Dear Illinois Nurse Colleagues,
The word legacy refers to a gift or bequest that one leaves to another It can be something inherited from a predecessor like an outright gift of money or property The word often refers to a heritage that might take the form of the work or actions one is known for
Since I wrote my last column we have experienced a lot of change – the only constant in life – some good, some bad!

Maureen Shekleton PhD, RN, DPNAP, FAAN
The 2016 Chicago Cubs became the World Champions after 108 long years! Their legacy of being the “lovable losers” changed to that of being “fun loving” world champs! As the election cycle grew to a close, we heard a lot about the legacy of the departing administration and how history would view it According to its creator, Lin-Manuel Miranda, the current Broadway hit, Hamilton, is a show about the characters grappling with their legacy (Interview with Chris Tribune, Sunday, 9/11/16, Section 4, p. 2).
So, legacy, what has been given and is left behind, what is in people’s minds, what one is known for, is

Published by: Arthur L. Davis Publishing Agency, Inc.





important Why is it important? It is a starting point for future action In a way, it is a platform for creating change in the future -both positive and negative
In nursing, the legacy of others got us to where we are today Nurses who spoke out for patients’ rights, quality care, educational opportunity, a clear, strong code of ethics, a voice in the governance of institutions where care and education occurs left a legacy of being viewed by the public as the most trusted of professions The most recent Gallup poll (December, 2016) asking the public to rate the honesty and ethical standards of professions showed nurses receiving the highest public rating for the 15th year in a row
Here in Illinois we want to continue and build on this legacy of trust and respect! We can do this through philanthropy Philanthropy is all about legacy A Foundation exists as a mechanism for philanthropists to create or support and leave a legacy – one that they believe in and support A donation to the Illinois Nurses Foundation allows you to support the legacy of trust and respect for nurses and nursing in Illinois Your donation supports education and leadership development and

INF
Officers
Maureen Shekleton, PhD, RN, DPNAP, FAAN President
Alma Labunski, PhD, MS, RN Vice President
Cathy Neuman, MSN, RN, CNAA Secretary/Treasurer
Directors
Cheryl Anema, PhD, RN
Maria Connolly, PhD, CNE, ANEF, FCCM
Karen Egenes, EdD, MSN, MA, RN
Jacqueline Garcia, MSN, APN, NP-BC
Rhys Gibson, RN, BSN
Guadalupe Hernandez, MSN, APN, FNP-BC
P Joan Larsen, RN
Linda Olson, PhD, RN, NEA-BC
Bonnie Salvetti, BSN, RN
Kathryn Serbin, MS, DNPc, RN




Dan Fraczkowski, MSN, RN
Ann O’Sullivan, MSN, RN, CNE, NE-BC, ANEF
Pam Brown, PhD, RN, ANEF
Kathryn Serbin, MS, DNPc, RN
Amanda Buechel, BSN, RN
Karen Egenes, EdD, MSN, MA, RN
Elaine Hardy, PhD, RN
Crystal Vasquez, DNP, MS, MBA, RN, NEA-BC
Bonnie Salvetti, BSN, RN
Editorial Committee
Alma Labunski, PhD, MS, RN
Lisa Anderson-Shaw, DrPH, MA, MSN
Karen Mayville, MSN, PhD, RN
Cheryl Anema, PhD, RN
Nancy Brent, RN, MS, JD
Kathy Long-Martin, BSN, MSN, RN
Linda Olson, PhD, RN, NEA-BC
Lisa Woodward, DNP, RN, CENP
Swart, MS, RN, CAE
ANA-Illinois/Illinois Nurses Foundation
editing by the INF Executive Director & Editorial submissions ONLY as an attachment (word document preferred) syswart@ana-illinois org Nursing Voice Submission: Name of the article name of the author and a title. the right to pull or edit any article / news submission for space and availability and/or deadlines • If requested, notification will be given to authors once the final draft of the Nursing Voice has been submitted • INF does not accept monetary payment for articles.
Article submissions, deadline information and all other inquiries regarding the Nursing Voice please email: syswart@ana-illinois org
Article Submission Dates (submissions by end of the business day) January 15th, April 15th, July 15th, October 15th
Advertising: for advertising rates and information please contact Arthur L Davis Publishing Agency, Inc , 517 Washington Street, P.O. Box 216, Cedar Falls, Iowa 50613 (800-626-4081), sales@ aldpub com ANA-Illinois and the Arthur L Davis Publishing Agency, Inc. reserve the right to reject any advertisement. Responsibility for errors in advertising is limited to corrections in the next issue or refund of price of advertisement.
Acceptance of advertising does not imply endorsement or approval by the ANA-Illinois and Illinois Nurses Foundation of products advertised, the advertisers, or the claims made Rejection of an advertisement does not imply a product offered for advertising is without merit, or that the manufacturer lacks integrity, or that this association disapproves of the product or its use ANA-Illinois and the Arthur L Davis Publishing Agency, Inc shall not be held liable for any consequences resulting from purchase or use of an advertiser’s product Articles appearing in this publication express the opinions of the authors; they do not necessarily reflect views of the staff, board, or membership of ANA-Illinois or those of the national or local associations
Greetings! By the time you read this we will be well into the 100th Illinois General Assembly, a new Congress and new President Huge changes are likely and we need to make sure our voices are heard to advocate for our patients As you think back to the recent election- did you stay on the sidelines or were you an active participant? Did you get out to vote, canvass for a candidate, or phone bank?

Dan
Fraczkowski MSN, RN
In the new year, it’s time to recommit to becoming active in the political process as a nurse That can include volunteering to serve on a local school council or running for school board You can serve on your state legislator’s advisory committees, or participate in professional nursing organizations If you do not have time, but a few extra dollars to spend, consider donating to the Nurses Political Action Committee (Nurses PAC), to ensure that we elect candidates at the state level who value and support the nursing profession The ANA-Illinois Nurses PAC supports nurse friendly legislators through campaign contributions We contribute to candidates in both political parties to advance the legislative agenda to support our patients and the profession
For the 15th year in a row the Gallup Poll rated nurses as the most trusted profession We have an opportunity to influence our elected officials because we understand healthcare, and we are trusted It is never too late to get
involved at the state or local level Thank you to so many of you who were involved this election season
On behalf of the Board of Directors we are proud to announce that ANA-Illinois is one of the states that has been selected to participate in the ANA pricing pilot Through our participation, we will be able to offer an even more affordable membership price More details will be coming soon Our long-term goal is to allow every individual an opportunity to experience ANA at one attractive and extremely affordable membership rate. If you haven’t yet joined us, there is no better time to belong!
We hope to see you at our upcoming Student Nurse Political Action Day, on Tuesday, March 28th or Nurse Lobby Day on Wednesday, March 29th in Springfield, Illinois There are numerous other events we will be hosting throughout the state, so keep an eye on our email communication and social media feeds Also, if you are a nursing student, I hope you can join the Student Nurses Association of Illinois who is hosting their leadership workshop on Saturday, March 18th at Illinois Wesleyan University – more info is available at www snaillinois com I hope to see you there! As Nurses Week approaches, do not hesitate to reach out if your organization is hosting an event or function that you would like ANA-Illinois to attend, since our calendar is already beginning to fill up
Thank you for all you do for your patients and the profession
Sincerely,
Dan Fraczkowski MSN, RN
President- ANA-Illinois
@NurseDanF
Ricki Loar, Ph.D., APN-CNP President, ISAPN
ISAPN is pleased to share with you the winners for The Marie Lindsey Spirit of Advanced Practice Nursing and the ISAPN Member of the Year awards These awards were

The Marie Lindsey Spirit of Advanced Practice Nursing award is given to a licensed advanced practice nurse in Illinois who exemplifies the characteristics of leadership, commitment, and achievement in advanced practice nursing The criteria for this award for the outstanding ISAPN member includes: demonstrating excellence in clinical practice and as role model, creatively making a significant contribution to the improvement of care, using current research to enhance quality of care and having a positive effect on both clients’ care and on colleagues’ professional growth Brittany Sell nominated
the 2015 winner of the Marie Lindsey Spirit of Advanced Practice Nursing, and this honor was awarded to Reenu Varghese for her dedication to her patients as well as to improvements in care in her community

The second award presented at the Midwest Conference is the ISAPN Member of the Year Award This award was developed to recognize an ISAPN member who has worked diligently to achieve the goals set forth by the association, including leadership and visibility The criteria for this award includes active participation and leadership on the Board of Directors or service on one or more ISAPN committees, APN representation and role modeling, and presenting/follow through with new ideas that advance ISAPN as an organization Mary Barton and Beth Mathews nominated the 2016 winner of the Member of the Year Award, and Julie Aistars was selected to receive this honor Ms Aistars has not only facilitated changes to the ISAPN nominations committee, but has demonstrated excellence in her Oncology CNS role at Northwest Community Hospital She not only works with patients with lung cancer, but has been fundraising to provide programming to assist low income people with cancer detection and treatment, and to assist them in their smoking cessation efforts She recently ran a 500-kilometer run across the state of Tennessee that is 314 miles in 10 days or less!
Please join me in congratulating Reenu Varghese and Julie Aistars our two award winners!
Friday, April 7th, 2017 - the Illinois Chapter of the American Psychiatric Nurses Association (APNA) presents the 16th Annual Illinois State Meeting. Event will be held at the beautiful Northwestern Prentice Conference Center right between the Magnificent Mile and Navy Pier in downtown Chicago The destination is great for a day or bring the family for a weekend get away The Illinois chapter conference is the biggest state chapter conference in the country and sold out last year in two and a half weeks!
"Psychiatric Nursing: meeting today's crises head on" is a full-day program with breakfast, lunch, posters and a day's worth of CNE with a reception to follow
Free parking comes with the conference registration
The program features Cook County Sherriff Tom Dart on mental health in corrections, as well as two champions of nursing in the General Assembly, Assistant Majority Leader Sara Feigenholtz and Senator Heather Steans will attend Diana Knaebe, Director of the division of Mental Health for Illinois DHS will also talk about the upcoming major changes to behavioral health in the Medicaid system
Other programs will include Naloxone treatment of opioid overdose, violence and the brain, veterans treatment and more
Fee is only $75 non-member, $50 APNA member. Student rates are available at $35, $25 for APNA student members A limited number of psychiatric nursing student scholarship slots are available Registration information is available at http:// www apna org/illinois If registration is not yet open and you would like to be notified when it does or would like to apply for a student scholarship Please send an email to illinoisAPNAevents@gmail com



Katherine Barclay, RN
Five years into her practice, nurse Susan started a new job five months ago to realize her dream of becoming a kidney transplant nurse Throughout her nursing career, Susan has enjoyed working alongside her coworkers, and feeling like a valued team member But she has been struggling these last five months to be accepted by this group of staff members on her transplant unit She noticed some of her colleagues laughing at her expense when she asked a question about her work, and it seemed lately that when she needed help turning her patients, no one was available
Just last week Susan was unsure about administering a medication due to her patient’s hemodynamics, but when she sought guidance about her concern, the charge nurse informed her that after five months Susan should be able to work independently Susan gave the medication, which caused the patient to become hypotensive Susan had to write an incident report as well as receive a reprimand from her manager for this “avoidable mistake " Every day since then, Susan has felt anxious before starting her shifts, and has had diarrhea due to an upset stomach. She stopped asking questions of her colleagues, even though she was unsure how to handle certain situations, praying she made the correct decisions and had not caused harm to her patients After completing her latest shift, Susan went home and cried herself to sleep, vowing to call her former manager tomorrow and ask for her old job back.
Nurse Susan was unable to get rehired with her former employer, so she transferred to the cardiac transplant unit, and was being trained by Molly, a 25-year veteran nurse on the unit Susan found Molly to be a bit gruff during her training, and Molly watched Susan closely as Susan practiced her newly acquired skill set on their patients Four weeks into Susan’s training, Molly gave Susan a surprise quiz on anti-rejection medication frequently administered to the heart transplant patients on the unit, but Susan could not answer the medication questions because she had not studied the medication as she should have Molly instructed Susan on the importance of knowing these lifesaving medications, and informed Susan that she was not to give the patients’ medications until she demonstrated her knowledge of these drugs to Molly
It is hoped that Susan’s experience does not sound similar to your own but it is very possible that it does. Healthcare professionals are exposed to an increase in bullying at a startling rate. Clearly et al. (2010) writes that several studies have demonstrated that more than 50% of nurses have admitted to being involved in bullying behavior in the work environment One wonders how much higher would that number be if it included those nurses who did not admit to being a






bully? Another study by Walrafen, Brewer and Mulvenon (2012) found that nurses reported witnessed horizontal bullying (nurse to nurse) is as high as 77%. These are alarming, shameful statistics that should bring about needed changes to eradicate bullying in the workplace
Bullying: What It Is and Is Not
Although there are many definitions of bullying in the research literature, DeKeyser Ganz et al. (2015) define it as “repeated, offensive, abusive, intimidating, or insulting behaviors; abuse of power; or unfair sanctions that make recipients feel humiliated, vulnerable, or threatened, thus creating stress and undermining their self-confidence ” The key word here is repeated Bullying behavior also includes withholding information, responsibility, or tools needed to do the job effectively, trivial fault finding, and setting unrealistic goals or deadlines (Chapovalov & Van Hulle, 2015; Gould, 2016; Granstra, 2015). After reading these two definitions, it is clear that in the first hypothetical, bullying behaviors were displayed by nursing staff In the second hypothetical, Susan is not being bullied by Molly Molly is giving Susan needed professional guidance during her training, and constructively criticizing Susan for not meeting unit expected knowledge of medications, to ensure patient safety. Behaviors such as constructive and timely feedback, expression of differing opinions, performance evaluations (in non-bullying situations), normal instruction or on the job training, personality conflict, or an unintended offense, are not considered bullying, and nurses should be trained to know the difference (Granstra, 2015).
In the opening scenario, Susan experiences some of the negative effects bullying had on her: anxiety, nervous stomach and diarrhea before beginning her shift, afraid to ask important questions regarding patient care, and quitting her dream job. These are just a few of the negative effects caused by bullying. Others include, but are not limited to, depression, post-traumatic stress disorder (PTSD), sleep and eating habit disturbances, headaches, low morale and efficiency, high burnout and turnover rate, high absenteeism rate, compromised patient safety, and cardiovascular problems (DeKeyser Ganz et al., 2015; Ekici & Beder, 2014; Hogh et al., 2011; Weaver Moore et al., 2013; Srabstein & Leventhal, 2010).
The negative effects of bullying reach beyond nursing staff Healthcare organizations also suffer greatly, not only in their statewide and national standing, but financially as well. Granstra (2015) cites several articles with interesting numbers about the financial impact of bullying. J.S. Murray (2009) states that the cost of workplace bullying can exceed $4 billion per year. This cost was looked at more closely by Becher & Visovsky (2012). These authors’ calculated the annual expense to be in the range of $30,000-$100,000 per person, due to high absenteeism, low work productivity, worker’s compensation, and high turnover rate amongst staff
Most importantly, patient care and safety is compromised in hostile work environments. A nurse victim (also known as a target) of a bullying colleague(s) is afraid to ask for help, is likely to make patient care errors, and is more likely to call in sick or leave their job entirely, thus creating a shortage of staff on the unit (Weaver Moore, et al. 2013).
The Code of Ethics for Nurses With Interpretive Statements: Are You in Violation?
The Code of Ethics for Nurses With Interpretive Statements (2015) is the ethical benchmark to which nurses are held accountable to. The 2015 revision of the Code of Ethics for Nurses and its Interpretive Statements provide guidance when nurse bullying occurs in the workplace. Although direction exists throughout the Code, Provision 6 is one of the Provisions to carefully examine.
Provision 6 states that “The nurse, through individual and collective effort, establishes, maintains, and improves the ethical environment of the work setting and conditions of employment that are conducive to safe, quality health care.”
Interpretative statement 1 requires all those in the nursing profession, including nurse managers and executives, to cultivate and maintain high moral character of respect, patience and compassion, not just for our patients, but for each other (Lachman, et al. 2015). If you, as a nurse, are not practicing these attributes, you are not fulfilling your ethical obligations in the workplace and with your fellow nurse colleagues
Interpretive statement 2 of Provision 6 maintains that “Nurses in all roles must create a culture of excellence and maintain practice environments that support nurses and others in the fulfillment of their ethical obligations” (Lachman, et al 2015). One wonders if those nurses who reported witnessing horizontal bullying at 77% rate remained as a silent bystander? Undoubtedly, this Statement requires one to act as a deterent to bullying. Therefore, if you have witnessed, or witness bullying behavior in your workplace, you must intervene Interventions could include, confrontation of the bullying colleague, using positive peer pressure to show solidarity of zero tolerance for bullying, or calling security if the hostile act escalates However, always remember to maintain your own safety when confronting a bully
Interpretative statement 3 stresses, “The workplace must be a morally good environment to ensure safe, quality patient care and professional satisfaction for nurses and to minimize and address moral distress, strain, and dissonance " (Lachman, et al 2015). To minimize does not mean to ignore disparaging workplace issues Nurses are held responsible to work together respectfully and supportively as a team, to keep moral distress, strain, and dissonance at the lowest level possible, while openly and collectively addressing and resolving the negative impact of their existence.
Nursing Administration and Health Care Institution’s Role
Nurse managers and nurse executives play a key role in identifying and eradicating bullying conduct within their respective units and institutions and to value their team members and foster healthy interactions (Chapovalov & Van Hulle 2015). Nurse Executives must also empower nurses to appropriately intervene if
they witness a hostile interaction Through this support nurses can be helped to intervene confidently and fulfill their ethical and moral obligations
Nurse executives also need to support the development of institutional policies that allow nursing staff to intervene in bullying behavior without fear of retaliation by fellow staff members and/or by nursing administration
Health care organizations must also be proactive in recognizing the increasing occurrence of workplace bullying Workplace bullying awareness campaigns and mandatory training strategies can be created and implemented, not only with nurses, but with all healthcare institution employees in order to change a corporate culture that supports bullying to one of cooperation, respect and support among and for all staff. (Srabstein & Leventhal 2010).
Conclusion
Bullying behavior is at an alarmingly high rate in nursing It is furtively eroding the interpersonal relationships of those who practice nursing More than 50% of nurses have admitted to participating in bullying behavior (Granstra, 2015) but sadly, this percentage would likely be higher if more nurses chose to confess their culpability Without a doubt, all nurses, regardless of their position, are morally and ethically obligated to address, and stop, workplace bullying
One way in which to address, and stop, bullying, is to take the time to evaluate your relationships with your nurse colleagues Are you a nurse who conducts her/himself with patience, compassion, and respect towards patients, families, and peers? Or do you somehow set out to squash the morale and confidence of a colleague, or crush a new coworker’s dream of becoming an expert in your specialty of practice?
If you truly care, you will be honest in your selfassessment If you find that you have conducted yourself in violation of the Code of Ethics for Nurse With Interpretive Statements, and your unprofessional behavior is contributing to the erosion of the nursing profession’s ethical obligations toward fellow workers and others in the workplace, there is still hope Chapovalov & Van Hulle (2015) state, “Bullying is a behavior, and behavior is a choice " Only you can change your own attitude and conduct The question is: Will You?
References American Nurses Association (2015). Code for Nurses With Interpretive Statements. Silver Spring, MD: author. Becher, J., & Visovsky, C. (2012). Horizontal violence in nursing [Journal] MEDSURG Nursing, 21(4), 210-213, 232. Chapovalov, O., & Van Hulle, H. (2015, Fall/Winter). Workplace bullying in nursing-Part 1: Prevention through awareness [Journal] OOHNA Journal, 20-24.
Clearly, M., Hunt, G. E., & Horsfall, J. (2010). Identifying and addressing bullying in nursing [Journal] Issues in Mental Health Nursing, 31(5), 331-335 DeKeyser Ganz, F , Levy, H , Khalaila, R , Arad, D , Bennaroch, K., Kolpak, O., Raanan, O. (2015). Bullying and its prevention among intensive care nurses [Journal] Journal of Nursing Scholarship, 47(6), 505-511. Retrieved from doi.org/10.1111/jnu.12167
Ekici, D., & Beder, A. (2014, June/August). The effects of workplace bullying on physicians and nurses [Journal] Australian Journal of Advanced Nursing, 31(4), 24-33. Gould, T. (2016). Watch out for these 8 workplace bully personality types Retrieved from https://www. hrmorning.com/8-workplace-bully-personality-types/ Granstra, K. (2015, July/August). Nurse against nurse: Horizontal bullying in the nursing profession [Journal] Journal of Healthcare Management, 60 (4), 249-257. Hogh, A., Hoel, H., & Carneiro, I. G. (2011, March 6). Bullying and employee turnover among healthcare workers: A three-wave prospective study [Journal] Journal of Nursing Management, 19 742-751. http://dx.doi. org/10.1111/j.1365-2834.2011.01264.x
Lachman, V. D., O’Connor Swanson, E., & Winland-Brown, J. (2015, September-October). The new ’Code of Ethics for Nurses with Interpretive Statements’ (2015): Practical clinical application, part II [Journal] MEDSURG NURSING, 24 (5), 363-368. Retrieved from https://www. nursingworld org/MainMenuCategories/Ethicsstandards/ Codeofethicsfornurses/The-New-Code-of-Ethics-forNurses-PartII pdf
Murray, J. S. (2009). Workplace bullying in nursing: A problem that can’t be ignored [Journal] MEDSURG Nursing, 18 (5), 273-274.
Srabstein, J. C., & Leventhal, B. L. (2010). Prevention of bullying-related morbidity and mortality: A call for public health policies. Retrieved from doi:10.2471/ BLT.10.0077123
Walrafen, N., Brewer, M. K., & Mulvenon, C. (2012). CNE series. Sadly caught up in the moment: An exploration of horizontal violence [Journal]. Nursing Economic$: The Journal for Health Care Leaders, 30 (1), 6-12, 49.
Weaver Moore, L., Leahy, C., Sublett, C., & Lanig, H. (2013, May-June) Understanding nurse-to-nurse relationships and their impact on work environments [Journal] MEDSURG Nursing, 22(3), 172-179.
Mary Beirne LLM, BN, RN-BC, NCSN New York
As the healthcare industry transitions from fee-forservice to value-based reimbursement models, there will be winners and losers As school nurses, our challenge is to find our place in the winners group!
What do winners look like in this new era?
In this new era of accountable care and value-based reimbursement models, winners are paid for good, measurable outcomes Ultimately, this is an issue of funding If we, as school nurses, contribute to enhanced outcomes - and there is a large body of school nursing research to demonstrate that we do - then our programs should be appropriately reimbursed in order for these good outcomes to be sustainable over time. This is a winwin-win proposal: the individual student and his/her family benefits; the student’s Patient-Centered Medical Home (PCMH) benefits, and the government and/or third party payer benefits On a broader societal level we all benefit
School nurse positions are currently funded at the local level and come from funds primarily designated for education, not health care The decision-makers in the education system are educators, not health care providers In other words, in terms of outcomes, educators are focused on educational outcomes, not health outcomes The perception - and perhaps the reality - is that they have less ‘skin in the game’ of health outcomes than health care providers We all know that many school nurse positions have been eliminated over the past few years, arguably because our value has not been fully appreciated by the educational system
Our Present Opportunity:
There is no doubt that state/governmental agencies, health care providers and parents are already very aware of our value as registered nurses to the healthcare system in general and to the actual health outcomes experienced by individual students! We are a wonderful resource, and, typically, our professional services come at no cost to the health systems and providers which stand to benefit financially from our professional services in this new era of health care reimbursement
Our Value to State/Governmental Agencies:
• We engage in vitally important population health activities for our respective Departments of Health: we generate immunization surveys and track and follow-up on outstanding immunizations For most if not all of us, these vitally important population health-level activities are unfunded mandates
• Many of us provide biometric screening data to our respective Departments of Health This is another mandate which - for most of us - is unfunded
• We are the eyes and ears of our local Departments of Health We may be the first to recognize and report a communicable disease outbreak to the DOH
Our Value to Students’ PCMH:
• This new interest in care management among health care providers arises from the transition from fee-for-service to value-based care Providers and hospitals are now being paid for actual outcomes, rather than for isolated episodes of care So, their focus has shifted from an isolated office visit, to health maintenance and 24/7/365 chronic condition management, so that costly ER visits and hospital admissions can be avoided for ambulatory care sensitive conditions, such as asthma
• School nurses have always engaged in care management; indeed, we are experts in care management A school nurse with a good asthma action plan will keep a child in the school and out of the ER, ultimately saving money for the PCMH which is rewarded for keeping their ‘covered lives’ out of the ER
Our Value to Students and Families:
The families of students with chronic health conditions know our value, and are frequently our staunchest supporters when school nurse positions are threatened with downsizing
Our Challenge:
Our challenge is to get a seat at the table, and to have our contribution to students’ health outcomes recognized and appropriately funded

28, 2017
Join us for our 19th annual event! 1000s of students from across the state will converge on Springfield to learn about the importance of advocacy
REGISTRATION at http://conta.cc/2hRSzc9

March 29, 2017

Join us for the 2nd Annual Nurse Lobby Day Nurses from around the state will join together to advocate for our patients and advance our profession as we wrap up our efforts on the Sunset of the Nurse Practice Act
REGISTRATION at http://conta.cc/2h7fOS9

Introduction
Suzanne P. Carroll, RN
The rising rates of obesity have become a national health priority, with several objectives of Healthy People 2020 aimed at increasing physical activity, prevention of childhood obesity, and aiding in the management of existing obesity. Knowing that over one-third of adults in the United States is considered overweight or obese, as well as the growing rates of childhood obesity, the Food and Drug Administration (FDA) developed a health policy that is now requiring chain restaurants and retail food establishments to post the nutritional information, as well as caloric value, of their menu items This paper will aim to explain the health policy developed by the FDA and its relevance to health care, discuss issues and arguments against the implementation of the policy, and outline supportive evidence for this public health change
Health Policy Explained
As a part of the Affordable Care Act (ACA), the FDA issued a final rule on menu-labeling in December 2014, which is to be fully implemented by December 1, 2016. This ruling is definitely a shift in health policy for the FDA, as it now includes fast-food restaurants, beverages, grocery store salad bars, and chain restaurants (Goldman, 2015). The first-time menu labeling was addressed/regulated by the FDA was in 1993, and it was last updated in 2003 when the acknowledgement of trans fats on nutrition label was mandated (Food labeling, 2014). Many reasons exist as to the need for updating these guidelines Cardiac disease, cancer and stroke are the leading causes of death in the United States today, while additional chronic diseases such as diabetes and obesity are becoming more prevalent Diets high in trans-fats, sodium, cholesterol, and sugar can add to the development of these diseases, as it has been revealed that poor diet can contribute to morbidity and mortality of an individual (Food labeling, 2014). Encouraging individuals to maintain healthy lifestyles and make educated and appropriate decisions regarding their diet is one of the main goals of this health policy
This health policy requires all chain restaurants, drive-through restaurants, vending machines, take out and made-to-order restaurants, coffee shops, alcoholic beverages, and convenience stores display nutritional information, caloric value, and recommended daily caloric intake in a clear and visible way (Food labeling,

2014). Restaurants that are excluded include those who are not part of a chain that has 20 or more locations. Providing this nutritional information will cost the restaurants money, but the FDA estimates that this policy will result in anywhere from 3.7-10.4 billion dollars of benefits over the next twenty years, (Goldman, 2015).
Relevance to Health Care
As previously stated, more than one of every three adults is considered either overweight or obese, and childhood obesity is also on the rise Much like many other chronic diseases, the best way to manage these increasing rates is with prevention and education of the patient Education has always been an integral part of the job for nurses, mid-level practitioners, and physicians alike Promotion of a balanced, healthy diet along with exercise and increasing activity are ways to help prevent the development of obesity However, with the information that over half of a consumers’ annual food dollars are spent on food that are not made at home, it can be suggested that chain restaurants are locations in which individuals are spending their money (Food labeling, 2014). Targeting individuals who are dining outside the home with education regarding their food choices is one way to promote healthier eating and prevention of obesity
A large study of over 2,000 participants revealed that one fourth of adults, adolescents, and children all underestimate the caloric values of their fast food meals by nearly 500 calories (Block et al., 2013). This information shows that individuals do not correctly estimate the caloric value of their fast-food meals, which is a critical point and can easily add to the obesity epidemic Would the knowledge of the caloric value of their meal options change the order? One could assume if an individual sees that their order is over half the daily recommended caloric intake, that this would make someone doublethink about their choice, and possibly choose a healthier option A study through Yale University evaluated this question, with 303 participants. Overall, the results showed that consumers who had menus, which showed the caloric values of the meal options overall consumed less calories and orders healthier options than those who were not aware of the caloric value, with an average of 250 less calories consumed by the calorieaware group (Roberto, Larsen, Agnew, Baik & Brownell, 2010).
A cross-sectional study was done in Philadelphia in 2011 of 648 consumers at seven different restaurants, two with menu-labeling and the other five did not When comparing the orders of the two different consumers, it was found that those that dined that the restaurant with menu-labeling overall consumed 400 less calories, 370mg less sodium, and 10g less saturated fat (Auchincloss, Mallya, Leonberg, Ricchezza, Glanz & Schwartz, 2011). Additionally, consumers reported positive feeling regarding having the nutritional information available regarding the menu items
In King County, Washington, a group of 50 restaurants from 10 different chains including McDonalds, Starbucks, Subway, Taco Time, Taco del Mar, Burger King, Quizo’s, Jack in the Box, and Tully’s, participated in a study to evaluate the effect that menu labeling has on customers. With 7325 customers participating, the major measurement outcome was the number of calories purchased It was noted that during the first 4-6 months of the implementation of the menu labeling, there was not a significant difference from baseline ordering (Kreiger, Chan, Sealens, Ta, Solet & Fleming, 2013). However, after 18-months after the initial implementation of menu labeling, there was a decrease the in mean number of calories from both food chains and coffee chains (Kreiger et al., 2013). Importantly, there was a drastic increase of labelawareness among the customer base, from 18.8% to 61.7%, though only one third of customers reported using the menu labels (Kreiger et al., 2013). This study demonstrates that there is a definite change in the mean amount of calories after implementation of menu labeling, but that it takes time for the consumer to become aware of the labeling and change their order to healthier options
The results of these studies show that consumers are not accurately estimating their caloric intake when dining in restaurants; and if they were educated regarding the caloric value of their meal options, they would choose healthier, lower-calorie, meals These studies are suggestive that implementing the health policy of menu labeling could largely benefit the overall population
The successful implementation of a health policy is never done without significant push back There is an argument that menu labeling places a large financial burden on the restaurants, which would then impact






























the consumers’ prices (Armstrong, 2009). Additionally, the restaurant industry is claiming that these additional mandated costs would easily put small restaurant chains out of business (Armstrong, 2009). However, it should be noted that the majority of restaurant chains already assess and evaluate the nutritional values of their menu items, so adding calorie or nutritional labeling would not pose as much of a cost to the company as the argument is implying Opponents of this health policy state that proper menu labeling is not possible due to the ever-changing daily specials, and while this is a good argument, many specialty items or daily specials are exempt from the policy (Armstrong, 2009).
There is some research that challenges and opposes the value of menu labeling in restaurants In a systemic review of seven studies, published in the International Journal of Behavioral Nutrition and Physical Activity, did not find supportive evidence that menu labeling is effective in assisting consumers to purchase healthier option at restaurants (Swartz, Braxton & Viera, 2011). Only two of the seven studies reviewed had statistically significant evidence that menu labeling impacts calorie consumption, but overall there was not strong support that menu labeling had any effect on a consumer (Swartz, Braxton & Viera, 2011). This directly puts into question the reason for making menu labeling a national health policy, and of course the opposition to the health policy uses this information in order to argue against the implementation of the policy
Preemption is the main legal argument targeted by the opposition when it comes to the implementation of the health policy (Armstrong, 2009). Preemption is the notion that a greater and more powerful government creates laws or policies that prevents certain actions by a lower level of government Many public health care laws are affected by the preemption doctrine in the Constitution In this case, the federal law of requiring chain restaurants to provide nutritional labeling on their menus would supersede the state and local laws that currently exist. However, state and local governments are allowed to create additional policies that fall outside the preemptive rule or apply to restaurants that are not covered by the federal law
The First Amendment of Protection of Commercial Speech is another argument that the restaurant industry uses to oppose the policy The argument is that this health policy of menu labeling forces certain messages regarding their foods (Armstrong, 2009). Supporters of the policy state that the law that promotes commercial speech of factual information regarding the product being sold and the government should have interest in providing customers with nutritional information on the food being sold (Armstrong, 2009).
Implications for Nursing and Clinical Practice
The health policy of menu labeling makes a large impact on health care, and a primary care provider’s practice As stated in the supportive evidence for the
health policy, customers who were aware of the menu labeling more likely purchased a lower-calorie meal option Education of the public and patients regarding the menu labeling, and how to read nutritional labels, can now be easily incorporated into an annual physical exam or given as bedside teaching to the patient before discharge from the hospital Increasing awareness of the recommended daily caloric intake will also apply when promoting patients to choose the healthier options from a menu
This health policy is relevant to the ANA Code of Ethics in provisions 3 and 8. Provision 3 is that the nurse promotes, advocates for, and strives for the health, safety and rights of the patient; provision 8 states that the nurse collaborates without healthcare professionals and the public in promoting community, national, and international efforts to meet health needs ( American Nurses Association (ANA), 2001). By implementing this health policy to display menu labeling at chain restaurants, there is direct promotion of health by allowing the consumer to recognize food options, caloric intake, and hopefully choose lower-calorie options Nurses should be in support of this policy as it helps educate the public regarding the recommended daily caloric intake whilst also alerting the individual to the caloric value of each meal they order off a menu Giving the ability to choose lower-calorie, and healthier, options off the menu should help those who are trying to lose weight, but also ignite a change in those who did not realize they were ordering the least-healthy menu item One would hope that this policy will overall make a positive impact on the overall health of Americans
The health policy reviewed here is the most updated version of the policy. In July 2015, there were two proposed changes to the health policy made by the FDA The first was that there would be a required declaration of the daily value for added sugars, and the second proposal was to change the footnote on the nutrition facts label to increase understanding of the concept of “daily value” (Proposed changes, 2015). Both of these proposals seem to appropriate to enhance the customer understanding and literacy of the menu label and nutritional facts
Conclusion
This paper aimed to review the health policy regarding menu labeling, its relevance to health care, discuss the arguments for and against the implementation of this policy, the politics surrounding the policy, and the implications for clinical practice Clinicians should support the successful execution of this health policy as it would promote education to consumers regarding their eating habits at restaurants and provide them with clear, healthier options to order Increasing education to the population would help the obesity epidemic in this country, and help add to the success of healthy living for future generations
References available upon request.

CE Offering
1.0 Contact Hours
This offering expires in 2 years: April 1, 2019
Learner Outcome:
After reading the article, the nurse will be able aimed to discuss health policy regarding menu labeling, its relevance to health care, the arguments for and against the implementation of this policy, and the implications for clinical practice
HOW TO EARN CONTINUING EDUCATION CREDIT
This course is 1.0 Contact Hours
1 Read the Continuing Education Article
2. Go to https://ilnursesfoundation.wufoo.com/ forms/mar-2017self-study/ to complete the test and evaluation This link is also available on the INF website www illinoisnurses foundation under programs
3. Submit payment online.
4. After the test is graded, the CE certificate will be emailed to you
HARD COPY TEST MAY BE DOWNLOADED via the INF website www illinoisnurses foundation under programs
DEADLINE
TEST AND EVALUATION MUST BE COMPLETED BY APRIL 1, 2019
Complete online payment of processing fee as follows:
ANA-Illinois members- $7.50
Non members- $15.00
ACHIEVEMENT
To earn 1.0 contact hours of continuing education, you must achieve a score of 80%.
If you do not pass the test, you may take it again at no additional charge
Certificates indicating successful completion of this offering will be emailed to you
The planners and faculty have declared no conflict of interest
ACCREDITATION
This continuing nursing education activity was approved by the Northeast Multi-State Division (NE-MSD), an accredited approver by the American Nurses Credentialing Center’s Commission on Accreditation
CE quiz, evaluation, and payment are available online at https://ilnursesfoundation.wufoo.com/forms/ mar-2017self-study/ or via the INF website www illinoisnurses foundation under programs



On December 3rd, 2016 INF held its annual Holiday Fundraising Gala It was a great night for the Foundation and all those in attendance at the Sheraton in Lisle This year we had several organizations purchase entire tables for their supporters, members, association, friends or family This proved to be a great way for groups to get together over the holidays without all the planning and support a great cause at the same time In fact, many did their Holiday shopping at the Gala The event was a great success with nearly $10,000 raised for the INF!
Again this year the Foundation invited guests to support 2 veterans health initiatives - A Safe Haven and Canine Companions for Independence.
Since 1994, A Safe Haven has offered three types of Veteran housing based on individual need, assessment and eligibility, including transitional housing, per diem housing and permanent affordable housing
Veterans have access to the appropriate level of housing which may include full wrap-around services; supportive housing and employment services; to independent permanent affordable housing
Canine Companions for Independence has provided many assistance dogs to US war veterans across the country
Canine Companions was the first assistance dog organization to be accredited by Assistance Dogs International, and has provided assistance dogs to over 5000 people with disabilities.
Based on the assessment and eligibility, a Veteran can start at the transitional housing stage and work their way progressively through our housing programs They can



also start at the per diem program level or go directly to independent permanent affordable housing
Guests were encouraged to purchase ornaments for the “giving tree” and through the generosity of all in attendance over $500.00 was raised.
The evening was filled with raffle ticket buying (there were over 100 items) Silent Auction bidding and a special Travel Voucher Giveaway The winner of the giveaway will enjoy $2500.00 toward a getaway of his choosing! What a way to support the Foundation! Thank you to everyone who purchased tickets
Everyone enjoyed a plated 4-course dinner, cash bar, and some great live music by The Danhattans. Guests danced to familiar tunes from Frank Sinatra, Eric Clapton, Miles Davis, Allman Bros, Ray Charles, Neville Bros , and Springsteen
INF hopes that this event continues to expand and that this becomes the MUST ATTEND event for nurses and those that support nursing Just remember, when the invitation is released for the next event, book your tickets early. A special thank-you goes to each of our major sponsor – ANA-Illinois, and our many donors Thank-you also go to the many volunteers it took to make this a success event Thank you for your support and dedication to INF!
















Thank you to our generous sponsors and donors!
PLATINUM SPONSOR
ANA-Illinois
DIAMOND SPONSORS
Arthur L Davis Publishing
Texas Roadhouse - Dyer
TABLE SPONSORS
ANA-Illinois
Chamberlain College of Nursing
ISAPN
Marcella Niehoff School of Nursing
Olivet Nazarene University
The Council of Catholic Nurses of the Archdiocese of Chicago
GOLD SPONSORS
Cheryl Anema
Maureen Shekleton
SILVER SPONSORS
Laurie Anema
Maria Connolly
Mary Ann Tuft
Ruthann Sanders
Space Golf - Orland Park
BRONZE SPONSORS
Alpha Eta Chapter Inc
Art & Company - Orland Park
Cathy Neuman
Edible Arrangements
Forest Preserve National
Grand Lux Café
Hooters - Dyer, IN
Joanne Buckley


Karen Egenes
Lynwood Bowl
Mary Barton
P Joan Larsen
Pam DiVito
Thomas
Silver Lakes Golf
Smits Funeral Home
Stepping Stone Financial - So Holland
Susanna Gonzalez
Tasting DeVine
Vicki Keough
Wild Fire
GENERAL DONORS
Aurelio’s Pizzeria - So Holland, IL
Carraba’s - Highland
Coopers Hawk
John Kamp CPA
Kathy Serbin
Linda Olson
Linda Roberts
Linea Salon
Made in Italy
Massage Envy
Mindys - Mokena
Pat Wienski
PS Flowers
Red Lobster
Schultz Insurance - Lansing
The Pit Ribhouse - Hickory Hills
Theo’s Steakhouse - Dyer
Trio’s Restaurant
Walts Foods
Which Wich - Dyer





On Saturday, May 13 from 11:00 AM to 1:00 PM, Hektoen Nurses and Humanities and the Irish American Heritage Center are partnering to present the first ever Tea with Florence Nightingale.
What could be more fitting during the 2017 Nurses Week than to have tea with Florence Nightingale, “The Lady with the Lamp,” on the occasion of her 197th birthday? Participate in a rare opportunity to explore her influence on nursing today and the continuing relevance of her work
The character of Florence Nightingale will be brought to life by well-known Chicago actress Megan Wells (http:// meganwells com/Progams_Products html) Ms Wells has appeared as many famous women from history including Eleanor Roosevelt and Helen of Troy
She has vast experience in theater and storytelling. Ms Wells is developing the character of Florence Nightingale in collaboration with the members of the Nurses and Humanities advisory committee under the leadership of Sandra Gaynor PhD, RN and Mary Ann McDermott PhD, RN
The Hektoen Nurses have sponsored programs to expose nurses to arts and humanities activities across the Chicago area since 2010. The goal is to expose healthcare workers, nurses in particular, to the use of arts and culture to manage the stress of modern caregiving

Tea with Florence Nightingale is Saturday, May 13 at 11am-1pm will be held at the Irish American Heritage Center located at 4626 North Knox Avenue, Chicago. It is part of the ongoing Saturday Morning Tea Series at the Center, featuring performances on notable women in history and literature
Tickets are $25 for adults & $8.00 for children under 12.
You may reserve your tickets online at Irish American Heritage Center http://irish-american.org/ or by Phone: 773-282-7035 ext. 10XX
Bring your nursing, healthcare interested colleagues, and children to this event Join in the celebration of the life and work of the world’s most famous nurse, Florence Nightingale

For more information: Hektoen Nurses and the Humanities on Facebook https://www.facebook. com/NursesandHumanities/ or Sandra Gaynor at 773-774-9276.
The National Association of Hispanic Nurses – Illinois Chapter (NAHN-IL) celebrated their Annual Scholarship Award Recognition ceremony during Hispanic Heritage Month This annual event was held at the National Museum of Puerto Rican Arts and Culture on October 20, 2016; the primary sponsors were AT & T and Resurrection University – Illinois. This year they awarded $12,000 in scholarships.

The event was chaired by NAHN-IL President Susana Gonzalez, MHA, MSN, CNML, RN and President-Elect Elizabeth Florez, PhD, RN The awards were distributed by Senator Omar Aquino who also presented opening remarks on the value of nursing along with the need for culturally sensitive health care providers Scholarship recipients:

Carols Becerra, Cassandra Cisneros, Brenda Pacheco, Maribelia Martinez, Victoria Monterrubio, Quennia Montoya, Diana Ortega, Karen Salasblancas, and Isis Nisivaco (Resurrection University Scholarship recipient).
The NAHN-IL, a professional, voluntary and non-profit healthcare organization, is dedicated to enriching the lives of Hispanic nurses through the promotion of academic attainment, professional advancement, cultural awareness, and active participation in the Hispanic community
NAHN-IL Board members: President, Susana. Gonzalez; Treasurer, Nancy Garcia; Illinois State Senator, Omar Aquino; President-Elect, Elizabeth. Florez; and SecretaryElect, Irene Mendez.




Nurses want to provide quality care for their patients.
The Nurses Political Action Committee (Nurses- PAC) makes sure Springfield gives them the resources to do that.
Help the Nurses-PAC, help YOU!
So. . . . . . . if you think nurses need more visibility if you think nurses united can speak more effectively in the political arena if you think involvement in the political process is every citizen’s responsibility.
Become a Nurses-PAC contributor TODAY!
❑ I wish to make my contribution via personal check (Make check payable to Nurses-PAC).
❑ I wish to make a monthly contribution to NursesPAC via my checking account. By signing this form, I authorize the charge of the specified amount payable to Nurses-PAC be withdrawn from my account on or after the 15th of each month. (PLEASE INCLUDE A VOIDED CHECK WITH FORM)
❑ I wish to make my monthly Nurses-PAC contribution via credit card. By signing this form, I authorize the charge of the specified contribution to Nurses-PAC on or after the 15th of each month.
❑ I wish to make my annual lump sum Nurses-PAC contribution via a credit or debit card. By signing this form, I authorize ANA-Illinois to charge the specified contribution to Nurses-PAC via a ONE TIME credit/debit card charge.
❑ Mastercard ❑ VISA
Credit card number Expires CVV
Signature:
Date:
Printed Name:
E-Mail:
Address:
City, State, Zip Code:
Preferred Phone Number:
Please mail completed form & check to:
ANA-Illinois
Atten: Nurses-PAC PO Box 636 Manteno, Illinois 60950

















The Illinois Department of Financial and Professional Regulation (IDFPR) Board of Nursing (BON) collects information on an annual basis from all Illinois prelicensure nursing education programs Disclosure of this annual mandatory report is required to maintain BON pre-licensure nursing education program approval, which is required for a nursing student to be eligible to take the nursing license examination. Therefore, the response rate for this annual survey is 100%.
The Rules for the Administration of the Illinois Nurse Practice Act, Sections 1300.230 (LPN) Approval of Programs, b) Continued Program Approval and 1300.340 (RN) Approval of Programs, b) Continued Program Approval states: “Nursing education programs shall submit annual evaluation reports to the Division on forms provided by the Division. These reports shall contain information regarding curriculum, faculty and students and other information deemed appropriate by the Division.” Completion of this annual BON survey form is necessary to accomplish the statutory purpose as outlined in 225 ILCS 65/5-1, et al. For a current copy of the IDFPR Nurse Practice Act, go to http://www.idfpr. com/profs/nursing asp
The BON survey is conducted with the intent to capture data on the demographics of both nursing students and faculty; faculty education levels and employment status; and enrollment and graduation figures for pre-licensure nursing education programs The data collected is based on fiscal year, with a fiscal yearend date of June 30. This retrospective survey includes definitions of terms, request for three years of faculty and student data, verification of school name, address, chief administrator and minor curriculum revisions All surveys are required to be signed by the dean or director
of the nursing education program prior to acceptance by the Illinois Board of Nursing Surveys may be returned to IDFPR by United States mail or by e-mail A comprehensive record of the questions contained in the annual survey is provided in Appendix A.
After review of other state board of nursing surveys and past Illinois Board of Nursing annual surveys, the survey process and its content was standardized, beginning in 2008. The standardizations include definitions, time of year data is collected, collection based on fiscal year (similar to other state agencies) and only requesting three years of data. In 2011, IDFPR began the inclusion process of National Forum of State Nursing Workforce Centers Minimum Dataset for Education (http://nursingworkforcecenters. org/ ) items, with all items included by 2012. This standardization occurred under the direction of Michele Bromberg, MSN, RN (IDFPR Nursing Coordinator) with the assistance of Linda B Roberts, MSN, RN (Illinois Center for Nursing Manager).

and adequate resources to prepare the next generation of high quality professional nurses
Includes both full-time and part-time students; LPN Ladder program students are included in the ADN Program calculations.
This report provides an analysis of trends in Illinois pre-licensure nursing education, in regards to both faculty and students, from the years 2011-2015 (unless otherwise noted) A special thanks to Stephanie GedzykNieman, MSN, RNC-MNN, Lewis University DNP student on data analysis and compiling these reports Additional copies of this report may be found on the Illinois Center for Nursing website, http://nursing.illinois.gov/ ResearchData asp
Nurses are the largest group of healthcare providers in both acute-care and community settings in Illinois An adequate, well-prepared and diverse nursing workforce depends upon academically rigorous education programs


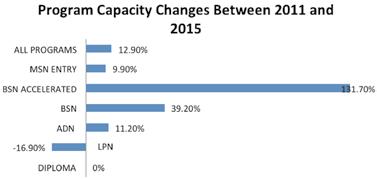
Programs: There are 146 pre-licensure programs in Illinois-113 for RNs and 33 for LPNs; in 2011, there were 142. This growth aligns with the Illinois Board of Higher Education’s (IBHE) Report of the Higher Education Commission on the Future of the Workforce’s goal to have 60% of the adult population in Illinois obtaining a highquality post-secondary credential or degree by 2025. The report also concurs with the Institute of Medicine’s (IOM) (2011) recommendation to increase the proportion of nurses with a BSN to 80% by 2020.
The number of graduates from all Illinois programs combined saw a steady increase until 2013, after which
IDFPR continued on page 12

















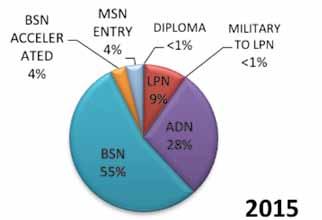
IDFPR continued from page 11
the number of graduates began to decline; however, the number of graduates in 2015 was still 9.1% greater than in 2011. Until 2014, Associate Degree Nursing (ADN) programs produced the largest percentage of graduates in Illinois. However, by 2015, BSN programs produced the largest percentage of graduates in Illinois (39%). The number of graduates from BSN Accelerated programs grew from 2% to 6% of all prelicensure graduates in Illinois while MSN Entry programs’ graduates grew from 3% to 4% of all pre-licensure graduates in Illinois Illinois’ nursing schools are the critical supplier of the nursing workforce and these educational programs prepare excellent nurses. To enter practice, nursing students must not only successfully graduate with their nursing degree, but they must also pass their respective National Council Licensure Examination (NCLEX®) prior to obtaining a nursing license. The first-time pass rate for Illinois students taking the NCLEX-RN® exam has met or exceeded the national total pass rate annually while the first-time pass rate for Illinois students taking the NCLEX-PN® exam to become Licensed Practical Nurses (LPNs) has exceeded the national total pass rate annually.
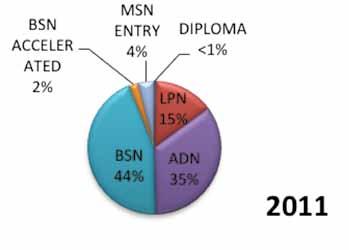
Over the period of this report, enrollment in pre-licensure nursing programs has increased almost 19% with approximately 23,000 students enrolled in a prelicensure nursing program in 2015. The largest growth in enrollment has been in the University setting among bachelor’s degree (including accelerated programs) and master’s degree programs. Associate degree (ADN) programs’ enrollment experienced a downward trend after a large growth period in 2012; however, this is a modest decline (-2.4%) considering the closure of four ADN programs by 2015.
The pre-licensure nursing student body in Illinois essentially emulates that of the general population in Illinois, except for having slightly less Hispanic and nonHispanic/Black than the Illinois population (United States Census Bureau, 2015). Although still predominately Caucasian, the percentage of pre-licensure nursing students in Illinois belonging to a racial or ethnic minority has grown 2.6% since 2012. The largest minority group among all pre-licensure programs in Illinois is non-Hispanic Black, except for the MSN Entry program where the largest group is Asian (11.4% in 2015) and the BSN program where the largest group is Hispanic (12.3% in 2015).
Compared to 2014 national data reported by NLN (2014b), there were more non-Hispanic/Black, Hispanic and Asian/Native Hawaiian/other Pacific Islander prelicensure students in Illinois than the national average Male student enrollment in pre-licensure nursing programs in Illinois has remained essentially the same at 12.9%, which is slightly less than the 2014 national average of 15% (NLN, 2014e).
Includes both full-time and part-time students; LPN Ladder program students are included in the ADN program percentages.
Students: In order to plan for both future nursing workforce and healthcare needs in Illinois, it is important to explore the demographics of the nursing student population in addition to program enrollment figures

Faculty: A critical resource affecting the ability of schools of nursing to educate the future nurses needed for Illinois is having readily available, highly-educated faculty
The age distribution among pre-licensure nursing faculty has essentially remained unchanged since 2011 and the largest age group among faculty continues to be 41-50 years old. In 2015, 18.6% of pre-licensure nursing faculty were 61 years or older, up from 14.6% in 2011. The percentage of full-time pre-licensure faculty in Illinois aged 61 or older is also higher than national rates (IL-22%; US-20%) (NLN, 2016a). Faculty aged 61 years or older are eligible for retirement and if this occurs, without the ability or a plan to replace them, program capacities and student admissions could be negatively impacted (IOM, 2011).
Diversity among Illinois nursing faculty has slightly increased, with the percentage of pre-licensure nursing faculty belonging to a racial or ethnic minority increasing 1.3% since 2012. 73% of faculty is non-Hispanic/White, a 5% decrease from 2012. The largest minority group represented among all pre-licensure nursing faculty remains non-Hispanic/Black (12% in 2015). The ethnic diversity of Illinois’ pre-licensure faculty essentially emulates that of national figures The only difference was among the number of Hispanic full-time pre-licensure faculty, which was 1% in Illinois but 3.7% nationally (NLN, 2016a). The percent of male pre-licensure nursing faculty has increased by 1.3%, to 6.0% in 2015, yet male faculty still remain the minority. Of all of the programs in Illinois, LPN program faculty are the most diverse and BSN program faculty experienced the largest growth in diversity.
A key component in meeting nursing workforce supply is Illinois’ ability to produce new nurses through the pre-licensure nursing education system To evaluate this system, it is important to examine the type, demand and outcomes of the programs provided, in addition to student and faculty characteristics, which was the intent of this report A copy of the full report is available on the IDFPR/Illinois Center for Nursing website: http://nursing.illinois.gov/ResearchData.asp


Many Illinois universities offer online nursing courses that lead to a degree The Illinois Center for Nursing Website http://nursing.illinois.gov/education.asp highlights online nursing education. For example, three of the four RN-baccalaureate completion programs at public universities offer either the majority or a significant portion of the courses leading to a BSNc online Many graduate nursing education programs also make a significant portion of their classes available online Online education is tied to a goal of the Commission on the Future of the Illinois Workforce http://www. ibhe state il us/WorkforceCommission/default htm

The Commission is led by the Illinois Board of Higher Education and is comprised of legislators, presidents of institutions, and representatives of business and industry The Illinois Center for Nursing website contains links to Illinois preand post-licensure nursing programs, including online options for education advancement The State of Illinois Department of Professional Regulation does not regulate or give approval for post-licensure nursing education programs
Nursing is an aging profession causing a shortage and increasing the demand for nurses In addition, the demand for quality healthcare and patient-acuity levels are increasing exponentially. Nurses’ experience, education, and professional environment affect each of us in various ways As the profession focuses on meeting patient needs and providing quality care in a multitude of specialized areas, we are also facing increased interpersonal violence as well as increased exposures to occupational hazards. It comes as no surprise that workplace safety is a widely-discussed topic in nursing Although each of our stories is unique, there are identified common experiences that need to be addressed to improve workplace safety
and enhancing workplace safety This survey series supports nurses and their patients in Illinois
A new survey topic and link will be published in the Voice each quarter The survey will be open to all nurses We are asking for your help in making this survey a success by taking part in it, so please take a few minutes to complete it online and share the link with other Illinois nurses
We appreciate your support in helping ANAIllinois study and improve nurses’ workplaces
Thank you for doing your part in improving the workplace for Illinois nurses!
Submitted by the Expert Panel on Workplace Safety
Timbolin Holmes MSN, APN, CNP (chair)
The Illinois Department of Financial and Professional Regulation website http://idfpr.com is regularly updated to provide Illinois licensed professionals with useful resources From our home page, a variety of licensing user guides and additional tools can be found by clicking “Online Resources ”

Print a copy of your license or store a copy on your smartphone or tablet:
The tab “eLicense Search” allows “Licensed Professionals” (the middle option) the opportunity to print a free copy of their license Licensees only need to provide their individual license number and date of birth or last four digits of your social security number
For licensees wishing to store an electronic license pocket card on their smartphone or tablet, please visit: www idfpr com/GetMyLicense Electronic pocket cards may be saved as a PDF file or by taking a screenshot and storing as a photo
To Change your Address:
A change of address, including email address or change of phone number can be accomplished online https://www.idfpr.com/applications/LicenseReprint/ A change of name cannot be completed via online process, supporting documents must be submitted to Licensing in Springfield, IL
If you have questions, is there someone to talk to? Yes, assistance is available Monday through Friday by contacting the IDFPR call center at: 1-800-560-6420; or by email at: FPR LMU@illinois gov
Thus, the strategic plan of the ANA-Illinois called for an Expert Panel on Workplace Safety. This panel, comprised of members with rich and varied nursing backgrounds, has been charged with the task of assessing Illinois nurses’ perception of workplace safety They have worked as a team to create a comprehensive survey, which will provide data for the State of Illinois, and a foundation for improving THaNk
Lauren Martin RN
Carolyn Ruud MSN, RN
Pam Brown PhD, RN, ANEF
Jessica Gerdes MS, RN, NCSN
https://www.surveymonkey.com/r/ WORKPLACESAFETYPART2

Piotrowski, Paulette
Smith, Ann
Cody, William
Shekleton, Maureen
Miller, Mark
Hannon, R
Ellingsen, T
Dalicandro, M
Olson, Linda
Egenes, Karen

Connolly, M
Labunski, A
Olson, Linda
Serbin, Kathryn
Larsen,P. Joan
Kamp, J
Tuft, Mary Ann
Salvetti, Bonnie
Langer, S





Lecturer/Assistant Professor – Nursing
Full-time, 9 month positions to begin August 2017.
Summary: The School of Nursing and Health Professions has vacancies for three (3) Lecturers/Assistant Professors. Two (2) positions in adult or maternal/child, and one (1) position in mental health.
Responsibilities: Clinical and didactic teaching, recruitment and advising of students; participation on committees; university/regional service; scholarship.
Qualifications: Masters of Science in Nursing. Minimum of three years of clinical experience in adult health, maternal/ child, or mental health as a registered nurse. Eligible for RN licensure in Kentucky. Preferred doctorate in nursing or related field; preferred teaching experience at the collegiate level; preferred experience in gerontology.
Application Deadline: April 10, 2017
To apply please visit:
http://www.murraystatejobs.com/postings/6317


Balance your life for a healthier you.
In recognition of the impact that increased nurse health, safety, and wellness has on patient outcomes, quality of care, and overall nurse satisfaction and quality of life, American Nurses Association (ANA) has designated 2017 as the “Year of the Healthy Nurse” with the tagline of “Balance your life for a healthier you ” Each month will highlight various health, safety, and wellness topics important not only to nurses, but to their co-workers, families, patients, and the communities in which they live, work, and play Nurses struggle with multiple health, safety, and wellness challenges. ANA’s 2016 Health Risk Appraisal shows alarming trends for registered nurses (RNs) and nursing students:
• An average BMI of 27.6 (overweight)
• 12% have nodded off while driving in the past month
• Only 16% eat the recommended daily amount of fruits and vegetables
• Less than half perform the recommended quantity and time of muscle-strengthening exercises (ICG & ANA, 2016)
is now seeking Nurse Care Coordinators to join our team
For more information & to apply for this role, please visit our website. www. F hnchicago.com

RNs continue to rate workplace stress as a hazardous occupational risk well above the national average (ICG & ANA, 2016). Yet nurses’ very calling, professionalism, and strong sense of ethics demand that they become better role models, advocates, and educators
2017 brings a focus on the Year of the Healthy Nurse, and will include the launch of the Healthy Nurse, Healthy NationTM Grand Challenge (HNHN GC) and the continuation of #FitNurseFriday ANA’s HNHN GC is a sweeping social movement to increase the health of the United States’ 3.6 million RNs, thereby impacting and improving the health of the nation HNHN GC focuses on five fundamental indicators of wellness: rest, nutrition, activity, quality of life, and safety These five wellness indicators are incorporated into ANA’s Year of the Healthy Nurse topics to ensure RNs receive cohesive messaging and assistance on their journey toward their best health ever!
Visit www.nursingworld.org/2017-Year-of-HealthyNurse today for more information!
Reference:
Insight Consulting Group (ICG) & American Nurses Association (ANA), (2016). Health risk appraisal exploratory data analysis: November 30, 2016. (PowerPoint slides).
YeaR OF THe HeaLTHY NURSe CaLe NDaR
MONTH
January
February
March
April
May
June
July
August
September
October
November
December
• Worksite Wellness
• Cardiovascular Health
• Nutrition
• Combatting Stress
• Women’s Health
• National Fitness and Sports Month
• Men’s Health
• Cancer Awareness
• Skin Health
• Healthy Sleep
• Happiness
• Recovery
• Work-Life Balance
• Infection Control
• Immunizations
• Moral Resilience/Moral Distress
• Mental Health
• Wellness
• Healthy Eating/Healthy Holidays
SILVER SPRING, MD – The American Nurses Association (ANA) is steadfast in its commitment to improve the health of people across the country We look forward to sharing the valuable expertise of nurses with the new Administration and Congress
“As President Trump looks to improve America’s health care system we are ready to work with his administration to advance health care that is accessible, affordable, equitable, integrated and innovative,” said Pamela F Cipriano, PhD, RN, NEA-BC, FAAN, president of ANA
“This new Administration also has an opportunity to unite the country around a shared vision that puts protecting and promoting quality health care for all Americans above partisan politics,” said Cipriano “ANA



stands ready to offer support and assistance to make this opportunity a reality ”
In addition to the presidential race, many advocates of health care and nursing priorities were elected to the U.S. Congress. In total, 83 percent of the 52 candidates endorsed by ANA’s Political Action Committee (PAC) won their election and will serve in the 115th Congress Nurses are the largest single group of health care professionals, and the nursing profession has been voted as the most trusted profession for 15 years straight ANA will continue to leverage this trust to advocate for access to quality, affordable health care, optimal nurse staffing and other policies that remove barriers to health care for the broader community
For more information, visit NursingWorld org
From the American Nurse Today Journal
November 2016, Vol. 11 No. 11
Authors: Janet Haebler, MSN, RN, and Tim Casey
Nowhere in the nation are we immune to the ravages of the opioid epidemic The crisis has struck our cities, suburbs, and rural communities Across party lines, lawmakers at the state and federal levels are searching for solutions. Registered nurses (RNs) are uniquely positioned to help tackle this public health crisis, and ANA has been busy educating legislators about how As the most trusted direct-care providers on the frontlines of the epidemic, RNs help patients understand pain treatment options and play a key role in the prevention of opioid overuse and dependence ANA has sought to advance nursing’s role in fighting the opioid crisis by addressing barriers and expanding access to treatment, as described below
Expand access to medication-assisted treatment
Medication-assisted treatment (MAT), combined with counseling, serves as one of the most effective forms of treatment for opioid use disorders For millions of opioid addicts who are uninsured, homeless, or recently incarcerated, however, getting on – and staying on –medication is a struggle To improve access to treatment, ANA has advocated for MAT prescribing authority for nurses, as well as expanded private insurance coverage and Medicaid health benefits
Expand access to overdose reversal drug
Unfortunately, addiction to opioids, including heroin, is difficult to treat Not everyone recovers Among those


who do, most relapse at least once before sustained recovery With that in mind, ANA has advocated strongly for the expansion of naloxone access. Naloxone is a lifesaving medication that rapidly blocks the effects of opioids when signs and symptoms of a prescription opioid or heroin overdose first appear Some states have looked for ways to expand access to naloxone while protecting health professionals from criminal, civil, and professional liability (Good Samaritan Overdose Immunity Law).
Increase use of physician drug monitoring programs
Physician drug monitoring programs (PDMPs) are integral to reducing inappropriate prescribing and abuse of prescription medications PDMPs are staterun electronic databases that can provide a prescriber or pharmacist with information regarding a patient’s prescription history, thereby allowing them to identify patients who potentially are knowingly or unknowingly misusing medications ANA supports efforts to increase utilization of PDMPs The Department of Health and Human Services is working toward the goal of doubling the number of healthcare providers registered with their PDMP in the next 2 years.
ANA recognizes that we must also look beyond legislative and regulatory solutions to address the opioid epidemic As educators and patient advocates, nurses embrace a holistic approach to addressing pain, including nonopioid therapy alternatives, such as rehabilitative therapy, regional anesthetic interventions, surgery, psychological therapies, and complementary and alternative medicine

In 2017, the ANA Enterprise will launch the Healthy Nurse, Healthy NationTM Grand Challenge, a national movement designed to transform the health of the nation by improving the health of the nation’s 3.6 million registered nurses.
The Grand Challenge will:
• Broadly connect and engage individual nurses, employers of nurses, state nurses organizations, and specialty nurse associations to take action within five domains: physical activity, rest, nutrition, quality of life, and safety
• Provide a web platform to inspire action, cultivate friendly competition, provide content and resources to users, gather data and serve to connect registered nurses with each other, with employers and organizations
In a number of significant indicators, nurses are less healthy than the average American Nurses are likely to be overweight, have higher levels of stress, and get less than the recommended hours of sleep. Because health care delivery requires 24/7 support, the demands of shift work challenges the health of nurses In addition, hazards such as workplace violence and musculoskeletal injuries are contributing factors to poorer health. According to the Bureau of Labor Statistics, registered nurses have the fourth-highest rate of injuries and illnesses that result in days away from work when compared with all other occupations
As the largest group of health care workers, nurses are critical to America’s healthcare system Nurses protect, promote, and optimize the health of their patients by preventing illness and injury, facilitating healing, and alleviating suffering. Their well-being is fundamental to the health of our nation. Nurses should be viewed as exemplars of health, and serve as role models for their patients, colleagues, families, and communities
\’Grand ‘Chal·lenge\: bold, socially beneficial goals that successfully address a systemic and embedded problem through collaboration and joint leadership
The domains of Healthy Nurse, Healthy NationTM will include the areas of:

ANA believes nurses can lead culture change around pain management and opioid prescribing
To that end, we are working closely with the White House to promote and educate nurses on the new Centers for Disease Control and Prevention guidelines for opioid prescribing, which aim to improve clinical decision making and reduce inappropriate prescribing
Additionally, ANA continues to support innovative industry partners who are stepping up to promote valuable medication take-back programs, as well as those conducting research to improve abuse-deterrent formulas for prescription medications
In recent years, ANA and its state affiliates have advocated successfully for many of these changes—and more At the federal level, ANA argued strongly for MAT prescribing authority, increased access to the overdosereversal drug naloxone, and expanded treatment options for those living in areas most affected by the opioid crisis Passage of the Comprehensive Addiction and Recovery Act (CARA) in Congress this summer marked an important victory in the battle against substance abuse disorders
While CARA and the laws enacted in the states represent enormous progress in addressing this epidemic, we must now work to ensure the necessary funding is appropriated Only then will we truly begin to expand access to critical treatment services and turn the tide on this devastating public health crisis
For ANA resources on the opioid epidemic, visit • nursingworld org/MainMenuCategories/ WorkplaceSafety/Healthy-Work-Environment/ Opioid-Epidemic
• ( http://nursingworld.org/MainMenuCategories/ WorkplaceSafety/Healthy-Work-Environment/ Opioid-Epidemic)
Janet Haebler and Tim Casey are senior associate directors in Government Affairs at ANA.