



Providence St. Vincent | 1875-2025




Providence St. Vincent | 1875-2025
On July 19, 1875, “Portland’s first true hospital was opened with appropriate dedication ceremonies,” penned writer Ellis Lucia in “Cornerstone.” The book, published in 1975 to commemorate St. Vincent Hospital and Medical Center’s 100th anniversary, pays tribute to the five remarkable Sisters of Providence who traveled to this “rawboned lumbering seaport” and built Oregon’s first permanent hospital through their sheer force of will and devotion.
“The entire town was fully aware of the cornerstone of progress that this new institution represented,” wrote Lucia, “the beginning of a new age for Oregon and the Pacific Northwest.”
A new age, indeed. What started as a small hospital on Northwest 12th and Marshall streets in Portland has matured into a statewide health care organization, now numbering eight hospitals, a health insurance organization, a medical group, research and education programs, long-term and assisted-living facilities, and a

broad network of services provided by nearly 20,000 caregivers. All this, from five women with a Mission.
While much has changed, the sisters’ Mission of care and service remains vividly alive in the people of Providence today, and in our promise to answer the call: “Know me, care for me, ease my way.”
Today, we celebrate the 150th anniversary of Providence St. Vincent Medical Center. As we reflected on the rich history of this foundational institution, which has meant so much to us, we knew that we wanted to commemorate this milestone by preserving and sharing that history. So, we’re picking up the story of St. Vincent where “Cornerstone” left off, 50 years ago.
We hope you enjoy this collected history, as told by people who lived it and helped shape it. We offer these reflections in warm recognition of those who have gone before us, and as inspiration for those who follow.
With deep gratitude,
LYNDA WERNER
FORMER MARKETING AND COMMUNICATIONS DIRECTOR
GREG VAN PELT
FORMER HOSPITAL ADMINISTRATOR
DON VOLLUM
MEDICAL FOUNDATION TRUSTEE AND FORMER PRESIDENT, COUNCIL OF TRUSTEES




At Providence St. Vincent, we have a long tradition of opening gatherings with a reflection.
These reflections – whether they are memories, stories, quotes or prayers –remind us of who we are, why we are here, and what we aspire to be.
In the pages that follow, we continue that tradition as we reflect on 150 years of serving Oregon.

When Mother Joseph arrived in Washington Territory from Montreal in 1856, she encountered a strange new world of physical hardships, cultural and religious diversity, and rapid change. There were no hospitals, few schools, and little in the way of charitable services. Equipped with simple tools, enormous gifts for creating and building, and deep faith in Divine Providence, she and her four companion Sisters of Providence stepped into the breach to fill these unmet needs.

Within four months of settling in Fort Vancouver, they had constructed a school and orphanage, the foundation for what became Providence Academy. Barely a year later, in a small, converted building originally intended as an on-site laundry and bakery, they opened St. Joseph Hospital, the first permanent hospital in the Pacific Northwest.
Soon, the sisters were besieged with requests to bring their good works to other communities. The archbishop of the Diocese of Oregon City tried for years to persuade them to open a hospital in Portland, but for such an endeavor, they knew they would need a great deal of support from the community.

That support finally came on July 19, 1874, when the St. Vincent de Paul Society offered a block of land on Northwest 12th Avenue between Marshall and Northrup streets, plus a generous gift of $1,000 for construction costs. The sisters accepted this offer and got to work, raising thousands more in donations for what was to be called St. Vincent Hospital, after its benefactor.
The enterprising Mother Joseph drew up the architectural plans and oversaw construction of the hospital herself. Known as a perfectionist, she handselected the bricks, lumber and other materials for St. Vincent and other hospitals to follow, checking them carefully for quality. According to one story, she once tore down and reconstructed an entire chimney herself when the masonry didn’t meet her standards. This was a woman who insisted on excellence in every detail. And in this way, brick by brick, she laid the foundation not only for Oregon’s first hospital, but for Providence Health & Services today.

St. Vincent’s first patient, George Allen, was admitted on June 24, 1875, before the hospital had even opened. Young Mr. Allen was desperately ill and, while the building had no place yet to put a patient, the sisters took him in and nursed him back to health.
On July 19, 1875 – the traditional feast day of St. Vincent de Paul – the hospital was dedicated and officially opened. The sisters had built the three-story, wood-frame building, with space for 75 beds, in a year. The staff consisted of five sisters and a single general practitioner, Dr. Alfred Kinney.
In its first year, St. Vincent admitted 320 patients, treating everything from gunshot wounds and fractures to typhoid and toothaches. By the second year, it had accepted 103 charity patients, a figure “that would rise steadily as word spread of the kind and caring ways of the sisters,” wrote Ellis Lucia in his book “Cornerstone.” “This was far more than a hospital; it was a Mission project.”


As the years passed, Lucia continued, “The hospital seemed to be moving ahead amazingly well, and becoming, as intended, a cornerstone institution for both Portland and all of Oregon.” However, “within a decade, the rapidly growing seaport and manufacturing center was pushing to (the hospital’s) very doorsteps.” As the town grew, it became clear to the sisters that the hospital needed more room.
Mother Joseph began her tenacious fundraising again – even soliciting donations from California gold miners – and the sisters were able to purchase a five-acre tract near Northwest Westover Road. Soon, Mother Joseph was drawing up plans and overseeing construction of a new hospital in Portland’s West Hills.

The new hospital opened on Northwest Westover Road just five days short of the original hospital’s 20th anniversary. Widely recognized as a model institution for the region and the nation, it incorporated such advancements as electric lighting, an electric elevator for transporting patients in their beds, an early telephone system with bells and speaking tubes, and a spacious operating room. For years, doctors, builders and designers “would travel to St. Vincent to gain ideas and knowledge from what had been developed in this hospital of the future,” wrote Lucia. “The sisters were once again pioneering.”
At the dedication of the 275-bed hospital, Dr. William Jones said:
“A great hospital, like a great university, is something more than a collection of buildings and their furniture. … It must have a history, traditions, achievements behind it, and a promising future before it. To thousands of people, St. Vincent Hospital is something more than a name. In thousands of homes, it is a household word.”
For the next 70 years, wrote Lucia, “through the raging influenza epidemics of post-World War I … the shipyard times of the two great wars … the Great Depression years … the terror of
the wild Columbus Day Storm of 1962 … and the day-by-day human dramas and challenges … the hillside hospital grew steadily to keep abreast with the times and the latest medical techniques.”
During those years, he continued, “There were many firsts, starting with the nursing school (one of Oregon’s first) and the school of anesthesia, extending into pioneering research and training programs to Oregon’s first coronary intensive care and heart catheterization units, open heart surgery, and the world’s first cardiac telemetry station. The hospital became the first locally to be standardized by the American College of Surgeons, which was the precursor to the Joint Commission on Accreditation of Hospitals; and bearing out forecasts, developed into one of the foremost medical institutions of the West and the nation.”
By the early 1960s, however, the hospital was again outgrowing its space. After many studies, the Sisters of Providence selected the rapidly growing Beaverton area as the site for St. Vincent’s new home. Soon, under the leadership of Sister Rita Ferschweiler, SP, the hospital’s administrator, they were building again.




Four years shy of its 100th anniversary, St. Vincent Hospital and Medical Center opened in its new and current location on Southwest Barnes Road, overlooking the Tualatin Valley. By this time, the hospital staff had grown from those original five sisters and one physician to 475 doctors, 365 nurses, more than 1,000 other caregivers and 200 volunteers.
Through their continued involvement, their leadership and their daily example, the sisters instilled their values of compassion, dignity, justice, excellence and integrity in everyone who followed. For 150 years, St. Vincent Hospital – now known as Providence St. Vincent Medical Center – has continued to build on Mother Joseph’s example, growing with the community, for the community, and with the generous support of the community. As one of the sisters put it many years ago:
“If today our hospital is filled with patients … if today we enjoy the esteem of all Portland and its environs … if all classes of people come here to be cured … we are amply rewarded by the help we can give body and soul.”


The cornerstone of the hospital’s former building on Northwest Westover Road stands at the entrance of today’s Providence St Vincent Medical Center. In Catholic tradition, JMJ stands for Jesus, Mary and Joseph.


As the sisters had anticipated, the population around the new St. Vincent Hospital and Medical Center boomed. The recently opened Vista Ridge Tunnels and soon-to-becompleted Oregon Highway 217 opened up easy access to the area, making it an attractive place to live and work. With bustling campuses nearby, Tektronix and Intel, and later Nike and Columbia Sportswear, became major catalysts for growth.
At the same time, the demand for health care was growing exponentially in the wake of the introduction of Medicare and Medicaid in 1965. And another boom was occurring in medical technology, bringing computed tomography (CT), magnetic resonance imaging (MRI) and other advancements to patient care. All of these trends meant that the new hospital on Southwest Barnes Road faced exceptionally high demand from its very first days. The sisters were ready for it.
On opening day, Jan. 31, 1971, 82 patients were moved from the old hospital on Northwest Westover Road and settled into their new rooms in just over four hours. At the end of the year, the sisters hired Tom Underriner, a leader well known to Providence, to succeed Sister Rita Ferschweiler, SP, as administrator, marking the first time that St. Vincent had a layperson at its helm.




One of Tom’s first hires was facility manager Ken Zinsli, who laid out the footprint for the hospital’s services. Designed to emulate airport traffic flow, the site placed high-traffic and acute care services at the east end of the hospital, flowing toward moreintensive care services to the west, with support services expanding northward as needed. That footprint still serves the medical center well today.
The rest of the decade focused on implementing a 10-year plan developed collaboratively with the St. Vincent Hospital Medical Foundation, a group of local citizens who had taken an interest in the hospital’s future. The plan envisioned – and helped realize – a combined hospital and health sciences campus that included on-site medical offices, a family medical care unit, urgent care, and outpatient radiology, pharmacy and laboratory services. Endowed chairs in medicine and surgery also were established to train new physicians and continue the flow of new ideas to the St. Vincent health care community.
Throughout this decade of new beginnings, the sisters continued to serve, overseeing patient care services, providing nursing care, greeting visitors at the information desk, offering comfort through pastoral care, and guiding the hospital steadily into the future.
JAN. 31: St. Vincent Hospital and Medical Center opens at its new location on Southwest Barnes Road. The nine-story, 403-bed hospital provides modern and expansive facilities. It replaces the old hospital on Northwest Westover Road, built in 1895.

The Isidor C. Brill Chair of Medicine is created, the first endowed professorship in a private hospital in the Pacific Northwest. Dr. Brill served on the St. Vincent staff for 59 years, providing care and educating medical students. Kenneth Melvin, M.D. (below), is named the first chair, and is later succeeded by Steven Freer, M.D.

The Maybelle Clark Macdonald Cancer Center is established at St. Vincent, laying the foundation for what will become Providence Cancer Institute.
The Sommer Memorial Chair of Surgery is established. Ernst A. Sommer, M.D., was a prominent surgeon and former chief of staff at the hospital. Along with the Brill Chair of Medicine, the endowed professorship demonstrates St. Vincent’s commitment to training physicians.
St. Vincent celebrates a century of providing health care in Portland. Events are held throughout the year to honor the centennial of Oregon’s first permanent hospital.
JULY 3: St. Vincent works with Centro Cultural, Sisters of Providence Seattle and other organizations to open the Virginia Garcia Memorial Health Center in Washington County. The clinic provides care to migrant and seasonal farmworkers.

St. Vincent’s campus starts to grow, with the completion of Medical Office Building #1. To meet growing demands for space, Medical Office Buildings #2 and #3 open in 1980 and 1986.
The St. Vincent Home Care Department begins service, allowing patients to remain at home while receiving care that otherwise would require hospitalization. Within the first five years, 26,750 home visits are made to 1,535 patients.
St. Vincent assumes management of Newberg Community Hospital, and later signs a similar contract with Seaside General Hospital. Under these arrangements, St. Vincent assists smaller community hospitals by sharing its resources.
KATHY JOHNSON, RN NURSING
“It’s about more than medicines and charting. It’s about human life.”
“Everywhere I’ve been at Providence, the day always starts with a prayer or a reflection or some deeper thought that puts you in touch with what you’re all about, here today. It’s about more than medicines and charting. It’s about human life. And I think that’s been a very, very important part of the culture.
“In nursing leadership, one of the most important things we did was to hire the very best nursing staff and ensure that every patient had a registered nurse at their bedside. Every single RN was vetted deeply for their clinical and overall knowledge and their communication skills, because this excellence is the lifeline for every patient.
“When we first received Magnet nursing designation in 2000, we were one of only 23 hospitals in the nation, and the only medical center in Oregon, to achieve that status. I was so pleased that our nurses’ everyday professionalism, dedication and compassionate care were deemed by their peers to be at the top tier in the country.
“The St. Vincent administrative team really valued nursing, trusting that we would do the right thing for the patient. So, nurses were able to make their own governance decisions and participate in rigorous nursing research and education. Earning Magnet designation was a demanding test. And St. Vincent nurses did it proudly.”
Kathy’s St. Vincent memories go back to 1962, when she started as a nursing assistant at the old Westover Road hospital. She was St. Vincent’s assistant administrator for nursing and patient care from 1992 to 2002, and went on to serve as chief nursing officer for Providence in Oregon until her retirement in 2008.


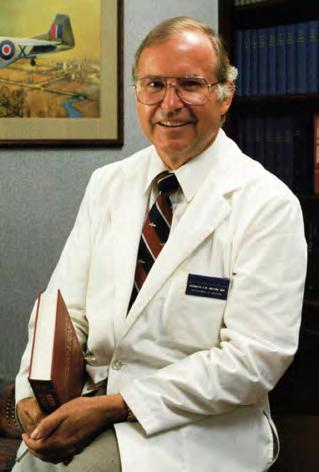
KENNETH MELVIN, M.D. MEDICAL EDUCATION
“There is no question that this is a prize.”
“In 1972, I was happily engaged in endocrine practice and research in Boston when my name came into consideration for the Brill Chair of Medicine, which had recently been endowed at St. Vincent Hospital in a place called Portland, Oregon. Despite being urged to remain in Boston on the faculty at Harvard, I decided to visit.
“It was a May day with brilliant sunshine and the rhododendrons in full bloom when I visited the hospital, which had been open only a few months. The environs reminded me of my native New Zealand, so things were already falling into place.
“What impressed me immediately was the ambiance of the building – and the people. It is the people I continue to admire, who make St. Vincent’s, St. Vincent’s. As an ex-fighter pilot in the Air Force, I had learned what it’s like to belong to a unit; the esprit de corps that goes with being part of a team with a sense of ownership and pride and competitiveness. I saw that camaraderie in the days I was being interviewed by the medical staff.
“I’ve been all over the world, seen it all and practiced in many different settings, and there is no question that this is a prize. St. Vincent will always remain in my mind as that wonderful example of how medicine should be practiced.”
A nationally recognized endocrinologist, Dr. Melvin was the hospital’s first Isidor C. Brill Chair of Medicine. The gifted teacher played a significant role in the development of the internal medicine residency and the hospital-based internal medicine faculty practice, in continuing education, and in the placement of many physicians in leadership roles.
DEB TUKE BAHLMAN, RN NURSING
“I was immediately greeted by a very cheerful nun, who practically tackled me when I said I was looking for a job.”
“In July 1974, at the age of 19, I arrived in Portland from Cincinnati and immediately fell in love with the area. I decided to stay, so I needed a job. Since my only work experience was as a nurse’s aide, I went to a nearby hospital, where I was handed an application and sent on my way.
“My next stop was at a hospital that had just recently opened, way out on Highway 26. I walked through the door and was immediately greeted by a very cheerful nun, in her customary habit, who practically tackled me when I said I was looking for a job. She sat me down and we got to know each other. She was interested in hearing my story.
“While there were no positions open for nurse’s aides, she told me, they did have an orderly position that I looked capable of doing. A couple of days later, I had my first job with St. Vincent, as an orderly on the orthopedic unit.
“For the next 43 years, I made Providence my home, working in a variety of roles and making a lifetime of wonderful friends and memories. I often wonder what might have happened if that sister hadn’t given me such a warm welcome and such an incredible opportunity.”
Deb worked full time at St. Vincent while attending nursing school. She then moved into nursing in the critical care, emergency and laser research departments before earning a master’s degree in applied information management. She culminated her career in information services, helping 42 hospitals transition to the Epic electronic medical record system before she retired in 2017.


KAREN NEILSON (ZIVIN), RN NURSING
“The standard for excellence is set the minute you walk in the door.”
“When I started at St. Vincent on Barnes Road, there was only the main hospital building, with none of the adjacent structures. And we all parked outside. I remember looking out the window in the middle of an ice storm, watching nurses trying to pick ice off their cars with their keys so they could go home.
“We had a partnership among primary care doctors, specialists, nurses, rehab, social services and more. We all worked together for the benefit of our patients. It was interesting, often fun and very rewarding.
“It’s incredibly important that nurses understand they do a really important job. It requires scientific knowledge and compassion, and as Florence Nightingale noted, nurses must know what and how to observe concerning their patients.


“To nurses coming in, I would say, make this job what you want it to be.
A Magnet hospital provides additional opportunities to do that; to put your expertise to work and be involved in improvements.
“When I walked into St. Vincent recently, I was immediately aware of how beautiful it is. That’s a superficial thing, really – except the standard for excellence is set the minute you walk in the door. And then, when you get into a patient’s room, you can expect the same kind of caring.”
Karen began her 34-year St. Vincent career in 1976 as a staff nurse, later becoming a charge nurse and unit manager. She served as a leadership coach and did special projects, such as a wall display honoring nurses, from 2004 until her retirement in 2010.

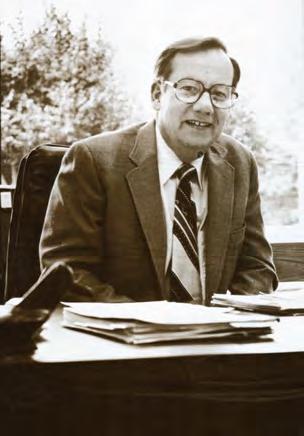
GREG VAN PELT HOSPITAL ADMINISTRATION
“To spend my entire career as a ‘Person of Providence’ changed my life.”
“I had the privilege of joining St. Vincent in 1975 as an administrative fellow, one week after my wedding to Joan. Over the next 38 years, I learned from the visionary leadership of Tom Underriner, John Lee and John Koster; from the sisters’ humble yet disciplined commitment to compassion and service; from foundation members who took us under their wings; from volunteers who taught us to give back; from physicians and nurses who set professional examples; and from countless caregivers who shared a common commitment to excellence.
“When our son, Andy, was born eight weeks prematurely at OHSU (St. Vincent didn’t have an NICU then), the first person to meet us there was Sister Yvonne LeBlanc, St. Vincent’s pastoral services director. From that moment, we knew
that the sisters and our colleagues would play an intimate part in our lives.
“Today, both Andy and our daughter, Emily –a nurse at Providence St. Vincent – have chosen health care as their vocation, and two of our granddaughters are studying nursing. We’ve all been touched by the remarkable spirit of this place and these people.
“To spend my entire career as a ‘Person of Providence’ changed my life, just as Providence St. Vincent has changed the lives of so many over the last 150 years. Our opportunity, and responsibility, is to sustain that spirit for the next 150 years.”
Over the course of 38 years with Providence, Greg served in many capacities, including director of planning, associate administrator and administrator/chief executive at Providence St. Vincent. Greg completed his career with Providence as chief executive, Oregon region, retiring in 2013.

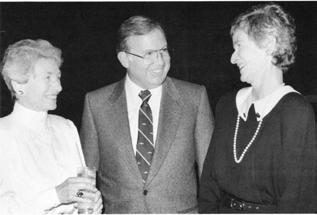
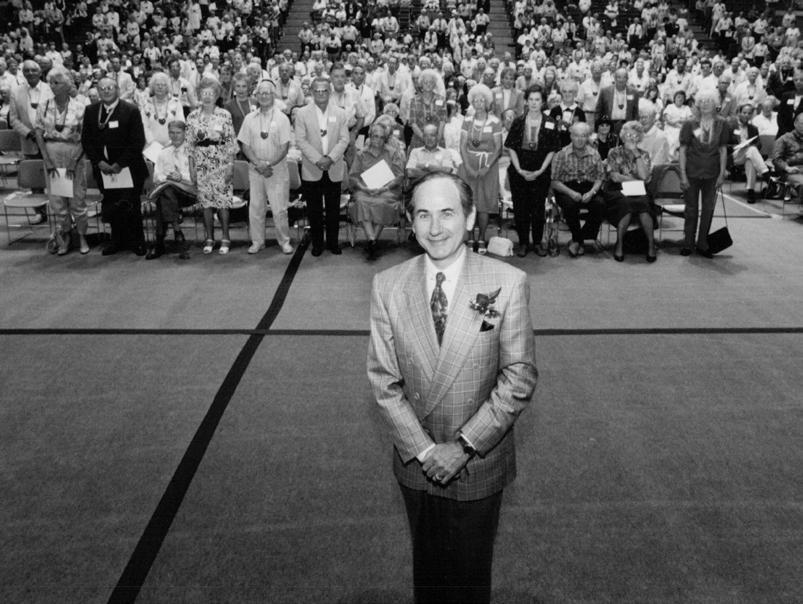
Left: As hospital administrator, Greg (in front) takes a break with St. Vincent “People of Providence.” Below: As chief executive of the Oregon region, Greg dishes out service with a smile at a barbecue for employees.

“Now … there might be less chance that a case like Virginia’s will be repeated.”
In 1975, 6-year-old Virginia Garcia was traveling from Texas to Oregon with her parents, migrant farmworkers who were following the annual strawberry harvest. Along the way, Virginia cut her foot, and by the time the family arrived in Washington County, the wound was infected. Her parents sought help in a local hospital, but were denied care due to lack of insurance. By the time they made their way to St. Vincent, Virginia had developed an acute blood infection. She died at the hospital.
Virginia’s tragic and preventable death raised critical questions about how to ensure accessible and culturally appropriate care for migrant and seasonal farmworkers. A countywide proposal process began, but it was slow, complex and cumbersome. Fearing that migrant health care would be lost for another year, St. Vincent administrator Tom Underriner took action.
Teaming up with Centro Cultural, a Cornelius nonprofit serving the Latino community, St. Vincent staffers helped renovate a large garage, brought in medical equipment, hired bilingual caregivers, and opened the Virginia Garcia Memorial Health Center in one month.
As the farming season waned, questions arose about whether the clinic was sustainable. But the community rallied behind it. As Arturo Cortez, then-executive director of Centro Cultural, said, “Now, with the services we have at the center, there might be less chance that a case like Virginia’s will be repeated.”



Today, the Virginia Garcia Memorial Health Center operates under its own governance. Each year, it provides care for more than 52,000 patients who speak 62 languages. Care is provided through seven primary care clinics, six dental clinics, five schoolbased health centers and three mobile clinics. In 2025, the center celebrates its 50th anniversary.

BARBARA BLAKELEY VOLUNTEER SERVICES AND MISSION EFFECTIVENESS
“That’s what I ... want people to know from me, is how much I loved it here.”
“I started volunteering at St. Vincent in 1975 and was hired as director of volunteers in 1977. I loved the volunteers. They were just wonderful, giving, thoughtful, generous people. It was such a privilege to be connected to them.
“From that role, I moved to human resources, where we developed the service excellence and spirit programs. Those programs were inspired by a passage from ‘Cornerstone,’ by Ellis Lucia, describing the early days of the sisters in the first St. Vincent Hospital:
‘Mother Godfrey said, “Be polite. Give orders as you would like them given you. Avoid speaking of faults. Treat all gently and compassionately. Be simple and truthful and kind.” And so, the Mission was and is today focused not only on the quality of care, but on the spirit with which we serve. The spirit of St. Vincent.’
“Service excellence is how we lived this spirit.
“I remember a time when my husband and I both got very sick, so I drove us to the emergency room. The triage nurse asked me, ‘How did you get here?’ And I said, ‘I drove.’ She said, ‘Weren’t you frightened?’ And I said, ‘No. I was coming home.’
“That’s what I primarily want people to know from me, is how much I loved it here.”
Barbara has been a part of St. Vincent for 50 years, serving as director of volunteer services and director of Mission effectiveness and continuing her service today as a foundation trustee. The St. Vincent Mission Effectiveness Program calls on all people of St. Vincent to be “caretakers of (the sisters’) tradition of love” (Crescent, June 1987).




JEFFREY SWANSON, M.D. CARDIOTHORACIC SURGERY
“I really think there’s a sense of divinity in it.”

“I started my internship in general surgery at St. Vincent in 1977. I chose the hospital partly because I knew that Dr. Albert Starr was here – he was a name internationally, and I had learned about him during cardiac surgery classes and rotations that I did in France. Over time, it dawned on me that heart surgery was my true love.
“Besides training with excellent surgeons, I had the very good fortune of being affiliated with the medical team, including cardiologists Henry Garrison and Bob Gibson, who were instrumental in building the heart program. I also had the opportunity to work with, among others, Toshio Inahara, a pioneering vascular surgeon, and Dee Wallo, a real firecracker of a nursing leader.
“I operated on many of the people who, in those early years, meant a lot to me. Over the course of 33 years, I operated on more than 10,000 heart patients.
“The sense of compassionate community here was very real. It still is a community of compassionate caregivers all working toward a shared goal. I really think there’s a sense of divinity in it.
“And within that culture, there was also the excellence of the heart surgery program. As Vince Lombardi was fond of saying, ‘Perfection is not attainable, but if we chase perfection, we can catch excellence.’ We truly had a team focused on achieving excellence.”
Dr. Swanson served as a cardiothoracic surgeon on the medical staff from 1987 until his retirement in 2020. With an endorsement from Dr. Starr, he secured a fellowship in Paris with renowned surgeon Dr. Alain Carpentier, known as the father of modern mitral valve repair.

MICHELLE HAUN-HOOD, RN
NURSING AND QUALITY MANAGEMENT
“It was exciting to be back where I started and to see the great leadership still in place.”

“I started in health care at St. Vincent in 1977. In nursing school, I had done my senior project at the pretty new hospital with the wonderful folks in cardiac care. So as a new graduate, I was very fortunate to get a job in the open-heart recovery room. The friendliness of the leadership was amazing.
“For a while, I lived in the apartments next to St. Vincent – my grandmother was friends with one of the sisters at the hospital, who got me a great deal. Every night I’d walk across the parking lot and be so excited and happy to work at such a great hospital.
“Eventually, I moved into trauma care and was recruited elsewhere. Although I was sad that St. Vincent didn’t get to be a trauma center, they always continued their support and advocacy for trauma care. My work with St. Vincent leaders Greg Van Pelt and Paula Derr helped to develop the great trauma system that we have in Oregon today.
“After working as the trauma coordinator for the state, I was invited to return to Providence St. Vincent as the quality director. I was excited to be back where I started, and to see the great leadership still in place.
“I’ll always be grateful to the Providence people for their care, leadership and kindness.”
Michelle joined St. Vincent as a new nursing graduate. Today, she serves as regional director of operations for Providence Oregon Q uality Management.

KAREN FOLEY OCCUPATIONAL THERAPY
“No wonder you love this place.”

“In 1978, when I was hired as an occupational therapist at St. Vincent Hospital, the sisters were still providing direct care as nurses and social workers. I was so impressed with their influence, their active involvement, and the way they modeled the behaviors and values they expected to see.
“On my first day of work, the hospital administrator, Tom Underriner, noticed a new person sitting in the cafeteria and sat down to welcome me – a day I will never forget.
“On another day, my father, who was a minister, came to visit me at work. As we walked out of the hospital, pausing to ‘feel’ the moment, he turned to me and said, ‘No wonder you love this place. It’s a community of love, giving and healing.’
“During my 38 years with Providence, there were so many times when I felt the passion and experienced the love that the sisters spread all around them. They grew with the times, yet never wavered in their Mission, their values, or their commitment to the healing work – physical, mental and spiritual – that needed to be done. Those years are deeply ingrained in my heart.”
St. Vincent had two occupational therapists when Karen joined the team. As the OT and rehabilitation programs grew, she took on leadership roles within the hospital and the region, culminating her career as executive director of Providence Orthopedic Institute, Oregon. Karen was part of the team that created the Providence Sports Care Center, a partnership with the Portland Timbers and Portland Thorns.

DOLORES FOGLIO, RN EMERGENCY NURSING AND LEADERSHIP
“That culture came naturally from the example of the sisters and rubbed off on everyone around them.”
“Alice Denford was a volunteer who worked primarily in the emergency department for more than 30 years. She was there every single day and would not go home until the last family member was out of the lobby. Her main concern was always: What’s best for the patient and family? The goal, she’d tell me, was for each person to go out the door saying, ‘I’m sorry this happened, but I’m sure glad I came here.’

“Alice was always sticking a piece of licorice in your pocket in case you missed lunch. And she’d say, ‘Hey, kid. How are we doing?’ She was an amazing presence who made our lives easier and richer. Alice was a demonstration of what I think Emilie Gamelin, the founder of the Sisters of Providence, would have been like if she were still here today. She always reminded us of the importance of equity, justice and compassion.
“The culture at St. Vincent made a difference for those of us who stayed 30, 40 or 50 years. Many people still stay because of the culture and Mission. I think that culture came naturally from the example of the sisters and rubbed off on everyone around them. For me, it had a huge impact on how I looked at my life, how I practiced my work, and how I interacted with people.”
Dolores began her career in 1978 as a nurse in the St. Vincent emergency department, and eventually became its administrative director, leading it through a major expansion in the early ’90s. After earning a nurse practitioner degree, she practiced internal medicine at Providence Plaza and worked in immediate care at Providence Willamette Falls Medical Center. She retired from Providence in 2020.


DAVID CRAIG, M.D. EMERGENCY MEDICINE
“At first, we were seen as cowboys. Now we consult for the medical staff on almost any medical emergency.”

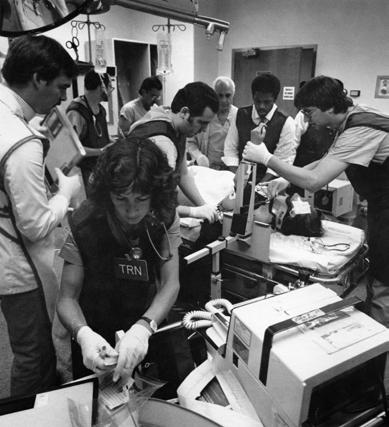
“It may come as a surprise to my colleagues that I was not around 150 years ago. But I was around 50 years ago, in medical school, when the specialty of emergency medicine was unknown. At that time, the medical staff covered the emergency department on a rotating basis. So, if you came in on Tuesday with a heart attack, it might be an ophthalmologist or dermatologist who’d come down before calling for a heart specialist.
“People eventually realized there was a need for specially trained people to run emergency departments. St. Vincent had the foresight to see this, and in 1979, three of us came on as the first emergency medicine residency-trained physicians in Portland.
“We had the opportunity to be on the forefront of emergency medicine. At first, we were seen as cowboys. Now we consult for the medical staff on almost any medical emergency. We’ve been here through the early days of the AIDS and COVID pandemics, and through the advent of CT scans and everyday drugs like ibuprofen. Some of the most satisfying days are when you can tell a family, ‘Good news. Everything’s OK.’
“I had the privilege of training under Peter Rosen in Denver, who is considered the grandfather of emergency medicine. To paraphrase him, ‘I had meaning in what I did. I worked in an emergency department.’”
Dr. Craig was one of Portland’s first board-certified emergency medicine doctors and a founding partner of Oregon Emergency Physicians. OEP started at St. Vincent in 1979 and now provides care in three Portland-area Providence emergency departments. The independent group teams with Providence caregivers and is very closely aligned with the medical staff. Dr. Craig retired in 2015.





The 1980s were years of explosive growth for St. Vincent, so it was fitting that the decade began with a blast. On May 18, 1980, Washington’s Mount St. Helens erupted with spectacular fury. Weeks later it blew again, this time spewing windborne clouds of ash toward Portland. Fine, gray silt coated the city, and also infiltrated St. Vincent’s air intake systems. Thinking fast, facility managers redeployed insulation, intended for a construction project, to replace clogged air filters, keeping patients and caregivers breathing easily.
As the decade progressed, the mountain settled down, but the winds of change continued to blow. Hospitals and physicians, who had traditionally operated independently of each other, began forming new relationships focused on improving quality and accountability. Providence Medical Group and Providence Health Plan were two outgrowths of these new arrangements.
Outside the hospital walls, St. Vincent met growing demand for convenient outpatient care by opening community-based clinics. These provided primary care, urgent care and diagnostic services in Hillsboro, Lake Oswego and Hillsdale. A fourth clinic opened in Tigard in 1991.
Within the hospital, programs and clinical service lines continued to align their services, evolving naturally into comprehensive institutes. Cardiac services, the largest of these programs, became the first to distinguish itself as an institute. Under the leadership of Albert Starr, M.D., The Heart Institute at St. Vincent was soon performing more than 1,000 cardiac bypass surgeries each year, and worldclass physicians were gravitating to the hospital to practice at this leading institute.
Other centers of excellence followed, including the Critical Care Center and the Oregon Spine Center. As more patients traveled from farther away to receive specialized care at St. Vincent, the hospital opened new guest housing to enable families to stay close to their loved ones. A new chapel provided peace and solace for patients, families and caregivers. And new medical ethics and hospice steering committees formed to help families and caregivers grapple with the sensitive issues that arose around patients facing complex medical and end-of-life needs.
In the years ahead, the times kept changing, and St. Vincent stepped up to meet them, both anticipating and responding to the needs of its community.
1981
The St. Vincent Sleep and Breathing Study Clinic opens. It is the first clinic of its kind in the Pacific Northwest.
1984
St. Vincent and Providence Portland develop the Physician InterHospital Health Plan, a new health maintenance organization (HMO). Later known as the Good Health Plan of Oregon, it is the first HMO sponsored by the Sisters of Providence and lays the foundation for the current Providence Health Plan.
JUNE: The Holy Spirit Chapel and Pastoral Services Building opens, thanks to major support from Howard and Jean Vollum.

1985
NOVEMBER: The Heart Institute at St. Vincent is established to coordinate cardiac activities, including research, education, diagnosis, treatment and rehabilitation.

DEC. 31: MRI Associates, a joint venture between the Sisters of Providence and 24 physicians on staff at St. Vincent, begins offering magnetic resonance imaging at the medical center.
The St. Vincent Medical Foundation establishes the Howard Vollum Endowment Fund, following the death of the Tektronix co-founder.
DEC. 7: The new Critical Care Center opens. It consolidates St. Vincent’s three critical care units – the intensive care unit, cardiac recovery room and coronary care unit – into one building.
St. Vincent forms an HIV/AIDS task force to provide recommendations on policies, procedures, services and actions in response to the AIDS epidemic.
St. Vincent establishes the Women’s Health Program to coordinate existing services, such as obstetrics and gynecology, and to develop new ones, such as prenatal genetic testing.

St. Vincent and Providence Portland jointly launch AirCare, an air ambulance service that transports critical care patients from community hospitals to Providence medical centers. In 1993, AirCare merges with Emanuel Life Flight to become Life Flight Network. The collaborative air transport system continues to serve the Pacific Northwest.
To make primary care more accessible to the community, St. Vincent opens satellite facilities as part of its medical care network. They include Tanasbourne Medical Plaza in Hillsboro, Mercantile Medical Plaza in Lake Oswego, Vermont Medical Plaza in Hillsdale and, in 1991, Scholls Medical Plaza in Tigard.
JOHN BERLAND, M.D.
INTERNAL MEDICINE
“You all made St. Vincent the only place where I admitted my patients and the only hospital I would want to be admitted to, myself.”

“So many things transpired over the years – I don’t even know where to begin. However, throughout my entire professional life, I could not have asked for a better institution to be associated with.
“The administration and nursing were outstanding in all respects, particularly in their partnering with the medical staff to bring the best quality of care to the patients and their families. It had to be a joint effort, and from Dr. Kirby Griffin in the family
medical care unit to Providence Medical Group to the new ICU, emergency department and heart transplant program, the end product of enhancing efficient, quality care was always achieved.
“I consider myself extremely lucky to have been surrounded by such a dedicated, talented, skilled team of administrators, nurses and physicians. You all made St. Vincent the only place where I admitted my patients and the only hospital I would want to be admitted to, myself.”
Dr. Berland practiced internal medicine for nearly 40 years and served as president of the Providence St. Vincent medical staff. He remains passionate about physician education and palliative care. The Goldman-Berland Lectureship in Palliative Medicine, established in 2006, honors Dr. Berland and the late Robert Goldman, M.D., for their advocacy for exceptional palliative and end-of-life care.

ED NELSON
GROUNDSKEEPING AND VOLUNTEERISM
“You just put it in your heart that we are here for the patient, 100 percent.”
“When I started at St. Vincent, I was just handling garbage, mowing, pruning and other grounds work. But as I stayed on, they increased my responsibilities. I replaced roads, roofs. My crew was responsible for maintaining access to everything, including Barnes Road. That sometimes meant snow and ice removal, because we have to stay open.
“I learned as I went along, and I had good bosses –John Casessa, Art Rigg, they taught me a lot. Mike Tierney hired me, and if you did the job, he had your back, period.
“When I was adopting my daughter, I mentioned to Mike how much it was going to cost. Mike took me up to the credit union and introduced me, and they loaned me the money just for a signature. Where else can that happen?
“I enjoyed my job, and I enjoyed the people I worked with. This is family. It was easy to come to work here.
“That’s why I’m volunteering now. Father Freddy Ocun set me up. I couldn’t say no. They call me a wayfinder. When people come in and need help finding where they’re going, I either take them or explain how to get there. I love it. It’s a good job. If you’ve got some free time, we could use extra help.
“St. Vincent has always been for the patient. Whoever that patient is who walks through the door, our only task is to make sure they get what they need. Everybody here has that in their heart – I really believe that. You just put it in your heart that we are here for the patient, 100 percent.”
Ed joined St. Vincent as a groundskeeper and retired as the head groundskeeper in 2018 after nearly 40 years on the job. His crew of two to four people managed 38 acres, including nine buildings, three parking structures and 276 garbage cans.


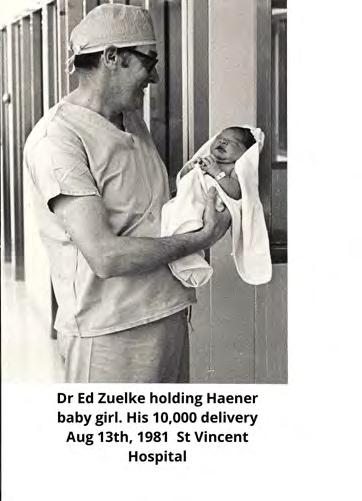
“There was a kid in a T-shirt that read ‘I’m a Zuelke Baby.’”
Through decades of delivering babies, Paul Edward Zuelke, M.D., always felt a thrill when bringing a child into the world. In particular, he said, he loved seeing the reactions of the parents.
Joyful reactions abounded in the St. Vincent maternity unit and beyond when the beloved obstetrician performed his 10,000th delivery. Dr. Zuelke welcomed the new baby girl on Aug. 13, 1981, at 11:03 a.m.
“By the time he retired in 1988, he’d delivered more than 11,000 babies. What a legacy,” says his daughter Lynne Magner. “He also quit charging any
patient who was delivering her sixth child – he felt those mothers needed a break! He was so kind.”
As she recalls that milestone delivery, Lynne says, “Dad received letters from the Portland mayor, the archbishop, the governor, U.S. Senator Mark Hatfield and others. It was in newspapers throughout Oregon and Washington and all over the local news. He said it must have been a slow news day! The reception the hospital had for Dad was well attended, and there was a kid in a T-shirt that read ‘I’m a Zuelke Baby.’”
Lending an occasional hand in Dr. Zuelke’s office was his wife, Inarose, a registered nurse. “He and Mom raised nine kids,” says Lynne, noting that the sizable Zuelke clan continues to welcome new babies into the family.

The late Dr. Zuelke joined the St. Vincent medical staff in 1949. After his retirement, he and Inarose traveled to southern Africa to work in a small Lesotho mission hospital. He taught the student midwives and did OB-GYN care while Inarose worked with the student nurses.
Below: Dr. Zuelke admiring the 10,000th baby he delivered.
MIRIAM ODERMANN, RN CARDIAC CARE
“I fondly remember Sister Scholastica Lee. ... Her great sense of humor helped lift morale amid the intensity of patient care.”

“Working in multiple nursing roles in the coronary care unit from 1976 to 1985, I enjoyed the wonderful camaraderie among the nursing staff. Cardiologists and medical residents worked closely with the nurses, while other hospital staffers, from pharmacists to dietitians, were also part of the team. It was a joy
“I have wonderful memories of the efficient way patients were admitted from the emergency department, and of patients’ families that sometimes were too large to count. It could be difficult keeping visitors to only two at a time.
“A house supervisor made rounds on each shift, and a chaplain rounded during the day shift and whenever a patient or family needed the support. I fondly remember Sister Scholastica Lee, whose rounds included seeing each patient as well as providing compassionate support for the nursing staff. Her great sense of humor helped lift morale amid the intensity of patient care.
“During those years, we saw advances in care for CCU patients, such as Swan-Ganz catheters for monitoring cardiac output pressures, and temporary transvenous pacemakers for stabilizing the heart rate. A procedure room with fluoroscopy was designed for inserting these devices. CCU staff floated to the cardiac recovery and intensive care units as needed. And in 1985, planning began for the CCU’s move to a new home in the future West Pavilion.”


Miriam was nurse manager of the coronary care unit before becoming a clinical specialist in cardiac rehabilitation in 1985. Next, she was coordinator of cardiac rehab and cardiac support services. Miriam served as Providence in Oregon’s chief executive for ambulatory services from 2010 until her retirement in 2017.
“When researchers work hand in hand with outstanding clinicians, each pushes the other to expand knowledge and create better ways to heal patients.”
Healing the human heart was a lifelong calling for Albert Starr, M.D., whose extraordinary skill and passion helped bring Providence Heart Institute into being. The world-renowned cardiac surgeon’s contributions as a physician, scientist, inventor, teacher and humanitarian revolutionized the practice of cardiovascular medicine and saved countless lives around the globe.

Dr. Starr and his surgery partner, James Wood, M.D., built a practice of bright and committed cardiac surgeons at St. Vincent. These surgeons, along with excellent cardiologists, constantly challenged themselves to find or develop the next, best standard in cardiac care – from valve replacement techniques to advances in bypass surgery to diabetes control measures. From these efforts emerged the heart institute in 1985.
“Our willingness,” Dr. Starr said, “to embrace new technologies and stay on the leading edge of cardiac innovations is an assurance to our patients that they will always get the most up-to-date treatments available.”
An innovator in clinical and outcomes research, Dr. Starr noted, “When researchers work hand in hand with outstanding clinicians, each pushes the other to expand knowledge and create better ways to heal patients. There is no better place to advance the frontiers of medicine than a high-volume, superb clinical center that is also committed to research and study.”
Today, Providence Heart Institute is the largest provider of cardiac services in Oregon – and touches lives far beyond.
Dr. Starr was noted for co-inventing and, in 1960, implanting the world’s first successful artificial heart mitral valve. He performed the first heart transplant in Oregon. A former director of the heart institute, he helped develop its high-caliber research and academic programs and enjoyed training post-resident international fellows. The much-honored Dr. Starr passed away in 2024.




than 1,000

patients,
turned out Aug.
successful
help celebrate the 30th anniversary of the
on

KRISTY WAYSON, RN NURSING
“They donated everything it took to bring him to this country and do his surgery for him.”
“Early in my career at St. Vincent, I had the nursing responsibility for the cath labs. We were part of imaging then and didn’t yet have an identity around cardiac services. Eventually, through medical advances and facility improvements, we started to develop a heart hospital within a hospital. With cardiac services integrated and connected to the ER, we became known nationally for our short time to treatment, because it was a straight shot for that heart patient coming through the door.
“Dr. Albert Starr was a true visionary and was committed to clinical research. He had Dr. Gary Grunkemeier, a biostatistician, create a database that I think was unheard of then, and they started collecting clinical data on valve patients. The infrastructure that Dr. Starr established helped us create an institute that could stand up to any nationally renowned cardiac center.
“A favorite memory involved our spiritual leader, Father Freddy Ocun, whose uncle was a prominent person in a Ugandan village. The uncle needed aortic valve surgery, but his village didn’t have the necessary facilities for it. I went around and talked to our doctors, administrators and medical device companies, and to a person, they donated their time, equipment, and everything it took to bring him here and do his surgery for him.
“The values of the sisters still resonate with everyone who works here.”
Kristy joined St. Vincent in 1981, serving as a night nurse in the intensive care unit before moving to the imaging department as its first nurse. She went on to become the executive director of Providence Heart Institute of Oregon.



JOHN FLETCHER HEALTH CARE LEADERSHIP
“Then magic started to happen.”
“When I was asked to join the newly created heart institute in 1987, I had no idea what an ‘institute’ was. But I knew St. Vincent had the largest cardiac surgical program on the West Coast, and I jumped at the chance to be part of it.
“In the beginning, the people pictured in the institute’s brochure identified mainly with their own practices and departments. To realize the vision of the institute, we needed to be a team.
“Our team building started modestly with monthly meetings. But increasingly, people took notice that the institute could effect change and help patients. Then magic started to happen.
“If this works for cardiac care, some wondered, why not do it for all our clinical services? This process of breaking down departmental silos and bringing people together, initially dubbed service-line management, became known as program management. As with the heart institute, we envisioned building programs for cancer, neurosciences, mental health, women and children’s health, and other services.
“We had the vision. Now we needed data. The brilliant Gary Grunkemeier, Ph.D., brought in David Lansky, Ph.D., and transformed our research group into the Center for Outcomes Research and Education. With data from CORE, and a lot of hard work, doctors and administrators began to embrace the clinical programs and their potential for outcomes management. Today, our clinical institutes benefit thousands of patients.”
John (at top) had a large and lasting impact on St. Vincent. He served as executive director of The Heart Institute at St. Vincent, known today as Providence Heart Institute, during the formative years of 1987 to 1992. During that time, he also assumed the role of assistant administrator for clinical programs. His career with Providence spanned more than 30 years.


CURTIS HOLZGANG, M.D.
CRITICAL CARE MEDICINE
“The best thing we did was to bring nurses in to help us make decisions.”
“When I became director of critical care at St. Vincent, the intensive care, coronary care and cardiac surgery recovery units were each in a different part of the hospital. The new Critical Care Center we completed in 1986 brought these units together and made significant improvements for patients and staff alike.

“The best thing we did was to bring nurses in to help us make decisions about the building’s design. They wanted to be sure we had single-bed rooms for privacy, arranged in four-room pods so the nurses could see the face of each patient from their stations. They also wanted each room to have a large digital clock, a television, and a big window to bring in the sunlight. And we all agreed that we needed a comfortable area for families.
“The centralized location made it easier for me to make rounds every day on the patients. Residents working with the patients would present cases to me, and often nurses, dietitians, social workers, respiratory therapists and others would make rounds with me and report on their patients. This helped ensure that we were looking at the whole patient and that person’s entire care.
“Not long ago, I was invited to a reunion of retired ICU nurses. That experience just emphasized to me what a great bunch of critical care nurses we had.”
Dr. Holzgang joined St. Vincent in 1980 as associate director of the department of medicine, and soon became the director of critical care medicine. He enjoyed making bedside teaching rounds with internal medicine residents and received the Howard P. Lewis Distinguished Teacher Award from the American College of Physicians, Oregon Chapter, in 1992.


JOHN MCDONALD, M.D. NEONATAL INTENSIVE CARE
“I knew we were doing things in a thoughtful way for the community.”
“When I came to St. Vincent in 1986 as a neonatal medical adviser, my work was to organize the pediatricians around newborn care. By 1989, the hospital decided to build a neonatal intensive care unit, and they asked me to be the medical director. It took about five years to get everything in place, and eventually we became the largest, busiest NICU in the state.
“I felt blessed by the caregivers I had day-to-day contact with and by the great support from the administrators. It was just a really inspirational group of people to work with. Our decisionmaking principles and practices always left me with peace of mind, because I knew we were doing things in a thoughtful way for the community.
“We were allowed to be curious and innovative. In one instance, we worked very hard to eliminate the risk of kernicterus, which is brain damage from very high levels of jaundice in a newborn. We reduced the risk to as close to zero as you can get.
“Early on, I remember excitedly telling the administrator that there were seven languages being spoken by the families in the NICU. I always felt good that in a small space you could have a wealthy family’s little premature baby next to a migrant’s baby, and they were all treated with the same caring.”
During his long career at Providence St. Vincent, Dr. McDonald cared for hundreds of babies. He helped create the hospital’s neonatal intensive care unit and served as its medical director from 1992 to 2011. He also served as director of neonatal services for Providence Health & Services in Oregon from 1996 to 2012, and as medical director of the regional Providence Women and Children’s Program from 2010 to 2021.



AKIKO ERWIN FAMILY MEMBER
“ St. Vincent Hospital became far more than a house of medicine: it was a hundred friends, a home, a haven.”

During the final years of Mutsumi Shinoda’s life, St. Vincent became a “life-sustaining force,” recalls her daughter, Akiko Erwin. “Mitsie” had served the hospital as a guild volunteer and medical staff services secretary before succumbing to cancer in 1988. After Mitsie’s death, Akiko sent a letter to then-administrator Greg Van Pelt, expressing what the hospital had meant to her mother:
“To her, St. Vincent Hospital became far more than a house of medicine: it was a hundred friends, a home, a haven, a place of fulfillment. The people of St. Vincent – you – adopted her. You fortified her with friendship and prayer and caring. More than treating her body, you nourished her soul. More than giving her hope, you gave her happiness, recognition, and the kinds of personal fulfillment she had never before experienced.
“She was immensely proud to be part of the St. Vincent family – as employee, as volunteer, as patient – to be woven more deeply into the institution’s fabric than she had ever been, anywhere. You made that pride possible. You made that quiet, enduring courage possible. You helped keep that smile beaming.
“I know ... that she touched many of you in return. It has been a rare and beautiful symbiosis: my mother and you. It has also been a tribute to St. Vincent that medical professionalism and human values have worked so wonderfully together.”
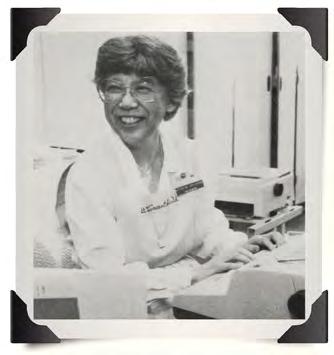
A longtime volunteer like her mother (at right), Akiko helps out in the hospital’s Basecamp Prevention + Wellness program. She also volunteers in schools and with Japanese immigrants. “It’s something that I feel we need to do: to care for others,” she says. Akiko donated rhododendrons to the hospital as living memorials to her mother.

“ The pastoral services department, it seems to me, is the real heartbeat of the facility.”
At certain times of day, warm hues of rose and orange stream through stained-glass windows into the chapel at Providence St. Vincent, lending an aura of comfort and support. The beautiful space is imbued, as well, with the warm generosity of Howard and Jean Vollum.
The couple’s major gift to the medical foundation’s fundraising campaign for the Holy Spirit Chapel and Pastoral Services Building in 1982 helped bring the structure into being. Over many years, the Vollums gave significant time and treasure to St. Vincent. Howard served on the foundation’s council of trustees, Jean on the hospital’s advisory board.
“People tend to think of a hospital in medical terms, but remember–most people who come to St. Vincent also have non-medical concerns,” reflected Howard, thenchairman of the board of Tektronix, Inc. “They need all the help, sustenance and support they can get.”

Jean agreed. “The pastoral services department, it seems to me, is the real heartbeat of the facility. It creates a different feeling. I’ve talked to many members of the St. Vincent staff who have commented about the environment of spiritual understanding. That’s why supporting pastoral services and the chapel is such a pleasure for us.”
A fine-arts devotee, Jean helped shape the chapel’s “spiritual aesthetic that happens when you’re surrounded by simple but very beautiful design … very comforting to a person in great need.”


Don Vollum, son of the late Howard and Jean Vollum (pictured), carries on his family’s legacy of engagement and leadership at St. Vincent. In his recent role as president of the foundation’s council of trustees, one of Don’s contributions was advocating financial support for honoring the medical center’s 150th anniversary.
Two terms – regionalization and clinical integration – defined the 1990s at St. Vincent. Amid sweeping changes in the nation’s health care delivery system, the Sisters of Providence in Oregon took major steps toward becoming a regionally integrated health system –one that would provide seamless care across the communities it served.
In a 1992 letter to all employees, John Lee, vice president of operations for the Sisters of Providence in Oregon, explained the changing landscape in which health care would be provided in Oregon by a handful of regional delivery systems, including the Sisters of Providence. “To carry on the historic Mission of the sisters and to hold to our traditional values,” he wrote, “our regional health system will be challenged to forge even closer relationships with purchasers and physicians; to improve quality; to control costs; and to ensure that employees find satisfaction and meaning in their work.”
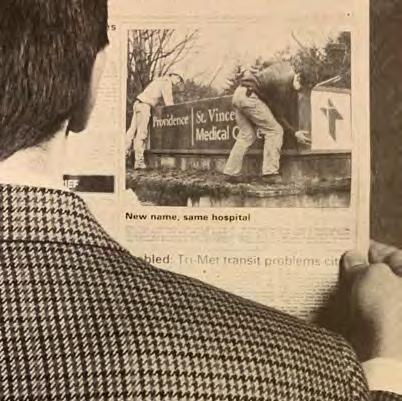
Throughout the decade, the hard work of regionalization progressed. St. Vincent Hospital and Medical Center became Providence St. Vincent Medical Center to better identify it as part of the unified Sisters of Providence Health System.




Managers took on regional roles, and the clinical departments, foundations and governance teams at the individual hospitals combined efforts, leading Providence to become the largest health care organization in the state.
Meanwhile, on the Providence St. Vincent campus, an expansion of the West Pavilion continued the hospital’s movement toward providing more clinically integrated services for its patients. In the new maternity center on the third floor, for example, mothers and babies now received all of their care, from admission to discharge, in the same room. One floor down, the newly expanded and integrated heart institute elevated the hospital’s cardiac facilities to “literally, the most advanced in the world,” according to director Albert Starr, M.D.
In the middle of this exciting decade, St. Vincent celebrated its 25th anniversary at Southwest Barnes Road. Sister Rita Ferschweiler, SP, the hospital’s original administrator at this location, spoke at a Mass commemorating the event. “What will happen next?” she asked the crowd. “I threw my crystal ball away.” If change is the only constant, she said, “I hope we can combine the new techniques and TLC and give our patients the best care possible, and always with the dignity of the patient in mind.”
A multiyear process of regional integration begins, with St. Vincent joining Providence Portland Medical Center and Providence Milwaukie Hospital to form the Sisters of Providence Health System in Oregon. Using a managed care approach, regionalization enables the hospitals to seamlessly deliver health care to the communities they serve.
St. Vincent partners with Washington County Health and Human Services, Virginia Garcia Memorial Health Center, Oregon Health Sciences University and Tuality Hospital to form Healthy Start. The nonprofit organization is dedicated to providing pre- and postnatal care to underserved communities. It merges with St. Vincent in 1993.

St. Vincent becomes the first hospital in the world to use laser thrombolysis to vaporize blood clots. This procedure, developed by hospital researchers, stops a heart attack in progress and saves the patient’s life.
The Sisters of Providence Health System forms Providence Medical Group, a primary care division. It hires physicians and also signs contracts with existing primary care group practices.
The Oregon Medical Laser Center is established at St. Vincent to develop new diagnostic and therapeutic applications for lasers. The center also initiates federally sponsored trials of emerging laser technologies.

OCT. 29: St. Vincent’s Committee on Cultural Diversity holds its first meeting. It seeks to build an organizational culture that fosters respect and recognition for one another, carrying on the tradition of the Sisters of Providence.
St. Vincent is recognized as one of the top 100 hospitals in the United States. This is the first time the medical center appears in the annual 100 Top Hospitals National Benchmarks for Success study by HCIA, a Baltimore-based health data company.
JULY: The West Pavilion, the most significant campus addition since St. Vincent moved to Barnes Road, opens. The stateof-the-art facility houses three of the hospital’s fastest-growing services: cardiac, emergency and maternity.
JAN. 25: The St. Vincent Family Maternity Center opens in the West Pavilion. It includes an upgraded neonatal intensive care unit (NICU).
OCT. 14: St. Vincent Hospital and Medical Center is renamed Providence St. Vincent Medical Center. This change more clearly identifies the medical center as being a part of the Sisters of Providence Health System in Oregon.
APRIL: Providence St. Vincent becomes a plan hospital for the Kaiser Permanente health plan as the latter works to close Bess Kaiser Hospital. With the influx of Kaiser patients, volumes for all Providence St. Vincent services increase significantly.
Providence St. Vincent physicians perform the first minimally invasive aortic and mitral valve replacement surgery in Oregon.
JULY 30: The Travis and Beverly Cross Guest Housing Center is dedicated. Built entirely with funding from the Providence St. Vincent Medical Foundation, the center provides housing for out-of-town patients and their families.
DAVID COOK, M.D. GENERAL SURGERY
“St. Vincent rotations were, and still are, the most desired rotations of the OHSU residency program.”

“In my first year as an OHSU surgical intern, I had seven rotations at St. Vincent and was the envy of my classmates. St. Vincent rotations were, and still are, the most desired rotations of the OHSU residency program. That’s due not only to the volume of procedures, but also to the quality of teaching, the facilities, and the friendly, welcoming environment.
“In 1990, I was thrilled to join the surgical practice of Drs. Dan Dennis, William McAllister and Kim Swartz. They were great surgeons who were also very involved in teaching. This was the best of both worlds to me. What a great experience! I’ve been teaching ever since.
“Having served in many leadership roles, I’ve observed the involvement, cooperation and investment of the administration in issues that matter most to physicians. CEOs from Greg Van Pelt to Don Elsom, Janice Burger and Jennifer Burrows have always been willing to listen to concerns and to work together to solve problems.
“Since my days as an intern, I’ve seen many changes on campus: new office buildings, a new ER, expanded women’s services, development of the heart institute, new ICUs and larger, remodeled operating rooms. I hope and believe that despite barriers in health care funding and other challenges, Providence St. Vincent will continue to be at the forefront of innovative, thoughtful and community-directed expansion.”
Dr. Cook began his time at Providence St. Vincent as a surgical intern in 1984. He has served on the Providence St. Vincent Medical Executive Committee and in other leadership roles. As the department of surgery’s director of surgical education, he enjoys mentoring medical students and residents as those before him did.

Left and below: The intraoperative MRI suite is one of myriad technological advances Providence St. Vincent has seen in the past four decades.

SUSAN KIRCHOFF, RN EMERGENCY NURSING AND LEADERSHIP
“I thought, wow. ... These guys are very serious about what they do.”

“I was an ER director in Arizona when I got recruited by St. Vincent in 1991. I came to Portland mainly to visit family, but then in the interview, I just fell in love with the people in the emergency department and what their vision was for the future.
“They broke ground on the West Pavilion one week after I arrived, so the first two years were a whirlwind. We made the transition from these big four-bed rooms to this emergency department that seemed really enormous at the time, but which clearly isn’t big enough anymore.
“Having worked in emergency medicine before, I was struck by the group’s rigorous peer review. They were just really frank with each other, and I had not experienced that before. They were so intent on getting it right, and on owning when they didn’t and figuring out what the lessons were for the whole group.
“That was one of my early first impressions: I thought, wow – this is really impressive. These guys are very serious about what they do, and about getting it right.”
Susan joined Providence St. Vincent in 1991 as director of the emergency department. Two years later, just after the ED moved to the West Pavilion, she became Providence’s first regional director of emergency services, leading the Providence St. Vincent, Portland and Milwaukie EDs until 1998. Today, with medical foundation support, the emergency department is expanding again.

Project coordinator
Karen Weylandt and Ken Zinsli, assistant administrator for facilities, at the groundbreaking for the West Pavilion.
DONALD SUTHERLAND, M.D. CARDIOLOGY
“You would squeeze the heart with your hands. That was CPR until 1960.”
“In 1960, during my residency training at Massachusetts General Hospital, a speaker from Johns Hopkins came to explain external cardiac massage. Back then, each nursing station had a scalpel to open the chest during cardiac arrest, and you would squeeze the heart with your hands. That was CPR until 1960. And we didn’t have electronics. There were no coronary care units, no monitors.
“When I came to St. Vincent in 1963, it was a time of rapid and remarkable change in cardiac care. I went and watched three coronary angiograms up at OHSU, then did the first ones performed at St. Vincent. We established the hospital’s first coronary care unit in 1964.
“The technology and knowledge available became markedly broader in the ’80s and ’90s. Dr. Dan Oseran made a huge difference in expanding and compartmentalizing specialties and subspecialties in cardiology.


“From my standpoint, the goal was to be excellent in every way that you understood that word, in every aspect of what you did in taking care of a patient. That was the goal, always, all the time, every day.
“I retired from fulltime patient care in 2002, then worked in the office for several years. And the continuing growth I’ve seen in taking care of a human being, in a great variety of ways, is just remarkable.”
Dr. Sutherland served in many capacities at St. Vincent, from educator to medical staff leader to head of Columbia Cardiology Associates. He actively contributed to the growth and development of heart specialty services at the hospital from the early 1960s to the heart institute of today.

DANIEL OSERAN, M.D. CARDIOLOGY
“There is something different about working here.”
“In 1992 I moved back to Portland, where I’d grown up, to set up the first electrophysiology laboratory and arrhythmia center at St. Vincent. It was kind of an inflection point when things were changing.
“Within a couple of years, the whole West Pavilion infrastructure was built, which created the opportunity to co-locate many cardiac services: the electrophysiology lab, dedicated cardiac operating rooms, a series of cath labs. You suddenly had this integrated heart institute area. And now we’re planning the next iteration of what those inpatient services could look like.
“Throughout my entire experience here, there’s been great partnership between administrative leadership, physician leadership, and the community in terms of philanthropy. In the last couple of decades, philanthropy has allowed us to be really innovative. Our ability to launch the digital operating suite for robotic-assisted surgery, the transplant program, catheter-based aortic valve replacement – it all depended on philanthropic support.
“At St. Vincent there is a culture of excellence, of leadership, of wanting to be the best, along with the Catholic health care Mission of treating the poor and the vulnerable. The old tagline – ‘A caring difference you can feel’ – is actually true. From the nurses to the transporters, people feel there is something different about working here.”
Dr. Oseran is the executive medical director of Providence Heart Institute of Oregon. After starting St. Vincent’s arrhythmia center, he helped to grow the program into the highest-volume electrophysiology center in the Northwest. He has personally performed several thousand catheter ablation procedures as well as numerous pacemaker and defibrillator implants.


ADRIENNE SIMMONS PLANNING
“ Fact-based decision-making … meant focusing on the impact decisions would have on the broader community.”
“When I started as planning director at St. Vincent, the emphasis was on fact-based decision-making. Rather than defaulting to a political process, this meant focusing on the impact decisions would have on the broader community. One example stands out.
“When St. Vincent’s neonatal intensive care unit was level 1, insurance companies didn’t routinely cover the costs of prenatal care or delivery. Women would sometimes arrive at the emergency department in labor without having had any prenatal care. Premature babies needed care beyond the capabilities of a level 1 nursery. And families having to travel to be with their baby in a higher-level NICU could face hardship, especially if their financial resources were limited.
“We followed a process of discernment and fact-based decision-making before deciding to offer level 2, and later level 3, NICU care. For example, we reviewed population projections for Washington County and considered physicians’ needs in providing continuity of care between hospitals for these babies.
“Work also was needed upstream so that women could receive prenatal care when they couldn’t afford it. St. Vincent was a key partner in developing Healthy Start, which provided prenatal care in Washington County.
“I feel grateful and proud to have had the opportunity to work at St. Vincent. I learned so much from leaders who took the Mission seriously – especially their commitment to serving the poor and vulnerable.”

Adrienne joined St. Vincent in 1981 as director of planning. During her 30-year career with Providence, she also held regional director roles in planning, in program management for end-of-life and palliative care, and in medical education programs. She has a special interest in change management and strategic planning.
KATHERINE CRISWELL, RN
WOMEN AND CHILDREN’S HEALTH
“ It’s the feeling, when you go home, that you did the right thing.”
“After Providence regionalized in the mid-1990s, I took on the leadership of women and children’s services for the region. Our commitment was to provide the same evidence-based standard of care when you had your baby at any facility with the name Providence on it.
“High-quality, safe care is our standard. It has led to state-level policies for testing babies for hearing and elevated bilirubin levels before they leave the hospital.
“So much of our care is driven by what the community is asking for. We’ve been responsive in listening to our patients, to their feedback, to what’s important to them.

“At St. Vincent, it was always, always so important that we respect every single person’s humanity. I remember when I’d see our administrator, Greg Van Pelt, hurrying off to a meeting – if he noticed someone who was lost, he’d stop and walk them to their destination. The rest of us would emulate that example. We had tremendous leaders.
“When people join St. Vincent, they’re joining an organization with deep commitment, deep values, a deep Mission that’s been here for a very long time. It carries a lot of responsibility. But it carries great reward in seeing good work done every day.
“It’s joyful responsibility. It’s the feeling, when you go home, that you did the right thing for others.”
After helping develop obstetrical services at Providence Portland Medical Center, Katherine served as executive director of Providence Women and Children’s Services from 1993 to 2015. Under her leadership, obstetrical and neonatal services grew. Today, Providence delivers one out of four babies born in Oregon and is a premier provider of services for women and children.

PAUL DUWELIUS, M.D.
ORTHOPEDIC SURGERY
“I feel blessed to have had the support of a great hospital.”
“I left an academic practice at OHSU in 1995. Orthopedic and Fracture Specialists was the group that I wanted to join because of their ‘privademic’ track record (as a private practice with a proven research record).
“Our partners are nationally known and recognized in their specialties. Dr. Henry Blair, a founding member, developed the Blair ankle fusion. Another founding member, Dr. Howard Cherry, developed an easy-out nail extraction device. Dr. Joe Davis developed the Davis hip fusion. Dr. Jay Butler was instrumental in designing the anatomic femoral hip stem and acetabular cup and liners. And Dr. John Hayhurst developed a patented suture anchor that has changed the field of sports medicine.
“Our group is intimately involved in the teaching of OHSU residents and the future physicians who will provide for our patients. We have our pick of residents. And with the tremendous research support of the Orthopedic Center of Excellence at St. Vincent, we’ve published multiple clinical outcome studies.

“COVID and anesthesia shortages have made orthopedic practice more challenging, and times have changed since the sisters founded St. Vincent. But if we keep their Mission in mind, that will be best for the care of our patients.
“I feel blessed to have been a member of this group and to have had the support of a great hospital that provided outstanding care for our patients.”
Dr. Duwelius retired from an active surgical practice in 2022 after many years at Providence St.Vincent. He continues to serve as the hospital’s director of orthopedic research and stays involved in teaching and clinical research. Orthopedic and Fracture Specialists now has 23 surgeons on its team.

“The guest house … has become a cocoon of comfort.”
Comfort, caring and freshly baked cookies are in plentiful supply at the Travis and Beverly Cross Guest Housing Center, a convenient home away from home for patients and loved ones from out of town. Since its opening in 1997, countless guests have expressed their gratitude. Here are some of their comments:
“Your housing was the answer to my prayers. We both feel like we fell into a nest – the bright colors in the kitchen, the music, the cookies, and above all, a staff that always met us with a smile.”
v v v
“What a delight it has been to stay at the guest house, which has become a cocoon of comfort with people who truly care and make us feel so much like family! A hospital experience can be terrifying; thank God for those who conceived of this place to soften the emotional and financial blows that buffet the nervous system while a loved one is in the hospital.”
v v v



“You have given us a refuge from which we could care for our very ill daughter. This is a wonderful place – a calm and safe place – and I’m so glad it will be here for others.”
v v v
“My husband always felt that I was safe and secure here, and I was able to visit him [at all hours] without worrying about a drive home. My only problem is that I don’t want to leave!”
Travis and Beverly Cross (pictured), known for their compassion and hospitality, were surprised to learn that a guest house would be built in their honor. During his 17 years with St. Vincent, Travis directed the foundation and then was assistant administrator for public affairs. Beverly served as a longtime St. Vincent guild volunteer.
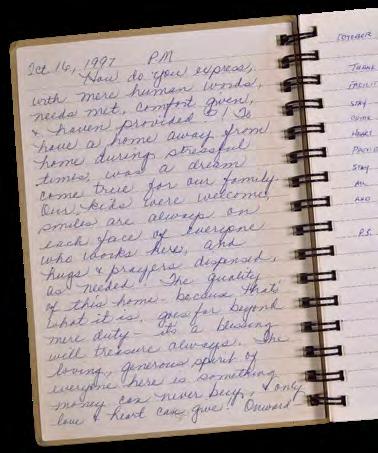

It was a new millennium, and the world breathed a sigh of relief as the dreaded Y2K disasters failed to materialize. The calm, however, was short-lived. On Sept. 11, 2001, terrorist attacks shook the nation. A delegation of St. Vincent nurses flew to New York City to offer solace and support.
Later in the decade, the Great Recession hit, affecting everyone. In Oregon, unemployment rates reached 12%, and the number of residents receiving their health care through the Oregon Health Plan rose to nearly 30% of the population. Reimbursements for care declined, and the demand for charity care increased. To meet the pressing needs of the community, the Sisters of Providence embarked on a large-scale cost-containment effort to ensure that limited resources were allocated as wisely as possible.
At Providence St. Vincent, the decade’s events propelled a sustained effort focused on stewardship and quality – familiar values rooted in the sisters’ Mission. Among many new initiatives, the hospital




established Oregon’s first certified primary stroke center, its first certified ALS center, a multiple sclerosis center, a breast health center and a children’s surgery center. These and other efforts earned the hospital national recognition for its quality of care, including repeated designations as a Magnet hospital for nursing (American Nurses Credentialing Center) and as a Top 100 Hospital (Reuters).
The recognition was a credit to the physicians, nurses and staff members who put their patients first every day; to the foundation trustees and donors who raised funds and support for critically needed programs; and to the volunteers who contributed generously to all of these efforts.
The value of the Providence St. Vincent Volunteer Guild cannot be overstated. By the guild’s 50th anniversary in 2000, more than 5,000 volunteers had donated 2 million hours of their time and raised $2.7 million for the hospital. 2025 marks the guild’s 75th anniversary of loving service to the people and patients of Providence St. Vincent.
Providence Heart Institute introduces a robotic-assisted surgery program. Providence St. Vincent becomes the first medical center west of the Mississippi River to utilize this technology.
MAY 17: The Providence St. Vincent Volunteer Guild celebrates 50 years of service to the medical center.
NOVEMBER: Providence
St. Vincent becomes a Magnetdesignated hospital, the first medical center in Oregon to achieve this recognition. The designation by the American Nurses Credentialing Center is the highest national honor for professional nursing practice.
DEC. 8: The Providence Center for Health Care Ethics is established to provide ethics consultation, research, education and scholarship to Providence Health System. It addresses ethics concerns across the continuum of care.
JULY 12: Providence St. Vincent celebrates the grand opening of the Ruth J. Spear Breast Center. The new center brings together diagnostic, treatment, counseling and education services in one location.
OCTOBER: One thousand Oregonians, including five Providence St. Vincent nurses, participate in the Flight for Freedom. In the aftermath of the 9/11 terrorist attacks, they fly to New York City, bringing resources to local residents. The Providence St. Vincent employees tour St. Vincent Hospital in Manhattan and deliver cards signed by medical center employees.
The Providence Stroke Center at Providence St. Vincent launches the first statewide stroke registry in Oregon. Providence researchers are able to gather and use care data to identify ways to improve stroke care in the state.
The Providence Brain Institute is established to provide coordinated care and treatment for all brain conditions. It is renamed Providence Brain and Spine Institute two years later to reflect Providence’s continued commitment to excellence in the neurosciences.
Providence St. Vincent becomes the first certified primary stroke center in Oregon after earning both the Gold Seal of Approval for stroke care and certification by the Joint Commission on Accreditation of Healthcare Organizations.
MARCH 25: The Gerry Frank Center for Children’s Care opens at Providence St. Vincent. It provides pediatric surgery and procedures with a family-focused approach.

OCT. 20: Providence St. Vincent celebrates the opening of the East Tower. The building includes a new pediatric unit, a mental health wing, and space for cardiac, neurology and medical/ surgical patients.
The Providence ALS Center at Providence St. Vincent becomes the first in Oregon to be certified by the national ALS Association. It is the first ALS multidisciplinary clinic in the state.
The “Pink Glove Dance” video makes national news. The video, created in November by Providence St. Vincent nurses and staff members to promote breast cancer awareness, goes viral and tops 5 million views by the end of the year.

SUE JOHNSON, RN NURSING
“ Nobody else in the community could take care of someone with her needs.”
“Starting here as a neurology staff nurse, I had come to St. Vincent because it was a good place to work. But I stayed because of the Mission. We were not-for-profit and it wasn’t about money – it was about the patients and the staff and doing the right thing for people.
“Part of the hospital’s culture is the musicthanatology ministry, and sometimes the thanatologist would show up on our nursing unit when we were running around with our hair on fire. She would sit and play the harp for the staff.


You could feel everybody kind of relax into that.
“Over the years, one patient who stands out in my mind is a woman who had suffered a spinal cord stroke. She was ventilatordependent, had to be in a special bed, and was our patient for probably two years. Nobody else in the community could take care of someone with her needs. She was lucid and able to communicate, and she became part of the St. Vincent family.

“It was very difficult to take care of a patient for that long and see all the iterations she went through – and, in the end, to lose her. But the nursing staff, physicians and other caregivers all rose to the occasion. The hospital did a beautiful job of caring for her, and doing the right thing.”
Sue spent her entire nursing career, from 1983 to 2020, at St. Vincent in neurology. She served as a charge nurse for 15 years before retiring. Sue recalls how former nursing director Jane Smith, RN, encouraged her interest in ethics and emphasized “always striving for excellence.”
LAURA MOYA PASTORAL SERVICES
“ When curing the body is no longer possible, caring for the soul comes to the fore.”
“Most of us recognize the healing force of music, with its power to make us cry, smile, grow calm or dance. Music-thanatologists are professional clinicians who use harp and voice in support of those receiving palliative and end-of-life care.
“Meeting with your mortality or that of a loved one can be challenging. Dying is a time of letting go. Music-thanatology is offered so that patients and their loved ones simply receive without effort or expectation of response. Introducing beauty into a clinical space can remind us of our humanity and connection to one another.
“I have a blessed career with St. Vincent as a musicthanatologist and spiritual care provider, working alongside exceptional caregivers. At the time of dying, when curing the body is no longer possible, caring for the soul comes to the fore so that death can be as meaningful, peaceful and beautiful as possible.
“I have witnessed many beautiful deaths. A particularly poignant one came when a young man was actively dying. His mother sat at his bedside and, in rhythm to the music, stroked his head and arms. She spoke to him softly, letting him know she loved him. Within that love, she encouraged him to ‘let go.’ Peace settled on his face and remained until he died.
“Each day, I am reminded of how life and love are a gift.”
Certified in music-thanatology, Laura joined the Providence St. Vincent Pastoral Services Department in 2001. She is a faculty member of Accorda Music-Thanatology Training Institute. Music-thanatologists are specially trained to offer music in a way that is uniquely tailored to respond to patients’ physical, emotional and spiritual needs.

CURTIS HOLZGANG, M.D. CRITICAL CARE MEDICINE
“The ethics center is something that we should be very proud of.”

“The story of the Providence Center for Health Care Ethics begins with Andy Honzel, a longtime friend of St. Vincent and a member of the medical foundation’s council of trustees. He came to me particularly happy one day because his family’s foundation had started an ethics center at Santa Clara University.
“This got us talking about ethics in health care, including issues that we deal with in the intensive care unit and that we might face in the new NICU. I didn’t think anything more about it. But a month later, Andy came to my office with a business plan for a Providence ethics center based at St. Vincent. For the Honzels’ foundation to initiate this was really generous.


“It worked out beautifully. Father John Tuohey, an experienced medical ethicist, was named the center’s director. Every time I was with him at the bedside with an ethical problem, I agreed with his conclusions and the principles behind them.
“Father Tuohey developed outstanding ethics education for Providence people and others. A fellowship in biomedical ethics was recently funded, and we now have three full-time medical ethicists.
“The ethics center is something that we at St. Vincent should be very proud of. Andy and Beverly Honzel are both deceased now, but I’m glad they lived long enough to see it happen.”
The Providence Center for Health Care Ethics opened in 2000. Dr. Holzgang, former director of critical care medicine at Providence St. Vincent, now serves on the center’s advisory board and is the namesake for the center’s longest-running lectureship in medical ethics. In honor of his late wife, the center includes the Darrelyn Holzgang Fireside Room featuring a beautiful stained-glass window.

NICHOLAS KOCKLER, PH.D. HEALTH CARE ETHICS
“We always seek to keep the dignity of the person at the center of compassionate care.”
“On an autumn day in 2019, a Providence medical resident paged an ethicist for assistance. A patient was dying of advanced dementia, and her adult child was showing signs of complicated grief.
“The resident and his team were concerned about the harm they would inflict on the patient if they tried to resuscitate her in the event of a cardiopulmonary arrest. Her family member was insisting she be in ‘full code’ despite recommendations to ensure her comfort and allow a natural death. With compassion, the ethicist and a palliative care physician provided expert consultation.
“This difficult scenario is but one example of the numerous touchpoints for the Providence Center for Health Care Ethics. Our staff members strive to empower caregivers and others to address ethical issues directly. We offer health professionals a range of services, including ethics education, consultations, rounding, discernments, research, outreach and leadership.

“Thanks in part to a major fundraising campaign, our ethics center has grown into a prominent center of excellence in education, consultation and scholarship. We are a nationally and internationally known thought leader in health care ethics. In 2010, we were pleased to host the International Conference on Clinical Ethics Consultation, with countries from all over the world represented.
“Whatever the challenges may be, we always seek to keep the dignity of the person at the center of compassionate care.”
Nicholas is vice president for System Ethics Services, Providence St. Joseph Health. Kevin Dirksen, MDiv, serves as chief integrated ethics officer at the Providence Center for Health Care Ethics and holds the Andy & Bev Honzel Endowed Chair in Applied Health Care Ethics.

“It took me to the wholeness of my patients.”
“When I was a hospitalist, I would see a patient’s treatment plan get readjusted, sometimes daily, according to the preferences of the hospitalist on duty. This occasionally led to confusion and frustration. It seemed best to create a consistent care plan around the patients’ own wishes for their lives.
“The new medical discipline of palliative care offered instruction for doing ‘goals of care’ conversations with patients and families. Several of us, including critical care and geriatric physicians, traveled to learn about this care. In 2007 we launched a palliative care program, ‘Connections,’ serving St. Vincent and Providence Portland.
“I discovered that palliative care was where my heart and soul were. It was the best part of my practice, because it took me to the wholeness of my patients. We were not just doctors – we were
nurses and chaplains and social workers – and I could really get to know my patients in all these dimensions through working in a multidisciplinary team. Seeing the wholeness of the person you’re serving – that has been deeply satisfying.
“This mantra ‘Know me, care for me, ease my way’ summarized all the wonderful things that I remember from my career at St. Vincent. Because you’re focused on another person, but in the bigger context of us as a community, and maybe something more, you know – it’s me, thee, and something bigger.”
Dr. English, a specialist in infectious diseases, established the hospitalist service at Providence St. Vincent in 1998. He led the program until 2007, when he co-founded the hospital’s palliative care service. He went on to serve as the regional medical director of palliative care for Providence in Oregon until his retirement in 2013.

Left: Connections colleagues.
Below: Dr. English with Elise Newman, M.D., hospice and palliative care internist.

“We’re really all called to this.”
Through her life of compassionate action, Emilie Gamelin of Montreal brought hope to the hurting and inspired countless others to do the same. In 1843, she founded the Sisters of Providence, devoted to serving the poor, sick, disabled, elderly, orphaned and imprisoned.
While caring for victims of cholera, Mother Gamelin contracted the disease herself in 1851. With her final words, she urged the sisters to carry on in humility, simplicity and charity.
A century and a half later, on Oct. 7, 2001, the humble founder was beatified by Pope John Paul II. Beatification is Catholicism’s second of three steps toward sainthood.
Monica Anderson, then-director of Providence St. Vincent Pastoral Services, traveled to Vatican City for the ceremony. As she gazed up at the huge portrait tapestry of Mother Gamelin displayed on the facade of St. Peter’s Basilica, she reflected, “We’re really all called to this. Most of us are never going to have our picture hanging in the Vatican, and yet we’re all called to live holy lives – to take whatever gifts we have and to fulfill the potential that we each have within us, and to extend our hearts as far as they’ll extend. That’s what our lives are all about.”
As Pope John Paul II told the throng, Blessed Emilie Gamelin “wanted to give without counting the cost.”
“Blessed” is the title bestowed on a person who has been beatified. “The depth of her devotion to the lives of people who were poor and marginalized is remarkable,” Russ Danielson, then-chief executive of Providence in Oregon, said of Blessed Emilie Gamelin. More than 800 Sisters of Providence, friends and associates attended the beatification ceremony in Vatican City.



DOUGLAS SHUMAKER, M.D. GASTROENTEROLOGY
“I was so touched by the caring that I felt.”
“My history with St. Vincent goes way back. In June of 1980, I had my appendix removed here. I was 12 years old and obviously frightened, but that experience set me on the pathway to where I am today.
“I will never forget – I was waiting on a gurney in the pre-op area, and there on the ceiling was a poster with the 23rd Psalm on it. I went from being this scared kid to feeling this incredible peace, like I was in connection with God. I was so touched by the caring that I felt from the people in the hospital, and I had confidence in them.
“After that, I thought, ‘Boy, that is something I want to give others someday, because it was such a gift.’ It really solidified my goal of becoming a physician, and my dream of someday practicing in this hospital. So, to sit here all these years later, having spent 22 years as a staff member and served as president of the St. Vincent medical staff, is just a complete and utter honor.
“My three children were born at St. Vincent, and I watched my daughter give birth to my grandson here, surrounded by those same caring kinds of people who treated me years ago. It was a reminder of what we have here, and what we should really hold onto and cherish.”
Dr. Shumaker completed his internal medicine residency at St. Vincent and joined the staff as a gastroenterologist in 2001. He served as president of the medical staff from 2022 until his retirement in 2024.


STEVEN FREER, M.D. MEDICAL EDUCATION
“The practice of medicine is an extraordinary gift.”
“Back in 2003, I was running a very large residency program in Virginia when I arrived at St. Vincent to interview for the Brill Chair of Medicine position. I was struck by the incredible pride that people took in St. Vincent.
“More than one person there said to me, ‘Most of the people in this community would tell you that St. Vincent is the best hospital in Portland, hands down.’ I was impressed by the commitment to excellence throughout the environment. Everybody I met on the professional staff was polished, had excellent credentials and was committed to providing the best possible care.

“I continue to be inspired by the people I work with. I have great faith in the quality, leadership and decency of the medical staff. The nursing staff is excellent, and has been from the day I walked in the door.
“The hospital feels like a place of great comfort, not only professionally but personally. My grandkids were born here; my son and I had surgeries here.
“For residents in our internal medicine residency program, our goal is to help them believe that they are part of something magnificent. The practice of medicine is an extraordinary gift. It is a privilege to be somebody’s doctor, and it’s a privilege to work in a place like St. Vincent.”
Dr. Freer succeeded Kenneth Melvin, M.D., as the hospital’s Isidor C. Brill Chair of Medicine in 2003. He continued to serve in that role until retiring in January 2025.

“Each of us makes a difference to at least one patient and one family, every single day.”
Years after helping create Providence Brain and Spine Institute, Frederick “Rick” Waller, M.D., looked back on serving alongside fellow physicians and other Providence people. “It has been a great team effort,” he said. “I retire with great satisfaction, knowing that each of us makes a difference to at least one patient and one family, every single day.”


In 1980, Dr. Waller and Calvin Tanabe, M.D., opened a neurosurgery practice at St. Vincent. They, along with neurologists and other neurosurgeons, joined in a journey of innovation and growth in patient care, applying such advances as surgical operating microscopes, CT scanning and intraoperative MRI.
Continuing medical advances, coupled with Dr. Waller’s inspirational leadership, led to the formation of Providence Brain Institute in 2004. Its reputation soon attracted other top physicians. Today, Providence Brain and Spine Institute provides comprehensive care ranging from treatments for stroke and ALS to brain tumor surgery and neurologic critical care.
After moving from the surgical suite into other roles, Dr. Waller made another significant impact: He implemented standardized surgical order sets with the goal to “make doing the right thing easy.” His work dramatically reduced the risk of surgical errors in Providence hospitals and beyond and contributed greatly to patient safety, says former administrator Janice Burger. “Overall, I think he saved thousands of people’s lives.”
Dr. Waller joined the St. Vincent medical staff in 1978 and retired in 2012. After stepping down in 2004 from performing surgery, he took on leadership roles including medical staff president, medical director of quality management and chief of surgery. Dr. Waller passed away in 2022.

FATHER FREDDY OCUN, AJ PASTORAL SERVICES
“Knowing that a spiritual care provider is available to listen … makes St. Vincent stand out as a place of hope, healing and wellness.”
“From the very day I joined Providence St. Vincent as a chaplain in 2005, coming from my home village in northern Uganda and a culture so far away from Portland, Oregon, I felt welcomed and valued in this community of caregivers. I witnessed our Mission and values lived out in the way other caregivers treated me, as well as the people they are called to serve.
“I am honored to have led the pastoral services department for the last 15 years as we have cared for the spiritual needs of our ever-changing, growing and diverse community of patients and caregivers. We believe that each person deserves whole-person care – excellent and compassionate care of mind, body and spirit regardless of belief, background, language, culture or ethnicity.
“This belief has informed our development of spiritual care initiatives such as music-thanatology, the Sister Rita Peace Garden, Providence Rooms for caregivers’ meditation or reflection, peer support programs and critical incident debriefings. In affirmation of this belief, we work with leaders from multiple faith communities, who visit patients on request.
“For patients and caregivers alike, knowing that a spiritual care provider is available to listen to their story and to provide support – through lifechanging events, difficult diagnoses, loss and grief – makes St. Vincent stand out in our community as a place of hope, healing and wellness.”
Father Freddy is a Catholic priest of the Apostles of Jesus order. Touched by how the hospital community comes together each year for the caregiver memorial service, he says, “In the words of Psalm 100, our Mission and ministry witness to our ongoing conviction that ‘Love is eternal, and faithfulness lasts forever.’”


MARTIE MOORE, RN NURSING
“Magnet exemplifies the best, the heart, of nursing.”

“As chief nursing officer at St. Vincent from 2007 to 2014, I had the opportunity to lead us through two Magnet nursing redesignations. The hospital was really focused on elevation of nursing practice and on quality of care.
“For me, Magnet exemplifies the best, the heart, of nursing. The first time we received our redesignation, I saw the pride that swelled throughout the organization.
“A CEO once said to me at the start of my career, ‘Beat me there, Martie. Don’t meet me there.’ So many times, St. Vincent nurses would beat me there with ideas on how we could improve our care, our nursing practice, our environment. They showed a spirit of inquiry while acknowledging our past.
“When we look at our heritage, the spiritual connection is one of the things I value most about our nursing practice – that we understand mind, body and spirit, and that our nurses are very willing to embrace that holistic aspect.
“There was a grounding moment for me one day when I visited the gravesite of Mother Joseph. As I stood there as a nursing leader, I thought about the tenaciousness, the unwillingness to be defeated, that she and the other Sisters of Providence demonstrated. And yet, they had the kindness of spirit, the graciousness. I wanted to exemplify those qualities during my time with St. Vincent.”
Under Martie’s leadership, Providence St. Vincent was redesignated as a Magnet hospital by the American Nurses Credentialing Center in 2009 and 2014. Long after her Providence service, Martie continued to quote the Providence byword, “Know me, care for me, ease my way.”

“Going viral is a bad thing in health care, but it’s a great thing on YouTube.”
Pink gloves and plenty of smiles flashed when St. Vincent staffers showed off their dance moves in a playful video supporting breast cancer awareness in 2009. “Going viral is a bad thing in health care, but it’s a great thing on YouTube,” noted Martie Moore, RN, then-chief nursing officer. “People appreciated the joy and the hope we showed.”
Some 200 caregivers danced to the beat of the hit song “Down,” by Jay Sean, in the life-affirming video produced by Medline Industries. The video surpassed 5 million views on YouTube in just over a month and gained national media coverage.
Countless calls and messages praising the “Pink Glove Dance” poured in. Many came from breast cancer patients, survivors and loved ones who felt touched by the uplifting images of hospital
workers rallying for the health cause. Some viewers even applied for jobs at the hospital.
“For me,” said Martie, “the Pink Glove Dance really exemplified the spirit of St. Vincent and the love that employees had for one another, the hospital and the sisters.”

Shortly after the video took off, a group of sisters surprised Martie before a meeting. “They had boxes of pink gloves,” she said, “and they wanted me to teach them how to do jazz hands so they could do that at their governing board meeting.”
Martie danced in the video in honor of her mother, a breast cancer survivor, and recruited scores of her fellow caregivers to participate. Medline donated some of the money from the sale of its pink gloves to pay for mammograms for women who couldn’t afford them.





Many who worked and practiced at Providence St. Vincent during this time will remember the 2010s as an Epic decade. Following the Health Information Technology for Economic and Clinical Health (HITECH) Act of 2009, health care providers had strong incentives to adopt electronic medical records. Recognizing the clear benefits to patient safety, quality, privacy and data security, Providence made the decision to implement a single platform –the Epic electronic health record system – across all of its facilities statewide.
On April 21, 2012, Providence St. Vincent became the first Providence hospital in Oregon to go live with Epic. The launch culminated months of planning, hardware and software conversions, and training. From winter to spring, reported the hospital’s Chronicles, it was “all Epic all the time” at the hospital. Epic trainers took over every conference room and classroom, leading more than 2,300 classes for some 10,000 attendees. The transition was “an enormous commitment,” “an amazing dance” and an “incredible collaboration,” said Marla London, RN, who coordinated the onsite training effort.
Other technological transformations also were occurring in every corner of the hospital. Specialty



drugs, genomics and precision medicine were improving diagnostics and opening up new avenues of treatment for a multitude of conditions.
One major clinical advancement was the development of the SAPIEN heart valve. The artificial, collapsible valve made it possible to perform heart valve replacements through a catheter, without open heart surgery. Providence St. Vincent was the first medical center in Oregon, and one of the first in the country, to successfully implement this new technology.
Meanwhile, telehealth was expanding the reach of the hospital’s care far beyond its walls. In 2010, a new telestroke program made it possible for stroke specialists at Providence St. Vincent to examine patients in rural hospitals remotely, accelerating access to lifesaving treatment. The following year, a new tele-ICU program began offering remote consultations for patients needing intensive care in outlying hospitals with fewer resources. Closer to home, many patients who needed routine primary care and follow-up were now taking advantage of virtual visits, which added a new level of convenience and access. It was a brave new world, and with a global pandemic looming, the timing of these advancements could not have been more fortuitous.
Providence Brain Institute launches a telestroke program, linking Portland-based neurologists to Providence hospitals in Medford, Seaside, Newberg and Hood River. The program enables stroke specialists to examine patients remotely while providing immediate consultation services to community providers.

APRIL: My Little Waiting Room opens, providing free drop-in childcare for families while they receive medical care at Providence St. Vincent.
SEPTEMBER: Providence St. Vincent adds tele-ICU to its list of telehealth services. As in the telestroke program, critical care physicians at Providence St. Vincent now can provide consultations remotely to community hospitals.
FEBRUARY: Providence St. Vincent becomes one of only a few medical centers in the United States, and the first in Oregon, to successfully implant a SAPIEN heart valve. The collapsible aortic heart valve is inserted into a patient using minimally invasive techniques.
APRIL 21: Providence St. Vincent becomes the first Providence hospital in Oregon to utilize Epic, an electronic medical record system.
OCTOBER: Upgrades to Providence St. Vincent’s main building begin. These include seismic retrofitting, a new exterior and renovated patient rooms.

JULY: The emergency department at Providence St. Vincent opens a space designed specifically for children and their families. It is the only dedicated children’s emergency department on Portland’s west side.

Providence opens Basecamp Prevention + Wellness on the Providence St. Vincent campus. It provides heart clinics, imaging and screening, rehabilitation and education. Recognizing that 80% of heart disease is preventable through lifestyle changes, Basecamp also offers nutrition and cooking classes, yoga, tai chi, stress management and support groups.

SEPTEMBER: Providence St. Vincent receives Magnet nursing designation for the fifth consecutive time since its original designation in 2000, becoming Oregon’s most longstanding Magnet hospital. The American Nurses Credentialing Center recognizes Providence St. Vincent for outstanding patient care, nursing excellence and innovations in nursing practice.
OCTOBER: The Sister Rita Peace Garden opens outside of the emergency department. The space is dedicated to Sister Rita Ferschweiler, SP. A Sister of Providence for 77 years, she became a nurse at St. Vincent in 1956 and later served as director of nursing and then hospital administrator.
“Our caregivers are beautifully capable of continuing the Mission.”
“I loved Providence St. Vincent. There was something about walking in the door – a brightness, and a graciousness to our caregivers. Every single person was attentive to your needs.
“Sometimes I’d forget to take off my badge, and people out in the community would say, ‘You work for Providence. I love Providence.’ It was beautiful to see that expression of the reputation that I feel we still have.
“In 2010, the sisters recorded their ‘Hopes and Aspirations’ to ensure that their Mission is carried into the future. They reminded us that we won’t always have a blueprint, so we need to walk forward in faith, using our creativity, discernment and wisdom to solve issues.

“I want people to know that our caregivers are beautifully capable of continuing the Mission. Even if you don’t see the sisters here, you can embody their spirit by knowing that you’re carrying out the work that we began.
“And you are vital. Talk to anyone who’s had care at Providence St. Vincent, and what they remember is not so much the post-op instructions as the person who held their hand right before they went into surgery and told them, ‘It’s going to be OK.’
“The next 150 years might look different. But this ministry will go on, by the grace of God and by the devotion and dedication of our caregivers.”
Sister Maggie entered the Sisters of Providence in 1969, beginning in teaching and then coordinating women’s and children’s services and educational programs for seniors through Providence Health & Services in Portland. She was the Mission integration director for Providence Health Plans from 1998 to 2016. Today, as a sponsor for Providence St. Joseph Health, she helps guide its ministry.

MELISSA MOORE
FRIEND AND PARENT
“My Little Waiting Room truly is a place where children thrive as families heal.”
“After my dear friend Amy Paterson went through multiple cancer treatments, she and I approached the Providence St. Vincent Medical Foundation with an idea. As fellow moms, we wanted to bring drop-in childcare to the hospital. We made the case that families visiting St. Vincent are often anxious or in crisis, and having on-site childcare would give parents one less thing to worry about. Our idea received immediate and enthusiastic support.
“Seeing that it would help fulfill the hospital’s commitment to ‘ease my way,’ the foundation presented the idea to the administration. With the foundation’s support, St. Vincent formed a team, hired a professional childcare provider, created a space at the hospital, and opened My Little Waiting Room in April 2010.


“Since then, the free drop-in service has had more than 60,000 child visits. It has provided trusted childcare for parents heading to tests, outpatient treatments or physical therapy; unexpectedly landing in the emergency room; visiting relatives in the ICU; bringing another child to the Gerry Frank Center for Children’s Care; or bringing another child into the world in our maternity center.
“Families have thanked My Little Waiting Room for making it easier to access medical care. This nonprofit service, still funded by the foundation, has received the Providence Mission Leadership Award and national recognition. It truly is a place where children thrive as families heal.”
Melissa is now a member of the foundation’s council of trustees. S he credits Dick Clark, the foundation’s director at the time, and Alex Jackson in administration for helping to make My Little Waiting Room a reality. Her friend Amy (in red at right with Melissa), who helped conceive the idea, passed away in 2018.

“I
enjoyed patient care. … That’s really what it’s all about.”
For more than 100 years, alumni of the St. Vincent Hospital School of Nursing have come together at annual reunions to reconnect and reminisce. Although the school no longer exists, its influence on nursing in Oregon continues.
The Sisters of Providence started the nursing school in 1892 to support the hospital’s growing medical staff, graduating the first full, eight-person class in 1897. In 1934, the school began partnering with the University of Portland to offer a four-year degree program.
When the hospital-based school closed in 1962, the program moved to the university, which assumed oversight of the College of Nursing, but students continued to train at St. Vincent. Today, Providence Health & Services continues to support nursing education by sponsoring a scholarship program for future nurses at the university.
2012 marked the 100th reunion of the St. Vincent nursing school alumni. One faithful alum who attended the celebration was Dee Wallo, RN, a


1946 graduate. The longtime nurse leader enjoyed a 40-year career at St. Vincent, bridging both the Westover Road and Barnes Road locations. “It’s two different worlds,” she said of the two hospitals, “and I think I had the best of all of it. I worked with really good people.”
Reflecting on her career, Dee added, “I enjoyed patient care, patient contact. That’s really what it’s all about.”
Dee Wallo retired in 1987 as the associate director of nursing services, overseeing critical care at Providence St. Vincent. During her career, she helped care for the first open heart surgery patients of Albert Starr, M.D., and the first vascular surgery patients of Toshio Inahara, M.D. She passed away in 2018 at the age of 93.


KRISTINE BELL, RN WOMEN AND CHILDREN’S HEALTH
something to be proud of
“The word that comes to mind is excellence.”

“When I think of St. Vincent’s culture, the word that comes to mind is excellence. The physicians, midwives, nurses, anesthetists, everybody who has worked in obstetrics really does commit to that.
“One case that stands out led to redesigning the electronic health record to screen for risk of maternal hemorrhage. I can only imagine how many lives that has helped.
“We also got involved in national quality initiatives for improving neonatal care, and brought in high-reliability principles for promoting safety and reducing harm. And in 2013, we opened a perinatal special care unit to serve high-risk moms and babies before and after delivery.
“At our NICU reunions, the kids who graduated from the neonatal intensive care unit would come back to St. Vincent with their families. I remember all the love and hugging that they shared with us. It was so wonderful to see these kids grow up.
“As we face the challenges in health care –economic pressures, an aging population – it’s good to look back and remember what made us so high-quality in our care, and to build on that in the future.
“So much has happened in 150 years. And so much more will happen within this ministry. To be a part of that history, to contribute every single day, is something to be really proud of.”
Kristine joined St. Vincent in 1996, and worked in women and children’s health as a nurse, educator, manager, director and chief nurse executive. She now serves as the executive director for the Women & Children’s Institute in the central division for Providence St. Joseph Health.

Please join us as we welcome our NICU graduates to the
DANIEL OSERAN, M.D. CARDIOLOGY
“We’ve been able to screen more than 40,000 kids.”

“Cardiologist Jamie Beckerman, M.D., came to me one day and asked if I’d seen the news story about a high school basketball player who had dropped dead on the court. We would see these terrible tragedies every once in a while. ‘Some of these could be prevented,’ Dr. Beckerman told me, ‘if we’d screen high school athletes before they participated in sports. A simple EKG screening can pick up that needle in a haystack.’
“That was the genesis of a Providence program he started called Play Smart. With philanthropic support from the community, we’ve been able to screen more than 40,000 kids in the community over the last 10-plus years.
“Dr. Beckerman went on to say, ‘Look, we really need a broader prevention and wellness strategy for our heart institute.’ And he created a large series of programs around prevention – diet, exercise, mindfulness, all of that – called Basecamp.
“Basecamp has really become a model for prevention and wellness programs in the greater Providence system. It’s a key thing that we’ve done.”
Dr. Oseran is the executive medical director of Providence Heart Institute of Oregon. The preventive Play Smart program, the brainchild of Jamie Beckerman, M.D. (right), screens young people for certain heart rhythm disorders and other cardiac conditions. Basecamp Prevention + Wellness focuses on “The 80% Opportunity” – the concept that about 80% of heart disease is preventable through healthy behaviors.




TRICIA ROSCOE PHYSICIAN SERVICES AND DEVELOPMENT
“I watched as their quiet presence lent courage and strength.”
“Once upon a time, I was a newly minted leader just starting out at St. Vincent. I remember walking the halls and seeing the amazing photo history of the Sisters of Providence and learning the stories of their many ministries.
“What struck me most over nearly 17 years with the health system was how the leaders I grew up with so loved the Mission of the sisters, and how tirelessly they worked to keep it alive.

“I had the privilege of getting to know some of the sisters who worked with us when I began –Sister Karen, Sister Barbara, Sister Maggie, Sister Suzanne, Sister Scholastica. I watched as their quiet presence lent courage and strength to making hard decisions in the face of challenges and, equally important, how they reminded us to celebrate every good thing.
“As the sisters retired and handed over the reins of leadership, I saw and experienced the same courage, faith and grace in so many Providence leaders. And always, at the core, was the Mission to serve those most vulnerable in our communities. Those leaders had a profound impact on me and on the type of person and leader I wanted to be.
“When I think of my time at Providence, I will always treasure those leaders who shared their joy of serving and their passion for those we served.”
Tricia’s Providence career spanned the years from 1997 to 2013. She began as director of Mission integration at Providence St. Vincent and held several regional and system roles as leader of Providence Physician Services and Development.

On Jan. 20, 2020, a 35-year-old man was admitted to Providence Regional Medical Center in Everett, Washington, with a novel virus never before seen in the United States. “There had to be a first case somewhere,” epidemiologist Scott Lindquist, M.D., told reporters, and it happened to be at a Providence hospital. From that day on, the world changed.
The impact of COVID-19 on Providence St.Vincent was swift and dramatic, and the hospital’s caregivers responded with remarkable courage, agility and compassion. As patients filled hospital beds, caregivers labored for long hours under extreme infection-control measures to provide compassionate care while protecting other patients and staff members. Soon, the need for care exceeded resources to such an extent that the Oregon National Guard was enlisted to help in any way they could.
As the pandemic wore on, the hospital paused elective surgeries to make room for increasing numbers of COVID patients. A specialized clinic opened to see “long-haulers” with lingering virus symptoms. And new supportive services attempted to address the very real problem of caregiver burnout. Still, many caregivers near retirement age chose to leave direct patient care, leading to significant staffing shortages.



Necessity, however, truly is the mother of invention. This time of great need became a catalyst for technological ingenuity – particularly in artificial intelligence. New applications of AI in virtual care, patient-treatment algorithms, vaccines and other pharmaceutical developments finally began to ease the strain on frontline care, and caregivers, at last, were able to catch their breath.
Good health care happens in the moment: A timely diagnosis. A lifesaving intervention. A hand on a shoulder. At Providence St. Vincent, each moment is influenced by our past and the Mission of care that brought us here.
Providing the best care for our community also requires continually looking ahead to anticipate where the next great need will be. “Tomorrow Starts Today,” an ongoing capital campaign launched in 2024, will support expansions in two urgent areas of need: Providence St. Vincent’s emergency department, the busiest in the Portland metro area, and Providence Heart Institute, a national leader that is seeing many more critically ill patients.
Other changes will surely come. Guided by the Mission of the Sisters of Providence, and supported by the community, Oregon’s first and future hospital will stand ready.
The COVID-19 pandemic reaches Oregon on Feb. 28. Governor Kate Brown declares a state of emergency on March 8. On March 16, Providence Health & Services, Kaiser Permanente, Legacy Health and OHSU form a coalition to better address the outbreak. Providence St. Vincent caregivers continue to rise to



The West Pavilion is renamed the Phil and Penny Knight Pavilion. The Nike co-founder and his wife have generously supported Providence for many years.
Providence St. Vincent receives the top ranking from Healthgrades, America’s 50 Best Hospitals Award. The medical center also earns the Top 25 Environmental Excellence Award, the highest honor for hospitals from Practice Greenhealth.



JULY: Providence Heart Institute performs its first heart transplant. Thanks to a major gift from Phil and Penny Knight, the transplant program was established the year before.
Providence announces the “Tomorrow Starts Today” capital campaign, with $177 million in investments to address the most urgent health care challenges in Portland. Work begins on expanding the emergency department and cardiac critical care facilities at Providence St. Vincent.

JANUARY: Ray Moreno, M.D., is named chief executive of Providence Oregon’s West Service Area, becoming the first physician ever to lead Providence St. Vincent.

JULY 19: Providence St. Vincent celebrates its 150th anniversary.
JANICE BURGER
HOSPITAL ADMINISTRATION
“It is the most heart-wrenching and powerful thing, this love that is just put out there for the family.”
“It’s a devastating moment, when a family learns that their loved one is not going to make it, but they feel some solace when they have an opportunity to donate a heart to save another life.
“When Providence St. Vincent became a heart transplant center, a small group of people led by nurse leader Andrew Stuchiner met to talk about how best to honor families during these last moments of the life of their loved one. And they created the walk of honor.
“First, the caregivers gather in the room with the patient and have a prayer or reflection with the family. Then, when it’s time to move the patient from critical care down the long hallway to the surgical suites, they make a call over the overhead. And every person who can – from doctors

and nurses to housekeepers, groundskeepers and administrators – drops what they’re doing and comes to that hallway for the procession. And they all line the hall in silence, standing together in honor of this family.
“It is the most heartwrenching and powerful thing, this love that is just put out there for the family as they’re giving the greatest gift. That’s St. Vincent at its best, doing things that make a difference to patients and families.”
Janice joined St. Vincent as an administrative fellow in 1986 and stayed with Providence for 37 years, serving as the hospital’s chief executive from 2005 to 2021 before retiring in 2023. She helped expand and renew the hospital campus and added many new services to the heart, brain and spine, and women and children’s programs. The hospital performed its first heart transplant in 2020.

JENNIFER BURROWS, RN NURSING LEADERSHIP AND HOSPITAL ADMINISTRATION
“This place will change you. And it changes you for the better.”
“While I was Providence St Vincent’s chief nursing officer, the main hospital tower underwent a seismic retrofitting. A new exterior was created that added three-and-a-half feet to the patient rooms to play with. We spent a lot of time considering how to use that extra space for the benefit of patients and their families. Working through the challenging renovation, like a board game with moving pieces, was a bonding time for all the medical/surgical teams working together.
“I think that experience set up St. Vincent to respond well to the COVID-19 pandemic. Once again, we were in a situation where we didn’t have the answers but were going to use the best evidence, together, to figure out how to take care of our community. People really leaned in and said, ‘I’ve been called to this profession, to taking care of patients. Teach me how to keep myself and my family safe – but I’m here and I’m ready to serve the community.’
“After having nursing leadership roles with Providence, I returned to St. Vincent in the spring of 2021 as chief executive.
“We stand on the shoulders of the people who have been here before us. It’s a privilege to get to work at St. Vincent. Whether you come for a while or you spend your whole career here, this place will change you. And it changes you for the better.”
Jennifer joined Providence St. Vincent in 2014 as chief nursing officer. She became the regional chief nursing officer in 2019, then returned to Providence St. Vincent as CEO in 2021. Jennifer was appointed chief executive, Providence Oregon, in 2024.



RAY MORENO, M.D.
EMERGENCY MEDICINE AND LEADERSHIP
“Oh, I get it. It’s not just a place. It’s a culture.”
“Emergency medicine is the ‘anyone, anytime, for anything’ specialty. St Vincent’s emergency department has served the community for a very long time.
“When I was an attending at OHSU, the residents would intermittently work at St. Vincent for a ‘community’ experience. Without fail, each would return from the St. Vincent rotation happy and smiling. The residents spoke glowingly about the doctors and nurses, and were impressed by the quality of the medicine and the kindness of the interactions. I’d roll my eyes and think, ‘Enough already!’ I thought they were exaggerating.
“Then one day I got a call asking if I’d consider working there. Though I was very happy where I was, that ‘mythical place’ the residents talked about pulled at me. It didn’t take many shifts in the St. Vincent ED before I concluded, ‘Oh, I get it. It’s not just a place. It’s a culture.’
“That St. Vincent culture has been self-sustaining in the ED for almost 50 years now. ‘Self-sustaining’ may sound like it has taken no effort, but it’s the exact opposite – new caregivers inherit the tradition from those before them and then strive to evolve and improve it. Even with the everincreasing complexity and challenges of modern health care, I don’t think there are many better places to give or get care. I’m proud to have been part of that tradition.”
Dr. Moreno joined the Providence St. Vincent team two decades ago as part of Oregon Emergency Physicians (OEP), the ED’s private practice. He has served in many leadership roles, including as the ED’s medical director, OEP’s president and the hospital’s chief medical officer. In 2025, he was named chief executive of Providence Oregon’s West Service Area.


NANCY BRYANT MEDICAL
“ We have always believed that you need to support the communities you’re a part of.”
“Providence St. Vincent is in the middle of our community. We are the community. And I think it’s the medical foundation that helps keep the hospital so connected with our community and the patients we serve.
“When I first got involved with the foundation about 20 years ago, there were only a few women on the board. Now, women are very well represented, and we’ve got women in many of the top leadership roles at the hospital. They’ve really stepped forward, which is great, given that St. Vincent was founded by women.
“We have always believed that you need to support the communities you’re a part of, whether it’s the larger community or that of your child’s soccer team. If you benefit from it, you owe it your support. Our family has been blessed tremendously, so we feel a big responsibility to do what we can to help our community.
“For us, nothing touches more people in the community than the emergency department. Supporting it was just an obvious thing to do. The community needs St. Vincent. If we value having a first-class hospital, then we have to step in to support it. Because it takes our support to hang onto it.”
Nancy, a medical foundation trustee, and her husband, Andy, a lifetime trustee, are co-chairs of the Providence “Tomorrow Starts Today” capital campaign and are major contributors toward the new emergency department at Providence St. Vincent. A former public relations consultant, Nancy is a community leader dedicated to supporting education, health care, and women and children.

JANEEN MCANINCH MEDICAL FOUNDATION
“ St. Vincent has found a way to attract caregivers with heart, who can touch with empathy.”

“I got involved with the Providence St. Vincent Medical Foundation about 30 years ago at the behest of my clients and dear friends, the Clark family. Through their relationship with Carolyn Winter, the late director of the foundation, they became very engaged and provided significant funding for the Maybelle Clark Macdonald Radiation Oncology Center at St. Vincent. Carolyn played an incredible role in building the foundation and its strong, caring board. She touched many of our lives.

“For 40 years, I’ve also watched the practice of medicine through my husband, a physician who treats patients primarily at St. Vincent. I’ve seen the empathy that patients receive from every person on the staff, and the respect that the staff has for every individual, no matter who they are. When our own loved ones have needed care at St. Vincent, the service, compassion and empathy were constant throughout their entire stay.

“I’m extremely proud of St. Vincent and its outreach, particularly to Hispanic and underserved communities. Much of that care happens through the emergency department. That service for those who are most in need goes back to the Mission of the sisters who founded the organization.
“St. Vincent has found a way to attract caregivers with heart, who can touch with empathy and love the patients they care for and the people they work with.”
Janeen was president and CEO of Becker Capital Management for more than two decades. In addition to her involvement with Providence St. Vincent, she has served on the boards of the Oregon Food Bank, Meals on Wheels, Jesuit High School, Medical Teams International and other nonprofits. Her husband, Malcolm McAninch, M.D., is a retired internist.
MARTY BRANTLEY MEDICAL FOUNDATION
“Sister Rita … injected the DNA into the hospital and made it a house of hope.”
“Any successful organization needs to have two important elements. One, it has to be on plumb. That means the foundation, the structure and the vision have to be there from the very beginning. The other element is people, and the passion of those people. At St. Vincent, it all starts with the sisters. Sister Rita Ferschweiler, SP, was one who injected the DNA into the hospital and made it a house of hope.
“When you walk into a hospital, there can be a chilling effect. You’re giving your trust to somebody to make you or a friend better, and often that’s a defensive feeling. But not here. Here, it’s warm, it’s caring. You tend not to have those fears. I don’t know of any other hospital that has two harpists and an ethicist. I can’t tell you what that means in terms of comfort.
“Change will come, but as long as we infuse the organization with the importance of the individual, of the staff, of the caring, and reinforce everything that is part of our DNA, then we’ll be OK.
“We are one of the top 50 hospitals in the United States, and consistently so. The degree of excellence that St. Vincent has achieved is pretty astounding. Speaking for the trustees, we look forward to the next 150 years of excellence with St. Vincent.”
Marty has been a Providence St. Vincent Medical Foundation trustee for some 35 years. Known for his long history in broadcasting and civic engagement, he has served as president of KPTV-TV and as chair of the Portland Development Commission, Portland Chamber of Commerce and Portland Art Museum. Marty’s three sons were born at Providence St. Vincent.



Anot-for-profit hospital is a collaborative endeavor. It takes a community to build and sustain it. When the Sisters of Providence brought their Mission of care to Oregon, they knew they could not achieve it alone. Partnering with the community was essential.
From the first $1,000 contributed by the St. Vincent de Paul Society in 1874, to the dimes and dollars donated by local citizens during the sisters’ horseback “begging tours,” Oregon’s first permanent hospital was funded by the community. In addition to monetary support, the sisters sought the advice and counsel of their neighbors to ensure that St. Vincent Hospital would serve everyone. This close partnership with the community continues today through the Providence St. Vincent Medical Foundation.

Formed in 1969 by then-hospital administrator
Sister Rita Ferschweiler, SP, and a group of community leaders, the foundation was designed as an “action organization.” Its objective: “Creating together – joining the work of the hospital with the work of many interested citizens, to provide improved health care for now and the future.” (Vincentury, Jan. 1971)
One of the first actions taken by the foundation and its council of trustees, shortly after St. Vincent moved to Barnes Road in 1971, was to draw up a 10-year development plan for the hospital. That plan laid out the vision for the medical center of
today – a center that “assures the highest quality of care,” “trains new medical personnel for the needs of the future” and “extends the frontiers of health care.”
Within this plan, the trustees, led by business leader and public servant Glenn Jackson, committed their support and enshrined the foundation’s philosophy:
“Man searches for wisdom, freedom and a better, healthier way of life. He can only hope to reach and maintain his goals by being concerned that others achieve theirs, too.”


Since the medical foundation’s beginnings, every significant advancement in care at Providence St. Vincent Medical Center has been realized with the collaborative leadership and financial support of the community. The reflections shared in these pages show what is possible when concerned and visionary people work together for the good of all.
And there are many more examples. Just in the last year, foundation donors helped to fund specialized care for patients with dementia; warming beds and medical equipment for premature and fragile newborns; advanced training for cancer caregivers; a new fellowship in clinical ethics and health justice; and leading-edge research and treatment for multiple sclerosis.
Looking ahead, the foundation’s “Tomorrow Starts Today” campaign is focusing on two large areas of immediate and future need: emergency services and cardiac critical care. With support from the foundation, Providence St. Vincent’s emergency department – already the busiest in the Portland metro area – will expand to serve more than
100,000 patients each year. Within Providence Heart Institute, a newly designed cardiac intensive care unit will be equipped to meet the increasingly complex needs of a growing and aging patient population for the next 50 years.

“Providence St. Vincent serves everyone in our community with excellence,” says Barbara Palmer, president of the council of trustees and a longtime member. “The foundation makes it possible to provide compassionate care to our neighbors, to advance cutting-edge research, to develop new programs and to expand the hospital’s ability to serve our growing community. I’m proud of the foundation and its trustees for their huge hearts, and for allowing Providence St. Vincent to stay true to our amazing Mission of over 150 years.”



SISTER LYNDA THOMPSON, SNJM MISSION INTEGRATION
“ We are honored with the incredible privilege of being able to touch people, whether with our eyes or our hearts or our hands.”

“In my interview for the position of Mission integration director at St. Vincent, I learned that my role would be to tell the stories of this hospital and to help carry forward the legacy that the Sisters of Providence left us. That tied in with my own belief that Catholic health care has a vision that needs to be communicated – a vision rooted in the heritage of the sisters, but being lived out by lay leadership.
“St. Vincent was a welcoming community, with highly energetic, ambitious leaders often looking for the next possibilities. Very visionary, and I was impressed with that.
“We are a human organization, with warts, wrinkles and all the limitations of being human. But we do the right work. We are honored with the incredible privilege of being able to touch people, whether with our eyes or our hearts or our hands.
“When I do new-caregiver orientation, I find that the people coming in are very attracted to our Mission. That’s because we claim, and work actively on, the value of integrity – doing the right thing when no one is watching, knowing we can be trusted. I think our people want that more than anything.
“That’s been our history. There are challenges, because the winds of change are blowing. But integrity means you stand steadfast. That word is in our Mission statement: ‘steadfast.’”
Sister Lynda is a Sister of the Holy Names of Jesus and Mary. She joined Providence St. Vincent in 2005 as the director of Mission integration and continues to serve as the chief Mission officer today. Mission integration arose from the sisters’ desire to ensure that the Mission was carried forward in the service of every caregiver, every day.

As expressions of God’s healing love, witnessed through the ministry of Jesus, we are steadfast in serving all, especially those who are poor and vulnerable.
Financial support for “Cornerstone: Reflections on Oregon’s First and Future Hospital” was provided by the Providence St. Vincent Medical Foundation.
For sharing the stories of Providence St. Vincent, the foundation thanks:
Deb Tuke Bahlman, RN
Kristine Bell, RN
John Berland, M.D.
Barbara Blakeley
Marty Brantley
Nancy Bryant
Janice Burger
Jennifer Burrows, RN
David Cook, M.D.
David Craig, M.D.
Katherine Criswell, RN
Paul Duwelius, M.D.
Woodruff English, M.D.
Akiko Erwin
John Fletcher
Dolores Foglio, RN
Karen Foley
Steven Freer, M.D.
Michelle Haun-Hood, RN
Curtis Holzgang, M.D.
Kathy Johnson, RN
Sue Johnson, RN
Susan Kirchoff, RN
Nicholas Kockler, Ph.D.
Lynne Magner
Janeen McAninch
John McDonald, M.D.
Kenneth Melvin, M.D.
Martie Moore, RN
Melissa Moore
Ray Moreno, M.D.
Laura Moya
Karen Neilson (Zivin), RN
Ed Nelson
Father Freddy Ocun, AJ
Miriam Odermann, RN
Daniel Oseran, M.D.
Barbara Palmer
Sister Maggie Pastro, SP
Nancy Roberts
Tricia Roscoe
Douglas Shumaker, M.D.
Adrienne Simmons
Donald Sutherland, M.D.
Jeffrey Swanson, M.D.
Sister Lynda Thompson, SNJM
Greg Van Pelt
Don Vollum
Kristy Wayson, RN
Karen Weylandt, RN
Ken Zinsli
Valuable assistance also was provided by these foundation team members and friends:
Amy Brooks
Keri Brown
Kelsi Charlesworth
Dick Clark
Kevin Finn
Nicole Philippi
Shelly Werner
For the images that illustrate the Providence St. Vincent story, we are grateful to:
Lara Janzen Photography
Library of Congress
The Oregonian
Providence Archives, Seattle
Providence Health & Services
Providence St. Vincent Medical Center
Virginia Garcia Memorial Health Center
Many of the reflections shared in these pages began as recorded conversations. For providing both video and still photography for our anniversary celebration, we thank the Providence St. Vincent Surgical Services videography team:
Eric Mellor
Nick Perkiss
Haden Peterson
Hugh Potter
Sawyer Purman
Thi Truong
In partnership with Historical Research Associates, Inc., “Cornerstone: Reflections on Oregon’s First and Future Hospital” was written, edited and designed by Providence St. Vincent alumni:
Sally Booth
Katherine Keniston
Ellisa Valo
Greg Van Pelt
Lynda Werner
The foundation sincerely appreciates everyone involved in this project for reminding us of the people and events that shaped the soul of Oregon’s first and future hospital.

All I know of tomorrow is that Providence will rise before the sun.
Our Mission
As expressions of God’s healing love, witnessed through the ministry of Jesus, we are steadfast in serving all, especially those who are poor and vulnerable.
Our Values
Compassion • Dignity • Justice Excellence • Integrity
Our Vision Health for a Better World
Our Promise
“Know me, care for me, ease my way.”