

INF Holds Successful Holiday Gala & Fundraiser and Names the 2nd Annual Nurse of the Year
The Illinois Nurses Foundation (INF) held its annual Holiday Fundraising Gala on December 8th, 2018 at the Hilton in Lisle. It was a blissful evening for the Foundation and all those that came to celebrate. Multiple organizations and supporters of the foundation purchased entire tables for the event, which provided a wonderful way to spend time with friends and family during the holiday season while supporting a great cause. As always, the Holiday Gala provided its guests with the opportunity to do some Holiday shopping, with an abundance of baskets and gifts to choose from. Thanks to the overwhelming support of all the attendees, the Fundraising Gala thrived in raising funds for Illinois Nurses Foundation.
Guests socialized as they browsed through rows of raffle and silent auction items. Everyone in attendance also enjoyed a plated dinner and cash bar as holiday melodies played in the background.
Again this year, the Foundation held its “Honor a Nurse” campaign. The project was designed to Honor nurses who have inspired us; who have fought for the advancement of the profession; and who deserve recognition for their commitment to their patients and the work they do every day.
Nominations for the “Honor a Nurse” campaign were received throughout the year. The outpour of touching stories received were reviewed and narrowed down to five finalists, chosen by the Foundation Board members.

The five finalists were Christine Durbin, PhD, JD, RN, Jane Llewellyn, PhD, RN, NEA-BC, Jennifer M. Grenier, DNP, RN-BC, Donna Plonczynski, PhD, CNP and Mary Kelly, MBA, RN, CNRN, FAHA. The 2018 Nurse of the Year award was then presented to Mary Kelly. The story submitted to honor her read:

“Mary Kelly, BS, RN is a Certified Neuroscience Registered Nurse whose focus and passion is expert and timely care of the patient experiencing a stroke. Her background in nursing includes critical care and neuroscience nursing. Prior to studying nursing, she began a business career in accounting. She is currently a Disease Specific Care Reviewer for The Joint Commission. In that capacity she participates in and leads Comprehensive and Primary Stroke & Traumatic Brain Injury reviews of stroke centers across the nation. She has helped to develop reviewer tools and precepts new reviewers in this role.
Past positions have included the Director of Stroke Network Operations for a major health system in the Chicago area and Stroke Program Coordinator for a major suburban acute care hospital and trauma center. She applied her business and nursing backgrounds as a

Practice Manager to initiate, develop, and manage a suburban neurosurgical practice of MDs and an APRN where she was responsible for daily clinical and financial operations, interfaced with two hospital systems for clinical services, managed staff at three physical locations, communicated with law firms for litigation and expert witness services and achieved fiscal stability within six months of opening the practice. She has also been a critical care staff RN at suburban acute care trauma hospitals. Throughout her career trajectory she has developed expertise in TJC/CMS Standards, Organizational Development, Shared Governance, Quality Improvement, Fiscal Planning, and Critical Care. She is a member of the American Heart/Stroke Association and reviews abstracts for, attends and speaks at the International Stroke Conference. She is a member of the American Association of Neurological Nurses and served on the steering committee to develop INF Holiday Gala continued on page 3

MESSAGE FROM INF DIRECTO R
Alma J. Labunski, INF Director
Dear Colleagues:
New Year’s greetings to each one of you. On behalf of the Illinois Nurses Foundation (INF) Board of Directors, I thank you for your desire to keep apprised of goingson within our state of Illinois. This newsletter, which is mailed to all nurses in the state of Illinois, is especially designed for that purpose!
As you may well know, one of the hallmark’s of being a professional is continuing our growth and development for life. Moreover, the Foundation is a significant venue that assists in promoting our growth, service and the welfare of others. As one who has been involved since its inception in 2001, INF’s purpose remains clear: to collaborate with community partners in promoting the health of the public by supporting nurses through charitable research and educational initiatives. Dedicated to serving colleagues throughout the entire state of Illinois, the Foundation strives to accomplish this through philanthropic activities, such as providing scholarship funding to graduate and undergraduate students, funding scholarly initiatives that promote the health of people and develop the nursing profession, informing the public about health issues and nursing, and assisting in supporting nurses in need and/or crisis. Some examples which reflect its philanthropic dedication follow.
During 2018, numerous scholarships were available for undergraduate and graduate nursing students. The Foundation awarded a total of $16,968 in scholarships to deserving students. Also, numerous applications have been submitted for 2019, which has a return rate of March 15, 2019.
Additionally, the Foundation has striven to recognize our young professionals for their exceptional dynamic practice. Entitled, “40 Under 40” the commemoration was initiated four years ago. Selected by peers/colleagues, 40 emerging nurse leaders were honored September 13, 2018. The next commemoration is currently being planned to recognize accomplished nurse professionals. Leaders will be awarded on September 12, 2019. You will not want to miss this celebration, hence, mark your calendars NOW and check the VOICE for further details regarding the venue.
Furthermore, our Annual Holiday Gala and Fundraiser on December 8, 2018, held at the Hilton in Lisle, IL continued to promote our spirit of camaraderie, support, and service. The event was a delightful evening with dinner, opportunities to network, donate and serve the profession as well as prepare for holiday shopping via a silent auction. Although it was a festive celebration to honor all professionals, the “Nurse of the Year,” a relatively new initiative in its second year, was honored at the gala. In preparation, candidates were selected by professional nurse colleagues with a minimum donation of $25.00. Of all the nominees, five were most highly recommended, and of those five, one was selected by the INF Board to be honored. The forthcoming gala is already scheduled for December 7, 2019, at the Hilton Hotel in Lisle, IL. Do not forget to mark the special date on your calendar.
Moreover, although not widely known, INF provides opportunities to donate funds for colleagues who are in financial crisis, illness or encounter other personal tragedy. All contributions to the INF are deductible. For more information, donors may contact INF at 815-4688804 or check the website for further information.
Also, a beautiful unprecedented tribute honoring the life and legacy of Dr. Mary Lebold, who lived to serve so many of us throughout her professional life was presented at the gala. Dr. Lebold’s caring, compassionate, innovative research, as an educator and administrator were freely shared with all of us who served with her. Guests affirmed that we will always remember Dr. Lebold’s life as making an indelible impact and blessing to us and our profession.
Finally, dear Colleagues, as an active long-term member of our professional organization for over 62 years, I am thankful to be able to share these news items and continue serving you and our profession in this new year of 2019. I trust you will find these pages of NURSING VOICE enriching, stimulating and rewarding toward your future involvement in the initiatives of your profession.
Alma J. Labunski, Ph.D., M.S., R.N.; Director, former Vice-President IL Nurses Foundation; Editor Emeritus NURSING VOICE; ANA-IL Program Committee; INF Fund Raising Committee; Consultant, Educational Challenges Within a Global Culture; Retired Dean and Professor, North Park University, Chicago, IL





The Nursing Voice
INF Board of Directors
Officers
Cheryl Anema PhD, RN
Brandon Hauer MSN, RN
Cathy Neuman MSN, RN
Karen Egenes EdD, RN
Directors
Maria Connolly PhD, RN, CNE, FCCM, ANEF
Maureen Shekleton PhD, RN, DPNAP, FAAN
Alma Labunski PhD, MS, RN
Linda Olson PhD, RN, NEA-BC
Melissa Bogle DNP, APRN, FNP-BC, ACNP-BC
Linda Doling MSN, RN
ANA-Illinois Board Rep
Karen Egenes EdD, RN
Kathryn Serbin DNP, MS, RN
Bonnie Salvetti BSN, RN

ANA-Illinois Board of Directors
Officers
Dan Fraczkowski, MSN, RN-BC
Karen Egenes EdD, MSN, MA, RN
Pam Brown, PhD, RN, ANEF
Kathryn Serbin, DNP, MS, BSN, CCM
Directors
Lauren Martin, RN, CEN
Colleen Morley, MSN, RN, CMCN, ACM
Crystal Vasquez, DNP, MS, MBA, RN, NEA-BC
Kathryn Weigel, MS, RN, GCNS
Stephanie Yohannan, DNP, MBA, RN, NE-BC
Editorial Committee
Editor Emeritus
Alma Labunski, PhD, MS, RN
Chief Editors
Lisa Anderson-Shaw, DrPH, MA, MSN
Karen Mayville, MSN, PhD, RN
Members
Kathy Long-Martin, BSN, MSN, RN
Linda Olson, PhD, RN, NEA-BC
Lisa Hernandez, DNP, RN, CENP
Nancy Brent, RN, MS, JD
Executive Director
Susan Y. Swart, EdD, RN, CAE
ANA-Illinois/Illinois Nurses Foundation
Article Submission
• Subject to editing by the INF Executive Director & Editorial Committee
• Electronic submissions ONLY as an attachment (word document preferred)
• Email: kristy@sysconsultingsolutions.com
• Subject Line: Nursing Voice Submission: Name of the article
• Must include the name of the author and a title.
• INF reserves the right to pull or edit any article / news submission for space and availability and/or deadlines
• If requested, notification will be given to authors once the final draft of the Nursing Voice has been submitted.
• INF does not accept monetary payment for articles.
Article submissions, deadline information and all other inquiries regarding the Nursing Voice please email: kristy@sysconsultingsolutions.com
Article Submission Dates (submissions by end of the business day) January 15th, April 15th, July 15th, October 15th
Advertising: for advertising rates and information please contact
Arthur L. Davis Publishing Agency, Inc., 517 Washington Street, P.O. Box 216, Cedar Falls, Iowa 50613 (800-626-4081), sales@ aldpub.com. ANA-Illinois and the Arthur L. Davis Publishing Agency, Inc. reserve the right to reject any advertisement. Responsibility for errors in advertising is limited to corrections in the next issue or refund of price of advertisement.



Acceptance of advertising does not imply endorsement or approval by the ANA-Illinois and Illinois Nurses Foundation of products advertised, the advertisers, or the claims made. Rejection of an advertisement does not imply a product offered for advertising is without merit, or that the manufacturer lacks integrity, or that this association disapproves of the product or its use. ANA-Illinois and the Arthur L. Davis Publishing Agency, Inc. shall not be held liable for any consequences resulting from purchase or use of an advertiser’s product. Articles appearing in this publication express the opinions of the authors; they do not necessarily reflect views of the staff, board, or membership of ANA-Illinois or those of the national or local associations.

new Stroke Nurse Certification. She is a Founding Member of the Midwest Stroke Action Alliance & past facilitator of Midwest stroke coordinators and supporting networks.”
The INF strives to continue evolving and making this event a MUST ATTEND for all those in the nursing profession and its supporters. A very special thank-you to each of our major sponsors and our many donors, as well as the volunteers who worked to make this event a success. Thank you for all that you do to support Illinois Nurses Foundation!



Call for Article Submission
Submit your article or research for publication in the Illinois Nurses Foundation (INF) quarterly print publication. The Nursing Voice is mailed to all 195,000+ RNs in the state. The INF and ANA-Illinois welcomes submission of nursing and health related news items and original articles. We encourage short summaries and brief abstracts for research or scholarly contributions with an emphasis on application. To promote inclusion of submitted articles, please review the Article guidelines available on the INF website at www.ana-illinois.org/news-events/publications. An “article for reprint” may be considered if accompanied by written permission from the author and/or publisher as needed. Authors do not need to be ANA-Illinois members. Submission of articles constitutes agreement to allow changes made by editorial staff and publishers. See Article Guidelines for more information. Submit your articles to syswart@ana-illinois.org
ANA PRESIDENT'S ME S S AGE
Greetings,
The healthcare environment is rapidly changing, as new care technologies emerge, while state and federal policies and priorities fluctuate. Amidst never-ending change, public trust of nurses remains unwavering. At the end of 2018, the Gallup Organization released its annual ranking of the most trusted professions in America as determined by the public. For the 17th year in a row, nurses were at the top of the list. However, trust alone cannot advance the interests of our patients and the profession. We must transform our collective voices into action.

This year we have numerous opportunities to act. ANA partnered with the Health Information Management Systems Society (HIMSS), a health-IT non-profit association to host NursePitch at their annual conference in February. This startup competition was created to increase the voice and visibility of nurse-led and nurse developed innovation in the digital health ecosystem. Funding was provided to several projects.
I hope you can join us this year in Springfield, Illinois for advocacy in action as we lobby legislators on Tuesday, April 2nd, for Student Nurse Political Action Day, or Wednesday, April 3rd for Nurse Lobby Day, registration is available online.
It is also essential that we recognize nurses of all types, LPN’s, RN’s and APRN’s who are doing outstanding work to advance the profession in Illinois. Nominations for the annual Illinois Nurses Foundation 40 under 40 Emerging Nurse Leader Award will soon be underway. I encourage you to nominate a colleague who is under the age of 40, demonstrates exemplary professional practice and also makes an impact outside of the workplace. Visit www.illinoisnurses.foundation to learn more or nominate a nurse.
With spring fast approaching, our Healthy Nurse Healthy Nation Activities will resume, and our first event, the Shamrock Shuffle takes place in Downtown Chicago on Sunday, March 24th. There will a two mile walk, or 8k, and we hope you can participate with us at the event. Don’t forget to request to join our Healthy Nurse Healthy Nation Facebook page and watch your email for more upcoming events.
Finally, before you know it, Nurses Week will be here. The theme for 2019 is “4 Million Reasons to Celebrate,” recognizing the milestone numbers of nurses. If your organization is seeking a speaker, please reach out.
Thank you for all you do on behalf of our patients and the profession.
Dan Fraczkowski MSN, RN-BC
President – ANA-Illinois @NurseDanF



















Dan Fraczkowski MSN, RN
INF Holiday Gala

On March 22, 2019 the Illinois Organization for Associate Degree Nursing will be hosting Legal Hot Topics for Nursing Program Academic Administrators and Faculty at Heartland Community College.
This program is applicable to any faculty member or coordinator of a health career program.
Some presentation topics will include:
• An overview of higher education student due process rights
• Student discipline policy considerations and recommended procedures
• Legal considerations governing student use of social media
• Accommodating students with disabilities.
Presenter Emily P. Bothfeld, Attorney, Robbins Schwartz
Date: March 22, 2019
Time: 9am-3pm
Location: Heartland Community College, 1500 W Raab Rd., Normal, IL 61761
Cost: $90 IOADN member
$100 non-member
$110 at door
5 CE hours will be awarded.
To register please submit the following information along with a check payable to IOADN.
Name Address
Phone number
Email School
Send registration to: Kankakee Community College, Attention Kellee Hayes, 100 College Drive, Kankakee, IL 60901





Michael Almeida CRNA, President-Elect
IANA
2018 was a big year for the Illinois Association of Nurse Anesthetists and 2019 looks to be no different. 2019 will be the IANA’s 80th anniversary and we look to celebrate this at our Spring and Fall conferences which will be held in Champaign on May 18th and in Chicago at Northwestern Memorial Hospital September 14th-15th. Make sure to visit our website ILcrna.com for more details! The mission statement of the IANA is “Promote and support the profession of nurse anesthesia in Illinois through health policy advocacy, education and transformational leadership to advance patient safety and access to quality care.” The IANA’s priority is to focus on each one of these aspects of our mission statement. We start by promoting and supporting the profession through increasing grass roots effort while improving our social media presence. This year we began by forming a successfully ran public relations committee and completely revamping our website to provide everyone throughout the state easily accessible information about Nurse Anesthetists. In January we celebrate National Nurse Anesthetist week and have done so by placing billboards for the public to see our message. 2018’s billboard was in Springfield and this
year it is located near O’hare on interstate 294 for the months of January and February. The IANA’s annual lobby day in 2018 saw more than 80 CRNA’s and student nurse anesthetists attend. We look to continue to grow this number in 2019 and beyond. We celebrate with all other APRN specialties on the passing of the changes to the Nurse Practice Act, however, look to include Nurse Anesthetists in the list of APRN specialties to achieve full practice authority in Illinois. Access to care is another important aspect of our mission and for the people of Illinois, remains a top priority of ours. CRNA’s are the primary anesthesia provider in 89% of counties in Illinois and the only anesthesia provider in 29% of counties in Illinois. It is imperative that any legislation that looks to restrict the practice of ICRNAs not gain any traction as this would only harm the citizens of our state, particularly in the rural and critical access hospitals. The last part of our mission is to advance patient safety and focus on education. We are extremely proud that in Illinois we have five Nurse Anesthesia Programs throughout the state that continue to advance the field of anesthesia. Each one of these are now entry level Doctoral programs. Please visit our website for more information or contact us directly with any questions. On behalf of the IANA, I wish you and your loved ones a healthy and happy 2019!
THANK YOU TO OUR GENEROUS SPONSORS AND DONORS
Platinum Sponsor
Bronze Sponsors Table Sponsors



ANA-Illinois
St. Xavier University School of Nursing
Stepping Stones – Clint Verhagen Walter Schultz Insurance
Emmanuel Olaifa
Angela Gorazd Cheryl Anema ISAPN
SNAI UPDAT E
This year, the Student Nurses Association of Illinois (SNAI) is encouraging students to be more involved by going to high schools and colleges to talk more about what they are and how they can be involved. They have also started the ‘Pay It Forward’ movement. This movement is centered on inspiring positivity in others and encouraging them to brighten someone else’s day. To achieve this, individuals are presented a two-sided card with one side containing a positive message and request to pass the sentiment along and the other side providing a description of the movement (see image). SNAI would like to thank Muroo Hamed of Chamberlain University Addison for sharing her wonderful idea with her local Student Nurses Association and with SNAI. To broaden the impact of this movement, SNAI is planning themed monthly postings to demonstrate various other ways in which nursing students can “Pay It Forward.” If you or your organization would like to join the movement, be on the lookout for the upcoming SNAI video on how you can put the “Pay It Forward” movement into action in your community.

Everything happens for a reason, sometimes it just takes time to find yours.
Be the reason three people smile today.
An example of a pre-filled SNAI Pay It Forward (PIF) movement card. The cards will have empty spaces on the back where members can place a motivational phrase and a way people can pay it forward.
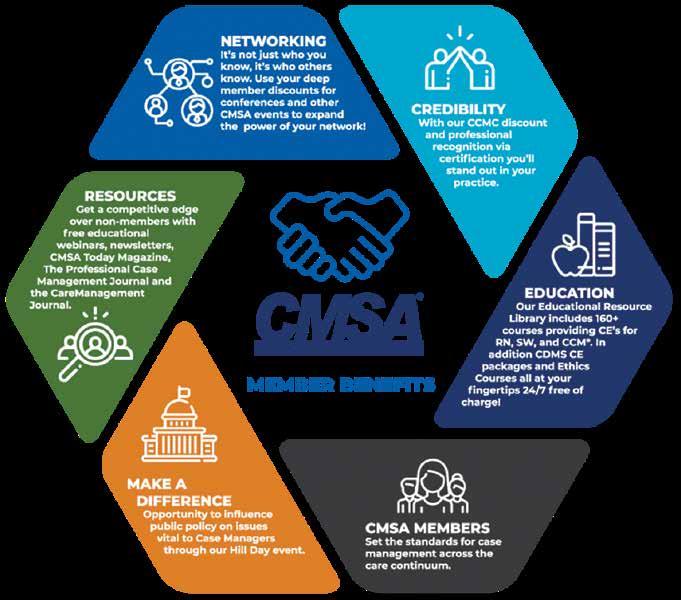
CMSA UPDATE
The Chicago chapter of the Case Management Society of America (CMSA Chicago) is excited to join ANA-IL as part of the consortium of nursing/ healthcare organizations working collaboratively to support our profession. CMSA is the leading, oldest, and largest membership association providing professional collaboration and education across the healthcare continuum. CMSA facilitates the growth and development of professional case managers across the full health care continuum, promoting high quality, ethical practice benefitting patients and their families.
We strive for improved health outcomes by providing evidence-based resources, impacting health care policy and sustaining the CMSA-developed Standards of Practice for Case Management.
CMSA Chicago’s largest event of the year is our local annul conference, It’s Not Luck, It’s Skill, which we will host at Drury Lane in Oak Brook on April 11, 2019 from 7:30a.m. – 5:00p.m. Come and earn seven CE’s for RNs and CCMs, and enjoy a day packed with networking, learning and fun. For more information visit our website: cmsa-chicago.org

LAW OFFICES OF JOSEPH J. BOGDAN, LLC
Providing legal and consultation services within the healthcare field for over 18 years.
PROVIDING LEGAL REPRESENTATION AND ASSISTANCE IN THE FOLLOWING AREAS
Illinois State Nursing Licensing and Regulatory Boards Drug Enforcement Administration (DEA) State Medicaid Agencies Centers for Medicare and Medicaid Services (CMS) Federal Drug Administration (FDA) Drafting Legal Opinion Letters Expert Witness Services Licensure and Provider Application Submission
THE LAW OFFICES OF JOSEPH J. BOGDAN, LLC 5950 E. LINCOLN AVE. SUITE 200 LISLE, IL 60532 jbodgdanlawoffice@gmail.com 630-310-1267 WWW.JJBLAWOFFICE.COM


The Illinois Nursing Workforce Center RN Workforce Report
What are the changes in the nursing workforce in Illinois? Are there nursing specialties that are more in demand than others? The Illinois Nursing Workforce Center (INWC) collected data with RN on-line license renewal that ended May 31, 2018. The report, executive summary, and talking points are available on the INWC website http://nusing.illinois.gov, tab: Data/Reports. In general, the 2018 survey results are similar to those collected during the 2016 RN on-line license renewal, trends and differences are highlighted in the report.
Data on the characteristics, supply and distribution of RNs in the State of Illinois is essential to maintaining access to health care and planning for the provision of essential primary care and other health services. This report contains data on the demographics of the current RN workforce, the relative numbers of RNs in each age group, their cultural diversity, educational preparation, and specialty practice area. Based on these findings, issues and concerns around the capacity, distribution and diversity of the nursing workforce are identified.
Aging workforce: The report presents important information about the aging of the RN workforce. In 2018, 52% of respondents are 55 years or older, which although only a 2% increase since 2016 is approximately 10% increase in this cohort of Illinois RNs since 2014. The

relatively rapid increase in RNs in older age categories has significant implications for workforce planning. Similar to 2016, approximately 27% of the respondents indicated intent to retire within the next five years. This combination of aging workforce and retirement plans indicate the potential of an impending nursing shortage within the next five years.
Diversity: Consistent with the increase in cultural and racial diversity in Illinois, data indicated a slight increase in the cultural diversity of the RN workforce in select groups of the younger cohorts. For those identifying as Hispanic/Latino, 32% are younger than age 36 years, while only 6% are over age 55 years. In the multiracial category, 27% are 35 years of age or younger, while 11% are over the age of 65 years. The increase in younger age cohorts did not hold true for all age groups, 9% of Black/ African American respondents reported being younger than 35 years, compared to the 17% in those over 65 years. White females with initial licensure in the U.S. constitute a substantial majority, approximately 80% of respondents.
Specialty foci: The respondents reported employment in these top five nursing specialties: acute care specialties, family focus, medical, surgical and community-health promotion. The data also
Online Resources – Print a copy of your license, update your address, and more
To print a copy of your license or store a copy on your smartphone or tablet, go to the Illinois Department of Financial and Professional Regulation website https:// idfpr.com/
The icon on the far left, “Get My License,” opens to a page with three options. Click on “Licensed Professionals”



(the middle option), an opportunity to print a free copy of your license. Licensees only need to provide their individual license number and either date of birth or last four digits of social security number.
For licensees interested in storing an electronic license pocket card on their smartphone or tablet, the link is at the bottom of this same page, “Electronic Pocket Card Overview.” Electronic pocket cards may be saved as a PDF file or by taking a screenshot and storing as a photo.
Please note that all IDFPR correspondence are now delivered electronically, including renewal reminders (in lieu of the paper postcard). Licensees are strongly encouraged to visit IDFPR’s online address change webpage (https://www.idfpr.com/applications/ LicenseReprint/ ) to provide a current email address and ensure contact information is up-to-date and accurate.
Change of name CANNOT be completed via this online process. If your name has changed, you must submit a written notice to the Department and include documentation of the name change (marriage license, court order, or divorce decree). For a copy of the written notice, please use this link https://www.idfpr.com/Forms/ DPR/DPRCOAnamechange.pdf
If you have questions, assistance is available Monday through Friday by contacting the IDFPR call center at: 1-800-560-6420; or by email at: FPR.PRFGROUP09@ illinois.gov

demonstrated the distribution of nurses in specialties by age cohorts, revealing significantly fewer younger nurses in specialties such as psychiatric mental-health, school, home health, gerontology, and community health nursing. These trends stand in contrast to the Illinois report, The Workforce Implications of New Health Care Models (2014), which forecasts a significant increase in ambulatory services, as well as a concomitant need for RNs to practice in community-based models of care. Past reports show that the Illinois nursing workforce shares many characteristics of our national picture: approximately 40% of nurses are 55+ years old and one third intend to retire in the next five to ten years. Collectively, the 2018 Illinois Registered Nurse (RN) workforce survey is a useful resource as health care planners project the human health care capital that will be needed in Illinois. The information will allow the Illinois Nursing Workforce Center (INWC) to address questions around the current RN supply, and if it will be adequate to meet the health care needs of Illinois citizens. Health care workforce planners should use these data to help determine what types of RN (e.g. specialty) will be in greatest demand, in what locales, as well as the types of specialties and skills that will be required in future models of care.

2019: A Promising Year for the Illinois Organization of Nurse Leaders
The Illinois Organization of Nurse Leaders has developed a strategic plan through 2020 that will help guide nurses in advancing leadership and education throughout the year. By offering programming that teaches specific skillsets crucial for success in the current world of Illinois healthcare, as well as providing timely discussions and policy statements regarding healthcare policy on the national level, IONL is consistently focused on the future of nursing.
New this year, IONL will be focusing its educational efforts on exciting tracks that will be held in conjunction with its Annual Conference, September 19-20 in Oak Brook, Illinois. These tracks include the Finance Workshop, Midwest Institute for Healthcare Leadership, and the Aspiring Nurse Leaders Workshop.
In addition to these in-person workshops, IONL is dedicated to enhancing education through the informative NC-3 live webinars that take place each month, free for IONL members and $40 for nonmembers. Our February 4 webinar, “Happiness – The Highest Form of Health” will teach the importance of personal well-being and its impact on productivity, engagement and performance. Need more CE credits? Take advantage of the new IONL Digital Library, a database of over 30 archived webinars, available as yearly subscriptions for individuals or organizations, providing CE from anywhere at any time.

In addition to in-person and remote educational opportunities, IONL is also committed to providing opportunities for nurses to build their networks with fellow healthcare leaders and find mentors and collaborators to work with. The IONL Fellowship Program connects nurses from throughout the State of Illinois with experienced educators to build leadership skills. Additionally, IONL’s regional events provide the perfect opportunity to connect with other local nurses in your area. Many members attribute their success to a connection they’ve made at one of IONL’s networking events, and you could be next!
For more information on these opportunities and IONL membership, visit www.ionl.org
Indian Nurses Association of Illinois’ Trifold Design served many - An activity update
The Indian Nurses Association of Illinois (INAI) mission is to serve as a professional body to identify and meet the professional, educational, cultural and social needs unique to nurses of Indian origin and heritage.
INAI professional development, community outreach, and charity initiatives served many people including the nurses in Illinois and the local and international community,” said Association’s President Beena Vallikalam. Beena and the team crafted a trifold activity design to effectively provide activities to benefit nurses and the community. The activities included professional specialty conferences, free and discounted rate continuing education sessions, workshops, career development opportunities, community outreach, interdisciplinary collaboration, mentoring programs, professional recognition, participation in medical missions, response to calamities, charity contributions, participation in legislative initiatives, encouraged membership in the Association, organized social events, encouraged community relations, and empowered nurses.
The professional development activities were also crafted in a trifold design- clinical, community and APRN tracks. Two APRN Pharmacology conferences, a Cardiology conference, a Physical Assessment Workshop, and informational seminars were the highlights of the professional track. Participants received a total of 25 CEs for these sessions. Nurses were recognized for their clinical excellence, leadership and advanced practice registered nurse roles. Their contributions during Nurses’ Day and APRN Week celebrations were also acknowledged.
INAI maintained its alliance with universities and CE providers for tuition discounts. Members also presented topics on regional and national platforms.
The Association’s commitment to the community was evidenced by outreach programs such as the Friends and Family CPR Series and health fairs. INAI conducted these series in four different venues. The series provided an opportunity to create an awareness of heart diseases and to teach CPR. The Health Fair served 150 people and included screening for vision, blood pressure, and diabetes, mini-presentations on GI disorders, stroke, diabetes, cardiac arrest, sleep apnea, breast examination, and advance directives.
During its 2017-2018 term, the INAI was recognized for its service to the community by the Government of Cook County.
INAI has reached out to the victims of natural calamities in United States and India and has participated in charity missions. As a member association of National Indian Nurses Association of America (NAINA), INAI participated in all educational and community outreach programs. INAI contributed toward the medical missions in India and Haiti through NAINA. INAI has also been significantly supportive to the cleft lip and palate repair and cataract treatment programs.
INAI has been working in close alignment with the American Nurses Association-Illinois (ANA-IL) and is a proud active partner of the ICNO (Illinois Coalition of Nursing Organizations). INAI continues to show its valuable presence in the community and among nurses of Indian origin and their professional peers. The Association welcomes all nurses to join its activities and urges them to become proud partners in fulfilling its multifaceted goals and actions.
Executive Board (2017-2018): Beena Vallikalam (President), Mary Xavier (Executive Vice President), Rani Kappen (Vice President), Sunina Chacko (Secretary), Lisy Peters (Treasurer), Dr.Simi Jesto Joseph (APRN track), Dr. Susan Mathew (clinical track).




Nurses want to provide quality care for their patients.
The Nurses Political Action Committee (Nurses- PAC) makes sure Springfield gives them the resources to do that.
Help the Nurses-PAC, help YOU!
So. . . . . . . if you think nurses need more visibility if you think nurses united can speak more effectively in the political arena if you think involvement in the political process is every citizen’s responsibility.
Become a Nurses-PAC contributor TODAY!
❑ I wish to make my contribution via personal check (Make check payable to Nurses-PAC).
❑ I wish to make a monthly contribution to NursesPAC via my checking account. By signing this form, I authorize the charge of the specified amount payable to Nurses-PAC be withdrawn from my account on or after the 15th of each month. (PLEASE INCLUDE A VOIDED CHECK WITH FORM)
❑ I wish to make my monthly Nurses-PAC contribution via credit card. By signing this form, I authorize the charge of the specified contribution to Nurses-PAC on or after the 15th of each month.
❑ I wish to make my annual lump sum Nurses-PAC contribution via a credit or debit card. By signing this form, I authorize ANA-Illinois to charge the specified contribution to Nurses-PAC via a ONE TIME credit/debit card charge.
❑ Mastercard ❑ VISA
Credit card number Expires CVV
Signature:
Date:
Printed Name: E-Mail:
Address:
City, State, Zip Code:
Preferred Phone Number:
Please mail completed form & check to:
ANA-Illinois
Atten: Nurses-PAC PO Box 636 Manteno, Illinois 60950


So what IS climate change?
At a recent nursing meeting that I attended I asked nurses to pair up and role play the following: “Your neighbor has just asked you - so what IS climate change?” Each nurse had to take a turn with a partner and answer that question, as though she/he were telling her neighbor the answer. After completing the role play, I asked how many of the nurses were able to answer that question with a high level of confidence and only about 10% raised their hands. When I ask how many could answer with reasonable confidence only another 10% raised their hands. How about you, would you feel confident answering the question? What everyone discovered from this activity was how unprepared many nurses are to talk about what climate change is. While nurses are more familiar with what climate change seems to be causing, such as more extreme weather events, sea level rise, and extensive wildfires, a large portion are unable to explain what climate change is in simple terms.
So here is a little primer:
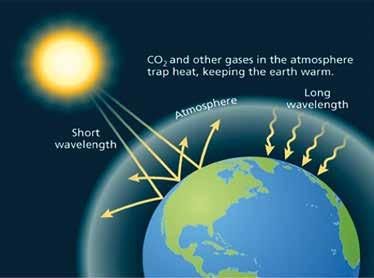
The earth’s temperature has historically been modulated by the sun’s rays beating down, warming the land and water, and then radiating heat back out beyond the earth’s atmosphere. This process has kept the earth at a livable temperature for humans and other lifeforms to flourish.

However, we now have a “blanket” of gases that are surrounding the earth, gases created substantially by human activities such as transportation, energy production, industry, cooking/heating, and agriculture. (See the image below) These gases are called greenhouse gases because they create the same warming effect as a greenhouse and are slowly warming the earth – both the land and particularly the oceans. And in the process, they are changing our climate. Climate is distinguished from weather in that weather is what occurs from day to day or week to week, but climate is what occurs over longer periods of time, month to month and year to year.
The process is a bit like what happens to your car when you leave it outside in the sun with the windows up. The sun’s rays heat the inside of the car and that heat cannot adequately escape, so the car heats up.
Just as there is a small range of body temperatures at which humans can be healthy, the same is true for all species on earth. When human temperatures rise from 98.6 to 100.4 degrees it means the difference from feeling fine to having a fever and not feeling well. When our temperatures get even higher we begin to see bodily system distress and damage. What happens when the earth has a fever?
As the earth warms, we are beginning to see shifts in climate which are resulting in some areas seeing much more rain and others much less, some colder
winters, some hotter summers.

As we encounter more extreme heat days and extended heat waves, we are going to see many more heat-related illnesses and even deaths in humans. People who work outside in agriculture, utilities, construction, gas/oil, and many other fields will be at higher risk for hyperthermia. And, of course, extreme storms and wildfires have been taking an enormous toll on human and ecological health.
Changes to the earth’s climate can have irreversible effects on plants, including our agricultural food crops. Rising ocean temperatures is affecting plankton which is the foundation of the food chain for fish and sea mammals. An estimated billion people are dependent on fish as their main source of protein. In addition to interrupting the world’s food supply, there are a great many other health threats that are associated with the changes we are seeing. For an extensive list of how climate change affects human health, visit https://bit.ly/2qNLNtW
While there are some natural sources of greenhouse gases, the ones that we have the most capacity to reduce are those that are manmade. As individuals we can assess our household’s contribution to greenhouse gases by using a “carbon footprint calculator,” such as this one from the U.S. Environmental Protection Agency: https://bit. ly/1XIc9pa. As nurses, we can help promote climate healthy purchasing and practices in our health care facilities, K – 12 schools, faith-based organizations, universities, and any other settings in which we have influence.
The new International Council of Nurses (which ANA is a member of) announced its new position statement on climate change in September 2018 and calls on all nurses to help address climate change (see: https://www.icn.ch/sites/default/files/inline-files/PS_E_ Nurses_climate%20change_health.pdf). It calls for us to heed the scientific evidence which, in the case of climate change, is abundant. We must be able to talk about this issue with a degree of confidence and we must engage both individually and as a profession to advocate for policies and practices that will decrease greenhouse gas production from a wide range of its sources. The truth is climate change is a health issue and that’s what we nurses are all about.

For more resources on climate change and health, including nurse-focused guides and webinars, visit the Alliance of Nurses for Healthy Environments Climate and Health Toolkit: climateandhealthtoolkit.org. To join our free monthly calls on Climate Change and Nursing please email the authors.
Authors: Barbara Sattler, RN, DrPH, FAAN, Professor, University of San Francisco, bsattler@usfca.edu and Cara Cook, MS, RN, AHN-BC, Climate Change Program Coordinator, Alliance of Nurses for Healthy Environments, cara@enviRN.org




ANA-Illinois Expert Panel Workplace Safety Survey 5: Staffing
Pamela Brown, Ph.D., RN, ANEF
First, I want to thank all of you who responded to Survey 5: Staffing. The response was very gratifying and made the results more powerful. I also invite you to send your staffing related stories to ANA-Illinois, as stories deliver a greater impact than numbers. Over 700 nurses responded to Survey 5, with 75% of respondents indicating they provide direct patient care, and 80% indicating they have access to continuing education offerings, specific to patient care, provided by their employer. This group is predominantly female (91%), between 26-39 years of age 49%). Most live (54%) and work (46%) in urban and suburban areas, earn over $50,000 (83%) annually, and have a BSN or higher degree (77%). The majority work 12-hour shifts (66%) on days (55%). Most (56%) work on Medical-Surgical and higher acuity Medical-Surgical units.
Only 27% of respondents reported working in a facility that has a Staffing Committee, and only 18% report that the staffing plan is being used on their unit. Most (73%) report that they are not sure (37%) or they do not have (36%) a Staffing Committee, and predominantly (81%) report that the staffing plan is not used (36%) or they are not sure (45%) if their unit uses the staffing plan.
Respondents reported being responsible for an average of 10 patients per shift, with an average of four additional admissions, transfers, and/or discharges. Other added responsibilities included: being charge nurse or team leader (25%), preceptor/teacher (16%), part of the code or rapid response team (10%) and providing consults or procedures (5%) for other nurses. Most (75%) work through their break time and most (63%) work overtime. The majority (55%) report their workload as higher than they are comfortable with.
Respondents predominantly (79%) report having discussions about staffing at least weekly (78%) with 25% having discussions daily. Over the past month this group reported experiencing “dangerous” staffing levels 33% of the time. When asked if it was safe to report staffing concerns, almost 70% reported feeling safe (69%) to report concerns and 31% feeling unsafe. The majority (57%) reports they have enough qualified staff to handle the number of assigned patients, with 40% indicating they
do not have enough qualified staff. Over 60% of nurses feel they rarely (46%) or never (18%) feel unqualified to care for patients with specialized equipment or certain conditions. Solutions during short staffing include nurses taking a heavier load (85%), use of float nurses (55%), nurses volunteering for overtime (51%), managers/ supervisors fill in (25%), pulling in agency nurses (20%), and altering routine (19%) care.
Conclusions
1. It is past time to listen carefully to bedside nurses about staffing issues and include them in developing solutions.
2. Illinois has legislation in place that requires staffing committees to create staffing plans based on patient acuity. These committees are mandated to include bedside nurses. According to over 70% of bedside nurses, the plans are not in existence or are not being used.
3. Bedside nurses report working in “dangerous” staffing levels over 30% of the time.
4. Bedside nurses (63%) consistently work overtime and work through their break times (75%).
5. Bedside nurses (55%) report that their workload is consistently higher than they are comfortable with.
Recommendations
1. Share results of this survey to raise awareness of this issue.
2. Collaborate with IONL to plan staffing summits throughout Illinois.
3. Assess legislation from other states and ANA policies for ways to increase accountability of agencies.
4. Further explore how bedside nurses cope with low staffing issues, and what are the ramifications of work-arounds, or short cuts.
5. Further explore the relationship between staffing and retention.
6. Further explore the ratio of novice nurses to experienced nurses on units, and how that affects staffing and retention.

Alpha Eta Chapter of Chi Eta Phi Sorority Awards Nursing Scholarships

Chi Eta Phi Sorority, Incorporated, is an international sorority of professional nurses and nursing students. The nursing sorority was established in Washington DC at Freedman’s Hospital in 1932 and has a membership of more than 4,000 nurses. There are 90 Graduate Chapters and 40 Undergraduate Chapters in the United States including the Virgin Islands. Chi Eta Phi Sorority is a recognized leader in “Developing Healthy Communities through Advocacy, Collaboration, Education, Leadership, Research and Service.”
On March 31, 2018, Alpha Eta Chapter, Incorporated, of the Chicago Chapter of Chi Eta Phi Sorority, Incorporated, hosted its 30th Annual Robert Reid Scholarship Fundraiser Luncheon at the Hilton Oak Lawn in Oak Lawn, IL. The luncheon is named in honor of Mr. Robert Reid who was the first black male nurse to join Alpha Eta Chapter, Incorporated and Chi Eta Phi Sorority, Incorporated. Charted in May 1980, Alpha Eta Chapter, Incorporated, has given over $75,000.00 in scholarships in the last 30 years to nursing students enrolled in AAS, BSN and MSN nursing programs. To purchase tickets for the March 31, 2019 luncheon and to learn more about Alpha Eta Chapter, Incorporated, visit our website at alphaeta-chietaphi.org
Thank you for our 2018 Donors
Catherine Neuman
Nancy Spector
Alma Labunski
Maureen Shekleton
TIAA Charitable
Linda Olson Stepping Stone Financial, Inc
Joanne Buckley
Karen Egenes
Cheryl Anema
Margaret Miller
P. Joan Larsen
Dan Fraczkowski
Jim Plonczynski
Nicole Wynn
Maureen Murphy
Donna Plonczynski
Trish Hatten
Carol Anaski-Figurski
Maria Connolly
Gayle Peterson
Walter W. Shultz Agency Inc.
Donna Plonczynski
Jennifer M. Grenier
Gloria Simon
Mildred Taylor
Mary Lebold
Lauren Martin
Christine R. Durbin
Mary M. Lebold
Linda Roberts
Josh Wajtkowski
Dr. Patrick Durbin
Kevin & Mary Kelly
Terri Robinson
Mary Eileen Kloster
Emmanuel Olaifa
Smits Funeral Homes, Ltd
Bonnie Salvetti
Woundcare on Wheels, Inc
Dorothy Stratman Lucey
From July 7-13, 2019, Alpha Eta Chapter, Incorporated along with the chapters from Waukegan, Illinois, Nu Phi Chapter, Incorporated, and from Milwaukee, Wisconsin, Theta Chi Chi Chapter, Incorporated, will be supporting Chi Eta Phi Sorority, Incorporated’s biennial national educational conference. The Conference will be held at the Westin in Lombard, Illinois. For additional information regarding registration, vendor opportunities and sponsorship, visit the national website at www. chietaphi.com

To access electronic copies of the Illinois Nursing Voice, please visit

Toni L. Oats, BSN, RN, President
Self-Advocacy Skills for Nurses: Dealing with Incivility, Bullying and Workplace Violence Part I
Ann O’Sullivan, MSN, RN, CNE, NE-BC, ANEF
Karen Kelly, EdD, RN, NEA-BC
Objectives:
Determine causes and effects of verbal violence and bullying.
Demonstrate strategies to respond to verbal violence. Identify resources to use in the workplace to reduce verbal violence.
This continuing education article is the first in a two-part series on Dealing with Incivility, Bullying and Workplace Violence. Part 1 discusses the definition, causes, prevalence, costs and effects of incivility, bullying and workplace violence. Part 2 will be published in the July edition of The Voice and will discuss strategies and resources to respond and reduce workplace violence.
Advocacy
The American Nurses Association (ANA) declared 2018 The Year of Advocacy. Advocacy is defined as the act or process of pleading for, supporting, or recommending a cause or course of action. Advocacy may be for persons or for an issue. (ANA, 2015). Every day, in countless large and small ways, nurses make the world a better place. These moments of everyday advocacy we change the lives of vulnerable people and improve conditions for those around us. Nurses inspire, innovate, and influence at the bedside and beyond.
CE Offering
1.0 Contact Hours
This offering expires in 2 years: February 25, 2021
Learner Outcome:
80% of those reading the article and completing the post-test, the nurse will be able to describe the causes and effects of workplace violence, use effective strategies to respond to workplace violence and identify one or more resources to use to reduce violence in the workplace.
HOW TO EARN
CONTINUING EDUCATION CREDIT
This course is 1.0 Contact Hours
1. Read the Continuing Education Article 2. Go to https://www.surveymonkey.com/r/22192 to complete the test and evaluation. This link is also available on the INF website www.illinoisnurses. foundation under programs.
3. Submit payment online.
4. After the test is graded, the CE certificate will be emailed to you.
HARD COPY TEST MAY BE DOWNLOADED via the INF website www.illinoisnurses.foundation under programs
DEADLINE
TEST AND EVALUATION MUST BE COMPLETED BY February 25, 2021
Complete online payment of processing fee as follows:
ANA-Illinois members- $8.00 Nonmembers- $15.00
ACHIEVEMENT
To earn 1.0 contact hours of continuing education, you must achieve a score of 80%
If you do not pass the test, you may take it again at no additional charge
Certificates indicating successful completion of this offering will be emailed to you.
The planners and faculty have declared no conflict of interest.
ACCREDITATION
This continuing nursing education activity was approved by the Ohio Nurses Association, an accredited approver by the American Nurses Credentialing Center’s Commission on Accreditation. (OBN-001-91)
CE quiz, evaluation, and payment are available online at https://www.surveymonkey.com/r/22192 or via the INF website www.illinoisnurses.foundation under programs.
Nurses must also advocate for themselves.
How do we improve our work life?
How do we advocate for our self to stop bullying and workplace violence?
How do we empower ourselves?
We must start with advocating for ourselves before we can fully influence the direction of the profession and healthcare.
Many Names…Same Issue
The issues of bullying and workplace violence have many names: behaviors undermining a culture of safety; workplace conflict; lateral/horizontal violence; workplace abuse; bullying; mobbing; incivility; disruptive behavior; nurses eat their young; hazing, and more. No matter what we name this behavior — it creates a work environment that a reasonable person would find intimidating, threatening, violent or abusive and it affects a person’s psychological or physical wellbeing.
Definitions
Bullying can be defined as intentional, repetitive, intimidating behavior or repeated unwanted psychological, physical, or sexual abuse, or harassment. Incivility comprises a wide range of behavior others experience as disrespectful, thoughtless, or rude. Horizontal or lateral violence is described as nurse-tonurse abuse or aggression. No matter what term is used the similarity is that another person physically, verbally, or emotionally abuses another person.
The American Medical Association (2002) defines bullying as “personal conduct, whether verbal or physical, that affects or potentially may affect patient care negatively constitutes disruptive behavior.”
The National Institute for Occupational Safety and Health (NIOSH) defines workplace violence as “violent acts, including physical assaults and threats of assaults, directed at persons at work or on duty.” (OHSA, 2015)
Bullying includes verbal violence—threats, verbal abuse, hostility and harassment, which can cause significant psychological trauma and stress, even if no physical injury takes place. Verbal assaults can also escalate to physical violence.
Prevalence of Bullying
Numerous studies over the years have reported on the incidence of bullying among and of nurses in the workplace.
o 2013—30% of nurses in hospitals feel bullied (Papa & Venella, 2013)
o 2008—80% surveyed experienced violence in the workplace; 52% from colleagues (Hader, 2008)
o 2004—89% surveyed experienced verbal aggression, 61% was nurse to nurse violence (Dean, 2005)
o 65% reported experiencing lateral violence (Stanley, 2007)
o 2007—86% experienced “mobbing” and its outcomes (Yildirim, 2007)
More recently, Maxfield (2014) surveyed 2283 corporate employees and found that 96% of people have experienced workplace physical or emotional bullying/ violence. This author included instances of verbal violence including — emotional or controlling behavior (79% reported); sarcastic, cutting, disrespect (74%); silent treatment, cold shoulder, excluding (68%–very common in health care); gossip, rumors (64%); sabotage, undermining (52%); and physical assaults (11%). It is interesting to note that most bullying reports are in the form of verbal violence.
An ANA Study in 2015 surveyed 4118 nurses of which 42% were staff nurses, 16% were nurse managers, and 20% were nurse educators. Respondents reported that patients, families, and patients’ friends were most prone to committing a violent act. RNs, patients’ families, doctors, administrators, and managers were most likely to exhibit incivility. The most prevalent type of violence was worker on worker (52%) and patient on worker (45%). When asked if they positively intervene when they witness bullying/uncivil behaviors, 38% reported always, 59% reported sometimes, and 3% reported never.
The ANA-Illinois Expert Panel on Workplace Safety surveyed nurses in 2018 to determine what their experience of incivility and bullying behaviors was. Over 300 surveys were returned with the following results:
The following behaviors occurred one to three times in the past month:
• Leaders speaking or acting disrespectfully to them;
• Being the brunt of rude treatment from a peer;
• Being the brunt of rude treatment by a leader;
• Being the brunt of sarcastic remarks form a leader;
• Being yelled at by a peer;
• Being the brunt of sarcastic remarks from a physician;
• Being the brunt of sarcastic remarks from a peer;
• Being humiliated by a leader;
• Being humiliated by a peer;
• Being humiliated by a physician;
• Being yelled at by a leader.
In OSHA in 2015 reported that workplace violence is widespread and vastly underreported in healthcare professions. Surveys highlight the prevalence of workplace violence among healthcare occupations.
• 12 percent of emergency department nurses experienced physical violence—and 59 percent experienced verbal abuse—during a seven-day period (2009–2011 Emergency Nurses Association survey of 7,169 nurses).
• 13 percent of employees in Veterans Health Administration hospitals reported being assaulted in a year (2002 survey of 72,349 workers at 142 facilities).
• The numbers often only include incidents that led to time away from work. While some data are available for other violent incidents, surveys show that many incidents go unreported, even at facilities with formal incident reporting systems.
• A survey of 4,738 Minnesota nurses found that only 69 percent of physical assaults and 71 percent of non-physical assaults were reported to a manager.
• Another medical center found that half of verbal and physical assaults by patients against nurses were never reported in writing.
• Bullying and other forms of verbal abuse are particularly prone to underreporting. Reasons for underreporting include lack of a reporting policy, lack of faith in the reporting system, and fear of retaliation.
Costs of Disruptive Behavior
The costs of bullying and disruptive behavior have been widely reported in the literature: decreased retention/recruitment; increased turnover; decreased nurse satisfaction/morale; decreased knowledge, learning, creativity, quality; decreased patient satisfaction; and nurses leaving the profession. Joint Commission (2008) reported the effects of disruptive behavior as stress, a culture of fear, disengagement, lost productivity, absenteeism, psychological and physical harm, undermined culture of patient safety which fosters medical errors and plays a role in preventable adverse outcomes, increased cost of care, and the loss of qualified clinicians, administrators and managers to more professional work environments. All these factors have widespread effects on patient care and nurses’ morale.
Maxfield (2014) reported that 80% of those surveyed say that this bullying affects five or more people other than themselves; 20% report that dealing with the bullying takes seven plus hours/week with a projected $8,800 a year lost productivity.
OSHA (2015) states that workplace violence is costly.
• If an employee requires medical treatment or misses work because of a workplace injury, workers’ compensation insurance will typically have to pay the cost.
• One hospital system had 30 nurses who required treatment for violent injuries in a particular year, at a total cost of $94,156 ($78,924 for treatment and $15,232 for lost wages).
• If your organization self-insures, it will bear the full cost. If your organization does not, its claim experience can still affect insurance premiums.
• Caregiver fatigue, injury, and stress are tied to a higher risk of medication errors and patient infections.
• Studies have found higher patient satisfaction levels in hospitals where fewer nurses are dissatisfied or burned out.
• Injuries and stress are common factors that drive some caregivers to leave the profession. The estimated cost of replacing a nurse is $27,000 to $103,000. (OSHA, 2015)
Why Disruptive Behavior Still Occurs??
With all this evidence about the prevalence and cost of disruptive behavior, you may ask yourself—Why does this disruptive behavior still occur? Reasons cited in the literature (as noted by Joint Commission, 2008) are:
• Fear of retaliation;
• Stigma of blowing the whistle;
• History of it being ignored or excused as “acceptable;"
• Nurses feel helpless/victims;
• “No one really cares;"
• Tolerance contributes to escalating problem;
• Silence is permission—if you observe it & don’t speak up—that’s permission;
• Inexperienced nurses more likely to report;
• Experienced nurses more likely to perceive policies and procedures are ineffective;
• Nurses lack interpersonal, coping or conflict management skills;
• Stress: poor staffing levels, long hours;
• Pressures of healthcare environment.
Bullying persists because bullies are not being held accountable, people say nothing, stay away from them, avoid working with them, and vent to others (Maxfield, 2014). Nurses report they don’t speak up about the bullying because they don’t know how, fear of retaliation, and/or it takes too much time and energy with very little change in the bullying behavior.
Three Forms of Bullying
Maxfield (2014) discusses three forms of bullying:
• A personal attack which includes isolation, intimidation, and degradation;
• Erosion of professional competence and reputation, which damages professional identity and can affect career options; and
• Attacks through work orders or tasks, which includes obstructing work or denying due process.

Some examples of bullying include:
• Being accused of errors made by someone else;
• Nonverbal intimidation;
• Being belittled;
• Being gossiped about;
• Feeling ignored;
• Excluded from activities or conversations;
• Being humiliated in front of others;
• Being assigned undesirable work;
• Unwarranted or invalid criticism or blame;
• Exclusion or social isolation;
• Unreasonable demands;
• Denied advancement opportunities.
Remember, sometimes the more passive behaviors can be the most damaging and the most pervasive!
Factors contributing to increased bullying
In the complex, busy, understaffed organizations of today several factors have been suggested which contribute to increased bullying:
• Significant organizational change (restructuring, technology, finances, ACA);
• Worker characteristics (e.g., age, gender, parental status, new staff);
• Workplace relationships (poor information flow, lack of employee participation in decision-making);
• Work systems (e.g., lack of policies about behavior, high rate and intensity of work, staff shortages, interpersonal conflict, role ambiguity) (Maxfield. 2014).
Professional Standards of Behavior
ANA establishes standards for nurses in ethics, communication, leadership and collaboration which
provide direction about a nurse’s responsibilities in dealing with workplace bullying and incivility (ANA, 2015).
The registered nurse practices ethically:
• Takes appropriate action regarding instances of illegal, unethical, or inappropriate behavior that can endanger or jeopardize the best interests of the healthcare consumer or situation.
• Speaks up when appropriate to question healthcare practice when necessary for safety and quality improvement.
The registered nurse communicated effectively in all areas of practice:
• Assesses own communication skills in encounters with healthcare consumers, families and colleagues.
• Seeks continuous improvement of own communication and conflict resolution skills.
The registered nurse leads within the professional practice setting and within the profession:
• Treats colleagues with respect, trust and dignity.
• Develops communication and conflict resolution skills.
• Participates in professional organizations.
• Communicates effectively with the healthcare consumer and colleagues.
The registered nurse collaborates with the healthcare consumer and other key stakeholders in the conduct of nursing practice:
• Adheres to standards and applicable codes of conduct that govern behavior among peers and colleagues to create a work environment promoting cooperation, respect, and trust.
Nurse leaders have specific responsibilities in preventing and dealing with workplace bullying and incivility as outlined in the Nursing Administration Scope and Standards of Practice (ANA, 2015):
• Develop healthy work environments using evidence-based management practices.
• Create healthy work environments that are safe, empowering and satisfying.
• Promote ongoing evaluation and improvement or personal and team communication and conflict resolution skills.
• Evaluate effectiveness, consistency and fairness in interpersonal interactions and communication
• Create an environment that stimulates positive innovation and change.
• Support a work environment that promotes cooperation, respect and trust.
The ANA Code of Ethics (2015) provides further direction for nurses regarding bullying:
• Provision 6: The nurse establishes, maintains, and improves the ethical environment of the work setting and conditions of employment that are conducive to safe, quality health care.
o 6.2: Nurses are responsible for contributing to an environment that demands respectful interactions among colleagues, mutual peer support, and open identification of difficult issues.
o 6.2: Nurse executives have a particular responsibility to assure that employees are treated fairly and justly. Unsafe or inappropriate activities or practices must not be condoned or allowed to persist.
Summary
In summary, I quote from the American Nurses Association position statement on Incivility, Bullying, and Workplace Violence states that “all registered nurses and employers in all settings, including practice, academia, and research must collaborate to create a culture of respect, free of incivility, bullying, and workplace violence.” In other words, violence should never be an accepted part of practice. Stay tuned for Part 2 of this series to learn more about strategies and resources to deal with and prevent workplace violence.
779-529-2012















BJC is one of the largest nonprofit health care organizations in the nation, with 15 hospitals and multiple community health locations across the greater St. Louis, southern Illinois and mid-Missouri regions.


Based in St. Louis and with more than 30,000 team members, we are one of Missouri’s largest employers. Join our award-winning team, which includes hospitals with Magnet® status and recognition of excellence by U.S. News & World Report


8. Memorial Hospital East
9. Missouri Baptist Medical Center *
10. Missouri Baptist Sullivan Hospital
11. Northwest HealthCare
12. Parkland Health CenterBonne Terre
13. Parkland Health CenterFarmington
14. Progress West Hospital
15. St. Louis Children’s Hospital * * Magnet Hospitals










