The Official Publication of the Illinois Nurses Foundation Quarterly publication direct mailed to approximately 4,500 RNs and electronically via email to 96,000+ RNs in Illinois.


The Official Publication of the Illinois Nurses Foundation Quarterly publication direct mailed to approximately 4,500 RNs and electronically via email to 96,000+ RNs in Illinois.

On April 16, 2024, student nurses from across Illinois met for the 26th Annual Student Nurse Political Action Day (SNPAD). The event was held at the Bank of Springfield Convention Center in Springfield, Illinois. This year, SNPAD brought together nearly 600 nursing students from 23 nursing schools for a day of learning, networking, and advocacy. The day’s events and conversations had a lasting impact on nursing students.
Many Nursing Schools Represented
Of the 23 schools represented, City Colleges of Chicago – Malcolm X College had the most students attending! Thank you, City Colleges of Chicago – Malcolm X College, for your strong commitment to political action and empowerment! See the full list below.
STOP THE BLEED® Training
We appreciate Loyola University Medical Center’s willingness to provide STOP THE BLEED® Hands on Skills training to students and faculty in attendance. A special thanks to Amanda Oliver BSN, RN, CCRN, CPST for leading the workshop. The hands-on skills classes took place in the morning. Nearly 25 students participated in the workshop!
Advocacy-Focused Programming
The day-long conference featured a keynote address by Marcus D. Henderson MSN, RN, called “Student Nurse to Nurse Advocate: A Journey of Learning, Leadership and Action.” His inspiring and empowering keynote address gave practical advice for how new nurses can discover their passion and specific interest within healthcare, find mentors/sponsors, how to promote self-awareness and growth and much more!
Later, Debbie Broadfield of Capitol Edge Consulting LLC discussed “Legislative Hot Topics.” Debbie Broadfield, President of Capitol Edge Consulting, LLC, has been lobbying since 2008. In 2013, Broadfield, along with Sue Clark, formed Capitol Edge Consulting LLC, a BEP certified women owned and operated Illinois lobbying and consulting firm focused on relationship building, advocacy, and achieving desired results. Broadfield served as Vice President from 2013 until 2023. In January 2024, she became President of Capitol Edge Consulting, LLC. We were honored to have her share with us!
2024 Prize Winners
SNPAD included lots of opportunities to win money and prizes through both contests and drawings.
Additionally, the poster contest winners will have their posters featured in the June issue of the statewide publication The Nursing Voice. Look for posters from Jayden Ellis, Marissa Ellis, and Claudia Seiler of Millikin University, who won $100 for their winning poster. Alec Mallinder and James Turner, also of Millikin University, won $50 for second place.
• Kevin Barna from University of Illinois at Chicago won the photo contest with a $100 cash prize.
• Olivia Bachar, Illinois Wesleyan University, won a $500 scholarship.
• Ellen Paulsey, Malcolm X College of Nursing, won the $100 student giveaway drawing.
• Tracy Smith, Illinois Eastern Community College, won the $100 faculty giveaway drawing.
Western Governors University, St. John’s College of Nursing, Emergency Nurses Association, Illinois College , Olivet Nazarene University, and many more had donated items that were won in drawings that ranged from Starbucks gift cards to books to t-shirts.
Congratulations to all who won, and a big thank you to all who participated! Our warm appreciation to all who made the gifts possible.
March to the Capitol & Rally
After door prizes and winners were announced, student nurses and faculty marched to the Capitol to raise their voices and participate in political action.
The rally was the perfect ending to a powerful day.
THANK YOU
We are so grateful to all the student nurses and faculty who attended to learn how they can be engaged in the legislative process and in advocacy work to improve their lives and the lives of their patients. We know that in so many ways, the skills and lessons students learned at SNPAD are just the beginning of a lifetime of essential political action. Your involvement is so important, and we’re so thankful for all of you and all that you do!
2024 List of Colleges Participating
Thank you to the 23 colleges and universities who included the political engagement of their nursing students in their nursing education:
• Chamberlain University
• Chicago State University
• Frontier Community College
• Graham Hospital System
• Harper College
• Herzing University
• Illinois College
• Illinois State University Mennonite College of Nursing
• Illinois Wesleyan University
• Lewis & Clark Community College
• Lincoln Trail College
• Loyola University Chicago Marcella Niehoff School of Nursing
• City Colleges of Chicago Malcolm X College
• Methodist College
• Millikin University
• Northern Illinois University
• Purdue University Northwest
• South Suburban College
• Southern Illinois University Edwardsville
• St. John’s College
• University of Illinois at Chicago College of Nursing
• Wabash Valley College
• Western Illinois University
2024 Exhibitors
Many thanks to the following 21 exhibitors for their generous support of SNPAD and student nurses!
• Blessing Rieman College of Nursing & Health Sciences
• Chamberlain University
• Emergency Nurses Association
• Grand Canyon University
• Herzing University
• Hospital Sisters Health System
SNPAD 2024: A Powerful Day of...continued on page 3
We are thrilled to announce an exciting new partnership that promises to enhance your reading experience! The Illinois Nurses Foundation and ANAIllinois have teamed up with Nursing Network to bring you our esteemed quarterly publication, Nursing Voice.
About Our New Partner, Nursing Network:
• Award-Winning Technology: Dedicated to revolutionizing communication within the nursing industry.
• Community and Connection: A platform built to strengthen ties within the nursing community by connecting members with their associations, colleagues, and vital resources.
• Mission-Driven: Committed to continuous improvement and innovation, Nursing Network listens to its users and evolves to meet your needs.
As part of our new partnership with Nursing Network, Nursing Voice is transitioning from a traditional newspaper-like format to a dynamic, professional online responsive publication. This evolution is designed to enhance how you access and interact with the content that matters most to you.
News for Nursing Voice Readers! continued on page 5
As we bask in the warmth of the summer sun, I am thrilled to share some exciting news and upcoming events from the Illinois Nurses Foundation (INF). As the president of INF, I am honored to lead an organization dedicated to supporting and recognizing the outstanding contributions of nurses across our state.

First and foremost, I am delighted to announce that we will soon be unveiling the recipients of this year's prestigious INF scholarships. These scholarships are a testament to our commitment to fostering the next generation of nursing professionals. Through these awards, we aim to empower aspiring nurses to pursue their educational goals and make a positive impact on healthcare in Illinois and beyond.
In addition to celebrating academic excellence, we are eagerly anticipating another milestone event in the nursing community: the 10th annual 40 Under 40 Emerging Nurse Leader Event. Set to take place on September 19th, 2024, in Lisle, this event holds a special place in our hearts as we reflect on a decade of honoring remarkable nurses who are making waves in their careers.
Since its inception, the 40 Under 40 initiative has been a beacon of inspiration and recognition for the nursing profession. With this year’s celebration, we will have had the privilege of honoring 400 exceptional nurses who impact healthcare and the nursing profession. As we prepare to celebrate the 10th anniversary of this event, we are filled with gratitude for the opportunity to shine a spotlight on the outstanding achievements of these emerging leaders.
The 40 Under 40 Emerging Nurse Leader Event is more than just a celebration; it is a testament to the incredible talent and passion within our profession. Each honoree represents the future of nursing, and we are proud to support them on their journey to making a difference in the lives of patients and communities across Illinois.
If you or your organization would like to sponsor the 40 under 40 Emerging Nurse Leader event, please reach out to us and we would be happy to discuss all of the amazing opportunities to show your support.
As we look ahead to the remainder of the summer and beyond, I am filled with excitement and anticipation for the incredible milestones and achievements that lie ahead for INF and the nursing profession as a whole. Together, we will continue to champion excellence, empower future generations of nurses, and advance healthcare for all.
With warm regards,
Amanda
Oliver BSN, RN, CCRN, CPST President, Illinois Nurses Foundation
Dr. W. Zeh Wellington, President, ANA-Illinois
Excited. Encouraged.
Engaged. Enthusiastic.

W.
It was my honor and privilege to join the Student Nurses at the Student Nurse Political Action Day in Springfield on April 16, 2024, and to join my fellow nurses at Nurses’ Day at the Capitol on April 17, 2024. As nurses, we are well equipped to be politically active as we naturally lead and build teams, make data driven decisions, practice our listening skills with every encounter with patients, apply conflict management every day, have superior negotiation skills, we manage competing priorities and apply our communication skills with our patients, families, and fellow team members. As nurses, we are listeners and problem solvers. Nurses must lead the way. But, how? As nurses we can (and must) get involved, poll, vote, encourage others to vote, join our association, and communicate with our legislatures about policy that affects our practice every day. Please remember the Nurse Practice Act is a law that is determined by our state legislatures. If you are not
interested in speaking up politically – someone will speak up on our behalf.
On April 16, 2024, I was privileged to join others in Springfield at a legislative dinner where we had the opportunity – firsthand- to meet and talk with our leaders in Illinois. Thank you to all who attended, especially the leadership members of SNAI- Student Nurses Association of Illinois: President- Sarah Quick, 2nd Vice President- Jaden Beckwith and Treasurer- Dan Moralda. I am quite confident to add that the future of nursing is in excellent hands after meeting these inspiring students. Thank you for representing the student nurses of Illinois, for your insight, leadership, and passion for nursing.
Because of our advocacy efforts, the Nurses of Illinois have achieved a significant victory for nurses and healthcare. The Illinois Board of Higher Education (IBHE) has announced the award of $1.4 million in grants to 12 nursing schools across the state for the physical year 2024.
Remember there is no healthcare without Nurses.
Believe in the importance of elections, the importance of effecting change, the importance of voting – it is a tool for impact and change.
Thank you for your partnership, Dr. W. Zeh Wellington, DNP, RN, NE-BC President of the American Nurses Association (ANA)Illinois

INF Board of Directors
Officers
Amanda Oliver, BSN, RN, CCRN, CPST President
Brandon Hauer, MSN, RN Vice President
Karen Egenes, EdD, RN Treasurer
Directors
Cheryl Anema PhD, RN
Lisa Conley MSN, RN, CCM
Susana Gonzalez MHA, MSN, RN, CNML
Linda Olsen PhD, RN, NEA-BC, FAAN
Katherine de los Trinos-Ocampo MAT, MSN, APRN, FNP-C
Dawn Vollers MSN, RN, NEA-BC, NPD-BC
ANA-Illinois Board Rep
Jeannine Haberman DNP, MBA, RN, CNE
Stephanie Mendoza DNP, MSN, RNC-OB, C-EFM
Zeh Wellington DNP, MSN, RN NE-BC

ANA-Illinois Board of Directors
Officers
W. Zeh Wellington DNP, MSN, RN, NE-BC President
Monique Reed, PhD, MS, RN Vice President
Jeannine Haberman, DNP MBA, RN, CNE Treasurer
Gloria E. Barrera MSN, RN, PEL-CSN Secretary
Directors
Samuel Davis Jr MHA, RN, CNOR
Armando Valdez Martinez Jr. MSN, RN, MEDSURG-BC, CMSRN
Diana Ortega BSN, RN
Hannah Shufeldt MSHCM, BSN, RN
Stephanie Mendoza DNP, MSN, RNC-OB, C-EFM
Editorial Committee
Chief Editor
Lisa Anderson-Shaw, DrPH, MA, MSN
Members
Cheryl Anema PhD, RN
Deborah S. Adelman, PhD, RN, NE-BC
Nancy Brent, RN, MS, JD
Pamela DiVito-Thomas PhD, RN
Jeannine Haberman DNP, MBA, RN, CNE
Irene McCarron, MSN, RN, NPD-BC
Colleen Morley DNP, RN, CCM, CMAC, CMCN, ACM-RN
Linda Olson, PhD, RN, NEA-BC
Laura Wood DNP, RN, CMCN
Executive Director
Susan Y. Swart, EdD, MS, RN, CAE
ANA-Illinois/Illinois Nurses Foundation
Article Submission
• Subject to editing by the INF Executive Director & Editorial Committee
• Electronic submissions ONLY as an attachment (worddocument preferred)
• Email: info@ilnursesfoundation.com
• Subject Line: Nursing Voice Submission: Name of the article
• Must include the name of the author and a title.
• INF reserves the right to pull or edit any article / news submission for space and availability and/or deadlines
• If requested, notification will be given to authors once the final draft of the Nursing Voice has been submitted.
• INF does not accept monetary payment for articles.
Article submissions, deadline information and all other inquiries regarding the Nursing Voice please email: info@ilnursesfoundation.com
Article Submission Dates (submissions by end of the business day) January 1st, April 1st, July 1st, October 1st
Advertising: for advertising rates and information please contact Health eCareers, HEC_Nursing_Info@healthecareers.com
ANA-Illinois and Health eCareers reserve the right to reject any advertisement. Responsibility for errors in advertising is limited to corrections in the next issue or refund of price of advertisement.
Acceptance of advertising does not imply endorsement or approval by the ANA-Illinois and Illinois Nurses Foundation of products advertised, the advertisers, or the claims made. Rejection of an advertisement does not imply a product offered for advertising is without merit, or that the manufacturer lacks integrity, or that this association disapproves of the product or its use. ANA-Illinois and Health eCareers shall not be held liable for any consequences resulting from purchase or use of an advertiser’s product. Articles appearing in this publication express the opinions of the authors; they do not necessarily reflect views of the staff, board, or membership of ANA-Illinois or those of the national or local associations.
See photos from page 1
• IDFPR/Nursing Workforce Center
• Illinois College
• Illinois Nurses Foundation
• Illinois Public Health Association
• Indiana Wesleyan University
• Illinois State University Mennonite College of Nursing
• Memorial Health
• NCLEX Mastery
• Northern Illinois University School of Nursing
• Olivet Nazarene University
• Purdue University
• Student Nurses Association of Illinois
• St. John’s College of Nursing
• University of Illinois Chicago – College of Nursing
• Western Governors University
















Lisa Anderson-Shaw, DrPH, MA, MSN, HEC-C
Spirituality has been a part of the human experience almost from the beginning of time. The human experience includes all aspects of life, including spirituality, religion, health, and culture. The nursing profession has related to areas of spirituality since our beginning, perhaps as far back as the ancient Egyptian Society (Elhabashy & Abdelgawad, 2019).
The nursing profession in the United States began with Florence Nightingale
In 1872, the New England Hospital for Women and Children was established and with the hospital came the first nursing school in the United States. The development of the program and curriculum were influenced by Nightingale's nursing educational plans (O’Neill, 2019). From the beginning of her career, Nightingale intertwined spiritualty within nursing practice and education. Her idea of spirituality was being "intrinsic to human nature", which may also be applied to health and wholeness (Macrea,1995, para.1).
For Nightingale, the laws of science are the "thoughts of God". Because of her deep conviction about universal law, she did not believe in miraculous intervention as an answer to prayer. Human beings must discover the laws of God and apply them for health and wholeness. Prayer is attuning or joining one's personal self with the consciousness of God, which is found in the deepest recesses of one's own being. Nightingale's idea of spirituality as intrinsic to human nature and compatible with science can guide the development of future nursing practice and inquiry (Macrea, 1995).
In modern times, spirituality continues to be a special part of healthcare for many nurses, patients, and family members. The Joint Commission for the Accreditation of Hospitals includes specific standards that address spiritual needs of patients and stipulated that spiritual care should be included in medical and nursing education (Hodge, 2006).
So, how do we as nurses interact with patients regarding spirituality? Is it okay to talk with patients about their religious/spiritual beliefs as well as our own? The short answer is yes, it is okay. However, there are important guidelines that can help nurses when doing so. We must keep in mind that our actions and interactions do not impose our personal beliefs on our patients, but rather adds to our caring relationships with our patients.
Our professional Code of Ethics Provision 5 reflects on “The Nurse as Person of Dignity and Worth” which includes our own “preservation of wholeness of character” (American Nurses Association, 2015, p. 19) which may also reflect aspects of spirituality. Nurses can provide spiritual care through various actions, such as sitting with patients in silence, praying with patients and family members, providing privacy to patients, giving comfort, and assessing if patient/family would like to see a chaplain.
One of the four main principles in bioethics is beneficence, which means to be of benefit and is generally in relationship to do no harm (Varkey, 2021). Spirituality can take many forms and meanings for people and not everyone views spirituality in the same way.

FOR
At Lewis our graduate nursing students are living with intentionality, aspiring to make a difference wherever they are. Equipped with leading-edge knowledge and skills, you’ll continue to see the world in new ways
HIGHLIGHTS
Offered in multiple formats designed for the working nurse Programs can be taken parttime for added flexibility
Admission starts throughout the year –no GRE required Faculty are doctorallyprepared practitioners
Employer partnerships provide tuition discounts
(815) 836-5610 grad@lewisu.edu lewisu.edu/nursing
DNP MSN BSN to DNP MSN/MBA Healthcare Systems Leadership Nursing Education Family Nurse Practitioner (FNP)
Adult Gerontology Primary Care Nurse Practitioner (AGPCNP)
Adult Gerontology Acute Care Nurse Practitioner (AGACNP)
Psychiatric Mental Health Nurse Practitioner (PMHNP) School Nurse
POST-MASTER’S CERTIFICATES OF ADVANCED STUDY (all Nurse Practitioner tracks)
POST-MASTER’S NON-DEGREE PROGRAMS (Nursing Education and Healthcare Systems Leadership)
POST-BACHELOR’S NONDEGREE PROGRAM (School Nurse)
As nurses we have the opportunity to explore the meaning of spiritualty with our patients and their family. Exploring may be as simple as asking patients if they wish to see a chaplain, sharing a story that has meaning to you, or just spending quiet time with them.
References
American Nurses Association. (2015). Code of ethics for nurses. Author. https://www.nursingworld.org/practice-policy/ nursing-excellence/ethics/code-of-ethics-for-nurses/coeview-only/ Elhabashy, S., & Abdelgawad, E. M. (2019). The history of nursing profession in ancient Egyptian society. International Journal of Africa Nursing Sciences, 11, 1-7. https://www. sciencedirect.com/science/article/pii/S2214139119300113? via%3Dihub#section-cited-by
Hodge, D. R. (2006). A template for spiritual assessment: A review of the JCAHO requirements and guidelines for implementation. Social Work, 51, 317–326. https://doi. org/10.1093/sw/51.4.317
Macrae, J. (1995). Nightingale's spiritual philosophy and its significance for modern nursing. Image: Journal of Nursing Scholarship, 27 (1), 8-10. https://pubmed.ncbi.nlm.nih. gov/7721325/#:~:text=Prayer%20is%20attuning%20or%20 joining,future%20nursing%20practice%20and%20inquiry
O'Neill, T. M. (2019). History of professional nursing in the United States: Toward a culture of health. Nursing History Review, 27(1), 170-171. https://doi.org/10.1891/10628061.27.170
Varkey, B. (2021). Principles of clinical ethics and their application to practice. Medical Principles and Practice: International Journal of the Kuwait University, Health Science Centre, 30 (1), 17–28. https://doi.org/10.1159/000509119
Enhanced Features for Our Readers:
- Responsive Design: Enjoy an optimal reading experience on any device, whether you're on a computer, tablet, or smartphone.
- Easy Navigation: Find the articles and research you need with ease, thanks to a user-friendly interface and intuitive navigation.
- Faster Access: Get immediate access to the latest articles and updates, no more waiting for the next print issue.
This shift to an online platform not only aligns with modern digital consumption trends but also reflects our commitment to sustainability and accessibility. By embracing a web-based format, we reduce our environmental footprint and ensure that our valuable resources are accessible to more nurses across different regions and settings.
Continued Commitment to Excellence:
Our move online is accompanied by the same rigorous peer-review process and dedication to providing educational and research-driven content. The Editorial Committee and our new partner, Nursing Network, are dedicated to maintaining the high-quality standards you've come to expect from Nursing Voice.
We are excited to embark on this new chapter with Nursing Network We are thrilled about this update and look forward to continuing to publish a journal that brings relevant, timely, and easily accessible nursing information to your fingertips. Here's to new beginnings and continued excellence in nursing journalism!
Thank you for being a part of our community, and welcome to the future of Nursing Voice!

The Annual Nurses Day at the Capitol took place in Springfield, Illinois on April 17, 2024 and was attended by nurses from all around the state of Illinois. Registered nurses and advanced practice registered nurses attended to learn what is happening in Springfield and how to use their voice to make a difference.
The session provided attendees with the talking points necessary to educate their Senator and Representative on key issues of concern for nurses. Attendees heard from state health leaders, received education on advocacy, and found out how to connect with representatives and senators from their area. The event was successful in empowering and amplifying nursing's voices across the state.









NANCY J. BRENT, MS, JD, RN
Decisions by a patient to initiate health care treatment, or to refuse treatment, are based on many factors. Two factors that may influence such a decision are an individual’s religious beliefs and his or her spirituality.

Nancy J. Brent, MS, JD, RN
When a nursing assessment identifies these factors, their existence, and their role in a patient’s decision-making concerning treatment, must be acknowledged by nursing staff, and incorporated into the patient’s plan of care.
So, too, must be the nursing staff’s acknowledgement of the legal right of every patient to make informed decisions surrounding health care treatment. Not only is this right based in Federal laws such as the Patient Self Determination Act, it is also codified in Illinois law, including the Medical Patient Rights Act and the Patients’ Rights Established statute.
Ethics canons, including the American Nurses Association’s Code of Ethics for Nurses, also support this entitlement. The law and ethics cannons also require that consent for any and all treatments and procedures be an informed one.
An underlying legal principle of informed consent is that the practitioner who is performing a patient treatment or treatments is the one who must obtain the informed consent of the patient. This obligation is one of advanced practice nurses as well as physicians and other health team members’ responsibility.
So, what is the role of a staff nurse in informed consent after an assessment and documentation of the patient’s religious and spiritual views? Consent by a staff
nurse for care or treatment performed by that nurse is essential.
As an example, if a nurse takes a patient’s blood pressure, when a nurse asks the patient if his or her blood pressure can be taken and the patient answers yes, informed consent has been obtained. This is express consent. In the same example, if the patient extends his or her arm after asking if blood pressure can be taken, this is implied consent.
A staff nurse’s role in informed consent for treatment or procedures the nurse does not perform is different. Based on their institution’s policy, the nurse obtains and witnesses the signature of the patient and his or her dating of the signature on the informed consent form used by the facility. The nurse signs the form as the witness and adds the date next to that signature. The nurse also:
• Informs the patient of what he or she is signing,
• Documents that the patient signature was obtained, including the date and time, in the nurses’ notes,
• Addresses any hesitancy or confusion on the patient or family’s part by listening to the patient’s concerns, instructing the patient not to sign the form until the concerns are addressed by the health care practitioner performing the procedure or treatment, contacting the practitioner that is to perform the procedure or treatment, and documenting the same in the nurses’ notes,
• Contacts clergy or a spiritual adviser who can help the patient process the decision to be made concerning the prescribed treatment or procedure and documents same in the nurses’ notes,
• Provides comfort and support to the patient and the family until a resolution of the patient’s concerns occur.
The witnessing of the patient’s signature on the consent form may also require the nurse to attest to

the patient’s ability to understand what is being signed and if any questions or concerns about the procedure or treatment to be undertaken are raised.
Legally, competency to provide informed consent is presumed. However, if there is a question in the future about whether the patient was able to provide informed consent (e.g., a lawsuit by the family alleging the patient was unable to do so), the nurse may be called as a witness at trial to share his or her observations of the patient at the time the patient signed the form.
The nurse’s observations of the patient during the signing of the consent form do not form a medical determination of competency. Rather, they are simply the nurse’s statements under oath of the patient’s behavior and comments during the signing procedure.
The staff nurse also needs to remember that an adult—18 years or older—is considered competent to provide informed consent for treatment. Minors—17 and under—are not considered competent and therefore cannot provide consent for treatment, except in certain situations. The exceptions include when a minor is married or is emancipated. If no exceptions exist, it is the parent(s) or the guardian who provides consent for treatment.
A staff nurse’s role in informed consent is an important one. He or she holds the final opportunity to ensure that a patient’s religious, spiritual, and legal protections to initiate treatment, or refuse such treatment, are met.
You can access the Medical Patients’ Rights Act by placing 410 ILCS 50/0.01 in your search bar. The Patients’ Rights Established statute is located at 20 ILCS 301/30-5.
This information is for educational purposes only and is not to be taken as specific legal or any other advice by the reader. Nor does it create an attorney-client relationship. If legal or other advice is needed, the reader is encouraged to seek such advice from a nurse attorney, attorney or other professional.

Kathleen M. Clark, MSN, RN
Morgan L. Dutler, MSN, RN
Dr. Rachel Goldenstein, DNP, RN
Lisa Riecke, MSN, RN Purdue University Global School of Nursing
Abstract
The NCLEX examination serves as the defining entry point to practice for every registered nurse. The history and evolution of this exam has been influenced by historic events as well as reflecting changes in the healthcare system and role and function of registered nurses. It is the first in a 4-part series; Pulling Back the Curtain on the NCLEX, that covers the NCLEX exam from inception to its current, Next Generation form, including the driving need to close the gap between nursing theory and practice, current state including the most recent data from NCLEX pass rates, and, finally, the implications for the future of nursing education and practice.
Why a Licensing Exam
The profession of Nursing centers around facilitating optimum health & wellness of individuals, families, and communities as they navigate the healthcare continuum across the life span. Nurses play a crucial role in healthcare delivery, often linking vulnerable populations to essential healthcare services that can significantly impact survival, overall health, and quality of life (Taylor et al., 2023). Due to the impact of nurses on public health and safety, it is imperative that entry into practice is regulated to ensure competency in the knowledge and application of basic nursing principles. It has not always been the standard though, and while today’s practicing nurses have met these requirements, thoughts of the licensing process may tend to fade from view. However, looking back at the history of nursing regulation and the evolution of the NCLEX is important because it highlights the dedication to validate and advance the profession of nursing as an integral part of global health.
Historical Timeline of Nursing Regulation & Licensure Nursing began as the work of maternal figures in the home tending to the sick and has evolved throughout history as healthcare beliefs and needs changed. In the early 16th Century, in order to meet a growing need, women with criminal convictions were enlisted to care for the sick and injured in exchange for serving out jail sentences (Taylor et al., 2023). One can imagine that care was less than desirable, as was the reputation of nurses. Social reform in the 19th and 20th centuries sparked evolution, and as the role of women in general began to change, so did the role of the nurse, thanks in large part to the work of Nightingale and the development of formal nursing education.
From 1870 to 1944, individual states established their own nursing guidelines, regulations, and licensing exams. However, with inconsistencies in educational requirements and a lack of professional standards, legislation emerged as a way to safeguard both nurses and the public (Steviano et al., 2019). States established boards of nursing to help create and uphold nursing laws. Nurse registration was established and ultimately, written and practical examinations were developed. This was a monumental achievement for a young profession composed primarily of women who at the time were still fighting for the right to vote (Benefiel, 2011).
In 1944, the National League for Nursing introduced the State Board Test Pool Examination (SBTPE), which was adopted by all states, but with state specific passing score requirements. In 1978, the National Council of State Boards of Nursing (NCSBN) was established as a missiondriven organization to promote public safety and advance the profession of nursing through practice regulation. It then assumed responsibility and oversight of a national licensure by exam process in collaboration with state Boards of Nursing and adopted a new RN test plan. Then, in 1981, the name was changed to the National Council Licensure Examination (NCLEX) and criterion referenced scoring was adopted (NCSBN, 2024).
Ensuring consistent criteria for evaluation of practice readiness is crucial and one of the primary roles of the NCSBN in supporting nursing practice regulatory bodies is to develop reliable assessments of novice nurse proficiency, which is pivotal for ensuring public safety. This begins with ensuring that the NCLEX adequately reflects current nursing practices (NCSBN, 2018). The questions undergo a meticulous development and review process, led by The NCLEX Examination Committee (NEC)
made up of nurse educators and practice experts. Once endorsed by the NEC, questions are then followed by scrupulous pre-testing procedures (Clark, 2017).
In addition to evaluation of test question content, routine assessments must also include the evaluation of test results among varied test-taking demographics (Muirhead et al., 2022). Given the complexity of the discipline, evidence-based practice changes, and practice readiness indicators, the NCSBN updates the test plan every three years in order to ensure competency according to current best practice. The examination itself has undergone various changes over the years, from a traditional paper-and-pencil format to the current computerized adaptive testing model. However, guaranteeing a competent level of knowledge among successful testers remains the top priority, with consideration of fairness to all test takers through a thoughtful and rigorous design process.
The test plan outlines the structure of the exam based on Client Needs categories, Integrated Process, and Clinical Judgment. The blueprint of content distribution by category and weight in client needs categories is explained as follows (NCSBN, 2023):
• Safe and Effective Care Environment
o Management of Care (15–21%)
o Safety and Infection Control (10–16%)
• Health Promotion and Maintenance (6–12%)
• Psychosocial Integrity (6–12%)
• Physiological Integrity
o Basic Care and Comfort (6–12%)
o Pharmacological and Parenteral Therapies (13–19%)
o Reduction of Risk Potential (9–15%)
o Physiological Adaptation (11–17%)
This blueprint allows for the evaluation of knowledge and skills nurses need across diverse client populations and settings. For example, Safe and Effective Care Environment encompasses skills such as prioritizing patient needs, managing healthcare resources efficiently, and ensuring infection control measures. Health Promotion and Maintenance focuses on improving overall health, managing chronic conditions, and educating patients about healthy lifestyles. Psychosocial Integrity includes knowledge and understanding of various mental illnesses and their treatments, therapeutic communication, and addressing emotional needs.
Physiological Integrity, constitutes the most significant portion of the exam and, as the name suggests, evaluates proficiency in addressing the most basic, physiological needs reflected in 4 subcategories. This involves everything from providing basic care and comfort to mitigating potential risks. Basic Care and Comfort encompasses the essential aspects of nursing care, including assistance with mobility, pain management, provision of emotional support, and effective communication. Pharmacological and Parenteral Therapies incorporates safe medication administration and the nursing implications of pharmacology including monitoring for and responding to adverse drug reactions. Prevention of adverse events such as illness related complications, falls, healthcare associated infection and post-surgical complications is covered under Reduction of Risk Potential, and Physiological Adaptation includes concepts related to physiological response to illness and functions necessary to maintain homeostasis including

Illinois’ largest, most trusted live scan fingerprint vendor serving Illinois agencies for over 20 years.
● Convenient walk-in locations – statewide
● Simple path for out-of-state print processing for nursing
● On-site mobile fingerprinting for large groups
pathophysiology, hemodynamics, fluid & electrolyte balance and emergency care.
Integrated Processes evaluates the ability to prioritize care, adapt to changing situations, and collaborate effectively within the healthcare team. It encompasses clinical reasoning, critical thinking, clinical judgment, problem-solving, and effective communication. Clinical judgment is a crucial element that is captured within Integrated Processes and involves utilizing knowledge, experience, and critical thinking to make clinical decisions. It requires recognizing and analyzing significant information from multiple sources, and then applying it to develop and evaluate treatment plans. Evaluation of clinical judgment in addition to nursing knowledge is the crux of the Next Generation NCLEX.
Conclusion
The history of nursing regulation demonstrates a commitment to the pursuit of excellence in a profession that is rooted in the principles of promoting, maintaining and restoring health. Ensuring safe nursing practice requires evaluating the competency of entry level nurses and regulating licensure to practice based on completion of formal education and training, as well as the ability to demonstrate nursing knowledge and sound clinical judgment through examination (Steviano et al., 2019). The NCLEX undergoes a rigorous development and review process to ensure that new grad nurses are evaluated according to current best practice standards. Additionally, routine assessments of key indicators guide the revision process to ensure a fair test experience for a diverse nursing population. Finally, periodic surveys of new nurses and their employers assess the knowledge and skills of newly licensed nurses in their practice settings. This data is analyzed carefully to discover any gaps in the transition from student nurse to nursing practice and is also used to continuously refine and revise the NCLEX to provide a relevant and accurate means for evaluating entry-level understanding and application of nursing knowledge. The second article in the series will discuss the theory/practice gap and how the latest permutation of the NCLEX incorporates a clinical judgment model to evaluate practice readiness.
References
Benefiel, D. (2011). The story of nurse licensure. Nurse Educator, 36 (1), 16-20.
Clarke, S. (2017). What you need to know about NCLEX-RN. Nursing Management Springhouse, 48 (10), 21-23. http://doi. org/10.1097/01.NUMA.0000524821.72029.0a Muirhead, L., Cimiotti, J. P., Hayes, R., Haynes-Ferere, A., Martyn, K., Owen, M., & McCauley, L. (2022). Diversity in nursing and challenges with the NCLEX-RN. Nursing Outlook, 70(5), 762–771. https://doi.org/10.1016/j. outlook.2022.06.003
National Council of State Boards of Nursing (NCSBN). (2018). Next Generation NCLEX news: Examinations analysis and research. ncsbn.org/publications/ngn-news-winter2018 NCSBN. (2023). 2023 NCLEX-RN test plan https://www.ncsbn. org/publications/2023-nclex-rn-test-plan NCSBN. (2024). Explore NCSBN through the years. https:// timeline.ncsbn.org/ Stievano, A., Caruso, R., Pittella, F., Shaffer, F.A., Rocco, G., & Fairman, J. (2019). Shaping nursing profession regulation through history-a systematic review. International Nursing Review, 66 (1), 17–29. https://doi.org/10.1111/inr.12449
Taylor, C., Lynn, P., & Bartlett, J. L. (2023). Fundamentals of nursing: The art and science of person-centered care (10th ed.). Wolters Kluwer.
“YOU’RE
The phone rings and a conversation commences with a family member who is lost, not knowing what their loved one might need for care services in their home. What I have learned since 2013 as I take these calls is to remember what the caller needs most is empathy and education about appropriate services. It’s common for me to say, “You’re not alone, I’m here to guide you”, this always seems to resonate with the caller as I hear their tone change. We all know that when we feel that someone cares we can be more relaxed.
However, in the age of Covid-19 those conversations were different than the years prior. Many families could not visit their loved one, so it made things more stressful. In addition, even though case managers or social workers connected with them they felt helpless since they couldn’t see their loved one in person. They got more distressed as they were unable to describe what their loved one needed. Also, many people were being discharged needing both personal and skilled care which is a lengthier conversation and process for private duty in-home care. The calls during Covid are also more emotional or it is just that it’s the tears we here as they talk. They must be assured that it is okay sometimes to not be okay… usually followed by saying again, “You’re not alone, I’m here to guide you”.
My goal for every call- listen, educate, supply resources, and offer solutions in plain English.
During the calls I do some education explaining that home care includes any professional support services that allow a person to live safely in their home. In-home care services can help someone who is aging and needs assistance to live independently; it is helping a special needs child or adult; it is assisting anyone of any age managing chronic health issues; it is for recovering from a medical setback or surgery; or for those who have a disability. Professional caregivers such as nurses, aides, and therapists provide short-term or long-term care in the home, depending on a person's needs.
Home Health Services
Often, we hear about the doctor sending someone home with “Home Health”. This is prescribed by the doctor with an order to an Insurance or Medicarecertified home health agency that can provide intermittent skilled care, therapy or visiting nurse services. This is very short term and may provide a nurse visit once a week or some teach and learn sessions to train family members on special care needs.
Palliative and Hospice Services
A hospice and palliative care provider works alongside an existing care structure and is not meant to take the place of a medical professional. Instead, the hospice care will integrate themselves into the care routine and provide pain and symptom management within any treatment. The primary difference in hospice care compared to palliative care is that hospice is for patients with a limited lifespan. In fact, hospice care is a type of palliative care - given to address the unique needs of people with terminal illness and their families. Both palliative and hospice care help patients living with a variety of medical conditions, such as cancer, heart disease, dementia, stroke, and many others.
A licensed Private Duty Home Care many times will only be non-medical agency. These agencies can provide caregivers for companion or personal care. This is a service to assist people with their activities of daily living. Which may include bathing, ambulation, meal prep, medication reminders, light housekeeping and more. These services can be combined with Home Health or the Palliative and Hospice Services to fill the gaps in the care with hours designed to help a family have even 24-hour, 7 day a week schedule.
A licensed Private Duty Home Care may also offer skilled care services. These skilled care services are for nursing needs to complement Home Health insurance/ Medicare. Private Duty Skilled services are an out-ofpocket expense. Typically, these in-home skilled services are when a patient is be discharged with a ventilator, an ostomy/gastrostomy, feeding tube, catheter and some other nurse provided care. For Skilled nursing services through an agency, it is required that they do an assessment prior to the need for services as time is needed to process. After the in-depth Skilled assessment, some paperwork is completed by a nurse that goes to the client’s doctor. The doctor must send back approval of
the plan of care/POC and the orders for the skilled care requested. This process can take 3 to 7 business days depending on the doctor. If private duty skilled care is needed upon discharge to home arrangements need to be made about a week prior to the patient leaving a facility.
Private Duty Home Care agencies may be contracted with the Veteran’s Administration, Worker’s Compensation insurances, Long Term Care insurance organizations and more. These are things I can help remind families to check if any of these options are available as they may provide care that is paid for by that source.
Important Considerations when Choosing or Referring a Private Duty Home Care
• Has the agency received an accreditation, such as Joint Commission (aka JACHO)? Private duty agencies are not required to get an accreditation. So if they have one it was done voluntarily to show they are holding themselves to a higher standard of providing care.
• Do they provide non-medical and skilled care? This is important should a patient need to have a more advanced care in the home. It’s great to be with one agency that can do many levels of care.
• Does the agency provide a RN or a non-skilled staff member to conduct an initial assessment before the start of services? Do they follow up with reassessments at least every 90 days?
• Does the agency guarantee compatibility?
• Are the staff competency tested by a nurse? This helps the agency know if they have staff with special skills such as caring for someone with Alzheimer’s/Dementia, ALS, Parkinson’s and more.
So Many Families and Stories
The agency I am with receives nearly a 1,000 calls a year and each one is a unique story and each patient is treated individually based on their needs. During the Covid-19 pandemic the cases became more complex.
One patient who had had a stem cell procedure needed on-going infusions and personal care. One of the daughters was a nurse but had a family and job of her own so she assisted her dad when she could. Right from the start our Director of Nursing (D.O.N.) and I met with the daughters. Due to Covid our D.O.N. went to meet their dad and do an assessment for skilled and personal care services. Because the infusions orders were constantly changes due to his medical needs our D.O.N. visited often. He would have a hospital stay and we’d update and schedule for 24/7 care. When he contracted Covid-19 we called the family daily to check on him and them. He did pass due to Covid complicating his condition. One day near the December holidays one of the daughters showed up and gave each of us in the office a token of their gratitude. As with many of our clients this case hit us all emotionally as well. So, if you see a healthcare professional with a tear in their eye know it’s because of their big hearts and dedication to serving people in a special, individual way.
Linda has been with BrightStar Care of Chicago and BrightStar Care of La Grange since 2013. Her background includes a lengthy tenure in health care as well as a strong business background. While her primary focus has been management, training and marketing, Linda has taken on and succeeded at roles in Sales, Human Resources, and Project Management. Every position she’s had has allowed her to fulfil her passion to service others from children to seniors, which gives her joy each day. Her experience has led her to being on the board of the Chicago Chapter of the Case Management Society of America for multiple terms and serving on many committees for Aging Care Connections and local Health and Wellness groups.
Linda’s pathway to BrightStar began as being the caregiver for her mother and grandmother. Her personal experience has given her perspective into the growing need for high quality care in our society, from pediatrics to senior citizens. And she takes great pride in the Gold Seal of the Joint Commission Accreditation earned by BrightStar. It confirms her decision to make this company her employer of choice.
Linda has also owned Shetland Sheepdogs aka Shelties most of her life. For many years, she has been involved in activities with Shelties that have guided her to earn championship and performance titles on many of her own dogs and help others do the same.
Linda’s favorite quote, “You will get all you want in life if you help enough other people get what they want.” Zig Zigler
On behalf of the ANA-Illinois Nominating Committee and Board of Directors, the Nominating Committee invites you to participate in the 2024 ANA-Illinois Board of Directors Call for Nominations. In the coming months, the Nominations Committee will seek your help in identifying and encouraging strong and emerging leaders to seek board service and serve on the Nominations Committee. In 2024, the ANA-Illinois membership will select 10 colleagues for the following positions:
• Vice President
• Treasurer
• Two (2) Directors
• One (1) Director – Recent Student Graduate
• Three (3) Nominations Committee
• Two (2) ANA Representatives (1 rep/1 alternate)
Candidates may only apply for ONE of the following positions: vice president, treasurer, director, or Nominations Committee member. Candidates may apply to run for ANA representative or for ANA representative and one of the elected positions noted above (i.e., Vice President, Treasurer, Director, or Nominations Committee member).
The Nominations Committee members will be reaching out to members to encourage members from across the state to run for the open positions.
The Nominations Committee is charged with creating a ballot with two candidates for each open position. To ensure candidates for each position on the ballot, the Committee may request that candidates consider another elected position. Leaders and emerging leaders are encouraged to consider running for a position.

ALL TERMS ARE FOR 2 YEARS https://bit.ly/2024Electionnominations
You are invited to provide feedback regarding our state's nursing publication. We need your input in developing a new approach that meets your needs better. This questionnaire will take approximately 5 minutes to complete. In appreciation for your time, if you provide your name and preferred email address, you will be entered to win a $100 Visa Gift Card.
Survey may be accessed at the link or the QR code. https://www.surveymonkey.com/r/2WPZF2J


Nurses want to provide quality care for their patients.
The Nurses Political Action Committee (Nurses- PAC) makes sure Springfield gives them the resources to do that.
Help the Nurses-PAC, help YOU!
So. . . . . . . if you think nurses need more visibility if you think nurses united can speak more effectively in the political arena if you think involvement in the political process is every citizen’s responsibility.
Become a Nurses-PAC contributor TODAY!
❑ I wish to make my contribution via personal check (Make check payable to Nurses-PAC).
❑ I wish to make a monthly contribution to NursesPAC via my checking account. By signing this form, I authorize the charge of the specified amount payable to Nurses-PAC be withdrawn from my account on or after the 15th of each month. (PLEASE INCLUDE A VOIDED CHECK WITH FORM)
❑ I wish to make my monthly Nurses-PAC contribution via credit card. By signing this form, I authorize the charge of the specified contribution to Nurses-PAC on or after the 15th of each month.
❑ I wish to make my annual lump sum Nurses-PAC contribution via a credit or debit card. By signing this form, I authorize ANA-Illinois to charge the specified contribution to Nurses-PAC via a ONE TIME credit/debit card charge.
❑
Tiffany Ponder, MSN, RN Tiffany.ponder@aah.org Pondertk7@gmail.com
It is no secret that the healthcare workforce consists of about four generations of nurses that all began their careers in very different work and economic climates. Individuals who began their nursing careers just before the 2020 pandemic are now inquiring about and entering leadership positions. However, there are stark generational differences that if leveraged correctly, have the potential to invigorate an impactful and multifaceted team.
Evaluating your team for potential threats to the success of a transgenerational team is a great place to start. Being conscious of low hanging fruit such as the language used when defining other generations could indicate generational biases and threaten your team (Moore, 2016). For example, it is normal to identify the differences in learning styles and execution of younger generations. It is nonproductive to define differentiating characteristics as laziness or an attempt to deprioritize organizational priorities.
Instead, focus on the strengths of a multigenerational team. Be intentional in increasing your team’s speed to action with a specific focus on how quickly your team adopts ideas from those individuals that offer different

perspectives (Moore, 2016). Exercise your team to define innovation and areas where innovation could occur. A good stretch assignment would encourage your team to reinvent a long standing, well-functioning process. These are often opportunities that will be identified by Millennial and Gen X leaders who typically focus on opportunities to lean processes, even if they are currently productive.
Ways in which individuals like to be acknowledged also differ from generation to generation. Millennials tend to want public recognition and tangible accolades. Previous generations tend to desire more personnel means of recognition that attributes their good job to a good work ethic and positive characteristics. Having mixed methods of recognizing your team helps ensure that individuals feel that their work is in alignment with their leader’s vision and expectations for the organization. This is also an opportunity to evaluate the organization’s leadership make up. Are there enough layers to your leadership structure to align talent with opportunities for promotion within the organization? Research reveals that later generations desire recognition in the form of promotion for consistent work (Adams, 2016) and will often track their own measurable impact to the institution.
Is Your Table Ready?...continued on page 15
Submitted by Jackie Smith, RN, jackiesmith93@ gmail.com and Carolyn Rimmer-Owens, RN, owenscarolyn1312@gmail.com
The 36th Annual Black Nurses Day Celebration was celebrated on February 23, 2024, hosted once again by Apostolic Faith Church, where Bishop Horace Smith is the Pastor. This year, the accomplishments of nurses in nontraditional and entrepreneurial roles were highlighted. The National Black Nurses Day Planning Committee consists of representatives of the Chicago Chapter National Black Nurses Association, Alpha Eta Chapter, Chi Eta Phi Sorority, Inc., and Beta Mu Chapter Lambda Pi Alpha Sorority. The goal of the committee continues to be celebrating excellence among African Americans and inspiring nursing students to be all that they can be, whether at the bedside, on a cruise ship, in a classroom, or in the boardroom. February 23, 2024, was declared Black Nurses Day by Governor J. B. Pritzker and Mayor Brandon Johnson.



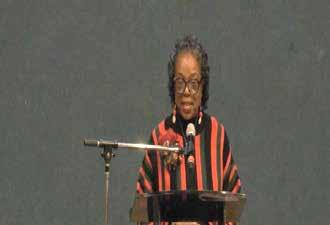

Ethel L Walton, RN President of the Chicago Chapter of the National Black Nurses Association.


This year, Vanessa Willis, RN, of Chicago Chapter National Black Nurses Association,set the tone for the evening by starting off with the Black National Anthem, “Lift Every Voice and Sing.” Written by James Weldon Johnson in the 1900. The audience joined in this traditional song.

Libation: Donna Feaster, RN, and Shannon King, RN, performed this year's ceremony to honor the life and legacy of our nursing colleagues. The ceremony is held annually to' invite the ancestors ‘into the space and welcome their blessings and protection.
The following nurses obtained their heavenly wings during this past year: Adrian Priester-Coary, RN, Alpha Eta Chapter, Chi Eta Phi Sorority; Gloria Ward, RN Alpha Eta Chapter, Chi Eta Phi Sorority; Cheryl Cool, RN, Alpha Eta Chapter, Chi Eta Phi Sorority, Dr. Iris Shannon, RN, Chicago Chapter National Black Nurses Association, Jiles TaylorGeorge, RN, Chicago Chapter National Black Nurses Association and Angie Lynn Thomas, RN, Chicago Chapter National Black Nurses Association.
The recognition of nursing schools was done by Jackie Smith. RN

The following schools were in attendance: CAAN Academy, Chicago State University, Loyola University, Malcolm X College, and Rush University all participated in this special ceremony.
The National Black Nurses Day Planning Committee (NBNDPC) named this year's scholarships after the late Louise Hoskins-Broadnax, RN. To qualify candidates must be nursing students enrolled in an accredited school of nursing and meet the required criteria to assist them financially in their pursuit of obtaining their nursing education. Ms. Broadnax holds many distinguished professional achievements and has served as a committed and active, longstanding NBNDPC member. She graduated from Provident Hospital School of Nursing in 1955 and served for several years as the president of the Provident Hospital Nurses’ Alumni Association, which is now defunct. She was appointed by Chicago Mayor Harold Washington as the first Black nurse to serve as Director of Institutional Care.

Louise Hoskins Broadnax Scholarship Recipients Nahaj Brown, Chicago State University; Kyra A Johnson, Chicago State University; Olivia Simone Murphy, Marquette University; Grace Ogunlana, Marquette University; Channing Brooke Payne, Rush University; Christina Pincham, Loyola University and Shundra Robinson, Northern Kentucky University.

Fallon M. Flowers, MSN, BS, RN, WHNP-BC, was the keynote speaker and has previously been one of 40 under- 40 emerging nurse leader honorees in 2016 by INF and in 2018 by NBNA. She spoke of the passion that most feel when entering nursing but said that that doesn’t mean that you can’t take what you have learned and create your own business. “It doesn’t have to be two separate entities; some nurses keep their day job and build their business until their business is their day job.” She spoke of the current rate of burnout and exodus from the nursing profession and said that many nurses are stepping out into a world we've never seen before. The catalyst for her was seeing that there was a lack of exposure to nursing for African American students in high schools and it was not that the interest was not there. She founded her business in 2017 Nursing Inspired, LLC, with the realization that it is hard to be what you cannot see and knowing that we need to lift as we climb and fulfill our duty of each one teach one. She is the Black Pre-Nursing coach and offers classes online to a multitude of high school and nontraditional adult students. She challenged the audience to look for a problem and look to someone who can help them solve that problem. She also spoke of the importance of mentorship and networking as a vehicle for successful entrepreneurship.

Member of National Black Nurses Day Planning Committee and honorees Rev. Dr. Evelyn Collier-Dixon, Carolyn Rimmer-Owens, President Ethel Walton of Chicago Chapter National Black Nurses Association. In the area of Nontraditional nurses are Dr. Michelle Myles, DNP, Fallon Flowers, APRN, (Keynote Speaker), Antrell Outlaw, LPN, Lisa-Jasmin Ford, RN, Martine Caverl, RN, Judy Powell, RN. (not shown), In the area of Entrepreneurial nurses, Shannon King, RN, Dr. Linda Howard, RN, Naomi Lockett, APN (not shown), and Donna Feaster, RN, President of the Alpha Beta Mu Chapter, Lambda Pi Alpha Sorority. Back row: Jackie Smith, RN, Dr. Sandra Webb-Booker, and Marilynn Parker.



Become a Psychiatric Mental Health Nurse Practitioner

There is a critical shortage of mental health professionals in the United States. Doctorallyprepared Psychiatric Mental Health Nurse Practitioners can fill that need and make an impact in their communities.

Rosalind Franklin University’s Psychiatric Mental Health Nurse Practitioner DNP program is designed with the working nurse in mind. Our PMHNP program is flexible, affordable and hybrid




JB PRITZKER Governor MARIO TRETO, JR. Secretary
idfpr.illinois.gov
CAMILE LINDSAY Acting Director
The Illinois Nursing Workforce Center conducted a voluntary survey participation with Illinois licensed Licensed Practical Nurses (LPNs) through two email blasts on February 16 and March 3, 2023. The data portal remained open from February 16 through March 21, 2023. A total of 8,367 LPNs completed the survey for a survey response rate of 31%.
Key Findings
• Employment: 94% are employed full-time in nursing, 78% work one job.
• Employment setting: 56% Practice in long-term care/outpatient clinic/assisted living.
• Diversity: the LPN workforce is the most racial and ethnically diverse of Illinois licensed nurses. There is more racial and ethnic diversity in the LPNs that are less than 45 years of age.
• Age: 40% of LPNs are age of 55 years or older.
• Education: 44% of licensed LPNs received community college education.
Diversity
• 7.3% of LPNs are male, lower than national average, with 36% of male LPNs under 45 years of age.
• 61% of Hispanic/Latino LPNs are less than 45 years of age.
• Approximately 45% of Asian, American Indian or Alaska Native or Native Hawaiian or Other Pacific Islander LPNs are 45 years of age or younger; and 50% Multiracial LPNs are in this 45 years or younger age range.
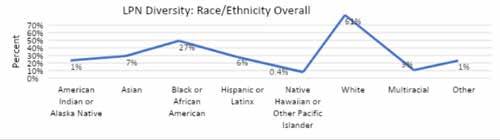
• 27% of LPNs identify as Black/African American, the largest reporting minority. 36% are less than 45 years of age.
Age of the LPN Workforce
• 40% of the LPN workforce is over 55 years of age.
• 24% of LPNs who practice in nursing homes/extended care facilities plan on retiring in 1-5 years.
LPN Employment Settings
• 48% practice in long-term care/rehabilitation/assisted living.
• 13% practice in outpatient settings such as ambulatory clinics, primary care clinics and offices.
• 9% practice in the home health setting.
• 4% of LPNs are school nurses.
LPN Position Role
• 74% provide direct patient care as staff nurses working primarily in long-term care and assisted living facilities, as well as outpatient and ambulatory settings.
• 7% identify as an administrator or manager.
• In Illinois the average staff nurse salary ranges from $55,000-$75,000.
Art glass is a combination of glass painting and architectural design common in the designs of gothic cathedrals. It originated as a form of painting, and with the integration of architecture, became a new three-dimensional artwork added to the design of buildings, and in smaller decorative pieces such as lampshades. Laura Polzin is our RN who supervises a High Acuity Unit (HAU) in an acute care hospital. A responsibility that can be challenging most of the time. What gives her a meaningful sense of work-life balance? Her passion for stained glass art, her other “heart” besides nursing! Laura explains that stained glass generally refers to the process of combining various colors and shapes. The color comes from the addition of metal salts during its manufacturing, that is melted and poured on a metal belt and put through a roller that flattens out the glass, and at the end, you have a sheet of glass ready to cut and sell. She adds “doing glass art takes me to my own little world where I find peace. Witnessing all the beautiful colors coming together is a sweet serenity, despite the tiny cuts it can cause on my fingers. It’s a hobby I look forward to the most, especially when I have another/new idea”. Laura likens her art to the critical thinking aspect of nursing. She exclaims, “just like deciding the safest way to provide patient care, the beauty of stained-glass art is in the process of making a pattern, uniquely yours, which is probably the hardest because I don’t do any drawing. It takes at least a couple of hours to put the picture in my head on paper, so be prepared, get a lot of pencils and erasers, and eventually, you’ll get there, so much like nursing care, just don’t give up!”

Editor’s note: Not only are they adept at patient care, but many also excel in fine arts, performing arts, culinary arts, and other activities that only confirm the many “hearts” of nurses. This new column features activities that showcase what is also meaningful and precious to nurses. We invite you to contribute an article, a play you participated in, a poem you composed, a recipe, a musical instrument you play, and other talents that must tell the world, nurses do not have a “heart” for patient care only, but also in all aspects of human interaction. Please submit your contribution via the link: syswart@ana-illinois.org



Cook County Health nurses are an exceptional group of individuals who are dedicated to our mission of providing compassion and high-quality care to all, regardless of the ability to pay, so all may live their healthiest life.
Opportunities for nursing at Cook County Health include:
• Acute care hospitals
• Ambulatory health centers
• Correctional health
• Public health We are
The Cook County Health nursing department proudly provides clinical education and career development programs that promote nurse competency, enhance role performance, and foster the professional development of nursing personnel to provide the highest-quality, patient–centered care.
Industry-Leading Nursing Benefits:
• 100% tuition reimbursement for nursing-related programs during employment with Cook County Health
• Pension Plan
• 4 weeks’ Vacation 0-1 years of service
• 5 Weeks’ Vacation 1+ years of service
• 3 weeks Sick leave annually
• Sick and Vacation days roll over
• 12 Holidays + 1 Floating Holiday
• Evening, nights, and weekend shift differentials
• Medical, Dental, and Vision Coverage
• Basic Term Life Insurance
• Deferred Compensation Program
* For nursing related programs during employment after one year of service
cookcountyhealth.org Join our expert, mission-driven care team.
CE Offering
1.0 Contact Hours
This offering expires in 2 years: June 1, 2026
Learner Outcome:
Learners will achieve an 80% on the post-test, indicating increased knowledge about medical modalities beyond traditional Western medicine.
HOW TO EARN
CONTINUING EDUCATION CREDIT
This course is 1.0 Contact Hours
1 Read the Continuing Education Article
2 Go to https://www.surveymonkey.com/r/2024-06111selfstudy to complete the test and evaluation. This link is also available on the INF website www. illinoisnurses.foundation under programs.
3 Submit payment online.
4 After the test is graded, the CE certificate will be emailed to you.
HARD COPY TEST MAY BE DOWNLOADED via the INF website www.illinoisnurses.foundation under programs
DEADLINE
TEST AND EVALUATION MUST BE COMPLETED BY MAY 31, 2026
Complete online payment of processing fee as follows: ANA-Illinois members- $8.00 Nonmembers- $15.00
ACHIEVEMENT
To earn 1.0 contact hours of continuing education, you must achieve a score of 80%.
If you do not pass the test, you may take it again at no additional charge.
Certificates indicating successful completion of this offering will be emailed to you.
The planners and faculty have declared no conflict of interest.
ACCREDITATION
Illinois Nurses Foundation is approved as a provider of nursing continuing professional development by Montana Nurses Association, an accredited approver with distinction by the American Nurses Credentialing Center’s Commission on Accreditation.
CE quiz, evaluation, and payment are available online at https://www.surveymonkey.com/r/2024-06111selfstudy or via the INF website www.illinoisnurses. foundation under programs.
Debbie Conner, PhD, MSN, ANP/FNP-BC, FAANP ihhealthflorida@gmail.com
In the rapidly evolving healthcare field, nurses are increasingly encountering a variety of medical modalities beyond traditional Western medicine. This article aims to introduce nurses to diverse healthcare practices, including allopathic, osteopathic, chiropractic, and Eastern modalities, highlighting their principles, approaches, and intersections. Understanding these different frameworks can enhance nurses' capacity to provide holistic and patient-centered care, foster better communication with healthcare providers from various disciplines, and ultimately improve patient outcomes. As healthcare embraces integrative practices, nurses' roles in navigating and incorporating these diverse modalities are becoming increasingly crucial.
Allopathic or Western medicine (traditional practice in the United States) focuses on diagnosing and treating symptoms and diseases using evidence-based practices, including drugs, surgery, and other technologies (Kowarski, 2020). It relies heavily on scientific methods and clinical trials to inform practice. Allopathic medicine is characterized by its rigorous standardization, specialization, and quick approach to acute problems rooted back to the ancient Greeks and Hippocrates. All medical doctor (MD) students who complete the degree take the Hippocratic Oath to guide their practice. This oath is a vow to do no harm. Nurse practitioners, physician associates (formerly assistants), or advanced practice providers traditionally practice this type of healthcare (Bauer et al., 2020).
Osteopathy deals with physical manipulation of the body's structure, but practitioners (DOs) in the United States are trained similarly to allopathic doctors (MDs) with an additional focus on the musculoskeletal system and manual therapy techniques (Bauer et al., 2020; Kowarski, 2020). D.O.s can prescribe medication and perform
surgery, similarly to M.D.s, but emphasizing touch-based diagnosis and treatment to facilitate the body's ability to heal itself and a holistic view of patient care. Also based on touch-based diagnosis and treatment is Chiropractic care, primarily practiced in the West. These providers focus on musculoskeletal and nervous disorders, often treating these issues with manual adjustment and manipulation, particularly of the spine. While chiropractic care shares a holistic approach to the body with Eastern medicine, it does not encompass the broad range of practices or the philosophical underpinnings of traditional Eastern approaches (Veazey, 2024).
Eastern medicine, also known as traditional Chinese medicine (TCM) or simply Eastern approaches, contrasts with Western (allopathic), chiropractic, and osteopathic medicine in several ways. Eastern medicine is considered holistic, emphasizing balance and harmony within the body's energy systems (Stefanov et al., 2020). Practitioners address health through acupuncture, herbal medicine, and Qi Gong. It is rooted in the concept of Qi (energy) and the balance of the Yin and Yang, aiming to correct imbalances in the body that lead to illness ("Traditional Chinese Medicine," n.d.). Recent discussions have highlighted the potential integration of Eastern and Western medicine, advocating for mutual respect and cooperation to enhance patient care (Stefanov et al., 2020). For instance, patients with neck pain would receive diagnostic X-rays and treatment with acupuncture and non-steroidal antiinflammatory drugs (Wong et al., 2012).
Some see the integration of Eastern and Western medical practices as a way forward, combining the strengths of each to provide more comprehensive care. For example, incorporating elements of Eastern medicine into Western practices can enhance patient choice and offer new avenues for treatment, especially for chronic conditions where conventional medicine may have limited solutions (Stefanov et al., 2020; Wong et al., 2012). However, this integration also faces challenges, including differing philosophical underpinnings, diagnostic methods, and treatment approaches ("Traditional Chinese Medicine," n.d.). Education and cooperation between practitioners are essential for overcoming these challenges and ensuring safe, effective patient care. Two of the mainstays of TCM medicine are acupuncture and herbal medicine.
Chines Medicine (CM) goes back more than 2000 years, with TCM being the modern standardized approach mandated in the 1950s by the Chinese government (Wong et al., 2012). Acupuncture involves inserting thin needles into specific points on the body. It is traditionally used in traditional Chinese medicine to balance the body's energy flow, known as the qi and meridians. Qi is described as channels in the body through which life energy flows ("Traditional Chinese medicine: what you need to know," n.d.; Zhang et al., 2018). Meridians are defined as the invisible channels through which the energy circulates throughout the body. Acupuncture seeks to restore the balance of energy and appropriate flow to allow the body to function normally and return to health. Meridians exist in corresponding pairs and have multiple acupuncture points along the channels. An acupuncturist places a needle into a certain point along the meridian to relieve pain or other symptoms, strengthening the immune system and balancing organ functions with each other, leading to improved health ("Traditional Chinese medicine: what you need to know," n.d.; Wong et al., 2012; Zhang et al., 2018). Studies are mixed regarding the efficacy of acupuncture. Some trials suggest that it stimulates the release of natural painkillers and affects areas in the brain processing pain. In contrast, others suggest it is a placebo effect (Traditional Chinese medicine: what you need to know", n.d.). TCM emphasizes customized therapeutic approaches tailored to the individual that may include infrared heat, cupping, and Chinese herbal products.
The herbal supplement's global market size was more than $86 billion in 2022 ("Herbal Supplements Market," 2024). These include natural, non-food, and non-pharmaceutical plant-based products. Dried leaves are the most extensive product, followed by tablets, capsules, powders, gels, and liquids ("Questions and Answers on Dietary Supplements," 2024). Alternative medicine (i.e., herbal remedies) and nutritional supplements continue to increase in popularity over synthetic medications. Recent estimates indicate that 80% of the world's population uses traditional medicine somehow. Asia and India are the largest exporters of herbal dietary supplements, with North America holding the second-largest market share.
In the U.S., the Food and Drug Administration (FDA) considers herbal and other supplements as food. With that said, they do not govern the manufacturing or marketing of these products (Williams, 2021). However,
they do prohibit claims to be made by producers or marketing. Hence, the FDA disclaimer "This product is not intended to diagnose, treat, cure, or prevent any disease" ("Questions and Answers on Dietary Supplements," 2024). When a new dietary ingredient is introduced to the market, the manufacturer or distributor must notify the FDA at least 75 days before interstate commerce. The notification must include the safety information under the conditions the supplement is recommended for or suggested in the labeling on the container. The manufacturer decides the size of the dietary supplement serving and does not require FDA approval. Consumers should be well informed about health-related products and consult with a healthcare professional before taking dietary supplements. Next, we will discuss some of the most common and popular supplements. It is important to note here that these are not recommendations, but a general overview of what consumers use. Always check the source of products, research each company's certifications, and test for heavy metals and product standards (Silva, 2024). Approximately 77% of Americans take at least one supplement regularly. These tend to include (but are not limited to) Vitamin D, Fish oil, CoQ10, Multivitamins, Probiotics, Turmeric, Vitamin C, B-Complex, and B-12. Next, we will discuss the use of supplements in stress and sleep, as they are two conditions individuals will seek help with regarding supplements in the U.S.
Stress is a common concern of many Americans. With 84% of the population reporting feeling stressed in 2022, several herbs and supplements have been marketed to help reduce this feeling (Black, 2022). Ashwagandha is herb known as an adaptogen. Along with relieving stress and anxiety, this plant is known for lowering blood sugar and triglycerides, increasing muscle and strength, women's and men's health, focus and memory, and heart health. This herb has been used for centuries, primarily in southeast Asia and areas of Africa (Black, 2022; Silva, 2024). While there is limited research on this herb, it is advised to consult with a provider if pregnant, immunocompromised, planning surgery, or having a thyroid condition. Also, allergies to nightshades or certain grasses can cause problems (Silva, 2024). Ashwagandha comes in many forms and can be consumed in many ways. Some complimentary herbs and supplements can assist with anxiety and stress in relation to the importance of sleep.
There are three popular herbs and supplements marketed for sleep in 2024. These are Magnesium (Mg), Melatonin, and Cannabidiol (CBD). We will discuss CBD from cannabis and hemp in more detail below. Mg is an essential mineral that plays a vital role in nurse and muscle function, development of bones, constipation, blood sugar control, and consistency of heart rhythm. In addition, magnesium status and sleep quality (daytime falling asleep, sleepiness, snoring, and sleep duration) have been associated with good results (Arab et al., 2023; Summer & Singh, 2023). For those who prefer to try whole food for Mg, nuts, whole grains, soy products, dairy, and leafy greens are the highest in content. Supplements may be more accessible to adjust to support sleep, with Mg glycinate being the easiest to absorb with fewer side effects. The recommended dose is 350mg a day or less, but some take more to get the sleep effects (Summer & Singh, 2023).
Melatonin is a hormone produced by the brain and appears to play a role in sleep quality. When evening approaches, the brain reacts to the darkness by producing melatonin ("Melatonin: What You Need to Know", n.d.). This hormone makes us feel tired and want to sleep. Some people may have circadian rhythm (24-hour internal clock) issues, such as delayed sleep-wake phase disorder, or are exposed to light at night (or have to sleep during the day). This can block average melatonin production. Supplemented melatonin (immediate or timed release) has been noted to improve sleep. Anecdotal evidence indicates that melatonin and Mg work well to assist with sleep ("Melatonin: What You Need to Know," n.d.; Summer & Singh, 2023). However, as with most supplements, there needs to be more robust evidence on the safety or effectiveness of melatonin. Let's move on to other popular modalities in alternative health care.
Energy healing (E.H.) practices evolved from the notion that an energy field surrounds our bodies. Practitioners believe this field can be manipulated to improve health and well-being like qi and meridians. E.H. has been used to reduce pain, depression, stress, and anxiety, as well as other conditions ("Energy Healing" n.d.). Energy medicine or therapy is a technique where the practitioner directs healing energy through their hands or other mediums, such as crystals, to restore the balance of the body in an effort to improve health and well-being. Physical touch is not always required but may depend on the modality
("Terms Related to Complementary and Integrative Health," n.d.). This modality began in TCM (qi) and Ayurveda (prana) to integrate mind, body, and spirit. In addition to these modalities, massage therapy, yoga, Reiki, healing/therapeutic touch, Qigong, and reflexology are also considered E.H. practices ("Energy Healing" n.d.). E.H. is generally considered safe, and some research studies support its use. Many are offered to hospital and cancer patients as part of their treatment. Some side effects might be dizziness, tiredness, or coughing, but overall, the effects are pleasant and noninvasive. Awakening the senses is very important in alternative healthcare practices. We will now move our discussion to aromatherapy and essential oils. Both use oils from plants for healing. Essential oils have been used since ancient times in cosmetics, perfumes, and drugs ("What is Aromatherapy?", 2024). These oils are also used in many cultures for spiritual, therapeutic, and ritualistic purposes. The oils are concentrated extracts from plant parts such as roots, leaves, seeds, or blossoms. Each plant part and oil have their own unique active ingredients. Oils have been used to heal wounds, treat swelling and infections, and are emotionally calming ("Aromatherapy with Essential Oils," 2023). We believe that the smell receptors in the nose communicate with the amygdala and hippocampus (the storage place for emotions and memories). When we use our nose to smell an essential oil, the scent stimulates these parts of the brain, resulting in a stimulation or sedative effect. It is important to note that scents associated with negative experiences may cause adverse reactions during use ("What is Aromatherapy?", 2024). For example, the smell of roses can be joyous and healing in many people, but others may associate it with a funeral or hospital room, and the scent can bring about sadness or fear. Essential oils in the United States are available without a prescription for inhalation and topical treatments. They are generally used in diluted forms with a carrier agent (such as in massage therapy) and, as such, will degrade over time. True, high-quality, pure essential oils do not have an expiration date. Topical application of essential oils may produce antibacterial, antifungal, anti-inflammatory, or analgesic effects ("Aromatherapy with Essential Oils," 2023). While not commonly taken in oral form, some oils, such as garlic for immunity, are commonly used. Remember, the U.S. Food and Drug Administration does not approve aromatherapy products unless there is a claim for treating a specific disease.
Sound therapy uses aspects of music to improve physical and emotional health and well-being. Healing with sound dates back to ancient Greece, when it was used to cure mental disorders. It is often used to boost morale, help people work faster, for religious and spiritual benefits, and health care recovery such as strokes. For example, when a stroke results in the inability to speak, it does not always affect the ability to sing. This phenomenon is also common in other head injuries and dementia-related disorders (Williamson, 2022). Research has shown benefits in boosting immune function, reducing stress, and improving the health of premature babies (Yue et al., 2021). Sound therapy spans multiple genres, including guided mediation or imagery (following voiced instructions, chanting, or repeating mantras or prayers), tuning fork therapy, binaural beats, and singing bowls. Tuning fork therapy has several uses, including testing for hearing loss, and is deeply relaxing. It also uses sound and vibration to stimulate the body's energy pathways. The vibrations resonate through body tissues, organs, and bones to promote healing (Bartel & Mosabbir, 2021). Tuning fork therapy is used in many modalities, including chiropractic and physical therapy. Another sound therapy known as Tibetan singing bowls also creates vibrations, which are said to improve physical and mental health. The bowl sings "ommmmmm" which is said to revive basic DNA codes. Om is considered the most sacred mantra in Hinduism and Tibetan Buddhism. There has not been any research on singing bowls. The convergence of Eastern and Western medical practices and chiropractic and osteopathic treatments represents a holistic approach to health that respects the diversity and complexity of human physiology and wellness. We can offer more comprehensive and personalized healthcare solutions by integrating allopathic medicine's precision and evidence-based approach with the holistic, energy-centered principles of Eastern medicine and the structural focus of chiropractic and osteopathic practices. This multidisciplinary approach encourages not only disease treatment but also health maintenance, emphasizing prevention, balance, and the interconnectedness of body systems. Such integration promises a more inclusive, effective healthcare system that caters to individuals' varied needs and preferences, ultimately leading to better patient outcomes and satisfaction.
References Arab, A., Rafie, N., Amani, R., & Shirani, F. (2023). The Role of Magnesium in Sleep Health: a Systematic Review of Available
Literature. Biological trace element research, 201(1), 121–128. https://doi.org/10.1007/s12011-022-03162-1
Bartel, L. & Mosabbir, A. (2021). Possible mechanisms for the effects of sound vibration on human health. Healthcare 9 (5), 597. https://doi.org/10.3390/healthcare9050597
Bauer, B. A., Townsend, K. M., Cutshall, S. M., Hazelton, J. F., Mahaptra, S., Meek, A., M., & Wahner-Roedler, D. L. (2020). Advanced practice providers’ knowledge, attitudes, and utilization of complementary and integrative medicine at an academic medical center. Alternative Therapies in Health Medicine (26) 5, 8-16. PMID: 32663179
Black, M. L., (2022). Americans’ stress levels- and financial anxiety- on the rise. Value Penguin. https://www. valuepenguin.com/stress-financial-anxiety-survey Emergen Research (2024). Herbal supplements market. https:// www.emergenresearch.com/industry-report/herbalsupplements-market
Kowarski, I. (2020, December 29). The difference between D.O. and M.D. degrees. US News. https://www.usnews.com/ education/best-graduate-schools/top-medical-schools/ articles/2019-11-07/the-difference-between-do-and-mddegrees
National Association for Holistic Aromatherapy. (2024). What is aromatherapy? https://naha.org/explore-aromatherapy/ about-aromatherapy/what-is-aromatherapy/
National Cancer Institute. (n.d.) Energy healing. https://www. cancer.gov/publications/dictionaries/cancer-terms/def/ energy-healing
National Cancer Institute. (n.d.). Traditional Chinese medicine. https://www.cancer.gov/publications/dictionaries/cancerterms/def/traditional-chinese-medicine
National Center for Complementary and Integrative Health. (n.d.). Melatonin: What You Need to Know. https://www. nccih.nih.gov/health/melatonin-what-you-need-toknow#:~:text=Melatonin%20is%20a%20hormone%20 that,in%20the%20body%20beyond%20sleep
National Center for Complementary and Integrative Health. (n.d.). Terms related to complementary and integrative health. https://www.nccih.nih.gov/health/providers/termsrelated-to-complementary-and-integrative-health
National Center for Complementary and Integrative Health. (n.d.). Traditional Chinese medicine: what you need to know. https://www.nccih.nih.gov/health/traditional-chinesemedicine-what-you-need-to-know
National Library of Medicine (2023). Aromatherapy with essential oils. PDQ Integrative, Alternative, and Complementary Therapies, Editorial Board. https://www. ncbi.nlm.nih.gov/books/NBK65874/
Stefanov, M, Stoev, S., Kim, J., Kim, S. (2020). Western medicine versus eastern medicine: Do both have a common root, scientific background, and worldwide recognition. Alternative Therapies in Health Medicine (26)2, 38-44. PMID: 31221936 Summer, J., & Singh, A. (2023). Using magnesium for better sleep. Sleep Foundation. https://www.sleepfoundation.org/ magnesium#references-239807
U. S. Food and Drug Administration (2024). Questions and answers on dietary supplements. https://www.fda.gov/ food/information-consumers-using-dietary-supplements/ questions-and-answers-dietary-supplements
U. S. Food and Drug Administration (n.d.). FDA regulation of cannabis and cannabis-derived products, including cannabidiol (CBD). https://www.fda.gov/news-events/ public-health-focus/fda-regulation-cannabis-and-cannabisderived-products-including-cannabidiol-cbd
Veazey, K. (2024). What’s the difference between an osteopath and a chiropractor? Healthline. https://www.healthline.com/ health/osteopath-vs-chiropractor
Williams C. T. (2021). Herbal Supplements: Precautions and Safe Use. The Nursing clinics of North America, 56 (1), 1–21. https://doi.org/10.1016/j.cnur.2020.10.001
Williamson, L. (2022). The healing power of music for stroke survivors. American Heart Association News. https://www. heart.org/en/news/2022/05/04/the-healing-power-ofmusic-for-stroke-survivors
Wong, E. Y., Gaster, B., & Lee, S. P. (2012). East meets West: current issues relevant to integrating Chinese medicine. Chinese Medicine (7)20. https://doi.org/10.1186/1749-85467-20
Yue, W., Han, X., Luo, J., Zeng, Z., & Yang, M. (2021). Effect of music therapy on preterm infants in neonatal intensive care unit: Systematic review and meta-analysis of randomized controlled trials. Journal of Advanced Nursing 77(2), 635632. https://doi.org/10.1111/jan.14630
Zhang, W-B., Jia, D-X, Li., Wei, H-Y., Wei, Y-L., Yan, H., Zhao, P-N., Gu, F-F., Wang, G-J., & Wang, Y-P. (2018). Understanding Qi running in the meridians as interstitial fluid flowing via interstitial space of low hydraulic resistance. Chinese Journal of Integrative Medicine 24 (4), 304-307. https:// doi,org/10.1007/s11655-017-2791-3
Questions
What is the focus of allopathic or Western medicine?
A) Energy healing
B) Physical manipulation of body's structure
C) Diagnosing and treating diseases using evidencebased practices
D) Balancing the body’s energy flow
Which oath do medical doctors (MD) take to guide their practice?
A) The Osteopathic Oath
B) The Chiropractic Oath
C) The Hippocratic Oath
D) The Eastern Medicine Oath
What additional focus do osteopathic doctors (DOs) in the United States have compared to MDs?
A) The musculoskeletal system and manual therapy techniques
B) Only drug prescriptions
C) Acupuncture and Qi Gong
D) Herbal medicine
Which of the following is NOT a characteristic of chiropractic care?
A) Focus on disorders of the nervous system
B) Manual adjustment and manipulation of the spine
C) Use of herbal medicines
D) Holistic approach to the body
What is the main emphasis of Eastern medicine?
A) Surgery and pharmaceuticals
B) Balance and harmony within the body’s energy systems
C) Quick approach to acute problems
D) Specialization in various fields
In Traditional Chinese Medicine (TCM), what is Qi?
A) A type of surgery
B) Channels in the body through which life energy flows
C) A form of manual therapy
D) An herbal supplement
What is one of the main differences between Eastern and Western medicine, as discussed?
A) Western medicine is older
B) Eastern medicine does not use any form of treatment
C) Philosophical underpinnings and diagnostic methods
D) Eastern medicine uses only surgery
According to the content, what is a challenge in integrating Eastern and Western medicine?
A) Too similar in approach
B) Lack of patient interest
C) Differing philosophical underpinnings
D) Western medicine is too advanced
Which herbal supplement market had the largest product base in 2022?
A) Tablets and capsules
B) Dried leaves
C) Powders
D) Gels and liquids
Which of the following is NOT a practice associated with energy healing (EH)?
A) Acupuncture
B) Massage therapy
C) Tuning fork therapy
D) Allopathic surgery
Is Your Table Ready?...continued from page 9
Networking ability across the organization is also incredibly important to later generations. Previous generations had a different respect for leadership structure (Moore, 2016). Senior level and C-Suite level recognition and acknowledgement is not seen as necessary. Many of these individuals of previous generations care more about the respect and acknowledgment of their direct supervisors. Later generations value tangible access to senior leaders. Having this level of access can indicate visibility and the opportunity to model the communication and behaviors that are thought to lead to more career advancement. Developing a functional and productive transgenerational team is what makes many of the top institutions across the world more productive. Continue to think beyond the benefit of technological advancement when considering the advantages of newer generations. Acknowledge opportunities for internal growth that allow for the full complement of having a multifaceted team. Prepare your table by helping your entire team envision the benefits of this change, uptrain their ability to adopt new ideologies and improve the overall management of the entire organization’s workforce.
References Adams, J. M. (2016). The influence of emerging nursing administrative and leadership researchers. JONA: The Journal of Nursing Administration, 46(1), 4-6. https://doi. org/10.1097/NNA.0000000000000293
Moore, J. M., Everly, M., & Bauer, R. (2016). Multigenerational challenges: Team-building for positive clinical workforce outcomes. Online Journal of Issues in Nursing, 21(2), 1. https://doi.org/10.3912/OJIN.Vol21No02Man03

• As required by the Illinois Nurse Practice Act, all nurses shall complete continuing education prior to license renewal. All Registered Nurses (RNs) shall complete 20 hours of approved continuing education per 2-year license renewal cycle. Advanced Practice Registered Nurses (APRNs) shall complete 80 hours of approved continuing education in the advanced practice registered nurse’s specialty per two-year license renewal cycle.
• To renew your Illinois nursing license, please visit the Online Renewal website https://ilesonline.idfpr.illinois. gov/DFPR and follow the instructions listed. The link takes you to the IDFPR online services portal to begin license renewal. We have provided renewal tips for accessing the Renewal System at https://idfpr.illinois. gov/content/dam/soi/en/web/idfpr/forms/online/ idfpr-general-license-instructions.pdf. If you currently do not have an Online Account, you will be required to open an account at https://online-dfpr.micropact.com/ before proceeding to the renewal application.
• For those requiring additional assistance with the renewal login process, you may contact the IDFPR by calling toll free, at 1-800-560-6420 or send questions to http://idfpr.illinois.gov/profs/Email/prfGrp09.asp. Please enter "RENEWAL" in the subject line of your e-mail.
• Beginning with the 2024 renewal, Illinois RNs who provide health care services to and have direct patient interaction with adults 26 years of age and older will be required to complete a one-hour course in diagnosis, treatment and care of Alzheimer's disease, along with other dementia types. CE Curriculum will involve how to identify and diagnose Alzheimer's, effective communication strategies and management and care planning. This course may count toward the regular CE requirements (Public Act 102-0399, 20 ILCS 2105/2105-365).
• There are additional new requirements beginning in 2024, including completing one (1) CE hour implicit bias awareness training. The Division of Professional Regulation (DPR) webpage has implicit bias awareness CE information: https://idfpr.illinois.gov/dpr.html Implicit bias is a form of bias that occurs automatically and unintentionally, that nevertheless affects judgments, decisions and behaviors.
• The CE requirement for implicit bias awareness training and the CE requirement for sexual harassment prevention training (each one CE hour), is included in the number of hours already required under the individual Nurse Practice Act and Rules. This does not
increase the number of CE hours required to renew a license, which is 20 CE hours. For details, please see the CEU FAQ sheets on the Nursing Workforce Center website: https://nursing.illinois.gov/nursing-licensure/ continuing-education.html
• The Illinois Department of Financial and Professional Regulation (IDFPR) is providing renewal assistance for individuals and businesses that are having difficulty with the online renewal process: https://idfpr. illinois.gov/dpr.html. These steps will help licensees better navigate the account matching process on the Department's updated online portal. This portal is only open during the renewal process, through May 31, 2024: http://idfpr.illinois.gov/profs/Email/prfGrp09.asp
• For US residents with an Illinois nurses license, to change your email address, U.S. mailing address or phone number, please click on this link to update the information: https://idfpr.illinois.gov/fpr-applications/ licensereprint.html. This form is not for international residents who must download a paper form found on that same page.
• Military families: Members and Spouses who are an active duty member or whose active duty service concluded within the preceding two years before application. In addition to expedited review of your application (30 days), the Department’s dedicated Military Liaison will work with you and your military installation’s military and family support center to help you through the licensing process. Learn more here: https://idfpr.illinois.gov/military.html. You may also email the Military Liaison using this email address: fpr. militarylicense@illinois.gov
• To print your license or download an electronic copy to your phone, just head to the IDFPR website https:// idfpr.illinois.gov/fpr-applications/getmylicense/ loginprof.html
• The IDFPR “Requirements of an Internationally Educated Nurse” document is available online here: https://idfpr.illinois.gov/content/dam/soi/en/web/ idfpr/renewals/apply/forms/cgfns-02.pdf. Resources on this document include the names of Board of Nursing approved vendors for items required to apply for an Illinois nurse license.
o Information includes that endorsing an active license from another state requires: an application by Endorsement.
o If the state of original licensure required a Credential Evaluation Service (CES) report at the time of original licensure, a (CES) report is not required for the Illinois licensure endorsement process.
o An English equivalency test is not required as long as the nurse applying for Illinois endorsement took and passed the NCLEX® national licensure examination.

• On the IDFPR Nurses web page there is a list of all 138 Illinois Board of Nursing approved RN/Registered Nurse and LPN/Licensed Practical Nurse pre-licensure nursing education programs: https://idfpr.illinois.gov/content/ dam/soi/en/web/idfpr/forms/dpr/nurseschools.pdf
• A complete copy of the Illinois Nurse Practice Act and the Rules may be found on the Division of Professional Regulation (DPR) Nurses webpage (https://idfpr.illinois. gov/profs/nursing.html). or on the Illinois Nursing Workforce Center’s website (https://nursing.illinois.gov/nursing-licensure/nursingact-rules.html).
• Applications for Full Practice Authority APRN (277) and Full Practice Authority APRN Controlled Substance (377) licenses may now be completed online. Create an account on IDFPR’s online portal (https://online-dfpr. micropact.com), select the applications, and complete and submit them to IDFPR. Find helpful checklists for completing your application here: https://idfpr.illinois. gov/dpr/professional-licensing-illinois.html
• Complaints against any individual or entity regulated by the Division of Professional Regulation may be filed by following the instructions here: https://idfpr.illinois. gov/admin/dpr/dprcomplaint.html. For a complete list of professions licensed by DPR, please click here: https://idfpr.illinois.gov/Forms/Brochures/DPR.pdf
• Please note: Pursuant to Illinois law (20 ILCS 2105/2105-117), all information collected by the Department during an examination or investigation of a licensee, registrant, or applicant is confidential and cannot be publicly disclosed. This includes complaints and any information collected during an investigation. Exceptions to this law exist only for law enforcement, other regulatory agencies with appropriate regulatory interest, or a party presenting a lawful subpoena. The Division of Professional Regulation online complaint form may be found here: https://idfpr.illinois.gov/ admin/dpr/complaint.html
• Reports: https://nursing.illinhois.gov/resources/datareports.html
In 2022, the RN, APRN and FPA-APRN license renewal was closed on August 31, 2022. Data was voluntarily collected through two email blasts sent to all 229,426 licensed RNs, 17,999 APRNs, and 2,000 FPA-APRNs in October-November 2022. The voluntary surveys captured data on the demographics, education, workplace settings, practice foci and practice role of licensed nurses in Illinois. Data was collected from October 5, 2022 through November 15, 2022 with a response rate of 26% for RNs; 24% for APRNS; and 41% for FPA-APRNs . These workforce survey reports are a useful resource. Past IDFPR licensed nurse reports dataing back to 1984 are also on this webpage.
The purpose of the Illinois Nursing Workforce Center (INWC) is to address issues of supply and demand in the nursing profession, including issues of recruitment, retention, and utilization of nurse manpower resources. The INWC has sections with links to all levels Illinois nursing education from pre-licensure to APRN specialization, links to continuing education requirements for license renewal, links to annual IBHE and ISAC scholarships and applications during application windows, and there are reports created with data collected with past license renewal. Find those resources and more at https://nursing.illinois.gov
