




Key highlights
• Human Papillomavirus (HPV) infection remains one of the most prevalent sexually transmitted infections worldwide, affecting millions of individuals annually.
• Cervical cancer is the most common HPV-related cancer in Romania and the third most prevalent among women.
• Romania records the highest rates of incidence and mortality from cervical cancer in the European Union (2.7 and 3.2 times higher, respectively, than the European average). Each year, approximately 3,368 women are diagnosed with cervical cancer in Romania, and 1,793 die from the disease.
• The estimated direct healthcare costs for treating cervical cancer in Romania were estimated at RON 53,176,858, or approximately €10.7 million, in 2022 alone
• Given the high incidence and mortality due to cervical cancer, HPV is a considerable burden on the healthcare system, accounting for 17.97% to 29.56% of hospital-treated cases over the last decade and 15% to 30% of annual surgical procedures. Also, the cost per case has doubled in the past three years, amounting to RON 15,732, or approximately €3,167, per case.
• Other HPV-related cancers in Romania include cancers of the oral cavity, vulva, vagina, anus, penis, and oropharynx. While these cancers are often linked to an HPV infection, the association is less definitive compared to cervical cancer.
• Comprehensive data on the costs associated with these non-cervical HPV-related cancers in Romania is scarce, which poses significant challenges in fully understanding and addressing the economic impact of HPV-related diseases in the country.
• Indirect costs associated with HPV-related diseases are considerable, with future lost productivity due to HPV-related cancer mortality estimated at €53,9 million, or approximately RON 268,039,902.
• The country's primary preventive measures focus on combating cervical cancer due to its high incidence and mortality. However, these efforts will also yield broader benefits by addressing other HPV-related diseases.
• The coverage vaccination rate in Romania is extremely low, with the most recent data showing that only 12%–13% of the eligible population is vaccinated.
• In 2023, Romania launched one of Europe's largest programs to combat HPV-related cancers, offering free vaccinations to boys and girls aged 11 to 18 and subsidizing the vaccine by 50% for women aged 19 to 45, which is expected to lead to significant improvement in terms of overall health outcomes and reduce societal and healthcare costs.

• Educational campaigns in Romania are crucial for dispelling misconceptions about the HPV vaccine and ensuring higher vaccination coverage as scepticism towards these vaccinations remains the primary obstacle.


Abbreviations
Abbreviation Definition
CC Cervical cancer
CIN Cervical intraepithelial neoplasia
HPV Human Papillomavirus
NIP National Immunization Program

Human Papillomavirus (HPV) infection remains one of the most prevalent sexually transmitted infections worldwide, affecting millions of individuals annually. In Romania, as in many other countries, HPV poses a significant public health challenge due to its association with various cancers, including cervical, anal, and oropharyngeal cancers, among others. These diseases not only impact individual health but also impose substantial socioeconomic burdens on healthcare systems and society at large.
Understanding the socioeconomic impact of HPV-related diseases is crucial for several reasons. Firstly, the direct medical costs associated with treating HPV-induced cancers are substantial, encompassing diagnosis, treatment, and long-term care. Moreover, indirect costs such as productivity losses due to morbidity and premature mortality further exacerbate the economic burden. The economic impact of HPV-related diseases underscores the importance of effective prevention strategies, including vaccination and screening programs, in mitigating both health and financial consequences.
Investigating the socioeconomic aspects of preventive measures against HPV is imperative for accurately allocating resources to mitigate the health burden caused by HPV-related diseases. Vaccination against high-risk HPV types has demonstrated significant effectiveness in reducing infections and subsequently, preventing cancers. Early detection through screening programs allows for timely intervention, potentially preventing the progression of precancerous lesions to invasive cancer. By assessing the cost-effectiveness of these interventions, policymakers and healthcare providers can make informed decisions about resource allocation and public health policies.
In Romania, as elsewhere, the socioeconomic impact of HPV-related diseases and the effectiveness of preventive measures warrant comprehensive analysis. This report aims to explore these facets, providing insights into the current landscape, identifying gaps in knowledge, and recommending strategies to enhance public health outcomes and economic efficiency in managing HPV infections and associated diseases.
To this aim, we performed a literature and information search in PubMed to identify indexed literature as well as grey literature sources to identify additional and complementary sources

of information. For the PubMed search, articles were screened and identified using key terms such as "economic," "costs," "cost-effectiveness," and "cost of illness," along with HPVrelated terms. Studies focusing on the economic impact of HPV-related diseases and studies reporting the economic effects of preventive measures were included in our review Furthermore, a targeted Google search was conducted to identify any additional relevant information. Only credible sources, such as governmental websites (e.g., the Romanian Ministry of Health), were considered. The identified articles and documents were then reviewed to extract relevant data on the costs associated with HPV-related diseases, including direct medical costs, indirect costs, and broader economic impacts. This methodology ensures a comprehensive overview of the economic burden, incorporating both peerreviewed studies and authoritative grey literature sources.

Statistics for Romania
• Population (2024) (1) 19.6 million
• GDP per capita (2024) (2)
$43,180
• Currency
Romanian Leu (L)
• National HPV prevention programs Vaccination (2020) –Cervical cancer screening (2012)
• Vaccine coverage (3) 12%
Cervical cancer (CC) is the most prevalent HPV-related cancer in Romania and the third most common cancer in the country among women, after breast and colorectal cancer which differs from the pattern across the EU (4). Romania has the most unfavourable epidemiological profile and the highest disease burden caused by CC in the European Union, with the most significant contribution to the incidence and mortality from CC in the EU27. Therefore, approximately 12% of women newly diagnosed with CC (over 1 in 8 cases) and 13% of deaths (nearly 1 in 8 cases) across all 27 EU Member States are from Romania. With 3,368

new cases recorded in 2022 and 1,793 deaths (4), Romania records the highest rates of incidence and mortality from CC in the European Union (2.7 and 3.2 times higher, respectively, than the European average) (5)
Although Romania has experienced economic growth in recent decades, its age-standardized incidence rate of CC (32.6 per 100,000 inhabitants) is comparable to rates observed in countries with a significantly lower level of economic development (e.g., Venezuela, Peru, Congo, or Myanmar) (6) Regarding mortality, the situation for women in Romania is more unfavourable compared to incidence. With a crude mortality rate of 16.8 deaths per 100,000 women, CC is the fourth most common cause of cancer-related death among women in Romania (7) Other HPV-related cancers in Romania include cancers of the oral cavity, vulva, vagina, anus, penis, and oropharynx, which are also often consequences of HPV infection. After CC, the second most frequent HPV-related cancer is oral cavity cancer, with a crude incidence rate of 17.2 per 100,000 individuals for males and 3.26 for females (8). However, it is important to note that, unlike CC, not all cases of oral cavity cancer are directly associated with HPV. A summary of the annual number of cases and deaths for cervical and other HPVrelated diseases is presented in Table 1
3.2. Socioeconomic burden of HPV-related diseases in Romania
HPV-related diseases are not only associated with increased mortality but also impose significant costs on individuals and society. The socioeconomic burden of these diseases was estimated using available data that we obtained from the literature. This involved extracting reported healthcare costs incurred by both the healthcare system and patients for each HPVrelated disease. Whenever possible, we also extracted societal costs, which include, for instance, productivity losses due to absenteeism or mortality, informal care costs, and productivity losses related to caregiving.

3.2.1. Healthcare costs
3.2.1.1.
Data on the economic burden of HPV-related diseases in Romania is, in general, limited. Nonetheless, a study conducted in 2023 by Simion et al. provided some information on the treatment costs associated with CC (10). By searching the electronic database of the Bucharest Oncology Institute, it found that CC places a large burden on the healthcare system in Romania, both in terms of the number of cases and the severity of the disease. Over the last decade, CC accounted for:
• 17.97% to 29.56% of the total cases treated in the hospital over this period, and
• 15% to 30% of all surgical procedures performed in a year. Moreover, most cases (>87% each year) were diagnosed at advanced stages (>stage Ib) of the disease which resulted in more than just local treatment with 3.5%–5.9% of the surgical cases treated each year requiring extreme surgical procedures (such as pelvic exenterations) to ensure optimal treatment for the patient.
These factors combined with the severity of the associated pathology of patients (many being elderly or having cardiac, pulmonary, renal, or other chronic illnesses), led to an increase in the median duration of hospital stay for each being 7.62 days in 2022. Consequently, due to both increased stay and costs of treatment, also the cost per case has doubled between 2020 and 2022, reaching a value of RON 12,149/case/year treated in 2022 (RON 15,732 per case, or approximately €3,167, inflated to 2024) (vs. RON 5,146 per case treated in 2020). This cost represents the total amount paid by the hospital for the medication, equipment, and devices needed for treating a case and the costs associated with the patient’s hospital stay (electricity, water, cleaning services, food, etc.) (10). When taking into account the incidence number of CC in 2020 (3,380), the estimated direct healthcare costs of CC in Romania per year were RON 41,063,620 in 2022 (RON 53,176,858, or around €10.7 million, inflated to 2024).
Despite the considerable socioeconomic burden imposed by HPV-related CC, it is important to acknowledge that HPV is also linked to several other cancers, including oropharyngeal, vulvar, vaginal, anal, and penile cancers. Unfortunately, comprehensive data on the costs associated with these non-cervical HPV-related cancers in Romania is scarce. This poses significant challenges in fully understanding and addressing the economic impact of HPVrelated diseases in the country.
The absence of detailed information on the costs of non-cervical HPV-related cancers leads to an underestimation of the true burden of HPV in Romania. Without accurate cost data, it

is difficult to assess the full economic impact, which includes direct medical costs, indirect costs due to productivity losses, and intangible costs related to quality of life. Consequently, public health strategies may not fully reflect the extent of the problem, potentially leading to insufficient resource allocation and inadequate healthcare responses.
One possible explanation for the scarcity of data on non-cervical HPV-related cancers is Romania's very low HPV vaccination coverage rate. As of recent years, the coverage rate for HPV vaccination in Romania remains significantly lower compared to other European countries. This low vaccination uptake may contribute to a higher incidence of CC, thereby directing public health efforts and resources primarily towards CC prevention and treatment. In such a context, the focus on CC can overshadow the need to address other HPV-related cancers, leading to less attention and fewer studies on their economic impact.
Furthermore, the low vaccination coverage rate indicates that a large proportion of the population remains at risk for HPV infection and its associated diseases. This situation underscores the urgent need for comprehensive public health initiatives that not only prioritize CC but also consider the broader spectrum of HPV-related diseases. Enhancing HPV vaccination coverage could significantly reduce the incidence of all HPV-related cancers, thereby mitigating their overall socioeconomic burden.
3.2.2. Indirect costs
Studies on indirect costs associated with HPV-related diseases in Romania were very scarce in the literature. These costs can be substantial, particularly in the case of cancer, and consist primarily of productivity losses. The productivity losses arise from absenteeism due to cancer treatment, premature death, and the caregiving responsibilities shouldered by family members or other caregivers. Additionally, the emotional and psychological impact on patients and their families may lead to further mental health care costs.
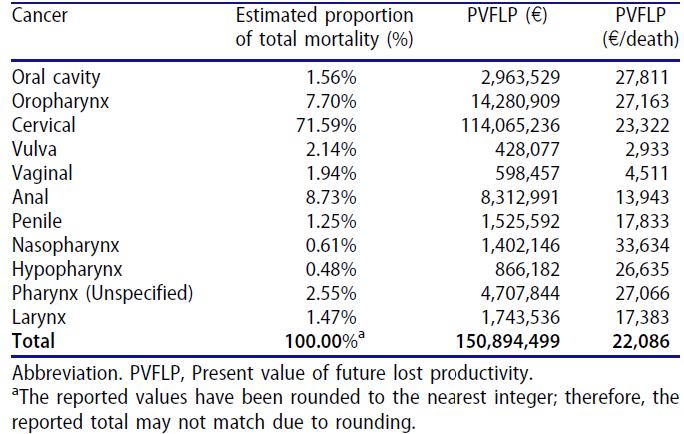
A study by Sabale et al. estimated the impact of premature mortality due to HPV-related cancer on societal costs in Central and Eastern Europe in 2019. To identify the impact, three factors were taken into account (1) years of life lost (2) years of productive life lost (3) present value of future lost productivity, with this last one being the monetary value of the premature death. The finding showed that Romania had the second-highest total number of deaths HPVassociated deaths (1,957) which, considering the total population size, resulted in the highest crude mortality rate of 0.0101%. This resulted in 31,617 years of life lost and 9,718 years of productive life lost due to premature death. Using these values, the present value of future lost productivity associated with HPV-related cancer mortality was estimated at approximately €44.5 million (€53.9 million, or around RON 268,039,902, inflated to 2024) corresponding to €22,757 (€27,582, or around RON 136,980, inflated to 2024) of the present

value of future lost productivity per death, which is higher than the value compared to all the countries included for the region of Central and Eastern Europe (€22,086 per death) (11)
Moreover, this study presented the present value of future lost productivity stratified by cancer in Central and Eastern Europe. CC was estimated to contribute the most to the total mortality of HPV-related cancer (71.59% of deaths), leading to the highest present value of future lost productivity amounting to more than €114 million (€138.2 million, or around RON 686,594,883, inflated to 2024) Oropharynx cancer, despite accounting for only 7.70% of mortality, resulted in more than €14 2 million (€17 3 million, or around RON 85,961,325, inflated to 2024) of lost productivity. However, the present value of future lost productivity per death for CC is lower compared to other cancers ( Figure 2). This is because CC primarily affects women, who generally have lower average incomes and earlier retirement ages than men, resulting in a reduced economic impact from lost productivity. In contrast, nasopharyngeal cancer, despite having a lower productivity loss of €1.4 million (€1.7 million, or around RON 8.4 million, inflated to 2024) due to a low HPV attribution fraction (10.8%), exhibits the highest productivity loss per death (€33,634), largely because a significant proportion of deaths occur among men (76%).
3.2.3. Total
Information on the total costs associated with HPV-related cancers is scarce; however, a rough calculation could be performed using information from previous sections. Taking into account the direct CC costs (approximately RON 53.1 million, or around USD 10.7 million inflated to 2024) and the indirect costs from HPV-related cancer (RON 268 million, or USD

Economic burden HPV-related diseases (RO)
53.9 million inflated to 2024), the total annual economic burden of HPV-related cancers in Romania would be around RON 321.1 million, or USD 64.6 million.
As mentioned in the previous sections, Romania has the highest incidence and mortality of CC in Europe. To combat this issue, in 2008, Romania started alongside other European countries a vaccination program against HPV, fully covered by national health authorities (12) Aimed at 10–11-year-old girls, the vaccination program saw only a 2.6% coverage rate due to parental refusal, consequently leading to the suspension of the program. In 2009, following an awareness campaign, a new vaccination campaign started, aiming at 12–14-year-old girls. Furthermore, in 2011, vaccination was extended first to the age groups of 15–19 years old, and then to 20–24 years old women (13) Still, the coverage remained low, once again leading to the suspension of the program. Despite further attempts at introducing vaccination programs in 2013 and 2019, data from 2020 and 2021 indicate that less than 50,000 girls got vaccinated and the vaccine coverage remained at 2%, largely also attributable to the COVID19 pandemic which has caused disruptions in immunization in several countries (14-16). The rest of the female population and male adolescents were not eligible for free vaccination through the program.
To ensure higher uptake, as of 2023, Romania is a part of the European ReThinkHPVaccination initiative which aims to support EU Member States in achieving the HPV vaccination and cancer prevention objectives of Europe's Beating Cancer Plan and Mission on Cancer and reduce inequalities. The specific objectives are:
- a virtual HPV vaccination knowledge centre for countries with low vaccination rates and synergies with the EU Knowledge Centre on Cancer;
- a communication strategy for Romania and an HPV vaccination behaviour matrix;
- International training courses for HPV vaccination communication based on the behaviour matrix;
- guidelines and a handbook for combating false and misleading information about HPV vaccination (17).
As of December 2023, HPV vaccination in Romania is fully reimbursed for both sexes, for individuals aged 11 to 19, and 50% reimbursed for women aged 19 to 45. The transition to a reimbursement system can enable a more widespread use of vaccination, consequently. Nevertheless,the most recent data indicate that only 12%–13% of the eligible population in the country is vaccinated (3).

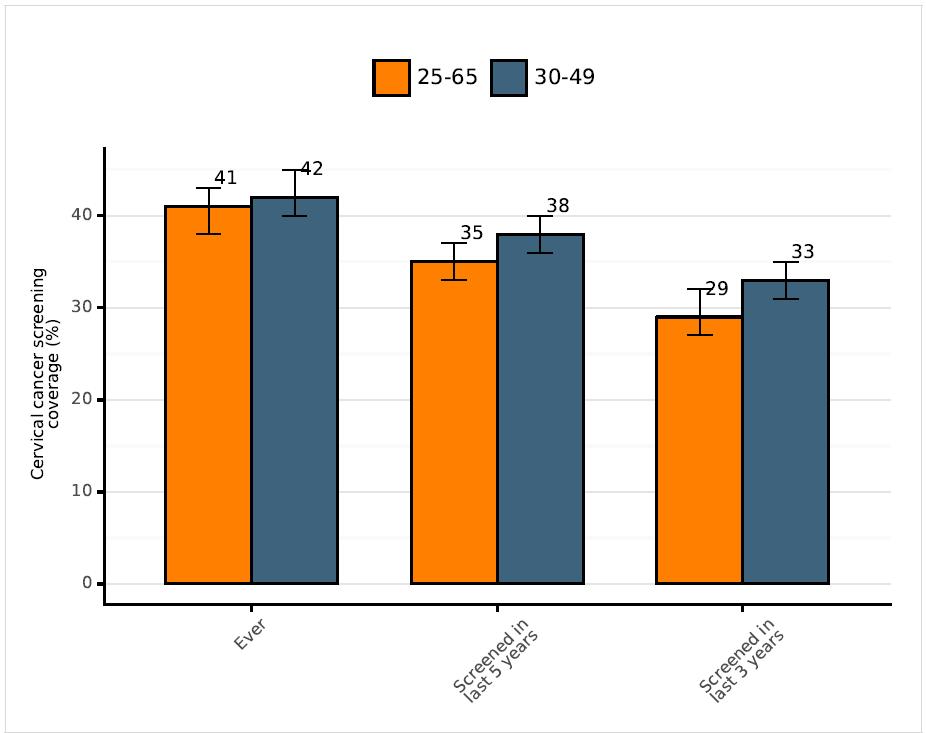
In addition to the vaccination program, in 2012, a national CC screening programme aimed at 25–64-year-old women was initiated (8) The screening in Romania is conducted cytology and women are recommended to undergo screening every five years, irrespective of their insurance status, presence of symptoms and previous CC diagnosis or total hysterectomy The national organized CC screening program was recently updated with the introduction of HPV testing (18) However, there is no active invitation system in place (e.g. letters, telephone calls, etc.), which potentially results in a lower number of individuals using the available program General practitioners and gynaecologists are supposed to provide information and instructions on the screening. The coverage of CC screening in Romania in 2019 is shown in Figure 3, showing coverage rates below 50% and decreasing rates over the years.
Economic evaluation studies are crucial for helping policymakers and healthcare providers allocate resources efficiently, ensuring that funds are directed towards the most beneficial and cost-effective measures. However, these studies are lacking in the literature on Romania.
3.3.1. Cervical cancer screening
CC screening presents significant economic benefits by reducing the incidence and mortality associated with the disease. However, in Romania, the coverage rates for CC screening are low, highlighting a substantial gap in preventive healthcare. No study was identified highlighting the socioeconomic benefits of prevention in Romania. However, a study, in 2009,

assessed factors contributing to inequalities in cervical screening(19) Several factors contribute to these low screening rates, particularly socioeconomic disparities. Women with lower levels of education and financial resources, as well as those living in smaller or rural settlements, are among the most under-served groups. Additionally, ethnic disparities are evident, with women of Turkish and Roma descent having notably lower screening rates.
Economic conditions significantly influence screening history, often mediated by structural barriers within the healthcare system. Women face multiple challenges in accessing smear tests, including lack of insurance, irregular contact with healthcare professionals, and inconvenient or time-consuming services. The healthcare system's emphasis on curative care over preventive measures further exacerbates these issues, as providers prioritize resources for treatment rather than screening. The structural barriers within the healthcare system are a major predictor of the lack of cervical screening history and serve as a critical mediator of the effects of socioeconomic status on screening (19). Women from socioeconomically vulnerable backgrounds are particularly affected by these barriers, which significantly impact their ability to access necessary preventive care. Improving the coverage of CC screening in Romania requires addressing these socioeconomic and structural barriers, especially by increasing awareness and accessibility of screening. This could consequently lead to an increase in screening and detection of CC, and reduced mortality derived from it.
The socioeconomic benefits of HPV vaccination in Romania are substantial, as highlighted by the potential cost savings and the reduction in HPV-related disease burden. The study referenced, albeit in abstract form, demonstrates significant economic advantages of implementing a mass vaccination program using either the bi-valent or 4-valent vaccine (20). Specifically, over a one-year time horizon, the bi-valent vaccine is projected to save RON 17,706,490 (around €3.5 million), primarily due to the avoidance of 820 hospitalizations for CC, amounting to savings of RON 1,273,898 (around €256,490). Similarly, the 4-valent vaccine would save RON 16,432,592 (around €3 3 million), with an additional RON 153,395 (around € 30,885) saved by preventing 205 cases of genital warts.
The lack of comprehensive data on the full economic burden of HPV-related diseases and the benefits of vaccination may reflect the limited data available on HPV prevalence and disease burden in Romania, as well as the historically low coverage rates of HPV vaccination. However, the persistently low vaccination coverage rates, along with recent changes in vaccination policy such as the reimbursement of vaccines and the introduction of the 9valent vaccine highlight the need for further evidence to showcase the full scope of vaccination benefits. Moreover, future studies should account for potential savings from preventing other HPV-related cancers, such as oropharyngeal, anal, vulvar, and penile cancers

as well as savings that could result from averted productivity losses due to reduced absenteeism, decreased disability and avoided premature mortality. These omissions likely result in an underestimation of the true economic benefits of HPV vaccination.
Despite the potential benefits, the primary obstacle to the successful implementation of a vaccination program in Romania has been the acute lack of information provided to parents and eligible girls (10) Many parents obtain information from dubious sources such as social media, the internet, and mass media, leading to widespread misinformation. Additionally, parents' beliefs, attitudes, and social prejudices contribute to the low uptake of the vaccine. Poor participation in vaccination campaigns is also attributed to deficient public health strategies. Despite having sufficient vaccine doses to cover the targeted population, widespread distribution in many accessible locations (including schools), and adequate numbers of doctors to administer the vaccine, the programs have failed. The primary reason for this failure is the lack of adequate information campaigns addressing the connection between HPV and cancer, and the general lack of recognition of the importance and benefits of HPV vaccination. A more recent study, conducted in November 2023 as part of the ReThinkHPVaccination project, provides valuable insights into the state of HPV vaccination in the country (21) The study, based on a nationally representative sample of over 1,100 adults, reveals that while 79% of respondents have heard of HPV, only 7% of adults and 5% of their children are vaccinated. Notably, 90% of unvaccinated respondents indicated they had not been advised to get vaccinated. Despite low vaccination rates, over half of respondents consider HPV vaccination to be safe, and 54% believe it should become mandatory. These findings emphasize the critical need for improved public education, better vaccination recommendations from healthcare providers, and targeted efforts to increase vaccine uptake, particularly in light of Romania's current low vaccination rates
In conclusion, Romania's struggle to implement effective HPV-related preventive measures, such as vaccination and CC screening, highlights the significant economic and public health implications of underutilizing these programs. Despite various attempts to introduce HPV vaccination since 2008, coverage rates remain critically low, partly due to misinformation, lack of public awareness, and inadequate health communication strategies. Although recent policy changes, including the reimbursement of vaccines and the introduction of the 9-valent vaccine, offer hope for increasing vaccination rates, only 12%–13% of the eligible population is currently vaccinated. Additionally, the low coverage of CC screening, exacerbated by socioeconomic and structural barriers, further underscores the challenges in combating HPVrelated diseases in Romania. Future efforts must prioritize not only increasing vaccination and screening uptake but also generating robust economic evidence to demonstrate the full benefits of HPV vaccination. This includes preventing not just CC but other HPV-related cancers and conditions, such as genital warts, as well as reducing long-term healthcare costs

and improving public health outcomes. Enhanced public education and targeted communication campaigns are critical to overcoming barriers and fostering greater acceptance of vaccination in Romania.

1. World population review - Romania population 2024 [updated 1 January 2024. Available from: https://worldpopulationreview.com/countries/romania-population.
2. International Monetary Fund - GDP per capita, current prices 2024 [updated 1 January 2024. Available from: https://www.imf.org/external/datamapper/PPPPC@WEO/HUN/ROU.
3. Simion L, Chitoran E, Cirimbei C, Stefan DC, Neicu A, Tanase B, et al. A Decade of Therapeutic Challenges in Synchronous Gynecological Cancers from the Bucharest Oncological Institute. Diagnostics (Basel). 2023;13(12).
4. Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J Clin. 2021;71(3):209-49.
5. ECIS - European Cancer Information System, European Comission. Incidence and mortality of cervical cancer. 2022 [Available from: https://ecis.jrc.ec.europa.eu/.
6. Ferlay J, Colombet M, Soerjomataram I, Parkin DM, Pineros M, Znaor A, et al. Cancer statistics for the year 2020: An overview. Int J Cancer. 2021.
7. ECIS - European Cancer Information System, European Comission. Cancer burden statistics and trends across Europe. [Available from: https://ecis.jrc.ec.europa.eu/.
8. Bruni L AG, Serrano B, Mena M, Collado JJ, Gómez D, Muñoz J, Bosch FX, de Sanjosé S. Human Papillomavirus and Related Diseases in Romania. 2023 10 March 2023.
9. Hartwig S, Syrjänen S, Dominiak-Felden G, Brotons M, Castellsagué X. Estimation of the epidemiological burden of human papillomavirus-related cancers and nonmalignant diseases in men in Europe: a review. BMC Cancer. 2012.
10. Simion L, Rotaru V, Cirimbei C, Gales L, Stefan DC, Ionescu SO, et al. Inequities in Screening and HPV Vaccination Programs and Their Impact on Cervical Cancer Statistics in Romania. Diagnostics (Basel). 2023;13(17).
11. Sabale U, Karamousouli E, Popovic L, Krasznai ZT, Harrop D, Meiwald A, et al. The indirect costs of human papillomavirus-related cancer in Central and Eastern Europe: years of life lost and productivity costs. J Med Econ. 2024;27(sup2):1-8.
12. European Centre for Disease Prevention and Control. Introduction of HPV vaccines in EU countries – an update. Stockholm: ECDC; 2012.
13. Pistol A, Stanescu A. National Immunization Programme in Romania. Institutul national de sanatate publica; 2018.
14. HPV Rethink Vaccination. HPV Vaccination and Screening [Available from: https://rethink-hpv.eu/en/wiki/romania-hpv/hpv-vaccination-in-romania/.
15. Gountas I, Favre-Bulle A, Saxena K, Wilcock J, Collings H, Salomonsson S, et al. Impact of the COVID-19 Pandemic on HPV Vaccinations in Switzerland and Greece: Road to Recovery. Vaccines (Basel). 2023;11(2).
16. Wahner C, Hubner J, Meisel D, Schelling J, Zingel R, Mihm S, et al. Uptake of HPV vaccination among boys after the introduction of gender-neutral HPV vaccination in Germany before and during the COVID-19 pandemic. Infection. 2023;51(5):1293-304.

17. European Commision. ReThinkHPVaccination, Europe’s Beating Cancer Plan. 2023. 18. Ministry of Health, Romania - Approval of the screening methodology for colorectal cancer. 2024.
19. Todorova I, Baban A, Alexandrova-Karamanova A, Bradley J. Inequalities in cervical cancer screening in Eastern Europe: perspectives from Bulgaria and Romania. Int J Public Health. 2009;54(4):222-32.
20. Preda AL, Moise M, Van Kriekinge G. A Cost-Consequence Analysis of Human Papillomavirus Vaccination in Romania. Value Health. 2014;17(7):A631.
21. HPV Rethink Vaccination. Sondaj național: Analiza percepțiilor și atitudinilor privind vaccinarea HPV în România 2024 [Available from: https://rethinkhpv.eu/ro/rethinkhpvaccination-analiza-perceptii-atitudini-vaccinare-hpv-romania/
