








At Provide Digital we don’t just build digital tools – we design smart, cost effective solutions in close collaboration with healthcare services.
As part of Provide Community, an employee owned Community Interest Company, we specialise in healthcare digital transformation, with proven platforms improving everything from referral management to feedback and compliance. All of our flag ship products were developed to provide solutions to challenges our own services and frontline teams were facing, ensuring they meet actual needs and deliver measurable impact.

Real-time feedback collection Simplifies Autism and ADHD referrals
Confidential access to free sexual health resources for young people
safer patient referrals

P R E V E N T V I O L E N C E
R E L I A B L E
E A S Y T O U S E
E F F I C I E N T
S T A F F A L A R M
S Y S T E M S
V i s i t P i n p o i n t , t h e U K & I r e l a n d ' s
l e a d i n g p r o v i d e r o f s t a f f s a f e t y s y s t e m s
t o h i g h - r i s k w o r k p l a c e s .
T O W A R D S T A F F P I N P O I N T . L T D . U K


















The prime minister has launched the longawaited 10-Year Health Plan.
Under the new plans, millions of patients will be treated closer to home under new teams of health professionals. A Neighbourhood Health Service will see teams set up in local communities across the country, in a bid to improve access to the NHS.
As part of the Government’s aim to shift care out of hospitals and into communities, the teams will free up hospitals from ‘perpetual firefighting’.
The neighbourhood health centres will provide easier, more convenient access to a full range of healthcare services on people’s doorsteps, preventing them from travelling to hospitals.
The neighbourhood teams will include nurses, doctors, social care workers, pharmacists, health visitors, palliative care staff, and paramedics. Community health workers and volunteers will also play a role. The teams will be encouraged to trial innovative schemes like community outreach door-to-door.
Prime Minister Keir Starmer said: “The NHS should be there for everyone, whenever they need it.
“But we inherited a health system in crisis, addicted to a sticking plaster approach, and unable to face up to the challenges we face now, let alone in the future.
“That ends now. Because it’s reform or die. Our 10 Year Health Plan will fundamentally rewire and future-proof our NHS so that it puts care on people’s doorsteps, harnesses game-changing tech and prevents illness in the first place...


The government has announced that new innovation squads will be rolled out to boost public services.
The squads will back community ideas and work with the frontline as part of a £100 million ‘Test, Learn and Grow’ reform programme to deliver the Plan for Change.
The teams will be deployed from central government and will work alongside local government and service users to tackle the biggest challenges affecting local communities.
This includes establishing neighbourhood health services as well as increasing the uptake of Best Start Family Hubs to support parents and young children, better supporting children with special needs, getting more people into work, rolling out breakfast clubs, and tackling violence against women and girls.
The squads will work with tech experts and will be empowered to try new things and be creative.
The approach has already seen success in trials across the country. In Sheffield, innovation squads tested new ways to get more families through the door of local family hubs, resulting in many more local families using the hubs and in Liverpool, they worked with the council to build an innovative data-led platform to manage temporary accommodation.
Cabinet Office Minister, Georgia Gould said: “For too long residents and frontline workers have had to navigate fragmented and underfunded public services, people feeling like they have to arm up to battle to get the support they need...
PSE Lighting deliver smart lighting control systems that cut energy costs, simplify maintenance, and improve comfort across your healthcare estate.
With proven results – like the Oak Cancer Centre – we combine in-house expertise with smooth project delivery and long-term value. Talk to us about improving performance, compliance, and sustainability in your next build or upgrade.







The Government has launched a new Life Sciences Sector Plan to grow the economy and
As part of the Industrial Strategy, the new plan sets out a ten-year mission to harness British science and innovation to deliver long-term economic growth and a stronger, prevention-
The life sciences sector is already worth around £100 billion to the UK economy and
The plan is built around three core pillars: enabling world-class R&D; making the UK an outstanding place to start, scale and invest; and driving health innovation and NHS reform.
supported over the lifetime of the Spending Review by government funding of over £2 billion, as well as funding from UKRI and NIHR.
The plan includes six actions to kickstart change. The first is unlocking NHS data to find new cures, with up to £600 million of investment to build the world’s most advanced
There is a commitment to speed up clinical trials, cutting red tape so patients can join trials
Up to £520 million will be available to invest in life sciences manufacturing projects, to create jobs and make more treatments and medical
Support for MHRA will be boosted with extra investment to make regulation safer and faster. There will be support for doctors to use new technology, and a new NHS passport to roll out
SCAN THE QR CODE AND SEE HOW MUCH YOU CAN SAVE



The Medicines and Healthcare products Regulatory Agency (MHRA) has published a Statement of Policy Intent, which sets out initial thinking on a new Early Access service to help patients benefit sooner from innovative medical devices that address unmet clinical needs.
The Early Access service will provide timelimited, conditional access to promising technologies ahead of full regulatory approval, where there is clear clinical need and supporting evidence of benefit for patients.
The scheme is designed to support innovators, including small and medium-sized enterprises, and aims to help bring safe and effective medical devices to patients more quickly.
The focus will initially be on innovative diagnostic devices, particularly those supporting the NHS’s most urgent needs.
The Early Access service will use learnings from the Unmet Clinical Need Authorisation (UCNA) tool piloted in the Innovative Devices Access Pathway (IDAP), and be shaped by stakeholder engagement with key sector representatives.


The Cyber Assessment Framework (CAF), provided by the National Cyber Security Centre (NCSC), has been updated in response to growing threats.
The tool helps organisations improve their cyber security and resilience, so they can protect critical services from cyber threats.
The CAF is mainly designed for CNI organisations operating essential services in areas including energy, healthcare, transport, digital infrastructure and government sectors, helping them to meet legal and regulatory requirements such as the NIS Regulations. It provides a comprehensive framework for assessing how well an organisation is meeting expected security and resilience outcomes, identified as appropriate in relation to a particular level of threat.
The last version was published in April 2024 and its adoption has continued to spread. It’s now used by nearly all UK cyber regulators and GovAssure, the cyber security assurance scheme for assessing the UK’s critical national infrastructure (CNI).
Meanwhile, the cyber threat to the UK’s CNI has continued to increase.
The CAF has been updated to ensure it remains relevant and ensure that organisations’ defences are up to date.
Version 4.0 introduces four major changes including a new section on building a deeper understanding of attacker methods and motivations to inform better cyber risk decisions and a new section on ensuring software used in essential services is developed and maintained securely...






The government has announced a £63 million investment package for the UK’s electric infrastructure, which will provide £8 million to electrify NHS vehicles.
£8 million will go towards NHS England to power the electrification of ambulances and medical fleets across over 200 NHS sites, saving money and making a big step towards net zero. This comes alongside 1,2000 new charging sockets to support this electric expansion.
There will also be a £25 million scheme for local authorities to expand access to cheaperat-home charging and the government has committed to modernising EV signs on major roads, to increase accessibility.
The government is also launching a major new grant scheme to help businesses install charging points at depots nationwide, supporting the nation’s heavy goods vehicles, vans and coach drivers in the transition to zero emissions.
NHS chief sustainability officer Chris Gormley said: “The NHS has already implemented hundreds of projects that reduce emissions and drive significant cost savings, all while improving patient care.
“This new £8 million investment, across 62 NHS Trusts and around 224 sites, supports the renewed commitment in the government’s 10 Year Health Plan to deliver a more sustainable NHS while also helping hospitals to save millions on fuel and maintenance costs and reducing air pollution. These savings can be reinvested directly into frontline care, ensuring the NHS continues to deliver for our patients and communities.”...

First phase of 10 Year Plan underway: READ MORE
New NHS Wales chief executive announced: READ MORE
Extra funding for appointments in Scotland: READ MORE
NHS launches review to tackle LGBT+ health inequalities: READ MORE
Regulators set out plans to deliver medicines faster: READ MORE
Charities to help people with long-term conditions: READ MORE
In October, 2,000 more GPs were hired, which has led to millions more GP appointments for patients. Seeing as the average GP is responsible for 2,300 patients, the new tranche could deliver over four million additional appointments each year.
With this, new data from the Office for National Statistics (ONS) shows that the number of patients who found it difficult to contact their practice has fallen from 18.7 per cent in July/ August 2024 to 10.6 per cent in May/June this year. This shows that the ‘8am scramble’ is improving.
Additionally. 96.3 per cent of patients who tried to contact their practice in the past four weeks were successfully, and those who had a poor experience of their GP practice fell from 15 to 10.9 per cent in the same period.
In May 2025, 12,000 more GP appointments were carried out every working day compared to May 2024.
Health and social care secretary Wes Streeting said: “We said we’d deliver 1,000 more GPs this year — and we’ve busted that target, bringing 2,000 more GPs on board. With proper investment and reform we are turning the tide on our NHS, and patients are beginning to feel the benefit.
“We still have a long road ahead, and this government is determined to keep our foot on the gas...

Compliance and regulatory standards must be met to keep buildings safe and operational Risks, quality and compliance must be managed and maintained within healthcare. Whether you are a hospital, a doctor’s surgery, or a dental practice, fmfirst® can support:
Asset management
Cleanliness audits
Document management
Efficacy audits
Incident reporting
Risk assessments
Task management - Helpdesk

Having a trusted cleaning audit system is imperative for any healthcare organisation to help manage its cleaning compliance requirements

When launched, the National Standards of Healthcare Cleanliness 2021 emphasised the importance of digital systems to evidence organisations were meeting the compliance requirements. This led to an expansion of software options in the market, and even to this day, it can be confusing as to which system would suit your organisation best.
Choosing the right system is not just about demonstrating that compliance standards are met. Essentially, most systems function the same, but what often gets overlooked is the ease of use. A systems interface can look like the bee’s knees, but when using the system day to day, it can feel quite clunky and much more complicated than it needs to be. We live in a world of technology, but there is nothing to say a system can’t be clear, simple, and easy to use, while still
What does fmfirst® Cleaning offer
fmfirst® Cleaning is Asckey’s auditing application designed to simplify and support the undertaking, reviewing, and reporting of the cleaning audit process. Its functionality can speed up the auditing process, increase productivity, reduce overall costs, and meet relevant compliance requirements, including the updated National Standards of Healthcare Cleanliness 2025.
fmfirst® Cleaning has been purposefully built to have minimum click-through options and be an easy-to-use application. Its design automates report emails on the completion of audits and includes any corrective actions that are required. This method of providing instant fault reporting and the option for rectifying allows users to act immediately. This allows for time and resources to be proportionately allocated.
“It is an exceptionally user-friendly and intuitive tool that has significantly contributed to the enhancement of service delivery. Additionally, it features an excellent reporting system and offers substantial flexibility at the user level.” Serco NNUH.
Asckey has a unique and personal understanding of the cleaning standards, which fmfirst® Cleaning was designed to support. As a member of the Association of Healthcare Cleaning Professionals, they continue to be part of the conversation around the development of these standards. Their fmfirst® Cleaning is already used by NHS Trusts across the UK but can be used in any health and social care setting. M
Asckey is also accredited with ISO 9001, ISO 27001, ISO 14001, and Cyber Essentials Plus, and is a member of SFG20’s Digital Partner Programme, meaning quality, data security, and sustainability are woven into their processes to provide clients with the best possible solution and support.
To discover more about fmfirst® Cleaning
and Asckey, visit www.asckey.com








Since its launch in 2017, the ABHI US Accelerator has become the flagship international growth programme for UK HealthTech innovators

Designed to help UK companies navigate the complexities of the US healthcare system, the initiative has supported over 100 businesses with their export strategies – facilitating commercial success, clinical partnerships, and increasingly, reciprocal investment back into the UK. At a time when global collaboration in healthcare is more vital than ever, the programme is also delivering benefits much closer to home, particularly for the NHS.
Delivered by the Association of British HealthTech Industries (ABHI), the US Accelerator helps UK companies establish and grow in the world’s largest health market. Participants receive year-long support, including tailored
advice, mentoring from in-market experts, and introductions to decision-makers across hospitals, investors, and supply chain partners.
A key part of the programme is the series of trade missions to leading health ecosystems across the US. These visits – now taking in States such as New Jersey, Pennsylvania, Florida, Texas, California, Tennessee and more – enable participants to meet with potential customers and collaborators face-to-face, often resulting in new commercial partnerships and clinical studies.
The value of this real-world engagement cannot be overstated. In a highly competitive market like the US, having a structured route to trusted networks is transformative. Over the past seven years, the programme has E


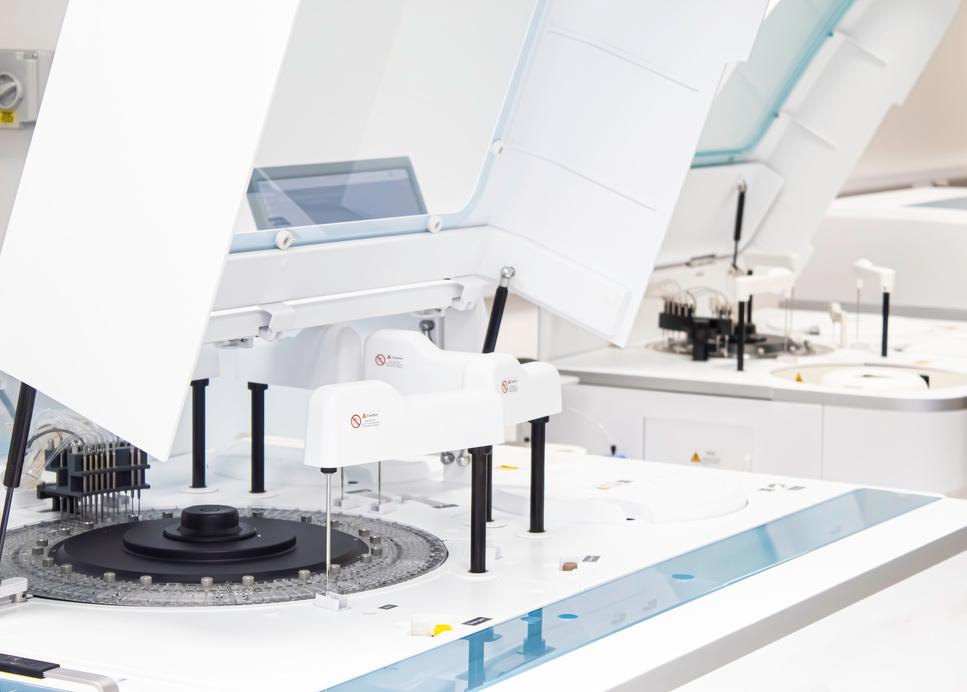
Fortress Diagnostics celebrates 25 years of innovation in medical diagnostics, launching Fortress Clinical to expand its impact.
Fortress Diagnotics now operates in over 100 countries, delivering cutting-edge diagnostic solutions





The new venture integrates advanced technology and precision medicine to transform patient care globally
fortressdiagnostics.com
fortressclinical.com








Mobile Healthcare Solutions is a leading provider of surgical and diagnostic medical systems and instrumentation for hire.
With the financial backing of our parent company GAP Hire Solutions, it affords us the ability to source from best-in-class suppliers, medical systems for hire. Whether you’re maintaining or expanding services or having to cover maintenance downtime, we’re here to support your clinical needs. Please contact Mobile Healthcare Solutions to see how we can assist you with your medical equipment and instrumentation hire requirements:






F helped secure multiple distribution deals, pilots, and even permanent US operations for UK HealthTech businesses. For companies navigating reimbursement pathways or navigating complex state-level procurement processes, these partnerships often prove crucial to success.
While the programme’s primary focus is international expansion, the benefits for the NHS are also clear. Several participating companies have been able to refine their technologies with US clinical partners and bring those improvements back to the UK. Others have secured investment and market insights that have helped them scale domestically, offering improved tools and services to NHS institutions.
Crucially, many of the technologies within the Accelerator address challenges shared by both US and UK health systems – like early diagnosis, surgical efficiency, digital transformation, and remote care. By gaining traction abroad, these solutions gain the credibility and capital needed to expand at home.
One example is the increasing number of UK companies that have entered strategic E

Many of the technologies within the Accelerator address challenges shared by both US and UK health systems


F partnerships with US hospital systems to undertake clinical trials, generating real-world evidence that has supported NHS adoption. In doing so, these businesses bring home not just commercial success, but new capabilities and data that can support value-based procurement and more personalised care for NHS patients.
investment and international collaboration
Beyond exports, the ABHI US Accelerator has also stimulated inward investment into the UK.
A growing number of US-based health systems and investors are now looking to the UK as a hub for innovation and partnership, and in 2024, the programme helped host the Governor of New Jersey in London, where high-level meetings took place with healthcare leaders and HealthTech entrepreneurs.
Such partnerships not only drive innovation, but also contribute to the UK economy, create jobs, and enhance the global visibility of British healthcare expertise.
“The ABHI US Accelerator has always been about more than just export – it is about
building meaningful partnerships that deliver real benefits on both sides of the Atlantic,” says Paul Benton, managing director, International at ABHI. “We are proud to be helping UK companies succeed in the US, but just as importantly, we are seeing how these connections are enhancing innovation and care back in the NHS.”
The US and UK face many similar health challenges, from managing chronic conditions to deploying digital technologies at scale. The Accelerator provides a platform for shared learning, where NHS clinicians and executives can see how US providers are implementing HealthTech solutions, and vice versa.
For example, NHS partners involved in past missions have observed best practice in areas such as integrated care, virtual wards, and AI deployment in diagnostics – insights which have informed their own local innovations. Similarly, US providers benefit from the UK’s strengths in population health management and its robust clinical research infrastructure.

In turn, UK companies in the programme frequently leverage their NHS credentials to build credibility overseas, and the ability to demonstrate efficacy and value within the NHS environment is a powerful tool for companies when entering new markets.
Looking ahead, the ABHI US Accelerator is aligning more closely with the UK’s broader industrial strategy, supporting government priorities around economic growth, exports, and inward investment. It also reflects the ambitions set out in the Life Sciences Vision, particularly in fostering adoption and scaling of innovation.
In 2025, the programme will continue to expand, offering tailored support. And through ABHI’s network of in-market experts and hospital partners, companies will gain bespoke insights into local reimbursement, procurement, and clinical integration.
The NHS, as a key stakeholder in the health innovation ecosystem, stands to benefit directly from this pipeline of globally-validated
technologies and partnerships. In many cases, the lessons and relationships gained via the US Accelerator feed directly back into UK-based care improvements, workforce support, and health system efficiencies.
At its core, the ABHI US Accelerator is a powerful example of how trade and health innovation can go hand-in-hand. By helping UK companies succeed abroad, we are also strengthening the foundations for innovation at home – bringing back investment, insight, and new tools to support patients and healthcare professionals across the NHS.
As global health systems grapple with rising demand and constrained resources, it is partnerships, between countries, sectors, and companies, that will define the next era of care. Programmes like the ABHI US Accelerator are enabling the UK to lead that charge, with HealthTech at its heart. M




Staff are feeling the pressure at the moment, and keeping track of how they are feeling is important for any organisation. Whether a comprehensive long survey, or a short pulse survey, being able to implement one can be a time-consuming activity in and of itself

Survey Solutions aims to help clients through the process, making it as smooth and painless as possible to design the questionnaire, get the survey out to participants, and them makes sure that there are solid actionable insights identified in the results. These allow organisations to focus attention on the areas which will make a difference to staff.
Organisations who demonstrate their commitment to listening, attract and retain the best staff, are more likely to achieve goals and deliver better services.
At Survey Solutions, our clients come in all shapes and sizes, public sector, not-for-profit and commercial businesses, and we can compare survey results to help show what ‘good’ looks like, and where improvements can be achieved.
Office based staff and ‘deskless’ workers such as drivers, staff who work outside, and building maintenance are all encouraged to participate with a range of approaches available to ensure they have access to the survey and can give their views.
So many issues are challenging the working environment—the constant need to ensure limited budgets are spent well, changing in working practices such as introducing AI tools, or managing hybrid/remote working, and the needs of organisation to change and adapt— often causing uncertainty and stress for staff. Expectations of employers is also shifting with those who have joined the workforce having different views on working life.
Exploring perception on topics such as wellbeing, bullying and harassment, leadership and management, communications, reward and benefits is a means for employers to keep on top of key issues and take actions quickly to avoid small concerns becoming major issues.
The team at Survey Solutions are expert researchers and can provide advice to clients with examples of how other clients have responded to feedback, or how to design surveys to investigate specific challenges.
We work closely with clients to ensure they get the most value from the survey results, and are available for any follow up needed for a year after the survey closes.
If you’d like to find out more, feel free to get in touch with us! M
Colin Wheeler Managing Director, Survey Solutions

Simon Taylor, director of estates policy, strategy & capital projects at NHS Property Services, introduces the NHS Estate Optimisation Guide
The Government’s new ten-year health plan has refocussed the healthcare debate onto prevention and delivery of services in the neighbourhood. The NHS will be focussed on delivering more preventative services, including around 300 neighbourhood hubs – 40 to 50 within the lifetime of this Parliament.
To rapidly progress the objectives in the tenyear health plan, the existing NHS estate must work more efficiently and provide more without fundamental change. Empty and underutilised spaces will need to be transformed to support additional capacity, cutting-edge diagnostics, and health services in communities to prevent ill health.
Property is often one of an organisation’s biggest expenses: the NHS has more than 10,000 buildings covering 25 million square metres. The need to improve ICBs’ and Trusts’ ability to manage their existing estate is the very reason we have created this NHS Estate Optimisation Guide
NHS Property Services (NHSPS) owns about 10 per cent of the NHS estate, we also advise how buildings can be used more efficiently and deliver better value for money whilst maintaining patient care at a high level. We have the property, people, and professional expertise to support the delivery of the ten-year health plan’s neighbourhood hubs as well as the experience to maximise value for money by repurposing the existing estate.
Our long-term goal is to establish more efficient, more collaborative, and sustainable ways of working so that estate leaders can get more out of the space they have and better manage their costs.
Many assume that NHS spaces are fully used but our own recent research has revealed they are often only 40 per cent utilised or less. NHS England chair, Dr Penny Dash, recently commented on how much the NHS wastes money and that empty buildings are one major cause of this waste. She argued that it is
management and process systems that hinders good utilisation.
There are many reasons for space not being used effectively, estate leaders have told us they have low (32 per cent) or medium (55 per cent) understanding of how the space across their estate is being used.
And 41 per cent of estate leaders have told us they do not have the budget to look at vacant space and its use, while more than a half (55 per cent) said they do not have the ‘in-house capacity to manage change to spaces and deliver’ to optimise the space they have.
However, there are solutions and the best start to making better use of space is developing a detailed understanding of buildings and spaces, overlaying the estate strategy, and reviewing occupancy and utilisation on a regular basis.
One valuable tool NHSPS has created is NHS Open Space, first launched in 2016. Over half of NHS leaders surveyed stated they lacked the right data to make informed decisions, and a third said they lack the expertise to make the right changes to their estate.
Open Space is a digital platform which provides the NHS with booking and analytical tools as well as expert support and guidance to healthcare specialists so they can efficiently use their existing rooms and oversee who they are being used by. NHS organisations can then better manage the space they have in their buildings and make use of and better analyse underutilised space.
One case study is Greater Manchester Mental Health NHS Foundation Trust (GMMH). They successfully used NHS Open Space and drove 21 per cent cost efficiency through increased space utilisation and 32 per cent cost savings. Previously, the Trust had been reliant on a manual room booking process which meant spaces were not being booked efficiently. For example, clinical spaces were being booked for full-day sessions, even when only an hour was needed.
A further case study at Belmont Health Centre shows how important managing space is. Three GP practices and a community services provider needed more space for their 20,000 (and growing) patients. NHSPS held the headlease, which had 30 per cent vacant space at a cost of £110,000 per year to North West London ICB. We helped the ICB unlock £1.6m of capital to reconfigure and refurbish the building, increasing consulting room capacity,
Open Space is a digital platform which provides the NHS with booking and analytical tools
providing a new reception and colleague facilities, and improving accessibility. Now there is no vacant space, overall costs for the NHS have been saved, and more patients can be seen.
To gather the data needed to assess how space is being used, relatively affordable digital equipment can be used such as desk sensors to monitor desk occupancy, area sensors to monitor occupancy of a space and movement sensors which detect occupancy based on motion, these are infrared or ultrasonic based.
We have been using ongoing monitoring since 2019, collecting, and analysing room motion sensor data. The dashboards we use track property and financial data on a room which increases the use of the space. This space optimisation has unlocked £38.5million for the NHS since it was first launched.
In conclusion, the NHS needs to be ready to adapt and fully utilise the core, long-term estate to deliver the new ten-year plan’s goals, provide first-class patient care, and provide better value for money.
This NHS Estate Optimisation Guide provides a simple framework to help advise on what to look out for. We can help estate leaders better understand the value of monitoring space and how by doing so they can unlock greater value from their existing spaces. M

Take control of your workspaces, and discover hidden efficiencies.











































































Whether you’re booking consulting rooms, offices, desks or even parking spaces, Clearooms offers complete control of your setting – all within one easy-to-use system.


























Quick set-up and easy onboarding including floorplan support and creation
Supports SSO and integrates with Google and Outlook, as well as leading security systems
Detailed utilisation & contact trace reports to gain insight as to how your spaces are used
Great value pricing, based on the number of desks & rooms, not the number of users






UK-based and developed with responsive support
It has never been more crucial for NHS trusts to maximise space potential as more employees work flexibly or from home
In today’s healthcare landscape, NHS trusts are under mounting pressure to use space more efficiently while accommodating the realities of flexible and hybrid working. From busy outpatient departments to behind-the-scenes administrative teams, staff across the NHS need reliable access to rooms and desks that support safe, efficient, and collaborative working. Clearooms desk and room booking software is a powerful, cost-effective solution designed to meet these challenges.
Whether enabling hot-desking for clinical teams, managing shared administrative offices, or allocating space for multidisciplinary collaboration, the system replaces outdated manual processes with a seamless, intuitive experience.
Clearooms integrates effortlessly into existing IT systems, thanks to its single sign-on (SSO) capabilities, making onboarding as simple as it can be. This ensures easy, secure access for all staff, with minimal training required. From a single department to an entire trust with multiple sites, Clearooms can scale to support estates of any size, adapting to fluctuating demands, promoting agile space management. Better yet, pricing is based on the number of desks and rooms–not users–making it a cost-efficient solution for NHS environments with large and varied staff groups.
Clearooms is backed by a dedicated UK-based support team with extensive experience in the public sector, including healthcare. From floorplan creation to custom set-up and responsive ongoing support, the implementation
process is smooth and tailored to your needs. This ensures the system is quickly adopted with minimal disruption to current operations.
As a provider featured on the government procurement portal, Clearooms is already a trusted solution for many public sector bodies, bringing a deep understanding of the access, and resource-sharing needs that mirror many of the challenges faced by Health Care settings.
With detailed analytics and reporting, Clearooms provides facilities teams with real-time insights into room and desk usage. This supports more accurate space planning, identifies underutilised areas, and helps reduce waste, contributing to both operational efficiency and NHS sustainability targets. Our specialised trace reports can also help in mitigating the spread of infection across your settings, as can scheduled cleaning and ‘block out times’, ensuring spaces are safe to use.
For NHS trusts managing complex schedules, multiple departments, and diverse teams, Clearooms delivers a proven, secure, and scalable solution. It helps staff stay focused on what matters most–delivering outstanding patient care in well-managed, productive environments.
To book a demo and see how Clearooms can help improve efficiencies right across your organisation, please visit www.clearooms.com/ health. M

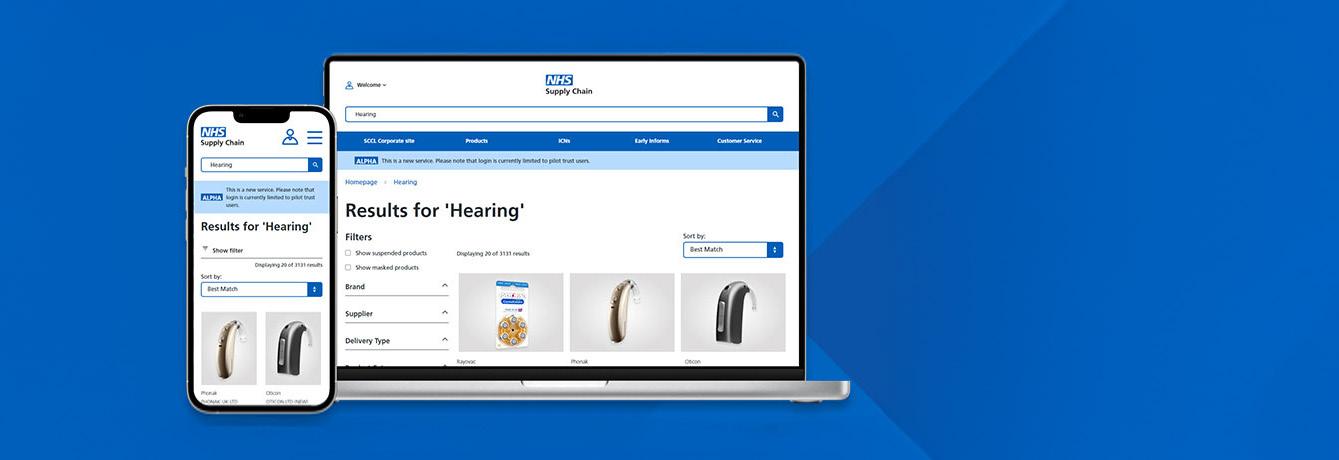

The NHS is entering a new era of procurement with the launch of a modern, user-led digital commerce platform. Designed in collaboration with NHS trusts, the new system from NHS Supply Chain streamlines product search and ordering, improves usability, and supports better operational performance across the health service
NHS Supply Chain manages the sourcing, delivery, and supply of healthcare products, services, and food for NHS trusts and healthcare organisations across England and Wales, processing more than 8 million orders per year, across over 129,000 order points, over 16,000 locations and consolidating orders from over 1,100 suppliers.
NHS Supply Chain customers spend over 33,000 hours a month using our online catalogue and ordering system, with over 100,000 individual users during that same period.
Customer feedback is very important to us and common themes included too much time being spent searching for and ordering products, with customers finding it hard to see what they are looking for, and quality of information being poor.
As part of our vision to be easier to work with, we have been working on a digital commerce programme to provide a new digital platform and interface, including our online catalogue, to make it easier for customers to search and order products on technology that’s scalable and flexible to adapt to evolving NHS needs.
Jodi Chapman, customer, communications and marketing executive director, NHS Supply Chain said: “We recognise that a modern digital
commerce experience is essential to resolve customer pain points and to ensure our service aligns to their expectations. We are working collaboratively with customers, internal teams and our tech partners to co-design the new platform, ensuring the needs of all users are considered. We want to be easy to work with across all NHS care settings.”
The new digital commerce platform aims to make it easier for customers to search for and order products, improving overall operational performance and effectiveness.
We’ve been working with a group of pilot trusts, delivering the platform and catalogue in incremental phases, getting the foundations and the basics right from the beginning and then, building on these improvements, have been introducing more features.
Manchester University NHS Foundation Trust have been instrumental in helping build the new platform as one of the first pilot trusts onboard since the launch of the Digital Commerce programme, feeding back each month as new features have been developed and deployed.
The trust will roll out the new and improved NHS Supply Chain catalogue to its Scan4Safety team, remarking on the much-improved search function.
Andrew Jackson, head of supply chain at Manchester University NHS Foundation Trust said: “I use the search function all the time because it is so much quicker, so I’m really keen to get other users onto the platform and using it.”
Emma Lowry, head of digital commerce, NHS Supply Chain said: “This is a great step forward, as we watch the data in the back end of the platform, we can learn from user journeys and understand the performance as we build up traffic.
“Other pilot trusts including, Barts Health, Nottingham University Hospitals, South Tees Hospitals and University Hospitals Sussex have also been adding more users to their platform. This shows the value of co-designing with our customers enabling them to expand access when they feel confident in the platform.”
Pilot users have been keen to share how the updates have made the ordering process easier.
Helen Sleeper, materials management team leader, Nottingham University Hospitals NHS Trust said: “I can see what’s in my basket at a glance, as it now includes images, which really speeds up the process”.
Sam Davison, clinical procurement lead nurse, South Tees Hospitals NHS Foundation Trust
said: “If I get called away from my desk halfway through placing an order, and my session times out, I can log back in again and my basket is still full.”
When on a visit, Bilal Ahmad, materials management team leader, Nottingham University Hospitals NHS Trust said: “The team use the mobile version a lot to look up products” recognising improvements to the platform making it easier to use when on the move, supporting the team and giving them flexibility when working across different sites.
There are many more developments coming up this year, and some great new features have been added to the platform recently, including: effective purchase controls, replacing masking; and product pricing, both including and excluding VAT.
As of June 2025, over 30 trusts across England and Wales have access to the new platform. As we work on our activation plan to give access to the new catalogue to all trusts, we invite any trusts interested in joining the initial tranche to get early access to the platform. M
If you are interested, please contact the Digital Commerce team at digital. commerce@supplychain.nhs.uk and copy in your NHS Supply Chain ICS Manager.

In today’s pressured healthcare environment, Provide Digital is proving that innovation and healthcare values can go hand in hand. Part of Provide Community, an employee-owned community interest company, Provide Digital delivers cutting-edge tech solutions rooted in purpose and social value

Unlike many commercial providers, Provide Digital reinvests its profits into community initiatives, colleague development and services across the Provide Community Group. This unique community interest company structure means priorities align naturally with the public sectors focus on outcomes, equity and longterm value.
Provide Digital brings rare agility to public health challenges. Whether teams need offthe-shelf tools or bespoke systems, they work collaboratively to meet service goals and budgets. Recently recognised winning two awards at the 2024 Health Tech Digital Awards, their work blends technical expertise with lived NHS experience.
At the core of Provide Digital’s offering is a suite of flagship applications, all initially designed to overcome Provide Community service challenges. They have all been built in collaboration with a deep understanding of frontline needs, creating real impact which has been experienced first-hand—tried, tested and trusted.
eC-Card : a secure, mobile platform replacing paper c-card schemes. Enables discreet access to condoms and sexual health resources, with real-time reporting and local customisation.
ProvideMyExperience: a fresh take on NHS feedback. This digital platform enhances the Friends and Family test, enabling fully customisable surveys with real-time analytics to drive continuous improvement in care.
eQuals : automates clinical training compliance with smart dashboards and alerts, reducing admin while enhancing quality.
Self-Referral System : centralises patient referrals, speeding up triage and freeing up clinical capacity.
MyCareBridge : streamlines the first step for autism and ADHD referrals, linking families, education and healthcare to support quicker, more empowering outcomes.
If you are seeking a partner who combines innovation with social value, Provide Digital is ready to help. Get in touch with the team for a free demo of any of their products, or to explore a tailored solution.
If you are attending HETT on Tuesday 7 or Wednesday 8 October, come and meet the team on stand C42!
In the hands of Provide Digital, technology doesn’t just solve problems, it builds lasting, positive change. M
FURTHER INFORMATION info@providedigital.com www.providedigital.com LinkedIn – @provide-digital

Following recent organisational changes within NHS England, the role of national leadership in shaping the future of health and care has never been more significant. As systems evolve and responsibilities shift, there’s a growing need for clarity, continuity, and collaboration. That’s why the presence of NHS England voices at HETT Show 2025 is so important
From policy direction and digital infrastructure to innovation, sustainability, and patient access, NHS England leaders are driving realworld change across the sector. This October, we’re proud to welcome a lineup of expert speakers from NHS England who are not only influencing national strategy but also
delivering practical solutions across frontline services.
These sessions are a unique opportunity to hear directly from the people at the centre of transformation, and to explore how their work connects with your challenges, priorities, and ambitions. E
Ming Tang, interim chief digital information Officer - Ming Tang is NHS England’s Interim CDIO and chief data and analytics officer, leading digital and data transformation across the system. Since joining the NHS in 2009, she has held senior roles in commissioning and driven major national programmes, including the Federated Data Platform. Her leadership ensures continuity and strategic progress as the organisation advances its digital agenda.
Vin Diwakar, interim national director of transformation - Vin leads the national rollout of major programmes like virtual wards, digital diagnostics, the NHS App, and AI strategy. His work spans frontline technology implementation and policy development— helping shape a more modern, connected NHS.
Mike Fell, executive director – national cyber security operations - From supporting the London 2012 Olympics to safeguarding NHS systems today, Mike brings deep expertise in national security. He leads teams building cyber
resilience across health and care, championing proportionate, transparent security that enables safe, uninterrupted care delivery.
Arrash Yassaee, deputy director MedTech Innovation - A doctor and transformation leader, Arrash has delivered major national programmes and helped launch breakthrough medical technologies. His focus on evidencebased innovation, regulation, and global digital health makes him a powerful voice on the future of MedTech in the NHS.
Ben Tongue, digital net zero lead, Greener NHS - Chartered environmentalist Ben Tongue is at the forefront of embedding sustainability into digital transformation. With a background in innovation and circular economy, he’s helping ensure digital health solutions also support the NHS’s net zero ambitions.
Claire Dellar, lead product manager & accessibility and inclusive design strategistClaire combines over two decades of experience in digital health with lived expertise in accessibility. She’s a powerful advocate for codesigned, trauma-informed digital services that


reduce inequalities and work for everyone—not just the majority.
Jules Gudgeon, national chief midwifery information officer - With nearly 35 years as a midwife and a track record in digital leadership, Jules is reshaping maternity and child health services. Her #FixingTheDigitalDivide initiative and advocacy for standardised digital leadership in midwifery are helping bridge gaps in access and care quality.
Rachel Hope, director of digital prevention services - Rachel heads up NHS England’s digital prevention portfolio, including the NHS Digital Health Check and screening services. Her work focuses on empowering individuals to manage their health and supporting proactive, population-level care through digital tools.
Join more speakers at HETT Show 2025 These speakers represent just a glimpse of the expert voices shaping health and care at HETT 2025. From cyber security and AI to
inclusion and innovation, they bring experience, insight, and action-oriented thinking to the conversations that matter most.
Whether you’re working to drive digital maturity, shape policy, improve patient access, or plan future services, the opportunity to connect with NHS England leaders in person is not to be missed.
Join us at our upcoming event, HETT Show on 7-8th October at ExCeL London to be part of the conversation. M
FURTHER INFORMATION
www.hettshow.co.uk

The ransomware attack on Synnovis in June 2024 exposed critical vulnerabilities in NHS cyber resilience, disrupting patient care and highlighting the growing threat to UK public services. As cyberattacks escalate, the government is responding with the Cyber Security and Resilience Bill
On 3rd June 2024, several NHS organisations, primarily based in South East London, were affected by a ransomware attack. Synnovis, a pathology partnership between SYNLAB, Guy’s and St Thomas’ NHS Foundation Trust and King’s College Hospitals NHS Trust and King’s College Hospitals NHS Trust, was hit by the ransomware cyber-attack, stealing data and halting blood tests in South East London.
Russian group Qilin later published almost 400GB of data stolen from Synnovis. More than 11,000 hospital appointments, GP appointments, and elective treatment, were disrupted by the attack, stolen data included patient names, dates of birth, NHS numbers and descriptions of blood tests. One patient died unexpectedly during the attack, which was later linked to the long wait for a blood test

result. The Health Service Journal additionally reported there were almost 600 “incidents” linked to the attack, with patient care suffering in 170 of these.
This cyberattack on the NHS has not been the first and will not be the last. In 2017, the NHS was one of several victims of a global ransomware attack known as ‘WannaCry’, which targeted computers running Windows by spreading a self-replicating worm that encrypted data and demanded ransom payments in the Bitcoin cryptocurrency. The attack disrupted over a third of England’s NHS trusts, cancelling over 6,900 NHS appointments, and costing the NHS around £92 million.
Critically, WannaCry’s effect on the NHS also had political implications. Many NHS trusts were using computers running Windows XP, an operating system first released in 2001 that Microsoft stopped supporting in 2014, and that the government had stopped paying for a cybersecurity package in 2015, which led to a Guardian article in 2017 entitled: ‘The ransomware attack is all about the insufficient funding of the NHS .” Then-health secretary Jeremy Hunt was accused of refusing to act on a critical note from Microsoft, the National Cyber Security Centre and the National Crime Agency, that might have been able to prevent the attack.


In
the
Following the attack, NHS Digital refused to foot the £1 billion bill to meet the Cyber Essentials Plus standard, which is a certification to show an organisation has cyber security protection. The WannaCry ransomware attack revealed critical holes in NHS’ cybersecurity, and outlined the need for adequate government investment in cyber protection.
In 2018, the Security of Network and Information Systems Regulations (NIS Regulations) were introduced, which provided legal measures to boost the overall level of security of network and information systems of both digital and essential services. These regulations currently cover five sectors (transport, energy, drinking water, health and digital infrastructure) and some digital services such as online marketplaces, online search engines, and cloud computing services. Twelve regulators are responsible for implementing these regulations. E

The tighter measures are to defend the public sector from a rapidly shifting cyber landscape
F As part of the government’s £2.6 billion 2022 National Cyber Strategy under the Johnson Conservative government, two Post-Implementation Reviews in 2020 and 2022 found that these regulations, although promoting positive change, were not thorough nor extensive enough.
Following a 2022 consultation, several recommendations to the NIS regulations were made, including giving the government power to amend NIS regulations in future to ensure they remain effective and improving cyber incident reporting to regulators. These changes, including several others, were implemented under the Sunak Conservative government. Starmer’s Bill, set to be introduced to Parliament this year, comes off the back of the NIS regulations.
First announced as part of the King’s Speech last July, the Bill will modernise the NIS Regulations to keep up to date with rising cybersecurity threats. The current NIS Regulations, inherited from EU law, have now been superseded in the
EU and require an urgent update should the UK wish to ensure their infrastructure and economy is not comparably more vulnerable.
The Bill makes changes to existing regulations, such as expanding the remit of said regulation to protect more digital services and supply chains, which are an increasingly more vulnerable entrance for would-be attackers. The Bill attempts to fill a gap in defences to prevent similar attacks to that on public health services, like the ransomware attack last year.
Additionally, the Bill would ensure that regulators were able to implement essential cyber safety measures, including potential cost recovery mechanism to provide resources to regulators and providing powers to investigate potential vulnerabilities before they escalate.
The Bill will also ensure that organisations adhere to reporting incidents to give government better data on cyber attacks, including where a company has been held to ransom. This is to help improve understanding of the threats and alert of potential attacks by expanding the type and nature of incidents that regulated entities must report.
The tighter measures are to defend the public sector from a rapidly shifting cyber landscape, in which cyber criminals continue to advance their technologies and improve the effectiveness of their strategies. Cyber attacks,
or attempted cyber attacks, are rife, with the 2024 Cyber Breaches Survey revealing that half of the participating businesses reported some form of cyber security breach in the past twelve months. Beyond the NHS, the Ministry of Defence, Leicester City Council, and the Post Office have all suffered cyber breaches with severe consequences within the last few years.
Cyber security, quite critically for the government, enables prosperity and growth, through allowing businesses to expand and attract investment. In 2024, Howden found that
cyber attacks have cost UK business £44 billion in the last five years, with half of UK businesses (52 per cent) having experienced at least one cyber attack in the past five years.
Peter Kyle, secretary of state for department for science, innovation and technology, said: “At the core of our proposals is this government’s number one mission: economic growth. Growth is the only route to creating new jobs and putting more money in working people’s pockets. But there is no growth without stability. By securing the digital infrastructure upon which a growing number of our businesses depend, we can deliver the stability they need to innovate and invest.
“Every business I have spoken to has said the same thing: we need agile, pro-innovation regulation that is designed for the digital world we live. Change has never been needed more.
“Together, we can grow our economy, rebuild our public services, and deliver a more secure, resilient and prosperous digital future for Britain.”

Consolidated Cyber Defence Solutions for the NHS and Healthcare
BlueFort empower healthcare organisations to deliver safe, efficient, and digitally secure patient care. From NHS trusts to integrated care boards to digital health providers, we deliver robust cybersecurity solutions that protect and ensure the availability of critical healthcare systems, protect sensitive patient data, and secure IT infrastructure.
Cyber Assessment Framework (CAF)

Meeting CAF requirements means proving security outcomes, not just controls. BlueFort helps organisations align with CAF expectations through practical, outcomedriven identity solutions
Secure
BlueFort helps manage thirdparty supplier risks by providing visibility into supplier and outsourced security practices, supporting audits, and ensuring that external partners meet your organisation’s cybersecurity standards through continuous assessment and control validation
BlueFort helps streamline and optimise security investments, reducing complexity while improving overall effectiveness.
Identity Security
Protect human and machine identities with scalable, practical solutions
Cloud Security
Secure hybrid and multi-cloud environments with cloud-native protection



Security Platforms
Maximise protection and efficiency with integrated, modern security platforms
Zero Trust
Simplify and strengthen remote access with Zero Trust architectures


How to embrace innovation and control costs without compromising NHS cybersecurity

At BlueFort, we work closely with NHS trusts across the UK, putting us at the coalface of the cyber threats targeting our health service. With digital transformation central to the government’s 10-year NHS plan, there’s a vital opportunity to build greater cyber resilience into the fabric of NHS operations.
But the challenges are significant. Trusts must navigate the demands of securing legacy infrastructure while protecting complex IT estates, often with limited resources. New regulatory frameworks, including the Cyber Assessment Framework (CAF) and Data Security and Protection Toolkit (DSPT), are raising the bar for security standards but add pressure to already stretched IT teams.
In May 2025, the NHS introduced the Cyber Security Charter for Suppliers This requires all suppliers to publicly affirm their commitment to NHS cyber safety, further underscoring the importance of high-assurance partnerships.
The adoption of AI tools within the NHS, such as Microsoft Copilot brings both innovation and risk. In a data-sensitive environment like the NHS, even unintentional misuse—such as sharing patient data across departments—can lead to GDPR breaches and loss of public trust. As AI becomes more embedded in healthcare workflows, the need for strong governance, data controls, and user education grows increasingly urgent.
At BlueFort we are lucky enough to partner with some of the most progressive IT security teams in the NHS. We work closely with trust IT teams to implement robust controls and achieve compliance with CAF while reducing the risk of accidental data exposure and enabling safe use of AI technologies.
A recent example is our work with South London and Maudsley NHS Foundation Trust. By replacing legacy infrastructure with a modern cybersecurity solution in partnership with iboss, the trust improved operational efficiency, boosted cyber resilience, and achieved demonstrable compliance with DSPT/ CAF requirements all while saving a significant amount in operating costs.
We also helped one London-based NHS trust’s security-conscious IT team deploy, configure and optimise a new MFA solution in just under three weeks.
As a signatory of the NHS Cyber Security Charter , BlueFort is committed to the highest technical and operational standards. Our team supports trusts and integrated care boards (ICBs) across the UK in navigating today’s threat landscape while preparing for the future.
Let’s work together to strengthen cyber resilience and support the digital evolution of the NHS. M
Darren Smith, Head of Public Sector – BlueFort Security Ltd.
Cornerstone, using their SMART knowledge, break down the difficulties of damp and mould, and how you can rid your buildings of them indefinitely
Cornerstone are proven independent Property Health Expert Surveyors aligned to assessing and reporting on a myriad of structures designed to uphold property health for those who manage, live, work and learn in them.
Our key services are aimed at all interested parties and occupants seeking reputable independent advice and guidance for cost effective solutions designed to resolve an issue for maintaining long-term healthy locations.
Of note, mould in structures is a ‘symptom’ of a problem and, with available SMART knowledge, can be readily assessed for determining its likely root causes.
Damp however, is a physical detriment that will show itself as spoiling, discolouring, cracking, and/or blistering. Remember that our everyday moisture generation (including breathing) releases more moisture into the atmosphere than a damp structure would.
Structural health surveys should embrace the interior and exterior of a building alongside its construction, orientation and existing insulation and breathability attributes because each can play a part in why the visual mould aspect is developing where it is alongside the pattern being generated. This approach serves to aid defining the number of root causes (because there is always more than one!) and painting over or cleaning mould affected areas does not deal with the issue.
And, did you know, as we have strived to seal our structures to uphold heat retention and our carbon footprint, over the years mould has retrospectively increased? This is mainly due to the significant emphasis the aforementioned
places on our new living protocols with a main focus on ‘adequate ventilation’.
A healthy dwelling or workplace requires a balance of heating and ventilation to maintain a desired internal environment and, in the absence of such, can affect the personal health of persons within the locations.
Our immune systems are different to each other and, is why some people may be readily affected by the initial onset of mould whereas others can reside within areas of significant mould development with no defined health issues.
However, immunocompromised personnel will be affected and aligns to a recommended broad-spectrum approach for all locations to uphold healthy environments for everyone.
Cornerstone are committed to sharing knowledge with CPD bespoke training for ventilation, damp and mould related issues that delivers reasoning alongside defined outcomes for a long-term healthy home, school, hospital, care home and workplace. M
To learn more of our trusted independent expert advice, please contact: Tel: 0344 846 0955 enquiries@cornerstone-ltd.co.uk www.cornerstone-ltd.co.uk


Back in May, the government announced that a £102 million cash injection would facilitate modernising over 1,000 GP surgeries, allowing them to create space to see more patients, improve their patient care, and boost productivity, resulting in an expected 8.3 million extra appointments each year
The funding is a much-welcome investment, seeing as primary care received the lowest share of NHS funding in 2023-24, at just 8.4 per cent, and saw it fall below inflation. A new contract in March 2024 included a 1.9 per cent baseline uplift, but was still below inflation levels. This is a marked decrease from a high point of 9.2 per cent on NHS spending in 2019-20.
NHS funding has historically been skewed towards the acute sector, namely hospitals, which was only exacerbated by the COVID19 pandemic: it is not a rare occurrence for
hospitals to use their capital budgets to plug shortages on day-to-day spending, and still needing more money to perform urgent, timeconstrained services, which differs from the majority of primary care’s job requirements. This is despite general practices receiving the most contact with the public, with an estimated 300 million appointments each year.
A February 2025 poll by the Health Foundation and Ipsos found that 38 per cent of those surveyed ranked easily accessing GP appointments as their top priority for the changes they’d like to see to the NHS under Starmer’s leadership. This is significantly E
M
I N T E N A N C E F R E E
m e a n s c o s t e f f e c t i v e w a l l a n d d o o r p r o t e c t i o n
H Y G I E N I C A N D E A S Y T O C L E A N
P reve n t eve r yd ay we a r a n d t e a r w i t h
Ye o m a n S h i e l d ’s ex t e n s ive ra n g e o f
e a s y - cl e a n , wa l l a n d d o o r p ro t e c t i o n
O u r a t t ra c t ive, m a i n t e n a n c e f re e, hyg i e n i c p ro d u c t s p ro t e c t h e a l t h c a re
e nv i ro n m e n t s f ro m c o s t l y i m p a c t
d a m a g e, m a k i n g re p a i n t i n g a n d re p a i r
a t h i n g o f t h e p a s t .
B l e n d i n g w i t h d e c o rs a n d ava i l a b l e i n

p r i m a r y d e m e n t i a - f r i e n d l y c o l o u rs,
o u r d e s i g n s c a n i n cl u d e s i g n a g e, t o
p ro m o t e t h e we l l - b e i n g o f p a t i e n t s
a n d a i d way fi n d i n g.

F




F ahead of other top priorities, such as improving A&E waiting times (33 per cent), staff retention (29 per cent), and routine hospital services (27 per cent). In 2023, only half (52.8 per cent) of patients were satisfied with their appointment times, a huge decrease from 64.7 per cent in 2019. Clearly, the situation is only getting worse.
Both a crumbling GP estate and a shortage of new GPs contribute to too many patients scrambling for not enough appointments. In 2024, the Institute for Government published a report, Delivering a general practice estate that is fit for purpose , that found that the NHS’s 2019 Long Term Plan, which introduced primary care networks, and the 2019 Conservative manifesto, which pledged to hire 6,000 more GPs, were largely unsuccessful. It warns that the NHS is unlikely to meet its Long Term Workforce Plan target of increasing new GP trainees by 50 per cent, from 4,000 in 2022 to 6,000 by 2032.
More GPs is crucial to unlocking more appointments, but in 2022, it was found that 22 per cent of 8,911 premises were built before the NHS was established in 1948. These buildings are cramped, crumbling, and outdated, with GPs reporting that 22.4 per cent of general practices are not fit for purpose. Having an agenda to increase the number of employees without simultaneously developing and upgrading the spaces they will work in is fruitless. A recent survey found that 88 per cent of GP respondents said they did not have
In 2022, it was found that 22 per cent of 8,911 premises were built before the NHS was established in 1948
a sufficient consulting room. While a mass recruitment campaign would be invaluable, it is also crucial that capital investment increases at the same rate, especially as GPs harness more and more digital tools in buildings that cannot accommodate them.
Since 2015, the number of qualified GPs has been in decline, with 1,167 fewer in December 2024 than in December 2015, despite an ambitious target in place to recruit 6,000 more by early 2024. However, it is difficult to recruit, train, and host thousands more GPs in buildings that do not have the capacity.
In the Autumn Budget, the government allocated £100 million, as part of an increased chunk of funding for the Department for Health and Social Care, to upgrade GP facilities, as well as hiring an extra 1,000 GPs. But the funding for upgrading GP practices was initially just for 200 surgery upgrades, rather than the new figure of 1,000.
The recent announcement follows the new 2025-26 GP contract that came with an extra £889 million, as announced in December. E






F In April, the government announced that over 1,503 GPs were hired from October 2024, which contributed to the delivery of achieving two million appointments seven months early, but did not address a primary estate that struggled to cope with current numbers, never mind an influx of new employees.
This funding represents the biggest investment in GP facilities in five years, with several deprived general practices being able to benefit, and is the first national capital fund for primary care estates since 2020. The first refurbishments are set to take place this summer for around one in six GP practices, and to be delivered up until April 2026.
Prospect Medical Practice in Norwich, for example, will be able to create new clinical rooms to deliver more consultations to its 7,000 patients.
Harden Health Centre in the Black Country will see vacant office spaces be converted into clinical consulting rooms, allowing more patients to access primary care and, vitally, more GPs to work in this practice.
Two surgeries in Redbridge, East London, have been awarded funding: Kenwood Medical Centre in Gants Hill and Loxford Polyclinic in Ilford. The former will use the funding to refurbish its ground and first floors to accommodate the relocation of up to two
Harden Health Centre in the Black Country will see vacant office spaces be converted into clinical consulting rooms
additional GP practices to create an extra 38,500 appointments each year, and the latter to create eight new clinical rooms, creating 22,000 extra appointments each year.
Rachel Power, chief executive of the Patients Association, said: “[This] investment in improving GP surgeries is a much-needed step towards better access to care closer to home.
“Our reporting shows nearly one-third of patients struggle to book GP appointments, and we have long highlighted what matters in healthcare facilities: truly accessible spaces where everyone receives care with dignity. The potential for 8.3 million additional appointments from these refurbishments will make a real difference to communities waiting for care.
“Crucially, it delivers on what patients themselves have called for: modern, accessible spaces that support high-quality care. We look forward to seeing these upgrades rolled out, with a continued focus on ensuring patients everywhere get timely support in settings that support their dignity. This investment represents a meaningful step toward realising what patients have long been asking for.” L






We’re proud to be exhibiting at Healthcare Estates in Manchester on 21–22 October. Join us on our stand for live demonstrations, every hour and discover how our latest innovations are transforming water safety across Healthcare Estates:
Aqua Remote™ – Digital monitoring for real-time visibility of water temperatures, usage, and compliance status.
Aqua ProTrack™ – Smart sample tracking with full chain-of-custody and faster, clearer lab results
Net Zero Commitments – Learn how Aqua Protec is aligning its operations and services with sustainable practices
Visit aquaprotec.co.uk to find out more and plan your visit. Come and meet the team, explore our solutions, and see how we’re supporting a safer, smarter, and more sustainable future for healthcare estates.
Don’t miss our Managing Director, Sophia Carter speaking on Water Safety Planning
Wednesday | 2:30pm in the Water & Infection Control Theatre





IHEEM’s flagship annual conference, exhibition and awards takes place on 21-22 October at the Manchester Central convention complex, and will once again act as an invaluable event for professionals involved in the funding, design, building, management and maintenance of healthcare estates and facilities
Bookings are now open on the event website— www.healthcare-estates.com—where the event programme is also now live. There is the option to attend for free (Exhibition Visitor Pass) or to upgrade to an access-all-areas Conference Delegate Pass.
The overarching theme for Healthcare Estates 2025 is ‘Prevention is better than cure’, a theme that will resonate deeply within the healthcare sector. With the next ten years set to see unprecedented investment in the NHS, it is more important than ever that healthcare professionals from the NHS, government, industry and academia come together to share lessons learned and build collective understanding of how we deliver a world-class healthcare service for patients.
Across its extensive programme of content— much of which is free to attend—and its comprehensive exhibition, Healthcare Estates 2025 will provide an invaluable opportunity
to share knowledge and gather the ideas, information and answers to navigate the evolving landscape.
Two exciting new features for day two of the event—which will be open to all attendees—have been announced, with more in development.
The first is a powerful new networking experience, taking place at the end of day two. This ‘event within the event’ will combine expert reflection, community celebration and meaningful connection. Open to all attendees and featuring complimentary refreshments to help refuel you for the journey home, this is your opportunity to reflect on key takeaways from the event, network with keynote speakers and fellow attendees, and recognise outstanding achievement with the IHEEM Branch Awards — celebrating leadership, innovation, and community across IHEEM’s UK branches. E
F The second new feature is the integration into the programme of live interviews with the newly crowned winners of the 2025 Healthcare Estates Awards. These sessions will offer behindthe-scenes stories and proven strategies from those setting the standard in innovation and operational excellence—a new and invaluable feature for 2025.
The Healthcare Estates Conference
Attending the conference gives an unparalleled opportunity to engage and interact with healthcare leaders, experts and fellow senior professionals from the public and private sector. It is an efficient way to engage with key issues and enhance knowledge.
As well as access to the keynote programme and the full exhibition (including the option to attend sessions in the exhibition theatres), conference delegates benefit from exclusive access to a broad programme of authoritative conference content, including presentations, panels and interactive workshops. Engaging in the programme provides the opportunity to gather insights and information, and to interact with speakers and fellow attendees to share knowledge and experience.
As in previous years, the programme is crafted to deliver specialist insight and guidance from those helping to shape the regulations, standards, and strategic direction of the sector.
Among many highlights, attendees will benefit from insights and updates from the New Hospital programme, NHS Estates, NHS SBS, NHS Commercial Solutions, multiple NHS
trusts, leading global suppliers and the IHEEM Technical Platforms.
2025 conference themes
Strategic health and social care planning; governance, assurance and compliance; digital technology and innovation; medical and healthcare engineering; and estates and facilities services.
The Exhibition Theatre programme
Visitors to the Exhibition also benefit from an extensive programme of free content, with six free-to-attend Theatres located within the Exhibition Hall. This provides all attendees with the opportunity to update their knowledge and interact with speakers and fellow attendees on subjects important to effective delivery in their role.
2025 Exhibition Theatre themes:
Design and construction (presented in association with Architects for Health); energy and sustainability (presented in association with The Carbon and Energy Fund); facilities management; HVAC and engineering; software and smart hospitals; and water and infection control (presented in association with The Water Management Society).
The keynote programme also takes place in the main theatre in the Exhibition Hall, with keynote presentations open to all attendees at no extra cost – providing everyone with access to the most authoritative updates for the current operating environment.


The Healthcare Estates Exhibition is the UK’s most comprehensive showcase of products, equipment and services to support those responsible for funding, designing, building, managing, and maintaining healthcare estates and facilities.
The 2025 floorplan has been expanded to provide visitors with access to the largest-ever selection of leading suppliers. Here you will find solutions and expertise covering all the key areas: planning, design and construction; energy and sustainability; facilities management and maintenance; HVAC and engineering services; software, data and smart tech; water management and infection control; and much more.
Visitors to the Exhibition can engage with teams from the New Hospital Programme and NHS England, both of which organisations will have stands in the Exhibition Hall. This is an opportunity to get the most up-to-date information and for representatives from NHP schemes to meet with each other and share knowledge and experience.
The Healthcare Estates Awards recognise outstanding organisations, teams and individuals in the fields of healthcare engineering and estates facilities management.
This year’s categories are: Apprentice of the Year; Architectural Practice of the Year; Consultancy of the Year; Diversity and Inclusion
Award; Estates and Facilities Champion of Champions; Estatesand& Facilities Team of the Year; Healthcare Supplier of the Year; New Build Project of the Year; Product Innovation of the Year; Refurbishment Project of the Year; and Staff Wellbeing Initiative of the Year; Sustainable Achievement Award.
Each year, the awards are presented at a sparkling gala dinner. This year’s dinner will be held on Tuesday 21 October, at the iconic Kimpton Clocktower Hotel in Manchester. Guests will enjoy a pre-dinner drinks reception, followed by a three-course meal. The evening will be further elevated by the presence of Michael Portillo—distinguished journalist, broadcaster, and former MP—who will mingle with guests before dinner before delivering the after-dinner address and presenting the Awards to outstanding individuals, teams, projects and products in 12 categories.
Reservations for the awards dinner can now be made via the Healthcare Estates website: www.healthcare-estates.com. Options include individual places and tables of ten, with a limited number of VIP tables available for organisations wishing to maximise their visibility at the event. M
www.healthcare-estates.com

Swiftclean can help you keep your residents safe with their award winning air & water hygiene services.
Kitchen Extract Fire Safety Cleaning to BESA TR19® Grease
Ductwork cleaning to BESA TR19®Air
Fire damper function testing to BS:9999
Indoor Air Quality testing & monitoring to BESA H&W002
Legionella Risk Assessment, sampling, testing, monitoring & remedials to ACOP L8

From unclear job roles to contaminated cleaning cupboards, Kelsey Hargreaves, technical manager at BICSc, explores the hidden challenges for improvement in healthcare cleaning
In my first few months of really working within the cleaning industry, I was in a place where using the words ‘infection control’ came as naturally as breathing. It seemed so amazing and official to me to be able to say those words. I wasn’t a nurse or a doctor, I was in the cleaning team, and yet I was able to share stories of infection risks and best practices for ‘infection control’. It took me a while to grasp the breadth of everything that was involved. And I think if we are all being honest, many parts of infection control are still unbeknownst to us, how deep we can go with it, classify a control measure, a risk and especially how to execute it fully. Infection control is often discussed in terms of visible actions – disinfecting surfaces, wearing gloves, using approved chemicals, and washing our hands. But beneath these surface-level practices lies a complex web of control mechanisms that determine whether
our actions are truly effective in preventing the spread of infection. In this article, I’m going to refer to the cleaning side of infection control, but the hidden dimensions of control that we often don’t talk about. A look at common practices or in practices that I have seen time and time again, that we all seem to bury our heads in the sand over and pretend it doesn’t happen.
The worst and most overlooked infection control risk, in my humble opinion, is the lack of transparency, clarity, understanding and standardisation of job roles. I often joke about the age-old question: “To clean blood or not to clean blood,” but it is a stark reminder of a real issue within healthcare cleaning.
You are lucky if there is specification or a scope that dictates who should do what task and E

F who is responsible for things like changing bed linen, handling bodily fluids; and cleaning blood spills.
These tasks often fall under clinical or specialist roles, yet in practice, they are often delegated informally or expected of the “cleaning staff” by those who do not want to spend time doing them. This blurring of responsibilities introduces risk, especially when operatives are not trained or equipped for such tasks. Standardising job descriptions and enforcing boundaries is essential to ensure that infection control protocols are followed correctly.
Additionally, many organisations confuse cleaning processes (the how) with cleaning elements (the what). For example, a checklist might include “clean the floor,” but not specify whether it involves bodily fluid contamination, which requires a different protocol. This lack of specificity can lead to inconsistent practices and increased infection risk. Develop processspecific protocols that clearly differentiate between routine cleaning and infection-related interventions.
All this ambiguity can lead to delayed responses or improper cleaning, both of which compromise infection control. Organisations must establish clear, written protocols for handling biohazards, including: who is responsible; what PPE is required; what cleaning agents are approved; and how waste should be disposed of.
formal protocols often leads to sustained malpractice
Outside of the healthcare environment, uniforms are often seen as protective, but they can also be vectors of contamination if not managed properly. I remember the shocks and choir of gasps that myself and Denise, commercial director of BICSc, received when we changed into our uniforms at work before commencing training and changed back out of them, washed ourselves and bagged/sealed the uniforms before leaving. Why wouldn’t we? Why aren’t we considering the cycle of our workwear as an IPC risk? Think about what we could take home to our loved ones, and think about what we could bring into spaces where others have loved ones? Another feature of the everyday that without proper management could have catastrophic results.
In any organisation, the ad-hoc request is often one filled with the most risks – cleaning is no different. Bypassing formal protocols often leads to sustained malpractice, untrained operatives completing the task quickly and improper risk assessments of the job that needs to be done.
Furthermore, there are problems with not just the clothes on our backs, but what we bring with us to work: CCCC – Cleaning cupboard cross-contamination.
Think of the average cleaning cupboard – what does it have in it? Mops, cloths, vacuums… what else? As much as it pains me to say it, other common features of a cleaning cupboard are: jackets, coffee mugs, shoes, hairbrushes, today’s lunch, or last week’s?
Cleaning cupboards are often used to store everything, from chemicals to personal items. This creates a high-risk environment for crosscontamination. The best advice that I can give is that we should be treating cleaning cupboards like preparation rooms for theatres. It should have only the equipment we need to perform the tasks we need to do. It should be kept tidy, clean and decontaminated after use. If it is in the cleaning cupboard, it is to be used to aid cleaning, not to be used to brush one’s hair, or hold a cup of tea. To help this become a zone of control and not a source of contamination,
companies should: provide individual lockers for personal items; separate chemical storage from equipment storage; regularly audit storage areas for compliance and remove unnecessary items; and provide separate spaces for lunch.
Another often overlooked aspect is the psychological safety of cleaning staff. When operatives feel empowered to speak up about unsafe practices or unclear instructions, infection control improves. Creating a culture where feedback is welcomed and acted upon can lead to better adherence to protocols and a stronger sense of responsibility among staff. This cultural shift requires leadership commitment and consistent reinforcement.
All these changes come with time, even with protocols in place, infection control fails without ongoing training and reinforcement. So is lack of reinforcement, lack of training and lack of assurance an infection control risk? Absolutely.
I can honestly say that I have received no formal infection control training, but I
True infection control in cleaning is not just about disinfectants and mops
have received training that has helped me understand the most important parts of control and allows me to be dynamic in my assessment of IPC risks.
True infection control in cleaning is not just about disinfectants and mops – it’s about control systems, role clarity, infrastructure, and culture. By addressing the hidden layers of control and standardisation, organisations can transform cleaning from a routine task into a frontline defence against infection. When we focus on these hidden layers of control, we move beyond surface-level hygiene. We create environments where cleaning is not just reactive, but proactive. Not just routine, but strategic. And in doing so, we protect not just spaces, but people. M
www.bics.org.uk





The Infection Prevention Society’s annual conference, Infection Prevention 2025 is taking place at the Brighton Centre on the 29th and 30th September. This world-leading event features an innovative scientific programme led by international and national experts in infection prevention
Dr Jude Robinson, IPS president says: “It is my pleasure to welcome you to IP2025, which is the Infection Prevention Society’s flagship event of the year. This event is for everyone working in or interested in infection prevention and control. The annual IPS conference, as always will bring you a high-quality educational experience, together with expert speakers, innovations, best practice solutions and research that will leave you energised with ideas, connections and networks to take back to your areas of work, be that clinical practice, research, education or industry.
Our lineup of expert speakers is phenomenal, with themes this year including AMR in action, sustainability, climate change, use of digital AI, the role of education, training and collaboration in the digital age, behavioural insights, built environment, IPC in specialist settings as well as topical pathogen specific sessions. With such
a diverse range of topics and speakers there is always something to learn here for everyone.
Beyond the speakers and sessions, networking is an integral part of the conference, offering like-minded individuals the opportunity to connect, collaborate, and unite in their shared mission to prevent infections. Thank you for your commitment to infection prevention, and I look forward to seeing you at our event.”
Don’t miss this world-leading infection prevention and control event!
Conference highlights Conference highlights include: an inspiring scientific programme covering infection prevention and control in all aspects of care; national and international expert speakers; largest UK infection prevention exhibition; call for abstracts: posters and oral presentations;
networking opportunities; flexible registration packages; and an engaging social event
Full details are available on the conference website
Secure your spot at the forefront of infection prevention. Explore our flexible registration packages and pricing options tailored to meet your professional needs. Join the global conversation and gain access to invaluable resources and networking opportunities.
There are a range of registration options on offer at IP2025 to suit your availability, including 1-, or 2-day registration packages, and discounted registration fees for members, groups, undergraduate students, and those from resource limited countries.
With IPS membership, not only do you gain access to exclusive benefits, but you also unlock discounted rates for IP2025 registration. Join now to enjoy instant savings on your conference visit! See more here and find out more and register here .
The programme
Dive into our 2-day cutting-edge scientific programme featuring a myriad of sessions led by international experts in infection prevention. Discover insightful topics, workshops, and discussions designed to advance knowledge and strategies in combating healthcare-related infections.
National & international expert speakers will discuss the following key topics: fundamentals of care; IPC in specialist settings; IPC risk in and from the built environment; improving quality through Patient Safety Incident Response Framework (PSIRF); digital / AI solutions; sustainability; AMR; and organism/site specific examples from practice.
We are delighted to confirm our keynote speakers for IP2025: Dr Neil Wigglesworth will open conference with this year’s Cottrell Lecture; Professor Michael Borg will deliver the Tina Bradley Lecture on “From Reminder to Reflex: Making IPC Second Nature”; and Professor Martin Llewelyn will deliver the Ayliffe Lecture on “Antimicrobial Stewardship: at the heart of infection prevention”.
Their specialised expertise and insights promise to make our sessions informative for all attendees.
View the programme in full here
Enhance your conference experience with our engaging social event! Enjoy our social event and awards where you can network with peers and experts in a relaxed setting while celebrating advancements in infection prevention.
This year’s social event and awards ceremony will be held at the Grand Hotel, Brighton and will start at 7pm. The evening will include a welcome drink, canapes, awards and entertainment. Tickets are included in all delegate registration types (except Tuesday only tickets). Find out more here .
Infection Prevention 2025 features the UK’s largest infection prevention exhibition, with approximately 70 companies in attendance showcasing a huge variety of products, services and innovations.
IP2025 is expected to attract over 500 professionals in this field. Exhibitors can collect quality leads from dedicated infection prevention and control professionals who are passionate about learning and improving their facilities.
If you are interested in finding out more about the exhibition and sponsorship opportunities available for your company at the Conference visit us here , or contact Michael.donaldson@ fitwise.co.uk
Thank you to those who have already signed up to support the event. To include our exclusive sponsors: GAMA Healthcare are this year’s platinum sponsor, and Tork are this year’s gold sponsor. M
The Infection Prevention Society (IPS) represents 2,300 members working in the field of infection prevention and control, and plays a key role in helping to protect the public. For more information visit: www.ips.uk.net
FURTHER INFORMATION
www.ip2025conference.co.uk


EPSO Total Cleaning Service Solutions (263_25) is a framework that provides access to a whole host of cleaning providers, from whom organisations can easily set up supply arrangements
A Department for Education-approved ESPO framework, it opened on the 1st January 2025 and will end on 31st December 2026, with the option to extend until the same date in 2028. Customers can go down the direct award route or through further competition.
The framework comprises three lots across different types and depth of cleaning required by the customer.
Lot 1: General cleaning (includes window and external cleaning):
Lot 1 covers the vast majority of general cleaning requirements, which includes but is not limited to: washing, buffing, mopping, sweeping and vacuuming of floors; cleaning and vacuuming mats and matwells; cleaning of walls including paintwork, doors, door frames, window frames and similar areas; cleaning furniture, fixtures and fittings such as vertical and horizontal surfaces, tables, desks, chairs, filing cabinets, cupboards, lockers, shelves, ledges, skirting boards, radiators, pipes, fire extinguishers, light switches, handrails, balustrades and other similar areas; cleaning any internal glazing such as
mirrors, windows, glass doors and partitions; cleaning windows externally; cleaning basins and general fittings such as wash and hand basins, splashbacks, pipes, plugs, sink units, taps, drinking fountains, shower fittings, soap dispensers, towel dispensers and cabinets, hand dryers, toilet roll holders, sanitary towel disposal units, and the like; cleaning toilets including urinal channels and bowls, WC pans, seats, seat hingers, handles, chains, and cubical walls; cleaning the insides and outsides of microwave ovens, refrigerators, cookers, and any other similar related items; emptying and cleaning the waste bin; wiping and sanitising phones and other similar items, and polishing bright metal work.
Lot 1 also includes ad-hoc deep and specialist cleaning services when they form part of a wider general cleaning contract, provided that the majority of cleaning services as part of this contract fall within the scope of general cleaning services.
Lot 2: Deep and specialist cleaning
Lot 2 comprises deep and specialist cleaning on a schedule and reactive (four hour or 24 hour
call out). Services under this Lot include but are not limited to: ambulance deep cleaning and ‘make ready’ services; biohazard cleaning; bird dropping removal; carpet and upholstery cleaning; chewing gum removal; flood damage clean-up; graffiti removal; healthcare cleaning; infection control; kitchen deep cleaning; kitchen ventilation cleaning; odour removal; police and prison cell cleaning; post-viral deep cleaning; sewage clean-up; sharps removal; trauma cleaning; void property cleaning; washroom deep cleaning; as well as other associated deep and specialist cleaning services such as bacteria and hygiene assessments.
Lot 3: Decontamination systems
Lot 3 covers decontamination services and is divided into four Lots, from 3A to 3D, and offers customers Hydrogen Peroxide Vapour or Ultraviolet-C to decontaminate environments or areas.
Lot 3A HPV Decontamination Systems deals with the purchase and/or rental of Hydrogen Peroxide Vapour (HPV) systems, whereas Lot 3C HPV Decontamination Services covers the
Lot 2 comprises deep and specialist cleaning on a schedule and reactive
same service on a scheduled and reactive basis.
Lot 3B UVC Decontamination Systems covers the purchase and/or rental of Ultraviolet-C (UVC) decontamination systems, and its partner Lot, Lot 3D Decontamination Services, covers decontamination services on a scheduled and reactive basis using Ultraviolet-C (UVC).
There are 63 suppliers across all three Lots, including AEFM Limited, Carlisle Cleaning Services Limited, Mr Bright’s Ltd, and Solo Service Group Ltd.
This framework serves to benefit your organisation through providing access to a large number of service providers who can accommodate your cleaning specifications, no matter how specialist. M
FURTHER INFORMATION
www.espo.org/total-cleaning-servicesolutions-263-25.html










With infrastructure challenges mounting across the NHS, the Building Safety and Fire Compliance Framework offers a trusted route to meet strict fire safety regulations, manage risk, and futureproof healthcare environments
Active until February 2029, the framework is open to the NHS and UK public sector organisations, and was procured under the new Building Safety Act (2022), a comprehensive law implemented in response to the Grenfell Tower fire to improve fire safety. The Act applies to new or existing occupied buildings over 18 metres high or seven stories tall, and sets strict rules for designing, constructing, and managing buildings, clearly defining the responsibilities of Duty Holders, those who own, design, or are contractors of the building, which includes care homes and hospitals.
The Act requires all parties involved in building safety to be competent and compliant with the safety regime, which includes providing evidence. As a result, NHS Shared Business Services’ Building Safety and Compliance Framework Agreement provides services from passive and active fire safety to PAT testing from a range of compliant suppliers for the healthcare sector, to ensure full accordance with The Building Safety Act.
Thorough fire safety is critical in healthcare settings: evaluations reveal that every £1 invested in the Fire Management Services results in a minimum saving of £2.52 in healthcare expenditure.
This comes at a critical time for the NHS, and the wider healthcare sector in the UK, as infrastructure challenges are widespread across the country. NHS England has estimated a maintenance backlog cost of £13.8 billion, which is more than the cost of running the entire estate at £13.6 billion. Lord Darzi’s 2024 Independent Investigation of the National Health Service in England, also known as the Darzi report, found that NHS capital budgets had regularly been raided to plug holes in dayto-day spending, resulting in an estate “starved of capital”. Crumbling buildings disrupted 13 hospitals each day in 2022-23, and the National Audit Office reported 5,400 clinical incidents E


agreement has been split into ten different lots, organised by category
F in 2023-24 due to infrastructure failures and poor conditions.
The government has since allocated £1 billion to tackle critical repairs and address a mounting maintenance backlog, with £102 million to start upgrading GP surgeries, which are also suffering from capital deprivation. The New Hospital Programme is an NHS initiative to rebuild and modernise healthcare facilities, including creating new hospitals, has been injected with £15 billion in funding, and aims to deliver upgrades and new builds in five-year waves. The framework will be vital for hospitals undergoing upgrades, as well as those being built now, in ensuring that these buildings are safe and fire compliant.
Valued at £200 million, this framework agreement from NHS SBS has numerous benefits, largely that customers can procure all of their building safety and compliance needs in once place. This additionally ensures that all providers meet British standards, Health Technical Memoranda (HTM) and all relevant industry accreditation, as well as being compliant with Asbestos Regulations 2012.
Ensuring that all suppliers uphold compliance and incorporate stakeholder rights, NHS SBS can guarantee that this framework is not only reliable, but essential for any entity to operate compliantly within the NHS ecosystem.
NHS SBS’s combination of both passive and active fire safety measures makes it an indispensable resource, covering the implementation of fire-resistant materials and structures like fire doors and fire-resistant walls, as well as the installation and maintenance of fire detection and suppression systems, such as smoke alarms, fire extinguishers, and sprinkler systems.
This framework agreement has been split into ten different lots, organised by category. Lot 1.1, 1.2, and 1.3 deal with fire safety, the former on passive fire safety, the middle on active fire safety, and the lattermost on fire risk assessments and consultancy services. Lots

2.1 and 2.2 concern asbestos management and removal, respectively.
The maintenance, design and installation of lifts is found under Lot 3, Legionella and water treatment services under Lot 4, and PAT testing under Lot 5.
Lot 6 comprises authorising engineer and Lot 7 handles pneumatic tube systems.
The range of available suppliers is extensive and set to further expand, including Pennington Choices Limited, Scrubs Contract Services Ltd, Hydrock Consultants Ltd, and BLS Asbestos Limited.
On the framework, senior category manager at NHS SBS, Brendan Griffin-Ryan, said: “The increased emphasis on fire safety brought about by the dreadful Grenfell Tower disaster has shown that some NHS buildings fail to meet modern safety standards and underscores why fire safety compliance and protocols are paramount….
“The NHS must prioritise fire safety to prevent similar incidents similar to Grenfell from occurring in healthcare settings, where the impact could be catastrophic.
“Our framework agreement provides the NHS with a comprehensive range of services. It aligns with key health and safety regulations –ensuring seamless integration and adherence to all compliance in critical areas like fire safety, water treatment, and asbestos management, crucial for maintaining the safety and integrity of NHS buildings, protecting patients, staff, and visitors.” M
The framework can be found here.
Whoever the user, whether that be healthcare professional, patient, or service user, protect against hot water scalding through thorough assessment and installation of thermostatic mixing valves
Thermostatic mixing valves (TMVs) are designed to mix hot and cold water to provide scald protection in a water system.
The use of TMVs has become common place, especially in healthcare and care facilities, but overuse can increase the risk of issues on site.
TMVs work by blending hot and cold water to a preset temperature through a valve body (or tap cartridge), which are composed of multiple parts including the main casing, strainers, O-rings, thermostatic piston, springs and seals.
Some TMVs can be broken down into up to 30 constituent parts.
Every element of this unit has the capacity to allow for biofilm development. Combine this with the fact that the valve actively blends water to a temperature that is within the typical growth range of legionella bacteria, and you have a very real possibility of an increased risk of bacterial proliferation in your water system.
These units can be invaluable in the safety of vulnerable users, however their potential to increase bacterial risk means it is important to ensure that their use is controlled.
So how do I know if I require one? The water system should be subjected to a scald risk assessment to identify areas that valves are required and areas that the scald risk can be controlled by alternative methods such as mixer taps or caution hot water notifications. This type of assessment will consider the type of user (staff, service user, patient etc), the vulnerability of that user, the environment in which the outlet is installed, and more to determine the requirement for the level of scald protection.
Once areas requiring TMVs have been identified, it is important to action this by either installation of required valves or potential removal of existing valves, replacing them with an alternative method of scald control.
If valves are installed, they must be subjected to a rigorous and routine servicing programme. This servicing programme should cover six main elements: removal of the TMV, stripping it down into constituent parts for descaling and disinfection; the replacement of worn or damaged O-rings to reduce the potential for leaks; lubrication of the piston, if required; reinstatement of the valve; temperature setting; and failsafe testing.
This servicing reduces the risk of biofilm development and bacterial growth, ensures ‘safe’ temperatures are dispensed from the outlet and that the valve will correctly shut off if there is a disruption in water pressure to the valve.
L EF
The team at HC Legionella Ltd are on hand if you require any support for TMV servicing or for scald risk assessments. M
FURTHER INFORMATION
www.hclegionella.co.uk

Written by the Legionella Control Association, this article explores the legal duties and practical steps required to manage Legionella risk in public and commercial buildings
In summer 2023, the Bibby Stockholm Barge hit the headlines for all the wrong reasons when traces of Legionella bacteria were found in the on-board water system. This was an embarrassment for the government at the time, but not entirely unexpected by “those in the know” given the size of the vessel and the low levels of occupancy (and hence, water use). Though no one contracted Legionnaires disease, the publicity was very damaging as these type of situations often are, but they can also sometimes result in prosecutions such as during 2024 when UK Health and Safety Executive (HSE) took two separate actions, one against Vincent Naughton Court sheltered housing accommodation in Birkenhead following discovery of the bacteria in their water and their failure to manage the risks of exposure, as well as a second against Amey Community Ltd who were the facility management company involved at HMP Lincoln when one of their inmates died from Legionnaires’ disease.
Legionnaires’ disease is a potentially fatal form of pneumonia, first identified in summer 1976 following an outbreak of an unknown infection at a convention of the American Legionnaires in Philadelphia. The causative bacteria was identified early the following year and since then, more than 60 species of the bacteria have been identified. These bacteria are widespread in nature so are often able to enter water systems at low levels (>10 per cent of water samples tested return a positive result for legionella bacteria), and presence of any of them in a water system could be indicative of a situation where there is a risk that it is not being adequately controlled. Exposure to this risk occurs when the water system is then able to create small droplets that could be inhaled by susceptible individuals. Correct management of these situations is therefore essential and there are legal implications if employers or businesses fail to manage these risks. E
COSHH requires the employer to: understand the risk of exposure to any hazardous substance
In most situations, there is an obligation on the employer to keep people safe and this stems from the Health & Safety at Work etc. Act (1974). This is further reinforced by supporting regulations that identify specific risks, and in this instance, as legionella is considered a hazardous substance, it falls under the Control of Substances Hazardous to Health (COSHH) Regulations (2002). Among other things, COSHH requires the employer to: understand the risk of exposure to any hazardous substance (including legionella); where a risk is identified, consider elimination, but if this is not possible, ensure suitable controls are put in place; and ensure that the identified controls are implemented and checked to ensure they are working correctly.
As legislation is sometimes considered “complicated”, UK HSE produce an “Approved Code of Practice” for legionella management (known as ACoP L8) that identifies what legislation applies and how to comply. The ACoP is further supported by a series of system specific technical guidance documents providing practical advice for systems known to be a likely legionella risk. These are known as the HSG274 parts 1-3 and they cover evaporative cooling systems (part 1), hot and
cold water systems (part 2) as well as many other types of industrial water systems (part 3).
ACoP L8 specifies the “high level” legal requirements of: identification of risk; creation of a suitable prevention or control scheme; implementation of the scheme including checks to manage effectiveness; and an appropriate management structure to ensure all tasks occur including a person in overall control of the scheme and an effective record keeping system to enable easy understanding of risk management.
In addition, within the ACoP, paragraph 59 identifies factors that can lead to bacterial growth, which in turn can provide a structure for control strategies by avoiding these situations.
To paraphrase the ACoP, attention should be given to: avoiding water temperatures between 20 °C and 45 °C as this is where legionellae are most likely to grow; avoiding water stagnation as this provides time (and location) for the bacteria to grow; avoiding the use of materials of construction that can act as a nutrient or environment where the bacteria could grow; and minimising (or containing) droplet creation (where possible) to avoid exposure. There should also be actions aimed at keeping water systems clean as any build ups can provide ideal nutrients and environment for growth; using an appropriate water treatment technique where necessary (chemical dosing, temperature maintenance, filtration etc) to actively reduce bacterial populations; and having action plans for if problems are identified.
The intention of the ACoP isn’t that all of the above can be applied in all situations, but rather

to identify controls that can reduce risk but if there are aspects that cannot be met, this might elevate the risk and greater attention should be given to alternative efforts.
The past 10 years have seen a seismic shift in how buildings and workplaces operate. Working from home, fewer staff, water saving efforts etc have all meant that systems that were perhaps installed when the building was built, may now not be aligned with current building use and risk management. If we compare the effect of all the above influences on water use today, we might find that we now have oversized tanks, pipework with no flow, temperatures that are no longer achieved, taps or showers that no longer used etc. Even if we have removed items that are no longer in use, have we left redundant pipework behind walls or under floors? This then leads to the question of whether our strategies of control have changed to reflect the way our building and water use has changed? The first step will always be to identify that there are systems that might present a risk (and almost all buildings will have them…) as this will trigger the need to manage this and follow the steps laid out in the ACoP (assess, control, manage etc).
You don’t have to tackle this alone, however. There are many organisations out there that can assist with this and an excellent first point of call would be to refer to the Legionella Control Association (LCA) which has ~400


Legionnaires’ disease is potentially fatal but is preventable with the correct, often simple measures
members who are legionella control specialists and have committed to comply with and be audited against the LCA Code of Conduct. This Code is highlighted in Paragraph 83 of ACoP and explains what standards a service user should expect. The Code itself has 28 requirements that must be followed in all cases, plus specific Service Delivery Standards for the eight key Legionella control service areas.
The need for consistent management procedures is emphasised and all audits focus on evidence that this is in place in all provided services. Where we find a member’s performance lacking, either at audit or as part of a complaint to us, they can face sanctions or even removal from the association unless improvements are made.
Legionnaires’ disease is potentially fatal but is preventable with the correct, often simple measures. Employers and those in control of premises have a legal duty to ensure risks are identified and controlled. It is not necessary for there to be a death or case of disease for a successful prosecution and these can result in hefty fines and custodial sentences. If your water system exposes individuals to risk of harm, you are committing an offence. M
www.legionellacontrol.org.uk











From 31 March, rules around workplace recycling changed, meaning that all workplaces must separate their waste before it is collected and this includes the NHS
The rules apply to all businesses, charities and public sector organisations, including offices; retail and wholesale; transport; hospitality; entertainment and sports venues; construction sites; and venues for temporary events like festivals and shows. They also apply to educational venues and healthcare places and care homes. While this is not a comprehensive list, it is likely that any workplace that employs more than 10 members of staff, will be in scope.
Micro firms with fewer than 10 full time employees have until 31 March 2027 to comply. In practice, the Simpler Recycling rules mean that workplaces must separate dry recyclable materials; food waste; and nonrecyclable waste (also called residual waste). Dry recyclable waste includes glass (e.g. drinks bottles and rinsed empty food jars); metal (e.g. drinks cans and rinsed empty food tins, empty aerosols, aluminium foil, aluminium food trays and tubes); plastic (e.g. rinsed empty food containers and bottles); and cardboard (e.g.
newspapers, envelopes, boxes and cardboard food packaging).
The rules apply to ‘domestic waste’, nonhazardous municipal waste. They do not apply to clinical waste.
Food waste must be collected separately, even if the workplace does not serve food or have a kitchen. This could include things like food leftovers, including from customer or staff meals; banana skins and apple cores; coffee grounds and tea bags; and waste from food preparation, such as onion skins or potato peel. So either workplaces need to have separate bins for each type of waste, or separate the waste before collection.
Workplaces can decide on the size of containers and frequency of collections based on the volume of waste produced.
If the workplace produces garden waste, it must be arranged for it to be recycled or composted if it delivers the best environmental outcome. E
Waste prevention not only reduces the environmental impact but also saves valuable resources
F Organisations should discuss the requirements with their waste collector and arrange separate dry recycling, food waste and non-recyclable waste collection. If your current waste collector does not offer the full range of collection services, you will need to arrange these services from other providers.
Workplaces have a legal duty to ensure waste disposal is safe, secure and legal and to also take all reasonable steps to keep waste to a minimum.
Waste Management contractors have a legal obligation to make sure any separately collected dry recyclables are sent for recycling and that any non-recyclable waste is correctly managed. Any workplace that does not comply with these requirements is at risk of receiving a compliance notice from the Environment Agency. It is an offence to not comply with a compliance notice and enforcement action may be taken by the Environment Agency.
As per the waste hierarchy, organisations are reminded that the most effective approach to waste management is to prevent waste from being created in the first place. Waste prevention not only reduces the environmental impact but also saves valuable resources and can lead to significant cost savings. In a public sector context, this means assessing procurement practices, reducing unnecessary packaging, and encouraging sustainable behaviours across staff and service users. If waste does occur, the next best option is to prepare it for reuse – extending the life of materials and equipment wherever possible. This could include reusing office supplies, donating surplus items, or implementing internal reuse schemes. Recycling should then be considered, ensuring materials like paper, plastics, metals, and food waste are properly sorted and processed. Recovery can then be considered, for example energy recovery from surplus waste. Disposal via landfill should always be the last

resort, given its long-term environmental consequences and associated costs. By following the waste hierarchy, public sector organisations can make informed, responsible decisions that align with both regulatory requirements and wider environmental goals. Recycling provides many significant benefits, both for the environment and within the workplace. Environmentally, it plays a vital role in reducing greenhouse gas emissions, conserving natural resources, and protecting ecosystems. According to RecycleNow, current UK recycling efforts are estimated to save more than 10–15 million tonnes of CO2 each year – an important contribution to the country’s climate goals. For public sector organisations, which are often bound by government sustainability targets and net zero commitments, recycling is not just a legal obligation but a strategic priority. Many councils, NHS trusts, schools, and other government bodies have set out clear environmental objectives, and effective recycling is a key component in achieving these. By actively managing and reducing waste, public sector organisations also set a positive example for the communities they serve. The NHS itself has its own net zero commitments, and recycling is a key contributing factor.
Beyond environmental impact, waste reduction and recycling can improve operational efficiency. When waste is prevented or materials are reused, it can streamline

As your organisation starts to recycle more, the amount of general waste you produce should also decrease
internal processes, reduce the need for frequent collections, and limit over-reliance on costly disposal methods. In many cases, recycling services are more cost-effective than general waste disposal, meaning organisations can realise financial savings alongside environmental gains.
Ultimately, embedding a culture of recycling and waste minimisation supports both longterm sustainability and smarter resource management across the public sector.
WRAP has guidance on its website aimed at different types of workplaces. This has specific guidelines for health and social care.
Communication
It is important to communicate the changes to your workforce – an email to all staff, posters in key areas and clearly marked bins are all simple and efficient steps to make your new regime effective.
Waste containers should be large enough to hold the waste and recycling between emptying, but not too large that they are difficult to move. They should also have lids or
covers to keep materials dry and to stop waste escaping. Containers should be labelled clearly. Remember, there is always room for improvement. As your organisation starts to recycle more, the amount of general waste you produce should also decrease. This means you should be able to reduce your number of general waste bins, or have them emptied less often, which in turn could save you money.
The introduction of Simpler Recycling rules represents an important shift in how waste is managed across all workplaces, including public sector organisations. From healthcare facilities and schools to council offices and emergency services, the requirement to separate dry recyclables, food waste, and residual waste supports the sector’s wider environmental goals, including net zero commitments. Public bodies have a responsibility not only to comply with these legal obligations but also to lead by example in sustainable waste management. By engaging with waste contractors, reviewing internal processes, and using sector-specific resources, public sector organisations can ensure smooth compliance. In doing so, they help reduce environmental impact, improve operational efficiency, and demonstrate their role as sustainability leaders in their communities. M
Simpler Recycling guidance can be found here.




© 2025 Public Sector Information Limited. No part of this publication can be reproduced, stored in a retrieval system or transmitted in any form or by any other means (electronic, mechanical, photocopying, recording or otherwise) without the prior written permission of the publisher. Whilst every care has been taken to ensure the accuracy of the editorial content the publisher cannot be held responsible for errors or omissions. The views expressed are not necessarily

Health Business is a member of the Independent Press Standards Organisation (which regulates the UK’s magazine and newspaper industry). We abide by the Editors’ Code of Practice and are committed to upholding the highest standards of journalism. If you think that we have not met those standards and want to make a complaint please contact Polly Jones or Angela Pisanu on 0208 532 0055. If we are unable to resolve your complaint, or if you would like more information about IPSO or the Editors’ Code, contact IPSO on 0300 123 2220 or visit www.ipso.co.uk




Prevent everyday wear and tear with Yeoman Shield’s extensive range of easy-clean, wall and door protection.
Our attractive, maintenance free, hygienic products protect healthcare environments from costly impact damage, making repainting and repair a thing of the past.
Blending with decors, and available in primary dementia-friendly colours, our designs can include signage, to promote the well-being of patients and aid wayfinding.
For more information call 0113 279 5854 or email info@yeomanshield.com
