




Key highlights
3.2.
3.2.1.
3.2.1.1.
3.2.1.2.
3.2.2.
3.3.1.

such as "economic," "costs," "cost-effectiveness," and "cost of illness," along with HPVrelated terms. Studies focusing on the economic impact of HPV-related diseases and studies reporting the economic effects of preventive measures were included in our review Furthermore, a targeted Google search was conducted to identify any additional relevant information. Only credible sources, such as governmental websites (e.g., Philippine Statistics Authority, Department of Health), were considered. The identified articles and documents were then reviewed to extract relevant data on the costs associated with HPV-related diseases, including direct medical costs, indirect costs, and broader economic impacts. This methodology ensures a comprehensive overview of the economic burden, incorporating both peer-reviewed studies and authoritative grey literature sources.

Statistics for the Philippines
• Population (2023) (1)
117 3 million
• GDP per capita (2022) (2)
USD3,498
• Currency Philippine peso (₱)
• National HPV prevention programs (3, 4) Vaccination (2015) –
Cervical cancer screening – not implemented (opportunistic)
• Vaccine coverage, last dose (5) 11.6% (2023)
3.1.
transmission and HPV-related diseases in the Philippines
Since sexual intercourse is the primary route of transmission, all sexually active individuals are at risk of genital HPV infection. In the Philippines, the median age at first sexual intercourse is 20.7 years (6). Given that 63.4% of the population is aged 18 and older (7), a substantial portion of the Filipino population is at risk of HPV infection and, consequently, HPV-related diseases.

Cervical cancer (CC) is the most prevalent HPV-related cancer in the Philippines and the second most common female cancer in women of all ages in the country (8). It has an incidence rate of approximately 14.5 cases per 100,000 women per year, leading to about 7,897 new CC cases being diagnosed annually in the Philippines (estimations for 2020) (8) Moreover, CC ranks as the second leading cause of female cancer in the Philippines, with a crude mortality rate of 7.43 deaths per 100,000 women per year, leading to about 4,052 death cases annually (estimations for 2020) (8)
Other HPV-related cancers in the Philippines include cancers of the oral cavity, vulva, vagina, anus, penis, and oropharynx, which are also often consequences of HPV infection
After CC, the second most frequent HPV-related cancer is laryngeal cancer, with a crude incidence rate of 2.46 per 100,000 individuals for males and 0.36 for females (8) However, it is important to note that, unlike CC, only a small proportion of laryngeal cancer (2.2%) is directly associated with HPV That way, other HPV-related cancers with a lower number of annual cases, but higher HPV attribution, such as oropharyngeal cancer (30.8% HPV attribution), could be considered more relevant HPV-related cancers. A summary of the annual number of cases and deaths for cervical and other HPV-related diseases is presented in Table 1
Table 1. Estimated annual number of new cases and annual number of new deaths per cancer type in the Philippines in 2020 (8)
Anal Cancer M: 113; W: 90 M: 61; W: 31
Oropharyngeal Cancer M: 339; W: 126 M: 203; W: 69
Oral Cavity Cancer M: 875; W: 686 M: 504; W: 366 2.2%
Laryngeal Cancer M: 1,354; W: 196 M: 885; W: 135 2.4%
Vulvar Cancer
Vaginal Cancer
Abbreviations: HPV, Human Papilloma Virus
Data on the prevalence and incidence of genital warts in the general population of the Philippines is, in general, not available. However, a 2019 study conducted in four major cities in the Philippines (Manila, Luzon, Mindanao, and Visayas) among men and women aged 18 to 60 years old assessed the prevalence of genital warts in this population. The reported prevalence in women was 3.39%, while genital warts were present in 8.0% of the men, resulting in a prevalence of 4.78% for the whole study population (10).

Notes: a The initial stage refers to the phase after cervical cancer is diagnosed; Remission stage has no detectable signs of cancer post-treatment; Persistence stage is the phase in which the cancer is still present after treatment; Recurrence stage is when the cancer returns after a period of remission. b Stages I, II, III and IV refer to the FIGO (International Federation of Obstetrics and Gynecology) cervical cancer stages. In stage I, cervical cancer has formed and is found in the cervix only; In stage II, cervical cancer has spread to the upper two-thirds of the vagina or the tissue around the uterus; In stage III, cervical cancer has spread to the lower third of the vagina and/or to the pelvic wall, and/or has caused kidney problems, and/or involves lymph nodes; In stage IV, cervical cancer has spread beyond the pelvis, or has spread to the lining of the bladder or rectum, or has spread to other parts of the body.
The data highlights the escalating costs of treating invasive CC in the Philippines as the disease progresses. In the initial stage, treatment costs range from PHP 111,662 (USD 1,979) for the early stages to PHP 152,553 (USD 2,704) for the advanced stages. The persistence stage incurs the highest expenses, particularly in the advanced stages, where costs can reach PHP169,702 (USD 3,008). Treatment during remission, where cancer is under control, is the least expensive, with costs as low as PHP23,692 (USD419). These figures underscore the economic burden of advanced cancer and the importance of early detection and effective treatment to potentially reduce costs.
Another study reported estimates of CC healthcare costs based on the 2018 insurance claims for the PhiHealth database (12) The total cost per treated case at each CC stage was calculated as a weighted average of the case rates for various treatment procedures at each CC stage. This was then adjusted based on the likelihood of accessing treatment, using data from the 2019 Philippine General Hospital annual report The healthcare costs from a government perspective, which exclude out-of-pocket expenditures, are reported in Table 3.
Notes: (1) Disease stages can be related to the traditional Tumour-Node-Metastasis (TNM) classification system as follows: “Local disease” corresponds to stages I and II TNM classification, i.e., localized primary tumour; “Regional disease” corresponds to stage III TNM classification system, i.e., metastasis to regional lymph nodes; “Distant disease” corresponds to stage IV TNM classification system, i.e., distant metastatic

diagnosed CC cases in the Philippines from a governmental perspective is estimated at PHP 6.6 billion (approximately USD 118.2 million) in that year.
CC is one of the most frequent and preventable cancers linked to HPV, making it a primary target for public health programs and data collection. However, the economic burden of other HPV-related cancers and indirect costs associated with HPV could be substantial, encompassing significant healthcare costs and productivity losses due to absenteeism, premature death, and caregiver costs. Therefore, more research is needed to assess the total costs of HPV in the Philippines including other HPV-associated cancers
3.3.
To fight the occurrence of HPV-related diseases and reduce the socioeconomic burden associated with the virus, the Philippines has published official recommendations for screening for CC, as well as implemented a national vaccination program.
3.3.1.
Screening for CC is a critical preventive measure, particularly in the Philippines, where the 5year survival rate for CC is just 44% due to most cases being diagnosed at an advanced stage (3). This survival rate has remained unchanged from 1980 to 2010, underscoring the importance of early detection and intervention before symptoms appear. Despite the publication of official screening recommendations in 2009, estimated coverage remains alarmingly low, with only about 1% of eligible populations receiving screening (14) (Figure 2). According to the WHO, as of 2021, fewer than one in ten eligible Filipino women had been screened in the past five years (15). The complex infrastructure and human resource requirements pose significant barriers to effective implementation, particularly in rural areas where cytologic screening facilities and cytopathologists are scarce. Most cytopathologists practice in the National Capital Region, leaving rural areas underserved (16). Additional barriers to an effective screening program in the Philippines include high out-ofpocket expenses, low health literacy, fear of pain, stigma associated with a cancer diagnosis, and general healthcare accessibility (17). Consequently, the national CC screening program has adopted visual inspection with acetic acid (VIA) as its primary screening test, targeting women aged 25 to 55 every 5–7 years (15) VIA is considered a more feasible option in low-resource settings, as it is cost-effective, can be performed by trained health workers, and provides immediate results.

A 2015 study evaluated the economic benefits of HPV vaccination combined with different screening strategies, including Pap smear and VIA, within the Philippines' existing screening program. The analysis found that VIA, particularly when performed on women aged 35 to 45, was the most efficient and cost-saving screening option. Shifting the primary screening method from Pap smear to VIA was shown to yield significant economic benefits, which could be further enhanced by expanding coverage (11).
In addition, to address the low screening coverage rates, several localized initiatives have been tested, though they have yet to be implemented nationwide. Opportunistic screening, where CC screening is offered to women during routine health visits, has shown potential. Also, educational initiatives were proven effective; for example, after a health lecture in a rural area, VIA screening acceptance rose from 0% to 78%, with 71.4% of the women opting to undergo testing (3).
However, a national approach is needed to significantly increase screening rates. A robust public health education campaign that addresses key factors influencing screening participation could improve compliance. While cost remains a significant barrier, combining targeted education with improved access to well-equipped screening facilities is crucial for the success of a national CC screening initiative (3).

Before the widespread introduction of HPV vaccines in the Philippines, studies showed varying levels of acceptance. For instance, a study with mothers at charity clinics revealed that 75.4% were willing to vaccinate their daughters despite limited awareness of HPV's link to CC. Similarly, 53% of adolescents at a pediatric hospital were open to vaccination if it were free. In Pampanga, commercial sex workers had a favorable attitude towards the vaccine, though the cost was a significant concern. Acceptance was generally higher when the vaccine was affordable, but barriers included fears of pain, the belief that vaccination might encourage risky behavior, and low awareness in certain groups (3).
In 2015, the Philippine government began its national HPV immunization program using either the bivalent or quadrivalent vaccine. Initially launched as a community-based initiative, the program transitioned to a school-based approach in 2017 to better reach girls aged 9 to 14 years, aiming to improve coverage and reduce dropout rates (18) Despite the vaccination being offered for free a key factor influencing its acceptance (19, 20) the Philippines continued to rank low among comparable countries in terms of HPV vaccination coverage (4) Coverage in the vaccination program population was reported by the WHO to be only 26% for the first dose and 10% for the final dose, with 27% coverage for the first dose and 3% for the final dose in 15-year-olds (3) The COVID-19 pandemic further complicated the program, leading to the suspension of in-person classes, although the government adapted by offering immunizations at health facilities, temporary stations, and even door-todoor services. The program plans to revert to its school-based approach once classes fully resume.
Regarding the cost-effectiveness of HPV vaccination in the Philippines, data have been relatively limited. However, a pivotal study published in 2022 examined the impact of routine HPV vaccination for 9-year-old girls over the period from 2022 to 2031 (12). The model projected that without vaccination, the Philippines would face 182,406 CC cases requiring treatment, 176,887 disability-adjusted life years (DALYs) lost, and 114,616 CC deaths among females born between 2012 and 2021. In the absence of vaccination, the estimated total discounted healthcare costs for treating CC in this population would reach approximately USD 33,093,804 from the government’s perspective and USD 216,468,126 from a societal perspective. Using a cost-effectiveness threshold of one times the Philippines' GDP per capita (USD 3,485 in 2019) per DALY averted, the study found that both the 2-valent and 4-valent HPV vaccines were cost-effective. However, the 9-valent vaccine was not considered costeffective for inclusion in the national immunization program, as its cost slightly exceeded the threshold. This outcome was primarily driven by the higher price of the 9-valent vaccine, despite its ability to prevent the highest number of CC cases and save the most DALYs. Overall,

HPV vaccination for 9-year-old girls from 2022 to 2031 in the Philippines is expected to avert between 97,922 and 127,166 CC cases compared to no vaccination. This prevention is projected to result in healthcare cost savings ranging from USD 17,765,888 to USD 23,071,649 from the government’s perspective and USD 116,207,508 to USD 150,912,740 from a societal perspective, excluding vaccination costs.
A more recent study from 2024 compared the use of a 4-valent compared to a 9-valent HPV vaccine to vaccinate girls 9-14 years old as part of the national immunization program (21)
Besides CC cases, other HPV-associated health outcomes included head and neck, vaginal, vulvar, penile, and anal cancers as well as genital warts Figure 3 and Figure 4 shows the cumulative reduction in HPV-related cases avoided and deaths for the strategy using the 9valent vaccine compared to using the 4-valent over 100 years
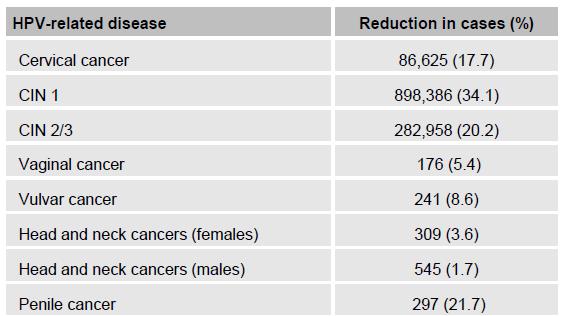
Figure 3. Cumulative reduction in HPV-related cases over 100 years: comparison between the 9-valent and 4valent vaccine strategies (21).

Figure 4. Cumulative reduction in HPV-related deaths over 100 years: comparison between the 9-valent and 4valent vaccine strategies (21)
Compared to the 4-valent vaccine, the 9-valent resulted in lower HPV-related deaths and a reduction in disease management costs by 7.9%.

16. Arcellana-Nuqui ER, Fontelo PA, Marcelo AB. Telepathology in the Philippines: A Review and Future Prospects. Acta Med Philipp [Internet]. 2016Dec.31 [cited 2024Aug.22];50(4). Available from: https://actamedicaphilippina.upm.edu.ph/index.php/acta/article/view/712
17. Ho FDV, Arevalo M, de Claro PTS, Jacomina LE, Germar MJV, Dee EC, et al. Breast and cervical cancer screening in the Philippines: Challenges and steps forward. Prev Med Rep. 2022;29:101936.
18. Department of Education, Republic of the Philippines. Inclusion of Human Papilloma Virus Vaccination in School-based Immunization Program. 2017.
19. Young AM, Crosby RA, Jagger KS, Casquejo E, Pinote L, Ybañez P, et al. Influences on HPV vaccine acceptance among men in the Philippines. Journal of Men's Health. 2011;8(2):126-35.
20. Young AM CR, Jagger KS, Richardson MB, Kloha RA, Safarian V,. HPV Vaccine Acceptability among Women in the Philippines. Asian Pacific Journal of Cancer Prevention. 2010;11(6):1781-7.
21. Uy GD, Paredes K, Sengson RF, Wang W, Sukarom I, Pavelyev A. Evaluating the Health Impact and Cost-Effectiveness of 9-Valent Human Papillomavirus Vaccination Among Females in the Philippines: A Dynamic Transmission Model Analysis. AOGIN Conference (Asia Oceania Research Organization in Genital Infection and Neoplasia); Seoul, Korea 2024.
