Key highlights
• Human Papillomavirus (HPV) infection remains one of the most prevalent sexually transmitted infections worldwide, affecting millions of individuals annually.
• In South Korea, where the median age at first sexual intercourse is 21.9 years for men and 24.1 years for women, all individuals aged 20 years and older, totalling 85.1% of the population, are potentially susceptible to HPV infection, depending on their sexual activity.
• The economic impact of HPV-related diseases highlights the crucial role of effective prevention strategies, including vaccination and screening programs, in mitigating both health and financial consequences.
• Cervical cancer is the most prevalent HPV-related cancer in South Korea, and the third most common female cancer in the country. The mean annual medical cost per incidence is highest among individuals aged 50 to 59 years, amounting to US$15,400 in 2015 (equivalent to US$20,182 when adjusted to 2024 values)
• According to the most recent data, direct medical costs attributable to cervical cancer amounted to KRW102.6 billion (US$91.2 million inflated to the year 2024)
• Other HPV-related diseases are, likewise, associated with increased mortality and impose significant costs on individuals and society. After cervical cancer, the highest healthcare costs among HPV-related diseases were for the anus and anal canal cancers, totalling US$5.1 million (US$6.7 million adjusted to 2024 values). This was followed by tonsil cancer at US$3.6 million (US$4.7 million adjusted to 2024 values) and vaginal cancer at US$1.1 million (US$1.4 million adjusted to 2024 values).
• Indirect costs of HPV-related diseases for both men and women were estimated at approximately US$205 million (US$272 million inflated to the year 2024).
• Preventive measures aimed at reducing the occurrence of HPV-related diseases and, consequently, their socioeconomic burden, include cervical cancer screening and three HPV vaccines have been approved in the country
• South Korea has two screening programs, targeting women aged 20 and older, with screening recommended every two years. Despite the availability of these programs and an active invitation system, the cervical cancer screening rate has declined in recent years among women aged 30 to 74, especially among women of lower socioeconomic status
• Since 2016, South Korea has had a vaccination program for girls aged 12 and older. As of 2024, new guidelines recommend administering bivalent and quadrivalent vaccines to girls and boys aged 11 to 12 and low-income women aged 18 to 26 as part of a catch-up program.

Abbreviations
Abbreviation Definition
CC Cervical cancer
CIN Cervical intraepithelial neoplasia
HPV Human Papillomavirus
NHIS National Health Insurance Service
NHISCSP National Health Insurance Service Cancer Screening Programme
NIP National Immunization Program

and older (7), a substantial portion of the Korean population is at risk of HPV infection and, consequently, HPV-related diseases.
Cervical cancer (CC) is the most prevalent HPV-related cancer in Korea and the third most common female cancer in women aged 15 to 44 years in the country (8). It has an incidence rate of approximately 12.6 cases per 100,000 women per year, leading to about 3,218 new CC cases being diagnosed annually in Korea (estimations for 2020) (8) Moreover, CC ranks as the ninth leading cause of female cancer in the country, with a crude mortality rate of 3.96 deaths per 100,000 women per year, leading to about 1,014 death cases annually (estimations for 2020) (8)
Other HPV-related cancers in Korea include cancers of the oral cavity, vulva, vagina, anus, penis, and oropharynx, which are also often consequences of HPV infection. After CC, the second most frequent HPV-related cancer is oral cavity cancer, with a crude incidence rate of 4.36 per 100,000 individuals for males and 2.90 for females (8) However, it is important to note that, unlike CC, not all cases of oral cavity cancer are directly associated with HPV. A summary of the annual number of cases and deaths for cervical and other HPV-related diseases is presented in Table 1
Table 1. EstimatedannualnumberofnewcasesandannualnumberofnewdeathspercancertypeinKoreain2020(8)
Cancer
Cavity Cancer
Laryngeal Cancer
564; W: 81
1,119; W: 742
; W:64
Abbreviations:HPV,HumanPapillomaVirus;M,men;W,women.
368; W:232
; W:31
HPV-related diseases other than cancer include cervical intraepithelial neoplasia (CIN), which is a precursor to CC. It is graded based on the extent of abnormal cell changes and can be detected through regular screening, enabling timely intervention to prevent progression to invasive cancer. The incidence rate of CIN 1/2 inflated to the year 2024 was 425.4 per 100,000 people, while for CIN 3 it was 39.8 per 100,000 people (10). More details regarding the differences between the incidences throughout the years can be found on Figure 2.

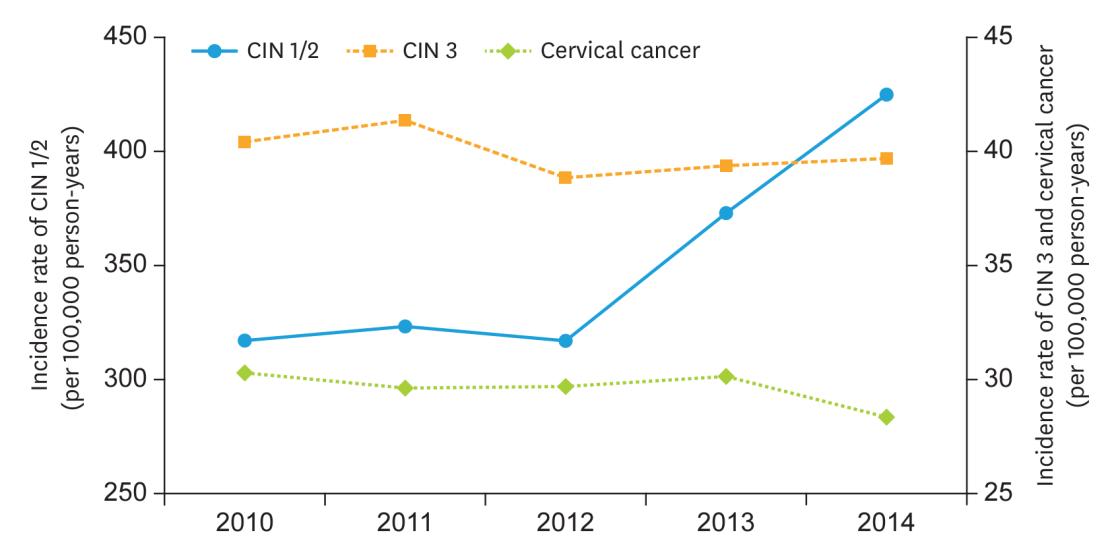
2. Incidence rate trend of CIN 1/2, CIN 3, and cervical cancer in Korea from 2010 to 2014 (10)
Data reporting the prevalence and incidence of genital warts in Korea is limited in the literature. According to data from the Health Insurance Review and Assessment of Korea, the incidence rate of genital warts was 11.6 per 100,000 men and 3.6 per 100,000 women in 2015 (11). Taking the Korean population into account (7), around 3,004 men and 931 women would present anogenital warts per year in the country.
3.2. Socioeconomic burden of HPV-related diseases in Korea
HPV-related diseases are not only associated with increased mortality but also impose significant costs on individuals and society. The socioeconomic burden of these diseases was estimated using available data that we obtained from the literature. This involved extracting reported healthcare costs incurred by both the healthcare system and patients for each HPVrelated disease. Whenever possible, we also extracted societal costs, which include, for instance, productivity losses due to absenteeism or mortality, informal care costs, and productivity losses related to caregiving
3.2.1. Healthcare costs
3.2.1.1. Cervical intraepithelial neoplasia (CIN) and cervical cancer
CIN is not considered a cancer, but its management and treatment can still generate considerable economic costs. Data from the Korean National Health Insurance Service (NHIS) from 2014 shows that the average medical costs per person for CIN 1/2 (USD 84.8, or USD 111/KRW 148,720 inflated to the year 2024) were more than five times lower than the costs related to CIN 3 (USD 466, or USD 619/KRW 829,351 inflated to the year 2024) (10) (Table 2)

Furthermore, the medical costs for people aged 30 years or older were higher than the costs for people aged 30 years or younger for CIN 1/2, CIN 3 and CC
Table 2. Medical costs per person related to CIN or cervical cancer in Korea (US$ 2014) (10)
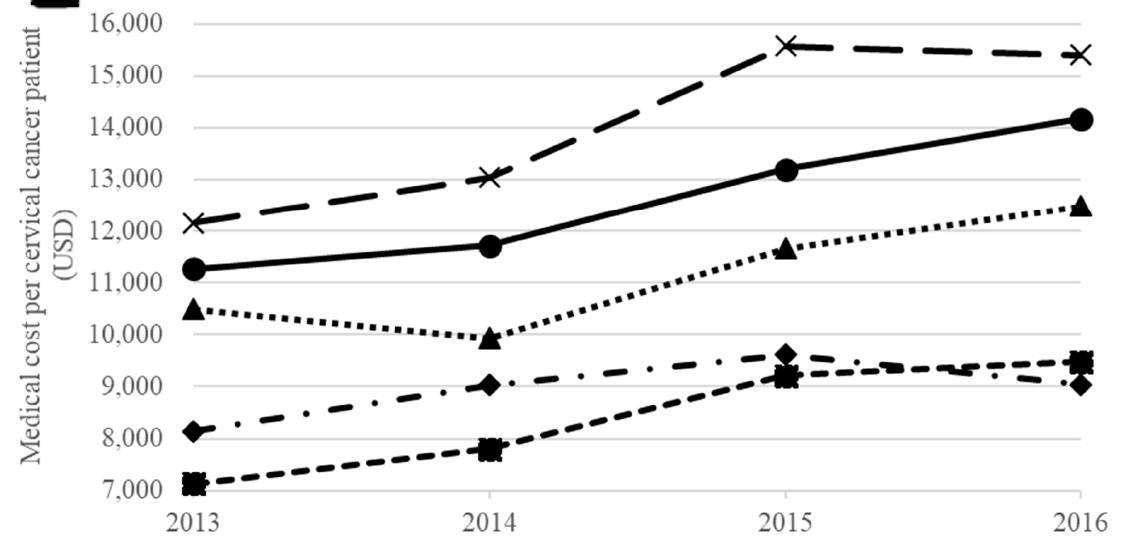
CC costs from 2015 and 2017 are also reported by the NHIS In 2015, the direct medical costs of CC in Korea amounted to USD 75.1 million (12) (USD 99.6 million/KRW 133.4 billion inflated to the year 2024), while in 2017 medical costs related to CC amounted to KRW 102.6 billion (USD 91.2 million inflated to the year 2024) (13) There were some variations in the average annual medical costs of CC per age group, with the highest mean costs seen in those aged 50 to 59 years old, amounting to USD 15,400 (USD 20,182/KRW 27,040,345 inflated to the year 2024) (14) (Table 3)
Table 3. Mean medical cost of cervical cancer per year between 2013 and 2016 per age group (14)
3.2.1.2.
Other HPV-related cancers and diseases
The economic burden becomes even more significant when considering the additional costs incurred by other HPV-related cancers and diseases. Evidence on the costs for HPV-related diseases other than CC and CIN is often lacking. However, the NHIS reported some data on HPV-related costs for diseases other than CC.
In 2015, the costs of several HPV-related cancers were reported considering only direct medical costs. As previously stated in this report, not all cases of these HPV-related diseases

are directly associated with HPV. Therefore, each HPV-related disease presented a fraction of the costs attributable to HPV according to the proportion of cases attributed to HPV. After CC, the healthcare costs of anus and anal canal cancers were the highest amongst HPVrelated diseases, amounting to USD 5.1 million (USD 6.7 million/KRW 8.9 billion inflated to the year 2024), followed by tonsil cancer (USD 3.6 million, or USD 4.7 million/KRW 6.2 billion inflated to the year 2024) and vagina cancer (USD 1.1 million, or USD 1.4 million/KRW 1.8 billion inflated to the year 2024) (12) (Table 4).
Table 4. HPV-related cancer costs in 2015, stratified by sex (12)
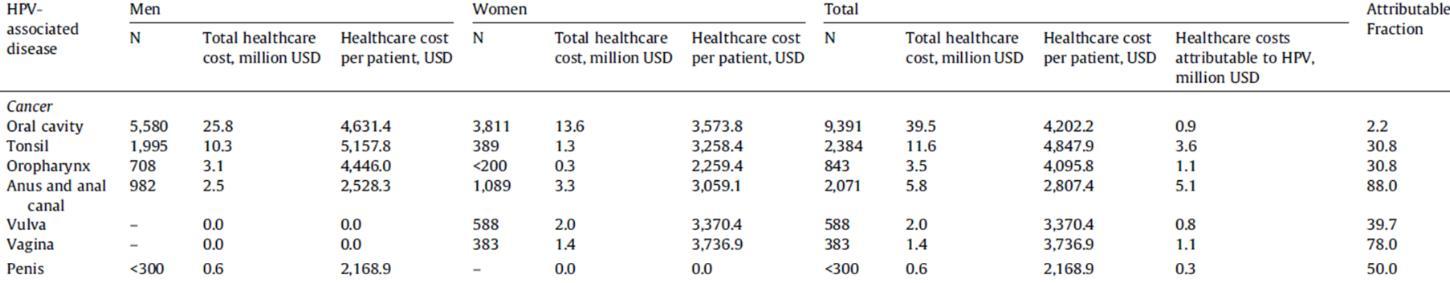
Besides CC, the highest healthcare costs per male patient were reported for tonsil cancer (USD 5,157, or USD 6,843/KWR9,168,421 inflated to the year 2024), whereas vagina cancer (USD 3,736, or USD 4,957/KRW 6,641,511 inflated to the year 2024) accounted for the highest healthcare cost per patient in women (12). Considering both sexes, the highest healthcare cost per patient was reported for tonsil cancer, amounting to a total of USD 4,847 (USD 6,432/KRW 8,617,753 inflated to the year 2024) per patient (12) Taking all HPV-related cancers other than CC into account (oral cavity, tonsil, oropharynx, anus and anal canal, vulva, vagina and penis), the total healthcare costs of HPV-related cancers in 2015 amounted to USD 12.9 million (USD 17.1 million/KRW 22,9 billion inflated to the year 2024) (12)
3.2.2. Indirect costs
Indirect costs associated with HPV-related diseases in Korea were also identified in the literature. In general, indirect costs can be substantial, particularly in the case of cancer, and consist primarily of productivity losses. They arise from absenteeism due to cancer treatment, premature death, and the caregiving responsibilities shouldered by family members or other caregivers. Additionally, there are emotional and psychological impacts on patients and their families, which may lead to further mental health care costs.
We identified one study reporting indirect costs related to HPV. This study, utilizing data from the NHIS, reported the indirect costs of HPV-related diseases in 2014, which included future costs arising from income loss, productivity loss during hospital visits, and job loss. In total, around USD 205 million (USD 272 million/KRW 364,4 billion inflated to the year 2024) of

indirect costs were reported in the country for both men and women (Table 5) (15) As CC presented the second highest economic burden among all cancer types in Korea in 2014, the costs reported for women accounted for the majority of the indirect costs in the country
3.2.3. Total costs
The total costs of HPV-related cancers in Korea reported in 2014 take into account direct medical (hospitalization and outpatient care), direct non-medical (transportation and caregiver costs) and indirect costs (future income loss, productivity loss during hospital visits, job loss costs). The total annual costs associated with HPV in Korea amounted to USD 312.6 million (USD 415.3 million/KRW 556.4 billion inflated to the year 2024) (15). The total HPV costs were considerably higher for women (USD 294.3 million, or USD 391 million/KRW 523.8 billion inflated to the year 2024) than for men (USD 18.2 million, or USD 24.1 million/KRW 32,2 billion inflated to the year 2024) (15). This difference is likely due to costs associated with CC, which account for a great share of the total costs and are only associated with women. Indirect costs accounted for around 2/3 of the total costs, while direct costs accounted for around 1/3 (15). A breakdown of the total annual costs can be found on Table 6.

3.3. Economic benefits of HPV-related preventive measures
To fight the occurrence of HPV-related diseases and reduce the socioeconomic burden associated with the virus, several preventive measures have been put in place in Korea. First of all, there is a cancer screening program to prevent CC by identifying risks and removing precancerous lesions. The Korean government has run two population-based cervical screening programs since 1999. The first one is the National Health Insurance Service Cancer Screening Programme (NHISCSP), which is available to NHIS beneficiaries in the upper 50% income bracket. The second is the National Cancer Screening Programme (NCSP), serving NHIS beneficiaries in the lower 50% income bracket. The NCSP also includes recipients of the Medical Aid Programme (MAP), which offers free or reduced-cost healthcare to low-income households and people with disabilities (11)
The Pap test was used as the primary screening tool in both programs up to 2021 when cytology became the most widely used screening method in the national screening program (11, 16) Initially, the programs targeted women aged 30 years or older but since 2016 the eligibility has been extended to individuals aged over 20 years, with all Korean women now recommended to undergo a screening every two years (11) Individuals receive an active invitation for screening (8), thereby facilitating participation in the program as they do not need to independently seek out information and services. This approach potentially results in higher utilization of the program compared to countries with no active invitation system The estimatedcoverageofcervicalscreeninginKoreacanbefoundon
Figure 3 The CC screening rate has notably declined in recent years among women aged 30 to 74 (Figure 4) (17). This decrease is more pronounced in groups with lower socioeconomic status, highlighting socioeconomic disparities in CC screening (17).

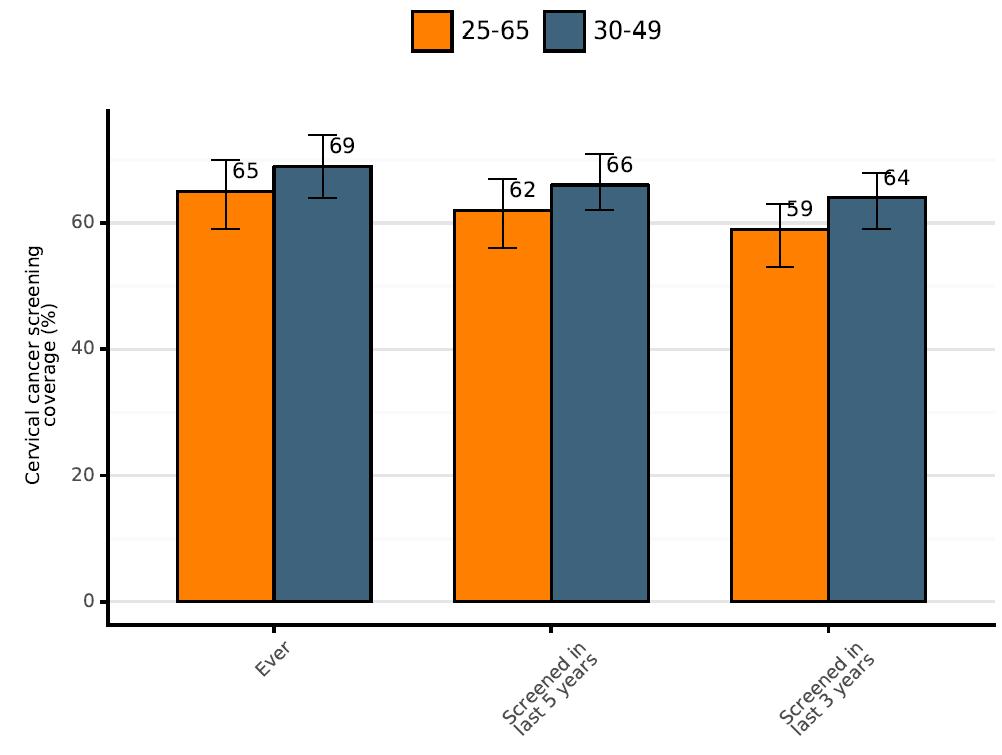
Figure 3. Estimated coverage of cervical screening in Korea in 2019 (8)
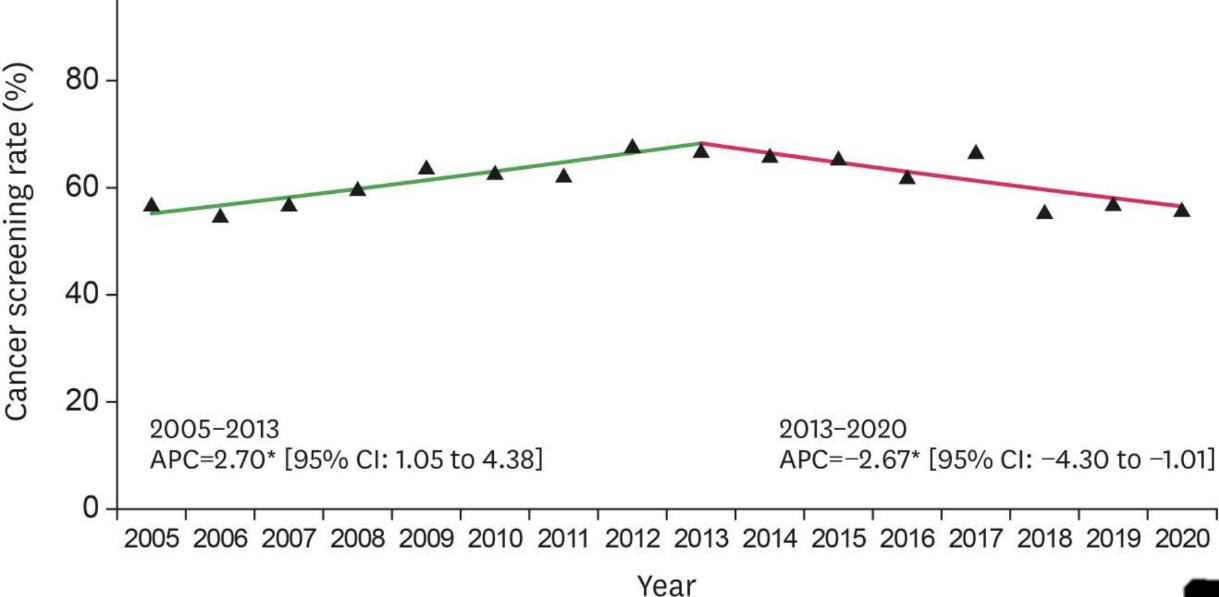
Figure 4 Trends in cervical cancer screening rates during 2005–2020. The solid green line denotes a rising trend; the solid pink line denotes a falling trend. APC, annual percent change; CI, confidence interval. (17)
Since 2016, the HPV vaccine has been part of the Korean National Immunization Program (NIP) (8), targeting 12-year-old girls (18). According to the WHO, the coverage for the last dose among women in 2023 was around 65%, with the coverage being slightly higher (66%) for girls up to 15 years old (5) (Table 7). Boys are not being targeted by the Korean National Immunization Program, consequently data between 2016 and 2018 reports considerably low

vaccination rates among Korean boys (0.7–1.3%) (19) However, the Korean Association of Urogenital Tract Infection and Inflammation and the Korea Disease Control and Prevention Agency published a guideline in 2024 extending the recommendations for the use of the bivalent and quadrivalent vaccines to both girls and boys aged between 11 and 12 years old and low-income young females aged between 18 and 26 years as a catch-up campaign (20)
Table 7. Yearly HPV vaccination coverage among females from 2020 to 2023 (5)
Numerous studies have been conducted to evaluate the preventive measures related to HPV to analyse the cost-effectiveness and socioeconomic benefits. These studies are crucial for helping policymakers and healthcare providers allocate resources efficiently, ensuring that funds are directed towards the most beneficial and cost-effective measures. Moreover, highlighting the economic and health benefits of HPV prevention can increase public support and uptake of vaccination and screening programs.
3.3.1.
Cervical cancer screening
Cervical screening is an effective measure to prevent CC A study from 2015 analyzed the costeffectiveness of CC screening strategies based on the Pap smear test in Korea, which was the most commonly used test up to 2021. Several screening strategies were analyzed, considering variations in starting age, the age at which screening should be discontinued, and different screening intervals Amongst all analyzed scenarios, the most cost-effective strategy was an annual screening starting at a target age of 30 years old (21) Other strategies presented lower lifetime costs, such as screening patients aged 30–79 years old every 5 years, but the clinical benefits from the strategy were also significantly lower, such as quality of life and life-years saved (21)
As mentioned in the section 3.3, cytology has been the most commonly used screening method since 2021. Therefore, it is crucial to conduct studies on its cost-effectiveness to assess the best strategy for the implementation of this method nationwide. Evaluating the economic benefits of this strategy will help determine its value in healthcare, ensuring that resources are used efficiently while maintaining effective CC prevention.
3.3.2.
Vaccination

4. References
1. World Bank. Population, total - Republic of Korea 2023 [
2. World Bank. GDP per capita, PPP (current international $), Republic of Korea 2022 [
3. Kim MA, Han GH, Kim JH, Seo K. Current Status of Human Papillomavirus Infection and Introduction of Vaccination to the National Immunization Program in Korea: an Overview. J Korean Med Sci. 2018;33(52):e331.
4. Lim SC, Yoo CW. Current Status of and Perspectives on Cervical Cancer Screening in Korea. J Pathol Transl Med. 2019;53(4):210-6.
5. WHO. Human Papillomavirus (HPV) vaccination coverage, Republic of Korea 2023 [Available from: https://immunizationdata.who.int/global/wiise-detail-page/humanpapillomavirus-(hpv)-vaccination-coverage?CODE=KOR&YEAR=.
6. Ahn ST, Kim JW, Park HS, Kim HJ, Park HJ, Ahn HS, et al. Analysis of Sexual Behaviors among Adults in Korea: Results from the "Korean National Survey on Sexual Consciousness". World J Mens Health. 2021;39(2):366-75.
7. KOSIS KOrean Statistical Information Service. Projected population, Republic of Korea [Available from: https://kosis.kr/statHtml/statHtml.do?orgId=101&tblId=DT_1BPA003&language=en.
8. Bruni L, Albero G, Serrano B, Mena M, Collado JJ, Gómez D, Muñoz J, Bosch FX, de Sanjosé S. ICO/IARC Information Centre on HPV and Cancer (HPV Information Centre). Human Papillomavirus and Related Diseases in Republic ofKorea. Summary Report 10 March 2023.
9. de Martel C, Plummer M, Vignat J, Franceschi S. Worldwide burden of cancer attributable to HPV by site, country and HPV type. Int J Cancer. 2017;141(4):664-70.
10. Chang HK, Seo SS, Myong JP, Yu YL, Byun SW. Incidence and costs of cervical intraepithelial neoplasia in the Korean population. J Gynecol Oncol. 2019;30(3):e37.
11. Kim YT, Serrano B, Lee JK, Lee H, Lee SW, Freeman C, et al. Burden of Human papillomavirus (HPV)-related disease and potential impact of HPV vaccines in the Republic of Korea. Papillomavirus Res. 2019;7:26-42.
12. Ki M, Choi HY, Han M, Oh JK. The economic burden of human papillomavirus infection-associated diseases in the Republic of Korea, 2002-2015. Vaccine. 2018;36(31):4633-40.
13. Center for Infectious Disease Surveillance & Response, KCDC. Study on the Expansion of HPV Vaccination for the Korean National Immunization Program. 2019.
14. Kim J, Lee D, Son KB, Bae S. The Burden of Cervical Cancer in Korea: A PopulationBased Study. Int J Environ Res Public Health. 2020;17(17).
15. Nguyen TXT, Han M, Ki M, Kim YA, Oh JK. The Economic Burden of Cancers Attributable to Infection in the Republic of Korea: A Prevalence-Based Study. Int J Environ Res Public Health. 2020;17(20).

16. WHO. Most widely used screening method in national cervical cancer screening program. 2022 [Available from: https://apps.who.int/gho/data/view.main.UHCCERVICALCANCERv.
17. Shin HY, Lee YY, Song SY, Park B, Suh M, Choi KS, et al. Trends in cervical cancer screening rates among Korean women: results of the Korean National Cancer Screening Survey, 2005-2020. J Gynecol Oncol. 2022;33(4):e39.
18. Kwak K, Hwang SS. Predicted Cervical Cancer Prevention: Impact of National HPV Vaccination Program on Young Women in South Korea. Cancer Res Treat. 2024;56(3):898908.
19. Choi J, Cuccaro P, Markham C, Kim S, Tami-Maury I. Human papillomavirus (HPV) vaccination in males: Associations of HPV-related knowledge and perceptions with HPV vaccination intention among Korean mothers of boys. Prev Med Rep. 2024;37:102566.
20. Choi CI, Lee SJ, Choi JB, Kim TH, Lee JW, Kim JM, et al. 2023 Korean sexually transmitted infections guidelines by the Korean Association of Urogenital Tract Infection and Inflammation: Human papillomavirus vaccination. Investig Clin Urol. 2024;65(2):108-14.
21. Ko MJ, Kim J, Kim Y, Lee YJ, Hong SR, Lee JK. Cost-effectiveness analysis of cervical cancer screening strategies based on the Papanicolaou smear test in Korea. Asian Pac J Cancer Prev. 2015;16(6):2317-22.
22. Lee H, Hur S, Jang H, Lee IH, Sohn WY, Van Kriekinge G, et al. Cost-Utility of a TwoDose Human Papillomavirus Vaccination Programme Added to Cervical Cancer Screening Compared with Cervical Cancer Screening Alone in Korea. Asian Pac J Cancer Prev. 2019;20(2):425-35.
23. Min KJ, Kwon SH, Kim K, Kim S, Kim HJ, Seong SJ, et al. Clinical guideline for 9-valent HPV vaccine: Korean Society of Gynecologic Oncology Guideline. J Gynecol Oncol. 2019;30(2):e31.
24. Kim Jh, Bae S, Son K, Choi I, Park J, Park J, et al. The Public Health Impact and CostEffectiveness of Nonavalent HPV Vaccination in South Korea: A Dynamic Transmission Model. 2019.
25. Park J, Park J, Yang G, Oh S, I.Sukarom, A.Pavelyev, et al. Public health impact and costeffectiveness of gender-neutral nonavalent human papillomavirus (9v HPV) vaccination in South Korea. 2023.

