September/October



September/October


The Curaprox Implant Care Kit contains everything patients need to care for their implants a er surgery and for ongoing maintenance and protection.






















































Rates: UK £39.95 per year; Overseas £83 - all cheques in sterling drawn on a UK bank made payable to ‘Smile’. 8 issues including 16 hrs CPD £39.95

Published by Purple Media Solutions
The Old School House, St Stephen’s Street Tonbridge, Kent TN9 2AD Tel: 01732 371 570
James Cooke T: 01732 371 581
E: james.cooke@purplems.com
Follow us : @SmileOHMmag
t’s been a big year for the British Society of Hygiene and Therapy, which has been celebrating its 75th birthday throughout 2024. To commemorate the milestone, the middle of this issue of Smile has been given over to the BSDHT’s members’ magazine: Dental Health . From page 23, you will find a preview of the Society’s publication that brings us Nick Coller’s Happy Birthday BSDHT Q&A, with answers provided from across the BSDHT membership.


Managing Editor James Cooke james cooke @purplems.com Tel: 01732 371 581
Commercial Director Gary Henson gary.henson@purplems.com Tel: 07803 505208
Production and Designer 1 Lorna Reekie lorna reekie @purplems.com Tel: 01732 371 584
Production and Designer 2 Rob Tremain rob.tremain@purplems.com
All of us here at Smile would also like to congratulate the BSDHT on three quarters of a century. Here’s to the next 75 years







There’s plenty more to find in this issue, including four hours of CPD content and a review of ISDH, which took place in Seoul this year – Miranda Steeples was there and provides the words and images from South Korea.
As always, enjoy the magazine!

been made to ensure that the information in this publication is correct and accurate, the publisher cannot accept liability for any consequential loss or damage, however caused, arising as a result of using information printed in this magazine. The views expressed in Smile OHM Magazine are not necessarily the views of the magazine, nor of Purple Media Solutions Editorial Advisory Board: Dr Barry Oulton, B.Ch.D. DPDS MNLP; Dr Graham Barnby, BDS, DGDP RCS; Dr Ewa Rozwadowska, BDS; Dr Yogi Savania BChD, MFGDP; Dr Ashok Sethi, BDS, DGDP (UK), MGDS RCS; Dr Paroo Mistry BDS MFDS MSc MOrth FDS (orth); Dr Tim Sunnucks, BDS DRDP; Dr Jason Burns, BDS, LDS, DGDP (UK), DFO, MSc; Prof Phillip Dowell, BDS, MScD, DGDP RCS, FICD; Dr Nigel Taylor MDSc, BDS, FDS RCS(Eng), M’Orth RCS(Eng), D’Orth RCS(Eng); Mark Wright BDS(Lon), DGDP RCS(UK), Dip Imp Dent.RCS (Eng) Adv. Cert, FICD; Dr Yasminder Virdee, BDS.


in association with:

Other titles include:
Divisional Administrator Francesca Smith francesca.smith@purplems.com Tel: 01732 371 570
Circulation Manager Andy Kirk
Managing Director Ed Hunt ed.hunt@purplems.com Tel: 01732 371 577



The Association of Dental Groups (ADG) launched a new report in September. ‘Patients First’ details seven core recommendations for Government that, “if implemented, will transform the experience for dental patients in every corner of the United Kingdom.”
The report was presented in Parliament on Wednesday 11 September to MPs and Peers from across the political aisle, as the ADG seeks to work with the new Government to improve dental care across the board. The ADG’s seven recommendations, most of which can be actioned in the short term without legislative change and with no cost to Government, are as follows:
1. Commit to support recruitment: Accelerate long-term workforce plan and unlock barriers preventing high-quality international dentists registering
2. Use commissioning solutions: To meet the needs of the population and roll out examples of successful flexible commissioning
3. Plan the workforce: Recognise the relationship between the mixed economy, skill mix and devolved nations
4. Invest in community prevention: Support water fluoridation, have policies for sugar reduction, hold Integrated Care Boards/ LA/ NHS to account for delivering community preventative schemes like supervised toothbrushing
5. Renumerate practice-based prevention: Offer realistic remuneration and promote flexible commissioning for practice-based prevention.
6. Protect the dental budget: Ringfence the budget and require ICBs to have a clear plan for dental underspend.
7. Support the retention of the workforce: Continue to reform the dental contract and ensure that pay review processes are transparent.
Neil Carmichael, Chair of the ADG and former MP explained that: “Our recommendations are centred around increasing the numbers of dentists working in order to provide better access for patients. Just 100,000 more dentists will create 750,000 more appointments, massively improving access for so many patients in dire need, and reducing pressure on NHS services elsewhere. We stand ready to support the new Government in putting patients first.”
When Parliament adjourned, the ADG was joined by MPs, representatives from various dental associations and press, for a launch event in Terrace

Dining Room A of the Houses of Parliament. among the speakers was Tom Whiting, Chief Executive and Registrar of the General Dental Council (GDC). “We welcome the ADG’s discussions about access for patients, oral health and creating a sustainable dental industry,” he said. “There is evidence that the recovery of dental services after the pandemic has not only stalled but may have gone into reverse. We believe that this needs urgent attention.
“If we want more dentists and other dental professionals, there needs to be a multi-point plan for the capacity needed to train them.”
The GDC Chief Exec went to on to explain that the supply of UK qualified dentists is fixed in the short term but that inquiries have been received by the
regulator from those seeking to establish new dental schools. He added that the GDC has tripled the number of places for part 1 of the ORE and increased capacity of the Part 2 exam by a third. “We are currently tendering for more capacity for next year.”
There is, however, no guarantee that increasing international registrants will solve the challenge of delivering NHS care. “Once a dentist is registered with the GDC, where and how they work and whether they provide NHS or private treatment is a matter for them,” Whiting explained.
“Furthermore, for the longer term, there’s a real need to modernise the legislation we work under –so that we can protect patients and support dental professionals effectively,” he concluded. n
Dental teams in the UK may help to detect the early signs of Type-2 diabetes, as new research aims to validate routine screening during oral health check-ups.
Diabetes is one of the most common chronic conditions in Europe and is widely recognised to have a strong link with severe gum disease (periodontitis). An estimated one in three people living with diabetes remain undiagnosed, with over 1 million undiagnosed in the UK alone. Left untreated, diabetes can lead to long-term complications or can be life-threatening.
Recognising this link, researchers at the University of Birmingham have secured funding from Haleon, the global consumer health company which owns oral health brands like Sensodyne, Corsodyl and Polident, and the support of the National Institute for Health and Care Research (NIHR) Birmingham Biomedical Research Centre (BRC), to continue the development of a new care pathway for early

case detection of Type-2 diabetes and prediabetes in high street dental practices.
In a study published in 2023, the group at the University of Birmingham comprising Dr Zehra Yonel and Professors Iain Chapple and Thomas Dietrich teamed up with Professor Laura Gray
from the University of Leicester to develop a new score called the Diabetes risk assessment in Dentistry Score (DDS), for use by dental teams to detect pre-diabetes and diabetes in dental settings.
As part of a recent pilot study called INDICATE, funded by NIHR and Diabetes UK, the DDS was used in conjunction with a finger-prick test for diabetes, called the HbA1c test. The INDICATE trial, which engaged 13 dental practices and 805 dental patients, found that almost 15% of people walking through dental practice doors perceiving themselves to be healthy, exceeded UK pre-diabetes / diabetes thresholds (≥ 42mmol/mol HbA1c).
Now, thanks to funding from Haleon and NIHR, INDICATE-2 will work with 50 dental practices across England and Scotland to screen more than 10,000 patients and develop a care pathway that could help health services detect and treat many more people with undiagnosed diabetes in the UK. n



Get discount when you Trade-in you current IOS scanner model from a different brand*, to and award-winning TRIOS 5 £6,350











3Shape makes it easy for you; just reach out and we’ll ensure a seamless Trade-in process. Take advantage of this exclusive PROMO and Trade -In to a new TRIOS 5.

Scan to know more GET £6,350 OFF WHENTRADEIN

Should you have any questions, please contact your Resellers or your 3Shape Sales specialist at sales@3shape.com *Terms and conditions

If you want to know more about 3Shape, please visit www.3shape.com

In a candid chat, BSDHT President Miranda Steeples shared her journey, the importance of succession planning, and why stepping into leadership roles is a game-changer for dental hygienists and dental therapists

What initially inspired you to stand for a role within the BSDHT?
Miranda: It all started about ten years ago when I saw a shout-out on social media from the South East regional group. They needed a new treasurer, and I remember thinking, “Someone really needs to do that; it would be a shame if the group couldn’t continue.” And then it hit me - why not me? I was already looking for a way to be part of something bigger, to make a difference. That initial step led me to stand for the Honorary Treasurer role and eventually for President Elect. It’s funny how just one decision to get involved can set you on an incredible path.
How do you think progressing through different roles has shaped the future of BSDHT?
Miranda: The great thing about the BSDHT is that there are so many different ways to get involved, and each role brings something unique to the table. We have this continuous flow of new people, ideas and energy, which keeps us fresh and relevant. We make a point of consulting with our members regularly to see what they care about and what they want us to focus on. This means we’re not just moving forward indiscriminately; we’re driven by what our members need and want.
There are quite a few positions up for election this year. How do you think new members and ideas can impact the Society?
Miranda: It’s super exciting! This year is packed with opportunities for members to get involved, from regional groups to council roles. We’re even welcoming representatives from the Education Group and the Diversity, Inclusion, and Belonging Group to the Council, which broadens our focus in a big way. It’s like a breath of fresh air when new
people come in. They bring different perspectives, new ideas, and it keeps us on our toes. You never know where the next great idea will come from, and that’s what makes it all so dynamic.
What are some of the benefits of putting yourself forward for these roles?
Miranda: Oh, there are so many! On a personal level, it’s a fantastic way to connect with likeminded professionals. Let’s be honest, working in practice can sometimes be a bit isolating, but the BSDHT is like having an extended family. The more you put into it, the more you get out of it, just like any good relationship. Professionally, you’re right at the heart of the latest news and developments, and you get to shape the direction of the Society. Plus, it looks great on your CV and shows that you’re committed to your profession.
Succession planning is obviously key. How does the BSDHT make sure there’s a smooth transition when new leaders step in?
Miranda: We’ve got this down to a bit of a science, really. There are clear pathways, guidance documents, and handovers to make sure new leaders feel supported. Outgoing members usually provide handover sessions, and they’re often happy to be a sounding board, if needed. Plus, the Head Office team is always there with loads of knowledge and support. It’s like having a safety net - no one is expected to go it alone.
Beyond the top roles like President, how important are other positions like Honorary Treasurer or Student Rep Coordinator?
Miranda: Every role matters. I like to think of the Society as one of those beautiful old clocks with all the cogs working together. Each piece, no matter
how big or small, plays a crucial role in keeping things running smoothly. The President might be the figurehead, but, without the rest of the team, nothing would get done. It’s a real team effort, and that’s what makes it so special.
What would you say to someone considering stepping up for a role?
Miranda: Just do it! Seriously, it’s one of the best decisions you’ll make. You’ll meet amazing people, learn new skills, and you’ll be part of something that’s bigger than just your dayto-day work. It’s not just about helping the BSDHT. It’s about giving back to your profession, setting an example, and maybe even inspiring others to follow in your footsteps. You never know, you might be the one who sparks the next big change in our field. And honestly, the experiences you’ll have, the friendships you’ll make, and the personal growth you’ll go through, are things you just can’t get by staying within the four walls of your practice.
Before we wrap up, is there anything else you’d like to share with the BSDHT community or those thinking of joining?
Miranda: I just want to say a massive thank you to everyone who’s been involved with the BSDHT, past and present. It’s the passion, generosity, and drive of our members that keeps this Society going. And if you’re not already a member, why not join us? It’s a fantastic community with so much to offer. Whether you’re looking for professional support, new friends, or just a way to give back, the BSDHT is your place. Let’s keep it moving forward together! n
For further details, please visit bsdht.org.uk

According to the paper Artificial intelligence and personalised diagnostics in periodontology: A narrative review1
“Although periodontal diseases share a multifactorial aetiology, it is essential to acknowledge that personalised diagnostics in periodontology is still in its primitive stages.” The authors highlight “patient participation” as one of the key challenges. AI is already making its mark in dentistry by enhancing workflows and optimising diagnostics, such as AI-driven X-ray detection and treatment planning. However, in a profession traditionally slow to embrace change, these advancements may seem gradual. Even in this exciting era of digital empowerment, patient education remains the cornerstone of effective care.
Tailoring treatment plans to unique needs is central to Sakina Syed’s clinical approach. An awardwinning dental hygienist and therapist at Bupa’s London Bank practice, she advocates for integrating new technologies into periodontal treatment— provided they have a solid evidence base.
“Dentistry is still far from fully embracing AI,” Sakina observes. “As an industry, we aren’t fully incorporating AI to create highly personalised periodontal treatment, though some practitioners are leading the way. For example, general healthcare metrics like weight and blood pressure are standardised across professionals, but periodontal disease is caused by an imbalance in the oral microbiome, making it more complex to address. Our parameters aren’t universally applicable to all patients, and implementation continues to evolve. It will be interesting to see how this field develops, and I believe it will improve.”
K Dhingra, author of the paper Artificial intelligence in dentistry: current state and future directions2 foresees AI becoming increasingly proficient at detecting complex dental conditions, enabling earlier intervention and improved outcomes. He suggests that personalised treatment plans will soon be based on a patient’s genetic and lifestyle factors, minimising adverse events. AI’s ability to analyse vast datasets could also uncover new trends and insights in oral health, giving researchers a deeper understanding of disease mechanisms and treatment responses.
Sakina points out that AI is already part of the tools we use, often without realising it. “We sometimes overlook the AI systems that help us dictate notes or integrate into our workflows. Tools for measuring periodontal pockets have been around for years, though they still need improvement. We increasingly rely on AI-driven software to simplify our work, from generating detailed periodontal charts to analysing patient data. While traditional methods are still prevalent, integrating AI into personalised periodontal care will require us, as the dental team, to lead the change. By presenting a unified front, we can build patient trust and encourage acceptance.”
In this digitally driven environment, patient education continues to play a crucial role in maximising understanding and ensuring that patients are fully engaged and proactive about their oral health.
“Patient education is the most critical stage of treatment,” Sakina emphasises. “It’s an inclusive and hands-on part of the appointment, involving oral hygiene instruction, behavioral change, and health education. This forms the backbone of clinical treatment and is how we measure patient compliance. The more experienced we get at discussing overall health with patients, the more natural it becomes.”
Sakina spends time explaining to her patients that the mouth is a gateway to the body, helping them understand that managing oral diseases can minimise risks for other conditions like diabetes and heart disease. This empowers patients to take ownership of their health.

She integrates medical and social history into her treatment plans, recognising that factors like smoking or drug use are critical to managing periodontal disease. “It’s important to foster ongoing care and track patient progress,” she notes. “Lifestyle factors, such as diet and family dynamics, are integral to the success of treatment. Patients change their behaviour over 90 days, and we play a key role in influencing this. By teaching patients, the right approaches and showing them the tools in a personalised protocol, we can significantly enhance outcomes.”
When more extensive treatments are required, Sakina often spreads them over several appointments, followed by a review. “Our practice emphasises a multidisciplinary, shared-care approach, especially with patients referred by other dentists,” she explains. “Whether working with referred or direct-access patients, collaboration is key. I prioritise developing flexible treatment plans, adjusting them as needed, and selecting the most appropriate tools and timings for each patient.”
She also believes in changing the narrative around periodontal care, starting with the language used. “I talk a lot about plaque biofilm rather than calcium deposits. We won’t get patients to change their outlook on periodontal care until we change the language around it. We emphasise that this isn’t just ‘a little bit of a tickle on the teeth’—it’s serious business. Talking about bacterial invasion helps engage patients.”
She also empowers patients by recommending oral health products, among them is the Gengigel product range, which uses the natural healing properties of hyaluronic acid to treat a range of oral conditions associated with soreness and inflammation. It is particularly beneficial for healing and protection following dental procedures.
‘Gengigel’s products definitely have a place in the bathroom cupboard,’ she says. ‘They are gentle, easy to use, and taste pleasant. I’ve found them particularly beneficial for patients dealing with inflammatory trauma in areas of gum recession, ulcerations, or mouth irritation – especially in women going through menopause. While there isn’t a direct link between gum disease and menopause, secondary factors can affect oral health during this time. The hyaluronic acid in the products aids in the body’s natural healing process by promoting tissue regeneration, which is crucial for recovery. Also, Gengigel’s products are vegan, kosher and free from SLS, making them suitable for use during pregnancy.’
In conclusion, while AI offers exciting possibilities for enhancing periodontal care, the human element— particularly patient education and personalised treatment—is what ensures these advancements translate into better health outcomes.
References available upon request
As we know, there are many medical conditions that can have a detrimental effect not only on our patient’s oral health, but also on our ability to provide comprehensive dental treatment. One of these conditions is called scleroderma.
Scleroderma is a rare condition that affects around 19,000 people in the UK. It occurs when the body produces too much collagen, causing the skin and other tissues to harden and become less flexible.
Collagen is found in connective tissues like cartilage, bones, tendons, ligaments, and skin. Scleroderma is an auto-immune condition, which means that the body is attacking itself. Whilst there is currently no cure for scleroderma, there are medications to reduce several of the symptoms, including drugs to:
• Dilate blood vessels
• Supress the immune system
• Reduce stomach acid
• Prevent infections
• Relieve pain
In some case, physiotherapy can help, too. Scleroderma can negatively impact oral health by making it difficult to brush and clean between teeth. Reaching the back of the mouth with a regular toothbrush can be challenging. Using a toothbrush with a long, slim neck or an electric toothbrush is often recommended, especially if the patient has trouble opening their mouth wide enough. Often, scleroderma can be linked with dry mouth, where the salivary glands do not produce enough saliva to protect teeth and gums, so prescribing a high fluoride toothpaste can help to reduce the risk of caries. Acid reflux is also common in scleroderma patients and can lead to enamel erosion.
If you suspect a patient may have undiagnosed scleroderma, it is advisable to refer them to their GP for further evaluation and diagnosis. Early detection and management are essential to prevent complications and improve the patient’s quality of life.
There are two main types of scleroderma that can affect your patients, making it more difficult for them to take care of their oral health.
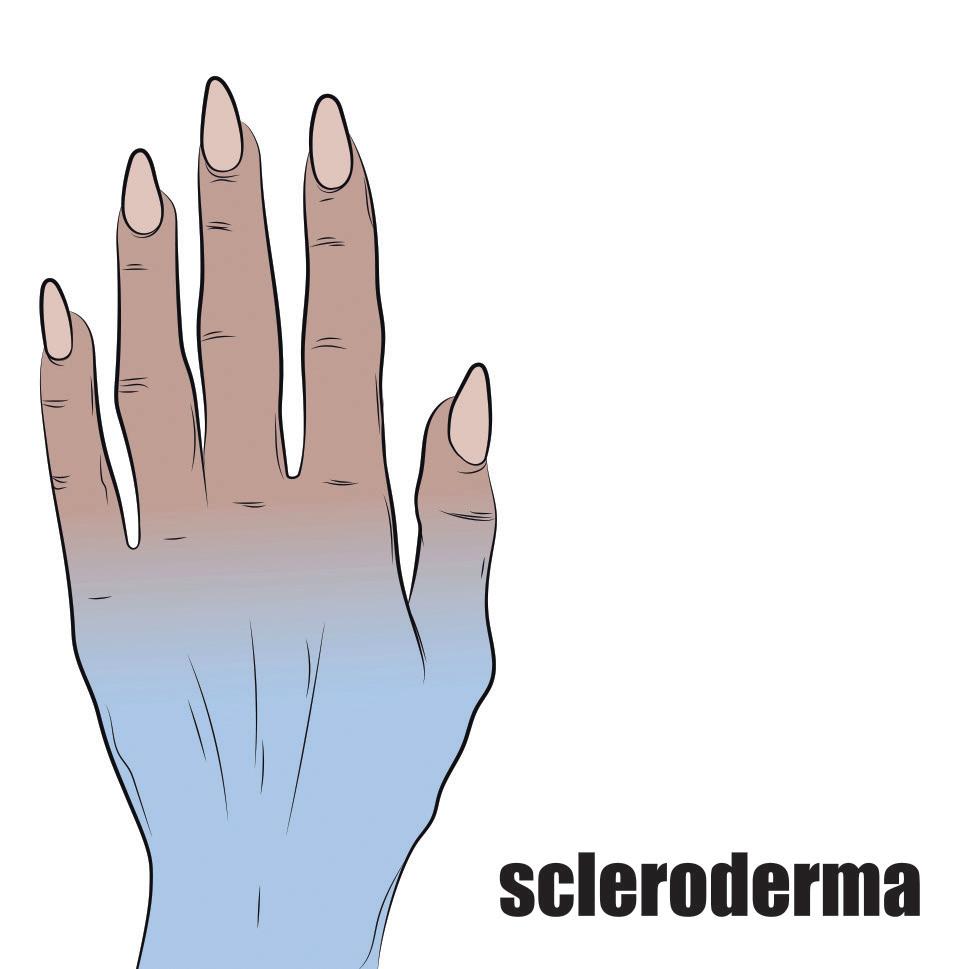
Localised scleroderma is the name given to scleroderma that usually affects localised areas of the body. It can appear as patches of hardened skin that look smooth and shiny, often on the main part of the body (the torso) but could be on the leg or arm.
Children can get a form of localised scleroderma that affects the scalp or temples, face and tongue. This condition can range from being painless or cosmetic to affecting the growth of bones in children.
Systemic scleroderma is the more serious type of scleroderma, known as SSc. This type of scleroderma also affects the internal organs and the skin. This can include the:
• Heart
• Oesophagus
• Blood vessels
• Kidneys
• Lungs
• Digestive system
• Mouth and teeth
This type of scleroderma is more likely to impact a patient’s oral health throughout their life.

Like others with problems that reduce the ability to open the mouth, there are a few ways that the oral health team can help.
Oral hygiene instruction to show the effective use of a toothbrush that has a long neck and a small head, or an electric toothbrush will make cleaning at home easier.
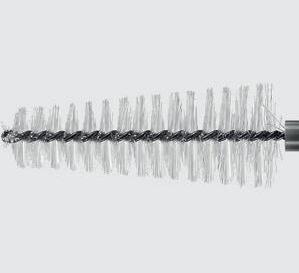
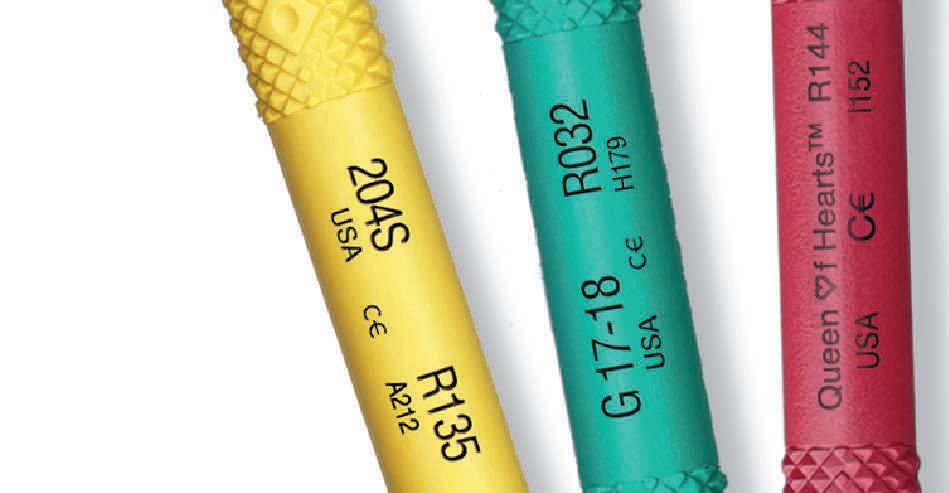
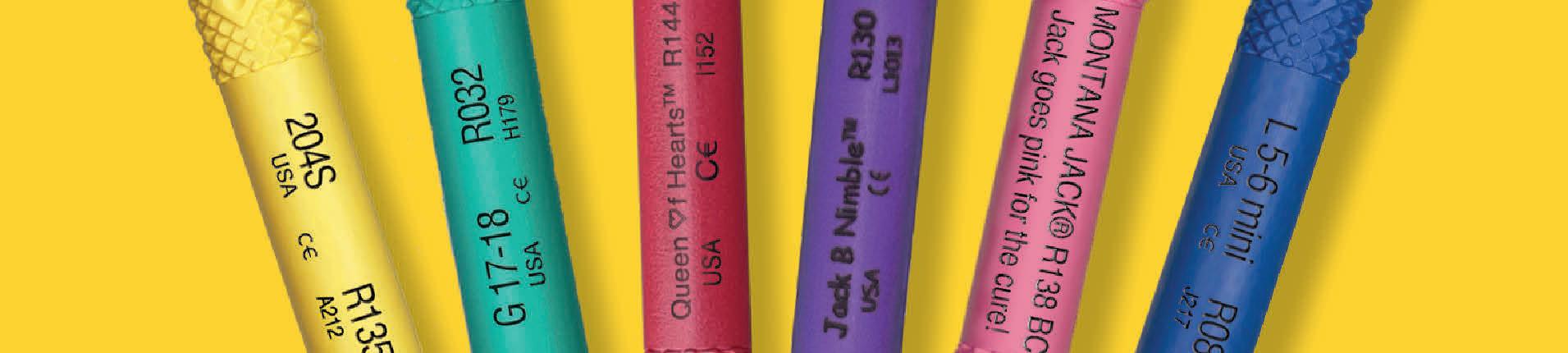
Demonstrate the use of an interdental brush with a long handle that will allow the patient to reach to clean in-between all their teeth. When it comes to interdental cleaning, they will usually find that an interdental brush will allow the best access and provide the best results.
Reduced mouth opening is caused by tightening of the skin around the mouth. Sometimes, facial exercises can help to improve the mouth opening. These exercises
should be carried out once or twice a day and should only take five-10 minutes.
Treating a patient with scleroderma may require patience and time. Short, regular appointments might be more comfortable for both the patient and the dental team than longer or double appointments.
If you would like to learn more about this condition, the charity Scleroderma & Raynaud’s UK has created a factsheet called Oral and Dental Aspects of Scleroderma, which is available on their website: www.sruk.co.uk




















Recently, Harry Morris sat down with Jolene Pinder and Louise Warden to discuss the upcoming ‘Confidence in Implant Dentistry’ course organised by EMS and hosted by Dr Barry Oulton
Harry: Let’s dive right in! Jolene, what initially inspired you to focus on implant dentistry as a dental hygienist?
Jolene: The first implants I saw placed were not long after I qualified in 2001 while I was working at the Royal Hospital Haslar in Portsmouth. I was fortunate enough to be involved with a fantastic oral and maxillofacial unit, where implants weren’t just for dental applications but were also used for other prosthetics in the head and neck region. The strict pre-placement protocols, especially around patient selection, really fascinated me. It was a long journey for patients even to be considered for an implant, and being part of that journey, providing supportive care, was incredibly rewarding. Over the years, seeing how implant placement has evolved and how it can restore a patient’s quality of life has kept me passionate about this field.
Harry: That sounds like an incredible start to your journey. Louise, how about you? What’s been the most rewarding aspect of your work with implants?
Louise: I started working in an implant referral practice in 2008 and, from the beginning, I was captivated by the field. I’ve been lucky to work with many implant dentists who have both taught and inspired me along the way. Perhaps the most rewarding part has been helping other dental professionals learn about implant maintenance and sharing the experience I’ve gained. It’s incredibly fulfilling to see the impact proper maintenance can have on the success of an implant and the overall health of a patient. The ability to teach and pass on this knowledge to others has been a highlight of my career.
Harry: It’s clear you both have a wealth of experience. Jolene, can you give us a sneak peek into what attendees can expect from your talk at the course?
Jolene: Absolutely! My talk will focus on implant maintenance, which I like to compare to an MOT and service for a car. Just as you would with a car, it’s crucial to keep implants in top condition to ensure their longevity. I’ll be discussing the checks we should carry out at each visit and how to address any issues that might arise. The key is consistent, careful monitoring and a tailored approach to each patient’s needs.
Harry: Louise, what about you? What will you be covering in your session?
ABOUT THE AUTHORS

Louise: I’ll be discussing the critical pre-implant stage, which is often overlooked but is crucial for implant success. We’ll talk about how to identify suitable implant patients, focusing on the S3 implant guidelines when it comes to patient selection and the importance of oral health before implants are fitted. I’ll also share some patient cases to highlight why this stage is so important.
Harry: It sounds like both of your talks will provide invaluable insights. Speaking of patient selection, how do you both determine if a patient is an appropriate candidate for implants?
Jolene: At the Dental Health Spa, we don’t place implants ourselves, so we refer patients out. However, we look at the patient’s social and medical history, previous disease progression, current disease status, patient compliance, and expectations before making a referral. When referring patients for assessment, I ensure they’re in optimal health and fully understand both the process and the commitment required for the treatment and ongoing maintenance. This way, they’re fully informed before making any financial investment.
Louise: We work closely with the dentists placing implants to assess which patients are suitable. Correct selection is key to avoiding implant loss, so we follow strict guidelines to ensure we’re making the right decisions. We also focus on building a strong relationship with the patient before the implant is placed, which helps ensure long-term success.
Harry: Implant maintenance is clearly a critical topic. Why is implant maintenance integral to the long-term success of dental implants, and what do you consider the most critical aspects of effective maintenance?
Jolene: Implants don’t have the same attachment as natural teeth, so they’re more vulnerable to loss if biofilm isn’t effectively removed. It’s crucial to establish baseline radiographs and pocket charts after implant placement. During each visit, we monitor indices and visually inspect around the implant, learning with the patient what is normal for their implant. There’s no one-size-fits-all measurement for implants, so having a baseline allows us to track any changes. Using tools like Airflow and Perioflow, along with the PI Max tip for removing hard deposits, helps ensure we maintain the implant in the least traumatic and most effective way possible.


Louise: There is no doubt that implant maintenance is key to long-term success. Mucositis and implantitis can have many causes, but biofilm accumulation is a major factor. That’s why it’s so important for patients to know how to maintain their implants at home and for us to check for any problems regularly. Correct maintenance helps prevent implant loss and ensures success not just for the patient, but for the practice overall.
Harry: That’s such an important aspect. What are some common misconceptions you encounter about implant dentistry, and how do you address them?
Louise: One big misconception is that implants are like fake teeth that don’t need care. We see patients the day their implant is fitted to give them tailored oral hygiene instructions and emphasise how crucial home care is. If patients don’t follow these instructions, there’s a real risk of implant failure.
Jolene: I completely agree. Another misconception is the fear some patients have

about us touching their implants. Education and trust are key here. We prepare patients before placement, so they understand the importance of regular maintenance. At our clinic, we also emphasise gentle, non-traumatic care to ensure the longevity of the implant.
Harry: It’s great to hear how you’re both addressing these challenges. Collaboration between dentists and hygienists is also crucial. How do you see this partnership contributing to the success of implant patients?
Jolene: Teamwork really does make the dream work! Without each of us playing our part, we won’t achieve the best outcomes for our patients. Good communication, especially when referring patients out for implant placement, is essential. We tailor our protocols to ensure every step is covered, and the patient feels supported throughout the process.
Louise: I couldn’t agree more. Collaboration is key from the initial consultation to long-term maintenance. Hygienists often see patients more regularly than dentists, so we’re responsible for maintaining the implants and motivating the patients. We need to communicate well with each other throughout the whole journey to ensure success.
Harry: For those just starting their journey in implant dentistry, what advice would you give them to build their confidence?
Louise: Don’t be scared! Many dental professionals are hesitant to work with implants, but it’s important to ask questions, seek help when needed, and continually learn through courses and networking. The more you know, the more confident you’ll become.
Jolene: Exactly! My advice is to attend courses and immerse yourself in learning. Networking with other professionals is also invaluable. Events like this one are fantastic for gaining new insights, sharing experiences, and building your confidence.
Harry: That’s some solid advice. Lastly, how do you both see events like the ‘Confidence in Implant Dentistry’ course contributing to the professional development of dental hygienists?
Jolene: These events are a goldmine for learning. They
provide a chance to hear from experts, discuss cases with peers, and bring new knowledge and confidence back to your practice. It’s an opportunity to grow both professionally and personally.
Louise: I completely agree. This course is unique because it covers everything from patient selection and preparation to maintenance and practice growth. It’s going to be an incredible day filled with knowledge-sharing and networking.
Harry: It sounds like an event not to be missed! We look forward to seeing you there! n





For those interested in building their confidence and knowledge in implant dentistry, be sure to attend the ‘Confidence in Implant Dentistry’ course on 1st November at the Royal College of Physicians in London. You can find more details and register https://bit.ly/3SJcblU




For dry mouth – when just water is not enough

































































1 in 5 suffer from dry mouth, and water is usually the standard remedy. But for many people, water only provides brief relief. TePe’s new hydrating mouthwash and mouth gel ease the feeling of dry mouth, provides comfort, and protects teeth. We recommend the gentle, unflavoured products for those with a very dry mouth and mildly flavoured products for those with moderate problems.















TePe® Hydrating Mouthwash - TePe’s mouthwash moistens the mucosa and leaves a pleasant feeling in the mouth. Not only does it help with dry mouth, but the added 0.2 % fluoride also gives that extra protection against caries.



TePe® Hydrating Mouth Gel - TePe mouth gel gives immediate and long-lasting comfort*, moistens and soothes the oral mucosa and is convenient and easy to use whenever needed – great for on-the-go.
Available from dental wholesalers. Find out more at tepe.com.






*The duration of the comfort is individual; people with no or very little saliva usually experience a more prolonged effect.









Mouth Cancer Action Month takes place every November, aiming to raise awareness about mouth cancer. For many, the word ‘cancer’ can be daunting, but increasing awareness and understanding can empower the public to take control of their oral health.
The landscape of mouth cancer in the UK
Mouth cancer, also known as oral cancer, is a significant and growing concern in the UK. In fact, we are now approaching 10,000 new cases every year – a number which has more than doubled over the past 20 years. In the last decade alone, the incidence of mouth cancer has risen by more than a third (34%). Mouth cancer does not discriminate; it affects individuals of all ages and genders. However, it is more commonly diagnosed in men, who account for nearly two-thirds (68%) of cases. Additionally, almost twothirds (64%) of mouth cancer cases are diagnosed in people over the age of 60. Tragically, over 3,000 people in the UK lose their lives to mouth cancer each year, which equates to about eight deaths per day.
Why Mouth Cancer Action Month is important
The primary goal of Mouth Cancer Action Month is to educate the public about the risks and signs of mouth cancer. Early detection significantly improves survival rates and outcomes. As dental professionals, you play a crucial role in this educational effort. By providing patients with the necessary information, you can help build stronger relationships within your community and make a tangible difference in people’s lives.
How dental professionals can support Mouth Cancer Action Month
Dental practices are uniquely positioned to support Mouth Cancer Action Month. Here are several ways you can get involved:
1. Displays and chairside information
Creating informative displays in your dental practice is a simple yet effective way to raise awareness. Use posters supplied by the Oral Health Foundation and provide instructions on how to perform a mouth cancer self-
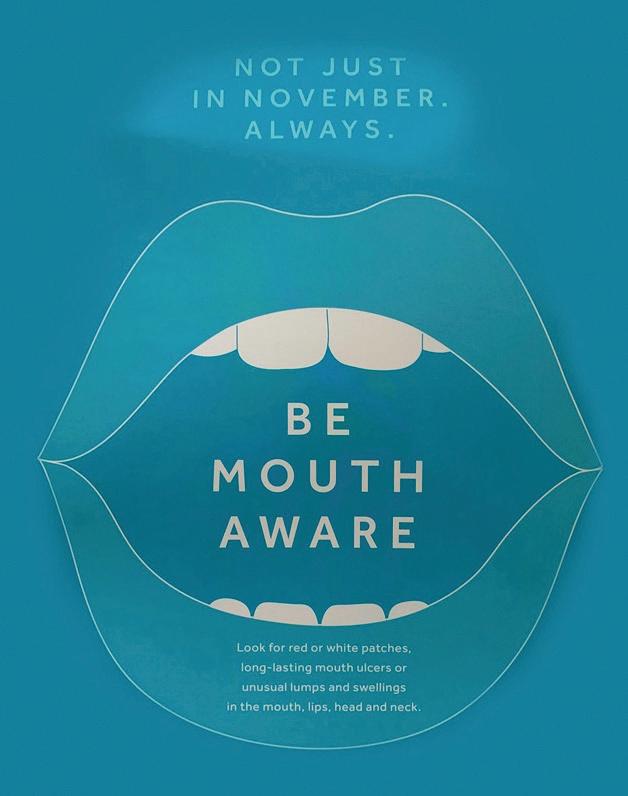
check at home. Adding small pieces of bunting can make the display more visually appealing and attract attention. However, this awareness must also translate to the chairside. During consultations, identify a patient’s possible level of risk by asking about lifestyle habits that link to mouth cancer, such as smoking, alcohol consumption, and diet. As you perform a visual examination of the mouth and neck, explain what you are doing and why it is important. This not only educates the patient but also reassures them about the thoroughness of their check-up.
2. Organise activities and events
Engaging in activities and events can be a fun and impactful way to raise awareness. Here are some ideas:
• Fundraising : Fundraising is a powerful way to raise awareness and collect donations for Mouth Cancer Action Month. These donations help the Oral Health Foundation continue its vital work in raising awareness and educating the public about mouth cancer. Fundraising not only supports
the campaign but also enhances your practice’s community presence, fosters team building, and boosts staff morale. On the campaign website there are lots of ideas to get you started.
• Community outreach: Going out into the local community to give talks and workshops is another impactful way to raise awareness about mouth cancer. By visiting local workplaces, sports clubs, care homes, and community centres, you can help people identify the early warning signs and understand the risks associated with mouth cancer. These outreach efforts can significantly enhance public knowledge and encourage early detection, ultimately saving lives.
Early detection of mouth cancer can significantly improve the chances of successful treatment and recovery. Encourage your patients to look out for common signs such as:
• Persistent mouth ulcers that do not heal.
• Lumps or swellings.
• Red or white patches in the mouth.
• Unexplained pain or numbness in the mouth or lips.
By promoting awareness and education, you can help reduce the number of lives lost to mouth cancer each year.
If you would like to get involved in Mouth Cancer Action Month, visit the Oral Health Foundation’s website at www.mouthcancer.org to find out how you can make a difference. Whether through fundraising, hosting events, or simply spreading the word, every effort counts.
Mouth Cancer Action Month is a vital campaign that brings attention to a serious health issue. As dental professionals, you have the power to make a significant impact. By participating in this campaign, you can help save lives and improve the overall health of your community.
Let’s come together this November to raise awareness, educate, and support the fight against mouth cancer. n
Ultrasonic and powder therapy in one unit
Ultrasonic Treatments
Wide range of ultrasonic tips for scaling, perio/ implant maintenance, restorative and endodontics.
Varios Combi Pro Combined Oral Hygiene Unit RRP £5,151 Y1002843

Supragingival and subgingival (optional extra) chambers, both with lightweight handpieces.


the NSK Varios Combi Pro Video
more about the NSK Varios Combi Pro



Choose from NSK’s range of 3 powders, all compatible with the Varios Combi Pro




There are many factors that affect the dental patient’s experience. Though some are more important that others, all must be considered in order to curate a consistently positive, effective and efficient patient journey. The consequences of getting it right are huge for the practitioner and for the practice. Not only are happy patients more likely to develop loyalty and return time after time, they are also more likely to recommend your services to friends and family, further supporting business growth. Furthermore, there is evidence demonstrating a positive correlation between patient satisfaction and clinical effectiveness.i
Clinical excellence remains king
As would be expected, one of the top contributors to a fantastic patient experience is high-quality treatment. A European studyii from 2023 found the quality of treatment received to impact everything from whether a patient would recommend the dentist to others to their relationship with the dentist. Interestingly, the same research found that patient satisfaction with the frequency of appointments also impacted their overall contentment with treatment and loyalty to the practice. There is also evidence to show that patient perception of pain and pain management may impact their overall experience. Efficient pain assessment and pain management options with fewer side effects have proven helpful in improving patient satisfaction with treatment.iii This further supports the importance of clinical excellence in dentistry, as with careful planning that includes an effective choice of analgesic,iv clinicians can help to reduce post operative pain.
A people thing
Physical environment and technologies
However, it doesn’t stop there. A combination of staff behaviours, facilities and basic environmental needs also influence the patient experience. Examples include practice opening hours and cleanliness.viii The physical environment may also impact patient outcomes and satisfaction, including the layout of the practice, room features, medical equipment visible, lighting and music.ix
Technology is another area that has become instrumental in delivering an excellent patient experience. Studies have touted the latest tech as having helped to enhance efficiency, safety and accessibility of dental care.x Specific solutions such as intraoral scanners have also become a widespread preference among patients,xi who appreciate the elimination of the traditional ‘gooey’ impressions.

However, it doesn’t stop there. There are social factors at play too. For instance, patient characteristics like age and education level can affect their perceived experience in any healthcare setting.v Broader influences like those from wider societal trends, or community and family contexts can also affect patient expectations and, therefore, satisfaction with the dental care they receive.
In addition, the communication between patients and healthcare professionals has been shown to influence their satisfaction with the service received.vi Specifically in dentistry, effective professional-patient communication has long been recognised as a cornerstone of high-quality care. Ensuring that patients understand their current oral health status and the need for recommended treatment, empowers them to be more involved in the oral health, improving their overall experience. This communication can also reduce the risk of dental anxiety among patients and increase trust in their practitioner.vii
Of course, imaging technology isn’t the only solution making waves in the dental profession. Innovative practice management software is streamlining the entire patient experience from the moment they book an appointment, through to their treatment and beyond. AeronaDental, for example, is a next generation cloud-based software that impacts every aspect of the patient journey. Add-ons like the Patient Portal facilitates online engagement, bookings, digital form-filling and online consultations, while integration with solutions like Dojo – a flexible and secure payment provider – make paying for treatment 58% faster than the average mobile card machine. Plus, the provider offers all this alongside exceptional customer support, so you know you have the experts on your side when it comes to optimising your patient experience.
Ultimately, everything about the modern dental profession is designed to support patients to better oral health. If patients have a positive experience in the practice, this is not only good for business, but it also means they are more likely to return for on-going treatment, boosting continuity of care and their long-term health. Considering every aspect of their journey through the practice is important for a truly patient-centred approach. For more information, please visit aerona.com or call 028 7000 2040
Follow us on LinkedIn: @AeronaDental Software and Instagram @aeronasoftware for the latest updates
References
i. Doyle C, Lennox L, Bell D. A systematic review of evidence on the links between patient experience and clinical safety and effectiveness
ii. BMJ Open 2013;3:e001570. doi: 10.1136/ bmjopen-2012-001570
iii. Szabó RM, Buzás N, Braunitzer G, Shedlin MG, Antal MÁ. Factors Influencing Patient Satisfaction and Loyalty as Perceived by Dentists and Their Patients. Dent J (Basel). 2023 Aug 28;11(9):203. doi: 10.3390/dj11090203. PMID: 37754323; PMCID: PMC10529870.
iv. Tawil S, Iskandar K, Salameh P. Pain management in hospitals: patients’ satisfaction and related barriers. Pharm Pract (Granada). 2018 Jul-Sep;16(3):1268. doi: 10.18549/PharmPract.2018.03.1268. Epub 2018 Sep 25. PMID: 30416629; PMCID: PMC6207353.
v. Becker DE. Pain management: Part 1: Managing acute and postoperative dental pain. Anesth Prog. 2010 Summer;57(2):67-78; quiz 79-80. doi: 10.2344/0003-3006-57.2.67. PMID: 20553137; PMCID: PMC2886920.
vi. Larson E, Sharma J, Bohren MA, Tunçalp Ö. When the patient is the expert: measuring patient experience and satisfaction with care. Bull World Health Organ. 2019 Aug 1;97(8):563-569. doi: 10.2471/ BLT.18.225201. Epub 2019 May 28. PMID: 31384074; PMCID: PMC6653815.
vii. Tian, Y. A review on factors related to patient comfort experience in hospitals. J Health Popul Nutr 42, 125 (2023). https://doi.org/10.1186/s41043023-00465-4
viii. Yuan S, Freeman R, Hill K, Newton T, Humphris G. Communication, Trust and Dental Anxiety: A Person-Centred Approach for Dental Attendance Behaviours. Dent J (Basel). 2020 Oct 13;8(4):118. doi: 10.3390/dj8040118. PMID: 33066178; PMCID: PMC7712465.
ix. Adhikary G, Shawon MSR, Ali MW, Shamsuzzaman M, Ahmed S, Shackelford KA, Woldeab A, Alam N, Lim SS, Levine A, Gakidou E, Uddin MJ. Factors influencing patients’ satisfaction at different levels of health facilities in Bangladesh: Results from patient exit interviews. PLoS One. 2018 May 16;13(5):e0196643. doi: 10.1371/journal.pone.0196643. PMID: 29768441; PMCID: PMC5955531.
x. Jamshidi, Saman & Parker, Jan & Hashemi, Seyedehnastaran. (2019). The effects of environmental factors on the patient outcomes in hospital environments: A review of literature. Frontiers of Architectural Research. 9. 10.1016/j. foar.2019.10.001.
xi. Gracco A, De Stefani A, Bruno G. Influence of New Technology in Dental Care: A Public Health Perspective. Int J Environ Res Public Health. 2023 Apr 3;20(7):5364. doi: 10.3390/ijerph20075364. PMID: 37047978; PMCID: PMC10093858.
xii. Sivaramakrishnan G, Alsobaiei M, Sridharan K. Patient preference and operating time for digital versus conventional impressions: a network metaanalysis. Aust Dent J. 2020 Mar;65(1):58-69. doi: 10.1111/ adj.12737. Epub 2019 Dec 19. PMID: 31749234. n
THE AUTHOR

Buy 2 get 1 free (while stocks last)
Directa’s ProphyCare, is one of the most well-known brands of prophylaxis paste worldwide, offering reliable results ranging from regular cleaning of the teeth to more complicated implant maintenance procedures.ProphyCare pastes are available in different grits from coarse to extra-fine and are colour coded for easy identification. All ProphyCare pastes have a mild minty taste and do not splatter, it stays in the polishing cup during the treatment.


As a busy dental professional, you probably don’t think about the water in your practice very often. And why would you – you have plenty of other things to occupy your thoughts on any given day in the practice. However, it is important to consider water quality in order to ensure the highest standard of patient care and safety, while also maximising the working life and return on investment for your decontamination equipment.
There are various reasons why water quality is important in the dental practice. The first is to protect patients and professionals from potential infection. According to HTM 01-05, registered managers of all dental practices are responsible for ensuring that the water supply, storage and distribution meets certain standards. This includes minimising the risk of Legionnaires’ disease, which can develop within the dental unit water lines (DUWL) if the relevant pathogens are allowed to colonise in stagnant water. Historical studies have established a significant risk of contamination throughout DUWLs, ii highlighting the importance of cleaning them sufficiently.
The Health and Safety Executive mandates that all businesses using any type of water supply where a risk of Legionella contamination exists implement adequate infection control measures. The SHTM 01-05iii necessitates similar in Scotland, with both bodies requiring a named individual to be responsible for this decontamination process.
Another reason to maintain water quality is to protect your decontamination equipment from malfunctions or breakdowns. This is especially important if you are located in an area of the UK with ‘hard’ water. Approximately 60% of the nation has a high concentration of calcium and magnesium dissolved in the mains water supply, which dries down into limescale.v
If you were using mains water for your dental units and handpieces, this limescale could build up and may cause problems rather quickly. Not only could your equipment stop functioning as efficiently as they should, but substantial limescale could stop it from working altogether. This could cause serious disruption to your services if it happens to essential pieces of equipment like your autoclave. Without cleaned and sterilised instruments rendered safe for reuse, patients would be inconvenienced by postponed appointments. Staff would also have more tasks to complete in addition to the stress of engaging with unhappy patients and arranging for engineers to fix the equipment. Of
course, all of this would also have financial implications for the practice, with the costs of engineer visits, spare parts and practice downtime adding up quickly.
An alternative solution
For all these reasons and more, dental practices in the UK should steer clear of using mains water to supply their equipment. One alternative solution is to use bottled water instead, but this comes with its own disadvantages. Bottled water can be expensive for the business, it is one of the least environmentally-friendly options and substantial space is required for bottle storage. Dental practices already generate unavoidable plastic waste and the use of bottled water would simply add to this unnecessarily.
A better option for most dental practices is to introduce a reverse osmosis (RO) water system. This reliably delivers safe and clean water in a cost-efficient and sustainable way. It is also a faster solution than a water distiller, delivering more water in a shorter space of time for optimal convenience and minimal running costs.
RO water units work by pushing tap water through a semi-permeable membrane, which removes contaminants. Everything from minerals like calcium and carbonate to totally dissolved solids (TDSs), bacteria and microorganisms are effectively removed from the water. Leading equipment combines the use of UV light technology to further ensure the highest water quality possible.

The WRAS-approved RO Water System from expert in decontamination, Eschmann, affords all these benefits and more, quickly and efficiently producing water in compliance with HTM 01-05 and SHTM 01-05 guidance compared to alternative methods. The 12-litre water tank comes as standard, and a 60-litre version is available to meet the needs of larger practices. Easy to connect to the mains cold water supply, the system affords a rapid return on investment, often in less than 12 months. Plus, the equipment can be maintained under the Eschmann Care & Cover servicing package, with technical telephone support and expert engineers on hand to keep equipment running efficiently for longer.
Water quality might not be an everyday topic of conversation for the dental team with so many other aspects to think about. However, it is crucial for patient safety and equipment longevity. RO water systems provide a reliable, cost-effective, sustainable and fast solution, find out more today.
For more information on the highly effective and affordable range of infection control products from Eschmann, please visit www.eschmann. co.uk or call 01903 753322
References
i. Health Technical Memorandum 01-05: decontamination of linen for health and social care. 2016: Guidance. https://www.england. nhs.uk/estates/health-technical-memoranda/ [Accessed August 2024]
ii. Spagnolo, A.M., Sartini, M., Di Cave, D., Casini, B., Tuvo, B. and Cristina, M.L. (2019). Evaluation of Microbiological and Free-Living Protozoa Contamination in Dental Unit Waterlines. International Journal of Environmental Research and Public Health, [online] 16(15), p.2648. Available at: https://www.ncbi.nlm.nih.gov/pmc/ articles/PMC6696308/ [Accessed August 2024].

iii. National Services Scotland. Scottish Health Technical Memorandum 01-05. Management, equipment and process of the decontamination of dental instruments in a Local Decontamination Units ()LDU) NHSScotland. Part A. https://www.nss.nhs. scot/publications/management-equipmentand-process-of-the-decontaminationof-dental-instruments-in-a-localdecontamination-unit-ldu-in-nhsscotlandshtm-01-05/#:~:text=The%20best%20 practice%20guidance%20Scottish,steam%20 sterilizers%2C%20SHTM%202030%20for [Accessed August 2024]
iv. www.scaleguard.co.uk. (n.d.). Water Hardness Areas in the UK. [online] https:// www.scaleguard.co.uk/hard-water-areas. html#:~:text=Around%2060%25%20of%20 the%20UK [Accessed May 2024].
v. Sengupta, P. (2013). Potential health impacts of hard water. International journal of preventive medicine, [online] 4(8), pp.866–75. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/ PMC3775162/ [Accessed May 2024]. n
NICKY
VARNEY,

Nicky Varney, Senior Marketing Manager at Eschmann Technologies Ltd.
























































































Expertly crafted to provide maximum comfort and tactile sensitivity
Flaws in a smile can inhibit self-confidence and affect interactions with peers, so it is unsurprising that the UK orthodontic market is expected to be worth £289.4 million by 2027, fuelled by a high demand for a dream smile and technological advancements in treatments.i
Whilst fixed braces may be perceived as the traditional orthodontic treatment for malocclusion, clear aligners have become increasingly popular in a post-Covid ‘Instagram smile’ market.ii As they are discreet and removable, clear aligners promote convenience and flexibility. The global market for clear aligners was valued at USD 5.13 billion, and is expected to grow by 30% every year.iii They represent an effective option for mild to moderate cases of misaligned teeth, but educating orthodontic patients on the importance of cleaning them is essential for treatment success.
Better than braces…
Whereas fixed braces are often noticeable and can make patients feel self-conscious, clear aligners satisfy the desire for more discreet and comfortable orthodontic appliances – they are virtually invisible.iv Ideally worn for 20-22 hours a day, only eating, drinking anything except water and oral cleaning should stop patients from wearing their clear aligner.v Despite being removable, the potential for bacterial growth on the appliance should not be ignored.
Identifying white spot lesions can indicate the early stage of caries. Orthodontic treatment increases the incidence of white spot lesions because fixed appliances impact the oral hygiene routine, leading to poorer oral health and an increase in the retention of plaque.vi For clear aligners, the prevalence of white spot lesions is lower: 26% of individuals undergoing conventional orthodontic treatment showed signs of white spot lesions compared to 1.2% of individuals who used clear aligners.iv This can be attributed to shorter treatment times and the ease of maintaining a good oral hygiene routine with a removable appliance.
But brace for bacteria…
Due to being repeatedly removed throughout the day, clear aligners can cause liquids and food particles to become trapped against the teeth if the oral cavity is not sufficiently cleaned before the aligners are worn. Confined to the tooth by the appliance, these particles can increase the risk of cavities and gingival diseases.v Educating patients on the importance of a consistent oral hygiene routine, especially daily interdental cleaning, can disrupt food remnants. Encouraging a rinse with water when eating or drinking throughout the day before putting the aligners back in can also promote good oral health.
Clear aligners may attract distinct microbial communities in the oral cavity.vii The grooves and ridges on the aligner surface may provide an optimal environment for bacterial adherence, as well as the development of plaque biofilms that can cause caries.iv After being worn for the maximum 14 days, microcracks and abraded areas conducive to bacteria growth have also been observed.iv Some of these bacterial species, including Streptococcus and Granulicatella, have an affinity for the biomaterials used in clear aligners; these can increase the prevalence of caries.iv Furthermore, there are other consequences to a poorly maintained clear aligner: the deterioration of the aesthetic appearance and a disagreeable odour may decrease patient compliance.viii This then prevents treatment success and can lead to patient dissatisfaction. It is therefore vital to maintain both oral health and the cleanliness of the clear aligner.

Despite having less of an impact on oral health outcomes than fixed appliances, clear aligners still carry a risk of accumulating bacteria, as well as trapping food particles that demineralise the enamel and cause gingival diseases.vii Besides a regular and effective oral hygiene routine, cleaning each clear aligner is an effective solution that lower caries risk and support the orthodontic treatment.
Using the Curaprox Aligner Foam is an excellent way of cleaning both the aligner and the oral cavity. It contains hyaluronic acid to moisturise and promote healthy teeth and also features the natural bioflavonoid CITROX®, formulated for its antibacterial, antioxidant and anti-inflammatory properties. Curaprox Aligner Foam revitalises and enriches teeth whilst leaving a smooth moisturising shield over them. Easily used, it can be either swished around the mouth after brushing or directly placed into aligners, retainers or mouthguards for more beneficial long-term effects. For better protection against caries and gingival diseases, recommend Curaprox Aligner Foam to your patients.
As clear aligners become increasingly sought after, educating orthodontic patients on the risks to their oral health and the cleaning measures needed to reduce them can ensure that they emerge from the treatment with the smile they have always wanted.
To arrange a Practice Educational Meeting with your Curaden Development Manager please email us on sales@curaden.co.uk
For more information, please visit www.curaprox. co.uk and www.curaden.co.uk
References
i. www.fortunebusinessinsights.com. (n.d.). U.K. Orthodontics Market Size, Share, Growth & Report [2027]. [online] Available at: https://www. fortunebusinessinsights.com/u-k-orthodonticsmarket-105048.
ii. Dentists warn of permanent damage from clear braces ordered online. (2023). BBC News. [online] 20 Jan. Available at: https://www.bbc.co.uk/news/ uk-58038752.
iii. www.grandviewresearch.com. (n.d.). Global Clear Aligners Market Size & Share Report, 2020-2027. [online] Available at: https://www.
grandviewresearch.com/industry-analysis/clearaligners-market.
iv. Rouzi, M., Zhang, X., Jiang, Q., Long, H., Lai, W. and Li, X. (2023). Impact of Clear Aligners on Oral Health and Oral Microbiome During Orthodontic Treatment. International Dental Journal. doi:https://doi.org/10.1016/j.identj.2023.03.012. v. Leber, C. (2024). Clear Aligner Therapy: The Discreet Way to Straighten Teeth. [online] American Association of Orthodontists. Available at: https://aaoinfo.org/whats-trending/clearaligner-therapy/.
vi. Dental, P.H. (2024). The Impact of Clear Aligners on Oral Health. [online] Pure Holistic Dental. Available at: https://www.pureholisticdentist. com/the-impact-of-clear-aligners-on-oralhealth/ [Accessed 9 Jul. 2024].
vii. Shokeen, B., Viloria, E., Duong, E., Rizvi, M., Murillo, G., Mullen, J., Shi, B., Dinis, M., Li, H., Tran, N.C., Lux, R. and Wu, T. (2022). The impact of fixed orthodontic appliances and clear aligners on the oral microbiome and the association with clinical parameters: A longitudinal comparative study. American Journal of Orthodontics and Dentofacial Orthopedics, 161(5), pp.e475–e485. doi:https://doi.org/10.1016/j.ajodo.2021.10.015.
viii. Charavet, C., Gourdain, Z., Graveline, L. and Lupi, L. (2022). Cleaning and Disinfection Protocols for Clear Orthodontic Aligners: A Systematic Review. Healthcare, 10(2), p.340. doi:https://doi. org/10.3390/healthcare10020340. n
ANDREW TURNER

Andrew Turner is Head of Marketing UK & Ireland, at Curaden UK

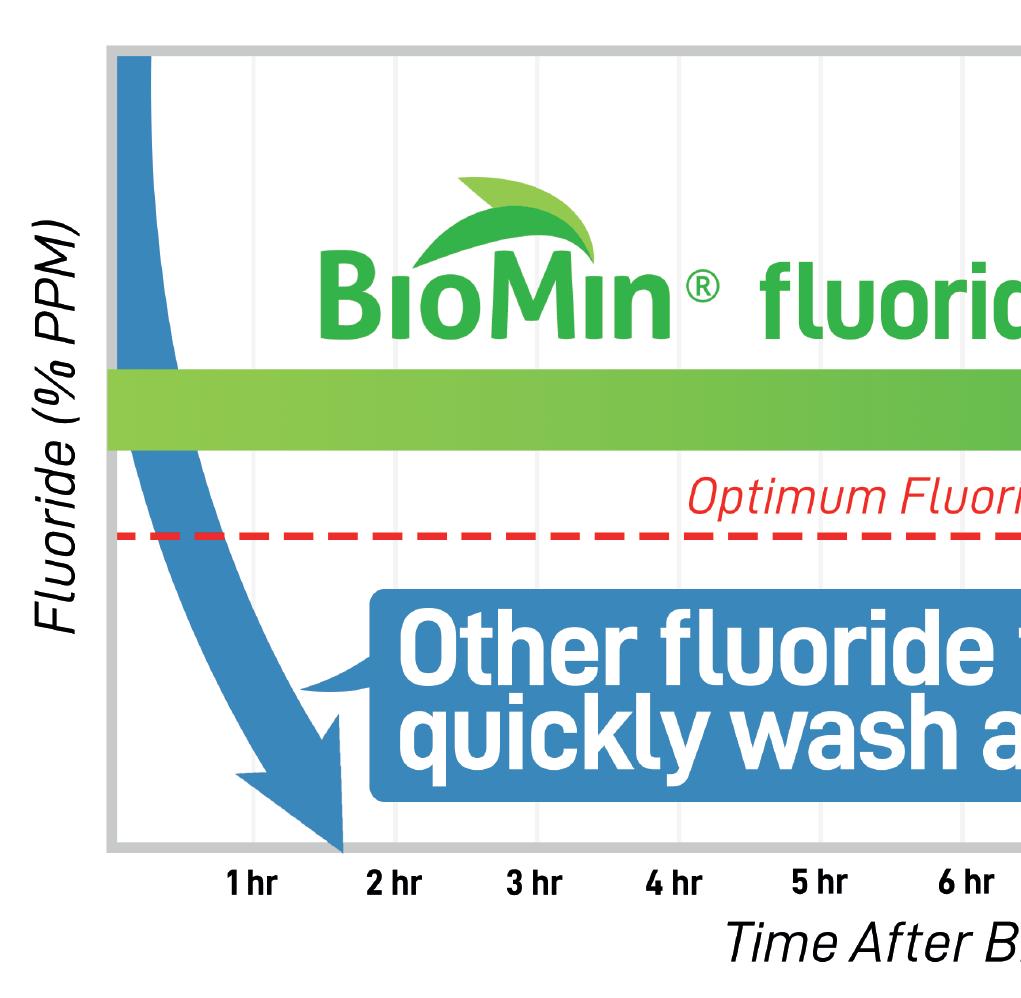
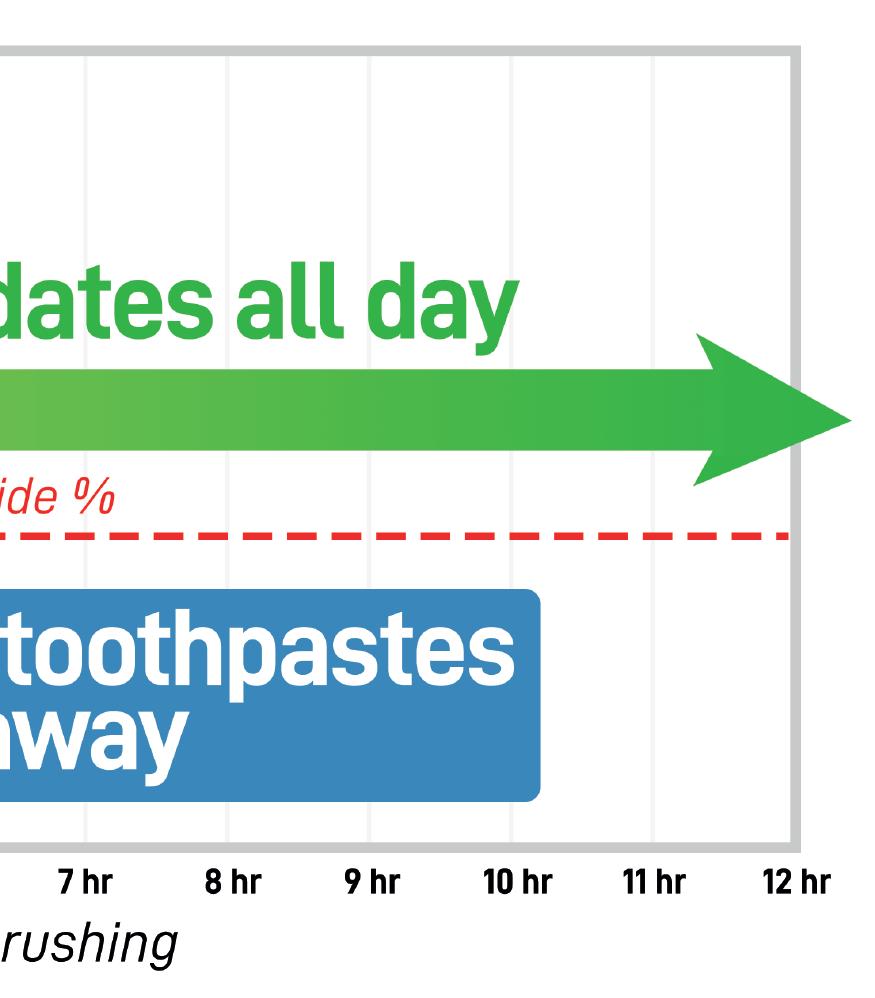
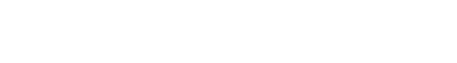
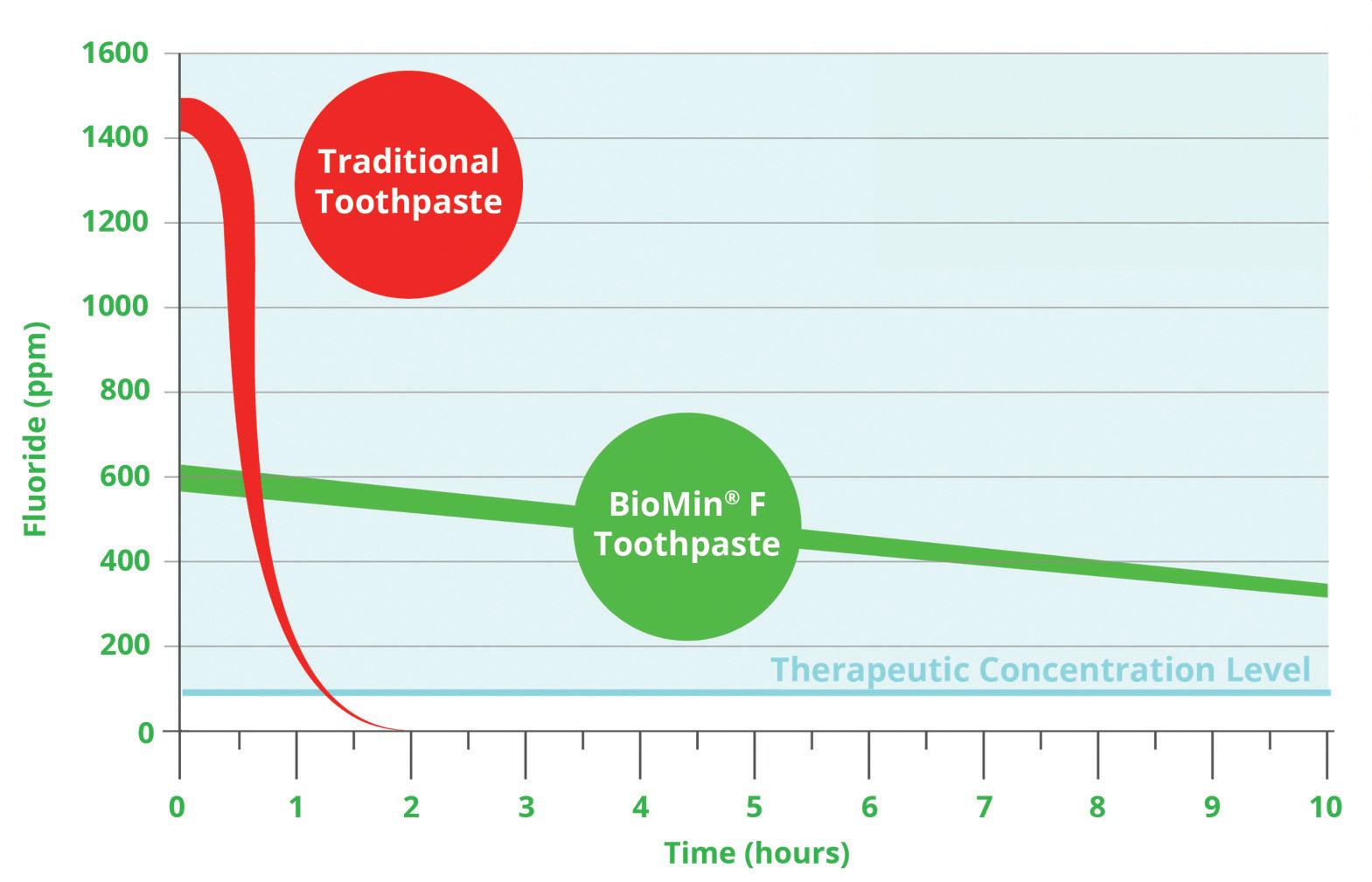
BioMin® F is the only toothpaste that delivers low level Fluoride with Calcium and Phosphate ions continuously for 12 hours after brushing. By contrast, soluble Fluoride used in all other toothpastes is rapidly washed away by saliva and has little clinical benefit just over an hour after brushing.
Bioglasses in toothpastes
Developed over 20 years ago, first generation NovaMin® bioglass was not originally developed for use as a toothpaste. It was initially formulated for orthopaedic bone grafting. Only later was it used in toothpastes because of its adherent and slow dissolving capabilities to release Calcium and Phosphate. It does not contain Fluoride or even optimum proportions of Calcium and Phosphate. NovaMin®, the active ingredient in Sensodyne Repair and Protect, is a bioglass without Fluoride. Repair and Protect incorporates additional soluble Fluoride which rapidly washes away like all other saliva soluble Fluoride toothpastes.
Resulting from 15 years research and development at Queen Mary’s University, London, BioMin® F is an advanced second generation bioglass, specifically developed for dental applications and uniquely formulated to slowly release Fluoride, Calcium
and Phosphate ions over a 12 hour period. It facilitates rapid and continual production of stable, acid-resistant Fluorapatite within dentinal tubules and on tooth surfaces. This constant Fluorapatite development increases the acid-resistance of teeth by 1000%. All other toothpastes contain soluble Fluoride which is washed away providing far less protection.
The Fluoride misconception
Some wrongly believe that the optimal toothpaste should contain 1450ppm of Fluoride. This figure is not based on clinical benefit, but is simply the legal maximum a toothpaste can contain without having to comply with onerous product registration requirements. No manufacturer can add more Fluoride to a toothpaste without a Pharmaceutical Product Licence. BioMin® F avoids this problem because of its controlled continuous release of Fluoride with Calcium and Phosphate.
The higher the Fluoride content the greater the risk of Fluorosis by accidental imbibition, especially amongst children and people prone to swallowing toothpaste.
With its dramatically lower 530ppm Fluoride content this risk is minimised, whilst still delivering 12 hour Fluoride protection!
BioMin® F contains Fluoride, Calcium and Phosphate ions in the optimum proportion. As the oral pH decreases after consuming sugary and acidic food and drink, the bioactive glass dissolves quicker, resulting in even faster release of these minerals, which in turn neutralises acid helping to stabilise the pH further and helping to protect the teeth from decay.
BioMin® F bioglass particles are 60% smaller than those found in NovaMin® products, resulting in less abrasivity and deeper penetration of the dentinal tubules with acid resistant Fluorapatite. So, formation of Fluorapatite is not just on the tooth’s surface, but also deep within dentinal tubules. The tubular occlusion achieved with BioMin® F is much more resistant to dissolution, providing more effective and longer-lasting relief from dentine hypersensitivity. No other toothpaste can deliver such effective strengthening and protection of enamel and long-term defence against dentine hypersensitivity
Published research shows that BioMin® F outperforms other sensitivity toothpastes in its ability to block dentinal tubules, resulting in superior and long-lasting sensitivity relief (Studies available upon request).
For further information visit the Trycare website, www.trycare.co.uk/biomin, contact your local Trycare representative or call 01274 885544. n
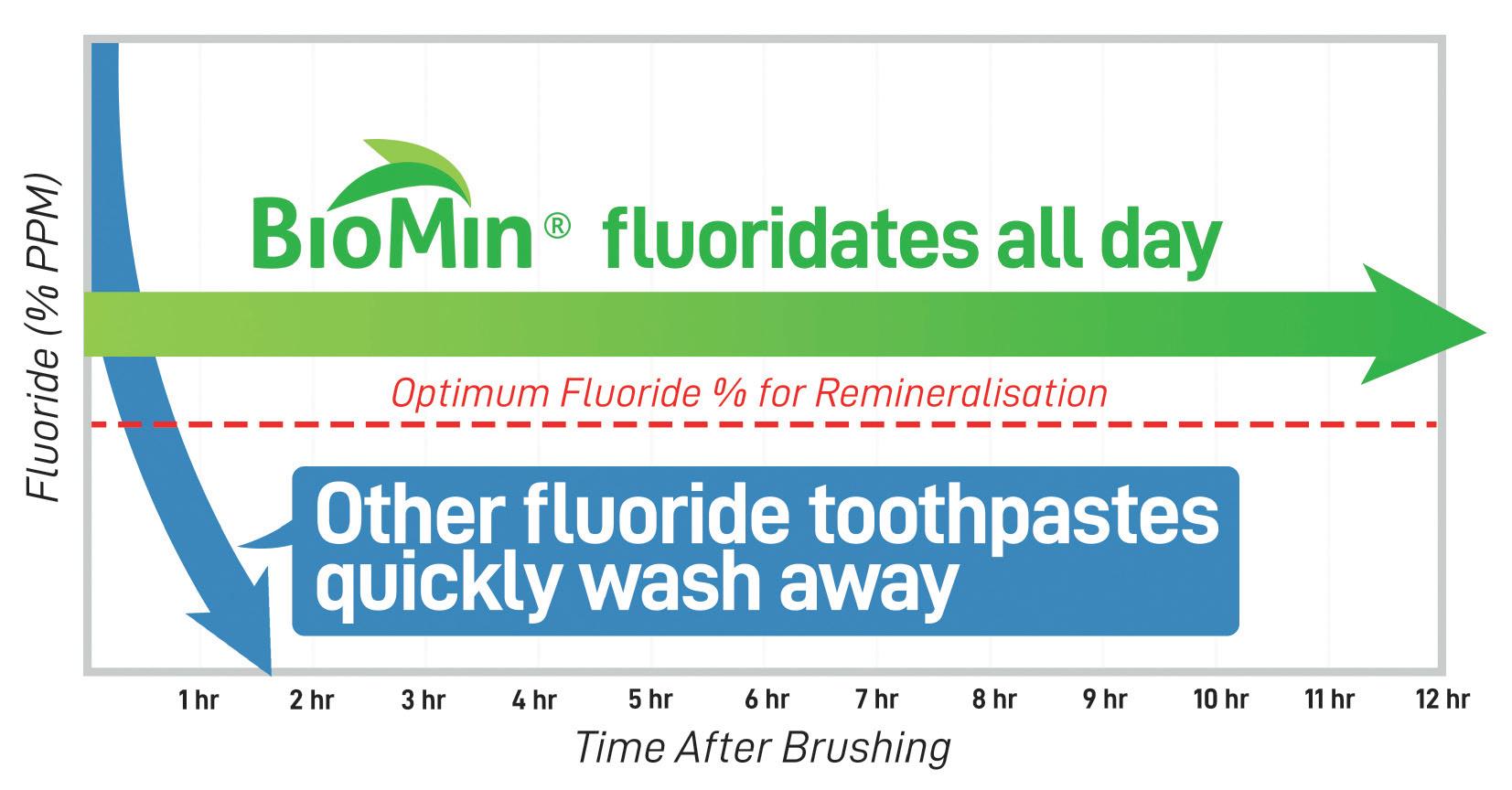
The NHS recommends that patients brush their teeth thoroughly with a fluoride toothpaste to effectively prevent tooth decay.i However, with many options available on the market containing varying levels of fluoride, it’s essential that clinicians are able to recommend the right solution for each patient, and understand the benefits and risks associated with it.
Fluoride is a naturally occurring mineral found in water in varying amounts, depending on where you are in the UK.ii It is widely accepted that fluoride plays a vital role in preventing tooth decay, and has been a standout ingredient in toothpastes since the 1970s.iii Because it is so widely used, it’s important to have a good understanding of the benefits it offers, as well as any potential risks, and
how to use it to help your patients protect their oral health more effectively.
What are the benefits afforded by fluoride?
Fluoride prevents demineralisation by travelling into the enamel sub-surface, where it absorbs into the crystal structure, and provides protection. It promotes remineralisation as it accelerates the growth of fluorapatite crystals on partially demineralised teeth. It absorbs into the surface and attracts calcium, in turn attracting more fluoride, resulting in a fluorapatite-like surface. This makes the tooth surface less vulnerable to acid. Additionally, it hinders plaque formation. At a low pH, fluoride ions are able to travel through the cariogenic bacterial cell wall. Once
Small amounts of fluoride over time offer benefits to oral health
inside, it acidifies the bacterial environment and inhibits the bacteria. iv
What are the risks of over-prescribing fluoride?
Whilst fluoride offers patients countless dental health benefits, it’s important to consider the potential effects of over-use.
Dental fluorosis
During childhood, whilst the teeth are still developing, exposure to high concentrations of fluoride can lead to mild dental fluorosis. These are small white streaks or specks on the enamel. Whilst this doesn’t affect patients’ health, the discolouration can be noticeable. To mitigate the risk, children should not use high concentrations of fluoride, and should be supervised when brushing their teeth to ensure they do not swallow their toothpaste.v
Skeletal fluorosis
Excessive exposure can impact bone health too, leading to a bone disease called skeletal fluorosis. Over time, this can cause pain and damage to bones and joints, and the risk of fractures may increase.iv
Other health problems
In addition, there are a number of other conditions which may occur due to excessive fluoride exposure. These include thyroid problems, neurological problems, acne, cardiovascular problems, and reproductive issues.iv
What are the legal limitations surrounding fluoride?
In the UK, there is a legal limit for the maximum concentration of fluoride that over-the-counter toothpastes can contain to protect patients’ safety. This is 1,500 ppm fluoride,vi and is why many popular
toothpastes contain just under this – usually 1,450 ppm. Some patients and clinicians may assume that this is the recommended concentration for clinical benefits, however, it should instead be viewed as an absolute maximum daily dosage. Although, dentists have the ability to prescribe higher dose fluoride toothpastes to those who are susceptible to caries.v
However, a high concentration doesn’t necessarily mean a toothpaste offers an effective result. The fluoride contained in toothpaste is usually soluble, meaning that its effects do not last very long, washing away very quickly.
As such, it’s important for clinicians to consider options that provide their patients with long-lasing results.
Low concentration and slow-release fluoride
Clinicians may instead consider recommending a toothpaste option which contains a lower concentration of fluoride, which is released over a longer period.
BioMin® F, the innovative fluoride-containing toothpaste from BioMin® incorporates fluoride in the structure of a bioactive glass, alongside phosphate and calcium ions. By capturing the fluoride within the toothpaste’s structure, it is able to adhere to the tooth surface and dissolve slowly – gradually releasing a continuous supply of fluoride over 12 hours. BioMin® F works with the saliva to produce fluorapatite which is deposited on the surface of the teeth and in the dentinal tubules, which strengthens and protects the tooth enamel. Additionally, BioMin® F acts as a pH buffer as it’s gradually released. This means that, when a patient consumes acidic food or drink, the levels of acid in the mouth are kept to a minimum.
By carefully considering the recommendations clinicians make to patients, taking into account all of the potential risks and shortfalls of particular fluoride toothpastes, they can offer their patients an effective, long-lasting solution.
For more information about BioMin®, and the innovative range of toothpastes, please visit www.biomin.co.uk or call 0203 281 7282.
References
i. NHS. Fluoride. August 24. https://www.nhs.uk/ conditions/fluoride/ ii. NHS. Flupride. July 24. https://www.nhs.uk/ conditions/fluoride
iii. UK Health Security Agency. Water fluoridation – what it is and how it helps dental health. July 24. https://
ukhsa.blog.gov.uk/2016/04/13/water-fluoridationwhat-it-is-and-how-it-helps-dental-health/ iv. Nassar, Yomna, and Melina Brizuela. “The role of fluoride on caries prevention.” StatPearls [Internet]. StatPearls Publishing, 2023.
v. Medical News Today. Why do we have fluoride in our water? July 24. https://www. medicalnewstoday.com/articles/154164
vi. Gov.uk. Chapter 9: Fluoride. July 24. https://www. gov.uk/government/publications/deliveringbetter-oral-health-an-evidence-based-toolkitfor-prevention/chapter-9-fluoride













Acareer break is generally defined as a period of unpaid leave from work lasting more than two months – often without a specific job to come back to afterwards. Around 90,000 people in the UK take some form of career break every year, and 32% of the working age population have had a career break at some point in their lives.i
There are many factors which could unexpectedly extend a clinician’s career break, for example in recent years the COVID-19 pandemic and overseas conflict.
Parents returning to a new workplace after a long break can find the process daunting, but especially so if they are also adapting to a new country and facing additional obstacles such as exams.
For example, Dr Clara Preethu qualified as a dentist in India in 2006. After a year in private practice, she moved with her husband to the UK, and took a career break to raise her two children. When she was ready to take the Overseas Registration Exam (ORE), COVID hit, meaning her progress was slower than she hoped, which affected her confidence.
International dentist, Dr Shameem Nisa Gulam Mohamed also struggled with her confidence after having to extend a career break. Following her qualification in India, she moved to the UK. However, soon afterwards, Dr Mohamed needed to take an extended career break to look after her severely ill son. Re-entering the profession after a ten-year gap, as well as practising in a new country, was a daunting experience.
For dental professionals, a career break from dentistry could represent an opportunity to dedicate time to professional development, raising a family, travel, pursuing personal interests or to benefit from an emotional reset. However, returning to a career after a long period of absence can require hard work, mentoring, flexibility, structure and support.
Resuming practice after a long pause can be especially challenging for overseas dental professionals who have not yet practised in the UK, or for those who have taken extended leave from practice due to challenging circumstances – like illness, caring responsibilities, or having refugee or asylum status. Those returning after addressing physical or mental health issues may also face additional worries about re-joining the profession.
More than a third of individuals returning to the workplace after a career break experience a dip in confidence. Women are more likely than men to take extended leave from their careers, and are twice as likely to feel less confident about returning to work.ii According to a 2022 survey, 64% of women have taken a career break, with 22% taking extended time away from work due to childcare commitments. Additionally, 60% of women say they were nervous about returning to work after taking time out to have children.iii
Those who have taken time away to deal with physical or mental ill health may lose confidence due to stigma associated with their illness, as well as possibly struggling with debilitating symptoms. Fearing judgement or discrimination, they may not wish to disclose their health condition to a new employer, meaning they miss out on reasonable adjustments and necessary support.
A lack of confidence can significantly impact performance and patient care, so alongside the relevant requirements,iv individuals are advised to take measures to address their emotional and mental resilience before returning to practice.v
Building confidence and returning to work
Dental professionals returning after a long career break benefit from mentoring and support as well as opportunities to work flexibly.vi

Rodericks Dental Partners works hard to accommodate the needs of those returning to practice after a career break. At the centre of the group’s culture is a philosophy that ensures colleagues are supported by dedicated mentors, that their clinical expertise is respected, and they are empowered to work as flexibly as they need. As Dr Preethu says: “I feel very lucky to have had a lot of support from encouraging and helpful mentors at Rodericks Dental Partners. It’s really helped me.” Dr Mohamed adds: “After a 10-year gap, I was afraid I wouldn’t get the support I needed, but I’ve got an excellent mentor – he’s given me back my confidence.”
Returning to practice after a long break requires courage, time and commitment. Those who are able to return within a supportive network and structured framework are much more likely to succeed and flourish in their renewed careers.vii
To find out more about what it’s like to work with Rodericks Dental Partners and to discuss current vacancies, you can visit https:// rodericksdentalpartners.co.uk/careers
References
i. Shoobridge G. The Power and Purpose of Taking a Career-Break! LinkedIn. June 2023. Available at: https://www.linkedin.com/pulse/time-take-careerbreak-gonzalo-shoobridge Accessed July 2024
ii. Morgan K. Why career breaks hit your confidence so hard. BBC.com. June 2021. Available at: https:// www.bbc.com/worklife/article/20210617-whycareer-breaks-hit-your-confidence-so-hard Accessed July 2024
iii. A new way to represent career breaks on LinkedIn. LinkedIn. March 2022. Available at: https://news.
linkedin.com/2022/march/new-way-to-representcareer-breaks-on-linkedin. Accessed July 2024
iv. Restoring your name to the register. General Dental Council. Available at: https://www.gdc-uk.org/ registration/your-registration/rejoining-the-register Accessed July 2024
v. Returner toolkit: helping you back to work. Gov. uk. March 2023. Available at: https://www.gov.uk/ government/publications/returner-toolkit-helpingyou-back-to-work/returner-toolkit-helping-youback-to-work. Accessed July 2024
vi. Returner toolkit: helping you back to work. Gov. uk. March 2023. Available at: https://www.gov.uk/ government/publications/returner-toolkit-helpingyou-back-to-work/returner-toolkit-helping-youback-to-work. Accessed July 2024
vii. Returner toolkit: helping you back to work. Gov. uk. March 2023. Available at: https://www.gov.uk/ government/publications/returner-toolkit-helpingyou-back-to-work/returner-toolkit-helping-youback-to-work. Accessed July 2024 n
GLENN RHODES

is










As part of the 75th anniversary celebrations of the BDHA (now BSDHT), Nick Coller spoke to some dental hygienists and therapists about the changing nature of their work and aspirations both inside and outside of dentistry. Many thanks to all those who took the time to share their experiences. Their responses make for interesting reading with clear themes often emerging.

by NICK COLLER
Nick Coller: What were your career aspirations when you first qualified?
Teaching, academia and research
• To be a tutor - Michelle Williams, Linzy Baker, Daniela Schadler, Harjot Bhogal and Maree Thomas
• To go into academia, research or teaching - Laura King
• To do a PhD - Ryan O'Donnell
• To work in community dental services (it was the only place dental therapists could work then) - Debbie Hemington
• To work as a paediatric dental therapist - Charlotte Eastwood-Bloom
• To do direct access dental therapy - Edith Gwatsvaira
• To have a career that would be compatible with being a mother one day - Maggie Jackson
To focus on excellence and serving the community
• To raise the pro le of dental hygienists in my local areaSarah Thorne
• To be the best DHT I could possibly be - Lisa Stone
• To work within remote and rural practice in ScotlandLizzie Aucott-Hall
• To own my own dental hygiene practice - Siobhan Kelleher
• To gain experience in every single sphere of dentistry that I could - Amanda Gallie
NC: Where has your career taken you?
Further education and research
• I am a clinical lecturer, part of the mentoring team and involved in published research at the University of Liverpool - Michelle Williams.
• I went into research and then studied for my master's degree. Now I lecture at Newcastle University, and have an NIHR fellowship - Ryan O'Donnell
• I am currently studying the nal module in the PGCert in teaching and learning in the clinical context - Julia Hollywood
• I was part of the Clinical Entrepreneur Programme (CEP) under NHS England and I did a Master’s in Global Public Health - Maria Martinez
• I completed a Masters of Education and now I teach the Masters of Education students at UHI -Lizzie Aucott- Hall
• I am working as a doctoral researcher full time in the Rural Insitute for Health at Lincoln University - Amanda Gallie
Dental voluntary work
• I volunteered as a hygienist in Kenya in the Maasai MaraRachael England
• I volunteered in Israel, working in a clinic set up for families unable to access dental treatment - Erica Leslie
• I undertook dental charity work with Dentaid in Uganda - Harjot Bhogal
Practice ownership
• I own my own practice - Pat Popat
• I am the clinical director of Dental Health and Aesthetics Dental Clinic - Luke Snelling
• I became a key opinion leader for Johnson and Johnson and clinical educator for NSK Ikigai Oral Hygiene Community - Gulab Singh
• I was a rep for for Dentocare , doing school visitsCharlotte Eastwood-Bloom




• I am a clinical educator for the NSK Ikigai oral hygiene programme and part of the clinical education team for TePe - Nina Farmer
• I work for Knowledge Oral Healthcare where I deliver mouthcare training to care home sta - Emma Clayton
• I lm content for Dentsply Sirona and Colosseum
Dental - Cherise Gould
of dental related businesses
• I launched DentalDirectives, which helps dental practices with Patient Group Directions. We also provide consultancy services to dental compliance services such as Agilio - Benji Blum
• I recently became a postgraduate course provider with Edqual - The PgDiploma in Oral and Positive Health. It is the rst course of its kind globally. I also run my own conference yearly, The Magic of Education - Siobhan Kelleher
• I worked with manufacturers and developed VisionPerio brushes - Maggie Jackson
Working for BSDHT and other societies and associations
• I served as BSDHT President Elect (2018-2020) and then as President (2020-2022) - Diane Rochford
• I joined the board of the Association of Dental Implantology. I am also on the board for Barts and the London Dental Club - Linzy Baker
Further training in other dental fields
• I quali ed as an orthodontic therapist - Amanda Borthwick, Benji Blum
longer
• I am Education and Public Health Manager at FDI World Dental Federation in Geneva - Rachael England
• I have now left clinical dentistry and run my own aesthetics clinic and training academy - Lisa Moore
• I am a compliance analyst, which involves using a wide range of skills from data analysis, policy writing and understanding dentistry as a business - Daniela Fowler
NC: Have you embarked on any work outside the profession of dental hygiene and therapy?
Sports and wellness
• I have undertaken seven teaching quali cations in ballroom, latin and classical sequence dancing including two fellowship quali cations - Michelle Williams
• I am a re exology practitioner, reiki master and therapeutic facial therapist. I have worked backstage
at music festivals treating various performers from the Kaiser Chiefs to Dizzee Rascal - Erica Leslie
• I am a nutritional therapist - Nina Farmer
• I was the Wales Masters Hockey Manager and was an international player all over the world - Maree Thomas
• I provide wellbeing training for companies and universities - Siobhan Kelleher
• I got into bodybuilding and competed from 2016-2019. This led me to buying a gym - Pat Popat
• I have become a yoga teacher - Amanda Borthwick
• I became an infant massage instructor - Shaheena Valimahomed
Healthcare
• I am a facial aesthetics trainer - Linzy Baker
• I studied to become a physician associate. I now work as a research o cer for the British Skin Foundation and in scienti c communications for the Skin Health AllianceSarah Thorne
Small business
• I currently have a ‘side hustle’ making cupcakes (Gouldylocks Bakes) - Cherise Gould
• I make and sell jewellery on Etsy - Harjot Bhogal
Community spirit
• I am a community leader helping to build healthy communities for women abroad - Vincenza Sgura
• I am secretary and treasurer for a UK-wide Land Rover club - Daniela Schadler
NC: What has been the biggest change in the profession since you qualified?
Aesthetic focus
• People are becoming more focused on their appearance and wanting to achieve the perfect smile - Amanda Jordan
Scope of practice and working practice
• Extending scope of practice for dental therapistsMichelle Williams, Ryan O’Donnell, Diane Rochford, Julia Hollywood
• Direct access - Kevin Oates
• More male DHTs - Gulab Singh
• Regulations. I quali ed the same year CQC came into being - Amy O’Brien
Professional importance and gravitas
• Respect for hygienists (and therapists) in and outside of our profession and the possibility to continue to post graduate quali cations - Maggie Jackson





• Patients are more aware of the link between oral health and their general health - Cherise Gould, Amanda Jordan
• The number of DCPs being trained each year (and the entry quali cations required) - Lisa Moore
NC: What changes do you see ahead in the profession of dental hygiene and therapy?
Influence of technology
• Increased use of digital technology - Asia Begum
• Beyond receiving our own performer number…fairer remuneration including pensions - Ryan O’Donnell, Maggie Jackson, Sarah Thorne
When the BDHA was founded who would have thought that as a profession we would have come so far. It is clear that we are a motivated and exceptionally talented workforce who relish every opportunity. Here’s to the next 75 years with the BSDHT continuing to ensure we are able to help our patients and society to our maximum capacity and reach our full potential.


• Arti cial intelligence will eventually provide individual patient care plans by identifying patients at high risk of oral disease - Rachael England
• Robots…Gulp! - Charlotte Eastwood-Bloom
Working Practice
• Therapy led practice model - Ryan O’Donnell, Erica Leslie
• Maggie Jackson 1961
• Debbie Hemington 1983 Therapist, 1987 Hygienist
• Erica Leslie 1986
• Amanda Jordan 1988
• Diane Rochford 1996
• Maree Thomas 1996
• Amanda Gallie 1996


• A ‘refer up’ model with the DHT being the rst contact who then refers on any treatment out with their remit to a dentist - Lizzie Aucott-Hall
• Mandatory nursing support - Erica Leslie, Diane Rochford, Shaheena Valimahomed, Asia Begum
• More environmentally focussed dentistry - Linzy Baker
• Importance and focus in good clinical note takingAmanda Jordan
The impact of the WHO's Global Health Action Plan
• The WHO is calling on the government to consult with mid-level professionals in the workforce to support prevention. I feel this could be our golden ticket - Siobhan Kelleher
• Dental hygienists and therapists within primary healthcare working closely with medical colleagues - Rachael England
• Increased recognition and involvement in oral health promotion programmes and international collaboration - Vincenza Sgura
Scope of practice
• The right to prescribe not just exemptions– Lisa Moore, Luke Snelling, Alisa Yalcin
• Conversion courses for hygienists and therapists to complete a BDS/BChD - Pat Popat, Linzy Baker, Rachel England
• Top up modules for therapists to be able to provide more treatment options, eventually leading to be able to sit BDS exams - Benji Blum

• Kevin Oates 2001
• Sarah Thorne 2002
• Siobhan Kelleher 2002
• Lisa Moore. 2003

• Rachael England 2006
• Michelle Williams 2008
• Benji Blum 2008
• Amanda Borthwick 2009
• Gulab Singh 2009
• Luke Snelling 2009
• Amy O’Brien 2010
• Lizzie Aucott-Hall 2010
• Shaheena Valimahomed 2011
• Maria Martinez 2012
• Pat Popat 2012 Therapist, 2014 Hygienist
• Nina Farmer 2013
• Vincenza Sgura 2013

• Emma Clayton 2013
• Lisa Stone 2013
• Charlotte Eastwood-Bloom 2014
• Cherise Gould 2014
• Harriet Elsworthy 2014
• Asia Begum 2015
• Linzy Baker 2017
• Julia Hollywood 2017
• Daniela Schadler 2019
• Harjot Bhogal 2019
• Ryan O'Donnell 2020
• Alisa Yalcin 2021
• Edith Gwatsvaira 2022







Kenvue is delighted to bring you this article, with the aim of supporting the ongoing Enhanced CPD needs of dental healthcare professionals in improving and maintaining the oral health of their patients.
The aim of this article is to explore the implementation of the stepwise approach from the British Society of Periodontology’s S3 Treatment Guidelines for Periodontitis (BSP-S3) within the parameters of the Avoidance of Doubt document and a phased treatment approach.
On completing this Enhanced CPD session, the reader will:
• Understand the phased treatment approach outlined in the updated ‘Avoidance of Doubt: provision of phased treatments’ document
• Understand the specific components and goals of each step in the BSP-S3 guidelines, from initial risk factor control and behaviour change in Step 1 to supportive periodontal care in Step 4
• Understand the importance of patient engagement, compliance and motivation in achieving successful periodontal treatment outcomes
• • Understand the criteria and processes for referring patients to Level 2/3 specialist services, particularly for complex cases of periodontal disease.
Learning Outcomes: A,B,C,D
This article explores the implementation of the stepwise approach from the BSP’s S3 Treatment Guidelines for Periodontitis within the parameters of the Avoidance of Doubt document and a phased treatment approach.
In July 2021, the Chief Dental Officer of England issued the updated ‘Avoidance of Doubt: provision of phased treatments’ (AoD) document to support dental professionals, and to clarify where it might be appropriate to provide phased treatment spanning over several courses of treatment (CoT).1
Phased treatment may include up to three courses within a 12-month period. The first course (CoT 1) typically involves an initial assessment, pain relief, disease stabilisation, and preventive measures, as a detailed plan for further treatment may not be possible at this stage.1
After completing CoT 1, the patient is reassessed to develop the second course of treatment (CoT 2). In some cases, a third reassessment and plan (CoT 3) may be needed. Patients should be informed from the start that additional treatment may be necessary, potentially incurring further NHS dental charges. The exact nature and cost of subsequent phases can only be determined after reassessment.1
The AoD update was developed to align with published guidelines on the prevention and treatment of periodontal disease, ensuring that care is prioritised for those with the greatest need.2 Thus, when the S3 Treatment Guidelines for Periodontitis were adapted for UK use, the British Society of Periodontology (BSP) took AoD into consideration.3
When describing the aim of the document, the BSP emphasised its role in supporting the delivery of optimal periodontal care under the existing General Dental Services (GDS) contract. This is to help ensure that dental professionals can focus their resources on patients who engage in behaviour change, risk factor control, and improved oral hygiene. The resulting goal is to achieve periodontal stability or, if necessary, refer patients to Level 2/3 services.3
On a practical level, the BSP implementation of the European S3-level evidence-based treatment guidelines for stage I-III periodontitis in UK clinical practice (BSP-S3) promotes a stepwise approach to periodontal therapy. This approach organises treatment into four structured steps, each incorporating key components of the guidelines.4
The Scottish Dental Clinical Effectiveness Programme states: ‘The first step of therapy, which is relevant to all patients, aims to build the foundations for optimum treatment in terms of risk factor control and behaviour change. For some patients (i.e. those with a diagnosis of health or gingivitis), this step of therapy may be all that is required. However, for patients with periodontitis, it is the start of the process of stabilising disease.’4
Adding to the picture, Keh and Yonel (2024) wrote: ‘Step 1 should be tailored for the patient throughout the treatment journey and jointly with clinical findings and medical history.’5
In line with this, components included in Step 1 are as follows:4,5
• Explaining the patient’s disease status and risk factors, discussing the risks and benefits of treatment or no treatment
• Emphasising the importance of patient-performed oral hygiene to control inflammation and providing instruction on effective toothbrushing and the use of appropriate interdental aids
• Building patient motivation and confidence to maintain daily oral hygiene, make necessary lifestyle changes (such as quitting smoking and managing diabetes) and attend professional visits
• Reducing risk factors through interventions like smoking cessation and diabetes control, and removing plaque-retentive factors
• Performing professional mechanical plaque removal (PMPR), including the removal of supra- and subgingival plaque biofilm and calculus from the clinical crown. (Note: Removing accessible calculus from root surfaces is acceptable in Step 1 of treatment)
• Continuously monitoring the response to treatment by assessing plaque levels, gingival bleeding and patient engagement.
Keh and Yonel (2024) further emphasised that it is crucial to communicate the seriousness of disease progression and the extensive inflammatory response to patients. The stepwise approach prioritises oral health education and prevention in Step 1, but some patients may still need referral to secondary or specialist periodontal care. According to UK referral criteria, this includes cases that exceed general dental practice capabilities, such as advanced disease in young patients, combined periodontal and orthodontic treatment, and complex periodontalrestorative treatment planning.5
Adding a note about Level 2 and 3 care, Keh and Yonel (2024) explained that the document ‘Delivering phased-care for periodontitis patients under UDA banding: Roadmap to prevention and stabilisation’ can be used when planning treatment for periodontitis patients with additional restorative needs.5
Step 2 involves subgingival instrumentation to control inflammation and remove subgingival plaque biofilm and calculus in periodontitis patients where complete calculus removal was not achieved in Step 1.4
As well as targeted subgingival PMPR, there needs to be ongoing support for risk factor control (e.g. oral hygiene, smoking cessation, diabetes control), and motivation reinforcement by addressing possible barriers.4
Guo and Sharma (2024) furthermore suggest that several potential adjunctive therapies may be used during Step 2, alongside mechanical plaque removal, to disrupt the subgingival biofilm or alter the host immune response, noting that the BSP-3 guidelines evaluated the evidence base for these therapies.6
Before starting Step 2, the benefits should be assessed based on Step 1 outcomes. Some patients may need to repeat Step 1 if they lack motivation, as Step 2 is time-consuming and relies on optimised plaque control.4
After Step 2, treatment response needs to be evaluated. If goals like improved plaque control and reduced pocket depths are met, moving to Step 4 (maintenance) is likely to be appropriate. If not, repeating Step 1 or moving to Step 3 should be considered.4
Moving on to Step 3, this focuses on treating nonresponding sites with residual deep probing depths unresolved by Steps 1 and 2. This phase may involve additional subgingival PMPR or referral to specialist care.4
As stated by Vithlani and Ide (2024), ‘The third step of periodontal treatment is aimed at treating those sites that have not responded adequately, targeting non-responding or residual deep pockets.
‘The purpose of non-regenerative surgery is to achieve access to root surfaces associated with residual pockets for further subgingival instrumentation, aiming to eliminate those lesions that add complexity to the management of periodontitis (such as infrabony defects, root concavities and furcations).’7
They continued to explain that at these localised sites, the primary goal of periodontal surgery is to enhance direct visibility and access for professional instrumentation. This helps in reducing or correcting anatomical factors, partially regenerating lost periodontal tissues where feasible, and ultimately fostering an environment that is both easy and comfortable for maintenance by the patient and dental professional.7
Ongoing support for risk factor control (e.g., oral hygiene, smoking cessation, diabetes control) should continue as needed. Patient motivation for further treatment or referral and the availability of specialist services should be considered in the treatment plan.4
If specialist referral is not an option, subgingival instrumentation is to be repeated at deep sites to achieve maximum improvement before progressing to Step 4.4
Step 4
Step 4 of therapy involves a programme of supportive periodontal care (SPC) aimed at preventing deterioration, maintaining stability, and identifying and managing early signs of deterioration, with BSP-3 providing clear direction of how to achieve successful SPC. It combines prevention and treatment, relying on the patient’s ongoing oral hygiene and risk factor control, along with disease monitoring by the dental team.4,8
Leyland and colleagues (2024) emphasised: ‘The long-term success of periodontal treatment is critically dependent on the implementation of a regular programme of supportive periodontal care (SPC). An SPC programme involves regular recall intervals of between 3 and 12 months according to a range of factors, including patient compliance, presence of risk factors and severity of initial disease.’8
Where disease recurrence is detected, (re)treatment should be considered and agreed upon with the patient. Over the long term, recall intervals can be adjusted based on individual risk and presentation.4
However, for patients where further treatment is unlikely to yield improvement, the transition from Step 3 to Step 4 is less defined. If periodontal stability is not achieved, Step 4 aims to maintain a steady state, even if some sites have probing depths greater than 4mm.4
It is also worth noting that SPC requires collaboration between dental professionals, especially general dentists, dental hygienists and dental therapists. Dental hygienists and therapists, focusing on early detection and timely
1. When was the updated ‘Avoidance of Doubt: provision of phased treatments’ document issued by the Chief Dental Officer of England?
a) January 2021
b) April 2021
c) July 2021
d) October 2021
2. What is typically involved in the first course of treatment (CoT 1) according to the phased treatment approach?
a) Complete periodontal surgery
b) Initial assessment, pain relief, disease stabilisation and preventive measures
c) Only preventive measures
d) Referral to specialist care
3. What is the primary goal of Step 1 in the BSP-S3 guidelines for periodontal therapy?
a) Perform advanced periodontal surgery
b) Build foundations for optimum treatment in terms of risk factor control and behaviour change
c) Immediate complete removal of all calculus
d) Referral to secondary care
4. What does Step 2 of the BSP-S3 guidelines primarily involve?
a) Subgingival instrumentation to control inflammation and remove subgingival plaque biofilm and calculus
b) Immediate periodontal surgery
c) Final maintenance therapy
d) Providing oral hygiene instructions
5. What is the focus of Step 3 in the BSP-S3 guidelines for periodontal therapy?
a) Final maintenance therapy
b) Treating non-responding sites with residual deep probing depths unresolved by Steps 1 and 2
c) Immediate referral to orthodontic care
d) Only professional mechanical plaque removal
intervention, are uniquely positioned to identify subtle changes in periodontal status, ineffective home care, adherence issues, and emerging risk factors.8
This proactive strategy helps prevent disease relapse and maintain periodontal stability by promoting regular monitoring and collaboration among clinicians. It embodies the MECC (make every contact count) philosophy of maximising the impact of each patient interaction.8
team effort
As stated succinctly by Leyland and colleagues (2024), ‘Periodontal health is a team effort between the patient and the dental team, with general dentists, dental hygienists and dental therapists collectively forming the backbone of supportive periodontal care. Patients are integral to the success of periodontal treatment and achieving long-term oral health. Their active and ongoing participation in maintaining meticulous oral hygiene practices, attending regular appointments, and communicating any concerns with their oral and systemic health is vital. Studies
of long-term outcomes of treatment for periodontitis consistently identify compliance as one of the main determinants of long-term success.’8
In addition, the patient must actively follow homecare recommendations and commit to attending scheduled recall appointments. These recall intervals should be evaluated and adjusted at each appointment based on the latest assessment. It is also important for the patient to understand that the frequency of these intervals may change.8
Ultimately, without SPC, there is an increased risk of relapse, attachment loss, bone loss, inflammation, deeper pockets, greater tooth mobility, and, finally, tooth loss.8 n References available upon request
Cat Edney DT PgDip(Dist) explores the most effective use of ultrasonic tips and how to match each treatment stage with the most appropriate tip selection
Learning aims and objectives
• Educate readers on the key shapes and indications of ultrasonic tips
• Give readers an understanding of Piezo technology and how this guides the technique
• Heighten awareness of how different ultrasonic tips can be used at different treatment stages of patient care
Learning Outcomes: C
Ultrasonic instruments have been used in dentistry since the 1950s. Initially they were used to cut teeth but quickly established a niche in scaling, being used to remove deposits from hard tissues. This aids the dental professional in the efficient removal of plaque retentive factors and aids the patient in better home care.
Why ultrasonic?
In an ultrasonic tip the mechanical ultrasonic vibrations are generated within a thin metal probe meaning the working tip is the active component of the instrument. Cavitation occurs at the free end of the tip and increases with power, while the area and width of the cavitation cloud varies for different shaped tips.
The cavitation starts at the antinodes, or points of highest displacement, with little or no cavitation at the node. High speed image sequences, combined with scanning laser vibrometry show individual microscopic bubbles imploding and bubble clouds lifting and moving away from the ultrasonic scaler tip. With larger tips displacement causes more cavitation.
The resulting ultrasonic vibration helps to break up calculus and disrupt biofilm in an easy and effective way. The addition of water helps to reduce the heat created by ultrasonic movement, provides lavage to remove bacteria and aids acoustic streaming which can disrupt biofilm around the ultrasonic tip.
What is biofilm and calculus ?
Dental biofilms are communities of disease-causing bacteria that build up on oral surfaces including teeth, gums, restorations and prostheses. Left alone they can cause gingivitis, decay, and periodontal disease. ii 70% of biofilm comprise live organisms, in comparison to calculus (calcified dental plaque - mainly calcium phosphate salts), which has far less viable species, iii so although calculus has been shown to house biofilm, it is less virulent in comparison.
What is ultrasonic instrumentation?
The versatility of power ultrasonics is seen in its ability to chip hard deposits from teeth and remove infected debris from root surfaces of the teeth. Cavitation and streaming forces in the associated cooling water provide improved cleaning forces and are useful in reaching inaccessible areas in and around the teeth. iv
Magnetostrictive: Magnetostrictive power scalers, i.e. Cavitron (Dentsply Sirona), operate

at an optimal frequency of 20kHz and 30 kHz. Magnetostrictive scalers have an elliptical stroke pattern and all surfaces of the tip are active in the removal of debris.
Piezoelectric: Piezoelectric power scalers, i.e. the Varios Combi Pro (NSK), operate at a slightly higher optimal frequency of 29 kHz to 50 kHz. Piezo tips have a linear stroke pattern (forward and backwards) via crystals activated by the ceramic handpiece. Only the lateral sides of the tips are effective in the removal of debris
Piezo requires less water to control heat.
A piezoelectric handpiece is wider and more ergonomic than a magnetostrictive one and because there is less vibration, it is easier to hold and gives more tactile sensitivity. v
What tip when?
There are a number of different structures to consider in the oral environment which all have different shape, morphology and access challenges. Tip shape needs to be selected based on the clinical situation, comfort of the clinician and effectiveness.
The shape of the tip denotes the shape of the active area in cross-section and influences the
degree of contact achieved between the tip and the surface to be treated. vi Tip cross-sections can be round, semi-circular, rectangular, rhombus or diamond coated and tip selection relates to the different stages of treatment.
Stages of treatment
Manufacturers of ultrasonic instruments offer a wide choice of tip configurations. Tip selection is made easier by assessing key elements of the design in relation to the three key treatment stages of patient care.
Stage I: The removal of gross calculus and deposits is an essential first step to create access for the patient to be able to continue their oral health regime at home.
The G8 Varios ultrasonic tip (NSK) is designed for gross calculus removal. Its semi-circular cross section and two working edges means less gingival trauma even at high power settings.
For next-stage gross calculus removal, the G6 Varios ultrasonic tip (NSK) has a longer, finer tip, thin enough to treat the gingival sulcus and deeper interproximal sites. This tip is ideal for accessing the posterior region and to remove staining.

Stage II: When gross calculus has been removed but patients still require non-surgical periodontal treatment, a long, fine tip that is able to access periodontal pockets is required. The G16 Varios ultrasonic tip (NSK) has a semi-circular crosssection that can be used on higher power settings for gross debridement and to reach subgingivally on posteriors and deeper interproximal sites. For difficult to reach areas and for fine removal of tenacious subgingival calculus that cannot be removed with hand scalers, diamond coated tips are an ideal, but less-well-known solution. The P1d (NSK) is a long, fine diamond-coated tip with a circular cross-section that makes it easy to get under buccal and lingual furcations and into deeper interproximal sites, working in a similar way to a curette. (Note that prolonged use of diamond coated ultrasonic tips can create some disruption to the surface of dentine.)
Maintenance: Ultrasonic tips play a key role in the ongoing maintenance and control of dental plaque, biofilm and calculus on natural teeth and dental implants, both supra and subgingivally/marginally. vii
The P20 (NSK) is a long, fine ultrasonic tip that can be used on moderate/high perio settings for fine removal of biofilm and soft calculus with a circular cross section ideal for furcations. Similarly, the P25 (NSK) with its long fine round tip can be used on all perio settings and has a left or right bend option for furcation access.
Tip care and maintenance
One of the main considerations with ultrasonic tips is maintenance and wear of the tips. Tips must be cleaned, sterilised and maintained in three stages.
Stage I - Cleaning: Tips should be unscrewed from the handpiece using a torque wrench and all surfaces, including the handle and lead, should be wiped with alcohol-free wipes.
Stage II - Sterilise: Handpieces are for single patient use and must be sterilised between every patient. Place tips and handpiece in an autoclave cassette and run on a normal cycle.
Maintenance: Tip maintenance is extremely important. If a tip is worn, the cavitational effects and efficacy of the tip will be reduced. To prolong tip life always use the correct power settings and use tips that are made for the handpiece. Using a manufacturer’s ‘tip wear guide’ will clearly
brought to you by

1. In an ultrasonic tip cavitation occurs at:
a. the side of the tip
b. the free end of the tip
c. within the handpiece
d. in the middle of the tip
2. What percentage of biofilm comprise live organisms?
a. 50%
b. 85%
c. 70%
d. 60%
3. Piezoelectric power scalers operate at an optimal frequency of:
a. 29-50 kHz
b. 30-60 kHz
c. 35-55 kHz
d. 40-75 kHz
4. A tip in the red zone of a Tip Guide will be operating at:
a. -25% efficacy
b. -30% efficacy
c. -45% efficacy
d. -50% efficacy
5. Piezo tips have:
a. a linear stroke pattern
b. an elliptical stroke pattern
indicate the amount of wear: a tip in the yellow zone will be -25% efficacy; a tip in the red zone will be at -50% efficacy. Worn tips must be replaced.
To find out more
NSK offers a wide range of Varios ultrasonic scaler tips for clinical applications. NSK’s Tip Guide illustrates all NSK ultrasonic tips, their applications and compatibility with other makes of ultrasonic scaler handpieces and includes a Power Guide for each tip and a guide for using the Varios Tip Card to assess tip wear.
NSK’s Tip Guide is free to download at https:// mynsk.co.uk/wp-content/uploads/2021/09/NSKTip-Guide-web.pdf
Find out more about Varios Ultrasonic Scaler Tips with Cat Edney’s series of Top Tips videos available at https://mynsk.co.uk/ikigai/videos/
References
i. Vyas N, Pecheva E, Dehghani H, Sammons RL, Wang QX, Leppinen DM, Walmsley AD. High Speed Imaging of Cavitation around Dental Ultrasonic Scaler Tips. PLoS One. 2016 Mar 2;11(3):e0149804. doi: 10.1371/journal. pone.0149804. PMID: 26934340; PMCID: PMC4775067.
ii. https://www.rdhmag.com/patient-care/ patient-education/article/14278024/its-allabout-that-biofilm
iii. Gupta, S et al 2016
iv. Power Ultrasonics Chapter 24 Ultrasonic dental instrumentation A. D. Walmsley https://
www.sciencedirect.com/science/article/ abs/pii/B9780128202548000154#previewsection-abstract
v. https://pocketdentistry.com/3-what-isultrasonic-instrumentation/ vi. https://pocketdentistry.com/4-ultrasonic-tipdesign-and-selection/ vii. https://www.periodontalcare.sdcep.org.uk/ guidance/treatment-components/pmpr/ n
CAT EDNEY DH DT PGDIP (DIST)

Award winning Dental Therapist Cat Edney has over fifteen years’ experience working in specialist and private practice where she has developed a passion for multidisciplinary team working in a dental setting. Cat lectures nationally as a clinical educator for NSK, is part of the Smile Dental Academy faculty and has developed hands-on dental courses under her training brand ‘The Modern Therapist’. She aims to educate the dental profession about the role and integration of dental therapy, alongside focusing on providing gold standard hands-on training and ongoing support to dental teams.
To complete the questions and gain one hour of Enhanced CPD, visit cpd.the-probe.co.uklog in and find this course under the title ‘Top Tips for Piezo Ultrasonic Tips’

Brushing twice a day is only the starting point for a consistent oral hygiene routine.
Toothbrushing alone may only reach 60% of the tooth surface and removes a lowly 42% of the overall dental biofilm.i Poor biofilm disruption can lead to dental caries, gingivitis and periodontal disease.
Some individuals may find oral hygiene challenging, particularly those with Developmental Coordination Disorder (DCD), often referred to as dyspraxia. This common disorder affects the motor coordination in children and adults; writing, typing, riding a bike, driving and DIY tasks are some everyday aspects that individuals with DCD may struggle with.ii Coordinating movements is a complex process involving many different nerves and parts of the brain, so any problems within this process can inhibit movement and coordination.
According to the Dyspraxia Foundation, DCD affects up to 6% of the UK population.iii Those with it can often have attention deficit hyperactivity disorder (ADHD), dyslexia, autism spectrum disorder, depression and anxiety.iv Most of these conditions have also been connected to poor oral hygiene.v
Brushing up on your oral health
Toothbrushing requires a level of coordination that individuals with DCD may struggle with, especially children. This can lead to non-compliance and the neglect of their oral health – if regular toothbrushing already misses 40% of tooth surfaces, then a poor

brushing technique, common among individuals with DCD, will add to the problem. This increases the risk of gingivitis and periodontal diseases.
It is paramount that individuals with DCD protect their teeth. Brushing must be supplemented by interdental cleaning to ensure that the plaque biofilm is sufficiently disrupted.
Interdental cleaning is always recommended by dentists to clean the places that toothbrushes struggle to reach. For individuals with DCD, string flossing has been reported as “near-impossible” –preparing the floss and then manipulating the floss successfully between the teeth requires the precise coordination that individuals with DCD struggle with.vi As such, flossing has a low compliance because of its technical difficulty.vii
A helping hand
Instead of flossing, interdental brushing should be recommended to individuals with DCD. Interdental brushes are more effective at removing plaque from between the teeth than toothbrushes and are as good, if not superior, to string floss at reducing plaque and the risk of gingivitis.viii They are especially good for periodontal patients and are the preferred method for cleaning around implants.ix
For individuals with DCD, interdental brushes still demand some coordination. However, only half the hands are needed when compared to string flossing and the movement of an interdental brush is like using a key, with a simple in-and-turn motion.
There is no cure for DCD and its symptoms are largely dependent on the self-management of the individual. However, with patience, encouragement and education, individuals with DCD can improve their ability with certain tasks such as interdental brushing. Not only will this be a huge victory for their oral health, but the successful completion of a coordinated task, no matter how simple or complex, will boost their self-confidence.x Moreover, increased patient convenience and acceptability towards something new promotes compliance and comfort with new oral hygiene practices.xi
Recommended action
Surprisingly, there is very little research on oral care and DCD.xii To help raise awareness of the impacts
that DCD can have on oral health, having brochures or posters highlighting some of the problems in your practice can increase the chance of a patient discussing it with you. This can therefore help you to steer DCD patients towards interdental brushes as a method of reducing biofilm that is less technically complicated than flossing.
For an ideal interdental brush, consider FLEXI interdental brushes from TANDEX. With 11 different sizes, the FLEXI reaches all the areas a toothbrush cannot, reducing plaque comfortably. The ergonomic handle is flexible and the brush can be shaped perfectly, making it easier for individuals with DCD to coordinate their brushing and achieve success. FLEXI works brilliantly with PREVENT Gel, from TANDEX, a non-abrasive substance used like toothpaste that strengthens enamel and adds an anti-bacterial effect through the application of fluoride. With the right interdental brush and gel, plaque won’t stand a chance.
The indirect health impacts of DCD make it an important condition to be aware of. By supporting DCD patients by offering manageable solutions, you can ensure that their oral health is sustained by a consistent hygiene routine.
For more information on Tandex’s range of products, visit https://tandex.dk/
Our products are also available from CTS Dental Supplies https://www.cts-dental.com/ n
References available upon request.

Whilst supplementary oral hygiene steps are not always required for patients’ daily routines, sometimes patients need a little extra help to maintain their periodontal health. In these situations, it’s important to recommend products which include high-quality ingredients that offer targeted care.
Perio plus mouthwash range from Curaprox is designed for either short- or long-term use, depending on the patient’s situation, to help manage acute problems. For example, Perio plus can be used following invasive procedures like extractions and dental implant treatment to reduce the risk of infections. It is also ideal for temporary use when patients have caries, gingivitis, periodontitis, and peri-implant diseases.
So, what ingredients are included in Perio plus mouthwashes? And, what are the benefits these offer patients?
The Perio plus superhero ingredients
Perio plus mouthwashes contain a range of key active ingredients to support patients’ oral health. These include:
• Varying levels of chlorhexidine for an antibacterial effect
• CITROX®/P – a natural bioflavonoid combined with polylysine amino acids
• Xylitol – tastes great, protects against caries, and supports strong teeth
• PVP/VA – produces a protective film over teeth
CITROX®, a natural ingredient extracted from bitter oranges, is a bioflavonoid which aids in healing and is effective against dangerous pathogens such as MRSA, C. Difficile, Hepatitis A, Hepatitis B, and Streptococcus. Chlorhexidine has been used in dentistry for almost 70 years, thanks to its powerful antibacterial effect. When it’s combined with chlorhexidine, CITROX® can protect the mouth against a wide range of bacteria which cause oral diseases like caries and periodontitis.
CITROX® quickly and efficiently breaks down bacterial biofilm, allowing it to act fast and offer long-lasting effects. Not only this, but CITROX® is strong, making it less prone to bacterial resistance and enabling it to protect the mouth against the re-infiltration of bacteria.
Further to this, CITROX® is non-toxic, non-corrosive, non-carcinogenic, and non-allergenic, making it suitable for the majority of patients who need additional help with their oral hygiene. Plus, it’s dermatologically tested, biodegradable, safe, and eco-friendly.
When can CITROX® help patients?
CITROX® offers a range of healing and protective benefits when included in oral hygiene products. As such, it’s ideal:
• Before and after oral surgery
• Against periodontal disease
• Against candida infections
• Combined with chlorhexidine for enhanced protection
When a patient could benefit from supplementary oral hygiene products, recommend the Perio plus range to help them protect their mouth and reduce the risk of infection.
Choose Perio plus for patient compliance Perio plus is easy and fast for patients to use, making it perfect for reducing bacteria in the mouth when they’ve undergone oral surgery or are experiencing oral diseases and inflammation.
In addition to this, patients are highly likely to comply with the use of Perio plus mouthwashes because they:
• Provide protection against a wide range of bacteria
• Eradicate biofilm quickly and protect against its regrowth
• Have a pleasant taste and minimal side effects
Perio plus when it’s needed
Usually, for many patients, twice daily tooth brushing and once daily interdental cleaning are sufficient for maintaining oral hygiene and removing biofilm. However, when patients are undergoing dental treatments, have infections, or have caries, additional oral hygiene supplements can help to maintain their oral health.

Therefore, be sure to recommend the right Perio plus mouthwash to each patient depending on their unique situation. Perio plus Forte is the strongest in the range, with a chlorhexidine concentration of 0.2%, recommended for use before and after invasive dental procedures. Regenerate is recommended for comprehensive protection against gum and implant-related issues, with a chlorhexidine concentration of 0.09%. Finally, Balance is designed for occasional use to offer protection against plaque, ideal for patients undergoing orthodontic treatment, containing the lowest concentration of 0.05% chlorhexidine.
Recommend Perio plus products to your patients who need an extra oral hygiene boost.
For more information, please visit www.curaprox. co.uk and www.curaden.co.uk n


Shortages in the UK for Ozempic, a brand name for semaglutide, have been reported for long over a year. It is an effective treatment for type 2 diabetes, amidst a group of drugs called glucagon-like peptide-1 (GLP-1) receptor agonists. ii These also cause weight loss, making them a treatment option for chronic weight management in people living with type 2 diabetes and that are overweight or obese. iii
Recently, GLP-1 receptor agonists have gained popularity – Ozempic in particular – and quickly become household names as weight loss aids for individuals no matter their diabetic status. An increased demand developed, creating the aforementioned shortage which was expected to last until at least mid-2024. iv At time of writing, it is yet to subside.
Patients that use Ozempic must be treated with individualised care that recognises the potential oral health issues that can result from its use and side effects.
At current, there is not sufficient evidence to suggest that semaglutide solutions such as Ozempic or Wegovy have a direct connection to oral health.v However, common side effects and impacts can have knock-on effects and must be considered.
Ozempic is used to lower blood sugar levels, and does so by increasing the amount of insulin that the body produces. It also slows the movement of food through the stomach, and limits the amount of sugar that is released into the bloodstream.vi With food movement slowed, patients feel full for longer periods of time and can limit their diet, causing weight loss.
This function has potential links to oral malodours, with the term ‘Ozempic breath’ gaining traction.vii One animal study has found that the use of GLP-1 receptor agonists slowed digestion, which lead to the creation of volatile sulphur compound (VSC) producing gut bacteria.viii These play a significant role in malodourous gas production. Professionals may be able to help by recommending or providing oral hygiene adjuncts that mask and eliminate the odour, such as an effective mouthwash.

However, halitosis is multi-causal, and could be linked to poor oral hygiene. Clinicians should ensure this is not the case and direct patients to keep regular and effective oral hygiene routines. Interdental cleaning is particularly essential, as studies have found that interdental plaque contains a uniquely diverse microbial community which harbours high levels of VSC producing bacteria. ix

Patients that take Ozempic may be prone to common side effects, and must understand the risk these present to the quality of their oral health.
One study observing semaglutide use in overweight or obese patients saw a nausea prevalence of 44.10%, vomiting of 24.58% and gastroesophageal reflux disease (GERD) of 6.28%. x These were each at least double the occurrence within a placebo group.
Vomiting and its effect on oral health has largely been studied in the context of eating disorders. Whilst the circumstances are different, the effect remains the same; dental caries risk increases due to cariogenic food content consumed before vomiting, and the risk for dental erosion increases as acidic content from the stomach reaches the oral cavity. xi If patients brush their teeth immediately after vomiting, they are further prone to dental erosion. xi
The impact of GERD is similarly devastating. Dental erosion is the most common dental manifestation from this condition, with prominent observed impacts on the buccal, occlusal and lingual surfaces of the dentition. xii Hyposalivation is also often seen in obese individuals with GERD, xii which is important to note as Ozempic users may be taking the medication for weight loss. Patients with dry mouth are at a heightened risk of dental caries development. xiii
Keep an oral hygiene routine
Whilst Ozempic or other semaglutide solutions may not directly cause oral health issues, it’s clear that their side effects can impact many patients. People must be advised to maintain a high-quality oral hygiene routine to minimise the development of caries, dental erosion and oral malodours.
This includes twice-daily brushing with an effective toothpaste, and cleansing of the interdental spaces, where bacteria or acidic content may be left undisturbed. A solution like the WaterpikTM Cordless Advanced Water Flosser can access the interproximal and subgingival spaces – areas toothbrushes cannot reach as easily. The Cordless Advanced Water Flosser is 50% more effective for protecting gum health than dental floss,xiv and removes up to 99.9% of plaque after a 3-second application at treated areas.xv
Ozempic is one of the most in-demand drugs today. When a patient discloses its use, clinicians should look out for any oral health impacts and ensure patients can maintain the health of their dentition. This is possible with close support and a brilliant oral hygiene routine.
For more information on WaterpikTM Water Flosser products visit www.waterpik.co.uk. WaterpikTM products are available from Amazon, Costco UK, Argos, Boots, and Tesco online and in stores across the UK and Ireland. n
References available upon request.
ANNE SYMONS


Experience exceptionally lightweight loupes with crystal clear optics, designed and optimised




For a t as unique as for you. • you are.
Custom Measurements
Custom Fitting


Custom Fabrication




The scope of the dental professional has expanded in recent years. We now provide information and advice on so much more than just oral hygiene, including exercise and diet recommendations. Our goal is to facilitate the overall wellbeing of our patients. Plus, all these areas connect so improving one will often simultaneously enhance a person’s physical, mental and oral health. When it comes to diet, I was interested to come across an article considering supplements and their effectiveness. Are they necessary? When are they most beneficial? Should we as dental professionals be recommending them to patients? I did some reading…

Common dietary supplements
The five most common supplements taken by adults in the UK are vitamin D, vitamin C, vitamin B complex, vitamin A and vitamin E, although half the population chooses a multivitamin to cover several bases at once.i
Vitamin D
Approximately 1 in 6 adults have low vitamin D levels in the UK, which increases their risk of rickets. The vitamin is also important for a lowest risk of oral health concerns like dental cariesii and periodontitis,iii with research suggesting beneficial indications for endodontic treatment in patients with systemic health conditions like diabetes.iv The majority of vitamin D is absorbed from sunlight and there are limited dietary sources. Current recommendations from the Department of Health and Social Care are that adults and children should consider taking 10mg supplements daily between October and March, with some at-risk groups advised to continue year-round.v
Vitamin C
Around 1 in 20 people in the UK has a vitamin C deficiency, otherwise known as scurvy. The body can usually get enough vitamin C through absorbing sunlight and eating adequate fruit and vegetables. Key symptoms of scurvy include yellowing of the skin and eyes, fever and bleeding gums.vi NHS guidance does not suggest that additional supplements are necessary for the general population,vii particularly as excessive intake can cause headaches, nausea and dizziness, and increase the risk of kidney stones.viii
Vitamin B12
Vitamin B12 helps the body make red blood cells, keep the nervous system functioning and release energy from food. The recommended daily amounts can usually be obtained from eating normal amounts of foods like meat, fish, milk, cheese and eggs. Official advice is not to take supplements unless specified by a doctor. Taking less than 2mg a day is unlikely to cause harm,ix though taking too much may lead to pain, fever, itching, numbness of joints, shortness of breath, rapid weight gain or bleeding, among other adverse effects.x However, there is some evidence to suggest that older adults, vegetarians, vegans and those with
pernicious anaemia or gastrointestinal disorders may be more prone to vitamin B12 deficiency and may therefore consider supplements.xi
Vitamin A
Supporting the immune system, aiding vision and improving skin health, vitamin A is an important retinoid for the body. It also plays a crucial role in oral leukoplakia, oral sub mucous fibrosis and wound healing in the mouth.xii This is another substance that daily recommended amounts should be easy to achieve through a balanced diet – food like cheese, eggs, oily fish, milk and yogurt are ideal, though supplements may be useful in those with a proven deficiency. Consuming over the advised daily 1.5mg of vitamin A over many years can reduce the health of your bones and increase the risk of fracture in older age.xiii Excessive intake can also damage the liver.xiv
Vitamin E
Good for healthy skin, eyes and immune response, vitamin E is another substance that can be consumed adequately through a balanced diet. Found in plant oils, nuts and seeds, it can be stored by the body until needed so does not need to be eaten every day.xv An overdose of vitamin E can cause internal bleeding as well as thyroid problems, emotional disorders and gastrointestinal issues – it only becomes toxic with the use of supplements and rarely if ever due to diet alone.xvi
The verdict on dietary supplements
The above is only a snapshot of the dietary supplements available to the general population and the research surrounding it. The general consensus seems to be that supplements may be useful for some people, some of the time – although they are not needed by the majority of adults. If anything, excessive intake of certain vitamins can actually do more harm than good. There is also evidence to suggest that supplements do not lower risk of cardiovascular disease or malignancies when taken by otherwise healthy people.xvii
Like everything in healthcare, the recommendation for dietary supplements must be made on a case-by-case basis and tailored specifically to the individual’s needs. It may also be worth asking patients whether they already take extra vitamins to be included in their notes for future reference. Some food for thought!
For further information please call EndoCare on 020 7224 0999, or visit www.endocare.co.uk n
References available upon request.
THE AUTHOR
DR MICHAEL SULTAN

EndoCare, led by Dr Michael Sultan, is one of the UK’s most trusted Specialist Endodontist practices. Through the use of the latest technologies and techniques, the highly-trained team can offer exceptional standards of care – always putting the patient first. What’s more, EndoCare is a dependable referral centre, to which dentists from across the country send their patients for the best in specialist endodontic treatment
Oral cancer is a growing public health problem, with its incidence increasing worldwide and becoming more common across all demographics, including women and young people. As such, it’s important that clinicians and patients alike are familiar with its early signs and risk factors, to help limit patients risk levels, and to help detect mouth cancer in its early stages.

Oral cancer is becoming more common, with an increase in new cases and deaths in recent years – in 2020 there were an estimated 377,713 new cases and 177,757 deaths. Oral cancer can affect the lips, mouth, and oropharynx, and is the 13th most common cancer worldwide, being more common in men and older people. In Europe and North America, mouth cancer is becoming more prevalent in younger people due to human papillomavirus (HPV), whilst tobacco, alcohol, and areca nut use are some of the leading risk factors for the disease.
Public awareness of mouth cancer is poor meaning that many patients may not know that their habits or lifestyle may be putting them at risk of the disease. Because of this, it’s essential to educate patients when they attend their appointments, to help make them aware of the signs and the importance of attending the practice regularly. Oftentimes, a visual exam is not sufficient to detect mouth cancer in its early stages. As such, it is important that clinicians take into account a patient’s oral health, and other risk factors, along with undertaking pre-diagnostic tests to determine a patient’s risk level for oral cancer.
There exist strong associations between mouth cancer and poor oral hygiene. Research suggests that having fewer missing teeth, regularly attending dental check-ups, and toothbrushing twice per day are associated with a reduced risk of oral cancer. Additionally, poor dental hygiene aids the cancercausing potential of other known carcinogens –such as tobacco and alcohol, for example. However, even when adjusted for these factors, poor oral health may present a higher risk of mouth cancer. This is due to poor dental hygiene and the accumulation of plaque leading to a chronic inflammatory process. The environment promotes the development of oral cancer. A study revealed that periodontitis is an independent risk factor for mouth cancer, with the risk of oral squamous cell carcinoma increasing in the more severe stages of periodontitis. Another study found that 93.4%
of patients with oral squamous cell carcinoma reported to brush their teeth only once per day, and the majority (57.85%) never attended dental appointments. With the maintenance of dental hygiene, dentists and dental hygienists/therapists can help to prevent oral cancer. Further to this, clinicians should evaluate patients’ socioeconomic statuses and lifestyle factors to establish their level of risk. By educating patients about the relationship between oral hygiene and mouth cancer, clinicians can help to prevent the development of periodontal diseases and, in turn, reduce the risk of cancer.
It can be very difficult to detect oral cancer in its early stages, with initial symptoms appearing visually similar to other common issues – like mouth ulcers, for example. However, detecting it in stages I and II is essential for giving patients the best outcomes. When diagnosed and treated in its later stages, oral cancer treatment can have a lasting effect on patients, impacting their quality of life. Further to this, survival rates significantly improve when mouth cancer is detected in the early stages. Research suggests a 95% survival rate at five years for stage I mouth cancer, with stage IV cancer having a 5% survival rate at five years. As such, to significantly improve a patient’s prognosis, early detection is essential.

A great way of doing this is by testing patients with the BeVigilant™ OraFusion™ System from Vigilant Biosciences® as part of a health checkup. The non-lesion test rapidly detects oral cancerassociated biomarkers in 15 minutes or less. It analyses the patient’s saliva for biomarkers associated with oral cancer, as well as their risk factors to produce a report of low, moderate, or high risk for cancer. Ideal for chairside use during dental appointments, it offers clinicians a straightforward and accurate way to test their patients, aiding in the early detection of mouth cancer.
In order to improve outcomes for your patients, regular dental appointments, education, and improved dental hygiene is essential. With
many risk factors affecting all demographics, and a rise in women and young people getting mouth cancer, it’s important to ensure clinicians are tailoring the advice they provide their patients, and carrying out thorough exams and pre-diagnostic testing frequently. This will allow them to detect oral cancer in its early stages, and improve survival rates for their patients.
For more information, please visit www.vigilantbiosciences.com or email info@vigilantbiosciences.com n
References available upon request.
ABOUT THE AUTHOR










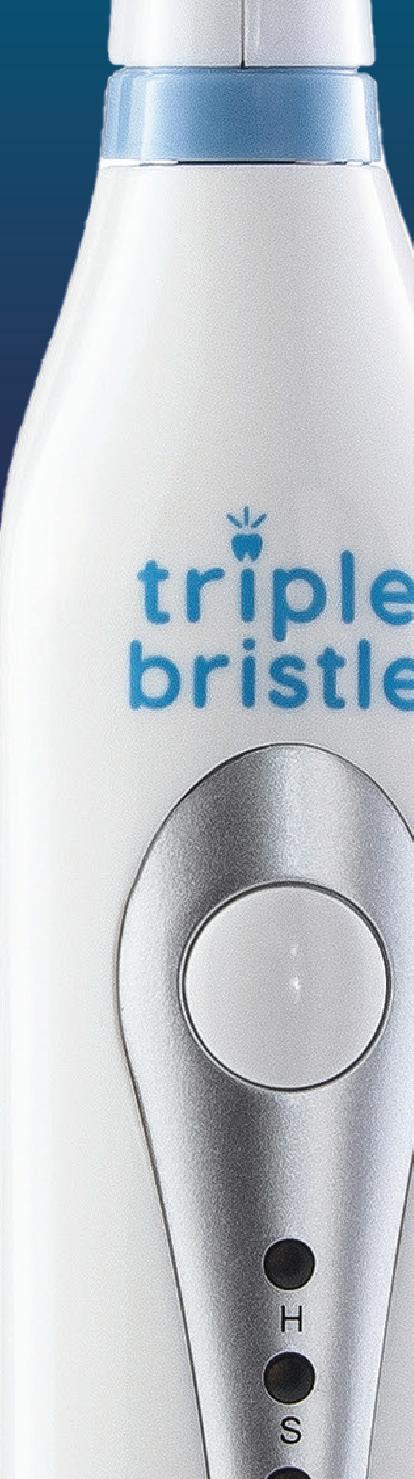
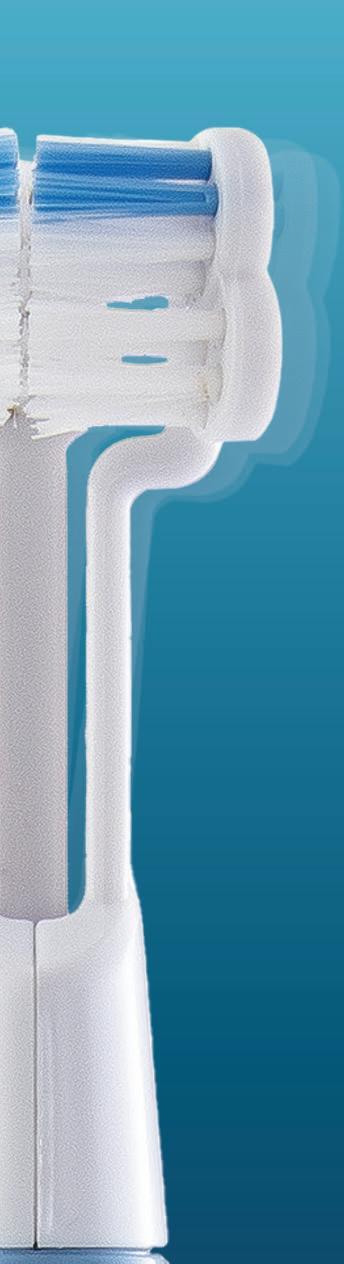






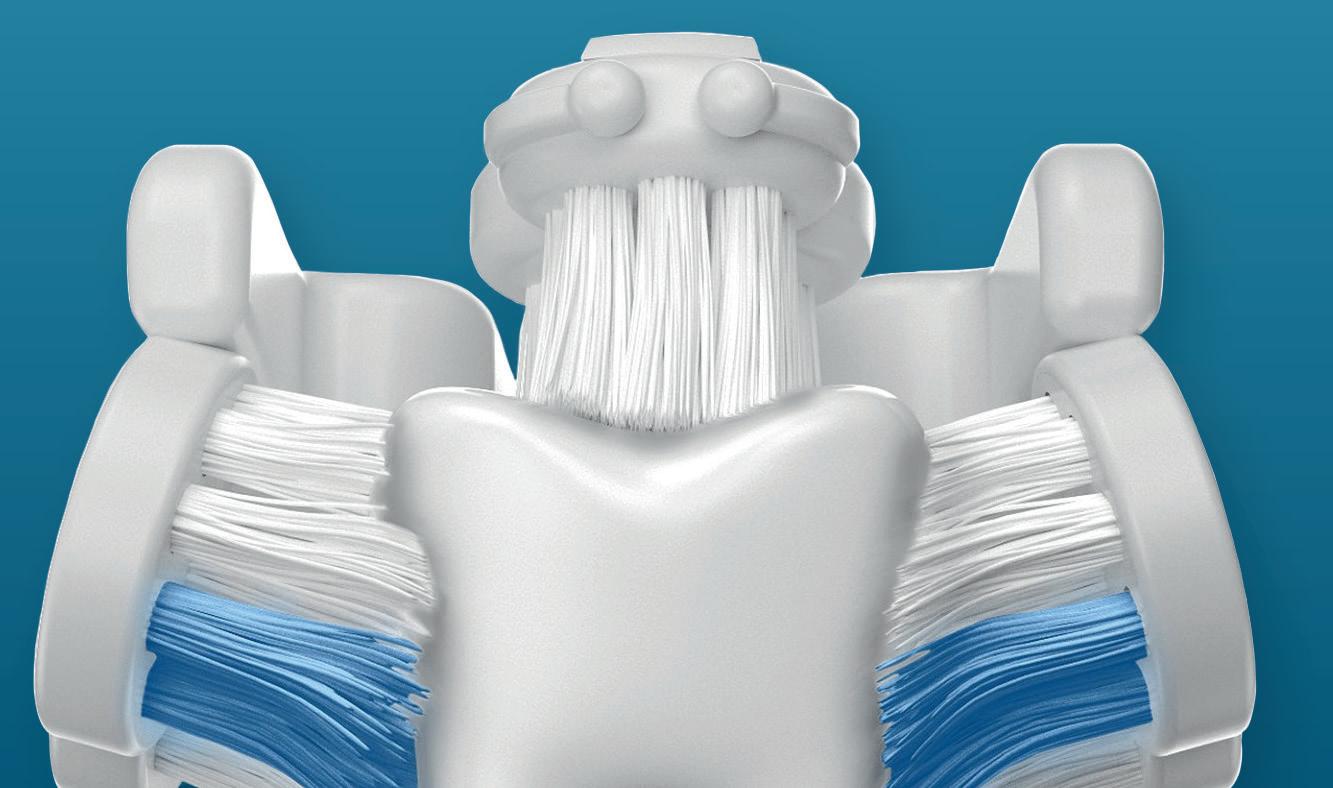




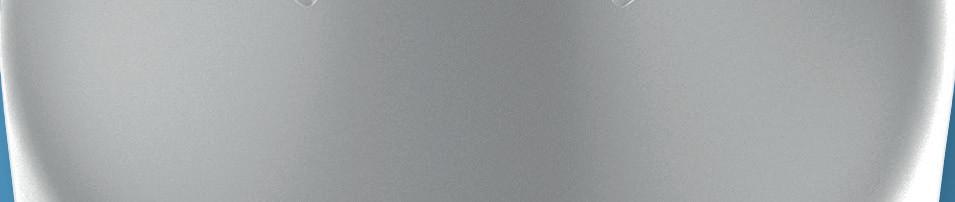
















Electric toothbrushes, especially sonic models, are proven to enhance oral hygiene significantly, yet many patients still face barriers to adopting this superior technology, writes Steve Wright
Electric toothbrushes, particularly Sonic Toothbrushes, have become recognised as a superior option in oral hygiene. Research consistently shows that electric toothbrushes are more effective at removing plaque and reducing gingivitis compared to manual brushing. A case in point, a systematic review highlighted that electric toothbrushes, especially those utilising sonic technology, can significantly improve oral health outcomes over time (Yaacob, 2014).1
Despite these benefits, half (51%) of adults who clean their teeth report that they use an ordinary manual toothbrush, according to the latest ‘Adult Oral Health Survey’ (Gov.uk, 2024).2 Understanding the barriers to electric toothbrush adoption can help dental professionals guide their patients towards better oral hygiene practices.
The evidence base
Sonic toothbrushes use high-frequency vibrations to enhance cleaning efficacy, reaching areas beyond where the bristles can physically touch. This technology helps to dislodge plaque, reduce gum inflammation, and support overall gum health, and it is essential in preventing periodontal diseases. Several studies have demonstrated that patients using sonic toothbrushes experience noticeable improvements in plaque removal and gum health when compared to manual toothbrush users.
For example, (Vibhute, 2012)3 systematic review compared the efficacy of manual and powered toothbrushes, including those with sonic technology. The findings consistently demonstrated that powered toothbrushes, particularly sonic types, are more effective at reducing plaque and gingivitis.
In addition, (FA, 2015)4 meta-review examined various homecare regimens, focusing on mechanical plaque removal, including using manual versus powered toothbrushes. The review concluded once again that powered toothbrushes, especially Sonic, provide superior results in managing gingivitis and plaque control over manual brushing.
Common barriers to adoption
1. Perceived cost
A major barrier for many patients is the perceived cost of electric toothbrushes. The upfront expense of an electric toothbrush, especially sonic models, can seem steep compared to manual options. However, patients often overlook the long-term benefits and cost savings associated with improved oral health and reduced need for dental interventions. Educating patients about the value of investing in a quality sonic toothbrush, such as those available from reputable brands like Kent Oral Care and its SONIK Toothbrush, can help shift this perception. Highlighting potential savings on dental treatments due to better oral hygiene can further motivate patients to make the switch.
2. Changing habits
For many patients, the thought of changing established oral hygiene habits can be daunting. The transition from manual to electric brushing can feel like an unnecessary complication, especially for those who have brushed manually for most of their lives. Dental professionals can play a key role in easing this transition by offering demonstrations and practical advice on how to use sonic toothbrushes effectively. Showing patients that these brushes do much of the work themselves can make the change seem less intimidating and more manageable.

3. Overwhelming range and confusion
The wide range of electric toothbrushes on the market can overwhelm patients. With options varying from basic models to those with multiple features and price points, the sheer variety can lead to confusion and decision paralysis. Patients might find it easier to stick with a familiar manual toothbrush rather than navigate the complexities of choosing an electric one. Dental professionals can assist by recommending reliable, user-friendly options that suit the patient’s specific needs, such as a straightforward sonic toothbrush that balances value, quality and ease of use.
4. Lack of education and awareness
Another potential barrier is a lack of awareness or understanding of the benefits of sonic toothbrushes. Some patients might not fully grasp how these brushes differ from manual ones or might harbour misconceptions that they are too aggressive for sensitive teeth or gums. Providing clear, evidencebased information about the advantages of sonic toothbrushes, including their gentle yet effective cleaning action, can help dispel these myths. Educating patients on proper usage can further boost their confidence in adopting this technology.
The role of dental professionals
Dental professionals hold a trusted position that enables them to influence their patients’ oral hygiene choices in an ethical manner. By offering informed recommendations and addressing common concerns, they can encourage patients to consider the benefits of electric toothbrushes, including sonic models, where appropriate. Judicial, individualised recommendations of reputable sonic toothbrushes can offer patients accessible and effective tools for enhancing their oral care routines without overwhelming them with options.
If you would like further information, please visit kentbrushes.com/oral-care n
References
1. FA, V. d. (2015). Efficacy of homecare regimens for mechanical plaque removal in managing gingivitis. National Library of Medicine.
2. Gov.uk. (2024, January 25). Adult oral health survey 2021: health-related behaviours. Retrieved from Office for Health Improvement & Disparities: https://www.gov.uk/government/statistics/adultoral-health-survey-2021/adult-oral-health-survey2021-health-related-behaviours
3. Vibhute, A. (2012). The effectiveness of manual versus powered toothbrushes for plaque removal and gingival health. National Library of Medicine.
4. Yaacob, M. (2014). Powered versus manual toothbrushing for oral health. London: John Wiley & Sons, Ltd.
THE AUTHOR

Many dental manufacturers claim their products make Dentists’ lives easier, but not every manufacturer makes it their mission. That’s unless it’s Centrix, the 50-years old dental innovator which launched the first direct-to-prep delivery system back in 1970.
Centrix continues to produce single-patient-use products designed to make dentistry easier. This includes the ubiquitous Benda Brush and Benda Micro brush; Tempit temporary filling materials; FluoroDose sodium fluoride varnish, which is now available in six patient-pleasing flavours and can be applied in less than a minute via its innovative LolliTray dispenser; NoMix moisture-activated temporary cement, which is designed for use in the surgery and at home in emergencies; Exposé disposable caries indicators which eliminate the need for measuring and mixing, and the risk of spillages; and many others.
Free sample of NEW DraganBerry flavoured FluoroDose!
Centrix have extended their range of Award Winning Fluorodose varnishes by launching NEW DraganBerry flavour! To obtain a free sample contact your local Trycare representative, telephone 01274 885544 or email dental@trycare.co.uk
Centrix’s FluoroDose 5% sodium fluoride varnish is easy to apply in less than a minute.
To make life easier, its packaging has patented features to enhance handling, comfort and patient safety. Containing a single dose of varnish, each LolliTray includes a Benda Brush applicator and is designed so that it “pops up” with one hand, making removal simple and safe.
Drying in seconds when contacting saliva, FluoroDose remains in situ for up to six hours for optimum fluoride uptake. It offers a smooth nonstringy or clumpy consistency, fast application and six patient-pleasing flavours – caramel, bubble gum, mint, cherry, melon and NEW DraganBerry! It is supplied in Introductory Packs containing the six original flavours and refills of all six individual flavours.
Freshly mixed prior to application it always has the optimum fluoride distribution, unlike syringes which frequently separate out leaving inconsistent mixes of ineffectively low and dangerously high fluoride concentrations. Each LolliTray contains enough varnish to protect a full adult dentition. Non-gritty and easy to apply in undetectably thin films, it is colourless so does not affect the appearance after bleaching etc.
Quick-drying and longlasting, FluoroDose is suitable for adults with caries risk factors and children. Applied as often as needed it is FDAapproved for treating dentinal sensitivity.

With today’s emphasis on minimally invasive dentistry, Clinicians want to ensure that their direct restorations remove as little healthy tooth tissue as possible. One thing that can help ensure this is a caries detection dye.

Exposé caries indicators make the use and application of a caries detection dye simple, mess-free and precise. Its wellknown Benda Micro brush applicator, available in either fine or extra-fine, is prefilled with a dry blue dye, which is simply touched onto a wet tooth to activate. The dye, which acts by staining caries by-products, stains active caries lesions thereby enabling the Clinician to identify precisely the tooth material to be removed. Plus, because it does not become liquid until it has touched the wet tooth there are no drips to stain clothing or soft tissue.
Benda Brush and Benda Micro brushes
While a brush is a seemingly simple tool, it’s important to have the right one for the job. When applying a precise amount of

material to a broad surface, the one-piece Benda Brush with its bendable brush head is ideal. The Benda Brush smoothly places and spreads fissure sealants, bonding and etching agents, whitening agents and other materials. Benda Micro brushes are perfect for applying smaller amounts of materials or when precise placement is required, such as with selective etching or single point placement.
Both brush heads can be angled with ease and remain in position without bouncing back. Their chemical-resistant, non-absorbent fibres are suitable for harsh substances. Disposable for easy clean-up, Benda Brush and Benda Micro brushes are available in two sizes and assorted colours, so they can be colour-coded to avoid cross-contamination.
All of these exciting innovations are now available from Trycare, the UK’s fastest growing dental dealer, who have been appointed sole UK Distributors for the complete range of Centrix problemsolvers. This expands further the comprehensive range of products available from Trycare, which includes everything you need from all the major manufacturers. Yet another reason to contact Trycare and “Discover the magic” for yourself!
For further information about the complete Centrix range contact your local Trycare representative, call 01274 885544 or visit www.trycare.co.uk/centrix.


Dental implantology produces a number of challenges, unique to this particular field. As such, it’s vital that those who provide implant dentistry come together to share their views, and experiences, to support the learning of others on their clinical journey. The Association of Dental Implantology (ADI) Team Congress is the perfect platform to experience this, with attendees able to hear from the leaders on topics relevant to them, and get involved in the discussions with their colleagues.
Spectacular speakers
The ADI Team Congress is delighted to introduce a range of excellent speakers, including both highcalibre clinicians and technicians, who are joining us to share their expertise in their sessions.
The line-up of clinicians includes:
• Tidu Mankoo
• Telmo Iceta
• Eddie Scher
• Professor Joseph Kan
• Raquel Zita Gomes
In addition to dental technicians:
• Bryan Matthews
• Peter Pizzi
• Alina Ceclan
• Lorant Stumpf
• Kevin Armstrong
• Hugo Patrao

This is a unique opportunity to expand your knowledge of dental implantology, with the ability to hear from a wide range of experts sharing their experiences, expertise, and techniques. This allows you to gather advice from various walks of life and form your own conclusions. At a Congress which is specifically tailored to those interested in dental implantology, the impressive line-up of speakers is able to expand your mind and help you achieve your ambitions.
Excellent education
The educational programme at ADI Team Congress 2025 is second to none. This is the ideal place to hear from internationallyrenowned speakers in a unique debate format. Speakers will be discussing key topics in implant dentistry. This is a great place to open your mind to other clinicians’ ways of work, enabling you to take these insights back to your practice and benefit your team and patients.
Hands-on workshops at the ADI Team Congress also promise to be a valuable educational tool. They are great opportunities to get expert advice and guidance on the latest developments, tools, and techniques in the world of implantology.
Further to this, the ADI Team Congress offers something for the whole dental team. This makes it ideal to attend with your colleagues, enabling the whole practice to benefit from high-standard education and great social events. Additionally, the

Next Gen programme means that clinicians who are new to implantology, and keen to find out more, are able to expand their knowledge of the field, and get to know the experts.
Attendees can gain up to 18.5 hours of eCPD from the ADI across the three days of Congress, all in one place.
The ADI Team Congress 2025 offers attendees a range of opportunities to socialise and network with their peers.
The Congress Drinks kicks off the festivities, celebrating the beginning of an event which enables new discussions and connections with other delegates. Additionally, the Congress Dinner promises to be an unforgettable experience –allowing you to enjoy a gourmet meal with friends and colleagues. Plus, for those who’d like to let their hair down, the Industry Party is a night of celebration and surprises.
Network with your peers and make new connections to support your day-to-day work at the ADI Team Congress 2025.
The ADI is delighted to offer a large trade exhibition at the ADI Team Congress, featuring your favourite brands in dental implantology and practice management. This is a great chance to browse the extensive stands and discover the latest technology and services that are on offer. The exhibition is a fantastic way to get in touch with brand representatives who are able to provide tailored advice to support your practice.
Join us in the free-thinking, vibrant city of Brighton and get involved in the ADI Team Congress. Indulge in the modern culture and admire the unrivalled architecture between lectures. With so much to do and see on the doorstep of the Congress, register and come along!
Register today for the ADI Team Congress 2025: adi.org.uk/association_dental_implantology_congress
For more information, please visit www.adi.org.uk Become a member today n
BSDHT
The International Federation of Dental Hygiene (IFDH) is an organisation that represents dental hygienists around the world. It was formed in 1986, and currently has 30 member countries, a number of individual members, and represents around 90,000 dental hygienists globally. Each member country may have up to two representatives who contribute to the annual House of Delegates meeting, which alternates between in-person and online meetings. This year, the UK was represented by BSDHT President Elect Rhiannon Jones and myself.
This year’s House of Delegates meeting was held at the Sheraton Grand Hotel in Incheon, South Korea, and, for the UK visitors, the first few days in Korea were raining and grey.
The week started with an afternoon of leadership workshops, which were run by Ondina Love and Tammy Filipiak. This was a valuable seminar where we shared the personal wins and challenges of being leaders. The group were empathetic and supportive of each other, and it really was a worthwhile afternoon.
Tuesday was an early start and we were reminded of the business of the IFDH, listening to the Board Member Reports and a brief overview from each of the member countries. The local organising committee and Chair from the Korean Dental Hygienists Association (KDHA) also gave an overview of what to expect during the next few days with some direction of the itinerary.
In the afternoon, we had the elections of the new board members, including my appointment to the role of Treasurer under the new President, Jill Rethman. Motions were debated that had been offered to the room in advance and one of the most exciting points that I’m able to share, is about how organisations for dental therapists, oral therapists, and oral health therapists, will now be permitted to join the IFDH as full members.
This is a positive step forwards because it demonstrates that the IFDH is an organisation that welcomes diversity and inclusion, and that it embraces all the preventive skills that the whole oral healthcare team offers. We all have a preventive mindset in common and that will not change. What could change is the opportunities for new and different trade companies to join the exhibition in the future. Companies that have not engaged with the IFDH before may now be keen to attend.
Wednesday saw the meeting continue and then it was a bus ride to the Gangnam region to check into our hotels before finding our way to the COEX conference centre for the rehearsal of the flag presentation part of the Opening Ceremony. It was so exciting walking to the COEX and seeing a huge gold sculpture of Psy’s Gangnam Style hands outside of the building.
There was free time after the flag ceremony rehearsal and people made their own plans for the evening. I joined the representatives from The Netherlands for a Korean BBQ meal which was an enjoyable experience. It was wonderful to share cooking and friendship together once again, having





met at previous meetings with the IFDH and the EDHF (European Dental Hygienist’s Federation).
Thursday was the official opening of the conference, commencing with a formal ribbon-cutting with the IFDH president, the President of the KDHA, and other dignitaries each playing their part.
The presentation of the flags of the member countries from around the world was so moving and such a moment of pride – it was a real honour to take part. The local organising committee from the KDHA had done a fantastic job of planning a most entertaining opening ceremony that was a feast of lights, music, and dance; we were thoroughly entertained and enthused, ready for the start of the Symposium.
The scene was very well set for the opening speeches from IFDH President Wanda Fedora and Conference Chair Jeongran Park before the conference got underway with the first speaker of the day. The entire Symposium saw numerous education streams in different rooms under the themes of ‘Collaboration’, ‘Optimisation’, ‘Reimagination’, and ‘Equality’, with varied presentations from speakers from around the world.
I was honoured to have been invited to judge four shortlisted entrants in the Oral Presentations category, an enjoyable group of presentations that showed merit in different ways. There was another group of five shortlisted presentations that were adjudicated in another room at the same time, and the overall winner was the first speaker that I enjoyed: Jiyoung Jung, a PhD student from the Yonsei University College of Dentistry, South Korea, with her presentation on ‘Patient autonomy and preference for dental decision-making with periodontitis patients’. Jiyoung and the other winners were awarded their prizes during the closing ceremony on Saturday afternoon.
The exhibition hall was just downstairs from the main auditorium, and this was where the posters could be viewed. This International Symposium of Dental Hygiene was generally supported by various sponsors and attended by numerous other companies. Intriguingly, there was a Bitcoin company stand that always appeared busy with a long queue, but I suspect this was due to the fact they were giving away free hot and iced coffees!
There was a Treasure Hunt card to complete with stickers throughout the exhibition, which you then traded for a lottery ticket, with the winners being drawn during the closing ceremony. The various trade stands were often well-engaged by the delegates, and I know I came home with bags and bags of samples that were generously provided by the different companies.
The KDHA had also arranged a Korean Culture Corner, which was a nice touch and a little bit of
fun. You could wear the traditional dress, a Hanbok, and have your photo taken. You even had the opportunity to buy local souvenirs or other gifts to help support the KDHA and could also ‘get your colours done’. There was another stand offering massages and nail treatments.
At the close of the first day, the House of Delegates and some invited guests had the President’s reception to attend, while there was a parallel reception open to other delegates at the same time. This was a lovely opportunity to unwind and talk with speakers and friends at the end of a successful opening day. Once the President’s reception had concluded, many of joined in with the larger reception and had the opportunity to catch up with industry friends.
On Friday morning, I had been invited to chair some presentations. Once again, new talent, new ideas, and some novice presentations were enjoyed by an enthusiastic audience who were keen to ask questions and learn some more detail.
The Gala Dinner was the social highlight of the Symposium and saw around 400 guests come together for an enjoyable meal and some varied entertainment to suit all tastes. This began with some musical theatre entertainers, who treated us to a selection of songs from the shows as well as wellknown Disney movies. A surprise of the evening was the Best Dressed competition, which saw 10 eager competitors take to the stage to strut their stuff. Finally, the moment we’d all been waiting for, the second best Psy in Korea appeared for our singing and dancing pleasure. ‘Fake-Psy’ and his dancers whipped the party into a frenzy, and one couldn’t help but get caught up in the moment. His energy and performance were a fantastic way to end the evening. Saturday’s presentations continued to offer opportunities for learning and the poster presentations continued in the exhibition hall. It was a final opportunity to visit the trade exhibition before the final presentation in the auditorium, which was Catherine Waldron from Ireland, and her work titled, ‘Let’s make toothbrushing the priority for people with disabilities: Practical tips and evidence to support people with disabilities achieve better toothbrushing routines’.
Before we knew it, it was time for the closing ceremony, including closing and farewell speeches. We enjoyed a slide show of the many photos that were taken across the course of the week, and this was a lovely tribute to everyone who had contributed. It was great to hear from Enrica Scagnetto, from the Italian Local Organising Committee, who shared with us the vision for the International Symposium of Dental Hygiene in 2026, in Milan. It is exciting to note that subsequent Symposia will be held in Dubai in 2028, and that The Netherlands successfully bid to host it in 2030, all of which we will look forward to.
As the Immediate Past President, Wanda Fedora received her pin badge, and introduced Jill Rethman as the new IFDH president. Jill paid tribute to Wanda and all that she has achieved during her tenure as IFDH President, before inviting the new IFDH Board to join her on stage. The Board were introduced to the audience; President-Elect, Fouzieh Elliasey; Vice-President, Sharon Friedman; Secretary, Carmen Lanoway; Treasurer, Miranda Steeples, and we all affirmed a pledge to the IFDH. This was a special moment and, so too, were all the goodbyes, and auf wiedersehens, that we shared.
To conclude this report, I want to say thank you to the IFDH, the local organising committee from the KDHA, and the BSDHT and sponsors who got me here and enabled me to participate in this fantastic event. n
On Friday 5th July, the winners of the 2024 Dental Awards gathered at The Ivy in London to receive their trophies and celebrate their victories along with members of the judging panel and sponsors
Following the virtual presentation that streamed in May on The Probe website and Youtube, the winners of the 2024 Dental Awards were invited to a celebratory awards lunch to be presented with their trophies in person.
The Private Room at The Ivy (the original on West Street) set the scene perfectly. While A-list celebrities dined on the ground floor, the best in British dentistry celebrated in style above.



After guests were greeted with a champagne reception, Dr Nigel Carter OBE, Chief Executive of the Oral Health Foundation, kicked off the proceedings with a warm welcome.
James Cooke, Editor of The Probe, presented the winners with their trophies and certificates before The Ivy’s signature savoury bowls were served.
As the plates were cleared and the dust settled, guests were treated to a performance

from renowned magician and mind reader Neb, who had been circling the room, executing close-up magic to the delight of all. His big performance for the entire room capped of the event by leaving jaws firmly on the ground.
Stay tuned in the coming weeks for details on how to enter the 2025 Dental Awards, and you too could find yourself celebrating next year!
























Dental Awards 2024 Winners
NATIONAL SMILE MONTH
Community Dental Services CIC – Oral Health Improvement Team at Colworth House, Sharnbrook, Bedfordshire1
Best Outreach or Charity Initiative KeepStokeSmiling2
Website and Digital Campaign of the Year
Cheadle Hulme Dental and Cosmetics, Manchester3
Front of House





Trudy Horne, Dorset Dental Clinic, Poole4
Dental Therapist of the Year
Natalie Peary, Smile Together Dental CIC, Bodmin5
Dental Hygienist of the Year
Amanda Harbrow-Harris, Sharrow Dental Group, Chelmsford6
Dental Nurse of the Year
Brittany Pittham, Inspired Dental Care, Exeter7






Practice Manager of the Year
Amanda Reast, The Dental Architect, Leeds8
Dentist of the Year
Rachel Derby, Chapel Dental, Flackwell Heath9
Practice of the Year
Smile Together Dental CIC, Bodmin10
Young Dentist of the Year
Chloe Harrington-Taylor, Hereford Dental Implant Clinic, Hereford
Dental Team of the Year
Glenhaven Dental, Cardiff



The most effective and body-friendly way of healing soft tissue and oral wounds.
















Patient Case Study – Before

Patient presented with Stage 4 Grade B Generalised Periodontitis.
Treatment: RSD Q&Q. blue®m TOOTh protocol










Patient Case Study – After

Recall at 12 months
Case study and photographs courtesy 0f Pat Popat BSc(Hons), PTLLS, RDH, RDT

Learning objectives
• To understand the known risks of hypertension and its range of causes
• To identify ways in which oral health and hypertension are linked at micro and macroscopic levels
• To recognise the opportunities that clinicians have to identify or raise concerns about high blood pressure, and when referrals to general practitioners may be appropriate
GDC Development Outcome: A, C
Stress, poor diets, and a lack of exercise are all reasons that patients lean on as they wave off warnings of high blood pressure. i Around 46% of adults with hypertension may not even be aware that they have the condition. ii It’s the most common risk factor contributing to the global burden of disease. iii
Established links between oral health and hypertension have placed dental professionals in an excellent position to raise awareness and aid patients in taking steps to reduce heightened blood pressure. Clinicians must understand the risks patients face, and the shared risk factors between hypertension and issues such as periodontal disease.
With this knowledge, they may be able to take a more holistic approach to dental and general healthcare.
Establishing ties
Blood pressure is recorded with systolic pressure, the force at which the heart pumps blood around the body, and diastolic pressure, which is the resistance to blood flow in the blood vessels between heartbeats.
High blood pressure is considered a recording of 140/90mmHg if the reading is taken in a clinical environment, or 135/85mmHg if it was read at home. For patients over the age of 80, high blood pressure is considered as 150/90mmHg in a pharmacy, GP surgery, or clinic, or 145/85mmHg at home.i

The need for the differentiation based on the environment is due to white coat hypertension. This is where blood pressure readings are higher in clinics, exceeding the cut-off for a high blood pressure diagnosis, but they are comfortably lower at home.iv This could be caused by stress in a healthcare environment; dental professionals will no doubt be familiar with nerves or dental anxiety from patients, the latter of which affects up to 53% of the UK population.v
High blood pressure has been identified as a major modifiable risk factor for cardiovascular disease,vi strokes, heart
failure, kidney disease and vascular dementia, amongst other conditions.i Clinicians must be able to identify the ways they can help patients lower their blood pressure, which may be possible by making changes to preserve oral hygiene and health.
Periodontal effects
The known links between periodontal diseases and high blood pressure are multifaceted. Adults under the age of 65 with hypertension have been seen to have significantly greater risks of stages III and IV periodontitis compared to those without the condition. vii
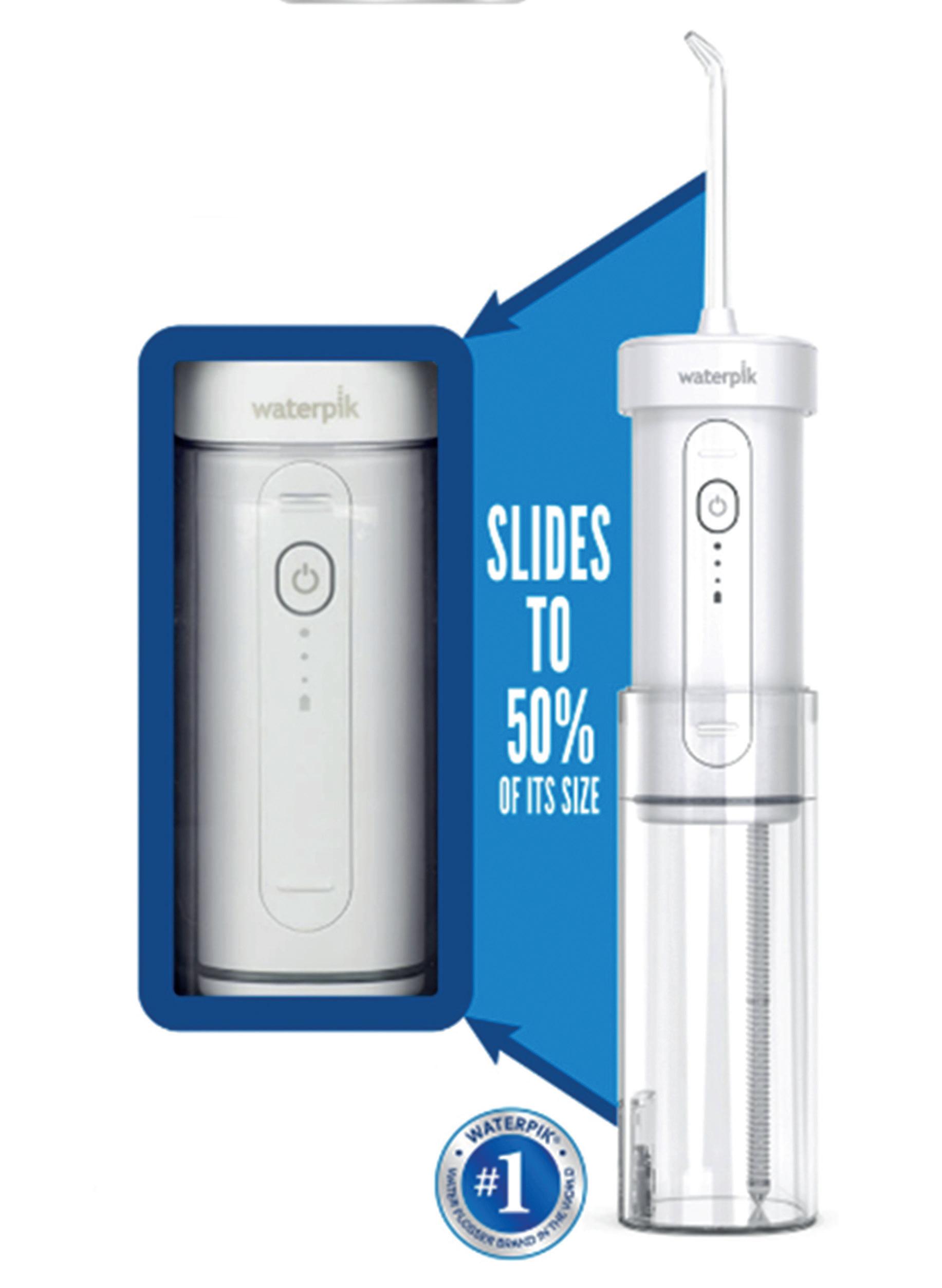
Inversely, patients with increased bacterial load and subgingival plaque have been observed to have greater blood pressure.viii Three pathogens in particular – campylobacter rectus (c. rectus), veillonela parvula (v. parvula), prevotella melaninogenica (p. melaninogenica) – were identified as hypertension-associated oral pathogens (HOP) in a 2019 study,ix setting them apart amongst 21 observed oral microorganisms. Elevated levels of each of these were consistently associated with high/uncontrolled blood pressure, with discrepancies of around +3/2 mmHg, and a 10%-13% greater chance of hypertension. These HOP were associated with a more active instance of periodontal disease, which was measured through bleeding on probing, probing depth and clinical attachment loss. Periodontitis also has well known effects on systemic inflammation, which has been proposed to induce vascular inflammation,
leading to endothelial dysfunction and disrupting the regulation of blood pressure.x Furthermore, periodontitis is associated with excessive reactive oxygen species (ROS) production,xi which is one of the regulators for vascular inflammation and vasoconstriction. The literature states a clear relationship between ROS and the development of hypertension.xii
However, dental professionals can also quickly assess the risk of developing hypertension on a macroscopic level, without having to identify the present strains of pathogens that surround the dentition. Telling signs of poor oral health include partial or complete edentulism; the association between tooth loss and hypertension is seen most in young adults.x
Whilst periodontitis may have a causative relationship with hypertension, clinicians
must also recognise that the two conditions share multiple risk factors. Smoking, nutrition, alcohol abuse, stress and aging have all been linked to increased risks of developing periodontal diseases and high blood pressure.xiii,i
Whilst patients may be warned about the risk of poor oral hygiene outcomes in an everyday check-up, clinicians could use some of this time to bring attention to the shared risks for hypertension.
Clinicians may have the opportunity to check a patient’s blood pressure and make appropriate recommendations when an individual needs to receive sedation for a procedure. It’s important to assess a patient’s blood pressure before administering a sedative. Procedures carried out with local anaesthetic containing epinephrine have been seen to increase systolic blood pressure by 4 mmHg, and procedures without epinephrine have seen blood pressure increases of 11.7/3.3 mmHg. xiv A pre-sedation assessment visit provides an excellent opportunity to screen for hypertension, which may prompt a referral where appropriate.iii
In the case of elective surgery, clinicians that are appropriately trained and confident in their skills may proceed with treatment for patients who record a blood pressure reading of <180/110 mmHg when measured in a clinic. If their blood pressure meets or exceeds 180/110 mmHg, treatment should be postponed, and the patient directed to their GP for primary care assessment and management of their blood pressure.iii The results may be indicative of a condition that they did not know of.
Some clinicians may offer blood pressure testing as a part of their everyday dental care, reinforcing the ability for dental professionals to aid systemic health. Identifying signs of periodontitis or using sedation pre-assessments are therefore not the only chances to make a difference. By taking a holistic approach to dentistry, clinicians are able to identify the risks of high blood pressure in patients, and advise them on steps they can take to manage the disease. This will include effective oral hygiene, which requires optimal solutions. The Waterpik™ Cordless Slide water flosser is one option to consider, and is clinically proven to be up to 50% more effective for improving gum health compared to string floss.xv It can remove up to 99.9% of plaque from treated areas,xvi helping to prevent gingival disease, and the space-saving collapsible design means it can be stored at 50% of its full size; this makes it ideal for travel or smaller storage spaces.
Hypertension is a condition that dental professionals must be aware of, and able to advise their patients on with oral health related observations and solutions. Guiding patients towards effective oral hygiene routines is essential, and may help to reduce the blood pressure of at-risk individuals, improving their general health for the foreseeable future.
For more information on Waterpik™ water flosser products visit www.waterpik. co.uk. Waterpik™ products are available from Amazon, Costco UK, Argos, Boots and Tesco online and in stores across the UK and Ireland.
References
i. NHS, (2023). High blood pressure (hypertension). (Online) Available at: https://www.nhs.uk/conditions/ high-blood-pressure-hypertension/ [Accessed
ii. World Health Organisation, (2023). Hypertension. (Online) Available at: https://www.who.int/news-room/factsheets/detail/hypertension [Accessed June 2024]
iii. Leader, R., Thayer, T., Maher, B., & Bell, C. (2019). Hypertension− an update for the dental (sedation) team. Dental Update, 46(6), 508-513.
iv. Franklin, S. S., Thijs, L., Hansen, T. W., O’brien, E., & Staessen, J. A. (2013). White-coat hypertension: new insights from recent studies. Hypertension, 62(6), 982-987.
v. Anxiety UK, Dental Phobia, (2019). How common Is dental anxiety and
what can you do about It (advertorial blog). Anxiety UK. (Online) Available at: https://www.anxietyuk.org.uk/blog/ how-common-is-dental-anxiety-andwhat-can-you-do-about-it-advertorialblog/ [Accessed July 2024]
vi. Fuchs, F. D., & Whelton, P. K. (2020). High blood pressure and cardiovascular disease. Hypertension, 75(2), 285-292.
vii. Zhan, Y., Jiao, J., Jing, W., Feng, X., Tai, B., Hu, D., ... & Meng, H. (2023). Association between periodontitis and hypertension: cross-sectional survey from the Fourth National Oral Health Survey of China (2015–2016). BMJ open, 13(3), e068724.
viii. Surma, S., Romanczyk, M., Witalinska-Łabuzek, J., Czerniuk, M. R., Łabuzek, K., & Filipiak, K. J. (2021). Periodontitis, blood pressure, and the risk and control of arterial hypertension: epidemiological, clinical, and pathophysiological aspects— review of the literature and clinical trials. Current Hypertension Reports, 23(5), 27.
ix. Pietropaoli, D., Del Pinto, R., Ferri, C., Ortu, E., & Monaco, A. (2019). Definition of hypertension-associated oral pathogens in NHANES. Journal of Periodontology, 90(8), 866-876.
x. Zhan, Y., Jiao, J., Jing, W., Feng, X., Tai, B., Hu, D., ... & Meng, H. (2023). Association between periodontitis and hypertension: cross-sectional survey from the Fourth National Oral Health
To answer the questions below, visit cpd.the-probe.co.uk and register/log in.
Click on ‘Courses’.
Search for the course with the same headline as the corresponding article.
CPD questions – Assessing oral health and hypertension
1. How many adults with hypertension could be entirely unaware?
a) 26%
b) 36%
c) 46%
d) 56%
2. Why does the criteria for high blood pressure change depending on the location it is measured in?
a) White coat hypertension
b) Differences in recording devices
c) The temperature of the environment changes
d) Techniques used to record blood pressure change
3. Hypertension is a modifiable risk factor for which condition?
a) Strokes
b) Kidney disease
c) Vascular dementia
d) All of the above
Survey of China (2015–2016). BMJ open, 13(3), e068724.
xi. Shang, J., Liu, H., Zheng, Y., & Zhang, Z. (2023). Role of oxidative stress in the relationship between periodontitis and systemic diseases. Frontiers in physiology, 14, 1210449.
xii. Loperena, R., & Harrison, D. G. (2017). Oxidative stress and hypertensive diseases. Medical clinics, 101(1), 169-193.
xiii. Darby, I. (2022). Risk factors for periodontitis & peri-implantitis. Periodontology 2000, 90(1), 9-12.
xiv. Bader, J. D., Bonito, A. J., & Shugars, D. A. (2002). Cardiovascular effects of epinephrine in hypertensive dental patients: summary. AHRQ Evidence Report Summaries.
xv. Rosema, N. A., HennequinHoenderdos, N. L., Berchier, C. E., Slot, D. E., Lyle, D. M., & van der Weijden, G. A. (2011). The effect of different interdental cleaning devices on gingival bleeding. J Int Acad Periodontol, 13(1), 2-10.
xvi. Gorur, A., Lyle, D. M., Schaudinn, C., & Costerton, J. W. (2009). Biofilm removal with a dental water jet. Compendium, 30(1), 1. n

4. According to a 2019 study, the presence of c. rectus, v. parvula and p. melaninogenica are associated with how much greater of a risk of developing hypertension?
a) 10%-13%
b) 24%-27%
c) 40%-43%
d) 60%-63%
5. What is a shared risk factor of periodontal disease and high blood pressure?
a) Poor nutrition
b) Smoking
c) Alcohol abuse
d) All of the above
6. In a pre-operative assessment, what result from a blood pressure measurement should prompt treatment to be postponed and a referral to a general practitioner?
a) ≥140/90 mmHg
b) ≥150/90 mmHg
c) ≥170/100 mmHg
d) ≥180/110 mmHg
Learning objectives
• To refresh knowledge on the ways Alzheimer’s disease can affect primary dental care interactions
• To recognise the links between oral health and Alzheimer’s disease established so far, and the implications that current findings have on oral hygiene routines
• To better understand how clinicians can support patients with an Alzheimer’s disease diagnosis
GDC Development Outcome: A, C

With an aging population, the UK has long been facing unique healthcare challenges caused by the increased prevalence of cognitive disorders. Around the world, someone develops dementia every 3 seconds on average, with the total number almost doubling every 20 years – 55 million people were estimated to have the condition in 2020, projected to reach 78 million by 2030, and 139 million in 2050.i Alzheimer’s disease is the most common cause of dementia in the UK, and whilst its aetiologies are not yet fully understood,ii progress is being made in testing, treatment and care. It accounts for 60-80% of dementia cases in total.iii
The condition can have an immense impact on oral health, and may require unique approaches to dental care
that ensure treatments are effective and appropriate. Understanding the condition, current established links to oral health, and how it affects everyday workflows in the practice is essential of all dental professionals.
Potential connections
The connections between oral health and Alzheimer’s are multifaceted. The literature reports extensively on a link between poor oral health and an increased risk or prevalence of dementia or Alzheimer’s disease-like pathologies, and that this is especially prevalent in older adults. iv One study found that, regardless of age and gender, patients with poor oral health demonstrate a 2.363-fold increased risk of developing Alzheimer’s Disease compared to those with standard oral health and hygiene.iv
Patients may carry over 200 bacterial species in their mouth at a given moment, and specific pathogens such as Porphyromonas gingivalis, Treponema denticola and Tannerella forsythia have each been associated with periodontal disease.v P. gingivalis and its virulence factors (lipopolysaccharide or LPS, and gingipains) have also been found in the brain tissue of patients with Alzheimer’s disease, indicating that it can enter this system.vi
In vivo animal studies have proven that P. gingivalis infection may enhance the permeability of the blood-brain barrier, which is the first line of defence for infection in the brain.vi It is a key structural and functional barrier that helps to regulate the movement of ions, molecules and cells between the blood and brain; its precise control allows for proper neuronal
function whilst providing protection from toxins and pathogens.vii Alterations caused by P. gingivalis, brought on by poor oral health, may therefore allow the progression of pathogens into brain tissue, where subsequent neuronal impairment can occur in the long-term.vi
Another key link between periodontitis and Alzheimer’s disease is inflammation. When experiencing oral bacterial infection, for example, in the development of periodontitis, individuals manufacture pro-inflammatory cytokines systemically.viii The presence of activated glial cells (which produce significant levels of these inflammatory cytokines) is a hallmark of Alzheimer’s disease.viii Whilst the body attempts to purge ß-amyloid plaques and tau aggregates –which are linked to cognitive decline – the inflammatory cytokines brought about by the presence of periodontal disease aggravate neurodegeneration.viii
Periodontal disease’s effect on the Alzheimer’s disease is not as well understood as the condition’s relationship with obesity or type 2 diabetes.ix Both potential pathologies still need to be explored further, but the current evidence requires patients to maintain effective oral hygiene as a preventative measure against the beginning or progression of neurological impairment and Alzheimer’s disease.
Memory problems are a commonly shared symptom of Alzheimer’s disease.x This may impair the ability to consistently carry out customary behaviours and daily activities, including oral hygiene routines.
As Alzheimer’s disease progresses, selfcare is compromised to an extreme level, and tooth brushing, flossing and periodic dental visits may not be maintained.xi The responsibility to regulate these may fall to caregivers, if an individual has one. There is a case to be made that, with early intervention, patient and carer education may be effective in preventing the development of oral diseases, even once a patient has received an Alzheimer’s diagnosis. Research into the care of Alzheimer’s patients found that improved oral health was observed after interventions with individuals and their carers.x Studies of professional caregivers in nursing homes have also found that educational interventions improve knowledge of and attitudes towards oral health, as well as the actual oral health of both guardians and their wards.x
Dental professionals must consider that cognitive decline is an unfortunate but unstoppable eventuality in many Alzheimer’s disease cases, and there may come a time where patients (especially those without a

designated caregiver) cannot reliably and regularly keep their oral hygiene routines. Taking action early in the diagnosis is key, and treatment that is long-lasting and improves the oral health quality of life whilst the disease progresses, will be essential in many cases.
Clinicians must understand that following an Alzheimer’s disease diagnosis, oral hygiene routines are at risk of falling by the wayside. With support that can prevent the pathology of the condition, as well as individualised care with a patient and their support circles, clinicians may help patients avoid the development of Alzheimer’s disease, or at the very least slow the progression of the disease as a result of inflammation and infection because of poor oral hygiene.
This requires an effective oral hygiene routine of regular brushing and interdental cleaning. A solution like the Waterpik™ Cordless Advanced water flosser could


be optimal. Proven to be up to 50% more effective than traditional dental floss, and up to 80% more effective than competitors for improving gingival health, the Cordless Advanced can minimise the progression of periodontal disease. Patients can remove up to 99.99% of plaque from treated areas in as little as 3 seconds, and the ergonomic design makes it simple to use every day. Alzheimer’s disease is a growing challenge in modern healthcare, and it has a closely intertwined – yet still to be further explored – relationship with oral health and hygiene. Clinicians must understand how care can be provided to patients in the early stages of the condition to have the greatest effect when it continues to develop.
For more information on Waterpik™ water flosser products visit www. waterpik.co.uk. Waterpik™ products are available from Amazon, Costco UK, Argos, Boots and Tesco online and in stores across the UK and Ireland.
References
i. Alzheimer’s Disease International, (N.D.). Dementia statistics. (Online) Available at: https://www.alzint. org/about/dementia-facts-figures/ dementia-statistics/ [Accessed June 2024]
ii. NHS, (2021). Alzheimer’s disease. (Online) Available at: https://www.nhs. uk/conditions/alzheimers-disease/ [Accessed June 2024]
iii. Alzheimers Association, (N.D.). What is Alzheimer’s Disease? (Online) Available at: https://www.alz.org/alzheimersdementia/what-is-alzheimers [Accessed June 2024]
iv. Kulkarni, M. S., Miller, B. C., Mahani, M., Mhaskar, R., Tsalatsanis, A., Jain, S., & Yadav, H. (2023). Poor Oral Health Linked with Higher Risk of Alzheimer’s Disease. Brain Sciences, 13(11), 1555.
v. López-Martínez, J., Chueca, N., PadialMolina, M., Fernandez-Caballero, J. A., García, F., O’Valle, F., & Galindo-Moreno, P. (2020). Bacteria associated with periodontal disease are also increased in health. Medicina oral, patologia oral y cirugia bucal, 25(6), e745.
To answer the questions below, visit cpd.the-probe.co.uk and register/log in. Click on ‘Courses’.
Search for the course with the same headline as the corresponding article.
CPD questions – Understanding the connections between Alzheimer’s disease and oral health
1. How many people worldwide are expected to develop Alzheimer’s disease by 2030?
a) 55 million
b) 66 million
c) 78 million
d) 99 million
2. According to the article, how much greater is the risk of developing Alzheimer’s disease for a patient with poor oral health, regardless of age and gender, compared to a healthy individual?
a) 1.636-fold
b) 2.363-fold
c) 4.939-fold
d) They are at an identical level of risk
3. What does the blood-brain barrier do?
a) Regulates the movements of ions between blood and the brain
b) Regulates the movements of molecules and cells between blood and the brain
c) Protects the brain from toxins and pathogens
d) All of the above
vi. Lei, S., Li, J., Yu, J., Li, F., Pan, Y., Chen, X., ... & Tang, X. (2023). Porphyromonas gingivalis bacteremia increases the permeability of the blood-brain barrier via the Mfsd2a/ Caveolin-1 mediated transcytosis pathway. International journal of oral science, 15(1), 3.
vii. Daneman, R., & Prat, A. (2015). The blood–brain barrier. Cold Spring Harbor perspectives in biology, 7(1), a020412.
viii. Bui, F. Q., Almeida-da-Silva, C. L. C., Huynh, B., Trinh, A., Liu, J., Woodward, J., ... & Ojcius, D. M. (2019). Association between periodontal pathogens and systemic disease. Biomedical journal, 42(1), 27-35.
ix. Hashioka, S., Wu, Z., & Klegeris, A. (2021). Glia-driven neuroinflammation and systemic inflammation in Alzheimer’s disease. Current Neuropharmacology, 19(7), 908-924.
x. Alzheimer’s Society, (2023). Alzheimer’s disease. (Online) Available at: https:// www.alzheimers.org.uk/aboutdementia/types-dementia/alzheimersdisease [Accessed June 2024]
xi. Hernández-Vásquez, A., BarrenecheaPulache, A., Aguirre-Ipenza, R., Comandé, D., & Azañedo, D. (2022). Interventions to improve the oral hygiene of individuals with Alzheimer’s disease: a systematic review. Dentistry Journal, 10(5), 92. n
4. What type of cells produce inflammatory cytokines and are considered a hallmark of Alzheimer’s disease?
a) Activated glial cells
b) White blood cells
c) Neurons
d) Paneth cells
5. Which lifestyle-related conditions have a better understood relationship with Alzheimer’s disease, according to the article?
a) Obesity and type 2 diabetes
b) Heart disease and type 2 diabetes
c) Only obesity
d) Chronic obstructive pulmonary disease and metabolic syndrome
6. What can early interventions with patients with Alzheimer’s disease and their caregivers improve?
a) Attitudes towards dentists and dental anxiety
b) The knowledge of and attitudes towards oral hygiene, and physical oral health levels
c) The understanding of the benefits of orthodontic treatment
d) Nothing
Preventive care is key for promoting long-term oral health. Interdental cleaning and using products which contain key ingredients such as fluoride and chlorhexidine are essential here, enabling patients to reduce levels of plaque and prevent future oral health issues. As such, it’s important to recommend products which boost oral hygiene, and are easy to use, like FLEXI interdental brushes and PREVENT GEL from TANDEX. When using both of these together, patients are able to remove plaque from in between the teeth with ease, whilst also applying 0.12% chlorhexidine for an antibacterial effect, and 900ppm fluoride to help strengthen enamel.
For the smooth running of your practice it is vital that you have sufficient staffing. From illness to holiday, quickly finding locum cover for absent staff keeps the workflow efficient.
Dental Elite can be your greatest asset for getting cover sorted, removing the stress and worry from your job.
On working with one of the Dental Elite team, Chalet Hill says “I can’t say enough good things about Luke [Arnold, Locum Controller]. He has been absolutely amazing in finding locum cover for multiple sites. His response is incredibly quick, and we never have any issues or worries.
“Every time we need a locum, he manages to provide us one within a week of asking. His

FLEXI interdental brushes have a flexible handle, making them easy to use, and are available in 11 different sizes, ensuring the perfect fit for each interdental space.
Contact the team at TANDEX for more information.
For more information on Tandex’s range of products, visit https://tandex.dk/ Our products are also available from DHB Oral Healthcare https://dhb.co.uk/
tandex.dk

BDIA Dental Showcase provides an exclusive opportunity to engage with leading dental manufacturers and suppliers, with several organisations making this the only UK exhibition they attend all year.
NSK (Official Handpiece Partner 2024) returned to BDIA Dental Showcase after seven years away from all major events. Alexander Breitenbach, UK Managing Director at NSK, shared why they chose to attend this exhibition above all others:
Leader in decontamination, Eschmann, offers comprehensive service and support for all its customers. It is one of the only providers in the market to deliver Enhanced CPD training with new equipment as it is installed, and annually thereafter if you are one of their Care & Cover contract customers.
ECPD training ensures that all appropriate members of the dental team know how to confidently use and maintain your infection control equipment. This includes efficient daily operation, as well as knowing how to perform the necessary daily, weekly and monthly testing required for compliance with regulations and optimised product life.
All training is provided by expertly qualified
Ortho-restorative care in a nutshell
The Align, Bleach and Bond course from the IAS Academy is the perfect base for clinicians to introduce clear aligner orthodontics and orthorestorative care into their everyday dentistry. Spanning over two days, delegates will first understand the workings of Inman and clear aligners, looking at appropriate case assessments and selection. Under the guidance of leading clinicians and dental educators, delegates will also explore occlusal planning and retention, before having a hands-on experience with Inman/clear aligner attachment placement.
Ortho-restorative workflows are covered comprehensively on day two, as dental professionals are presented with guidance on simple edge bonding and polishing, aesthetic tooth shaping, guidance on treatment techniques such as the
efficiency and dedication make our working lives so much easier. Highly recommend!”
For a consistent workflow and reliable locum cover, try Dental Elite.

For more information contact the Dental Elite team on 01788 545900 https://dentalelite.co.uk/
dentalelite.co.uk

Eschmann engineers, who have extensive experience with Eschmann equipment and with dental regulations. They are also available after the training should your team have any questions.
In addition, there is a technical helpline for any enquiries regarding the equipment.
To find out more, contact Eschmann today.
For more information on the highly effective and affordable range of infection control products from Eschmann, please visit the website or call: 01903 753322.
eschmann.co.uk
Dahl Principle, and so much more.

The course is expertly led by well-regarded IAS Academy tutors such as Tif Qureshi, Geoff Stone, Seb Wilkins and Guy Wells. Delegates can approach tutors with any and all questions about orthodontic and ortho-restorative care, and can receive clinical support long after the conclusion of the course.
To learn more about exceptional courses with the IAS Academy, contact the team today. For more information on upcoming IAS Academy training courses, please visit www.iasortho.com or call 01932 336470 (Press 1).
iasortho.com
“This event is all about BDIA member companies presenting their wares to the profession. There has been a really positive vibe from the audience and exhibitors. It’s great to come together as industry and profession to showcase what we have to offer and to promote clinical excellence. The benefits of attending for dental professionals are, without any doubt, the fact that everyone is here, so you can make informed decisions when looking to buy and invest.”
To make sure you have access to the greatest number of relevant dental organisations and industry experts in 2025, don’t miss BDIA Dental Showcase!
BDIA Dental Showcase 2025, 14th-15th March, ExCeL London dentalshowcase.com dentalshowcase.com
“I highly recommend Kiroku to anybody – sign up!”
Dr Thomas Munro shares his experience of using Kiroku, the digital note taking platform.
“I have been using Kiroku for over a year and a half, and the part I love the most about it is the fact that it’s always consistent.
The treatment notes are always uniform, and the questions we’re answering for our diagnostics are always the same. This means that, no matter who’s taking the notes, or who is performing the exam, key pieces of information are being recorded for all of our patients. This is particularly useful for larger orthodontic or implant cases. I really value this.
“The program itself is really intuitive, it always makes recommendations based on things that we are changing or adding on a constant basis – it recommends adding information in automatically so that it is just a single touch button in order to make changes.
“I highly recommend Kiroku to anybody. If you value consistency along with saving time and making your team’s life easier in that note taking process – sign up!”
To find out more about Kiroku, or to start your free trial, please visit trykiroku.com.
trykiroku.com

upheaval of a patient complaint could happen to anyone. Our dentolegal experts will help get things back to normal.


