Dependent Child(ren) - $100,000
$1,250 to $25,000
$450 to $6,000
Dislocation (closed reduction) percentage1
Fracture Benefits
25% of open reduction benefit amount25% of open reduction benefit amount
50% of open reduction benefit amount50% of open reduction benefit amount Partial dislocation percentage1
Fracture (open reduction) - based on bone involved$225 to $3,000
$450 to $6,000
Fracture (closed reduction) percentage1
Laceration Benefits
Based on length of laceration
Inpatient Surgery Benefits
25% of open reduction benefit amount25% of open reduction benefit amount
50% of open reduction benefit amount50% of open reduction benefit amount Chip fracture percentage1
$25 to $200/5 day
$50 to $400/5 day
Pays once per covered accident based on type of surgery
General Anesthesia1
Outpatient Surgery Benefits
25% of inpatient surgery benefit amount25% of inpatient surgery benefit amount
days Other miscellaneous surgery for repair
Tendon/ligament/rotator cuff/torn knee cartilagebased on type of surgery
Severe Burn Benefits
2nd degree & 3rd degree Burns
Pays once per covered accident based on degree and size of burn
Lodging and Travel Benefits
to $250
of severe burn benefit amount1% of severe burn benefit amount
Transportation for treatment for the injured covered person by train, bus, coach or plane must be at least 100 miles from the covered person’s primary residence. Not payable if ambulance benefit is payable.
to 3 round trips
Wheelchair, motorized scooter, walker, walking boot, any other medical device used for mobility, including a brace, cane and crutches - based on type of appliance
Pays once per covered accident, per plan year based on number of devices
Accident Screening Benefit Accident Screening1
day(s) per month, up to 12 day(s) per plan year
$50/1 per covered person, up to 4 per family. Additional screening tests included
$50/1 per covered person, up to 4 per family. Additional screening tests included
1 Spouse and/or dependent child(ren) benefit amount and/or percentage is the same as the insured’s benefit amount and/or percentage
*The premium and amount of benefits vary dependent upon Plan selected at time of application.

Refer to the Summary of Benefits for details specific to each plan.
Benefits are only paid as a result of injuries received in a covered accident that occurs while coverage is in force for a covered person. Payable once per covered accident, up to the defined number of days per plan year for each covered person, unless stated otherwise. All diagnosis, treatment, therapy and/or confinement, as a result of death or injuries, must begin/occur within the defined number of days after a covered accident.
A covered person means you and any dependent currently covered under the policy and the certificate. If dependent coverage is applicable to your plan, a dependent means your spouse, or your grandchild if claimed as a dependent on your federal tax return as of the date the grandchild’s application for coverage is submitted to APL, a child for whom the insured must provide medical or dental support regardless of whether the child resides with you, or your natural child, or legally adopted child, including where you are a party to a suit in which you seek to adopt the child, or stepchild who is under 26 years of age. Dependent also includes any minor under your charge, care, and control who has been placed in your home for adoption and is under 26 years of age.
A hospital is not an institution, or part thereof, used as: a place for rehabilitation, a place for rest or for the aged, a nursing or convalescent home, a long-term nursing unit or geriatrics ward or an extended care facility for the care of convalescent, rehabilitative or ambulatory patients.
Hospital Benefits
Hospital Admission – Not payable for treatment in an emergency room, urgent care facility or rehabilitation unit, for an observation unit short stay or for treatment as an outpatient.
Hospital Confinement - Not payable for any day for which a hospital admission benefit is payable, for treatment in an emergency room, urgent care facility or rehabilitation unit, for an observation unit short stay or for treatment as an outpatient.
ICU Confinement – Not payable for any day for which an ICU admission benefit is payable, for treatment in an emergency room, urgent care facility, rehabilitation unit or observation unit or for treatment as an outpatient. This benefit is payable in addition to the Hospital Confinement Benefit.
Initial Treatment Benefits
Observation Room Treatment (Short Stay) – Not payable for any day for which a hospital admission, hospital confinement, ICU admission or ICU confinement benefit is payable, if applicable to your plan.
Emergency Room Treatment – Treatment must occur within the defined number of days after the covered accident occurs. Payable once per covered accident, up to the defined number of days per plan year for each covered person. Payable only once per day.
Urgent Care Treatment – Benefit will not be paid for routine health examinations and immunizations, physical therapy, chiropractic care or other therapy services.
Physician’s Office Treatment – Benefit will not be paid for immunizations, routine health examinations, physical therapy, chiropractic care, other therapy services or treatment received through telemedicine.
Diagnostic Benefits
X-ray – Does not include a major diagnostic exam or lab test.
Major Diagnostic Exam – Major diagnostic exams include those defined in your certificate.
Therapy Benefits
Inpatient Rehabilitation – Not payable for any day for which a hospital admission, hospital confinement, ICU admission or ICU confinement benefit is payable, if applicable to your plan.
Physical Therapy – Physical therapy must begin within the defined number of days and be rendered within 365 days after the covered accident occurs. Payable up to the defined number of days per plan year for each covered person. Physical therapy must follow initial treatment in a hospital, emergency room or other medical facility for a covered accident for this benefit to be payable.
Extended Treatment – Treatment must begin within the defined number of days and be rendered within 365 days after the covered accident occurs. This benefit is payable up to the defined number of days per plan year for each covered person.
Coma and Paralysis Benefits
Coma – Must be diagnosed by a physician as having commenced within the defined number of days after the covered accident occurs.
Paralysis – Must begin within the defined number of days after the covered accident occurs and be determined by a physician as expected to be permanent. Only one paralysis benefit amount, the highest amount, is payable per covered accident.
Accidental Death Benefits
Accidental Death – If the covered accident that causes the covered person’s loss of life occurs while the covered person is on or occupying a common carrier, the common carrier accidental death benefit will be paid in lieu of the accidental death benefit, if applicable to your plan.
Dismemberment Benefits
Single, Double and/or Finger/Toe Dismemberment – If the covered person later dies as a result of the same covered accident, APL will pay the applicable death benefit less any amounts paid under this benefit, if applicable to your plan.
Dislocation Benefits - If multiple dislocations or partial dislocations, if applicable to your plan, are suffered as the result of one covered accident, APL will not pay more than two times the greatest dislocation benefit payable for an individual joint per covered accident for each covered person. No more than one dislocation benefit per joint per covered accident will be paid for each covered person.
Fracture Benefits - If multiple fractures or chip fractures, if applicable to your plan, are suffered as the result of one covered accident, APL will not pay more than two times the greatest fracture benefit payable for an individual bone per covered accident for each covered person. No more than one fracture benefit per bone per covered accident will be paid for each covered person.
Laceration Benefits – Treatment for the laceration must occur within 14 days after the covered accident occurs. Benefits are payable when laceration is repaired with stitches by a physician as a result of a covered accident. Payable up to the defined number of days per plan year for each covered person. Payable only once per covered accident for each covered person, even if treatment is received for more than one laceration.
Inpatient Surgery Benefits
Inpatient Surgery Benefits – Surgery must be performed by a physician within the defined number of days after the covered accident occurs.
General Anesthesia – Inpatient surgery benefit must be payable and general anesthesia must be received during inpatient surgery for this benefit to be payable.
Outpatient Surgery Benefits
Outpatient Surgery Benefits - Surgery must be performed by a physician within the defined number of days after the covered accident occurs.
Exploratory Surgery - Exploratory arthroscopic surgery must be performed by a physician within the defined number of days after the covered accident occurs.
Brain Injury Benefits - Concussion must be diagnosed by a physician. A severe traumatic brain injury (TBI) must be diagnosed by a neurologist, if applicable to your plan. If both a concussion and a severe traumatic brain injury (TBI) occur in the same covered accident, only the highest benefit will be payable, if applicable to your plan.
Severe Burn Benefits
Severe Burn Benefits – No benefits will be paid if the degree and percentage of the body surface burned is not shown as a covered benefit.
Skin Graft – Severe burns benefit must be payable and skin graft treatment undergone for this benefit to be payable.
Lodging and Travel Benefits
Non-Local Transportation – Treatment in a hospital must be advised by a physician because treatment for an injury is not available locally. Payable only once per round trip for up to the defined number of round trip(s) per plan year for each covered person. This benefit is not payable on any day that an ambulance benefit is payable.
Family Lodging – Expense must be incurred for lodging by an adult family member accompanying a covered person who is confined away from the family member’s primary residence for treatment as the result of a covered accident. Payable up to the defined number of nights per plan year for each covered person. Payable only once per night, even if more than one family member accompanies the covered person; if the adult family member is providing care for the covered person or is acting as an advocate on the behalf of the covered person; and while the covered person is receiving treatment in a hospital that is advised by a physician because treatment for an injury is not available locally. Proof of the expense incurred for lodging, evidenced by a receipt, invoice or another appropriate document, must be submitted with the claim. Mileage is measured as the geographic distance from the family member’s primary residence to the facility at which the confinement occurs.
Ambulance Benefits – Ambulance transportation, to or from a hospital or between medical facilities, must occur within 168 hours after the covered accident.
Emergency Dental & Vision Treatment Benefits – Emergency dental work or vision work must occur within the defined number of days after the covered accident. Payable once per plan year for each covered person and only once per covered accident even if multiple teeth or eyes are affected. If more than one type of procedure is performed on the same day, only the highest emergency dental and vision treatment benefit will be payable.
Appliance and Prosthesis Benefits
Appliance – Medical appliance must be prescribed within the defined number of days after the covered accident occurs. Payable the defined number of days per plan year for each covered person. If more than one type of medical appliance is prescribed on the same day, only the highest appliance benefit will be payable.
Prosthesis – Prosthetic device, artificial limb or artificial eye must be prescribed by a physician and received within the defined number of days after the covered accident occurs.
Other Benefits
Auto & Home Modification – Residence and/or vehicle modification must occur within 365 days after the covered accident occurs.
Blood/Plasma/Platelets - Payable up to the defined number of days per plan year for each covered person. Transfusion of blood, plasma or platelets must be received during a surgery for which an inpatient surgery or outpatient surgery benefit is payable.
Epidural/Pain Management – Epidural injection, for treatment of an injury, must occur within the defined number of days after the covered accident occurs.
Organized Sports Benefit Booster – Pays an additional percentage only if a covered person suffers an injury for which a benefit is payable under the certificate and the injury occurred while the covered person was participating in an organized sport.
Post-Traumatic Stress Disorder (PTSD) – Must be under the active care of a physician or mental health professional for the treatment of PTSD.
Prescription Drugs – Drug must be prescribed by a physician or medical professional within 365 days after a covered accident occurs. Benefit will not be paid for any drug that is received or prescription that is filled while a covered person is confined in any medical facility.
Accident Screening Benefit – Service must be rendered by a physician while the covered person is not an inpatient in a hospital and while the covered person is covered under the policy. Covered tests are defined in your certificate.
Exclusions
APL will not pay benefits for a claim that is caused by, contributed to by, or resulting from any of the following: voluntary intoxication (as defined by the law of the jurisdiction in which such intoxication occurred) or while under the influence of any narcotic, drug or controlled substance, unless administered by or taken according to the instructions of a physician or medical professional; voluntary intoxication through use of poison, gas or fumes, whether by ingestion, injection, inhalation or absorption; committing or attempting to commit a felony, or active participation in a riot, insurrection or terrorist activity; intentional self-harm or attempting or committing suicide, whether sane or not; war or any act of war, whether declared or undeclared, or any act related to war while serving in the military forces or any auxiliary unit thereto (the pro-rata portion of any premium paid for any such covered person will be refunded upon receipt of your written request); any injury that occurs while a covered person is engaged in an illegal occupation or activity, or legally incarcerated in a penal or correctional institution; cosmetic surgery or other elective procedure that is not medically necessary, except for reconstructive surgery incidental to or following surgery for trauma to the affected body part; diagnosis or treatment received outside the United States, its territories or Canada, except for emergency care received within seven days of an injury; treatment provided at a facility, office or other location owned or operated by a covered person or family member; treatment of mental or nervous disorder(s) that is not a direct result of trauma sustained by a covered accident; any bacterial infection (except pyogenic infections which shall occur with and through an accidental cut or wound); operating, learning to operate, serving as a crew member of any aircraft or hot air balloon, including those which are not motor-driven, unless flying as a fare paying passenger; travel or flight in any aircraft or hot air balloon, including those which are not motor-driven, if it is being used for testing or experimental purposes, used by or for any military authority, or used for travel beyond the earth’s atmosphere; participation in any organized sport in a professional or semi-professional capacity; riding or driving an air, land or water vehicle in any organized and scheduled race, speed or endurance contest; participation in base jumping, bungee jumping, cliff jumping, kite surfing, kiteboarding, luging, parachuting, paragliding, parakiting, parasailing, ski jumping, skydiving, spelunking, tricking or wingsuit flying; or an on the job injury, if applicable to your plan. Additionally, no benefits will be paid for an injury that occurs prior to a covered person being covered under the certificate.
Your coverage ends on the earliest of: the date you leave an eligible class under the certificate; any premium due date, if full payment for your coverage is not made within the grace period following the premium due date; the date the policy terminates and you have not elected coverage under the portability provision of the certificate; the last day of the month during which you attain the limiting age defined in your certificate. If dependent coverage is included in your plan, coverage for a dependent ends on the earliest of: your termination date; the last day of the month during which the dependent is no longer eligible for coverage due to a change to the policy; or the last day of the month during which a dependent no longer satisfies the definition of a dependent. Termination will not affect a claim that occurred while a covered person was covered by the policy.
If the accident insurance premium is paid on a pre-tax basis, the benefit may be taxable. Please contact your tax or legal advisor regarding tax treatment of your policy benefits.
This is not intended to be a complete description of the insurance coverage offered. While benefit amounts stated in this summary are specific to your coverage, other items may summarize our standard product features and not the specific features of your coverage. Provisions are provided in the certificate and this summary does not modify those provisions or the insurance in any way. This is not a contract. A certificate will be made available to you that describes the benefits in greater detail. Refer to your certificate for your maximum benefit amounts. Should there be a difference between this summary and the certificate, the certificate will govern.
Underwritten by American Public Life Insurance Company | This is a brief description of the coverage. This product contains limitations and exclusions. For complete benefits and other provisions, please refer to the policy/certificate. This is not a Medicare supplement policy. This product is inappropriate for people who are eligible for Medicaid coverage. | This policy is considered an employee welfare benefit plan established and/or maintained by an association, union or employer intended to be covered by ERISA, and will be administered and enforced under ERISA. Group policies issued to governmental entities and municipalities may be exempt from ERISA guidelines. | Policy Form GAO21APL Series | Texas | Group Accident Insurance | Limited Benefit Group Accident Insurance (02/22)
DID YOU KNOW?
are sent to the emergency room through ground or air ambulance every year * .
Insurance companies may not cover all air and ground ambulance expenses which can result in max in-network out-of-pocket** costs of:
$8,700 Individual $17,400 Family
Ground ambulance out-of-network transportation costs may be even higher than in-network since the No Surprises Act does not apply to ground ambulance at this time.
A MASA MTS Membership provides the ultimate peace of mind at an a ordablerateforemergencygroundand air transportation assistance expenses within the continental United States, Alaska, Hawaii, and while traveling in Canada, regardless of whether the provider is in or out of your group healthcare bene tsnetwork.Afterthe group health plan pays its portion, MASA works with providers to make certain our Members have no out-ofpocket expenses~ for emergency ambulance transportation assistance and other related services.
Emergency Air Ambulance Coverage1
MASA MTS covers out-of-pocket expenses associated with emergency air transportation to a medical facility for serious medical emergencies deemed medically necessary for you or your dependent family member.

Emergency Ground Ambulance Coverage1
MASA MTS covers out-of-pocket expenses associated with emergency ground transportation to a medical facility for serious medical emergencies deemed medically necessary for you or your dependent family member.
Hospital to Hospital Ambulance Coverage1
MASA MTS covers out-of-pocket expenses that you or a dependent family member may incur for hospital transfers, due to a serious emergency, to the nearest and most appropriate medical facility when the current medical facility cannot provide the required level of specialized care by air ambulance to include medically equipped helicopter or xed-wingaircraft.
Repatriation to Hospital Near Home Coverage1
MASA MTS provides services and covers out-of-pocket expenses for the coordination of a Member’s nonemergency transportation by a medically equipped, air or ground ambulance in the event of hospitalization more than one hundred (100) miles from the Member’s home if the treating physician and MASA MTS’ Medical Director says it’s medically appropriate and possible to transfer the Member to a hospital nearer to home for continued care and recuperation.
Contact Your Representative, to learn more:
The information provided in this product information sheet is for informational purposes only. The bene ts listed and the descriptions thereof do not represent the full terms and conditions applicable for usage and may only be o ered in some memberships. Premiums and bene ts vary depending on the bene ts selected. Commercial air and Worldwide coverage are not available in all territories. For a complete list of bene ts, premiums, and full terms, conditions, and restrictions, please refer to the applicable member services agreement for your territory. MASA MTS products and services are not available in AK, NY, WA, ND, and NJ. MASA MTS utilizes third-party transportation service providers for all transportation services. MASA Global, MASA MTS and MASA TRS are registered service marks of MASA Holdings, Inc., a Delaware corporation. Void where prohibited by law.
~If a member has a high deductible health plan that is compatible with a health savings account, bene ts will become available under the MASA membership for expenses incurred for medical care (as de ned under Internal Revenue Code (“IRC”) section 213 (d)) once a member satis es the applicable statutory minimum deductible under IRC section 223(c) for high-deductible health plan coverage that is compatible with a health savings account.
COVERAGE TERRITORIES:
1.All coverage provided by this membership is limited to the continental United States, Alaska, Hawaii, and Canada, and must originate and conclude therein.


SOURCES:
*ACEP NOW 2014
** Patient Protection and A ordable Care Act; HHS Notice of Bene t and Payment Parameters for 2022 and Pharmacy Bene t Manager Standards. May 5, 2021.



Limited Benefit Policy
How would cancer impact you and your family?
If you or a family member are diagnosed with cancer, APL’s Cancer Insurance may help cover the costs associated with the detection and treatment of cancer and help you be more financially prepared.
CHOOSE the benefit options that best protect you and your family.
RECEIVE treatment for a covered benefit.
FILE your claim online or mail it in.


Radiation Therapy, Chemotherapy, Immunotherapy
Experimental Treatments
Surgical and Anesthesia Benefits
Prescriptions, Transportation Benefits and more

Plus, multiple plan options to cover you, your spouse or your child(ren) with convenient payroll deduction
THE INSURANCE POLICY UNDER WHICH THIS CERTIFICATE IS ISSUED IS NOT A POLICY OF WORKERS’ COMPENSATION INSURANCE. YOU SHOULD CONSULT YOUR EMPLOYER TO DETERMINE WHETHER YOUR EMPLOYER IS A SUBSCRIBER TO THE WORKERS’ COMPENSATION SYSTEM.
Prosthesis
Surgical implantation
Non-surgical (not hair piece)
$1,000 per device
$100 per device
$2,000 per device
$200 per device
Patient Care Benefit Rider Level 3 Level 4
Hospital Confinement
Insured or Spouse: $200 per day of hospital confinement, days 1-30; $400 per day of hospital confinement, days 31+
Eligible Dependent Child(ren): $400 per day of hospital confinement, days 1-30; $800 per day of hospital confinement, days 31+
Insured or Spouse: $300 per day of hospital confinement, days 1-30; $600 per day of hospital confinement, days 31+
Eligible Dependent Child(ren): $600 per day of hospital confinement, days 1-30; $1,200 per day of hospital confinement, days 31+
Outpatient Facility
Attending Physician
Dread Disease
$400 per day surgery is performed$600 per day surgery is performed
$40 per day of hospital confinement$50 per day of hospital confinement
$200 per day of hospital confinement, days 1-30; $400 per day of hospital confinement, days 31+
$300 per day of hospital confinement, days 1-30; $600 per day of hospital confinement, days 31+
U.S. Government, Charity Hospital or HMO
$200 per day of hospital confinement, days 1-30; $400 per day of hospital confinement, days 31+
$300 per day of hospital confinement, days 1-30; $600 per day of hospital confinement, days 31+
Drugs and Medicine
$150 per inpatient confinement; $50 per outpatient prescription, maximum $150 per month
$150 per inpatient confinement; $50 per outpatient prescription, maximum $150 per month
and Lodging Transportation - maximum 12 trips per calendar year for all modes of transportation combined Lodging - up to a maximum of 100 days per calendar year
Family Member Transportation and Lodging
Transportation - maximum 12 trips per calendar year for all modes of transportation combined
Lodging - up to a maximum of 100 days per calendar year
Blood, Plasma and Platelets
Ambulance
Maximum of 2 trips per hospital confinement for all modes of transportation combined
Inpatient Special Nursing Services
actual coach fare or $0.75 per mile for travel by bus, plane or train; $0.75 per mile for travel by car; $100 per day for lodging
actual coach fare or $0.75 per mile for travel by bus, plane or train; $0.75 per mile for travel by car; $100 per day for lodging
actual coach fare or $0.75 per mile for travel by bus, plane or train; $0.75 per mile for travel by car; $100 per day for lodging
actual coach fare or $0.75 per mile for travel by bus, plane or train; $0.75 per mile for travel by car; $100 per day for lodging
$300 per day
Ground: $200 per trip
Air: $2,000 per trip
$300 per day
Ground: $200 per trip
Air: $2,000 per trip
$150 per day of hospital confinement$150 per day of hospital confinement
Outpatient Special Nursing Services $150 per day
$150 per day
Intensive Care Unit
Maximum of 45 days per confinement for any combination of intensive care unit or step down unit
Step Down Unit
Maximum of 45 days per confinement for any combination of intensive care unit or step down unit
$600 per day $600 per day
$300 per day $300
Increase in Coverage
Only available at annual renewal. Must be approved by APL and premium rates will be based upon the insured’s attained age. Subject to the Time Limit on Certain Defenses and Pre-Existing Condition provisions, as defined in the policy.
Only available at annual renewal. Must be approved by APL and premium rates will be based upon the insured’s attained age. Subject to the Time Limit on Certain Defenses and Pre-Existing Condition provisions, as defined in the policy. Additional Rider(s)
*Total premium includes the Plan selected and any applicable rider premium. The premium and amount of benefits vary dependent upon the Plan selected at time of application.
Benefits are only payable following a diagnosis of cancer for a loss incurred for the treatment of cancer while covered under the policy. A charge must be incurred for benefits to be payable. All benefits are per covered person per calendar year, unless otherwise stated. When coverage terminates for loss incurred after the coverage termination date, APL’s obligation to pay benefits also terminates for a specified disease that manifested itself while the person was covered under the policy. All benefits are subject to the benefit maximums proposed.
A covered person means a person who is eligible for coverage under the certificate and for whom coverage is in force. An eligible dependent means your lawful spouse who lives with you; your natural child, adopted child or stepchild who is under 26 years of age; a child under your charge, care and control, if placed with you for adoption, who is under the age of 26 and/or for whom you are a party in a suit in which adoption of the child is sought; any child under the age of 26 for whom you provide medical support under an order issued under Chapter 154 of the Texas Family Code, or enforceable by a court in Texas; or grandchildren under the age of 26 if those grandchildren are the insured’s dependents for federal income tax purposes at the time application for coverage of the grandchild is made.
A hospital is not an institution, or part thereof, used as: a hospice unit, including any bed designated as a hospice or a swing bed; a convalescent home; a rest or nursing facility; a rehabilitative facility; an extended-care facility; a skilled nursing facility or facility primarily affording custodial, educational care, or care or treatment for persons suffering from mental diseases or disorders, or care for the aged, or drug or alcohol addiction.
Cancer Treatment Benefits
Radiation Therapy, Chemotherapy or Immunotherapy - Benefits are payable for actual charges, the amount actually paid by or on behalf of the covered person and accepted by the provider for services provided, up to the maximum benefit amount per 12-month period. The 12-month period begins on the first day covered radiation therapy, chemotherapy or immunotherapy is received. Chemotherapy and immunotherapy coverage will be limited to drugs only. Benefits not covered are defined in your certificate.
Hormone Therapy - Must be prescribed by a physician. This benefit covers drugs and medicine only. This benefit does not cover associated administrative processes, anti-nausea drugs, pain medicine, administration of anti-nausea drugs or pain medicine, or any drugs or medicines covered under the radiation therapy, chemotherapy or immunotherapy benefit.
Experimental Treatment - Must be prescribed by a physician for treatment of cancer the same as any other non-experimental treatment covered under the policy and any attached riders.
No benefits will be paid for any of the following: treatment by any program engaged in research that does not meet the definition of experimental treatment; or losses or medical expenses incurred prior to the covered person’s effective date regardless of when specified disease was diagnosed. Loss must result from definitive cancer treatment including direct extension, metastatic spread or recurrence. Proof must be submitted to support each claim. The policy does not cover any other disease, sickness or incapacity which existed prior to the diagnosis of cancer, even though after contracting cancer it may have been complicated, aggravated or affected by cancer or the treatment of cancer.
No benefits are payable for any loss incurred during the defined pre-existing condition exclusion period following the covered person’s effective date of the certificate as the result of a pre-existing condition. Pre-existing conditions specifically named or described as excluded in any part of the policy are never covered.
Insurance coverage under the certificate and any attached riders will end on the earliest of these dates: the date the policy terminates; the end of the grace period if the premium remains unpaid; the date insurance has ceased on all persons covered under the certificate; the end of the certificate month in which the policyholder requests to terminate the coverage; the date you no longer qualify as an insured; or the date of your death.
Insurance coverage for a covered person under the certificate and any attached riders will end as follows: the date the policy terminates; the date the certificate terminates; the end of the grace period if the premium remains unpaid; the end of the certificate month in which the policyholder requests to terminate the coverage for an eligible dependent; the date a covered person no longer qualifies as an insured or eligible dependent; or the date of the covered person’s death. We may end the coverage of any covered person who submits a fraudulent claim.
All riders are part of the policy/certificate to which it is attached and are subject to all the provisions of the policy/certificate that are not in conflict with the provisions of the rider. A charge must be incurred for benefits to be payable, with the exception of the Internal Cancer First Occurrence Benefit Rider and the Heart Attack/Stroke First Occurrence Benefit Rider, if applicable to the plan. No benefits are payable for loss incurred during the defined pre-existing condition exclusion period following the covered person’s effective date of the rider as a result of a pre-existing condition, with the exception of the Hospital Intensive Care Unit Rider, if applicable to the plan.
Cancer Screening Benefit Rider
Diagnostic Testing - Must be a screening test that is generally medically recognized to detect internal cancer. Not payable for any test payable under the medical imaging benefit.
Follow-Up Diagnostic Testing - An abnormal result from a covered screening test must be received for an invasive screening test to be payable. For an invasive test involving an incision or surgery, this benefit will only be paid for a test that results in a negative diagnosis of cancer. For invasive tests that do not require an incision, this benefit will be paid regardless of the diagnosis.
Medical Imaging - CT, CAT, PET scan(s) or MRI must be requested by a physician and performed due to a diagnosis of cancer or treatment of cancer.
Limitations and Exclusions
No benefits will be paid for any of the following: treatment by any program engaged in research that does not meet the definition of experimental treatment, as defined in the policy; or losses or medical expenses incurred prior to the covered person’s effective date of the rider.
Surgical Benefit Rider
Benefits are only payable for a loss incurred and treatment of a diagnosed cancer or skin cancer while covered under the rider.
Surgical Operation - Must be performed for a covered diagnosed cancer, skin cancer or for reconstructive surgery due to cancer. Pays the lesser of the surgical unit value assigned to the procedure multiplied by the unit dollar amount or the maximum per operation amount. Two or more surgical procedures performed through the same incision will be considered one operation and benefits will be limited to the most expensive procedure. Reconstructive surgery to the non-diseased breast to establish symmetry with a diseased breast must occur within 24 months of the reconstructive surgery of the diseased breast. Diagnostic surgeries that result in a negative diagnosis of cancer, surgeries required to implant a permanent prosthetic device or bone marrow transplant or stem cell transplant surgeries are not covered under this benefit.
Anesthesia - Payable at 25% of the paid surgical benefit amount. Anesthesiologist services must be for the result of a covered surgery. Services of an anesthesiologist for bone marrow or stem cell transplants, skin cancer or surgical prosthesis implantation are not covered under this benefit.
Bone Marrow and Stem Cell Transplant - Payable in lieu of the surgical and the anesthesia benefits. If a bone marrow transplant and a stem cell transplant are performed on the same day, only the bone marrow transplant benefit will be payable.
Prosthesis - Surgically implanted prosthetic device must be prescribed by a physician as a direct result of surgery for cancer. Artificial limbs will be paid under the surgical implantation portion of this benefit. Temporary prosthetic devices used as tissue expanders are covered under the surgical benefit. Prosthetic related supplies and hair prosthesis are not covered under this benefit.
Limitations and Exclusions
No benefits will be paid for any of the following: treatment by any program engaged in research that does not meet the definition of experimental treatment; or losses or medical expenses incurred prior to the covered person’s effective date of this rider regardless of when a specified disease was diagnosed.
Patient Care Benefit Rider
Benefits are only payable for a loss incurred and treatment of a diagnosed specified disease while covered under the rider.
Hospital Confinement - Must be confined to a hospital for the treatment of a covered cancer or the treatment of a condition or disease directly caused by cancer or the treatment of cancer. Outpatient treatment or a stay of less than 18 hours in an observation unit or an emergency room is not covered.
Outpatient Facility - Facility fee must be charged and surgical procedure performed on an outpatient basis in a hospital or ambulatory surgical center. Surgical procedures for skin cancer are not covered under this benefit.
Attending Physician - Services of a physician, other than a surgeon, must be required while confined in a hospital for the treatment of cancer.
Dread Disease - Must be confined in a hospital for treatment of a dread disease, as defined in the policy.
Extended Care Facility - Confinement in an extended care facility must be due to cancer, at the direction of a physician and begin within 14 days after a hospital confinement. Payable for up to the same number of days benefits were paid for the covered person’s preceding hospital confinement.
Donor - Expenses must be incurred for treatment of cancer on behalf of a covered person for a surgery due to organ transplant, bone marrow transplant or stem cell transplant. Blood donor expenses are not covered under this benefit. Donor may not be the same covered person for which expenses are incurred.
Home Health Care - Care required due to cancer must be in lieu of hospital confinement, prescribed by a physician, provided by a nurse or by a home health nurse’s aide under the supervision of a registered nurse and must begin within 14 days after a covered hospital confinement. Payable up to the same number of days benefits were paid for the covered person’s preceding hospital confinement. Caregiver may not be a member of your immediate family. Physical, speech, occupational or audio therapies or psychotherapy are not covered under this benefit. If the covered person qualifies for coverage under the hospice care benefit, the hospice care benefit will be paid in lieu of this benefit.
Hospice Care - Must be diagnosed by a physician as terminally ill, as defined in the policy, and require hospice care due to cancer. Care must be directed by a licensed hospice organization in the patient’s home or on an outpatient or short-term inpatient basis in a hospice facility.
U.S. Government Hospital / Charity Hospital / HMO - An itemized list of services must not be available due to confinement in a charity hospital, U.S. Government owned or operated hospital or coverage under a Health Maintenance Organization (HMO) or a Diagnostic Related Group (D.R.G.) where no charges are made to the covered person. If this option is elected, this benefit will be paid in lieu of any amounts payable under the rider, base policy, cancer screening benefit rider, surgical benefit rider and miscellaneous benefit rider (except for the transportation and lodging benefits), if applicable to the plan.
Limitations and Exclusions
No benefits will be paid for any of the following: treatment by any program engaged in research that does not meet the definition of experimental treatment; or losses or medical expenses incurred prior to the covered person’s effective date of the rider regardless of when a specified disease was diagnosed. The rider only pays for loss for cancer or dread disease resulting from definitive cancer treatment including direct extension, metastatic spread or recurrence. Proof must be submitted to support each claim. The rider also covers other conditions or diseases directly caused by cancer or the treatment of cancer. The rider does not cover any other disease, sickness or incapacity, which existed prior to the diagnosis of cancer, even though after contracting cancer it may have been complicated, aggravated or affected by cancer or the treatment of cancer except for conditions specifically provided in the dread disease benefit.
Miscellaneous Benefit Rider
Benefits are only payable for a loss incurred and treatment of a diagnosed cancer while covered under the rider.
Cancer Treatment Center Evaluation or Consultation - Treatment opinion must be obtained at a national cancer institute designated comprehensive cancer treatment center. If the comprehensive cancer treatment center is located more than 50 miles from the covered person’s place of residence, an evaluation or consultation travel or lodging benefit is also payable. This benefit is payable in lieu of the transportation and lodging benefit and family member transportation and lodging benefit listed in the rider.
Second/Third Surgical Opinion - Surgery must be recommended by an attending physician as treatment for a diagnosed cancer. Second and/ or third surgical opinion must be obtained from the consulting physician prior to surgery. Surgical opinions for reconstructive, skin cancer or prosthesis surgeries are not covered under this benefit.
Drugs and Medicine - Anti-nausea and pain medication must be prescribed by a physician and administered while receiving radiation therapy, chemotherapy, immunotherapy, a covered surgery, bone marrow transplant or stem cell transplant due to cancer. This benefit does not in include coverage for associated administrative charges or drugs or medicines covered under the radiation therapy, chemotherapy, immunotherapy or hormone therapy benefits.
Hair Piece (Wig) - Must be needed as a direct result of cancer or treatment of cancer.
Transportation and Lodging - Travel by a covered person to the hospital that provides radiation therapy, chemotherapy, immunotherapy, bone marrow transplant, stem cell transplant or surgery due to cancer must be by scheduled bus, plane, train or car and be within the United States or its territories. Hospital must be prescribed by a physician, be the nearest hospital which offers the specialized treatment and be at least 50 miles away from the covered person’s residence, using the most direct route. Proof of coach fare for bus, plane, train transportation must be provided or the per mile benefit will be paid. Travel by car will be paid at the stated rate per mile for up to 1,000 miles round trip. Benefits will be provided for only one mode of transportation per round trip. If treatment is received while confined in a hospital, benefits for transportation will be paid once per hospital confinement. Lodging for the covered person must be in a single room in a motel, hotel or other accommodation acceptable to APL. Benefit will only be paid on the days the covered person receives specialized treatment on an outpatient basis.
Family Member Transportation and Lodging - Travel must be for an adult family to be near a covered person who is receiving treatment in the hospital at least 50 miles away from the covered person’s residence, using the most direct route. If the family member travels by bus, plane or train, you will have the option to receive the coach fare benefits or the per mile benefit. Proof of coach fare for bus, plane, train transportation must be provided or the per mile benefit will be paid. Travel by car will be paid at the stated rate per mile for up to 1,000 miles round trip. Benefits will be provided for only one mode of transportation per round trip. If the covered person receives treatment while confined in a hospital, benefits for travel and/or lodging will be paid once per hospital confinement. If the family member and the covered person who is receiving treatment travel in the same car or lodge in the same room, benefits for travel and lodging will only be paid under the transportation and lodging benefit.
Blood, Plasma and Platelets - This benefit does not include coverage for any laboratory processes or colony stimulating factors.
Ambulance - Transportation must be by licensed air or ground ambulance to a hospital or from one medical facility to another. Must be admitted as an inpatient and confined in a hospital for at least 18 consecutive hours for the treatment of cancer. If both air and ground ambulance is required on the same day, only the highest benefit amount will be paid.
Inpatient Special Nursing Services - Full-time special nursing care for the treatment of cancer (other than that regularly furnished by a hospital), must be provided by a nurse and prescribed by a physician. Care must be for at least eight consecutive hours during a 24-hour period.
Outpatient Special Nursing Services - Outpatient full-time private duty nursing for the treatment of cancer at the covered person’s home must be provided by a nurse, prescribed by a physician and begin within 14 days following a hospital confinement for the treatment of cancer. Care must be for at least eight consecutive hours during a 24-hour period. Payable for up to the same number of days of the covered person’s preceding hospital confinement. If both inpatient special nursing services and outpatient special nursing services occur within the same 24hour period, only the inpatient special nursing services benefit will be paid.
Medical Equipment - Rental or purchase of medical equipment, as listed in the rider, must be prescribed by a physician for the treatment of cancer. This benefit will not be paid while the covered person is confined in a hospital.
Physical, Occupational, Speech, Audio Therapy or Psychotherapy - Must be advised by a physician as a result of cancer or treatment of cancer and performed by a licensed caregiver. If two or more therapies occur on the same day, only one benefit will be paid.
Waiver of Premium
You must remain disabled for 60 continuous days due to cancer and disability must occur while receiving treatment for such cancer. Proof of disability must be provided to APL. Proof includes, but is not limited to, a physician’s statement containing the date the cancer was diagnosed, the date disability due to cancer began, the expected date, if any, the disability will end and an employer’s statement with the last date of work and expected date of return, if known. Waiver of Premium will continue for as long as you remain disabled until the earliest of the following: the date you are no longer disabled; the date coverage ends according to the termination provisions in the certificate; or the date coverage ends according to the termination provisions in this rider. Proof of disability must be provided for each new period of disability.
No benefits will be paid for any of the following: treatment by any program engaged in research that does not meet the definition of experimental treatment; or losses or medical expenses incurred prior to the covered person’s effective date of the rider regardless of when a specified disease was diagnosed.
First diagnosis of internal cancer must be while the rider is in force. Internal cancer must be positively diagnosed by a legally licensed doctor of medicine certified by the American Board of Pathology or American Board of Osteopathic Pathology. Diagnosis must be made based on microscopic examination of fixed tissue or preparations from the hemic system (either during life or postmortem). Internal cancer does not include other conditions that may be considered pre-cancerous or having malignant potential as defined in your certificate. Benefits reduce 50% at age 70.
Limitations and Exclusions
No benefits will be paid for a diagnosis of a metastasis to a new site of any cancer diagnosed prior to the covered person’s effective date, as this is not considered a first diagnosis of an internal cancer
Benefits will not be paid for an ICU or step-down unit confinement that begins prior to the effective date of coverage. Refer to your certificate for confinement not covered under this benefit. Benefits reduce by 50% at age 70.
No benefits will be paid for any loss caused by or resulting from an intentionally self-inflicted bodily injury, suicide or attempted suicide, whether sane or insane; alcoholism or drug addiction; any act of war declared or undeclared, or any act related to war, or active service in the armed forces, or military service for any country at war; (If coverage is suspended for any covered person during a period of military service, APL will refund the pro-rata portion of any premium paid for any such covered person upon receipt of the policyholder’s written request.); participation in any activity or event while intoxicated or under the influence of any narcotic unless administered by a physician or taken according to the physician’s instructions; participation in, or attempting to participate in, a felony, riot or insurrection (a felony is defined by the law of the jurisdiction in which the activity takes place); for a newborn child born within the 10-month period following the effective date for confinements that begin within the first 30 days following the birth of such child; or for confinements caused by any heart condition during the first two years following the effective date of coverage when any heart condition was diagnosed or treated prior to the end of the 30-day period following the covered person’s effective date. The heart condition causing the confinement need not be the same condition diagnosed or treated prior to the effective date.
Benefit Rider(s) Termination of Coverage
Rider(s) will terminate and coverage will end for all covered persons on the earliest of any of the following: the end of the grace period if the
premium for the rider remains unpaid; the date the policy or certificate to which the rider is attached terminates; the end of the certificate month in which APL receives a request from the policyholder to terminate the rider; the date of your death; if applicable to the plan, the date the lump sum benefit amount for the internal cancer first occurrence benefit rider has been paid for all covered persons under the rider; and if applicable to the plan, the date of covered person’s death or the date the lump sum benefit amount for the heart attack/stroke benefit rider has been paid for all covered persons under the rider. Coverage for an eligible dependent terminates under the rider when such person ceases to meet the definition of eligible dependent.
Additional Riders
Portability Rider
You may elect portability coverage when coverage ends under the policy for reasons other than non-payment of premium. The requirements for election of portability, election of dependent portability and termination of portability will be defined in rider attached to your certificate. When elected, APL will notify you of the amount of premium due, the frequency of the premium payments and the premium due dates
If the cancer insurance premium is paid on a pre-tax basis, the benefit may be taxable. Please contact your tax or legal advisor regarding tax treatment of your policy benefits.
Underwritten by American Public Life Insurance Company. This is a brief description of the coverage. This product contains Limitations, Exclusions and Waiting Periods. For complete benefits and other provisions, please refer to your policy/certificate. This coverage does not replace Workers’ Compensation Insurance. This product is inappropriate for people who are eligible for Medicaid coverage. This policy is considered an employee welfare benefit plan established and/or maintained by an association or employer intended to be covered by ERISA, and will be administered and enforced under ERISA. Group policies issued to governmental entities and municipalities may be exempt from ERISA guidelines. | Policy Form GC14APL Series | Texas | Limited Benefit Group Specified Disease Cancer Insurance | (02/22)







Apple and the Apple logo are trademarks of Apple Inc.,registered in the U.S. and other countries. App Store is a service mark of Apple Inc., registered in the U.S. and other countries. Android is a trademark of Google Inc

















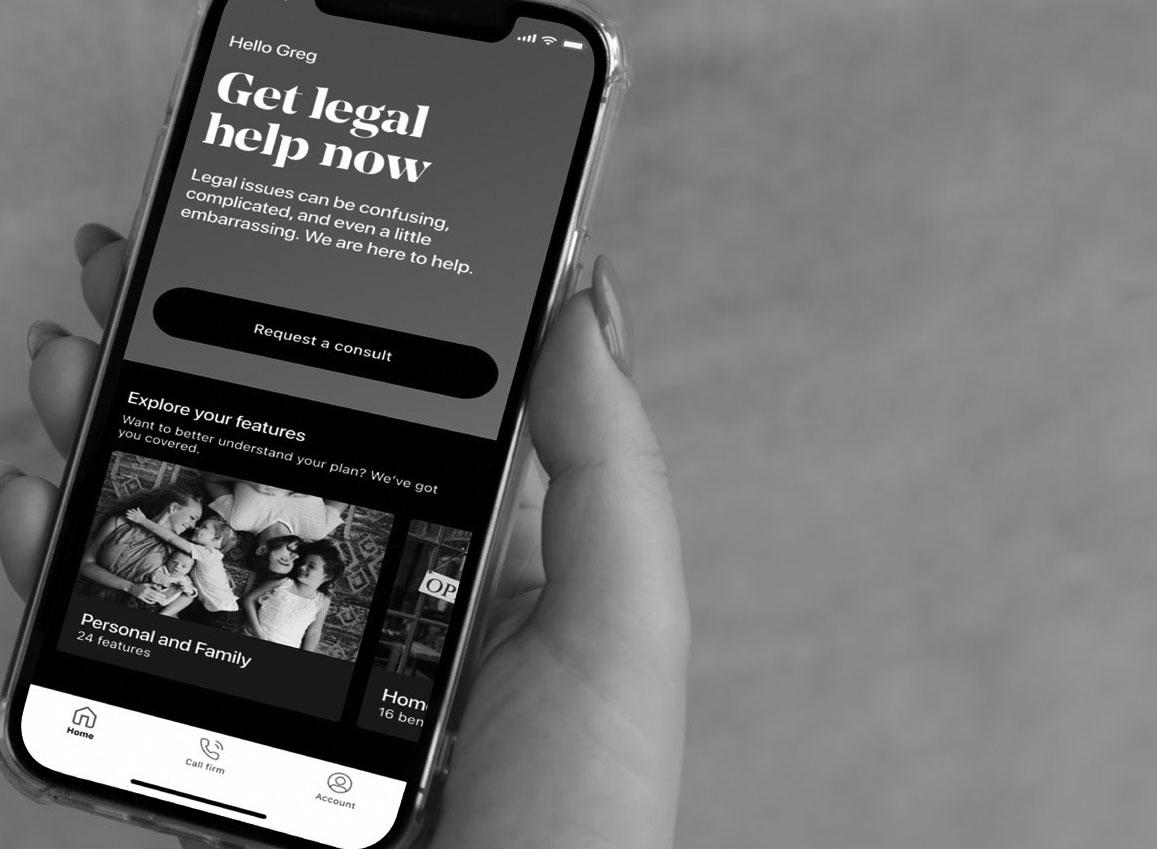

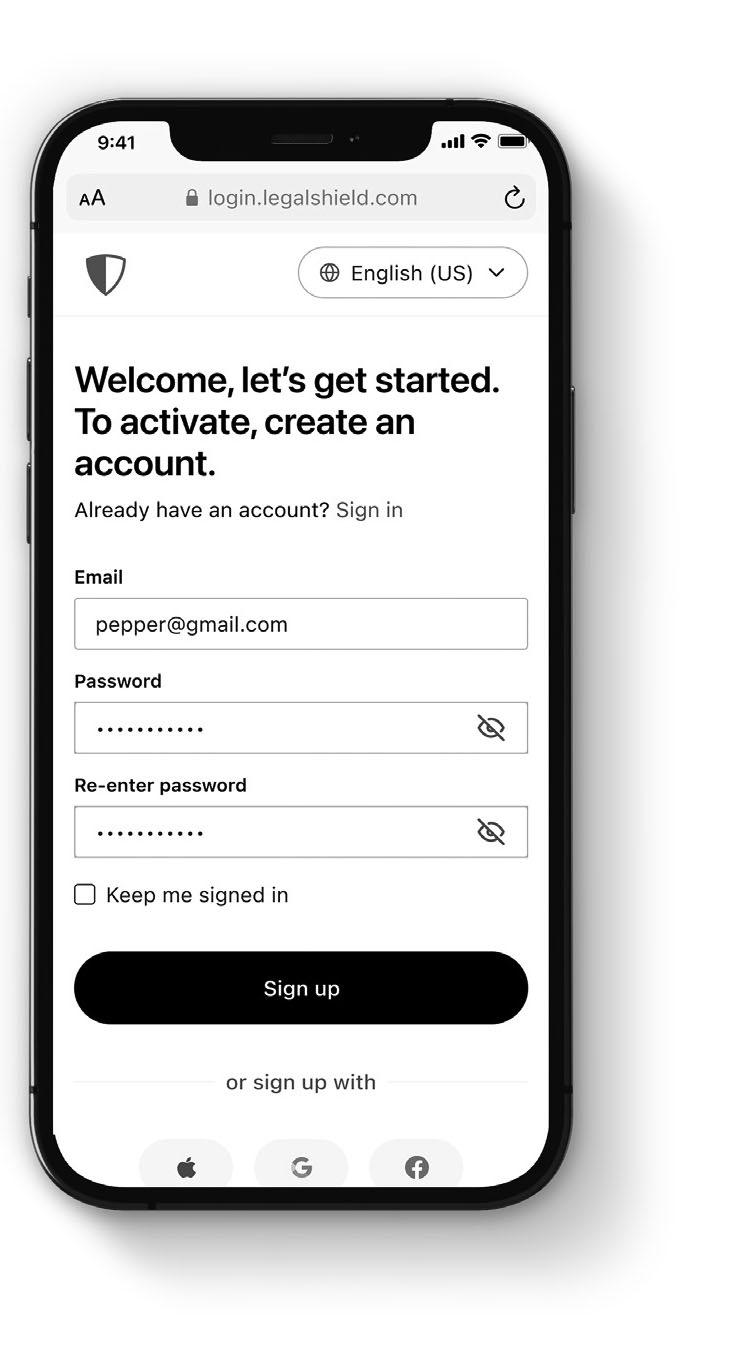









purelife-plus
You pay for it through convenient payroll deductions You
cover

Youcanqualifybyanswering just3questions–noexamsorneedles.
DURING
1.Beenactivelyatworkonafulltimebasis,performingusualduties?
2.Beenabsentfromworkduetoillnessormedicaltreatmentforaperiodof morethan5consecutiveworkingdays?
3.Beendisabledorreceivedtests,treatmentorcareofanykindinahospital ornursinghomeorreceivedchemotherapy,hormonaltherapyforcancer, radiation,dialysistreatment,ortreatmentforalcoholordrugabuse?
PureLife-plusisaFlexiblePremiumAdjustableLifeInsurancetoAge121.Aswithmostlifeinsuranceproducts, TexasLifecontractsandriderscontaincertain exclusions,limitations,exceptions,reductionsofbenefits,waitingperiodsandtermsforkeepingtheminforce.PleasecontactaTexasLiferepresentativeorsee thePureLife-plusbrochureforcostsandcompletedetails.ContractformICC18PRFNG-NI-18orFormSeriesPRFNG-NI-18.TexasLifeislicensedtodobusinessin theDistrictofColumbiaandeverystatebutNewYork.
21M058-CGeneric2001(exp0523)


Partial List of Eligible Expenses:
Flexible Spending Account (FSA)

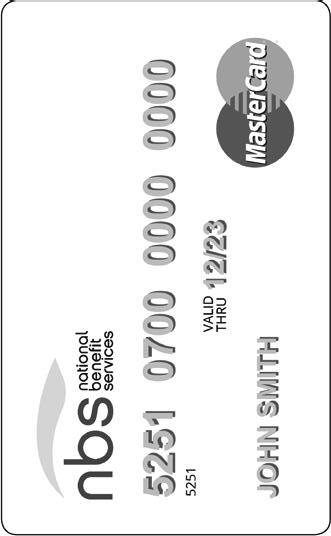








•American Fund/Capital Guardian
•Americo Financial Life/Annuity
•Equitable (formerly AXA)
•Horace Mann Life Ins. Co.
•National Life Group (LSW)
•PlanMember Services Corp.
•ROTH - Equitable (formerly AXA)
•ROTH - PlanMember Services Corp.
•ROTH - Vanguard Fiduciary Trust Co.
•Security Benefit
•Thrivent Financial for Lutherans
•Vanguard Fiduciary Trust Co.