






























































































































Dental professionals from across the UK recently attended an immersive event at Frameless in London to experience an exciting journey of discovery as Colgate ® Introduced a New Era in Active Prevention.
The audience had the opportunity to experience the Active Prevention journey whilst hearing insights from patients, scientists, academia and the dental profession. Simon Petersen, Senior Vice President and General Manager at Colgate, Northern Europe welcomed everybody, sharing Colgate’s success is built on valued, trust- based relationships with a range of partners, including the dental profession. He also highlighted that as a global brand in over two thirds of all households, Colgate’s leadership position presented opportunities to enter a new era in Active Prevention.

Katie Mitchell, Senior Insights Manager at Colgate shared insights around what good oral care means to patients. These insights highlighted the need for an increased focus on patient empowerment through prevention with

some saying they don’t feel they have the knowledge or know enough to optimise their oral health at home.
Dr Bayardo Garcia-Godoy, Senior Researcher at Colgate then introduced New Colgate Total ®, designed to support the dental team in extending their professional care into patients’ homes. New Colgate Total® toothpaste’s superior technology with uniquely* stabilised stannous fluoride formula is formulated to provide high levels of bioactive stannous, targeting the cause
of common health problems. Bayardo also highlighted the opportunity of personalised Active Prevention by the ability to recommend the New Colgate Total ® Active Prevention toothpaste range as well as New Colgate Total® Active Prevention toothbrush and mouthwash to complete the Regime.
Tim Newton, Professor of Psychology as Applied to Dentistry at Kings College, shared the road to effective behaviour change. Tim looked at barriers to prevention and gave suggestions on
how to overcome these including using GPS as an analogy to set goals; plan your route and satisfy yourself you are going the right way.
Dr Mohsan Ahmad, a GDP working predominantly in an NHS setting shared how his team gives personalised advice to create and enhance patient engagement, empowering them to start their own journey to self-prevention.
Jan Prisic, Professional Brand Manager for Colgate brought the event to its conclusion, emphasising that there has not been a more appropriate moment for prevention to be so crucial in supporting the oral health of the nation. Jan introduced the New Colgate Total ® Active Prevention Toolkit developed by Colgate ® , designed to support dental professionals help their patients with Active Prevention between visits. The toolkits, available from Colgate Oral Care Consultants includes a preassessment questionnaire, handheld mirror and a chairside coaching tool to help engage patients to quickly deliver personalised care, along with a £1 coupon for patients to redeem against the Colgate Total ® toothpaste range at all major retailers.
The event was a huge success with great feedback including ‘inspiring and Insightful’, ‘a wonderful event that went above and beyond’, great speakers and new information’.
To find out more about New Colgate Total ® Active Prevention, please visit https://www.colgateprofessional. co.uk/products/colgate-total
The Department of Health & Social Care (DHSC) has announced that 700,000 extra urgent dental appointments will be rolled out across England. Health Minister Stephen Kinnock made the announcement, with NHS England writing to Integrated Care Boards (ICBs) directing health chiefs in each region to stand up thousands of urgent appointments over the next year.
The appointments will be available from April and have been targeted at dental deserts – areas where patients particularly struggle to access NHS

dentists. The appointments will be for patients who are likely to be in pain –including those suffering from infections or needing urgent repairs to a bridge –and require urgent treatment.
Each ICB has a target of urgent appointments to roll out, based on estimated local levels of unmet need for urgent NHS care. Levels of unmet need are calculated by measures including looking at how many people tried and failed to get an NHS dentist appointment.
“We promised we would end the misery faced by hundreds of

thousands of people unable to get urgent dental care,” said Stephen Kinnock. “Today we’re starting to deliver on that commitment.
“NHS dentistry has been left broken after years of neglect, with patients left in pain without appointments, or queueing around the block just to be seen. Through our Plan for Change, this government will rebuild dentistry – focusing on prevention, retention of NHS dentists and reforming the NHS contract to make NHS work more appealing to dentists and increase

capacity for more patients. This will take time, but today marks an important step towards getting NHS dentistry back on its feet.”
The extra appointments would translate into each of the 24,200 dentists recorded as doing some NHS activity last year seeing the equivalent of little over two extra urgent cases a month. Based on BDA analysis of government data, total unmet need for NHS dental care in England amounts to 13 million, or 1 in 4 of the adult population.



Where to begin?
I’ll start by introducing you all to our new series: The Ultimate Guide to Direct Access. A new episode is premiering on our YouTube channel every Thursday and the reception so far has been overwhelmingly positive. Scan the QR code to watch the series so far or visit https://tinyurl.com/UGTDA, and head over to page 14 to check out this month’s Spotlight, featuring series contributor Lauren Long discussing direct access and scope of practice. Thank you to everyone involved in bringing this incredible project to life! Around the time this issue lands on your doormat, it will be International Women’s Day on 8th March. On page 8, Judith Husband pens the first of a two-part series of articles, diving deep into dentistry as a career for women. Don’t miss part two next month! February was a big month for dentistry, with the government announcement of 700,000 additional urgent dental appointments to be rolled out across England, while Colgate hosted a mammoth event at London’s Frameless to usher in a new era for prevention. Having attended the event, I was pleasantly surprised to find myself in conversation with young dentists at the start of their careers, in addition to some familiar faces. If you missed the news, head back to the previous page.
With that all said, who’s excited to see where the rest of 2025 takes us?









The Probe is published by Purple Media Solutions.
Registered in England.
Registered number 5949065
Managing Editor: James Cooke
Commercial Director: Gary Henson
Divisional Administrator: Francesca Smith






Production Designer 1 : Lorna Reekie
Production Designer 2: Rob Tremain
Digital Content Manager: Stephen Wadey
Circulation Manager: Andy Kirk
Managing Director: Ed Hunt
Regular Contributors: Lisa Bainham, Nigel Carter, Barry Cockcroft, Ollie Jupes and Pam Swain
E-mail news, stories or opinion to james.cooke@purplems.com
Circulation/Subscriptions: The Probe Subscriptions, Perception SaS, PO Box 304, Uckfield, East Sussex, TN22 9EZ, Tel: 01825 701520, https://purplems.my-subs.co.uk ©Purple
Media Solutions Ltd, 2014. All rights reserved. ISSN 0032-9185. The publisher’s written consent must be obtained before any part of this publication may be reproduced in any form whatsoever, including photocopies, and information retrieval systems. While every effort has been made to ensure that the information in this publication is correct and accurate, the publisher cannot accept

liability for any consequential loss or damage, however caused, arising as a result of using information printed in this magazine.
The views expressed in The Probe are not necessarily the views of the magazine, nor of Purple Media Solutions
Editorial Advisory Board: Dr Barry Oulton, B.Ch.D. DPDS MNLP; Dr Graham Barnby, BDS, DGDP RCS; Dr Ewa Rozwadowska, BDS; Dr Yogi Savania BChD, MFGDP; Dr Ashok Sethi, BDS, DGDP (UK), MGDS RCS; Dr Paroo Mistry BDS MFDS MSc MOrth FDS (orth); Dr Tim Sunnucks, BDS DRDP; Dr Jason Burns, BDS, LDS, DGDP (UK), DFO, MSc; Prof Phillip Dowell, BDS, MScD, DGDP RCS, FICD; Dr Nigel Taylor MDSc, BDS, FDS RCS(Eng), M’Orth RCS(Eng), D’Orth RCS(Eng); Mark Wright BDS(Lon), DGDP RCS(UK), Dip Imp Dent.RCS (Eng) Adv. Cert, FICD; Dr Yasminder Virdee BDS. Readers who





We need to defib!
The NHS dental crisis came to visit our household a few weeks ago. I confess, it really caught us out. None of us were prepared, least of all me. If I’d still been in practice, of course, I would have naturally jumped in to deal with the catastrophe, whilst undoubtedly cursing under my breath at being voluntarily emotionally blackmailed into turning out on a Sunday to deal with an afflicted relative.
Long story short – my stepson is currently temporarily living with us and looking for a house to buy near his work, following his breakup with a lovely girl – a dental nurse I was instrumental in introducing him to. I’m assured that it’s a short-term living arrangement, which my stepson said would be ‘about four or five weeks,’ as he was moving his stuff back in. That was in 2018.
One Thursday, Ben (‘tis not his real name) went to his dentist (he was lucky to get an NHS dentist after I withdrew my health service services) and had a troublesome, partially erupted upper third molar out. By all accounts (actually, one accountthe victim’s), it was a difficult tooth that needed quite a bit of help from “A long thing with a thick handle that was rammed up my gum.” For anyone not familiar with them, I believe the instrument used was an elevator. Give elevators a whirl some time. If nothing else, they give you an air of mystery. Anyway, the tooth came out and though reportedly a bit “achy” the day afterwards, all seemed to be okay.
Come Saturday morning, the picture had drastically changed. Ben had been awake much of the night and I guessed he had a dry socket. The answerphone message from his dental practice was simple: Call 111. A couple of hours or so later, Ben was given the advice to find the local minor injuries unit and try his luck there. At this point, I was nonplussed. When I retired at the end of 2018, we had a fully operational emergency dental service in my area run by the local health and care trust, which you could ring directly if you were in trouble. But, apparently, no more. When I did an online search, there was not one emergency NHS dental service listed in our county, or two adjacent counties.
Anyway, Ben went off to the ‘local’ minor injuries unit – which various family members had used for other medical conditions previously, and were very happy with – but alas, the MIU couldn’t help. Apparently, that particular unit wasn’t equipped to deal with dental problems, a fact, Ben was told, the operators at 111 were made aware of some time ago.
By this time, it was mid-afternoon. Ben returned home and rang 111 again. He waited another hour or so for a dental nurse to come on the line and she said there may be hope of treatment on Sunday, either in a large city 30 miles away, or a county town 25 miles away. She gave him self-help advice (which he had already been armed with par moi) and assured my stepson that he would receive

a call within 24 hours but was more likely to be early on Sunday morning.
Since no call came by 11.30am, Ben decided to go and view a house that he had been forced to cancel a week previously and, on the way back from that viewing, he took a call inviting him to go to the emergency dentist in a practice 25 miles away. The offending socket was duly flushed and dressed, but in view of the large diffuse swelling over the left side of his face, was also given antibiotics. This morning (Monday), he is in as much discomfort as he was in on Saturday and Sunday, and was told by his employer not to report for work.
Obviously, this is a whole new ballgame for us, but for millions who have been denied access to NHS dentistry, it must be a nightmare. This weekend has exposed the stark reality of the deficiencies in what appears to be a barely functioning service in a very in-your-face, personal way.
There have been no harder workers in the fight to bring some sanity back to NHS dentistry than those at the British Dental Association and the Toothless in England campaigns, but they appear to be not gaining any significant ground, bearing in mind the UK Government is fully aware of the problem and its ineffectuality in dealing with the matter. How could successive governments ignore the concerns raised by the Health and Social Care Committee in 2008 - SEVENTEEN YEARS AGO - which declared the UDAbased NHS dental contract “not fit for purpose,” if they TRULY wanted to do something about it.
More recently, in July 2023, the same parliamentary committee echoed the statement made by its predecessor in 2008, two years after the abominable contract was introduced. Despite the 2023 report, which underscored the unacceptable levels of pain and distress experienced by individuals unable to
secure NHS dental appointments and called for immediate action to overhaul the existing system, nothing has happened apart from vapid lip-service.
But the re-emergence of Trump 2.0 in the United States and his tenuous grasp on the truth made me want to explore some of the less than factbased statements UK politicians have made regarding NHS dentistry, which undermine their assertions that they truly are keen to see the survival of the dental health service.
As an example, in April 2023, Prime Minister Rishi Sunak asserted that the number of NHS dentists had risen by 500 in the previous year. But data from the BDA indicated a decrease of approximately 700 NHS dentists during that period, marking the lowest number in over a decade. That was 1,100 dentists down on pre-pandemic levels.
Meanwhile, in June 2024, a joint probe by the BDA and Daily Mirror completely destroyed repeated claims by the Tory Government and then Prime Minister Rishi Sunak that their ‘Recovery Plan’ was improving access to NHS dentistry. Earlier in 2024, Ministers and government officials had stressed that “500 dental practices have started accepting more NHS patients.” After the BDA managed to identify and call 100 of the 500 practices the Government declared to be accepting patients, it found that only 10 of the practices had the capacity to do so. BS, or lies? You decide.
There was then the misrepresentation of ‘Contract Reforms.’ The Prime Minister (Sunak) stated that recent reforms had led to more NHS dentists and increased funding. The BDA refuted this, clarifying that the minor contract changes implemented lacked additional funding and were unlikely to enhance patient access or retain dentists within the NHS.
But, of course, the biggest whoppers
probably came from the Labour Government, post 2006. They claimed the new contract would improve patient access to NHS dentistry, whereas in reality access declined after the contract was introduced. The BDA reported that 1 million fewer patients were able to see an NHS dentist in the first two years of the contract - many dentists reducing their NHS commitments or leaving entirely due to dissatisfaction with the system. Labour also claimed that the new contract would reduce bureaucracy and simplify payments, whereas the new contract introduced the UDA system, which many dentists found confusing and unfair. As for the claim that the new system would incentivise preventive care, that was total balderdash since the contract paid dentists on activity rather than rewarding dentists for preventive work.
And as for Keir Starmer’s Labour Government, its October 2024 budget introduced significant increases in employers’ National Insurance Contributions, which have been universally criticised for imposing substantial financial burdens on dental practices. The National Association of Specialist Dental Accountants and Lawyers (NASDAL) expressed concerns that these measures could lead to practice closures and reduced patient access to dental care.
But you know all that already.
What’s the saying? “Liar Liar, Alveogyl’s on Fire.” n
About the author ollie Jupes is the pseudonym of a former nHs dentist. He monitors dentistry on twitter X as @DentistGoneBadd






VistaScan Mini View 2.0 from Dürr Dental is compact and easy to use. The simplicity of the scanning process is matched by exceptional image clarity.
Anything else is a compromise.
For more information visit www.duerrdental.com/en/products/imaging/




Judith Husband, a leading dentist and member of Council at Medical Protection Society – of which Dental Protection is part – reflects on dentistry as a career as we mark International Women’s Day on 8 March
The second part of this article will be published next issue!
Thanks to the historical efforts of women, and men, in the UK, we have built a broad range of legal protections for women in work and society in general. The dental profession in the UK has long been in the vanguard of being considered as supportive and inclusive. I have had the great pleasure to meet some of the women at the forefront of the fight for fairness, most notably including maternity payments in the NHS.
Many dentists are self-employed, both in the NHS and private sectors. This affords benefits and was personally part of the attraction of general practice and dentistry for me – but it can also place additional pressures on women dentists. Women associates can find themselves responsible for sourcing locums to enable them to have maternity leave, and those in the private sector are not afforded the maternity packages other sectors provide. We must always be mindful that many women in the dental profession are not dentists and there are a wide range of opportunities in nursing and hygiene/therapy, with new roles developing with the expanding role of DCPs.
Dentistry is not one single career but a profession that has huge variety of workplace, employment status and specialities – this is its greatest selling point but also requires careful research and consideration.
In countries around the world as more girls and women are educated, gain personal autonomy and are given the opportunity to pursue careers, we see steadily increasing numbers joining the professions, including dentistry.
Dentistry, although incredibly technical, at its heart is about caring for people, building trust and relationships. Emotional intelligence and good communication skills are very important in the caring professions and traditionally women are perceived to excel in these key areas.
Dentistry is inherently a flexible career with the opportunity to work part time, or out of regular office hours. Some other professions are more prescriptive, especially in early
years training, and so dentistry can be a much more attractive option than, for example, medicine to some.
NHS dentistry is a very broad term encompassing a huge variety of workplaces and contracting models. It is possible to have a varied and flexible career within the NHS, working across a multitude of sectors and employment options. In primary care and, more specifically, general dental practice, NHS practice can have advantages with respect to maternity and superannuation options. Contracting models differ across the devolved nations, and it is important to understand the requirements to make an informed career choice.
Private practice carries advantages of greater control over treatment and patient choice but also added responsibilities, like out-of-hours care which can adversely impact personal and family life.
Career flexibility may be enhanced by practice ownership for some. For others, including myself, being an associate enabled significant diversification of my professional portfolio.
We return to the importance of understanding the options, researching and identifying each individual’s priorities.
There remains the systemic barrier in the workplace for dentists of the gender pay gap. This is reported in independent NHS figures and needs to be taken more seriously. In any reformed NHS contract, due consideration for all parties must be a golden thread running through modelling, negotiations, implementation and reviews.
Potential pay gaps in the private sector are more difficult to measure but, as a profession, we should be finding methods to investigate and not assume that everything’s just fine because there are high numbers of women dentists.
Within the sphere of political representation of dentists, there remains a significant leaning towards men. This is in part women not standing, but also an outcome of the electoral process. For example, the General
Dental Practice Committee of the BDA remains disproportionately male, and it still has never had a woman chair.
Women face bias, conscious or unconscious, both within the profession and from patients, with many women dentists facing multiple discrimination due to race and religion.
Registration reports show special care dentistry and paediatric dentistry have a higher female employment rate compared to specialities such as endodontics, oral surgery, prosthodontics and restorative dentistry. These are stark and clear differences that the profession really should be interested in, researching and addressing. These trends are not shifting despite the continued increasingly high proportion of women registered as dentists in the UK. The causes will be multifactorial and may well differ across individual specialities. If there are barriers to women entering our specialities, it is a stark warning for the future, both for patients and training future dentists.
Dental Protection data shows practice principal members are predominantly older males. Practice ownership has been a topic of debate during my entire career. With the increased number of women dentists, there has also been a seismic shift in the commercial landscape of dentistry in the UK. Effective deregulation of the market, enabling large corporate entities to form, has impacted adversely some individuals’ ability to purchase. NHS contracting in England and Wales dramatically affected the historical freedom and opportunities to open new practices, leaving younger dentists with rising practice values and few alternative options.
Financial institutions are actively targeting women dentists, so there are increasing opportunities for professional advice and support. Peer support is available with some excellent women dentist networks for those considering practice ownership. Practice ownership is also not the career choice of an increasing number of dentists. In the 90s, I was an outlier. Now, more
dentists, male and female, are choosing the opportunity to have flexibility and variety. From my student days, joining the BDA Students Committee, right up to being Deputy Chair of the BDA, there have been incredible women role models, many of whom I had the pleasure of knowing personally and working with. With Dental Protection, we have supportive and inspiring women, together with men who are true allies. We have spoken a lot about women, but greater inclusion and a fair profession relies on the support of our male colleagues. Role models and their support has been key to getting (and staying) involved with dental leadership and representation. The importance of seeing people you can identify directly with is really important, and having trusted colleagues or mentors invaluable.
In recent years, there has been little improvement in the balance of those representing us, and this has been a constant disappointment. Increasingly, there are courses and events with allmale line ups. There are incredible women dentists and wider team members able and willing to represent us, to teach us, to negotiate on our behalf and ,yet, time alone is not shifting the dial towards are more balanced representation.
About the author
Judith Husband served as an elected Non Executive Director of the British Dental Association for over ten years and continues to sit on their General Dental Practice Committee. From June 2019, she was a member of the Dental Board which advises MPS on developments within dentistry and on members’ needs. Judith was recently appointed to the Medical Protection Society Council.




Dentistry is one of the most stressful professions – 86% of dental professionals report stress, and over 50% experience burnout. Wellbeing in dental teams is often reduced to a poster or helpline – reactive solutions that fail to prevent deeper issues like team disharmony, retention struggles, and stalled business growth.
Picture this: A practice where the team is constantly stretched, with little time to focus on anything beyond the daily demands. The daybook is full, but instead of feeling motivated, everyone is just pushing through to the end of the day. There’s little space for enjoyment, conversation, or collaboration, and 5pm cannot come soon enough. Constant staff turnover adds another layer of strain – faces constantly changing, and you are stuck in the never-ending training cycle or having to make-do and tolerate lower standards. When was the last time your practice had the breathing room to focus on real growth?
The cost of ignoring wellbeing
(The G.A.P.S.)
• Growth decline: A stressed team is 13% less productive. You might notice tasks taking longer than they should, with team members making avoidable errors, appointments running late, proposed treatment not being followed up, and admin piling up because no one has the time to stay on top of it. The focus
shifts from delivering excellent care to just getting through the day. What could your team achieve if they had the mental and emotional clarity to drive through success instead of barely coping?
• Absenteeism and attrition: The cost of a revolving door – burnout leads to a 63% increase in sick days and significantly higher staff turnover. Every time a team member leaves, the practice bears the cost of recruitment, training, and lost productivity, which can amount to tens of thousands of pounds per employee, and even up to £30,000 in some cases. And the impact isn’t just financial. Constant turnover increases workload for remaining staff, reduces morale, and leads to a cycle where good team members burnout and leave, worsening the problem. Imagine how much easier it would be to manage a team that feels supported and engaged?
• Patient complaints and care decline: Team wellbeing directly impacts patient care. A disengaged, stressed workforce lacks the energy and focus to provide the best possible patient experience where every detail is paid attention to. The risk of patient complaints rises. Clinicians feel the pressure of constantly double-checking work, fearing mistakes beyond their control. The exhaustion grows, adding to stress and affecting patient outcomes. Practice reputation
and patient satisfaction and retention rates suffer. How would patients respond if they walked into a practice where the team was thriving, engaged, and genuinely happy to be there?
• Stress and toxicity: With just a ‘head down’ culture, communication and trust breaks down, leading to unresolved conflicts, disengagement, discontentment, and low morale. Have you ever seen a practice where frustration turns into gossip, blame, and negativity; no one sharing, helping, or supporting – just heads down in their own tasks? It’s not long before yet another letter of resignation or sickness certificate ensues.
Time for a cultural shift to leadership and wellbeing
If wellbeing initiatives remain surface-level or reactive, the stigma around seeking support will persist. Instead of waiting until teams are on the brink of collapse, we must create a culture where wellbeing is woven into the DNA of a dental practice, not just an afterthought. After facing burnout myself, watching colleagues leave, suffer depression, addiction, or worse, I’m on a mission to make real change. But it’s not just about the extremes. It’s about the daily frustration, overwhelm, and lack of fulfilment that so many in dentistry experience. The feeling of constantly being on the back foot, unable to switch off, and
questioning if this is what their career was supposed to feel like.
This is where initiatives like BREATHE and MedDent come in to close the G.A.P.S. BREATHE, the first-of-its-kind platform for dental team wellbeing, provides dentalspecific resources for stress management, team re-energising, and improved communication – just a fraction of what’s on offer. MedDent goes further, integrating leadership training, team building, and optimal performance strategies to create sustainable success.
Investing in leadership and wellbeing isn’t a luxury – it’s essential for any dental professional or practice that wants to thrive. It’s time to decide: Will your practice lead the way in wellbeing and leadership, or let the G.A.P.S. grow too big to fix?
The BREATHE platform is being launched at BDIA Dental Showcase at ExCeL on Saturday 15th March by CDO England, Jason Wong.
About the author Dr Rana Al-Falaki is founder of MedDent Leadership & Wellbeing Academy, working with dentists to achieve optimal performance.







Visionary tool or technological gimmick?
According to GDC guidelines, dental professionals need to obtain valid consent from the public.
The GDC divides informed consent into three main parts:
1. Before any treatment can begin, dental professionals need to obtain consent and explain all the relevant options and associated costs.
2. Patients must understand the decisions they are being asked to make.
3. Ensure that the patient’s consent remains valid at each stage of treatment.
Some dental professionals rely on simply giving out leaflets and believing that the information given is enough for the patient to give their informed consent. However, this can often create more questions than it answers, leaving it open to interpretation. Dental procedures, and the often-technical language used, are complex.
Over the past few years, in the medical and dental field, consent has become an increased concern. With more litigation and court cases, guidelines need to be clear and concise.
The Supreme Court of the UK established that, rather than being a matter for clinical judgment to be assessed by professional opinion, a patient should be told whatever they want to know, not what the professional thinks they should be told.
The principle of consent is an important part of ethics and international human rights law. Dental professionals need to think about how they would wish to be treated if they were in the chair.
In 2010, Martin Kelleher introduced the concept of the ‘The Daughter Test’. In simple terms this test asks, when considering elective cosmetic treatment, knowing the potential risks and what this could mean long-term, would you conduct this treatment on your own daughter.
It may be worth revisiting The Daughter Test in the current trend for more cosmetic procedures.
Communication is the most important method to gain informed consent. A point to remember is that consent may be given either verbally or written. Written is more secure, for both patient and dental professionals as each party will have a copy for future reference. Written consent should be comprehensive, it should not however, be used as well as a verbal discussion, so that any questions that may arise, can be answered effectively. This will reduce any misunderstandings later.
Verbal consent on its own can be open to interpretation. For example, if a patient says ‘okay,’ it could mean that a person is indicating that they are ready to engage in a discussion and they are listening to what you are saying, or it could mean ‘okay, I agree to all of this treatment.’
It is vital that patients are kept informed throughout the whole of the treatment process and informed if a treatment plan requires altering. This will usually require a face-to-face meeting to go over these changes and any financial differences. If a patient decides they want to stop treatment, they need to give ‘informed
refusal’ – understanding what will happen if they stop treatment at the point that the treatment has reached. If possible, the dental professional providing the treatment should ensure that the patient has understood the implications of ceasing treatment and agreed that they do not wish to continue. If the patient does not wish to sign anything to indicate this, this refusal needs to be documented on their records.
This record should include risk management and what the patient’s options are now. This must also include a record of the discussion that was had and what is clinically the best for option for the patient’s dental health in the future.
As dental professionals, it is unlikely that we will not come across at least one scenario in which we have to manage a patient’s expectations and oral health outcomes. It will be up to the dental professional whether they can continue to treat the patient within these limits, or whether the patient’s expectations cannot be met. Therefore, the dental professionals/patient relationship has irrevocably broken down and the patient should seek treatment elsewhere.
slippery slope of another’s consent
At the beginning of life, parents step in and provide consent as children are not able to understand decisions.
Children aged 16 and 17 years old are presumed to have sufficient capacity to give informed consent for medical and dental treatment.
Children under the age of 16 years old can consent to their own treatment if they are believed to have enough intelligence, competence and understanding to fully appreciate what is involved in their treatment. This is known as being Gillick competent.
Dementia, severe mental illness, or emergency treatment to save their life may prevent a patient from being able to give informed consent.
A dental professional should speak to a patient’s caregiver, friends, or family to gain informed consent, yet it is still important to try to communicate what is going on to the patient as much as possible. Dental treatment should always be in the best interests of the patient and not necessarily what their family or caregiver wishes.
thoughts going forward
Moving forward, it is clear that patients are at the heart of consent and, without including them, we are setting up for disaster. Dentistry is for the benefit of public health, and the more information, the better.
Patients can make better-informed decisions about their dental health with the backing of knowledge from professionals. This means face-to face communication, a written tailor-made treatment plan, and written documentation of everything that is discussed, with copies for the patient and the dental professional. This is something that could never be achieved with a generic leaflet. n
About the author Karen Coates, oral Health Content specialist at the oral Health Foundation, and RDn

polly Bhambra takes a deep dive into the National Dental Epidemiology Programme’s 2024 survey
The recent findings from the National Dental Epidemiology Programme’s 2024 survey present a concerning picture of oral health among five-year-old children in England.
According to the report, 22.4% of these children have experienced dentinal decay in their primary teeth, a slight decrease from 23.7% in 2022.
However, this national average masks significant disparities across regions, socio-economic statuses, and ethnic groups.
And 22.4% is still too high a percentage of children starting school with decay.
Regional and socio-economic disparities
The survey highlights pronounced regional variations in oral health.
For instance, the north west of England reports the highest prevalence of dentinal decay at 28.7%, while the east of England has the lowest at 17.5%.
Such disparities underscore the need for targeted interventions in regions where children are most affected. Socioeconomic factors play a pivotal role in these health outcomes. Children residing in the most deprived areas are more than twice as likely to experience dentinal decay (32.2%) compared to their counterparts in the least deprived areas (13.6%).
This stark contrast indicates that socioeconomic deprivation is a significant player in oral health. We need focused public health strategies to bridge this gap.
ethnic disparities in oral health
The survey also reveals significant disparities among different ethnic groups.
Children from the Asian or Asian British ethnic group exhibit a higher prevalence of dentinal decay (37.7%) compared to other groups. Within this category, Pakistani children are particularly affected, with a prevalence rate of 43.2%.
This highlights the need for culturally sensitive oral health interventions that address the unique challenges faced by different communities.
Government-funded educational initiatives
Given these concerning statistics, it is evident that more proactive measures are required to improve the oral health of young children in England.
One effective approach is the implementation of government-funded education programmes. These could provide training on proper oral health care for children and their families within school settings or early years settings.
Schools serve as pivotal platforms for health education. They offer access to children across various socio-economic and ethnic backgrounds. By integrating oral health education into the school curriculum, we can instil good dental hygiene practices from an early age. This will reduce the risk of decay and other oral health issues.
proposed educational programme
Develop age-appropriate modules that teach children the importance of oral hygiene, proper brushing techniques, and the impact of diet on dental health. Organise sessions for parents and caregivers to educate them on maintaining their children’s oral health. These sessions would also help to recognise early signs of dental issues and understand the importance of regular dental check-ups. Provide teachers and school staff with training to reinforce oral health messages and identify children who may need further dental care. Supply schools with dental care resources, such as toothbrushes, toothpaste, and educational materials, to support the programme’s implementation.
School-based programmes can reach children from diverse backgrounds, helping to reduce health disparities linked to socio-economic status and ethnicity
Benefits of school-based oral health education
Implementing such programmes can lead to several positive outcomes:
• Early intervention: educating children about oral health can lead to the early adoption of good practices, preventing the onset of dental issues.
• Parental engagement: involving parents ensures that oral health practices are reinforced at home, creating a consistent message for children. Children will often bring learnings home, too. So, schoolbased education could work in reverse.
• Equity in health education: schoolbased programmes can reach children from diverse backgrounds, helping to reduce health disparities linked to socio-economic status and ethnicity.
improving our nation’s oral health
The 2024 oral health survey underscores the pressing need for comprehensive strategies to improve the dental health of young children in England.
Government-funded educational initiatives within schools could offer a proactive approach to lifelong oral hygiene practices, address disparities, and enhance the wellbeing of our nation’s children. By investing in such programmes, we can work towards a future where every child has the opportunity to enjoy optimal oral health. n
For more useful tips in dentistry, follow me on instagram @pollybhambra
About the author polly Bhambra, practice principal at treetops Dental surgery.

The DDU’s Leo Briggs shares ideas on how best to retain colleagues
The UK goes into 2025 with 1,371 more registered dentists after the GDC recorded a 3.10% increase in numbers compared with 2024, following the latest annual renewal period. This is partly because more dentists decided to renew their registration this year, but the additional registrants is good news for over-stretched professionals and patients. Now we all need to do our bit to ensure that dentistry remains an attractive and rewarding place to be.
The government has announced its plan to recover and reform NHS dentistry, which includes the much publicised 700,000 more urgent dental appointments in England. In addition to more funding to improve access, the government also needs to address other factors which are damaging morale.
In our written evidence to the Public Accounts Committee inquiry into ‘Fixing NHS Dentistry’ (https://tinyurl.com/DDU-NHSfix), we drew attention to the disproportionately high legal costs for clinical negligence claims, which are many times more than the claimant can expect to receive. We cited one typical case where a claimant received £1,400 while their legal costs were £60,000. We also called for a fairer, more timely and more proportionate model of regulation as unnecessarily lengthy fitness to practice investigations by the GDC have a huge impact on professionals’ mental health, can reduce NHS capacity, and put further unwanted pressure on the workforce.
Progress on both these fronts has stalled, with no sign of the promised system of fixed recoverable costs in clinical negligence cases, nor the legislation required to modernise the GDC. But as the groundwork for both has already been done, they represent relatively straightforward ways for the government to show its commitment to dentists.
Another way we can optimise retention is to support registrants and make them feel part of the community of dentistry. The DDU has previously helped to highlight the issue of professional isolation, especially for newly registered dentists, which can cause real problems if they have no other sources of support and guidance. The nature of modern life makes it harder to keep in touch but it’s important that dental professionals make the effort to look out for each other and check in with colleagues if they have concerns.
Finally, I think dentists themselves need to show they have what it takes to make a success of their chosen career. Professionalism, willingness to learn and empathy with others are essential qualities for any dentist and will certainly help if the going gets tough. I’d also advise all registrants to join a dental defence organisation like the DDU to ensure they have professional indemnity, access to expert dento-legal advice and legal representation in the event of a complaint or claim. A crucial benefit
of DDU membership is being able to access support and discuss issues of concern with a fellow dentist when you phone our advice line.
While the current state of dental services leaves a lot to be desired, the dental professionals I meet still love treating patients and want to use
About the author Leo Briggs is deputy head of the DDU.

their knowledge and skills to achieve the best outcomes. We need to work together to make sure today’s new recruits always feel this way.

Award














Effective daily plaque control is key to tackling the causes of gum disease and stopping gingivitis in its tracks.

For patients, however, changing their oral health behaviours can be hard.
has developed a range of tools and resources for dental professionals to help power up your patients’ gum health.

Over 80% of UK adults show signs of gum disease.1 As dental professionals, you know that effective daily plaque control is key to tackling the causes of gum disease and stopping gingivitis in its tracks. Haleon recently hosted a panel of dental experts to discuss the barriers dental professionals face in encouraging behaviour change for improved gum health. Led by Professor Tim Newton, President of the Oral Health Foundation, the panel explored practical strategies for motivating patients.*
The experts included:













The panel discussion ranged over a series of different topics, with the panellists bringing their knowledge and insight to the conversation.
Topics discussed included:
Framing the issue
The role of the patient
Practical approaches
Working with commercial organisations Behaviour change


Listen to the conversation at Haleon HealthPartner
“BLEEDING GUMS IS SO NORMALISED.”
Dr.


“I THINK THERE’S A LACK OF UNDERSTANDING FROM A VERY YOUNG AGE OF ALL OF THE BENEFITS OF HAVING A HEALTHY MOUTH.”
Neha Mehta Rhiannon Jones



















Corsodyl has developed a range of tools and resources for dental professionals to help power up your patients’ gum health.
This includes our in-surgery discussion guide, designed to support conversations about simple steps to better gum health, and to help you explain to patients the potential impacts of gum disease on overall health.
Find out more at Haleon HealthPartner


Exploring the changing role of dental hygienists and dental therapists treating patients under direct access
Whether working independently under a direct access arrangement, or under the prescription of a dentist, dental hygienists and dental therapists often lead the way in patient care and are fundamental to the long-term success of today’s dental practices.
Direct access has been the catalyst to the changing role of dental hygienists and therapists across both the private and NHS sectors in the last decade, in terms of progression, integration and utilisation.
integrating direct access
Direct access was introduced in 2013 when the General Dental Council (GDC) removed its barrier to direct access for some dental care professionals after considering the impact on patient safety.
This meant dental hygienists, dental therapists and, in some cases, clinical dental technicians, were able to carry out their full scope of practice without the patient having to see a dentist first.
Dental Therapist and NSK Ikigai Educator, Lauren Long, explains: “For patients, direct access means they now have easier access to a range of dental professionals without referral from a dentist. Patients can approach hygienists and therapists directly for treatment within our scope of practice, as well as screening for conditions such as oral cancer, caries and periodontal disease, something previously only a dentist could do.
“Once we are confident of our provisional diagnosis, we can also make a direct referral to a relevant dental professional if the patient’s condition is outside our scope of practice.
“I think the whole practice team really benefits when we all embrace direct access. It’s not only good for patients, who can be seen more easily to get the treatment they need, it brings more patients into the practice who are able to access the additional range of services the team provides.”
information and consent
It is important to ensure patients are fully informed before and at the time of booking a direct access appointment to ensure they know which professional they are seeing and the possible limitations of direct access. Information that should be provided includes what treatment the dental hygienist or therapist will provide on the day, what treatment they can offer following consultation, and where they will refer the patient should treatment be required that they cannot provide.
Previously, under direct access, dental hygienists and therapists could administer treatments such as local anaesthetic and high-strength fluoride, but only after obtaining a prescription from a dentist, otherwise known as a patient-specific direction (PSD), or having a document known as a patient group direction (PGD) in place.
In a recent move to increase the capacity and efficacy of oral health care in the UK, changes to the Human Medicines Regulations 2012 (effective June 26, 2024) enable dental hygienists and therapists across the UK to legally supply and administer specific prescription-only medicines (POMs) under an exemption mechanism without needing a PSD or a PGD.
This move, initiated by the British Society of Dental Hygiene & Therapy (BSDHT) and the British Association of Dental Therapists (BADT) back in 2013, and developed over the past 11 years, aligns with the broader objectives of the NHS Long Term Workforce Plan, which aims to bolster direct patient care while liberating dentists to tackle more complex procedures within the NHS framework.
The GDC has welcomed this change, stating that it will improve direct access for patients to dental hygienists and therapists, while promoting better use of the skill mix in the dental team.
There is no obligation for dental hygienists or therapists to administer and supply

lauren long is a Dental therapist with over 15 years’ experience, working exclusively in private practice in Edinburgh. Alongside her clinical work, lauren currently holds the position of therapist Clinical Director for pain Free Dentistry group and is a Kol and educator for NsK ikigai. lauren is also secretary of the BADt
medicines under the exemptions noted above. However, all dental hygienists and therapists, regardless of previous training, experience, and qualifications, should ensure they are appropriately trained, competent and indemnified to supply and administer specific medicines under the exemptions mechanism, encouraging them to select a course that follows the developed training curriculum.
The approval of exemptions for dental hygienists and therapists to administer specific medications is a big forward step in the delivery of oral health care, directly benefiting patients and the dental profession alike.
“For a hygienist or therapist, it will make our job easier and more straightforward in terms of giving the care that our patients need,” says Lauren. “From our point of view, and from the patients’ point of view, it’s only a good thing, reducing dependency on dentists for prescriptions while allowing us to practice to our full potential.”

With these regulatory changes, the role of dental hygienists and therapists is ready to expand significantly, aligning with the government’s proposals to rebuild dentistry for the long term, reform the dental contract, and shift the focus towards prevention. NSK is dedicated to supporting dental hygienists and therapists as a vital cog in the wheel of preventive dentistry with equipment that is designed and manufactured with the needs of these dental professionals in mind.
Alongside this, NSK Ikigai provides an active community and professional hub that underscores the crucial role dental professionals play in oral health and the wider healthcare arena, providing a platform that allows fellow professionals to learn new skills, follow key opinion leaders and develop new professional relationships. To find out more about the NSK Ikigai Oral Health Community and to get details of the Spring 2025 oral health webinars and face-to-face hands-on events visit https://mynsk.co.uk/ikigai/ n

Don’t
The series covers all you need to know about Direct Access, from what it is to how it can be implemented, what the benefits are to patients and practices, and what the future may hold.
Watch noiw at the-probe.co.uk and at https://www.youtube.com/@theprobemag- or by scanning the QR code above.

The year ahead is set to offer ideal conditions for the practice sales market. With buoyant independent buyer activity, renewed corporate appetite and banks keen to lend to the sector, now is the perfect time to make plans if you are considering the sale of your practice.


• Advised on, valued or sold 900+ practices with a combined value of over £840m
• Arranged over 500 viewings
• Received in excess of 330 offers
• Sold 125+ practices
• Achieved an




It is vital that sellers seek trusted and professional advice when considering the sale of their practice.

THINKING OF SELLING YOUR DENTAL PRACTICE? SPEAK TO THE EXPERTS


The daily tsunami of adverts we see makes it difficult for many companies to stand out. Among the thousands of posters, trailers, social media reels and video advertisements, how can smaller businesses make an impact and be remembered?
Storytelling is almost as old as language itself; a universal experience found in all cultures, ancient and modern. An effective story promotes empathy and helps make sense of the events and people around us. It can also be used for marketing and enhancing a customer’s experience. For dental practitioners looking to grow their business, incorporating stories within the marketing plan can increase engagement with patients and reach a larger audience.
power
Jerome Bruner, a psychologist, discovered that messages communicated through a story are 22x better remembered than facts and figures alone. In isolation, facts are numbers or statements with no meaningful connection; a story is more effective because it moves the audience intellectually and emotionally, building a relationship that they are invested in. This makes it an ideal way to enhance your practice’s marketing and make sure your care is remembered. Forging emotional connections is an effective strategy. Businesses have received superior engagement and increased profits when they strengthen this bond with their audience: fully connected customers are 52% more valuable than the customers that are simply highly satisfied. To achieve this, businesses must appeal to the emotional motivators of the consumers, helping to meet and exceed their expectations. Much like customers of a brand, dental patients are also driven by emotional motivators, such as wanting safety and security, a sense of belonging, friendliness, and excellent treatment results. Using stories can better associate your dental practice with these motivators.
Once upon a time…
Story marketing creates consistency for the practice. It should revolve around the patients – placing the audience as the main character increases the resonance of a message. As well as identifying the treatments and services you offer, the stories should highlight the culture of the practice, the experience you have and the problems you’ve solved.
According to Christopher Booker, there are seven basic plots in storytelling. These includes examples like the ‘rags to riches’ story or the ‘quest’ narrative. One repeated and common storyline is ‘The Hero’s Journey’, where a hero is called to adventure, faces conflict, overcomes it, and is rewarded at the end. This archetype defines many of our favourite books, films and plays. It’s happy ending is so embedded into the culture that it has become part of the subconscious, making it an easy example to apply to marketing and patient interaction. Whether discussing treatment options or planning a social
media strategy, using something as simple as ‘The Hero’s Journey’ structure can better explain the values of your practice, such as how a patient overcame a problem with a successful treatment and left satisfied.
How you present stories in your marketing can vary. 90% of businesses use videos for promotion, exploiting the benefits of social media algorithms and search-engine optimisation. Whilst effective at reaching a wider audience, the planning, filming and editing of videos is time-consuming, especially for busy practices. Whether using the help of co-workers or an external videographer, creating marketing material that tells the story of your work can be effective for reaching new patients.
Besides videos, blog posts, social media posts, and leaflets can also utilise storytelling to generate a stronger emotional response. Patients will want truth in their marketing; by being authentic with the stories you share you can strengthen the emotional connection for the audience. This sets you apart from more corporate, manufactured marketing material and better builds your unique brand for a more prosperous future.

To learn the art of weaving a story into a sale, consider the Business and Mindset Mastery course from IAS Academy. Led by Dr Prav Solanki, this intensive yet fun opportunity lasts one day and provides excellent advice on creating and enacting an actionable plan for practice growth. Beyond encouraging storytelling and optimising the practice, the course will also emphasise work-life balance and how to declutter your mind from business for longer-term health benefits. With Dr Solanki’s invaluable experience, the course is a must for all dental practitioners looking to enhance their potential.
Stories inspire, improve understanding and deepen our emotional connections. Introducing storytelling into your daily marketing workflow can make you stand out, reaching new patients and strengthening the perception of your practice. For more information on upcoming IAS Academy training courses, please visit www.iasortho.com or call 01932 336470 (Press 1) n
about the author
tif Qureshi is founder and a clinical director of iaS academy,
Effective decontamination is the cornerstone of safety in the dental practice. Not only must the right equipment be employed, but it must also be used and maintained correctly to ensure optimum results and operational efficiency.
HTM 01-05 and SHTM 01-05 provide a baseline for the types of equipment required and the associated testing, servicing and validation of each. They outline general maintenance guidance and mandate the validation of specific equipment.
However, these are not the only documents that must be adhered to for compliant decontamination in dental practices. All must also comply with the Pressure Systems Safety Regulations 2000 (PSSR), which are applicable to any piece of equipment in any industry that contains a pressure system.
What are the pSSr?
The Pressure Systems Safety Regulations (PSSR) 2000 demand that all equipment incorporating pressure systems must undergo annual testing and certification to ensure their safety. This includes any systems ‘compromising of one or more pressure vessels of rigid construction, like autoclaves’. Dental practice owners are responsible for keeping all the machines in their practices in good condition, protecting both patients and staff from the potential hazards associated with faulty equipment.
To comply, owners must arrange for equipment testing by a qualified professional who is sufficiently skilled specifically in evaluating pressure systems. Often an equipment engineer, this individual will determine whether the autoclave is safe for ongoing use and has a Written Scheme and a valid, signed Report of Examination. These documents must be stored as evidence of PSSR compliance, detailing the specific parts of the pressure system inspected, their condition and any necessary repairs or modifications that were made.
The Written Scheme and Report of Examination is a requirement as part of the annual validation of every autoclave. It is a legality for both practice compliance and insurance.
So, it’s the same as servicing?
with PSSR can lead to significant safety risks for patients and staff, with substantial further consequences for the practice. Regulatory authorities can impose a range of financial penalties, with further actions possible should an accident or injury have occurred among patients or staff as a result of practice negligence in this area.

With just a few simple steps, every dental practice can ensure their compliance with PSSR:
• Understand your responsibilities by familiarising yourself with the regulations and how they apply to your practice.
• Safely store your Written Scheme and Report of Examination to demonstrate your compliance.
• Organise annual inspections and certification with a specifically-trained engineer.
• Train your whole team to safely and competently use, test and maintain your decontamination equipment.
All of the above can be more easily achieved by working with a trusted provider of high-quality decontamination equipment, servicing and support. Not only does this afford confidence that the equipment itself will function effectively for maximum safety standards, but it also provides access to ongoing advice and guidance from experts.
Eschmann is renowned across the UK for delivering exceptional service, with its equipment built for efficiency and longevity. The Care & Cover servicing and maintenance plan includes unlimited breakdown cover, Annual Validation and PSSR Certification by a trusted Eschmann engineer, unlimited original manufacturer parts and enhanced CPD user training upon installation for the dental team. There is also comprehensive support available through a dedicated telephone line and from a nationwide team of 50+ Eschmanntrained engineers.

Compliance with PSSR is necessitated as part of the annual validation of autoclaves. This is different from servicing. An annual service is a check of the machine to ensure it is in good working order and is fit for use from a mechanical and electrical perspective. Software upgrades as well as minor repairs can be conducted to prevent the development of any major issues later down the line. Though not a legal requirement, regular servicing will keep the autoclave operating correctly, optimising workflow efficiency and reducing the risk of malfunctions, breakdowns and the associated surgery downtime – saving the practice time and money in the long-run.
PSSR compliance follows a formal process whereby a specifically trained engineer has evaluated the equipment and certified it safe for continued use. Non-compliance
the safe side of the law
Adherence to PSSR is a legal requirement for all dental practices with an autoclave. It is in place to protect both patients and staff from harm. Make sure you’re compliant for the year ahead.
For details on the industry-leading decontamination equipment and unparalleled support available from Eschmann, including equipment validation and servicing, contact the team today at www.eschmann.co.uk or 01903 753322 n
about the author Nicky Varney, Head of Marketing at eschmann.

A complaint to the GDC can turn your world upside down. Our dentolegal experts are here to help turn it the right way up again.


The Misuse of Drugs Regulations 2001 provide a legal framework which dentists rely upon when prescribing patients with and managing controlled drugs. The act gives healthcare professionals the ability to possess, produce, supply and administer some drugs that would otherwise prompt prosecution under the Misuse of Drugs Act 1971.
Dental professionals should be aware of their responsibilities when supporting patients with these pharmaceutical products. This includes aspects of the General Dental Council’s ‘Standards for the Dental Team’, which requires clinicians to provide patients with treatment that is in their best interests, including the provision of controlled drugs exclusively when they are deemed necessary.
Clinicians must be knowledgeable about when these medications should be utilised. They should also recognise how to dispose of them safely and in line with waste workflows, to protect clinicians, patients and the wider world. This is just as important as the initial use of these products.
The Misuse of Drugs Regulations 2001 feature multiple schedules, the first five detailing seemingly endless lists of controlled drugs and the regulations to which they are subject. Dentists can prescribe select products to some patients on an NHS prescription form. This includes temazepam
tablets and oral solution, from Schedule 3; diazepam tablets and oral solution, from Schedule 4; and dihydrocodeine tablets, from Schedule 5. In addition, clinicians can provide midazolam, a Schedule 3 controlled drug, but an FP10D prescription is not required as it is not for use outside of the practice.
Three of these (temazepam, diazepam and midazolam) fall under the umbrella group of benzodiazepines. These are used to reduce anxiety over a short period, making them ideal for nervous patients.
Individuals may be advised to take the drug at home or in the practice. Clinicians should ensure patients are aware of all possible side effects, including increased anxiety, drowsiness and headaches, as well as trouble thinking clearly or making judgements in the ensuing 24 hours.
Dihydrocodeine is an example of an opioid, used for pain relief. Its use in NHS dentistry is poles apart from the wider prescription of opioids worldwide, especially in the United States. In 2016, dentists in England only prescribed dihydrocodeine from the opioid group, in a total of 0.6% of dental prescriptions. In the United States, the rate of opioid referral (including other solutions such as hydrocodone, codeine and oxycodone) was 37 times greater, at 22.3% of US dental prescriptions. This suggests a vastly different relationship with these medications amongst the two clinical populations and offers insights into the
We never stop solving for you. That is the leading promise from Solventum, formerly 3M Health Care, who set about making waves in the oral healthcare industry in early 2024. By bringing together ideas and experiences from a multitude of different clinical backgrounds, Solventum is able to craft new solutions to the issues that dental professionals face every day. Alongside this, Solventum partners with oral care providers to ensure each move to improve patient outcomes and transform practices is grounded in real world experiences. This makes certain that every new idea can truly add something to your workflow with immediate effect.
This also fosters discussions about existing solutions, including the award-winning products that are embedded throughout the Solventum offering. By having conversations with oral care professionals of all backgrounds, experiences and patient bases, Solventum can make the most relevant changes – no matter how minute – that allow clinicians to deliver more predictable workflows, and send patients home with brighter and bigger smiles.

Solventum shares the passion exuded by dental professionals for success and predictability, and have committed themselves to not only delivering industryleading materials and technologies, but also easy-to-access education and customer support. This helps to better inform the abilities of all practitioners, no matter their focused area of care.
Courses that are delivered by Solventum are presided over by trusted, world-class professionals. The featured educational materials are not just focused on clinical solutions. Dentists and their teams can even discover insights into aspects such as treatment presentation, to better reach patients when advising them on the solutions available to them.
Dental professionals can explore Solventum’s suite of dental solutions online, and be sure to find items that advance their oral care – no matter what field of dentistry they occupy, or the patients that come through their door.
For the indirect restorative workflow, it’s important to reduce complexity and maximise reliability and accuracy. The result is successful lasting treatments. Solventum understand these aims, and helps to offer predictability, every step of the way. This way, dental professionals can get it right first time – every time – with trusted solutions that can help you prevent costly rework and keep patients smiling.
For the truly universal adhesive, the RelyX Universal Resin Cement from
extent to which current legislation in the UK limits the prescription of controlled drugs.
Each medication mentioned can be dangerous in the wrong quantities and the hands of an unsuitable patient. In the outside environment, they can be threatening to wildlife too. For these reasons, clinicians must keep controlled drugs appropriately (whilst midazolam does not need to be kept in a controlled drug cabinet, temazepam does, for example), and dispose of them correctly.
All Schedule 2, 3 and 4 (part 1) controlled substances mentioned in the Misuse of Drugs Regulations 2001 must be denatured or rendered irretrievable before disposal.
Dental practices that store controlled drugs and expect needing to denature them – for example, when they have expired, or been partly used – must be covered by the Environment Agency exemption “Waste exemption: T28 sort and denature controlled drugs for disposal”. If practices or groups are set up across multiple locations, then a separate T28 exemption is needed for each site.
This waste can be stored in the practice for up to six months, and clinicians should organise collection by a specialist waste management service. Denatured pharmaceuticals, once unrecognisable as a drug, should be stored ready for disposal in a blue-lidded pharmaceutical container as per the Health Technical Memorandum 07-01

Solventum works as both a standalone, self-adhesive cement and as an adhesive cement when combined with Scotchbond Universal Plus Adhesive from Solventum. As a pairing, they were titled the Top Long-term Performer: Cement System at the Dental Advisor Awards 2024, taking gold as a total of 636 restorations were recalled without a single debond in either self-adhesive or adhesive modes.
On its own, the RelyX Universal Resin Cement is a formidable tool in the dental professional’s arsenal. A game-changing syringe ensures each application can be simple, with dispensing, cleaning and storage all optimised. The system’s unique chemistry also ensures excess outflow remains at the restoration margins for easy removal after tack curing. This makes the process simple for the clinician, and can put patients at ease.
Less time. Less mess. Less waste. Less stress. That is the aim when you use the RelyX Universal Resin Cement.
Simplicity is at the heart of a wide range of Solventum products, including the Filtek Supreme Flowable Restorative. It is a flowable composite that routinely delivers success, with 12 available shades helping to smooth the transition between restoration and tooth. The syringe is,
waste colour code. The blue waste stream is dedicated to medicinal waste, and as it can present chemical and environmental hazards it must be taken for incineration.
Initial Medical provides clinicians with safe and regulatory-compliant Controlled Drug Denaturing Kits. These are available in different sizes and are simple to implement in your practice, alongside pharmaceutical waste bins, like those in the small Eco Pharmi bin range. These are manufactured from 100% recycled plastic for environmentally-friendly impacts, or their new paper based Bio-bin range maximise safety against controlled drug waste within the dental practice.
The prescription, storage and disposal of controlled drugs must be managed safely to support patient populations and the wider environment. This requires clinicians to regularly review the regulations that impact their practice, and recognise how current workflows may be optimised to improve everyday care.
To find out more, get in touch at 0808 304 7411 or visit the website today www.initial.co.uk/medical n
about the author rebecca Waters works within the research and Development team at rentokil initial.


once again, designed for optimal material placement, virtually eliminating bubbles and material “run-on”.
If clinicians want a workflow that allows for optimal aesthetics, the Filtek Easy Match Universal Restorative is the system of choice. It is designed to streamline single-shade restorations from the start, whilst providing the flexibility necessary to match most patients.
The Natural shade can aid a majority of cases, and the complementary Bright and Warm shades help to fill-in the gaps on either end of the range. Whether working in the anterior or posterior, clinicians can intuitively select their solution and deliver a restoration that features the same exceptional performance and handling as is expected from all Filtek Dental Restoratives.
Solventum is proud to be opening up the conversations between all dental professionals that help to provide patients with more successful treatments. With an array of simple-to-use but impressively effective options on-hand, clinicians can be confident that they can help patients achieve their dream smile. This reduces the need to refer out of practice, keeping individuals comfortable and trusting in their oral care provider.
To learn more about the celebrated dental care solutions from Solventum, contact the team today, or visit solventum.com/en-gb/home/oral-care/ n

The project first started in 2022 when we updated the rear surgery in the two-surgery practice. We had decided to carry out the works in two phases as we were trying to get permission to install an external vent. The practice lies within a conservation area, so this proved to be a significant obstacle involving planning departments and building regulations.

I initially worked with Clark Dental when I updated the practice in 2001, however it had begun to look tired and outdated. Various work had been carried out over the years, so certain aspects appeared disjointed. Fortunately, there was nothing wrong with the existing equipment – it was all still working –but we felt that the practice as a whole could be more cohesive, and a renovation had been on the cards for a while.
The practice is set in an old office space, and the original plan was to install an air conditioning system and rejig to put in a decontamination corridor to better align with best practice. However, planning permission was denied, which meant we had to change our plans. Instead, we opted to update both surgeries with new equipment, and improve
the dirty to clean decon routine, and hence improve workflows in the practice.
For the first phase of the project – renovating the rear surgery – there was no impact on work at the practice and patients were seen as normal. Once work began on the front surgery, we planned for my colleague to take two weeks of annual leave, enabling me to move into the rear surgery to cover emergency appointments, whilst the rest of the practice staff were able to work remotely. During this time, everything was removed from the rest of the practice, allowing the contractors free rein to carry out the works, without any unnecessary obstacles.
Once the building work was completed, Clark Dental were able to come in and install our new equipment and cabinetry. We prioritised completion of the reception area and computer installation to allow the rear surgery to function as normal. The front surgery was completed two days later, enabling me to also return to work.
I decided to work with Clark Dental again on this project as, years ago, I redesigned Teeth @ W2 in Paddington, which was an old medical surgery. At this time, Clark Dental were the sole distributors of the very stylish Italian Anthos dental chairs. John and the team at Clark Dental were immensely helpful, and had a network of

contacts from finance to building works which meant the project went very smoothly.
When it came to selecting new equipment, I talked through quite a lot of options with the team at Clark Dental. Matt Rowlingson suggested options that would work for us, and I sought advice from others who made the same suggestions. I opted for two Sirona Intego Treatment Centres, Edarredo Cabinetry in Matte Black, and two Nomad handheld x-ray systems. The treatment centres we chose offer lots of options for customisation, including choosing the unit motors and scalers in each outlet.
Once a start date was agreed, the team drew up a schedule, organising when builders, electricians, plasterers and decorators would be onsite. Clark Dental then knew the exact dates to install the equipment and we were able to timetable our return to work. This was incredibly helpful as, once the schedule was finalised, everybody knew what would happen when enabling the works to be completed on time.
Even though, because planning permission was denied, all of the original drawings and schemes for airflow work were scrapped, I am very pleased with the result.
It looks amazing and is a pleasure to work in. The old surgeries were dated and difficult, having been patched up over the years. Now the practice is modern, clean and crisp. The team has a real sense of pride in where they work. And, most importantly, our patients are impressed with the transformation.
Those who have undertaken a similar project will certainly know, it’s handy to work with people who know each other and can communicate easily. This makes

Clark Dental invaluable, their expertise, knowledge, and connections make life a lot easier. It meant that we had a team of people from different companies working together, and it is crucial that builders and suppliers talk to each other. It’s a process, and if not managed properly a project like this could snowball, with small errors having a knock-on effect. Working with the team at Clark Dental meant the project was as efficient and seamless as it could be. I would absolutely recommend Clark Dental to anyone embarking on a refit or renovation. This is my third time working with them. Their service and attention to detail is truly outstanding.
For more information call Clark Dental on 01268 733 146, email info@clarkdental.co.uk or visit www.clarkdental.co.uk n
about the author Dr aayesha Meghji, owner of teeth @ W1, a boutique private dental clinic in the heart of Mayfair.

There are many reasons that a dental practice may require a quick turnaround time for lab work. With patients expecting ever-faster results, it can be challenging for dental professionals to meet their needs. Growing demand for precision and speed from dental labs means that dental technicians in turn need to focus on making internal processes more accurate and more efficient. There are a number of areas that labs might consider reviewing to meet these aims:
In order to continuously improve the quality of work and increase productivity, dental technicians should regularly receive training related to daily work in the lab as well as new techniques and technologies that may assist their workflows. A team that is highly skilled and well trained in the systems they use will be able to manage increasing demands more effectively.
Communication between members of the dental lab team can be the key to avoiding errors and improving workflows. Updating colleagues on project progress in real time is an important way to avoid problems cropping up, as all the necessary information is available to all when it is needed.
Adopting new technology is an excellent way to optimise processes in the dental lab, with modern solutions able to improve accuracy of fabricated prostheses whilst also speeding up workflows. Recent innovations which have drastically altered the way the dental lab works include 3D printing and milling machines. This technology has become more accessible in recent years, enabling technicians to quickly and efficiently produce prostheses and surgical guides.
A digital workflow can radically change a dental lab’s daily practices. In many cases, it can make workflows more efficient, make the team more productive, and enable enhanced collaboration both internally and externally. In order to implement a digital workflow in the dental lab, technicians must create or obtain a digital impression of the patient’s dentition. Intraoral scanners have risen in popularity amongst the dental profession in recent years as a result and, although considered by some to be more convenient, intraoral scans can have inaccuracies caused by gaps or holes in the image mesh, making them less effective for more complex treatment plans. Research suggests that, particularly in
edentulous patients, intraoral scanners can be inaccurate which will result in issues when it comes to denture retention. The most significant discrepancies arise when recording the compressible mucosal surfaces.
Because of these disadvantages, some dental professionals have decided not to adopt intraoral scanners, or not to use them for more complex treatment. This means that some are missing out on the benefits that digital dental workflows afford, particularly when it comes to digital planning, communication/collaboration, and speed. However, there is an alternative way to access the best of both worlds.
In cases where traditional impressions are more appropriate, the next generation digital scanner from Mimetrik is the ideal solution. The Cubit360, due to be unveiled at the IDS in Cologne, enables everybody involved in the clinical pathway to save time whilst maximising the accuracy of their digital work.
Unlike previous generations of digital scanner, the Cubit360 is portable and can be used chairside in the dental practice if needed. The Cubit360 does not require the scan object to be clamped, instead, the dentist can take an impression, and rather than posting it to the dental lab, the impression (or denture if
a copy denture is required) can be scanned immediately in the practice and the scan sent directly to the laboratory.
In the dental laboratory, the Cubit360 offers an extremely quick and efficient method of scanning both impressions and models. A full six axes of scanning freedom and the ability to scan without clamping the scan object means set-up time is hugely reduced and all scans, including articulated models, can be carried out in a fraction of the time taken using conventional lab scanners. Particularly important for busy or growing dental labs who would like to increase their productivity, implementing an effective digital workflow can be the step you need to take to make a difference. Choosing equipment carefully is important for ensuring you have the most appropriate solution for your unique needs. Finding practical ways to save time are essential when it comes to successfully digitising your workflow. For more information about Mimetrik, please visit https://mimetrik.co.uk/ n
about the author alyn Morgan is co-founder and ceO of a spin-out company from the University of Leeds, Mimetrik Solutions.




A day to support you with everything you need to effortlessly increase implant numbers and associated profits, regardless of your current implant numbers or your chosen implant system.
FOR GDP’S WHO:
Offer implants and want to do more Are just starting their implant journey
DENTAL HYGIENISTS & THERAPISTS WHO:
Are identifying potential implant patients
Supporting the long term maintenance of implants
TEAMS:
Looking at how implants can support practice growth





In the context of rapid technological change and evolving industry standards in dentistry, equipment, software, materials, and surgical techniques can quickly become obsolete. While innovations within the industry have greatly improved the efficacy of treatment, the pace of change presents some problems, including an environmental impact, an increased need for capital investment, and pressure on training budgets.
The challenge for innovators in dental technology is to continue to develop exciting solutions that meet the ongoing needs of clinicians and patients, which are also intuitive, repairable, maintainable and upgradeable. New technology should be designed to last, while enabling a sustainable approach to waste management at the end of their lifespan. As much as possible, digital technology should have capacity for growth and development, and should be upgradeable without clinicians having to relearn their use from the ground up.
The development of new technology in one area will often create a need for innovation in other areas. For example, artificial intelligence (AI) is a very powerintensive technology, which has required new specialist circuit design. Traditional data centres are designed with an average of 5-10 kilowatts per pack, while AI requires 60 or more. New data centres, and new strategies for data security have had to be built to accommodate this. There is a risk
that when one area of technology is left behind, a slew of inter-related technologies will then also become obsolete.
This is certainly true in the dental industry. For example, clinicians often encounter complications associated with vintage implants. The general incidence rate of prosthetic failure after 5 years due to screw loosening is 11%. Implant design has developed at such a rapid pace that there are occasions where available prosthetic components may no longer be compatible. In cases such as these, approaches to treatment can be complex and may sometimes require the removal and replacement of wellosseointegrated implants.
Software and hardware upgrades often make older digital systems incompatible, forcing practitioners to replace entire setups rather than parts. This includes computer systems, electronic point of sale (EPOS) systems, databases, and some digitallyassisted technologies like CAD/CAM equipment or intraoral cameras. Keeping up with the latest technology requires significant investment, which may not always be feasible for smaller or independent dental practices who may struggle to amortise the cost of expensive equipment before it becomes obsolete. Investments purchased at high costs may lose value quickly, offering limited returns or resale potential.
the environmental impact of electronic waste (e-waste)
As old equipment becomes obsolete, disposal becomes a concern, particularly
Every job can put strain on home life and many workers may find it difficult to juggle their personal and professional spheres. In the last few years, this balancing act has become more difficult, with 56% of people identifying work shifts as the top cause for hindering family time.

For dental practitioners, the responsibility of the job can have a detrimental impact –it’s well-established that burnout plagues the profession, inhibiting workplace satisfaction and impacting home life. However, spending more quality time with family and loved ones can help alleviate symptoms of stress, ensuring dental practitioners are confident and empowered to tackle each day as it comes.
Quality time is defined as a period of time relaxing or doing activities that are

for electronic devices or materials that require special handling. If not strategised responsibly, a focus on continuous change to dental devices can conflict with efforts to promote sustainability and reduce waste.
E-waste is one of the fastest growing sources of solid waste in the world. In 2022, an estimated 62 million tonnes of e-waste was produced globally. This is up by 8.4 million tonnes of e-waste reportedly produced in 2019. The United Nations university has estimated that only 17.4% of all e-waste was collected and recycled. Common e-waste includes non-renewable materials that are difficult to extract for re-use if not recycled properly.
To mitigate against obsolescence, dental practices can invest in scalable technology. Some modular systems can be upgraded rather than replaced entirely.
W&H has embraced sustainability as a core principle in the design, manufacture and distribution of its products. The Implantmed Plus offers the flexibility of upgradeability allowing it to remain up to
date, by utilising new software updates ensuring its sustained practicability as an advanced surgical device. The Implantmed Plus is a modular system which works with the Piezomed and Osstell Beacon. This flexible design ensures all the devices are in service for longer, saving money and valuable resources. The W&H sterilizer range also offers easy upgradeability via software upgrades and activation codes ensuring its extended working life.
Obsolescence in dentistry is a significant issue that impacts operational costs, patient care, and environmental sustainability. By planning strategically and adopting flexible solutions, practices can mitigate its effects while embracing innovation.

To find out more about the full range from W&H, visit www.wh.com/en_uk, call 01727 874990 or email office.uk@wh.com n
about the author Kate Scheer, Marketing executive, W&H (UK) Ltd.

enjoyable, and not worrying about work or other responsibilities. For quality time with the family, this means that everyone is engaged; no talking whilst scrolling on phones or other forms of multitasking. In the last five years, families are spending less quality time together – we collectively spend four hours fewer per month with our children, parents or siblings than we did five years ago. Further studies have found that of the time we do spend with family, only 44% of that can be considered ‘quality’ because of how much multitasking is done in other people’s presence.
The average amount of time spent with family each day is 51 minutes. This equates to the same average time for getting ready for work and preparing food for the day, and is under half the 132 minutes that humans spend on social media every day. Running in tandem, though not necessarily in correlation, to the prevalence of social media and screentime, is a growth in anxiety, fuelled by a perfect storm of international crises, inflated costs and professional pressures. Among a survey of dental workers, 42.2% placed themselves in the highest category of emotional exhaustion, highlighting the need for quality time spent with family and loved ones.
a healthy alternative
Time with family and friends can be an effective stress buffer against unhealthy coping mechanisms like smoking, alcohol and drug use. For those feeling
overwhelmed, being active, taking control and connecting with loved ones can be a welcome distraction, one that rests the brain and provides the time needed to return with a more controlled, confident mindset.
There are also many physical benefits of spending time with friends and family; older adults with larger social networks have good episodic memory, enhanced cognitive functions and a lower allostatic load, ensuring a better state of psychological wellbeing. Moreover, family activities involving sports or exercise keep everyone fit and healthy, and are especially good for a child’s development.
chill with the children
After work, homework and social media are the two biggest disruptors of family time. The rise of technology has brought people together – it’s never been easier to communicate with others around the world –but it has also made us less sociable, making it a big factor for the high levels of loneliness in the UK. Spending more time with family is not just beneficial for parents then, but also for the wellbeing of the next generation. In particular, spending time outdoors can establish deeper connections than time spent indoors, whilst sharing hobbies with your child can improve their self-esteem and promotes active communication.
For an unforgettable day out that is fun for the whole family, the PCA England Legends – Clover Dental Match is a cricket extravaganza for everyone. Presented by
Clover Dental Group, this cricket match pits an ex-England team against a talented pantheon of dentists. With an ideal date in the summer holidays – 22 August – the event also includes a Q&A with cricketing legends, great food and drink, a charity auction and a Bollywood Night, where music, dance and culture are whisked into one celebratory crescendo to mark the end of an action-packed day. For players, fans, non-fans and family, this is an excellent way of spending quality time together. By finding a better work-life split that incorporates quality time with family or loved ones, dental practitioners can be more motivated and more confident in their daily workflow. As a way of reducing stress and feeling supported, spending valuable time with family is as much a benefit for them as it is for you. exclusive: pca england Legends clover Dental Match 22 august 2025 Welbeck cricket club, Nottinghamshire
For more information on the events available from Clover Dental Group, please visit the https://cloverdentalfitout.co.uk or call 07961 669996 n
about the author Steve
Kettle, Director at clover Dental Fit Out.

None of us know what the future holds.
Having to take time off work because of an illness or injury can have a serious effect on your finances. This is where we come in – our income protection plans can help take away the worry by replacing the income you lose, until life gets back to normal.
For over a hundred years, our members have trusted us to give them peace of mind when they need it most. Isn’t it time you did the same?

To get a quote for an income protection plan please visit www.dentistsprovident.co.uk
To discuss a new plan just for you or review your current plan please contact our member services consultants on 020 7400 5710 or memberservices@dentistsprovident.co.uk
Protecting your lifestyle. Securing your future.
There are many reasons why patients’ oral health may suffer at any given time. The first and most obvious is poor oral hygiene, which is often neglected due to a lack of time or awareness regarding its importance. This can be exacerbated when the patient undergoes certain dental treatments, such as orthodontics, which create further challenges in achieving and maintaining a high standard of oral health. In order to optimise treatment outcomes and improve their oral health status, patients must fully appreciate their role in plaque control and oral health. For the dental team, this means successfully communicating the benefits of an effective at-home oral hygiene regime, as well as tailoring recommendations according to each individual’s needs and lifestyle preferences.
oral health education and knowledge retention
Although the need for dental hygiene may feel like a simple message to the dental profession, it is not yet a universal standard among the general public. In some cases, people lack the education to recognise what must be done, when and how. Health literacy remains an issue across the UK, with more than 40% of adults not fully understanding everyday health advice. This number increasing to around 60% when the health advice requires numeracy skills. Another issue is information retention. Research has shown that patients struggle to recall details provided to them during a dental appointment, particularly those regarding future dental health recommendations or agreed actions. This could significantly affect their compliance with oral health recommendations and have a detrimental impact on both their at-home routine and long-term oral hygiene. As such, it’s essential that the dental team considers these potential barriers and tailors their patient interactions accordingly. Information should be delivered in a way that each patient will understand. The use of visual aids or even video content has been shown to improve patient understanding of oral hygiene techniques and treatment procedures. Providing written instructions or diagrams for patients to take away with them can also help jog their memory and encourage their compliance at home.
Clinical and treatment considerations
Once a patient appreciates the importance of excellent oral hygiene, it’s necessary to think about clinical barriers that also need to be overcome. For example, malalignment of the teeth and malocclusion have been associated with a higher of dental caries. Periodontal disease is also more likely, because misaligned teeth make it more difficult to mechanically remove plaque from all surfaces.
However, the solution is more complex than simply aligning the teeth. For a start, orthodontic treatment can make oral hygiene even more difficult in the short-term. Clear aligners can harbour
a number of pathogens. One study found that bacterial count – especially of those species associated with dental caries, gingivitis, periodontitis and enamel demineralisation – increased on the aligners and in the patient’s saliva between 7 and 14 days of wear. The plaque biofilm also increased at 14 days, becoming more diverse and more pathogenic. This makes it vital for patients to frequently and adequately clean their aligners, removing bacterial biofilm and protecting their teeth and gums from problems.
When it comes to fixed appliances, food debris can get stuck between the brackets and wires, increasing biofilm formation and the risk of periodontal disease. The literature has found oral status to deteriorate in up to 60% of patients with fixed appliances. These can be a little more difficult to remove plaque from, often requiring patients to add a step to their daily oral hygiene routine to mechanically remove biofilm. This should be communicated at the outset of treatment so patients understand their responsibilities, but maintaining enthusiasm and compliance throughout an extensive course of treatment remains a challenge. Making the at-home routine as simple and as pleasant as possible is, therefore, a must. The introduction of a clinicallyproven solution like the Waterpik™ Ultra Professional water flosser can make a significant difference to these patients’ oral health before, during and after any type of orthodontic treatment. It’s part of a product portfolio that removes 99.9% of plaque from the treated area in just three seconds, with 10 pressure settings available for patients to customise their cleaning experience. With a dedicated Orthodontic Tip, the water flosser is also three times as effective as string floss for orthodontic patients.
Simple but essential
Orthodontic treatment remains a common solution for both children and adults across the UK who wish to enhance the function, cleansability and aesthetics of their teeth. However, it is crucial that they maintain good oral hygiene to achieve the best treatment outcomes. Despite the challenges that can be faced – whether undergoing treatment with clear aligners or fixed appliances – a few simple adjunctive oral hygiene steps can be all they need to help their smile really shine.
For more information on Waterpik water flosser products visit www.waterpik.co.uk. Waterpik products are available from Amazon, Costco UK, Argos, Boots and Tesco online and in stores across the UK and Ireland. n
about the author anne Symons is a Dental hygienist currently working in a specialist periodontal/ implant practice and also a busy NhS surgery. She has previously worked in a Max Fax unit, and also taught oral healthcare to staff in nursing and residential homes.


Sensitive teeth are very common, with an estimated 35% of UK adults affected, and similar numbers (34%) reflected worldwide. Dentine hypersensitivity (DH) presents as acute, sharp pain in otherwise healthy teeth in response to thermal (hot or cold), chemical (acidic, sweet, or salty), and mechanical stimuli (pressure or impact). With so many patients affected by DH, it can be helpful to discuss its causes with patients, and how best to overcome it, to help reduce their symptoms and prevent potentially harmful conditions from developing.
Causes and impacts
Sensitivity can occur in teeth which don’t have any other kind of defect or pathology, as such it is important to help patients understand what is causing their DH, and what triggers it. For example, loss of enamel due to attrition, abrasion, erosion, or abfraction can lead to sensitive teeth. For some patients, gingival recession may be the culprit, with abrasion from toothbrushing, surgical procedures, and preparing the tooth for a crown all potential causes. The facial surfaces are more commonly impacted by DH, with the canines and premolars affected in 25-30% of the adult population.
Biologically, what’s happening?
Naturally, the dentinal tubules are occluded by saliva which deposits calcium and phosphate ions into them. This plugs them and forms a protective layer. However, this process is slow and can be easily disturbed by acids in the diet, as well as mechanical removal through toothbrushing. Therefore, it does not provide lasting relief, and it is important to recommend that patients – particularly those who experience DH – supplement this process to reduce sensitivity. Because it is so freely available, toothpaste is a great way to make treatment for DH accessible. As such, much research has gone into creating new materials which deposit lost minerals in the exposed tubular endings, and help to mimic and restore the lost enamel structure.
treatment and prevention
Firstly, for patients who experience sensitivity, it is essential that they reduce any behaviours which may be contributing to enamel wear. This may mean cutting down on sugary and acidic foods and drinks, and switching to a softbristled toothbrush in an effort to reduce disruption to their natural dentinal tubule occlusion processes. Further to this, it
is also recommended that all patients –particularly those experiencing DH – use a high-quality toothpaste which contains the active ingredients needed to protect and replenish the minerals in their enamel. For some patients with more severe sensitivity, behavioural changes and the use of a desensitising toothpaste may not be enough. In these cases, it may be suitable to apply a fluoride varnish to affected areas, with composite bonding or dentine sealers also appropriate options for some patients.
the first line of defence Ideally, a desensitising toothpaste must not only reduce the dentine permeability, but also protect the dentinal tubules over a long period of time and resist the effects of acid. The consistent use of a specially designed sensitivity toothpaste should be the first line of defence for patients with DH, as they are relatively inexpensive compared to other treatment types, can drastically reduce symptoms of sensitivity, and are a non-invasive solution.
Its innovative formula makes BioMin F toothpaste the ideal solution for patients with sensitivity. The revolutionary bioactive glass is formed with extra-fine particles, which chemically bond to the tooth surface and slowly dissolve over 12 hours to release calcium, phosphate, and fluoride ions into the saliva. These ions crystalise to form a fluorapatite barrier over the tooth surface and within the dentinal tubules. As the bioactive glass continues to dissolve it offers the sustained release of minerals over 12 hours, for long term acid resistance. There are many different ways sensitivity may present, and some patients may have a more severe experience than others, so it’s important to offer patients tailored advice for them, depending on their needs. In many cases, recommending the consistent use of a desensitising toothpaste is the ideal way to tackle DH, without patients undergoing more involved treatment types.
For more information about BioMin, and their innovative range of toothpastes, please visit www.biomin.co.uk, or email marketing@biomin.co.uk.
Calling all dentists! Do you want samples or a practice visit? Speak to our UK dealers, Trycare on 01274 88 55 44 or email: dental@trycare.co.uk, or CTS on 01737 765400 or email: sales@cts-dental.com n
about the author alec hilton, Ceo at BioMin technologies ltd.





























Adental emergency could happen to any patient at any moment. Because of this, it’s important that you, your dental team, and your reception staff are aware of how best to assist and support patients in these scenarios.
In most cases of dental emergency, pain is a big factor. There are a number of things that might lead to dental pain, with causes including tooth decay, a dental abscess or other infection, a cracked tooth, a broken or loose filling, gingivitis, or bruxism.
When patients are experiencing a dental emergency, it is often recommended that they phone 111 to seek advice and help them find their nearest emergency dentist. However, it may take some time to get an appointment, perhaps waiting until the following day. As such, it’s important that the dental team can offer guidance about how to manage their pain in the meantime.
What constitutes a dental emergency
It is important that the dental team understands what qualifies as a dental emergency, to enable them to most effectively help patients get the treatment and potentially urgent appointments they may need.
There are a number of complaints that might constitute a dental emergency including heavy bleeding that doesn’t stop,

severe distracting tooth pain, swelling or infection, or a knocked-out tooth. It is important that patients are aware that they should contact an emergency dentist if they are experiencing these symptoms. Sometimes, dental problems are not considered emergencies, but should still be prioritised over routine care. For example, usually a cracked or chipped tooth isn’t considered a dental emergency, as well as toothache if it isn’t causing severe pain.
A missing crown or filling may also not be considered a dental emergency, however, dentists should aim to see these patients as a priority. This is not to say that patients shouldn’t contact their dental practice in these scenarios, but they may have to wait slightly longer for care.
Ultimately, toothache can have a wide range of causes – so it is essential that
patients receive care quickly to ensure the problem is treated.
Managing patients in pain & distress
With any painful dental issue, waiting for a dental appointment (no matter how quickly they can be seen) can feel like an eternity. As such, when talking to patients over the phone, it can be helpful to recommend ways that they can manage their pain in the meantime.
Some common recommendations for relieving dental pain include taking painkillers like ibuprofen or paracetamol, using a pain-relieving topical gel for the mouth, rinsing the mouth with salt water if an infection is suspected, eating only soft foods and avoiding chewing with the sore tooth, and using a soft toothbrush to clean the teeth, avoiding flossing or hard-bristled toothbrushes in the affected area.
Whilst these methods will not treat the source of the pain, they will help patients to soothe their discomfort while they wait for their dental appointment.
Before they get to the practice
Because it may be a number of hours or even days before a patient can attend an emergency appointment/before one can be made available, dental practices should recommend the use of Orajel to ease their discomfort.
In March, we celebrate No Smoking Day. It’s an important reminder for the almost 12% of UK adults who admit to smoking cigarettes regularly, that cessation is beneficial and possible. For the dental team, it also provides an opportunity to talk to patients about the impact their lifestyle choice can have on their systemic, oral and mental health.
a physical problem
It’s no secret that smoking cessation is essential for improved health. The habit is associated with an array of negative health effects and is cited in the literature as a significant risk factor for various chronic illnesses. Respiratory conditions are high on the risk list for smokers, with many of these illnesses made worse by a smoking habit. The cardiovascular and reproductive systems are also adversely affected, with some effects possible even from passive or second-hand smoke where exposure is high enough. In addition, smoking cigarettes has been shown to hinder the body’s immune system, enhancing the inflammatory response and increasing the risk of conditions like multiple sclerosis. Smoking tobacco also the largest avoidable risk factor for cancer, responsible for 15% of all cancer cases and up to 28% of all cancer deaths in the UK. When it comes to oral health, cigarette smoking is no better. There is an extensive body of evidence to show an increased risk of dental caries, periodontal pocketing, tooth mobility, oral lesions, and tooth loss. What’s more, the lifestyle choice can impact
a patient’s suitability of dental treatment because outcomes may be compromised.
For example, research shows that dental implants placed in smokers have an up to 140% higher risk of failure than implants placed in non-smokers. There is also evidence to suggest that smoking can delay healing of apical periodontitis after endodontic treatment.
However, smoking does not only have physical impacts on the body. It can also negatively affect mental health. A systematic review from 2014 found psychological quality of life to significantly increase in those who quit smoking, with improved positive mood and reduced stress also described.
A study published in 2023 supported this sentiment, reporting that smoking cessation for at least 15 weeks was associated with enhanced mental health outcomes. This was true for participants both with and without existing psychiatric disorders, in particular, leading to lower depression and anxiety scores six months after stopping.
There are various smoking cessation interventions available to people today. These consist of pharmacological therapy (including nicotine replacement therapy), behavioural therapy and a combination of the all the above. Smokers will often find different solutions useful, depending on their personal preferences and experiences. Not surprisingly, research has suggested that combination therapy may offer
the best option, with pharmacological and behavioural support leading to a success rate of approximately 24% after 12 months.
Of course, for any of these to work, it is crucial that individuals are sufficiently educated and motivated to remain dedicated to the cause. To this end, governments around the globe have invested substantially in educating their populations about the dangers of smoking and encouraging them to quit in recent years. Research into what has worked best shows that people are more likely to consider cessation after seeing these campaigns and general related health warnings. Tax increases have also been linked with a higher likelihood of individuals trying to kick the habit.
I was also interested to come across research about gradual versus immediate quitting. Although we hear that cutting down the cigarettes is better than doing nothing at all, the research actually suggests that going cold turkey is far more successful for most people in the long-term. Smokers, therefore, must be sufficiently prepared if they are to really quit.
The dental team also have an important role to play in helping patients to kick the habit for good. We likely see them more often than their GP and we are well-versed in discussing such topics with different people in a positive and non-judgemental manner. It is also common practice for dental practitioners to ask about smoking habits as part of our continuously updated patient histories, so we
Orajel Dental Gel offers rapid toothache relief where it is needed the most. The topical gel contains 10% benzocaine to reduce pain in a broken tooth, or tooth with a cavity, for example. Benzocaine temporarily blocks pain signals along the nerves, and numbs the problem area quickly. For patients in acute dental pain, Orajel Extra Strength features the maximum concentration (20%) of benzocaine to deliver a powerful local anaesthetic in a patient’s time of need. Patients can use Orajel up to four times a day, enabling them to manage their pain at home whilst they wait for an emergency appointment. In order to avoid toothache, recommend that patients attend the practice regularly and maintain a good oral hygiene routine. However, when a dental emergency does strike, ensure that your dental team is able to offer patients the care and advice they need to manage their pain before their appointment.
For more information, and to see the full range of Orajel products, please visit https://www.orajel.co.uk/ n

always know (as far as they tell us) what each patient’s smoking status is.
From here, the Very Brief Advice on Smoking (VBA) from the National Centre for Smoking Cessation and Training (NCSCT) can be helpful for all team members. This provides simple yet useful information to be used opportunistically in under 30 seconds when speaking to a current smoker. It offers a two-step pathway to establish whether a smoker is open to cessation and if it is an advantageous moment to signpost them towards support.
Aside from the initial motivation to quit, the dental team can also help individuals during their cessation journey. Social support has been proven to help people stay away from the cigarettes, and a little extra encouragement from the dental team certainly can’t hurt!
At the end of the day, smoking remains a harmful practise for anyone of any age or gender to partake in. For those ready to quit, they are embarking on a journey to a healthier version of themselves and that must always be commended.
For further information about the endodontic referral services available from EndoCare, please call 020 7224 0999 or visit www.endocare.co.uk n
about the author endoCare, led by Dr Michael Sultan, is one of the UK’s most trusted Specialist endodontist practices.

In the UK, some level of irreversible periodontitis affects almost half of all adults. Its high prevalence and association with over 50 systemic inflammatory disorders and comorbidities makes it an essential disease to combat. One promising area for tackling periodontitis and its symptoms is in immunotherapy. Recent studies have sought to deliver immune-modulating compounds to reduce symptoms of the oral disease, such as bone loss, and ultimately prevent it. Whilst the research continues gaining traction, dental practitioners that understand the role of the immune system can broaden the ways they can help patients affected by periodontitis.
The symptoms of periodontitis are numerous and well known: bleeding gingivae, swollen gingivae, halitosis and loosened teeth. For 70-80% of patients with periodontitis, regular hygiene appointments with a dental professional can reduce the symptoms and prevent disease development, but, when left unchecked, periodontitis can also trigger resorption in the alveolar bone. This occurs when harmful bacteria in the oral cavity activates the body’s immune system, sending white blood cells streaming into the affected area and causing inflammation. Chronic inflammation leads to the progressive destruction of the gingival connective tissue and collagen, causing bone loss. A reduction in the alveolar bone can have a serious dental impact, weakening the supporting
structures of the teeth and leading to tooth loss. This contributes to many health and wellness issues, such as:
• Changed facial aesthetics
• Increased patient self-consciousness in social situations
• Limited mastication and malnutrition
• Lowered quality of life, which may lead to low self-esteem and depression
The lack of successful therapy towards alveolar bone loss demands a solution, and immunotherapy is showing potential as an answer. For studying the interactions between microbes and the immune system, the oral cavity is more accessible than the gut and lungs and can provide more answers.
A recent study discerned that delivering immune-modulating microparticles directly to the gingivae inhibited bone loss and accelerated bone repair. By harnessing the immune system, the composition of bacteria can be shifted, reducing its harmful effects and preventing periodontal disease.
iii To do this, macrophages must be utilised.
Managing macrophages
Macrophages, the white blood cells that kill microorganisms, are crucial for preventing alveolar bone loss: macrophage levels rise from 1.4 to 20.9% in unhealthy periodontal tissue. There are two key types: M1 and M2. The former is activated by pathogen invasion to defend the body and are inflammatory, aggravating periodontitis and promoting bone loss. M2 is antiinflammatory and is integral for wound healing and tissue repair. By treating M1
A universal, dual-cure composite that can be used to fill any size cavity preparation, all the way up to the occlusal surface, without any need for additional layering. Ideal for posterior restoration.
Predicta® Bioactive Bulk releases calcium and phosphate ions and releases and recharges fluoride ions to stimulate mineral apatite formation and remineralization at the material-tooth interface.
T Unlimited depth of cure
T Two slightly fluorescent shades for a natural appearance
T Strong and durable to withstand occlusal forces
T Highly polishable & radiopaque
T Nanohybrid
Predictable results for any size cavities!



white blood cells with the cytokine CCL2, they can be shifted to become M2 type. Or, theoretically, M2 injections into periodontal tissue could suppress osteoclast activity. When paired with a consistent oral hygiene routine, an increase in anti-inflammatory activity can prevent bone loss and treat periodontitis.
As research into immunotherapy as a treatment for periodontitis continues, practitioners can get ahead by recommending ways of increasing M2 secretion to their patients. Diet is one key way to do this – Vitamins A and D control macrophage functions. Enjoying a diet rich in Vitamin A foods, such as carrots, watermelons, chicken, beef and butter, is vital for many health benefits, as a deficiency in Vitamin A can lead to a systemic proinflammatory state. Similarly, Vitamin D foods – oily fish, red meat, egg yolks, breakfast cereals – suppress the production of proinflammatory cytokines. In the non-summer months or for patients who do not see much sunlight, it is harder for the body to get Vitamin D, so these food types or supplements can provide all-round health benefits. Inflammatory foods, such as processed meats or carbonated drinks, should be avoided to reduce M1 prevalence in the oral cavity.
Along with a balanced, anti-inflammatory diet, practitioners must recommend daily interdental cleaning to patients at-risk of

periodontitis. To help achieve a superb standard of oral hygiene, recommend the FLEXI range of interdental brush from TANDEX. 11 different sizes ensure patients are able to reach all the areas where a traditional toothbrush struggles, cleaning the hidden tooth surfaces and massaging the gingivae. When used with the PREVENT Gel, from TANDEX, interdental cleaning gets an antibacterial boost for maximum protection against periodontitis. Chronic periodontitis is a major disruptor in a patient’s quality of life. Loss of the alveolar bone can be devastating, and immunotherapy may be a future solution to preventing this. Until then, practitioners can aid vulnerable patients by encouraging anti-inflammatory diets and maintaining a consistent oral hygiene routine.
For more information on Tandex’s range of products, visit https://tandex.dk/ Our products are also available from CTS Dental Supplies: www.cts-dental.com
About the author Jacob Watwood on behalf of Tandex.


Visit us at BDIA, Booth E20 or scan the QR code for further information and an exclusive trial offer.
“Our dental practice is growing more and more delighted with Predicta Bulk. I think Parkell came up with an excellent product. We like that it is chemically cured, you know it cures all the way even if you use a thick layer. Other bulk materials have a limited depth of cure. The colour match is surprisingly good, I didn’t expect that. “
Manouchehr Kiaei, DDS - Sweden
”Predicta Bioactive Bulk is a unique restorative material. There is no need for occlusal layering or adding a different composite on top of the restoration. I love the ease with which I can make large restorations; it’s a time saver! The initial chemical curing process is short, but not too short. My patients experience no postoperative pain. The restorations polish well and still look like new after several years.”
Sjobbe Besseling, DDS, Netherlands


Arthritis is a condition that causes pain and swelling in the joints. It is widespread, with 10 million people in the UK diagnosed with osteoarthritis, 450,000 adults diagnosed with rheumatoid arthritis (RA), and 190,000 adults estimated to have psoriatic arthritis (PsA). This high prevalence shows the need for a greater understanding of the disease.
The temporomandibular joint (TMJ) is the most used and complex joint in the human body, utilising a hinge and sliding movement that, if changed, can inhibit a patient’s ability to speak and eat. Arthritis can cause that change, leading to pain and discomfort that impacts quality of life if untreated. For dental practitioners, identifying at-risk patients for TMJ arthritis and finding solutions for them can restore function to the jaw and preserve their oral health.
osteoarthritis
Osteoarthritis is the arthritis type that most commonly affects the TMJ. The process, which becomes an increasing likelihood with age, particularly for those aged over 50, is characterised as the destruction of soft and hard tissue around the joint. This abrasion of the cartilage leads to the changing of the shape and function of the jaw, such as reducing an overbite or increasing an overjet.
TMJ osteoarthritis can be the result of physical factors like disc dislocation, trauma, developmental anomalies or overuse, as well as more systemic risk factors such as autoimmune diseases, gender, and age. Wearing down the cartilage in the joints from clenching and grinding also sets the stage for arthritis to develop, putting bruxism patients at risk. Those with osteoarthritis in the TMJ may feel a stiffness or tenderness in the joint region, pain when opening the mouth, and grating sounds when moving the jaw.
Osteoarthritis, be that in the TMJ or in the hands, can impact the daily oral hygiene routine by limiting access. Difficulty opening the jaw can make brushing and interdental cleaning a hardship, whilst arthritic joints in the hand can also inhibit the mobility needed for an effective routine. The risk of developing periodontitis or caries is therefore higher for patients who may struggle to maintain a consistent oral hygiene routine.
other arthritic diseases
Whilst osteoarthritis is the most prevalent form of arthritis, RA and PsA are also linked with temporomandibular disorders
(TMDs). RA attacks the cells that line the joints, leading to inflammation. It is more prevalent in women, those with a family history and smokers. Of those with RA, 17% had pain and swelling in the TMJ, though this is among the last joints effected by the disease.
RA is associated with periodontal disease, as bacterial growth in the oral cavity causes inflammation and tissue damage. At considerable risk of periodontal disease are the collagen-rich tissues around the joints; collagen is a protein used in tissue repair, immune response and cellular communication, meaning its decline or absence can magnify RA on joints like the TMJ. The interconnected nature of periodontal disease and RA means that practitioners must educate patients and provide solutions that promote an effective oral hygiene routine and/or stop the development of RA.
Psoriasis is a chronic skin condition that effects over a million people in the UK. Of that figure, 20% develop PsA which can affect the TMJ. Whilst patients with psoriasis are just as likely to have a TMD as those without it, the symptoms of a TMD are worse for those with psoriasis due to the development of fibrosis that greater limits the jaw movement. Patients with psoriasis can therefore face a more uncomfortable experience, prompting the need for treatment.
an answer to arthritis
Many TMDs caused by arthritis can be alleviated at home, as directed by a professional. Physical therapy can help, and the OraStretch® Press Jaw Rehab System from Total TMJ is an effective, user-operated device for treating TMD.
Squeezing the handles moves the mouthpieces apart up to 50mm wide, stretching the tissues and keeping the joint active. The variety in exercises that can be done with the device work to strengthen the muscles and mobilise the jaw, allowing the OraStretch® Press to help restore TMJ function so that patients can talk and eat with greater comfort.
Arthritis can change how people live each day. By identifying patients who may be at risk for arthritis in the TMJ, practitioners can guide them to solutions that can preserve their quality of life.
For more details about Total TMJ and the products available, please visit totaltmj.co.uk/products/orastretch/ n
about the author
Founded in 2018 by Phil Silver, total tMJ is a specialist provider of medical devices.
With heightened concerns about job security, the costof-living crisis, international conflict and climate change, it is unsurprising that anxiety is gripping the UK. 60% of individuals experience at least mild symptoms of anxiety, and 76% experience moderate to high levels of stress.
For dental practitioners, awareness and understanding of the growing prevalence of anxiety and stress is essential because of the oral health impacts it can have: 70% of bruxism occurs because of anxiety or stress. A major concern is that patients may overlook bruxism as a significant problem because they could be unaware that they are doing it – global sleep bruxism prevalence is 21%. As bruxism can damage the teeth and any restorations, dental practitioners should identify and help affected patients to reduce their anxiety or stress-induced bruxism.
anxiety and stress
Anxiety and stress are similar but different. Anxiety is a feeling of apprehension, even dread, for situations that may have no actual threat and is disproportionate to the situation faced. Stress is a condition or feeling that is experienced when a person believes that they do not have the available resources to meet the demands. Unlike stress, anxiety persists even after the event or situation has passed.
It has also been observed that men have higher job stressii whilst anxiety is more common in women. Both anxiety and stress can be detrimental to sleep; with medications disrupting how well a patient falls asleep and then stays asleep. An unrelaxed body is also likely to lead to sleep bruxism.
With the winter months comes a shift in mood, with seasonal depression and the worry of costs leading to anxiety and stress. These expenses include the very high costs of heating the home, purchasing Christmas gifts and, for parents, spending to entertain their children over the holidays. This is why 40% of UK residents believe that financial security would help prevent anxiety. As such, tooth grinding is more common in the winter months. Dental practitioners may be able to identify at-risk patients by both an inspection of the teeth and an understanding of the current circumstances, for instance if they have a stressful job.

For practitioners, identifying, educating and treating adolescent patients with anxiety and bruxism can be a challenge. It seems unreasonable to expect anxious teenagers to be honest about their worries to a dentist, and it may seem unreasonable to a teenager that a dentist is asking. Moreover, informing anxious patients of tooth wear can give them something more to worry over, potentially worsening the problem. A friendly, warming dental practice with posters or brochures about anxiety can help affected patients feel more comfortable and confident when dealing with it.

Patients with notable signs of bruxism – wear and early cracks on the outer layer of the tooth – should be asked if they are aware of grinding their teeth in the day. If they are not, a follow-up question could ask about any stress around work, school or other life events that could explain sleep bruxism. For patients who admit anxiety and stress, recommend that they find ways to relax before going to sleep, such as breathing exercises or listening to music. Keeping a regular bedtime and unwinding beforehand can improve sleep quality and reduce teeth grinding.
repairing the damage
Whilst adults are prone to teeth grinding, prevalence of sleep bruxism is at its highest in adolescents, with 15% found to grind their teeth at night. This number declines with age. Adolescents, the period from 10-19 years old, have many reasons to be anxious or stressed. These could be concerns about their academic performance, how people perceive their image at a new school, college or university, being bullied, or concern about pubescent changes in their body. Along with other risk factors, such as irregular sleeping patterns, drinking alcohol and substance abuse, these anxieties can cause sleep bruxism.
For some patients, bruxism may have already damaged their teeth, requiring restorative work and a reliable composite bloc. BRILLIANT Crios from COLTENE is an ideal solution for single-tooth restorations in both the anterior and posterior regions. Available in three translucencies and 15 shades, the reinforced composite bloc has superb mechanical properties for a natural bite Its high flexural strength gives restorations a sturdy resistance, helping minimise the damage of any future teeth grinding. Anxiety and stress are often experienced together, even though they are different. As the leading cause for bruxism, highlighting the impact anxiety and stress can have on the oral health of at-risk patients is crucial. Together, practitioners and patients can loosen the chokehold that anxiety and stress may have over their health. For more on COLTENE, visit coltene.com, email info.uk@coltene.com or call 0800 254 5115.n
about the author Nicolas Coomber, ColteNe National account & Marketing Manager.

































EthOss® is a 100% synthetic bone graft material for dental implant surgery. With no risk of cross-contamination, EthOss® works with the body’s healing process by creating a calciumrich environment and is completely absorbed.

























Paediatric dentistry requires an abundance of extra qualities from the clinician on top of the typical clinical skills needed to treat adults. Patients can be half the size and twice as difficult to manage in the dental chair, meaning delivering care can sometimes be a challenge.
There are many aspects that will be similar to general dental care. Oral hygiene advice will need to be given, periodontal health will need to be assessed, and radiographs may be required. What is obvious, however, is each aspect will need to be amended slightly for the patient in question. Communication is an obvious example; there are a variety of approaches that can be taken for typical dental procedures in children. These include the tell-show-do method to make patients comfortable with the practice, or the ask-tellask approach which can give better insights on the paediatric patient’s anxieties.
Radiography, however, creates new questions for practitioners and the carers of paediatric patients alike. Understanding how radiographic approaches may need to change is essential to ensure patients are safe and treated to a high standard.

radiographic exposure for the paediatric patient
Radiography has been refined to a safe art in modern healthcare, and offers professionals insights into the health of bones and organs at the cost of minimal radiation exposure. The average person in the UK is estimated to be subjected to about 2.7 millisieverts (mSv) of background radiation a year. The average radiation dose for a panoramic radiograph is just 0.007 mSv, equating to around a day’s extra exposure. For paediatric patients, this means that a typical exam will be safe, and not present a great risk of adverse outcomes.
However, do not take this to mean that professionals can become complacent and request a young patient undergoes a radiograph without good measure. Over time, repeated exposure to radiation increases the probability of stochastic damage, and so the development of an adverse outcome – for example, a tumour – is possible with frequent radiograph use. Note that children have an increased radiosensitivity when compared to adults.
The European Academy of Paediatric Dentistry recognises this, and reinforces the need to optimise radiographs that limit exposure whilst obtaining the minimum quality image necessary to inform treatment. This is, in effect, the same as the ALARP principle, meaning ‘as low as reasonably possible’, that is also laid out in the guidance issued by UK regulatory bodies.
Two key aspects of the ALARP principle include the justification and optimisation of a radiographic exposure.
Firstly, one must ask if it is necessary –could the information displayed change a treatment plan and help find a new solution to an oral health problem? And secondly, what is the best way to take the radiograph in each instance, with the minimum possible radiation exposure, whilst ensuring the clinician has all of the information needed to make a confident assessment?
A paediatric patient may require a radiograph for a variety of justifiable reasons.
The WHO Global Oral Health Status Report from 2022 estimated that 514 million children have caries in their deciduous teeth, and a further 2 billion people have caries in their permanent teeth – the latter will likely include paediatric patients. Assessing the extent of a carious lesion is vital when choosing the best care for a patient, and may justify a radiograph. This can minimise overtreatment, essential particularly in the primary dentition.
Dental trauma is a problem that mostly affects younger patients – 80% of cases occur in those under 20 years old – and also may require a radiograph to judge the extent of an injury. This can ensure any problems caused by the trauma are recognised and treated before they develop further.
Optimising a radiograph for a paediatric patient is a challenge in itself. Children are much more likely to move during a CBCT examination, which may indicate the need for radiographs with a single exposure where at all possible. If a patient does move, but the scan is still diagnostically acceptable, it should not be retaken.
Choosing a solution that is comfortable for the patient, and reliably provides a highquality diagnostic image is key to delivering a successful result. The CS 7200 Neo Edition imaging plate system from Carestream Dental can be ideal for many clinicians, delivering high-resolution images in just 8 seconds.
The three plate sizes available mean you can choose the optimal solution for your patient, whether they are a child, adult, or somewhere in between, and can help create high quality periapical, bitewing and paediatric images.
Radiography is an essential element of paediatric dentistry that must be managed safely to protect patients and deliver high quality results. In turn, clinicians can support young individuals get the care they need in a timely and appropriate manner.
For more information on Carestream Dental visit www.carestreamdental.co.uk
For the latest news and updates, follow us on Facebook and Instagram @carestreamdental.uk n
about the author
nimisha nariapara is the trade marketing manager at Carestream Dental covering the UK, middle east, nordics, South africa, russia and CIS regions.

When patients present with urgent endodontic problems, coming up with an accurate diagnosis is not always a straightforward process. Whether you are faced with a distressed patient with toothache or an asymptomatic patient presenting with vague symptoms, it is important to have a systematic approach to arriving at a final diagnosis.
Symptoms and clinical assessment
To begin, it is important to empathise and establish trust. Open questions are essential to allow the patient to share their complaint and to procure an accurate history (as well as get an indication of the patient’s attitude towards dental treatment). A popular mnemonic used by clinicians to gain a precise pain history is ‘SOCRATES’; site, onset, character, radiation, associations, time, exacerbating/relieving factors and severity. Any cases with a history of trauma will require more information regarding the time, date, location, loss of consciousness, medical history and any emergency treatment carried out. Extraoral examination will identify any facial asymmetry or swelling, and the patient’s general condition including fever, difficulty swallowing, difficulty breathing or malaise could point to spreading infection. Clinicians must be aware of cases which require hospital referral. Intraoral examination will identify the possible dental cause of the presenting complaint. Soft and hard tissue assessment will benefit from the use of good lighting and magnification.
Special tests for suspected endodontically affected teeth
When the teeth are potentially endodontically affected, there are a number of initial tests that may be used to identify the affected tooth/teeth, and indicate the diagnosis.
Thermal testing should be carried out with a cold (refrigerant spray) or hot (warm water, heated probe or heated gutta percha stick) stimulus first to a ‘control’ tooth located far from the suspect area to establish a baseline, and then to the suspected tooth. The responses from all the areas tested should be recorded (including lack of response) to help inform later diagnosis and severity.
Another widely used test is the electric pulp test. This uses a probe which applies an electrical stimulus to a tooth at varying intensities, and gives a digital reading which can help inform pulp vitality. It should be noted, however, that electric pulp tests are accurate when testing vital teeth, but not when testing non-vital teeth.
When it is difficult to locate the source of the pain, selective anaesthetic testing may also be appropriate. This is a diagnostic test that aims to localise the source of pain by progressively excluding areas of the dentition until the suspect tooth is found. For example, if the pain is poorly located between the upper and lower jaw, selective anaesthetic testing may be carried out to localise the source.
When carrying out these tests, there are a few things to consider. Clinicians must ensure that the stimuli mentioned above are applied to sound, and dry tooth structure along with isolation and that they avoid contact with restorations for the most accurate outcome. Additionally, an optimal response can be achieved when the stimulus is applied to the thinnest enamel area, or exposed dentine.
To ensure an accurate diagnosis, radiographic imaging must be used when justified following clinical examinations and special testing. This is in line with the ALARA principles, to ensure patients receive lower doses of radiation. As such, a conventional periapical radiograph should be taken first to assess for periapical pathology. If there is insufficient information gleaned from this, 3-dimensional imaging (Cone Beam CT) can be considered.
never stop learning
All clinicians will be involved in the diagnosis of endodontically affected teeth; therefore it is essential to keep up to date with the latest developments in the field, and solidify your understanding. By becoming a member of the British Endodontic Society (BES) clinicians join a group of likeminded dentists with an interest in endodontics, and a commitment to providing excellent treatment and furthering their knowledge. The BES values education, running a number of useful events for clinicians at all stages of their careers including the Spring Scientific Meeting, Regional Meeting, and Early Career Group Meeting, along with workshops aimed to help members expand their knowledge. The BES has also published its Guide to Good Endodontic Practice, to ensure the clinicians have a reliable document to refer back to when making decisions. Utilising all of the information gathered through clinical assessment, special testing, and radiographic imaging, clinicians are able to effectively form an accurate diagnosis and treatment plan accordingly. For more information about the BES, or to join, please visit www.britishendodonticsociety.org.uk or call 07762945847 n
Orthodontic care is a cornerstone in modern dentistry and is often paramount to the development of the adolescent patient.
Wearing braces and clear aligners is a rite of passage of sorts, with teenage orthodontics permeating popular media in all forms, as well as being seen on peers in everyday life. Because of this, teenage patients may have preconceived notions about the treatment and what the experience will be like for them.
Attempting to understand how adolescents feel about orthodontic treatment is the first step to enhancing care for this set of patients. Then, by taking the time to improve dedicated aspects of care, teenagers can have a better experience with orthodontic appliances.
Adolescent attitudes
Patients seek orthodontic care for a variety of reasons. Adolescents – who are of an age where they do not have full agency over their healthcare, but treatment can be on their mind – may seek it out themselves, or be prompted by a parent or clinician.
Expected treatment results are commonly an improved dental appearance, coinciding with increased dental confidence and a positive psychological impact, such as improved self-worth.
However, teenage patients often anticipate that the experience of fixed orthodontics, in particular, will cause pain and discomfort. Despite this relative torment, which occurs to such an extent that eating, sleeping and






hobbies can be affected, teenagers will typically tolerate and accept it in promise of the outcomes. Eventually, the presence of a brace or aligner becomes a new normal, with acceptance supported by the development of visible and measurable results.
Make the most of moments
The majority of orthodontic treatment takes place outside of the dental practice, with fixed appliances or compliant use of clear aligners producing good results. This being said, some of the most important and memorable aspects of care come in the dental chair, when patient and clinician can lay out problems and solutions, and discuss the next steps for an individual’s smile.
The literature notes that a devotion to communication at every point of treatment can better influence patient motivation and compliance, and that average communication, which fuels an average therapeutic relationship, is at the whim of a slight misunderstanding or incident. If an issue occurs and is not resolved effectively, the patient could lose trust in the clinician, and see results suffer through non-compliance.



































Practitioners should look to teenage patients and enquire about their desires for treatment. These can be led by intense emotional factors relating to their appearance, and what it means for their social acceptance, or the dysfunction of their dentition. With the patient given time to speak, practitioners can then deliver open ended questions that narrow down the specific elements needed to inform, reassure, and treat a patient.
Pairing all of this with positive reinforcement, teenage patients can enter a ‘therapeutic contract’ with a clinician, which can be a key element to maintain motivation over the duration of a long orthodontic treatment timeline. Motivation is strongly associated with treatment cooperation, meaning successful communication is imperative.
It’s essential that clinicians maximise the comfort of the orthodontic care they deliver to teenagers. This requires recognising potentially uncomfortable or painful elements of care that clinicians can support patients through.
Dental professionals can trace discomfort to long before an orthodontic appliance is placed or provided. Conventional impressions, necessary for treatment planning, can sometimes induce an uncomfortable gag reflex, whereas digital scans may be unfavourable due to the scanner size and the potential for excessive heat. Clinicians can work with patients to find the best approach for each individual.
As treatment begins, the appliance can be notoriously painful for some adolescents. Whilst patients do anticipate this issue, it doesn’t overcome the challenge it presents in the moment. Fixed appliances can be particularly challenging, as patients feel they have little respite from brackets and wires – but clinicians can have a solution at hand that maintains confidence in the process.
The Orthodontic Relief Wax from Kemdent is a soft gum protector for patients with braces that can alleviate pain in moments. Adolescent patients can keep the Ortho Relief Wax on them at all times with the 100% recyclable tins, before warming a small portion of wax in their hands, and applying it to the irritable site when needed. The wax simply flakes away or peels off and breaks down – it’s ideal before meals or oral hygiene routines.
Teenage patients are a large portion of the orthodontic patient base and understanding their views of treatment, and how care can be improved, is key. By choosing appropriate communication techniques and clinical materials, each appointment can be optimised for both clinician and patient. For more information about the leading solutions available from Kemdent, please visit www.kemdent.co.uk or call 01793 770 256
About the author Alistair Mayoh, Marketing Director, Kemdent.



































































For many modern oral health treatments, it’s possible to deliver successful results quickly. A filling may be placed to repair a carious lesion in just a few minutes, before the patient continues their day mostly unimpacted.
When it comes to dental implants, this can be more difficult. An invasive treatment, clinicians must manage soft and hard tissue, surrounding dentition, and the restoration for success. Conventionally, a delayed placement procedure will see an implant and restoration be provided over the course of months, but immediate implant dentistry has turned this on its head.
There are many cases where the extraction of a tooth and the placement and loading of an implant can now be completed in one sitting. It’s important that clinicians keep up with the latest findings concerning immediate implant placement. The literature and effective educational courses should be used as sources of support when looking to implement such a procedure into their practice.
a viable solution
The first question that clinicians must ask is how viable is the immediate implant procedure in 2025? Recent reviews of the literature note that it is typically extremely successful, even in comparison to a conventionally delayed placement.
A 2022 retrospective study on 4519 implants found that 98.5% of implants placed immediately following extraction survived, which was comparable to the 98.9% success rate of those placed in healed sockets. A similar 2023 systematic review declared no significant statistical difference in implant survival or complications between either approach but noted that case selection is important.
Immediate implant placement can be used alongside effective socket preservation techniques, creating a clinically advantageous approach for some patients. For a clinician to consider any implant placement, one must be confident that there is sufficient bone surrounding the extraction socket. This tissue begins to resorb immediately upon extraction, which is at odds with the healing period associated with a delayed protocol. The result may be that the conditions at implant placement are no longer ideal if waiting months postextraction for restorative surgery.
The placement of an implant immediately into the socket can reduce bone resorption, though this is typically most effective in conjunction with graft materials. A 2022 systemic review found that when compared to conventional alveolar ridge preservation, immediate implants had a lower success rate (in this sample of 915 cases, survival rates were 98.68% against 95.21%). However, hard and soft tissue analysis found no significant difference in preservation, aesthetic outcome, and patient satisfaction. This suggests that where success can be maximised, the approach is appropriate when targeting improved socket preservation and an accelerated final treatment outcome.
Clinicians must be aware of the treatment aspects that mean immediate implant protocols are not optimal in all clinical situations. Current clinical recommendations include the need for a strict criteria when placing immediate implants. This means that dental professionals must not only prioritise survival rates, but the possibility of avoiding aesthetic, biological, mechanical and technical complications. Studies routinely use connective tissue grafting in conjunction with immediate implant placement, improving soft tissue results in a number of cases. A study into immediate implant placement in the maxillary aesthetic zone cited such complications as a thin facial bone, thin soft tissue phenotype, and minor gingival recession.
Contraindications to immediate implant placement may include extensive gingival recession, obvious inadequacies in bone height or width, limited restorative space (for example, if a patient has a deep bite), adverse nerve location, and class III and IV sagittal root positions.
Broaden your horizons
To be able to deliver clinical success with immediate implant placement, clinicians must use what we know about current abilities and contraindications of the treatment, optimising case selection. The coming years may present new grafting solutions to use in conjunction with the protocol, or new approaches to utilise.
No matter the case, it is essential to delve into up-to-date education whenever possible. Clinicians could find out more about immediate implant placement protocols with the Postgraduate Diploma in Implant Dentistry from One to One Implant Education. The course, led by One to One founder Dr Fazeela Khan-Osborne and Dr Nikolas Vourakis, delves into immediate implant placement and loading techniques, as well as clinical aspects such as full arch implant dentistry, bone grafting, and peri-implantitis management. It is the ideal course for clinicians looking to pave their way in the field.
As of today, immediate implant placement is an effective and widely applicable treatment protocol. Whilst it is not suitable for every indication of edentulism, clinicians should keep note of the progress made in the coming years to understand how it can be implemented for aesthetic, functional and overall successful results.
To reserve your place or to find out more, visit https://121implanteducation.co.uk or call 020 7486 0000. n
about the authors
Dr Fazeela KhanOsborne, Principal Implant and restorative Surgeon.
Dr nikolas Vourakis, Senior Implant and restorative Surgeon in private clinics in London and edinburgh.
While implant treatment has become an increasingly predictable treatment for edentulism in patients with all bone types, several key principles are essential in preventing complications. These include careful patient selection, the management of environmental and systemic factors, and the formulation of a precise surgical strategy. Prosthetic planning is also increasingly recognised as a fundamental component.
The prosthetically driven implant restoration treatment plan incorporates several advancements in implantology, including digital technology, bone grafting materials, guided bone regeneration (GBR), all aimed at prioritising the desired prosthetic outcome. The determination of the final functional and aesthetic results informs implant planning in terms of length, position, angle, and depth, as well as decisions about bone and soft tissue augmentation and management.
Within this plan, the provisional implant restoration provides clinicians with greater control in designing gingival contours around the final restoration. A precise approach to soft tissue planning and management afforded by provisionals offers both aesthetic and clinical benefits, enhancing the overall outcome of treatment.
Soft tissue management and provisional restorations
Provisional restorations have a variety of purposes in implant dentistry. They act as a temporary, functional replica of the final restoration. They can improve patient comfort, aesthetics and function during the treatment process, while maintaining the position of adjacent or opposing teeth. They are also an important tool to shape and condition the soft tissue around the newly placed implant, allowing the dentist to encourage the desired emergence profile before placing the final restoration.
A properly shaped emergence profile is important in implant treatment. It protects the implant-restoration complex from peri-implant infections, enables the patient to perform optimal dental hygiene and is a key element in the aesthetic outcome of the procedure.
If the contours are not as expected after initial soft tissue healing, strategic modifications can be made with the incremental addition of composite or acrylic resin. Excessive pressure on the mucosa can lead to tissue inflammation or necrosis, so it is advisable to undertake this process in stages for the most effective results.


Once optimal contours have been achieved, these must be transferred to the final restorations. Ensuring the established contours are accurately maintained promotes tissue stability and health as well as more successful long-term aesthetics.
Provisionalisation is an important step to achieve aesthetic results in implant cases, and many different options are available when planning the fabrication of provisional restorations. Depending on the clinical need, different approaches and timescales will be considered. As micromovements
can have negative biological consequences to the osseointegration process as well as the soft tissue connection, the treatment plan should involve as few disconnections of the prosthetic as possible.
The prosthesis design is contingent on the goal to be reached, i.e. to maintain the gingival structure. In the case of delayed implants, provisional restorations might need to recreate lost gingival contours. To achieve the latter, concave or flat subcritical contour can be effective, while the critical contour may be positioned at the zenith level of the tooth.
When used with immediate implants the design of the provisional restoration should follow the natural margins of the gingiva at the critical contour to support soft tissue structure. This helps in maintaining the shape of the gingiva during the healing process, resulting in more successful softtissue integration with the final prosthesis.
A concave subcritical contour in the buccal area may be considered to create a space for a stable blood clot to form.
Retention of the provisional implant will be assessed on a case-by-case basis. A screw-retained provisional restoration allows for easy retrievability, and eliminates the risk of soft tissue irritation that can occur in the subgingival areas due to residual cement. In addition, the fastening screws provide a solid joint between the restoration and the abutment. In some cases where implants are well-positioned, screwretained provisionals can be fabricated intraorally using acrylic or composite resin.
The ICE Postgraduate Dental Institute and Hospital, under the guidance of renowned specialist oral surgeon Professor Cemal Ucer, presents a host of comprehensive hands-on courses for dentists wishing to add advanced implantology techniques to their practice. In a hands-on, one-day course: ‘The art and science of provisional and interim implant restoration’, participants can explore various options for provisional restorations and their specific indications. Additionally, the course will cover fabrication techniques, and methods for customising impression copings and accurately recording soft tissue contours. Provisional restorations have become an essential element of successful prosthetically driven implant placement therapy, in successfully managing the aesthetic and healthy contouring of soft tissue around implants. Gaining a high level of surgical skill along with advanced knowledge of prosthetic design and soft tissue management offers patients the best chance of success. n
Please contact Professor Ucer at ucer@icedental.institute or Mel Hay at mel@mdic.co 01612 371842 www.ucer-clinic.dental
about the author
Professor Cemal Ucer (BDS, mSc, PhD, Oral Surgeon, ItI Fellow).

Trycare are delighted to announce that Dr Abdelsalam Elaskary, founder of Vestibular Socket Therapy (VST), will be bringing his internationally popular VST One Day Hands-on Workshop to the UK for the first time on Saturday 10th May 2025. But there are only 20 places available so early booking is recommended to ensure you secure your place! An event not to be missed, Dr Elaskary’s unique one-day programme of presentations and hands-on workshop focuses on the most recent and updated implant protocols, in particular VST which allows treatment of fresh extraction sites with immediate placement that reliably delivers optimised outcomes even in the absence of labial walls. Special emphasis will be on managing and optimizing regenerative outcomes in the aesthetic zone.
VSt One day Hands-on Workshop
Hosted by Trycare at the Royal Leonardo Hotel, Tower Bridge, London, on 10th May 2025, successful applicants will have the opportunity to learn everything they need to know in order to place immediate implants in the absence of labial bone using Vestibular Socket Therapy. With 6.5 hours CPD with Learning Outcome C the Course fee is just £795.00 including vat,
Attending Delegates will receive one Soft Cortical Lamina and one OsteoBiol Gen-os 0.5cc free (total value £272.00 exc vat) so that they can start using Vestibular Socket Therapy in their Practices straight away.
To book your place contact your local Trycare Representative, visit www.trycare.co.uk or email Denise Law on events@trycare.co.uk

advantages of VSt and the “Six day Protocol”
VST is an extensively scientifically validated surgical technique invented by Dr Elaskary and employed by many leading Implantologists worldwide. It enables treatment of a wide range of socket varieties suffering from complete loss of their labial plates. This unique technique allows immediate placement in severely defective sockets and offers a protocol to place immediate implants in sockets with active infection via Dr Elaskary’s “Six Day Protocol”. Thanks to minimised intra-operative surgical trauma with less complicated surgical intervention, it saves treatment time and minimizes the number of interventions. This innovative surgical approach reduces post-extraction socket collapse and the need for long-term provisional restoration, and provides predictable aesthetic outcomes.

dr abdelsalam elaskary
Dr Elaskary graduated in Dental Science at the University of Alexandria in 1986 and Implantology at the University of Frankfurt in 1993. In 1993 he also graduated from the Periodontics Department at Tufts University in Boston, Massachusetts, US.
Dr Elaskary subsequently obtained his Master in Dental Implantology at the Periodontics Department at the Health and Science Center of San Antonio, Texas, US, in 1994.
Founder of the Vestibular Socket Therapy treatment, he is the owner of the Elaskary & Associates clinic and educational institute located in Alexandria, Egypt.
Formerly Assistant Clinical Professor at the University of Florida, Jacksonville, US, from 2000 to 2005, Dr Elaskary is currently Visiting Lecturer at the Dental School of the Implantology Department at the University of New York, US.
He is President of the Arab Society of Oral Implantology (ASOI) in Cairo, Egypt, and has authored three books in the field of dental implantology and oral reconstruction, which have been translated into several international languages. The books are “Reconstructive Aesthetic Implant Surgery”, Iowa State Press, Black Well Science. June 2003; “Fundamentals of Esthetic Implant Dentistry”, Blackwell publishing, John Wiley. January 2008; and “Advances of Estethic Implant Dentistry”, John Wiley, March 2019. Dr Elaskary has also authored many articles in the field of implant dentistry.
For more information including details of the d elegate’s Bonus Offer worth £ 272.00 excluding V at, contact your local trycare r epresentative, visit www.trycare.co.uk or email d enise l aw on events@trycare.co.uk n

Whilst dental implants are common treatment options, patients may have the unrealistic perception that an implant doesn’t require as much care as their natural teeth. This expectation must be changed so that there is a better understanding among patients of peri-implantitis for improved implant maintenance at home.
To help with this, oral hygiene routines that are tailored to the treatment modality are recommended. Cleaning the implant and restoration meticulously and regularly can minimise the risk of infection and therefore promotes the long-term success of the treatment.
Curaden is dedicated to lifelong oral health for all and has an excellent solution for post-treatment implant care: the Curaprox REGENERATE Implant Kit. A collection of the finest oral hygiene essentials, the kit contains everything needed to effectively maintain oral health around implants.
Triple-threat of toothbrushes
The Implant Kit includes a variety of toothbrushes. The CS Surgical toothbrush is designed for those who have had any surgical treatment. It features 12,000 flexible and extra-fine filaments to remove food particles and bacteria whilst also being tender on sensitive or healing gingivae, ensuring an all-round comfortable experience that doesn’t compromise on hygiene.

The CS 708 Implant toothbrush is compact but efficient, making it ideal for cleaning around implants. With its fully bendable head and soft Curen filaments ensuring a gentle clean, the CS 708 Implant toothbrush offers maximal access to the surfaces that were previously harder to reach with a normal toothbrush.
Complementing the set is the CS 5460 Ultra-Soft toothbrush, a reliable product for the oral hygiene routine. Taking its name from the 5,460 densely packed filaments on its brush head, this offers stunning cleaning power. The trio of toothbrushes in the Implant Kit are a reliable way to clean the implant surfaces.

As toothbrushes struggle to remove the plaque and food particles trapped between the teeth, interdental brushes easily access
Dental professionals have many regular patients, some that they may have treated for many years. As rewarding as giving an excellent treatment to a patient can be, especially when they display immense satisfaction, it can be disappointing to find that patient return months later with a number of complications.
Without effective biofilm management, the microbiome of the oral cavity becomes a breeding ground for harmful bacteria. For patients with inadequate oral hygiene knowledge or poor toothbrushing techniques, dental treatments can be undermined. For instance, a patient with an implant and poor plaque control may find themselves at a greater risk of peri-implantitis. Treatment failure leads to more appointments and, unless the patient’s at-home oral care improves, this could be repeated.
To avoid repeated appointments and ensure the success of a treatment, Curaden Academy has devised the iTOP (individually-trained oral prophylaxis) programme. This spotlights how dental professionals can change the habits and views of their patients on biofilm management, giving them the knowledge and skills to teach at-risk patients on how to brush correctly.
these areas and reduce the risk of cavities, gingival disease and, for implant patients, peri-implantitis. The mixed assortment of CPS implant interdental brushes that come with the Implant Kit are, therefore, essential. The range of sizes allows patients to effectively use the right brush for the right interdental space, disrupting the plaque and food particles hiding among them. The filaments are ultra-resilient and gentle, massaging and strengthening the gingivae for long-term protection.

Bleeding can be a normal consequence of implant treatment, with the opened gingivae needing time to heal. However, only 32% of implant patients have reported receiving guidance on managing the bleeding. Of this number, 33% were recommended to contact a dentist and 28.6% were advised to use a mouthwash. Contacting a dentist or booking another appointment can take time, but a mouthwash like Perio plus Regenerate, included in the Implant Kit, is ideal. It contains 0.09% of chlorhexidine to help eliminate bacteria and regenerate

the gingivae and mucosa. It also offers relief for xerostomia, and has a pleasant flavour due to the presence of xylitol and its natural Citrox formula – this encourages compliance.
For tackling ulcers, inflammation or other injuries, the addition of the Perio plus Focus gel can treat these. With 0.5% chlorhexidine content, the gel is a powerful adhesive that leads to fast results with only small amounts. The antibacterial qualities of Perio plus Regenerate and Perio plus Focus make them crucial warriors for the short term fight against implant infection.
To gain a greater understanding of the Curaprox REGENERATE Implant Kit, you can book a Practice Educational Meeting with Curaden. These can be conducted in the comfort of your practice where you can see these products – and many more from the innovative range – up close and in action.
Implant care is vital for successful outcomes. Educating patients on the importance of this can improve their results and enhance their quality of life going forwards. Join Curaden in their mission to secure lifelong oral health for all.
To arrange a Practice Educational Meeting with your Curaden Development Manager please email us on sales@curaden.co.uk
For more information, please visit curaprox.co.uk and curaden.co.uk

Master the basics
iTOP employs a Touch-to-Teach (T2T) philosophy that stems from the question: ‘How can you teach others if you can’t do it yourself?’
Students on an iTOP programme will be shown the preventative techniques for toothbrushing through practice. This approach strips learning down to the very basics then builds upon it for a comprehensive understanding of optimal hygiene techniques.



As part of the T2T section, dental professionals will be asked to teach their colleagues their newly learned optimal oral hygiene techniques as if they were showing a patient. After a demonstration, the ‘patient’ will try themselves. A correctly repeated technique means the dental professional will pass the examination and can then teach their patients.
Climbing the iTOP ladder T2T is one component within an educational system formed of four levels. The different iTOP programmes are Introductory, Advanced, Recall, and Educator, with T2T forming part of the latter three options.
iTOP Introductory is a one-day seminar that details evidence-based solutions for how daily biofilm management can manage plaque-related dental diseases. It also highlights the importance of patient motivation so that they look after their oral health continuously and not fall back to their previous routine, or lack of.
For the next step-up, iTOP Advanced provides a deeper insight into implementing the lessons learned into the daily dental workflow. Lasting two days, the seminar includes a T2T practice in a small group setting and offers a more personalised experience through individual feedback and the opportunity for questions and discussion. This will give dentists a greater degree of confidence when teaching their patients.
In the continuous educational journey of a dental professional, it may be necessary to have a refresher on certain topics. iTOP Recall is an annual programme that keeps dental professionals up to date on their oral
prophylaxis, as well as showcasing any new research or techniques.
The next generation
Having incorporated their new skills into the workflow and helped patients, dental professionals may wish to be an iTOP instructor themselves.
Across the four-day iTOP Educator programme, they can receive an in-depth study of iTOP methodology, scientific evidence and criteria. There is also a simulation of a practical session, with a specific focus on T2T skills, as well as the appropriate options for different types of patients, such as perio, implant or orthodontic. This gives dental practitioners an allencompassing knowledge to help their future students help their patients.
By completing an iTOP programme from Curaden Academy, dental professionals can guide patients to heal themselves on their own by showing the best techniques and motivating them towards an optimal biofilm balance.
To arrange a Practice Educational Meeting with your Curaden Development Manager please email us on sales@ curaden.co.uk
For more information, please visit curaprox.co.uk and curaden.co.uk







With Denplan as your partner we can help you unlock exciting opportunities to grow and develop your practice.









Universal all-in-one adhesive for a wide range of applications and adherends
Compatible with all etching techniques
No filler and no HEMA – protection against hydrolysis
Reliable strong bond, less technical sensitivity
Simplified procedure for any adherend surface
No additional primer ne eded



With many patients in recent years waiting extended periods of time and travelling long distances to receive dental care, dental pain has been at the forefront of public imagination for some time. As such, it’s important that practices are able to offer patients advice about how best to manage their pain, no matter the cause, whilst they wait to be seen by a dentist.
It is absolutely essential that those experiencing toothache visit the dentist for diagnosis and treatment. If the pain is caused by injury or disease, for example, their situation may worsen over time, eventually leading to tooth loss. However, minimising the symptoms and understanding triggers of dental pain can help alleviate its intensity in the meantime.

Avoiding common triggers such as cold food and drink, sweet food, biting down, or other pressure, whilst waiting for an emergency appointment can help reduce the intensity of the pain felt by patients. The NHS recommends eating soft foods, and avoiding chewing with the sore tooth, as well as using a soft toothbrush to help reduce pressure on the problem area, whilst still removing bacteria. It also suggests avoiding foods that are sweet, very hot, or very cold, as well as not smoking, to prevent the problem getting worse.
For further information, please contact the SHOFU office 01732 783580 or sales@shofu.co.uk
www.shofu.co.uk
Often, patients may opt to take pain killers like paracetamol or ibuprofen to manage their toothache, however, these can take time to start working, and may not be the most effective way to relieve pain. Instead, recommend that patients use Orajel, the dental gel which contains benzocaine, for rapid relief in under two minutes. Not only does it work quickly, but it enables patients to deliver the gel exactly where it’s needed, for targeted relief.
Orajel comes in a number of different forms, ensuring patients can get the type of relief they need, when it’s needed.
These are:

Orajel Dental Gel
This delivers rapid relief from dental pain when and where it’s most needed. It contains 10% benzocaine to reduce pain caused by a broken tooth, or a tooth in need of a filling until patients are able to attend the practice. Up to four times per day, patients are able to apply the powerful local anaesthetic directly to the source of the pain, blocking pain signals along the nerves, numbing the area.
Orajel Extra Strength
For acute toothache, recommend Orajel Extra Strength. It contains 20% benzocaine, the maximum level available without a prescription in the Orajel range. Similarly to Orajel Dental Gel, it enables patients to deliver the local anaesthetic to a targeted area, for rapid pain relief, and can be applied up to four times per day.
Orajel Mouth Gel
Designed specifically for relief from mouth ulcers and denture pain, Orajel Mouth Gel contains 10% benzocaine to provide relief right at the source of pain. It is suitable for use up to four times daily, for no longer than four days.
Orajel Sensitivity ProShield Toothpaste
For patients experiencing sensitivity, recommend that they use Orajel Sensitivity ProShield Toothpaste to reduce sensitivity, repair the enamel, and reduce plaque.
Patients may seek assistance with dental pain at any time of the day or night, as such it’s important to have information available to them when they need it most. Should a patient phone the practice out of hours, seeking emergency care, providing a helpful and informative answerphone message can help them to effectively manage their pain until they can be seen. In this message, advise patients to avoid the triggers mentioned above and use the appropriate Orajel product for their specific concern.
For more information, and to see the full range of Orajel products, please visit https://www.orajel.co.uk/















Meet the extraordinary line up of industry professionals that form the judging panel for this year’s Dental Awards

Anshu Sood – Clinical Practice Director on the Board of the British Orthodontic Society
Anshu, Joint Clinical Director of Helix House Healthcare, is a Specialist Orthodontist and qualified dentist renowned for creating beautiful smiles through tailored treatments, including aligners and fixed braces. Her commitment to excellence is complemented by leadership roles as former Chairperson of the Orthodontic Specialist Group and Clinical Practice Director on the Board of the British Orthodontic Society.

Lisa Bainham –President, Assoc. of Dental Administrators and Managers (ADAM).
Lisa originally trained to be a dental nurse at North Staffordshire Hospital and qualified in 1994. Originally working in an orthodontic practice, she then developed an interest in practice management and came to join Steve Lomas, as the practice manager at The Old Surgery, Crewe, when the practice opened in 1998. She has a true insider’s knowledge of what it takes to be a Dental Awards winner, having won the Practice Manager of the Year category in 2016. Lisa became President of ADAM, which has over 500 members throughout the UK, at the end of 2016.

Preetee Hylton –President, The British Association of Dental Nurses
Preetee works fulltime as a dental nurse and safeguarding lead at a private dental practice in London. She is actively involved in education and training as she delivers the NCFE CACHE Level 3 Diploma in Principles and Practice in Dental Nursing.
Additionally, she serves as an Associate Examiner for the National Examining Board for Dental Nurses (NEBDN). She is also an honorary ambassador for the Mouth Cancer Foundation. Preetee’s contributions to the dental community extend beyond her work – she is an editorial board member of the Dental Nursing Journal and regularly authors articles.


Debbie Hemington – President, British Association of Dental Therapists
Debbie is President of the British Association of Dental Therapists, and works to support and represent current and future dental therapists.

Paroo Mistry –Member of The Probe‘s editorial board.
Paroo is a Consultant Orthodontist. She divides her time between Chase Farm Hospital and her private practice in North London. Paroo has been a judge on the Dental Awards since 2008.

Tim Newton –President of the Oral Health Foundation
Tim Newton is a Psychologist who has spent over 30 years working in dental settings with the goal of ensuring that everyone has the opportunity to enjoy the benefits of good oral and dental health. He is particularly concerned with addressing the needs of people who are anxious about attending the dentist, and in encouraging dental healthcare professionals to work with patients to develop healthy behaviours.
Tim is employed by King’s College London as Professor of Psychology as Applied to Dentistry, spending half his time working as Honorary Consultant Health Psychologist. Tim’s clinical work is focussed on individuals with dental phobia, and support for individual’s facing challenging dental procedures.

Amanda Oakey –Director of Education, British Dental Health Foundation
Leading the educational resources team, Amanda manages all educational resources from the Foundation. This includes marketing and selling existing products as well as purchasing and developing new resources. Amanda executes the creation and implementation of agreed projects is in charge of creating campaign products including National

Smile Month and Mouth Cancer Action Month. She also is in charge of distribution of resources along with managing exhibition presentations.

Amit Patel – Specialist in Periodontics & Implant Dentist
Amit is registered with the General Dental Council as a Specialist in Periodontics.
Alongside his private practice, he also works as Associate Specialist in Periodontics and Honorary Clinical Lecturer at the University of Birmingham Dental School. His special interests are dental implants, regenerative and aesthetic periodontics. Amit graduated in Dentistry from the University of Liverpool in 1997. Following a training post in Restorative Dentistry at the Liverpool Dental School he gained significant experience in Oral and Maxillofacial surgery through 3 prestigious hospital posts. He obtained his Membership of the Faculty of Dental Surgeons at the Royal College of Surgeons in Edinburgh in 2000.This training involved acquisition of the most up-to-date techniques in Periodontics and Implantology under the expert supervision of Professor Richard Palmer who was appointed the first Professor of Implant Dentistry in the United Kingdom. Amit then obtained his Membership in Restorative Dentistry from the Royal College of Surgeons of England and became a registered Specialist in Periodontics.

Dr Davinder Raju –Dove Holistic Dental Centre
Dr Raju gained his dental degree from the University of Liverpool and a Masters in Advanced Minimum Intervention Restorative Dentistry (MSc) from Kings College, London. He developed his interest in sustainable dentistry while he was undertaking his MSc., deciding he wanted his approach to clinical dentistry to be reflected in all aspects of his life. He went on to establish the first fully sustainable practice in the UK, the Dove Holistic Dental Centre in Sussex. In 2021 he launched the Greener Dentistry Global toolkit and accreditation programme to share his knowledge and experience with colleagues wanting to embark on a more sustainable way of working.

Now a recognised authority on sustainable dentistry in general dental practice, Dr Raju has written and lectured widely. He is a contributor to a book aimed at primary care to be published later this year, and he has been nominated for a fellowship of the International College of Dentists.

Amanda Reast –Multi Award-Winning Practice Manager
Amanda is Business Manager at The Dental Architect –Practice of the Year Award winner in 2023.
In 2024, Amanda was recognised as Practice Manager of the Year by The Probe ’s Dental Awards and also at The Private Dentistry Awards, making her a Multi Award Winning Practice Manager.

Rhiannon F Jones – President, British Society of Dental Hygiene & Therapy
Rhiannon has been a dental clinician for over 25 years and is currently the President of the British Society for Dental Hygiene and Therapy. She works clinically as a dental hygienist and dental therapist and has worked in hospitals and general practice as well as a clinical lecturer on a dental hygiene and therapy course.
Rhiannon was elected as BSDHT’s President-Elect at the AGM in November 2022 and began her twoyear term serving as President in November 2024.

Pam Swain MBE –Chief Executive, BADN Pam began working for the Association in 1992, when she returned to the UK after several years abroad working for various multi-national organisations, including the Home Office, NATO, Hilton International and the Bank of Bermuda. She is editor of the British Dental Nurses’ Journal, a Fellow of the Institute of Association Management and of the Chartered Management Institute. She was awarded the City & Guilds Licentiate in Management in 2005 and an Open University MBA in 2007.












“Anyone who stops learning is old, whether at twenty or eighty. Anyone who keeps learning stays young”
Being a naturally curious person means that lifelong learning is an inevitability. But even without an innate ‘need to know’ about everything, fostering a healthy, positive approach to learning serves you on a number of levels and in different ways throughout life. Some of it you actively seek and some of it seeks you out! I love to learn and, equally, I love to teach. The two go hand-in-hand of course, and I learn from my students at every stage of their dental careers, whether they are just starting out or are further into their individual pathways and looking to focus more on endodontics. I learned early on that it’s no good only adopting a lecture-style approach; good education combines relaying information and facts and figures with step-by-step understanding and process, culminating in practical immersion in the new things that come your way. This ‘show, explain and do’ method is key to how I work with students and young dentists. The changing landscape and progression within dentistry is framed by education. Whether that’s academically, through theory and research, or via technology through cutting-edge equipment and being hands-on. I look for innovation in endodontics – to assess, absorb and share. I ran a workshop in Dubai last month and the delegates’ thirst for endo knowledge was really satisfying. Genuinely, I often wonder how many people love what they do as much as we dentists and dental professionals?

Inevitably, dentistry means we can’t get too involved in the work-fromhome trend, so we continue to be surrounded by the people who are in this with us – and that’s a great source of perspective and education. Listening to our team, looking at how we can improve together is often the kind of learning that happens within a specific context and seeks us out. The same applies when we’re with patients – taking slightly longer over examinations, asking
These articles are written influenced by one or more of three basic categories. First are my personal experiences as a practising dentist, which I was for more than 35 years. Second as a practice owner of a 100% NHS cold squat practice and its subsequent private conversion, which occupied 20 of those years. And third, after an intense immersion of 20 years as a coach, consultant and trouble-shooter.
I have often been asked why, if my practice was successful, did I sell up when I did? The brief answer is that I stopped enjoying it. The people in the form of patients and team were great, a privilege

the right questions, and giving the patient space to think and reply can nearly always teach us something we didn’t know.
Of course, formal training is a fundamental part of being a dentist – through necessary CPD, authentic interest and a desire to develop our skills. Attending lectures, conferences and workshops is a valuable part of our lives and something we should continue to seek out. The social side is quite motivational too!
to care for and to work alongside. To use a coaching analogy, the ladder I had built was beautiful, well crafted and maintained, and provided me with a good support.
However, when I reached the top of the wall against which it was leaning, I realised it was the wrong wall.
That meant that I became unhappy and, with plenty of working years left in me, had to change direction. An analysis of my core values (Independence, Integrity, Co-operation, Communication and Curiosity, in case you wondered) led me along my present path, as opposed to up another ladder.
It hasn’t always been a smooth path but I enjoy it, am fulfilled, and can contribute to others. One of the interesting descriptions levelled at me is that I am a ‘contrarian’, which may be from a willingness to point out ‘BS’ in all its forms, or to be deliberately out of step or challenging. I can live with that and if I make people think, my job is at least partly done.
I recently discovered the book, The Contrarian’s Guide to Leadership, which I thoroughly recommend. Like all good books, it is not intended for anyone to follow diligently and without questions, rather to encourage the reader to think for
themselves. The author, Steven Sample, says that contrarian leadership means, “breaking free of the bonds of conventional thinking” to become a freethinking leader.
There is no space here to explore the book fully, so I have selected two chapters for consideration, not because they are the most important but because they include lessons I wish I had known when starting out. I thought I did know them but was fooling myself.
Chapter 3 – experts: saviours and Charlatans.
Sample says that it is important to know that not all experts act in the best interests of your objectives, but for their own ego. I thought of the current crop of Key Opinion Leaders, often in the pay of a company or organisation whose products or services they promote. I include ‘Influencers’, ‘Thought Leaders’ and ‘Gurus’. You’re a scientist and should be a sceptic, evaluate the evidence and make up your own mind.
“Leaders who are most effective do not rely too heavily on experts.”
Chapter 7 – Know which hill you’re willing to die on.
I take this two ways. Firstly, know your chosen set of moral values over all
- Henry Ford
There are so many things waiting to be learned – and not all of it should be vocational training. Improving our presentation skills, understanding business management, people management and taking care of ourselves physically and mentally –these are all worthy of our time and efforts. Everything ultimately feeds into the improvement pot, even if it’s just 1% each day.
Lifelong learning recharges selfesteem and kickstarts confidence. It does great things for our brains, including helping with memory strength and cognitive functionality. And undertaking new challenges and absorbing new information gives us an immense sense of achievement, propelling us forward to the next challenge.
What are you learning this month? Go seek it out – but let it find you too. n
About the author Dr Dhiraj Arora BDs MJDf rCs (eng) Msc (endo) pG Cert Ce. owner of evo endo, with three practices (limited to endodontics) in Twickenham, Gerrard’s Cross and slough. Dhiraj is a passionate teacher and ambassador for all things endo. follow him on instagram: @drdij_evoendo

others and then take full responsibility for your actions based on those values. You need to know yourself and know you can be trusted.
Pick your battles. My good fortune has been to work with good lawyers, accountants and other professionals that I trust. This means that my choices are made having had the facts, risks and consequences explained to me before actions were taken. I hoped, both as a clinician and in subsequent roles, that I could have said that about myself but I know I have room for improvement.
“Ethical leadership requires that the leader choose one set of moral values over all others, and then take full responsibility for his actions based on those values.” n Steven Sample was an academic in the field or electrical engineering who was President of the University at Buffalo from 1982 - 1991 and Southern California from 1991 - 2010. First published in 2002, “The Contrarian’s Guide to Leadership” is still relevant. • https://josephwchan.weebly.com/ uploads/1/9/8/7/19870355/exec_ summary.pdf
Our 5 Star Google Reviews can’t be wrong. Get in touch today on: 01788 719119
Come and see us at the BDIA Dental Showcase (stand H22) on the 14-15 March 2025.
I had the pleasure of instructing Dental Elite and I was looked after by Senior Practice Consultant Julie Randle. I have to say that right from the word go, Julie was there supporting me and advising me of the best possible outcome and solutions available for me to secure the best Dental Tennant.
Julie has a host of knowledge and I admire the hard work and commitment she possessed in securing the best candidate for me. Julie is a real asset to Dental Elite and it's been an absolute pleasure working with her.
Thank you, I appreciate everything that you have done.
DILJIT MORRIS
By far one of the best dental agents we have used in the market. We have purchased and sold many practice through Dental Elite and found the process very smooth due the help provided by the team. Not many agents get involved in the administration work e.g. CQC registration but Dental Elite fill out all the forms for you and submit them. I have not found a single agent that does that so far.
We have also used them for recruitment and have found a good quality a ssociates, admin and nursing staff through them.
For a free valuation of your practice get in touch.
In the bustling environment of a dental practice, the focus often lands on procedures, patient care, and maintaining stringent professional standards. While these aspects are undeniably important, it’s crucial not to overlook the human element that powers the practice. Promoting selfhelp within our dental teams, encouraging kindness and support, and harnessing the power of empathy and humour, can transform the work atmosphere, leading to happier, more cohesive teams.
The essence of self-help
Self-help in a dental team context is about empowering each team member to take charge of their own well-being. When individuals are encouraged to seek personal growth and stress management, the entire team benefits. Simple practices, such as setting boundaries, seeking professional development opportunities, and taking time for self-care, can significantly enhance job satisfaction and reduce burnout.
Self-help doesn’t mean navigating challenges alone. It’s about providing resources and creating an environment where seeking assistance is seen as a strength, not a weakness. By fostering a culture of continuous improvement and support, dental teams can thrive, even in the face of daily challenges.
A kind word or a supportive gesture can go a long way in a busy dental practice. When team members feel valued and supported, they are more likely to extend the same kindness to their colleagues and patients. Simple acts like acknowledging a job well done, offering help when someone is overwhelmed, or just lending a listening ear can create a positive ripple effect throughout the practice.
Supportive behaviour builds trust and camaraderie. When dental teams function as a united front, they can tackle even the most stressful situations with resilience and grace. Encouraging kindness and support within the team not only boosts morale but also fosters a sense of belonging and mutual respect.
Empathy is a cornerstone of effective teamwork. Understanding and sharing the feelings of others creates stronger connections and a more harmonious work environment. In a dental practice, where stress levels can run high, practising empathy helps team members relate to one another’s experiences and challenges. When team members feel understood and valued, they are more motivated and
It’s showtime!
It’s that time of year again – when dentistry fluffs up its feathers, polishes its mouth mirrors, and struts its stuff in vast, cavernous exhibition halls.
BADN will be at all the major Shows this year:
north of england Dentistry show Manchester, 8 March
BADN Chair Michelle Brand, IT & Comms Admin Jacek Drozdek and I will be at this show in the associations’ area.
Dental showcase
ExCel London, 14-15 March – https://dentalshowcase.com
BADN President Preetee Hylton, Jacek and I will be at this show on Stand A30. In addition, Preetee will be speaking at 13:45 on Friday 14 March in the CDO Theatre as part of the ‘Training the Next Generation – What Do They Want and Need?’ presentation, and at 10:45 on Saturday 15 March in the Oral Health Theatre on ‘Empowering Dental Teams Against Abuse’.

BADN Panel of Representatives member, Rebecca Silver, will be speaking at 15:30 on Friday 14 March on ‘Safeguarding and the Dental Team’ in the Oral Health Theatre, where the headline speaker is Professor Brian Cox.
Dentistry show NEC Birmingham, 16-17 May – https://birmingham.dentistryshow.co.uk Preetee, Jacek and I will be at the BADN stand (J06). Additionally, we shall be chairing the Dental Nurse Forum on Saturday 17 May, when speakers will include Preetee (workplace abuse) and Rebecca (sexual harassment), former BADN Chair Dr Debbie Reed (career pathways for dental nurses), and me (workplace bullying), as well as the NEBDN-sponsored corporate coach and learning development specialist Sarah Kenyon. Apparently the headline speaker at this show is some footballer!

engaged in their work. Empathy fosters a culture of open communication and collaboration, where everyone feels safe to express their thoughts and concerns. This leads to more innovative problem-solving and a more cohesive team.
Humour is a powerful tool in maintaining a positive work environment. While the work we do is serious, it’s essential to not take ourselves too seriously. A good laugh can diffuse tension, build bonds, and make the workplace more enjoyable. Sharing a funny story or a light-hearted moment can create a sense of unity and camaraderie among team members.
Humour also acts as a stress reliever. In the midst of a hectic day, a well-timed joke or a moment of levity can provide muchneeded relief and recharge the team’s energy. It reminds us that while our work is important, it’s the people we work with who truly matter.
Maintaining professionalism doesn’t mean being devoid of personality or connection. Striking a balance between professional conduct and human warmth
is key to creating the best, happiest teams. Remember, it’s teeth at the end of the day, but it’s people who make the difference. When dental teams prioritise kindness, empathy, and humour, they create an environment where everyone feels valued and supported. This not only enhances job satisfaction but also improves patient care. Happy, well-supported teams are more motivated, more productive, and more likely to provide exceptional service.
In conclusion, promoting self-help within our dental teams, encouraging kindness and support, and harnessing the power of empathy and humour, are essential for creating a positive and productive work environment. It’s the people, not just the procedures, that matter most. By fostering these values, we can build the best, most happy teams, ensuring a thriving dental practice. n


scottish Dental show Braehead, 20-21 June – https://sdshow.co.uk/ Preetee, Jacek and I will be travelling up to Glasgow for the Scottish Dental Show, where we can be found at stand A07 in the Braehead Arena.
Bingo cards at the ready!
And yes – due to popular demand – BADN Bingo will make a welcome return at each of the above shows. Dental nurses can win up to a year’s free BADN membership on the wheel… well, actually it’s more of a hamster cage.
That’s not all AND, Preetee will be speaking at the ADI Congress in Brighton on Friday 2 May (https://www.adi.org. uk/association_dental_implantology_ congress/) on the Dental Nurses’ Programme on ‘Implants: A Dental Nurse’s Role’. BADN member dental nurses can join the ADI for free (see www.badn.org.uk for details). And

we will have a representative at the BAOS Conference Dental Nurse Day programme in Newport on 3 April (https://www.baos.org.uk/baosannual-scientific-conference/). So come along, have a chat, say hello and join YOUR professional association! n
About the author Lisa Bainham is president at ADAM and practice management coach at practice Management Matters. About the author pam swain MBe is Chief executive of BADn








Free
No
24-hour
Guaranteed

An internet user will spend, on average, 2 hours and 23 minutes on social media every day, accounting for 35.8% of their daily online activity. Social media consumption is everywhere; from endless scrolling on TikTok, to making a holidayhighlights reel for Instagram or sharing a random thought on X. Even music providers like Spotify, film-logging sites such as Letterboxd and fitness apps like Strava count as social media platforms as they allow people to share information and communicate with friends – the digital landscape is constantly evolving.
The dynamic arena of online content is driven by a conveyor belt of trends, making it difficult to stand-out in a crowded digital space. For dental practitioners, harnessing the powers of social media can boost the awareness of your dental practice and the services you offer. By doing so, younger generations can better engage with their oral care and patient retention can also increase for the practice. There are many different approaches to consider when promoting your work on social media.
Choosing a platform
The variety in major social media platforms
– Facebook, Instagram, X, TikTok, YouTube – gives dental practitioners a wealth of choice for promotion. However, different generations have different social media preferences: Gen Z prefer the quickly-edited videos available on YouTube, Instagram and TikTok, millennials are likely to have an account on each platform, and Facebook has lost its popularity with younger audiences but remains dominant with Baby
DBoomers. For dental practitioners looking to target a new demographic, it is crucial to identify the best platform. For instance, to engage with the millennial and Gen Z audience, then visual content is the best.
Go viral with video
Online videos have an audience reach of 92.3% among internet users worldwide, making them an effective format for marketing. When promoting a cosmetic dental treatment, practitioners should avoid some of the more complex scientific language and explanations, as these can be confusing for potential future patients seeking that treatment. As aesthetics are a major focus, cosmetic dentistry is instead better suited to the visual medium for showing, rather than telling. A classic example of this is the ‘Before vs After’ post. This juxtaposition demonstrates the excellent results you wish to promote, whilst a time-lapse approach that quickly flicks through the different stages of a treatment can concisely improve the understanding for those looking for a similar cosmetic treatment. Illuminating treatments through videos can also help patients with dental anxiety –preoperative information can reduce anxiety. By better preparing nervous patients with detailed videos – especially those with relaxing or upbeat music – a more satisfying and relaxing experience can be secured, enhancing the patient-practitioner bond. However, when preparing videos for social media, it is important to adjust them for the appropriate presentation; portrait videos with consistent centre-framing can be mobile-friendly on platforms such as

r Kareem Siddiqui is a passionate and meticulous dentist with a keen interest in oral surgery, implantology, and digital dentistry. He has completed hundreds of dental implant cases, and is dedicated to lifelong learning, having attained multiple postgraduate qualifications. His passion for dentistry is matched by his attention to detail and pride in his work. For nearly a decade, he has also served as an educational supervisor for other dentists in the North East and as an examiner for the Royal College of Surgeons of England.
Dr Siddiqui has been elected as the Regional Rep for North East England on the Association of Dental Implantology (ADI) Board, and shares a little bit about himself, and his experience with the ADI:
“I have been involved with the ADI for the last three to four years, and my journey with the organisation has been a rewarding one. The ADI has consistently provided a platform for dental professionals to expand their knowledge and skills in the field of dental implants. From the very beginning, I’ve been impressed by the wealth of knowledge shared

Instagram and TikTok, whereas YouTube is better suited to longer, wider videos.
One of the biggest benefits to using social media for marketing is that it is costeffective. Providing you have the time to film and edit – both of which can be done on a smart phone – then social media is cheaper, faster and more interactive than traditional marketing options, such as billboards and radio adverts. Social media platforms can build brand identity, highlighting the dental practice, the available treatments, the friendliness of the team and the satisfied smiles of existing patients. When doing so, it is essential to follow the guidance dictated by the General Dental Council for social media use, keeping you legally safe online. With a powerful online identity, you can build a consistent following and improve word-of-mouth among patients. Navigating social media can be a challenge, but a membership with the British Academy of Cosmetic Dentistry (BACD) can help you chart this new frontier. Members can access a 15%
discount on all HI Marketing Ltd social media training packages, with options for personalised support for beginners and creative assistance for marketing masters alike. Along with many other benefits and trade deals, BACD members can also seek promotional help through excellent networking opportunities and a mentoring programme, ensuring that your marketing stands out.
Social media is a powerful tool, one that offers an accessible way of promoting the first-class treatments you provide. Creating and sharing videos, posters, photos or reels is puts you ahead of competition for reaching younger generations, raising awareness for the cosmetic treatments they require for a life-changing smile. For further information and enquiries about the British Academy of Cosmetic Dentistry visit www.bacd.com n
About the author Dr sam Jethwa is president of the British Association of Cosmetic Dentistry.

by industry leaders, the high level of education available, and the camaraderie that exists within the community. My experience has been overwhelmingly positive, with the ADI serving as a key resource in staying updated with the latest innovations

and best practices in implant dentistry. I have attended many ADI webinars, lectures and Masterclass days and it has helped me become a better implant dentist.
“What I truly appreciate about the ADI is its commitment to professional development and education. The events and resources they offer are always of the highest quality, delivering both practical knowledge and cutting-edge research. The sense of community among members is also something that stands out – it’s invaluable to be part of a network where collaboration and learning are prioritised. The ADI events, whether regional or national, have always been a great opportunity to not only learn but also connect with likeminded professionals who are equally passionate about dental implants.”
He discusses his reasons for joining the ADI Board, and his role here:
“I was thrilled to join the board because I believe there is a tremendous opportunity to expand the presence and impact of the ADI, particularly in the North East of England. As someone who is deeply passionate about dental implants, I see this as a chance to give
back to the community that has given so much to me. I’m excited to bring fresh ideas to the table and help enhance educational opportunities for both established professionals and those just starting out. I am particularly enthusiastic about helping raise awareness of the ADI’s work and ensuring that implant dentistry continues to evolve and thrive in the region.
“I’d like to emphasise how important it is that we continue to foster a culture of excellence and innovation in implant dentistry. As a board, I believe we have a unique opportunity to not only build on the ADI’s strong foundations but also to push the boundaries of what’s possible. I am particularly looking forward to engaging more practitioners in the North East, ensuring they have access to the resources, education, and networking opportunities that the ADI provides. By doing so, we can continue to raise the standard of care and drive further advancements in our field.”
For more information, please visit www.adi.org.uk Become a member today! n
Choosing to move from NHS to private dentistry can be an extremely scary prospect. Making this move can be the biggest change a dentist may make in their career, so it’s little wonder that fear can become a factor in the final decision. ‘Will enough patients want to stay with the practice for the move to be viable? How will the local community react? What will my team think?’ These are common misgivings felt by those debating the merits of handing back their contracts.
For dentists who have trained in the UK and started their careers as NHS dentists, as well as these fears, there is also a strong emotional attachment to the service that can play a part in the decision-making process. Despite the toll years of ‘treadmill dentistry’ can take upon both their mental and physical health, many find the prospect of turning their back on the service a struggle.
After decades of working for the NHS, despite wrestling with the dilemmas mentioned above, Principal Dentist at Hanford Dental, Ged Cummings, decided he needed to hand back his NHS contract. Although he had been carrying out private dentistry since he bought the practice in 2009, around one third of the treatments at the practice were still NHS funded. However, over the past few years, Ged and his Practice Manager wife, Kate, had come to feel disenchanted with NHS dentistry and believed their future lay in private dentistry.
tugging at the heartstrings
The final decision to hand back the contract was not made lightly, as Ged explains: “Losing the NHS contract was difficult. It does tug at your heartstrings a bit. I’ve been qualified for over 25 years, and I’ve always done some NHS dentistry. So, it was difficult to give it up, but the time was right. It was getting more difficult every year to remain in the NHS and I feel I can provide a better service outside the NHS.”
When his Associate Dentist, Will Edlin, joined the practice, Ged had already been considering handing back the contract, so he and Kate were open with him about their intentions. “Very early on we had a conversation and made it clear that we didn’t want to keep our NHS contract for much longer,” Ged explained. “We felt that the NHS contract didn’t work for us anymore. We don’t like target-based dentistry. And it just seemed to be becoming more and more stressful to hit targets. So, our aim was to get rid of it as soon as we could.”

Getting the timing right
However, they wanted to ensure that they made the move at the time that was best for them. As Kate explains: “We bided our time with the conversion this time round because we felt it was the right time to do it. We’d waited and we’d been watching the dental market and what had been happening with the NHS contracts. We eventually felt with our own contract, and what was happening nationally, that it was the right time to go.”
They also believed that the actions of other practices supported the timing of their decision. “Other people were announcing that they were handing their contracts back or reducing their NHS commitment, so, we knew it was the right time to go and it was the right way to move forward for our dentistry in the future.”
Despite having gone through a partial NHS conversion with Practice Plan when he bought the practice originally, Ged admits there was still some trepidation about handing back the whole NHS contract. His main concern, as is the case with many practice owners, was whether sufficient patients would be prepared to pay for private dentistry. “Losing patients was a potential worry,” he acknowledges. “We were approximately one third NHS when we decided to lose the contract. Stoke-on-Trent is not the most affluent area in the country, so our concern was that we could lose patients to other practices.”
However, the problems with patient access and the increasingly widespread acceptance of patients that private dentistry is often their only option to maintain their oral health, meant Ged’s fears were unfounded. As he says, “Fortunately for us, there weren’t really any other practices in the area that were taking NHS patients on, so we had a bit of a captive audience. Luckily, the number of patients that have stayed with Will and the practice have been sufficient for us to continue to pay our bills. It’s worked well for us so far.”
Will echoes Ged’s positive take on the change. “Obviously, I’d done mostly NHS work up until a few years before. And you do worry that on day one you won’t have any patients to see if nobody wants to stay and see you,” he says. “However, the response has been overwhelmingly positive. Naturally, we lost some patients, but I think it would be impossible to expect one hundred percent retention. But I was pleasantly surprised with how many wanted to carry on their care with me. And a lot of them have been really positive about some of the changes we’re able to make outside of the NHS contract.”
practice plan: the obvious choice for support
The choice of Practice Plan to support them through the conversion was an obvious one for Ged. “I was already

with Practice Plan when I took over the practice in 2009,” he says. “I’d had good experiences as a Practice Plan customer, and they’d always been great with me. It’s a great team, and they’re always very helpful. Also, I’ve had the same Regional Support Manager (RSM) all the way through, Josie Hutchings, so it was a no brainer for me really to stick with Practice Plan and convert the rest of our NHS contract with their help.”
Ged and the team are appreciative of the way the team supported them during the change. “The support we received during our conversion was fantastic,” he enthuses. “I’d been through the procedure once before many years ago, so I kind of knew what to expect. But it’s still nerve wracking because you don’t know how many patients are going to stay with you. Fortunately, Practice Plan held our hand all the way through, and we hit our targets quite comfortably.”
Kate was equally glowing in her praise of Practice Plan’s assistance during the conversion: “I think the whole practice plan ethos is excellent,” she states. “They look at the whole practice from top to bottom and everybody’s included.”
Unrivalled support
And, as Ged, Kate and Will can attest, things don’t stop after the conversion has completed. Practice Plan customers are eligible to attend workshops and courses on topics including finance, marketing, and HR, many of which count towards CPD. Practices can also take advantage of subsidised Mental Health First Aid courses which are highly valued
by those who have completed them. In addition to courses and events practices can also tap into a network of industry leading business consultants as well as local ad hoc groups set up by our RSMs. However, the support most valued by customers comes from our teams. As well as our 25 field-based RSMs and customer service team, Practice Plan also has 10 Head Office-based Relationship Support Advisors (RSAs). Having both teams offers greater opportunities to build lasting relationships with customers and make sure that they get the service they deserve. Meaning whenever help is needed, it’s only ever a phone call away.
How much all this means to practices is summed up by Kate: “The support we get from our RSM, Josie, is amazing,” she comments. “The practice manager group that she has set up is so valuable. And the support we get from head office is also first class. Practice Plan is really the best, most supportive plan provider for dental practices.”
This year, Practice Plan celebrates 30 years of welcoming practices into the family, helping them to grow profitable businesses through the introduction of practice-branded membership plans. So, if you’re looking to switch provider or are considering a full or partial move away from the NHS and would like a provider who will hold your hand through the process whilst moving at a pace that’s right for you, why not start the conversation with Practice Plan, on 01691 684165, or for more information visit the Practice Plan website: https://www.practiceplan.co.uk n
Dr Mark McAlister is an Ordinary Member of the British Endodontic Society (BES) council. He shares a little bit about himself and his experience with the BES:
“I am from Northern Ireland, and based in Leeds. I work in primary care and split my time between endodontic practice and general practice. I was elected onto the BES council in 2024 – this is my second time on council. I am also involved with Dental Foundation Training and I am interested in representing the perspective of recently qualified dentists, those in primary care and those working in non-specialist endodontic practice.
“I think endodontics is the ultimate dental specialty. It’s challenging, frustrating and rewarding. Endodontics brings relief to patients and improves the quality of their lives. I am passionate about endodontics and take great satisfaction being involved in the area.
“I first joined the society over 10 years ago, just before I started postgraduate training in endodontics. I joined for the educational events, as I valued quality

education with an endo focus. I then got to know some people and it became a good way to meet with friends from courses and connect with people. I value the access to the IEJ which BES membership gives me and discounted attendance on the study days. Also, the monthly BES newsletter always makes me feel connected to the society and others with the same interest.
“I’m passionate about endo and being part of the society connects me to others who feel the same. Being involved with the society for a number of years, it makes me feel very proud to have seen the effort that the BES makes to provide guidance and support for dentists, whether providing guidelines during Covid or the recent Guide to Good Endodontic Practice. Attending study days and catching up with people who are now good friends is something I look forward to. I have been grateful for the support the BES has offered me in my career and the care it has shown for the profession.
“Outside of my work, I enjoy reading books and try and get through at least one a week. I love watching films with the family, especially sharing the 80’s classics with my children. I am also addicted to Lego and spend a large amount of time hiding new purchases from my wife.”
Acareer in dentistry should be inspiring, challenging and rewarding. The right approach to progression will empower dentists to continuously advance, whatever that might look like for them. Stagnation can creep in when you’re not paying close attention, but there are some simple steps to help you stay proactive.

recognising potential to excel
It can be difficult to recognise when a career is stagnating, or when you are not reaching your full potential. Although it will look different to different people, it often means someone has become overly comfortable in their role, perhaps even a little bored. It can apply when performance is good – but not great – or when the rate of learning and development declines. Individuals may also lose some of their passion and enthusiasm for what they do, no longer so inclined to go that extra mile for patients or colleagues.
While an off day is perfectly normal for us all, if you find yourself feeling this way more often than not, it’s vital to do something about it. With just a few simple steps you can take your dental career from stagnant to thriving.
overcoming career stagnation
To overcome such a situation and reverse its effects on your career, it’s important to acknowledge stagnation and be proactive in making a change. The below are some steps you might consider:
Assess your progression in the last year
What did you achieve? How does this compare to what you had hoped to achieve? If you’re left underwhelmed at this reflection, set yourself a goal for the year to come in order to reignite your commitment to advancement. Maybe you want to have started treating certain types of cases or taken on new responsibilities within your practice. Your goals can go beyond the practice too – maybe you want to move somewhere new or experience life and work in a more rural or city-based location.
identify skills to learn or expand
As a dentist, much of your career progression will be dictated by your clinical abilities. Learning new skills and/ or focusing your remit will help you unlock your potential to become an expert or

even a specialist in your chosen discipline. This should be approached systematically for the best results – identify where your techniques or confidence are lacking and concentrate training in these areas.
Give back
Beyond your regular work commitments, it can be hugely rewarding and fulfilling to partake in some form of volunteer work. Giving back to your local community or your profession can deliver new experiences while also diversifying your skills. What’s more, volunteering is also associated with increased job prospects for the future, potentially leading to exciting new opportunities in the coming months or years. It could also provide a gratifying new avenue for your business, perhaps offering dental care to the homeless community once a month or visiting a local care home to provide domiciliary care to residents. You’ll be doing new things, meeting new people and broadening your perspectives all at the same.
Hold yourself accountable
We are all guilty of complaining about things and then not taking any actions to change them. Hold yourself accountable for moving your career forwards by setting a deadline for your desired progression or goal. This will give you a timeframe to aim for and encourage you to be proactive.
new you, new environment
It is natural for most dentists to work in different practices over the course of their careers. A move may be motivated directly by career progression, or by income potential, physical location, work-life balance or various other reasons. If you are considering
For more information about the BES, or to join, please visit the website www. britishendodonticsociety.org.uk or call 07762945847 n

such a step, it’s important to ensure that the new environment will be conducive to your continuing professional ambitions. For a new and exciting opportunity to really thrive in your career, consider joining Clyde Munro Dental Group. Not only is it the leading provider of excellent dental care in Scotland dedicated to patients, but it also delivers proactive and structured opportunities for dentists who want to excel. From a purpose-built, cutting-edge training academy to a dedicated Clinical Support Team, first-class practice facilities and an ethos for excellence in all areas, Clyde Munro is an ideal fit for many ambitious dentists.
Be all that you can be Life is better when lived to the full. Dentistry can be a hugely rewarding and exciting profession so make the most of it by actively driving your career forward. By taking charge of your goals, learning new skills and seizing new opportunities, you can unlock your full potential for a truly dynamic and enjoyable career in dentistry.
To find out more about the career development opportunities available at Clyde Munro, please visit https://careers.clydemunrodental.com/. n









































































Ort r hodontics incorporating Cf Cfast s ome of o





















































Aligner Material Higher Memory























Less Aligners Required



















remium Tri Layered horter Treatment Time


















































































Patient Comfort Increased REE Bonded Ret e ainer















2 day, hands-on










H a T i ed & A gner C urse

























FREE Zendura Remov ovable Ret e ainer



















Treating TMD Essential Surgi Procedures Du Orthodontic Treatment Straightwire Th Introduction To Early Interceptive Orthodontics and Orthopae i i m i d M M g


ourses day ore Predictable Results
With Dr Stefan Cloete D r o 21hrs CPD e E










FREE Whitening Gel With Eve v ry Case reating Surg traightwire T ner da day, y han a ds d -on o 1 rs ith x Alig Co Miguel Polonia h and ical ring erapy dics Stefan Cloete s 16th-17th tand: ome u
















Come and visit us at the NEC 16th-17th May 2025 Stand: G67
dr Wail Girgis discusses a challenging bilateral sinus lift case using a trusted grafting material to rebuild significant bony defects ahead of implant restoration.
Implant success is largely dependent on achieving high primary stability upon placement. However, this is made difficult in an atrophic jawbone. In particular, reduced vertical bone height in the maxilla makes implant placement challenging. The sinus lift procedure has been utilised for several decades as a way of creating more space and facilitating bone augmentation in order to allow primary stability of placed implants. Both one- and two-stage surgeries have been described in the literature. Success of these procedures, both in terms of graft and implant survival rates, is shown to be high.i There is also evidence that a grafted sinus lift affords greater vertical bone height gain than non-grafted surgeries.ii
Though an autogenous bone graft material is viewed to be the gold standard and offers a potentially quicker healing time, the drawbacks of a second surgical site are less than ideal for many patients. Bone substitutes, therefore, offer an alternative that many patients and practitioners prefer, offering comparable clinical and radiological results.iii The following case demonstrates the successful implementation of using 100% allograft during a bilateral sinus lift procedure, with delayed implant placement after a six-month healing period.
case presentation
A male patient was referred by his routine clinician for implant treatment in the upper arch. He presented with a minimally retentive upper denture that was held in place by two grade III mobile canine teeth. The patient had already received two implants in the lower jaw that were retaining the lower denture with locators and, due to the success of this procedure, he was interested in something similar for the upper arch.
A comprehensive clinical assessment was conducted, including a full medical history and evaluation of the soft tissue, occlusal vertical dimension and freeway space. The denture was also assessed to determine whether it could be used to fabricate the new implant-retained prosthesis. A fractured incisor tooth had recently been extracted, leaving a relatively fresh extraction socket at the UR1 site. With regards to lifestyle factors, the patient was a regular smoker. However, he agreed to stop a month before surgery and remain smoke-free at least for the duration of the surgical phase of treatment but was made well aware of the increased failure rate with smokers.iv
treatment planning
A full suite of diagnostic images was taken, including a CBCT to assess the underlying bony infrastructure. Bilateral sinus lifts were indicated in order to place implants for an implant-retained denture. Two infected canines would also require extraction. The soft tissue was also assessed for mucosa health and volume, smile line, as

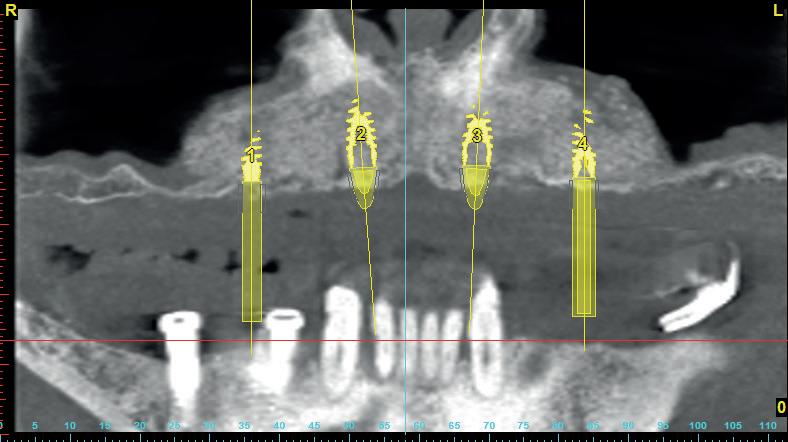
well as the sulcus depth and keratinised mucosa, determining whether soft tissue grafting would be necessary and if any other challenges should be anticipated during treatment.
Surgical treatment was digitally planned using Simplant software and a bone supported placement guide was made based on what was established to be the ideal implant position. The patient was informed that during the healing time, he would not wear the denture for three months to prevent pressure on the grafted area. A new CBCT would be taken after four months of healing following the sinus lift procedure. The implants would then be placed and another four months allowed before the restoration phase began.
surgical treatment
The bilateral sinus lifts were performed in two sessions, approximately two weeks apart. In each situation, the same procedure was followed. Local anaesthesia was administered and a flap raised. The sinus membrane was elevated and 3.5-5cc of MinerOss (BioHorizons Camlog) was placed into the site with the intention of not only creating bone vertically, but also horizontally. An allograft material was ideal as there was minimal autogenous bone present in the lower jaw, making harvesting adequate autogenous bone difficult –especially considering that the amount of graft material needed was more than what could be gathered from a single ramus or the chin. The patient also expressed a preference to avoid another surgical site. In addition, MinerOss provides rapid bone conversion to vascularised bone to allow for successful implant placement within the following months. This is preferable than when using xenograft or other synthetic grafting materials.
The soft tissue was closed over the surgical site and sutured without tension. Standard post-operative instructions were given to the patient to protect the site during initial healing


and encourage excellent oral hygiene. This meant avoiding chewing in the area and regularly using an antimicrobial mouthwash. The patient was delighted with the initial outcome achieved and the importance of his smoking cessation was emphasised.
Review and reflection
Sinus lifts are advanced procedures that should be approached only when the clinician has sufficient training and experience. Adding to the complexity in this case was the extremely large size of the sinus lift, which extended from the molar sites to the incisive canal in the midline. Another difficult aspect of this treatment was provisionalisation – the graft was extensive and could not come under any pressure while healing to avoid resorption. As well as this, it was important to place enough graft material to allow decent distribution of the implants placed while also maintaining height and width of bone around the implants. The sinus lifts were performed within two weeks of each other to allow the patient to chew on one side at a time. This was why it was important to avoid denture wear for at least three months during the healing process. The case also reflects why graft material selection is crucial. I have been using MinerOss for four-five years because the cortical component in the granules leads to very little bone resorption, while the cancellous particles promote revascularisation. It gives a much better tissue response with healing compared to other solutions – it does not get incorporated into the surrounding soft tissue and periostem, making second stage surgery neater as the mucosa lifts from the bone easily for effective soft tissue manipulation. MinerOss also exhibits simple handling, especially when mixed with blood, and I use it confidently in any case that requires grafting. It is part of a broad biomaterials portfolio that I utilise to meet different patient needs and
clinical scenarios, including Mem-Lok and NovoMatrix, which facilitate accurate implant placement and efficient soft tissue thickening respectively.
For product information from BioHorizons Camlog, please visit https:// theimplanthub.com/
References
i. Pjetursson BE, Tan WC, Zwahlen M, Lang NP. A systematic review of the success of sinus floor elevation and survival of implants inserted in combination with sinus floor elevation. J Clin Periodontol. 2008 Sep;35(8 Suppl):216-40. doi: 10.1111/j.1600051X.2008.01272.x. PMID: 18724852.
ii. Lie SAN, Claessen RMMA, Leung CAW, Merten HA, Kessler PAWH. Non-grafted versus grafted sinus lift procedures for implantation in the atrophic maxilla: a systematic review and meta-analysis of randomized controlled trials. Int J Oral Maxillofac Surg. 2022 Jan;51(1):122132. doi: 10.1016/j.ijom.2021.03.016. Epub 2021 Apr 10. PMID: 33849784.
iii. Hoveidaei, A.H., Ghaseminejad-Raeini, A., Esmaeili, S. et al. Effectiveness of synthetic versus autologous bone grafts in foot and ankle surgery: a systematic review and meta-analysis. BMC Musculoskelet Disord 25, 539 (2024). https://doi.org/10.1186/ s12891-024-07676-8
iv. Mustapha AD, Salame Z, Chrcanovic BR. Smoking and Dental Implants: A Systematic Review and MetaAnalysis. Medicina (Kaunas). 2021 Dec 27;58(1):39. doi: 10.3390/ medicina58010039. PMID: 35056347; PMCID: PMC8780868. n
about the author

Wail Girgis is a clinical director at devonshire House and a specialist Prosthodontist. He trained at King’s college Hospital dental school, London and went on to complete an Msc degree in conservative dentistry at the eastman dental Hospital, London, where he taught thereafter as a clinical lecturer. Wail was a tutor at the International centre for excellence in dentistry on the Implant certificate course and he is a member of the International team for Implantology for whom he is a clinical lecturer. Wail is also a clinical supervisor for the Msc in Implantology for Vss academy, part of the university of central Lancashire and works at the department of Prosthodontics at the eastman dental Hospital in London as a Locum consultant in Prosthodontics and Restorative dentistry.





The couple that helps you to achieve even better oral hygiene

FLEXI
• The special FLEXIBLE HANDLE makes it possible to angle the handle to achieve better and easier access to all interdental spaces.
• The non-slip handle ensures good grip even when fingers are wet.
• All brushes have plastic coated wire. This ensures no metal is in direct contact with teeth and gums, thus making them much more comfortable to use and preventing dental injuries.
• 11 sizes ensure that all needs are covered.



TANDEX PREVENT Gel
• Strengthens the enamel and has an anti-bacterial effect.
• 0.12% chlorhexidine and 900 ppm fluoride.
• The consistency combined with the needle shaped tube end make it easy to apply directly on the FLEXI brush and use wherever needed.
• Pleasant taste of peppermint.
• No alcohol or abrasives.
A36-year-old male patient presented to me with concerns about the aesthetics of his dentition, primarily regarding mild to severe wear on his anterior dentition. A regular attendee of the practice, we had discussed his compromised anterior envelope and how his teeth were in a non-harmonious position for optimal function in previous appointments. He was interested in learning about the potential treatment options available to him to improve function and aesthetics.
A full orthodontic assessment was carried out. Mild wear was observed on the upper incisors, and moderate to severe wear on the lowers, creating concerns about the functional viability of these teeth in the long-term. This was compounded by a Class II division 2 malocclusion and a restricted anterior envelope of function. Each of these factors can significantly exacerbate tooth wear which lead to his condition and, without appropriate intervention, would have worsened. Digital scans were used to assess the existing intercuspal positions, and unfavourable results were observed in the incisal areas.
X-ray assessments were completed, and the patient was deemed to have adequate bone health for orthodontic treatment. His oral hygiene was acceptable, but he was a habitual nail biter. This parafunctional habit is well known as a potential cause of tooth wear. Intraoral images were attained with a DSLR camera.
A number of treatment plans were prepared and presented to the patient. Soft splint therapy and continual monitoring of the dentition was discussed. Whilst this would be a more affordable form of treatment for the patient, it would not address the cause of tooth wear entirely, merely mask it.
Taking a Dahl approach was discussed, readjusting the bite to create space in the anterior dentition and then building up the incisors with composite to restore aesthetics and function. This too would not be enough to prevent long-term problems, as the restricted envelope of function meant that he would still be prone to wear upon the restorations. The patient appreciated the alignment of the dentition would need correcting.
To ensure longevity of the restoration, it was proposed that the patient undergo a course of orthodontic treatment to correct the mild crowding in the upper arch and moderate to severe crowding in the lower dentition, whilst intruding both the upper and lower anterior teeth, This would be achieved with a view to create space in the intercuspal positions in order to restore the lower incisors to the correct height and anatomy, in turn reversing years of non-carious tissue loss and minimising the risk of it happening again.
This approach leaned heavily on the skills and insights I acquired from the Align, Bleach & Bond (ABB) course with the IAS Academy. Without the experiences the course gave me in aligning and restoring complex cases, I may have only been able to provide a soft splint, which is ultimately not the most optimal outcome for the patient, and so would have needed to refer the case for orthodontic treatment. The approach also leant on the philosophy


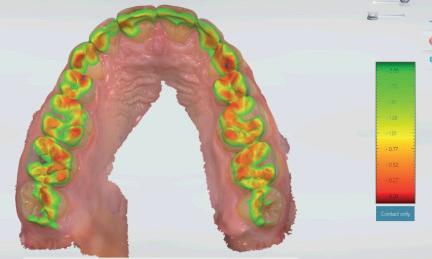




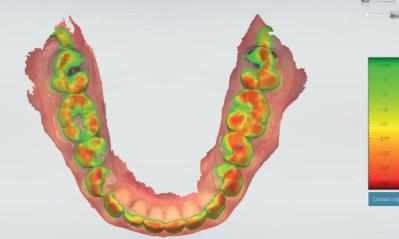






of minimally invasive, but long-term care, which was imparted onto me by the tutors.
Each treatment plan was presented to the patient with its positive and negatives, and he was receptive to each. He provided informed consent to proceed with orthodontic treatment with clear aligners, followed by composite restorations.
Clear aligners were the chosen orthodontic approach due to their aesthetic advantages. In total, 20 appliances were used throughout the process, with the patient instructed to wear them for a minimum of 22 hours a day. He was also advised on how to maintain his oral hygiene to an optimal standard, with direction to routinely clean the aligners. Each aligner was worn for around seven days at a time, and the patient experienced no issues. He was exceptionally compliant and the treatment plan tracked with the in vivo outcomes, requiring no adjustments during the process.
Post-treatment scans displayed that the desired movements had been achieved from the clear aligner therapy. With successful intrusion of the incisors, there was adequate intercuspal space for restorations to be built in the lower arch. A digital wax up allowed for precise planning of this aspect, and also the chance to visually display the treatment to the patient. Using technology in this way means clinicians can create a ‘trial smile’ which can assess function and aesthetics reliably before further treatment is provided, creating a more predictable outcome.







Following the completion of orthodontic care, the patient underwent a course of whitening to achieve an aesthetic, bright shade. His lower incisors were built up with the G-ænial Universal Injectable and the EXACLEAR clear VPS, utilising a composite injection moulding technique. This approach is favourable as it allows a clinician to effectively build height whilst retaining aesthetics and durability. The upper incisors were restored with free-hand edge-bonding, another technique that I was able to refine though the ABB course from the IAS Academy.
The restorations were checked to ensure they optimised the occlusal contacts, resulting in a restored anterior dentition with improved aesthetics and function in everyday life. Removable clear retainers were provided to be worn nightly, and the patient was instructed to keep up his oral hygiene routine and regularly clean the new appliances.
The patient was delighted with the outcome, and agreed that the extra steps for orthodontic treatment were worth the extended period of care. I was equally delighted, not least for the immediate result, but knowing that it would be a long-term solution. Had the teeth been left in malocclusion, the failure of restorative work is almost an eventuality, suffering the same fate as the natural dentition.
We discussed techniques the patient could implement to halt his parafunctional habits, but ultimately restoring a functional occlusion was the only way to optimise restorative results for years to come.


Without improving my clinical knowledge through advanced training courses, it would be impossible for me to deliver such results to my patients without referrals. Taking courses like the Align, Bleach & Bond course from the IAS Academy allows me to present these complex treatments in house, and make patients for life. For more information on upcoming IAS Academy training courses, please visit www. iasortho.com or call 01932 336470 (Press 1)
Reference i. Algadhi, A. (2021). Tooth surface loss: definitions, prevention and diagnosis. Saudi J Oral Dent Res, 6(3), 129-133. n
about the author dr Michael santangeli graduated from Liverpool dental school with honours and distinctions in all subjects. He received multiple academic prizes upon graduation, including the prestigious Malcom Foster Medal, awarded to the student with the highest overall finals grade. dr santangeli currently treats patients at starbeck dental centre in Harrogate, where he provides highquality general dentistry,

and restorative care. Outside of dentistry, he enjoys running and spending time with his wife
To make 3D printing really work for your practice, it’s crucial to invest in the right equipment for your business. You need reliability, predictability, durability, compatibility in the technology you choose – and more.
Where will you find all this? With Sprintray.
Proud to be the only supplier for a complete digital 3D printing ecosystem, SprintRay offers an array of industry-leading solutions designed to enhance patient outcomes and streamline professional workflows. In no product is this clearer than in the Midas 3D printer – the latest generation technology in a range of dentist favourites.
introducing Midas

Midas is the ultimate solution for fabricating high-quality chairside restorations. It is the world’s first digital restoration press, as well as the smartest and simplest method of 3D printing dental restorations.
It uses Digital Press Stereolithography, a patent-pending alternative printing method to the widely recognised (separate) resin, tank and build platform set up of today’s printers. It uses hydrodynamic principles to remove the need for lower viscosity resins, creating exciting opportunities for the use of new materials. It also utilises a 45 µm projector to deliver light directly into the print glass with minimal distortion, further optimising accuracy.
The result is:
• Implementation is fast and efficient, with little to no staff training required and no upkeep needed to maintain the equipment.
• AI-supported restoration design further streamlines the professional workflow.
• A highly affordable chairside workflow for both clinicians and patients to benefit from.
• Midas prints with highly filled resins which are more viscous than those that can be used on conventional 3D printers, removing any viscosity limitations.
• Multi-restoration printing is possible, increasing productivity and efficiency.
• A small carbon footprint that encourages a more sustainable production process, with no compromise in output.
The new king of chairside workflows, Midas consists for three capsules and is ideal for a range of cases. Full contour crowns with natural-looking aesthetics are possible for posterior, anterior and implantretained indications. Up to three can be printed across the three available capsules. Complex shapes for inlays and onlays can also be printed with pixel-perfect precision, with more than one restoration per

capsule possible depending on indication. Finally, various veneers, including no-prep solutions, can be printed, up to three at a time per capsule.
a simple workflow
Midas necessitates a straightforward workflow that any clinician (or dental nurse/ assistant) can implement in practice.
• Step 1: Upload scans – the AI studio automatically identifies the restorative margins.
• Step 2: Confirm the margins – adjust as needed.
• Step 3: Final design touches – make any final tweaks to the positioning and aesthetics of the AI-designed crown.
• Step 4: Print on Midas – send the crown design directly to the Midas printer for fabrication in under 10 minutes.
Complementary innovations
SprintRay has recently launched two brand-new materials that are perfect for use with Midas.
The NEW MDR-approved SprintRay

Ceramic Crown features a ceramicdominant (>51% nano ceramic infill) hybrid formula, delivering exceptionally strong and durable restorations. Speed and efficiency are also optimised, allowing crowns to be printed in just 10 minutes for an impressive total treatment time of 45 minutes or under.

Also NEW is the SprintRay OnX Tough 2 printing resin, which offers optimal performance and strength for the fabrication of long-lasting fixed hybrid dentures and full arch implant prosthetics. The availability of three shades also facilitates highly aesthetic outcomes, with fixed dentures created in just 30 minutes.

a small step for Sprintray, a quantum leap for dentistry
Midas is changing the game in 3D printing. Strong, durable and aesthetic restorations can quickly and simply be created chairside for a wide range of patients. The technology is easy-to-use and intuitive. The results are astounding.
Midas from SprintRay is revolutionising digital 3D printing workflows worldwide.
Can you afford not to book a demo and see what all the fuss is about?
For more information, please visit https://sprintray.com/en-uk/ n

Dr Kenny Doig of The Private Dental Centre in Boston marvels at the ‘Ooh’ reaction of patients as they sit in his new Planmeca Compact i5 dental unit
The Private Dental Centre was established in Boston by Dr Kenny Doig in 2004. Over the subsequent two decades, the practice has grown with the addition of new team members, its introduction to Investors in People and the British Dental Association’s Good Practice Scheme, gold membership status attained in both, as The Private Dental Centre developed into one of Lincolnshire’s premier private practices.
Dr Doig is no stranger to selfimprovement. Having graduated from Dundee Dental School, qualifying in 1988, he has undertaken further graduate training, holding a Diploma in Restorative Dentistry, and become a Fellow of the Royal College of Surgeons. In addition, Kenny has overseen undergraduate dentists, hygienists and therapists at Sheffield Dental School, and served as a lecturer for trainee dental nurses as well as delivering a series of seminars on infection control for the BDA.
As The Private Dental Centre reached its 20th birthday, it was in need of a little improvement of its own. “The previous chairs were getting a bit tired, and it was time for a bit of a refurbishment,” recalls Dr Doig. “We also wanted to introduce some additional specialities to the practice because we didn’t previously have an OPT facility.”
Following some good feedback from other clinicians, Kenny got in touch with Planmeca.
“We had very good feedback about Planmeca, not only about the quality of the scan and the Ultra Low Dose 3D imaging protocol, but also the fact that the software was intuitive and easy to use.”
Planmeca’s Ultra Low Dose enables CBCT images to be captured at even lower effective patient doses than standard 2D images.
“Within our area, there aren’t many practices with CBCT capabilities,” Kenny explains. “So, we take on plenty of referrals. A big plus point, therefore, of the Planmeca solution, is that it is simple to export the DICOM files. You even have the ability to include the reader for the referring clinician.”
To assist Dr Doig in making his decision, Planmeca brought their setup directly to his doorstep.



“Planmeca, along with our dental equipment dealer Promec Dental, made the fantastic offer of bringing their mobile demo facility to the practice,” says Kenny. “This allowed us to see how the Romexis dental software works in person.
“We were able to see a fully set-up surgery in the van, which gave us the opportunity to also look at the chairs. This subsequently led us to book in to see the full range at the Planmeca showroom.”
Browsing gave way to purchases.
“We’ve invested in Planmeca Compact i5 chairs. We opted to include the integrated X-ray facility in two of them, and this has been absolutely fantastic.”
The Planmeca Compact i5 dental unit has been designed to offer a smooth workflow for the dental team alongside an enjoyable treatment experience for all patients.
“We were setting up a brand new surgery in the practice in a much smaller room,” Kenny notes. “So, one of the big selling points for the system was the knee break chair.
“Another great feature of the Compact i5 is the overhead light. It’s gesture controlled, which is fantastic, and it has the light safe mode that’s easily activated for

composite placement. You can ramp up and down the intensity and the illumination over the patient has a great cut off point, so you can work safe in the knowledge that they are not getting blinded.”
As for how the patients themselves have found the Compact i5, Dr Doig hasn’t even needed to ask for their opinions. “Every patient, without exception, has come in, sat down on the chair, and said, ‘Ooh, this is a comfortable chair!’ That’s not an exaggeration and, on the top of that, they then notice that the whole setup is different. So, they can see that we’re investing in the practice and, therefore, delivering better patient care, for them.”
Kenny was equally impressed with features such as the flexibility that the Compact i5 offers to switch seamlessly between left- and righthanded clinicians, and the option to include the intra-oral camera as an integrated extra.
“Another great feature that I was previously unaware of was the flushthrough system,” Kenny continues. “It’s integrated within the cuspidor system and, at the end of the day we can flush through all of the lines, all within the system, which means there are no buckets to trip over.”


Watch the full interview with Dr Kenny Doig here: https://www.planmeca.com/testimonials/

While providing patients with a comfortable experience is of the utmost importance, the installation of Compact i5 dental units has provided several benefits for the practice.
“One of the main drivers in investing in good quality equipment was that it helps to attract any potential associates that want to come and work for me,” says Kenny. “The reason for having three identical chairs was we’ve got the ability to interchange surgeries across a busy multi surgery practice. One of the brilliant features of the Compact i5 is the touchscreen and its ability for different clinicians to log in with all of their settings configured.”
Kenny concludes that it gives him confidence to know that other dental practices are also installing Planmeca solutions. “In my mind, it’s a fantastic product and certainly something that you would want to be considering, as an option.”



Dr Kenny Doig of The Private Dental Centre in Boston marvels at the ‘Ooh’ reaction of patients as they sit in his new Planmeca Compact i5 dental unit.


Tepe is delighted to bring you this article, with the aim of supporting the ongoing Enhanced CPD needs of dental healthcare professionals in improving and maintaining the oral health of their patients
Aims
This article highlights the importance of interdental cleaning as part of a patients daily oral hygiene routine
Learning objectives:
• To appreciate the range of bacteria that have been found within the interdental spaces
• To understand some of the barriers to interdental cleaning among patients
• To have a better understanding of the benefits of interdental brushes for oral health
Learning Outcome: A, D
Interdental cleaning is an essential part of every patient’s daily oral hygiene routine. However, it remains a behaviour that few individuals adopt in the UK and around the globe. For dental professionals, the goal is to educate patients so that they fully appreciate the importance of disrupting plaque and bacteria in the interdental spaces. In doing so, the hope is that more people will dedicate the extra time and effort to looking after their teeth and gums moving forward. At this point, the dental team must ensure that patients understand what tools are available to facilitate interdental cleaning and which might be most suited to them.
The dangers lurking in-between Up to 19 periodontal bacteria have been identified within the interdental spaces, including several pathogens associated with the development of periodontitis –which are classed as red and orange Socransky complex bacteria. Blue, green, yellow and purple complex bacteria are linked with periodontal health. Of the red complex bacteria, all three – Porphyromonas gingivalis, Treponema denticola, Tannerella forsythia – have been detected within the interdental spaces. The theory is that these areas provide an ecologically niche environment for bacteria to grow in, which the body has few natural defences against. This means that when mechanical removal is lacking, the bacteria can thrive.ii Consequently, the risk of periodontal disease increases.
Toothbrushing is the key action associated with oral hygiene. However, studies have proven that brushing alone is not enough to maintain low plaque levels and keep dental disease at bay. One systematic reviewiii found manual toothbrushing achieved an average of only 42% plaque reduction. For this reason, dental professionals have long encouraged patients to incorporate adjunctive interdental cleaning aids within their daily routines to remove bacteria from these spaces. There is plenty of literature to support it too. Though this is an active area of research, regular interdental cleaning has been shown to significantly reduce the risk of periodontitis, caries and tooth loss.iv Daily interdental cleaning has also been associated with higher self-rated oral health among patients, with lower chances of gingival bleeding and gingivitis.v

The popularity of interdental cleaning remains unclear in the UK, although figures suggest there is still substantial room for improvement. The Adult oral health survey 2021vi found that only 30% of participants used dental floss, with 21% using interdental brushes (IDBs) and 11% choosing woodsticks or toothpicks. However, the data does not provide enough insight to determine if some individuals use multiple options and therefore how many people actually clean interdentally every day. There are several potential barriers to daily interdental cleaning for the general population. These include poor understanding of its advantages, difficulty in adapting routines and the time it takes.vii
The former of these can be addressed with improved education, which means reiterating the importance of interdental cleaning during every check-up and treatment appointment. Additional aids such as graphics and animations can also be utilised to help individuals better understand the oral health information they receive.viii
Behaviour change is another challenging aspect, requiring patients to actively make a change to their regime and stick to it for
some time before it becomes habitual. For this to be successful, the individual must have the physical and psychological ability to change, as well as the opportunity and motivation to do so.ix Both this and an acceptance that the extra minute will be spent wisely can be encouraged through enhanced education and appreciation for the importance of interdental cleaning.
The recommended cleaning aid and technique may also influence the patient’s decision to introduce an extra step to their daily oral hygiene regime. For example, the product used must be easy to use and comfortable in the hand to ensure simple manipulation in the mouth. Patients also need to know how to use the adjunctive solution and to make sure they are applying good technique. Many dental professionals will have encountered patients who claim floss is difficult to use, for example, which can put them off picking it up it every day.
The strength of IDBs IDBs are a great alternative that many individuals find easier to use than floss. There is evidencex that IDBs are more effective at removing plaque than other
solutions, especially traditional floss.xi Some of the researchxii goes as far as to recommend floss only be used where IDBs can’t fit an interdental space without causing trauma, making the latter the top interdental cleaning device of choice. Researchersxiii have reported that bleeding decreases by almost 50% after one week of using IDBs daily and by up to 85% after three months. The aforementioned red and orange Socransky complexes decrease significantly after IDB use, while blue, purple and yellow bacteria all increase at the test sites. This suggests improved periodontal health and reduced risk of disease when IDBs are implemented as part of a regular oral hygiene routine. This is, at least partly, why interdental cleaning is recommended as part of official guidelines for those with periodontitis.xiv Studiesxv have also found patients to prefer IDBs over alternatives like floss, due to their improved ease of use. Even early researchxvi found patient acceptance and hence compliance with interdental brushes to be better than floss.
Initial researchxvii in the area also suggests that using an IDB in combination with active substances – such as essential oils or chlorhexidine – delivers no additional

benefit to plaque removal or interproximal hygiene. This keeps it simpler for patients, who need only master the handling of a IDB to achieve maximum improvement in their oral hygiene. To make the process even easier, recommending solutions like the colour-coded range from TePe means you can help patients select exactly the right sized brush for each interdental space. The highly affordable and ergonomically designed solutions are also comfortable to hold in the hand, allowing even those with low dexterity to insert and remove the interdental brushes from the mouth correctly for optimal oral hygiene.
Making oral health more accessible
At the end of the day, all dental professionals are looking to make oral health more accessible to more people. That might mean communicating with them in a way that enhances their understanding of recommendations, or tailoring advice to suit their physical abilities. Whatever the solution, encouraging patients to incorporate interdental cleaning within their daily regime is crucial for their current and long-term oral and general wellbeing. For more information on the innovative new products available from TePe, please visit www.tepedirect.com
References
i. Chapple IL, Van der Weijden F, Doerfer C, Herrera D, Shapira L, Polak D, Madianos P, Louropoulou A, Machtei E, Donos N, Greenwell H, Van Winkelhoff AJ, Eren Kuru B, Arweiler N, Teughels W, Aimetti M, Molina A, Montero E, Graziani F. Primary prevention of periodontitis: managing gingivitis. J Clin Periodontol. 2015 Apr;42 Suppl 16:S71-6. doi: 10.1111/ jcpe.12366. PMID: 25639826.
ii. Carrouel F, Viennot S, Santamaria J, Veber P, Bourgeois D. Quantitative Molecular Detection of 19 Major Pathogens in the Interdental Biofilm of Periodontally Healthy Young Adults. Front Microbiol. 2016;7:840. doi: 10.3389/fmicb.2016.00840.
Brought to you by

iii. Slot DE, Wiggelinkhuizen L, Rosema NA, Van der Weijden GA. The efficacy of manual toothbrushes following a brushing exercise: a systematic review. Int J Dent Hyg. 2012 Aug;10(3):18797. doi: 10.1111/j.16015037.2012.00557.x. Epub 2012 Jun 6. PMID: 22672101.
iv. Marchesan JT, Morelli T, Moss K, Preisser JS, Zandona AF, Offenbacher S, Beck J. Interdental Cleaning Is Associated with Decreased Oral Disease Prevalence. J Dent Res. 2018 Jul;97(7):773-778. doi: 10.1177/0022034518759915. Epub 2018 Feb 26. PMID: 29481764; PMCID: PMC6728587. v. Chaffee BW, Persai D, Vora MV. Interdental Cleaning and Oral Health Status in an Adult Cohort, 2015 to 2018. J Dent Res. 2020 Sep;99(10):1150-1156. doi: 10.1177/0022034520926139. Epub 2020 May 28. PMID: 32464077; PMCID: PMC7443997.
vi. Office for Health Improvement & Disparities. Accredited official statistics. Adult oral health survey 2021: health-related behaviours. January 2024. https://www.gov. uk/government/statistics/adultoral-health-survey-2021/adult-oralhealth-survey-2021-health-relatedbehaviours [Accessed January 2025]
vii. Aroonratana, P., Lertpimonchai, A., Samaranayake, L. et al. The association between interdental cleaning and periodontitis in an urban Thai adult cohort: a cross-sectional study. BMC Oral Health 24, 1185 (2024). https:// doi.org/10.1186/s12903-024-04980-6
viii. Turkdogan S, Roy CF, Chartier G, et al. Effect of Perioperative Patient Education via Animated Videos in Patients Undergoing Head and Neck Surgery: A Randomized Clinical Trial. JAMA Otolaryngol Head Neck Surg. 2022;148(2):173–179. doi:10.1001/ jamaoto.2021.3765
ix. Department of Health & Social Care. Office for Health Improvement & Disparities. Guidance. Chapter 3: Behaviour change. Updated November 2021. https://www.gov.uk/ government/publications/deliveringbetter-oral-health-an-evidencebased-toolkit-for-prevention/chapter3-behaviour-change [Accessed January 205]
x. Amarasena, N., Gnanamanickam, E.S., Miller, J. (2019) Effects of interdental cleaning devices in preventing dental
1. How many periodontal bacteria have been found in the interdental spaces?
a) 9
b) 10 c) 19 d) 29
2. What colour Socransky complex bacteria are associated with periodontal disease?
a) Yellow and red
b) Red and orange
c) Orange and yellow
d) Blue, purple and yellow
3. Toothbrushing alone achieves how much plaque reduction?
a) 100%
b) 75% c) 62% d) 42%
4. What are the barriers to interdental cleaning cited in the article?
a) Time and ease of use
b) Poor understanding of the advantages
c) Difficulty changing routines
d) All of the above
5. Patients need what of the following to implement change to their routines?
a) Physical ability, opportunity and motivation
b) Opportunity and motivation only
c) To be told to change by their clinician
d) None of the above
6. According to the article, which interdental cleaning aid do patients prefer and therefore show good compliance with?
a) Floss
b) Interdental brushes
caries and periodontal diseases: a scoping review. Australian Dental Journalhttps://doi.org/10.1111/ adj.12722
xi. Rösing CK, Daudt FA, Festugatto FE, Oppermann RV. Efficacy of interdental plaque control aids in periodontal maintenance patients: A comparative study. Oral Health Prev Dent. 2006;4(2):99-103. PMID: 16813138.
xii. Chapple IL, Van der Weijden F, Doerfer C, Herrera D, Shapira L, Polak D, Madianos P, Louropoulou A, Machtei E, Donos N, Greenwell H, Van Winkelhoff AJ, Eren Kuru B, Arweiler N, Teughels W, Aimetti M, Molina A, Montero E, Graziani F. Primary prevention of periodontitis: managing gingivitis. J Clin Periodontol. 2015 Apr;42 Suppl 16:S71-6. doi: 10.1111/ jcpe.12366. PMID: 25639826.
xiii. Bourgeois D, Bravo M, Llodra JC, Inquimbert C, Viennot S, Dussart C, Carrouel F. Calibrated interdental brushing for the prevention of periodontal pathogens infection in young adults - a randomized controlled clinical trial. Sci Rep. 2019 Oct 22;9(1):15127. doi: 10.1038/s41598019-51938-8. PMID: 31641199; PMCID: PMC6805917.
c) Woodsticks
d) None of the above
xiv. Department of Health & Social Care. Office for Health Improvement & Disparities. Guidance. Chapter 8: Oral hygiene. Updated November 2021. https://www.gov.uk/government/ publications/delivering-better-oralhealth-an-evidence-based-toolkit-forprevention/chapter-8-oral-hygiene [Accessed January 2025]
xv. Imai, Pauline & Yu, Xiaoli & Macdonald, David. (2012). Comparison of interdental brush to dental floss for reduction of clinical parameters of periodontal disease: A systematic review. Can J Dental Hygiene. 46. xvi. Christou V, Timmerman MF, Van der Velden U, Van der Weijden FA. Comparison of different approaches of interdental oral hygiene: interdental brushes versus dental floss. J Periodontol. 1998 Jul;69(7):759-64. doi: 10.1902/jop.1998.69.7.759. PMID: 9706852.
xvii. Langa, Gerson & Dantas, Pedro & Lemus, Gloria & Silva, Carlos & Meza Mauricio, Edwin & Muniz, Francisco. (2022). Effectiveness of interdental cleaning devices with active substances: a systematic review. Clinical Oral Investigations. 26. 1-15. 10.1007/s00784-021-04327-3. n
Faye Donald reveals how dental professionals can elevate periodontal care using the innovative PIEZON® technology and AIRFLOW PLUS Powder for minimally invasive, patient-focused treatment
The aim of this article is to explore the innovative technologies behind the EMS PIEZON® system and AIRFLOW PLUS Powder, highlighting their role in delivering minimally invasive, patient-centred periodontal care.
On completing this Enhanced CPD session, the reader wil:
• Gain insight into the scientific principles and key components of the PIEZON® system, including “No Pain” technology
• Learn about the clinical applications and benefits of the AIRFLOW PLUS Powder in biofilm and stain management
• Develop knowledge of the protocols for optimising outcomes when using PIEZON® and AIRFLOW technologies, including power settings, tip selection and technique
• Explore how these tools enable minimally invasive care for challenging cases, including implants, restorations, and patients with high clinical needs
• Recognise the impact of these technologies on improving patient comfort, preserving tissues, and reducing clinician strain.
Learning Outcome: A, C, D
The EMS PIEZON ® system, combined with AIRFLOW PLUS Powder, has ushered in a new era of periodontal care, defined by precision, patient focus, and minimally invasive treatment. At its core, the system integrates three essential components: the piezoceramic handpiece; the PIEZON ® PS Instrument; and the innovative “No Pain” dynamic feedback module. Together, they offer efficiency and precision in biofilm and calculus management:
1. Piezoceramic handpiece: generates tiny linear vibrations providing gentle and effective calculus removal without harming tooth surfaces or compromising patient comfort
2. PIEZON ® PS Instrument: this slim, versatile tip operates at speeds of 30,000 strokes per second, enabling deep subgingival access (up to 10mm) with minimal effort. Its design aids access and ensures maximum efficacy while preserving surrounding tissues
3. Dynamic feedback module: by adjusting power output 125 times per second based on calculus consistency, this module enhances treatment precision, increases patient comfort and reduces the risk of over-treatment.
For optimal performance, the three elements of the “No Pain” trilogy must work in harmony. When used correctly, calculus is removed through the piezoelectric effect, biofilm is disrupted by cavitation (as water meets the vibrating tip, collapsing bubbles release energy that destroys bacterial cell walls), and toxins are flushed from the pocket via acoustic
turbulence or lavage. This process ensures maximum comfort for the patient while prioritising tissue preservation.
Mastering the PIEZON ® and AIRFLOW technologies requires a thorough understanding of their capabilities and proper application. There is a key difference between supra- and subgingival calculus in terms of mineralisation; subgingival calculus is harder to remove due to its mineralisation and hidden location.
Effective removal depends on carefully considering factors such as power settings, tip selection,
Patient profile
angulation, adaptation, position, pressure, and movement. Mastering the use of PIEZON ® technology requires time, practice, and a commitment to developing these skills.
Key protocols include but are not limited to:
• Power and water settings: begin with a low power setting (no more than 3) to maintain minimal invasiveness, adjusting as needed. Ensure ample water flow to cool the instrument, enhance visibility, and support pathogen elimination through cavitation (a flow between 70% and 100% is recommended)
• Tip selection and adaptation: the PIEZON® PS tip is suitable for
most cases (95%), while additional tips like PSL, PSR, and PI Max (more on this later) are designed for specific clinical scenarios. Proper adaptation ensures effective scaling with minimal discomfort
• Gentle pressure and slow movement: light pressure (30 to 50 micrograms) and deliberate, overlapping strokes are essential for optimal outcomes. Allow the instrument to perform the work without excessive force.
The luxury of having the technology do the heavy work limits musculoskeletal strain on the clinician and improves clinical outcomes for the patient. Thanks to its slender design, perfectly linear
A 54-year-old female with a history of alcohol dependency presented with a heavily restored dentition, including porcelain veneers in the upper arch, along with eroded and fractured teeth in the lower arch. She exhibited sensitive teeth throughout, periodontal pockets with subgingival calculus, and general staining.
Treatment approach
The patient required non-surgical periodontal therapy (NSPT) to stabilise periodontal health before restorative work. Using the AIRFLOW PLUS Powder for biofilm and stain management, and the PIEZON® PS and PI Max tips for subgingival debridement, treatment was performed with an emphasis on tissue preservation. The patient’s nervous disposition necessitated a gentle and empathetic approach.
Oucome
All appointments were completed without local anaesthetic, and the patient responded positively to the treatment. Periodontal health was stabilised allowing full-arch reconstruction to proceed. The patient is now a regular attendee for maintenance appointments.



1. What is the primary function of the PIEZON® dynamic feedback module?
a) To reduce water consumption during procedures
b) To regulate power output based on calculus consistency
c) To increase the speed of the PS Instrument
d) To minimise noise during treatments
2. Which characteristic of AIRFLOW PLUS Powder ensures it is minimally invasive?
a) Its particle size of 14 microns
b) Its high water solubility
c) Its use of chlorhexidine as a preservative
d) Its gluten-free formulation
3. What is the maximum subgingival depth the PIEZON® PI Max Instrument can reach?
a) 5mm
b) 8mm
c) 3mm d) 10mm
movements, and intuitive technology, patients treated with the PS Instrument experience less perceived pain, less bleeding, reduced post-operative discomfort, and greater preservation of tissues and the epithelium.
4. What is the recommended power setting range to start using the PIEZON® system for minimal invasiveness?
a) 3 or lower
b) 5 to 7
c) 7 to 9
d) Any setting below 10
5. What material is the PIEZON® PI Max Instrument made from, and why is it suitable for use around implants and restorations?
a) Stainless steel – for its durability and strength
b) Titanium – to ensure longevity and resistance to wear
c) Composite resin – for its lightweight properties
d) Carbon-reinforced PEEK – for flexibility and surface protection
Building on the protocols for optimised outcomes, the PIEZON ® PI Max Instrument offers a solution for managing calculus around
challenging areas such as implants, crowns, veneers, composite bonds and orthodontic appliances. Made from carbon-reinforced PEEK, the PI Max combines flexibility, durability, and a slim design to access tight


spaces without damaging implants or restorations.
Operating up to 3mm subgingivally, the PI Max Instrument uses the same "No Pain" system, warm water, and controlled linear movements as the PIEZON ® PS Instrument. This makes it highly effective for removing calculus in areas where traditional biofilm disruption techniques may struggle, such as narrow gingival necks or around intricate restorations. For clinicians, this tool enhances precision and accessibility, delivering excellent results with minimal effort.
AIRFLOW PLUS Powder is central to tissue-sparing, pain-free Guided Biofilm Therapy (GBT), offering scientifically and clinically optimised properties for effective biofilm management. Its unique formulation ensures both efficacy and safety, supporting a wide range of clinical applications.
The ultrafine 14-micron powder effectively disrupts biofilm, stains and young calculus within a single session, all while avoiding tissue damage. This efficiency not only reduces treatment time but also enhances patient comfort and clinical outcomes.
The primary ingredients – erythritol, a natural polyol, and chlorhexidine, a preservative – further enhance its anti-cariogenic and bacteriostatic properties. Completely soluble, the powder is safe for most and suitable for a variety of patient needs, including those who are vegan, gluten-intolerant, diabetic, or following low-sodium diets.
The PIEZON ® system and AIRFLOW PLUS Powder exemplify the future of minimally invasive dentistry. By adhering to the principles of GBT and employing the right techniques, dental professionals can provide exceptional care while preserving the natural structures of the teeth and supporting tissues.
For more information and access to clinical research on these technologies, visit swissdentalacademyonline.com. n
About the author Faye Donald is an award-winning dental hygienist with a focus on patient-centred care and minimally invasive dentistry. She works in general and special interest practices in the north of England, is a Guided Biofilm Therapy Ambassador, and a Swiss Dental Academy Trainer.

When percussion, ice, heat and radiographs are not enough, electric stimulation may be the diagnostic tool you need for determining the cause of your patient’s discomfort. That’s where Parkell’s Digitest®3 comes in.
The Digitest®3 electrically stimulates the tooth to test for vitality, resulting in a value ranging from 0 to 64. Comparing the response of the suspected tooth with a known healthy tooth’s response to an identical stimulus helps you identifying the source of your patient’s pain, assess tooth vitality and, most importantly, test and follow up traumatized teeth. Thanks to an intuitive single button
Cleaning and disinfection of instruments is a vital step in any infection control procedures. The greener and less hazardous chemical components in Bossklein IDactiv make for a much safer solution for both the user and the environment.

operation, Digitest 3 is extremely easy to use. The three speed settings accommodate your personal preferences and the clinical situation. The device comes with four autoclavable probes to promote easy access to all tooth surfaces and operates by a standard, easy replaceable 9V battery.
Available in the UK through the main dental dealers. For further information contact Parkell Europe AB, Sweden, infoeurope@parkell.com. n

The Planmeca Viso G3 CBCT unit brings new features to the market including video-based FOV placement and a new generation sensor with an even better signal-to-noise ratio. There is also an optional back of the head support for more comfortable positioning and a Graphical User Interface which matches the style of the Plameca Romexis software for ease of use.
With a field of view (FOV) ranging from 3 x 3 to 20 x 10 cm, the unit not only offers high-quality 3D images of the entire dentition, but is able to capture detailed panoramic as well as extraoral bitewing images for interproximal diagnostics.

Combine this with Planmeca CALM - an algorithm which analyses and compensates for slight patient movements during 3D X-ray scanning resulting in sharper final images – and you’ll eliminate the need for re-takes. It is a truly multifunctional CBCT device covering all extraoral imaging needs from 2D to 3D imaging, and it’s available to order now! n
a sphere of its own!
Tokuyama are the only composite manufacturer to use patented spherical filler particles within their composite materials. Each variant utilising spherical particles of different diameters to maximise their optical and physical properties for the desired indication.
matching, high polishability and stain resistance.

Tokuyama’s development of spherical filler particles has culminated in Omnichroma, the world’s only colourless universal composite which matches every tooth colour no matter what the shade.
For more information call 0800 132 373 or visit www.bossklein.com n
Bossklein IDactiv easily removes organic debris through manual or ultrasonic cleaning with the additional benefit being effective against a wide spectrum of micro-organisms including TB. The proven ability to be used on a wide range of different materials ensures delicate instruments remain in prime condition. IDactiv contains plant based and biodegradable ingredients alongside naturally occurring amino acids. The modern formula is free from alcohol, chloride and PHMB. A mild fresh aroma is a pleasant change from other solutions with harsh odours.
The ADI Team Congress is an educational haven for all members of the dental team with an interest in implantology, offering a plethora of informative lectures.
Dr Cristian Dinu will be delivering a talk, entitled “Implants in the Aesthetic Zone – Key Factors for Success,” that offers an overview of the challenges facing dental professionals in the aesthetic zone. He notes:
“The talk will be useful for all, from surgeons to prosthodontists to technicians. It will navigate how bone, soft tissue and implants are pivotal factors we must consider and manage when we develop a predictable and reproducible protocol for successful treatments. We must not forget the rules of biology in our decisionmaking.”
“I hope attendees will join me in escaping from
the fear of the aesthetic zone as this will allow us to better control biological factors and obtain excellent treatment outcomes.”
“The ADI Team Congress is an essential part of the implant landscape; it platforms the newest trends, technologies and possibilities in implantology so that we are more successful and predictable in our work. I look forward to speaking and also catching up with some old friends!”
1-3 May, The Brighton Centre https://www.adi.org.uk/association_dental_ implantology_congress/delegates_prices n
Omnichroma Flow Bulk is a low viscosity composite which can be placed in 3.5mm increments. Like the other Omnichroma materials it delivers unprecedented colour
Dr Duncan Park, principal of Green Square Dental & Implant Centre, comments on the new Tapered Pro Conical implant from BioHorizons Camlog:
“The Tapered Pro Conical implant achieves excellent stability in a range of situations. It is comparable to the BioHorizons Camlog Tapered Pro implant both in terms of design, which affords primary stability, and of simplicity to place, but builds further on the design of the previous generation of products.
“The connection is based on the proven CONELOG design which has been available for over 13 years and is among the best available.ii The emergence profile lends itself to create a very nice curvature of the gingiva, improving the soft tissue adaptation for
It also has low polymerization shrinkage compared with other bulk filled composite materials.
For more information about the complete Tokuyama range, including Omnichroma Flow Bulk, contact your local Trycare Representative, call 01274 885544 or visit www.trycare.co.uk. n
exceptional aesthetics and cleansability.

“The design and material of the implant as a titanium alloy (Ti-6AL-4V ELI) also means it affords the strength required to ensure implant stability even when used in a smaller diameter, should the case demand it.
“In effect, it is the best of both companies –BioHorizons and Camlog.”
For product information from BioHorizons Camlog, please visit https://theimplanthub.com/ n
Optimise simplicity, choose efficiency, and deliver exceptional patient outcomes with the CS 7200 Neo Edition from Carestream Dental.
The ultra-compact imaging plate system is designed to deliver high-resolution images within a fast and simple workflow. Using the CS 7200 in practice allows clinicians to attain high-quality images and develop them to be seen in just 8 seconds. This means assessments can be completed quickly, whilst maintaining optimal detail for a confident diagnosis.
To enable such speed, the CS 7200 works with “Scan & Go” technology, which electronically identifies plates prior to each exam. Once used for a radiograph, the system recognises the images and
sends them to an appropriate computer and patient file, meaning multiple plates can be scanned in any order without the risk of mix ups.
For the multi-surgery practice, images can be dispensed to different clinicians, all using the high-quality imaging solution.
To learn more about the CS 7200 Neo Edition, contact the team today.
For more information on Carestream Dental visit www.carestreamdental.co.uk
For the latest news and updates, follow us on Facebook and Instagram @carestreamdental.uk n
Working with an experienced team of suppliers can be helpful to ensure you invest in the tools which are best suited for your practice’s needs and capabilities. Clark Dental has been working with dental professionals for 49 years, enabling them to achieve their practice goals and upgrade their equipment. One of the newest products in its portfolio, the Primescan 2 intraoral scanner, is the first cloud-native intraoral scanning solution, offering clinicians a simple and versatile option without compromise. Primescan 2 is your assistant in the early diagnosis of caries, using fluorescence and nearinfrared technology to identify carious tissue, with visualisation through DS Core helping your patients to better understand

the treatment required.
For more information about the range of products and services available from Clark Dental, visit the website.
For more information call Clark Dental on 01268 733 146, email info@clarkdental. co.uk or visit www.clarkdental.co.uk n
Patients needing a restorative treatment may have concerns over the aesthetic of their new smile. Eliminate those concerns by using BRILLIANT EverGlow™ from COLTENE.
A world-class composite suitable for both anterior and posterior restorations, BRILLIANT EverGlow™ achieves the desired aesthetic thanks to its exceptional polishability and superb blend-in properties. Its long-lasting brilliance will satisfy restorative patients as it is able to harmoniously integrate into the oral cavity with the application of just one shade. Its sophisticated shade system offers three translucency levels and enhanced Duo Shades that allow for a flexible use for single-shade and multi-shade layered

restorations. BRILLIANT EverGlow™ therefore provides dentists with numerous aesthetic possibilities, making it an invaluable part of a dental restoration.
A composite of immense versatility, BRILLIANT EverGlow™ is one of COLTENE’s many excellent restorative solutions. Perfect the aesthetic today.
For more on COLTENE, visit https:// colteneuk.com/email info.uk@coltene.com or call 0800 254 5115.n
colteneuk.com
An enjoyable oral hygiene routine means kids are more likely to be compliant with toothbrushing, setting them up for a longlasting and healthy smile. To achieve this, recommend the Baby and Kids’ oral care product range from Curaprox. Included in the range is the comprehensive selection of toothbrushes that come in a variety of vibrant, inviting colours. Each one has a small head and handle, making it easier and more comfortable for children to use. The use of extra-fine Curen filaments promotes a gentle feel whilst still being effective at removing plaque.
When paired with one of the flavoured kids’ toothpastes – mint, strawberry, or watermelon – brushing teeth can be a fun

experience. With both fluoride and non-fluoride options available, the toothpastes can reliably reduce the risk of tooth decay. By combining bright colours and pleasing flavours with excellent oral hygiene outcomes, the Curaprox Baby and Kids’ product range helps protect the smiles of the next generation.
For more information, please visit www.curaprox.co.uk and www.curaden.co.ukn
curaprox.co.uk
When you refer a patient to EndoCare for advanced endodontic treatment, you will experience a high-quality, efficient, transparent and collaborative process. Our endodontic experts and specialists will work with you to determine the best treatment solution for your patient, keeping you up-to-date throughout the procedure. With state-of-theart technology and evidence-based
techniques, our team ensures predictable results while optimising patient comfort during treatment.
Upon completion of the referred procedure, your patient will return to your routine care and we will remain available to support you if and when needed.
You can read our full referral policy on the website, or give us a call to find out more about how we work.
For further information please call EndoCare on 020 7224 0999 Or visit www.endocare.co.uk n
Eschmann remains the expert partner in decontamination for dental practices across the UK. Not only does the organisation provide some of the most reliable, efficient and robust infection control equipment in the industry, but it is also one of the very few to offer enhanced CPD user training as part of the Care & Cover service and maintenance package. This means your team can optimise compliance, keeping themselves safe while conducting high-quality infection control processes in-practice. It also allows them to maintain the essential equipment in order to prolong product life, maximise on your investment and minimise potential downtime. In addition, Eschmann are available to
The brand-new SprintRay Ceramic Crown is truly one-of-a-kind. A hybrid nanoceramic containing 51% ceramic for optimal strength properties, it’s MDR-approved as a Class II resin for definitive crowns, partial crowns and veneers.
The resin also features excellent marginal fit and is radiopaque to make it easily visible on radiographs.
When combined with the SprintRay Pro 3D Printer, the SprintRay Ceramic Crown optimises workflow efficiency – crowns can be printed in just 10 minutes, for a total treatment time of 45 minutes or under. Faster, more efficient workflows mean time and cost savings for you and your patients. This is also achieved with no compromise in quality of patient care, with highly accurate

provide expert support to your practice. From a technical support telephone line who help to fix a large portion of issues over the phone, to a nationwide team of 50+ Eschmann engineers, Eschmann provides added value and peace of mind to all the practices it supports.
Find out more today!
For more details of the decontamination support, enhanced CPD user training and equipment Eschmann offers, please visit www.eschmann.co.uk or call: 01903 753322 n

and predictable prosthetic outcomes consistently achievable. Discover the 3D printed chairside solution for definitive crowns from the only provider of a comprehensive digital 3D printing ecosystem for dentists – SprintRay. For more information, please visit https://sprintray.com/en-uk/n
The team at Dental Elite are a hardworking group of dental specialists, ready to help with any practice sale or purchase. Their extensive industry knowledge and experience allows them to offer tailored support to all clients, getting the result they need.
When it comes to the sale of a practice, Dental Elite use their intimate knowledge of the market to smooth the process for everyone.
As Ken Stalker recently said in a 5-star review: “Lottie McBean, Sales Progression Manager at Dental Elite, and her team helped to successfully navigate the sale of my practice, overcoming a number of problems along the way.”
Health Technical Memorandum 07-01 details the colour scheme all dental practices must use when segregating clinical waste.
Choose Griff Pac containers from Initial Medical as a solution that optimises waste segregation, whilst protecting clinicians, patients and the wider environment.
The Griff Pac is a sturdy, puncture-proof bin made from corrugated polypropylene, with an integral HDPE liner. This means that despite its light-weight, flat-packed structure, it is also seepage-proof, and minimises waste spillage.
It is also an eco-friendly solution, with a 25% reduction in CO2 emissions during production, and a 64% reduction in CO2 emissions from raw materials when compared to standard rigid containers.
From initial consultation right through to completion, Dental Elite has what it takes to help you through.
To find out more, contact the team today!

For more information on Dental Elite visit www.dentalelite.co.uk, email info@dentalelite.co.uk or call: 01788 545 900n

The containers are available in orange, blue, and yellow to support correct waste segregation and in line with HTM 07-01, ensuring your dental practice is compliant with the latest regulations.
When managing clinical waste in your dental practice, choose solutions you can rely upon. Contact the Initial Medical team for more details.
To find out more, get in touch at 0808 304 7411 or visit the website today www.initial.co.uk/medicaln
Should a patient phone the practice out of hours, seeking emergency care, providing an answerphone message which offers advice about managing pain can help them to minimise their symptoms until they can be seen. The Orajel range of pain relief products can help patients to effectively manage their pain at home whilst they wait for an emergency dental appointment.
Orajel Dental Gel delivers rapid relief from dental pain when and where it’s most needed and contains 10% benzocaine to reduce pain. For acute toothache, recommend Orajel Extra Strength. It contains 20% benzocaine, the maximum level available without a prescription in the

Orajel range. Orajel enables patients to apply the powerful local anaesthetic directly to the source of the pain, blocking pain signals along the nerves, numbing the area in just two minutes – faster that over the counter painkillers. Contact the team at Orajel to find out more about the benefits of the range to your patients.
For more information, and to see the full range of Orajel products, please visit https://www.orajel.co.uk/ n
Interdental cleaning is an essential part of maintaining proper oral hygiene. FLEXI interdental brushes from TANDEX are flexible and easy to use. FLEXI comes in 11 different sizes, and the brushes can be shaped and reshaped to help patients maintain optimal oral health in even the hardest-to-reach areas of the mouth.
Applying PREVENT Gel from TANDEX to FLEXI interdental brushes is easy! Not only does it add remineralising and antibacterial effects, it has a pleasant taste and non-abrasive texture, making it the ideal solution for even the most sensitive patients.
When guiding patients to employ the very best habits they will find easy,
Find support for your imaging solutions with CS Advantage from Carestream Dental, the premium service programme designed to meet your needs.
CS Advantage gives clinicians a number of exclusive benefits, including warranty extensions on your Carestream Dental solutions to protect your investments for longer.
Clinicians can also get in touch with the experienced support team who are on hand to answer your questions and discuss your challenges, whilst helping you master your imaging system. You gain unlimited access to online training modules via the Carestream Dental Institute, and receive technical help through live telephone support and/or
Dental Elite, one of the UK’s most successful dental business transfer agencies, is announcing the formal opening of a division specialising in advising dental lab owners.
This means Dental Elite is now one of the only big players in the dental practice space to have a service specifically catering for the transition of dental laboratories.
Headed by Lottie McBean, Sales Progression Manager at Dental Elite for nearly four years, the team will bring their expertise from the dental practice market to dental technicians.
Luke Moore, co-founder of Dental Elite, remarked: “It’s a natural progression. We have been approached numerous times over the years about labs but never had a specific

recommend FLEXI range with PREVENT Gel from TANDEX.
Find out more about the fantastic range of products offered by TANDEX today! For more information on Tandex’s range of products, visit https://tandex.dk/ Our products are also available from CTS Dental Supplies https://www.cts-dental.com/ n
Dr Chris David Donaldson recently established a new practice in Cobham – One Orthodontics – working with Clark Dental to design and kit out the space. He shares his experience: “The motivation for the project was to create a best-in-class orthodontic and dento-facial orthopaedics clinic, with a simple, functional layout and design.
“We chose to work with Clark Dental after engaging with a number of suppliers; they won the contract as they had a very personal approach and a ‘can-do’, problem solving attitude.
“Clark Dental worked with our project manager to find the best layout for the space that had been identified. They listened to our project manager’s vision for the clinic’s look and functionality; this was an interactive process
and guidance from Clark Dental at this stage made the whole process work.
“The equipment installation and training later went smoothly with any minor issues responsively fixed.

“The biggest challenge of the project was keeping the many work streams on track in order to meet our strict deadlines. I am very proud to have developed and built a business in the area I grew up in.
“I would absolutely recommend Clark Dental to others.”
Call Clark Dental on 01268 733 146, email info@clarkdental.co.uk or visit the website belown
email.
Remote support capabilities with your products also help problems be identified and resolved immediately.

To learn more about CS Advantage, contact the Carestream Dental team today.
For more information on Carestream Dental visit www.carestreamdental.co.uk
For the latest news and updates, follow us on Facebook and Instagram @carestreamdental.uk n
Following implant treatment, it can be all too easy for a patient to neglect the recommended post-surgery care. This reduces the longterm success of the treatment and must be prevented.
The Curaprox Implant Care Kit is an ideal solution to help patients look after their implants. Easily stored in one small pack, the kit contains a variety of products and a detailed leaflet on implant care, highlighting why they need even better care than natural teeth and demonstrating how the products can help.
With clear instructions, patients can better use Curaprox products like the CS 708 Implant / Ortho brush, ensuring that the implant surfaces are well-cleaned. The addition of mixed CPS interdental brushes further
promotes the effective removal of food particles around the implant, reducing the risk of peri-implantitis.
The Implant Care Kit offers clarity for patients who are unsure on how to maintain the success of their implant, amassing the very best Curaprox products for a masterclass in efficient oral hygiene.

To arrange a Practice Educational Meeting with your Curaden Development Manager please email us on sales@curaden.co.uk
For more information, please visit www.curaprox.co.uk and www.curaden.co.uk n
service to advise them. This new division deals with that issue.”

Lottie McBean commented: “I’m really excited to take this step to advise dental lab owners. I normally spend my days pushing solicitors and accountants to move faster or more cohesively in dental transactions. I’m really looking forward to taking this experience to the dental lab space”
Contact the team to find out more!
For more information on Dental Elite visit www.dentalelite.co.uk, email info@dentalelite.co.uk or call 01788 545 900 n
It’s vital to create a warm and welcoming atmosphere within the practice to make dentally anxious patient more comfortable. That means optimising everything from the overall design of your business to the décor and the equipment.

A poor work-life balance can impact the practice, increase fatigue and lead to a higher risk of burnout. To avoid this and understand the benefits of taking time out, attend the Business and Mindset Mastery course from IAS Academy.
Under the excellent guidance of marketing scientist Dr Prav Solanki, you will be taken through multiple goal-setting exercises. These demonstrate how to meet and beat your growth targets, both personally and professionally, without burning out.
The course will also focus on how health, wealth, career, downtime and recreation can interlink, and that managing
these equally will lead to a better you and a stronger business.

In the capable and experienced hands of Dr Solanki, the one-day course will combine intense learning with fun training, creating an ideal environment for dental practitioners to enhance their professional and personal lives. Banish burnout and reach your highest potential with this essential IAS Academy course.
For more information on upcoming IAS Academy training courses, please visit www.iasortho.com or call 01932 336470 (Press 1) n
Healthcare experts highlight concern over increasing cases of dry mouth
Find out more today.
For more detail about the solutions and services available from RPA Dental, please visit www.dental-equipment.co.uk, call 08000 933 975 or email info@rpadental.net n
For expert support in designing, installing and maintaining a new practice tailored to cater for any patients’ needs, turn to RPA Dental. The team has decades of experience in tailoring surgery design for the benefit of patients and professionals alike, utilising their stella knowledge of dental specific regulations and general design concepts to help you create a truly stunning practice. Known for exceptional customer service, they will help you select the right dental equipment, cabinetry and finishings for you, staying on budget and bringing your dream business to life. They also provide long-term servicing and maintenance for equipment to help you maximise on your investment.
A recent survey conducted by Oralieve among 573 healthcare professionals, with nearly 70% from the dental profession, reveals a significant increase in the number of cases of dry mouth they are seeing. Over 80% of respondents reported an increase in the prevalence of dry mouth, citing polypharmacy and an ageing population as the main contributing factors. While medication remains the most commonly recognised cause of dry mouth, the survey also identified other increasingly significant factors, including diabetes, menopause, mouth breathing, treatment for head and neck cancer, and Sjögren’s syndrome.
The survey also revealed that Oralieve
is the No.1 recommended brand for dry mouth relief by healthcare professionals. Oralieve Dry Mouth Relief products have been specifically designed to help supplement the natural protective enzyme system in saliva, to provide effective and lasting relief from the symptoms of dry mouth.

For more information on the survey findings and how the Oralieve range can help manage dry mouth, please visit https://www.oralieve-direct.co.uk/blogs/news n
When different patients have different needs, a variety of treatment options are required. By tailoring the care for each patient, better outcomes are ensured.
The Perio plus range of mouthwashes are emblematic of the Curaprox mission to create a better, healthier world; each of the three are exceptional at maintaining good oral health over a short-term use.
Perio plus Forte fights plaque buildup and reinforces the gingivae, making it ideal for patients before or after dental treatment because of its 0.2% chlorhexidine content. For combating xerostomia and regenerating the gingivae and mucosa, recommend Perio plus Regenerate to patients, whilst Perio plus Balance reduces the risk of tooth decay,
Discover SprintRay OnX Tough 2 for the latest 3D printing resin designed for fixed hybrid dentures and full arch implant rehabilitation cases.
It sets new standards in quality and durability with cutting-edge NanoFusion™ technology. As such, the resin features significantly higher flexural strength, flexural modulus and impact strength than other resins for dentures and implantretained prostheses on the market.
Supporting excellent aesthetics, it also mimics the natural dentition with just the right amount of translucency and opacity.
The SprintRay OnX Tough 2 is the ideal solution for long-term provisionals or even final restorations delivered on the same
making it a superb option for supporting orthodontic treatments or patients with impaired motor skills.
For patients in need of a short-term mouthwash, the Curaprox Perio plus range can be easily tailored for optimal results. Discover their benefits today.

To arrange a Practice Educational Meeting with your Curaden Development Manager please email us on sales@ curaden.co.uk
For more information, please visit www.curaprox.co.uk and www.curaden.co.ukn

day using guided surgery. It facilitates shorter treatment times, fewer practice visits, increased efficiency and lowered costs for both patients and clinicians to benefit from. In fact, it’s tough to beat! Find out more today.
For more information, please visit https://sprintray.com/en-uk/ n
The Advanced Diploma course from IAS Academy advances the orthodontic skills and knowledge of dentists to an unparalleled level.
Dr Anuschuka Beneke, from Cowplain Dental Practice, shares her experience:
“Having delved into Inman aligners, clear aligners and fixed brackets over the last 10 years, I wanted to take a step further and gain an even deeper knowledge so that I could provide more treatments for more patients.

challenging, with plenty to learn over a long period of time. But it is also fascinating and I am enjoying it a lot. Once you learn one thing, you realise how much more there is and then you want to keep learning.”
All dental practices are required to protect and safely manage sensitive patient data. Clinicians should choose Sensei Cloud, the dental practice management software from Carestream Dental, which is equipped to improve your cybersecurity measures.
which work to actively prevent and deter potential threats.
Dental professionals can also securely analyse their practice’s activities, with realtime dashboards updating live metrics on performance and finances before your very eyes. This allows clinicians to track their chosen key insights, and use them to make effective, informed decisions.

Sensei Cloud allows clinicians to schedule appointments and access crucial information on the go whilst remaining GDPR compliant. To ensure this data is kept safe, Sensei Cloud is supported by leading experts and state-of-the-art tools in cybersecurity
Dental practices can choose safer information storage with Sensei Cloud today. Contact the team to find out more.
For more information on Sensei Cloud visit https://gosensei.co.uk/ For the latest news and updates, follow us on Facebook and Instagram @carestreamdental.uk n
gosensei.co.uk
There is a huge amount to think about when designing your dental practice to optimise style, function and accessibility. That’s why it’s essential to enlist the technical expertise and support of specialists in the field, such as the team at RPA Dental.
They will help you design, install and maintain a practice that will ensure an exceptional patient and professional experience. Even the smallest details will be carefully considered, creating a comfortable environment for individuals with a vast range of physical and cognitive disabilities or impairments.
With state-of-the-art design software, an array of industry-leading equipment and
Food trapped in between teeth can cause embarrassment for your patients. Not only can it be visible to others, it can also lead to halitosis. This can cause your patients to become self-conscious in social situations, affecting their quality of life.

unparalleled knowledge of dentistry, RPA Dental will be by your side throughout the process from start to finish. Give them a call or visit the brand-new website to find out more. For more detail about the solutions and services available from RPA Dental, please visit the BRAND-NEW website www.dental-equipment.co.uk, call 08000 933 975 or email info@rpadental.net n
An effective oral hygiene routine can vanquish trapped food debris, helping to maintain a fresh breath that empowers patients to be confident in social situations every day. Trust TANDEX products today. For more information on Tandex’s range of products, visit https://tandex.dk/ Our products are also available from DHB Oral Healthcare https://dhb.co.uk/ n Learn,
“From the start of the course, the mentoring was very important. Professor Ross Hobson was a superb mentor and I could count on him to guide me and ensure that I was doing the right thing for the right patient. “I definitely recommend the course. It is
With the Advanced Diploma course, dentists can unlock new opportunities and enhance their career. Contact a member of the IAS Academy and discover the benefits of this course, and many others, today.
For more information on upcoming IAS Academy training courses, please visit www.iasortho.com or call 01932 336470 (Press 1) n
To combat this, recommend interdental cleaning with the FLEXI series of interdental brushes from TANDEX. Consisting of 11 different sizes, the range ensures that every interdental space can be accessed for optimal hygiene standards, removing the food debris that a toothbrush may struggle reaching.
An excellent supplement is PREVENT Gel, from TANDEX, which can be applied to a FLEXI interdental brush like a toothpaste. It contains 0.12% chlorhexidine for an antibacterial boost, protecting the oral cavity
from infection. With a pleasant taste too, the combination of PREVENT Gel and a FLEXI brush freshens the mouth for a reliable and enjoyable experience.

iasortho.com tandex.dk

Dr Rob Oretti, a prominent dental clinician, teacher and international speaker, comments on the MinerOss grafting material from BioHorizons Camlog: “I regularly choose MinerOss because the combination of cortical and cancellous particulate delivers fast yet controlled bone remodelling. Its rapid turnover to bone allows
a shorter overall treatment time, creating a stable environment in which to place an implant only months after augmentation. I have also received excellent support from the team at BioHorizons Camlog for the approximately six years I have been working with them.”
A comprehensive full range of clinicallyproven biomaterials is available from BioHorizons Camlog, designed to enhance treatment outcomes for a wide array of cases. Find out more today. For product information from BioHorizons Camlog, please visit https://theimplanthub.com/ n
At Lily Head Dental Practice Sales, our primary goal is to provide the best possible service to our clients.
That’s why we decided to move from Harbury to the heart of Leamington Spa, a five-minute walk from the train station. Our new location makes us conveniently placed for our clients and gives our team a comfortable, collaborative working environment.
Here’s our new address: 1 Spencer Yard, Spencer Street, Leamington Spa, CV31 3NE.
Our Director, James Head, shares his thoughts: “We’re in this interesting part of

Leamington Spa, which are really stellar developments. We want to have our people motivated and they will then do a better job which really helps our clients. There’s everything from churches to parks and Jephson Gardens is only a three-minute walk away. It’s fantastic, it’s beautiful. We’re very proud to be here and we think it’s a great home for everybody.”n

There are various signs that life is waking from its winter hibernation – lighter evenings, gambolling lambs and chocolate eggs. Another is the end of the tax year on 5 April 2025. This is a key financial date, as many allowances reset to zero and have a ‘use it or lose it’ feature attached to them. However, there are one or two exceptions to this, where some allowances can be carried forward. It’s, therefore, essential for dentists to understand the allowances available to them and their various limitations. The first is the Individual Savings Account (ISA) allowance. There is no option to carry forward any ISA allowances, so it’s important to use it before the end of the tax year. The annual limit is £20,000, which can be in one type of ISA or spread across the four different types (Cash, Stocks and Shares, Innovative Finance and Lifetime). Although, it’s worth noting that the Lifetime ISA has a limit of £4,000 per tax year up to the age of 50. Any interest, investment returns or capital gains from ISAs are tax-free. Another allowance that doesn’t allow you to carry forward is the Capital Gains Tax allowance. This allows you to make tax-free gains of up to £3,000. There is also the option for spouses and registered civil partners to transfer assets between themselves to utilise their annual exemptions, which can be very tax efficient.
One allowance that doesn’t get as much attention is the gifting allowance. This allows everyone to gift up to £3,000 per tax year without attracting any Inheritance Tax (IHT).
The good news with this allowance is that you can carry forward one year’s allowance if it hasn’t been used in the previous tax year. Therefore, you could potentially gift £6,000 in a tax year without any Inheritance Tax implications. In today’s climate and with a media spotlight on increasing IHT costs, this can be beneficial to factor into your financial plans.
One of the most tax-efficient ways of saving is through a pension, which has its own limit (the Annual Allowance).
In 2024/25, the Annual Allowance is the lower of £60,000 or 100% of your earnings. You can carry forward any unused Annual Allowance from the last three tax years, which means eligible individuals can make pension contributions well above the usual limit.
An important point to note here that is particularly relevant to dentists is that high earners may fall foul of the tapered Annual Allowance. This is where it gets complicated and it is important to consult an accountant and a financial adviser if you feel that this could be an issue for you, as it introduces two definitions of income – ‘threshold income’ and ‘adjusted income’.
Threshold income is your total taxable income minus certain deductions (like pension contributions), while
adjusted income includes pension contributions, including those from an employer (such as the NHS). The Annual Allowance is reduced by £1 for every £2 your adjusted income is over £260,000. However, this doesn’t apply if your threshold income is £200,000 or less. The minimum Annual Allowance is £10,000.
It’s important to remember that many dentists have benefits in the NHS Pension Scheme, whether they’re currently active members or deferred members. The “contribution” to a defined benefits pension scheme, like the NHS Scheme, isn’t based on actual contributions but on the scheme’s actuarial growth in a tax year, which can catch people off guard. Assuming that you have Annual Allowance available, making pension contributions is also an excellent method of regaining your Personal Allowance if you have lost some or all of it by earning more than £100,000 per annum. Your Personal Allowance allows you to earn up to £12,570 taxfree annually. However, once you earn more than £100,000, you start to lose this allowance by £1 for every £2 over £100,000 that you earn. Therefore, once you earn £125,140 or more, you will completely lose this allowance.
Pension contributions lower your taxable income, so they offer benefits both now and in retirement by reducing the amount of income tax you pay each year. It’s important
to remember that tax rules can be complex, and getting it wrong can be costly, so it’s essential to take professional advice based on your own specific circumstances before making any significant decisions to ensure that you spring into the new financial year in great financial health.
speak to a specialist
If you would like help with tax-efficient saving strategies, you can book a financial review with a dental Specialist Financial Adviser at Wesleyan Financial Services by visiting wesleyan.co.uk/ dentists or calling 0808 149 9416. Please note: Tax treatment depends on your individual circumstances and may be subject to change in future.
Inheritance Tax planning is not regulated by the Financial Conduct Authority. Charges may apply. You will not be charged until you have agreed to the services you require and the associated costs. Learn more about our charges at wesleyan.co.uk/charges. n
about the author simon cosgrove is a Dental Regional Manager at Wesleyan financial services, guiding a team of Dental specialist financial advisers to support dentists, their families, and their practices with financial planning to secure their financial future.



























































Most people think about buying a house for years before they even start viewing them – browsing online sales platforms, researching areas and using online mortgage calculators.
Buying a business is a much bigger decision, yet there are currently few online tools and no central marketing register due to confidentiality, making advance research much more difficult. However, you will still need to prepare for this decision some time in advance, so here are some of our top tips to help you prepare in the years prior to buying a dental practice.
1. Define your goals and vision
Before diving into the buying process, take time to clarify your professional and personal goals. Ask yourself:
• What type of practice do I want (NHS, private, mixed, general dentistry or specialist)?
• Do I prefer a rural, residential, or city centre location?
• What size practice am I comfortable managing?
• Am I looking for an established practice or a growth opportunity?
Having a clear vision will help you narrow down suitable options when the time comes to look on the open market.
2. Gain clinical and business experience
Owning a dental practice requires clinical expertise and strong business acumen. To prepare:
• Work as an associate to refine your clinical skills –lenders will usually require three years’ associate accounts for your loan application.
• Consider taking courses in practice management, leadership, advertising and financial management.
• Where possible, take on management responsibilities in your associate role for additional experience. Learning how to handle staff, patients and finance will benefit you greatly when you own your own practice.
3. build financial stability
Lenders want to see that you are already in a good financial position before they lend to you. Consider:
• Reducing debt: try to keep personal loans, car finance and credit card debt to a minimum, if any. Don’t be put off if you do have existing loans – a business loan can still be achievable.
• saving a deposit: try to aim for a 10% deposit where possible. 95%-100% funding is possible, providing you have an excellent overall financial position. However, lenders usually request anywhere between a 10-25% deposit.
• Maintaining reasonable living costs: the more you require to live on month by month, the more you will need to earn from the target practice to be able to service the loan repayment. As such, higher living costs will restrict the practices you can buy as some may not offer the level of profit you require to maintain your living costs in addition to your loan repayments.
• Maintaining a good credit score: A strong credit history will give you a better chance of securing a loan and, in some cases, offer you better loan terms.
4. understand the market
Consider market trends and conditions, such as:
• Population and demographics in potential locations –how does this fit with what type of income you want to generate?
• Competition in the area – if you are looking to grow private income, are there already practices providing the same treatments in the area?
• Current practice valuations and sales trends –consider attending a purchase seminar to get a feel for the practice sales market.
• Emerging technologies and patient expectations –consider if you are willing to purchase a practice that requires financial investment to update systems and processes.
5. evaluate potential practices carefully
Once you’re ready to start looking at practices, assess each opportunity carefully. Key factors to examine include:
• How the practice is valued: determine whether you are looking for a practice valued on an Associate Led or Principal Led model. Visit PFM Dental’s website to read our ‘Dental Practice Buying Guide for Dentists,’ which explains the difference between the models.
• accounts vs Prospectus: arm yourself with information about any assumptions made in the sales prospectus, such as cost reductions, principal
At Connect My Marketing, we have closely monitored, utilised, and implemented the growth of Artificial Intelligence (AI) in the dental industry. There are various benefits of the use of AI, especially with respect to dental practices engaging with patients and streamlining processes. AI-driven tools can enhance dental marketing by making it more personalised, efficient, and cost-effective. Among some of the most influential advancements are AI-powered chatbots and virtual assistants, which help dental practices generate leads and provide patient support around the clock. But how exactly do these tools improve patient engagement, and when is team intervention still necessary?
increased lead generation
For dental practices, generating leads and maintaining engagement is paramount. Virtual assistants respond instantly, answer common questions, collect patient details, and even schedule appointments. This realtime interaction increases conversion rates
by keeping potential patients engaged with tailored responses, without requiring manual effort from the practice. Personalising these interactions builds trust and strengthens relationships. AI tools can gather necessary patient information – such as their name, contact details, and dental concerns – and use this data to offer a more human-like experience. However, while AI excels at initial engagement, a balance between automation and human intervention is essential to maintain these relationships. AI can only take the conversation so far before a human team member needs to step in.
24/7 availability
One of the biggest advantages of AI-driven virtual assistants is their ability to operate 24/7. Many dental practices receive a high influx of patient enquiries daily, which can be overwhelming and difficult to manage. AI chatbots ensure that every enquiry is addressed, even outside business hours, capturing leads that might otherwise have gone unanswered or elsewhere. However, there are concerns about whether AI can replicate the interaction

income and property costs. If a prospectus model assumes a principal undertaking specialist treatment that you don’t have the skills for, you may not be able to purchase that practice.
• staff and operations: evaluate employee experience and office efficiency – e.g. who will manage the practice and do you need to computerise?
• facilities and equipment: determine if any major upgrades or renovations will be needed and when, plus if you have the cash to do these.
6. engage industry professionals
Having a dental specialist network of advisors to hand will provide you with valuable insights into the market and potentially give a greater opportunity to find the right practice for you. Consider having discussions with and/ or instructing a:
• Dental specialist accountant.
• Dental specialist finance broker.
• Dental specialist solicitor.
A strong support team will guide you through the complexities of purchasing a practice.
Preparation for a dental practice purchase takes time, consideration and financial planning. Ensure to engage with dental specialist advisors who have experience of the market and buying process alongside your own research.
At PFM Dental, we want every buyer to enter into their practice purchase with confidence and excitement, which is why we offer all of the purchase services under one roof. Please get in touch for a free, no obligation chat about your future purchase plans. PFM’s next ‘Preparing for a Practice Purchase’ seminar is on Wednesday 21st May in Leeds. n
about the author samantha Hodgson is a finance broker and practice valuer at PfM Dental.
of a real team member. While chatbots efficiently answer FAQs and book appointments, some patients prefer speaking to a human. We recommend using AI as the first point of contact while ensuring human touchpoints remain for more complex or sensitive conversations.
cutting costs and improving efficiency
AI helps reduce administrative workload and costs, which is a major benefit for dental practices. Virtual assistants free up staff time, allowing them to focus more on in-practice care. AI tools can also personalise responses, suggesting treatments based on the patient’s specific concerns. With multilingual capabilities, AI can broaden accessibility, reaching a more diverse audience. While the efficiency benefits of AI are significant, we always advise practices to use AI as a complement to their dental team, rather than relying on it entirely. A well-integrated AI system can enhance workflow, but human expertise remains irreplaceable when it comes to building long-term patient relationships.

How beneficial are ai virtual assistants for dental marketing? From our experience, AI virtual assistants are transforming dental marketing by boosting lead generation, improving accessibility, and reducing operational costs. The personalisation achieved by AI assistants enhances patient interactions, helping dental practices refine their marketing strategies and connect better with potential patients.
However, the key question remains: Does AI truly enhance the patient experience? The answer lies in balance. While AI can handle repetitive tasks efficiently, human interaction is still vital for building trust and ensuring patients feel valued. By strategically integrating AI into a dental practice’s marketing efforts, we can create a seamless, patient-centred experience that blends automation with personal care. n
about the author Meg stables, Marketing assistant at connect My Marketing.

Rhys Jones outlines the essential steps dental practices must take to ensure electrical safety, minimise risks, and stay compliant with regulatory requirements
Electrical safety is a fundamental aspect of running a dental practice, yet it can often be overlooked. Failing to maintain electrical equipment or address hazards can put patients, staff and the practice itself at serious risk.
Regulatory bodies expect dental practices to meet strict safety standards, and non-compliance can lead to enforcement action, invalidated insurance or even legal consequences.
Therefore, taking a proactive approach ensures not only compliance but also a safer working environment for everyone.
Why electrical safety matters
From dental chairs and autoclaves to IT systems and compressors, modern dental practices rely on a range of electrical equipment. A failure in any of these systems can cause significant disruption and create hazards such as electric shocks or fire risks.
Regulatory bodies such as the Care Quality Commission (CQC) in England and Healthcare Inspectorate Wales (HIW) expect dental practices to demonstrate that their premises and equipment are safe. The Electricity at Work Regulations 1989 outline the legal responsibilities, requiring businesses to ensure electrical systems are properly maintained and do not pose a danger.
Practices that fail to meet these standards could face regulatory action, invalidated insurance policies, or even criminal or civil legal proceedings if an incident occurs.
What practices need to do
A structured approach to electrical safety reduces risk and ensures compliance. One of the most important steps is scheduling regular fixed wire inspections, known as Electrical Installation Condition Reports (EICRs). These should be carried out by a qualified electrician at least every five years. The assessment checks the integrity of a practice’s electrical systems, identifying potential hazards such as outdated wiring, overloaded circuits or faulty installations. Addressing any issues promptly can prevent more serious problems in the future.
Portable Appliance Testing (PAT) is another key element of electrical safety. While not a legal requirement, it is widely regarded as best practice and is expected by regulators as evidence of compliance. PAT helps identify faults in portable electrical equipment such as curing lights, autoclaves and IT devices. High-risk appliances should be tested annually, while lower-risk items may only need testing every two to three years, depending on usage and wear.
Meanwhile, overloaded extension leads are a common safety issue in dental practices. Many practices rely on them without considering the load capacity, which can lead to overheating and fire risks. Most extension leads have a maximum load of 13A, yet high-energy appliances such as kettles, microwaves and toasters can easily exceed this limit if used in an extension lead simultaneously. Ensuring that high-power appliances are plugged directly into wall sockets rather than extension leads is a simple but effective way to mitigate this risk.
Regular visual inspections can also help prevent electrical hazards. Frayed cables, cracked plugs, loose sockets or signs of overheating (e.g. burn marks or discolouration) should be addressed immediately. Any appliances found to be faulty must be taken out of use until they are repaired or replaced. The truth is that while formal inspections are essential, everyday awareness among the dental team plays a crucial role in identifying potential dangers before they become serious problems.
Ensuring compliance with the right expertise
Electrical testing and maintenance should only be carried out by professionals with the right expertise. When selecting a contractor for EICRs or PAT testing, practices should look for those registered with schemes such as the National Inspection Council for Electrical Installation Contracting (NICEIC) and the Electrical Contractors Association (ECA). These certifications provide reassurance that the work will be carried out to the required standards.
For some practices, particularly smaller ones, there may be concerns about the cost of regular inspections and maintenance. However, delaying essential checks often leads to higher costs in the long run. An electrical system that is well-maintained is less likely to require expensive emergency repairs, and a proactive approach reduces the risk of unexpected failures

that could disrupt the practice. PAT testing, in particular, is relatively inexpensive, with costs as low as £0.80 to £2 per appliance, making it a cost-effective way to demonstrate compliance.
Maintaining clear documentation is also vital. Keeping detailed records of all inspections, PAT tests and maintenance work provides a clear evidence trail for regulators and helps practices stay on top of their compliance responsibilities. Having a structured system in place for scheduling checks and recording results ensures that electrical safety remains a priority rather than an afterthought.
Have a compliance question?
Send it to compliance.hotseat@agiliosoftware.com and it could be featured in a future Compliance Hotseat We may even get in touch to discuss it further.
For more details on iComply, visit agiliosoftware.com/icomply


About the author Rhys Jones is Head of Compliance at Agilio.




















‘’A Banker is a fellow who lends you his umbrella when the sun is shining, but wants it back the minute it begins to rain’’ – Mark Twain

Mark Twain’s views on the world of finance were directed at US Banks in the 19th century. However, there is, within these words, a reminder to add Funding Risk to Cyber Crime, Data Protection and a host of other risks that you have to manage as a busy entrepreneur.
identifying potential business risk in your current funding
Now, I should emphasise that I am not proposing that a fresh banking crisis is around the corner. However, what I am going to suggest is some simple steps that you might want to take over the next few months to run the rule over your existing funding arrangements, explore any potential business risks and, if necessary, formulate some mitigating actions.
Organising your business risk and facility agreements
Firstly, make sure that you have hand-signed hard and soft copies of all facility agreements for senior debt, Covid-related facilities, shortterm business loans and asset finance facilities. In our experience, there are always gaps, which can present hidden business risk. It is good practice to maintain a summary schedule of all these agreements – the original amount borrowed, purpose of the funding, date drawn, current monthly repayments, interest rate, exit fees if applicable, and the final
repayment date. Keep abreast of the cash flow implications of adding to this list of agreements – particularly new agreements with relatively short repayment terms. Include any cashflow funding against contracted income or credit card receipts. If your facilities are subject to Financial Covenants, these could include, for example, a minimum tangible net asset position, debt service minima, and loan-to-value maxima, among others. Make a note of these on your schedule and establish a system to check compliance both on a ‘look-forward’ basis and by measuring against actual results to help manage any business risks associated with covenant breaches.
Secondly, examine the commitment clauses – those conditions in the agreement that determine whether the agreement can be terminated, and under what circumstances. Medium Term bank loans may have a set commitment period that is shorter than the repayment term. Record the date when the commitment period ends on your schedule and make a diary note for six months prior, perhaps even 9-12months prior. This gives you valuable time to explore the lender’s appetite to renew the facility for a further period and what conditions and pricing might apply.
addressing potential business risk with your lender
Next, think back to the last substantive meeting you had with your main funder. How long ago was that meeting? What was discussed? Have you kept the Bank informed of all material developments in the business since that date? If there have been changes, then it may be time to ‘refresh your business story’, anticipate any questions or concerns the bank may have about the financial performance of the business and its direction of travel. It is not advisable to leave this type of conversation to the final few months of the commitment period.
banking relationships
How do you rate the strength of your banking relationship? Has there been frequent and/or recent changes in your relationship team? How well networked are you within the Bank? For example, have you met the line manager of your main relationship contact, or anyone else at a senior level who knows you and your business?
Have you formulated a Plan B should your lender exhibit any cooling towards your business sector? Bank credit appetite can be tidal – you don’t want to be left high and dry on the beach. Examining any business risk takes time to analyse, quantify and formulate actions. It can be an unwelcome but perhaps necessary diversion from growing your business and other priorities. You probably have
a lawyer to advise you on property and employment matters, and an accountant to prepare your accounts and calculate your tax liability. You may also have a wealth manager.
The role of a debt advisory firm in managing business risk
A specialist corporate debt advisor should also be an important member of your professional support team. Debt Advisory firms traditionally served the large and Mid-Corporate market segments. This expertise is increasingly available in the SME market. Navigating the debt markets remains a challenge for all business owners – an experienced debt advisory firm will develop a deep understanding of the business of your business and your objectives, and is therefore equipped to tell your business story, present your financial results and discuss your business objectives and the finance required to deliver them. They will have hands-on experience of raising finance for a whole range of transactions and their extensive banking network will enable them to select the most appropriate banks to approach for your specific requirements. A competitive tender process will ensure you get the most competitive terms. n
about the author
Martin How, Managing Director, Lily Head finance Debt advisory services.







www.practiceplan.co.uk
You have the dream practice
– a great team, just the right services for your location, your marketing brings in a lot of transactional dentistry, and your EBITDA (earnings before interest, taxes, depreciation, and amortization) is enviable. There’s even room for growth. So why does it feel like corporates are snubbing you when you go to sell your practice?
To answer this question, we used our market insights to look at purchasing criteria trends for larger dental groups. It is helpful to understand the history of corporate mergers and acquisitions within the dental market, how they have developed, and what this means for you.
A brief history of corporate acquisitions
The Dental Act changes in 2006 allowed for more corporate investment in the dental space. This was a highly competitive environment, and an EBITDA land grab followed. Purchasers were backed by private equity, who at that time took a short-term approach to acquisition – churning out buys and buy-and-builds over 3 years. However, this changed after some notable casualties due to the NHS recruitment crisis. Private equity firms faced being unable to sell businesses that couldn’t meet targets.
Apprehension around problems like this have resulted in corporates
prioritising sustainability. They are now locking in responsibility and accountability through deferred consideration. Their margins are such that many will likely look to buy at no more than 7.5x and will lock in an exit EBITDA multiple of 12x. With head office costs, slippage and investment costs totalling at least 2x, this will leave them with 2.5x, which they will want to leverage and develop as much as possible.
Where does this leave you?
A very talented, high-grossing associate will have been a great asset to the success of your practice, but to a corporate this presents a risk. Associates could leave after a significant change like a merger or acquisition, taking EBITDA with them. In areas where recruitment is a challenge this is a significant challenge. Not only can you not achieve the profits that gave you positive EBITDA calculations, your healthy marketing budget and any specialisms promised but not achievable, could become a liability overnight.
Risks posed to a corporate by your successful associate, or certain specialisms will prompt them to offer a lower EBITDA multiple. You may well be better off holding on to the practice for 2 years, pocketing the profits, then selling to a tier 4 buyer (4-10 practices) with a lower exit deal, but without all the stringent deal terms.

While on paper, deals can look fantastic, the reality is more complex. Within your deferred consideration will be pressure to ensure business continuity, and that the 2.5x margin can be met and softened. You can receive significant bonuses from some corporates if you do so. However, before selling, you should be very confident you can bring in those additional funds so you don’t lose out.
The average 30% deferred consideration plus any bonus comes out of your hard work over that time. The corporate doesn’t borrow to secure this money for you, so their initial 70% outlay is their only investment. If you do want to sell to a corporate, finding a trustworthy buyer recommended by others, who is open to ideas to decrease risk, will create a far greater chance of a successful transition.
With a month left until the end of the current tax year, it’s important that all dentists get their ducks in a row. The 5th April will be here before you know it, and as is true of all financial aspects, it is better to be prepared ahead of time than risk the dreaded last-minute panic.
Dentists can claim a number of deductions from their declared profit for various costs associated with working in or running a dental practice. Like anything that involves HMRC, the rules must be followed meticulously and carefully to avoid falling foul of the regulations, which is why so many individuals work with an accountant or independent financial adviser (IFA). It is also vital to ensure that the ‘wholly, exclusively and necessary’ rule can be applied – the expense must have been required specifically for work and for no other reason, and it must have been essential to allow you to do your job.
Potential deductibles include professional indemnity, membership of professional associations, marketing
costs, training and educational expenses, phone and internet bills, and accountancy fees. All should be documented clearly to show the associated costs, which can be used to recalculate your taxable profit.
Applicable to the wider population, it is important to maximise on your general allowances in order to optimise your finances for the end of the tax year. For example, check that you are utilising your full ISA Allowance of £20,000.
It is also necessary to leverage your Pension Contributions Annual Allowance to ensure that you are saving the maximum amount that qualifies for tax relief. The Annual Allowance is currently £60,000, with tax relief available for a sum equal to your income or £3,600 (whichever is higher). The Annual Allowance is tapered for higher earners, reducing by £1 for every £2 a person earns over £260,000, capped at £10,000. It can also be beneficial to check National Insurance Contributions (NICs) to ensure you are not

Who is actually buying?
Tier 1 groups often own hundreds of practices, and represent only 4% of the activity Dental Elite acted on last year. 70% of the sales in our goodwill report were to independents buying their first, second or third practice. Over the last year, we have also seen a rise in tier 4 buyers. The mid-market section represents about 24-26% of sales.
Dental Elite is a team of specialist dental experts with all the skills and knowledge needed to closely support all clients – whatever their goals within the dental market. Arm yourself with the knowledge you need to make your sale smooth, successful, and profitable with Dental Elite.
Before taking your business to market, a detailed understanding of your options, informed by expert advice will save you from taking unnecessary risks. Instead of chasing a corporate that calculated your practice is too good for them, you may decide to pursue a deal that leaves you far better off overall.
For more information on Dental Elite visit www.dentalelite.co.uk, email info@dentalelite.co.uk or call 01788 545 900
About the author Luke Moore is one of the

overpaying. This is especially important for self-employed associates or dental hygienists/therapists, whether working in NHS dentistry or private. Adjustments will often need to be made in the tax return to ensure any excess NICs are reclaimed.
When it comes to completing your tax return, the document itself can be complex and time-consuming. Mistakes or misunderstandings can prove costly further down the line if your return gets rejected or investigated by HMRC, creating further and unnecessary stress for you. Enlist the help of IFAs such as those at money4dentists to avoid this hassle and gain peace of mind that your tax year ends smoothly. They will review your finances to ensure you are maximising on all the allowances and tax relief options available to you, looking after your current and future financial stability.
For more information, please call 0845 345 5060 or 0754DENTIST.
Email info@money4dentists.com or visit www.money4dentists.com















•



























• Carry out supra and subgingival instrumentation



• Use a combination of our products if surgical intervention is required
• Continue to monitor and support the patients’ oral health throughout their life






























































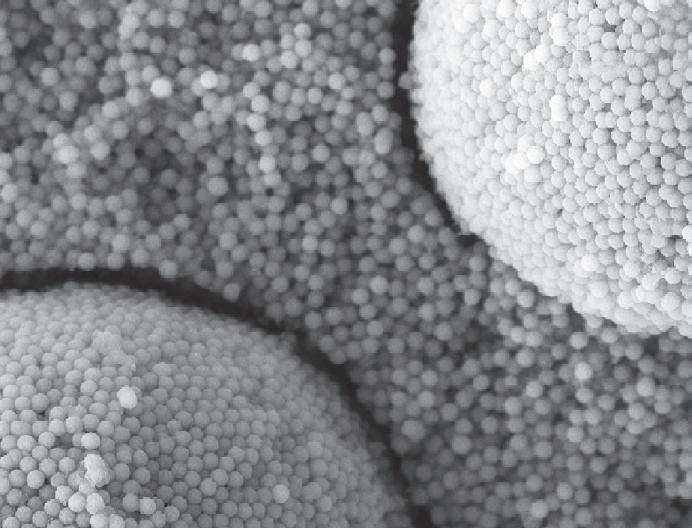





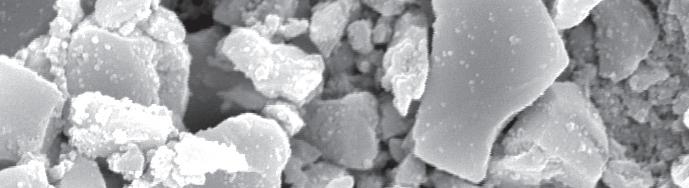



































Bis-GMA-free formulation: for better biocompatibility
Easy stocking: only 1 shade for economic sustainability

Structural shade without artificial colour pigments: adapts seamlessly to any tooth shade from A1 to D4


