A POSITIVE FORCE
TEVI HELLAND-NERGAARD ON A LIFETIME OF SUPPORT

SPRING/SUMMER 2025
BALANCING TREATMENT AND CARE
DR. KURIAN JOSEPH ON THE VALUE OF QUALITY OF LIFE

THE CANCER JOURNEY
LIVED EXPERIENCE AND EXCELLENCE IN CARE
THE MORE EXCELLENCE ISSUE

TEVI HELLAND-NERGAARD ON A LIFETIME OF SUPPORT

SPRING/SUMMER 2025
DR. KURIAN JOSEPH ON THE VALUE OF QUALITY OF LIFE

LIVED EXPERIENCE AND EXCELLENCE IN CARE
THE MORE EXCELLENCE ISSUE
JOHN SEXSMITH ON THE DIFFERENCE DONORS CAN MAKE




14
EXPERT ADVICE
Dr. Alda Aleksi raises awareness of neuroendocrine and endocrine tumours.
Cancer care in Alberta continues to advance because of the pursuit of excellence — by patients and their families, donors who support them, clinicians who care for them and researchers making groundbreaking discoveries to treat them. Meet Albertans who find purpose and hope in improving all facets of cancer care, now and into the future.
Dr. Perri Tutelman works to improve adolescent and young adult cancer care in Alberta; and learn how cancer clinical trials move cancer care forward. 9
About the Alberta Cancer Foundation Lottery.
Research shows how plant-based foods
Dr. Kurian Joseph works to improve outcomes for people diagnosed with cancer, but also ensures they have quality of life.
Inspired by The Tragically Hip, GEDfest founders embark on a mission of giving through music.
34
TRUE CALLING
Oncology nurse Tevi Helland-Nergaard puts her innate sense of caring to work supporting clinical trial patients.
37
IMPACT
Stephen Murphy is driven to give fellow Calgarians on cancer journeys an emotional and literal lift.
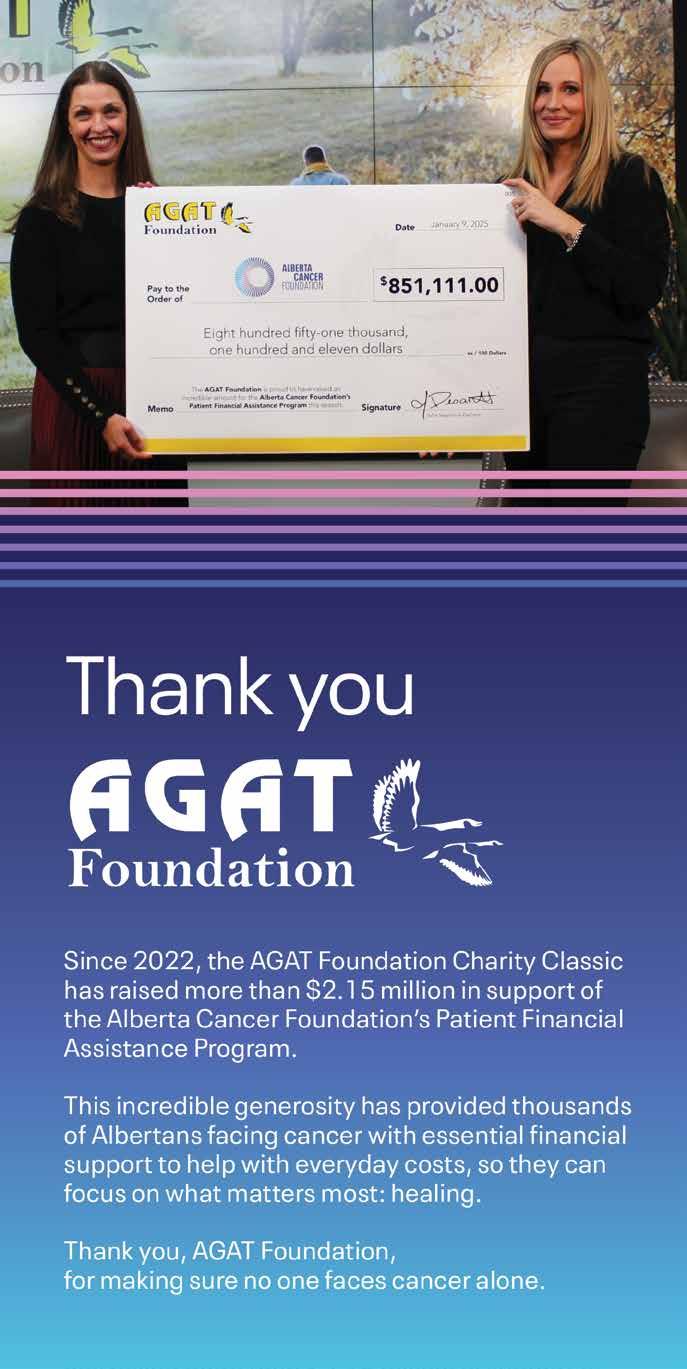
38 DONATIONS IN ACTION
The Riddell Centre for Cancer Immunotherapy makes revolutionary cancer treatments a reality for Albertans. 41
APPLAUSE, PLEASE
Dr. Cheng-Han Lee accelerates the drug development process to provide more treatment options.
42
GAME CHANGER
John Sexsmith helps build the future of cancer care — one donor at a time.
Tom Valentine
(Interim Board Chair)
Darren Baumgardner
Scott Budau
Max Chan
Kathryn (Kate) Chisholm
Rajko Dodic
Joan Forge
Brenda Hubley
Sandra Lau
Lynn Mandel
Gelaine Pearman
Shelley Powell
Dr. Dean Ruether
Kiren Singh
Wayne Steinke
Danielle Thorkelsson
Trustees list current at time of publication.
At the Alberta Cancer Foundation, we believe excellence isn’t a destination — it’s a mindset. It’s a shared commitment to doing better, reaching higher and never settling for “good enough,” especially when it comes to Albertans facing cancer.
In this issue of Leap, you’ll find stories that embody the pursuit of more. More innovation. More collaboration. More compassion. More excellence in cancer research, care and community support — all made possible because of you, our donors and partners.
You’ll read about Evelyn Roy, a vibrant young girl whose legacy is transforming pediatric cancer care in Alberta. Thanks to her family’s heartfelt advocacy, a child life specialist is now supporting young patients at the Arthur J.E. Child Comprehensive Cancer Centre (Arthur Child) — ensuring no child feels alone in their cancer journey (pg. 16).
You’ll also meet Nashrin Mitha, a cancer survivor whose experience helped shape the design of the new Arthur Child. Her story is a powerful reminder that even the smallest moments of kindness can have a lasting impact (pg. 18).
Excellence is also about access —
ensuring every Albertan, regardless of where they live, can receive world-class care close to home. That’s why we’re proud to share the story of Greg Forchuk, a multiple myeloma patient benefiting from a groundbreaking clinical trial made possible by our donors (pg. 19), and the story of the new linac machines at the Jack Ady Cancer Centre in Lethbridge, bringing life-saving radiation therapy to more Albertans (pg. 26).
And, of course, excellence is driven by brilliant minds committed to pushing the boundaries of what’s possible. In this issue, you’ll hear from researchers and clinicians across Alberta, including Dr. Kurian Joseph (pg. 30), who is focused on improving quality of life during treatment, and Dr. Khaled Barakat (pg. 22), who is developing next-generation immunotherapies in labs powered by donor support.
These stories — and so many more — are a testament to what we can accomplish when we work together. You, our community of supporters, are the reason excellence isn’t just an aspiration — it’s a reality.
Thank you for believing in the power of progress. Thank you for making more excellence possible.

Spring/Summer 2025 | VOL. 15 | NO. 1
ALBERTA CANCER FOUNDATION EDITORS
Breanne Kraus, Tamara Fiddler, Mariko Macken, Vanessa Ridden
DIRECTOR, STRATEGY & CONTENT
Meredith Bailey
MANAGING EDITOR
Colleen Seto
ART DIRECTOR
Veronica Cowan
STAFF PHOTOGRAPHER
Jared Sych CONTRIBUTORS
Elizabeth Chorney-Booth, Buffy Goodman, Nathan Kunz, Fabian Mayer, Eula Mengullo, Ryan Parker, Olivia Piché, Alex Rettie, John Ulan
PUBLISHED FOR
Alberta Cancer Foundation
Calgary Office 300-1620 29 St. NW Calgary, Alberta T2N 4L7 Provincial Office 710-10123 99 St. NW
Edmonton, Alberta T5J 3H1
Toll free: 1-866-412-4222
acfonline@albertacancer.ca
PUBLISHED BY
RedPoint Media Group
cSPACE Marda Loop 375-1721 29 Ave. SW Calgary, Alberta T2T 6T7 (Letter mail only)
Tel: 403-240-9055
Toll free: 1-877-963-9333
Fax: 403-240-9059
info@redpointmedia.ca
PM 40030911
Return undeliverable Canadian addresses to the Edmonton address above.
CEO, CO-OWNER
Roger Jewett
PRESIDENT, CO-OWNER
Käthe Lemon

DR. PERRI TUTELMAN HELPS ADDRESS CARE PRIORITIES FOR ADOLESCENTS AND YOUNG ADULTS LIVING WITH CANCER.
As a psychosocial oncology researcher and clinician, Dr. Perri Tutelman works to improve adolescent and young adult cancer care in Alberta.
by OLIVIA PICHÉ
photographs by JARED SYCH
r. Perri Tutelman has always known she wanted to work with children. She began volunteering with young people at the age of 15.
“I got to know a lot of kids during that time, and I really developed a passion for working with kids and families who were experiencing life-threatening illnesses like cancer,” Tutelman says. “To be a part of their journey and help support them, specifically

with their psychosocial needs in addition to the medical care, is really what inspired me to pursue a career as a psychologist in the cancer care setting.”
Tutelman, a clinical psychologist and assistant professor at the University of Calgary, is now also the co-lead of the Adolescents and Young Adults Cancer Priority Setting Partnership (AYA Cancer PSP), a project she conceived that identifies the key areas of research needed to improve care for adolescents and young adults (AYA) with cancer in Canada.
In 2023, Tutelman pitched the project to Chantale Thurston, a young cancer survivor and chair of AYA CAN, who was thrilled to help. From there, they put together a team, including Dr. Fiona Schulte, a psychologist who works with AYA patients with cancer, as a co-lead, to begin the work. The project consists of a steering committee of 16 individuals from different backgrounds — patients, caregivers, family members, cancer patient navigators and clinicians — who share their lived experiences, a fairly uncommon approach in research.
“Generally speaking, the research that gets done in the medical and scientific fields is decided by researchers and industry,” says Tutelman, whose research lab is at the Arthur J.E. Child Comprehensive Cancer Centre. “What’s really missing is the patient’s perspective on what’s important to be researched. Very little research
that gets done is actually directed by the people that it’s intended to benefit. And that’s a problem because we know that patient priorities often differ from those of researchers and the pharma industry.”
Tutelman completed a postdoctoral fellowship at the University of Calgary in 2024, where she specialized in psychosocial oncology as a researcher and as a psychologist, working exclusively with clinical AYA patients through Cancer Care Alberta. There, she saw the unique factors that affect this demographic facing cancer and first had the idea to start AYA Cancer PSP to help address them.
Canada recognizes people aged 15 to 39 as AYAs. This age group includes people studying at school, starting their careers, entering partner relationships, buying their first homes, considering having kids or raising young children.
“Cancer really throws a wrench into all of those plans,” says Tutelman. Of course, cancer changes the course of anyone’s life, but for younger people, certain conversations play out differently from those of the general adult population. A lot of people are uncomfortable talking about the potential of death in young people, explains Tutelman. Discussions surrounding what young people want or don’t want in end-oflife care are often missing. Legacy-making looks different for AYAs, as do finances, fertility and other aspects of life that cancer impacts. With AYA Cancer PSP, Tutelman hopes to address these differences.
“Nobody wants to go through a cancer experience, but we want to help AYAs have an experience where they feel supported and where they feel that they can move forward and live beyond cancer, to become contributing members of society and to live out some of the hopes and dreams they’ve had, whether it’s in school, a career or having a family.”
In November 2024, after 18 months of work and research, which consisted of two national surveys and a two-day prioritysetting workshop, the AYA Cancer PSP reached a consensus on the top 10 priorities for AYA cancer research.
All 10 priorities ask questions about ongoing issues and gaps in care these patients face. The hope is finding the answers that will lead to protocols for improved care. The research priorities range from highlighting the impacts of cancer on youth mental health, finances and fertility to end-of-life care, transitioning back to work during early-career stages and life beyond cancer. AYA Cancer PSP also prioritizes improving treatment and care, such as the diagnostic process, access to healthcare services, screening for earlier detection and monitoring for recurrence, and the development and implementation of treatments.
“These questions should be what the next 10 to 20 years of AYA cancer care focuses on in Canada because this is what the community has told us is most important,” says Tutelman. “The hope is that we have a healthcare system that is responsive to the needs of AYAs. We want to see improved outcomes in terms of survival, late effects [health problems that don’t show up until months or years after treatment] and satisfaction. We want to look at if patients are feeling more satisfied, more supported, less anxious and if they feel like they can navigate the system.”
Prioritizing the research fields was the first step on a long journey toward clinical change and more excellence in healthcare, particularly for the younger generation. Change in the healthcare system demands a lot of time and research, but Tutelman is in it for the long haul.
“This is a long game, but this is where we need to start because if we continue doing research that has not been deemed important by patients and families, then we’re missing the mark.”
“It’s not enough to provide the medical care. We also need to offer psychosocial resources and recognize the very significant and real impact that cancer has on the lives of all patients, particularly young people.”

Dr. Randeep Sangha at the Cross Cancer Institute in Edmonton plays a key role in running cancer clinical trials.
Clinical trials are the key to moving cancer care forward.
by MIREILLE FARKOUH
So much has changed in cancer care in the last 30, 20 and even five years. That’s because research and cancer clinical trials continually identify and determine if new treatments, such as drugs, therapies or medical innovations, are safe and effective and can become the standard of care for people facing cancer. Researchers study better ways to detect cancer, new combinations of existing treatments, ways to prevent cancer from returning and how to improve patient care overall. Without clinical trials, many of the treatments in use today would not exist.
While advancements in cancer care have improved survival rates and quality of life for many, there are still cancers that remain difficult to treat and side effects of current therapies can be unbearable. That is why cancer research and clinical trials remain critical.
Even when clinical trials don’t lead to immediate results, they provide valuable insights that benefit future patients. Cancer clinical trials offer hope to those with no other options, granting access to innovative therapies that might not be otherwise accessible.
The Cross Cancer Institute (Cross) in Edmonton hosts many of Alberta’s clinical trials. In fact, last year alone, the Cross ran more than 100 different clinical trials, each
IN 2024: 972 PATIENTS PARTICIPATED IN A CANCER CLINICAL TRIAL, 72 NEW CLINICAL TRIALS OPENED AND 221 CLINICAL TRIALS WERE ACTIVE IN ALBERTA.

with the potential to change the future of cancer care.
Additionally, the Cross places more than 600 patients on new treatments being trialed each year. This recruitment is one of the highest per capita in Canada. Fourteen per cent of cancer patients treated at the Cross participate in a clinical trial, compared to the national average of about eight per cent.

Plus, a newly developed clinical trials unit is now open at the Cross, an important step in doubling the capacity for cancer clinical trials in Edmonton.
Some of the world’s best and brightest are exploring uncharted territories in cancer treatment and care, right here in Alberta. With donor support for research and clinical trials, Alberta leads the way in cancer clinical trial work in the country, and the Alberta Cancer Foundation supports every cancer clinical trial in the province.
As this vital work continues, there’s sure to be more made-in-Alberta solutions to cancer along with improved access to novel treatments in the province and beyond.
Learn more at albertacancerclinicaltrials.ca
Your questions answered about this exciting life-changing opportunity.
Every ticket purchased for the Alberta Cancer Foundation Lottery supports the More Hope Movement, ensuring that Albertans facing cancer have access to the support they need and the very latest treatments, now and in the future. When you buy a ticket, you help:
IMPROVE THE CANCER EXPERIENCE FOR MORE ALBERTANS
Funding vital programs, like the Patient Financial Assistance Program and Cancer Patient Navigation Program, reduces financial burdens and ensures patients get the care they need at every stage of their journey.
UNITE AND EMPOWER OUR COMMUNITY AGAINST CANCER
Building a network of researchers, caregivers and donors working together to transform cancer treatment and care in Alberta helps to attract and retain top talent at our cancer centres.
BRING LIFE-SAVING TREATMENTS TO ALBERTANS SOONER
Supporting world-leading research and every cancer clinical trial in the province accelerates innovation and access to the most advanced treatments.
By purchasing a lottery ticket at albertacancerlottery.ca, you create more hope and ensure that no Albertan facing cancer walks alone.
The lottery supports the Foundation’s goal of providing a way for every Albertan, no matter their means or interest, to support a cause that impacts so many. It is a way for the Foundation to engage Albertans in making a difference, while having the chance to win a life-changing prize!
To make clear to Albertans — no matter how they choose to support the Alberta Cancer Foundation — the incredible impact they make. By re-naming the lottery from Cash & Cars Lottery, the Foundation aims to quickly connect a potential ticket buyer with the cause of supporting Albertans facing cancer and their families. This name change encourages Albertans to get in on the excitement and to make a difference at the same time.
The 2025 lottery opens for loyal supporters in June and will launch publicly in August. The Alberta Cancer Foundation Lottery aims to have the most cash prize choices in Alberta, so almost all the signature prizes come with a cash prize option. You can choose to live like a millionaire or be a millionaire! Choose a dream home in Calgary or Edmonton, several once-in-a-lifetime trips and experiences, or luxury cars — there’s more than 1,000 prizes in the mix.
Over the last 10 years, the lottery has raised more than $20 MILLION IN PROCEEDS for Albertans facing cancer and their families across the province.
Oncology physiotherapist Nicole Goerz explains why staying limber and mobile during a cancer journey is essential.
by OLIVIA PICHÉ
Mobility is a combination of strength and range of motion that allows us to move freely and easily. Our level of mobility can change throughout our lives. As people age, they lose muscle mass and, with that, mobility. Living with a chronic disease, such as cancer, can also impact mobility. Staying mobile helps maintain a wide range of motion in our joints and reduces risk of injury. It’s essential for everyday activities, like getting out of bed, in and out of a car or walking to get the mail.
“Mobility is important because it’s fundamental. It maintains your independence,” says Nicole Goerz, a physiotherapist for outpatients at the Arthur J.E. Child
Comprehensive Cancer Centre. “It lets you do things that you want to do and keep active, whatever that looks like for you, whether you’re a gardener or a walker or you just want to spend time with your family or your grandkids.”
One of the most common symptoms of cancer and side effects of cancer treatment is fatigue. Fatigue can impair a patient’s ability and desire to move regularly or at all. Lack of movement can affect your mobility as you may lose muscle — affecting your strength — and flexibility, which can impair your range of motion. But even small, daily movements, like going up and down stairs or doing everyday household tasks, are enough to maintain mobility during treatment.
Goerz says a large part of physiotherapy in oncology is working toward what life after cancer can look like. For some, that may mean being able to run again. For others, that may mean daily walks with their dog.
With varying treatment side effects and symptoms, patients may need to adjust their lifestyles and activities. It’s
important to adjust the expectation of what exercise looks like during and after a cancer journey.
“Exercise can be walking with your kids or family or gardening. It can be any activity that you enjoy. It doesn’t have to be something structured,” says Goerz. “If people are willing to reframe that, it really opens up a lot of venues that they might not have previously considered. It makes it a lot more attainable, and then it’s consistent too because if you’re doing something that you enjoy, you’re way more likely to actually stick with it.”
When you’re not feeling the best, Goerz suggests focusing on everyday movements. Try to go up the stairs an extra time. At dinner, fill up a plate of food yourself instead of having someone bring it to you, or tackle a household chore, like laundry or vacuuming. Just do what you can because any movement is better than none.
“Mobility is something that a lot of people just assume will get worse,” says Goerz. “That’s not always the case. It’s about finding what you actually enjoy so that you’re going to stick to it more. Be optimistic and have hope.”
Using a firm and stable chair, practice standing up and sitting back down. This is a highly functional motion most people use multiple times a day. It works large muscles in the lower body and is safe when done correctly or with someone there to help. Goerz says if you’re struggling with this exercise, it’s a good indication your body needs it. She suggests putting a thick, hard book on the seat to raise the height of the seat, and to keep trying to do it even when it’s hard.
Grab a hold of something steady, like the kitchen sink, and squat as low as you feel comfortable and come back up. Goerz says there’s no need to squat so deep that you feel pain in your back or knees; even a small dip can make a difference.
Calf raises are good for mobility and balance, and can reduce leg swelling. They can be done either standing, sitting or even lying down. From standing or sitting, try raising your heels off the ground. For a modified version, point your toes away from your body while lying down, bring them back to you until you feel a stretch in your calves and repeat.
“Exercise can be walking with your kids or family or gardening. It can be any activity that you enjoy. It doesn’t have to be something structured.”
—NICOLE GOERZ

Research shows plant-based foods can reduce the risk of cancer and treatment side effects.
by FABIAN MAYER
You are what you eat. While that nugget of wisdom may oversimplify things, what we put in our bodies can have a profound effect on our health and well-being. In particular, the relationship between nutrition and cancer is a complicated one, but researchers are beginning to better understand what foods and diets may help reduce risk.
Foods like onions, cauliflower and garlic contain allicin, a compound that may lower cancer risks. Some studies suggest that allicin has antitumour properties that work against gastric carcinoma, breast cancer, glioblastoma and cervical cancer.
A review of studies recently published by experts at the Memorial Sloan Kettering Cancer Center in New York City examined two popular diet trends — a whole-food, plant-based diet and a keto diet. The review found that when comparing the two, people following more plant-based diets appeared less likely to develop cancer and that prevalence of cancer was higher in individuals consuming more animal protein.
The study also examined the effects various kinds of diets could have during cancer treatment. It found that plant-based diets might help
Many citrus fruits, like lemons and oranges, contain flavonoids, natural compounds with a wealth of health benefits. The peel of a lemon, specifically, may have several anticancer properties.
Start by thinking about what your diet currently looks like and what foods or meals could easily be substituted for a plant-based alternative. Consider what meals you are already eating that are mostly or wholly plant-based, and start there.
Changing your diet is a process. Don’t feel like you need to make a plantbased switch overnight. Try going meal by meal; start with breakfast and incorporate more plant-based foods like oatmeal, baked sweet potatoes or granola with fruit. Once you’ve consistently done so, move on to lunch and dinner.
Don’t be dogmatic. The goal is to incorporate more plant-based foods to make your overall diet healthier. That doesn’t mean you have to go 100 per cent plant-based or never look at an egg again.
reduce the severity of certain treatment side effects, such as gastrointestinal toxicity from chemotherapy and joint pain from hormonal treatments for breast cancer.
Vincci Tsui, a Calgary-based registered dietician who has worked with individuals who are mid- or post-cancer treatments, isn’t surprised by the study’s findings.
“We know that plant-based foods have a lot of beneficial
Research has shown some red foods, like tomatoes, may lead to a reduced risk of prostate cancer. Red and pink foods, like tomatoes and grapefruit, are rich in lycopene, an antioxidant that studies have found to be connected with cancer prevention.
nutrients like antioxidants and polyphenols that we can’t necessarily find in animal-based foods,” says Tsui. “There’s also some evidence that plant-based foods may lead to less inflammation in general in the body, which can be beneficial for reducing cancer risk, but also for people who are in cancer treatment or recovering from treatment.”
Tsui points out that the nature of the cancer therapies themselves often makes it more difficult for individuals to meet their nutritional needs. “Cancer as a disease process really increases a person’s nutrient needs, but when you’re going through treatment, whether it’s chemotherapy, radiation or surgery, all of these treatments can make it harder to get the right nutrition,” she says. “Fatigue, nausea, intense treatment schedules — they all make it harder to buy, prepare and eat food.”
Just getting enough nutrients and calories during treatment can be a challenge. Tsui says that should be the number one priority, and patients shouldn’t stress too much about where they are getting their calories.
“That being said, if it is within a person’s capacity or a caregiver’s capacity to implement more plant-based foods in a patient’s diet while making sure they still meet their needs, that could be beneficial,” says Tsui. “As you’re feeling better, as you have more capacity to make some of these changes, then absolutely go ahead and make them, but don’t feel pressured to do it.”
When it comes to making the switch to a more plant-based diet, getting enough protein can be tricky. Legumes such as beans, chickpeas and lentils are excellent sources of plantbased protein, and Tsui recommends incorporating them into recipes you’re already familiar with. She suggests adding protein to meals that might not traditionally have any. Scooping some hemp hearts into your salad or putting dessert tofu in a smoothie can significantly boost protein intake.
Tsui’s final piece of advice is to make use of available resources through your healthcare team. She recommends working with an oncologist or getting a referral to a dietician to help zero in on what makes the most sense for you and your unique needs during your cancer journey.
Blueberries contain anthocyanins, powerful antioxidants that can help protect against tumours and reduce inflammation — part of why they’re considered a superfood! Purple cabbage, blackberries and eggplants also offer these antioxidants.
Leafy greens like kale are a great source of lutein, a type of carotenoid that may be protective against certain cancers. Consuming lutein in increased amounts may decrease the risk of breast, kidney and bladder cancers.

Medical oncologist Dr. Alda Aleksi explains the importance of knowing about this lesser-known cancer.
by FABIAN MAYER | photographs by JARED SYCH
The neuroendocrine system plays a crucial role in producing and releasing hormones that regulate essential bodily functions, such as breathing, digestion, growth, reproduction and metabolism. Neuroendocrine and endocrine tumours (NETs and ETs) arise from specialized neuroendocrine cells, which are found throughout the body. Therefore, these tumours can develop in various organs rather than being confined to a single location. Dr. Alda Aleksi, a medical oncologist at the Arthur J.E. Child Comprehensive Cancer Centre (Arthur Child) and a clinical assistant professor at the University of Calgary’s Cumming School of Medicine, specializes in NETs and ETs. She’s working to increase awareness and dispel misconceptions about this lesserknown form of cancer. Here, we chat with Dr. Aleksi to learn more.
What are NETs and ETs, and what makes them different from other kinds of cancer?
“NETs and ETs can develop anywhere endocrine cells are present. Given neuroendocrine cells are distributed throughout the body, these tumours can arise in any organ. That is different from all other tumours that you’ve probably heard of. Breast cancer, for example, comes from the breast, lung cancer comes from the lung, etc. NET and ETs are very unique in this respect.”
Where in the body are they typically found?
“By far, the most common site of origin for NETs and ETs are the gut and the pancreas, followed by lung NETs and thyroid tumours. These tumours have another unique capability in that they can secrete unwanted hormones that disrupt the normal functioning of the endocrine system. However, only a minority of NETs do this.”
Are there symptoms people should watch for?
“Unfortunately, for most of these tumours, the onset is very insidious, so patients might not have any symptoms. Furthermore, because these tumours might not cause any symptoms at all during their initial phases, they are usually diagnosed at a later stage, when patients start feeling sick. There are no screening tests for NETs or ETs, so we are unable to predict who is going to develop one. Most NETs and ETs are sporadic, but a small percentage could be hereditary. Often, these tumours are diagnosed incidentally during routine investigations or through imaging done for other reasons. The imaging technology available today is so sensitive that it can pick up tumours and masses less
than 0.5 centimetres in size. Imaging remains our main diagnostic tool in detecting these tumours.”
People may not have heard about this category of tumours before; are they rare?
“I call NETs the ‘forgotten tumour site,’ but these tumours are not rare. They are currently the fastest-growing tumours in Canada and worldwide. Globally, NET incidence has doubled from 4.90 per 100,000 in 2000 to 8.19 per 100,000 in 2018. I have seen more than 100 new cases this past year alone. This is mostly because of technological advancement and increased detection rates. That’s why NETs and ETs deserve public attention.”

Globally, NET incidence has doubled from 4.90 per 100,000 in 2000 to 8.19 per 100,000 in 2018.
What are the latest treatment strategies and are they available in Alberta?
“Treatment will depend on a variety of factors such as the organ of origin, if it can be resected surgically and the aggressiveness of the tumour. For early-stage NETs, the treatment of choice is surgery. For advanced NETs, the initial treatment is typically an injected hormone therapy agent. These agents are the treatment backbone for advanced NETs. Depending on the aggressiveness of the tumour, we employ other systemic treatments such as molecular agents, chemotherapy and recently approved peptide receptor radionuclide therapy (PRRT). As of February 2025, Albertans have access to PRRT as standard of care for NETs and a targeted radiotherapy, Lutathera, is now provincially funded. Approval of Lutathera for NETs marks a historic milestone in advancing cancer care in Alberta. We are excited to offer these NET treatments at the Arthur Child.”
What is being done to change misconceptions and advance therapies?
“The Calgary NET Group and I launched the first Provincial NET Awareness Campaign in 2024. This multi-pronged initiative includes: the creation of the Canadian Cancer Theranostic Foundation, the establishment of the first comprehensive NET and ET provincial database, the formation of the first NET Patients’ Advocacy Committee and the organization of the annual NET Fundraising Gala. Public awareness of NETs and ETs remains limited. Therefore, education and outreach are our top priorities.”
by OLIVIA PICHÉ
Every cancer journey has its highs and lows; it can be challenging, yet can also hold vital pockets of hope. Some patients become active volunteers, and some family members create long-lasting legacies on behalf of their loved ones, all while holding onto hope for the future of cancer research. The patient experience continues to evolve, bringing positive change, including dedicated supports and resources for the younger population, a state-of-the-art cancer centre with improved patient-focused care and promising cancer clinical trials.
Patient experiences help to shape and advance more excellence in cancer care today and in the future.

Eleven-year-old Evelyn Roy loved Star Wars, Harry Potter and dance parties. She had a quick, dry sense of humour and is described as “bright, joyful and so much fun to be around.” In early 2020, Evelyn passed away from stage 4 neuroblastoma, a cancer that starts in immature nerve cells and commonly affects babies and young children. Her legacy is remembered through the impactful work she inspired, helping other children facing cancer.
Evelyn’s family — mom Heather, dad Mike and sister Harper — stood by her side through every step of treatment — holding her hand during chemotherapy, MRIs, X-rays and CT scans. But radiation therapy is different. Children must face it alone, and the unfamiliar sights and sounds of the cancer centre can feel anything but kid-friendly.
“The feeling of that big steel door closing behind Evelyn just made my heart sink. I wanted to be with her, but I couldn’t safely be in there,” recalls Heather.
While anxiety-inducing for both parents and children, Heather explains how the staff went above and beyond to make Evelyn feel less alone by playing her favourite music and talking to her through the speaker. “It means so much, and we are forever grateful for how much compassion they put into her treatment.”

Heather continues to be an advocate and local leader in the pediatric cancer community. Driven by her desire to ease the cancer journey, she strives to equip cancer centres with vital resources that make a lasting impact. Through her support of programs and projects inspired by Evelyn, Heather helps to reduce the stress of treatment, bringing more comfort and more hope to young patients and their families.
“Childhood is supposed to be wonder-filled and fun,” she says. “If we can do what we can to improve these experiences and to honour childhood by giving them some control back and valuing their experiences, we are reducing those long-term deficits of trauma and anxiety, and we are giving them some wonder back in their days.”
Much of Heather’s philanthropic work focuses on making the radiation process more kid-friendly, which includes advocating for child life specialists in cancer centres. Child life specialists are uniquely trained positions that provide trauma-informed care; these specialists teach kids strategies to get through hard things. Providing this support is standard of care in children’s hospitals, but not at major cancer centres like the Arthur J.E. Child Comprehensive Cancer Centre (Arthur Child), where children receive their radiation. Radiation is intimidating. Having a child life specialist present during cancer treatment means pediatric patients have one more person on their team to help them cope with the experience.


Evelyn working on an original song with Marc, a music therapist at the Alberta Children’s Hospital, one of her favourite people to spend time with at the hospital.
“Ev used to always say when she was having radiation, ‘This would be so much easier if I had a Cindy here,’” recalls Heather, referencing Cindy Baxter, Evelyn’s child life specialist at the Alberta Children’s Hospital.
Heather and her family have been raising funds for a child life specialist at the Arthur Child, something Evelyn wanted not only for herself but also to support other children. Thanks to Evelyn and her family, a child life specialist is now working at the Arthur Child.
“We just love knowing that the child life specialist is there and honouring this dream of Evelyn’s,” affirms Heather. “Ev has really inspired all of this through her words and her actions. We will always be immensely proud of her for taking really hard times and channelling that energy in such a positive way toward helping people. Ev cared very, very deeply about other people and their experiences.”

When Nashrin Mitha was diagnosed with stage 1 breast cancer in 2010 at the age of 46, she was given a private room to process the news and weigh her treatment options as her family arrived to gather around her. She was told to take as much time as she needed. “It wasn’t like one of those appointments where you’re just kind of rushed through the door,” she recalls. “What has really stayed with me throughout my journey were the small moments of humanity.”
Although difficult, Mitha recalls her cancer journey in a positive light, one with excellent care, encouraging results and moments of hope and humanity: a doctor holding her hand and saying, “We’re in this together,” a nurse wiping a tear rolling down her cheek, an anesthesiologist reminding her, “You have cancer, cancer does not have you.”
“As small as these gestures may seem, they were moments of hope for me,” says Mitha.
Throughout it all, Mitha remained optimistic, believing that attitude is 50 per cent of the challenge. “I strongly believed if you had a positive outlook, there would be positive outcomes,” she says.
MRIs and seven years of medication. Doctors officially declared her in remission, and for Mitha, this meant it was time to give back for the loving care she had received.
An active volunteer her entire life, Mitha’s community involvement took an even more personal turn after her cancer journey. Her strong faith has always nurtured a commitment to giving back and caring for others. “I have always felt volunteering to be in my DNA. It’s not something you have to do; it’s something you want to do,” she says.
She joined a group of dedicated volunteers that came together in 2014 to form the Patient and Family Advisory Council for what is now the Arthur J.E. Child Comprehensive Cancer Centre (Arthur Child). The council, composed of individuals facing or who have faced cancer and family members of patients, helped to inform, advise and advocate for patient-centred care.
“We were given the opportunity to help cultivate the environment that we were looking for in the new centre,” she says. “We wanted you to feel like hope was floating wherever you are. We wanted a building that would house courage and research, state-of-the-art equipment and facilities, but most importantly, a building that felt like a home away from home for all who came through its doors.”
After a lumpectomy, she received 16 rounds of radiation therapy, countless scans and bloodwork, Dr. Kevin Hay
And that is just what the Arthur Child is. Beyond cutting-edge equipment and world-renowned talent, Mitha affirms that the staff, as stewards of the centre, are the heart and soul of the building and make it feel like home. As a council member, she and her team remind staff how impactful even the smallest kind gestures or discussions can be for patients. Mitha truly believes that when we accept disappointment, we should never lose hope. By sharing her journey, Mitha aspires to see more patients experiencing moments of hope, just as she did.
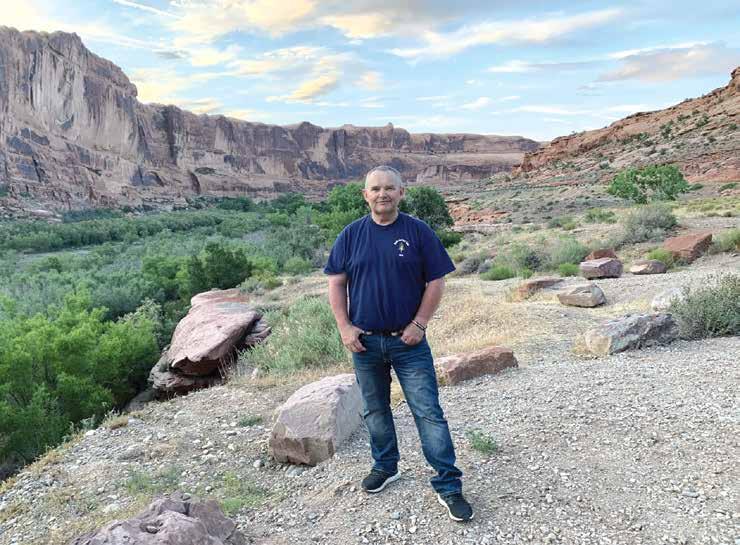
Two years after a dirt biking accident caused an injury to one of his sit bones, Greg Forchuk was still dealing with serious pain. He had to use a cane when the pain worsened. In 2014, to try to remedy the pain, a then-46-year-old Forchuk went in for an X-ray, where doctors discovered he had multiple myeloma, a blood cancer that forms in the plasma cells mostly found in bone marrow.
Forchuk underwent a successful stem cell transplant at the end of 2014, keeping his cancer markers (substances in the body, when in increased amounts, may indicate the presence of cancer) quite low for years. Currently, there is no cure for multiple myeloma, and patients experience relapse, even after being in remission. That’s why Forchuk had his bloodwork done every eight weeks following his transplant to monitor his health. In 2022, Forchuk faced the news no patient wants to receive: his cancer markers had increased, and his multiple myeloma had returned.
Thankfully, eight years after Forchuk’s initial diagnosis, and thanks to advanced research, new treatment options became available for multiple myeloma. That includes the clinical trial MagnetisMM-5, a phase three study looking at different drug regimens to identify which show the most promise in treating relapsed multiple myeloma. Although skeptical at first, Forchuk joined the trial.
Greg receives his treatment with his wife, Kim, by his side.

“When I was told that my previous drug had quit working, that was pretty hard to take,” says Forchuk. “There are few other options for treatment with this cancer, so I just decided to go with it. I jumped in with both feet and told them to do what they had to do, and I’m glad I did. I’ve had good results. I’m just thankful for it.” Since joining the trial, Forchuk’s numbers have remained very low, even lower than the first time he was considered in remission. He confirms the clinical trial drugs are working better than his previous medications. At first, Forchuk received a dose of two drugs every two weeks as part of the trial. He then moved to a threeweek frequency, and today, he goes every four weeks to the Arthur J.E. Child Comprehensive Cancer Centre for his dose. This regimen continues to successfully keep his cancer at bay. These results hold great benefit not only for Forchuk, but also for people who will face multiple myeloma in the future.

In 2018, Forchuk and his wife, Kim, started participating in the Enbridge Tour Alberta for Cancer (Tour) as part of the support team for a family friend. While they don’t ride, they donate, attend fundraisers and cheer her on during the Tour and at the finish line. All cancer clinical trials in the province are supported by the Alberta Cancer Foundation, including Forchuk’s, so he knows all too well what that investment means. “Funding is very important to do the research to hopefully come up with these new medications that can help people survive,” he says.
Beyond raising funds for critical research like clinical trials, events like the Tour help create a sense of community, one that the Forchuks are proud to be a part of. “When these fundraisers come together, and you get that many people that come out to support, it’s really something incredible,” Forchuk affirms.
Meet the professionals who are elevating excellence in cancer care in Alberta.
by NATHAN KUNZ




Throughout the province, cancer care professionals work to improve every stage of the patient journey. From answering the tough questions following a child’s diagnosis to finding improvements for already innovative treatment methods, teams of dedicated researchers, clinicians and behind-the-scenes experts are building a better today and tomorrow for Albertans facing cancer. Here, four cancer care leaders share what inspires them, how they’re working with other bright minds in Alberta and beyond, and what their work could mean for people living with cancer in years to come.
DIRECTOR
CANCER RESEARCH INSTITUTE OF NORTHERN ALBERTA
PROFESSOR
FACULTY OF MEDICINE AND DENTISTRYMEDICAL MICROBIOLOGY AND IMMUNOLOGY
DEPARTMENT, UNIVERSITY OF ALBERTA
Whether she’s researching how to better use cancerkilling cytotoxic T lymphocytes (white blood cells) in the lab or fixing up a project car in her home garage, Dr. Hanne Ostergaard says she’s always searching for new problems to solve.
“I love when we get a result where you’re just scratching your head,” says Ostergaard. “When you see a result that just doesn’t work out as predicted — that’s fun.”
The California-born immunologist serves as the director of the University of Alberta’s Cancer Research Institute of Northern Alberta (CRINA) — one of the largest comprehensive cancer research institutes in Western Canada, with a team of 170 researchers working together to better understand and treat cancers.
Originally from Los Angeles, Ostergaard moved north with her husband, a fellow immunologist, in 1991. Finding a location that not only had openings for two immunologists but also aligned with Ostergaard’s collaborative-focused research philosophy was a tall task, but the pair found a home that checked both boxes in Edmonton.
“When you work on having a good research environment, that ‘lifts all boats,’” says Ostergaard. “That helps not just a single researcher but all of the researchers. And Edmonton has that.”
Three decades later, Ostergaard continues to foster CRINA’s collaborative environment. She credits the institute’s success to its culture of connection, strengthened by initiatives she’s maintained as director, like newsletters and social events. A constant on the CRINA calendar is the annual Research Day, where cancer researchers, postdocs and graduate students showcase their work while networking.
Ostergaard has also introduced her own initiatives, such as the CRINA Connects seminar series, where CRINA members and external experts lead lectures based on what they’re working on. “One of my primary goals is to get people working in teams and in groups — not just to solve little problems, but to solve the bigger problems,” says Ostergaard. “You need to work in teams to solve those big problems in cancer.”

The big problems are exactly what CRINA is built to address, and the institute attracts world-class researchers to Edmonton to solve them. Ostergaard says a recent project in which oncology researchers and biochemists are working together to better understand the entire tumour micro-environment perfectly exemplifies the innovative crossdiscipline work that makes CRINA special.
It’s cutting-edge research like this, Ostergaard explains, that’s kept her in Edmonton and keeps her excited to lead the collaborative team at CRINA.
“The thrill of discovery! For me, there is nothing that compares to the excitement of seeing new data from my research team that has never been done by anyone else. Sometimes it may be short-lived, but it is still very exciting.”
FACULTY OF PHARMACY AND PHARMACEUTICAL SCIENCES, UNIVERSITY OF ALBERTA

As a professor at the University of Alberta, a biophysicist and an electrical engineer specializing in super computers, Dr. Khaled Barakat is constantly surrounded by complex systems. His mission, however, is simple.
“My lab is focused on fulfilling my dream: using computer simulations to find a universal cure for cancer,” he says.
For nearly 20 years, Barakat has been using his unique skillset to help bridge the worlds of physics, pharmaceutical sciences and technology, all in search of better immunotherapy treatment options. Using computer simulations that mimic the human body, Barakat’s lab can test millions of chemical combinations in a shorter time frame and at a fraction of the cost of traditional methods. When a compound is effective in triggering a positive response, it’s translated into realworld models for further investigation.
Through this approach, Barakat recently contributed to an Alberta Cancer Foundation-backed, multi-lab study, resulting in the discovery of Compound B — a molecular compound that shows promise for use in future immunotherapies.
The water-soluble compound could allow for oral administration, quickly and effectively triggering an immune response. A short half-life, Barakat explains, would allow patients to be taken off the drug if they experienced severe side effects without long-term implications. Its tiny size may also allow Compound B to cross the blood-brain barrier and treat tumours that are inaccessible to the larger antibodies currently used for immunotherapy.
Compound B’s potential is exciting, but Barakat likens the project’s current stage to having only two sides of a Rubik’s Cube complete. While Compound B triggers an immune response with low toxicity, it’s lacking other features that will elevate it to “clinical lead” status. Next steps will see Barakat use generative artificial intelligence to produce derivatives of the compound, tweaking it to solve the rest of the metaphorical Rubik’s Cube.
From there, Barakat hopes to partner with a pharmaceutical company to bring Compound B to people living with cancer. With the right results and investments, Barakat says it could enter clinical research stages as early as 2027.
Barakat stresses that the road ahead is not an easy one. It takes hard work and some good fortune to translate a promising discovery into a game-changing treatment, and setbacks are all but inevitable. Despite the challenge, Barakat remains positive.
“I think every researcher is immune to failure. We get more negative results than we get positive,” he says. “But we don’t care about failing because that’s normal. And you only need to succeed one time.”
“I’m inspired by the potential to make a positive impact on people’s lives. Knowing that the work I do could contribute to better treatments for diseases motivates me every day. I’m inspired by the creativity and dedication of the people I work with. Science is a team effort, and I learn so much from others.”
CLINICAL ASSOCIATE PROFESSOR
CUMMING SCHOOL OF MEDICINE,
DEPARTMENT OF OBSTETRICS AND GYNECOLOGY,
UNIVERSITY OF CALGARY
DIVISION HEAD
PEDIATRIC AND ADOLESCENT GYNECOLOGY, ALBERTA HEALTH SERVICES
PROGRAM DIRECTOR
PEDIATRIC AND ADOLESCENT GYNECOLOGY
FELLOWSHIP PROGRAM, UNIVERSITY OF CALGARY
A child’s cancer diagnosis comes with a lot of big, overwhelming questions. For many families, they may not even think about anything related to the potential impact of treatment on future fertility. Thanks to Dr. Sarah McQuillan, these questions get prompted and discussed early on now, and come with more answers.
“I feel really fortunate to work with families to provide the best care,” says McQuillan, who treats patients under 18 with ovaries as a pediatric and adolescent gynecologist. “When they walk away feeling secure, feeling that their situation has been slightly improved — I find that really rewarding.”
Alongside Dr. Philippa Brain, an obstetrician and gynecologist, McQuillan helped develop Alberta’s first pediatric and adolescent gynecology fellowship program in Calgary in 2013.
McQuillan says many of her patients face the same gynecologic difficulties as adults. Her work, however, also includes specialized care, including exploring options for young patients undergoing treatments that may impact future fertility, such as those facing cancer.
Notably, Calgary is one of only a few Canadian cities to offer ovarian tissue cryopreservation (OTC) — in which a portion of the ovary is removed prior to treatment and frozen. After treatment, and when a patient is ready to start having children, that ovarian tissue is then reinserted. Unlike egg freezing or other fertility preservation methods, OTC is effective for even pre-pubescent patients.
“[Offering these options] provides long-term hope to families,” says McQuillan, citing multiple studies that link preservation exploration to survivors’ long-term selfsatisfaction and quality of life. “Even just having that discussion creates some hope.”
Starting in 2024, treatments that may affect fertility trigger a pop-up when entered into Alberta’s electronic medical record, prompting standardized early discussions. Young patients are also connected with McQuillan’s team to explore how they can help.
Alberta’s pediatric and adolescent gynecology clinic has grown exponentially since 2013, with McQuillan attributing the success to fruitful collaborations with

oncology and bone marrow transplant teams and the regional fertility program. There are now five gynecologists serving young patients in Calgary versus just one 12 years ago. McQuillan is also investing in the future by leading Alberta’s pediatric and adolescent gynecology fellowship program.
While the progress is meaningful, there’s still work to be done. Because tissue freezing, processing and storage are not covered by healthcare or many insurance programs in Canada, treatments remain cost-prohibitive — an obstacle McQuillan and her colleagues hope to knock down.
“In the next 10 years, I hope there are no barriers stopping families from exploring and receiving fertility preservation,” she says.
What inspires you?
“I love working with patients and seeing their resilience in difficult situations. With my children, I love watching the world through their eyes and learning new ways of seeing something as adults we take for granted.”
DIRECTOR
Like many, Chris Normandeau’s path to cancer care came from close-to-home connections. Born and raised in St. Albert, Normandeau supported his brother during his cancer journey while they were young adults. Shortly after Normandeau graduated from the University of Alberta with a Bachelor of Commerce, a close friend passed away from the disease. The loss, Normandeau says, inspired him to shift his career ambitions.
“A lot of times you feel a bit helpless when you know someone who has a cancer diagnosis,” says Normandeau, who started as a data manager with the Alberta Cancer Board (now part of Alberta Health Services) in 2007. “Once I moved into the cancer world, it felt like I was making a difference.”

Today, Normandeau helps to improve cancer journeys throughout the province as executive director of Cancer Care Alberta’s Cancer Research & Analytics (CR&A) team.
In this role, he oversees the strategic direction of two worlds. On the research side, Normandeau supports projects led by CR&A teams and external researchers, while also managing biobanks — such as tumour banks and blood samples collections — and working with frontline staff to address systemic shortcomings.
The data side sees Normandeau working with epidemiologists, IT analysts and biostatisticians to gather numbers, find meaning in them and use them to improve care.
When a 2015 national report ranked Alberta as the province with the lowest rate of mastectomies as day surgeries (1.3 per cent in Alberta vs. 34.4 per cent in Ontario), for example, the cancer data team jumped into action. Working alongside the Cancer Strategic Clinical Network and clinical leads, they helped shift standard care practices towards same-day mastectomies, all while maintaining positive patient outcomes. By 2022, 74 per cent of mastectomies in Alberta were performed as day surgeries, allowing more patients to get home sooner and freeing up more beds in the process.
Normandeau credits his success to collaborating with his colleagues. There are no better moments, he says, than when he’s helped bring the right people together. “What’s most exciting is meeting with people with so many different perspectives but the same common desires: to improve patient outcomes, create efficiencies and make the whole system run smoother.”
“It’s always most exciting when there is a new initiative being planned out and people across multiple departments come together with the same goal — of figuring out the best way to make a difference.”
New radiation therapy equipment in Lethbridge provides better access to critical treatment.
by FABIAN MAYER

Healthcare services are often concentrated in major urban centres, especially when it comes to those requiring extremely expensive equipment. In a province as big and diverse as Alberta, that can be challenging for people living in rural and remote communities. A new initiative to bring rural access to radiation therapy, representing millions of dollars in investment, is helping to improve availability of cancer care.
Radiation therapy is one of the most effective cancer treatment options. Approximately half of all individuals diagnosed with cancer will receive radiation therapy at some point during their journey. New radiation therapy machines recently purchased for the Jack Ady Cancer Centre in Lethbridge help make this critical treatment more convenient and accessible.
Known as a medical linear accelerator, or linac for short, these advanced machines perform roughly 90 per cent of all radiation therapy. The machines accelerate electrons through an evacuated tube; these electrons reach close to the speed of light before
crashing into a metal target. The rapid deceleration releases extremely high-energy X-rays, which are then directed at the tumour with extreme precision to target cancer cells, concentrating cellular damage there to destroy the diseased cells.
ACCESS TO RADIATION THERAPY
Due to the linac’s complex and expensive nature, these machines have not always been widely available outside major centres, which can make accessing radiation treatment challenging. Rural patients, for example, must often travel hundreds of kilometres into major cities to undergo radiation therapy, adding to an already exhausting regimen.
Radiation therapy is typically administered over a number of weeks, with the total radiation dose often broken up across 25 to 30 treatments, delivered on consecutive days. This process can be highly disruptive to patients’ lives, especially for those with hours-long commutes to a cancer centre. Dr. Marc MacKenzie, a professor of medical physics in the department of oncology at the University of Alberta, says the new machines help to change that.
“We have patients availing themselves of treatment that would have been really incompatible with their lives otherwise. Suddenly, you can get treatment within a 15-minute or half-hour drive from your home; it’s a game changer.”
—DR. MARC MACKENZIE
“We have patients availing themselves of treatment that would have been really incompatible with their lives otherwise,” says MacKenzie. “Suddenly, you can get treatment within a 15-minute or half-hour drive from your home; it’s a game changer.”
MacKenzie says linac technology is constantly getting better at directing radiation exactly where it needs to go. The new machines recently installed at the Jack Ady Cancer Centre in Lethbridge are some of the most advanced linacs in the country, especially when it comes to imaging.
“There’s been nothing but steady improvements in
the technology,” says MacKenzie. “Those newest and highest quality images unlock a whole new capability to accurately reconstruct daily radiation doses. We know with greater precision than ever exactly what dose to administer, where, and on what day.” This type of precision oncology can make a real difference in outcomes by targeting cancer cells and not damaging healthy ones.
The new machines were purchased through a partnership with the Chinook Regional Hospital Foundation with the help of a $2 million gift from the Estate of Bruce and Edna Moffat. Beyond making radiation therapy, across the continuum of care, more convenient to access, the new machines also provide therapy to patients who might otherwise have opted out of such treatments altogether.

“About half of our patients were palliative patients who were seeking comfort for symptoms,” says MacKenzie. “Radiation is not only great for curative purposes, but it’s also excellent for palliation. We had patients who were not really wanting to travel hours for that, but it’s available now locally.”
Having this access to radiation therapy in Lethbridge means that more rural patients, at any stage of their cancer journey, can receive the care they need, when they need it.
IN THIS LEAP SERIES, WE CAPTURE THE BRAVERY, STRENGTH, HONESTY, HOPE AND RESILIENCE OF ALBERTANS LIVING WITH CANCER.


As told to OLIVIA PICHÉ
In 2004, days before her 50th birthday, Andrea McManus (right) was diagnosed with bilateral breast cancer. Nearly 20 years later, at the end of 2023, her daughter Alexandra was also diagnosed with breast cancer at age 33.
Two decades ago, Andrea joined the MA41 clinical trial, where she received dose-dense treatment. This involved a higher dose of chemotherapy, given more frequently. It was eventually deemed a successful trial with dose-dense chemotherapy becoming a common treatment. Today, Andrea is cancer-free.
While Alexandra is still in active treatment to lower the risk of recurrence, she has had no detectable cancer following her mastectomy. In 2024, she went through eight rounds of chemotherapy, where she, too, received dosedense treatment, though it was much more refined compared to her mother’s clinical trial treatment. Within two generations, the McManus family has seen first-hand remarkable improvements to cancer care, particularly through enhanced patient experience.
Andrea: “I wish that Alex had not had to deal with it at all, but I’m grateful that I was able to contribute something to her care. I’ve always believed in the value of research. I considered myself to be paying it forward. I just never thought that it would get put forward in quite this way.
“My chemo treatment was a blanket treatment; everybody would have gotten the same thing [at the time], whether you were in a clinical trial or not. Alex’s treatment is tailored to her tumour pathology. They know so much more now.
“Watching her treatment, how it was delivered and how it had been refined [since I received it] was a window into the value of how important research is.”
Alexandra: “Now, there’s a big focus on what’s available with your treatment experience. I remember my mom feeling quite nauseous and sick, and that being a big thing. In comparison, my nausea was very well controlled, which was huge. For my chemotherapy, I also did cold capping, which is when you wear a cold cap to try to preserve your hair. It’s just amazing that stuff like that is offered for patients.
“Having a mother who’s gone through breast cancer and a grandmother who went through cancer three times, you definitely feel the generational connection, not in a negative way of it being passed down, but in the sisterhood of the women who’ve come before and what they’ve dealt with.
“It’s a stark visualization of the improvements that have been made. Often, in cancer care and treatment, it can feel like the pace of research is slow. It’s different for different cancers, but I think, as a whole, it’s easy to look at it and say, ‘Why aren’t we moving faster?’ or ‘We hoped we’d be further ahead in 2025.’ But actually, if you compare our experiences, there have been significant improvements.”

Dr. Joseph works to improve outcomes for people diagnosed with cancer, and ensures they have quality of life both during and post-treatment.
by ELIZABETH CHORNEY-BOOTH | photographs by JOHN ULAN

Like most healthcare professionals, Dr. Kurian Joseph is passionate about maintaining his patients’ comfort and quality of life. Of course, caring for patients’ well-being is part of the job. But Joseph, a radiation oncologist and researcher at the Cross Cancer Institute (Cross) in Edmonton, has made it his mission to figure out innovative ways to make things better for patients wherever he can.
In addition to treating patients diagnosed with gastrointestinal, skin and breast cancer, Joseph has dedicated his career to a series of research studies designed to improve outcomes and help patients live their best lives possible both during and after treatment. It’s a calling that comes not only from Joseph’s compassionate personality, but also from a friendship in his youth that changed the course of his life. Most recently, it has led him to lead a new research project that could significantly reduce the number of surgeries that patients diagnosed with low rectal cancer (tumours that occur in the lower six centimetres of the rectum) may need to undergo.
When Joseph was at university in India, a close friend was unexpectedly diagnosed with lymphoma and passed away from the disease. Struck by the feeling that a life had ended far too soon, Joseph pursued a career in oncology to honour his friend who also had dreams

of becoming a doctor. Although Joseph doesn’t specialize in lymphoma, his friend’s passing inspired him to dedicate his career to advancing cancer care.
“He would have lived if it had happened now,” Joseph says. “At the time, there was no successful treatment. So many things have improved since then.”
Remission and extension of life are always the first goals for patients and oncologists. Researchers like Joseph are concerned about finding effective treatments that not only eradicate a patient’s cancer but also leave them able to enjoy life as fully as possible posttreatment. Joseph has been involved in dozens of research projects since joining the team at the Cross in 2006, often with an emphasis on investigating ways to use existing treatments efficiently and effectively while minimizing negative impacts.
Joseph has published work looking at the effects of providing patients diagnosed with anal cancer breaks in their treatment schedule to reduce the toxicity of the therapy and ultimately improve outcomes, which has since been adopted as a standard of care. His recent research includes a breast cancer study demonstrating how older women with low-risk, early-stage breast cancer can achieve better outcomes with a short course of radiotherapy instead of prolonged endocrine therapy, reducing difficult side effects. These studies may not seem to have much in common, but they showcase Joseph’s curiosity and determination to reduce discomfort for patients while still providing effective results.
“I’m basically interested in outcome research,” Joseph says. “Our research is all done to improve the quality of care of patients.”
Joseph applies the same approach in his latest trial, which uses enhanced imaging techniques on patients with low rectal cancer. Currently, all patients
with low rectal cancer undergo surgery after receiving radiation therapy and chemotherapy, regardless if any remaining cancer is detected. The practice of routinely prescribing potentially unnecessary invasive surgery to all patients didn’t sit well with Joseph, prompting him to use a unique piece of technology to address the situation.
The issue with using standard imaging equipment such as magnetic resonance imaging (MRI) is the machine is not reliable enough to definitively rule out any remaining cancer. Positron emission tomography (PET) scans detect metabolically active tumours, but Joseph says they can miss up to 30 per cent of low rectal cancers. Alternately, MRI gives good imaging of patients’ rectums but can’t always differentiate between a tumour and scar tissue or swelling caused by radiation or chemotherapy.
The Cross is fortunate enough to have a relatively rare PET-MRI machine, which is a hybrid of the two kinds of scans, allowing doctors to utilize both the imaging power of the MRI and the cancer-detecting skills of the PET simultaneously. Joseph’s new phase two trial follows 40 patients who receive a PET-MRI scan before their radiation and chemotherapy treatments, then scanning again right before surgery. The goal is to compare scan results with surgical pathology findings to assess how accurately the PET-MRI is at ruling out any remaining cancer.

“Meta-analysis shows the PET-MRI will improve the detectability, sensitivity and specificity of the imaging,” Joseph says. If the enhanced imaging results with a PET-MRI show that a patient has had a complete response to radiation and chemotherapy, meaning the cancer has been effectively treated, then those patients would be considered for a “wait and watch” approach without surgery.
Joseph predicts as many as 30 per cent of low rectal cancer patients could avoid surgery if the PET-MRI proves to be accurate at identifying patients with no remaining cancer. Not only would this free up operating rooms and surgical schedules, patients would not have to deal with the pain of recovering
Where do you get your best ideas from?
“From day-to-day life when I meet with patients. Things will come up, and I’ll think, ‘Okay, we should look into that.’”
What job would you have if you weren’t an oncologist?
“My initial plan was to get my masters in chemistry and become a college lecturer. I was planning to teach. When my buddy passed away, I switched my focus as it motivated me to become an oncologist.”
What motivates or inspires you in your day-to-day work?
“I’m passionate about improving the quality of life for patients. I won’t ever delay patients — if I get a referral, I’ll try to see them the same day or next day. That’s the way I work.”
from surgery. Surgeons often have to remove part or all of a patient’s rectum and occasionally other organs in the adjacent area, such as ovaries or prostate glands. The result is these surgeries can drastically affect a patient’s well-being, leaving them with chronic pain or lasting bowel issues.
“It will significantly affect quality of life for patients,” he says. “If the rectum itself or a portion of the rectum is removed, it will cause a lot of symptoms like abdominal pain and cramps — so many things that wouldn’t happen if we can avoid surgery.”
Joseph says he has seen an increase in rectal cancer diagnoses in recent years, particularly in patients under 50, and these improvements in imaging will have a particular impact on relatively young people who want to preserve their rectal function and quality of life for potentially several decades. He expects his research to be completed by the end of the year, and if the findings are positive, patients diagnosed with low rectal cancer in Edmonton should have access to the PET-MRI machine to either avoid surgery altogether or feel confident that the surgeries they do undergo are absolutely necessary to remove remaining cancer.
“These patients do not want to lose a portion of the rectum,” he says. “Hopefully, we can use the PET-MRI to gather very important information and in the future, avoid surgery for many others.”
Inspired
by EULA MENGULLO

On August 1, 2016, Julie Johnson and Keith Dyck saw The Tragically Hip perform the first of their final two Calgary concerts. It was a bittersweet night as, a year later, the band’s vocalist, Gord Downie, passed away from glioblastoma, a type of brain cancer. The Calgary couple were longtime fans of the band, and that evening inspired them to find a way to commemorate Downie’s musical legacy while raising funds for cancer research.
“After that concert, it really sparked us to think about ways that we could honour the legacy of Gord Downie and the music of The Tragically Hip,” shares Johnson. “To bring people together and raise money for cancer research and to keep his legacy alive.”
In 2018, Johnson and Dyck hosted their first annual rock concert and music festival, now known as GEDfest (GED stands for Gordon Edgar Downie). Today, this one-day charitable celebration is hosted across Calgary and Edmonton along with Kelowna. The event is headlined by The Tragically Hip tribute band called Trickle Down, for which Dyck is the drummer.
Speaking about their motivation to
give back to different cancer-related initiatives across the country, including the Alberta Cancer Foundation, the founders emphasize contributing to the community, no matter how small.
“Part of the motivation is to simply lead by example,” says Dyck. “In the community, everyone can do something, and this is our something.”
“Inspiring others to make a difference too, in whatever grassroots way that people are able to,” Johnson adds. “Just coming to GEDfest, you might be standing beside someone who has faced cancer. That support is meaningful and does not necessarily have to translate to giving a dollar; it can be just giving your presence in support of someone else who’s gone through or going through a cancer journey.”
Dyck and Johnson aspire to one day host the concerts simultaneously across different major Canadian cities while continuing to raise funds for local cancerrelated charities. “We’d like to arrive at something similar to the Terry Fox event that happens every year, on a similar day, for a similar cause,” says Dyck. “That’s what we

had in mind when we set about trying to put this together.”
The core of GEDfest includes preserving Canadian music traditions to be enjoyed by future generations. “Keeping the [work going] against cancer, including Gord Downie’s life and legacy at the forefront, is the key to GEDfest, but keeping Canadian music traditions alive is another big part,” Johnson says.
“We’re hoping that through GEDfest, not only will we raise money and bring awareness to cancer, but also raise awareness for Gord Downie’s desire for a more unified Canada and keep his legacy alive for the next generation.”

Tevi Helland-Nergaard puts her innate sense of caring to work supporting cancer clinical trial patients.

Many advancements have been made in cancer treatment over the decades.
While academic researchers are justifiably cheered on for breakthroughs in new drugs and therapies, credit should also go to the clinicians, nurses and patients who are at the frontline making cancer clinical trials possible. Enrolling in a clinical drug trial can be both exciting and anxiety-inducing for a patient who is already in the midst of cancer treatment.
Tevi Helland-Nergaard, an oncology nurse at the Arthur J.E. Child Comprehensive Cancer Centre (Arthur Child), has been a positive force in guiding patients through the process of testing the potential of new and emerging treatments and drugs.
Helland-Nergaard is the lead clinical trial nurse with the genitourinary (GU) tumour group at the Arthur Child. She’s held that position since 2007 (beginning at the Tom Baker Cancer Centre), making her the longest-serving nurse in the group and an invaluable expert on the patient side of trial research. Helland-Nergaard educates, supports and administers medication to patients with GU cancers — including kidney, bladder, prostate, testicular and
other cancers pertaining to the urinary tract — who are approved for clinical trial participation. It’s an important job requiring a passion for enabling research as well as the ability to keep patients informed and well cared for. These patients volunteer to help advance research while also undergoing the physical and mental challenges of standard cancer care.
The nature of trials requires consistent care involving nurses who are well-versed on the potential effects of new drugs and drug combinations being tested as well as each patient’s unique set of health concerns. This gives Helland-Nergaard the opportunity to serve as each of her patient’s long-term point person, a unique situation in oncology, where patients rarely see the same nurse from appointment to appointment. As a result, she gets to know her patients well over the course of several months, or even years, with post-trial
follow-up visits, and can provide an extra level of comfort thanks to that familiarity.
“It’s such a privilege to be able to walk through the cancer journey with patients and families facing this life-threatening disease,” she says. “I’ll do anything I can to make their trip to the Arthur Child better. It’s a relationship that continues even after they’re no longer under your care.”
As a young girl, Helland-Nergaard always knew she wanted to be a nurse. Her maternal grandmother was a matron nurse in southern Saskatchewan, and HellandNergaard remembers watching in awe as she left for work dressed in her starched white cap and cape. That inspiration, coupled with her own innate aptitude for caregiving and her warm demeanor, led Helland-Nergaard to what seemed like her natural vocation.
Helland-Nergaard initially gravitated towards ICU care, where she embraced the immediate impact of her work and the gratification of helping a patient in need of acute care. Eventually, though, while working at a hospital in Penticton, B.C., she shifted towards systemic oncology care — the administration of chemotherapy and similar treatments. The daytime schedule was more convenient for an experienced nurse who was also busy raising a family, and Helland-Nergaard also got a taste of the odd bit of research work at the relatively small hospital. She continued in systemic care after a move to Calgary in 2004. Three years later, she seized the opportunity to pursue her growing interest in research when she transferred to the Clinical Research Unit for the position she still holds today.
“I really loved the adrenaline rush of critical care,” she says. “But even though I didn’t know much about research, I saw these new drugs coming in with names I couldn’t even pronounce, and I wanted to be part of it.”
“Tevi is more than a nurse to me. She has stood by my side during both my good days and the incredibly tough ones, providing support that goes beyond her job and medical care. Tevi’s warm smile and genuine interest in my well-being makes a profound difference. I can confidently say that without Tevi being Tevi, I am not sure I would still be here today.” —MICHAEL PICHNEJ
In addition to the relationships she forms with patients, witnessing the development of new drugs and therapies keeps Helland-Nergaard passionate about her role with the GU Clinical Research Unit. Being in the same position for almost two decades means she has seen significant advancements in cancer care that have extended or greatly improved the lives of patients and have even become standard of care across the province.
As an example, starting in 2012, Helland-Nergaard worked in trials involving immunotherapy treatments and saw how that research not only improved outcomes, but also allowed patients to avoid some of the infamously harsh side-effects of chemotherapy (which she notes have improved greatly over the course of her tenure thanks to the work of cancer researchers). The trials she and her patients have been involved in have brought about revolutionary treatments that are now becoming part of standard cancer care. Helland-Nergaard finds that immensely rewarding.
“Being part of immunotherapy — a [treatment] that helps the patient’s own immune system attack the cancer — and to witness that response in patients’ cancer has been pretty exciting,” she says. “Even though I don’t have any part in actually creating these therapies, just being part of seeing the change over time has been incredible.”
The research aspect of her job certainly inspires Helland-Nergaard and has led her to get involved in the larger world of oncology nursing, holding positions in various professional groups and committees, not to mention winning the Award of Excellence in Kidney Cancer Nursing at last year’s Canadian Association of Nurses in Oncology conference. But as rewarding as her professional accolades may be, Helland-Nergaard’s purpose

remains rooted in caring for others.
The one-on-one time spent with patients and the focus on continuity of care keep Helland-Nergaard enthusiastic about getting up every day. She continually checks on her patients and makes sure they feel cared for.
And that they do. “Tevi treats each patient with exceptional care and empathy,” says Michael Pichnej, one of her patients. “Her presence has been a source of comfort, and it’s hard to express how grateful I am for her support. Tevi has not only helped me navigate the complexities of my treatment, but has also become an extended member of my family. I am thankful for her unwavering dedication and compassion. These relationships truly make a difference in the lives of patients.”
Helland-Nergaard knows her patients leave an enduring legacy even if their own outcomes aren’t ultimately positive, and feels honoured to have cared for so many people willing to volunteer to make a difference.
“I have a flood of memories of faces and names of people I have cared for over the many years of my career,” she says. “I have built lasting relationships with patients and families. Years after patients have succumbed to their disease, I have run into family members, and we reminisce about their loved one. That leaves a lasting impact on me.”
“Tevi goes beyond what is expected of her; she has the ability to make me feel that I am important to her. She takes my concerns seriously and truly wants me to have the best outcome. My journey has been a long one but the one constant bolstering me up has been Tevi with her quiet compassion and positivity.”
—VAL MARR
1984
Started her nursing career at Moose Jaw Union Hospital in Sask.
1988 to 2003
Worked as an ICU nurse at Penticton Regional Hospital in B.C.
2004
Moved to Calgary and began working in the systemic day care unit at the Tom Baker Cancer Centre
2007
Joined the genitourinary (GU) tumour group at the Clinical Research Group at the Tom Baker Cancer Centre
2024
Received the Award of Excellence in Kidney Cancer Nursing at Canadian Association of Nurses in Oncology conference
2024
Continues as lead clinical trial nurse with the GU tumour group after moving to the Arthur J.E. Child Comprehensive Cancer Centre

STEPHEN MURPHY IS GEARING UP FOR HIS 10TH ENBRIDGE TOUR ALBERTA FOR CANCER.
Inspired by his own and his family’s cancer experiences, Stephen Murphy gives fellow Calgarians on cancer journeys an emotional and literal lift.
by FABIAN MAYER
When it comes to making things better for people living with cancer in Alberta, Stephen Murphy is on a roll. Whether it’s on two wheels or four, the 67-year-old cancer survivor has plenty of reason to stand up against the disease.
Even before his own diagnosis, cancer had profoundly affected Murphy’s family. His father, two of his brothers and his sister have all faced a diagnosis. Given the impact of the disease on his family, Murphy wanted to
find a way to contribute to the cause. He had heard about the Enbridge Tour Alberta for Cancer (Tour) but was a little apprehensive. He called the Tour office with his questions.
“I said, ‘How the hell am I going to ride 200 kilometres?’” Murphy recalls. “I’d hang up, then phone back 10 minutes later and say, ‘Well, how am I going to raise $2,500?’ It took four phone calls, and [the Tour staff member] finally said, ‘Steve, just sign up.’” So, in 2016, he did.
In 2019, Murphy began his own cancer journey after he spotted some blood in his urine and went to the doctor. A cystoscopy revealed cancer in his bladder. Murphy underwent a successful surgery to remove the tumour, and the cancer has not returned. Now riding for himself as well as his family, Murphy will hit the road for his 10th Tour this year.
Murphy’s latest commitment to helping fellow individuals facing cancer required less encouragement. Watching TV one day, he saw an ad for Wheels of Hope and signed up on the spot. The volunteer driving program provides rides for people facing cancer who are receiving treatment or attending follow-up appointments. Murphy started with the program in March 2024 and gives rides to and from Calgary-area hospitals every Monday.
“I know how [hard] it can be getting to and from appointments,” he says. “I wanted to help make it better for people getting into the vehicle, to help them feel a little more comfortable.”
Murphy says he has driven all kinds of patients, some without cars of their own and others unable to drive after exhausting treatments. He has found volunteering to drive extremely rewarding and often shares his own cancer journey with passengers.
“Once they get in the car and I open up about my own journey, it makes them at ease,” he says. “Then they can open up, and they feel like someone understands.”
Murphy’s commitment to both the Tour and volunteer driving is steadfast. He has vowed to continue participating in the Tour until he’s physically unable.
“It’s going to take a whole army to move us all forward,” says Murphy. “If we can make even the simplest changes, it’s going to make things better.”
The Riddell Centre for Cancer Immunotherapy’s fully integrated bench-to-bedside-and-back research ecosystem makes revolutionary cancer treatments a reality for Albertans.
by COLLEEN SETO

Thanks to a transformational $25-million gift from the Riddell Family Charitable Foundation to the OWN.CANCER campaign, the Riddell Centre for Cancer Immunotherapy (Riddell Centre) has become a leading research hub advancing immunotherapy treatments for patients facing cancer. The Riddell Centre, at the Arthur J.E. Child Comprehensive Cancer Centre, is a fully integrated research centre that is accelerating the development of innovative therapies that harness the body’s own immune system to target cancer.
The Riddell Centre team includes researchers, trainees, staff scientists and experts in biomanufacturing, adult and pediatric oncology and other specialties. Projects range from fundamental research surrounding unexplored cell therapies to clinical trials that could save lives.
“The science that we get to do here is just mind-blowing,” says Riddell Centre director Dr. Douglas Mahoney. “There’s nothing more exciting than having the ability to follow an idea — especially when it could turn into something meaningful for people.”
At the Riddell Centre, researchers are advancing chimeric antigen receptor (CAR) T-cell therapy, a groundbreaking form of immunotherapy. This treatment involves modifying a patient’s T-cell, a type of immune cell, by equipping them with genetic instructions to recognize specific cancer cells. Once reintroduced into the body, these enhanced T-cells seek out and target cancer cells with precision.
“CAR T-cell therapy didn’t happen overnight — it’s the result of decades of research and collaboration among scientists around the world,” says Nubia Zepeda, associate director at Riddell Centre. “While it might seem like progress has happened quickly in recent years, it’s really built on years of dedicated research and innovation.”
One of the Riddell Centre’s most significant milestones has been the development of a Canadian-first CAR T-cell therapy — designed, manufactured and brought to patients entirely within a Canadian academic research environment. This innovative therapy targets alveolar soft part sarcoma, a rare and aggressive soft tissue cancer, by using synthetic biology to reprogram a patient’s own T-cells to identify and destroy cancer cells.
“This innovation led to a single-patient study to assess its safety and early effectiveness,” says Mahoney. “The study began in the fall of 2023 with a patient from Quebec who traveled to Calgary for treatment. Now, the findings from this study are under review at a leading scientific journal, marking an exciting step forward in the field.”
More than a dozen experimental immunotherapies are being developed within
the Riddell Centre. “Right now, immunotherapy is used to help children, adolescents and adults with certain forms of cancer. At the Riddell Centre, we are working to make it an option for more cancer patients, including those with rare and hard-totreat cancers,” says Mahoney.
While CAR T-cell therapy is a standard treatment for some blood cancers, including certain forms of leukemia and lymphoma, researchers at the Riddell Centre are exploring its potential for treating solid tumours — one of the biggest challenges in the cancer immunotherapy field today.
“The Riddell Centre is one of the first in Canada to use precision cellular therapy to tackle treatment-resistant solid tumours, pushing the boundaries of what’s possible in immunotherapy,” says Zepeda.
In Canada, the first CAR T-cell therapy was approved in 2018 for B cell leukemia and B cell lymphoma, making it the first genetically engineered cell therapy to reach the healthcare
system. Since then, Health Canada has approved six CAR T-cell therapies, including one in 2023 for multiple myeloma.
Donor generosity has played a vital role in driving forward the life-changing research happening at the Riddell Centre. But it’s only a taste of what’s possible. To call the immunotherapy research “innovative” may be an understatement. Zepeda says when she first heard about the centre’s work, she likened it to science fiction. “It feels like something that should be very far off in the future. It’s incredible that it’s happening now, locally.”
The Riddell Centre holds a clear mission: to reduce the burden of cancer and improve patient outcomes by rapidly developing and testing new immunotherapies. And it’s doing just that.
“This isn’t just about research — it’s about getting novel treatments to patients faster,” affirms Mahoney. “The Riddell Centre is dedicated to advancing next-generation immunotherapies for children, adolescents and adults, with a focus on making them safer, more effective and more widely available. The impact of this work is already being felt, and there’s so much more to come.”
Driven by a commitment to advance cancer care and bring more hope to Albertans, the Riddell Family Charitable Foundation is helping transform the future of treatment through the creation of the Riddell Centre for Cancer Immunotherapy. Their visionary $25-million gift to the OWN.CANCER campaign is advancing groundbreaking research and accelerating the development of innovative new treatments — benefiting patients today and for generations to come.

We are proud to celebrate the exceptional individuals currently holding philanthropically funded fellowships, professorships, and endowed chairs. These roles are made possible through the generosity of our donors, whose support empowers leading minds in cancer care and research to drive innovation, advance discoveries and create more hope for Albertans facing cancer.
AWARD
Dr. Tasneem Dawood Ernest and Gladys Archinuk Clinical Research Fellowship in Oncology
Cristina Rai Fred C. Coles Cancer Research Fellowship
Dr. Kiran Paskalice Michael J Hutchison Fellowship in Radiation Oncology
Dr. Zamina Alam Papadopoulos Fellowship in Radiation Oncology
Dr. Maxime Mermod Papadopoulos Head and Neck Surgical Fellowship in Oncology
Dr. Egiroh Omene Wayne Foo and Lynne Marshall Clinical Research Fellowship
Dr. Kevin Hay Dixon Professorship in Clinical Hematology
Dr. Oliver Bathe Wayne Foo Professorship in Surgical Oncology
Dr. Fred West Allard Research Chair in Oncology
Dr. John Lewis Bird Dogs Chair in Translational Oncology
Dr. Frank Wuest Dianne and Irving Kipnes Chair in Radiopharmaceutical Sciences
Dr. Linda Carlson Enbridge Research Chair in Psychosocial Oncology
Dr. Paola Neri Engineered Air Chair
Dr. Adam Kinnaird Frank and Carla Sojonky Chair in Prostate Cancer Research
Dr. Cheng-Han Lee Sawin-Baldwin Chair in Ovarian Cancer Research
Recipient list current at time of publication.
PROFESSORSHIP
HOST
INSTITUTION
University of Alberta
University of Calgary
University of Alberta
University of Alberta
University of Alberta
University of Alberta
University of Calgary
University of Calgary
University of Alberta
University of Alberta
University of Alberta
University of Calgary
University of Calgary
University of Alberta
University of Alberta
CATEGORY
Dr. Cheng-Han Lee accelerates the drug development process to provide those facing the deadliest of cancers more treatment options.
by FABIAN MAYER
Dr. Cheng-Han Lee is on the front lines of cancer diagnosis. As a clinical pathologist specializing in ovarian and endometrial cancers, Lee sees firsthand the devastating impact of the disease. In his current role as the Sawin-Baldwin Chair in Ovarian Cancer, Lee has expanded his scope with the goal of improving treatment and lifespans of women with these cancers.
“As a pathologist, we are in a unique position where we make the diagnosis, therefore we know what is causing the most harm. I’m able to position my resources to bring forward better therapies based on my findings,” says Lee.
Lee decided to focus his research on some of the most deadly forms of cancer he regularly sees, known as dedifferentiated endometrial and ovarian cancers. Dedifferentiated tumours are relatively rare, but they are extremely aggressive. And despite advances in diagnostics, the life expectancies of those affected continue to be extremely short — measured in months rather than years.
“We’ve gotten very good at predicting who’s going to die, but we can’t do anything about it,” says Lee. “That’s a very frustrating and helpless feeling, which

is what motivates me to take it one step further to help the patients who have that disease.”
Lee harnessed a unique approach in hopes of accelerating the often painstaking drug development process. Rather than test individual drugs on patients, he and his team used cancerous tissue donated by women who underwent surgery to remove tumours. They then split that tissue up into tiny pieces and were able to test a multitude of drugs to see if any were effective.
“That identification process enabled us to test drugs that you wouldn’t have thought would be effective in killing cancer cells,” he says. “We’re able to test thousands of drugs and really expedite that drug development process.”
One of those drugs turned out to be surprisingly effective in slowing the aggressive growth of the specific cancer cells Lee was targeting. Digoxin has been around for decades and is typically used to improve heart strength and efficiency in patients with congestive heart failure. In the next phase of research, Lee and his team hope to identify another drug to pair with digoxin to maximize its effectiveness.
“Increasingly in cancer treatment, we’re not just talking about giving a patient one drug; we want to do a combination treatment,” says Lee. “It’s kind of like playing chess; you’re making two moves at a time on cancer so that it doesn’t have an escape.”
John Sexsmith helps build the future of cancer care — one donor at a time.
by ALEX RETTIE
photographs by RYAN PARKER

With a career of 35 years in journalism, John Sexsmith had already made a lasting impression when he joined the Alberta Cancer Foundation’s philanthropy team specializing in legacy giving in 2023. Now, the former Global TV sports anchor is building a different kind of personal legacy — a legacy of hope.
Sexsmith was first diagnosed with prostate cancer in 2012, and underwent a prostatectomy surgery. That was followed by radiation treatment at Edmonton’s Cross Cancer Institute (Cross). “I’m indebted to the medical professionals who treated me,” he says.
That sense of indebtedness is what led him to apply to the Alberta Cancer Foundation. “I wanted to give people with a cancer diagnosis more hope,” he says. And his work with legacy donors gives him the opportunity to do just that.
“Legacy giving is about seeing the big picture. When someone gives to the Alberta Cancer Foundation in a planned way, that lets the Foundation plan as well. It lets us pave the way for the future of excellence in cancer treatment.”
Sexsmith’s extensive journalism and
community engagement experience has been a great asset in his donor stewardship work. The efforts of the legacy philanthropy team contribute so much to making the amazing support the Alberta Cancer Foundation provides possible. “I know the value of connecting with people, and this work is all about building connections with donors,” he affirms.
Sexsmith works with more than 300 donors, most of whom have some experience with cancer either as survivors or as family members. “They’re really motivated to help others in the same situation. When I meet them at the Cross, they can look around and see the difference their giving makes.”
Legacy giving to the Alberta Cancer Foundation takes a number of different forms, including bequests in wills, naming the Foundation as a beneficiary of a life insurance policy or donating a portion of RRSPs, RRIFs or other retirement funds — they are all ways of helping Albertans facing cancer. “We tend to think of estate planning as something older people do,” says Sexsmith, “but I’m seeing a lot more people in their 30s and 40s thinking ahead about
how they want to make a difference.”
The difference donors make is something Sexsmith sees first-hand on a regular basis, both at work and in his personal life. His prostate cancer recurred in 2024 and he’s currently undergoing chemotherapy treatment at the Cross. It’s a challenging time, but he’s optimistic. “It’s pretty easy to stay positive when you see all the people willing to help. That’s the power of giving.”


